Abstract
The ongoing pandemic has dramatically disrupted daily life, increasing the risk of developing psychiatric disorders and poor mental wellbeing. The compound effects of social, political and psychological stressors have increased psychological symptoms among adolescents and young people, with worries about COVID-19 playing a central role in the clinical course of their mental health problems caused by the pandemic. The aim of this cross-cultural study was to examine the social psychological effects of COVID-19 on adolescents’ and young people’s mental health and wellbeing in Ibero-American population. Participants involved 6,283 adolescents and young adults from five different Spanish-Speaking countries (83.7% female) aged between 12 and 30 years (M = 18.79; SD = 3.48). Participants completed the Worries about COVID-19 and its Consequences Scale (W-COV), the Satisfaction with Life Scale (SWLS), and the Depression, Anxiety and Stress Scale (DASS-21). Descriptive analyses, multivariate ANOVAs and Pearson correlations were performed, as well as Structural Equation Modelling (SEM) testing a mediational model. The results indicate cross-cultural difference in COVID-19 related worries, emotional symptoms and life satisfaction. Results from SEM confirmed the overall indirect effects of COVID-19 cases, political response and participants’ conditions during lockdown on depression, anxiety, stress and life satisfaction mediated by COVID-19 related worries. These findings suggest that the social psychological factors underlying psychological symptoms could be partly explained by increased worries about COVID-19 and its personal, social, economic and political consequences, which may offer guidance to policy makers and health services for safeguarding youth mental well-being.
Keywords: Trans-cultural, youth, life satisfaction, emotional symptoms, Ibero-American population, structural equation modelling
Introduction
The COVID-19 pandemic has become the hardest, most impactful health crisis of the modern era (Lin, 2020). Since the very beginning, the compound effect of cases, deceases and overload of the health services has threatened to shatter the system’s economic, political and social resources (Codagnone et al., 2020). This situation is true for many nations around the world, and more specifically, to the Spanish-speaking areas (Graetz et al., 2021).
Although Spanish-speaking nations share some aspects in their socio-cultural backgrounds, they entered the COVID-19 pandemic with very different health and political circumstances (Atun et al., 2015). In Chile, for instance, a military dictatorship was established from 1973 to 1990, which heavily impacted the public health system, while countries such as Mexico, Colombia and Ecuador had earlier democratic agency to provide public resources to their population. Similarly, Spain is one of the leading countries in the Organisation for Economic Co-operation and Development (OECD) regarding its universal health system, in terms of public investment, equity and user satisfaction, including the lower rates of child and cancer-related mortality (Rico et al., 2007).
Despite these different starting points, all the above mentioned countries are assisting to a severely difficult situation related to the continuous coronavirus outbreaks (Caqueo-Urízar et al., 2020; García-Fernández et al., 2021). Nonetheless, there have been notable differences among these countries in the number of cases and deaths associated with the pandemic. In the first week of May, when the data for this study started to be collected, 5,877 new cases of COVID-19 and 1,233 deaths were registered in Spain; in Mexico, the count was on 10,783 cases and 1,188 deaths; in Colombia, 3,045 cases and 114 deaths; in Ecuador, 1,354 cases and 333 deaths; and in Chile, 8,784 cases and 57 deaths (The World Bank, 2019). The outline of the spread and contagion has been different for each country, as well as the various restriction policies they have implemented according to their specific situation (World Health Organization, 2020). Every country’s political response has been developed according to their economic, sociopolitical and demographic characteristics, as well as their sanitary infrastructures—these factors combined have shaped the stringency level of the restriction measures during lockdown, as well as their mobility and security protocols (Kavanagh & Singh, 2020).
In addition to these social and political circumstances, scientific literature highlights the severe psychological implications of this pandemic, because its sudden and pervasive nature has had a major impact in the individual mental stability, and these effects have been registered worldwide (Satici et al., 2020). Adolescents and young adults have been among the most vulnerable groups regarding their mental health during the ongoing global crisis (Liang et al., 2020; Marques de Miranda et al., 2020). Closure of schools and universities, academic and work-related uncertainty, and digital divide regarding the socio-economic status of their families have become severe stressors targeting youth around the world (Gilead & Dishon, 2021). Furthermore, adolescence and young adulthood is a critical period for establishing attachment bonds and seeking validation between peers, which has been affected by social distancing and home isolation (Okabe-Miyamoto et al., 2021).
Emotional symptoms have been significantly prevalent during this pandemic—the youth-specific stressors, combined with the fear of the disease and the lingering feeling of uncertainty have all taken its toll on mental and emotional health (Lima et al., 2020; Purtle, 2020). One of the most frequently observed psychological conditions have been depression symptoms, that have either worsened in those who already had mental health problems or have emerged as a consequence of the sudden worldwide crisis (Campos et al., 2021; Valero-Moreno et al., 2021). Anxiety levels have also become one of the main indicators of poorer mental health during lockdown (Tamarit et al., 2020), together with stress symptoms, that have been observed to increase exponentially in the general population (Vinkers et al., 2020). The rising prevalence in emotional symptoms has been associated with a decrease in subjective well-being (Trzebiński et al., 2020).
Subjective well-being can be defined as the individual’s assessment of their own lives [15, 16], and this evaluation includes the person’s perception of their own life satisfaction and their mood, whether it comprises positive or negative emotions (León-Pinilla et al., 2015). Since life satisfaction during the pandemic has been considerably impacted by the wide range of hardships the population has endured, it has become one of the most reliable indicators of mental stability and welfare (Mónaco et al., 2019)–also considered the most stable indicator of subjective well-being, thus more frequently used than positive and negative affect (Ausín et al., 2021). One of the main threats to subjective well-being during the COVID-19 era are the fears specific to the pandemic (Prime et al., 2020).
COVID-19-related worries have also been observed to severely influence mental health (Horesh et al., 2020). Among the most common are health worries, concerning the welfare of one’s own physical and mental health during the pandemic, or those of their loved ones (Puci et al., 2020). Economic worries are also relevant—this health crisis has not only entailed individual financial problems, but it has also put at risk the entire global economic system, making this one of the biggest concerns in the population (Prime et al., 2020).
Together with COVID-19-related worries, other pandemic-specific risk factors have been observed to affect youth’s mental health, such as the individual life circumstances that influenced coping with quarantine and restrictions (Losada-Baltar et al., 2020). Personal variables, such as having been infected with the virus, social isolation (Sandín et al., 2020) and coronavirus-related internet searches (Igartua et al., 2020) have been associated with an increase in COVID-19-related fears and worries. Frequency of leaving the house to go to work during lockdown (Aloi et al., 2020), obligation to work outside the home (Filgueiras & Stults-Kolehmainen, 2021), COVID-19-related information search (Igartua et al., 2020), household size and cohabitation (Okabe-Miyamoto et al., 2021), whether one has been infected with COVID-19 or a loved one has, all have been identified as significant factors that may influence mental health at any age (Moya-Lacasa et al., 2021). Evidentially, age has been found to be a relevant factor moderating the relationship between concern about COVID-19 and mental health (Barber & Kim, 2020; Wilson et al., 2020). According to the literature, older people are more capable of reorienting their emotions and cope with the stress caused by the virus, while children and adolescents seem to be especially vulnerable to the development of emotional distress during the COVID-19 pandemic (Marques de Miranda et al., 2020; Ravens-Sieberer et al., 2021).
Although research on the social psychological impact of COVID-19 pandemic has developed strongly in a short time, there are significant gaps in this area. Most of the research has been conducted in general adult population above 18 years old (Rossi et al., 2020; Sandín et al., 2020; Şimşir et al., 2021). Several studies were developed with older adults (Bergman et al., 2020; García-Portilla et al., 2020; Mistry et al., 2021), healthcare workers (Barzilay et al., 2020; Chen et al., 2021; Lima et al., 2020; Yıldırım et al., 2020) and other vulnerable population (Fish et al., 2020; Gonzales et al., 2020). Furthermore, few studies have investigated the risk and protective factors for adolescents and young people’s mental health and well-being during the pandemic (Magson et al., 2021; Tamarit et al., 2020), but none of them included a cross-cultural perspective. Indeed, there are no empirical studies that provide information about adolescents and young people’s mental health and well-being during COVID-19 pandemic of the Ibero-American population. Research in this area has been conducted in North American population (Fish et al., 2020; Gonzales et al., 2020; Rogers et al., 2021), European population (Gómez-Becerra et al., 2020; McElroy et al., 2020; Mensi et al., 2021; Ravens-Sieberer et al., 2021), Australian population (Fisher et al., 2020) and Asian population (Duan et al., 2020; Isumi et al., 2020; Tang et al., 2021).
