Abstract
Objective
To describe how and why patient contracts are used for the management of chronic medical conditions.
Data sources
A scoping review was conducted in the following databases: MEDLINE, Embase, AMED, PsycInfo, Cochrane Library, CINAHL, and Nursing & Allied Health. Literature from 1997 to 2017 was included.
Study selection
Articles were included if they were written in English and described the implementation of a patient contract by a health care provider for the management of a chronic condition. Articles had to present an outcome as a result of using the contract or an intervention that included the contract.
Synthesis
Of the 7528 articles found in the original search, 76 met the inclusion criteria for the final review. Multiple study types were included. Extensive variety in contract elements, target populations, clinical settings, and cointerventions was found. Purposes for initiating contracts included behaviour change and skill development, including goal development and problem solving; altering beliefs and knowledge, including motivation and perceived self-efficacy; improving interpersonal relationships and role clarification; improving quality and process of chronic care; and altering objective and subjective health indices. How contracts were developed, implemented, and assessed was inconsistently described.
Conclusion
More research is required to determine whether the use of contracts is accomplishing their intended purposes. Questions remain regarding their rationale, development, and implementation.
Résumé
Objectif
Décrire comment et pourquoi les contrats avec les patients sont utilisés pour la gestion de problèmes de santé chroniques.
Sources d’information
Une revue exploratoire a été effectuée dans les bases de données suivantes : MEDLINE, Embase, AMED, PsycInfo, Bibliothèque Cochrane, CINAHL et Nursing & Allied Health. Les articles parus de 1997 à 2017 ont été inclus.
Sélection des études
Les articles ont été retenus s’ils étaient rédigés en anglais et s’ils décrivaient la mise en œuvre d’un contrat avec un patient par un professionnel de la santé pour la gestion d’un problème chronique. Les articles devaient présenter une issue comme étant le résultat de l’utilisation du contrat ou d’une intervention qui incluait le contrat.
Synthèse
Des 7528 articles recensés dans la recherche initiale, 76 répondaient aux critères d’inclusion dans la revue finale. De multiples types d’études ont été inclus. Une diversité considérable dans les éléments de contrat, les populations visées, les milieux cliniques et les interventions conjointes a été observée. Les raisons de conclure un contrat incluaient des changements comportementaux et le perfectionnement des compétences, y compris l’établissement d’objectifs et la solution de problèmes; la modification des croyances et des connaissances, notamment la motivation et l’auto-efficacité perçue; l’amélioration des relations interpersonnelles et la clarification des rôles; l’amélioration de la qualité et des processus des soins chroniques; la modification des indicateurs objectifs et subjectifs de la santé. Les descriptions de l’élaboration, de la mise en œuvre et de l’évaluation des contrats manquaient de cohérence.
Conclusion
Il faut plus de recherches pour déterminer si l’utilisation de contrats permet d’atteindre les objectifs prévus. Des questions demeurent sans réponses quant à leur justification, leur élaboration et leur mise en œuvre.
Chronic disease management is a substantial part of the clinical workload in primary care. Many practitioners use a patient contract to manage these conditions,1 which is defined as “any type of agreement, verbal or written, by which one or both parties agree to a set of behaviours related to the care of a patient.”1 Examples include no-smoking agreements, treatment plans, and medication agreements. Given the dominance of the chronic care model for disease with patient self-management and a collaborative approach to these activities, it is apparent why these are applied broadly in primary care.2
At the time of this study, there were only 2 reviews of patient contracts and their effectiveness. In 2007, the Cochrane Collaboration conducted a systematic review of randomized controlled trials (RCTs) to assess the effectiveness of contracts between patients and health care practitioners on patient adherence to treatment, prevention, and health promotion.1 They concluded that there was not enough reliable evidence to recommend the routine use of contracts.1 A review of opioid contracts in 2016 by the Centers for Disease Control and Prevention found limited evidence regarding benefits and harms of opioid contracts for preventing the abuse and selling of opioids.3 The Cochrane Collaboration article focused on RCTs that evaluated the effects of contracts on patient adherence to health care provider recommendations and limited the scope to interventions in high-income countries.1 Even within this subset of contracts, there was substantial complexity and heterogeneity in patient contracts, making it difficult to determine their overall effectiveness.1 The review noted that trials testing contracts that demonstrated positive effects, particularly in the realm of substance addiction, were small and their quality uncertain.1 Many studies failed to consider potential harms of contracts.1
Despite their lack of reliable evidence, practitioners continue to use patient contracts across a range of activities, adapting them to their settings, populations, and scopes of practice.1 The Cochrane review suggests there may be extensive heterogeneity in the way patient contracts are used, even within the limited populations and indications considered in the review.1 A broader understanding of patient contracts is required to understand the pervasiveness of their use, despite the lack of convincing evidence to support contracts. Second, capturing a comprehensive description of how contracts are rationalized, developed, implemented, and assessed will enable further research in determining their effectiveness.
We conducted a scoping review to increase breadth of knowledge around how and why patient contracts are used for the management of chronic medical conditions in health care settings. Specifically, we sought to understand the purpose, development, implementation, and composition of contracts.
METHODS
Data sources
We conducted a scoping review using the 5 steps outlined by Arksey and O’Malley.4,5 The protocol is available from https://medm-backend.fammedmcmaster.ca/wp-content/uploads/2018/05/Contracts-scoping-review-protocol-17-July-2019-EG.pdf. We searched the following databases: MEDLINE, Embase, AMED, PsycInfo, Cochrane Library, CINAHL, and Nursing & Allied Health. To balance feasibility with breadth and comprehensiveness, we included literature from 1997 to 2017. The final search was conducted on June 6, 2017.
