Abstract
Background
Sleep is vital for recovery during hospital stay. Many sleep-promoting interventions have been investigated in the past. Nurses seem to overestimate their patients sleep and their perspective is needed for these interventions to be successfully implemented.
Objectives
To assess the patient's and nurse's agreement on the patient's sleep and factors disturbing sleep.
Methods
The instruments used included 1) five Richard-Campbell Sleep Questionnaire (RCSQ) items plus a rating of nighttime noise and 2) the Consensus Sleep Diary (CSD). The mean of the five RCSQ items comprised a total score, which reflects sleep quality. Once a week, unannounced, nurses and patients were asked to fill in questionnaires concerning last night's sleep. Neither nurses nor patients knew the others' ratings. Patient-nurse agreement was evaluated by using median differences and Bland-Altman plots. Reliability was evaluated by using intraclass correlation coefficients.
Results
Fifty-five paired patient-nurse assessments have been completed. For all RCSQ subitems, nurses' scores were higher (indicating “better” sleep) than patients’ scores, with a significantly higher rating for sleep depth (median [IQR], 70 [40] vs 50 [40], P = .012). The Bland-Altman plots for the RSCQ Total Score (r = 0.0593, P = .008) revealed a significant amount of variation (bias). The intra-class correlation coefficient (ICC) indicated poor reliability for all 7 measures (range −0.278 – 0.435). Nurses were relatively overestimating their own role in causing sleep disturbances and underestimating patient-related factors.
Conclusions
Nurses tend to overestimate patients’ sleep quality as well as their own role in causing sleep disturbances.
Highlights
-
•
There is a relatively poor agreement between patient self-reported and nurse proxy-reported sleep quality.
-
•
Nurses tend to overestimate inpatients' sleep quality.
-
•
Nurses overestimate their own role in causing sleep disturbances.
1. Introduction
Sleep is essential for the development and maintenance of physical and psychological health. The most important functions of sleep comprise memory processing and consolidation, cellular repair, brain development and hormonal regulation [[1], [2], [3], [4], [5]]. Short-term consequences of sleep disruption include increased stress responsivity, somatic pain and emotional distress [6], whereas long-term health consequences include anxiety, hypertension, cardiovascular disease, weight-related issues, dyslipidemia, and type 2 diabetes mellitus [[6], [7], [8]].
Hospitalized patients are at risk for sleep disturbances caused by disease-related factors (e.g. pain and discomfort), environmental factors (e.g. care-related routines, noise and light), and psychological factors (e.g. anxiety or fatigue) [[9], [10], [11]]. These sleep disturbances may interfere with the course of the disease and/or recovery, hence it is important to minimize sleep disturbances in patients. Few studies have researched sleep promotion in hospital by using relaxation techniques, aromatherapy, adopting quiet time and introducing artificial light therapy [12]. Such interventions to reduce sleep disturbances can only be successful if nurses are aware of the sleep quality of their patients, so that they know how and when to intervene. Previous research showed that nurses tend to overestimate patients' sleep quality at the Intensive Care Unit (ICU) [13]. Another study showed a slight to moderate patient-nurse interrater reliability at the ICU [14]. However, nursing care for patients in the ICU is often based on a 1:1 ratio, hence, findings cannot be extrapolated to regular wards. Therefore, the aim of this study is to assess the patient-nurse agreement on the patient's sleep quality. In addition, understanding the difference in perceived sleep disturbances between patients and nurses could provide a basis for the development of sleep interventions in the hospitals.
2. Methods
2.1. Setting and participants
An observational survey study was conducted at the Amsterdam UMC, Location VUmc, the Netherlands. The data was collected at the Gastroenterology and Liver Disease Department as well as the Plastic Surgery Trauma Unit. Data collection took place from November 2019 until January 2020. Patients were included if they met the following criteria: 1) ≥18 years of age, 2) admitted to the hospital for at least one night, and 3) a completed questionnaire by the night nurse. Exclusion criteria were: 1) no written informed consent due to severe illness or cognitive dysfunction 2) non-Dutch speaking. All nurses who were on duty on the selected nights were asked to participate in the study. The Medical Ethics Review Committee of VU University Medical Center (IRB00002991) ruled that the Medical Research involving Human Subjects Act did not apply to this study. A convenience sample was used, but a minimum of 30 heterogeneous samples (with a minimum of 3 different nurses) was obtained, which is required to assess reliability of nurse proxy-reported scores [15].
2.2. Study design
One day per week (Tuesday to Friday) was selected for data collection, using an online random number generator. Data collection did not take place on Saturdays to Mondays to avoid potential bias caused by the weekend. On selected days, one of the members of the research team approached the night nurses at the end of their shifts to fill in the questionnaire concerning the sleep of the patients they cared for that night. Potentially eligible patients were already determined and put in random order, to minimize the risk of recall bias in case a nurse had insufficient time to fill in all questionnaires. The patients, whose questionnaires were completed by the nurses, were approached by the researcher to ask whether they wished to participate in the study. If consent wasn't obtained, the filled-in questionnaire from the nurse was destroyed without being seen by the researchers. If patients expressed their interest in participation, they were asked to fill in the questionnaire. Patients nor nurses did get to see the filled-in questionnaires from the other.
