Abstract
Background
Surgical treatment of displaced distal radius fractures (DRF) in older patients has increased, despite lacking evidence of its superiority over non-operative treatment. How treatment choice affects these patients after the initial 12-month period remains unknown. This study presents a clinical and radiographic follow up at an average of 3 years after treatment in the context of a randomized clinical trial comparing outcomes in patients aged ≥70 years, with a dorsally displaced distal radius fracture treated either surgically with volar locking plate or non-operatively.
Methods
Between 2009 and 2017, 140 patients aged ≥70 years with dorsally displaced DRF were randomized to surgery with volar locking plate (VLP) or non-operative treatment. At an average of 3 years after inclusion the participants were invited to an additional follow-up. The primary outcome was Patient Rated Wrist Evaluation (PRWE). Secondary outcomes included additional Patient Reported Outcome Measures (PROM), grip strength, range of motion, complications and radiological results.
Results
Sixty six patients were available for a 3 year follow-up, 33 in the non-operatively treated group and 33 in the VLP-group. The mean age at injury was 77 years. At 3 years the median PRWE was better (0 points) in the VLP-group than in the non-operative treatment group (9 points) p-value: 0.027. No statistically significant difference was found in Disabilities of the Arm, Hand, and Shoulder (DASH), EuroQol 5 Dimensions (EQ-5D) or grip strength. Total arc of range of motion was larger in the operatively treated group. No significant difference in osteoarthritis was found. Both groups had regained grip strength. The complication rate was similar. Outcomes improved from the 1 year to the 3 year follow-up.
Conclusions
Surgery with volar locking plate gave less long-term disability compared to non-operative treatment for severely displaced distal radius fractures in patients aged ≥70 years. Our findings were statistically significant but in the lower range of clinical importance.
Trial registration
The study was registered at : NCT02154620 03/06/2014 and NCT01268397 30/12/2010. Ethical approval was obtained from Ethical Committee in Stockholm, Sweden (2009/37–31/3, 2013/105–31/2, 2014/1041–32, 2017/611–32).
Keywords: Distal radius fracture, Geriatric fracture, Volar locking plate, Non-operative treatment, Fracture fixation, Aged, Quality of life
Introduction
Distal radius fracture (DRF) is the most common fracture in the general population. In the aged population it is the second most common after hip fracture [1, 2]. The incidence rate of distal radius fracture increases with age [1, 3–5] and women are more vulnerable due to a high rate of osteoporosis [6, 7].
Most DRF are treated non-operatively. If the fracture is unstable, non-operative treatment often results in displacement of the fracture and malunion. Surgical treatment with open reduction and internal fixation increases the probability of fracture healing in anatomical alignment [8, 9]. In younger adults malunion results in inferior function of the wrist and hand [10–13]. This correlation is weaker in older individuals [14] and becomes even weaker with increasing age [15]. Surgery with volar locking plates has become increasingly popular even in the oldest population [3, 16–19] despite inadequate scientific support [20–25]. To the best of our knowledge there are no publications presenting comparative treatment results in the oldest population beyond 2 years after injury. A study comparing the results between 6 and 12 months in geriatric patients shows decrease in PRWE during that timeline [26] and it’s unknown if the PRWE will continue to decrease and if any benefit seen at 1 year would still be present after an extended period of time. In younger patients, continuous improvement with regards to PROM has been reported beyond 1 year [27, 28].
The aim of this study was to perform a 3 year follow-up of individuals who, at time of DRF injury, were ≥ 70 years and randomized either to surgery with volar locking or non-operative treatment with closed reduction and cast immobilization. The primary outcome was Patient Rated Wrist Evaluation (PRWE) [29] score at 3 years and secondary outcomes include additional patient reported outcome measures (PROM), range of motion (ROM), grip strength, radiographic results and complications.
Material and methods
Design
This study is a 3 year follow-up of a previously published randomized controlled study [30] conducted at Södersjukhuset Hospital (SH) and Danderyd Hospital (DH), both level II trauma centers in Stockholm, Sweden. Patients participating in the original study were allocated to non-operative treatment or surgery with open reduction and fixation with a volar locking plate by one to one ratio. At DH inclusion of study participants took place between December 2009 and January 2017 and at SH, April 2013 to January 2017. Initially this was two separate studies including patients ≥75 but due to a low inclusion rate and similar study protocols they were merged in 2017. The DS study had DASH as the primary outcome while SH had PRWE, but the same data was obtained. The SH study had lowered the inclusion age to 70 years to increase the inclusion rate. The collection of data for the present study was conducted August 2016 – January 2020 and took place at Södersjukhuset hospital, department of orthopedic surgery. The study ended 3 years after the last patient of the original study had been asked to participate and been evaluated.
Participants
Patients were eligible for inclusion if they participated in the 1 year follow-up of the previously published study and 3 years had elapsed from injury. The DH patients included 2009–2011 were excluded from the study due to too long time elapse between fracture and start of the follow-up study. All eligible patients had presented to hospital with an acute dorsally displaced distal radius fracture, arbeitsgemeinschaft für osteosynthesefragen/Orthopaedic Trauma Association (AO/OTA) classification A and C with a dorsal tilt ≥20 degrees from a plane perpendicular to the length axis of the radius and met all inclusion criteria and none of the exclusion criteria listed in Table 1.
Table 1.
Inclusion and Exclusion Criteria of a randomized controlled study comparing non-operative treatment with volar locking plate in patients > 70 years of age
| Inclusion criteria | Patient age ≥ 75 years (≥70 years after September 2015 at SH) |
| Fracture diagnosed no more than 3 days from injury at SH or 6 days at DH | |
| Resident of the catchment area of either study site | |
| Wrist radiograph of ≥20°dorsal tilt from plane perpendicular to the length axis of the radius (or ≥ 4 mm ulnar variance at DH) | |
| Exclusion criteria | Associated ulna fracture |
| Intraarticular displacement exceeding 1 mm step-off or 1 mm gap (SH) | |
| Injury to the ipsilateral upper extremity | |
| High energy trauma (SH) | |
| Former disability at either wrist | |
| Rheumatoid arthritis or severe joint disorders | |
| Dementia or Pfeffer score < 5 at SH or < 8 at DH | |
| Substance abuse or psychiatric disorder | |
| Dependency in activities of daily living | |
| Not fit for surgery or American Society of Anesthesiology class ≥4 |
Interventions
Interventions have been described in detail in the previous publication [30]. All patients were treated with closed reduction and immobilization with a dorsal underarm splint. Patients allocated to non-operative treatment retained the splint for 4–5 weeks. Patients allocated to surgery were treated with open reduction and internal fixation with a volar locking plate. Implants used were 2.4-mm Variable Angle LCP Two-Column Volar Distal Radius Plate (DePuy Synthes), or DVR plate (ZimmerBiomet), Acu-Loc plate (Acumed) or Königsee plate (Swemac). All study participants were referred to an occupational therapist.