Study selection
We originally selected articles using the search terms contract or contracts. As familiarity with the literature increased, exclusion terms were added through an iterative process to further refine the search results (Appendix A, available from CFPlus*). Two university librarians were consulted in developing the search strategy. The research team was composed of physicians and public health professionals with expertise in the management of chronic conditions and experience with scoping review methodology. Inclusion criteria were the following: articles had to be written in English, they had to describe the implementation of a patient contract by a health care provider for the management of a chronic condition, and the contract had to specify at least 1 treatment, prevention, or health promotion activity to be observed. Articles were excluded if they only addressed a process of informed consent for a treatment, were not primary research articles (eg, review or commentary articles), or were inaccessible to the researchers. The first 35 articles from the Cochrane database were reviewed by 2 independent researchers for possible inclusion. Disagreements were discussed in detail until consensus was reached. A detailed article selection protocol was then developed and 3 researchers were recruited to participate in the remainder of the article selection process. A subset of 30 articles was initially reviewed by all 3 researchers to ensure consistency in the selection for inclusion, where there was unanimous agreement. The rest of the articles were divided among the 3 researchers, with uncertainty decided upon by consensus of all 3 researchers.
Data collection and management
We extracted data onto a standardized form using a broad set of variables (Box 1). The research team, composed of physicians and public health professionals with expertise in the management of chronic disease and patient contracts, approved the variables used. Three screening researchers independently extracted these data for the first 10 articles and then met to check agreement. Each screening researcher then proceeded independently; any uncertainties were discussed with the other 2 screening researchers and final decisions were reached through consensus.
Box 1. Data extraction variables.
General study characteristics (title, author, year, country, health care setting)
Chronic condition and target population
Purpose of the contract and specific target or desired outcome
Contract development characteristics (underpinning behaviour theory, development process, and contract elements)
Contract implementation characteristics and processes (training for use [how health care providers were trained to use the contracting details], cointerventions or incentives, and opportunity for patient input and goals)
Consistent with scoping review methodology,4 the quality of the studies was not formally assessed, as the substance of all studies was considered important for understanding concepts to address the research question. While our interest was in primary care use, with the general move toward vertical integration of care, we decided to include descriptions of primary research in primary care, primary health care, and secondary and tertiary health care settings. Data were summarized quantitatively using simple frequency counts of general, development, and implementation variables for contracts. We used thematic (semantic) analysis to describe commonly occurring themes in terms of the purposes of contracts.6 Having multiple members of the research team with expertise in the use of contracts also contributed to rigour of this analysis. We applied PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews) to ensure all essential items were reported for a scoping review (Appendix B, available from CFPlus*).
SYNTHESIS
General information
In total, 76 articles met the inclusion criteria (Figure 1). Charting for each variable within each article can be found in Appendix C, available from CFPlus.* There were 21 articles from 1997 to 2003, 29 articles from 2004 to 2010, and 26 articles from 2011 to 2017. Most studies were based in the United States (n=51, 67%). The remaining 33% were from the United Kingdom (n=4); Australia and the Netherlands (n=3 each); France, Canada, and Germany (n=2 each); and Malawi, Korea, Portugal, Cameroon, Sweden, Puerto Rico, Norway, Japan, and Thailand (n=1 each).
Figure 1.
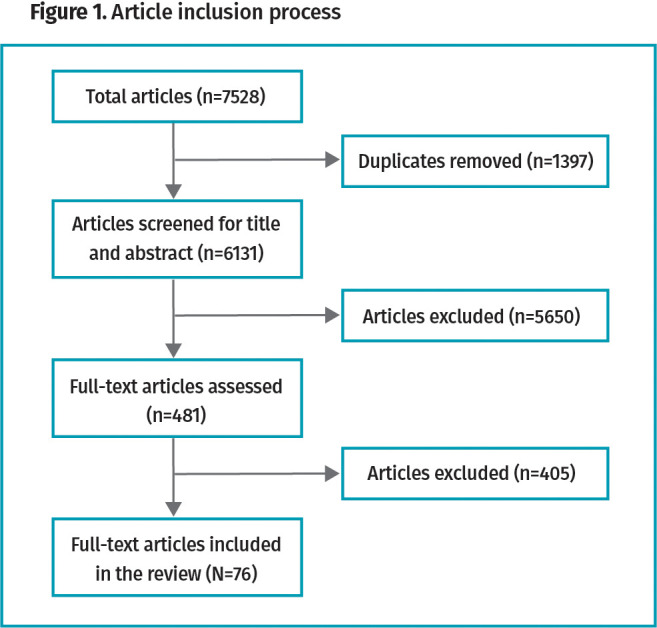
Article inclusion process
The most common study design was RCTs (n=42, 55%), followed by observational studies (n=23, 30%) and non-randomized interventional studies (n=11, 15%). We found an extensive variety of chronic conditions commonly encountered in primary care (Table 1).7-82 While we found that contracts were interchangeably referred to using other terms in the studies, only 3 did not include the word contract in their names, instead referring to an agreement8,78 or plan.38 In general, the contract terminology identified the process of care or treatment, the purpose of the contract, and the parties in the contract.
Table 1.
