Abstract
Objective: This study aimed to test the feasibility and efficacy of a self-guided online cognitive behaviour therapy (iCBT) for university students in Hong Kong during COVID-19. Method: One group pre-post-test design with convenient sampling was adopted in this study, involving 84 university students who received a newly developed iCBT within an 8 week intervention period. The iCBT offered eight online modules for students to learn the skills of CBT at home through an online platform which was accessible any time anywhere anonymously with technical support only. Standardized assessment tools were used for outcomes assessment at the pre- and post-intervention periods. Results: Three quarters of participants completed all iCBT modules. The results of paired t-tests showed that, after completing the iCBT, participants showed reduction in anxiety, depression, and perceived stress. Conclusion: This study provides preliminary evidences to support the feasibility and efficacy of the self-guided iCBT for university students during COVID-19.
Keywords: anxiety, depression, online cognitive behavioral therapy, COVID-19 outbreak, feasibility of self-guided online cognitive behavioral therapy for university students during COVID-19
The first confirmed case of COVID-19 in Hong Kong was identified on Jan 23, 2020, which induced a high level of anxiety and depression among university students and general population (Choi, Hui, & Wan, 2020; Hou et al., 2021). In fact, mental health problems are highly prevalent among college students, which has become an alarming issue. According to a recent large-scale international study conducted by the World Health Organization (Auerbach et al., 2016), one-fifth (20.3%) of college students suffer from a mental disorder, with anxiety disorder being the most common (11.7%), followed by depressive disorder (4.5%) and substance use disorder (4.5%). The high prevalence of mental disorders among college students is due to the various kinds of stress such as the transition to adulthood, academic stress, financial problems, and poor social relationships (Hunt & Eisenberg, 2010). Local college students in Hong Kong have suffered higher levels of stress compared to most other societies (Lun et al., 2018; Ng, Chiu, & Fong, 2016). Moreover, due to the stigmatization of mental illness by traditional Chinese culture, college students with anxiety disorder are perceived as having a mental illness due to their own weaknesses, and failing to comply with the basic duties advocated by Confucianism, and subsequently they experience “shame,” “devaluation,” and “loss of face” (Young & Ng, 2016), which, in turn, has an adverse effect on their mental health (Boyd, Adler, Otilingam & Peters, 2014). Thus, it is not surprising to find that recent surveys reported a relatively high prevalence of mental disorders among Hong Kong college students, with anxiety disorder ranging from 20.0% (Lun et al., 2018) to 29.1% (Cheung, Tam, Tsang, Zhang, & Lit, 2020), and depressive disorder ranging from 9.0% (Lun et al., 2018) to 11.9% (Cheung et al., 2020). In fact, the outbreak of COVID-19 have induced a higher prevalence of anxiety and depression among all Hong Kong people, including university students (Ahmed et al., 2020; Choi et al., 2020; Hou et al., 2021), and that the prevalence of anxiety and depression of university students are higher than those of general population during COVID-19 outbreak (Wang & Zhao, 2020). It is evident that anxiety and depressive disorders negatively influence the lives of college students and are associated with lower academic performance, less satisfaction with friendships, lower self-confidence, pessimism towards the future, and poor sleep (Lun et al., 2018). Thus, it is important to develop therapeutic interventions that promote mental health recovery for college students.
A variety of different treatments, including psychiatric drug and various psychological treatments, have been developed to effectively treat anxiety and depressive symptoms. In particular, cognitive behavioral therapy (CBT) has been widely used to help people to deal with anxiety and depression through various kinds of strategies such as changing thinking patterns (Beck, 2011). A recent meta-analysis suggests that CBT is an effective psychological intervention for Chinese participants with various mental disorders including anxiety and depression in both short-term and long-term effects (Ng & Wong, 2018).
However, the majority (>75%) of those with anxiety and/or depressive disorder are resistant to traditional face-to-face counseling services and have not received any assessment or counseling services (Auerbach et al., 2016; Hunt & Eisenberg, 2010; Lam et al., 2015), which is detrimental to their mental health. Barriers to traditional face-to-face counseling services include stigmatization and local social-distancing precautionary measures during COVID-19 outbreak. It is vital to overcome these treatment barriers so that college students can receive early assessment and treatment to facilitate their mental health recovery as soon as possible.
Self-Guided Online Cognitive Behavioral Therapy
Recently, a self-guided internet-delivered Cognitive Behavioural Therapy (iCBT) program has been developed so that cognitive behavioral therapy can be delivered through the Internet (Beevers et al., 2017). Different from the traditional face-to-face CBT, the self-guided iCBT provides participants for learning the rationales and skills of CBT through self-learning online modules without the need for counselor support (Gratzer & Khalid-Khan, 2016; Johansson & Andersson, 2012). The self-guided iCBT is found to overcome the above barriers from traditional face-to-face psychological treatment with the following advantages: available for 24 hours a day and 7 days a week, accessible at any time anywhere, anonymous, structured, and self-learned (Ebert et al., 2015). A series of studies have demonstrated the treatment effectiveness of self-guided iCBT on reducing anxiety and depressive symptoms, often comparable to face-to-face treatment (Carlbring, Andersson, Cuijpers, Riper, & Hedman-Lagerlöf, 2018).
However, this type of effective self-guided internet-delivered CBT is not available in Hong Kong. In light of this service deficiency, this project therefore aimed to develop a self-guided iCBT model for university students in Hong Kong. Moreover, as existing models of iCBT are based on Western culture and societies, the contents of the iCBT for Hong Kong need to be indigenized in nature and adapted to the local context in order to meet the needs of the local university students with anxiety and depressive symptoms.
A Self-Guided iCBT in Hong Kong
In Hong Kong, a new online platform of a self-guided iCBT was developed on January 01, 2019 (please see https://icbthk.com) to facilitate the mental health recovery for university students during COVID-19 outbreak. The self-guided iCBT aimed to overcome the above barriers from traditional face-to-face psychological treatment by offering flexible learning opportunities for the participants to read and learn the techniques and skills of CBT through an online platform that was accessible at any time anywhere anonymously, short-term, structured, and self-learned (Beevers et al., 2017; Ebert et al., 2015; Webb, Rosso, & Rauch, 2017). The self-guided iCBT provided eight self-learning modules for participants to read and learn via the Internet and/or smart phone app to learn a variety of skills that have been developed from the CBT to handle their anxiety and depressive symptoms. The self-guided iCBT did not provide any counselor support, and only provided technical support for those who had difficulties in using the iCBT online platform and modules through telephone call and WhatsApp message.
Objectives and Hypothesis
The study aims to pilot test the feasibility and efficacy of a newly developed self-guided iCBT for university students in Hong Kong during the COVID-19 outbreak, with the following hypotheses:
1. The dropout rate of participants would be less than 50%;
2. The individual adherence rate of participants would be more than 66.6%;
3. Participants would show reduction in anxiety symptom after completing the self-guided iCBT.
4. Participants would show reduction in depressive symptom after completing the self-guided iCBT.
5. Participants would show reduction in perceived stress after completing the self-guided iCBT.
6. Individual’s improved outcome assessment scores due to the completion of the self-guided iCBT are related to and predicted by individual adherence rate.
Method
One Group Pre–Posttest Design
The first confirmed case of COVID-19 in Hong Kong was identified on Jan 23, 2020, which induced a high level of anxiety and depression among community residents (Choi et al., 2020). Owing to the common fear of COVID-19 and a lack of effective medical treatment and vaccination in the beginning stage of COVID-19 outbreak, social distancing measures were implemented in Hong Kong, including the suspension of traditional classroom teaching, offering online teaching, and restrictions in social contacts at local universities. Accordingly, this iCBT project had difficulties in openly promoting and recruiting participants cross different local universities, and conducting a randomized controlled trial. Instead, a one group pre–posttest design with convenient sampling was adopted. This iCBT project was promoted to the university students who were studying a master program in counseling at a local university through emails and online class announcements. Those university students who gave their consent to participate in this research project were allocated to use the self-guided iCBT. Subjects were eligible to participate in this study if they: (i) aged between 18 or above years old; (ii) were currently studying a master program in counseling at a local university in Hong Kong; (iii) were accessible to any computer and smart phone; and (iv) had given informed consent. Outcome measures were assessed with standardized assessment tools at baseline (t1) and within 2 weeks after completing all the online modules of the self-guided iCBT (t2). The ethical considerations of this study were evaluated and approved by the Research Committee of the Hong Kong Baptist University. Written informed consent were obtained from all participants on the day of pre-treatment assessment.