Follow-up
The present study contains data from an assessment conducted at 3 years after inclusion. Close to the three-year mark of injury patients were contacted by post and over the phone and were invited to participate. Patients who could not come for investigation exactly 3 years after injury were invited to participate at an occasion convenient to the patient even if it delayed the appointment. After signing a written consent, patients filled in PROM questionnaires and underwent radiographic and clinical examinations at an outpatient visit attended by an orthopedic surgeon from the study group and an independent occupational therapist. Some patients declined to come to the hospital for examination and radiography but provided PROM results by mailing their questionnaires. The study was registered at clinicaltrail.gov (NCT02154620 and NCT01268397). Ethical approval was obtained from Ethical Committee in Stockholm, Sweden (2009/37–31/3, 2013/105–31/2, 2014/1041–32, 2017/611–32).
Outcomes
The primary outcome of this 3 year follow-up was the score of Patient Rated Wrist evaluation (PRWE) [29, 31] 3 years after fracture. PRWE is a wrist-specific measure of function and pain where results from 15 factors translate to a continuous ordinal score ranging 0–100. Lower scores indicate less disability. The questionnaire has been validated for evaluation of distal radius fractures [29, 31–33]. Minimal clinical important difference (MCID) in PRWE-score for distal radius fractures has been suggested to be 11.5 points [34] but varies in different studies from 7.7–19 [35]. Disabilities of the Arm, Hand, and Shoulder (DASH) [36–38] was used as a secondary outcome. DASH ranges from 0 to 100 and the higher the number, the higher the disability. The MCID for DASH has been suggested to be 10 points [39]. Quality of life was assessed by EuroQol 5 dimensions 3 levels (EQ-5D 3 L) [40, 41] with the UK EQ-5D Index Tariff [41, 42]. The value 1 represents full quality of life and values closer to zero represent poorer quality of life. MCID is considered 0.074 points [43].
Measurement of grip strength and range of motion was performed by an unblinded occupational therapist. Grip strength was presented as absolute values in N/m2 and as percentages of the contralateral side. Grip strength was measured three consecutive times per hand using a Martin vigorimeter (Sammons Preston Rolyan). Results from right-handed individuals with an injury to the dominant hand were adjusted to compensate for 10% greater strength compared to the non-dominant hand [44]. Unadjusted percentages are also presented [45]. A goniometer was used to measure range of motion.
Radiographic evaluation of anteroposterior and lateral radiograph was performed by an experienced surgeon specialized in orthopedic and hand surgery (MW). Ulnar variance, dorsal tilt (presented as dorsal angulation from a plane perpendicular to the length axis of the radius), radial inclination and scapholunar angle were measured and presented in millimeters and degrees. Osteoarthritis in the radiocarpal and distal radioulnar joint was classified according to Knirk and Jupiter [46]. The presence of ulnar impaction was assessed and was defined as a radiographic conflict between the distal ulna and triquetrum or lunate in combination with signs of subchondral affection. Osteoarthritis and ulnar impaction were presented as the proportion of patients with positive radiological findings.
Complications were registered by reading medical charts and by an interview and clinical investigation of the patient. Assessment of medical charts was performed for patients who declined coming to the hospital.
Every participant was asked to score their overall impression of their wrist function 0–100 where 0 is worst possible and 100 is level of function before the injury. They were also asked whether they would recommend the treatment they were given to a friend in a similar situation.
Sample size
Sampling in this study was a convenience sampling from the original study cohort representing all available patients for which approximately 3 years had elapsed from injury.
The original sample size was set to 120 patients (SH) and 130 (DH), to allow for an estimated 20% (SH) and 25% (DH) drop out and to have 90% power to detect a difference of 10 points in PRWE with a significance level set to 0.05.
Randomization and blinding
The patients were randomized 1:1 to either treatment using randomly ordered sealed opaque envelopes. No stratification was used. Patients and researchers were not blinded to treatment. Research team and research nurse enrolled the patients and assigned patents to interventions.
Statistical methods
Intention to treat analyses were performed for all outcomes, meaning that analysis was conducted on the data from available patients as they were randomized. Most variables were not normally distributed and were therefore presented as medians with corresponding interquartile range (IQR). Means, 95% confidence intervals and ranges were also presented. Mann-Whitney U test was used to compare numerical values between groups. When the samples were related, Wilcoxon signed rank test was used. Categorical variables were presented as numbers and proportions expressed as percentages. Two-sided Fishers exact test and Chi-square test were used for group comparisons. Mixed models were used to analyze difference over time and interaction between time and treatment. Correlation between numerical values was investigated by scatterplots and ANOVA regression. SPSS Statistics 25 (IBM) was used for statistical analysis.
Results
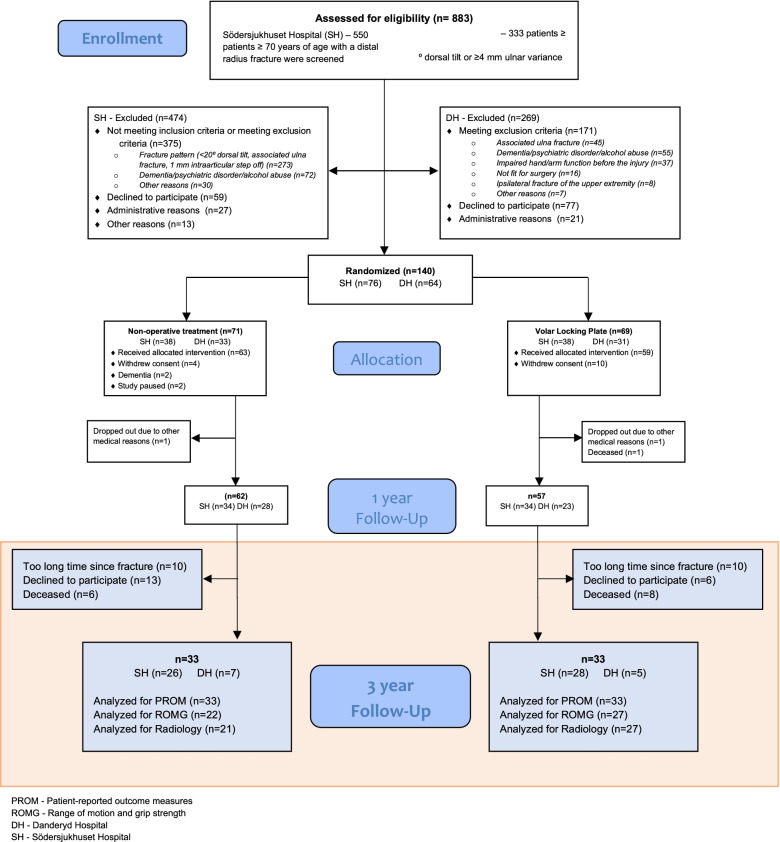
Out of 119 eligible study persons 66 patients were analyzed for the primary outcome (Fig. 1): 33 in the non-operative treatment group and 33 who were treated with a volar locking plate. Some patients were deceased, and some declined to participate for other reasons (Fig. 1). The baseline characteristics were similar between groups (Table 2). The patients available for follow-up after 3 years were younger than the patients not available. The distribution of gender and fracture characteristics did not differ between patients randomized for the one-year follow-up and the patients analyzed in the present study (Fishers Exact Test). The PRWE and DASH mean and median scores at the 1 year follow up did not differ between individuals participating in the 3 year follow-up and the individuals who did not participate, nor from the total population participating in the one-year follow-up (Mann-Whitney U-test). If there were any unmeasured differences between the groups remain unknown. The mean time for follow-up was 38 months, range 33–52 months.
