Abstract
Objective
The study objective was to assess sociodemographic disparities in telehealth use among patients in an urban adult rheumatology clinic during the coronavirus disease 2019 (COVID‐19) pandemic.
Methods
In this retrospective cohort study, patient‐level sociodemographic data associated with all rheumatology visits in the following two periods were reviewed: pre‐COVID‐19 (March 1, 2019 to February 28, 2020) and COVID‐19 (April 1, 2020 to March 31, 2021). Data were extracted from the electronic health record. Multivariable logistic regression analyses were performed to determine sociodemographic factors associated with video visits during the COVID‐19 period.
Results
In the pre‐COVID‐19 period, 1503 patients completed 3837 visits (100% in person). In the COVID‐19 period, 1442 patients completed 3406 visits: 41% in person, 30% video, and 29% telephone only. Several factors were associated with decreased video use: preference for Spanish language (adjusted odds ratio [aOR] 0.27, 95% confidence interval [CI] 0.15‐0.47) or other non‐English languages (aOR 0.34, 95% CI 0.21‐0.55), Black or African American race/ethnicity (aOR 0.50, 95% CI 0.35‐0.73), Medicaid payer, and increasing age.
Conclusion
Decreased video visit use among rheumatology patients was associated with non‐English language preference, minority race/ethnicity, increasing age, and indicators of low income. Rapid deployment and expansion of telehealth during the COVID‐19 pandemic likely has improved access for some but widened preexisting disparities for others. As medical care evolves toward ongoing digital care delivery, clarifying and addressing causes of telehealth disparities is essential for delivering equitable health care.
Significance & Innovations.
Little is known about telehealth disparities in adult ambulatory rheumatology care.
In our cohort, we observed socioeconomic disparities in video visit use that may reflect widespread digital care inequities in the United States.
In the wake of the coronavirus disease 2019 pandemic, digital care disparities are likely to persist or widen unless their underlying causes are identified and addressed.
INTRODUCTION
The coronavirus disease 2019 (COVID‐19) pandemic forced major changes in ambulatory care delivery around the world, including the expansion of telehealth services (1). Prior to the pandemic, compensation for synchronous telehealth visits by telephone or video in the United States was restricted by Centers for Medicare & Medicaid Services (CMS) regulations to select patients. In response to national lockdown orders and other emergency measures, CMS relaxed restrictions on telehealth to make it easier for most patients to receive care while minimizing their risk of coronavirus exposure. Telehealth opportunities have increased markedly, with 64% of CMS beneficiaries in one survey reporting telehealth access in late 2020 compared with just 18% prior to the pandemic (2). Video visits are thought to be more advantageous than phone‐only visits because they allow for nonverbal communication, visual examination, and sharing of images and documents. A recent observational study (3) of ambulatory rheumatology care for patients with rheumatoid arthritis demonstrated that video plus in‐person visits could deliver similar quality care as in‐person visits alone. During the COVID‐19 pandemic, asynchronous telehealth services, such as patient portals (PPs), have allowed select patients, usually at no additional cost, to communicate securely with their care teams, request medication refills, and schedule appointments.
Outside of rheumatology, disparities in telehealth are well documented, with lower rates of access or use among people who are Black, Latinx, older, or poor (2, 4, 5, 6, 7, 8). In addition, non‐English language preference has been associated with lower telehealth use in several US‐based studies (9, 10, 11). Similar disparities have been described for PP access and use (12, 13, 14). Given the unprecedented telehealth expansion during the COVID‐19 pandemic, there is concern that these disparities have widened and that new disparities have been created (8). A recent analysis (15) of a multistate, community‐based network of rheumatology clinics during the COVID‐19 pandemic demonstrated that patients with lower socioeconomic status or those who were older were less likely to use telehealth services to offset pandemic‐related cancellation of in‐person clinic visits. However, little is known about racial, ethnic, and language‐based disparities in telehealth and PP use among rheumatology patients in the United States.
We sought to investigate telehealth disparities in a county hospital rheumatology clinic that serves a sociodemographically diverse population centered in Seattle, Washington. The aim of our study was to examine patient sociodemographic features associated with completed video visits in order to identify inequities in telehealth use during the COVID‐19 pandemic. Secondarily, we aimed to evaluate disparities in PP use in the same population. To our knowledge, ours is the first study to focus on disparities in video visit and PP use in rheumatology.
PATIENTS AND METHODS
Study site
Patient‐level data were acquired from a single county hospital that serves a sociodemographically diverse population in and around Seattle, Washington. Before April 1, 2020, the hospital's adult rheumatology clinic offered only in‐person visits with providers. Beginning in April 2020, in response to the COVID‐19 pandemic, all hospital clinics began offering video and phone visits in addition to traditional in‐person visits. Professional language interpretation in the patient's preferred non‐English language was available for all visit types during the entire study period. For video visits, interpreters were video based. For phone visits, interpreters were phone based. For in‐person visits, interpreters were either in person or phone based, depending on interpreter availability. Interpreters were engaged at all visits for patients indicating non‐English language preference; however, patients and families could decline interpreter services and still complete the visit. Video visits required a smartphone or computer and broadband internet service. During the entire study period, including the COVID‐19 pandemic, all patients completing in‐person or video visits were offered in‐visit assistance in registering for the PP. Assistance consisted of helping patients register using their own devices (during video visits or in‐person visits) or using hospital computers (in‐person visits). There was no specific effort to increase PP registration during the pandemic. The PP interface is English language only, and registration requires a completed visit within our health care system, a computer or smartphone, internet service, and an email address.