2.3. Study measures
The Richards Campbell Sleep Questionnaire (RCSQ) and the Consensus Sleep Diary (CSD) were used to measure sleep quality. The RCSQ has previously been validated against polysomnography recordings in an ICU population [16]. It is a brief five-item questionnaire used to evaluate perceived sleep depth, sleep latency, nocturnal awakenings, return to sleep, and sleep quality. Each RCSQ response is recorded on a 100-mm visual-analogue scale, with higher scores representing better sleep and the mean of these five items (“total score”), representing the overall perception of sleep. Mean total scores falling within the lowest quartile are considered very poor sleep and mean total scores falling within the highest quartile are considered very good sleep. A sixth item was added, as done in prior studies, evaluating perceived nighttime noise, ranging from “very quiet” to “very noisy”. The CSD was used to quantify sleep; sleep time, wake time, sleep latency, number of awakenings, and wake after sleep onset (WASO) [17]. The RCSQ and CSD were translated into Dutch by the researchers using back translation [18]. A pilot version was tested amongst a nurse and patient and adjusted where appropriate. In addition to the RCSQ and CSD, medication use, sleep disturbers and patient characteristics (like gender, age, educational level) were gathered.
2.4. Statistical analysis
The collected data were analyzed using IBM SPSS Statistics, version 26 (IBM Corp., Armonk, N.Y, USA). Descriptive data-analyses provided mean, median, standard deviation and interquartile range (IQR) for continuous variables and percentages for categorical variables. Unpaired Student's t-test was used to identify differences between two independent groups (e.g. differences between all patients and all nurses) and paired t-test for dependent groups (e.g. difference between scores within patient-nurse pairs) for normally distributed variables; Mann-Whitney U tests and Wilcoxon Signed Rack tests were applied otherwise.
Agreement between patient self-reported and nurse proxy-reported sleep quality (using each sub-item as well as the total RCSQ score) was also depicted in Bland-Altman plots, which visually represent differences in paired responses from patients and nurses (y-axis) in relation to the average of patient's and nurse's responses (x-axis). In addition, interrater reliability was calculated by using the intra-class correlation coefficient (ICC), which represents the proportion of total variation that can be explained by differences across patients. Larger ICCs indicate greater reliability of the nurses' and patients' reports. The ICCs were computed by a single-rating, absolute-agreement, 2-way random-effects with 2 raters (patient/nurse). ICC values less than 0.5 are indicative of poor reliability, values 0.5–0.75 indicate moderate reliability, 0.75–0.9 good reliability and values greater than 0.90 indicate excellent reliability [15].
Statistical significance was defined by a 2-sided P value less than 0.05.
3. Results
3.1. Population
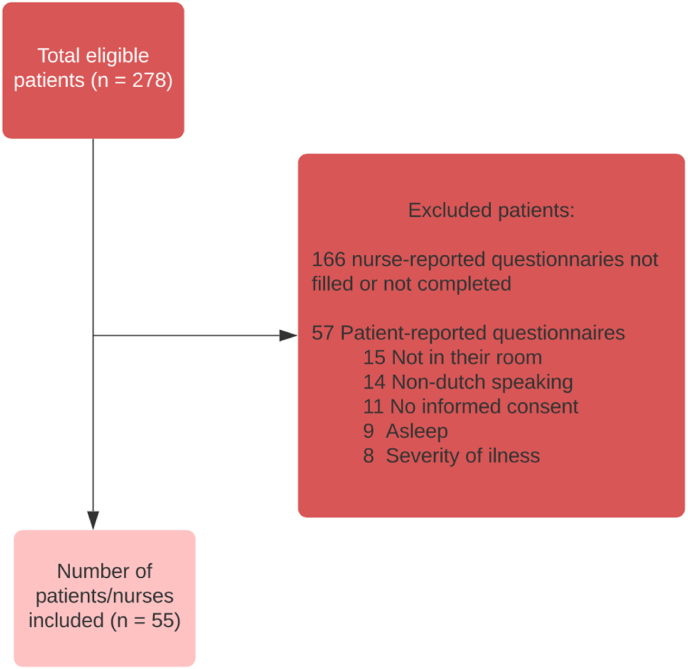
A total of 278 patients were admitted to the wards at the days of data collection and 112 questionnaires were completed by nurses. However, 57 questionnaires were not included in this study due to the following reasons: patient was not in the room, asleep, too ill or unable to speak Dutch or sign informed consent. In the end, a total of 55 nurse-reported questionnaires and 55 patient-reported questionnaires were included (Fig. 1).
Fig. 1.
