Abstract
Background
Pregnant women were excluded from investigational trials of COVID-19 vaccines. Limited data are available to inform pregnant and postpartum women on their decisions to receive a COVID-19 vaccine.
Methods
The goal of this observational, prospective cohort study is to evaluate the immunogenicity and safety of various Emergency Use Authorization (EUA) or licensed COVID-19 vaccines administered to pregnant or lactating women and describe the transplacental antibody transfer and kinetics of antibodies in mothers and infants. The study is adaptive, allowing additional groups to be added as new vaccines or vaccine regimens are authorized. Up to 20 clinical research institutions in the United States (U.S.) will be included. Approximately 200 pregnant women and 65 postpartum women will be enrolled per EUA or licensed COVID-19 vaccine formulation in the U.S. This study will include pregnant and postpartum women of all ages with and without chronic medical conditions. Their infants will be enrolled and followed beginning at birth in the pregnant cohort and beginning at the earliest possible time point in the postpartum cohort. Blood samples will be collected for immunogenicity outcomes and pregnancy and birth outcomes assessed among women and infants. Primary analyses will be descriptive and done by vaccine type and/or platform.
Discussion
Given the long-standing and legitimate challenges of enrolling pregnant individuals into clinical trials early in the vaccine development pipeline, this study protocol describes our current study and provides a template to inform the collection of data for pregnant individuals receiving COVID-19 or other vaccines.
Trial registration
Supplementary Information
The online version contains supplementary material available at 10.1186/s12884-022-04500-w.
Keywords: Pregnant women, Postpartum women, COVID-19 vaccines, Immunogenicity, Infant immune responses
Background
Pregnant women are susceptible to infection and complications from SARS-CoV-2. Observational data in the U.S. demonstrate that, while the absolute risk for severe health effects may be low, pregnant women have an increased risk of developing severe COVID-19, including illness that results in pneumonia, intensive care unit (ICU) admission, need for mechanical ventilation, and death compared with non-pregnant women of reproductive age with COVID-19 [1–5]. Pregnant women who acquire COVID-19 are more likely to experience adverse consequences including preterm birth, and their infants have an increased risk of neonatal intensive care unit (NICU) admission [2, 4, 6–9]. Maternal immunization may be a strategy to provide protection to both the mother and the infant against complications associated with COVID-19.
Several COVID-19 vaccines utilizing different platforms (e.g., mRNA, viral vectored, protein-based, inactivated virus), are available or will soon be available under EUA in the U.S. or will soon be licensed. Pregnant women were not included in pivotal efficacy trials of these vaccines, and currently, only the Pfizer/BioNTech mRNA vaccine is being tested in a randomized controlled trial among pregnant women [10]. Conducting placebo-controlled trials in pregnant women is increasingly problematic given the widespread availability of these vaccines in the U.S. and many other countries, where approved vaccines are being administered to individuals who are pregnant or postpartum, as part of national vaccination campaigns. Safety data are being collected through various surveillance systems in the U.S., with reassuring results to date [11, 12]. However, many knowledge gaps remain regarding the use of COVID-19 vaccines during pregnancy and after delivery. Data on kinetics and durability of maternal antibodies, transplacental antibody transfer to the infant, breast milk antibodies, and kinetics of antibodies in infants, are limited [13, 14].
We designed an observational study in pregnant and postpartum women in order to fill knowledge gaps on use of COVID-19 vaccines in these populations. The purpose of this manuscript is to share our rationale and study design, laboratory evaluations, and analyses plans, and to serve as a template for similar studies of COVID-19 and other vaccines in pregnant and postpartum populations (including those who are lactating). It is expected that the results of this study will inform policy recommendations and personal decision-making on the use of approved COVID-19 vaccines in pregnant and postpartum individuals in the U.S. and globally.
Trial overview
The goal of this observational, prospective cohort study is to evaluate the immunogenicity and safety of various EUA or licensed COVID-19 vaccines administered to pregnant or lactating women and describe the transplacental antibody transfer and kinetics of antibodies in mothers and infants. The adaptive study design allows the evaluation of up to 5 vaccines, with groups added as new vaccines are authorized and vaccination recommendations evolve.
Methods
Approximately 1000 total study participants who receive or plan to receive a COVID-19 vaccine during pregnancy and/or postpartum and their infants will be enrolled. Pregnant women during any trimester of pregnancy will be enrolled either prior to or after receipt of vaccine(s) and followed with periodic blood draws for immunogenicity assessments. Pregnancy status will be confirmed through medical records, and vaccination status will be confirmed through medical records or vaccination card. Infants will be enrolled at birth. At that time, maternal and cord blood samples will be obtained, and details of the birth will be collected. Mother and infants will be followed through 12 months with periodic immunogenicity sampling and safety follow-up. Thus, the study duration of participation for pregnant women will be up to 20 months. A cohort of postpartum women will be enrolled either prior to or after receipt of vaccine(s) within the first 2 months of delivery. Their infants will be enrolled at the same time and will be followed through 12 months with periodic immunogenicity sampling and safety follow-up. A schedule of events is found in Tables 1 and 2.
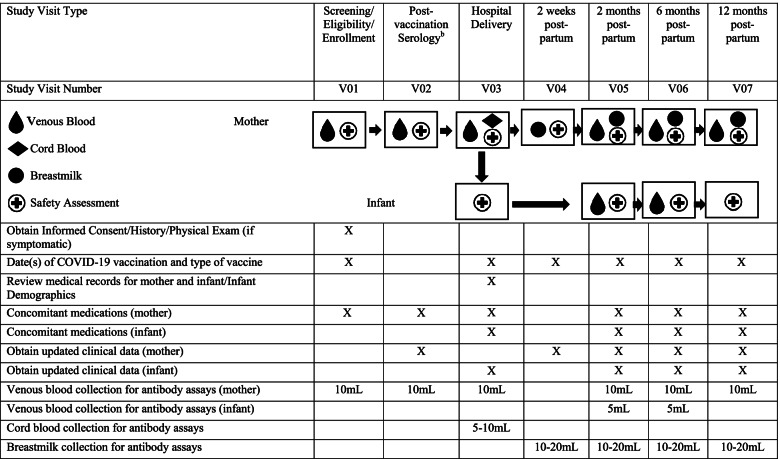
Table 1.