Fig. 1.
CONSORT flow diagram of an RCT comparing treatments for dorsally displaced distal radius fractures
Table 2.
A presentation of demographic and radiologic parameters in patients fulfilling the one- and three-year follow-up of a randomized controlled study comparing non-operative treatment (non-op) with volar locking plate (VLP) in patients > 70 years of age
| Available at follow-up at 3 years (n = 66) |
Not available at follow-up at 3 years (n = 54) | |||
|---|---|---|---|---|
| Non-op n = 33 |
VLP n = 33 |
Non-op (n = 30) |
VLP (n = 24) |
|
| Median age at injury (range) | 76 (70–89) | 78 (70–90) | 80 (71–98) | 81 (75–89) |
| Female sex, n (%) | 27 (82%) | 32 (97%) | 28 (93%) | 22 (92%) |
| Injury to dominant hand, n (%) | 11 (33%) | 15 (45%) | 11 (37%) | 11 (46%) |
| AO/OTA-classification, n (%) | ||||
| A2 | 4 (12%) | 3 (9%) | 5 (17%) | 4 (17%) |
| A3 | 13 (39%) | 19 (58%) | 14 (47%) | 13 (54%) |
| B1 | 0 | 0 | 0 | 1 (4%) |
| B2 | 0 | 0 | 2 (7%) | 0 |
| B3 | 0 | 0 | 2 (7%) | 1 (4%) |
| C1 | 13 (39%) | 7 (21%) | 4 (13%) | 2 (8%) |
| C2 | 3 (9%) | 3 (9%) | 3 (10%) | 3 (13%) |
| C3 | 0 | 1 (3%) | 0 | 0 |
| Dorsal displacement at primary x-ray, degrees mean ± SD (median;IQR) | 27 ± 7 (27;12) | 30 ± 12 (30;18) | 27 ± 9 (27;9) | 26 ± 12 (26;18) |
| PRWE at 12 months mean ± SD (median;QR) | 22 ± 22 (15;39) | 15 ± 16 (9;23) | 23 ± 22 (16;34) | 11 ± 13 (6;17) |
n numbers, AO/OTA arbeitsgemeinschaft für osteosynthesefragen/Orthopaedic Trauma Association, SD standard deviation, IQR inter quartile range
Patient reported outcome measures
The median PRWE was lower (representing lower disability) in the volar locking plate group (0 points) compared to the non-operatively treated group (9 points) (p = 0.027, Mann-Whitney U-test), Fig. 2, Table 3. In DASH scores and EQ-5D, no statistically significant difference was found.
Fig. 2.
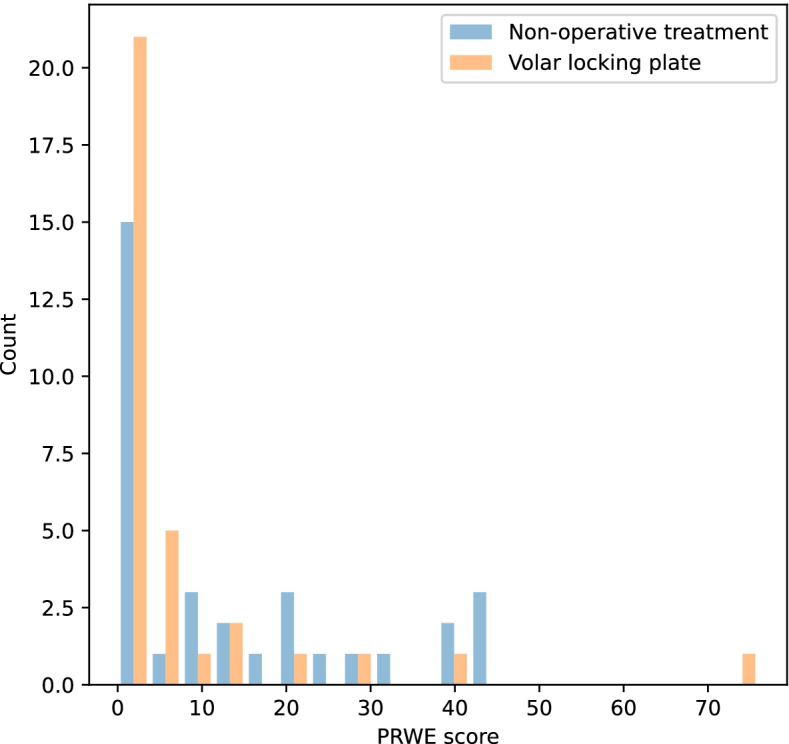
Histogram of PRWE (Patient Rated Wrist Evaluation) 3 years after a distal radius fracture in patients ≥70 years in a randomized to non-operative treatment or surgery with volar locking plate
Table 3.
Patient Reported Outcome Measures in patients included in the 3 year follow-up of a randomized controlled study comparing non-operative treatment with volar locking plate in patients > 70 years of age
| Outcome | Non-operative treatment N = 33 | Volar Locking Plate N = 33 | p-value |
|---|---|---|---|
| Mann-Whitney U-test | |||
| PRWE score (points) | |||
| Mean (95% CI) | 13 (8–19) | 7 (2–12) | |
| Median (IQR) | 9 (23) | 0 (7) | 0.027 |
| Range | 0–46 | 0–76 | |
| DASH score (points) | |||
| Mean (95% CI) | 15 (10–21) | 11 (5–16) | |
| Median (IQR) | 10 (18) | 3 (16) | 0.065 |
| Range | 0–57 | 0–63 | |
| EQ5D score (points) | |||
| Mean (95% CI) | 0.85(0.79–0.91) | 0.80(0.72–0.88) | |
| Median (IQR) | 0.80(0.24) | 0.80(0.31) | 0.311 |
| Range | 0.19–1 | −0.02-1 | |
CI confidence interval, IQR interquartile range
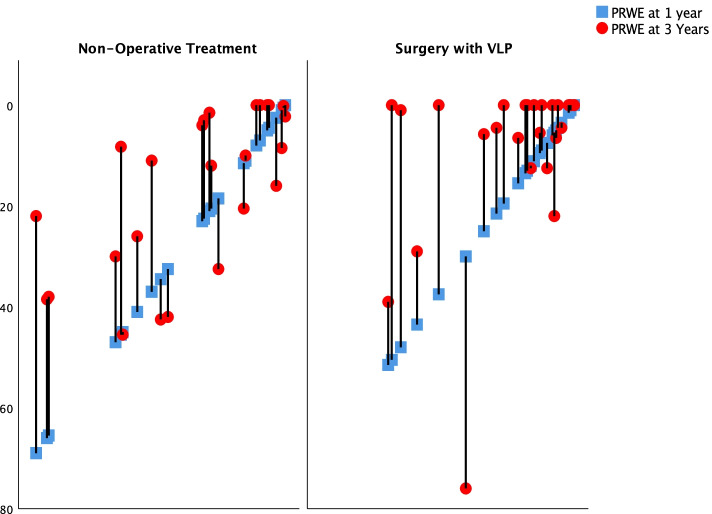
As a secondary outcome the differences between 1 and 3 years were explored. There was no significant difference in mean differences between one and 3 years between the treatment groups 95% CI (− 8) – (+ 9) (t-test). There was, however, a decrease in PRWE within each group between the 1 and 3 year follow-up (Fig. 3). In the VLP group the median PRWE decreased from 9 to 0 (p = 0.004) and in the non-operatively treated from 15 to 9 (p = 0.02) (Mann-Whitney U-test) representing a mean difference of − 7 (95% CI − 1 to − 14) for the VLP group versus − 8 (95% CI − 2 to − 14) for the non-operative group (t-test).
