Abstract
Background:
The use of minor field sterility in hand/upper extremity cases has been shown to improve workflow efficiency while maintaining patient safety. As this finding has been limited to specific procedures, we investigated the safety of performing a wide array of hand/upper extremity procedures outside the main operating room using minimal field sterility with Wide-Awake Local Anaesthesia No Tourniquet (WALANT) anaesthesia by evaluating superficial and deep infection rates across a diverse series of cases.
Methods:
This study was a case series conducted between October 2017 and June 2020. Of all, 217 patients underwent hand/upper extremity procedures performed in a minor procedure room via WALANT technique with field sterility. Primary outcome measures include superficial and deep surgical site infections within 14 days post-surgery.
Results:
Of all, 217 patients were included in this study; 265 consecutive hand/upper extremity operations were performed by a single surgeon, with notable case diversity. The majority of patients (n = 215, 99.1%) did not report or present with signs of infection before or after their operation. We report 0% 14-day and 0.37% 30-day surgical site infection rates for such hand/upper extremity procedures performed in a minor procedure room with field sterility.
Conclusion:
Hand/upper extremity procedures performed via WALANT technique with field sterility in a minor procedure room are associated with low surgical site infection rates. These rates are comparable to surgical site infection rates for similar surgeries performed in main operating rooms with standard sterilization procedures. Thus, the implementation of this technique may allow for improved workflow efficiency and reduced waste, all while maintaining patient safety.
Keywords: field sterility, hand, surgical site infection, WALANT
Abstract
Historique:
Il est démontré que le recours à un champ stérile mineur dans les interventions de la main et des extrémités supérieures améliore le déroulement du travail tout en maintenant la sécurité du patient. Comme cette observation se limite à des interventions particulières, les chercheurs ont examiné la sécurité d’un large éventail d’interventions de la main et des extrémités supérieures au moyen de la technique d’anesthésie de WALANT (acronyme anglais d'anesthésie locale en plein éveil sans tourniquet) hors de la salle d’opération principale. Pour ce faire, ils ont évalué le taux d’infections superficielles et profondes dans une série de cas variés.
Méthodologie:
La présente série de cas a été réalisée entre octobre 2017 et juin 2020. Au total, 217 patients ont subi une intervention mineure de la main ou des extrémités supérieures exécutée dans une salle d’intervention mineure sur champ stérile au moyen de la technique d’anesthésie de WALANT. Les mesures de résultat primaire incluaient des infections superficielles et profondes au foyer chirurgical dans les 14 jours suivant l’intervention.
Résultats:
Au total, 217 patients ont participé à l’étude. Un seul chirurgien a effectué 265 opérations consécutives de la main ou des extrémités supérieures, d’une diversité remarquable. La majorité des patients (n = 215, 99,1 %) n’ont pas déclaré ni présenté de signes d’infection avant ou après leur opération. Les chercheurs ont déclaré un taux d’infection de 0 % au foyer chirurgical au bout de 14 jours et de 0,37 % au bout de 30 jours pour les interventions de la main et des extrémités exécutées sur champ stérile dans une salle d’intervention mineure.
Conclusion:
Les interventions de la main et des extrémités supérieures exécutées sur champ stérile par la technique d’anesthésie de WALANT dans une salle d’intervention mineure sont liées à un faible taux d’infection au foyer chirurgical. Ces taux sont comparables à ceux des infections au foyer chirurgical lors d’interventions semblables exécutées dans une salle d’opération principale dotée d’interventions de stérilisation standard. Ainsi, la mise en œuvre de cette technique pourrait améliorer le déroulement du travail et réduire le gaspillage, tout en maintenant la sécurité du patient.
Introduction
Recent studies have demonstrated that moving common hand procedures from the main operating room (OR) to a minor procedure room provides benefits in waste reduction, cost-efficiency, time savings, and risk attenuation without compromising patient safety and satisfaction. 1 -10 In the setting of a small procedure room or clinic, the full OR sterile procedure can be consolidated to “minor field sterility.” This practice involves fewer disposable items, which results in a reduction of excess OR waste and costs. 11 Additionally, these procedure rooms require less preparation than the main OR, resulting in decreased turnover and wait times. 1,2,10 Minor field sterility in hand surgery has partially been made possible with the adoption of the Wide-Awake Local Anaesthesia No Tourniquet (WALANT) technique. With this technique, sedation is replaced with local anaesthesia that is administered by the surgeon rather than an anaesthesiologist. Tourniquet use is replaced with the addition of epinephrine to the anaesthetic injection. Decreased staffing and equipment use may further minimize costs. Codding et al 12 reports the additional benefit of decreased recovery times.