Schedule of Events for Multi-site Observational Maternal and Infant COVID-19 Vaccine Study (MOMI-Vax). Schedule of Events: Pregnant Women and their Infantsa
Abbreviations: mL milliliters
an = approximately 200 pregnant women who are scheduled to receive or have completed any licensed or EUA COVID-19 vaccine series per vaccine type and approximately 200 infants born to pregnant women per vaccine type
bOnly applicable if V01 was completed pre-vaccination
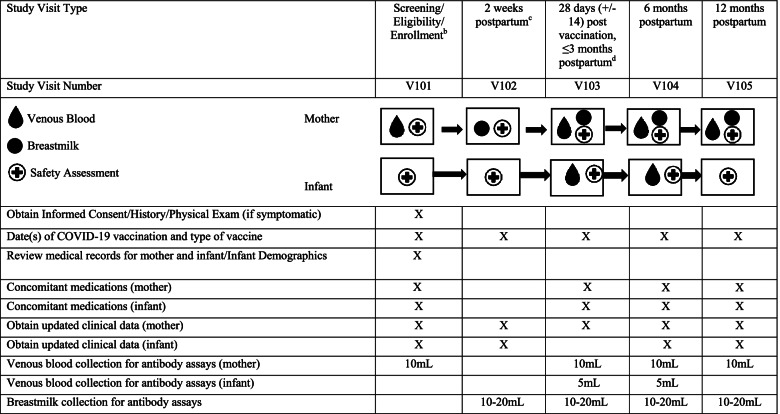
Table 2.
Schedule of Events for Multi-site Observational Maternal and Infant COVID-19 Vaccine Study (MOMI-Vax). Schedule of Events: Postpartum Women and their Infantsa
Abrreviations: mL milliliters
an = approximately 65 postpartum women who are scheduled to receive or have initiated any licensed or EUA COVID-19 vaccine series within first 2 months of delivery; n = approximately 65 infants of postpartum women
bFor mothers vaccinated prior to enrollment: Document COVID-19 vaccination date(s) and type
cOptional, for mothers enrolled at delivery
dIf visit overlaps with Visit 101 (i.e., mother received full series prior to enrollment), the two visits will be combined
Written informed consent will be obtained from the pregnant and postpartum participants at the enrollment visit. Informed consent will be obtained from the mother for the infant either at the time of birth or for postpartum individuals, at time of enrollment (see Additional Files 1, 2 and 3). This study will be carried out in accordance with Good Clinical Practice (GCP) guidelines. The Vanderbilt University Medicine Center Institutional Review Board (IRB) has reviewed and approved this protocol, consent forms and associated documents. Each institution engaged in this research will hold an Office of Human Research Protections (OHRP)-approved Federal Wide Assurance (FWA). All study records will be kept in a locked file cabinet or maintained in a locked room at the site. Electronic files will be password-protected. Only people who are involved in the conduct, oversight, monitoring, or auditing of this study will be allowed access to the PHI that is collected. Any publications from this study will not use information that will identify subjects by name. Organizations that may inspect and/or copy research records maintained at the site for quality assurance (QA) and data analysis include groups such as the local or central IRB, NIAID, and the FDA.
Quality oversight procedures will be implemented by FHI 360 in consultation with the Infectious Disease Clinical Research Consortium (IDCRC) Clinical Operations Unit (COU). Quality oversight will include review of each participating site’s Clinical Quality Management Plan - Quality Management Summary Report on a quarterly basis, as well as overall enrollment tracking and oversight of performance trends.
Study population
This observational study was designed to be broadly inclusive to reflect the need to collect information on pregnant and postpartum women of all ages, with and without chronic medical conditions, and with singleton or multiple gestations. The study will include postpartum women whether or not they choose to breastfeed. The exclusion criteria are limited to behavioral or cognitive impairment, psychiatric disease or any condition that might pose a health risk and interfere with the individual’s ability to participate and/or the evaluation of study objectives (Table 3).
Table 3.
Study Inclusion and Exclusion Criteria
| Inclusion Criteria |
Pregnant Women 1. Pregnant individuals scheduled to receive or have received complete vaccination series of any licensed or EUA COVID-19 vaccinea 2. Willing and able to provide consent for study participation for herself and for her infant prior to initiation of any study procedures. |
|
Postpartum Women 3. Individuals scheduled to receive or who have initiated vaccination series of any licensed or EUA COVID-19 vaccine within the first 2 months postpartumb 4. Willing and able to provide consent for study participation for herself and for her infant prior to initiation of any study procedures (a separate consent form will be used for their infants). | |
|
All participants 5. Understands and agrees to comply with all study procedures. 6. Agrees to sign medical release for herself and her infant to allow study staff to gather pertinent medical information, pregnancy outcome data, and medical information as needed. | |
| Exclusion Criteria |
1. Behavioralc or cognitive impairment or psychiatric disease that, in the opinion of the investigator, may interfere with the participant’s ability to participate in the study. 2. Any condition which, in the opinion of the investigators, may pose a health risk to the participant or interferes with the evaluation of the study objectives |
Abbreviations: EUA Emergency Use Authorization
aNo limitation on age of mother, health status, or gestational age at enrollment
bNo limitation on maternal age or health status
cIncludes having a history of alcohol or drug abuse within 1 year prior to study enrollment
Study procedures
Recruitment and screening
Participants will be recruited from up to 20 academic affiliated, IDCRC sites throughout the U.S. Study staff will inform potential participants/legally authorized representatives of the study, obtain informed consent, and determine study eligibility.
Enrollment
Screening and enrollment visits will occur sequentially or on the same day. Study staff will collect baseline information on participants (e.g., demographics, medical history, obstetric history, history of respiratory illnesses) (Tables 1 and 2). Pregnant individuals who meet all eligibility criteria will be enrolled. Infants born to pregnant individuals will become study participants upon delivery and maternal consent. Postpartum individuals who meet all eligibility criteria will be enrolled along with their infants. Once enrolled, each individual will be registered in a study database. Enrollment will continue until number of participants is reached for a particular vaccine type/study group. If new vaccines receive EUA or licensure, vaccine types will be added.