Data capture and cohort identification
Using the electronic health record, we extracted sociodemographic data for all patients completing at least one visit at our hospital's rheumatology clinic between March 1, 2019, and March 31, 2021. Patient‐level data from the following two cohorts or periods were collected: 1) a pre‐COVID‐19 period (visits between March 1, 2019, and February 28, 2020) and 2) a COVID‐19 period (visits between April 1, 2020, and March 31, 2021). Completed visits were determined by billing codes. These dates were based on when statewide shelter‐in‐place orders were issued (March 2020) and when video visits were first made available to all clinic patients (April 2020). During the COVID‐19 period, all patients were called by telephone (with the aid of language interpreters, if needed) to schedule or reschedule phone, video, or in‐person visits based on patient preference, provider recommendations, and clinic in‐person capacity, which was limited due to safety requirements. However, all visit types remained available to all patients in all months during the COVID‐19 period. All patients scheduled for a visit of any type received reminder phone calls, and technical assistance was made available on the day of visit via telephone (all languages) and via text messaging (English only). In addition, patients could use the PP to receive technical assistance (English language only). Neither PP registration nor login was required to schedule or complete a video visit.
Sociodemographic and clinical data
Patient sociodemographic features associated with the first completed visit in the period of interest were used. Age was categorized to detect differences in Medicare‐eligible and older patients, who have been found to be less likely to use video visits (2, 5, 6, 7, 8). Distance from the hospital was derived from ZIP codes and rounded down to the nearest integer. Distance categories were chosen to differentiate local patients less than 10 miles from the hospital, patients living in surrounding neighborhoods (10‐24 miles), those within the Puget Sound region (25‐49 miles), patients throughout the state (50‐99 miles), or patients potentially out of state (≥100 miles). Race, ethnicity, and language preference were self‐identified. Race categories were White, American Indian or Alaska Native, Asian, Black or African American, Native Hawaiian or other Pacific Islander, and Missing (unknown or did not answer). Ethnicity categories were Hispanic or Latino, Not Hispanic or Latino, and Missing (unknown or did not answer). Hereafter, “Hispanic or Latino” is referred to as Latinx. In order to better understand the relationships between Latinx identity and video use, we combined race and ethnicity into a single variable (race/ethnicity) with the following categories: White (non‐Latinx), American Indian or Alaska Native (non‐Latinx), Black or African American (non‐Latinx), Native Hawaiian or other Pacific Islander (non‐Latinx), Latinx, and Missing (missing for both race and ethnicity). Medical insurance payer groups were defined as commercial (includes Blue Shield), self‐pay (includes charity care), Medicaid (includes those applying for Medicaid), Medicare (includes MedAdvantage plans), and other (includes Department of Labor and Industries and pharmacy benefit visits). Established patients were defined as those with more than or equal to three completed visits during the pre‐COVID‐19 period. To better assess the relationships between race/ethnicity and language preference, we analyzed language preference according to race/ethnicity. We did not have access to data on patient diagnoses or medication use. Finally, because many patients relied on PP during the COVID‐19 pandemic and the PP platform was English language only, we also collected data on PP login for all patients.
Primary outcome identification
The primary outcome was completion of at least one video visit during the COVID‐19 period (April 1, 2020, to March 31, 2021). Analysis was restricted to completed visits as determined by billing codes; therefore, data regarding no‐show and cancelled visits were not collected. Visits with all rheumatology providers were included. Completed video visits required the establishment of simultaneous audio and video connection. Scheduled video visits when only phone connection was established were coded as phone visits.
Patient Portal (PP) use
We collected data on PP use for patients completing visits during the COVID‐19 period because it was observed to be an important mode of care for many patients, PP use requires some of the same resources and services as video visits, and we anticipated language‐based disparities in its use. Only the most recent PP login date for each patient was available. Therefore, in order to maximize sensitivity in detecting disparities in PP use, we defined PP use as any recorded login, even those outside the COVID‐19 period. Registration for PP alone did not constitute PP use.
Statistical analyses
Frequencies were used to describe the cohort. Univariable and multivariable logistic regression analyses were used to identify associations with the primary outcome. All testing was two‐tailed, with P < 0.05 designated as statistically significant. Variables with P < 0.05 on univariable analysis were included in multivariable logistic regression models. Fisher's exact tests and the χ2 tests were performed using Prism v.5 (GraphPad); logistic regression analyses were performed using SPSS Statistics v.27 (IBM Corporation). Because PP use was observed to have a strong association with our primary outcome, we excluded it from the model. To evaluate factors associated with PP use, a secondary analysis using similar univariable and multivariable analyses was performed. To look for important interactions between race/ethnicity and language, we created a race/ethnicity × language (English or non‐English) interaction term and included it in separate multivariable analyses of video and PP use.
Research approvals
The University of Washington Human Subjects Division has determined that this study does not involve human subjects as defined by federal regulations and does not require exempt status or institutional review board review.
RESULTS
In the pre‐COVID‐19 period, a total of 1503 patients completed 3837 visits; all except one (phone) visit were coded as in‐person visits (Figure 1). In the COVID‐19 period, a total of 1442 patients completed 3406 visits, of which 1382 (41%) were in‐person visits, 1036 (30%) video visits, and 988 (29%) phone visits. A total of 864 patients completed at least one visit in both the pre‐COVID‐19 and COVID‐19 periods (Supplementary Table 1). The sociodemographic features of pre‐COVID‐19 and COVID‐19 groups were similar (Table 1). The COVID‐19 cohort was predominantly female, with the majority of patients being aged 55 years or younger. More than half of patients self‐identified as non‐White, and one third preferred a non‐English language. Less than one third of patients had commercial insurance.
Figure 1.
