Abstract
Background
Digital health technologies have been proposed to support hospital-to-home transition for older adults. The COVID-19 pandemic and the associated physical distancing guidelines have propelled a shift toward digital health technologies. However, the characteristics of older adults who participated in digital health research interventions to support hospital-to-home transitions remain unclear. This information is needed to assess whether current digital health interventions are generalizable to the needs of the broader older adult population.
Objective
This rapid review of the existing literature aimed to identify the characteristics of the populations targeted by studies testing the implementation of digital health interventions designed to support hospital-to-home transitions, identify the characteristics of the samples included in studies testing digital health interventions used to support hospital-to-home transitions, and create recommendations for enhancing the diversity of samples within future hospital-to-home digital health interventions.
Methods
A rapid review methodology based on scoping review guidelines by Arksey and O’Malley was developed. A search for peer-reviewed literature published between 2010 and 2021 on digital health solutions that support hospital-to-home transitions for older adults was conducted using MEDLINE, Embase, and CINAHL databases. The data were analyzed using descriptive statistics and qualitative content analysis. The Sex- and Gender-Based Analysis Plus lens theoretically guided the study design, analysis, and interpretation.
Results
A total of 34 studies met the inclusion criteria. Our findings indicate that many groups of older adults were excluded from these interventions and remain understudied. Specifically, the oldest old and those living with cognitive impairments were excluded from the studies included in this review. In addition, very few studies have described the characteristics related to gender diversity, education, race, ethnicity, and culture. None of the studies commented on the sexual orientation of the participants.
Conclusions
This is the first review, to our knowledge, that has mapped the literature focusing on the inclusion of older adults in digital hospital-to-home interventions. The findings suggest that the literature on digital health interventions tends to operationalize older adults as a homogenous group, ignoring the heterogeneity in older age definitions. Inconsistency in the literature surrounding the characteristics of the included participants suggests a need for further study to better understand how digital technologies to support hospital-to-home transitions can be inclusive.
Keywords: older adults, digital technology, transitions, older adult population, digital health, Digital Hospital, health intervention, aging, gender diversity, home transition, epidemiology
Introduction
Background
Transitioning across health care settings is a complex experience for older adults and their caregivers [1,2]. Older adults [3] and family caregivers (ie, family members, friends, or neighbors) who provide unpaid assistance or care to someone living with an injury, disability, or illness [4] frequently experience unmet care needs as the patients leave the hospital and transition to home [5-10]. Transitions in care are often more difficult for older adults who experience frequent hospitalizations and are often discharged with ongoing and complex care needs exceeding those that existed at the initial hospitalization [11,12]. Thus, researchers have urged integrated care strategies to better meet their care needs after hospitalization [12]. Here, we define integrated care as “the promotion of the comprehensive delivery of quality services across the life-course, designed according to the multidimensional needs of the population and the individual and delivered by a coordinated multidisciplinary team of providers working across settings and levels of care” [13].
Unsupported hospital-to-home transitions can result in adverse events, such as medication-related problems (eg, harmful drug effects) [14], readmissions to hospitals [15], lack of continuity of care [16], and even mortality [17,18]. To help overcome challenges during this transition period, older adults and their family caregivers attempt to develop, integrate, and use knowledge and skills to manage transitions in care settings and related changes in illness trajectories [19]. Improving transitions in care can help improve the quality and cost of care and promote more equitable care for vulnerable older adults [20]. An emerging area of research is the use of technology to help support hospital-to-home transitions for patients and their family caregivers [2,20-22].
Technological advances may help integrate health and social care in at-risk populations [23]. Technologies aimed at improving health outcomes for older adult populations as they transition across care settings have demonstrated success and promise [20,24-28]. Technologies to support care transitions can increase access to support for older adults as they transition from hospital-to-home by reducing architectural and physical barriers to accessing care in the community [20,29,30]. Other benefits of technology in supporting care during transitions include eliminating barriers to attending in-person support programs, such as restricted mobility, time constraints, transportation costs, and a lack of respite care for individuals caring for others [31].
Spurred by the COVID-19 pandemic, as face-to-face care options became less available initially, health systems and providers turned to digital tools as an alternate means of supporting older adults and families [32-34]. During this digital revolution [35], there has been increasing attention to whether or how health technologies support equitable access and use for all older adults who may benefit [36,37]. The rapid virtualization of health and social care to support hospital-to-home transitions poses a risk to access and equity and may create structural inequalities [38].
Older adults may be most vulnerable to inequitable access to and use of digital health technologies, given their overall lack of use of existing technologies [39]. Barriers to using technology for older adults include lower levels of digital literacy, lack of perceived usefulness, and physical and cognitive deficits that may make using digital tools challenging [40]. Similarly, previous studies have shown that older adults are overlooked in technological health research [41,42]. Barriers to technology use are even more prevalent in older adults from racial or ethnic minorities and socioeconomically disadvantaged groups [43]. Therefore, an equity-informed review of existing programs is required to create equity-informed guidelines to guide future development, delivery, and implementation of technologies to support hospital-to-home transitions for older adults. In the context of human experiences, including experiences with transitions in case, experiences are shaped by multiple social positions [44,45]. Moreover, a one-size-fits-all approach to transitional interventions may not work well for all people, of all social identities, given the high adverse events during transitional periods among persons from minority groups (eg, racial minority groups [46] and nonheterosexual individuals living in poverty [47]). Researchers have a growing interest in examining intersectionality in qualitative and quantitative research [44]. By including both qualitative and quantitative research in our review and noting how well the characteristics of particular groups have been reported, we hope to provide direction for future studies to better examine the multiple social positions left out of digital transitional care intervention research. Despite growing awareness of digital inequity, there are current knowledge gaps related to intersectionality and transitions, particularly within digital health interventions [48]. Addressing these knowledge gaps is a priority for the digital bridge intervention currently being developed by our research team [2,49]. Moreover, our results will provide recommendations that will inform the design and structure of other future digital health interventions that support hospital-to-home transitions for older adults.
Objectives
To help inform recommendations for future technologies to assist with hospital-to-home transitions for older adults, we conducted a secondary analysis of a rapid review of existing technologies. The protocol for this broader review has been published elsewhere [21]. The initial review mapped the published literature on studies that tested digital health interventions to support hospital-to-home transitions. This review included all relevant interventions with samples of at least one older adult for comprehensiveness. Preliminary findings from the review indicated that less than one-fifth of the included studies were conducted exclusively with older adults and highlighted the need to explicitly examine interventions with older adults [21]. The broader review did not consider sex nor gender in its analysis, nor any other intersectional factors that influence participation in digital technology interventions. A secondary analysis focusing on sex, gender, and other intersectional factors was not part of the planned protocol [21]. Thus, the purpose of this secondary analysis was to (1) identify the characteristics of older adults targeted by studies testing the implementation of digital health interventions to support hospital-to-home transitions; (2) identify the characteristics of the samples included within studies testing digital health interventions to support hospital-to-home transitions; and (3) create recommendations for enhancing equity, diversity, and inclusion in future digital health intervention research. The specific research questions for this secondary analysis were as follows: “What are the targeted populations within existing digital health interventions supporting hospital-to-home transitions?” “What are the actual participants within existing digital health interventions supporting hospital-to-home transitions?”
Methods
Design
A rapid review was deemed appropriate, given the need to generate timely recommendations for future digital health interventions, as the COVID-19 pandemic has prompted an immediate need for novel technological supports [21,50,51]. Consistent with prior studies that conducted a secondary analysis of reviews [52-54], a secondary analysis entailed reexamining relevant data to answer different research questions and addressing knowledge gaps identified in the initial review [55]. We used modified and hybrid guidelines for rapid reviews [56] and the systematic guidelines of Arksey and O’Malley for scoping reviews [57,58]. This approach was deemed appropriate because scoping reviews allow for an iterative approach to data collection and analysis, whereas rapid reviews allow a timely synthesis of the existing literature. For example, we limited the search to select databases and conducted this review in a short period [59]. Our 5-stage rapid scoping review model included (1) identifying the research question, (2) identifying relevant studies, (3) selecting studies, (4) charting data, and (5) summarizing and reporting the results [58]. In the remainder of this section, we outline the specific steps undertaken to complete the review. As this secondary analysis aimed to answer different research questions than intended within the published protocol, the methods used in this study necessitated some deviations from the original protocol, as described in the following sections [21].
As there are no reporting guidelines for rapid reviews, we relied on elements of the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) Protocols checklist as a guide for reporting this review [60].
Theoretical Framework
This study was theoretically informed by a Sex- and Gender-Based Analysis Plus (SGBA+) lens [61]. The SGBA+ lens has been applied in the context of other reviews in health research [62,63]. As a theoretical framework, SGBA+ draws on intersectionality frameworks. Other intersectional frameworks include the Theoretical Domains Framework [64] and intersectionality-based policy analysis framework [65]. However, SGBA+ was specifically chosen, as it allowed researchers to examine sample characteristics within research processes and data, including biological sex and the multiple social positions that older adults hold (eg, ethnicity, income, age, race, education, and gender) to determine whether intervention findings are relevant to the needs of all older adults [61,66]. For this review, sex is defined here as a biological construct. In contrast, gender is defined as a social construct that refers to the socially prescribed dimensions of being a female or male [67].
This review explores how existing digital health interventions supporting hospital-to-home transitions represent sex, gender, and identity perspectives within their target and actual samples. These insights can be used to create equity-informed recommendations for future digital health interventions.
Identifying the Research Question
The widespread shift to digital health during the COVID-19 pandemic has revealed digital equity to be a critical issue [38]. During the analysis phase of the larger rapid review [21], we identified the need to re-examine the data for identification.
Identifying Relevant Studies
Relevant literature on digital health solutions currently applied to facilitate the transition from hospital-to-home for older adults was searched for as part of a larger review. A comprehensive, peer-reviewed search was created by an experienced information specialist in consultation with the research team and translated by the information specialist to MEDLINE (Ovid), CINAHL, and Embase (Ovid). The search was run on these databases by HC on November 26, 2020, for the larger review. In addition, the reference lists of 20 included articles were examined, and 6 content experts were consulted to identify additional studies for the larger review.
For this analysis, KMK and HS reran this search on September 20, 2021, using established guidelines [68] to ensure articles are up-to-date. KMK and HS used the same search strategy reported in the published protocol, including concepts related to digital health, navigation, and transition of care from hospital to home [21]. New (unique) articles retrieved from the updated search were reviewed as described in the following sections.