With its gaining popularity, it is important to consider risks that field sterility may pose, particularly, surgical site infection (SSI). LeBlanc et al 9 reports a low incidence of post-operative wound infection with field sterility in carpal tunnel release (CTR), and Rhee et al 6 reports similarly low rates in a variety of procedures performed at a military medical centre. In this study, we assessed the rate of SSI in a wide range of hand procedures using WALANT technique and field sterility practices. We expected to see a low incidence of SSIs, indicating that patient safety would be maintained under these circumstances.
Materials and Methods
After obtaining institutional review board approval, consent was obtained from consecutive patients undergoing hand/upper extremity surgery via WALANT technique, and they were prospectively enrolled in this study. All cases were performed at a single institution from October 1, 2017, to June 30, 2020. A single, board-certified and hand/microsurgery fellowship-trained orthopaedic surgeon performed all cases in the same ambulatory surgery outpatient procedure room with minor field sterility. The surgeon operates at this institution a half day a week on all pathology presenting to the hand clinic. From October 1, 2017, to January 1, 2019, only soft tissue surgeries were performed in the procedure room. However, this was broadened in January 2019 by the hospital administration to permit all patients with elbow-distal pathology the option of WALANT surgery in the procedure room, to include the implantation of hardware. Patients were excluded from the study if they had peripheral arterial disease, Raynaud’s disease, or scleroderma. These patients were operated on in the main OR utilizing Monitored Anaesthesia Care (MAC), regional or general anaesthesia. No patients were excluded based on pathology. Demographic information, including sex, age, race, and body mass index (BMI), were collected from patients’ electronic charts, and the Charlson Comorbidity Index (CCI) was calculated for each patient. The CCI provides weighted scores based on mortality risk of different medical conditions. 13
The minor field sterility procedure is as follows: One circulating nurse and one resident assisted the surgeon for each procedure. No surgical scrub technician was present for any operation. All surgeries were performed using the WALANT technique in a minor procedure room, outside the traditional OR setting. The room structures were not washed in between procedures, and there was no defined control of airflow within the procedure room. No preoperative prophylactic antibiotics were given for any case performed in this room. Prior to surgery, patients were taken to the holding area and consent was obtained. The incision site was prepped with betadine and 1% buffered lidocaine with epinephrine injected per WALANT technique. Patients then waited at least 27 minutes before the start of surgery for epinephrine to take effect. After this waiting period, patients were brought into the procedure room. Patients were dressed in their street clothing with their shoes on and did not wear a cap or gown. In the procedure room, the hand and forearm were prepped with Chloro-Prep, and draped with 4 surgical towels, with 1 towel around the elbow and 3 towels under the forearm. The surgeon used an alcohol-based surgical scrub and wore 1 set of surgical gloves for each procedure. A surgical mask was worn by the surgeon, in addition to scrubs and a cloth scrub cap (Figure 1).
Figure 1.

Intraoperative setup. Main surgical attending (left), accompanied by a resident surgeon (right), during a carpal tunnel release procedure. A surgical table is present in the minor procedure room and is managed entirely by the surgeons.
On a typical operating day at this minor procedure room, the surgeon obtains consent from and injects each patient within the first 30 minutes. Patients undergoing bony procedures are injected first and operated on last to ensure full anaesthetization, thus maximizing the amount of time the patients have to become numb. There is approximately a 5-minute turnover time between cases, during which the room is broken down, sheets are changed, the existing surgical instrument tray is replaced with a sterile one, and the sterile instruments are laid out (Figure 2 and Figure 3). There is no mopping or wiping down of surfaces unless visibly soiled.
Figure 2.