Patient inclusion flow diagram.
Average age of the patients was 63.8 years (SD 17.4) and 45.5% of the patients was male. Thirty-five patients (65.6%) were admitted at the Plastic Surgery Trauma Unit, others at the Gastroenterology and Liver Disease Department (Table 1). Twenty nurses (36.4%) had less than five years of experience, while 22 nurses (40%) had over 10 years of experience. The average number of patients under nurses’ responsibility during the night was 8.3 (SD 2.0) (Table 2).
Table 1.
Patient characteristics.
| Characteristics (n = 55) | Frequency (%)a |
|---|---|
| Age (mean, (SD)) | 63.8 (17.4) |
| Gender | |
| Male | 30 (45.5%) |
| Female | 25 (54.5) |
| Department | |
| Gastroenterologoy and Liver Disease | 20 (36.4) |
| Plastic Surgery and Trauma Unit | 35 (63.6) |
| Educational Levelb | |
| Primary school | 1 (1.8) |
| Lower general secondary school | 7 (12.7) |
| Higher general secondary school | 7 (12.7) |
| A-level education | 2 (3.6) |
| Intermediate vocational education | 15 (27.3) |
| Higher vocational education | 17 (30.9) |
| University education | 5 (9.1) |
All data are presented as frequency (%) unless stated otherwise.
Missing data n = 1 (1.8%).
Table 2.
Nurses' characteristics.
| Characteristics | Frequency (%)a |
|---|---|
| Work experience | |
| <5 years | 27 (49.1) |
| 5–10 years | 5 (9.1) |
| >10 years | 22 (40.0) |
| Number of patients to care for (mean, (SD)) | 8.3 (2.0) |
b Missing data (n = 10).
All data are presented as frequency (%) unless stated otherwise.
3.2. RSCQ
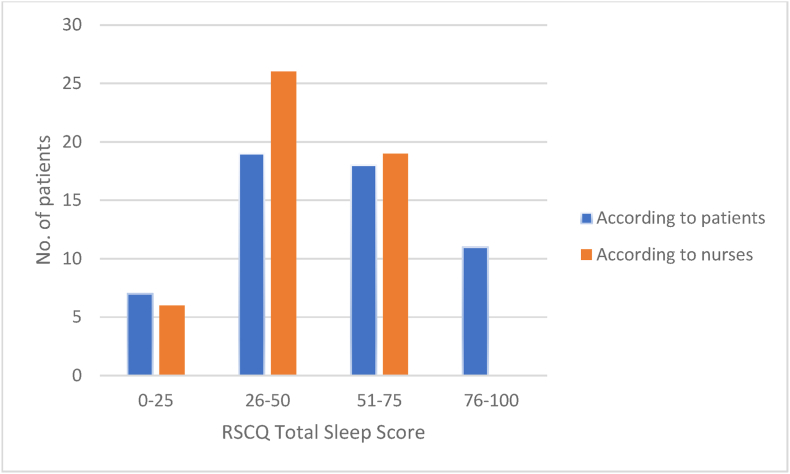
Patients’ ratings of how well they slept varied substantially, with some sleeping not at all, and some very well. Fig. 2 shows the variation in RSCQ Total score according to patients and nurses. The patient self-reported and nurse proxy-reported RCSQ were generally not normally distributed and thus subjected to non-parametric statistics. Table 3 presents median and interquartile range (IQR) for the patient self-reported and nurse proxy-reported RSCQ-scores. Except for the RSCQ Sleep Depth Score (p = .012), there was no statistically significant difference between the patient self-reported and the nurse proxy-reported RSCQ scores. Despite this lack of significance, there was a pattern of nurses reporting higher scores (better sleep) than patients.
Fig. 2.
Patients divided into four groups based on RSCQ total sleep score; 0–25 indicate very poor sleep quality; 76–100 indicate very good sleep quality. Responses patients = 55; Nurses = 51 (4 missing).
Table 3.
RCSQ questionnaire: patients' versus nurses' estimates.
| Scale | Patient median score (IQR) | Nurse median score (IRQ) | Median difference (95%-CI)d | Intra-class correlation coefficients (95%-CI) |
|---|---|---|---|---|
| Total scorec Patient(n = 55) Nurse (n = 51) |
54 (40) | 50 (18) | −4 (−11.5–3.5) p = .247a | .343 (−.149 – .625) p = .071 |
| Sleep depth Patient(n = 55) Nurse (n = 55) |
50 (40) | 70 (40) | 12.5 (2.5–20) p = .012 | .235 (−2.30 – .536) p = .137 |
| Sleep latency Patient(n = 55) Nurse (n = 52) |
70 (40) | 70 (30) | 2.5 (5.0–10.0) p = .552 | .065 (−.641 – .466) p = .406 |
| Awakenings Patient(n = 55) Nurse (n = 55) |
50 (30) | 60 (25) | 5.0 (−5.0 – 11.5) p = .341 | .435 (.039–.669) p = .018 |
| Return to sleep Patient(n = 55) Nurse (n = 54) |
57 (45) | 62.5 (31) | 10 (-1 – 20.0) p = .094 | .135 (−.436 – .486) p = .290 |
| Sleep Quality Patient(n = 55) Nurse (n = 54) |
60 (60) | 60 (30) | 10 (0.0–20.0) p = .068 | .338 (−.105 – .608) p = .058 |
| Noise levelb Patient(n = 55) Nurse (n = 55) |
80 (30) | 70 (30) | −10 (−17.50–0.0) p = .055 | -.278 (−1.118 – .240) p = .828 |
95%-CI = 95%-confidence interval, IQR = Interquartile range.