Chronic conditions for which patient contracts were used and the names given to the contracts by the health care provider
| CHRONIC CONDITIONS* | CONTRACT NAMES† |
|---|---|
| Substance use (marijuana, tobacco, alcohol, opioids)7-32 | Contract, no-smoking agreement, deposit contract, behavioural continuing care contract, trilateral opioid contract, treatment contract, behavioural contract(ing), substance use disorder contract, monitoring contract, verbal contract, aftercare (participation) contract, moral contract, alcohol contract, Antabuse [ie, disulfiram] contract, contingency contract, quit contract, substance monitoring contract, commitment contract |
| Psychiatric disorders (suicidal, borderline personality disorder, depression, posttraumatic stress disorder, schizophrenia, bipolar disorder, disruptive behaviour, attention deficit hyperactivity disorder, dissociative identity disorder, anorexia nervosa)11,16,18,19,21,33-45 | Contract(ing), contract for safety, no-suicide contract, behavioural continuing care contract, treatment contract, treatment plan, behaviour(al) contract, mental and behavioural health contract, monitoring contract, therapeutic contract, weight contract, self-referral to inpatient treatment contract, parent-teen contract |
| Risk factors (diet, exercise, obesity)46-52 | Physical activity contract, behavioural contract, health contract calendar, contract for change tool, deposit contract, social support contract |
| Respiratory conditions (asthma, chronic obstructive pulmonary disease)53-61 | Contingency contract(ing), behavioural contract, health contract, family contract, contract |
| Cardiovascular conditions (angioplasty, percutaneous coronary intervention, hypertension)27,54,62-65 | Behavioural contract, treatment contract, weight-loss contract |
| Musculoskeletal conditions (osteoarthritis, fibromyalgia)66-69 | Patient contract, therapeutic contract, negotiated follow-up contract, physical activity maintenance contract, behavioural contract |
| Infectious diseases (HIV, hepatitis C virus, latent tuberculosis)16,70-72 | Contract referral, treatment contract, contingency contracting |
| Disabilities (intellectual, developmental, physical, neurologic)73-76 | Behavioural contract, contract, contingency contract |
| Chronic pain77,78 | Medication contract, pain contract, medication contract or agreement, provider-patient agreement, opioid contract |
| Organ failure (dialysis, liver transplant)79,80 | Health contract, self-contracting |
| Diabetes62,81 | Treatment contract, contingency contract |
| Contact lens wearers and glasses wearers82 | Health care contract |
Some articles covered more than 1 chronic condition.
Some articles referred to contracts by more than 1 name.
We found that contracts were initiated across a broad spectrum of health care settings, including in the community, primary care clinics, and hospital outpatient clinics (Table 2). The interventions typically targeted adults (n=57, 75%), with some directed at adolescents and young adults (n=11, 14%), children (n=2, 3%), geriatric populations (n=5, 7%), or unknown populations (n=1, 1%). Most contracts were between the patients and their health care providers (n=51, 67%) (Table 3).
Table 2.
Settings where contract interventions were initiated to manage chronic medical conditions
| SETTING* | ARTICLE FREQUENCY |
|---|---|
| Community (pharmacy, call centre, patient home, optometry clinic, public health clinic, school) | 32 |
| Specialty outpatient medical clinic | 24 |
| Primary care medical clinic | 18 |
| Inpatient unit | 4 |
| Emergency department | 2 |
| Unknown | 1 |
Some articles covered more than 1 setting.
Table 3.
Included parties of contracts for managing chronic medical conditions
| PARTIES IN THE CONTRACT | ARTICLE FREQUENCY |
|---|---|
| Patient and health care provider | 51 |
| Guardian or patient and health care provider | 13 |
| Patient and peer or health care provider | 5 |
| Unknown | 7 |
Contract purpose and development
We assessed contract purpose and found 5 common categories (Table 4).37,39,74,78,82 Only 11 articles (14%) described how the contracts had been developed, with 33 articles (43%) reporting using patient input in devising the contracts, although the range of initial input varied considerably. While many theories of behaviour were used to rationalize the use of a particular intervention, it was not always clear if the theory was specific to the use or development of the contract (Box 2).12,17,31,36,48-50,53,55,58,71,73,79,81 Only 14 articles (20%) mentioned health behaviour theories specific to their respective contracts (Box 2).12,17,31,36,48-50,53,55,58,71,73,79,81
Table 4.
Purposes of patient contracts
| CONTRACT PURPOSE | EXAMPLE |
|---|---|
| Altering objective or subjective health indices | A contract specifying goal weights for patients with anorexia nervosa37 |
| Improving interpersonal relationships and role clarification | A contract clarifying the roles of family members in managing the illness of their family member with schizophrenia39 |
| Behaviour change and skill development, including goal development and problem solving | Mandating a paraplegic patient to receive regular wound care before being accepted for a surgical intervention74 |
| Improving the quality or process of chronic care | Improving the safety of care by using a contract outlining the conditions for which controlled medications would be prescribed for the management of chronic noncancer pain78 |
| Altering beliefs and knowledge, including motivation and perceived self-efficacy | An educational program for contact lens wearers regarding proper lens and eye care82 |
Box 2. Theories of behaviour behind interventions in contracts aimed at managing chronic medical conditions.
Contract implementation
Only 11 articles (14%) mentioned or described training of health care professionals for the implementation of the contract. Six articles (8%) included only a contract, while most included contracts as part of complex cointerventions. The most common follow-up duration was 1 year or less (n=57, 75%), with only 2 studies following patients for more than 2 years. Follow-up duration could not be determined in 8 articles (11%). A minority of articles (n=16, 21%) described a process for reviewing the contracts following their initial implementation. Some form of incentive for patients was used in 20 articles (26%). Examples of incentives included financial rewards,10,50 the prospect of doing enjoyable activities,56 and the promise of further treatments.74 Twenty-five articles (33%) included patient goals in their contracts, which ranged from patients selecting them off a menu to having full authority over what was to be accomplished.
Contract composition
A number of easily identifiable elements existed within the contracts, including but not limited to prescribed and forbidden behaviour; rewards or incentives; consequences; medication and treatment prescriptions; action plans; information on risks and benefits of treatment; schedules for prescribed activities; explanation of threats and barriers to success, and suggested techniques to overcome them; responsibilities of those signing the contract; instructions, education, and rationale for the content of the contract; goals and targets for patient behaviour; identified social support for the patient; and objective assessment of health status. Patient input into the contract could occur through the inclusion of incentives and self-identified goals.
Identified gaps
There was extensive variability in the purposes, elements, development, and implementation processes for patient contracts. We have also identified major gaps in reporting around contracts, particularly around contract development and implementation processes (Appendix C*).