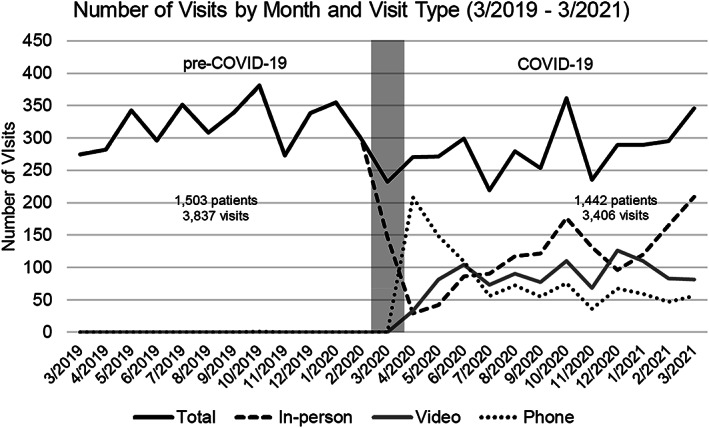
Number of completed visits by type per month in the pre‐COVID‐19 and COVID‐19 periods. The month of March 2020 (shaded) was excluded from analysis. No video visits were completed in the pre‐COVID‐19 period. ‐COVID‐19, coronavirus disease 2019.
Table 1.
Sociodemographic features and visit type use for patients during pre‐COVID‐19 (March 2019‐Feburary 2020) and COVID‐19 (April 2020‐March 2021) periods
| Patients, pre‐COVID‐19 period (n = 1503) | Patients, COVID‐19 period (n = 1442) | |
|---|---|---|
| n (%) | n (%) | |
| Age, years | ||
| <55 | 843 (56.1) | 850 (58.9) |
| 55‐64 | 363 (24.2) | 310 (21.5) |
| 65‐74 | 216 (14.4) | 193 (13.4) |
| ≥75 | 81 (5.4) | 89 (6.2) |
| Sex | ||
| Female | 1011 (67.3) | 968 (67.1) |
| Male | 491 (32.7) | 473 (32.8) |
| Distance from hospital, miles | ||
| <10 | 596 (39.7) | 606 (42.0) |
| 10‐24 | 498 (33.1) | 485 (33.6) |
| 25‐49 | 200 (13.3) | 172 (11.9) |
| 50‐99 | 98 (6.5) | 86 (6.0) |
| ≥100 | 111 (7.4) | 92 (6.4) |
| Race/ethnicity | ||
| White | 692 (46.0) | 635 (44.0) |
| American Indian or Alaska Native | 27 (1.8) | 28 (1.9) |
| Asian | 182 (12.1) | 164 (11.4) |
| Black or African American | 234 (15.6) | 215 (14.9) |
| Native Hawaiian or other Pacific Islander | 21 (1.4) | 26 (1.8) |
| Latinx | 232 (15.4) | 242 (16.8) |
| Missing | 115 (7.7) | 132 (9.2) |
| Language | ||
| English | 1187 (79.0) | 1121 (77.7) |
| Spanish | 160 (10.6) | 174 (12.1) |
| Non‐English/non‐Spanish a | 156 (10.4) | 147 (10.2) |
| Payer | ||
| Commercial | 439 (29.2) | 423 (29.3) |
| Self‐pay | 59 (3.9) | 77 (5.3) |
| Medicaid | 354 (23.6) | 340 (23.6) |
| Medicare | 336 (22.4) | 285 (19.8) |
| Other | 315 (21.0) | 314 (22.0) |
| Patient portal login | ||
| No | 533 (35.5) | 455 (31.6) |
| Yes | 970 (64.5) | 987 (68.4) |
| Established patient b | ||
| No | 922 (61.3) | 956 (66.3) |
| Yes | 581 (38.7) | 486 (33.7) |
| Visits | ||
| In person | 3836 (100) | 1382 (40.6) |
| Telemedicine | 0 (0) | 1036 (30.4) |
| Phone | 1 (0) | 988 (29.0) |
Abbreviation: COVID‐19, coronavirus disease 2019.
Most frequent non‐English/non‐Spanish languages, in descending order: Vietnamese, Amharic, Cambodian, Cantonese, Somali, Panjabi (Punjabi), Arabic, Tagalog, Farsi (Persian), Russian, and Tigrinya.
Established patient: any patient completing three or more visits during the pre‐COVID‐19 period.
We also compared features of pre‐COVID patients completing at least one visit versus no visit in the COVID‐19 period (Supplementary Table 1). More likely to have completed a visit in the COVID‐19 period were those who had a PP login (odds ratio [OR] 1.43, 95% confidence interval [CI] 1.16‐1.77), were established (OR 7.36, 95% CI 5.70‐9.51), identified as Native Hawaiian or other Pacific Islander (OR 3.55, 95% CI 1.18‐10.66) or Latinx (OR 1.62, 95% CI 1.19‐2.21), preferred Spanish language (OR 1.48, 95% CI 1.05‐2.10), or had self‐pay insurance (OR 2.21, 95% CI 1.23‐3.96). Patients older than the age of 75 were less likely to have completed a visit in the post‐COVID‐19 period (OR 0.60, 95% CI 0.38‐0.95).