p-values in this column are calculated with a Wilcoxon Signed Rank test (based on the lowest n).
Question about noise levels is not part of the original 5-item Richards-Campbell Sleep Questionnaire (RCSQ) and is therefore not included in the Total Score (= mean of 5-items); it was included in this research for consistency with other studies that used the RCSQ.
Total score is the mean of 5-items (sleep depth, sleep latency, awakenings, returning to sleep, quality of sleep).
Median difference is calculated for complete pairs and is the difference between the patient's score and nurses' score.
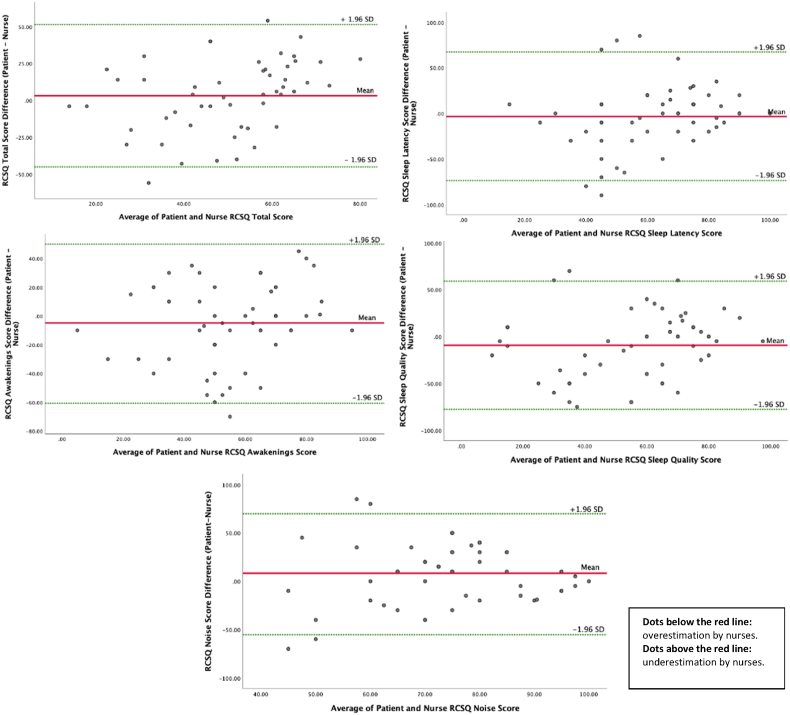
The Bland-Altman plots, providing information about agreement, revealed a significant amount of variation (bias) for the RSCQ Total Score (r = 0.0593, p = .008) (Fig. 3). This indicates relatively poor agreement between patient self-reported versus nurse proxy-reported RSCQ. Noise (r = 0.312, p = .575), sleep latency (r = 0.448, p = .099), awakenings (r = 0.293, p = .152), sleep quality (0.367, p = .094) did not reveal a significant amount of variation bias. The ICCs indicated poor reliability for all 7 measures (range −0.278 – 0.435). A significant difference between patient and nurse responses for sleep depth and returning to sleep were observed (p = .005 and p = .043, respectively) and therefore, no Bland-Altman plots were created for these variables.
Fig. 3.
Bland-Altman plots for the RCSQ Total, Sleep Latency, Awakenings, Sleep Quality and Noise scores show the relationship between the average of patient and nurse scores (x axis) and the difference between the patient's score and the nurse's score (y axis). The solid linear represents the mean of differences (bias), and the two dotted lines are the ± 1.96 Standard Deviation (SD). Help with interpretation: the median difference (average discrepancy) between patient and nurse scores is called the bias. If sometimes a patient scores 2 points higher than the nurse, but just as often it is the other way around, the average of differences will be zero and nurses and patients will generally agree (no bias). If all points are above or below zero, this means that nurses systematically under or over-estimate scores in comparison to patients (bias).
A significant difference between patients reported RSCQ Total score and nurses’ proxy-reported RSCQ Total score for nurses with more than 10 years of experience was observed (58 (20), 68 (44) respectively, p = .006), while no difference was present for nurses having <5 years or 5–10 experience (p = .432, p = .465, respectively).