The Present Study
The aim of this cross-cultural study was to examine the social psychological impact of COVID-19 on adolescents’ and young people’s emotional distress (COVID-19 related worries and emotional symptoms) and subjective well-being (life satisfaction):
(a) to test for cross-cultural difference in COVID-19 related worries, emotional symptoms and life satisfaction.
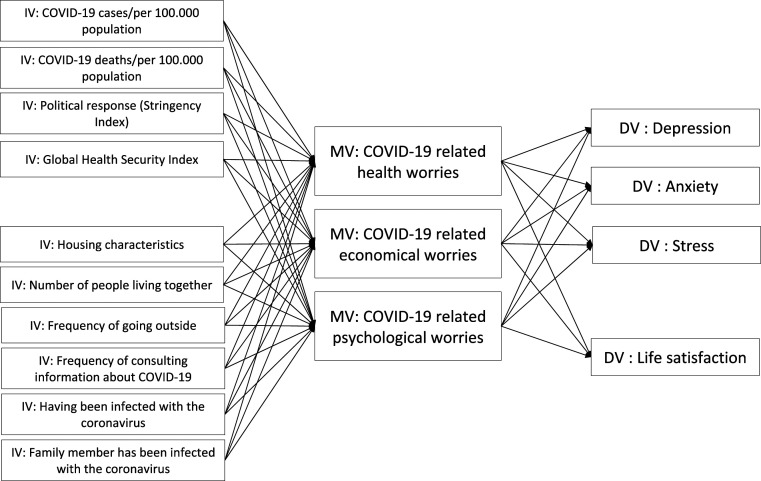
(b) to test the accuracy of a mediational model in which COVID-19 related worries (health, economic and psychosocial) mediate the association of personal and country-specific impact of the COVID-19 (conditions during lockdown, COVID-10 deaths and cases, political response) with emotional symptoms (depression, anxiety, stress) and life satisfaction (Figure 1).
Figure 1.
Graphic depiction of the mediational model tested in this study. Note. IV: independent variable; MV: mediator variable; DV: dependent variable.
Methods
Participants and Procedure
Participants were 6,283 adolescents and young adults from five different Spanish-Speaking countries, 5,260 of them were women (83.70%), 955 were men (15.20%), 34 identified as non-binary (0.54%), 8 as genderfluid (0.13%) and 15 did not state their gender (0.24%). The participants’ ages ranged from 12 to 30 years (M = 18.79; SD = 3.48). The participants spent their lockdown in Spain (n = 347, 5.50%), Colombia (n = 636, 10.10%), Mexico (n = 342, 5.40%), Ecuador (n = 1158, 8.40%) and Chile (n = 3800, 60.50%).
The inclusion criteria were (1) having spent the lockdown in one of the studied countries, (2) being aged between 12 and 30 years and (3) scoring a minimum of 75% on the Oviedo Infrequency Scale (INF-OV) (Fonseca-Pedrero et al., 2010), a scale that detects randomly answered responses.
The data was collected according to the Helsinki Declaration guidelines (World Medical Association, 2013) and was approved by the corresponding ethics committee. The instruments were applied via Limesurvey, a secure online survey platform, that was spread through official (educational centres and institutions) and unofficial (social media, websites) digital media using a snowball sampling method. The data were collected from May to June 2020, during the first COVID-19 outbreak while lockdown was mandatory in the studied countries. All the participants were informed of the purposes of the study and agreed to participate voluntarily. All data collected are anonymous and confidential.
Instruments
Socio-Demographic Measures
The COVID-19 impact and political response data in the studied countries were collected manually through Our World in Data (Lab, 2021) and the World Health Organization online Database (World Health Organization, 2021). An ad hoc questionnaire was used to assess the personal variables: Number of people living together, household characteristics, frequency of outings, frequency of searching for COVID-19 related information, and whether the participant or a loved one had become ill with COVID-19.
COVID-19 Related Worries
COVID-19 related worries were assessed through the COVID-19 related worries scale (COVID-19-RWS) (Mónaco et al., 2021). This questionnaire was designed to assess the participant’s concerns about the individual, social, economic and political impact of the pandemic. The participants are asked to follow the premise “During confinement, I was worried about….” This 16-item scale is divided into three dimensions: worries about health (e.g., “Becoming ill or dying because of COVID-19”), economic worries (e.g., “My economic situation, or my family’s, getting worse”) and psychosocial worries (e.g., “My psychological state”). The items are scored on a 5-point Likert scale, ranging from 1 (almost never) to 5 (almost always). In this study, the reliability indices were satisfactory for health worries (Cronbach’s α =.69), economic worries (Cronbach’s α =.74) and psychosocial worries (Cronbach’s α =.74).
Symptoms of Depression, Anxiety and Stress
The Spanish version of the Depression, Anxiety, and Stress Scales (DASS-21) assessed emotional symptomatology (Daza et al., 2002). The 21-item scale is formed by three subscales (Lovibond & Lovibond, 1995): depression symptoms (e.g., “I felt down-hearted and blue”), anxiety symptoms (e.g., “I felt scared without any good reason”) and stress symptoms (e.g., “I was aware of dryness of my mouth”). The items are scored on a 3-point Likert scale ranging from 0 (Did not apply to me at all) to 3 (Applied to me very much, or most of the time). The three subscales showed adequate reliability indices (α =.84 for depression; α =.70 for anxiety; and α =.82 for stress).
Life Satisfaction
Life satisfaction was assessed through the Spanish version of the Satisfaction With Life Scale (SWLS) (Vázquez et al., 2013). It is a 5-item, one-dimensional scale (Diener, 1984) that measures the participants' assessment of their own lives, and the items are ranked on a 7-point Likert scale scoring from 1 (Totally disagree) to 7 (Totally agree) (e.g., “If I could live my life all over again, I wouldn’t change a thing”). Reliability indices for this scale were adequate in this study (Cronbach’s α = 88).
Data Analysis
Descriptive analyses were conducted to indicate lockdown conditions, COVID-19 impact and political response for each country. Chi-square tests and one-way ANOVAs were carried out to test cross-cultural differences in the participant’s socio-demographic characteristics. Multivariate ANOVAs were then conducted to assess cross-cultural differences in COVID-19 related worries, emotional symptoms and life satisfaction, taking into account potential effects for gender and age. Furthermore, we used the statistical program Mplus (V.16) to conduct Structural Equation Modelling (SEM), in order to test the accuracy of the mediational model displayed in Figure 1. The model tested was a total mediation, and the goodness-of-fit was analysed through chi-square index (X2/df), the Comparative Fit Index (CFI), the Tucker-Lewis Index (TLI), the Root Mean Square Error of Approximation (RMSEA), and the Standardized Root Mean Square Residual (SRMR). Direct and indirect effects are reported together with the goodness-of-fit indicators. Finally, we tested whether paths in the mediation model were significantly different among gender and age using the Wald test (Wald chi-squared test).
Results
Descriptive Statistics
Descriptive statistics for participants’ conditions during lockdown and COVID-19 impact and response for each country are displayed in Table 1. Results from χ2 tests of cross-cultural differences were significant for all variables of nominal scale (p < .01). In addition, the analyses of variance (one-way ANOVA) of cross-cultural differences were significant for all variables of interval scale (p < .01).
Table 1.
Participants’ Conditions During Lockdown and COVID-19 Impact for Each Country.