Sociodemographic features of video users (n = 598) and nonusers (n = 844) during the COVID‐19 period are shown in Table 2. For the 598 patients completing more than or equal to one video visit, 64% of total visits were video, 15% were phone, and 21% were in person; for the 844 patients without a video visit, 42% of visits were phone and 58% were in person (data not shown). Compared with patients aged less than 55 years, older age groups were less likely to use video, with patients aged 65 to 74 showing the greatest difference (OR 0.37, 95% CI 0.26‐0.52). Male patients were less likely than female patients to use video (OR 0.72, 95 CI 0.57‐0.90). Compared with patients listing addresses less than 10 miles from the hospital, those listing more distant addresses were more likely to use video, the difference being greatest for those living 50 to 99 miles away (OR 2.38, 95% CI 1.51‐3.76). Established patients did not have an increased odds of video visit use compared with unestablished patients. PP use was associated with the highest odds of video use (OR 6.20, 95% CI 4.67‐8.22). Compared with White patients, Asian (OR 0.52, 95% CI 0.36‐0.75), Black or African American (OR 0.36, 95% CI 0.26‐0.51), and Latinx (OR 0.40, 95% CI 0.29‐0.55) patients were less likely to use video visits. Compared with those preferring English, those preferring Spanish (OR 0.27, 95% CI 0.19‐0.40) or other non‐English (OR 0.23, 95% CI 0.15‐0.44) languages were far less likely to use video. Compared with commercially insured patients, those with other types of coverage were less likely to use video, with self‐pay showing the biggest difference (OR 0.25, 95% CI 0.14‐0.44).
Table 2.
Sociodemographic features of video users and non‐users during the COVID‐19 period (April 2020‐March 2021)
| ≥1 video visit (n = 598) | No video visit (n = 844) | Odds ratio | P value a | |
|---|---|---|---|---|
| n (%) | n (%) | (95% CI) | ||
| Age (years) | ||||
| <55 | 427 (71.4) | 423 (50.1) | Reference | N/A |
| 55‐64 | 92 (15.4) | 218 (25.8) | 0.42 (0.32‐0.55) | <0.001 |
| 65‐74 | 52 (8.7) | 141 (16.7) | 0.37 (0.26‐0.52) | <0.001 |
| ≥75 | 27 (4.5) | 62 (7.3) | 0.43 (0.27‐0.69) | <0.001 |
| Sex | ||||
| Female | 427 (71.4) | 541 (64.1) | Reference | N/A |
| Male | 171 (28.6) | 302 (35.8) | 0.72 (0.57‐0.90) | 0.004 |
| Distance from hospital (miles) | ||||
| <10 | 210 (35.1) | 396 (46.9) | Reference | N/A |
| 10‐24 | 203 (33.9) | 282 (33.4) | 1.36 (1.06‐1.74) | 0.017 |
| 25‐49 | 90 (15.1) | 82 (9.7) | 2.07 (1.47‐2.92) | <0.001 |
| 50‐99 | 48 (8.0) | 38 (4.5) | 2.38 (1.51‐3.76) | <0.001 |
| ≥100 | 47 (7.9) | 45 (5.3) | 1.97 (1.27‐3.06) | 0.004 |
| Established patient b | ||||
| No | 395 (66.1) | 561 (66.5) | Reference | N/A |
| Yes | 203 (33.9) | 283 (33.5) | 1.02 (0.82‐1.27) | 0.910 |
| Patient portal login | ||||
| No | 71 (11.9) | 384 (45.5) | Reference | N/A |
| Yes | 527 (88.1) | 460 (54.5) | 6.20 (4.67‐8.22) | <0.001 |
| Race/ethnicity | ||||
| White | 321 (53.7) | 314 (27.2) | Reference | N/A |
| American Indian or Alaska Native | 10 (1.7) | 21 (2.5) | 0.47 (0.22‐1.00) | 0.064 |
| Asian | 56 (9.4) | 105 (12.4) | 0.52 (0.36‐0.75) | <0.001 |
| Black or African American | 58 (9.7) | 157 (18.6) | 0.36 (0.26‐0.51) | <0.001 |
| Native Hawaiian or other Pacific Islander | 16 (2.7) | 10 (1.2) | 1.57 (0.70‐3.50) | 0.320 |
| Latinx | 70 (11.7) | 172 (20.4) | 0.40 (0.29‐0.55) | <0.001 |
| Missing | 67 (11.2) | 65 (7.7) | 1.00 (0.69‐1.47) | 1.000 |
| Language | ||||
| English | 537 (89.8) | 584 (69.2) | Reference | N/A |
| Spanish | 35 (5.9) | 139 (16.5) | 0.27 (0.19‐0.40) | <0.001 |
| Non‐English/non‐Spanish | 26 (4.3) | 121 (14.3) | 0.23 (0.15‐0.36) | <0.001 |
| Payer | ||||
| Commercial | 225 (37.6) | 198 (23.5) | ||
| Self‐pay | 17 (2.8) | 60 (7.1) | 0.25 (0.14‐0.44) | <0.001 |
| Medicaid | 120 (20.1) | 220 (26.1) | 0.48 (0.36‐0.64) | <0.001 |
| Medicare | 87 (14.5) | 198 (23.5) | 0.39 (0.28‐0.53) | <0.001 |
| Other | 149 (24.9) | 168 (19.9) | 0.78 (0.58‐1.05) | 0.1024 |
Abbreviations: CI, confidence interval; COVID, coronavirus disease 2019; N/A, not applicable.
Fisher's exact test, two‐sided.
Established patient: any patient completing three or more visits during the pre‐COVID period's exact test, two‐sided.
We assessed language preference among the various race/ethnicity groups (Supplementary Table 2). Twenty‐two percent of all patients in COVID‐19 period preferred a non‐English language. Forty‐four percent of Asian patients preferred a non‐English or non‐Spanish language, whereas 66% of Latinx patients preferred non‐English languages, almost exclusively Spanish. Seventeen percent of Black or African American patients preferred a non‐English language. White and American Indian or Alaska Native patients largely preferred English.