Fig. 3.
Sixty-six patients over the age of 70 sustained a dorsally displaced distal radius and were allocated to surgery with a volar plate or non-operative treatment. The diagram illustrates the change in Patient Rated Wrist Evaluation (PRWE) for each individual between the 1 year (blue square) and 3 year follow-up (red circle). The patients are displayed according to worst to best wrist-function (left to right) at 1 year
Range of motion and grip strength
Forty nine patients were clinically examined for range of motion (ROM) and grip strength (Table 4). There was no significant difference in grip strength between the groups (Mann-Whitney U-test). The group treated with volar locking plate had more volar flexion and, when compared to the non-injured side, a larger ROM in supination. Other ROM measurements were similar between groups. When comparing the total ROM with the contralateral hand there was a difference in favor of the volar locking plate group (Mann-Whitney U-test).
Table 4.
Range of motion and grip strength in patients included in the 3 years follow-up of a randomized controlled study comparing non-operative treatment with volar locking plate in patients > 70 years of age
| Non-operative treatment (n = 22) | Volar Locking Plate (n = 27) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | 95% CI | Median | IQR | Mean | SD | 95% CI | Median | IQR | p-value* | |
| Adjusted grip strength (%) | 97 | 20 | 89–106 | 93 | 17 | 100 | 17 | 93–107 | 104 | 27 | 0.191 |
| Grip strength % | 95 | 20 | 86–104 | 88 | 23 | 101 | 17 | 94–107 | 98 | 23 | 0.095 |
| Grip strength injured hand (N) | 22 | 9 | 18–25 | 20 | 9 | 20 | 4 | 19–22 | 19 | 5 | 0.904 |
| Dorsal extension (%) | 93 | 11 | 88–98 | 100 | 14 | 91 | 11 | 87–96 | 95 | 17 | 0.585 |
| Dorsal extension (°) | 56 | 8 | 52–59 | 56 | 11 | 54 | 8 | 50–57 | 55 | 10 | 0.465 |
| Volar flexion (%) | 81 | 24 | 71–91 | 76 | 34 | 96 | 25 | 86–106 | 100 | 11 | 0.005 |
| Volar flexion (°) | 61 | 15 | 54–68 | 60 | 21 | 68 | 17 | 61–75 | 72 | 20 | 0.022 |
| Flexion-extension arc range (%) | 86 | 14 | 79–92 | 86 | 20 | 93 | 14 | 87–99 | 95 | 14 | 0.015 |
| Flexion-extension arc range (°) | 117 | 19 | 108–125 | 114 | 29 | 122 | 19 | 115–129 | 126 | 22 | 0.150 |
| Ulnar deviation (%) | 97 | 17 | 89–104 | 100 | 0 | 105 | 15 | 100–112 | 100 | 9 | 0.192 |
| Ulnar deviation (°) | 26 | 5 | 24–29 | 30 | 9 | 29 | 5 | 27–31 | 30 | 5 | 0.157 |
| Radial deviation (%) | 93 | 12 | 88–98 | 100 | 13 | 99 | 19 | 92–107 | 100 | 9 | 0.224 |
| Radial deviation (°) | 24 | 5 | 22–27 | 25 | 10 | 23 | 4 | 22–25 | 23 | 5 | 0.437 |
| Radial-ulnar deviation arc (%) | 95 | 13 | 89–100 | 100 | 10 | 99 | 11 | 95–103 | 100 | 9 | 0.244 |
| Radial-ulnar deviation arc (°) | 51 | 9 | 47–55 | 53 | 10 | 52 | 6 | 50–55 | 50 | 9 | 0.824 |
| Supination (%) | 90 | 12 | 84–95 | 90 | 19 | 98 | 9 | 94–101 | 100 | 7 | 0.007 |
| Supination (°) | 102 | 15 | 70–120 | 110 | 21 | 109 | 15 | 104–115 | 110 | 16 | 0.100 |
| Pronation (%) | 95 | 6 | 93–98 | 100 | 11 | 98 | 9 | 94–101 | 100 | 0 | 0.073 |
| Pronation (°) | 86 | 8 | 83–90 | 87 | 10 | 88 | 9 | 85–92 | 90 | 7 | 0.130 |
| Total rotation range (%) | 92 | 8 | 88–96 | 93 | 15 | 98 | 6 | 95–100 | 93 | 15 | 0.016 |
| Total rotation range (°) | 188 | 21 | 179–197 | 197 | 34 | 198 | 20 | 190–206 | 205 | 30 | 0.107 |
| Total ROM (%) | 90 | 9 | 86–94 | 89 | 13 | 96 | 7 | 94–99 | 98 | 5 | 0.004 |
| Total ROM (°) | 356 | 43 | 337–375 | 353 | 74 | 372 | 32 | 359–384 | 370 | 58 | 0.157 |
Values in actual degrees (°) or in percentages of the contralateral side (%)
*Mann-Whitney U Test
Adjusted for dominant right hand by reducing the value to 0.9091 times the measured value
ROM Range of motion, CI confidence interval, N newton/m2, n numbers
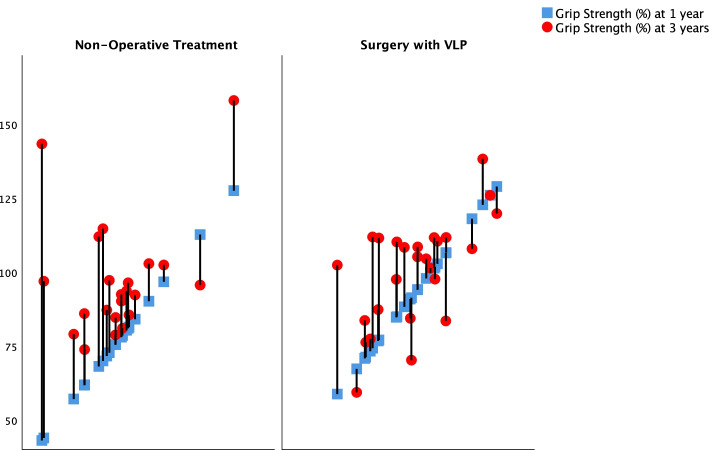
There was no statistically significant difference in the increase of corrected grip strength in percent of the non-injured hand over time between treatments (p = 0.068) using a mixed models analysis, with allocation and time as main effects and allocation combined with time as the interaction. An overall increase in grip strength not taking allocation under consideration was confirmed (p < 0.001). Within the non-operative treated group there was a statistically significant increase of median from 77 to 93% (p < 0.001). Within the VLP-group the increase from 93 to 105% was non-significant (p = 0.25) (Wilcoxon signed rank test) (Fig. 4).
Fig. 4.