| Spain (n = 347) | Colombia (n = 636) | Mexico (n = 342) | Ecuador (n = 1,158) | Chile (n = 3,800) | |
|---|---|---|---|---|---|
| COVID-19 Lockdown conditions | n (%) | n (%) | n (%) | n (%) | n (%) |
| Number of people living together [M (SD)] | 3.82 (0.93) | 4.08 (1.71) | 4.42 (2.82) | 5.05 (1.12) | 4.26 (1.96) |
| Household characteristics | |||||
| Flat or apartment without outside zones (balcony, courtyard, etc.) | 75 (21.61) | 171 (26.89) | 20 (5.85) | 89 (7.69) | 217 (5.71) |
| Flat or apartment with outside zones (balcony, courtyard, etc.) | 175 (50.43) | 177 (27.83) | 4 (1.17) | 139 (12.00) | 428 (11.26) |
| House with outside zones (e.g., garden) | 73 (21.04) | 234 (36.79) | 289 (84.50) | 689 (59.50) | 2,777 (73.08) |
| House with large outside zones (e.g., a chalet in a mountain area) | 23 (6.63) | 45 (7.08) | 9 (2.63) | 206 (17.79) | 284 (7.47) |
| Other | 1 (0.29) | 9 (1.42) | 20 (5.85) | 35 (3.02) | 94 (2.47) |
| Frequency of outings (for shopping, doing exercise, meeting friends, etc.) | |||||
| I have not going out since the beginning of the lockdown | 13 (3.75) | 82 (12.89) | 72 (21.05) | 208 (17.96) | 11194 (31.42) |
| Less than 1 time per week | 31 (8.93) | 238 (37.42) | 108 (31.58) | 290 (25.04) | 1,455 (38.29) |
| Once a week | 46 (13.26) | 137 (21.54) | 70 (20.47) | 263 (22.71) | 599 (15.76) |
| Two or three times a week | 131 (37.75) | 119 (18.71) | 63 (18.42) | 294 (25.39) | 406 (10.68) |
| Almost every day | 126 (36.31) | 60 (9.43) | 29 (8.48) | 103 (8.89) | 146 (3.84) |
| Frequency of searching for COVID-19 related information per day | |||||
| Less than 30 min | 284 (81.84) | 541 (85.06) | 282 (82.46) | 938 (81.00) | 3,062 (80.58) |
| Between 30 min and 1 hr | 46 (13.26) | 73 (11.48) | 43 (12.57) | 179 (15.46) | 517 (13.61) |
| Between 1 and 2 hr | 7 (2.02) | 15 (2.36) | 15 (4.39) | 28 (2.42) | 131 (3.45) |
| More than 2 hr | 10 (2.88) | 7 (1.10) | 2 (0.58) | 13 (1.12) | 90 (2.37) |
| Has someone from your family had symptoms of COVID-19 or tested positive? | |||||
| No | 245 (79.61) | 497 (78.14) | 249 (72.81) | 591 (51.04) | 2,800 (73.68) |
| Has had symptoms but has not been tested | 20 (5.76) | 26 (4.09) | 30 (8.77) | 76 (6.56) | 293 (7.71) |
| Yes, has been tested positive | 51 (14.70) | 88 (13.84) | 53 (15.50) | 417 (36.01) | 533 (14.03) |
| I do not know | 31 (8.93) | 25 (3.93) | 10 (2.92) | 74 (6.39) | 174 (4.58) |
| Have you had symptoms of COVID-19 or tested positive? | |||||
| No | 288 (83.00) | 595 (93.55) | 316 (92.40) | 959 (82.82) | 3,498 (92.05) |
| I had symptoms but have not been tested | 14 (4.03) | 9 (1.42) | 4 (1.17) | 60 (5.18) | 122 (3.21) |
| Yes, I have been tested positive | 2 (0.58) | 4 (0.63) | 2 (0.58) | 41 (3.54) | 25 (0.66) |
| I do not know | 43 (12.39) | 28 (4.40) | 20 (5.85) | 98 (8.46) | 155 (4.08) |
| COVID-19 impact and response | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) |
| COVID-19 cases/per 100,000 population | 5.41 (0.77) | 60.95 (43.65) | 22.20 (4.11) | 28.60 (11.50) | 151.84 (28.59) |
| COVID-19 deaths/per 100,000 population | 0.53 (0.12) | 2.08 (1.41) | 2.91 (0.49) | 2.19 (4.41) | 1.86 (0.81) |
| Political response (stringency index) | 62.70 (5.00) | 86.82 (1.96) | 72.10 (2.18) | 68.64 (13.47) | 78.55 (1.53) |
Cross-Cultural Differences in COVID-19 Related Worries, Emotional Symptoms and Life Satisfaction
Results from multivariate ANOVAs (Table 2) indicated statistically significant cross-cultural differences in COVID-19 related worries (Wilks’s Lambda, L = 0.92, F(3,16599) = 6.78, p < .001, η2 = .03). Specifically, Tukey’s HSD tests showed that Spanish participants showed significantly lower levels of COVID-19 related health worries than participants form Ecuador (p < .001, CI 95% [−0.45, −0.18]), Mexico (p < .001, CI 95% [−0.48, −0.14]) and Chile (p < .001, CI 95% [−0.61, −0.36]). The Spanish participants also reported significantly lower levels of COVID-19 related economic worries in comparison to participants from the other four countries (Colombia p < .001, CI 95% [−0.74, −0.41]; Mexico p < .001, CI 95% [−0.75, −0.37]; Ecuador p < .001, CI 95% [−0.75, −0.45]; Chile p < .001, CI 95% [−0.86, −0.59]). Finally, Spanish participants presented lower levels of COVID-19 related socio-psychological worries compared to the other participants (Colombia p < .001, CI 95% [−0.44, −0.12]; Mexico p < .05, CI 95% [−0.38, −0.01]; Ecuador p < .001, CI 95% [−0.51, −0.21]; Chile p < .001, CI 95% [−0.85, −0.58]). In addition to cross-cultural differences, significant effects in COVID-19 related worries for gender (Wilks’s Lambda, L = 0.98, F(3,6274) = 40.34, p < .001, η2 = .02) and age (Wilks’s Lambda, L = 0.98, F(3,6274) = 47.04, p < .001, η2 = .22) were observed (Table 2). Women showed higher levels of COVID-19 related worries than men (health worries p < .001, CI 95% [−0.31, −0.21]; economic worries p < .05, CI 95% [−0.24, −0.13]; socio-psychological worries p < .001, CI 95% [−0.35, −0.24]), and adolescents were less worried about the pandemic and its consequences compared to young adults (health worries p < .001, CI 95% [0.02, 0.04]; economic worries p < .05, CI 95% [0.01, 0.03]; socio-psychological worries p < .001, CI 95% [−0.02, −0.01]).
Table 2.
Mean, SDs, Analysis of Variance for Cross-Cultural Differences in COVID-19 Related Worries, Emotional Symptoms and Life Satisfaction.
| Spain (n = 347) | Colombia (n = 636) | Mexico (n = 342) | Ecuador (n = 1,158) | Chile (n = 3,800) | Test of between-subjects effects for country | Test of between-subjects effects for gender | Test of between-subjects effects for age | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | F (gl) | p (η2) | F (gl) | p (η2) | F (gl) | p (η2) | |
| COVID-19 related worries | |||||||||||
| Health worries | 2.83 (.82) | 2.95 (.92) | 3.14 0.91) | 3.15 (.79) | 3.32 (.83) | 36.56 (5) | <.001 (.03) | 102.62 (1) | <.001 (.02) | 81.59 (1) | <.001 (.01) |
| Economic worries | 2.52 (.78) | 3.10 (.89) | 3.08 (.95) | 3.12 (.97) | 3.24 (.89) | 35.19 (5) | <.001 (.03) | 40.66 (1) | <.001 (.01) | 36.02 (1) | <.001 (.02) |
| Psychosocial worries | 2.80 (.88) | 3.08 (.91) | 2.99 (.93) | 3.16 (.93) | 3.34 (.91) | 83.34 (5) | <.001 (.06) | 115.254 (1) | <.001 (.02) | 5.12 (1) | 0.02 (.01) |
| Emotional symptoms | |||||||||||
| Depression | 9.97 (10.03) | 14.42 (11.07) | 12.36 (10.09) | 14.56 (11.74) | 19.17 (11.88) | 91.57 (5) | <.001 (.07) | 23.33 (1) | <.001 (.01) | 82.26 (1) | <.001 (.01) |
| Anxiety | 7.22 (8.64) | 10.56 (9.21) | 9.58 (8.90) | 11.85 (10.15) | 14.00 (10.51) | 48.15 (5) | <.001 (.04) | 67.73 (1) | <.001 (.01) | 35.64 (1) | <.001 (.01) |
| Stress | 12.32 (10.21) | 16.52 (10.17) | 13.95 (9.69) | 16.34 (10.43) | 18.38 (10.62) | 29.88 (5) | <.001 (.02) | 79.83 (1) | <.001 (.01) | 2.90 (1) | .09 (.00) |
| Life satisfaction | 22.97 (6.49) | 24.39 (6.43) | 24.24 (6.82) | 23.35 (6.87) | 21.66 (6.84) | 37.26 (4) | <.001 (.03) | 0.01 (1) | .94 (.00) | 61.02 (1) | <.001 (.01) |
Furthermore, participants showed significant cross-cultural differences in emotional symptoms (Wilks’s Lambda, L = 0.92, F(3,16599) = 45.80, p < .001, η2 = .03). Thus, Tukey’s HSD tests showed that Spanish participants showed significantly lower levels of depression than participants from Colombia (p < .001, CI 95% [−6.54, −2.34]), Ecuador (p < .001, CI 95% [−6.52, −2.67]) and Chile (p < .001, CI 95% [−10.96, −7.43]). The Spanish participants also reported significantly lower levels of anxiety in comparison to participants from the other four countries (Colombia p < .001, CI 95% [−5.18, −1.49]; Mexico p < .05, CI 95% [−4.46, −0.25]; Ecuador p < .001, CI 95% [−6.32, −2.93]; Chile p < .001, CI 95% [−8.33, −5.23]). Finally, Spanish participants presented lower levels of stress compared to the other participants (Colombia p < .001, CI 95% [−6.11, −2.29]; Ecuador p < .001, CI 95% [−5.77, −2.27]; Chile p < .001, CI 95% [−7.67, −4.46]), except those from Mexico. Similarly, significant differences in emotional symptoms were observed for gender (Wilks’s Lambda, L = 0.99, F(3,6274) = 30.80, p < .001, η2 = .02) and age (Wilks’s Lambda, L = 0.98, F(3,6274) = 52.52.01, p < .001, η2 = .02). Women showed higher levels of emotional symptoms than men (depression p < .001, CI 95% [−2.41, −1.01]; anxiety p < .05, CI 95% [−3.19, −1.96]; stress p < .001, CI 95% [−3.53, −2.25]), and adolescents presented higher levels of depression and anxiety symptoms compared to young adults (depression p < .001, CI 95% [−0.50, −0.32]; anxiety p < .05, CI 95% [−0.32, −0.16]; stress p = .07, CI 95% [−0.16, 0.01]).