Follow-up
For women enrolled during pregnancy, a pre- and post-vaccination serology will be obtained if the subject had not received a vaccine prior to screening/enrollment, and post-vaccination serology will be obtained at any time after receipt of vaccine at the time of screening/enrollment if the subject had previously completed their full vaccination series. Routine follow-up visits for the women and infants include hospital delivery date, 2 weeks, 2, 6, and 12 months postpartum. Routine visits for postpartum women and their infants include visits at 2 weeks postpartum (or earliest enrolled date), 28 days (+/− 14) after last vaccination/ ≤3 months postpartum, 6 and 12 months postpartum. All routine visits will consist of obtaining updated clinical data, concomitant medications, collection of venous blood for antibody assays, obtaining date(s)/type of COVID-19 vaccine, date and severity of confirmed COVID-19 illness, and optional collection of breast milk samples (Tables 1 and 2). Unscheduled visits may be needed to complete study procedures that could not be conducted at the routine visits.
Study outcomes
Outcomes of pregnancy, both maternal and fetal/infant, will be collected. Since this is an observational protocol, no serious adverse events (SAEs) or adverse events of special interest (AESIs) will be collected during this study. Potential non-serious adverse events that could occur in association with study procedures such as blood sample collection will be reported to the IRB. Maternal outcomes that will be recorded include death of mother or fetus, maternal hospitalization or prolonging of existing hospitalization, or important medical events reported after vaccination requiring treatment. Infant outcomes that will be recorded include neonatal or infant death through 12 months post-delivery, infant hospitalization, a congenital defect or genetic anomaly, preterm delivery/prematurity (defined as live birth prior to 37 weeks gestation). The assessment of these maternal and infant events will be harmonized by using existing Brighton Collaboration case definitions [15].
Pregnancy outcome data include the type of delivery (e.g., vaginal vs. Cesarean section), and any complications during labor and delivery for both the mother as well as the neonate. Neonatal assessments include but are not limited to gestational age, birth weight, Apgar scores, congenital and genetic abnormalities, infection, hematological and metabolic complications, admission to nursery or NICU and the need for respiratory support or other life sustaining interventions.
All information on COVID-19 cases during the study will be collected via medical records including polymerase chain reaction (PCR) or antigen testing results and severity of illness.
Laboratory assays
Serum
Primary and secondary endpoint assays to determine serum levels of total and SARS-CoV-2 antigen-specific immunoglobulin G (IgG) [16] and live [17] and pseudovirus [ 18] neutralizing antibodies will be performed at central IDCRC laboratories utilizing qualified assays (Table 4). Reagents will include vaccine-matched and emerging variants to evaluate the ability of variants to escape antibody generated by vaccine in this cohort. Additional exploratory endpoint analyses may include Ig subclass, and SARS-CoV-2 IgG Fc glycosylation (Table 4) [20].
Table 4.
Assays
| Study Endpoint | Specimen | Assay | Readout |
|---|---|---|---|
| Primary | Venous and Cord Blood Serum | MSD® V-Plex SARS-CoV-2 Panel 2 [16] | Spike, RBD and N IgG binding Ab |
| FRNT-mNG [17] | Ab neutralizing SARS-CoV-2 | ||
| Pseudoneutralization [18] | Ab neutralizing SARS-CoV-2 | ||
| Secondary | Breast Milk | MSD® V-Plex SARS-CoV-2 Panel 2 [16] | Spike, RBD and N IgG and IgA binding Ab |
| FRNT-mNG [17] | Ab neutralizing SARS-CoV-2 | ||
| Pseudoneutralization [18] | Ab neutralizing SARS-CoV-2 | ||
| Exploratory |
Venous and Cord Blood Serum; Breast Milk |
MSD® V-Plex SARS-CoV-2 Panel 2 [16] – emerging variant reagents | Vaccine-induced Ab binding to emerging variants |
| FRNT-mNG [17] - emerging variant reagents | Vaccine-induced Ab neutralizing emerging variants | ||
| Pseudoneutralization [18] - emerging variant reagents | Vaccine-induced Ab neutralizing emerging variants | ||
| Luminex [19] or MSD® | Antigen-specific Ab isotype and subclass profiles | ||
| IgG glycan analysis [20] | IgG Fc glycosylation | ||
| Ancillarya | Whole Blood | RNAseq, single-cell RNAseq [21] | Gene signatures to identify vaccine biomarkers |
| PBMC | ELISpot/flow cytometry [22–24] | T and B memory cells, plasmablasts | |
| ICS/flow cytometry [25] | CD4/CD8 T cells | ||
| Tetramer-staining | SARS-CoV-2 specific T cells | ||
| MSD® cytokine panel | Th1/Th2 cytokines |
Abbreviations: MSD Meso Scale Discovery®, RBD receptor binding domain, FRNT-mNG Focus Reduction Neutralization Test mNeonGreen, Ab antibody, ICS intracellular cytokine staining
aCollection of whole blood and PBMC under consideration in a subset of participants and/or at a subset of sites
Breast milk
Measurement of total and SARS-CoV-2 antigen-specific immunoglobulin IgA (IgA) and IgG and live and pseudovirus neutralizing antibodies will be performed at the same central laboratories as with serum (see above and Table 4). These assays are being qualified using breast milk samples from vaccinated and/or COVID-19 infected women.
Other samples
The collection of whole blood and its processing for peripheral blood mononuclear cells (PBMC) in a subset of participants and/or subset of clinical sites are under discussion in order to conduct additional ancillary studies (Table 4).
Data collection, quality and management
Data collection is the responsibility of the study personnel at the participating clinical study site under the supervision of the site PI. During the study, the site PI must maintain complete and accurate documentation for the study.
The site PI is responsible to ensure the accuracy, completeness, legibility, and timeliness of the data reported. All source documents should be completed in a neat, legible manner to ensure accurate interpretation of data.
Copies of the electronic Case Report Form (eCRF) will be provided for use as source CRFs, as needed, and maintained for recording data for each subject enrolled in the study. Data reported in the eCRF derived from source CRFs should be consistent or the discrepancies should be explained.