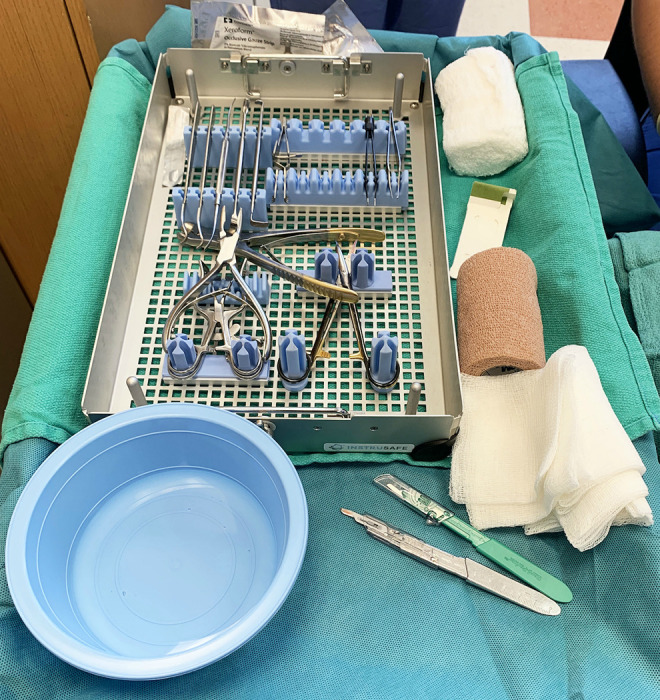
Surgical table present during CTR procedure. Close-up of surgical table in the minor operating room, holding a single-use tray of sterile instruments, sutures, wound dressing, gauze, Coban wrap, and a water basin.
Figure 3.
Surgical instruments used during CTR procedure. Instruments contained in a single use sterile tray for carpal tunnel releases.
With the exception of those undergoing fracture and tendon repairs, patients were instructed to remove their own dressing after 5 days, at which point normal hand hygiene with soap and water could resume. Upon discharge, patients were provided with return instructions, listing signs of post-operative infection to be vigilant of. Otherwise, patients were instructed to follow-up with their surgeon 2 weeks after their operation, except for patients with active, non-surgical infections or tendon repairs, who were instructed to return to clinic 1 week after surgery. No post-operative prophylactic antibiotics were prescribed for any case, and patients were instructed to use over-the-counter non-opioid analgesics as needed for pain control. At the follow-up appointment, the surgeon searched for potential post-operative infections and documented any signs of superficial or deep infection. Patients were directly contacted at these specified time points, and their medical records were further surveyed at the time of data collection for any additional visits or complications regarding their hand surgery.
Results
Data from a total of 217 patients was analyzed in this study. There was a 63:37 ratio between female and male patients, and the mean age was 45.0 years. The majority of analyzed patients were African-American (n = 167, 76.9%). The mean BMI was 28.1 kg/m 2, and the mean CCI was 1.21 (Table 1).
Table 1.
Patient Demographics.
| Patient demographics | n |
|---|---|
| Total patients | 217 |
| Mean age | 45.0 |
| Sex | |
| Male | 80 (36.9%) |
| Female | 137 (63.1%) |
| Race | |
| African-American | 167 (76.9%) |
| Caucasian | 8 (3.7%) |
| Other | 28 (12.9%) |
| Unknown | 14 (6.5%) |
| Mean BMI | 28.1 kg/m2 |
| Mean CCI | 1.21 |
| Insurance type | |
| Commercial insurance | 38 (17.5%) |
| Medicaid | 115 (53%) |
| Medicare | 8 (3.7%) |
| No insurance | 56 (25.8%) |
Abbreviations: BM, body mass index; CCI, Charlson Comorbidity Index.
Across the 217 patients analyzed, a total of 265 upper extremity procedures were performed. The most frequent procedures performed included mass excisions (21.5%), CTR (13.6%), and trigger finger release (TFR; 12.8%). A full list of procedures can be found in Table 2. Please see Supplemental Material Video 1, which demonstrates a wide awake forearm open reduction internal fixation (ORIF) procedure.
Table 2.
Catalogue of Performed Procedures.