Selecting Studies
Studies were included in the larger review [21] if they (1) empirically tested a digital health intervention and (2) supported a hospital-to-home transition (ie, continued from the hospital-to-home or community settings). The intervention had to be (3) tested with older adults (aged ≥65 years) who were recruited before their hospital discharge, (4) conducted in high-income countries [69], and (5) published in English in or after the year 2010 [21]. No limitations were imposed on the study design. The larger review was limited to interventions conducted in high-income countries for two reasons: digital and health infrastructure and resources can differ between high- and low-income countries, and the intent of the primary review was to provide recommendations for the digital bridge (a digital health intervention currently under development) [21,70]. As per the protocol, studies were excluded if the hospital setting was ambulatory (eg, emergency department visits) or if the discharge destination was an institution (eg, long-term care) [21]. We deviated from the protocol by limiting this review to technological interventions that are not strictly telephone based, given the extensive investigations and syntheses of telephone-based health interventions [71-75]. We also reduced the age of older adults to ≥55 years to be comprehensive to ensure young old adults are included [76].
As per the published protocol [21], study selection within the larger review used a single screener strategy after minimum interrater reliability was achieved (κ=0.80) during the title and abstract screening phases (ie, reviewed titles and abstracts together). Owing to the complexity of the inclusion criteria and limited information in titles and abstracts, we only screened for inclusion criteria 1, 4, and 5 during the title and abstract screening, whereas the remaining were screened for full-text review [21]. Interrater reliability was not reexamined during the full-text review stage, as we decided that 2 reviewers (KMK and HS) would independently screen articles at this stage because the papers had already undergone rigorous screening and interrater calculations. This secondary analysis did not need to be screened, as the purpose was to conduct an additional analysis to explore a question not addressed in the original study.
The study selection for this secondary analysis was modified from the published protocol to enhance comprehensiveness. The first author (KMK) independently reviewed the titles and abstracts of articles excluded from the larger review on August 31, 2021, to ensure that no potential article was missed with the single screener approach. However, no additional relevant articles were identified. After the search was updated for this review, 4 authors (KMK, DP, CMJ, and HS) reviewed the titles and abstracts (ie, 2 reviewers independently screened each article) over a 3-week period. After screening all titles and abstracts, 2 individuals (KMK and HS) reviewed articles from the initial full-text review and the updated search over an additional 3-week period. Team discussions, led by the senior author (HS), were used to resolve conflicts for both searches (ie, discrepancies in inclusion and exclusion and reasons for exclusion) until 100% agreement was obtained. Covidence software was used to facilitate the screening process [77].
Charting the Data
The first author extracted data from the included articles using a modified form from the larger study. Extracted data included the study characteristics (ie, author, year, country, and design), details of the study inclusion criteria (ie, target sample), and details of the participants (ie, actual sample). Next, a spreadsheet was used to categorize the studies into three categories informed by SGBA+: sex, gender, and other identity constructs. All extracted data were reviewed and verified by a second reviewer (HS) to enhance the data quality and accuracy. Data were collected over approximately 2 months.
Summarizing and Reporting the Data
Data were organized numerically using descriptive statistics and summarized using a narrative descriptive synthesis [78]. The narrative descriptive synthesis entailed the first and senior author mapping the findings into deductive themes informed by the SGBA+ framework, including sex, gender, geography, culture, age, and disability [61,66]. After coding all studies, the data were classified into 9 broad identity constructs. The constructs represented in this review included age, patient population, race and ethnicity, sex and gender, sexual orientation, education, disability, language, and technology access and comfort.
Results
Overview
In total, 34 articles met the inclusion and exclusion criteria. The search process is outlined in Figure 1. A total of 16 studies were conducted in Europe [79-94], 12 were conducted in North America [3,73,95-105], 3 in Asia [106-108], and 2 in Australia [109,110]. Multimedia Appendix 1 shows the distribution of studies based on location. In addition, of 34 studies, 1 (n=1, 3%) study used qualitative methodology [111], 1 (n=1, 3%) study was a report [98], and another used a case study design (n=1, 3%) [81]. A total of 9% (n=3) of studies used a mixed methods methodology [3,87,96], whereas the remaining studies (28/34, 82%) used a quantitative methodological approach. Of the 28 quantitative studies, 8 (n=8, 28%) used a randomized controlled trial design [89,90,97,101,106,107,109,110]. Other quantitative studies have used observational or nonrandomized trial designs.
Figure 1.
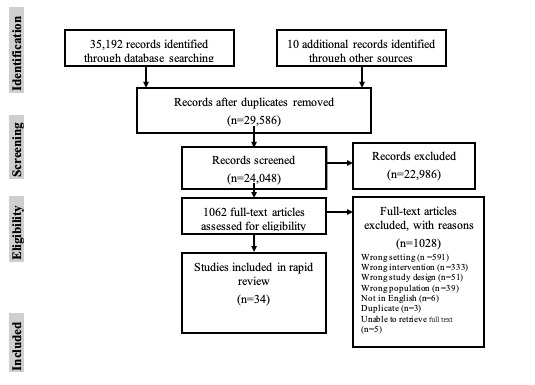
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) diagram adapted from Moher et al [60].
Across all studies, 9809 participants were included (mean 297 participants per study, range 1 [65] to 3661 [70], SD 383). Across the 8 randomized controlled trials, 4434 participants were included (sample size mean 986 per study).
A total of 7 studies reported smaller sample sizes because of particular inclusion and exclusion criteria and limitations of the interventions (eg, dropouts) [3,87,90,91,100,102,105]. However, a small sample size was a deliberate choice for scholars in 2 studies [3,100].
Digital Health Interventions
Overview
Multimedia Appendix 2 [3,83-94,100-103,105-108,110,111] summarizes the breadth of the methodological characteristics, aims of the studies, and a brief description of the digital interventions in detail. Briefly, web-based, tablet, and mobile app tools are the most common means of delivering digital interventions [3,83-94,100-103,105-108,110,111]. Electronic health records and databases [79,81,95,97,98,102,104] have been widely used for digital innovation. The use of wearable body sensors or devices [80,99,107], web-based chatting platforms [82], and automated emails [109] were less common.
The focus of digital health interventions varied. For example, some were related to medication reconciliation [79,81,97,104], whereas others aimed at providing education (eg, about rehabilitative exercises), internet-based care, and resources [83,86,89,92,94,96,100,104-106,111] and improved communication and care coordination with older adults’ care providers [3,82,91,104,108]. A total of 2 interventions aimed to improve communication processes among health care providers regarding discharge processes and care plans [93,109]. Many interventions aimed at monitoring bodily function and health status (including mental health) [80,84,85,88,90,94,99,101-103,107,110], often to alert members of the older adult’s care team of the need to schedule follow-up appointments or calls to help prevent adverse effects [97,98]. One study used digital technology to support home-delivered meals [87].
Regarding the targeted samples in the studies, the minimum age for inclusion in 3 studies was 55 years [3,99,105]. Other studies required participants to have a minimum age of 60 to 65 years, except for one that used 70 [94] and 75 years [79]. Conversely, 2 studies had a maximum age of 75 [79,106] and 80 years [89]. Justifications for maximum ages were not provided. A total of 7 studies did not report on their targeted age but instead referred to geriatric patients [81,83,101,102,109,110] or “elders” [98]. Multimedia Appendix 3 [3,83-94,100-103,105-108,110,111] outlines the targeted populations of the included studies. It is worth noting that none of these studies specifically set out to include an analysis of heterogeneous groups of patients.
There was heterogeneity in the mean age of the participants included in the studies. The mean of age included older adult participants ranged from 65 to 69 years [83,99,105,111], 70 to 74 years [3,80,84,85,89,94,101,106,108], and 75 to 79 years [82,87,92,97,101] to 80 to 84 [86,88,90-93,96,104,107,109,110]. Only 2 studies had a mean age of ≥85 years [79,109]. A few studies did not specify the mean patient age [88,95,98,100,102,112].
The patient populations in all the studies included mainly frail geriatric patients or older adults. Only one study purposely examined older adults with cognitive impairment (ie, patients with mild cognitive impairment) and vascular cognitive impairment (eg, vascular dementia) [89]. In terms of their targeted population, many studies (n=14, 41%) excluded older adults with cognitive impairments [82, 84-86, 88-90, 92, 94, 101, 102, 105, 110, 111]. These studies excluded older adults who could not communicate because of cognitive challenges [107], postoperative delirium [112], and dementia [82,86,88,89,107].
Owing to the nature of our inclusion criteria, all patients were hospitalized, although the reasons for hospitalization varied. Hospitalizations included patients identified with nutritional risk (n=1, 3%) [87], chronic obstructive pulmonary disease (n=1) [88], heart failure (n=4) [88,90,94,101], diabetes (n=2) [81,105], and stroke (n=2) [3,83]. Two studies required participants to live with multimorbidity, defined as living with ≥2 chronic conditions [3,107]. One study included patients hospitalized for any nonelective reason [104]. A total of 14 studies included patients who underwent or had been scheduled for a surgical procedure [102], such as elective surgery [80], hip surgeries [82,86,92,96,108,111], total knee arthroplasty [106], oncological surgeries [84,85,100] (eg, lung or gastrointestinal cancers) [91], or cardiac or major vascular surgery [112]. The family caregivers of patients participated in 5 studies [96,100,102,107,110].
Racial, Ethnic, and Cultural Diversity in Digital Health Transition Interventions
Racial, ethnic, cultural, and religious diversity were rarely considered in the inclusion criteria or target sample.
A total of 23% (8/34) of studies described their actual sample’s ethnicity, race, and culture [85,96,100,101,104,105,111,112]. The samples within all these studies were primarily White, except one, which included participants who were primarily Black (75% of the sample) [105]. This study also included 1 Asian participant (5%) [105]. In contrast, one of the studies dichotomized participants’ race and ethnicity as White or others [100]. Participants were racially diverse in a study conducted by Choi et al [111], whereby participants were White (60%), African American (20%), Asian or Pacific Islander (7%), and Hispanic (13%). Similarly, in a study by Madigan et al [101], most of the sample was White, and the minority was African American (26%) [101]. Another study included participants who were White (68%), Hispanic (13%), Black (13%), and Asian (7%) [104]. Similarly, another study included African (15%) and Asian (4%) participants [112]. Multimedia Appendix 4 [3,83-94,100-103,105-108,110,111] describes the details of the participants (ie, actual sample). It is worth noting that none of these studies specifically set out to include an analysis of heterogeneous groups of patients.