Data were collected between January 2020 and June 2021, and two cohorts of university students at a local university joined in the research. The first cohort consisted of 40 university students enrolled in AY2019/20, while the second cohort consisted of 43 university students enrolled in AY2020/21. The first cohort and second cohort suffered from different wave(s) of COVID-19 outbreak in Hong Kong between January 2020 and June 2021, with each wave of COVID-19 outbreak would properly induce different impacts on the severity of anxiety and depression among university students. Thus, the outcome assessments of the first cohort and second cohort at the pre- and post-intervention periods were presented separately in this study.
Subjects Characteristics
A total of 85 university students who were studying a master program in counseling at a local university in Hong Kong were invited to join in the research project. All, except one, gave their consent to join in the research. 84 participants completed outcome assessment at pre-intervention period (t1). Among them, 66 completed all the online modules. Among those who completed all online modules, 15 did not complete any outcome assessment at the post-intervention period (t2). Thus, this study involved 51 completers and 33 non-completers.
Table 1 provides the baseline demographic data and outcome assessment of the participating university students. Analyses from the t-test and chi-square test showed no significant differences between the first cohort and second cohort participants in all baseline demographic variables.
Table 1.
Demographic and Clinical Characteristics of Participants.
| Characteristics | Total (n = 84) | Cohort 1 (n = 40) | Cohort 2 (n= 44) | t (p) | χ2 (p) |
|---|---|---|---|---|---|
| Age, mean ± SD (years) a | 27.10 ± .76 | 26.9 ± 1.26 | 27.27 ± .92 | −.24 (.81) | |
| Female, n (%) b | 59 (72.8%) | 33 (82.5%) | 26 (63.4%) | 3.73 (.05) | |
| Marital status, n (%) b | 2.90 (.24) | ||||
| Single | 74 (89.2%) | 37 (92.5%) | 37 (86.0) | ||
| Married | 8 (9.6%) | 2 (5.0%) | 6 (14.0%) | ||
| Divorce, or separated | 1 (1.2%) | 11 (2.5%) | 0 (0.0%) | ||
| Education level, n (%) b | |||||
| Master degree | 84 (100%) | 40 (100%) | 44 (100%) | ||
| Occupational status, n (%) b | 6.78 (.08) | ||||
| Student | 49 (59.0%) | 26 (65.0%) | 23 (53.5%) | ||
| OE (FT) | 29 (34.9%) | 11 (27.5%) | 18 (41.9%) | ||
| OE (PT) | 3 (3.6%) | 3 (7.5%) | 0 (0.0%) | ||
| Unemployed | 2 (2.4%) | 0 (0.0%) | 2 (4.7%) | ||
| Main source of income, n (%) b | .46 (.80) | ||||
| Family support | 42 (52.5%) | 22 (55.0%) | 20 (50.0%) | ||
| Work | 35 (43.8%) | 17 (42.5%) | 18 (45.0%) | ||
| Other | 3 (3.8%) | 1 (2.5%) | 2 (5.0%) | ||
| Living situation, n (%) b | .26 (.88) | ||||
| With family | 58 (72.5%) | 27 (71.1%) | 31 (73.8%) | ||
| With co-tenants | 11 (13.8%) | 6 (15.8%) | 5 (11.9%) | ||
| Alone | 11 (13.8%) | 5 (13.2%) | 6 (14.3%) | ||
| Place of birth, n (%) b | .53 (.77) | ||||
| Hong Kong | 49 (59.0%) | 22 (55.0%) | 27 (62.8%) | ||
| Mainland China | 32 (38.6%) | 17 (52.5%) | 15 (34.9%) | ||
| Others | 2 (2.4%) | 1 (2.5%) | 1 (2.3%) | ||
| Period of stay in HK | 1.93 (.59) | ||||
| Born in HK | 46 (59.7%) | 21 (56.8%) | 25 (62.5%) | ||
| > 7 years | 7 (9.1%) | 3 (8.1%) | 4 (10.0%) | ||
| 1–7 years | 6 (7.8%) | 2 (5.4%) | 4 (10.0%) | ||
| < 1 year | 18 (23.4%) | 11 (29.7%) | 7 (17.5%) | ||
| Adherence rate (%), mean ± SDa | 84.52 ± 27.00 | 82.85 ± 26.74 | 86.11 ± 27.44 | −.56 ± .58 | |
| Pre-BAI, mean ± SDa | 7.83 ± .92 | 7.28 ± 1.30 | 8.34 ± 1.30 | −.58 ± .57 | |
| Pre-BDI, mean ± SDa | 12.31 ± 1.32 | 12.40 ± 2.19 | 12.53 ± 1.58 | .075 ± .95 | |
| Pre-PSS, mean ± SDa | 16.86 ± .65 | 16.75 ± .85 | 16.96 ± .97 | −.16 ± .88 |
Notes: * p <.05; p= p value.
Abbreviations: a = independent sample t-test; b = Pearson Chi-Square; χ2 = Pearson chi-square value; t = independent sample t-test value; BAI = Beck Anxiety Inventory; BDI: Beck Depression Inventory; PSS: Perceived Stress Scale; OE: Open employment. OE(FT): Full-time open employment; OE(PT): Part-time open employment.
Considering all participants (n = 84), the participants had a mean age of 27.2 years (SD = 0.76), and most were female (72.8%, n = 59), single (89.2%, n = 74), and were living with their families (72.5%, n = 58). Over half of the participant (59.0%, n = 49) were full time students. Among those participants who were studying the master program on a part-time mode, the majority had a full time job (85.3%, n = 29), few had a part-time job (8.8%, n = 3), or were unemployed (5.9%, n = 2). Over half (52.5%, n = 42) replied on family financial support, while nearly half (43.8%, n = 35) supported by the income from their work. Over half (59.0%, n = 49) were born in Hong Kong. Over one third were born in mainland China (38.6%, n = 32), and less than one third lived in Hong Kong less than 7 years (31.2%, n = 24). None of the participants had received any diagnosis of a mental disorder.
Outcome Assessment Tools
The Beck Anxiety Inventory (BAI) is a widely used assessment scale for measuring self-reported anxiety (Beck & Steer, 1993). The Chinese BAI has been reported to have very good validity and reliability (α= .95) (Cai et al., 2020; Che, Lu, Chen, Chang, & Lee, 2006). The BAI consists of 21 items. The score is summed over items, with a possible score that ranges from 0 to 63. A higher score indicates more serious anxiety symptoms: a score of 0–7 indicates minimal or no anxiety; 8–15, mild anxiety; 16–25, moderate anxiety; and 29–63, severe anxiety. In view of previous studies (Cai et al., 2020; Che et al., 2006), a cut-off point of a BAI score ≥ 16 was adopted as indicative of clinical anxiety for the participants.
The Beck Depression Inventory II (BDI) is a widely used assessment scale for measuring self-reported depression (Beck, Steer, & Brown, 1996). The reliability and validity of the Chinese BDI has been tested to be very good (α=.91) (Byrne et al., 2004; Zhu, Zhang, Sheng, & Wang, 2018). Also, the BDI has been used as an outcome assessment tool in various research work on iCBT with satisfactory results (Cuijpers et al., 2011; Johansson & Andersson, 2012). The BDI has 21 items. The score is summed over items, with a possible score that ranges from 0 to 63. A higher score indicates more serious depressive symptoms: a score of 0–13 indicates minimal or no depression; 14–19, mild depression; 20–28, moderate depression; and 29–63, severe depression. In view of previous studies (Beck et al., 1996; Byrne et al., 2004), a cut-off point of a BDI score ≥14 was adopted as indicative of clinical depression for the participants.