Sixty-six patients over the age of 70 sustained a dorsally displaced distal radius and were allocated to surgery with a volar plate or non-operative treatment. The diagram illustrates the change in Corrected grip strength as a percent of the strength of the non-injured hand for each individual between the 1 year (blue square) and 3 year follow-up (red circle). The patients are displayed according to worst to best corrected grip strength (left to right) at 1 year
Radiographic outcome
There was no statistically significant difference in the prevalence of osteoarthritis (Table 5) (Fishers Exact test). The nonoperatively treated group had statistically significant greater dorsal tilt and ulnar variance, and less radial inclination (Table 6) (Mann-Whitney U-test). When performing a post-hoc ANOVA investigating dorsal angulation and PRWE, there was a statistically significant small correlation (r2 = 0.13) between larger dorsal tilt and lower PRWE outcome (p = 0.011).
Table 5.
Radiographic outcome in patients included in the 3 year follow-up of a randomized controlled study comparing non-operative treatment with volar locking plate in patients ≥70 years of age
| Non-operative treatment (n = 21) | Volar Locking Plate (n = 27) | P-Value | |
|---|---|---|---|
| Radiocarpal osteoarthritis | 0.738* | ||
| No osteoarthritis | 14 (67%) | 20 (77%) | |
| Grade 1 | 7 (33%) | 6 (23%) | |
| Grade 2 | 0 (0%) | 0 (0%) | |
| Grade 3 | 0 (0%) | 0 (0%) | |
| Ulnar Impaction | 9 (40.9%) | 5 (19.2%) | 0.122* |
| Distal ulnar radial joint osteoarthritis | 2(9.5%) | 3 (11.5%) | 1.000* |
| DISI | 5 (25%) | 5 (19.2%) | 0.726* |
Radiocarpal osteoarthritis according to Knirk and Jupiter,
* Fishers exact test
DISI Dorsal intercalated segment instability, Scapholunate angle > 80°
n = numbers
Table 6.
Radiographic outcome in patients included in the 3 years follow-up of a randomized controlled study comparing non-operative treatment with volar locking plate in patients > 70 years of age
| Non-operative treatment (n = 21) | Volar Locking Plate (n = 27) | P-value* | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | Std D | 95% CI | Median | IQR | Mean | Std D | 95% CI | Median | IQR | ||
| Dorsal tilt (°) | 11 | 10 | 6–16 | 15 | 20 | −3 | 8 | (−6)-1 | −5 | 12 | < 0.001 |
| Radial Inclination (°) | 16 | 6 | 13–18 | 15 | 5 | 21 | 4 | 20–23 | 21 | 6 | < 0.001 |
| Ulnar variance (mm) | 3 | 2 | 2–4 | 3 | 4 | 0.8 | 2 | 0–2 | 0 | 2 | 0.003 |
| Scapholunar angulation (°) | 71 | 10 | 67–75 | 70 | 14 | 67 | 9 | 63–70 | 69 | 13 | 0.272 |
n: numbers
°: degrees
Std D Standard deviation, CI confidence interval for the mean
* Mann-Whitney u-test
Complications
All complications are presented in Table 7. At the 3 year follow-up, eight of the 66 study patients had undergone additional surgery in the wrist or hand: 5 (15%) of the non-operatively treated and three (9%) of the surgically treated patients. Only one patient had a reoperation performed between the 1 year and the 3 year follow-up (a correction osteotomy in the non-operatively treated group).
Table 7.
Complications in patients included in a 3 year follow-up of a randomized controlled study comparing non-operative treatment with volar locking plate (VLP) in patients > 70 years of age
| Major complications | ||
| Non-operative treatment (n = 33) | Volar Locking Plate (n = 33) | |
| Additional surgery with VLP due to unacceptable secondary displacement | 1 | 0 |
| Corrective osteotomy | 2 | 0 |
| Plate extraction and carpal tunnel release | 0 | 1 |
| Plate extraction | 0 | 1 |
| Carpal tunnel release | 2 | 1 |
| Total | 5 (15%) | 3 (9%) |
| Minor complications | ||
| Non-operative treatment (n = 24) | Volar locking plate (n = 28) | |
| Numbness | 1 | 5 |
| Scar adherence | 0 | 1 |
| Ulnar pain | 4 | 1 |
| Total | 5 (21%) | 7 (25%) |
n numbers
Other
When patients were asked to rate their wrist on an overall 100-point scale, the VLP group rated their overall wrist function higher, with a median of 99 points (IQR 4), while the non-operative treated group rated their wrist at 80 points (IQR 25). This difference was statistically significant (p-value = 0.001) (Mann-Whitney U-test). 75% of patients treated non-operatively would recommend the treatment to a friend compared to 100% in the volar locking plate group (p = 0.007) (Fishers exact test).
Discussion
This 3 year follow-up of a randomized clinical trial of dorsally displaced distal radius fractures in a population over the age of 70 provided evidence of a benefit of surgical treatment with volar locking plate over non-operative treatment with respect to patient reported wrist function as measured by PRWE.
Our finding of a lower PRWE in the non-operatively treated group 3 years after treatment was statistically significant. The difference was present already at 1 year and did not change significantly between one and 3 years. The difference in PRWE medians between groups was 9 points and thus in the lower range of what has been suggested as the threshold for clinical significance that has been reported to vary between 7.7 and 19 [35]. In the context of a questionnaire outcome this might be due to a floor effect, where a large portion of the responders choose the lowest possible number in estimated disability. Floor values may be considered to reveal insufficient measuring qualities of the instrument used. It may also illustrate an acceptance of lost function, or rather a new idea of normal developing after 3 years where patients no longer perceive an acquired disability. Up to 9 months after an injury no flooring effects have been reported for the PRWE [47]. However, in this material, 3 years after injury, we had a considerable flooring effect, with a total of 46% of patients scoring 0 points and 67% of patients scored below 10 points. The low points we measured could clearly affect the MCID. We speculate that one cannot assume linearity of MCID along all values of PRWE, and different levels of MCID are probably relevant at different stages of recovery. The distribution of PRWE was skewed, which is a common feature for PROM results at long term follow up regardless diagnosis. Moreover, although a numerical value, PROM values cannot be considered an interval scale measurement. For these reasons non-parametric test of the medians was used for comparisons. Testing differences using the PROM means by parametric analysis would violate the assumption of normality.
This study was designed to evaluate potential differences in PRWE at 3 years after a distal radius fracture. Our choice of a region specific PROM as primary outcome, containing a pain scale and measuring function, is supported by other authors [48]. Many of our secondary outcome measures did not reveal significant differences between treatments 3 years after injury. All secondary outcomes in our study should be interpretated with caution firstly due to lack of power and secondly due to risk of random findings due to multiple sampling caused by the amount of outcome measures.
There was no difference in decrease rate in PRWE from 1 to 3 years between treatments but both groups showed improvement in PRWE, DASH as well as in grip strength between one and 3 years. The 95% CIs of mean differences for PRWE and DASH both involve MCID levels. It may be reassuring for patients to be informed that they can still expect improvement after 1 year.