The data coordinating center for this study will be responsible for data management, quality review, analysis, and reporting of the study data.
Clinical (including, but not limited to, AEs, concomitant medications, medical history, physical assessments) and immunogenicity data will be entered into a 21 CFR 11-compliant Clinical Data Management System provided by the data coordinating center. The data system includes password protection and internal quality checks, such as automatic range checks, to identify data that appear inconsistent, incomplete, or inaccurate. Clinical data will be entered directly from the CRFs completed by the study personnel.
Statistics
This study will generate descriptive data that is supportive of the hypothesis that COVID-19 vaccines elicit adequate immune responses among pregnant and postpartum individuals and will describe the transplacental antibody transfer for SARS-CoV-2 and serum SARS-CoV-2 antibodies in mother and infants of vaccinated mothers.
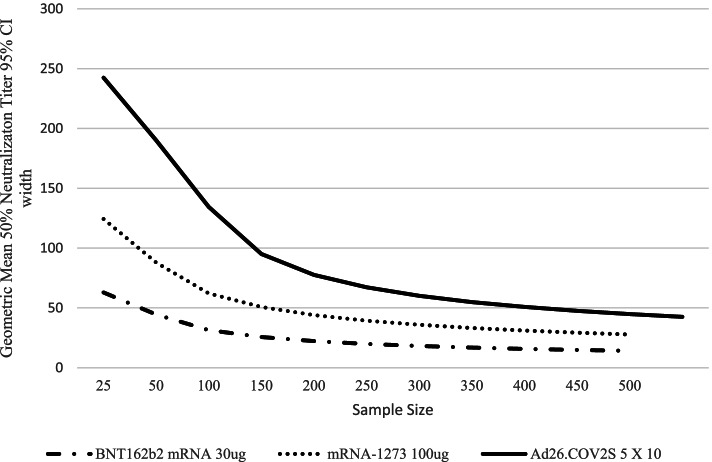
Approximately 200 pregnant individuals and their infants and up to 65 postpartum individuals and their infants per SARS-CoV-2 vaccine type (Groups 1–4) will be enrolled in this protocol. Two additional groups (Groups 5 and 6) have been added since beginning enrollment following approval of administration of a booster dose in late 2021. It is important to generate data on kinetics and durability of maternal and infant antibodies for all vaccine regimens, including those with additional doses beyond the primary series administered during pregnancy. Figure 1 illustrates the study precision of estimation of GMT of Neut antibodies the study with various sample sizes using Phase 1 data from the Pfizer, Moderna, and Janssen COVID-19 vaccines [26–28]. In addition, there will be good precision for estimation of transplacental transfer ratios.
Fig. 1.
Sample Size Calculation based on Width of 95% Confidence Intervals for Neutralizing Antibodies for COVID-19 Vaccines included in MOMI-Vax. Legend: The curve shows neutralizing antibody from Phase 1 studies and demonstrates the inflection point for sample size at approximately 150 individuals per group, with little gain in precision with higher samples sizes. Results similar using binding antibody data (results not shown)
The analysis groups are:
Group 1: Individuals who receive a COVID-19 vaccine during pregnancy (up to 200 individuals per vaccine type).
Group 2: Individuals who receive a COVID-19 vaccine postpartum (up to 65 individuals per vaccine type).
Group 3: Infants of individuals who receive COVID-19 vaccine during pregnancy (approximately 200 infants per vaccine type).
Group 4: Infants of individuals who receive COVID-19 vaccine postpartum (approximately 65 infants per vaccine type).
Group 5: Individuals who receive additional COVID-19 vaccine(s) (booster) during pregnancy (up to 200 individuals).
Group 6: Infants of individuals who received additional COVID-19 vaccine(s) (booster) during pregnancy (approximately 200 infants).
The study will not randomize participants between vaccines, and statistical analyses will seek to adjust for covariates when deemed appropriate to account for potential confounders. All analyses will be done by vaccine type and/or platform or vaccination regimen on all available data, and analyses for each endpoint are outlined in Table 5. Multiple imputation may be used if there is substantial missingness. Additional analysis details will be included in a statistical analysis plan.
Table 5.
Primary, Secondary and Exploratory Objectives, Endpoints and Analyses
| Objectives | Endpoints | Analyses | |
|---|---|---|---|
| Primary | 1. Immunogenicity: To describe kinetics and durability of maternal serum antibodies following receipt of COVID-19 vaccine in individuals vaccinated during pregnancy, by vaccine type and platform. | • Geometric Mean Titer (GMT) of serum immunoglobulin G (IgG) enzyme-linked immunosorbent assay (ELISA) and neutralizing (Neut) antibodies after vaccination and up to 12 months after delivery, by vaccine type and platforma | • Geometric Mean Titers (GMTs) and 95% Confidence Intervals (CIs) will be calculated in Group 1. Plots such as reverse cumulative distributions or longitudinal presentations of GMTs will be presented. |
| 2. Immunogenicity: To describe the transplacental antibody transfer of SARS-CoV-2 antibodies among individuals vaccinated during pregnancy, overall and by vaccine type and platform. | • GMT and ratio of cord blood to maternal serum IgG ELISA and Neut antibodies overall and by vaccine type and platform. | • GMTs and ratio of cord blood to maternal serum and 95% CIs will be calculated in Group 1. | |
| 3. Immunogenicity: To describe kinetics and durability of serum SARS-CoV-2 antibodies in infants of mothers vaccinated during pregnancy, by vaccine type and platform. | • GMT of serum IgG ELISA and Neut antibodies at birth (cord blood) and at approximately 2 and 6 months of age in all infants, by vaccine type and platform. | • GMTs and 95% CIs will be calculated in Group 3. Plots such as reverse cumulative distributions or longitudinal presentations of GMTs will be presented. | |
| Secondary | 1. Safety: To describe pregnancy outcomes in individuals who receive COVID-19 vaccine during pregnancy or postpartum, and their infants, by vaccine type and platform. | • Frequency of maternal and infant outcomes vs. background rates in the US, overall and by vaccine type and platform. | • A comparison of frequencies to background rates will be reported in Groups 1–4 (no formal statistical testing). |
| 2. Immunogenicity: To evaluate immune responses and durability of antibodies in individuals who received different COVID-19 vaccines during pregnancy or postpartum compared to non-pregnant populations of women of childbearing age and to a correlate of protection (if available), by vaccine type and platform. | • GMT of serum IgG ELISA and Neut antibodies after vaccination in pregnancy or postpartum vs. mean titers achieved by non-pregnant participants in clinical trials and to a correlate of protection if available, by vaccine type and platform. | • One sample t-tests will be done in Group 1. | |