The Chinese Perceived Stress Scale (PSS) is a 10-item self-administered instrument for measuring the perception of stress with satisfactory validity and reliability (Cronbach’s α= .81) (Ng, 2013). The score is summed over the items, with a higher score indicates more severity in perceived stress.
The dropout rate was referred to the percentage of participants failing to complete all the modules of self-guided iCBT and/or post-intervention assessment.
The individual adherence rate to the self-guided iCBT was calculated based on the percentage of completion of the 8 online modules and the post-intervention assessment by an individual participant.
Design of Intervention
Each treatment group participant received the self-guided iCBT which consisted of eight self-learning modules for participants to read and learn via the Internet and/or mobile phone app to learn a variety of skills that have been developed from the CBT to handle their anxiety and depressive symptoms. Each module and related online assignments were to be completed on a weekly basis over a period of 8 week. The eight self-learning modules of the indigenized iCBT included the following themes: psychoeducation about depression and anxiety, normalizing the experiences of emotional distress, and breathing exercises (session 1); introducing ABC-model (Antecedents, Behavior, and Consequences) and relaxation skills, including abdomen breathing, imagery relaxation, and listening relaxation music (session 2–3); learning cognitive restructuring techniques (session 4–6); promoting a healthy lifestyle by re-scheduling daily activity (session 7); and preventing relapse based on vulnerability-stress model (session 8). Additionally, these online modules consisted of case studies, exercises on identifying and transforming cognitive distortions, audio navigation files on relaxation skills, and homework assignments.
Additionally, it has been suggested that culturally adapted psychological intervention produces better treatment effects than non-adapted psychological interventions for people with mental disorders (Chowdhary et al., 2014; Griner & Smith, 2006), and culturally adapted CBT is found to produce a better treatment effect than non-adapted CBT for people with mental disorders (Ng & Wong, 2018). Thus, this self-guided iCBT had the following aspects of adaptation to make it acceptable among Chinese participants. First, in relation to the language of the intervention, the technical terms of CBT in English were expressed in more culturally appropriate words in Chinese to improve cultural relevance and acceptability (Wong, 2008). For example, “cognitive distortion” was replaced by “mistakes in analyzing methods.” Second, the short-term and well-structured learning modules and homework assignments suited the needs of local university students with busy college life and stressful academic studies (Lun et al., 2018; Ng et al., 2016). Third, this self-guided iCBT applied life examples that were familiar to the locals rather than examples based on western societies.
A standardized and detailed manual of the eight modules of iCBT was designed and written for the treatment group by the researchers. The content of the iCBT modules and related multi-media resources were examined by the authors to ensure that the iCBT adhered to the principles, concepts, and intervention skills of CBT.
The self-guided iCBT did not provide any counselor support, and provided only technical support for those who had difficulties in using the iCBT online platform and modules through telephone calls and WhatsApp messages.
Results
Handling Missing Data
Analyses from the t-test and chi-square test showed no significant differences between the completers and non-completers for all, except one, baseline demographic variables and outcome assessment scores (see Table 2). The completers had a higher percentage of female than that of the non-completers. Thus, the completers and non-completers were very similar. Additionally, the non-completers did not give any prior notice or reason for their withdrawal from the study, which is perhaps not uncommon in Hong Kong. Thus, the missing data was assumed to be random. To maintain the full sample for data analysis, a multiple imputation method was conducted to replace the missing data prior to the data analysis.
Table 2.
Demographic and Clinical Characteristics of Completers and Non-Completers.
| Characteristics | Completer | Non-completer | t (p) | χ2 (p) |
|---|---|---|---|---|
| (N= 51) | (N= 33) | |||
| Age, mean ± SD (years) a | 27.15 ± 1.01 | 26.09 ± 1.14 | 1.06 ± .29 | |
| Female, n (%) b | 39 (81.3%) | 20 (60.6%) | 4.21 (.04) * | |
| Marital status, n (%) b | 1.54 (.46) | |||
| Single | 45 (90.0%) | 29 (87.9%) | ||
| Married | 5 (10.0%) | 3 (9.1%) | ||
| Divorce, or separated | 0 | 1 (3.0%) | ||
| Cohort | 2.16 (.14) | |||
| Cohort 1 (AY2019-20) | 21 (41.2%) | 19 (57.6%) | ||
| Cohort 2 (AY2020-21) | 30 (58.8%) | 14 (42.4%) | ||
| Occupational status, n (%) b | 3.35 (.34) | |||
| Student | 26 (52.0%) | 23 (69.7%) | ||
| OE (PT) | 20 (40.0%) | 9 (27.3%) | ||
| OE (PT) | 2 (4.0%) | 1 (3.0%) | ||
| Unemployed | 2 (4.0%) | 0 (0.0%) | ||
| Main source of income, n (%) b | .32 (.85) | |||
| Family support | 24 (50.0%) | 18 (56.3%) | ||
| Work | 22 (43.8%) | 13 (40.6%) | ||
| Other | 2 (3.8%) | 1 (3.1%) | ||
| Living situation, n (%) b | 2.05 (.36) | |||
| With family | 32 (66.6%) | 26 (81.3%) | ||
| With co-tenants | 8 (16.7%) | 3 (9.4%) | ||
| Alone | 8 (16.7%) | 3 (9.4%) | ||
| Place of birth, n (%) b | .67 (.72) | |||
| Hong Kong | 28 (56.0%) | 21 (63.6%) | ||
| Mainland China | 21 (42.0%) | 11 (33.3%) | ||
| Others | 1 (2.0%) | 1 (3.0%) | ||
| Period of stay in HK | 1.03 (.79) | |||
| Born in HK | 26 (55.3%) | 20 (66.7%) | ||
| > 7 years | 5 (10.6%) | 2 (6.7%) | ||
| 1–7 years | 4 (8.5%) | 2 (6.7%) | ||
| < 1 year | 12 (25.5%) | 6 (20.0%) | ||
| Pre-BAI, mean ± SDa | 8.00 ± 1.33 | 7.58 ± 1.14 | .23 ± .82 | |
| Pre-BDI, mean ± SDa | 12.59 ± 1.56 | 11.88 ± 2.38 | .26 ± .80 | |
| Pre-PSS, mean ± SDa | 17.08 ± .85 | 16.52 ± 1.01 | 4.19 ± .68 |
Notes: * p <.05; p= p value.
Abbreviations:a = independent sample t-test; b = Pearson Chi-Square; χ2 = Pearson chi-square value; t = independent sample t-test value; BAI = Beck Anxiety Inventory; BDI: Beck Depression Inventory; PSS: Perceived Stress Scale; OE: Open employment; OE(FT): Full-time open employment; OE(PT): Part-time open employment.