Sex and Gender Diversity of Digital Health Transition Interventions
None of the articles aimed to recruit a specific sex or gender in their inclusion criteria or had sampled for both sex and gender diversity.
In their actual samples, the percentage of females (sex) in the studies ranged from 0% [81] to 100% [106]. All but 3 studies (n=31, 91%) [93,98,102] reported the sex of the included participants. One study had only females in the study [106]. One case study included only 1 male participant [81]. Most studies had almost equal proportions of males and females, with approximately 50% in each category [3,88,95,97,100] or proportions of sexes ranging between approximately 40% and 59% [79,80,91,99,105,107,111]. Most of the other studies had much higher (ie, ≥60%) proportion of females than males within the sample (n=15, 44%) [82, 86, 87, 90, 92, 96, 99, 101, 103, 104, 107-111]. A total of 18% (6/34) of studies had a higher proportion (≥60%) of males compared with females within the sample [80,81,84,85,89,94]. None of the studies reported on participants’ gender identities or representations of gender-diverse older adults.
Sexual Orientation
Sexual orientation was not reported in the inclusion criteria or the sample of any of the included studies.
Education
Education level or literacy was a requirement for participation in 3 studies. One had limited inclusion to “those with junior high school-level education or higher” [108], and the others had limited inclusion to “school attendance >3 years” [89] and “low-literate older adults” [111].
A total of 8 studies reported the educational level of the sample [85,87,89,96,100,105,111,112]. Of these studies, 2 reported the length of education (between an average of 8-10 years [87,89]), but they did not report the educational details (eg, level and type of education). Of the remaining studies, 5 primarily included participants with an educational level of high school or less [85,96,105,111,112]. Participants with predominantly higher-level education, such as college, university, or graduate training, have been reported in a few studies [96,100,105,111,112].
Disability
A few studies excluded older adults with sensory or communication impairments (eg, severe aphasia or hearing loss) to ensure their ability to use the technology [83-88, 102, 106-108, 111] and vision [84-86,88,89,102,106,111]. Studies have also excluded older adults with arthritis [106] and neurological disorders [106]. A total of 21% (7/34) of studies excluded older adults with life-threatening illnesses [86-88,92,99,104,107]. Having a good health status or efficient disease control was a requirement in some studies [101,106]. Older adults with psychological conditions (eg, depression) were excluded from some studies [82,83,88,89]. Older adults with stroke were excluded from 6% (2/34) of studies [86,89]. Finally, studies excluded older adults using a wheelchair [99], severe ambulatory impairment [84,85], or inability to walk independently with a gait aid [86].
Language
The participants’ language proficiency was not discussed in the actual sample. However, some studies identified language as an inclusion criterion, but the reasons were not specified. Specifically, English-speaking proficiency was required in 20% (7/34) of the studies [3,96,100,103,105,110,111]. Other language requirements included Dutch [84,85], Italian [89], Danish [86], and Swedish [83,88]. It is worth noting that these were the primary languages of the countries in which these studies were conducted.
Technology Access and Comfort
Although some studies required participants or a caregiver to have internet access in their home [84,85,92] or working telephone line [101,102,108,110], access to the internet or device was not a requirement in all studies [86]. For example, Backman et al [96] provided participants with a loaner device if they did not have access to a mobile phone or computer. Similarly, because of low recruitment, the inclusion criteria were broadened in 2 studies to include those who did not have a phone [84,85].
Some studies included those with low technical literacy, providing training on device use and assistance with device setup [80,86,96,103,107,111]. However, others require participants to have technical literacy, including the capability to use [84,85,87,107] or familiarity with the tested device [82,106].
Discussion
Principal Findings
To our knowledge, this is the first rapid review to synthesize the characteristics of older adults (aged ≥55 years) within digital health interventions supporting hospital-to-home transition using an equity lens. Specifically, we described the target and actual sample characteristics of the 34 studies. Our findings indicate that many older adults were not recruited within these interventions and remain understudied (eg, older adults with cognitive impairment and oldest older adults). This study relied on an intersectionality framework to understand how different social identities influence participation in digital health interventions to improve hospital-to-home transitions and, in turn, the digital divide. On the basis of the study findings, we created a list of research implications to enhance the consideration of equity variables to ensure meaningful participation for diverse groups of older adults within the target and actual samples of digital health interventions (Multimedia Appendix 5).
We noted variability across studies in the age groups of older adults who were targeted and, in turn, who were included in the studies. It is well known that the hospitalization experiences and subsequent health and social service needs of older adults differ significantly depending on age [113-116]. Some studies did not specify a target age group of older adults [81,83,98,101,102,109,110] and recruited participants based on setting or program (eg, aged acute ward [109] and geriatric ward [102]). However, others were limited to a maximum age of 80 years [89]. However, justification within studies limiting the maximum age was poor.
The theorization of fourth age typically starts around age 80 years (when studies cut older adults off) and is seen as a time of dependence in which additional care needs may be needed [115], which inevitably translates into differing needs among older adults and requires important consideration for future intervention development. Thus, we used an equity-informed lens to identify older adults aged >80 years as an understudied group. Others have also noted this gap in the literature; thus, older adults aged >80 years should be considered in future digital health interventions [117].
In addition to age, 2 studies required older adults to have a good health status because of the perceived ability of the researcher to use technology [83,102]. Many studies have excluded older adults with cognitive and functional impairments or a poor health status. Older adults with poor health status have worse outcomes during transitions in care than the general older adult population [118]. Thus, excluding older adults with a poor health status may result in greater health inequities [48]. Furthermore, this limits the transferability of evidence to practice, given the high number of older adults with dementia and other comorbidities requiring hospitalization and returning home [119]. An equity perspective taken by our review elucidates the need for future research to consider how interventions can be designed for or adapted to understudied groups of non–English-speaking older adults with poor health from racial and ethnic minority groups [120], as these groups may be most vulnerable to adverse events during hospital-to-home transitions [120-123].
In addition, many studies have limited their interventions to older adults with access to and comfort with technology. This criterion runs the risk that novel technologies to support hospital-to-home transitions are exclusionary rather than inclusive of the older adults they aim to help. Older adults often face numerous barriers to the effective use of technological interventions because of a lack of access to and experience and skills with digital tools [124,125]. In addition, older adults with lower socioeconomic status have reduced access to digital resources and may be unable to afford the technology or internet required to use digital tools [126]. Socioeconomic status affects digital access and health status [127]. Such interventions may cause or worsen access disparities, as specific groups of patients are known to fall behind the average population in terms of their use of virtual services (this is often referred to as the digital divide) [128]. Some of the included studies posited suggestions for recruiting individuals from lower socioeconomic status, including the provision of a loaner device that had data (providing internet access) to mitigate the reliance on a personal device or internet access and financial barriers [84,85,96]. Other studies included those with low technology comfort by providing training on device use and assistance with device setup [80,86,96,103,107,111]. However, some studies have excluded older adults with impaired sensory, cognitive, or communication functions. As these impairments are common in the oldest older adults [129], commonly referred to as the oldest old or old old (ie, ≥85 years) [130], this restriction may explain why studies tended to include those younger within the older adult category. Although these impairments could reduce participants’ ability to use digital intervention, their participation can be supported by adapting technologies that are compatible for people with disabilities to use [131]. Thus, hospital-to-home interventions seeking to incorporate digital technologies should consider the intersection between disability and age and offer training and practice for the implemented technology [132]. Future research should explore ways to meet the needs of older adults with various impairments by designing technology that is as inclusive as possible [133]. In efforts to reduce inequities related to age and disability, strategies such as including individuals with disabilities (eg, dementia [134]) in technological development have been used [135].
The digital divide (ie, the disadvantage of those who are either unable or do not choose to use technologies) is the largest among older adults with low education, older adults with limited English proficiency, and certain racial or ethnic groups (eg, Hispanic or Black) [136,137]. Simultaneously, there are also cohorts of older adults that commonly face health inequities in low-income countries [138,139]. Many of the studies included in this review did not report the minority languages or race and ethnicity of the sample. Systematic reviews have noted inequalities and disparities in access to various health services among racial, ethnic, and language minorities [140,141]. To help overcome barriers to care for minority populations, reliable reporting of such characteristics is necessary to target improvement efforts to ensure equitable access to care [142]. Future studies should report on racial, ethnic, and cultural backgrounds and experiences to ensure that the needs and experiences of these groups are considered [143]. Moreover, future studies should include strategies for recruiting diverse groups of participants by offering technologies in different languages [144]; using racially, ethnically, and culturally diverse research staff [145,146]; and providing compensation for participation [146]. Carefully worded recruitment advertisements can also support gender diversity within these groups [147]. Highlighting the various genders incorporated into current interventions can help make research recommendations for including more diversity in future interventions and studying sex- and gender-based differences.
Limitations
In this secondary review of 34 articles describing the inclusion of older adult participants in hospital-to-home interventions, we experienced some limitations. First, our findings are limited to the data reported in the studies, and not all studies have reported particular characteristics (eg, education, race). Another limitation of our review is that we only included a synthesis of data that pertained to the SGBA+ framework and may have inadvertently excluded commentary on other meaningful measures of diversity (eg, immigration status). Second, we only included a synthesis of data that pertained to the SGBA+ framework and may have inadvertently excluded commentary on other meaningful measures of diversity (eg, immigration status). Third, our review was also limited by its rapid review methodology, whereby only one person screened the titles and abstracts in the larger review. In addition, we may have missed potentially relevant articles because of our use of a rapid methodology and searching for a limited number of databases. Fourth, there is a risk that articles may have been missed because of our search strategy, as digital health interventions are not described consistently [21]. However, it is worth noting that the intent of that study was not to capture all articles but to provide an overview of the literature [21]. Fifth, the results should be interpreted with caution, as we could not confidently determine which studies reported unique interventions versus the reported results of one intervention within multiple studies. Finally, we recommend that future studies examine digital health interventions in low- and middle-income countries, as our review is limited to digital health interventions in high-income countries.