| 3. Immunogenicity: To assess the effect of gestational age at vaccination (trimester of gestation), maternal age, health and risk status, on immune responses and durability of antibodies in individuals who receive different COVID-19 vaccines during pregnancy or post-partum, by vaccine type and platform. | • GMT of serum IgG ELISA and Neut antibodies after vaccination in pregnancy by gestational age at vaccination (trimester of gestation) and interval between vaccination and delivery, by vaccine type and platform. GMT of serum IgG ELISA and Neut antibodies after vaccination in pregnancy or postpartum by maternal age, health status, and risk status (e.g., occupation, priority vaccination group) overall and by vaccine type and platform. | • GMTs and 95% CIs will be calculated for Group 1 by strata. Student’s t-tests and linear regression (controlling for potential confounders) will be used to compare strata. | |
| 4. Immunogenicity: To describe the transplacental antibody transfer of SARS-CoV-2 antibodies among individuals vaccinated during pregnancy, by gestational age at vaccination, by interval from vaccination to delivery and maternal age, health and risk status, overall and by vaccine type and platform. |
• GMT and ratio of cord blood to maternal serum IgG ELISA and Neut antibodies at delivery by gestational age at vaccination (trimester of gestation) and interval between vaccination and delivery, overall and by vaccine type and platform. • GMT and ratio of cord blood to maternal serum IgG ELISA and Neut antibodies at delivery by maternal age, health status, and risk status, overall and by vaccine type and platform. |
• GMTs and ratios of cord blood to maternal serum and 95% CIs will be presented for Group 1 by strata. Student’s t-tests and linear regression (controlling for potential confounders) will be used to compare strata. | |
| 5. Immunogenicity: To describe the kinetics of SARS-CoV-2 antibodies in breast milk of mothers who received vaccine during pregnancy or postpartum, overall and by vaccine type and platform. | • GMT of IgG and immunoglobulin A (IgA) ELISA and Neut antibodies in breast milk at approximately 2 weeks, and 2, 6, and 12 months postpartum, in individuals vaccinated during pregnancy or postpartum, overall and by vaccine type and platform. | • GMTs and 95% CIs will be calculated in Group 1. Plots such as reverse cumulative distributions or longitudinal presentations of GMTs will be presented. | |
| 6. Immunogenicity: To describe the kinetics and durability of maternal serum antibodies following receipt of COVID-19 vaccine in individuals vaccinated postpartum, by vaccine type and platform. | • Postpartum individuals: GMT of serum IgG ELISA and Neut SARS-CoV-2 antibodies pre- and/or post-vaccination, and at approximately 2, 6, and 12 months after delivery, overall, and by vaccine type and platform. | • GMTs and 95% CIs will be calculated in Group 3. Plots such as reverse cumulative distributions or longitudinal presentations of GMTs will be presented. | |
| 7. Immunogenicity: To describe the kinetics and durability of serum SARS-CoV-2 antibodies in infants of individuals vaccinated postpartum, by vaccine type and platform. | • GMT of serum IgG ELISA and Neut antibodies at approximately 2 and 6 months of age in infants of postpartum individuals, overall and by vaccine type and platform. | • GMTs and 95% CIs will be calculated in Group 4. Plots such as reverse cumulative distributions or longitudinal presentations of GMTs will be presented. | |
| Exploratory | 1. To describe the effectiveness of COVID-19 vaccines against maternal COVID-19 infection during pregnancy and postpartum. | • Incidence of laboratory confirmed COVID-19 and severity of disease during study participation assessed through passive surveillance in individuals vaccinated during pregnancy or postpartum vs. rates in unvaccinated population of women of childbearing age, overall and by vaccine type and platform. | • Incidence rates and 95% CIs will be calculated in Groups 1 and 3. |
| 2. To describe the effectiveness of maternal antibodies to provide protection against SARS-CoV-2 infection/symptomatic disease/severity in infants in the first 12 months of life. | • Incidence of laboratory confirmed COVID-19 and severity of disease during study participation assessed through passive surveillance in infants of individuals vaccinated in pregnancy or postpartum vs. background rates in infants of unvaccinated population, overall and by vaccine type and platform. | • Incidence rates and 95% CIs will be calculated in Groups 2 and 4. | |
| 3. To describe the effectiveness of breast milk antibodies to provide protection against SARS-CoV-2 infection/symptomatic disease/severity in infants in the first 12 months of life. |
• Incidence of laboratory confirmed COVID-19 and severity of disease during study participation through passive surveillance in breastfed infants vs. not breastfed infants, by vaccine type and platform. • Incidence of laboratory confirmed COVID-19 and severity of disease during study participation through passive surveillance in breastfed infants of individuals vaccinated during pregnancy vs. postpartum, overall and by vaccine type and platform. |
• Incidence rates and 95% CIs will be calculated in Groups 2 and 4. |
Abbreviations: GMT Geometric Mean Titer, IgG immunoglobulin G, ELISA enzyme-linked immunosorbent assay, Neut neutralizing, IgA immunoglobulin A
aPregnant individuals: pre- and/or post-vaccination, at delivery, and at approximately 2, 6, and 12 months postpartum
Discussion
The observational and opportunistic study design outlined in this paper will provide meaningful data within the context of the current state of the ongoing pandemic due to SARS CoV-2 in pregnant women and newborns. The favorable decision by the Centers for Disease Control and Prevention (CDC), the Food and Drug Administration (FDA), and the American College of Obstetricians and Gynecologists (ACOG) in late 2020 to adopt a permissive approach, paving the way for pregnant and breastfeeding individuals to make a personal choice to take the available mRNA vaccines, was a major step forward in the inclusion of pregnant women in vaccine implementation early in the pandemic [3, 29–32]. However, it did present the frequent and suboptimal situation of women weighing the decision to choose the intervention based on an overall paucity of data. Thus, pregnant individuals are continuing to weigh the decision to receive these vaccines under EUA in a setting of limited clinical trial data on safety and efficacy specific to this population despite the reassuring observational data that are accumulating [11, 33].