Cross-cultural differences were also observed in adolescents’ and young people’s life satisfaction (F(4) = 46.59, p < .001, η2 = .03). Tukey’s HSD tests indicated that Chilean participants showed significantly lower levels of life satisfaction in comparison to participants from the other four countries (Spain p < .01, CI 95% [−2.34, −0.26]; Colombia p < .001, CI 95% [−3.52, −1.93]; Mexico p < .05, CI 95% [−3.63, −1.53]; Ecuador p < .001, CI 95% [−2.31, −1.07]). Finally, age showed a significant effect on life satisfaction (F(1) = 61.64, p < .001, η2 = .01), while the effect for gender was non-significant (F(1) = 0.00, p = .99, η2 = .00). Thus, adolescents showed significantly lower levels of life satisfaction in comparison to young adults (p < .01, CI 95% [0.16, 0.26]).
Structural Equation Modelling: Cross-Cultural Mediation Analyses
The potential mediational effect of COVID-19 related worries (health, economic and psychosocial) on the association of personal and country-specific impact of the COVID-19 (conditions during lockdown, COVID-19 deaths and cases and political response) with emotional symptoms and life satisfaction (Figure 1) was tested using SEM. A total mediation model was tested, where goodness-of-fit indices were satisfactory: χ2 (df) = 363.73 (36), CFI = .98; TLI = .96; RMSEA = .04 (CI 95% [0.03, 0.04]), SRMR = .02. However, modification indices suggested a direct effect between COVID-19 cases and depression. Thus, we included the direct effect and ran the mediation model, which showed excellent indices: χ2 (df) = 243.43 (35), CFI = .99; TLI = .98; RMSEA = .03 (CI 95% [0.02, 0.03]), SRMR = .02.
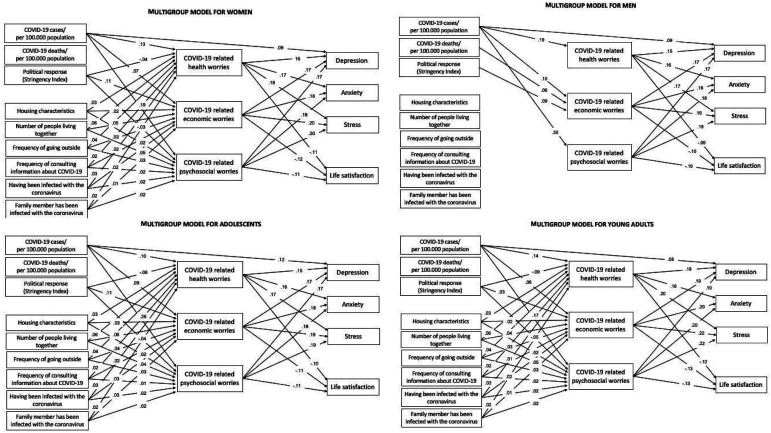
Standardized parameter estimates are presented in Figure 2. Significant direct effects were observed from COVID-19 cases, political response, and participants’ conditions during lockdown on COVID-19 related worries, explaining 4.3% of the variance of health worries, 3.9% of economic worries and 5.8% of psychosocial worries.
Figure 2.
Tested structural equation model: interplay between COVID-19 deaths and cases, political response and conditions during lockdown on depression, anxiety, stress and life satisfaction mediated by COVID-19 related worries. Note. All parameters are standardized and significant. Non-significant effects have not been included to facilitate the interpretation.
Furthermore, COVID-19 related worries had a direct positive effect on depression anxiety and stress, except the effect of health worries on depression was negative. In turn, COVID-19 related worries had a direct negative effect on life satisfaction, except the effect of health worries on life satisfaction was positive. In addition, a direct effect positive effect from COVID-19 cases on depression was included in the mediation model.
The total indirect effects of COVID-19 cases, political response and participants’ conditions during lockdown on depression, anxiety, stress and life satisfaction mediated by COVID-19 related worries are displayed in Table 3. The total mediation was significant, meaning that high levels of COVID-19 related worries mediate between the negative impact of COVID-19 cases, political response and participants’ conditions during lockdown on emotional symptoms and life satisfaction.
Table 3.
Total Indirect Effects of COVID-19 Cases and Deaths, Political Response and Participants’ Conditions During Lockdown on Depression, Anxiety, Stress and Life Satisfaction Mediated by COVID-19 Related Worries.
| DV | M | IV | Total indirect effect | |||
|---|---|---|---|---|---|---|
| c’ | SE | CI 95% | p | |||
| Depression | COVID-19 related worries | COVID-19 cases/100,000 population | .11 | .01 | [.03, .04] | <.001 |
| COVID-19 deaths/100,000 population | ‒.01 | .01 | [‒.14, .02] | .14 | ||
| Political response | ‒.00 | .01 | [‒.02, .02] | .78 | ||
| Number of people living together | .01 | .01 | [‒.05, .12] | .39 | ||
| Household characteristics | .00 | .01 | [‒.15, .23] | .69 | ||
| Frequency of going outside | .02 | .01 | [.07, .34] | .002 | ||
| Frequency of consulting COVID-19 related information | .02 | .01 | [.15, .64] | .001 | ||
| Having been infected with coronavirus | .03 | .01 | [.14, .48] | <.001 | ||
| Family member has been infected with the coronavirus | .02 | .01 | [.03, .45] | .02 | ||
| Anxiety | COVID-19 related worries | COVID-19 cases/100,000 population | .11 | .01 | [.02, .02] | <.001 |
| COVID-19 deaths/100,000 population | ‒.01 | .01 | [‒.12, .02] | .15 | ||
| Political response | ‒.01 | .01 | [‒.03, .01] | .23 | ||
| Number of people living together | .01 | .01 | [‒.04, .10] | .38 | ||
| Household characteristics | .00 | .01 | [‒.12, .20] | .61 | ||
| Frequency of going outside | .02 | .01 | [.07, .28] | .001 | ||
| Frequency of consulting COVID-19 related information | .03 | .01 | [.30, .71] | <.001 | ||
| Having been infected with coronavirus | .03 | .01 | [.15, .41] | <.001 | ||
| Family member has been infected with the coronavirus | .02 | .01 | [.09, .35] | .005 | ||
| Stress | COVID-19 related worries | COVID-19 cases/100,000 population | .13 | .01 | [.02, .02] | <.001 |
| COVID-10 deaths/100.000 population | ‒.01 | .01 | [‒.15, .02] | .12 | ||
| Political response | ‒.01 | .01 | [‒.03, .01] | .19 | ||
| Number of people living together | .01 | .01 | [‒.05, .12] | .44 | ||
| Household characteristics | .00 | .01 | [‒.14, .24] | .62 | ||
| Frequency of going outside | .02 | .01 | [.08, .34] | .001 | ||
| Frequency of consulting COVID-19 related information | .03 | .01 | [.26, .73] | <.001 | ||
| Having been infected with coronavirus | .03 | .01 | [.15, .49] | <.001 | ||
| Family member has been infected with the coronavirus | .02 | .01 | [.07, .47] | .009 | ||
| Life satisfaction | COVID-19 related worries | COVID-19 cases/100,000 population | ‒.07 | .01 | [‒.01, −.01] | <.001 |
| COVID-19 deaths/100,000 population | .01 | .01 | [‒.11, .05] | .27 | ||
| Political response | ‒.01 | .01 | [‒.02, .00] | .07 | ||
| Number of people living together | ‒.01 | .01 | [‒.05, .01] | .22 | ||
| Household characteristics | ‒.00 | .00 | [‒.08, .07] | .84 | ||
| Frequency of going outside | ‒.01 | .01 | [‒.12, −.02] | .008 | ||
| Frequency of consulting COVID-19 related information | ‒.01 | .00 | [‒.23, −.04] | .006 | ||
| Having been infected with coronavirus | ‒.02 | .01 | [‒.18, −.05] | .001 | ||
| Family member has been infected with the coronavirus | ‒.01 | .00 | [‒.15, .01] | .08 | ||
The combination of direct and indirect effects explains 29.3% of the variance of depression, 24.3% of the variance of anxiety, 31.8% of the variance of stress and 12.0% of the variance of life satisfaction.