Conclusions
To the best of our knowledge, this is the first review that has mapped the literature focusing on the characteristics of older adults included in studies of digital interventions supporting hospital-to-home transition. These findings suggest that the literature on digital health interventions tends to operationalize older adults as a homogenous group, ignoring the heterogeneity in older age definitions. In addition, few studies have reported on racial, ethnic, cultural, or gender diversity, which can facilitate a further digital divide among older adults. Inconsistency in the literature surrounding the characteristics of the included participants suggests a need for further study to better understand how digital technologies to support hospital-to-home transitions can be inclusive. Specifically, the SBGA+ framework can inform future research and interventions to support older adults during hospital-to-home transitions.
Acknowledgments
This study was funded by the Canadian Institute for Health Research through a Team Grant in Transitions in Care (FRN 165733).
Abbreviations
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- SGBA+
Sex- and Gender-Based Analysis Plus
Geographical spread of studies.
Supplementary table of study characteristics.
Targeted populations of the included studies.
Details of the participants (ie, actual sample).
List of research implications.
Footnotes
Conflicts of Interest: None declared.
References
- 1.Norlyk A, Deleuran CL, Martinsen B. Struggles with infrastructures of information concerning hospital-to-home transitions. Br J Community Nurs. 2020 Jan 02;25(1):10–5. doi: 10.12968/bjcn.2020.25.1.10. https://www.magonlinelibrary.com/doi/abs/10.12968/bjcn.2020.25.1.10?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed . [DOI] [PubMed] [Google Scholar]
- 2.Steele Gray C, Tang T, Armas A, Backo-Shannon M, Harvey S, Kuluski K, Loganathan M, Nie JX, Petrie J, Ramsay T, Reid R, Thavorn K, Upshur R, Wodchis WP, Nelson M. Building a digital bridge to support patient-centered care transitions from hospital to home for older adults with complex care needs: protocol for a co-design, implementation, and evaluation study. JMIR Res Protoc. 2020 Nov 25;9(11):e20220. doi: 10.2196/20220. https://www.researchprotocols.org/2020/11/e20220/ v9i11e20220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Markle-Reid M, Valaitis R, Bartholomew A, Fisher K, Fleck R, Ploeg J, Salerno J. An integrated hospital-to-home transitional care intervention for older adults with stroke and multimorbidity: a feasibility study. J Comorb. 2020 Apr 22;10:2235042X19900451. doi: 10.1177/2235042X19900451. https://journals.sagepub.com/doi/10.1177/2235042X19900451?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed .10.1177_2235042X19900451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kokorelias KM, Gignac MA, Naglie G, Rittenberg N, MacKenzie J, D'Souza S, Cameron JI. A grounded theory study to identify caregiving phases and support needs across the Alzheimer's disease trajectory. Disabil Rehabil. 2020 Jul 20;:1–10. doi: 10.1080/09638288.2020.1788655. [DOI] [PubMed] [Google Scholar]
- 5.Hestevik CH, Molin M, Debesay J, Bergland A, Bye A. Older patients' and their family caregivers' perceptions of food, meals and nutritional care in the transition between hospital and home care: a qualitative study. BMC Nutr. 2020 Mar 18;6:11. doi: 10.1186/s40795-020-00335-w. http://europepmc.org/abstract/MED/32206325 .335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen L, Xiao LD, Chamberlain D. An integrative review: challenges and opportunities for stroke survivors and caregivers in hospital to home transition care. J Adv Nurs. 2020 Sep;76(9):2253–65. doi: 10.1111/jan.14446. [DOI] [PubMed] [Google Scholar]
- 7.Schick-Makaroff K, Karimi-Dehkordi M, Cuthbertson L, Dixon D, Cohen SR, Hilliard N, Sawatzky R. Using patient- and family-reported outcome and experience measures across transitions of care for frail older adults living at home: a meta-narrative synthesis. Gerontologist. 2021 Apr 03;61(3):e23–38. doi: 10.1093/geront/gnz162. http://europepmc.org/abstract/MED/31942997 .5707329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Connolly T, Mahoney E. Stroke survivors' experiences transitioning from hospital to home. J Clin Nurs. 2018 Nov;27(21-22):3979–87. doi: 10.1111/jocn.14563. [DOI] [PubMed] [Google Scholar]
- 9.Isenberg SR, Killackey T, Saunders S, Scott M, Ernecoff NC, Bush SH, Varenbut J, Lovrics E, Stern MA, Hsu AT, Bernstein M, Zimmermann C, Wentlandt K, Mahtani R. "Going home [is] just a feel-good idea with no structure": a qualitative exploration of patient and family caregiver needs when transitioning from hospital to home in palliative care. J Pain Symptom Manage. 2021 Sep;62(3):e9–19. doi: 10.1016/j.jpainsymman.2021.02.026.S0885-3924(21)00213-X [DOI] [PubMed] [Google Scholar]
- 10.Nikbakht-Nasrabadi A, Mardanian-Dehkordi L, Taleghani F. Abandonment at the transition from hospital to home: family caregivers' experiences. Ethiop J Health Sci. 2021 May;31(3):525–32. doi: 10.4314/ejhs.v31i3.9. http://europepmc.org/abstract/MED/34483609 .jEJHS.v31.i3.pg525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mistiaen P, Francke AL, Poot E. Interventions aimed at reducing problems in adult patients discharged from hospital to home: a systematic meta-review. BMC Health Serv Res. 2007 Apr 04;7:47. doi: 10.1186/1472-6963-7-47. https://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-7-47 .1472-6963-7-47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Araujo de Carvalho I, Epping-Jordan J, Pot AM, Kelley E, Toro N, Thiyagarajan JA, Beard JR. Organizing integrated health-care services to meet older people's needs. Bull World Health Organ. 2017 Nov 01;95(11):756–63. doi: 10.2471/BLT.16.187617. http://europepmc.org/abstract/MED/29147056 .BLT.16.187617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Strengthening people-centred health systems in the WHO European region: a framework for action towards coordinated/integrated health services delivery (CIHSD) World Health Organization. 2016. [2022-04-02]. https://www.euro.who.int/__data/assets/pdf_file/0005/231692/e96929-replacement-CIHSD-Roadmap-171014b.pdf .
- 14.Daliri S, Bekker CL, Buurman BM, Scholte Op Reimer WJ, van den Bemt BJ, Karapinar-Çarkit F. Barriers and facilitators with medication use during the transition from hospital to home: a qualitative study among patients. BMC Health Serv Res. 2019 Mar 29;19(1):204. doi: 10.1186/s12913-019-4028-y. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-019-4028-y .10.1186/s12913-019-4028-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Suksatan W, Tankumpuan T. The effectiveness of transition care interventions from hospital to home on rehospitalization in older patients with heart failure: an integrative review. Home Health Care Manag Pract. 2021 Jun 03;34(1):63–71. doi: 10.1177/10848223211023887. [DOI] [Google Scholar]
- 16.Mesteig M, Helbostad JL, Sletvold O, Røsstad T, Saltvedt I. Unwanted incidents during transition of geriatric patients from hospital to home: a prospective observational study. BMC Health Serv Res. 2010 Jan 04;10:1. doi: 10.1186/1472-6963-10-1. https://bmchealthservres.biomedcentral.com/articles/10.1186/1472-6963-10-1 .1472-6963-10-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Storm M, Siemsen IM, Laugaland KA, Dyrstad DN, Aase K. Quality in transitional care of the elderly: key challenges and relevant improvement measures. Int J Integr Care. 2014 Apr;14:e013. doi: 10.5334/ijic.1194. http://europepmc.org/abstract/MED/24868196 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nelson ML, Armas A, Thombs R, Singh H, Fulton J, Cunningham HV, Munce S, Hitzig S, Bettger JP. Synthesising evidence regarding hospital to home transitions supported by volunteers of third sector organisations: a scoping review protocol. BMJ Open. 2021 Jul 05;11(7):e050479. doi: 10.1136/bmjopen-2021-050479. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=34226235 .bmjopen-2021-050479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fitzgerald Miller J, Piacentine LB, Weiss M. Coping difficulties after hospitalization. Clin Nurs Res. 2008 Nov;17(4):278–96. doi: 10.1177/1054773808325226.17/4/278 [DOI] [PubMed] [Google Scholar]
- 20.Ahmed L, Jensen D, Klotzbach L, Huntley G, Alexander A, Roger V, Rutten LF. Technology-enabled transitions of care in a collaborative effort between clinical medicine and public health: a population health case report. NAM Perspectives. 2016 Mar 31;6(3):1–7. doi: 10.31478/201603h. [DOI] [Google Scholar]
- 21.Singh H, Armas A, Law S, Tang T, Steele Gray C, Cunningham HV, Thombs R, Ellen M, Sritharan J, Nie JX, Plett D, Jarach CM, Thavorn K, Nelson ML. How digital health solutions align with the roles and functions that support hospital to home transitions for older adults: a rapid review study protocol. BMJ Open. 2021 Feb 25;11(2):e045596. doi: 10.1136/bmjopen-2020-045596. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=33632755 .bmjopen-2020-045596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holland DE, Vanderboom CE, Mandrekar J, Borah BJ, Dose AM, Ingram CJ, Griffin JM. A technology-enhanced model of care for transitional palliative care versus attention control for adult family caregivers in rural or medically underserved areas: study protocol for a randomized controlled trial. Trials. 2020 Oct 28;21(1):895. doi: 10.1186/s13063-020-04806-0. https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-020-04806-0 .10.1186/s13063-020-04806-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Øvretveit J. Digital technologies supporting person-centered integrated care - a perspective. Int J Integr Care. 2017 Sep 25;17(4):6. doi: 10.5334/ijic.3051. http://europepmc.org/abstract/MED/29588629 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bauer AM, Thielke SM, Katon W, Unützer J, Areán P. Aligning health information technologies with effective service delivery models to improve chronic disease care. Prev Med. 2014 Sep;66:167–72. doi: 10.1016/j.ypmed.2014.06.017. http://europepmc.org/abstract/MED/24963895 .S0091-7435(14)00218-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bauer AM, Hodsdon S, Hunter S, Choi Y, Bechtel J, Fortney JC. Lessons from the deployment of the SPIRIT app to support collaborative care for rural patients with complex psychiatric conditions. Proc ACM Int Conf Ubiquitous Comput. 2017 Sep;2017:772–80. doi: 10.1145/3123024.3125610. http://europepmc.org/abstract/MED/29075683 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bauer AM, Iles-Shih M, Ghomi RH, Rue T, Grover T, Kincler N, Miller M, Katon WJ. Acceptability of mHealth augmentation of collaborative care: a mixed methods pilot study. Gen Hosp Psychiatry. 2018;51:22–9. doi: 10.1016/j.genhosppsych.2017.11.010. http://europepmc.org/abstract/MED/29272712 .S0163-8343(17)30287-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Campion Jr JT, Vest JR, Ancker JS, Kaushal R, HITEC Investigators Patient encounters and care transitions in one community supported by automated query-based health information exchange. AMIA Annu Symp Proc. 2013 Nov 16;2013:175–84. http://europepmc.org/abstract/MED/24551330 . [PMC free article] [PubMed] [Google Scholar]
