Abstract
Objective:
Recent studies have observed that racial or ethnic adult health disparities revealed in national data dissipate in racially integrated communities, supporting the theory that “place, not race” shapes the nature and magnitude of racial/ethnic health disparities. We test this theory among children.
Methods:
In 2020, we estimated racial/ethnic childhood obesity disparities within integrated schools and between segregated schools, using statewide cross-sectional data collected in 2019 on 5th, 7th, and 9th grade students from California public schools.
Results:
School segregation accounted for a large part of the obesity disparities between White children and children of color (Latinos, Blacks and Filipinos). In racially integrated schools, obesity disparities were much smaller than those in state-wide data, whereas racial or ethnic childhood obesity disparities were larger when comparing children in majority White schools to those attending schools with majority enrollment of children of color, except for Asians, who generally had lower obesity rates than their White peers.
Conclusions:
School-level racial segregation is a salient contributor to racial/ethnic childhood obesity disparities. Reducing obesity disparities may be particularly effective if place-level interventions target socioeconomically disadvantaged integrated schools and segregated schools attended primarily by children of color.
Keywords: child obesity, segregation, racial/ethnic disparities
INTRODUCTION
Obesity rates among youth 2–19 years old in the United States have remained stable in the last several years, for some but not all population subgroups1,2. Black and Latino youth relative to White peers, as well as socioeconomically disadvantaged youth compared with affluent youth, have not experienced the same levelling off in obesity rates3. For example, between 2000 and 2016, youth obesity prevalence among White females increased from 12% to 13.6% but increased from 21.5% to 25.1% among African American females and from 15.4% to 23.5% among Hispanic females. Among male youth, during the same period, obesity increased from 11.0% to 14.7% among Whites, from 16.5 to 19% among African Americans, and from 22.9% to 28% among Hispanics.3 Since children with obesity are more likely to have obesity as adults, racial/ethnic obesity disparities during childhood may be a mechanism that gives rise to adult disparities in chronic disease and other outcomes associated with obesity4,5. Given the US’s demographic trends, it is imperative that we identify salient factors associated with childhood obesity disparities to create effective solutions to achieve health equity.6,7
Recent studies among adults have shifted the focus from quantifying racial/ethnic disparities nationally to examining disparities within racially integrated neighborhoods, thereby testing the theory of “place (not race)”8–12. Building on prior work that names racial residential segregation as a fundamental cause of health disparities13, this theory posits that the characteristics of places where people live, not individual-level characteristics, are the primary drivers of health disparities and highlights the need for analytical strategies that can overcome confounding of individual-level race and racial segregation10. Analyses that fail to accurately account for racial/ethnic residential segregation may incorrectly attribute racial/ethnic disparities to person-level characteristics/behaviors instead of community-level factors and their upstream determinants including structural racism14,15.
To estimate racial disparities while tightly controlling for racial residential segregation, the authors8–12 concentrated their data collection on an integrated Baltimore neighborhood—i.e., adjustment through stratification that focused on one strata of the integrated/segregated spectrum. In this neighborhood, where neither African Americans or Whites had a clear majority, residents’ health behaviors are similarly constrained/supported by the characteristics of the neighborhood. Importantly, by calculating disparities between African American and White residents within the same neighborhood, the authors held all characteristics of place constant by design, regardless of whether neighborhood characteristics were measured or not. They showed their theory held because racial/ethnic disparities in a range of outcomes were consistently smaller in the racially integrated neighborhood compared to national-level disparities that used individual-level race/ethnicity as a variable, but did not consider residential segregation8–12.
It is less clear if health disparities among child populations are smaller within racially integrated places in comparison to state- or national-level disparities. Intrinsically linked with residential segregation16,17, school segregation/integration may play an important role in childhood obesity disparities because children spend a large proportion of their time in or around schools. Emerging literature shows that racial/ethnic disparities in childhood obesity are attenuated after adjustment for school neighborhood factors16–20 and that school factors can explain a large fraction of observed racial/ethnic disparities for many health outcomes, highlighting schools’ unique effect on children’s health disparities21. School racial/ethnic segregation can shape obesity disparities through multiple, interrelated mechanisms. Direct mechanisms include resources, constraints and opportunities to consume a healthy diet and engage in physical activity, given that segregated schools attended primarily by children of color tend to have higher exposures to obesogenic factors such as greater availability of unhealthy foods inside and nearby schools and fewer resources for physical activity19,22–27 in comparison to schools attended primarily by White children. In addition, minority segregated schools also have higher levels of exposure to violence and social stressors inside and near schools that can influence physical activity, mental health, and other biological factors that are directly or indirectly linked to higher obesity risk.28–31
This study investigates whether school segregation is a driver of childhood obesity disparities. Though the effects of residential and school segregation are difficult, if not impossible, to disentangle, this study uses a state-wide surveillance dataset from California public school children to examine racial/ethnic obesity disparities in relation to school integration/segregation. First, as predicted by the place (not race) theory, our central hypothesis is that racial/ethnic disparities within integrated schools are smaller compared to state-wide disparities that do not account for racial/ethnic school segregation/integration. As in the integrated Baltimore neighborhood study8–12, this disparity measure is intrinsically adjusted for all observed and unobserved school-level factors among children attending integrated schools. Second, we also estimate disparities comparing obesity rates among children of color who attend minority segregated schools to obesity among White children who attend White segregated schools. We hypothesize disparities calculated between-segregated schools will be larger than state-level disparities given the differences in obesogenic features of the environments inside/near minority- vs. White segregated schools. Together, the disparities within-integrated and between-segregated schools shed light on the effect of school segregation.
METHODS
Study Design, Population and Outcome
This cross-sectional study evaluated disparities in childhood obesity using overweight/obesity rates obtained from the California Department of Education (CDE) for students enrolled in fifth, seventh and ninth grade attending California public schools in the 2018–2019 school year, who participated in the California Fitnessgram test. Fitnessgram is a physical fitness test required for all children in those grades and is administered in the spring of the academic year. De-identified Fitnessgram datasets are publicly available.