Wald test of path differences showed that paths were significantly different for women and men [Wald test of parameter constraints (8) = 24.12, p < .01], as well as for adolescents and young adults [Wald test of parameter constraints (8) = 17.16, p = .03]. Overall, these findings indicate that the social psychological impact of COVID-19 on emotional symptoms and life satisfaction differ across gender and age (Figure 3). When looking at the paths between independent and mediator variables, there were significant difference in the association between personal and country-specific impact of the COVID-19 and COVID-19 related worries with regard to gender [Wald test of parameter constraints (4) = 18.33, p < .01] and age [Wald test of parameter constraints (4) = 10.60, p = .03]. However, when considering the paths between mediator and dependent variables, there were no significant difference in the impact of COVID-19 related worries on emotional distress and life satisfaction regarding gender [Wald test of parameter constraints (3) = 5.79, p = .12] nor age [Wald test of parameter constraints (3) = 5.58, p = .13]. Additionally, women and men, adolescents and young adults did not differ significantly in terms of COVID-19 cases that predict depression [Wald test of parameter constraints for gender (1) = 0.07, p = .78; for age (1) = 0.79, p = .37]. Regardless, these findings indicate we cannot assume that the associations are equal across gender.
Figure 3.
Tested multigroup structural equation models separated for women, men, adolescents and young adults. Note. All parameters are standardized and significant. Non-significant effects have not been included to facilitate the interpretation.
Discussion
The present study contributes to the recent literature on the social psychological impact of the COVID-19 pandemic on adolescents and youth mental health and well-being providing novel insights from a cross-cultural perspective. Given the ongoing global health crisis, it is crucial to gather empirical evidence that increase our understanding of possible protective and risk factors that could influence COVID-19-related stressors, which is especially important for vulnerable populations such as adolescents and young people. Thus, the aim of this cross-cultural study was to examine the social psychological effects of COVID-19 on adolescents’ and young people’s emotional distress (COVID-19 related worries and emotional symptoms) and subjective well-being (life satisfaction).
We first hypothesized to find cross-cultural difference in COVID-19 related worries, emotional symptoms and life satisfaction. The results from multivariate ANOVAs confirmed this hypothesis, indicating that adolescents and young people from Spain reported to be less worried about the individual, social, economic and political impact of the pandemic compared to those living in Latin-American countries. Additionally, Spanish participants also experienced significantly less symptoms of depression, anxiety and stress in comparison to participants from the other four countries. Furthermore, our results revealed that adolescents and young people from Chile were the once most affected in terms of well-being, showing significantly lower levels of life satisfaction than the participants from Colombia, Ecuador and Spain. These findings suggest that there are differences in how adolescents and young people from different Ibero-American countries experience and cope with the difficulties caused by the COVID-19 pandemic, observing a greater impact on the mental health and well-being of participants from Latin-American countries, especially Chile. These results are in line with a recent commentary on the mental health and COVID-19 pandemic in Chile (Caqueo-Urízar et al., 2020) stressing the fragile situation of Chileans’ population––high index of emotional disorders among adults and adolescents––prior to the coronavirus outbreak, which has been exacerbated by the public health measures such as lockdowns, social distancing and closings.
In addition to cross-cultural differences in COVID-19 related worries, emotional symptoms and life satisfaction, the results also indicated significant effects for gender and age. Thus, women were more worried about the pandemic than men, presenting also higher levels of emotional symptoms but lower levels of life satisfaction compared to men. Indeed, previous studies have suggested that the pandemic may have a greater impact on women’s health. A plausible explanation for the greater vulnerability reported by women could derive from the fact that women are predominant when it comes to taking up caregiving tasks, letting them more exposed to a higher risk of infection than men and, consequently, to a higher negative impact in psychophysiological variables (Almeida et al., 2020). It is worth noting that most women took up both domestic and job-related tasks, which can also explain a rise in the workload and a subsequent increment of stress levels (Czymara et al., 2021). Regarding the effect of age, our results indicated that adolescents were less worried about the pandemic and its consequences, although they presented higher levels of depression and anxiety symptoms, as well as lower levels of life satisfaction in comparison to young adults. In line with previous studies, younger people seem to be more vulnerable to the development of emotional distress during the COVID-19 pandemic due to their limited resources to cope with distress, boredom, and lack of social interactions caused by the current health crisis (Marques de Miranda et al., 2020; Ravens-Sieberer et al., 2021).
Regarding our second hypothesis, we expected to find a mediation effect of COVID-19 related worries in the association of personal and the country-specific impact of the COVID-19 pandemic with emotional symptoms and life satisfaction. The results from our structural equation model (SEM) confirmed this hypothesis, demonstrating the accuracy of the proposed mediation model, both gender and age groups accordingly. Specifically, direct effects were observed from COVID-19 cases, political response, and participants’ personal conditions during lockdown on COVID-19 related worries, however some different paths were observed across gender and age. Thus, adolescents and young adults, women as well as men, living in countries with a higher incidence of COVID-19 case and higher level of stringency in restriction measures during the lockdown reported being more concerned about the pandemic and its consequences. COVID-19 related worries were more strongly fuelled by the living conditions during lockdown, the frequency of going outside and seeking COVID-19 related information, as well as having been infected with the coronavirus oneself and/or a family member, expect this association was not significant for men. Our findings confirm the results from recent studies, showing that the personal and sociopolitical circumstances during lockdown have a psychological impact on the population increasing their worries and fears (Filgueiras & Stults-Kolehmainen, 2021; Horesh et al., 2020; Mensi et al., 2021; Tamarit et al., 2020).
Furthermore, the results obtained by our SEM showed that COVID-19 related worries had a direct positive effect on depression, anxiety and stress, with psychosocial worries being the strongest predictor, for both gender and age groups equally. Surprisingly, the effect of health worries on depression was reversed in the overall model, however in the separated models for women, men, adolescents and young adults the association was positive as expected. One possible explanation might be the suppression effects of all three COVID-19 related worries on depressive symptoms in this complex prediction models with interrelated mediators (Paulhus et al., 2004). That is, most of the variance explained by health worries may be shared with the variance explained by economic and psychosocial worries, which would indicate a negative association. However, the remaining variance accounted by health concerns alone is smaller and, in this case, indicates a positive association. Such suppression effects disappear in the multigroup models, thus testing the mediation model separately for gender and age groups provides a better understanding of the actual association between health worries and depression.
In addition, a direct effect positive effect from COVID-19 cases on depression was included in the mediation model. Thus, adolescents and young adults, women as well as men, who were more concerned about the psychosocial, economic and political impact of the pandemic presented more symptoms of depression, anxiety and stress. The increasing number of COVID-19 cases contributes to higher levels of depression, while concerns about one’s own and others' health status may reduce such symptoms. This result is in line with previous studies reporting that COVID-19-related worries and fears are strong predictors of the development of mental health problems during the pandemic (Şimşir et al., 2021).
Our results also indicate that COVID-19 related economic worries and to a greater extend psychosocial worries had a negative effect on life satisfaction, while the effect of health worries on life satisfaction was positive. Our findings confirm the results from recent studies, showing that COVID-19 worries and fears have a direct impact on reducing life satisfaction (Satici et al., 2020). The unespected positive association between health worries and life satisfaction in the overall model could be explained by the suppression effects that might emerge due to high intercorrelaion among COVID-19 worries, which have been explained above. These suppression effects also disappear in the separated models for women, men, adolescents and young adults, where the association was negative as expected. The mediation model that have been tested separately for gender and age groups provides a better understanding of the actual association between health worries and life satisfaction.
Finally, the SEM mediation analysis confirmed the overall indirect effects of COVID-19 cases, political response and participants’ conditions during lockdown on depression, anxiety, stress and life satisfaction mediated by COVID-19 related worries. Thus, our results showed that adolescents and young people living in Ibero-American countries with higher incidence of COVID-19 cases and higher levels of stringency in the political response, who also were more likely to go outdoors and consult COVID-19 related information and who had been infected by the coronavirus themselves or a family member, reported higher levels of depression, anxiety, and stress and lower levels of life satisfaction, which could be explained by their increased concern about COVID-19 and its consequences. Our findings are consistent with recent studies, showing the risk of COVID-10 related worries and fears threating adolescents and young people’s mental health and well-being (Magson et al., 2021).