Data Analysis
All analyses were performed in accordance with the intent-to-treat principle adopting multiple imputation method analysis for any missing data. For all analyses, two-tailed p-values of < 0.05 were considered statistically significant. Data analyses were performed using SPSS 27.0 (IBM Corporation, 2019). The baseline demographic and clinical characteristics between the completers and non-completers were compared using chi-square (χ2) tests for categorical variables and independent t-tests for continuous variables. For hypothesis 1, the dropout rate referred to the percentage of participants failing to complete all the modules of self-guided iCBT and/or post-intervention assessment at t2. For hypothesis 3 to 5, paired t-tests were used to analyze the significant changes in the outcome assessment scores between the pre-intervention (t1) and post-intervention (t2) periods. Additionally, the general linear model 2 x 2 repeated measures analysis of variance (ANOVA) was used to compare the changes in outcome assessment scores between the subgroups of participants, such as first cohort and second cohort. The effect size for the paired t-tests was calculated using Hedges g, in which values of 0.2, 0.5, and 0.8 indicated small, medium, and large respectively, which is in line with the recommendation of Cohen (1988). The effect size for the ANOVA was calculated using the partial η2, in which values of 0.01, 0.06, and 0.14 were considered as small, moderate, and large effects, respectively (Cohen, 1988). With regard to hypothesis 6, those variables relating to the improved outcome assessments scores were identified by using one-way analysis of variance (ANOVA) for the categorical variables and Spearman’s correlation analysis for the continuous variables. The predicting variables for the improved outcome assessment scores were identified by adopting multiple linear regression analyses with the improved outcome assessment scores included as the dependent variables and their related baseline variables included as the independent variables. A stepwise selection method was adopted to compare the importance of the individual variables in predicting the improved outcome assessment scores. The collinearity of each regression model was examined with a variance inflation factor (VIF); a VIF less than 10 was considered to be non-collinear.
Baseline Outcome Assessment Scores
Table 1 provides the baseline outcome assessment scores of participants. The results of the independent t-test showed that the first cohort and second cohort did not show any significant difference in baseline BAI, BDI, and PSS scores. These results suggests that although first cohort and second cohort participants suffered from different wave(s) of COVID-19 outbreak in Hong Kong, the impacts of different wave(s) of COVID-19 outbreak on the severity of anxiety and depressive symptoms of first cohort and second cohort participant were more or less the same. Considering all participants, they reported a minimum to mild level of anxiety with a mean BAI score of 7.83 (SD = .92). In particular, one eighth (13.1%, n = 11) of all the participants were found to have current clinical anxiety, as assessed by the BAI (BAI score ≥ 16). Additionally, they reported a minimum to mild level of depression with a mean BDI score of 12.31 (SD = 1.32). In particular, one-third (36.9%, n = 31) of all the participants were found to have current clinical depression, as assessed by the BDI (BDI score ≥ 14).
Treatment Outcomes
Feasibility and Acceptability
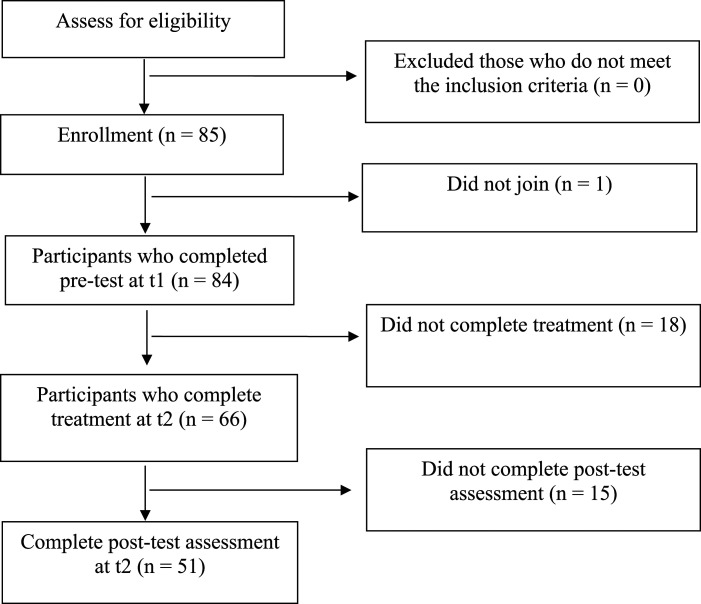
Hypothesis 1 and 2: Dropout and Adherence Rate. Figure 1 illustrates the flow of clients through each stage of the study. In particular, 33 out of 84 participants failed to complete the iCBT and/or post-intervention assessment, giving rise to a dropout rate of 39.3%.
Figure 1.
Flow of participants through each stage of the study.
The individual adherence rate was found to be 84.5% (SD = 27.00). Additionally, 66 out of 84 participants completed all the online modules, giving rise to a completion rate of 78.6%.
Preliminary Evidence for Efficacy
Tables 3 and 4 summarize the changes in the outcome scores for participants.
Table 3.
Paired Samples t-Tests on Outcome Measures.
| Outcome measures | T1 | T2 | t (p) | Effect size |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Hedges g | ||
| BAI | ||||
| Total (n = 84) | 7.83 ± 8.04 | 4.20 ± 3.73 | 4.13 *** | .45 |
| Cohort 1 (n = 40) | 7.28 ± 8.22 | 3.84 ± 2.89 | 2.67 * | .42 |
| Cohort 2 (n= 44) | 8.34 ± 8.63 | 4.53 ± 4.37 | 3.13 ** | .47 |
| BDI | ||||
| Total (n = 84) | 12.31 ± 12.12 | 5.09 ± 5.27 | 6.38 *** | .69 |
| Cohort 1 (n = 40) | 12.40 ± 13.85 | 5.05 ± 4.70 | 4.44 *** | .70 |
| Cohort 2 (n= 44) | 12.23 ± 10.47 | 5.13 ± 5.80 | 4.53 *** | .68 |
| PSS | ||||
| Total (n = 84) | 16.86 ± 5.93 | 14.97 ± 5.62 | 2.86 ** | .31 |
| Cohort 1 (n = 40) | 16.75 ± 5.38 | 14.21 ± 5.50 | 2.74 ** | .43 |
| Cohort 2 (n= 44) | 16.96 ± 6.46 | 15.66 ± 5.71 | 1.38 (ns) | .21 |
Notes: * p < .05; ** p < .01; *** p < .001; p = p value.
Abbreviations: ns = not significant; T1 = pre-test; T2 = post-test; BAI = Beck Anxiety Inventory; BDI = Beck Depression Inventory; PSS = Perceived Stress Scale.
Table 4.
Paired Samples t-Tests on Outcome Measures.
| Outcome measures | T1 | T2 | t (p) | Effect size | Between group analysis | Effect size |
|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Hedges g | F(p) | Partial η2 | ||
| BAI | ||||||
| Clinical anxiety | ||||||
| No (n = 73) | 5.23 ± 3.86 | 3.64 ± 3.31 | 2.84 ** | .33 | 149.13 *** | .65 |
| Yes (n = 11) | 25.09 ± 10.10 | 7.95 ± 4.36 | 4.77 ** | 1.38 | ||
| BDI | ||||||
| Clinical depression | ||||||
| No (n = 53) | 5.45 ± 4.87 | 3.69 ± 2.90 | 2.79 **2.79 ** | .38 | 78.18 ** | .49 |
| Yes (n = 31) | 24.03 ± 11.84 | 7.49 ± 7.27 | 8.47 *** | 1.50 | ||
Notes: * p < .05; ** p < .01; *** p < .001; p = p value.
Abbreviations: T1 = pre-test; T2 = post-test; BAI = Beck Anxiety Inventory; BDI = Beck Depression Inventory; Clinical Anxiety = BAI score ≥ 16; Clinical Depression = BDI score ≥ 14.
Hypothesis 3: Reducing Anxiety. The results of the paired t-test indicated that, after completing the self-guided iCBT, BAI score of all participants decreased significantly from 7.83 (SD = 8.04) at baseline (t1) to 4.20 (SD = 3.73) at post-test (t2), which was significant (t = 4.13, p < .001; 95% CI [1.880, 5.376]) with an effect size close to medium (Hedges g = 0.45; 95% CI [0.22, 0.67]).
Moreover, the results of the paired t-test indicated that, after completing the self-guided iCBT, BAI score of those with clinical anxiety decreased significantly from 25.09 (SD = 10.10) at baseline (t1) to 7.95 (SD = 4.36) at post-test (t2), which was significant (t = 4.77, p < .01; 95% CI [9.13, 25.16]) with a large effect size (Hedges g = 1.38; 95% CI [0.56, 2.28]). On the other hand, the results of the paired t-test indicated that, after completing the self-guided iCBT, BAI score of those without clinical anxiety decreased significantly from 5.23 (SD = 3.86) at baseline (t1) to 3.64 (SD = 3.31) at post-test (t2), which was significant (t = 2.84, p < .01; 95% CI [.48, 2.81]) with a small effect size (Hedges g = 0.33; 95% CI [0.10, 0.57]).