| Procedure types | n |
|---|---|
| Mass excision | 57 |
| Carpal tunnel release (CTR) | 36 |
| Trigger finger release (TFR) | 34 |
| Flexor tendon repair/reconstruction | 25 |
| Wrist or forearm Open reduction internal fixation (ORIF) | 16 |
| Closed reduction percutaneous pinning | 15 |
| Extensor tendon repair | 13 |
| Amputation (interphalangeal (IP) level and ray) | 10 |
| Local hand flaps | 10 |
| Contracture releases | 9 |
| Tendon transfer—Forearm level | 8 |
| Major nerve reconstruction/grafting | 7 |
| Digital nerve repair | 7 |
| DeQuervain’s release (DQ) | 7 |
| Incision and drainage | 4 |
| Removal of deep hardware | 4 |
| Nail reconstructions | 3 |
Of the patients evaluated in this study, the vast majority (n = 215, 99.1%) did not report or present to the surgeon with any signs of infection before or after their operation and did not require post-operative care involving antibiotics. Prophylactic antibiotics were indicated for one patient presenting preoperatively to the clinic with an open injury and contaminated wound. Another patient presented to the clinic with eschar and active infection in his fourth digit. In both cases, antibiotics were prescribed post-operatively to treat the active infection. Antibiotics were not prescribed to prevent surgical-borne infections in any case.
Only one patient in this study developed a deep infection. The 29-year-old female patient initially underwent repair of the tendons of her small finger’s flexor digitorum superficialis and flexor digitorum profundus after suffering a laceration. The patient had an unremarkable 14-day post-operative visit and on day 28, after following up with a hand therapist, she was noted to have erythema and swelling of her small finger. She was seen the same day at the surgeon’s hand clinic, and was indicated for a same-day irrigation, debridement, and washout. She returned to the same minor operation room for this procedure 28 days after her first operation. Upon discharge, she was prescribed antibiotics. At her next follow-up, the infection had resolved, and she recovered unremarkably. No other surgical complications from this patient population were observed or reported. Overall, we observed a 0% 14-day infection rate, with a 0.37% deep (n = 1) and 0% superficial infection within the 30-day post-operative period, across this diverse case series.
Discussion
Across a wide variety of minor outpatient surgical procedures, we report a 0% 14-day SSI rate, and a 0.37% 30-day SSI rate. Additionally, prophylactic antibiotics were not prescribed except in cases of active infection prior to surgery. The low incidence of SSI following hand procedures in the main OR has been well-documented. Menendez et al 14 found a 14-day infection rate of 0.17% for all types of outpatient hand surgery, including CTR, DeQuervain’s release, TFR, wrist ganglion excision, cubital tunnel release, Dupuytren’s release, and basal joint arthroplasty. Since our patients were not prescribed pre- or post-operative prophylactic antibiotics, it is important to understand SSI rates specifically under these conditions as well as the fact that our patients’ surgeries were performed under minor field sterility. Multiple studies have found that there is no benefit to prophylactic antibiotics in clean hand surgery. 15 -19 Surgical site infection rates of 0.26%, 0.77%, and 0.70% in hand surgeries conducted with normal sterilization methods without antibiotic prophylaxis have been reported in the main OR. 17,19,20 Under this lens, our results are comparable to the reported literature.
The vulnerability to SSI in hand surgery conducted outside of the main OR is still being investigated, however, the current literature reports insignificant differences between settings. 9,21 Our results support a Canadian study comparing infection rates in CTR performed in main ORs and minor procedure rooms. Here, LeBlanc et al reports 14-day superficial and deep infection rates as 0.4% and 0%, respectively. 9 Rhee and colleagues published previously their experience on 100 WALANT patients. 6 While the vast majority were soft tissue cases, there were 9 finger fracture pinnings and 1 flexor tendon repair, and no plate fixations. This is considerably less diverse than our case list, which included 16 wrist/forearm plate fixation cases (3 both bone forearm and 13 distal radius open reduction internal fixation cases) in addition to a menagerie of other cases. Rhee et al reported a 1% superficial infection rate while also following field sterility protocols for their soft tissue cases—higher than our experience. 6
Hand surgery is a diverse practice, and thus surgeons may be unable to adjust their schedules to accommodate a workday outside of the main OR, particularly if field sterility is only applicable to one procedure type. By our demonstration of field sterility in a wider range of hand procedures, including complex hand and forearm procedures using hardware, hand surgeons and institutions may be able to justify the time and effort required to move an operating day into minor procedure rooms. While we did have 1 deep infection that occurred in a flexor tendon repair, 24 (96%) other flexor tendon repairs/reconstructions were performed without complications. We do not consider this procedure to be a contraindication to field sterility. Our study yields results comparable to previously published infection rates from similar procedures carried out in the main OR, and thus suggest that field sterility allows hand surgeries other than CTR to be performed safely in a minor procedure room.