At this point in the pandemic multiple vaccines are available via EUA, and thousands of pregnant and lactating individuals are opting to take them. This fact makes prospective placebo-controlled trials in pregnant and lactating persons challenging to conduct at the present time. Many within the fields of maternal/neonatal health, reproductive infectious diseases, and biomedical ethics believe the ideal approach for COVID-19 (and future emerging infectious diseases) could have included contemporaneous enrollment of pregnant and lactating individuals into clinical sub-studies in the late summer and fall of 2020 of appropriate vaccine candidates that had cleared the mandatory animal studies known as basic Developmental and Reproductive Toxicology (DART) studies as well as early human Phase 1 and II studies [34]. It is appreciated that such an approach would have necessitated special consideration and attention early in the process of vaccine development and clinical trial planning. However, it would have undoubtedly provided much needed data to optimize provider counseling and maternal decision making for this population at high risk for adverse outcomes from COVID-19 [1, 2]. There are no compelling reasons to believe the mRNA-based non-live vaccines pose real harm to women or their unborn babies and the emerging observational registry data from the CDC also demonstrate a highly favorable risk-benefit ratio of these vaccines [9]. However, uptake (and thus disease prevention) in this high-risk population has been suboptimal, due in part to the lack of information and the ambiguity around safety in pregnancy. In absence of clear data (and thus clear recommendations) care providers are left to fill in data gaps with anecdotal and/or personal beliefs that may complicate decision making for pregnant persons. While that approach can sometimes be helpful for individual patients, on the whole it is suboptimal and leads to haphazard public health practices. We believe the current protocol format offers an appropriate approach to build on what can be currently done to inform this important data gap for healthcare providers, pregnant individuals, and their babies.
This protocol template has additional advantages for prospective consideration for the current and/or future emerging infectious diseases outbreaks. Given the long-standing and legitimate challenges of enrolling pregnant individuals into clinical trials early in the drug and vaccine development pipeline, this adaptive design can help gather useful data for pregnant individuals that are being offered interventions. These populations often suffer from a disproportionate impact from infectious diseases and having the ability to rapidly design and roll-out an opportunistic approach allows for more rapid data gathering that can inform patient and provider decision making as the epidemic unfolds. This design also serves as a template for investigating current and future global vaccine dissemination, immunogenicity, and safety in pregnancy. Such an approach becomes especially relevant with the associated global variability in vaccine availability and logistical realities affecting supply and distribution, with attention to low and middle-income countries. The protocol outlined herein is adaptable to whichever vaccine products are available in varied locations, making it an attractive way to garner global data that can feed-forward and drive prospective vaccine uptake with demonstrations of immunogenicity and safety for various vaccine platforms. For example, when booster doses of COVID-19 vaccines were recommended in the US, we amended this protocol to include a group of pregnant women receiving booster doses of vaccine. Lastly, use of the Brighton Collaboration standardized case definitions for studies conducted in pregnancy further adds to the value of this work as a template for future investigations [15].
The field of research in pregnant and lactating individuals has many real and perceived challenges. It is our collective belief and hope that this protocol design can better inform and thus drive optimal decision making for all stakeholders during the ongoing COVID-19 global pandemic and future outbreaks as well. Further, the adaptive design allows for additional of new vaccines as well as evaluation of booster doses or combination vaccines as recommendations evolve.
Trial status
This paper reflects Protocol Version 1.0, April 12, 2021 and relevant amendment for the addition of a pregnancy booster group. Recruitment began on July 6, 2021 and is expected to be completed by March 2022 (or six months after individual site activation).
Supplementary Information
Additional file 1. Infants_PostpartumICF_Munoz et al.
Additional file 2. Pregnancy_and_InfantsICF_Munoz et al.
Additional file 3. Postpartum_WomenICF_Munoz et al.
Acknowledgements
We acknowledge Denise J. Jamieson, MD, MPH of Emory University for contributions to study design, Jeannie Murray, MS of University of Maryland School of Medicine for program management and assistance with manuscript, and Wendy Buchanan, BSN, MS of the National Institutes of Health (NIH) for contributions to study design and operations.
Abbreviations
- EUA
Emergency Use Authorization
- U.S.
United States
- ICU
Intensive Care Unit
- NICU
Neonatal Intensive Care Unit
- GCP
Good Clinical Practice
- IRB
Institutional Review Board
- OHRP
Office of Human Research Protections
- FWA
Federal Wide Assurance
- IDCRC
Infectious Diseases Clinical Research Consortium
- COU
Clinical Operations Unit
- SAE
Serious Adverse Event
- AESI
Adverse Events of Special Interest
- PCR
Polymerase Chain Reaction
- IgG
Immunoglobulin G
- IgA
Immunoglobulin A
- PBMC
Peripheral Blood Mononuclear Cells
- CDC
Centers for Disease Control and Prevention
- FDA
Food and Drug Administration
- ACOG
American College of Obstetricians and Gynecologists
- DART
Development and Reproductive Toxicology
Authors’ contributions
FMM, RHB, CMP, BAR, HYC, KB, JC, CC, ED, RWF, MM, JMP, JS, AM, KMN contributed to study design and have read and approved the final manuscript.
Funding
This work is supported by the IDCRC through the National Institute of Allergy and Infectious Diseases (NIAID), part of the NIH, under award number UM1AI148684. This protocol went through the review process associated with these networks, including IDCRC and NIH review. The sponsor contact is Jordan A. Kindbom, Jordan.kindbom@nih.gov. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. NIAID participated in protocol design.