Additionally, the results of the 2 x 2 repeated measures of ANOVA demonstrated that compared to those without clinical anxiety, those with clinical anxiety had showed a significantly better reduction in the BAI score (F = 149.13, p < .01) with a large effect size (partial η2 = 0.65), while there was no significant difference in the reduction of BAI score between first cohort and second cohort (F = 0.62, p = 0.43 > .05).
Hypothesis 4: Reducing Depression. The results of the paired t-test indicated that, after completing the self-guided iCBT, BDI score of all participants decreased significantly from 12.31 (SD = 12.12) at baseline (t1) to 5.09 (SD = 5.27) at post-test (t2), which was significant (t = 6.38, p < .001; 95% CI [9.468, 6.380]), with a medium effect size (Hedges g = 0.69; 95% CI [0.45, 0.93]).
Moreover, the results of the paired t-test indicated that, after completing the self-guided iCBT, BDI score of those with clinical depression decreased significantly from 24.03 (SD = 11.84) at baseline (t1) to 7.49 (SD = 7.27) at post-test (t2), which was significant (t = 8.47, p < .001; 95% CI [12.55, 20.53]) with a large effect size (Hedges g = 1.50; 95% CI [1.00, 2.00]). On the other hand, the results of the paired t-test indicated that, after completing the self-guided iCBT, BDI score of those without clinical depression decreased significantly from 5.45 (SD = 4.87) at baseline (t1) to 3.69 (SD = 2.90) at post-test (t2), which was significant (t = 2.79, p < .01; 95% CI [.50, 3.03]) with a small effect size (Hedges g = 0.38; 95% CI [0.10, 0.66]).
Additionally, the results of the 2 x 2 repeated measures of ANOVA demonstrated that compared to those without clinical depression, those with clinical depression had showed significantly a better reduction in the BDI score (F = 78.18, p < .001) with a large effect size (partial η2 = 0.49), while there was no significant difference in the reduction of BDI score between first cohort and second cohort (F = 0.00, p = 0.98 > .05).
Hypothesis 5: Reducing Stress. The results of the paired t-test indicated that, after completing the self-guided iCBT, PSS score of all participants decreased significantly from 16.86 (SD = 5.93) at baseline (t1) to 14.97 (SD = 5.62) in post-test (t2) which was significant (t = 2.86, p < .01; 95% CI [.573, 3.200]) with a small effect size (Hedges g = 0.31; 95% CI [0.09, 0.53])).
Additionally, the results of the 2 x 2 repeated measures of ANOVA indicated that the reduction of PSS score for those with clinical anxiety (M = −8.22; SD = 6.23) showed a larger reduction in PSS score as compared with that of those without clinical anxiety (M = −0.93; SD = 5.46), which was significant (F = 8.60, p < .01) with a moderate to large effect size (partial η2 = 0.10). Similarly, the results of the 2 x 2 repeated measures of ANOVA indicated that the reduction of PSS score for those with clinical depression (M = −4.43; SD = 6.85) showed a larger reduction in PSS score as compared with that of those without clinical depression (M = −0.40; SD = 5.03), which was significant (F = 24.36, p < .001) with a large effect size (partial η2 = 0.23). On the other hand, the results of the ANOVA repeated measures indicated that the there was no significant difference in the reduction of PSS score between first cohort and second cohort (F = 0.59, p = 0.44 > .05).
Predictive Power of Individual Adherence Rate
Hypothesis 6: Higher Adherence Rate Predict Better Treatment Outcome. Table 5 shows the results of one way ANOVA and Spearman’s correlation analysis of the change in outcome measures, i.e. △BAI, △BDI, and △PSS. The △BAI and △BDI scores were not related to all demographic variables. The △PSS score was not related to any, except one, demographic variables. As compared with male participants, female participants showed a better reduction of PSS score (F = 4.58, p < .05). The △BAI score, △BDI score, and △PSS score were negatively related to the baseline BAI score, baseline BDI score, and baseline PSS score, but not the individual adherence rate.
Table 5.
Variables Related to the Change in Outcome Measures.
| Variables | △BAI | △BDI | △PSS | |||||
|---|---|---|---|---|---|---|---|---|
| ρ (p) | F (p) | ρ (p) | F (p) | ρ (p) | F (p) | |||
| Gender a | 3.87 (.053) | .43 (.510) | 4.58 (.036) * | |||||
| Marital status a | .64 (.294) | .73 (347) | 4.93 (.613) | |||||
| Occupational status a | .27 (.850) | .73 (.540) | .140 (.250) | |||||
| Main source of income a | .25 (.776) | .29 (.747) | .27 (.767) | |||||
| Living situation a | .89 (.597) | 1.57 (.880) | 1.13 (.266) | |||||
| Place of birth a | .38 (.685) | .42 (.786) | .10 (.905) | |||||
| Period of stay in HK a | .08 (.971) | .15 (.931) | .28 (.841) | |||||
| Cohort a | .05 (.833) | .01 (.912) | .89 (.349) | |||||
| Completer a | .37 (.546) | .63 (.430) | .52 (.474) | |||||
| Age b | −.01 (.905) | −.18 (.108) | −.04 (.693) | |||||
| Adherence rate b | −.11 (.314) | −.17 (.115) | −.10 (.377) | |||||
| Baseline BAI b | −.86 *** | −.73 *** | −.43(.001) ** | |||||
| Baseline BDI b | −.72 *** | −.89 *** | −.38 *** | |||||
| Baseline PSS b | −.36 *** | −.47 *** | −.49 *** | |||||
Notes: * p < .05; ** p < .01; *** p < .001; p= p value.
Abbreviations: a = ANOVA; F = ANOVA F value; b = Spearman correlation; ρ = Spearman’s rho; BAI = Beck Anxiety Inventory; BDI = Beck Depression Inventory; PSS = Perceived Stress Scale; △BAI = change in BAI score; △BDI = change in BDI score; △PSS = change in PSS Scale.
Table 6 shows the stepwise multiple linear regression analyses of the change in outcome measures, i.e. △BAI, △BDI, and △PSS. The collinearity is verified, and the collinearity statistics suggest that collinearity can be neglected for the regression model (VIF < 10). As shown in Table 5, the stepwise multiple linear regression model of △BAI explained 83.0% of its total variance (adj. R2). The baseline BAI score is the strongest predictor of △BAI and contributes to 80.6% of its total variance, while the baseline PSS contributes to 3.2% of the total variance of the △BAI. The stepwise multiple linear regression model of △BDI explained 83.0% of its total variance. The baseline BDI score is the strongest predictor of △BAI and contributes to 81.3% of its total variance (adj. R2), while the baseline BAI and baseline PSS contributes to 1.0% and 1.5% of the total variance of the △BDI, respectively. The stepwise multiple linear regression model of △PSS explained 31.0% of its total variance. The baseline PSS score is the only predictor of △PSS and contributes to 31.0% of its total variance (adj. R2).
Table 6.