The low incidence of SSIs within this case series is also notable given the demographics of our patient population. The vast majority of our patients hail from underserved backgrounds: 76.9% of patients reported their race as African-American, 25.8% were uninsured, and 53% reported Medicaid as their primary insurance. Underserved patients may report worse surgical outcomes, possibly due to socioeconomic barriers that prevent such patients from properly following post-operative instructions. 22 Sanford et al found increased SSI rates for African-American patients following spine surgery. 23 Studies investigating the rates of SSIs across different insurance statuses within the field of orthopaedic surgery have shown that Medicaid patients experience a significantly higher SSI rate than privately insured patients. 22,24,25 In contrast, we still observed a low SSI rate across our entire patient population. Thus, minor field sterility here is successful in maintaining low SSI rates for this medically underserved, minority population.
Use of the WALANT technique provides an added benefit of time efficiency to both the surgeon and the patient. This operative team achieved a turnover time of approximately 5 minutes, which is significantly shorter than turnover times of up to 66.5 minutes reported by other groups. 26,27 By removing the need for an anaesthesiology team and staggering lidocaine injections during the preoperative setup, there is an efficient workflow within the minor procedure room. 28 While this setup requires a considerable amount of scheduling on the surgeon’s part, it ensures higher operative efficiency and allows for more cases to be scheduled per day. The use of local anaesthesia also reduces post-operative recovery time substantially, increasing patient satisfaction. 29,30
It has been estimated that health care facilities in the United States (US) produce 4 billion pounds of waste per year, 30% to 70% of which is estimated to come from the OR. 11,29,30 Efforts to reduce surgical waste throughout the US have shown promising results. Examples of initiative focuses include proper waste sorting, 29,31 recycling blue polypropylene wrap used for surgical equipment sterilization, 30 -32 and streamlining surgical equipment trays and disposable packs. 32 -35 Moving hand procedures from the main OR to the minor OR accomplishes similar goals by minimizing surgical equipment use and reducing disposable material waste, as reported by Van Demark et al. 10 Their initiative saved $13,250.42 (US Dollars) and 2.8 tons of waste over a 14-month period including 1099 hand cases. Figure 4 displays the few waste materials generated during one procedure following our protocol. Waste reduction goes hand in hand with cost savings, making field sterility an attractive solution for institutions and their hand surgeons.
Figure 4.
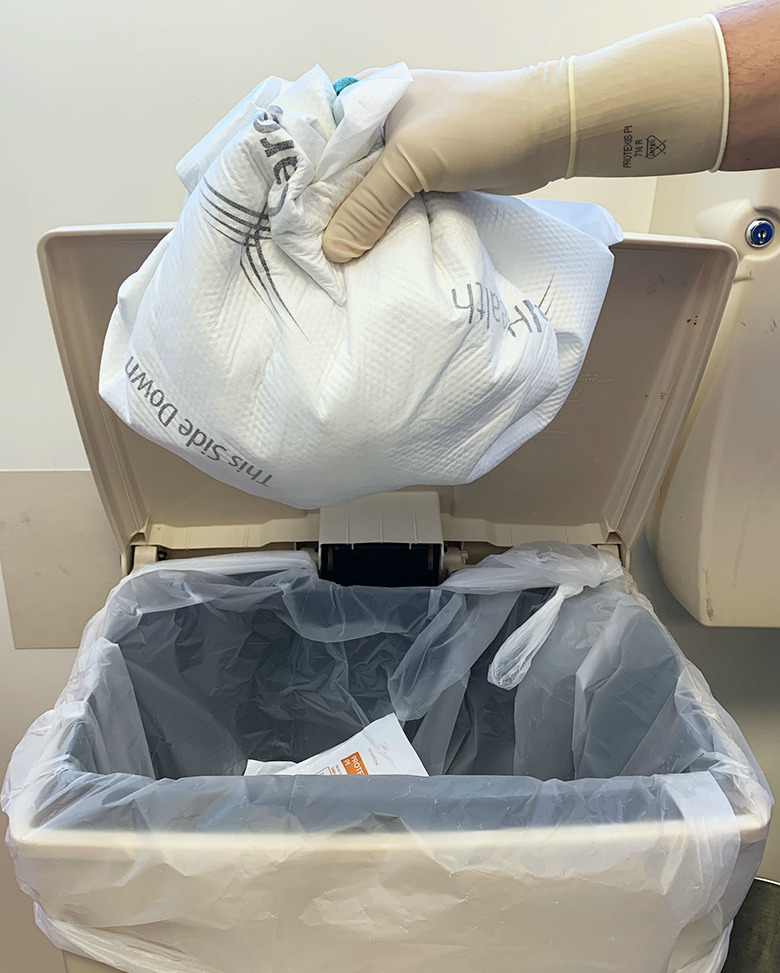
Collection of all disposable materials from one CTR procedure.