Strengths and Limitations
Our findings shed light on the role of political and personal factors that are involved in coping with COVID-19 related stressors during the early stages of COVID-19 pandemic in five Ibero-American countries. The study presented data from a large cross-cultural sample during the first year of the COVID-19 pandemic reflecting on the different circumstances of the Ibero-American population. One of our main findings was that adolescents and young people from Spain reported lower levels of COVID-19 related worries, anxiety, depression and stress compared to the other countries, while Chileans’ mental health and well-being was particularly impaired by the COVID-19 pandemic. Another main finding was the related to the mediating effect of worries about COVID-19 that mediated the impact of the political and personal circumstances during lockdown on adolescents and young people’s mental health and well-being. Although mediational models do not test causality directly, they are very insightful by providing empirical evidence to identify the social psychological factors that underly this relationship, which may offer guidance to policy makers, health services and social services and parents for safeguarding the mental health of adolescents and young people. We aim to identify their needs during the pandemic from a cross-cultural perspective, while most of previous research had primarily studied the psychological impact of the COVID-19 on the general population. That is, in order to mitigate adolescents’ mental problems and foster their well-being, it is important to address their worries and fears about COVID-19, mitigating their negative effect. For instance, previous studies have identified the important role of family and social support (Fish et al., 2020; Magson et al., 2021; Tang et al., 2021), which are essential resources for young people to express, discuss and eventually overcome their fears and concerns with the help of a family member, their peers or even a professional.
Although the findings contribute to the literature on the social psychological impact of the COVID-19 pandemic on adolescents and youth mental health and well-being, this study is not without limitations. Cross-cultural data from five Ibero-American countries have been analyzed in this study with a 60% of the sample from the Chilean population, which may have a representativeness bias. Collecting data through an online survey has an inherent limitation in terms of generalizing our results to the general population. However, participants in this study did not receive any payment or financial reward to mitigate careless responding, so their main motivation for completing the survey was to share their views. Although the use of self-report measures was appropriate for the sample studied, with adolescents and young people being reliable reporters of their feelings and thoughts, future research may use mixed methods (qualitative and quantitative), or include objective measures to reduce common method bias. The study used a cross-sectional design that does not permit the establishing of causal relationships between the variables studied. Therefore, further research based on longitudinal data is needed to determine the social and psychological mechanisms underlying the mental health conditions and well-being of young people during the ongoing COVID-19 pandemic.
Conclusions
In conclusion, the COVID-19 pandemic continues to carry new waves of infection and new variants are appearing, which makes it necessary to continue implementing a series of health measures such as social distancing, quarantine, mobility restrictions, among others. Society seems to be adapting to the current pandemic and the new circumstances it has created on a social, political and personal level, as there is nothing, we can do to prevent it–––at least there is an attempt to reduce its impact through vaccination. However, there is much empirical evidence accumulated over the last year that many of these circumstances are a threat to the mental health and well-being of adolescents and young people, especially in some Latin American countries such as Chile with a particularly fragile situation prior to the pandemic. Our findings could provide a reference point for designing effective interventions to help young people in Ibero-America to alleviate their suffering. Indeed, as the model proposed in this research indicates, the psychological mechanism underlying mental health problems could be partly explained by increased worries and concerns about COVID-19 and its personal, social, economic and political consequences. Therefore, addressing adolescents and young people’s fears, giving them the opportunity to talk about their concerns, discussing the situation and the extent to which it interferes with young people’s lives, offering alternatives to cope with this stressful situation could make a significant difference. Thus, parents, teachers, health professionals and communities should make a collective effort to restore adolescents and young people’s self-confidence so that they can overcome this crisis, reducing their emotional distress and enhancing their happiness.
Author Biographies
Konstanze Schoeps, Department of Personality, Psychological Assessment and Treatment, Universitat de València, Valencia, Spain.
Alicia Tamarit, Department of Personality, Psychological Assessment and Treatment, Universitat de València, Valencia, Spain.
Usue De la Barrera, Department of Personality, Psychological Assessment and Treatment, Universitat de València, Valencia, Spain.
Laura Lacomba-Trejo, Department of Personality, Psychological Assessment and Treatment, Universitat de València, Valencia, Spain.
Inmaculada Montoya-Castilla, Department of Personality, Psychological Assessment and Treatment, Universitat de València, Valencia, Spain.
Constanza del Rosario, Fundación Relaciones Inteligentes, Santiago, Chile.
Fernanda Coello, Department of Clinical Psychology, Universidad de Azuay, Cuenca, Ecuador.
Sebastián Herrera, Department of Clinical Psychology, Universidad de Azuay, Cuenca, Ecuador.
Ángela Trujillo, Department of Psychology, Universidad de La Sabana, Chía, Colombia.
Fernando Riveros Munevar, Department of Psychology, Universidad de La Sabana, Chía, Colombia.
Nancy Alejandra Amador Esparza, Department of Social Sciences, Universidad Autónoma de Ciudad Juárez, Ciudad Juárez, Mexico.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by grants from the Spanish Ministry of Science, Innovation and Universities (PSI2017-84005-R) and the European Regional Development Fund (FEDER) from the European Union.
Informed Consent: The Ethics Committee of Research in Humans of the Ethics Commission in Experimental Research of the University of Valencia approved study consent, procedures and research protocol (Reference number: 1595575567385, July 23th 2020). Before accessing the survey, participants gave their informed consent to participate in the study.
Data Availability Statement: The datasets generated and analysed during the current study are not publicly available due to the fact that they constitute an excerpt of research in progress but are available from the corresponding author on reasonable request.
ORCID iD
Konstanze Schoeps https://orcid.org/0000-0002-6312-7055
References
- Almeida M., Shrestha A., Stojanac D., Miller L. (2020). The impact of the COVID-19 pandemic on women’s mental health. Archives of Women’s Mental Health, 23(6), 741–748. 10.1007/s00737-020-01092-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aloi A., Alonso B., Benavente J., Cordera R., Echániz E., González F., Ladisa C., Lezama-Romanelli R., López-Parra Á., Mazzei V., Perrucci L., Prieto-Quintana D., Rodríguez A., Sañudo R. (2020). Effects of the COVID-19 lockdown on urban mobility: Empirical evidence from the city of Santander (Spain). Sustainability (Switzerland), 12(9), 1–18. 10.3390/su12093870 [DOI] [Google Scholar]
- Atun R., De Andrade L. O. M., Almeida G., Cotlear D., Dmytraczenko T., Frenz P., Garcia P., Gómez-Dantés O., Knaul F. M., Muntaner C., De Paula J. B., Rígoli F., Serrate P. C. F., Wagstaff A. (2015). Health-system reform and universal health coverage in Latin America. Lancet 385(9974), 1230–1247. 10.1016/S0140-6736(14)61646-9 [DOI] [PubMed] [Google Scholar]
- Ausín B., González-Sanguino C., Castellanos M. Á., Muñoz M. (2021). Gender-related differences in the psychological impact of confinement as a consequence of COVID-19 in Spain. Journal of Gender Studies, 30(1), 29–38. 10.1080/09589236.2020.1799768 [DOI] [Google Scholar]