The main outcome of interest is the body composition assessment of Fitnessgram32. For this assessment, objectively measured height and weight are used to obtain children’s body mass index (BMI). Then, BMI is compared to the CDC’s age- and sex- specific BMI reference distributions to categorize children into three groups: Healthy Fitness Zone (HF), Needs Improvement (NI), and High Risk (HR), which correspond to the BMI categories of “normal weight”, “overweight”, and “obese”, respectively based on the CDC reference distribution32. We use the term “overweight/obesity” to refer to the combined category of NI and HR.
Students missing body composition data were excluded. Missing data was primarily due to data masking implemented by CDE to protect children’s confidentiality. Specifically, CDE purposefully marks data as ‘missing’ when there are <10 children within each subgroup defined by grade and race/ethnicity at a given school. The sample size threshold of 10 was selected by CDE; sample sizes fewer than this were deemed to increase the risk of identifying individual children and their weight status.33
School segregation/integration measure
To compare overweight/obesity rates for each group of children of color (Asians, Blacks, Filipinos, and Latinos) to those of White children, independently of the presence of other children in the schools, we: (a) developed a straightforward definition of segregated and relatively more integrated schools that maximized the use of unmasked (i.e., available) Fitnessgram data, and (b) conducted sensitivity analyses using more restrictive definitions described below. We used the CDE sample size threshold of 10 to classify schools into one of four categories for each group of children of color: (1) The label of “integrated schools” was used for schools that had >10 children of color and >10 White children with unmasked data. Schools in this category are relatively more integrated in the sense that they have enough White children and enough of children of color such that children in neither group have high risk of being personally identified. Though the level of integration may vary within these schools, this definition can be considered as a minimum level of integration. With this definition, schools with very large percentages of minority children could be considered integrated if the number of White children is sufficiently large such that they are not personally identifiable, and vice versa. (2) Schools segregated toward children of color were those that had data available for >10 children of color, but ≤10 White children had available data. In these schools obesity rates for White children were masked because the low number of White children posed a risk to confidentiality. This label was applied to each school for each race ethnicity group; we use labels such as “Black segregated schools,” and similarly for other groups. (3) “White segregated” schools (i.e., the reverse of category 2) were those that had data on ≤10 children of color but had data on >10 White children. (4) For a given racial/ethnic vs. White comparison, “excluded schools” were those that had data on ≤10 children of color and ≤10 White children. These schools are excluded since outcome data are masked for children of both groups. These categories maximize the use of available data and are correlated with the percent of white children in the school (see also sensitivity analyses described below). These categories were also created for each grade level, to conduct grade-specific analyses.
Other variables
For descriptive purposes, data from the 2015 American Community Survey was used to determine socioeconomic characteristics of the school’s neighborhoods, including census-tract level median annual household income and percent of adults ≥25 years in the census tract with ≥16 years of education.34 The percentage of children who qualified for free or reduced meals and student enrollment by race/ethnicity within each school was obtained from the CDE.35
Statistical Analyses
Descriptive statistics were calculated for all schools combined, and by school segregation category. Analysis of variance was used to determine if school characteristics differed significantly across school segregation categories. For each racial/ethnic group, two disparity measures were calculated. First, within each integrated school, we compared overweight/obesity prevalence among each racial/ethnic subgroup to the overweight/obesity prevalence among White children. We then calculated the average disparity across all integrated schools. This analysis, which we call “disparity within integrated schools,” automatically adjusts for observed and unobserved school- and school-neighborhood level factors.
A second disparity measure compared each group of children of color attending their respective Asian-, Black-, Filipino- or Latino- segregated schools to White children attending White segregated schools. Thus, comparisons between racially segregated schools reflect the average difference in overweight/obesity prevalence between White children in White segregated schools and children of color in minority segregated schools. This comparison is called the “disparity between segregated schools”. Regression adjustment for school-level factors of this disparity measure was not conducted, as it would result in biased inferences about child-level disparities because not all other variables can be “held constant”, including school-level segregation. Moreover, since segregation gives rise to differences in other neighborhood level factors that are consistently related to weight status (e.g., obesogenic environments), as well as to individual-level socioeconomic disadvantage for individuals living in segregated areas (e.g., limited access to employment opportunities15), adjustment for these factors would be consistent with a mediation analysis, which is not of primary interest in this study.
The Appendix gives the formulas for the calculation of the disparities and their standard errors. Standard errors were used to calculate 95% confidence intervals for the disparities.
Sensitivity analyses
We used two alternative definitions of school segregation/integration based on the school-wide enrollment for each racial/ethnic group. As in prior studies about place not race8, the first alternative definition of integrated schools required that neither of the racial/ethnic groups being compared had a majority (>50%) of the school’s enrolled student population. The alternative definition of schools segregated toward children of color required enrollment of children of color to be a majority (>50%) of the school’s student body, and analogously for White segregated schools. The second definition of segregation/integration was based on the index of concentration at the extremes (ICE)36, computed separately for each group of children of color. The index ranges from −1 to 1, where −1 reflects no White children are enrolled in the school, and 1 is interpreted as only white children are enrolled. The continuous ICE was then categorized into tertiles. Schools in the lower tertile were labeled as segregated toward children of color; those in the middle tertile were labeled as integrated; and those in the upper tertile were categorized as White segregated. Further, because the masking of data is more likely among schools with lower enrollment, we also conducted sensitivity analysis among schools with enrollment above the first quartile of enrollment across all schools.
Analyses were conducted using SAS V9.4.
Ethics
The study was exempt by the author’s universities institutional review boards given that we use publicly available data.
RESULTS
The body composition assessment of the Fitnessgram test was applied to 1,363,961 children during the 2018–2019 school year, of whom 54% were Latino, 23% were White, 9.5% Asian, 5.4% Black, and 2.4% Filipino. Other races/ethnicities were excluded from the analyses because the small sample sizes within schools led to masking most of their data. Data for the five major race/ethnic groups included in the analysis (N=1,271,980) was collected within 8,933 schools.
Among all groups of children of color, Asians were the most likely to attend integrated schools (Table 1). Seventy-two percent of Asian students attended Asian-White integrated schools, whereas 50% of Black students attended Black-White integrated schools, and 50% and 56% of Filipino and Latino children attended Filipino-White and Latino-White integrated schools, respectively. Latino children were the most likely to attend schools with few to zero white peers: 43% of Latino children attended Latino segregated schools, whereas 15%, 24% and 9% of Asian, Black and Filipino children had few to zero White schoolmates.