Availability of data and materials
Data collected for the study will be made available to others as a de-identified patient data set after finalization of clinical study report at the discretion of the IDCRC. Analyses of data, including data from staged analyses, will be available for presentation at scientific meetings and publication to inform the scientific community. If preliminary analyses are considered of public health importance or relevant to inform research, development, and implementation of SARS-CoV-2 vaccine in pregnancy, results may be shared with public health officials and partners to inform the global scientific community. The study will be conducted in accordance with the NIH Public Access Policy publication and data sharing policies and regulations. To request study data once complete, contact Flor M. Munoz, florm@bcm.edu.
Declarations
Ethics approval and consent to participate
Ethical approval of this protocol was received on May 28, 2021 by Vanderbilt University Medicine Center IRB, a single IRB as part of an NIH-funded consortium, IDCRC. Written informed consent will be obtained from each participant.
Consent for publication
Not applicable.
Competing interests
F.M.M. is an investigator of pediatric studies of COVID-19 vaccines for Pfizer and Moderna, and for a pediatric remdesivir study conducted by Gilead Sciences, Inc.; serves as investigator on projects supported by an NIH contract for a Vaccine Treatment and Evaluation Unit (VTEU), serves as member of the Data Safety monitoring Board (DSMB) for clinical trials conducted by Pfizer, Moderna, Meissa Vaccines, Virometix, and the NIH; and is a member of the American Academy of Pediatrics Committee of Infectious Diseases (COID_, the Immunization Expert Group of the American College of Obstetrics and Gynecology (ACOG), and Co-Chair of the COVAX Maternal Immunization Working Group.
K.M.N. is a member of the World Health Organization (WHO) Strategic Advisory Group of Experts on Immunization, serves as co-investigator on an NIH contract for a Vaccine Treatment and Evaluation Unit (VTEU), serves as Co-chair of the NIH COVID Prevention Network (CoVPN), and served as an investigator for Phase I/II Pfizer COVID-19 vaccine grant, with a grant to the institution, but no salary support.
B.R. currently holds a position on the Data and Safety Monitoring Board (DSMB) for clinical trials at Gilead Sciences, Inc.
All authors have completed relevant conflicts of interest in the Disclosure of Potential Conflicts of Interest section of the Authorship Form.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Flor M. Munoz, Email: florm@bcm.edu
Cristina Cardemil, Email: cristina.cardemil@nih.gov.
References
- 1.Ellington S, Strid P, Tong VT, et al. Characteristics of women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status - United States, January 22-June 7, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:769–775. doi: 10.15585/mmwr.mm6925a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zambrano LD, Ellington S, Strid P, et al. Update: characteristics of symptomatic women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status- United States, January 22-October 3, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(44):1641–1647. doi: 10.15585/mmwr.mm6944e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dooling K, Marin M, Wallace M, et al. The advisory committee on immunization practices’ updated interim recommendation for allocation of COVID-19 vaccine — United States, December 2020. MMWR Morb Mortal Wkly Rep. 2021;69(5152):1657–1660. doi: 10.15585/mmwr.mm695152e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Villar J, Ariff S, Gunier R, et al. Maternal and neonatal morbidity and mortality among pregnant women with and without COVID-19 infection: the INTERCOVID multinational cohort study [published online April 22, 2021]. JAMA Pediatr. 10.1001/jamapediatrics.2021.1050. [DOI] [PMC free article] [PubMed]
- 5.Lokken EM, Taylor GG, Huebner EM, et al. Higher severe acute respiratory syndrome coronavirus 2 infection rate in pregnant patients [published online February 16, 2021]. Am J Obstet Gynecol. 10.1016/j.ajog.2021.02.011. [DOI] [PMC free article] [PubMed]
- 6.Knight M, Bunch K, Vousden N, et al. Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: national population based cohort study. BMJ. 2020;369:m2107. doi: 10.1136/bmj.m2107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hantoushzadeh S, Shamshirsaz AA, Aleyasin A, et al. Maternal death due to COVID-19. Am J Obstet Gynecol. 2020;223(1):109.e101–109.e116. doi: 10.1016/j.ajog.2020.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Metz TD. LB02 maternal and neonatal outcomes of pregnant patients with coronavirus disease 2019 (COVID-19): a multistate cohort. Am J Obstet Gynecol. 2021;224(2):S722–S723. doi: 10.1016/j.ajog.2020.12.1204. [DOI] [Google Scholar]
- 9.Mirbyek M, Saghazadeh A, Rezael N. A systematic review of pregnant women with COVID-19 and their neonates [Epub ahead of print]. Arch Gynecol Obstet. 2021;304(1):5–38. [DOI] [PMC free article] [PubMed]
- 10.Study to Evaluate the Safety, Tolerability, and Immunogencity of SARS-CoV-2 RNA Vaccine Candidate (BNT162b2) Against COVID-19 in Healthy Pregnant Women 18 Years of Age and Older. ClinicalTrials.gov identifier: NCT04754594. Updated April 14, 2021. https://clinicaltrials.gov/ct2/show/NCT04754594. Accessed 12 May 2021.
