Editor:
We previously reported cardiac MRI findings in a cohort of patients with COVID-19 vaccine–associated myocarditis in an in-press article published online in Radiology in February 2022 (1). The majority of patients had mild imaging abnormalities at the time of acute symptoms. However, little is known about later evolution of the cardiac MRI abnormalities.
The institutional ethics committee approved this retrospective analysis and waived the requirement for written informed consent. Cardiac MRI examinations were performed at 1.5 T or 3.0 T (Siemens) and were analyzed blinded to all clinical information (Circle cmr42). Global longitudinal, circumferential, and radial strain was analyzed using feature-tracking analysis. Late gadolinium enhancement (LGE) was quantified by using a signal intensity threshold of 4 SD. Maximum native T1 and T2 were converted to z scores by using scanner-specific local reference values (1).
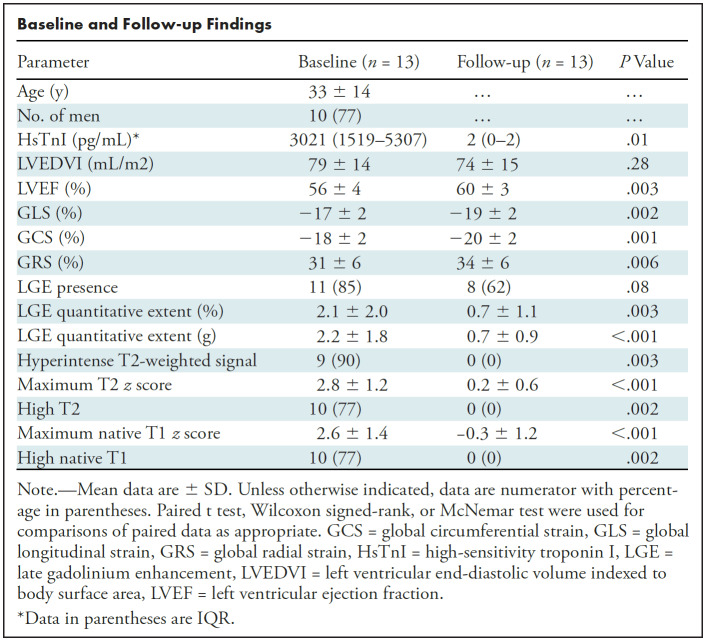
Thirteen patients underwent follow-up cardiac MRI (mean age, 33 years ± 14; 77% men) (Table). All patients presented with chest pain that followed mRNA-1273 in nine (69%) and BNT162b2 in four (31%) patients. Six patients (46%) required hospitalization. Six patients were treated with colchicine (46%), three were treated with aspirin (23%), and three were treated with ibuprofen (23%).
Baseline and Follow-up Findings
At follow-up MRI (median, 100 days after vaccination; IQR, 74–237), myocardial edema had resolved in all patients (Table). LGE had resolved in three of 13 (23%), decreased in eight of 13 (62%), and remained absent in two of 13 (15%) patients. In patients with residual LGE, the extent at follow-up was minimal (range, 1–2 g). Left ventricular ejection fraction increased and was normal in all at follow-up (56% ± 4 vs 60% ± 3; P = .003).
Median clinical follow-up duration was 159 days (IQR, 107–232 days). All patients were asymptomatic with normal troponin levels and no adverse cardiac events (death, sustained atrial or ventricular arrhythmia lasting ≥ 30 seconds, or heart failure hospitalization).
In summary, in our case series of 13 patients with acute myocarditis after COVID-19 vaccination, follow-up MRI showed resolution of myocardial edema, normalization of left ventricular function, and interval decrease in LGE. These findings are consistent with the typical rapid decrease in myocardial inflammation in other causes of myocarditis (2). However, minimal LGE without edema was present in 62% of patients at follow-up, likely reflecting myocardial fibrosis. In conjunction with lack of any adverse events at 5-month follow-up, this raises the likelihood that vaccine-associated myocarditis might have a favorable prognosis despite the persistence of minimal LGE.
Footnotes
Disclosures of conflicts of interest: M.F. No relevant relationships. P.T. No relevant relationships. G.R.K. No relevant relationships. H.A.Q. No relevant relationships. J.A.U. Grants to author institution from AstraZeneca, Bayer, Boehringer Ingelheim, Janssen, Novartis, Sanofi. R.M.W. No relevant relationships. K.M. Payment for lectures from Sanofi Genzyme, Amicus, Medscape; participation on a data safety board or advisory board from Sanofi Genzyme.
References
- 1. Fronza M, Thavendiranathan P, Chan V, et al. Myocardial Injury Pattern at MRI in COVID-19 Vaccine-associated Myocarditis. Radiology 2022;304(3):553–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sanchez Tijmes F, Thavendiranathan P, Udell JA, Seidman MA, Hanneman K. Cardiac MRI Assessment of Nonischemic Myocardial Inflammation: State of the Art Review and Update on Myocarditis Associated with COVID-19 Vaccination. Radiol Cardiothorac Imaging 2021;3(6):e210252. [DOI] [PMC free article] [PubMed] [Google Scholar]