Randomized trials similar to ours comparing non-operative treatment with volar locking plates in elderly patients have been carried out in the last decade but few studies present data beyond 1 year of follow-up. In contrast to our findings, most authors do not report any significant benefit of surgical treatment [9, 20, 22, 23, 25]. The inclusion criteria however differ between studies in both age range and degree of fracture displacement, making comparisons complicated. Arora et al. present no differences between groups at 12 months, but the fractures in their study healed in nearly anatomical positions, even in the non-operative group [20]. Lawson et al. showed no benefit as measured in PRWE in the RCT with patients > 60 years including fractures with more than 10-degrees of dorsal displacement [22]. At 12-months follow-up Egol et al. did not find surgery to be superior according to DASH, in a case control study of patients aged > 65 years. Their inclusion criteria may include patients with a less pronounced displacement [9]. Hassellund et al. designed a non-inferiority RCT including patients > 65 years with dorsal displacement of > 10 degrees. Non-operative treatment was not found to be inferior to surgical treatment according to quickDASH 12 months after fracture [23]. In our study we only included fractures dorsally displaced more than 20 degrees from a plane perpendicular to the length axis of the radius. We present an advantage with surgery valid for patients with severely displaced fractures, whereas other authors present results for mildly displaced fractures in which surgical treatment is not needed to achieve a good clinical outcome. Our finding of a correlation between increasing dorsal angulation and worse PRWE scores supports that opinion.
Our results, showing the benefits of surgical treatment in the long-term, are supported by Martinez-Mendez et al. [49] who investigated patients 60 years or older at least 24 months after injury and showed a superior outcome in the surgically treated group. Their radiologic inclusion criteria of initial displacement were not defined, but all included patients had a dorsal angulation of less than 15 degrees after closed reduction.
Even though many studies have been conducted investigating treatment of distal radius fractures in the aged population consensus on how these patients should be treated is still lacking. It could indicate that chronological age alone may not be sufficient for decision-making regarding treatment for displaced distal radius fractures. We speculate that other patient factors are more important. One factor that could be useful for treatment choice could be to judge functional levels in patients, as has been suggested by the Swedish guidelines for the management of distal radius fractures [50, 51].
According to our analysis of postoperative complications one correction osteotomy due to severe malunion with pain and loss of function was the only major complication occurring between 1 and 3 years after treatment. No flexor tendon ruptures were found in our material. Tendon injuries maybe expected to occur more often after volar plating in an ageing population as compared to younger individuals where tendon ruptures have been reported in 1–3% of patients surgically treated with a VLP [52–54]. However, the mean age of patients with complications has in fact shown to be lower than the mean age of patients without complications [52]. Generally, these complications are rare, and our study was not designed nor powered to detect and quantify rare complications. Future studies are needed to evaluate complication burdens after surgical treatment of older patients.
Strengths and limitations
In this study 3 years after injury, there was a significant loss to follow-up. Only 66 of eligible 119 patients were able to participate and thus our pre-determined sample-size calculations that were used for the one-year follow-up was not met at 3 years. This large study drop-out could introduce confounding factors earlier neutralized by randomization. Even though our presentation of demographic and radiographic features reveals no differences between our follow-up patient sample and the original cohort, it is unknown whether new selection bias was introduced by patients choosing not to participate. All cohorts of the age-group under study are challenging for long term follow-up. Some patients died and some patients were unable to complete the forms and make the trip to the hospital for examination. Baseline PROM data are missing, limiting the possibility to address missing data and confounding or preform sensitivity analysis. The injury had already happened when the patients were included and the attempt to collect PROM as before resulted in unreliable data. The lack of blinding is another limitation that could affected the patient’s perception of the result. This study included many secondary outcomes and in situations with multiple testing there is always a risk of finding differences by chance. The major strength of this study is its unique presentation of 3 year follow-up data of a randomized cohort of distal radius fracture patients in aged individuals (mean age at follow-up of 80 years). Previous publications encompass only 1 year of follow-up.
Conclusion
This study shows small but statistically significant less disability after surgery with volar locking plate compared to non-operative treatment with regards to PRWE 3 years after a dorsally displaced distal radius fracture in a population over the age of 70.
Acknowledgements
The authors wish to thank Elisabeth Skogman and Hans Pettersson for their contributions.
Abbreviations
- AO/OTA
Arbeitsgemeinschaft für osteosynthesefragen/Orthopaedic Trauma Association
- EQ-5D 3 L
EuroQol 5 dimensions 3 levels
- DH
Danderyd Hospital
- DRF
Distal radius fracture
- IQR
interquartile range
- MCID
Minimal Clinical Important Difference
- RCT
Randomized clinical trial
- ROM
Range of motion
- PROM
Patient reported outcome measures
- PRWE
Patient Rated Wrist Evaluation
- SH
Södersjukhuset Hospital
- VLP
volar locking plate
Authors’ contributions
HS: took part in the study design, data collection, data analysis and was a major contributor in writing the manuscript. SS: Data collection of the 1 year data of the DH patients, writing the manuscript. MW: Study design, Data collection by performing all the radiological analyses, writing the manuscript. JS: Data collection of the 1 year data of the SH patents, writing the manuscript. OS: Study design, writing the manuscript. CMN: study design, data collection, data analysis and was a major contributor in writing the manuscript. The authors read and approved the final manuscript.
Funding
Open access funding provided by Karolinska Institute. This study was funded by the Swedish Research Council and the Regional Agreement on Medical Training and Clinical Research between the Stockholm County Council and Karolinska Institute (ALF).
Availability of data and materials
The datasets generated and analysed during the current study are not publicly available due to limitations in the ethical approval but are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
All patients received written and oral information about the study and provided informed consent. They were informed about the possibility to withdraw at any point. Ethical approval was obtained from Swedish Ethical Review Authority in Stockholm, Sweden reference number: 2009/37–31/3, 2013/105–31/2, 2014/1041–32, 2017/611–32. These include both the original study and this extended three-year follow up. The study was performed according to the Helsinki declaration.
Consent for publication
Not applicable, no individual data is presented.