Table 1.
Number of students in 5th, 7th and 9th grade participating in the 2018–2019 California Fitnessgram, and characteristics of schoolsa to which students attended.
| Integrateda,d Schools | Schools with Segregateda,d children of color | Schools with Segregateda,d white children | Schools Excludeda,d | |
|---|---|---|---|---|
| Asian-White comparison | ||||
| N Asian students | 93,232 (72%) | 19,584 (15%) | 10,112 (8%)b | 5,727 (4%)b |
| N White students | 161,927 (53%) | 2,399 (1%)b | 127,729 (42%) | 13,258 (4%)b |
| N Schools | 1720 (21%) | 509 (6%) | 2756 (34%) | 3184 (39%) |
| School Enrollment | 1,166 | 656 | 643 | 521 |
| % of enrolled students who are White | 31% | 5% | 40% | 10% |
| % of enrolled students who are Asian | 20% | 33% | 3% | 3% |
| % students in FRPM | 37% | 64% | 53% | 80% |
| Median household incomec | 91,544 | 67,749 | 68,556 | 51,395 |
| % with ≥16 years of educationc | 43 | 29 | 30 | 18 |
| Black-White comparison | ||||
| N Black students | 36,351 (50%) | 17,819 (24%) | 10,882 (15%)b | 7,642 (10%)b |
| N White students | 102,808 (34%) | 2,628 (1%)b | 186,848 (61%) | 13,029 (4%)b |
| N Schools | 1,116 (13%) | 680 (8%) | 3,360 (40%) | 3,210 (38%) |
| School Enrollment | 1,347 | 654 | 678 | 515 |
| % of enrolled students who are White | 24% | 4% | 41% | 10% |
| % of enrolled students who are Black | 9% | 23% | 2% | 4% |
| % students in FRPM | 57% | 84% | 43% | 77% |
| Median household incomec | 71,913 | 48,653 | 79,292 | 54,483 |
| % with ≥16 years of educationc | 31 | 18 | 36 | 20 |
| Filipino-White comparison | ||||
| N Filipino students | 16,497 (50%) | 3,132 (9%) | 9,227 (28%)b | 4,190 (13%)b |
| N White students | 70,282 (23%) | 722 (0.2%)b | 219,374 (72%) | 14,935 (5%)b |
| N Schools | 610 (8%) | 142 (2%) | 3,866 (48%) | 3,434 (43%) |
| School Enrollment | 1,590 | 825 | 727 | 528 |
| % of enrolled students who are White | 23% | 4% | 38% | 9% |
| % of enrolled students who are Filipino | 7% | 15% | 2% | 1% |
| % students in FRPM | 44% | 64% | 47% | 78% |
| Median household incomec | 83,323 | 69,124 | 76,513 | 52,912 |
| % with ≥16 years of education | 36 | 25 | 35 | 19 |
| Latino-White comparison | ||||
| N Latino students | 407,134 (56%) | 312,777 (43%) | 4,401 (1%)b | 3,997 (1%)b |
| N White students | 253,362 (83%) | 12,303 (4%)b | 36,294 (12%) | 3,354 (1%)b |
| N Schools | 3,808 (43%) | 3,475 (39%) | 668 (8%) | 955 (11%) |
| School Enrollment | 912 | 567 | 460 | 353 |
| % of enrolled students who are White | 33% | 6% | 55% | 31% |
| % of enrolled students who are Latino | 44% | 76% | 19% | 35% |
| % students in FRPM | 49% | 81% | 33% | 55% |
| Median household incomec | 72,760 | 51,553 | 87,203 | 66,439 |
| % with ≥16 years of educationc | 33 | 18 | 43 | 30 |
Integrated schools defined as those attended by >10 white children and >10 children of the specific race/ethnicity subgroup; schools with segregated children of color have >10 children of the specific race/ethnicity subgroup, and <10 white children; vice-versa for segregated white schools; excluded schools have <10 white children and <10 children of the specific race/ethnic subgroup.
Children with missing data due to masking of data for confidentiality purposes.
Characteristic of census tract where school is located
ANOVA p-values comparing school characteristics across the level of integration/segregation in the schools are all p<0.001.
Given segregation, it is unsurprising that segregated and integrated schools were situated in neighborhoods with significantly different socioeconomic profiles (Table 1). Asian-White and Filipino-White integrated schools were in more affluent neighborhoods (e.g., median household income $92K and $83K, respectively) compared to their comparison White segregated schools ($69K, $76K), which were in turn more affluent than Asian ($68K) and Filipino ($69K) segregated schools. In contrast, Black-White ($72K) and Latino-White ($73K) integrated schools were more socioeconomically disadvantaged than their comparison White segregated schools ($79K and $87K, respectively), but much more affluent than Black ($49K) and Latino ($52K) segregated schools. Supplementary Table 1 shows confidence intervals for all disparity estimates discussed below.
Disparities State-wide
Across 5th, 7th, and 9th grades combined, White children had an overall 28% overweight/obesity prevalence state-wide, whereas the prevalence was significantly higher among Latino (48%), Black (42%) and Filipino (31%) populations (Figure 1, top). Asian children had a slight but significantly lower (24%) overweight/obesity prevalence than White children (28%), hence demonstrating a ‘reverse’ disparity. When analyzed separately by grade, these state-wide patterns generally held across each grade although the disparities were smaller in higher grades (data not shown).
Figure 1.