DISCUSSION
We found extensive variety in the nature and implementation of patient contracts for managing chronic medical conditions. Five general purposes for initiating a contract were discovered: to encourage behaviour change and skill development, to alter beliefs and knowledge, to improve interpersonal relationships and clarify roles, to improve the quality and process of chronic care, and to alter objective and subjective health indices. Many elements were included in individual contracts, such as prescribed and forbidden behaviour; rewards and incentives; consequences; medication and treatment prescriptions; action plans; risks and benefits of treatment; schedules; threats and barriers to success and techniques to overcome them; responsibilities of those signing the contract; instructions, education, and rationale; goals and targets; social support for the patient; and assessment of health status.
Strengths and fit with the broader literature
The Cochrane review of patient contracts for managing chronic conditions was limited in scope.1 This review found inadequate evidence for their effectiveness, with most research failing to consider potential harms.1 Despite the paucity of evidence for effectiveness, we discovered that reporting of contracts in the literature has not tapered off in the past decade or more. This may be in part because contracts seem to fit into popular behaviour change theories (ie, self-determination theory, theory of planned behaviour, stages of change, self-efficacy theory) that are tied to concepts of motivation, intention, and self-efficacy.83-86 This scoping review highlights the lack of explicit application of such theories in contract intervention development and implementation, likely hindering support of effectiveness.
Similar to the findings of the Cochrane review,1 addiction, hypertension, and obesity were common targets for contracts. This study identified many additional chronic conditions for which these tools are applied (Table 1).7-82
Weaknesses
A focus on the word contract in the search string may have resulted in missing literature, but this provides a clearer conceptual analysis regarding the term contract. It is possible that interventions labeled as agreements, plans, or other related terminology may imply or demand alternative theories or processes for implementation. We did not search the gray literature because of limitations on time and resources for the project.
The fact that at least 2 researchers did not review and extract data from each article created potential for reporting bias. Nevertheless, this approach was deemed appropriate for our study in which we simply describe the literature as opposed to assessing the quality of the evidence or systematically reviewing it.
Practice and policy implications
Most of the literature on contracts was produced in the United States, a society that reputedly values personal autonomy. The patient’s desire for personal autonomy can create tension, as contracts often do not take patient input and goals into consideration. Contracts are frequently targeted toward vulnerable populations, including those with mental illness and substance use disorder. While targeting groups with greater need is the most effective way to improve health equity, if a contract does not take into consideration patient input and goals, this goes against the process of empowerment that vulnerable populations often require, including skill development and continuity of resources.87
Most contracts in the literature occur in the outpatient community setting between a patient and health care provider, with fewer than 25% occurring in primary care clinics. It is possible that lack of frequent contact and a specialized focus are, and will continue to be, motivating factors for use of contracts in non–primary care settings.
Research implications
The development process for patient contracts, which underpins theory and rationale, and training for contract implementation were rarely included in the literature. In many cases, it was difficult to assess the rigour and fidelity with which contracts were implemented. The follow-up time generally appeared short, considering that behaviour change is often necessary for chronic disease self-management and this may take some time for the patient to implement. Few studies reported details of contract development and implementation, and there was no systematic approach for describing the composition elements. Tools such as the TIDierR (template for intervention description and replication) checklist can improve reporting of interventions and support more effective analysis and replication.87 These details are important if effectiveness is demonstrated, as they will help clarify the key elements of a contract. More comprehensive description and reporting in studies of contracts, including the elements we have described, would help determine contract effectiveness and key elements (see our example checklist in Table 5). These deficiencies could be addressed in future research.
Table 5.
Checklist for reporting patient contract interventions
| CHECKLIST ITEM | DESCRIPTION |
|---|---|
| Contract development | |
|
What behaviour does the contract intend to influence? What are the desired outcomes? |
|
Did formal behavioural theory influence the choice of contract as an intervention or influence contract development? |
|
How was the contract developed? Who developed the contract (were patients involved)? |
|
How was the contract validated? |
|
What elements made up the contract? Were incentives included? |
|
Who did the contract intend to target? Include all demographic variables |
|
Who initiated the contract? Who signed the contract? |
| Contract implementation | |
|
Did the overall intervention take place in a primary health care, primary care, secondary care, or tertiary care setting? |
|
What training took place for those implementing the contract? |
|
What other types of interventions took place alongside the contract? How were these accounted for in assessing outcomes? |
|
Was there an opportunity for the patient to alter the implementation of the contract or its content? |
|
How was the contract implemented? Was there opportunity for review and revision? |
|
How much time passed between the implementation of the contract and measurement of outcomes? |
|
Was the contract used in the way it was intended? To what extent was implementation faithful to the intervention description? |
|
What was the measure of effectiveness of the contract intervention? |
Development of a common set of relevant outcome measures would also be useful in systematic analyses across heterogeneous purposes and settings to determine whether contracts can be used to achieve their intended purposes. Finally, research aiming to provide further conceptual clarity between contracts and related terminology, such as agreements and plans, may provide further insight into which elements of interventions support positive changes for chronic disease management, if they in fact differ.
Conclusion
The nature and use of patient contracts for the management of chronic medical conditions are highly variable, and the existing review literature describes variable quality and comprehensiveness. Questions remain regarding the rationale, development, implementation, and effectiveness of patient contracts. Given their current broad application and the commitment required of health care providers and patients in their implementation, future research is needed to address this knowledge gap.
Supplementary Material
Acknowledgments
We thank Laura Banfield and Stephanie Sanger, librarians who helped with search strategy development; Cindy Cheng and Bethina Loiseau for their help with data extraction; Dr Fran Scott, Director of the Master of Public Health Program at McMaster University in Hamilton, Ont; and Dr Derelie Mangin, Larkin Lamarche, and Dr Michelle Howard for their editing contributions.
Editor’s key points
▸ Extensive variety exists in terms of why and how patient contracts are used for managing chronic medical conditions.
▸ Patient contracts tend to be used in North America despite limited evidence, are used to target vulnerable populations, and are used in outpatient and community settings.