Competing interests
Non to declare.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Baron JA, Karagas M, Barrett J, Kniffin W, Malenka D, Mayor M, Keller RB. Basic epidemiology of fractures of the upper and lower limb among Americans over 65 years of age. Epidemiology. 1996;7(6):612–618. doi: 10.1097/00001648-199611000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37(8):691–697. doi: 10.1016/j.injury.2006.04.130. [DOI] [PubMed] [Google Scholar]
- 3.Mellstrand-Navarro C, Pettersson HJ, Tornqvist H, Ponzer S. The operative treatment of fractures of the distal radius is increasing: results from a nationwide Swedish study. Bone Joint J. 2014;96-b(7):963–969. doi: 10.1302/0301-620X.96B7.33149. [DOI] [PubMed] [Google Scholar]
- 4.Wilcke MK, Hammarberg H, Adolphson PY. Epidemiology and changed surgical treatment methods for fractures of the distal radius: a registry analysis of 42,583 patients in Stockholm County, Sweden, 2004-2010. Acta Orthop. 2013;84(3):292–296. doi: 10.3109/17453674.2013.792035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nellans KW, Kowalski E, Chung KC. The epidemiology of distal radius fractures. Hand Clin. 2012;28(2):113–125. doi: 10.1016/j.hcl.2012.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JA. Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA) Arch Osteoporos. 2013;8(1–2):136. doi: 10.1007/s11657-013-0136-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mallmin H, Ljunghall S. Distal radius fracture is an early sign of general osteoporosis: bone mass measurements in a population-based study. Osteoporosis Int. 1994;4(6):357–361. doi: 10.1007/BF01622198. [DOI] [PubMed] [Google Scholar]
- 8.Ochen Y, Peek J, van der Velde D, Beeres FJP, van Heijl M, Groenwold RHH, Houwert RM, Heng M. Operative vs nonoperative treatment of distal radius fractures in adults: a systematic review and Meta-analysis. JAMA Netw Open. 2020;3(4):e203497. doi: 10.1001/jamanetworkopen.2020.3497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Egol KA, Walsh M, Romo-Cardoso S, Dorsky S, Paksima N. Distal radial fractures in the elderly: operative compared with nonoperative treatment. J Bone Joint Surg Am. 2010;92(9):1851–1857. doi: 10.2106/JBJS.I.00968. [DOI] [PubMed] [Google Scholar]
- 10.McQueen M, Caspers J. Colles fracture: does the anatomical result affect the final function? J Bone J Surg Brit. 1988;70(4):649–651. doi: 10.1302/0301-620X.70B4.3403617. [DOI] [PubMed] [Google Scholar]
- 11.Foldhazy Z, Tornkvist H, Elmstedt E, Andersson G, Hagsten B, Ahrengart L. Long-term outcome of nonsurgically treated distal radius fractures. J Hand Surg. 2007;32(9):1374–1384. doi: 10.1016/j.jhsa.2007.08.019. [DOI] [PubMed] [Google Scholar]
- 12.Gartland JJ, Jr, Werley CW. Evaluation of healed Colles' fractures. J Bone Joint Surg Am. 1951;33-A(4):895–907. doi: 10.2106/00004623-195133040-00009. [DOI] [PubMed] [Google Scholar]
- 13.Gliatis JD, Plessas SJ, Davis TR. Outcome of distal radial fractures in young adults. J Hand Surg (Br) 2000;25(6):535–543. doi: 10.1054/jhsb.2000.0373. [DOI] [PubMed] [Google Scholar]
- 14.Blakeney WG. Stabilization and treatment of Colles' fractures in elderly patients. Clin Interv Aging. 2010;5:337–344. doi: 10.2147/CIA.S10042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grewal R, MacDermid JC. The risk of adverse outcomes in extra-articular distal radius fractures is increased with malalignment in patients of all ages but mitigated in older patients. J Hand Surg. 2007;32(7):962–970. doi: 10.1016/j.jhsa.2007.05.009. [DOI] [PubMed] [Google Scholar]
- 16.Chung KC, Shauver MJ, Yin H, Kim HM, Baser O, Birkmeyer JD. Variations in the use of internal fixation for distal radial fracture in the United States medicare population. J Bone Joint Surg Am. 2011;93(23):2154–2162. doi: 10.2106/JBJS.J.012802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huetteman HE, Shauver MJ, Malay S, Chung TT, Chung KC. Variation in the treatment of distal radius fractures in the United States: 2010 to 2015. Plast Reconstr Surg. 2019;143(1):159–167. doi: 10.1097/PRS.0000000000005088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jo YH, Lee BG, Kim JH, Lee CH, Kim SJ, Choi WS, Koo JW, Lee KH. National Surgical Trends for distal radius fractures in Korea. J Korean Med Sci. 2017;32(7):1181–1186. doi: 10.3346/jkms.2017.32.7.1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chung KC, Shauver MJ, Birkmeyer JD. Trends in the United States in the treatment of distal radial fractures in the elderly. J Bone Joint Surg Am. 2009;91(8):1868–1873. doi: 10.2106/JBJS.H.01297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arora R, Lutz M, Deml C, Krappinger D, Haug L, Gabl M. A prospective randomized trial comparing nonoperative treatment with volar locking plate fixation for displaced and unstable distal radial fractures in patients sixty-five years of age and older. J Bone Joint Surg Am. 2011;93(23):2146–2153. doi: 10.2106/JBJS.J.01597. [DOI] [PubMed] [Google Scholar]
- 21.Bartl C, Stengel D, Bruckner T, Gebhard F, Group OS The treatment of displaced intra-articular distal radius fractures in elderly patients. Dtsch Arztebl Int. 2014;111(46):779–787. doi: 10.3238/arztebl.2014.0779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lawson A, Naylor JM, Buchbinder R, Ivers R, Balogh ZJ, Smith P, Xuan W, Howard K, Vafa A, Perriman D, et al. Surgical plating vs closed reduction for fractures in the distal radius in older patients: a randomized clinical trial. JAMA Surg. 2021;156(3):229–237. doi: 10.1001/jamasurg.2020.5672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hassellund SS, Williksen JH, Laane MM, Pripp A, Rosales CP, Karlsen Ø, Madsen JE, Frihagen F. Cast immobilization is non-inferior to volar locking plates in relation to QuickDASH after one year in patients aged 65 years and older: a randomized controlled trial of displaced distal radius fractures. Bone Joint J. 2021;103-b(2):247–255. doi: 10.1302/0301-620X.103B2.BJJ-2020-0192.R2. [DOI] [PubMed] [Google Scholar]
- 24.Mellstrand Navarro C, Brolund A, Ekholm C, Heintz E, Hoxha Ekström E, Josefsson PO, Leander L, Nordström P, Zidén L, Stenström K. Treatment of radius or ulna fractures in the elderly: a systematic review covering effectiveness, safety, economic aspects and current practice. PLoS One. 2019;14(3):e0214362. doi: 10.1371/journal.pone.0214362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stephens AR, Presson AP, McFarland MM, Zhang C, Sirniö K, Mulders MAM, Schep NWL, Tyser AR, Kazmers NH. Volar locked plating versus closed reduction and casting for acute, displaced distal radial fractures in the elderly: a systematic review and Meta-analysis of randomized controlled trials. J Bone Joint Surg Am. 2020;102(14):1280–1288. doi: 10.2106/JBJS.19.01442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thorninger R, Wæver D, Pedersen J, Tvedegaard-Christensen J, Tjørnild M, Lind M, Rölfing JD. Objective outcome measures continue to improve from 6 to 12 months after conservatively treated distal radius fractures in the elderly-a prospective evaluation of 50 patients. J Clin Med. 2021;10:1831. 10.3390/jcm10091831. [DOI] [PMC free article] [PubMed]
- 27.Landgren M, Teurneau V, Abramo A, Geijer M, Tägil M. Intermediate-term outcome after distal radius fracture in patients with poor outcome at 1 year: a register study with a 2- to 12-year follow-up. J Hand Surg. 2019;44(1):39–45. doi: 10.1016/j.jhsa.2018.10.015. [DOI] [PubMed] [Google Scholar]