- 11.Shimabukuro TT, Kim SY, Myers TR, et al. Preliminary findings of mRNA Covid-19 vaccine safety in pregnant persons [published online April 21, 2021]. N Engl J Med. 10.1056/NEJMoa2104983. [DOI] [PMC free article] [PubMed]
- 12.Rasmussen SA, Jamieson DJ. Pregnancy, postpartum care and COVID-19 vaccination in 2021. JAMA. 2021;325(11):1099–1100. doi: 10.1001/jama.2021.1683. [DOI] [PubMed] [Google Scholar]
- 13.Collier A-rY, McMahan K, Yu J, et al. Immunogenicity of COVID-19 mRNA vaccines in pregnant and lactating women [published online may 13, 2021]. JAMA. 10.1001/jama.2021.7563. [DOI] [PMC free article] [PubMed]
- 14.Perl SH, Uzan-Yulzari A, Klainer H, et al. SARS-CoV-2–specific antibodies in breast Milk after COVID-19 vaccination of breastfeeding women. JAMA. 2021;325(19):2013–2014. doi: 10.1001/jama.2021.5782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jones CE, Munoz FM, Kochhar S, et al. Guidance for the collection of case report form variables to assess safety in clinical trials of vaccines in pregnancy. Vaccine. 2016;34:6007–6014. doi: 10.1016/j.vaccine.2016.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johnson M, Wagstaffe HR, Gilmour KC, et al. Evaluation of a novel multiplexed assay for determining IgG levels and functional activity to SARS-CoV-2. J Clin Virol. 2020;130:104572. doi: 10.1016/j.jcv.2020.104572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vanderheiden A, Edara VV, Floyd K, et al. Development of a rapid focus reduction neutralization test assay for measuring SARS-CoV-2 neutralizing antibodies. Curr Protoc Immunol. 2020;131(1):e116. doi: 10.1002/cpim.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Crawford KHD, et al. Protocol and reagents for Pseudotyping lentiviral particles with SARS-CoV-2 spike protein for neutralization assays. Viruses. 2020;12(5):513. doi: 10.3390/v12050513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Atyeo C, DeRiso EA, Davis C, et al. COVID-19 mRNA vaccines drive differential Fc-functional profiles in pregnant, lactating, and non-pregnant women [Preprint April 5, 2021]. bioRxiv. 10.1101/2021.04.04.438404. [DOI] [PMC free article] [PubMed]
- 20.Atyeo C, Pullen KM, Bordt EA, et al. Compromised SARS-CoV-2-specific placental antibody transfer. Cell. 2021;184(3):628–642.e10. doi: 10.1016/j.cell.2020.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aghaeepour N, Ganio EA, Mcilwain D, et al. An immune clock of human pregnancy. Sci Immunol. 2017;2(15):eaan2946. doi: 10.1126/sciimmunol.aan2946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nguyen-Contant P, Embong AK, Kanagaiah P, et al. S Protein-Reactive IgG and Memory B Cell Production after Human SARS-CoV-2 Infection Includes Broad Reactivity to the S2 Subunit. mBio. 2020;11(5):e01991–e01920. doi: 10.1128/mBio.01991-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nguyen-Contant P, Embong AK, Topham DJ, Sangster MY. Analysis of antigen-specific human memory B cell populations based on in vitro polyclonal stimulation. Curr Protoc Immunol. 2020;131(1):e109. doi: 10.1002/cpim.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Amanat F, Thapa M, Lei T, et al. The plasmablast response to SARS-CoV-2 mRNA vaccination is dominated by non-neutralizing antibodies that target both the NTD and the RBD [Preprint March 9, 2021]. medRxiv. 10.1101/2021.03.07.21253098.
- 25.Sadoff J, Gray G, Vandebosch A, et al. Safety and efficacy of single-dose Ad26.COV2.S vaccine against Covid-19 [Epub ahead of print April 21, 2021]. N Engl J Med. 10.1056/NEJMoa2101544. [DOI] [PubMed]
- 26.U.S. Food and Drug Administration. Pfizer-Biontech COVID-19 Vaccine (BNT162, PF-07302048), Vaccines and Related Biological Products Advisory Committee Briefing Document, Meeting Date: 10 December 2020. https://www.fda.gov/media/144246/download. Accessed on 8 June 2021.
- 27.Sadoff J, Le Gars M, Shukarev G, et al. Interim results of a phase 1-2a trial of Ad26.COV2.S Covid-19 vaccine. N Engl J Med. 2021. 10.1056/NEJMoa2034201 NEJMoa2034201. [DOI] [PMC free article] [PubMed]
- 28.Jackson LA, Anderson EJ, Rouphael NG, et al. An mRNA vaccine against SARS-CoV-2 - preliminary report. N Engl J Med. 2020;383(20):1920–1931. doi: 10.1056/NEJMoa2022483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wallace M, Woodworth KR, Gargano JW, et al. The advisory committee on immunization practices’ interim recommendation for use of Pfizer-BioNTech COVID-19 vaccine in adolescents aged 12–15 years — United States, may 2021. MMWR Morb Mortal Wkly Rep May 2021;70(20);749–752. 10.15585/mmwr.mm7020e1. [DOI] [PMC free article] [PubMed]
- 30.MacNeil JR, Su JR, Broder KR, et al. Updated recommendations from the advisory committee on immunization practices for use of Janssen (Johnson & Johnson) COVID-19 vaccine after reports of thrombosis with thrombocytopenia syndrome among vaccine recipients -United States, April 2021. MMWR Morb Mortal Wkly Rep. 2021;70:651–656. doi: 10.15585/mmwr.mm7017e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Oliver SE, Gargano JW, Scobie H, et al. The advisory committee on immunization practices’ interim recommendation for use of Janssen COVID-19 vaccine- United States, February 2021. MMWR Morb Mortal Wkly Rep. 2021;70:329–332. doi: 10.15585/mmwr.mm7009e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.The American College of Obstetricians and Gynecologists. Vaccinating Pregnant and Lactating Patients Against COVID-19, Practice Advisory. https://www.acog.org/en/clinical/clinical-guidance/practice-advisory/articles/2020/12/vaccinating-Pregnant-and-Lactating-Patients-Against-COVID-19. Accessed 19 Apr 2021.
- 33.Centers for Disease Control and Prevention. V-Safe After Vaccination Health Checker. https://www.cdc.gov/coronavirus/2019-ncov/caccines/safety/vsafe.html. Updated May 21, 2021. Accessed on 8 June 2021.
- 34.Beigi RH, Krubiner C, Jamieson DJ, et al. The need for inclusion of pregnant women in COVID-19 vaccine trials. Vaccine. 2021;39(6):868–870. doi: 10.1016/j.vaccine.2020.12.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Infants_PostpartumICF_Munoz et al.
Additional file 2. Pregnancy_and_InfantsICF_Munoz et al.
Additional file 3. Postpartum_WomenICF_Munoz et al.
Data Availability Statement
Data collected for the study will be made available to others as a de-identified patient data set after finalization of clinical study report at the discretion of the IDCRC. Analyses of data, including data from staged analyses, will be available for presentation at scientific meetings and publication to inform the scientific community. If preliminary analyses are considered of public health importance or relevant to inform research, development, and implementation of SARS-CoV-2 vaccine in pregnancy, results may be shared with public health officials and partners to inform the global scientific community. The study will be conducted in accordance with the NIH Public Access Policy publication and data sharing policies and regulations. To request study data once complete, contact Flor M. Munoz, florm@bcm.edu.