- 28.Samal L, Dykes PC, Greenberg J, Hasan O, Venkatesh AK, Volk LA, Bates DW. The current capabilities of health information technology to support care transitions. AMIA Annu Symp Proc. 2013 Nov 16;2013:1231. http://europepmc.org/abstract/MED/24551404 . [PMC free article] [PubMed] [Google Scholar]
- 29.Kohnke A, Cole ML, Bush RG. Incorporating UTAUT predictors for understanding home care patients' and clinician's acceptance of healthcare telemedicine equipment. J Technol Manag Innov. 2014 Jun 19;9(2):29–41. doi: 10.4067/s0718-27242014000200003. [DOI] [Google Scholar]
- 30.Kemp E, Trigg J, Beatty L, Christensen C, Dhillon HM, Maeder A, Williams PA, Koczwara B. Health literacy, digital health literacy and the implementation of digital health technologies in cancer care: the need for a strategic approach. Health Promot J Austr. 2021 Feb;32 Suppl 1:104–14. doi: 10.1002/hpja.387. [DOI] [PubMed] [Google Scholar]
- 31.Banbury A, Nancarrow S, Dart J, Gray L, Parkinson L. Telehealth interventions delivering home-based support group videoconferencing: systematic review. J Med Internet Res. 2018 Feb 02;20(2):e25. doi: 10.2196/jmir.8090. https://www.jmir.org/2018/2/e25/ v20i2e25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cuffaro L, Di Lorenzo F, Bonavita S, Tedeschi G, Leocani L, Lavorgna L. Dementia care and COVID-19 pandemic: a necessary digital revolution. Neurol Sci. 2020 Aug;41(8):1977–9. doi: 10.1007/s10072-020-04512-4. http://europepmc.org/abstract/MED/32556746 .10.1007/s10072-020-04512-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Su Z, McDonnell D, Liang B, Kue J, Li X, Šegalo S, Advani S, Flores BE, Wang J. Technology-based health solutions for cancer caregivers to better shoulder the impact of COVID-19: a systematic review protocol. Syst Rev. 2021 Feb 01;10(1):43. doi: 10.1186/s13643-021-01592-x. https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-021-01592-x .10.1186/s13643-021-01592-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Egan K. Digital technology, health and well-being and the Covid-19 pandemic: it's time to call forward informal carers from the back of the queue. Semin Oncol Nurs. 2020 Dec;36(6):151088. doi: 10.1016/j.soncn.2020.151088. http://europepmc.org/abstract/MED/33229183 .S0749-2081(20)30103-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Keesara S, Jonas A, Schulman K. Covid-19 and health care's digital revolution. N Engl J Med. 2020 Jun 04;382(23):e82. doi: 10.1056/NEJMp2005835. [DOI] [PubMed] [Google Scholar]
- 36.Lee S. COVID-19 amplifiers on health inequity among the older populations. Front Public Health. 2020 Jan 15;8:609695. doi: 10.3389/fpubh.2020.609695. doi: 10.3389/fpubh.2020.609695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shaw J, Brewer LC, Veinot T. Recommendations for health equity and virtual care arising from the COVID-19 pandemic: narrative review. JMIR Form Res. 2021 Apr 05;5(4):e23233. doi: 10.2196/23233. https://formative.jmir.org/2021/4/e23233/ v5i4e23233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.van Deursen AJ. Digital inequality during a pandemic: quantitative study of differences in COVID-19-related internet uses and outcomes among the general population. J Med Internet Res. 2020 Aug 20;22(8):e20073. doi: 10.2196/20073. https://www.jmir.org/2020/8/e20073/ v22i8e20073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McDonough CC. The effect of ageism on the digital divide among older adults. J Gerontol Geriatr Med. 2016 Jun 16;2(1):1–7. doi: 10.24966/ggm-8662/100008. [DOI] [Google Scholar]
- 40.Gitlow L. Technology use by older adults and barriers to using technology. Phys Occup Ther Geriatr. 2014 Aug 12;32(3):271–80. doi: 10.3109/02703181.2014.946640. [DOI] [Google Scholar]
- 41.Helsel BC, Williams JE, Lawson K, Liang J, Markowitz J. Telemedicine and mobile health technology are effective in the management of digestive diseases: a systematic review. Dig Dis Sci. 2018 Jun;63(6):1392–408. doi: 10.1007/s10620-018-5054-z.10.1007/s10620-018-5054-z [DOI] [PubMed] [Google Scholar]
- 42.Dinh-Le C, Chuang R, Chokshi S, Mann D. Wearable health technology and electronic health record integration: scoping review and future directions. JMIR Mhealth Uhealth. 2019 Sep 11;7(9):e12861. doi: 10.2196/12861. https://mhealth.jmir.org/2019/9/e12861/ v7i9e12861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yoon H, Jang Y, Vaughan PW, Garcia M. Older adults' internet use for health information: digital divide by race/ethnicity and socioeconomic status. J Appl Gerontol. 2020 Jan;39(1):105–10. doi: 10.1177/0733464818770772. [DOI] [PubMed] [Google Scholar]
- 44.Bauer GR, Churchill SM, Mahendran M, Walwyn C, Lizotte D, Villa-Rueda AA. Intersectionality in quantitative research: a systematic review of its emergence and applications of theory and methods. SSM Popul Health. 2021 Jun;14:100798. doi: 10.1016/j.ssmph.2021.100798. https://linkinghub.elsevier.com/retrieve/pii/S2352-8273(21)00073-2 .S2352-8273(21)00073-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Crenshaw KW. On intersectionality: essential writings. New York, NY, USA: The New Press; 2017. [Google Scholar]
- 46.Wang SY, Hsu SH, Aldridge MD, Cherlin E, Bradley E. Racial differences in health care transitions and hospice use at the end of life. J Palliat Med. 2019 Jun;22(6):619–27. doi: 10.1089/jpm.2018.0436. http://europepmc.org/abstract/MED/30615546 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ross LE, Gibson MF, Daley A, Steele LS, Williams CC. In spite of the system: a qualitatively-driven mixed methods analysis of the mental health services experiences of LGBTQ people living in poverty in Ontario, Canada. PLoS One. 2018 Aug 15;13(8):e0201437. doi: 10.1371/journal.pone.0201437. https://dx.plos.org/10.1371/journal.pone.0201437 .PONE-D-18-09154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Crawford A, Serhal E. Digital health equity and COVID-19: the innovation curve cannot reinforce the social gradient of health. J Med Internet Res. 2020 Jun 02;22(6):e19361. doi: 10.2196/19361. https://www.jmir.org/2020/6/e19361/ v22i6e19361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Digital bridge: using technology to support patient-centered care transitions from hospital to home (DB) Clinical Trials. 2021. [2022-04-02]. https://clinicaltrials.gov/ct2/show/NCT04287192 .
- 50.Langlois EV, Straus SE, Antony J, King VJ, Tricco AC. Using rapid reviews to strengthen health policy and systems and progress towards universal health coverage. BMJ Glob Health. 2019 Feb 5;4(1):e001178. doi: 10.1136/bmjgh-2018-001178. https://gh.bmj.com/lookup/pmidlookup?view=long&pmid=30899562 .bmjgh-2018-001178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Garritty C, Gartlehner G, Nussbaumer-Streit B, King VJ, Hamel C, Kamel C, Affengruber L, Stevens A. Cochrane Rapid Reviews Methods Group offers evidence-informed guidance to conduct rapid reviews. J Clin Epidemiol. 2021 Feb;130:13–22. doi: 10.1016/j.jclinepi.2020.10.007. https://linkinghub.elsevier.com/retrieve/pii/S0895-4356(20)31146-X .S0895-4356(20)31146-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Halas G, Schultz AS, Rothney J, Goertzen L, Wener P, Katz A. A scoping review protocol to map the research foci trends in tobacco control over the last decade. BMJ Open. 2015 Jan 28;5(1):e006643. doi: 10.1136/bmjopen-2014-006643. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=25631312 .bmjopen-2014-006643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Moore B, Poss C, Coast E, Lattof SR, van der Meulen Rodgers Y. The economics of abortion and its links with stigma: a secondary analysis from a scoping review on the economics of abortion. PLoS One. 2021 Feb 18;16(2):e0246238. doi: 10.1371/journal.pone.0246238. https://dx.plos.org/10.1371/journal.pone.0246238 .PONE-D-20-01150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.White GW, Gonda C, Peterson JJ, Drum CE, RRTC Expert Panel on Health Promotion Interventions Secondary analysis of a scoping review of health promotion interventions for persons with disabilities: do health promotion interventions for people with mobility impairments address secondary condition reduction and increased community participation? Disabil Health J. 2011 Apr;4(2):129–39. doi: 10.1016/j.dhjo.2010.05.002.S1936-6574(10)00036-1 [DOI] [PubMed] [Google Scholar]
- 55.Payne G, Payne J. Secondary analysis. In: Payne G, Payne J, editors. Key concepts in social research. Thousand Oaks, CA, USA: Sage Research Methods; 2004. pp. 214–9. [Google Scholar]
- 56.Tricco AC, Langlois EV. Rapid reviews to strengthen health policy and systems: a practical guide. World Health Organization. 2017. [2022-04-02]. https://www.who.int/alliance-hpsr/resources/publications/rapid-review-guide/en/
- 57.Daudt HM, van Mossel C, Scott SJ. Enhancing the scoping study methodology: a large, inter-professional team's experience with Arksey and O'Malley's framework. BMC Med Res Methodol. 2013 Mar 23;13:48. doi: 10.1186/1471-2288-13-48. https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/1471-2288-13-48 .1471-2288-13-48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005 Feb;8(1):19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 59.Tricco AC, Antony J, Zarin W, Strifler L, Ghassemi M, Ivory J, Perrier L, Hutton B, Moher D, Straus SE. A scoping review of rapid review methods. BMC Med. 2015 Sep 16;13:224. doi: 10.1186/s12916-015-0465-6. https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-015-0465-6 .10.1186/s12916-015-0465-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–41. doi: 10.1016/j.ijsu.2010.02.007. https://linkinghub.elsevier.com/retrieve/pii/S1743-9191(10)00040-3 .S1743-9191(10)00040-3 [DOI] [PubMed] [Google Scholar]
- 61.Gender-based analysis plus (GBA+) at CIHR. Canadian Institute of Health Service Research. 2019. [2022-04-02]. http://www.cihr-irsc.gc.ca/e/50968.html .