Mean RCSQ total score for patients indicating very poor sleep quality (≤ 25), was 14.2 (SD 5.5), while nurse proxy-reported Total Score for this group was 41.0 (SD 17.9) (p-value for median difference = 0.015). The ICCs also indicated poor reliability (c = −0.042, 95%-CI (−0.459, 0.609)).
3.3. Sleep quantity
Patients' reported bedtime was 11:21 p.m. (SD 1:47), which was not significantly different from nurses’ reported bedtime. However, a significant difference was observed for the wake time (patient mean 06:06 a.m. (SD 1:45), nurse mean 5:38 a.m. (SD 1:32), p < .001) (Table 4). Self-reported sleep duration (e.g. time between sleep onset and final wakeup time) was 6:41 (hour:minutes) (SD 2:21), which did not significantly differ from proxy-reported sleep duration.
Table 4.
Sleep quantity.
| Parameter | Total Sample | P |
|---|---|---|
| Bedtime Patient n = 54 Nurse n = 50 |
11:19 p.m. (1:41) 11:17 p.m. (3:34) |
.959a |
| Nocturnal awakenings Patient n = 55 Nurse n = 55 |
3.6 (3.2) 3.2 (2.9) |
.530a |
| Waketime Patient n = 55 Nurse n = 42 |
6:04 a.m. (1:38) 5:38 a.m. (1:32) |
.000a |
| Sleep Duration, hh:mm Patient n = 55 Nurse n = 38c |
6:41 (2:21) 5:54 (2:06) |
.247a |
| Medication usage Patient (n = 55) Nurse (n = 55) |
38.2% 23.6% |
.077b |
| Start vital sign checks | 5:09 a.m. (0:15) | |
| Start administering medication | 5:21 a.m. (0:28) | |
| Number of visits by nurse during night | 4.1 (3.6) |
SD = standard deviation, IQR = Interquartile range, n = number included, hh:mm (hours:minutes).
p-values are calculated with a Paired T-Test.
p-values are calculated using the McNemar Test.
Seventeen out of 55 nurses did not fill in either the bedtime or the wakeup time. Out of those 17 nurses, 5 nurses indicated that the shift had ended before the patient woke up.
3.4. Sleep disrupters in the hospital
Three questions about possible sleep disrupters were included in the questionnaire. A distinction was made between disrupters causing prolonged sleep latency, awakenings during the night and waking up in the morning (see Appendix 1 for answers provided). Patients’ top five disrupters for falling asleep were pain, uncomfortable sleeping position, hospital staff, uncomfortable bed/pillow and light (29%, 20%, 18%, 11%, 11%, 11%, respectively). Nurses also thought pain to be the most disturbing factor, mentioned this in only 9% of the patients. Twenty-five percent of patients (14) and nurses (14) selected at least one disrupter causing prolonged sleep latency. According to patients, nocturnal awakenings were mainly caused by care-related routines (including the noise associated with it), pain, noises from other patients, visiting the toilet and an uncomfortable sleeping position (40%, 29%, 24%, 24%, 22% respectively). In general, this was in line with responses from the nurses, except they 1) accounted care-related routines as more disruptive as perceived by patients and 2) had noises from medical equipment in their top five instead of uncomfortable sleeping position. Nurses visited patients on average 4.1 (SD 3.6) times per night for care-related routines (Table 4). The main reason for patients to wake up in the morning were caused by healthcare professionals (60%), which was also mentioned by the nurses as being most disruptive (45%). A possible explanation would be the average time for vital checks in the morning being 05:09 a.m. (SD 00:15).
4. Discussion
The aim of this research was to assess the patient-nurse agreement on the patient's sleep quality and factors disturbing sleep in two non-ICU inpatient nursing units. Sleep quality was scored using the RCSQ questionnaire and information on sleep quantity was gathered using the CSD. A tendency for nurses to overestimate sleep quality was found, with a statistically significant difference in estimated sleep depth. In addition, when evaluating the interrater (patient versus nurse) agreement, nurses' sleep quality ratings were found to have poor reliability compared with patients' ratings, underpinning the tendency to overestimate sleep quality. To our knowledge, this is the first study to evaluate the differences between nurses and patients view on sleep quality in non-ICU settings.
These findings are like reported reliability/agreement studies in ICU patients. Some studies showed a wide range of differences in patients' and nurses' scores, suggesting poor agreement [19], [20]. Another study found slight to moderate reliability for nurses ratings compared with patients' ratings with all RCSQ scores being significantly different between patient reported scores and nurses proxy-reported scores [14]. Compared to our findings, no significant difference for ICC was observed in the latter for Sleep latency, Awakenings, Returning to sleep, Total RCSQ score, Sleep depth and Sleep Quality (.07 (−0.64 – 0.47) vs 0.21 (0.00–0.49); 0.44 (0.04–0.67) vs 0.22 (0.00–0.49); 0.14 (−0.44 – 0.49) vs 0.14 (0.00–0.40); 0.34 (−0.15 – 0.63) vs 0.49 (0.26–0.67); 0.24 (−2.3 – 0.54) vs 0.24 (0.00–0.52); 0.34 (−0.11 – 0.61) vs 0.17 (0.00–0.45), respectively) [14]. So, although nursing care for patients in the ICU is often based on a 1:1 ratio, nurses working at regular wards (often with a ratio of 1:8) do not seem to predict patient's sleep different.