Primary model: evaluating factors associated with video visit use
Multivariable logistic regression results are summarized in Table 3. We found that decreased video use was associated with increasing age, male sex, and increasing distance from the hospital. American Indian or Alaska Native patients were less likely than White patients to use video (adjusted OR [aOR] 0.55, 95% CI 0.15‐0.94). Black or African American patients also were less likely than White patients to use video (aOR 0.50, 95% CI 0.35‐0.73). Compared with patients who preferred English, those preferring Spanish or other non‐English languages were less likely to use video visits (aOR 0.27, 95% CI 0.15‐0.47 and aOR 0.32, 95% CI 0.19‐0.53, respectively). Compared with commercial payer, only Medicaid showed reduced video use (aOR 0.61, 95% CI 0.44‐0.82). Inclusion of a race/ethnicity × language (English or non‐English) interaction term in the model revealed no significant interactions with video use (data not shown). Lower video use among non‐English‐preferring patients was accompanied by higher in‐person visit use (Supplementary Figure 1).
Table 3.
Sociodemographic features associated with video use during COVID‐19 (April 2020‐March 2021)
| Not including patient portal login | ||
|---|---|---|
| aOR (95% CI) | P value a | |
| Age, years (vs <55) | ||
| 55‐64 | 0.42 (0.31‐0.56) | <0.001 |
| 65‐74 | 0.43 (0.28‐0.65) | <0.001 |
| ≥75 | 0.54 (0.31‐0.95) | 0.032 |
| Sex (vs female) | ||
| Male | 0.69 (0.54‐0.89) | 0.003 |
| Distance from hospital, miles (vs <10) | ||
| 10‐24 | 1.45 (1.11‐1.90) | 0.007 |
| 25‐49 | 1.77 (1.23‐2.57) | 0.002 |
| 50‐99 | 1.92 (1.17‐3.14) | 0.009 |
| ≥100 | 1.58 (0.98‐2.54) | 0.059 |
| Race/ethnicity (vs White) | ||
| American Indian or Alaska Native | 0.55 (0.15‐0.94) | 0.036 |
| Asian | 0.82 (0.57‐1.33) | 0.525 |
| Black or African American | 0.50 (0.35‐0.73) | <0.001 |
| Native Hawaiian or other Pacific Islander | 1.48 (0.64‐3.43) | 0.365 |
| Latinx | 0.80 (0.51‐1.27) | 0.344 |
| Missing | 1.11 (0.74‐1.67) | 0.608 |
| Language (vs English) | ||
| Spanish | 0.27 (0.15‐0.47) | <0.001 |
| Non‐English/non‐Spanish | 0.32 (0.19‐0.53) | <0.001 |
| Payer (vs commercial) | ||
| Self‐pay | 0.61 (0.31‐1.18) | 0.142 |
| Medicaid | 0.60 (0.43‐0.82) | 0.002 |
| Medicare | 0.70 (0.47‐1.04) | 0.075 |
| Other | 0.99 (0.72‐1.36) | 0.957 |
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval; COVID‐19, coronavirus disease 2019.
Logistic regression analysis; all variables included in analysis are shown.
Secondary analysis: evaluating factors associated with PP use
Socioeconomic features of PP users (n = 987) and nonusers (n = 455) are shown in Table 4. Similar to video use, PP use was lower in older age groups and men. Compared with patients living within 10 miles of the hospital, those living in the 50‐ to 99‐mile range were more likely to use PP (OR 2.37, 95% CI 1.34‐4.19). Established patients were less likely than unestablished patients to use PP (OR 0.77, 95% CI 0.61‐0.97). Compared with White patients, those of all other racial/ethnic categories except Native Hawaiian or other Pacific Islander were much less likely to use PP; the lowest OR was for Latinx patients (OR 0.12, 95% CI 0.09‐0.17). Compared with English speakers, Spanish speakers (OR 0.07, 95% CI 0.05‐0.11) and non‐English and non‐Spanish speakers (OR 0.19, 95% CI 0.13‐0.28) were far less likely to use PP. Compared with commercial payer, patients of all other payer groups were less likely to use PP, the lowest OR being for self‐pay (OR 0.12, 95% CI 0.07‐0.20).
Table 4.
Sociodemographic features of patient portal users and non‐users among patients served during the COVID‐19 period (April 2020‐March 2021)
| PP login (n = 987) | No PP login (n = 455) | Odds ratio | P value a | |
|---|---|---|---|---|
| n (%) | n (%) | (95% CI) | ||
| Age, years | ||||
| <55 | 625 (63.3) | 225 (49.5) | Reference | N/A |
| 55‐64 | 185 (18.7) | 125 (27.5) | 0.53 (0.41‐0.70) | <0.001 |
| 65‐74 | 119 (74) | 74 (16.3) | 0.58 (0.42‐0.80) | 0.0014 |
| ≥75 | 58 (5.9) | 31 (6.8) | 0.67 (0.42‐1.07) | 0.104 |
| Sex | ||||
| Female | 685 (69.4) | 283 (62.2) | Reference | N/A |
| Male | 302 (30.6) | 171 (37.6) | 0.73 (0.58 ‐ 0.92) | 0.009 |
| Distance from hospital, miles | ||||
| <10 | 393 (39.8) | 213 (46.8) | Reference | N/A |
| 10‐24 | 334 (33.8) | 151 (33.3) | 1.20 (0.93‐1.55) | 0.175 |
| 25‐49 | 123 (12.5) | 49 (10.8) | 1.36 (0.94‐1.97) | 0.120 |
| 50‐99 | 70 (7.1) | 16 (3.5) | 2.37 (1.34‐4.19) | 0.002 |