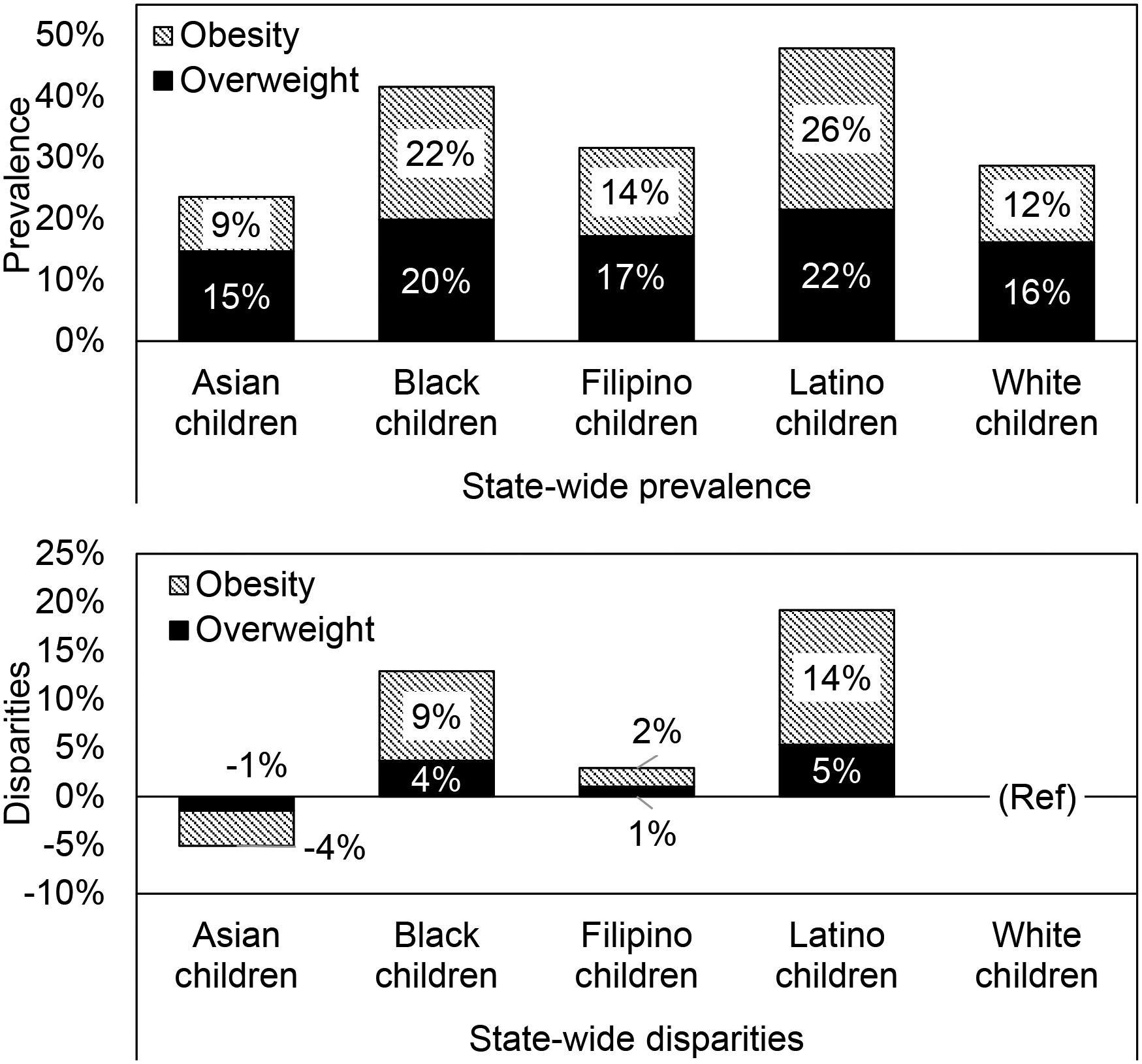
State-wide (top) prevalence of overweight and obesity, and (bottom) disparities, among children attending California public schools, by race/ethnicity (5th, 7th and 9th grades combined). Fitnessgram data for the 2018–2019 school year, California, USA.
Among Latino and Black youth, the disparities are concentrated in the obesity (vs. overweight) classification (Figure 1, bottom). For example, of the 19% absolute Latino/White difference in overweight/obesity prevalence, about three fourths of it (14%) is due to obesity.
Disparities within Integrated Schools
The overweight/obesity gaps between Latino, Black and Filipino students compared to White students were smaller within integrated schools relative to the state-wide average disparities (Figure 2). In general, White students in both integrated and segregated schools had a similar prevalence of overweight/obesity as reported for White children in state-wide data. The state-level difference in overweight/obesity between Latino and White children was 19%, but this disparity narrowed to 11% when comparing rates between White and Latino children in integrated schools. The difference in overweight/obesity prevalence between Black and White children also narrowed from 13% state-wide to 6% within integrated schools. Further, for Filipino relative to White children, the state-wide overweight/obesity disparity was 3% but reversed to −1% within integrated schools. In contrast, the magnitude of the difference between Asian children and White children attending integrated schools (4%) was similar to the state-wide difference (5%). The disparities within integrated schools differ only slightly by grade, with slightly more notable grade-related differences among Black and Filipino children (not shown).
Figure 2. (Top) Overweight and obesity prevalence in integrated schoolsa by child race/ethnicity; (bottom) state-wide disparities and disparities within integrated public schools in California. Fitnessgram data for the 2018–2019 school year, California, USA.