The results also show that nurses with more years of working experience (>10 years), tend to estimate patients' sleep quality (e.g. RCSQ total score) higher (or better) than their patients, and fellow nurses with zero to 10 years of experience. A possible explanation for this finding could be that experienced nurses are accustomed to the hospital routine and therefore more blind to hospital-related sleep-disrupting factors. Another explanation could be that experienced nurses are better in estimating patients' overnight deterioration, which could result in less frequent nursing checks during the night. In this case, it would be important that nurses are able to distinguish poor sleepers and moderate/good sleepers. The results suggest, however, that nurses find it difficult to assess patients' sleep quality especially when the overall sleep quality is poor. As a result, it is important to realize that healthcare professionals – in this case nurses – are not that good in estimating patient's sleep. Hence it is imperative they explicitly ask patients in the morning how they've slept, so that proactive action can be taken to prevent a recurrence of a bad night's sleep. Previous research showed that nurses lack a complete knowledge about basis sleep physiology [21], which could potentially explain this inadequacy.
With respect to sleep disturbances, results show that nurses are relatively overestimating their own role in causing sleep disturbances and underestimating patient-related factors (such as pain and uncomfortable sleeping position). Despite this overestimation by nurses about their own role, our results do show that awakenings are mostly caused by care-related routines (like vital checks). However, these assessments are often important to improve patient safety (and prevent deterioration over the night) and are therefore seen as necessary. Recent research has shown that machine-learning algorithms could help to predict overnight in-hospital deterioration [22]. This could potentially reduce sleep disturbance from checkups in the near future. Care-related routines were also one of the main reasons reported by patients for waking up in the morning. This was also empathized by the average starting time for the vital check rounds around 5 a.m. Under normal circumstances (e.g. at home), most individuals would be still asleep at that time. Understanding the need to provide uninterrupted periods of sleep and leave patients to sleep for as long as possible in the morning is key. Waking an individual during the sleep cycle and/or limiting the total length of sleep might cause sleep deprivation, and therewith negative health outcomes. Our results underscore the need for restructuring routine care, to support uninterrupted sleep. In addition, light was mentioned by 11% of patients to be disruptive for both sleep latency as well as awakenings compared to 3% of nurses, suggesting the necessity of improving environmental factors in the medical care setting.
The strengths of this study are in the theme and its design. This was the first study to assess patient-nurse agreement on sleep in a general hospital population. The nurses did not know on which days the study would take place, to minimize information bias. To avoid nurses choosing the ‘easy-to-remember’ patients first, questionnaires were offered in a random, but fixed order. The included 55 patient-nurse pairs are many more than the pre-set sample size of 30 pairs.
This study had potential limitations. First, including only two wards from one hospital may limit the generalizability of the findings to other wards and hospitals. However, the results were similar to scores reported in prior studies, limiting this concern. Second, night nurses usually take care of many patients during their shift (average 8.2 (SD 2.0)), potentially leading to a recall bias. To minimize this risk, nurses were approached in the early morning at the end of their shift. Thirdly, observer bias may have occurred. It is possible that nurses have rated sleep more negatively, considering that patients often complain of poor sleep. Finally, patients who were too ill or cognitive unable to give informed consent were excluded. As we know that ill and cognitive impaired patients often suffer from extreme sleep disruption, this sampling bias might have caused an overestimation of the quality of sleep of hospitalized patients. As our data showed an especially poor patient-nurse agreement in poor sleepers, this might also have caused an overestimation of the patient-nurse agreement found in this study.
Our results might suggest that nurses' RCSQ is not suitable for the evaluation of patient's sleep. However, it did demonstrate to be a suitable way to highlight the discrepancies between nurses and patients. Future research could focus on designing a questionnaire for nurses to score patients sleep more appropriately. In addition, it would be interesting to focus on the patient-nurse agreement in different ward settings and patients' characteristics (e.g. age, comorbidity) to understand the underlying reasons for disagreement. Including a third objective assessment of sleep (for instance actigraphy) to overcome the potential bias in self-report could also be of interest.
5. Conclusion
In conclusion, patient-nurse agreement of the RCSQ-based sleep questionnaire was poor, with nurses tending to overestimate sleep quality compared to their patients. In addition, nurses are relatively overestimating their own role in causing sleep disturbances and underestimating patient-related factors (such as pain and uncomfortable sleeping position). A recommendation for nurses (and other professionals) would be to explicitly ask hospitalized patients about (potential) sleep disturbances. Future sleep improvement initiatives could focus on expanding knowledge about basic sleep physiology, to learn how to discern and (better) support poor sleepers.