We are limited in our ability to make direct comparisons between full versus minor field sterility due to the nature of this study. Future research may include a control group receiving surgeries in the main OR with full sterility. However, we are able to compare the infection rates in main ORs from previously published studies and report similar rates. Our cohort was limited to one institution and one surgeon, impeding on the generalizability of our findings, but is an overall strength for this report. The small scale of this study allowed us to avoid confounding variables such as differences in procedure technique, supplies, and surgical experience. However, the small sample size is certainly a limitation, but intrinsic to the frequency with which this procedure room is utilized by the attending hand surgeon. The surgeon operates at this institution a half day a week on all pathology presenting to the hand clinic. While a diverse procedure list was included in our experience, there is a preponderance of soft tissue cases due to the fact that from October 1, 2017, to January 1, 2019, only soft tissue surgeries were performed in the procedure room. However, this was broadened in January 2019 by the hospital administration to permit all patients with elbow-distal pathology the option of WALANT surgery in the procedure room, to include the implantation of hardware—even including 16 wrist/forearm plate fixation cases (3 both bone forearm and 13 distal radius open reduction internal fixation cases). Future studies should document and compare cost-effectiveness, time efficiency, and waste reduction of field sterility in a diverse set of hand procedures across multiple institutions.
Conclusions
Updating current surgical practices may provide a multitude of benefits to the patients and surgeons, as well as the environment. The techniques discussed in this report may decrease turnover and wait times, improve cost-efficiency, and reduce waste without compromising patient safety. Our study provides evidence that a variety of hand and upper extremity procedures performed with the WALANT technique under minor field sterility conditions yield a low infection rate, comparable to previously published rates for surgeries performed in the main OR.
Supplemental Material
Supplemental Material, sj-docx-1-psg-10.1177_22925503211003840 for WALANT Hand and Upper Extremity Procedures Performed With Minor Field Sterility Are Associated With Low Infection Rates by Alba Avoricani, Qurratul-Ain Dar, Kenneth H. Levy, Joey S. Kurtzman and Steven M. Koehler in Plastic Surgery
Footnotes
Authors’ Note: Informed consent was obtained from all individual participants included in the study. Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Steven M. Koehler is a committee member of the American Society for Surgery of the Hand (ASSH), a paid consultant and speaker for Integra LifeSciences, Inc, a paid consultant for Tissium, Inc., a stockholder and member of the medical advisory board for Reactiv, Inc., a member of the advisory board for Androes, LLC, and a speaker for TriMed, Inc.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Steven M. Koehler, MD https://orcid.org/0000-0002-7690-2401
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Chatterjee A, McCarthy JE, Montagne SA, Leong K, Kerrigan CL. A cost, profit, and efficiency analysis of performing carpal tunnel surgery in the operating room versus the clinic setting in the United States. Ann Plast Surg. 2011;66(3):245–248. doi:10.1097/SAP.0b013e3181db7784 [DOI] [PubMed] [Google Scholar]
- 2. Leblanc MR, Lalonde J, Lalonde DH. A detailed cost and efficiency analysis of performing carpal tunnel surgery in the main operating room versus the ambulatory setting in Canada. Hand. 2007;2(4):173–178. doi:10.1007/s11552-007-9043-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Thomson CJ, Lalonde DH, Denkler KA, Feicht AJ. A critical look at the evidence for and against elective epinephrine use in the finger. Plast Reconstr Surg. 2007;119(1):260–266. doi:10.1097/01.prs.0000237039.71227.11 [DOI] [PubMed] [Google Scholar]