| ≥100 | 67 (6.8) | 25 (5.5) | 1.45 (0.89‐2.37) | 0.157 |
| Established patient b | ||||
| No | 673 (68.2) | 283 (62.2) | Reference | N/A |
| Yes | 314 (31.8) | 172 (37.8) | 0.77 (0.61‐0.97) | 0.027 |
| Race/ethnicity | ||||
| White | 535 (54.2) | 100 (22.0) | Reference | N/A |
| American Indian or Alaska Native | 20 (2.0) | 11 (2.4) | 0.34 (0.158‐0.73) | 0.011 |
| Asian | 110 (11.1) | 51 (11.2) | 0.40 (0.27‐0.60) | <0.001 |
| Black or African American | 118 (12.0) | 97 (21.3) | 0.23 (0.16‐0.32) | <0.001 |
| Native Hawaiian or other Pacific Islander | 22 (2.2) | 4 (0.9) | 1.03 (0.35‐3.05) | 1.000 |
| Latinx | 95 (9.6) | 147 (32.3) | 0.12 (0.09‐0.17) | <0.001 |
| Missing | 87 (8.8) | 45 (9.9) | 0.36 (0.24‐0.55) | <0.001 |
| Language | ||||
| English | 887 (89.9) | 234 (51.4) | Reference | N/A |
| Spanish | 38 (3.9) | 136 (29.9) | 0.07 (0.05‐0.11) | <0.001 |
| Non‐English/non‐Spanish | 62 (6.3) | 85 (18.7) | 0.19 (0.13‐0.28) | <0.001 |
| Payer | ||||
| Commercial | 360 (36.5) | 63 (13.8) | Reference | N/A |
| Self‐pay | 31 (3.1) | 46 (10.1) | 0.12 (0.07‐0.20) | <0.001 |
| Medicaid | 201 (20.4) | 139 (30.5) | 0.25 (0.18‐0.36) | <0.001 |
| Medicare | 184 (18.6) | 101 (22.2) | 0.32 (0.22‐0.46) | <0.001 |
| Other | 211 (21.4) | 106 (23.3) | 0.35 (0.24‐0.50) | <0.001 |
Abbreviations: CI, confidence interval; COVID‐19, coronavirus disease 2019; N/A, not applicable; PP, patient portals.
Fisher's exact test, two‐sided.
Established patient: any patient completing three or more visits during the pre‐COVID‐19 period.
Multivariable logistic regression analysis for PP use is shown in Table 5. In this model, older age groups (except for ≥75 years) and male sex were associated with significantly lower odds of PP use, the greatest difference being observed for patients aged 55 to 64 years (aOR 0.53, 95% CI 0.41‐0.70). Of the distance categories, only 10 to 24 miles showed a statistically significantly increased odds of PP use (aOR 1.49, 95% CI 1.10‐2.03). Established and nonestablished patients showed similar PP use. The strong negative associations between race/ethnicity categories and PP login observed in univariable analysis were attenuated in multivariable analysis, with differences between White and Asian patients no longer reaching statistical significance. However, the strong negative associations between PP use and non‐English language preference remained, the lowest aOR being for Spanish language preference (aOR 0.07, 95% CI 0.04‐0.14). The negative associations between noncommercial payer groups (except self‐pay) and PP use remained statistically significant, albeit weaker than in univariable analysis, the lowest aOR being for Medicaid patients (aOR 0.34, 95% CI 0.23‐0.51). Inclusion of a race/ethnicity × language (English or non‐English) interaction term in the model revealed no significant associations with PP use (data not shown).
Table 5.
Sociodemographic features associated with patient portal use among patients served during the COVID‐19 period (April 2020‐March 2021)
| aOR (95% CI) | P value a | |
|---|---|---|
| Age, years (vs <55) | ||
| 55‐64 | 0.45 (0.32‐0.63) | <0.001 |
| 65‐74 | 0.58 (0.37‐0.91) | 0.017 |
| ≥75 | 0.74 (0.40‐1.38) | 0.342 |
| Sex (vs female) | ||
| Male | 0.58 (0.44‐0.77) | <0.001 |
| Distance from hospital, miles (vs <10) | ||
| 10‐24 | 1.49 (1.10‐2.03) | 0.011 |
| 25‐49 | 1.01 (0.66‐1.57) | 0.950 |
| 50‐99 | 1.58 (0.83‐2.99) | 0.165 |
| ≥100 | 1.05 (0.59‐1.88) | 0.859 |
| Established patient b (vs not established) | ||
| Established patient | 1.03 (0.77‐1.38) | 0.829 |
| Race/ethnicity (vs White, non‐Latinx) | ||
| American Indian or Alaska Native | 0.32 (0.14‐0.76) | 0.010 |
| Asian | 0.86 (0.52‐1.42) | 0.550 |
| Black or African American | 0.30 (0.21‐0.45) | <0.001 |
| Native Hawaiian or other Pacific Islander | 1.05 (0.34‐3.25) | 0.926 |
| Latinx | 0.47 (0.27‐0.80) | 0.006 |
| Missing | 0.47 (0.29‐0.75) | 0.002 |
| Language (vs English) | ||
| Spanish | 0.07 (0.04‐0.14) | <0.001 |
| Non‐English/non‐Spanish | 0.21 (0.14‐0.33) | <0.001 |
| Payer (vs commercial) | ||
| Self‐pay | 0.71 (0.37‐1.38) | 0.321 |
| Medicaid | 0.34 (0.23‐0.51) | <0.001 |
| Medicare | 0.45 (0.28‐0.73) | 0.001 |
| Other | 0.48 (0.32‐0.72) | <0.001 |
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval; COVID‐19, coronavirus disease 2019.
Logistic regression analysis; all variables included in analysis are shown.
Established patient: any patient completing three or more visits during the pre‐COVID‐19 period.