Stepwise Multiple Linear Regression Analysis for Change in Outcome Measures.
| Model | Predictor | Adj. R2 | B | β | t | F | Collinearity Statistics | |
|---|---|---|---|---|---|---|---|---|
| Tolerance | VIF | |||||||
| Dependent variable: △BAI | ||||||||
| 1 | (Constant) | .80 | 3.114 | 5.84 *** | 341.71 *** | |||
| Baseline BAI | −.861 | −.898 | −18.49 *** | 1.00 | 1.00 | |||
| 2 | (Constant) | .83 | −.88 | −.79 (ns) | 209.54 *** | |||
| Baseline BAI | −.97 | −1.02 | −18.93 *** | .69 | 1.44 | |||
| Baseline PSS | .29 | .21 | 3.97 *** | .69 | 1.44 | |||
| Dependent variable: △BDI | ||||||||
| 1 | (Constant) | .81 | 2.277 | 3.24 ** | 356.53 *** | |||
| Baseline BDI | −.771 | −.902 | −18.88 *** | 1.00 | 1.00 | |||
| 2 | (Constant) | .82 | 2.523 | 3.61** | 188.22 *** | |||
| Baseline BDI | −.669 | −.782 | −10.72 *** | .41 | 2.44 | |||
| Baseline BAI | −.192 | −.155 | −2.13 * | .41 | 2.44 | |||
| 3 | (Constant) | .83 | −.84 | −.57 (ns) | 136.27 *** | |||
| Baseline BDI | −.73 | −.85 | −11.30 *** | .36 | 2.75 | |||
| Baseline BAI | −.23 | −.19 | −2.61* | .40 | 2.51 | |||
| Baseline PSS | .26 | .15 | 2.56 * | .61 | 1.63 | |||
| Dependent variable: △PSS | ||||||||
| 1 | (Constant) | .31 | 7.74 | 4.65*** | 37.47*** | |||
| Baseline PSS | −.57 | −.56 | −6.12*** | 1.00 | 1.00 | |||
Notes: * p < .05; ** p < .01; *** p < .001; p= p value.
Abbreviations: ns = not significant; Adj. R2: Adjusted R2; BAI = Beck Anxiety Inventory; BDI: Beck Depression Inventory; PSS: Perceived Stress Scale; △BAI = change in BAI score; △BDI = change in BDI score; △PSS = change in PSS score.
Discussion and Application for Practice
In this study, the demographic characteristics of participants largely resemble those of the most recent surveys on the prevalence of depression and anxiety among college students in Hong Kong (Cheung et al., 2020 & Lun et al., 2018). When compared with the results of these surveys, this research sample reported a higher prevalence rate of clinical depression and anxiety. In particular, in this study, about one-third (36.9%) of university students were found to have current clinical depression, as assessed by the BDI (BDI score ≥ 14), while about one-eight (13.1%) were found to have current clinical anxiety, as assessed by the BAI (BAI score ≥ 16). These differences in the reported prevalence rates of depression and anxiety among university students were probably because these recent surveys reported the prevalence rate of depression and anxiety before the outbreak of COVID-19 and social movement. As shown by recent studies, the recent social movement and outbreak of COVID-19 have induced a significantly higher prevalence rate of anxiety and depression among all Hong Kong residents, including university students (Choi et al., 2020; Hou et al., 2021). Thus it is not surprising that to find a higher prevalence rate of depression and anxiety among participating university students in this study as compared with the previous studies (Cheung et al., 2020 & Lun et al., 2018).
Hypothesis 1 and 2 are supported. This study aims to investigate the feasibility and acceptability of the self-guided iCBT for university students in Hong Kong during COVID-19 outbreak. In particular, a high dropout rate has been a great concern for self-guided iCBT as a high overall dropout rate (i.e., 57%) was reported across overseas studies of self-guided iCBT (Webb et al., 2017). In this study, this self-guided iCBT reported a comparatively lower dropout rate of 39.3%. Additionally, individual’s overall adherence was found to be high (84%), and about three quarters (78.6%) of participants completed all online modules of the self-guided iCBT. The results of this study demonstrate that this self-guided iCBT is feasible and accepted by many university students during COVID-19 outbreak. The participating university students were receiving a master degree of counseling, familiar with the concepts and skills of cognitive behavioral therapy, and receiving the technical support offered by this iCBT, and all these factors contribute to a comparatively lower dropout rate and higher adherence rate of this self-guided iCBT (Schmidt, Forand, & Strunk, 2019).
Hypotheses 3 to 5 are supported. This study also explores the efficacy of the self-guided iCBT for university students in Hong Kong during COVID-19 outbreak. During COVID-19 outbreak, the provision of online counseling has been recommended to help local university students with anxiety and/or depressive disorder (Choi et al., 2020; Liu et al., 2020), and there is increasing trend among local students to receive online counseling service (Li & Leung, 2020). Nevertheless, at present, limited research has been conducted to on evaluating the effectiveness of an online intervention in reducing anxiety and depressive symptoms for university students in Hong Kong. The results of this study demonstrate that the self-guided iCBT is efficacy in reducing anxiety symptoms, depressive symptoms, and perceived stress for university students in Hong Kong during the COVID-19 outbreak, which are also supported by the results of previous research studies (Andersson, 2015; Cuijpers et al., 2011; Webb et al., 2017). In particular, this self-guided iCBT was effective in reducing anxiety and depressive symptoms with a medium effect size (i.e., 0.45 for clinical anxiety and 0.69 for clinical depression). Interestingly, this self-guided iCBT produced a large treatment effect in reducing anxiety symptoms, depressive symptoms and perceived stress for those university students who reported clinical anxiety and/or depression, with a large effect size (Hedges g) of 1.3 on clinical anxiety and 1.5 on clinical depression respectively. The effect sizes of this self-guided iCBT are higher than those early studies which reported a small effect size of 0.28 for treating depressive and anxiety symptoms (Cuijpers et al., 2011; Webb et al., 2017). In fact, due to the local social distancing measures during COVID-19 outbreak in Hong Kong, university students with anxiety and depressive symptoms were unable or very resistant to receive treatment from traditional counseling units. At that time, this self-guided iCBT became the only way to help them to manage their anxiety and depressive symptoms. This may explain the efficacy of the self-guided iCBT for students with higher level of anxiety and/or depressive symptoms.
Hypothesis 6 is not supported. It has been suggested that the adherence rate determines the effectiveness of online CBT for anxiety and depressive disorders (Hilvert-Bruce, Rossouw, Wong, Sunderland, & Andrews, 2012). However, the results of the multiple regression analysis found that the improvement in anxiety, depression, and perceived stress was not predicted by the individual adherence rate of iCBT nor all, except gender, baseline demographic variables, but by baseline clinical variables, that is, baseline anxiety, depression, and perceived stress. These findings suggested, in line with Karyotaki et al. (2018) and Furukawa et al. (2021), that those participants who were more severe in anxiety, depressive and perceived stress before treatment benefited most from the self-guided iCBT by showing a greater reduction in anxiety, depression and perceived stress.
This self-guided iCBT has the following characteristics to meet the special needs of Hong Kong university students during COVID-19: (1) accessibility at any time anywhere; (2) anonymity and avoiding stigmatization; and (3) facilitating self-learning with technical support, which deserve more discussions.
First, accessibility any time anywhere: This self-guided iCBT offered flexible learning opportunities for the participants to read and learn the techniques and skills of CBT through an online platform that is accessible at any time anywhere, which are the typical advantages of iCBT over traditional face-to-face CBT (Smoktunowicz et al., 2020). During the early stage of COVID-19 outbreak, many university students, even though suffering from anxiety and depressive symptoms, were resistant to traditional face-to-face counseling services and have not received an assessment or counseling services, which is detrimental to their mental health (Auerbach et al., 2016; Hunt & Eisenberg, 2010; Lam et al., 2015). Barriers to traditional face-to-face counseling services included local social-distancing precautionary measures during COVID-19 outbreak, difficulties in accessing traditional counseling centers, and social stigmatization (De Witte et al., 2021). This self-guided iCBT overcame these treatment barriers by providing an online counseling platform that is accessible at any time anywhere anonymously so that university students with anxiety and depressive symptoms received early and timely assessment and treatment to facilitate their mental health recovery during COVID-19 outbreak.