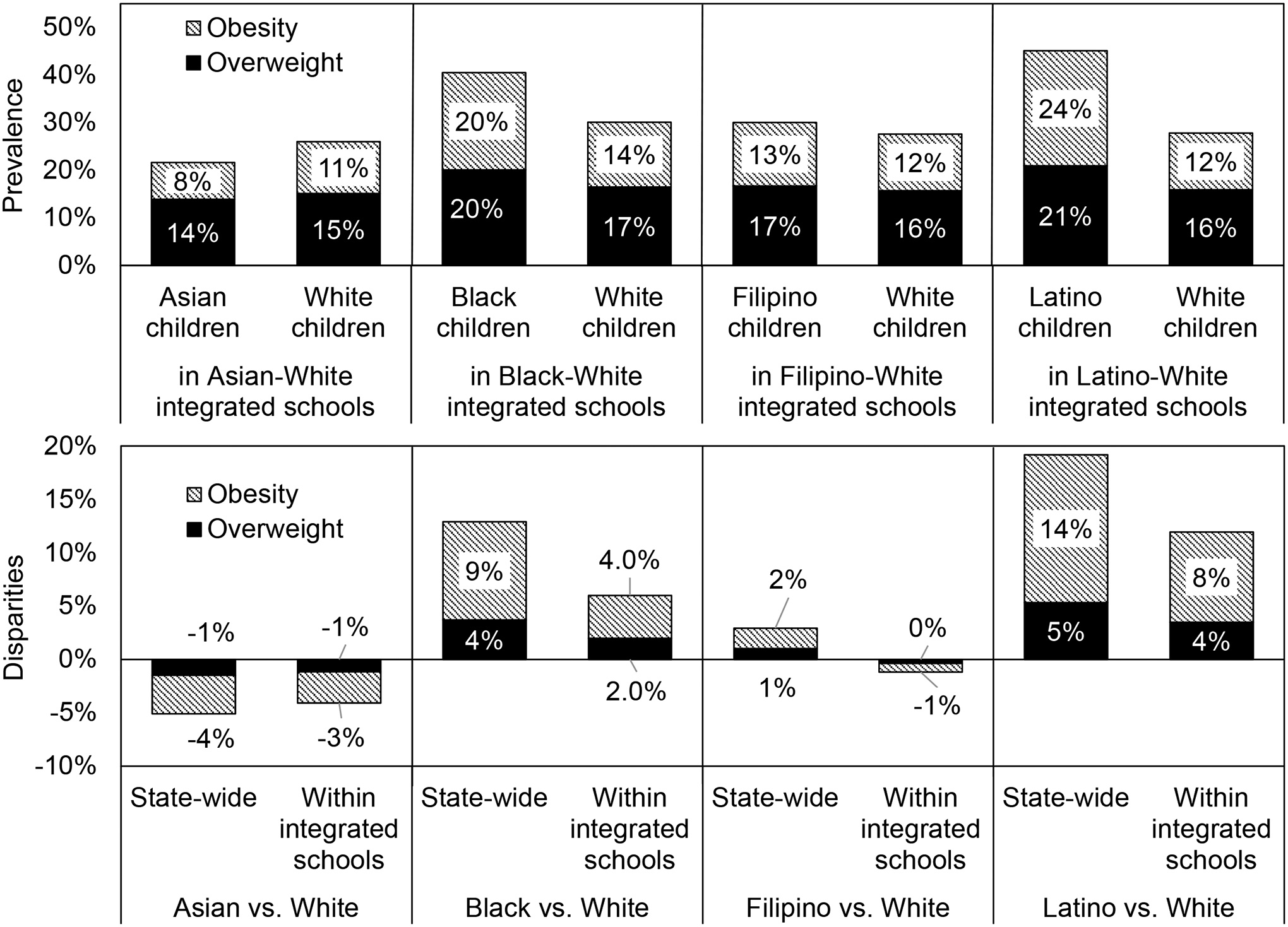
a. Schools with data available for >10 white children and >10 children of the specific race/ethnicity subgroup.
Disparities between Segregated Schools
By contrast, the overweight/obesity gap between Latino, Black and Filipino children compared to White children was larger between segregated schools, relative to state-wide disparities (Figure 3, next page). While the disparity in overweight/obesity between Latino and White children was 19% at the state level, it was 22% when comparing Latino children in Latino segregated schools to White children in White segregated schools. The state-wide disparity in overweight/obesity prevalence between Black and White children was 13% but rose to 18% between segregated schools, as did the disparity between Filipino and White children (state-wide: 3%; between segregated schools: 8%). Overweight/obesity differences between Asian and White children were similar state-wide and between segregated schools. The disparities between segregated schools were larger than the disparities within integrated schools for all groups except Asian children (Supplementary Table 1).
Figure 3. (Top) Overweight and obesity prevalence among children in segregated schools; (bottom) state-wide disparities and disparities between segregated schoolsa public schools in California. Fitnessgram data for the 2018–2019 school year, California, USA.
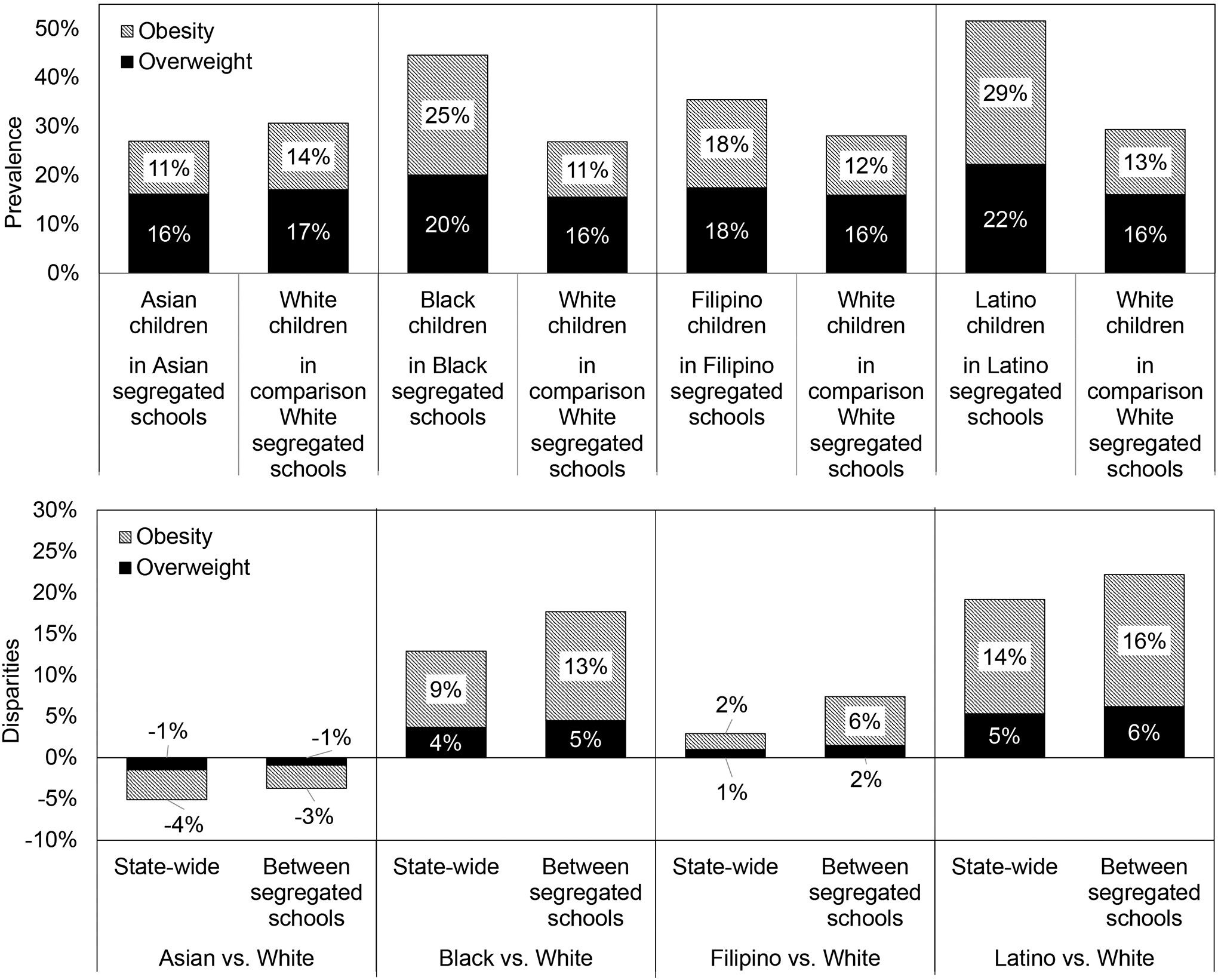
a. Attended by greater than 10 children of one group and fewer than 10 children of the corresponding comparison group
Sensitivity analyses
As shown in Supplementary Figure 1, the analysis using alternate definitions of integrated/segregated schools and those focused on schools with larger enrollments did not give meaningfully different results.