- 4. Kang SW, Park HM, Park JK, et al. Open cubital and carpal tunnel release using wide-awake technique: reduction of postoperative pain. J Pain Res. 2019;12:2725–2731. doi:10.2147/JPR.S210366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Alter TH, Warrender WJ, Liss FE, Ilyas AM. A cost analysis of carpal tunnel release surgery performed wide awake versus under sedation. Plast Reconstr Surg. 2018;142(6):1532–1538. doi:10.1097/PRS.0000000000004983 [DOI] [PubMed] [Google Scholar]
- 6. Rhee PC, Fischer MM, Rhee LS, McMillan H, Johnson AE. Cost savings and patient experiences of a clinic-based, wide-awake hand surgery program at a military medical center: a critical analysis of the first 100 procedures. J Hand Surg Am. 2017;42(3):e139–e147. doi:10.1016/j.jhsa.2016.11.019 [DOI] [PubMed] [Google Scholar]
- 7. Van Demark RE, Becker HA, Anderson MC, Smith VJS. Wide-awake anesthesia in the in-office procedure room: lessons learned. Hand. 2018;13(4):481–485. doi:10.1177/1558944717715120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lalonde D, Bell M, Benoit P, Sparkes G, Denkler K, Chang P. A multicenter prospective study of 3,110 consecutive cases of elective epinephrine use in the fingers and hand: the Dalhousie project clinical phase. J Hand Surg Am. 2005;30(5):1061–1067. doi:10.1016/j.jhsa.2005.05.006 [DOI] [PubMed] [Google Scholar]
- 9. LeBlanc MR, Lalonde DH, Thoma A, et al. Is main operating room sterility really necessary in carpal tunnel surgery? A multicenter prospective study of minor procedure room field sterility surgery. Hand. 2011;6(1):60–63. doi:10.1007/s11552-010-9301-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Van Demark RE, Smith VJS, Fiegen A. Lean and green hand surgery. J Hand Surg Am. 2018;43(2):179–181. doi:10.1016/j.jhsa.2017.11.007 [DOI] [PubMed] [Google Scholar]
- 11. Yu J, Ji TA, Craig M, McKee D, Lalonde DH. Evidence-based sterility: the evolving role of field sterility in skin and minor hand surgery. Plast Reconstr Surg—Glob Open. 2019;7(11):e2481. doi:10.1097/GOX.0000000000002481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Codding JL, Bhat SB, Ilyas AM. An economic analysis of MAC versus WALANT: a trigger finger release surgery case study. Hand. 2017;12(4):348–351. doi:10.1177/1558944716669693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi:10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 14. Menendez ME, Lu N, Unizony S, Choi HK, Ring D. Surgical site infection in hand surgery. Int Orthop. 2015;39(11):2191–2198. doi:10.1007/s00264-015-2849-9 [DOI] [PubMed] [Google Scholar]
- 15. Rizvi M, Bille B, Holtom P, Schnall SB. The role of prophylactic antibiotics in elective hand surgery. J Hand Surg Am. 2008;33(3):413–420. doi:10.1016/j.jhsa.2007.12.017 [DOI] [PubMed] [Google Scholar]
- 16. Whittaker J, Nancarrow J, Sterne G. The role of antibiotic prophylaxis in clean incised hand injuries: a prospective randomized placebo controlled double blind trial. J Hand Surg Am. 2005;30(2):162–167. doi:10.1016/J.JHSB.2004.10.015 [DOI] [PubMed] [Google Scholar]
- 17. Bykowski MR, Sivak WN, Cray J, Buterbaugh G, Imbriglia JE, Lee WPA. Assessing the impact of antibiotic prophylaxis in outpatient elective hand surgery: a single-center, retrospective review of 8,850 cases. J Hand Surg Am. 2011;36(11):1741–1747. doi:10.1016/j.jhsa.2011.08.005 [DOI] [PubMed] [Google Scholar]
- 18. Hoffman RD, Adams BD. The role of antibiotics in the management of elective and post-traumatic hand surgery. Hand Clin. 1998;14(4):657–666. [PubMed] [Google Scholar]
- 19. Tosti R, Fowler J, Dwyer J, Maltenfort M, Thoder JJ, Ilyas AM. Is antibiotic prophylaxis necessary in elective soft tissue hand surgery? Orthopedics. 2012;35(6):e829–e833. doi:10.3928/01477447-20120525-20 [DOI] [PubMed] [Google Scholar]