Upcoming similar investigations of evaluating patient-nurse differences in sleep should evaluate the effect of different settings and patients’ characteristics to evaluate any potential proxy-related bias.
Data availability statement
The anonymized dataset will be made available on reasonable request after approval of the corresponding author.
Ethics statement
This study was part of a larger research project exploring the sleep of acutely admitted patients. The Executive Committee of the Medical Ethics Review Committee of VU University Medical Center (IRB00002991) decided that the Medical Research involving Human Subjects Act did not apply (reference No. 2019.246). Written informed consent was obtained from all participants.
Funding
No funding was received for this study.
CRediT authorship contribution statement
Eva S. van den Ende: designed the study, was responsible for data collection and the statistical analysis. Pia Burger: was responsible for the statistical analyses and wrote the first draft of the manuscript. Marjolein Keesenberg: designed the study and was involved during datacollection. Nurse students (see acknowledgments): were involved in recruiting participants and collecting the data. All authors: reviewed and approved the final version of the manuscript.
Declaration of competing interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to express great appreciation to all patients and nurses who participated in this study. We would also like to extend our gratitude to the nurse students of Hogeschool Inholland who contributed to the inclusion of participants; Melissa Blom, Tim Sol, Peggy Sue Verburg, Roman Verbruggen, Roisin Gevers, Lana Schouten, Lisa van den Berg, Lyba Chaudhry and Bonnie de Boer, and their mentors; Karina Meijers Verhoeven, Anne Francine Kanneworff and Dyanne Kelderman.
Appendix 1.
| Sleep latency |
Awakenings during the night |
Waking up in the morning |
|||
|---|---|---|---|---|---|
| Patient | Nurse | Patient | Nurse | Patient | Nurse |
| Pain (29%) | Pain (9%) | Hospital staff (40%) | Hospital staff (55%) | Hospital staff (60%) | Hospital staff (45%) |
| Uncomfortable sleeping position (20%) | Hospital staff (7%) | Pain (29%) | Toilet visit (29%) | No reason (18%) | Toilet visit (13%) |
| Hospital staff (18%) | Uncomfortable sleeping position (7%) | Noise other patients (24%) | Noise other patients (22%) | Other reason (18%) | Pain (11%) |
| Uncomfortable bed/pillow (11%) | Noise other patients (5%) | Toilet visit (24%) | Pain (22%) | Pain (15%) | Medical equipment (9%) |
| Light (11%) | Worries (5%) | Uncomfortable sleeping position (22%) | Medical equipment (20%) | Medical equipment (9%) | No reason (7%) |
| Noises other patients (11%) | Toilet visit (5%) | No reason (15%) | Worries (9%) | Noise other patients (9%) | Uncomfortable sleeping position (5%) |
| Noises staff (9%) | No reason (5%) | Light (11%) | No reason (9%) | Bed or pillow not comfortable (9%) | Noise other patients (4%) |
| Nausea (9%) | Light (3%) | Bed of pillow not comfortable (11%) | Move to other room (5%) | Toilet visit (9%) | Light (2%) |
| Other reasons (9%) | Fear (3%) | Too warm (9%) | Bed of pillow not comfortable (5%) | Worries (7%) | Bed or pillow not comfortable (2%) |
| No reason (7%) | Nausea (2%) | Medical equipment (7%) | Uncomfortable sleeping position (5%) | Too cold (7%) | Fear (2%) |
| Toilet visit (5%) | Slept too long during the day (2%) | Too cold (7%) | Other reasons (5%) | Light (4%) | Worries (2%) |
| Too hot (5%) | Too cold (2%) | Other reasons (7%) | Light (4%) | Too warm (4%) | Other reasons (2%) |
| Dyspneu (5%) | Too hot (2%) | Move to other room (5%) | Nausea (4%) | Set alarm (4%) | No reason provided (47%) |
| Fear (3%) | No reason provided (75%) | Fear (5%) | Slept too long during the day (4%) | Move other room (2%) | |
| Medical equipment (2%) | Worries (5%) | too hot (2%) | No reason provided (7%) | ||
| Too cold (2%) | Nausea (5%) | too cold (2%) | |||
| No reason provided (40%) | Slept too long during the day (4%) | No reason provided (25%) | |||
| Dyspneu (4%) | |||||
| Set alarm (2%) | |||||
| No reason provided (15%) | |||||
References