▸ Gaps in the literature include limited descriptions of contract rationale, development, implementation, and evaluation processes. More comprehensive reporting and research are required to determine whether contracts are being used successfully to accomplish their intended purposes.
Points de repère du rédacteur
▸ Il existe une variété considérable de raisons et de modalités entourant l’utilisation de contrats avec les patients pour la prise en charge de problèmes de santé chroniques.
▸ Les contrats avec les patients ont tendance à être utilisés en Amérique du Nord, malgré des données probantes limitées à cet égard; ils sont utilisés pour cibler des populations vulnérables, dans les milieux ambulatoires et communautaires.
▸ Au nombre des lacunes dans la littérature médicale figuraient les descriptions limitées des processus de justification, d’élaboration, de mise en œuvre et d’évaluation des contrats. Des rapports et des recherches plus approfondis sont nécessaires pour déterminer si les contrats peuvent atteindre les objectifs prévus.
Footnotes
Appendices A, B, and C are available from https://www.cfp.ca. Go to the full text of the article online and click on the CFPlus tab.
Contributors
Dr Erin Gallagher conceived and designed the study, conducted the literature review, executed data gathering, contributed to data interpretation, and helped develop the final research paper as her master of public health thesis project. Dr Elizabeth Alvarez was the project supervisor and contributed to project development and knowledge synthesis. Dr Lin Jin helped with data acquisition and interpretation. Drs Dale Guenter and Lydia Hatcher sat on the thesis committee as content experts, refining the research question, data gathering, and interpretation processes. Dr Andrea Furlan was invited as an external reviewer for thesis defence and substantial improvements to the final paper resulted from her input.
Competing interests
None declared
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
References
- 1.Bosch-Capblanch X, Abba K, Prictor M, Garner P.. Contracts between patients and healthcare practitioners for improving patients’ adherence to treatment, prevention and health promotion activities. Cochrane Database Syst Rev 2007;(2):CD004808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bodenheimer T, Lorig K, Holman H, Grumbach K.. Patient self-management of chronic disease in primary care. JAMA 2002;288(19):2469-75. [DOI] [PubMed] [Google Scholar]
- 3.Dowell D, Haegerich TM, Chou R.. CDC guideline for prescribing opioids for chronic pain—United States, 2016. MMWR Recomm Rep 2016;65(1):1-49. Erratum in: MMWR Recomm Rep 2016;65(11):295. [DOI] [PubMed] [Google Scholar]
- 4.Arksey H, O’Malley L.. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8(1):19-32. [Google Scholar]
- 5.Levac D, Colquhoun H, O’Brien KK.. Scoping studies: advancing the methodology. Implement Sci 2010;5:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Braun V, Clarke V.. Using thematic analysis in psychology. Qual Res Psychol 2006;3(2):77-101. [Google Scholar]
- 7.Bernstein E, Edwards E, Dorfman D, Heeren T, Bliss C, Bernstein J.. Screening and brief intervention to reduce marijuana use among youth and young adults in a pediatric emergency department. Acad Emerg Med 2009;16(11):1174-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Den Exter Blokland EA, Engels RC, Harakeh Z, Hale WW 3rd, Meeus W.. If parents establish a no-smoking agreement with their offspring, does this prevent adolescents from smoking? Findings from three Dutch studies. Health Educ Behav 2009;36(4):759-76. Epub 2009 Jan 9. [DOI] [PubMed] [Google Scholar]
- 9.Crealey GE, McElnay JC, Maguire TA, O’Neill C.. Costs and effects associated with a community pharmacy-based smoking-cessation programme. Pharmacoeconomics 1998;14(3):323-33. [DOI] [PubMed] [Google Scholar]
- 10.Dallery J, Meredith S, Glenn IM.. A deposit contract method to deliver abstinence reinforcement for cigarette smoking. J Appl Behav Anal 2008;41(4):609-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DeMarce JM, Lash SJ, Stephens RS, Grambow SC, Burden JL.. Promoting continuing care adherence among substance abusers with co-occurring psychiatric disorders following residential treatment. Addict Behav 2008;33(9):1104-12. Epub 2008 Feb 23. [DOI] [PubMed] [Google Scholar]
- 12.Feeney GF, Young RM, Connor JP, Tucker J, McPherson A.. Cognitive behavioural therapy combined with the relapse-prevention medication acamprosate: are short-term treatment outcomes for alcohol dependence improved? Aust N Z J Psychiatry 2002;36(5):622-8. [DOI] [PubMed] [Google Scholar]
- 13.Feeney GF, Young RM, Connor JP, Tucker J, McPherson A.. Outpatient cognitive behavioural therapy programme for alcohol dependence: impact of naltrexone use on outcome. Aust N Z J Psychiatry 2001;35(4):443-8. [DOI] [PubMed] [Google Scholar]
- 14.Fishman SM, Mahajan G, Jung SW, Wilsey BL.. The trilateral opioid contract. Bridging the pain clinic and the primary care physician through the opioid contract. J Pain Symptom Manage 2002;24(3):335-44. [DOI] [PubMed] [Google Scholar]
- 15.Fleming MF, Manwell LB, Barry KL, Adams W, Stauffacher EA.. Brief physician advice for alcohol problems in older adults: a randomized community-based trial. J Fam Pract 1999;48(5):378-84. [PubMed] [Google Scholar]
- 16.Gallucci G, Smolinski J.. Treatment contracts for patients with hepatitis C, psychiatric illness, and substance abuse. Psychosomatics 2001;42(4):353-5. [DOI] [PubMed] [Google Scholar]