- 28.Costa ML, Achten J, Rangan A, Lamb SE, Parsons NR. Percutaneous fixation with Kirschner wires versus volar locking-plate fixation in adults with dorsally displaced fracture of distal radius: five-year follow-up of a randomized controlled trial. Bone Joint J. 2019;101-b(8):978–983. doi: 10.1302/0301-620X.101B8.BJJ-2018-1285.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.MacDermid JC, Turgeon T, Richards RS, Beadle M, Roth JH. Patient rating of wrist pain and disability: a reliable and valid measurement tool. J Orthop Trauma. 1998;12(8):577–586. doi: 10.1097/00005131-199811000-00009. [DOI] [PubMed] [Google Scholar]
- 30.Saving J, Severin Wahlgren S, Olsson K, Enocson A, Ponzer S, Sköldenberg O, Wilcke M, Mellstrand Navarro C. Nonoperative treatment compared with volar locking plate fixation for dorsally displaced distal radial fractures in the elderly: a randomized controlled trial. J Bone Joint Surg Am. 2019;101(11):961–969. doi: 10.2106/JBJS.18.00768. [DOI] [PubMed] [Google Scholar]
- 31.Mellstrand Navarro C, Ponzer S, Tornkvist H, Ahrengart L, Bergstrom G. Measuring outcome after wrist injury: translation and validation of the Swedish version of the patient-rated wrist evaluation (PRWE-Swe) BMC Musculoskelet Disord. 2011;12:171. doi: 10.1186/1471-2474-12-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.MacDermid JC. Development of a scale for patient rating of wrist pain and disability. J Hand Ther. 1996;9(2):178–183. doi: 10.1016/S0894-1130(96)80076-7. [DOI] [PubMed] [Google Scholar]
- 33.Kleinlugtenbelt YV, Nienhuis RW, Bhandari M, Goslings JC, Poolman RW, Scholtes VA. Are validated outcome measures used in distal radial fractures truly valid? A critical assessment using the COnsensus-based standards for the selection of health measurement INstruments (COSMIN) checklist. Bone Joint Res. 2016;5(4):153–161. doi: 10.1302/2046-3758.54.2000462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Walenkamp MM, de Muinck Keizer RJ, Goslings JC, Vos LM, Rosenwasser MP, Schep NW. The minimum clinically important difference of the patient-rated wrist evaluation score for patients with distal radius fractures. Clin Orthop Relat Res. 2015;473(10):3235–3241. doi: 10.1007/s11999-015-4376-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mehta SP, MacDermid JC, Richardson J, MacIntyre NJ, Grewal R. A systematic review of the measurement properties of the patient-rated wrist evaluation. J Orthop Sports Phys Ther. 2015;45(4):289–298. doi: 10.2519/jospt.2015.5236. [DOI] [PubMed] [Google Scholar]
- 36.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The upper extremity collaborative group (UECG) Am J Ind Med. 1996;29(6):602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 37.Atroshi I, Gummesson C, Andersson B, Dahlgren E, Johansson A. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: reliability and validity of the Swedish version evaluated in 176 patients. Acta Orthop Scand. 2000;71(6):613–618. doi: 10.1080/000164700317362262. [DOI] [PubMed] [Google Scholar]
- 38.Gummesson C, Atroshi I, Ekdahl C. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord. 2003;4:11. doi: 10.1186/1471-2474-4-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Roy JS, MacDermid JC, Woodhouse LJ. Measuring shoulder function: a systematic review of four questionnaires. Arthritis Rheum. 2009;61(5):623–632. doi: 10.1002/art.24396. [DOI] [PubMed] [Google Scholar]
- 40.The EuroQol group. EuroQol--a new facility for the measurement of health-related quality of life. Health policy (Amsterdam, Netherlands). 1990;16(3):199–208. [DOI] [PubMed]
- 41.Rundgren J, Enocson A, Mellstrand Navarro C, Bergström G. Responsiveness of EQ-5D in patients with a distal radius fracture. Hand (New York, NY) 2018;13(5):572–580. doi: 10.1177/1558944717725378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kind P, Dolan P, Gudex C, Williams A. Variations in population health status: results from a United Kingdom national questionnaire survey. BMJ (Clinical research ed) 1998;316(7133):736–741. doi: 10.1136/bmj.316.7133.736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Walters SJ, Brazier JE. Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual Life Res. 2005;14(6):1523–1532. doi: 10.1007/s11136-004-7713-0. [DOI] [PubMed] [Google Scholar]
- 44.Crosby CA, Wehbé MA, Mawr B. Hand strength: normative values. J Hand Surg. 1994;19(4):665–670. doi: 10.1016/0363-5023(94)90280-1. [DOI] [PubMed] [Google Scholar]
- 45.Armstrong CA, Oldham JA. A comparison of dominant and non-dominant hand strengths. J Hand Surg (Br) 1999;24(4):421–425. doi: 10.1054/JHSB.1999.0236. [DOI] [PubMed] [Google Scholar]
- 46.Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am. 1986;68(5):647–659. doi: 10.2106/00004623-198668050-00003. [DOI] [PubMed] [Google Scholar]
- 47.Jayakumar P, Teunis T, Vranceanu AM, Lamb S, Williams M, Ring D, Gwilym S. Construct validity and precision of different patient-reported outcome measures during recovery after upper extremity fractures. Clin Orthop Relat Res. 2019;477(11):2521–2530. doi: 10.1097/CORR.0000000000000928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Goldhahn J, Beaton D, Ladd A, Macdermid J, Hoang-Kim A. Recommendation for measuring clinical outcome in distal radius fractures: a core set of domains for standardized reporting in clinical practice and research. Arch Orthop Trauma Surg. 2014;134(2):197–205. doi: 10.1007/s00402-013-1767-9. [DOI] [PubMed] [Google Scholar]
- 49.Martinez-Mendez D, Lizaur-Utrilla A. de-Juan-Herrero J: intra-articular distal radius fractures in elderly patients: a randomized prospective study of casting versus volar plating. J Hand Surg Eur. 2018;43(2):142–147. doi: 10.1177/1753193417727139. [DOI] [PubMed] [Google Scholar]
- 50.Swedish National Guidelines for Distal Radius Fractures [https://d2flujgsl7escs.cloudfront.net/external/Nationellt+vårdprogram+för+behandling+av+distala+radiusfrakturer.pdf]. Accessed Feb 2022.
- 51.Schmidt V, Mellstrand Navarro C, Ottosson M, Tägil M, Christersson A, Engquist M, Sayed-Noor A, Mukka S, Wadsten M. Forecasting effects of "fast-tracks" for surgery in the Swedish national guidelines for distal radius fractures. PLoS One. 2022;17(2):e0260296. doi: 10.1371/journal.pone.0260296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Thorninger R, Madsen ML, Wæver D, Borris LC, Rölfing JHD. Complications of volar locking plating of distal radius fractures in 576 patients with 3.2 years follow-up. Injury. 2017;48(6):1104–1109. doi: 10.1016/j.injury.2017.03.008. [DOI] [PubMed] [Google Scholar]
- 53.Tarallo L, Mugnai R, Zambianchi F, Adani R, Catani F. Volar plate fixation for the treatment of distal radius fractures: analysis of adverse events. J Orthop Trauma. 2013;27(12):740–745. doi: 10.1097/BOT.0b013e3182913fc5. [DOI] [PubMed] [Google Scholar]
- 54.Alter TH, Sandrowski K, Gallant G, Kwok M, Ilyas AM. Complications of volar plating of distal radius fractures: a systematic review. J Wrist Surg. 2019;8(3):255–262. doi: 10.1055/s-0038-1667304. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analysed during the current study are not publicly available due to limitations in the ethical approval but are available from the corresponding author on reasonable request.