DISCUSSION
Consistent with our a priori hypothesis, compared to state-level estimates, racial/ethnic obesity disparities were smaller or nonexistent in integrated schools. Further, relative to state-level racial/ethnic disparities, differences in obesity rates were larger between Latino, Black, and Filipino children in segregated schools compared to White children in White segregated schools. We also found that Asian children as a whole tended to have a lower overweight/obesity prevalence than White children.
To our knowledge, this is the first investigation to examine childhood obesity disparities specifically within integrated schools to begin to elucidate the role of school segregation in the racial/ethnic patterning of obesity among youth. This study contributes to emerging literature separating the potential effects of individual-level race/ethnicity from the influences of segregation. The finding that disparities were smaller in integrated schools than at the state-level further supports the theory of “place, not race”9. LaVeist et al9 examined several adult health outcomes found that disparities were smaller in a racially integrated low-income neighborhood in Baltimore compared to those estimated from national data. Consistent those findings, the present study suggests that place-level factors that are often consequences of segregation have more influence on health disparities than individuals’ race itself.13,15
Other studies among children have examined the association between residential and or school segregation and childhood obesity or how their adjustment attenuates disparities18–27, but have not estimated disparities within integrated areas. This study’s analytical approach, which stratified schools according to whether or not they are integrated, served a dual purpose. First, the within-school differencing approach calculated person-level disparities within integrated schools, while tightly controlling for characteristics of places where integrated schools are situated. This allowed us to compare obesity between children of color and White children who share the same school environment. By design, the approach equalizes observed and unobserved school- and school-neighborhood level factors linked to segregation, such as area-level income. Further adjustments for child-level socioeconomic differences would be expected to yield even smaller disparity estimates within integrated schools. Second, our analytic approach also makes explicit that the difference in overweight/obesity rates between children of color in segregated schools and White children in White-segregated schools is a comparison of populations that attend schools in vastly different places. While adjusted estimates can be useful for certain purposes, e.g., monitoring population-level disparities, the difference in place characteristics for Latino- and Black- compared to White-segregated schools is so vast that attempting to adjust for covariates, either at the school- or individual-level, would yield an invalid estimate of individual-level disparities due to regression extrapolation11,29.
Multiple interrelated mechanisms operating at multiple levels play a role in racial/ethnic obesity disparities. At the macro-level, structural racism and related institutional policies and practices result in racial segregation and systemic economic disinvestment in neighborhoods13–15. In this study, minority segregated schools were in far less affluent places compared to integrated schools. Less affluent places are more likely to have obesogenic features, and this likely explains the higher rates of obesity among Latino, Black, and Filipino children in minority segregated schools compared to their co-ethnic peers in integrated schools. In racially integrated schools, those attended by a mix of Latino-White and Black-White students were situated in places with fewer socioeconomic resources than White segregated schools. Hence, in integrated schools, White children were exposed to the same area-level disadvantage as their non-White counterparts and had slightly higher overweight/obesity rates compared to White children in White segregated schools. Similarly, White adults in an integrated Baltimore had worse health than estimated in national data9. While the socioeconomic circumstances of individual children and their families likely vary across integrated and segregated schools, those circumstances are likely driven by larger economic and social processes that shape racial segregation.13–15
Racial residential segregation is associated with reduced availability of healthy food outlets, less space and fewer resources and opportunities for physical activity, but greater availability of unhealthy food outlets at the neighborhood-level. These neighborhood attributes influence health behaviors and related outcomes including diet, physical activity, and health outcomes including body weight.37 In particular, differential food enviornment exposure is one of the most direct and well documented mechanisms for obesity disparities among schoolchildren. Schools attended primarily by children of color tend to have lower quality food enviornments both inside schools and in the school neighborhoods24,25; junk food availablitly and advertisement are associated with purchasing and consumption of unhealthy foods and poorer quality diets and obesity38–41. Differential availability of material and social resources that support physical activity across vayring levels of school integration/segregation is another possible mechansim27,42. A nationally representative study documented that disparities in physical activity levels among Hispanic and Black compared to White adolescents were greatly diminished or reversed when accounting for the characteristics of the schools they attended, including racial composition and economic resources.23 These mechanisms are part of a broader constellation of differences in material and social characteristics across levels of school segregation16,19,22,26–28,30,42,43, including exposure to violence, a barrier to physical activity.29 Identifying place-based mechanisms linking school racial/ethnic segregation to child obesity disparities is critical for the design of interventions to advance health equity beginning in childhood.18
Future research should examine the joint role of individual-level economic factors and racial/ethnic segregation to shed additional light on disparities and ways to reduce them43. We examined racial/ethnic segregation specifically, but we were unable to conduct analyses that jointly examine economic and race/ethnic disparities because the publicly available data from CDE does not allow cross-classification of these factors within schools. Additionally, future research should employ analytical approaches to disentangle the confounding effects of segregation and race/ethnicity and produce valid estimates of individual-level disparities attributable to person-level factors and thus amenable to individual-level interventions, vs. disparities driven by segregation and concomitant place based or structural interventions. Given findings from this and previous studies, estimating disparities within more granular levels of geography is critical to more accurately account for environmental factors. As shown here, disparities estimated at large levels of aggregation are confounded by place characteristics, and thus under or overestimate disparities at more granular geographical levels where interventions typically are implemented.