- 17.Hovell MF, Zakarian JM, Matt GE, Liles S, Jones JA, Hofstetter CR, et al. Counseling to reduce children’s secondhand smoke exposure and help parents quit smoking: a controlled trial. Nicotine Tob Res 2009;11(12):1383-94. Epub 2009 Oct 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jaffee WB, Chu JA, Woody GE.. Trauma, dissociation, and substance dependence in an adolescent male. Harv Rev Psychiatry 2009;17(1):60-7. [DOI] [PubMed] [Google Scholar]
- 19.Knight JR, Sanchez LT, Sherritt L, Bresnahan LR, Fromson JA.. Outcomes of a monitoring program for physicians with mental and behavioral health problems. J Psychiatr Pract 2007;13(1):25-32. [DOI] [PubMed] [Google Scholar]
- 20.Kraft D. Successful treatment of heavy smoker in one hour using split screen imagery, aversion, and suggestions to eliminate cravings. Contemp Hypn Integr Ther 2012;29(2):175-88. [Google Scholar]
- 21.Lash SJ, Stephens RS, Burden JL, Grambow SC, DeMarce JM, Jones ME, et al. Contracting, prompting, and reinforcing substance use disorder continuing care: a randomized clinical trial. Psychol Addict Behav 2007;21(3):387-97. [DOI] [PubMed] [Google Scholar]
- 22.Lash SJ. Increasing participation in substance abuse aftercare treatment. Am J Drug Alcohol Abuse 1998;24(1):31-6. [DOI] [PubMed] [Google Scholar]
- 23.Lash SJ, Burden JL, Parker JD, Stephens RS, Budney AJ, Horner RD, et al. Contracting, prompting and reinforcing substance use disorder continuing care. J Subst Abuse Treat 2013;44(4):449-56. Epub 2012 Oct 31. [DOI] [PubMed] [Google Scholar]
- 24.Magneberg R. The effect of electronic surveillance on alcohol misuse and everyday behavior. Addict Behav 1998;23(3):281-301. [DOI] [PubMed] [Google Scholar]
- 25.Masson S, Marrow B, Kendrick S, Elsharkawy AM, Latimer S, Hudson M.. An ‘alcohol contract’ has no significant effect on return to drinking after liver transplantation for alcoholic liver disease. Transpl Int 2014;27(5):475-81. Epub 2014 Mar 15. [DOI] [PubMed] [Google Scholar]
- 26.O’Farrell TJ, Choquette KA, Cutter HS.. Couples relapse prevention sessions after behavioral marital therapy for male alcoholics: outcomes during the three years after starting treatment. J Stud Alcohol 1998;59(4):357-70. [DOI] [PubMed] [Google Scholar]
- 27.Piotrowski NA, Tusel DJ, Sees KL, Reilly PM, Banys P, Meek P, et al. Contingency contracting with monetary reinforcers for abstinence from multiple drugs in a methadone program. Exp Clin Psychopharmacol 1999;7(4):399-411. [DOI] [PubMed] [Google Scholar]
- 28.Resnicow K, Royce J, Vaughan R, Orlandi MA, Smith M.. Analysis of a multicomponent smoking cessation project: what worked and why. Prev Med 1997;26(3):373-81. [DOI] [PubMed] [Google Scholar]
- 29.Stanger C, Budney AJ, Kamon JL, Thostensen J.. A randomized trial of contingency management for adolescent marijuana abuse and dependence. Drug Alcohol Depend 2009;105(3):240-7. Epub 2009 Aug 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vinson DC, Devera-Sales A.. Computer-generated written behavioral contracts with problem drinkers in primary medical care. Subst Abus 2000;21(4):215-22. [DOI] [PubMed] [Google Scholar]
- 31.White JS, Dow WH, Rungruanghiranya S.. Commitment contracts and team incentives: a randomized controlled trial for smoking cessation in Thailand. Am J Prev Med 2013;45(5):533-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Young RM, Connor JP, Feeney GF.. Alcohol expectancy changes over a 12-week cognitive-behavioral therapy program are predictive of treatment success. J Subst Abuse Treat 2011;40(1):18-25. Epub 2010 Sep 22. [DOI] [PubMed] [Google Scholar]
- 33.Born C, de la Fontaine L, Winter B, Müller N, Schaub A, Früstück C, et al. First results of a refeeding program in a psychiatric intensive care unit for patients with extreme anorexia nervosa. BMC Psychiatry 2015;15:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bryan CJ, Mintz J, Clemans TA, Leeson B, Burch TS, Williams SR, et al. Effect of crisis response planning vs. contracts for safety on suicide risk in U.S. Army soldiers: a randomized clinical trial. J Affect Disord 2017;212:64-72. Epub 2017 Jan 23. [DOI] [PubMed] [Google Scholar]
- 35.Callan JA, Howland RH.. Borderline personality disorder: inpatient psychiatric nursing management. J Psychosoc Nurs Ment Health Serv 2009;47(5):13-4. [DOI] [PubMed] [Google Scholar]
- 36.Foelsch PA, Kernberg OF.. Transference-focused psychotherapy for borderline personality disorders. In Session-Psychoth 1998;4(2):67-90. [Google Scholar]
- 37.Hartmann A, Wirth C, Zeeck A.. Prediction of failure of inpatient treatment of anorexia nervosa from early weight gain. Psychother Res 2007;17(2):218-29. [Google Scholar]
- 38.IJff MA, Huijbregts KML, van Marwijk HWJ, Beekman ATF, Hakkaart-van Roijen L, Rutten FF, et al. Cost-effectiveness of collaborative care including PST and an antidepressant treatment algorithm for the treatment of major depressive disorder in primary care; a randomised clinical trial. BMC Health Serv Res 2007;7:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kanahara S. The outcome of behavioral intervention with a person living with schizophrenia who exhibited medication noncompliance: a case study. Int J Behav Consult Ther 2009;5(3-4):252-63. [Google Scholar]
- 40.Strik Lievers L, Curt F, Wallier J, Perdereau F, Rein Z, Jeammet P, et al. Predictive factors of length of inpatient treatment in anorexia nervosa. Eur Child Adolesc Psychiatry 2009;18(2):75-84. Epub 2008 Sep 22. [DOI] [PubMed] [Google Scholar]