- Barber S. J., Kim H. (2020). COVID-19 worries and behavior changes in older and younger men and women. The Journals of Gerontology: Series B, 76(2), e17–e23. 10.1093/geronb/gbaa068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barzilay R., Moore T. M., Greenberg D. M., DiDomenico G. E., Brown L. A., White L. K., Gur R. C., Gur R. E. (2020). Resilience, COVID-19-related stress, anxiety and depression during the pandemic in a large population enriched for healthcare providers. Translational Psychiatry, 10(1), 1–8. 10.1038/s41398-020-00982-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergman Y. S., Cohen-Fridel S., Shrira A., Bodner E., Palgi Y. (2020). COVID-19 health worries and anxiety symptoms among older adults: The moderating role of ageism. International Psychogeriatrics, 32(11), 1371–1375. 10.1017/S1041610220001258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campos J. A. D. B., Campos L. A., Martins B. G., Valadão Dias F., Ruano R., Maroco J. (2021). The psychological impact of COVID-19 on individuals with and without mental health disorders. Psychological Reports, 21, Article 332941211026850. 10.1177/00332941211026850 [DOI] [PubMed] [Google Scholar]
- Caqueo-Urízar A., Urzúa A., Aragón-Caqueo D., Charles C. H., El-Khatib Z., Otu A., Yaya S. (2020). Mental health and the COVID-19 pandemic in Chile. Psychological Trauma: Theory, Research, Practice, and Policy, 12(5), 521. 10.1037/tra0000753 [DOI] [PubMed] [Google Scholar]
- Chen J., Liu X., Wang D., Jin Y., He M., Ma Y., Zhao X., Song S., Zhang L., Xiang X., Yang L., Song J., Bai T., Hou X. (2021). Risk factors for depression and anxiety in healthcare workers deployed during the COVID-19 outbreak in China. Social Psychiatry and Psychiatric Epidemiology, 56(1), 47–55. 10.1007/s00127-020-01954-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Codagnone C., Bogliacino F., Gómez C., Charris R., Montealegre F., Liva G., Lupia F., Folkvord F., Veltri G. A. (2020). Assessing concerns for the economic consequence of the COVID-19 response and mental health problems associated with economic vulnerability and negative economic shock in Italy, Spain, and the United Kingdom. Plos One, 15(10), 1–17. 10.1371/journal.pone.0240876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czymara C. S., Langenkamp A., Cano T. (2021). Cause for concerns: Gender inequality in experiencing the COVID-19 lockdown in Germany. European Societies, 23(1), S68–S81. 10.1080/14616696.2020.1808692 [DOI] [Google Scholar]
- Daza P., Novy D. M., Stanley M. A., Averill P. (2002). The depression anxiety stress scale-21: Spanish translation and validation with a Hispanic sample. Journal of Psychopathology and Behavioral Assessment, 24(3), 195–205. 10.1023/A:1016014818163 [DOI] [Google Scholar]
- Diener E. (1984). Subjective well-being. Psychological Bulletin, 95(3), 542–575. 10.1037/0033-2909.95.3.542 [DOI] [PubMed] [Google Scholar]
- Duan L., Shao X., Wang Y., Huang Y., Miao J., Yang X., Zhu G. (2020). An investigation of mental health status of children and adolescents in China during the outbreak of COVID-19. Journal of Affective Disorders, 275, 112–118. 10.1016/j.jad.2020.06.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filgueiras A., Stults-Kolehmainen M. (2021). Risk factors for potential mental illness among Brazilians in quarantine due to COVID-19. Psychological Reports, 125(2), 723–741. 10.1177/0033294120976628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fish J. N., McInroy L. B., Paceley M. S., Williams N. D., Henderson S., Levine D. S., Edsall R. N. (2020). “I’m Kinda stuck at home with unsupportive parents right now”: LGBTQ Youths’ experiences with COVID-19 and the importance of online support. Journal of Adolescent Health, 67(3), 450–452. 10.1016/j.jadohealth.2020.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher J. R. W., Tran T. D., Hammarberg K., Sastry J., Nguyen H., Rowe H., Popplestone S., Stocker R., Stubber C., Kirkman M. (2020). Mental health of people in Australia in the first month of COVID-19 restrictions: A national survey. Medical Journal of Australia, 213(10), 458–464. 10.5694/mja2.50831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fonseca-Pedrero E., Paino M., Lemos-Giráldez S., Muñiz J. (2010). Propiedades psicométricas de la depression anxiety and stress scales-21 (DASS-21) en universitarios españoles. Ansiedad y Estres, 16(2–3), 215–226. [Google Scholar]
- García-Fernández L., Romero-Ferreiro V., Padilla S., Lahera G., Rodriguez-Jimenez R. (2021). Different emotional profile of health care staff and general population during the COVID-19 outbreak. Psychological Trauma, 14(2), 266–272. 10.1037/tra0001024 [DOI] [PubMed] [Google Scholar]
- García-Portilla P., de la Fuente Tomás L., Bobes-Bascarán T., Jiménez Treviño L., Zurrón Madera P., Suárez Álvarez M., Menéndez Miranda I., García Álvarez L., Sáiz Martínez P. A., Bobes J. (2020). Are older adults also at higher psychological risk from COVID-19? Aging and Mental Health, 25(7), 1297–1304. 10.1080/13607863.2020.1805723 [DOI] [PubMed] [Google Scholar]
- Gilead T., Dishon G. (2021). Rethinking future uncertainty in the shadow ofCOVID 19: Education, change, complexity andadaptability. Educational Philosophy and Theory, 1–14. 10.1080/00131857.2021.1920395 [DOI] [Google Scholar]
- Gómez-Becerra I., Flujas J. M., Andrés M., Sánchez-López P., Fernández-Torres M. (2020). Evolution of psychological state and fear in childhood and adolescence during COVID-19 lockdown. Revista de Psicologia Clinica Con Ninos y Adolescentes, 7(3), 11–18. 10.21134/rpcna.2020.mon.2029 [DOI] [Google Scholar]
- Gonzales G., Loret de Mola E., Gavulic K. A., McKay T., Purcell C. (2020). Mental health needs among lesbian, gay, bisexual, and transgender college students during the COVID-19 pandemic. Journal of Adolescent Health, 67(5), 645–648. 10.1016/j.jadohealth.2020.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graetz D., Agulnik A., Ranadive R., Vedaraju Y., Chen Y., Chantada G., Metzger M. L., Mukkada S., Force L. M., Friedrich P., Lam C., Sniderman E., Bhakta N., Hessissen L., Dalvi R., Devidas M., Pritchard-Jones K., Rodriguez-Galindo C., Moreira D. C. (2021). Global effect of the COVID-19 pandemic on paediatric cancer care: A cross-sectional study. The Lancet Child & Adolescent Health, 4642(21), 1–9. 10.1016/S2352-4642(21)00031-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horesh D., Kapel Lev-Ari R., Hasson-Ohayon I. (2020). Risk factors for psychological distress during the COVID-19 pandemic in Israel: Loneliness, age, gender, and health status play an important role. British Journal of Health Psychology, 25(4), 925–933. 10.1111/bjhp.12455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Igartua J.-J., Ortega-Mohedano F., Arcila-Calderón C. (2020). Communication use in the times of the coronavirus. A cross-cultural study. El Profesional de La Información, 29(3), Article e290318. 10.3145/epi.2020.may.18 [DOI] [Google Scholar]
- Isumi A., Doi S., Yamaoka Y., Takahashi K., Fujiwara T. (2020). Do suicide rates in children and adolescents change during school closure in Japan? The acute effect of the first wave of COVID-19 pandemic on child and adolescent mental health. Child Abuse & Neglect, 110(P2), Article 104680. 10.1016/j.chiabu.2020.104680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavanagh M. M., Singh R. (2020). Democracy, capacity, and coercion in pandemic response: COVID-19 in comparative political perspective. Journal of Health Politics, 45(6), 997–1012. 10.1215/03616878-8641530 [DOI] [PubMed] [Google Scholar]
- Lab G. C. D. (2021). Our world in data. https://global-change-data-lab.org/ [Google Scholar]
- León-Pinilla R., Prado-Gascó V. J., Jiménez Ivar M. A. (2015). Scale of positive and negative experience (SPANE) © Copyright by Ed Diener and Robert Biswas-Diener, 2009. [Google Scholar]
- Liang L., Ren H., Cao R., Hu Y., Qin Z., Li C., Mei S. (2020). The effect of COVID-19 on youth mental health. Psychiatric Quarterly, 91(3), 841–852. 10.1007/s11126-020-09744-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lima C. K. T., Carvalho P. M. M., Lima I. A. A. S., Nunes J. V. A. O., Saraiva J. S., de Souza R. I., da Silva C. G. L., Neto M. L. R. (2020). The emotional impact of coronavirus 2019-nCoV (new coronavirus disease). Psychiatry Research, 287, Article 112915. 10.1016/j.psychres.2020.112915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin C. Y. (2020). Social reaction toward the 2019 novel coronavirus (COVID-19). Social Health and Behavior, 3(1), 1–2. 10.4103/SHB.SHB [DOI] [Google Scholar]
- Losada-Baltar A., Jiménez-Gonzalo L., Gallego-Alberto L., del Sequeros Pedroso-Chaparro M., Fernandes-Pires J., Márquez-González M. (2020). “We are staying at home.” Association of self-perceptions of aging, personal and family resources, and loneliness with psychological distress during the lock-down period of COVID-19. Journals of Gerontology: Psychological Sciences, 76(2), e10–e16. 10.1093/geronb/gbaa048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond P. F., Lovibond S. H. (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the beck depression and anxiety inventories. Behaviour Research and Therapy, 33(3), 335–343. 10.1016/0005-7967(94)00075-U [DOI] [PubMed] [Google Scholar]