The study has several limitations. The findings may not be generalizable beyond California, though given that this state is one of the most diverse in the country, results are likely generalizable to similarly diverse metropolitan areas. This study was based only on children attending public schools, because private schools were not required to report Fitnessgram data. However, since only 7.6% of all children in California attended private schools in the 2018–2019 school year and such students likely have higher socioeconomic advantage and lower prevalence of overweight/obesity, this population is unlikely to have a significant effect on disparity estimates reported here. Additionally, the study had a smaller number of Filipino children, potentially making estimates less robust for this subgroup. Our primary definition of integration/segregation relied on the number of children with reported body composition data and maximized the number of children included in the analysis. However, the results could have been influenced by the definition. Yet, multiple sensitivity analyses showed the results are robust to the definition of integration/segregation.
CONCLUSION
This study found that racial/ethnic overweight/obesity disparities were larger between racially segregated schools and smaller or non-existent within integrated schools, a critical distinction that is likely driven by differences in social and built environment factors associated with segregation. Research and interventions must carefully consider segregation to understand, address and monitor progress in health equity. Place-level interventions that target integrated schools in socioeconomically disadvantaged neighborhoods and segregated schools attended primarily by children of color may be more fruitful than individual-level behavioral interventions in improving health equity.
Supplementary Material
Study Importance Questions:
What is already known about this subject?
Racial/ethnic obesity disparities among adults are smaller in integrated residential areas, and larger between segregated areas
What are the new findings in your manuscript?
The theory of “place, not race” is supported by data on childhood obesity.
School segregation is a contributor to racial/ethnic child obesity disparities.
How might your results change the direction of research or the focus of clinical practice?
Findings imply school segregation matters more than individual-level race.
Interventions must prioritize non-white segregated schools and disadvantaged schools.
Funding:
This research was partially supported by NIH grants R01-HL131610 and R01-HL136718.
Footnotes
Disclosure: The authors declared no conflict of interest.
Contributor Information
Nuha Mahmood, The University of Michigan Medical School, Ann Arbor, MI
Emma Sanchez-Vaznaugh, San Francisco State University, San Francisco, CA.
Mika Matsuzaki, Johns Hopkins University School of Public Health, Baltimore, MA.
Brisa N. Sánchez, Drexel University Dornsife School of Public Health, Philadelphia, PA.
REFERENCES
- 1.Datar A, Chung PJ. Changes in Socioeconomic, Racial/Ethnic, and Sex Disparities in Childhood Obesity at School Entry in the United States. JAMA Pediatr. 2015;169(7):696–697. [DOI] [PubMed] [Google Scholar]
- 2.Ogden C, Carroll MD, Fakhouri TH, et al. Prevalence of Obesity Among Youths by Household Income and Education Level of Head of Household—United States 2011–2014. Morbidity and Mortality Weekly Report. 2018;67(6):186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Skinner AC, Ravanbakht BA, Skelton JA, Perrin EM, Armstrong SC. Prevalence of obesity and severe obesity in US children, 1999–2016. Pediatrics. 2018;141(3):e20173459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mijailovic M, Mijailovic V, Micic D. Childhood onset of obesity: does an obese child become an obese adult? J Pediatr Endocrinol Metab. 2001;14 Suppl 5:1335–1338; discussion 1365. [PubMed] [Google Scholar]
- 5.Mijailovic V, Micic D, Mijailovi M. Effects of childhood and adolescent obesity on morbidity in adult life. J Pediatr Endocrinol Metab. 2001;14 Suppl 5:1339–1344; discussion 1365. [PubMed] [Google Scholar]
- 6.Colby SL, Ortman JM. Projections of the Size and Composition of the U.S. Population: 2014 to 2060. In: Bureau USC, ed 2015. [Google Scholar]
- 7.National Institues of Health. Strategic plan for NIH obesity research. In:2011.