- 1.Leproult R., Van Couter E. Role of sleep and sleep loss in hormonal release and metabolism. Endocr Dev. 2010;17:11–21. doi: 10.1159/000262524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kopasz M., Loessl B., Hornyak M. Sleep and memory in healthy children and adolescents - a critical review. Sleep Med Rev. 2010;14:167–177. doi: 10.1016/j.smrv.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 3.Tononi G., Cirelli C. Sleep function and synaptic homeostasis. Sleep Med Rev. 2006;10(1):49–62. doi: 10.1016/j.smrv.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 4.Dinges D.F. The state of sleep deprivation: from functional biology to functional consequences. Sleep Med Rev. 2006;10(5):303–305. doi: 10.1016/j.smrv.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 5.Stickgold R., Walker M.P. Sleep-dependent memory consolidation and reconsolidating. Sleep Med. 2007;8(4):331–343. doi: 10.1016/j.sleep.2007.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Medic G., Wille M., Hemels M.E. Short- and long-term health consequences of sleep disruption. Nat Sci Sleep. 2017;9:151–161. doi: 10.2147/NSS.S134864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alvarez G.G., T A.N. The impact of daily sleep duration on health: a review of the literature. Prog Cardiovasc Nurs. 2004;19:56–59. doi: 10.1111/j.0889-7204.2004.02422.x. [DOI] [PubMed] [Google Scholar]
- 8.Chorney D.B., Detweiler M.F., Morris T.L., Kuhn B.R. The interplay of sleep disturbance, anxiety and depression in children. Journal of Paediatric Psychology. 2008;33(4):339–348. doi: 10.1093/jpepsy/jsm105. [DOI] [PubMed] [Google Scholar]
- 9.Aktas Y.Y., Yilmaz E.B. The association of pain, anxiety, depression, and sleep patterns in postoperative Turkish patients. Kuwait Medical Journal. 2017;49(4):306–312. [Google Scholar]
- 10.Adib-Hajbaghery M., Izadi-Avanji F., Akbari H. Quality of sleep and its related risk factors in hospitalized older patients in Kashan's Hospitals, Iran 2009. Iran J Nurs Midwifery Res. 2012;17(6):414–420. [PMC free article] [PubMed] [Google Scholar]
- 11.Foo C.T., O'Driscoll D.M., Ogeil R.P., Lubman D., Young A.C. Sleep & breathing = Schlaf & Atmung; 2021. Barriers to sleep in acute hospital settings. [DOI] [PubMed] [Google Scholar]
- 12.Tamrat R, Huynh-Le Mp Fau - Goyal M, Goyal M. Non-pharmacologic interventions to improve the sleep of hospitalized patients: a systematic review. (1525-1497 (Electronic)). [DOI] [PMC free article] [PubMed]
- 13.Frisk U, Nordström G. Patients' sleep in an intensive care unit--patients' and nurses' perception. (0964-3397 (Print)). [DOI] [PubMed]
- 14.Kamdar B.B., Shah Pa Fau, King L.M., King Lm Fau, Kho M.E., Kho Me Fau, Zhou X., Zhou X Fau, Colantuoni E., Colantuoni E Fau, Collop N.A., et al. 2012. Patient-nurse interrater reliability and agreement of the Richards-Campbell sleep questionnaire. (1937-710X (Electronic)) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koo T.K., Li M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. Journal of chiropractic medicine. 2016;15(2):155–163. doi: 10.1016/j.jcm.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Richards KC, O'Sullivan Ps Fau - Phillips RL, Phillips RL. Measurement of sleep in critically ill patients. (1061-3749 (Print)). [PubMed]
- 17.Carney C.E., Buysse D.J., Ancoli-Israel S., Edinger J.D., Krystal A.D., Lichstein K.L., et al. The consensus sleep diary: standardizing prospective sleep self-monitoring. Sleep. 2012;35(2):287–302. doi: 10.5665/sleep.1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yu D.S.F., Lee D.T.F., Woo J. Issues and challenges of instrument translation. West J Nurs Res. 2004;26(3):307–320. doi: 10.1177/0193945903260554. [DOI] [PubMed] [Google Scholar]
- 19.Bourne R.S., Minelli C Fau, Mills G.H., Mills Gh Fau - Kandler R., Kandler R. 2007. Clinical review: sleep measurement in critical care patients: research and clinical implications. (1466-609X (Electronic)) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nicolás A., Aizpitarte E Fau, Iruarrizaga A., Iruarrizaga A Fau, Vázquez M., Vázquez M Fau, Margall A., Margall A Fau, Asiain C., Asiain C. 2008. Perception of night-time sleep by surgical patients in an intensive care unit; pp. 1478–5153. [Electronic))] [DOI] [PubMed] [Google Scholar]
- 21.McIntosh A.E., MacMillan M. The knowledge and educational experiences of student nurses regarding sleep promotion in hospitals. Nurse Educ Today. 2009;29(7):796–800. doi: 10.1016/j.nedt.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 22.Tóth V., Meytlis M., Barnaby D.P., et al. Let Sleeping Patients Lie, avoiding unnecessary overnight vitals monitoring using a clinically based deep-learning model. npj Digit Med. 2020;3:149. doi: 10.1038/s41746-020-00355-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The anonymized dataset will be made available on reasonable request after approval of the corresponding author.