- Magson N. R., Freeman J. Y. A., Rapee R. M., Richardson C. E., Oar E. L., Fardouly J. (2021). Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. Journal of Youth and Adolescence, 50(1), 44–57. 10.1007/s10964-020-01332-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marques de Miranda D., da Silva Athanasio B., Sena Oliveira A. C., Simoes-e-Silva A. C. (2020). How is COVID-19 pandemic impacting mental health of children and adolescents? International Journal of Disaster Risk Reduction, 51, Article 101845. 10.1016/j.ijdrr.2020.101845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McElroy E., Patalay P., Moltrecht B., Shevlin M., Shum A., Creswell C., Waite P. (2020). Demographic and health factors associated with pandemic anxiety in the context of COVID-19. British Journal of Health Psychology, 25(4), 934–944. 10.1111/bjhp.12470 [DOI] [PubMed] [Google Scholar]
- Mensi M. M., Capone L., Rogantini C., Orlandi M., Ballante E., Borgatti R. (2021). COVID-19-related psychiatric impact on Italian adolescent population: A cross-sectional cohort study. Journal of Community Psychology, 48(5), 1457–1469. 10.1002/jcop.22563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mistry S. K., Ali A. R. M. M., Hossain M. B., Yadav U. N., Ghimire S., Rahman M. A., Irfan N. M., Huque R. (2021). Exploring depressive symptoms and its associates among Bangladeshi older adults amid COVID-19 pandemic: Findings from a cross-sectional study. Social Psychiatry and Psychiatric Epidemiology, 56(8), 1487–1497. 10.1007/s00127-021-02052-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mónaco E., Schoeps K., Montoya-Castilla M. (2019). Attachment styles and well-being in adolescents: How does emotional development affect this relationship? International Journal of Environmental Research and Public Health Article, 16(14), 2554. 10.3390/ijerph16142554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mónaco E., Schoeps K., Valero-Moreno S., Castro-Calvo J., Montoya-Castilla I., del Rosario C., Coello M. F., Herrera S., Trujillo Cano Á. M., Riveros Munevar E. F., Amador Esparza N. A. (2021). Cross-cultural validation of the worries about COVID-19 and its consequences scale (W-COV) in adolescents. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moya-Lacasa C., Alvarez-Vázquez C. M., González-Blanco L., Valtueña-García M., Martín-Gil E., Seijo-Zazo E., De la Fuente-Tomás L., García-Alvarez L., Sáiz P., García-Portilla M. P., Bobes J. (2021). Impact of the coronavirus outbreak on mental health in the different Spanish regions. Actas Espanolas de Psiquiatria, 49(2), 64–70. [PubMed] [Google Scholar]
- Okabe-Miyamoto K., Folk D., Lyubomirsky S., Dunn E. W. (2021). Changes in social connection during COVID-19 social distancing: It’s not (household) size that matters, it’s who you’re with. Plos One, 16(1), e0245009. 10.1371/journal.pone.0245009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okabe-Miyamoto K, Folk D, Lyubomirsky S, Dunn EW. (2021). Changes in social connection during COVID-19 social distancing: It’s not (household) size that matters, it’s who you’re with. PLOS ONE, 16(1), e0245009. 10.1371/journal.pone.0245009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulhus D. L., Robins R. W., Trzesniewski K. H., Tracy J. L. (2004). Two replicable suppressor situations in personality research. Multivariate Behavioral Research, 39(2), 329–358. 10.1207/s15327906mbr3902 [DOI] [PubMed] [Google Scholar]
- Prime H., Wade M., Browne D. T. (2020). Risk and resilience in family well-being during the COVID-19 pandemic. American Psychologist, 75(5), 631–643. 10.1037/amp0000660 [DOI] [PubMed] [Google Scholar]
- Puci M. V., Nosari G., Loi F., Puci G. V., Montomoli C., Ferraro O. E. (2020). Risk perception and worries among health care workers in the COVID-19 pandemic: Findings from an Italian survey. Healthcare, 8(4), 535. 10.3390/healthcare8040535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purtle J. (2020). COVID-19 and mental health equity in the United States. Social Psychiatry and Psychiatric Epidemiology, 55(8), 969–971. 10.1007/s00127-020-01896-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravens-Sieberer U., Kaman A., Erhart M., Devine J., Schlack R., Otto C. (2021). Impact of the COVID-19 pandemic on quality of life and mental health in children and adolescents in Germany. European Child and Adolescent Psychiatry, 25, 1–11. 10.1007/s00787-021-01726-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rico A., Freire J. M., Gérvas J. (2007). El sistema sanitario español (1976-2006): factores de éxito en perspectiva internacional comparada. In Estado de Bienestar y Competitividad. La experiencia Europea (pp. 401-444). Dialnet, 978-84-323-1303-5. [Google Scholar]
- Rogers A. A., Ha T., Ockey S. (2021). Adolescents’ perceived socio-emotional impact of COVID-19 and implications for mental health: Results from a U.S.-based mixed-methods study. Journal of Adolescent Health, 68(1), 43–52. 10.1016/j.jadohealth.2020.09.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossi R., Socci V., Talevi D., Mensi S., Niolu C., Pacitti F., Di Marco A., Rossi A., Siracusano A., Di Lorenzo G. (2020). COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Frontiers in Psychiatry, 11, 790. 10.3389/fpsyt.2020.00790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandín B., Valiente R. M., García-Escalera J., Chorot P. (2020). Impacto psicológico de la pandemia de COVID-19: Efectos negativos y positivos en población española asociados al periodo de confinamiento nacional. Revista de Psicopatología y Psicología Clínica, 25(1), 1. 10.5944/rppc.27569 [DOI] [Google Scholar]
- Satici B., Gocet-Tekin E., Deniz M. E., Satici S. A. (2020). Adaptation of the fear of COVID-19 scale: Its association with psychological distress and life satisfaction in Turkey. International Journal of Mental Health and Addiction, 19(6), 1980–1988. 10.1007/s11469-020-00294-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Şimşir Z., Koç H., Seki T., Griffiths M. D. (2021). The relationship between fear of COVID-19 and mental health problems: A meta-analysis. Death Studies, 46(3), 515–523. 10.1080/07481187.2021.1889097 [DOI] [PubMed] [Google Scholar]
- Tamarit A., de la Barrera U., Mónaco E., Schoeps K., Montoya-Castilla I. (2020). Psychological impact of COVID-19 pandemic in Spanish adolescents: Risk and protective factors of emotional symptoms. Revista de Psicologia Clínica Con Niños y Adolescentes, 7(3), 73–80. 10.21134/rpcna.2020.mon.2037 [DOI] [Google Scholar]
- Tang S., Xiang M., Cheung T., Xiang Y. T. (2021). Mental health and its correlates among children and adolescents during COVID-19 school closure: The importance of parent-child discussion. Journal of Affective Disorders, 279(2020), 353–360. 10.1016/j.jad.2020.10.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The World Bank . (2019). Population, total | data. [Google Scholar]
- Trzebiński J., Cabański M., Czarnecka J. Z. (2020). Reaction to the COVID-19 pandemic: The influence of meaning in life, life satisfaction, and assumptions on world orderliness and positivity. Journal of Loss and Trauma, 25(6–7), 544–557. 10.1080/15325024.2020.1765098 [DOI] [Google Scholar]
- Valero-Moreno S., Lacomba-Trejo L., Tamarit A., Pérez-Marín M., Montoya-Castilla I. (2021). Psycho-emotional adjustment in parents of adolescents: A cross-sectional and longitudinal analysis of the impact of the COVID pandemic. Journal of Pediatric Nursing, 59(2021), e44–e51. 10.1016/j.pedn.2021.01.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vázquez C., Duque A., Hervás G. (2013). Satisfaction with life scale in a representative sample of Spanish adults: Validation and normative data. The Spanish Journal of Psychology, 16, E82. 10.1017/sjp.2013.82 [DOI] [PubMed] [Google Scholar]
- Vinkers C. H., van Amelsvoort T., Bisson J. I., Branchi I., Cryan J. F., Domschke K., Howes O. D., Manchia M., Pinto L., de Quervain D., Schmidt M. V., van der Wee N. J. A. (2020). Stress resilience during the coronavirus pandemic. European Neuropsychopharmacology, 35, 12–16. 10.1016/j.euroneuro.2020.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson J. M., Lee J., Shook N. J. (2020). COVID-19 worries and mental health: The moderating effect of age. Aging and Mental Health, 25(7), 1289–1296. 10.1080/13607863.2020.1856778 [DOI] [PubMed] [Google Scholar]
- World Health Organization . (2020). Country & technical guidance-coronavirus disease (COVID-19). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance-publications [Google Scholar]
- World Health Organization . (2021). WHO coronavirus (COVID-19) Dashboard. [Google Scholar]
- World Medical Association . (2013). World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. Journal of American Medical Association (JAMA), 310(20), 2191–2194. 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- Yıldırım M., Arslan G., Özaslan A. (2020). Perceived risk and mental health problems among healthcare professionals during COVID-19 pandemic: Exploring the mediating effects of resilience and coronavirus fear. International Journal of Mental Health and Addiction, 20(2), 1–11. 10.1007/s11469-020-00424-8 [DOI] [PMC free article] [PubMed] [Google Scholar]