- 20. Harness NG, Inacio MC, Pfeil FF, Paxton LW. Rate of infection after carpal tunnel release surgery and effect of antibiotic prophylaxis. J Hand Surg Am. 2010;35(2):189–196. doi:10.1016/j.jhsa.2009.11.012 [DOI] [PubMed] [Google Scholar]
- 21. Jagodzinski NA, Ibish S, Furniss D. Surgical site infection after hand surgery outside the operating theatre: a systematic review. J Hand Surg Eur Vol. 2017;42(3):289–294. doi:10.1177/1753193416676408 [DOI] [PubMed] [Google Scholar]
- 22. Manoso MW, Cizik AM, Bransford RJ, Bellabarba C, Chapman J, Lee MJ. Medicaid status is associated with higher surgical site infection rates after spine surgery. Spine (Phila Pa 1976). 2014;39(20):1707–1713. doi:10.1097/BRS.0000000000000496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sanford Z, Taylor H, Fiorentino A, et al. Racial disparities in surgical outcomes after spine surgery: an ACS-NSQIP analysis. Glob Spine J. 2019;9(6):583–590. doi:10.1177/2192568218811633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Onyekwelu I, Yakkanti R, Protzer L, Pinkston CM, Tucker C, Seligson D. Surgical wound classification and surgical site infections in the orthopaedic patient. JAAOS Glob Res Rev. 2017;1(3):e022. doi:10.5435/jaaosglobal-d-17-00022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Browne JA, Novicoff WM, D’Apuzzo MR. Medicaid payer status is associated with in-hospital morbidity and resource utilization following primary total joint arthroplasty. J Bone Joint Surg Am. 2014;96(21):e180. doi:10.2106/JBJS.N.00133 [DOI] [PubMed] [Google Scholar]
- 26. Saha P, Pinjani A, Al-Shabibi N, Madari S, Ruston J, Magos A. Why we are wasting time in the operating theatre? Int J Health Plann Manage. 2009;24(3):225–232. doi:10.1002/hpm.966 [DOI] [PubMed] [Google Scholar]
- 27. Fletcher D, Edwards D, Tolchard S, Baker R, Berstock J. Improving theatre turnaround time. BMJ Qual Improv Rep. 2017;6(1): u219831.w8131. doi:10.1136/bmjquality.u219831.w8131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cerfolio RJ, Ferrari-Light D, Ren-Fielding C, et al. Improving operating room turnover time in a New York city academic hospital via lean. Ann Thorac Surg. 2019;107(4):1011–1016. doi:10.1016/j.athoracsur.2018.11.071 [DOI] [PubMed] [Google Scholar]
- 29. Lee RJ, Mears SC. Greening of orthopedic surgery. Orthopedics. 2012;35(6):e940–e944. doi:10.3928/01477447-20120525-39 [DOI] [PubMed] [Google Scholar]
- 30. Babu MA, Dalenberg AK, Goodsell G, Holloway AB, Belau MM, Link MJ. Greening the operating room: results of a scalable initiative to reduce waste and recover supply costs. Neurosurgery. 2019;85(3):432–437. doi:10.1093/neuros/nyy275 [DOI] [PubMed] [Google Scholar]
- 31. Kwakye G. Green surgical practices for health care. Arch Surg. 2011;146(2):131. doi:10.1001/archsurg.2010.343 [DOI] [PubMed] [Google Scholar]
- 32. Albert MG, Rothkopf DM. Operating room waste reduction in plastic and hand surgery. Plast Surg. 2015;23(4):235–238. doi:10.4172/plastic-surgery.1000941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Farrelly JS, Clemons C, Witkins S, et al. Surgical tray optimization as a simple means to decrease perioperative costs. J Surg Res. 2017;220:320–326. doi:10.1016/j.jss.2017.06.029 [DOI] [PubMed] [Google Scholar]
- 34. Dyas AR, Lovell KM, Balentine CJ, et al. Reducing cost and improving operating room efficiency: examination of surgical instrument processing. J Surg Res. 2018;229:15–19. doi:10.1016/j.jss.2018.03.038 [DOI] [PubMed] [Google Scholar]
- 35. Nast K, Swords KA. Decreasing operating room costs via reduction of surgical instruments. J Pediatr Urol. 2019;15(2):153.e1–153.e6. doi:10.1016/j.jpurol.2019.01.013 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-docx-1-psg-10.1177_22925503211003840 for WALANT Hand and Upper Extremity Procedures Performed With Minor Field Sterility Are Associated With Low Infection Rates by Alba Avoricani, Qurratul-Ain Dar, Kenneth H. Levy, Joey S. Kurtzman and Steven M. Koehler in Plastic Surgery