- 62.Doull M, Runnels VE, Tudiver S, Boscoe M. Appraising the evidence: applying sex- and gender-based analysis (SGBA) to Cochrane systematic reviews on cardiovascular diseases. J Womens Health (Larchmt) 2010 May;19(5):997–1003. doi: 10.1089/jwh.2009.1626. [DOI] [PubMed] [Google Scholar]
- 63.Subirana-Malaret M, Gahagan J, Parker R. Intersectionality and sex and gender-based analyses as promising approaches in addressing intimate partner violence treatment programs among LGBT couples: a scoping review. Cogent Soc Sci. 2019 Aug 01;5(1):1644982. doi: 10.1080/23311886.2019.1644982. [DOI] [Google Scholar]
- 64.Etherington C, Rodrigues IB, Giangregorio L, Graham ID, Hoens AM, Kasperavicius D, Kelly C, Moore JE, Ponzano M, Presseau J, Sibley KM, Straus S. Applying an intersectionality lens to the theoretical domains framework: a tool for thinking about how intersecting social identities and structures of power influence behaviour. BMC Med Res Methodol. 2020 Jun 26;20(1):169. doi: 10.1186/s12874-020-01056-1. https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-020-01056-1 .10.1186/s12874-020-01056-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hankivsky O, Grace D, Hunting G, Giesbrecht M, Fridkin A, Rudrum S, Ferlatte O, Clark N. An intersectionality-based policy analysis framework: critical reflections on a methodology for advancing equity. Int J Equity Health. 2014 Dec 10;13:119. doi: 10.1186/s12939-014-0119-x. https://equityhealthj.biomedcentral.com/articles/10.1186/s12939-014-0119-x .s12939-014-0119-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Johnson JL, Beaudet A. Sex and gender reporting in health research: why Canada should be a leader. Can J Public Health. 2012 Nov 08;104(1):e80–1. doi: 10.1007/BF03405660. http://europepmc.org/abstract/MED/23618110 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Johnson JL, Repta R. Sex and gender: beyond the binaries. In: Oliffe JL, Greaves L, editors. Designing and conducting gender, sex, and health research. Thousand Oaks, CA, USA: Sage Publications; 2012. pp. 17–38. [Google Scholar]
- 68.Systematic reviews, scoping reviews, and other knowledge syntheses. McGill Library. 2021. [2022-04-02]. https://libraryguides.mcgill.ca/knowledge-syntheses/updating .
- 69.World Bank country and lending groups. The World Bank. 2020. [2022-04-02]. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups .
- 70.Campbell BR, Ingersoll KS, Flickinger TE, Dillingham R. Bridging the digital health divide: toward equitable global access to mobile health interventions for people living with HIV. Expert Rev Anti Infect Ther. 2019 Mar;17(3):141–4. doi: 10.1080/14787210.2019.1578649. http://europepmc.org/abstract/MED/30721103 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Joe J, Demiris G. Older adults and mobile phones for health: a review. J Biomed Inform. 2013 Oct;46(5):947–54. doi: 10.1016/j.jbi.2013.06.008. https://linkinghub.elsevier.com/retrieve/pii/S1532-0464(13)00083-X .S1532-0464(13)00083-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Park LG, Howie-Esquivel J, Dracup K. A quantitative systematic review of the efficacy of mobile phone interventions to improve medication adherence. J Adv Nurs. 2014 Sep;70(9):1932–53. doi: 10.1111/jan.12400. [DOI] [PubMed] [Google Scholar]
- 73.Matthew-Maich N, Harris L, Ploeg J, Markle-Reid M, Valaitis R, Ibrahim S, Gafni A, Isaacs S. Designing, implementing, and evaluating mobile health technologies for managing chronic conditions in older adults: a scoping review. JMIR Mhealth Uhealth. 2016 Jun 09;4(2):e29. doi: 10.2196/mhealth.5127. https://mhealth.jmir.org/2016/2/e29/ v4i2e29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lilje SC, Olander E, Berglund J, Skillgate E, Anderberg P. Experiences of older adults with mobile phone text messaging as reminders of home exercises after specialized manual therapy for recurrent low back pain: a qualitative study. JMIR Mhealth Uhealth. 2017 Mar 30;5(3):e39. doi: 10.2196/mhealth.7184. https://mhealth.jmir.org/2017/3/e39/ v5i3e39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Bahr SJ, Solverson S, Schlidt A, Hack D, Smith JL, Ryan P. Integrated literature review of postdischarge telephone calls. West J Nurs Res. 2014 Jan;36(1):84–104. doi: 10.1177/0193945913491016.0193945913491016 [DOI] [PubMed] [Google Scholar]
- 76.The demographics of aging. Transgenerational. 2009. [2022-03-08]. http://transgenerational.org/aging/demographics.htm .
- 77.Babineau J. Product review: covidence (systematic review software) J Can Health Libr Assoc. 2014 Aug 01;35(2):68–71. doi: 10.5596/c14-016. [DOI] [Google Scholar]
- 78.Paré G, Trudel MC, Jaana M, Kitsiou S. Synthesizing information systems knowledge: a typology of literature reviews. Inf Manag. 2015 Mar;52(2):183–99. doi: 10.1016/j.im.2014.08.008. [DOI] [Google Scholar]
- 79.Moro Agud M, Menéndez Colino R, Mauleón Ladrero MD, Ruano Encinar M, Díez Sebastián J, Villamañán Bueno E, Herrero Ambrosio A, González Montalvo JI. Analysis of an electronic medication reconciliation and information at discharge programme for frail elderly patients. Int J Clin Pharm. 2016 Aug;38(4):996–1001. doi: 10.1007/s11096-016-0331-4.10.1007/s11096-016-0331-4 [DOI] [PubMed] [Google Scholar]
- 80.Aziz O, Atallah L, Lo B, Gray E, Athanasiou T, Darzi A, Yang GZ. Ear-worn body sensor network device: an objective tool for functional postoperative home recovery monitoring. J Am Med Inform Assoc. 2011;18(2):156–9. doi: 10.1136/jamia.2010.005173. http://europepmc.org/abstract/MED/21252051 .jamia.2010.005173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Boeni F, Hersberger KE, Arnet I. Success of a sustained pharmaceutical care service with electronic adherence monitoring in patient with diabetes over 12 months. BMJ Case Rep. 2015 Jun 02;2015:bcr2014208672. doi: 10.1136/bcr-2014-208672. http://europepmc.org/abstract/MED/26038379 .bcr-2014-208672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gao SS, Wang YJ, Zhang GX, Zhang WT. Rehabilitation guidance for hip fracture patients during the COVID-19 pandemic using chat software: a new model. J Back Musculoskelet Rehabil. 2021;34(3):337–42. doi: 10.3233/BMR-200324.BMR200324 [DOI] [PubMed] [Google Scholar]
- 83.Guidetti S, Gustavsson M, Tham K, Andersson M, Fors U, Ytterberg C. F@ce: a team-based, person-centred intervention for rehabilitation after stroke supported by information and communication technology - a feasibility study. BMC Neurol. 2020 Oct 23;20(1):387. doi: 10.1186/s12883-020-01968-x. https://bmcneurol.biomedcentral.com/articles/10.1186/s12883-020-01968-x .10.1186/s12883-020-01968-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Jonker LT, Lahr MM, Oonk MH, de Bock GH, van Leeuwen BL. Post-discharge telemonitoring of physical activity, vital signs, and patient-reported symptoms in older patients undergoing cancer surgery. Ann Surg Oncol. 2021 Oct;28(11):6512–22. doi: 10.1245/s10434-021-09707-3. http://europepmc.org/abstract/MED/33641013 .10.1245/s10434-021-09707-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Jonker LT, Plas M, de Bock GH, Buskens E, van Leeuwen BL, Lahr MM. Remote home monitoring of older surgical cancer patients: perspective on study implementation and feasibility. Ann Surg Oncol. 2021 Jan;28(1):67–78. doi: 10.1245/s10434-020-08705-1. http://europepmc.org/abstract/MED/32602060 .10.1245/s10434-020-08705-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Jørgensen BB, Gregersen M, Pallesen SH, Damsgaard EM. A group-based real-time videoconferencing telerehabilitation programme in recently discharged geriatric patients: a feasibility study. Eur Geriatr Med. 2021 Aug;12(4):801–8. doi: 10.1007/s41999-020-00444-6. http://europepmc.org/abstract/MED/33544388 .10.1007/s41999-020-00444-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lindhardt T, Nielsen MH. Older patients' use of technology for a post-discharge nutritional intervention - a mixed-methods feasibility study. Int J Med Inform. 2017 Jan;97:312–21. doi: 10.1016/j.ijmedinf.2016.10.017.S1386-5056(16)30232-5 [DOI] [PubMed] [Google Scholar]
- 88.Lyth J, Lind L, Persson HL, Wiréhn AB. Can a telemonitoring system lead to decreased hospitalization in elderly patients? J Telemed Telecare. 2021 Jan;27(1):46–53. doi: 10.1177/1357633X19858178. [DOI] [PubMed] [Google Scholar]
- 89.Mosca IE, Salvadori E, Gerli F, Fabbri L, Pancani S, Lucidi G, Lombardi G, Bocchi L, Pazzi S, Baglio F, Vannetti F, Sorbi S, Macchi C. Analysis of feasibility, adherence, and appreciation of a newly developed tele-rehabilitation program for people with MCI and VCI. Front Neurol. 2020 Nov 27;11:583368. doi: 10.3389/fneur.2020.583368. doi: 10.3389/fneur.2020.583368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Pedone C, Rossi FF, Cecere A, Costanzo L, Antonelli Incalzi R. Efficacy of a physician-led multiparametric telemonitoring system in very old adults with heart failure. J Am Geriatr Soc. 2015 Jun;63(6):1175–80. doi: 10.1111/jgs.13432. [DOI] [PubMed] [Google Scholar]