- 41.Martinez-Taboas A, Rodriguez-Cay JR.. Case study of a Puerto Rican woman with dissociative identity disorder. Dissociation 1997;10(3):141-7. [Google Scholar]
- 42.Mishara BL, Daigle MS.. Effects of different telephone intervention styles with suicidal callers at two suicide prevention centers: an empirical investigation. Am J Community Psychol 1997;25(6):861-85. [DOI] [PubMed] [Google Scholar]
- 43.Moljord IEO, Lara-Cabrera ML, Salvesen, ØRise MB, Bjørgen D, Antonsen DØ, et al. Twelve months effect of self-referral to inpatient treatment on patient activation, recovery, symptoms and functioning: a randomized controlled study. Patient Educ Couns 2017;100(6):1144-52. Epub 2017 Jan 11. [DOI] [PubMed] [Google Scholar]
- 44.Sibley MH, Graziano PA, Kuriyan AB, Coxe S, Pelham WE, Rodriguez L, et al. Parent-teen behavior therapy + motivational interviewing for adolescents with ADHD. J Consult Clin Psychol 2016;84(8):699-712. Epub 2016 Apr 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Van der Voort TY, van Meijel B, Goossens PJ, Hoogendoorn AW, Draisma S, Beekman A, et al. Collaborative care for patients with bipolar disorder: randomised controlled trial. Br J Psychiatry 2015;206(5):393-400. Epub 2015 Mar 19. [DOI] [PubMed] [Google Scholar]
- 46.Gerber JB, Bloom PA, Ross JS.. The physical activity contract—tailored to promote physical activity in a geriatric outpatient setting: a pilot study. J Am Geriatr Soc 2010;58(3):604-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cloutier MM, Wiley J, Huedo-Medina T, Ohannessian CM, Grant A, Hernandez D, et al. Outcomes from a pediatric primary care weight management program: steps to growing up healthy. J Pediatr 2015;167(2):372-7.e1. Epub 2015 Jun 12. [DOI] [PubMed] [Google Scholar]
- 48.Haber D, Rhodes D.. Health contract with sedentary older adults. Gerontologist 2004;44(6):827-35. [DOI] [PubMed] [Google Scholar]
- 49.Heneman K, Block-Joy A, Zidenberg-Cherr S, Donohue S, Garcia L, Martin A, et al. A “contract for change” increases produce consumption in low-income women: a pilot study. J Am Diet Assoc 2005;105(11):1793-6. [DOI] [PubMed] [Google Scholar]
- 50.John LK, Loewenstein G, Troxel AB, Norton L, Fassbender JE, Volpp KG.. Financial incentives for extended weight loss: a randomized, controlled trial. J Gen Intern Med 2011;26(6):621-6. Epub 2011 Jan 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lemstra M, Rogers MR.. The importance of community consultation and social support in adhering to an obesity reduction program: results from the Healthy Weights Initiative. Patient Prefer Adherence 2015;9:1473-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Washington WD, McMullen D, Devoto A.. A matched deposit contract intervention to increase physical activity in underactive and sedentary adults. Transl Issues Psychol Sci 2016;2(2):101-15. [Google Scholar]
- 53.Burkhart PV, Rayens MK, Oakley MG, Abshire DA, Zhang M.. Testing an intervention to promote children’s adherence to asthma self-management. J Nurs Scholarsh 2007;39(2):133-40. [DOI] [PubMed] [Google Scholar]
- 54.Charlson ME, Wells MT, Peterson JC, Boutin-Foster C, Ogedegbe GO, Mancuso CA, et al. Mediators and moderators of behavior change in patients with chronic cardiopulmonary disease: the impact of positive affect and self-affirmation. Transl Behav Med 2014;4(1):7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cruz J, Brooks D, Marques A.. Walk2Bactive: a randomised controlled trial of a physical activity-focused behavioural intervention beyond pulmonary rehabilitation in chronic obstructive pulmonary disease. Chron Respir Dis 2016;13(1):57-66. Epub 2015 Dec 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hillman HL, Miller LK.. The effects of a spouse implemented contingency contract on asthma medication adherence. Behav Anal Today 2009;10(1):1-6. [Google Scholar]
- 57.Kegler MC, Haardörfer R, Alcantara IC, Gazmararian JA, Veluswamy JK, Hodge TL, et al. Impact of improving home environments on energy intake and physical activity: a randomized controlled trial. Am J Public Health 2016;106(1):143-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kirschenbaum DS, Germann JN, Rich BH.. Treatment of morbid obesity in low-income adolescents: effects of parental self-monitoring. Obes Res 2005;13(9):1527-9. [DOI] [PubMed] [Google Scholar]
- 59.Mancuso CA, Choi TN, Westermann H, Wenderoth S, Hollenberg JP, Wells MT, et al. Increasing physical activity in patients with asthma through positive affect and self-affirmation: a randomized trial. Arch Intern Med 2012;172(4):337-43. Epub 2012 Jan 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mancuso CA, Sayles W, Allegrante JP.. Randomized trial of self-management education in asthmatic patients and effects of depressive symptoms. Ann Allergy Asthma Immunol 2010;105(1):12-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sherman JM, Baumstein S, Hendeles L.. Intervention strategies for children poorly adherent with asthma medications; one center’s experience. Clin Pediatr (Phila) 2001;40(5):253-8. [DOI] [PubMed] [Google Scholar]
- 62.Labhardt ND, Balo JR, Ndam M, Manga E, Stoll B.. Improved retention rates with low-cost interventions in hypertension and diabetes management in a rural African environment of nurse-led care: a cluster-randomised trial. Trop Med Int Health 2011;16(10):1276-84. [DOI] [PubMed] [Google Scholar]