DISCUSSION
Little is known about sociodemographic disparities in digital care use among rheumatology patients in the United States. To our knowledge, ours is the first study to examine patient‐level sociodemographic features associated with video visit and PP use in outpatient rheumatology care. We observed strong negative associations between video use and non‐English language preference, Black or African American race/ethnicity, American Indian or Alaska Native race/ethnicity, male sex, Medicaid payer status, and increasing age. Similarly, we observed strong negative associations between PP use and non‐English language preference, male sex, minority race/ethnicity, and noncommercial payer status.
In accordance with previously published studies (7, 8, 9), we observed decreased video use among patients preferring non‐English languages. Decreased video visit use did not appear to reflect reduced access to care, because language preference was similar in pre‐COVID‐19 and COVID‐19 periods, and patients preferring non‐English languages were not less likely than English‐preferring patients to have completed visits in both periods. Others have shown that patients preferring non‐English languages more frequently experience problems using video platforms (11), which typically offer an English‐only interface. Together, these findings strongly suggest that non‐English language preference itself was a barrier to video visit use in our patients. English language proficiency was not assessed in our study. We were also unable to determine whether access to digital resources or proficiency with digital platforms affected video use. However, in a population similar to our study's, access to broadband internet was identified as a barrier to video visits among Spanish‐speaking patients (16).
Low video visit use among Black or African American patients in outpatient primary and specialty care settings (including rheumatology) has been reported by others (7, 8). In our study, although approximately 17% of Black or African American patients preferred non‐English languages, we identified no significant interactions between Black or African American identity and language in determining video use. Low video use among English‐preferring Black or African American (17) and American Indian or Alaska Native patients could involve patient concerns over privacy, trust, and efficacy.
Similar to previous studies (5, 7, 8), we observed reduced video visit use among older patients, Medicaid recipients, and men. Our data set did not allow us to identify underlying causes of these disparities. However, for patients on Medicaid, a potential surrogate for low income (18), lower video use could reflect lower access to necessary equipment and services. Lower video use among men in our study remains unexplained, but other studies have correlated male sex with telehealth unreadiness (19), difficulty navigating the video platform (11), and lower likelihood of choosing video visits over in‐person visits (20). We observed uniformly increased odds of video visit use among patient groups greater than or equal to 10 miles from the hospital (except for those ≥100 miles, P = 0.06), which could reflect incentive for reduced travel.
Although disparities in PP registration and use have been described for various outpatient populations (6, 12, 21, 22, 23), they have not been reported, to our knowledge, for rheumatology patients. In our study, non‐English language preference was the strongest predictor of low PP use. This could reflect difficulty in using an English‐only platform as well as lack of support for message translation. As with video use, it seems likely that non‐English language preference itself is a barrier to PP use. We also observed ethnic/racial disparities in PP use that did not appear to reflect language preference. Lower PP use among American Indian or Alaska Native, Black or African American, and Latinx patients could reflect factors related to access to and use of necessary equipment, patient perceptions about PP, and clinic or provider counseling and assistance for PP use (13, 23).
Despite highlighting many important factors associated with video visit and PP use, our study had certain limitations. First, our data set did not allow us to confirm the causes of disparities in video and PP use. Second, the relatively small size of our cohort limits the generalizability of our findings. Finally, our findings are restricted to the pandemic setting.
Taken with previous studies, our findings have implications for rheumatology research and policy. Given the advantages of video and PP use for patients and health care systems, and the unique demographics and care needs of rheumatology patients, rheumatology‐focused research on digital care disparities is needed in order to shape a more equitable health care system. Based on our results, this might take the form of non‐English language support for digital care platforms and outreach to communities with low digital care use.
The rapid deployment of telehealth across the United States during the COVID‐19 pandemic has improved health care for some but simultaneously widened existing disparities and possibly created new ones. As the United States moves to strengthen its digital infrastructure, telehealth promises to become an increasingly important mode of care delivery. Thus, clarifying and addressing causes of telehealth disparities is essential for delivering equitable health care.
AUTHOR CONTRIBUTIONS
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be published. Dr. Hughes had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design
Thomason, Bays, Mantilla, Huang, Najjar, Singh, Wysham, Hughes.
Acquisition of data
Hughes.
Analysis and interpretation of data
Thomason, Bays, Mantilla, Huang, Najjar, Singh, Wysham, Hughes.
Supporting information
Disclosure Form
Figure S1 Supplementary Figure
Supplementary Table 1 Sociodemographic Features of Pre‐COVID‐19 Patients Completing vs. Not Completing At Least 1 Visit During the COVID‐19 Period (April 2020 – March 2021)
Supplementary Table 2. Language Preference and Race/Ethnicity of Patients Served During COVID‐19 Period (April 2020 – March 2021)
ACKNOWLEDGMENT
The authors gratefully acknowledge E. Aas for assistance with data acquisition.
The views expressed herein are those of the authors and do not necessarily represent the position or policy of the Department of Veterans Affairs or the US Government.
Dr. Huang's work was supported by the Arthritis Foundation Cultivating a New Generation of Rheumatologists Fellowship Award. Dr. Najjar's work was supported by NIH National Institute of Arthritis and Musculoskeletal and Skin Diseases grant T32‐AR‐007108. Dr. Wysham's work was supported by the Rheumatology Research Foundation Scientist Development Award and the Department of Veterans Affairs. Dr. Hughes's work was supported by the Robert F. Willkens, M.D. – Lucile T. Henderson Endowed Professorship in Rheumatology and the Arthritis Foundation supplemental grant for diversity, equity, and inclusion.
No potential conflicts of interest relevant to this article were reported.
Author disclosures are available at https://onlinelibrary.wiley.com/action/downloadSupplement?doi=10.1002%2Facr2.11407&file=acr211407‐sup‐0001‐Disclosureform.pdf.