- 91.Piau A, Crissey R, Brechemier D, Balardy L, Nourhashemi F. A smartphone Chatbot application to optimize monitoring of older patients with cancer. Int J Med Inform. 2019 Aug;128:18–23. doi: 10.1016/j.ijmedinf.2019.05.013.S1386-5056(19)30210-2 [DOI] [PubMed] [Google Scholar]
- 92.Ortiz-Piña M, Molina-Garcia P, Femia P, Ashe MC, Martín-Martín L, Salazar-Graván S, Salas-Fariña Z, Prieto-Moreno R, Castellote-Caballero Y, Estevez-Lopez F, Ariza-Vega P. Effects of tele-rehabilitation compared with home-based in-person rehabilitation for older adult's function after hip fracture. Int J Environ Res Public Health. 2021 May 20;18(10):5493. doi: 10.3390/ijerph18105493. https://www.mdpi.com/resolver?pii=ijerph18105493 .ijerph18105493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sabir FR, Tomlinson J, Strickland-Hodge B, Smith H. Evaluating the connect with pharmacy web-based intervention to reduce hospital readmission for older people. Int J Clin Pharm. 2019 Oct;41(5):1239–46. doi: 10.1007/s11096-019-00887-3. http://europepmc.org/abstract/MED/31392581 .10.1007/s11096-019-00887-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Villani A, Malfatto G, Compare A, Della Rosa F, Bellardita L, Branzi G, Molinari E, Parati G. Clinical and psychological telemonitoring and telecare of high risk heart failure patients. J Telemed Telecare. 2014 Dec;20(8):468–75. doi: 10.1177/1357633X14555644.1357633X14555644 [DOI] [PubMed] [Google Scholar]
- 95.Amroze A, Field TS, Fouayzi H, Sundaresan D, Burns L, Garber L, Sadasivam RS, Mazor KM, Gurwitz JH, Cutrona SL. Use of electronic health record access and audit logs to identify physician actions following noninterruptive alert opening: descriptive study. JMIR Med Inform. 2019 Feb 07;7(1):e12650. doi: 10.2196/12650. https://medinform.jmir.org/2019/1/e12650/ v7i1e12650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Backman C, Harley A, Kuziemsky C, Mercer J, Peyton L. MyPath to home web-based application for the geriatric rehabilitation program at Bruyère continuing care: user-centered design and feasibility testing study. JMIR Form Res. 2020 Sep 14;4(9):e18169. doi: 10.2196/18169. https://formative.jmir.org/2020/9/e18169/ v4i9e18169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Gurwitz JH, Field TS, Ogarek J, Tjia J, Cutrona SL, Harrold LR, Gagne SJ, Preusse P, Donovan JL, Kanaan AO, Reed G, Garber L. An electronic health record-based intervention to increase follow-up office visits and decrease rehospitalization in older adults. J Am Geriatr Soc. 2014 May;62(5):865–71. doi: 10.1111/jgs.12798. http://europepmc.org/abstract/MED/24779524 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Hewner S, Seo JY. Informatics’ role in integrating population and patient-level knowledge to improve care transitions in complex chronic disease. Online J Nurs Inform. 2014 Jun 1;18(2) [Google Scholar]
- 99.Kim B, Hunt M, Muscedere J, Maslove DM, Lee J. Using consumer-grade physical activity trackers to measure frailty transitions in older critical care survivors: exploratory observational study. JMIR Aging. 2021 Feb 23;4(1):e19859. doi: 10.2196/19859. https://aging.jmir.org/2021/1/e19859/ v4i1e19859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Lafaro KJ, Raz DJ, Kim JY, Hite S, Ruel N, Varatkar G, Erhunmwunsee L, Melstrom L, Lee B, Singh G, Fong Y, Sun V. Pilot study of a telehealth perioperative physical activity intervention for older adults with cancer and their caregivers. Support Care Cancer. 2020 Aug;28(8):3867–76. doi: 10.1007/s00520-019-05230-0. http://europepmc.org/abstract/MED/31845007 .10.1007/s00520-019-05230-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Madigan E, Schmotzer BJ, Struk CJ, DiCarlo CM, Kikano G, Piña IL, Boxer RS. Home health care with telemonitoring improves health status for older adults with heart failure. Home Health Care Serv Q. 2013;32(1):57–74. doi: 10.1080/01621424.2012.755144. http://europepmc.org/abstract/MED/23438509 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.McCloskey R, Jarrett P, Stewart C, Keeping-Burke L. Recruitment and retention challenges in a technology-based study with older adults discharged from a geriatric rehabilitation unit. Rehabil Nurs. 2015;40(4):249–59. doi: 10.1002/rnj.149. [DOI] [PubMed] [Google Scholar]
- 103.McGillion MH, Duceppe E, Allan K, Marcucci M, Yang S, Johnson AP, Ross-Howe S, Peter E, Scott T, Ouellette C, Henry S, Le Manach Y, Paré G, Downey B, Carroll SL, Mills J, Turner A, Clyne W, Dvirnik N, Mierdel S, Poole L, Nelson M, Harvey V, Good A, Pettit S, Sanchez K, Harsha P, Mohajer D, Ponnambalam S, Bhavnani S, Lamy A, Whitlock R, Devereaux PJ, PROTECT Network Investigators Postoperative remote automated monitoring: need for and state of the science. Can J Cardiol. 2018 Jul;34(7):850–62. doi: 10.1016/j.cjca.2018.04.021. https://linkinghub.elsevier.com/retrieve/pii/S0828-282X(18)30319-2 .S0828-282X(18)30319-2 [DOI] [PubMed] [Google Scholar]
- 104.Sorensen A, Grotts JF, Tseng CH, Moreno G, Maranon R, Whitmire N, Viramontes O, Atkins S, Sefilyan E, Simmons JW, Mangione CM. A collaboration among primary care-based clinical pharmacists and community-based health coaches. J Am Geriatr Soc. 2021 Jan;69(1):68–76. doi: 10.1111/jgs.16839. http://europepmc.org/abstract/MED/33026662 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Whitehouse CR, Long JA, Maloney LM, Daniels K, Horowitz DA, Bowles KH. Feasibility of diabetes self-management telehealth education for older adults during transitions in care. Res Gerontol Nurs. 2020 May 01;13(3):138–45. doi: 10.3928/19404921-20191210-03. http://europepmc.org/abstract/MED/31834415 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.An J, Ryu HK, Lyu SJ, Yi HJ, Lee BH. Effects of preoperative telerehabilitation on muscle strength, range of motion, and functional outcomes in candidates for total knee arthroplasty: a single-blind randomized controlled trial. Int J Environ Res Public Health. 2021 Jun 04;18(11):6071. doi: 10.3390/ijerph18116071. https://www.mdpi.com/resolver?pii=ijerph18116071 .ijerph18116071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Liang HY, Hann Lin L, Yu Chang C, Mei Wu F, Yu S. Effectiveness of a nurse-led tele-homecare program for patients with multiple chronic illnesses and a high risk for readmission: a randomized controlled trial. J Nurs Scholarsh. 2021 Mar;53(2):161–70. doi: 10.1111/jnu.12622. [DOI] [PubMed] [Google Scholar]
- 108.Luo J, Dong X, Hu J. Effect of nursing intervention via a chatting tool on the rehabilitation of patients after total hip arthroplasty. J Orthop Surg Res. 2019 Dec 09;14(1):417. doi: 10.1186/s13018-019-1483-4. https://josr-online.biomedcentral.com/articles/10.1186/s13018-019-1483-4 .10.1186/s13018-019-1483-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Chen Y, Brennan N, Magrabi F. Is email an effective method for hospital discharge communication? A randomized controlled trial to examine delivery of computer-generated discharge summaries by email, fax, post and patient hand delivery. Int J Med Inform. 2010 Mar;79(3):167–72. doi: 10.1016/j.ijmedinf.2009.12.006.S1386-5056(10)00004-3 [DOI] [PubMed] [Google Scholar]
- 110.Wade R, Cartwright C, Shaw K. Factors relating to home telehealth acceptance and usage compliance. Risk Manag Healthc Policy. 2012;5:25–33. doi: 10.2147/RMHP.S30204. doi: 10.2147/RMHP.S30204.rmhp-5-025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Choi J, Jacelon CS, Kalmakis KA. Web-based, pictograph-formatted discharge instructions for low-literacy older adults after hip replacement surgery: findings of end-user evaluation of the website. Rehabil Nurs. 2017;42(5):254–61. doi: 10.1002/rnj.274. [DOI] [PubMed] [Google Scholar]
- 112.McGilton KS, Chu CH, Naglie G, van Wyk PM, Stewart S, Davis AM. Factors influencing outcomes of older adults after undergoing rehabilitation for hip fracture. J Am Geriatr Soc. 2016 Aug;64(8):1601–9. doi: 10.1111/jgs.14297. http://europepmc.org/abstract/MED/27351370 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Baltes PB, Smith J. New frontiers in the future of aging: from successful aging of the young old to the dilemmas of the fourth age. Gerontology. 2003;49(2):123–35. doi: 10.1159/000067946.67946 [DOI] [PubMed] [Google Scholar]
- 114.Lee SB, Oh JH, Park JH, Choi SP, Wee JH. Differences in youngest-old, middle-old, and oldest-old patients who visit the emergency department. Clin Exp Emerg Med. 2018 Dec;5(4):249–55. doi: 10.15441/ceem.17.261. doi: 10.15441/ceem.17.261.ceem.17.261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Higgs P, Gilleard C. Rethinking old age: theorising the fourth age. London, UK: Bloomsbury Publishing; 2015. [Google Scholar]
- 116.Wallace DC, Hirst PK. Community-based service use among the young, middle, and old old. Public Health Nurs. 1996 Aug;13(4):286–93. doi: 10.1111/j.1525-1446.1996.tb00252.x. [DOI] [PubMed] [Google Scholar]
- 117.Neves BB, Franz RL, Munteanu C, Baecker R, Ngo M. "My hand doesn't listen to me!": adoption and evaluation of a communication technology for the 'oldest old'. Proceedings of the 33rd Annual ACM Conference on Human Factors in Computing Systems; CHI '15; April 18-23, 2015; Seoul, South Korea. 2015. pp. 1593–602. [DOI] [Google Scholar]