Second, anonymity and avoiding stigmatization: Owing to the stigmatization of mental illness by traditional Chinese cultural values, college students with anxiety disorder are perceived as having a mental illness due to their own weaknesses, and failing to comply with the basic duties advocated by Confucianism, and subsequently they experience “shame,” “devaluation,” and “loss of face” (Young & Ng, 2016; Young, Ng, Corrigan, Chiu, & Yang, 2020). “Face concern” (mianzi) has been an important issue among local Chinese people seeking counseling, and “loss of face” leads to additional psychological distress for them (Mak, Chen, Lam, & Yiu, 2009). The self-guided iCBT allowed participants to use the online modules anonymously, without meeting with any counselor in-person, protecting participants’ privacy, avoiding social stigma, and avoiding any embarrassment that may be raised during face-to-face counseling. This is in line with Chinese cultural values, which emphasize on avoiding social stigmatization and saving “face” for seeking mental health services (Lam et al., 2015; Mak et al., 2009; Young & Ng, 2016).
Third, facilitating self-learning with technical support: According to previous studies, it was common for service users of iCBT to express technical difficulties in using iCBT and navigating the online platform of iCBT (Soucy, Hadjistavropoulos, Pugh, Dear, & Titov, 2019), and technical difficulties in using iCBT led to their dropout (Schmidt et al., 2019). In order to facilitate participants’ self-learning, it was found to be helpful for this self-guided iCBT project to offer technical support via telephone calls and WhatsApp messages provided by a technical staff. The short-term, well-structured and self-learning modules and homework assignments suited the needs of local university students with a busy and stressful college life (Lun et al., 2018; Ng et al., 2016), and matched with the pragmatism of Chinese cultural values which recognizing the practical solutions and believing that action and persistence would lead to success (Hodges & Oei, 2007).
Some methodological limitations of this study must be acknowledged. First, the research sample is limited to those university students who were receiving a master degree of counseling and were familiar with the concepts and skills of cognitive behavioral therapy, and thus this research sample cannot represent the whole population of university students. Second, the generalizability of the research results is also limited by the small sample size, dominance of female participants, adopting convenience sampling, and the lack of a control group for comparison. Additionally, third, an attribution rate of 39.3% reported in this study may give rise to biased estimation of intervention effects. Nevertheless, the close similarities between the completers and the non-completers in almost all baseline characteristics minimize any bias to the research results. Fourth, there was a lack of long-term follow-up study for those who completed the self-guided iCBT; thus, the long-term treatment effects of the self-guided iCBT remain uncertain. In the future, a larger scale randomized controlled trial with a long-term follow-up study across various demographic and cultural backgrounds of university students is needed to further validate the effectiveness of this self-guided iCBT in Chinese societies.
Acknowledgments
The authors would like to sincerely thank the participants for their cooperation and support towards this research study.
Footnotes
Author Contributions: YOUNG Daniel Kim-wan, Study concept and design, negotiating with other social service organizations involved in this project, acquisition of subjects and data, analysis and interpretation of data, and preparation of manuscript; Per CARLBRING, Study concept and interpretation of data; NG Petrus Yat-nam, Study concept and interpretation of data; CHEN Qi-rong, Data analysis and preparation of manuscript.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: The ethical considerations of this study have been evaluated and approved by the Research Committee of Hong Kong Baptist University. Written informed consent has been obtained from all participants on the day of the pre-treatment assessment.
ORCID iDs
Daniel K. W. Young https://orcid.org/0000-0002-6136-7389
Qi-rong J. Chen https://orcid.org/0000-0002-0981-4364
Per Carlbring https://orcid.org/0000-0002-2172-8813
Petrus Y. N. Ng https://orcid.org/0000-0002-1313-752X
References
- Ahmed M.Z., Ahmed O., Aibao Z., Hanbin S., Siyu L., Ahmad A. (2020). Epidemic of COVID-19 in China and associated psychological problems. Asian Journal of Psychiatry, 51, 102092. 10.1016/j.ajp.2020.102092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersson G. (2015). The internet and CBT: A clinical guide. London: CRC Press. [Google Scholar]
- Auerbach R. P., Alonso J., Axinn W. G., Cuijpers P., Ebert D. D., Green J. G., Bruffaerts R. (2016). Mental disorders among college students in the World Health Organization World Mental Health Surveys. Psychological Medicine, 46(14), 2955–2970. 10.1017/S0033291716001665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck A. T., Steer R. A. (1993). Beck anxiety inventory manual. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Beck A. T., Steer R. A., Brown G. K. (1996). Manual for the beck depression inventory–II. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Beck J. S. (2011). Cognitive behavioral therapy: Basics and beyond (2nd ed.). New York, NY: Guilford Press. [Google Scholar]
- Beevers C. G., Pearson R., Hoffman J. S., Foulser A., Shumake J., Meyer B. (2017). Effectiveness of an internet intervention (Deprexis) for depression in a United State adult sample: A parallel-group pragmatic randomized controlled trial. Journal of Consulting and Clinical Psychology, 85(4), 367–380. 10.1037/ccp0000171 [DOI] [PubMed] [Google Scholar]
- Boyd J. E., Adler E. P., Otilingam P. G., Peters T. (2014). Internalized stigma of mental illness (ISMI) scale: A multinational review. Comprehensive Psychiatry, 55(1), 221–231. 10.1016/j.comppsych.2013.06.005 [DOI] [PubMed] [Google Scholar]
- Byrne B. M., Stewart S., Lee P. W. H. (2004). Validating the beck depression inventory–II for Hong Kong community adolescents. International Journal of Testing, 4(3), 199–216. 10.1207/s15327574ijt0403_1 [DOI] [Google Scholar]
- Cai Q., Feng H., Huang J., Wang M., Wang Q., Lu X., Liu Y. (2020). The mental health of frontline and non-frontline medical workers during the coronavirus disease 2019 (COVID-19) outbreak in China: A case-control study. Journal of Affective Disorders, 275, 210–215. 10.1016/j.jad.2020.06.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlbring P., Andersson G., Cuijpers P., Riper H., Hedman-Lagerlöf E. (2018). Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: An updated systematic review and meta-analysis. Cognitive Behaviour Therapy, 47(1), 1–18. 10.1080/16506073.2017.1401115 [DOI] [PubMed] [Google Scholar]
- Che H. H., Lu M.L., Chen H. C., Chang S. W., Lee Y. J. (2006). Validation of the Chinese version of the beck anxiety inventory. Formosan Journal of Medicine, 10(4), 447–454. 10.6320/FJM.2006.10(4).05 [DOI] [Google Scholar]
- Cheung K., Tam L. Y., Tsang H., Zhang L. W., Lit S. W. (2020). Depression, anxiety and stress in different subgroups of first-year university students from 4-year cohort data. Journal of Affective Disorders, 274, 305–314. [DOI] [PubMed] [Google Scholar]
- Choi E., Hui B., Wan E. (2020). Depression and Anxiety in Hong Kong during COVID-19. International Journal of Environmental Research and Public Health, 17(10), 3740. 10.3390/ijerph17103740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowdhary N., Jotheeswaran A., Nadkarni A., Hollon S. D., King M., Jordans M, J. D., Patel V. (2014). The methods and outcomes of cultural adaptations of psychological treatments for depressive disorders: A systematic review. Psychological Medicine, 44(6), 1131–1146. 10.1017/S0033291713001785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). New York: Lawrence Erlbaum Associates. [Google Scholar]