REFERENCES
- 1. Webster P. Virtual health care in the era of COVID‐19. Lancet 2020;395:1180–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Koma W, Cubanski J, Neuman T. Medicare and telehealth: coverage and use during the COVID‐19 pandemic and options for the future. 2021. URL: https://www.kff.org/medicare/issue‐brief/medicare‐and‐telehealth‐coverage‐and‐use‐during‐the‐covid‐19‐pandemic‐and‐options‐for‐the‐future/.
- 3. Ferucci ED, Day GM, Choromanski TL, Freeman SL. Outcomes and quality of care in rheumatoid arthritis with or without video telemedicine follow‐up visits. Arthritis Care Res (Hoboken) 2020. E‐pub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Vogels, EA . Digital divide persists even as Americans with lower incomes make gains in tech adoption. URL: https://www.pewresearch.org/fact‐tank/2021/06/22/digital‐divide‐persists‐even‐as‐americans‐with‐lower‐incomes‐make‐gains‐in‐tech‐adoption/.
- 5. Hsiao V, Chandereng T, Lankton RL, Huebner JA, Baltus JJ, Flood GE, et al. Disparities in telemedicine access: a cross‐sectional study of a newly established infrastructure during the COVID‐19 pandemic. Appl Clin Inform 2021;12:445–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sinha S, Garriga M, Naik N, McSteen BW, Odisho AY, Lin A, et al. Disparities in electronic health record patient portal enrollment among oncology patients. JAMA Oncol 2021;7:935–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Eberly LA, Kallan MJ, Julien HM, Haynes N, Khatana SA, Nathan AS, et al. Patient characteristics associated with telemedicine access for primary and specialty ambulatory care during the COVID‐19 pandemic. JAMA Netw Open 2020;3:e2031640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ye S, Kronish I, Fleck E, Fleischut P, Homma S, Masini D, et al. Telemedicine expansion during the COVID‐19 pandemic and the potential for technology‐driven disparities. J Gen Intern Med 2021;36:256–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chen E, Andoh J, Nwanyanwu K. Socioeconomic and demographic disparities in the utilization of telemedicine for ophthalmic care during the COVID‐19 pandemic. Ophthalmology 2021;129:15–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Xiong G, Greene N, Lightsey H, Lightsey HM IV, Crawford AM, Striano BM, et al. Telemedicine use in orthopaedic surgery varies by race, ethnicity, primary language, and insurance status. Clin Orthop Relat Res 2021;479:1417–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cheung S, Capote J, Fan W, Mishkin AD. Pilot assessment of patient and provider characteristics associated with satisfactory consultation‐liaison telepsychiatry encounters. J Acad Consult Liaison Psychiatry 2021;26:582–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Obeid JS, Shoaibi A, Oates JC, Habrat ML, Hughes‐Halbert C, Lenert LA. Research participation preferences as expressed through a patient portal: implications of demographic characteristics. JAMIA Open 2018;1:202–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Anthony DL, Campos‐Castillo C, Lim PS. Who isn't using patient portals and why? Evidence and implications from a national sample of US adults. Health Aff (Millwood) 2018;37:1948–54. [DOI] [PubMed] [Google Scholar]
- 14. El‐Toukhy S, Mendez A, Collins S, Perez‐Stable EJ. Barriers to patient portal access and use: evidence from the Health Information National Trends survey. J Am Board Fam Med 2020;33:953–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. George MD, Danila MI, Watrous D, Reddy S, Alper J, Xie F, et al. Disruptions in rheumatology care and the rise of telehealth in response to the COVID‐19 pandemic in a community practice‐based network. Arthritis Care Res (Hoboken) 2021;73:1153–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Khoong EC, Butler BA, Mesina O, Su G, DeFries TB, Nijagal M, et al. Patient interest in and barriers to telemedicine video visits in a multilingual urban safety‐net system. J Am Med Inform Assoc 2021;28:349–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. George SM, Hamilton A, Baker R. Pre‐experience perceptions about telemedicine among African Americans and Latinos in South Central Los Angeles. Telemed J E Health 2009;15:525–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Casey JA, Pollak J, Glymour MM, Mayeda ER, Hirsch AG, Schwartz BS. Measures of SES for electronic health record‐based research. Am J Prev Med 2018;54:430–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lam K, Lu A, Shi Y, Covinsky K. Assessing telemedicine unreadiness among older adults in the United States during the COVID‐19 pandemic. JAMA Intern Med 2020;180:1389–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Reed ME, Huang J, Graetz I, Lee C, Muelly E, Kennedy C, et al. Patient characteristics associated with choosing a telemedicine visit vs office visit with the same primary care clinicians. JAMA Netw Open 2020;3:e205873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Goel MS, Brown TL, Williams A, Hasnain‐Wynia R, Thompson JA, Baker DW. Disparities in enrollment and use of an electronic patient portal. J Gen Intern Med 2011;26:1112–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gerber D, Laccetti A, Chen B, Yan J, Cai J, Gates S, et al. Predictors and intensity of online access to electronic medical records among patients with cancer. J Oncol Pract 2014;10:e307–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Clarke M, Lyden E, Ma J, King KM, Siahpush MM, Michaud T, et al. Sociodemographic differences and factors affecting patient portal utilization. J Racial Ethn Health Disparities 2021;8:879–91. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Disclosure Form
Figure S1 Supplementary Figure
Supplementary Table 1 Sociodemographic Features of Pre‐COVID‐19 Patients Completing vs. Not Completing At Least 1 Visit During the COVID‐19 Period (April 2020 – March 2021)
Supplementary Table 2. Language Preference and Race/Ethnicity of Patients Served During COVID‐19 Period (April 2020 – March 2021)