- 63.Ogedegbe GO, Boutin-Foster C, Wells MT, Allegrante JP, Isen AM, Jobe JB, et al. A randomized controlled trial of positive-affect intervention and medication adherence in hypertensive African Americans. Arch Intern Med 2012;172(4):322-6. Epub 2012 Jan 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ostfeld RJ, Cheung YW, Saal I, Janis G, Cabeza Y, Du Y, et al. A brief office intervention is associated with improved health measures. Int J Cardiol 2007;119(2):239-41. Epub 2006 Oct 27. [DOI] [PubMed] [Google Scholar]
- 65.Peterson JC, Charlson ME, Hoffman Z, Wells MT, Wong SC, Hollenberg JP, et al. A randomized controlled trial of positive-affect induction to promote physical activity after percutaneous coronary intervention. Arch Intern Med 2012;172(4):329-36. Epub 2012 Jan 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chassany O, Boureau F, Liard F, Bertin P, Serrie A, Ferran P, et al. Effects of training on general practitioners’ management of pain in osteoarthritis: a randomized multicenter study. J Rheumatol 2006;33(9):1827-34. Epub 2006 May 15. [PubMed] [Google Scholar]
- 67.Desai PM, Hughes SL, Peters KE, Mermelstein RJ.. Impact of telephone reinforcement and negotiated contracts on behavioral predictors of exercise maintenance in older adults with osteoarthritis. Am J Health Behav 2014;38(3):465-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hughes SL, Seymour RB, Campbell RT, Desai P, Huber G, Chang HJ.. Fit and strong!: bolstering maintenance of physical activity among older adults with lower-extremity osteoarthritis. Am J Health Behav 2010;34(6):750-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lundervold DA, Talley C, Buermann M.. Effect of behavioral activation treatment on chronic fibromyalgia pain: replication and extension. Int J Behav Consultation Ther 2008;4(2):146-57. [Google Scholar]
- 70.Brown LB, Miller WC, Kamanga G, Nyirenda N, Mmodzi P, Pettifor A, et al. HIV partner notification is effective and feasible in sub-Saharan Africa: opportunities for HIV treatment and prevention. J Acquir Immune Defic Syndr 2011;56(5):437-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hovell MF, Sipan CL, Blumberg EJ, Hofstetter CR, Slymen D, Friedman L, et al. Increasing Latino adolescents’ adherence to treatment for latent tuberculosis infection: a controlled trial. Am J Public Health 2003;93(11):1871-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kominski GF, Varon SF, Morisky DE, Malotte CK, Ebin VJ, Coly A, et al. Costs and cost-effectiveness of adolescent compliance with treatment for latent tuberculosis infection: results from a randomized trial. J Adolesc Health 2007;40(1):61-8. Epub 2006 Oct 27. [DOI] [PubMed] [Google Scholar]
- 73.Binkley CJ, Johnson KW, Abadi M, Thompson K, Shamblen SR, Young L, et al. Improving the oral health of residents with intellectual and developmental disabilities: an oral health strategy and pilot study. Eval Program Plann 2014;47:54-63. Epub 2014 Jul 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Browne A, Dickson B, van der Wal R.. The ethical management of the noncompliant patient. Camb Q Healthc Ethics 2003;12(3):289-99. [DOI] [PubMed] [Google Scholar]
- 75.Gonda-Kotani C, White GW.. The effects of contingency contracts and performance feedback on completing data entries to self-monitor community participation of people with physical disabilities: an ecological momentary study. J Prev Interv Community 2017;45(2):86-99. [DOI] [PubMed] [Google Scholar]
- 76.Shaw SE, Morris DM, Uswatte G, McKay S, Meythaler JM, Taub E.. Constraint-induced movement therapy for recovery of upper-limb function following traumatic brain injury. J Rehabil Res Dev 2005;42(6):769-78. [DOI] [PubMed] [Google Scholar]
- 77.Chelminski PR, Ives TJ, Felix KM, Prakken SD, Miller TM, Perhac JS, et al. A primary care, multi-disciplinary disease management program for opioid-treated patients with chronic non-cancer pain and a high burden of psychiatric comorbidity. BMC Health Serv Res 2005;5(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hariharan J, Lamb GC, Neuner JM.. Long-term opioid contract use for chronic pain management in primary care practice. A five year experience. J Gen Intern Med 2007;22(4):485-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Cho MK. Effect of health contract intervention on renal dialysis patients in Korea. Nurs Health Sci 2013;15(1):86-93. Epub 2012 Oct 29. [DOI] [PubMed] [Google Scholar]
- 80.Sagawa M, Oka M, Chaboyer W.. The utility of cognitive behavioural therapy on chronic haemodialysis patients’ fluid intake: a preliminary examination. Int J Nurs Stud 2003;40(4):367-73. [DOI] [PubMed] [Google Scholar]
- 81.Schlenk EA, Boehm S.. Behaviors in type II diabetes during contingency contracting. Appl Nurs Res 1998;11(2):77-83. [DOI] [PubMed] [Google Scholar]
- 82.Claydon BE, Efron N, Woods C.. A prospective study of the effect of education on non-compliant behaviour in contact lens wear. Ophthalmic Physiol Opt 1997;17(2):137-46. [PubMed] [Google Scholar]
- 83.Deci EL, Ryan RM.. Intrinsic motivation and self-determination in human behavior. Boston, MA: Springer; 1985. [Google Scholar]
- 84.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process 1991;50(2):179-211. [Google Scholar]
- 85.Prochaska JO, DiClemente CC.. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol 1983;51(3):390-5. [DOI] [PubMed] [Google Scholar]
- 86.Bandura A. Self-efficacy: the exercise of control. New York, NY: Worth Publishers; 1997. [Google Scholar]
- 87.Starfield B, Gérvas J, Mangin D.. Clinical care and health disparities. Annu Rev Public Health 2012;33:89-106. Epub 2012 Jan 3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