- Cuijpers P., Donker T., Johansson R., Mohr D. C., Van Straten A., Andersson G. (2011). Self-guided psychological treatment for depressive symptoms: A meta analysis. PLoS One, 6, e21274. 10.1371/journal.pone.0021274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Witte N. A. J., Carlbring P., Etzelmueller A., Nordgreen T., Karekla M., Haddouk L., Van Daele T. (2021). Online consultations in mental healthcare during the COVID-19 outbreak: An international survey study on professionals’ motivations and perceived barriers. Internet Interventions, 25, 100405. 10.1016/j.invent.2021.100405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebert D. D., Zarski A. C., Christensen H., Stikkelbroek Y., Cuijpers P., Berking M. (2015). Internet and computer-based cognitive behavioral therapy for anxiety and depression in youth: A meta-analysis of randomized controlled outcome trials. PLoS One, 10(3), e0119895. 10.1371/journal.pone.0119895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furukawa T. A., Suganuma A., Ostinelli E. G., Andersson G., Beevers C. G., Shumake J., Cuijpers P. (2021). Dismantling, optimising, and personalising internet cognitive behavioural therapy for depression: A systematic review and component network meta-analysis using individual participant data. The Lancet. Psychiatry, 8(6), 500–511. 10.1016/S2215-0366(21)00077-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratzer M., Khalid-Khan F. (2016). Internet-delivered cognitive behavioural therapy in the treatment of psychiatric illness. Canadian Medical Association Journal, 188(4),263–272. 10.1503/cmaj.150007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griner D., Smith T. B. (2006). Culturally adapted mental health intervention: A meta-analytic review. Psychotherapy (Chic), 43(4), 531–548. 10.1037/0033-3204.43.4.531 [DOI] [PubMed] [Google Scholar]
- Hilvert-Bruce Z., Rossouw P. J., Wong N., Sunderland M., Andrews G. (2012). Adherence as a determinant of effectiveness of internet cognitive behavioural therapy for anxiety and depressive disorders. Behaviour Research and Therapy, 50(7–8), 463–468. 10.1016/j.brat.2012.04.001 [DOI] [PubMed] [Google Scholar]
- Hodges J., Oei T. P. S. (2007). Would confucius benefit from psychotherapy? The compatibility of cognitive behaviour therapy and Chinese values. Behaviour Research and Therapy, 45(5), 901–914. 10.1016/j.brat.2006.08.015 [DOI] [PubMed] [Google Scholar]
- Hou W. K., Lee T. M. C., Liang L., Li T. W., Liu H., Ettman C. K., Galea S. (2021). Civil unrest, COVID-19 stressors, anxiety, and depression in the acute phase of the pandemic: a population-based study in Hong Kong. Social Psychiatry and Psychiatric Epidemiology, 56(8), 1499–1508. 10.1007/s00127-021-02037-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt J., Eisenberg D. (2010). Mental health problems and help-seeking behavior among college students. Journal of Adolescent Health, 46(1), 3–10. 10.1016/j.jadohealth.2009.08.008 [DOI] [PubMed] [Google Scholar]
- IBM Corp . (2019). IBM SPSS statistics for windows (Version 27.0). IBM Corp. [Google Scholar]
- Johansson R., Andersson G. (2012). Internet-based psychological treatments for depression. Expert Review of Neurotherapeutics, 12(7), 861–870. 10.1586/ern.12.63 [DOI] [PubMed] [Google Scholar]
- Karyotaki E., Ebert D. D., Donkin L., Riper H., Twisk J., Burger S., Cuijpers P. (2018). Do guided internet-based interventions result in clinically relevant changes for patients with depression? An individual participant data meta-analysis. Clinical Psychology Review, 63, 80–92. 10.1016/j.cpr.2018.06.007 [DOI] [PubMed] [Google Scholar]
- Lam L. C., Wong C. S., Wang M. J., Chan W. C., Chen E. Y., Ng R. M., Bebbington P. (2015). Prevalence, psychosocial correlates and service utilization of depressive and anxiety disorders in Hong Kong: The Hong Kong Mental Morbidity Survey (HKMMS). Social Psychiatry and Psychiatric Epidemiology, 50(9), 1379–1388. 10.1007/s00127-015-1014-5 [DOI] [PubMed] [Google Scholar]
- Li M. H., Leung S. Y. (2020). Exploring student mental health and intention to use online counseling in Hong Kong during the COVID‐19 pandemic. Psychiatry and Clinical Neurosciences, 74(10), 564–565. 10.1111/pcn.13117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Yang L., Zhang C., Xiang Y. T., Liu Z., Hu S., Zhang B. (2020). Online mental health services in China during the COVID-19 outbreak. The Lancet. Psychiatry, 7(4), e17–e18. 10.1016/S2215-0366(20)30077-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lun K. W., Chan C. K., Ip P. K., Ma S. Y., Tsai W. W., Wong C. S., Wong C. H., Yan D. (2018). Depression and anxiety among university students in Hong Kong. Hong Kong Medical Journal, 24(5), 466–472. 10.12809/hkmj176915 [DOI] [PubMed] [Google Scholar]
- Mak W. W. S., Chen S. X., Lam A. G., Yiu V. F. L. (2009). Understanding distress: The role of face concern among Chinese Americans, European Americans, Hong Kong Chinese, and Mainland Chinese. The Counseling Psychologist, 37(2), 219–248. 10.1177/0011000008316378 [DOI] [Google Scholar]
- Ng S. M. (2013). Validation of the 10-item Chinese perceived stress scale in elderly service workers: One-factor versus two-factor structure. BMC Psychology, 1, 9. 10.1186/2050-7283-1-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng K. C., Chiu W. K., Fong Y. F. (2016). A review of academic stress among Hong Kong undergraduate students. Journal of Modern Education Review, 6(8), 531–540. 10.15341/jmer(2155-7993)/08.06.2016/003 [DOI] [Google Scholar]
- Ng T. K., Wong D. F. K. (2018). The efficacy of cognitive behavioral therapy for Chinese people: A meta-analysis. Australian & New Zealand Journal of Psychiatry, 52(7), 620–637. 10.1177/0004867417741555 [DOI] [PubMed] [Google Scholar]
- Schmidt I. D., Forand N. R., Strunk D. R. (2019). Predictors of dropout in internet-based cognitive behavioral therapy for depression. Cognitive Therapy and Research, 43(3), 620–630. 10.1007/s10608-018-9979-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smoktunowicz E., Barak A., Andersson G., Banos R. M., Berger T., Botella C., Carlbring P. (2020). Consensus statement on the problem of terminology in psychological interventions using the internet or digital components. Internet Interventions, 21, 100331. 10.1016/j.invent.2020.100331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soucy J., Hadjistavropoulos H., Pugh N., Dear B., Titov N. (2019). What are clients asking their therapist during therapist-assisted internet-delivered Cognitive Behaviour Therapy? A content analysis of client questions. Behavioural and Cognitive Psychotherapy, 47(4), 407–420. 10.1017/S1352465818000668 [DOI] [PubMed] [Google Scholar]
- Wang C., Zhao H. (2020). The Impact of COVID-19 on anxiety in Chinese University students. Frontiers in Psychology, 11, 1168. 10.3389/fpsyg.2020.01168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb C. A., Rosso I. M., Rauch S. L. (2017). Internet-based cognitive-behavioral therapy for depression: Current progress and future directions. Harvard Review of Psychiatry, 25(3), 114–122. 10.1097/HRP.0000000000000139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong D. F. K. (2008). Cognitive and health-related outcomes of group cognitive behavioural treatment for people with depressive symptoms in Hong Kong: Randomized wait-list control study. Australian and New Zealand Journal of Psychiatry, 42(8), 702–711. 10.1080/00048670802203418 [DOI] [PubMed] [Google Scholar]
- Young K. W., Ng P. (2016). The prevalence and predictors of self-stigma of persons with mental illness in two Chinese cities. International Journal of Social Psychiatry, 62(2), 176–185. 10.1177/0020764015614596 [DOI] [PubMed] [Google Scholar]
- Young D. K., Ng P. Y. P., Corrigan P., Chiu R., Yang S. (2020). Self-stigma reduction group for people with depression: A randomized controlled trial. Research on Social Work Practice, 30(8), 846–857. 10.1177/1049731520941594 [DOI] [Google Scholar]
- Zhu J., Zhang J., Sheng Z., Wang F. (2018). Reliability and validity of the beck depression inventory-II applied to Chinese construction workers. Social Behavior and Personality, 46(2), 249–258. 10.2224/sbp.6638 [DOI] [Google Scholar]