- 8.LaVeist T, Pollack K, Thorpe R Jr., Fesahazion R, Gaskin D. Place, not race: disparities dissipate in southwest Baltimore when blacks and whites live under similar conditions. Health Aff (Millwood). 2011;30(10):1880–1887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.LaVeist T, Thorpe R Jr., Bowen-Reid T, et al. Exploring health disparities in integrated communities: overview of the EHDIC study. J Urban Health. 2008;85(1):11–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Laveist TA, Thorpe RJ Jr., Mance GA, Jackson J. Overcoming confounding of race with socio-economic status and segregation to explore race disparities in smoking. Addiction. 2007;102 Suppl 2:65–70. [DOI] [PubMed] [Google Scholar]
- 11.Seamans MJ, Robinson WR, Thorpe RJ Jr., Cole SR, LaVeist TA. Exploring racial differences in the obesity gender gap. Ann Epidemiol. 2015;25(6):420–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thorpe RJ Jr., Kelley E, Bowie JV, Griffith DM, Bruce M, LaVeist T. Explaining Racial Disparities in Obesity Among Men: Does Place Matter? Am J Mens Health. 2015;9(6):464–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public health reports. 2001;116(5):404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lynch EE, Malcoe LH, Laurent SE, Richardson J, Mitchell BC, Meier HCS. The legacy of structural racism: Associations between historic redlining, current mortgage lending, and health. SSM Popul Health. 2021;14:100793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bailey ZD, Feldman JM, Bassett MT. How Structural Racism Works - Racist Policies as a Root Cause of U.S. Racial Health Inequities. N Engl J Med. 2021;384(8):768–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Piontak JR, Schulman MD. School Context Matters: The Impacts of Concentrated Poverty and Racial Segregation on Childhood Obesity. The Journal of school health. 2016;86(12):864–872. [DOI] [PubMed] [Google Scholar]
- 17.Richmond TK, Dunn EC, Milliren CE, Rosenfeld Evans C, Subramanian S. Disentangling overlapping influences of neighborhoods and schools on adolescent body mass index. Obesity. 2016;24(12):2570–2577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Elbel B, Corcoran SP, Schwartz AE. Neighborhoods, Schools and Obesity: The Potential for Place-Based Approaches to Reduce Childhood Obesity. PLoS One. 2016;11(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Piontak JR, Schulman MD. Racial Disparities in Context: Student-, School-, and County-Level Effects on the Likelihood of Obesity among Elementary School Students. Sociology of Race and Ethnicity. 2018;4(2):245–260. [Google Scholar]
- 20.Springer AE, Li L, Ranjit N, Delk J, Mehta K, Kelder SH. School-level economic disadvantage and obesity in middle school children in central Texas, USA: a cross-sectional study. International Journal of Behavioral Nutrition and Physical Activity. 2015;12(1):S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schuster MA, Elliott MN, Kanouse DE, et al. Racial and ethnic health disparities among fifth-graders in three cities. New England Journal of Medicine. 2012;367(8):735–745. [DOI] [PubMed] [Google Scholar]
- 22.O’Malley PM, Johnston LD, Delva J, Bachman JG, Schulenberg JE. Variation in obesity among American secondary school students by school and school characteristics. Am J Prev Med. 2007;33(4 Suppl):S187–194. [DOI] [PubMed] [Google Scholar]
- 23.Richmond TK, Hayward RA, Gahagan S, Field AE, Heisler M. Can school income and racial/ethnic composition explain the racial/ethnic disparity in adolescent physical activity participation? Pediatrics. 2006;117(6):2158–2166. [DOI] [PubMed] [Google Scholar]
- 24.Delva J, O’Malley PM, Johnston LD. Availability of more-healthy and less-healthy food choices in American schools: a national study of grade, racial/ethnic, and socioeconomic differences. Am J Prev Med. 2007;33(4 Suppl):S226–239. [DOI] [PubMed] [Google Scholar]
- 25.Sanchez-Vaznaugh EV, Weverka A, Matsuzaki M, Sanchez BN. Changes in Fast Food Outlet Availability Near Schools: Unequal Patterns by Income, Race/Ethnicity, and Urbanicity. Am J Prev Med. 2019;57(3):338–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martin MA, Frisco ML, Nau C, Burnett K. Social stratification and adolescent overweight in the United States: how income and educational resources matter across families and schools. Soc Sci Med. 2012;74(4):597–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Turner L, Chaloupka FJ, Chriqui JF, A. S School Policies and Practices to Improve Health and Prevent Obesity: National Elementary School Survey Results: School Years 2006–07 and 2007–08. Vol 1. Chicago, IL: Bridging the Gap Program, Health Policy Center, Institute for Health Research and Policy, University of Illinois at Chicago; 2010. [Google Scholar]
- 28.Eitle D, McNulty T. Segregation and School Violence. Social Forces. 2003;82(2):589–616. [Google Scholar]
- 29.McDonald NC. Critical factors for active transportation to school among low-income and minority students. Evidence from the 2001 National Household Travel Survey. Am J Prev Med. 2008;34(4):341–344. [DOI] [PubMed] [Google Scholar]
- 30.Walsemann KM, Bell BA, Maitra D. The intersection of school racial composition and student race/ethnicity on adolescent depressive and somatic symptoms. Soc Sci Med. 2011;72(11):1873–1883. [DOI] [PubMed] [Google Scholar]
- 31.Bernell SL, Mijanovich T, Weitzman BC. Does the racial composition of the school environment influence children’s body mass index? J Adolesc Health. 2009;45(1):40–46. [DOI] [PubMed] [Google Scholar]
- 32.Cooper Institute. Documentation of Changes in FITNESSGRAM® Healthy Fitness Zones. 2013.
- 33.Education CDo. PFT Statewide Research Files. https://www.cde.ca.gov/ta/tg/pf/pftresearch.asp. Published 2020. Accessed February 28, 2020.
- 34.Bureau UC. American Community Survey, 5-year Summary file. https://www.census.gov/programs-surveys/acs/data/summary-file.2015.html. Published 2018. Accessed Jan 21, 2018.
- 35.Education CDo. California Department of Education. Downloadable Data Files https://www.cde.ca.gov/ds/ad/downloadabledata.asp. Published 2020. Accessed February 1, 2020.
- 36.Massey D The prodigal paradigm returns: ecology comes back to sociology. In: Booth A, Crouter A, eds. Does It Take a Village? Community Effects on Children, Adolescents, and Families. Mahwah, NJ: Lawrence Erlbaum Associates; 2001:41–48. [Google Scholar]
- 37.Goodman M, Lyons S, Dean LT, Arroyo C, Hipp JA. How Segregation Makes Us Fat: Food Behaviors and Food Environment as Mediators of the Relationship Between Residential Segregation and Individual Body Mass Index. Front Public Health. 2018;6:92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.An R, Sturm R. School and residential neighborhood food environment and diet among California youth. Am J Prev Med. 2012;42(2):129–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Babey SH, Wolstein J, Diamant AL. Food environments near home and school related to consumption of soda and fast food. Policy Brief UCLA Cent Health Policy Res. 2011(PB2011–6):1–8. [PubMed] [Google Scholar]
- 40.Rossen LM, Curriero FC, Cooley-Strickland M, Pollack KM. Food availability en route to school and anthropometric change in urban children. J Urban Health. 2013;90(4):653–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Matsuzaki M, Sanchez BN, Acosta ME, Botkin J, Sanchez-Vaznaugh EV. Food environment near schools and body weight-A systematic review of associations by race/ethnicity, gender, grade, and socio-economic factors. Obes Rev. 2020;21(4):e12997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gill M, Chan-Golston AM, Rice LN, et al. Correlates of Social Support and its Association With Physical Activity Among Young Adolescents. Health Educ Behav. 2018;45(2):207–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Boen CE, Kozlowski K, Tyson KD. “Toxic” schools? How school exposures during adolescence influence trajectories of health through young adulthood. SSM Popul Health. 2020;11:100623. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