- 118.Arbaje AI, Kansagara DL, Salanitro AH, Englander HL, Kripalani S, Jencks SF, Lindquist LA. Regardless of age: incorporating principles from geriatric medicine to improve care transitions for patients with complex needs. J Gen Intern Med. 2014 Jun;29(6):932–9. doi: 10.1007/s11606-013-2729-1. http://europepmc.org/abstract/MED/24557511 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Fox MT, Sidani S, Butler JI, Skinner MW, Macdonald M, Durocher E, Hunter KF, Wagg A, Weeks LE, MacLeod A, Dahlke S. Optimizing hospital-to-home transitions for older persons in rural communities: a participatory, multimethod study protocol. Implement Sci Commun. 2021 Jul 22;2(1):81. doi: 10.1186/s43058-021-00179-w. https://implementationsciencecomms.biomedcentral.com/articles/10.1186/s43058-021-00179-w .10.1186/s43058-021-00179-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Graham CL, Ivey SL, Neuhauser L. From hospital to home: assessing the transitional care needs of vulnerable seniors. Gerontologist. 2009 Feb;49(1):23–33. doi: 10.1093/geront/gnp005.gnp005 [DOI] [PubMed] [Google Scholar]
- 121.Callahan CM, Arling G, Tu W, Rosenman MB, Counsell SR, Stump TE, Hendrie HC. Transitions in care for older adults with and without dementia. J Am Geriatr Soc. 2012 May;60(5):813–20. doi: 10.1111/j.1532-5415.2012.03905.x. http://europepmc.org/abstract/MED/22587849 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Hirschman KB, Hodgson NA. Evidence-based interventions for transitions in care for individuals living with dementia. Gerontologist. 2018 Jan 18;58(suppl_1):S129–40. doi: 10.1093/geront/gnx152.4816738 [DOI] [PubMed] [Google Scholar]
- 123.Leniz J, Higginson IJ, Stewart R, Sleeman KE. Understanding which people with dementia are at risk of inappropriate care and avoidable transitions to hospital near the end-of-life: a retrospective cohort study. Age Ageing. 2019 Sep 01;48(5):672–9. doi: 10.1093/ageing/afz052.5499172 [DOI] [PubMed] [Google Scholar]
- 124.Vaportzis E, Clausen MG, Gow AJ. Older adults perceptions of technology and barriers to interacting with tablet computers: a focus group study. Front Psychol. 2017 Oct 04;8:1687. doi: 10.3389/fpsyg.2017.01687. doi: 10.3389/fpsyg.2017.01687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Portz JD, Bayliss EA, Bull S, Boxer RS, Bekelman DB, Gleason K, Czaja S. Using the technology acceptance model to explore user experience, intent to use, and use behavior of a patient portal among older adults with multiple chronic conditions: descriptive qualitative study. J Med Internet Res. 2019 Apr 08;21(4):e11604. doi: 10.2196/11604. https://www.jmir.org/2019/4/e11604/ v21i4e11604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Tirado-Morueta R, Aguaded-Gómez JI, Hernando-Gómez Á. The socio-demographic divide in internet usage moderated by digital literacy support. Technol Soc. 2018 Nov;55:47–55. doi: 10.1016/j.techsoc.2018.06.001. [DOI] [Google Scholar]
- 127.Kivimäki M, Batty GD, Pentti J, Shipley MJ, Sipilä PN, Nyberg ST, Suominen SB, Oksanen T, Stenholm S, Virtanen M, Marmot MG, Singh-Manoux A, Brunner EJ, Lindbohm JV, Ferrie JE, Vahtera J. Association between socioeconomic status and the development of mental and physical health conditions in adulthood: a multi-cohort study. Lancet Public Health. 2020 Mar;5(3):e140–9. doi: 10.1016/S2468-2667(19)30248-8. https://linkinghub.elsevier.com/retrieve/pii/S2468-2667(19)30248-8 .S2468-2667(19)30248-8 [DOI] [PubMed] [Google Scholar]
- 128.Beynon-Davies P, Hill R. Evaluating a digital divide index in a regional context. J Sys Inf Technol. 2007;9(1):46–59. doi: 10.1108/13287260710817683. [DOI] [Google Scholar]
- 129.Schroyen S, Meillon C, Marquet M, Dartigues JF, Pérès K, Amieva H. Subjective age in the oldest old: what is the association with disability and sensory impairment? J Am Acad Audiol. 2020 Apr;31(4):257–61. doi: 10.3766/jaaa.18087. [DOI] [PubMed] [Google Scholar]
- 130.Garfein AJ, Herzog AR. Robust aging among the young-old, old-old, and oldest-old. J Gerontol B Psychol Sci Soc Sci. 1995 Mar;50(2):S77–87. doi: 10.1093/geronb/50b.2.s77. [DOI] [PubMed] [Google Scholar]
- 131.Zhai Y. A call for addressing barriers to telemedicine: health disparities during the COVID-19 pandemic. Psychother Psychosom. 2021;90(1):64–6. doi: 10.1159/000509000. http://europepmc.org/abstract/MED/32498070 .000509000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.LoBuono DL, Leedahl SN, Maiocco E. Teaching technology to older adults: modalities used by student mentors and reasons for continued program participation. J Gerontol Nurs. 2020 Jan 01;46(1):14–20. doi: 10.3928/00989134-20191118-02. [DOI] [PubMed] [Google Scholar]
- 133.Jovanović M, De Angeli A, McNeill A, Coventry L. User requirements for inclusive technology for older adults. Int J Hum Comput Interact. 2021 May 12;37(20):1947–65. doi: 10.1080/10447318.2021.1921365. [DOI] [Google Scholar]
- 134.Orpwood R, Chadd J, Howcroft D, Sixsmith A, Torrington J, Gibson G, Chalfont G. Designing technology to improve quality of life for people with dementia: user-led approaches. Univ Access Inf Soc. 2010;9(3):249–59. doi: 10.1007/s10209-009-0172-1. [DOI] [Google Scholar]
- 135.Noel K, Ellison B. Inclusive innovation in telehealth. NPJ Digit Med. 2020 Jun 25;3:89. doi: 10.1038/s41746-020-0296-5. doi: 10.1038/s41746-020-0296-5.296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Thronson LR, Jackson SL, Chew LD. The pandemic of health care inequity. JAMA Netw Open. 2020 Oct 01;3(10):e2021767. doi: 10.1001/jamanetworkopen.2020.21767. https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.21767 .2771185 [DOI] [PubMed] [Google Scholar]
- 137.Romano MF, Sardella MV, Alboni F, Russo L, Mariotti R, Nicastro I, Barletta V, Di Bello V. Is the digital divide an obstacle to e-health? An analysis of the situation in Europe and in Italy. Telemed J E Health. 2015 Jan;21(1):24–35. doi: 10.1089/tmj.2014.0010. [DOI] [PubMed] [Google Scholar]
- 138.Jaffe DH, Lee L, Huynh S, Haskell TP. Health inequalities in the use of telehealth in the United States in the lens of COVID-19. Popul Health Manag. 2020 Oct;23(5):368–77. doi: 10.1089/pop.2020.0186. [DOI] [PubMed] [Google Scholar]
- 139.Garcia MA, Homan PA, García C, Brown TH. The color of COVID-19: structural racism and the disproportionate impact of the pandemic on older black and Latinx adults. J Gerontol B Psychol Sci Soc Sci. 2021 Feb 17;76(3):e75–80. doi: 10.1093/geronb/gbaa114. http://europepmc.org/abstract/MED/32756973 .5881410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Chauhan A, Walton M, Manias E, Walpola RL, Seale H, Latanik M, Leone D, Mears S, Harrison R. The safety of health care for ethnic minority patients: a systematic review. Int J Equity Health. 2020 Jul 08;19(1):118. doi: 10.1186/s12939-020-01223-2. https://equityhealthj.biomedcentral.com/articles/10.1186/s12939-020-01223-2 .10.1186/s12939-020-01223-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Watson H, Harrop D, Walton E, Young A, Soltani H. A systematic review of ethnic minority women's experiences of perinatal mental health conditions and services in Europe. PLoS One. 2019 Jan 29;14(1):e0210587. doi: 10.1371/journal.pone.0210587. https://dx.plos.org/10.1371/journal.pone.0210587 .PONE-D-18-30070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Fremont A, Lurie N. The role of racial and ethnic data collection in eliminating disparities in health care. In: Ver Ploeg M, Perrin E, editors. Eliminating health disparities: measurement and data needs. Washington, DC, USA: National Academies Press (US); 2004. pp. 202–31. [PubMed] [Google Scholar]
- 143.Green DO, Creswell JW, Shope RJ, Clark VL. Grounded theory and racial/ethnic diversity. In: Bryant A, Charmaz K, editors. The Sage handbook of grounded theory. Thousand Oaks, CA, USA: Sage Publications; 2007. pp. 472–92. [Google Scholar]
- 144.Casado BL, Negi NJ, Hong M. Culturally competent social work research: methodological considerations for research with language minorities. Soc Work. 2012 Jan;57(1):1–10. doi: 10.1093/sw/swr002. [DOI] [PubMed] [Google Scholar]
- 145.Ibrahim S, Sidani S. Strategies to recruit minority persons: a systematic review. J Immigr Minor Health. 2014 Oct;16(5):882–8. doi: 10.1007/s10903-013-9783-y. [DOI] [PubMed] [Google Scholar]
- 146.Waheed W, Hughes-Morley A, Woodham A, Allen G, Bower P. Overcoming barriers to recruiting ethnic minorities to mental health research: a typology of recruitment strategies. BMC Psychiatry. 2015 May 02;15:101. doi: 10.1186/s12888-015-0484-z. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-015-0484-z .10.1186/s12888-015-0484-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.van den Berg AC, Giest SN, Groeneveld SM, Kraaij W. Inclusivity in online platforms: recruitment strategies for improving participation of diverse sociodemographic groups. Public Adm Rev. 2020;80(6):989–1000. doi: 10.1111/puar.13215. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Geographical spread of studies.
Supplementary table of study characteristics.
Targeted populations of the included studies.
Details of the participants (ie, actual sample).
List of research implications.


