Since the COVID-19 pandemic began over 2 years ago, its global impact has been enormous. Our growing understanding of the pathophysiology of this disease has particular links to hematology. Introduced by Ortel and Berliner, this Review Series provides up-to-date overviews of the many areas in which COVID-19 has implications for hematology practice.
Visual Abstract
Abstract
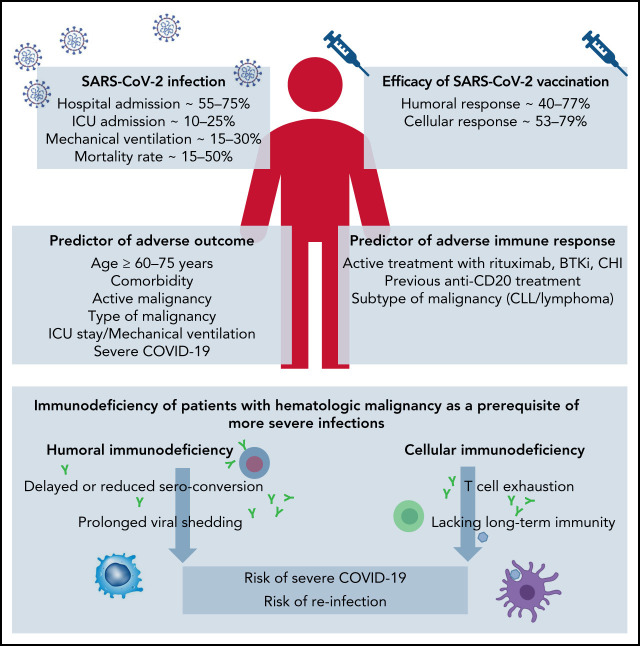
The coronavirus infectious disease (COVID-19) shows a remarkable symptomatic heterogeneity. Several risk factors including advanced age, previous illnesses, and a compromised immune system contribute to an unfavorable outcome. In patients with hematologic malignancy, the immune response to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is significantly reduced explaining why the mortality rate of hematologic patients hospitalized for a SARS-CoV-2 infection is about 34%. Active immunization is an essential pillar to prevent SARS-CoV-2 infections in patients with hematologic malignancy. However, the immune response to SARS-CoV-2 vaccines may be significantly impaired, as only half of patients with hematologic malignancy develop a measurable antiviral antibody response. The subtype of hematologic malignancy and B cell–depleting treatment predict a poor immune response to vaccination. Recently, antiviral drugs and monoclonal antibodies for pre-exposure or postexposure prophylaxis and for early treatment of COVID-19 have become available. These therapies should be offered to patients at high risk for severe COVID-19 and vaccine nonresponders. Importantly, as the virus evolves, some therapies may lose their clinical efficacy against new variants. Therefore, the ongoing pandemic will remain a major challenge for patients with hematologic malignancy and their caregivers who need to constantly monitor the scientific progress in this area.
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was identified as the causative agent of the coronavirus infectious disease (COVID-19) in early 2020. Since December 2020, variants of concerns with increased transmissibility or with an escape to prior immunization have been reported.1-5 Since November 2021, variant B.1.1.529 (Omicron) was discovered in Botswana. This variant of concern encodes the largest number of genomic mutations reported thus far, including 32 mutations in the spike protein alone.6
It has become apparent that the clinical course of COVID-19 is more severe in patients with hematologic malignancy (HM). Therefore, we wished to summarize the current knowledge on COVID-19 in these diseases and performed a systematic literature search using the terms “hematologic malignancy,” “immunosuppressive,” and “COVID-19.”
COVID-19 in patients with hematologic malignancy
In light of the complex and profound immune dysfunction of patients with HM, already the first reports from Wuhan, China, demonstrated a more severe course of COVID-19 and a higher case fatality rate for patients with HM.7 Although hospitalized patients with HM had a similar case rate of COVID-19 compared with normal health care providers (10% and 7%), the case fatality rate was significant higher, with 62% for patients with HM compared with 0%, respectively. Thereafter, cohort studies and surveys from Europe, North America, South America, and Asia evaluated larger case series of patients with HM with COVID-19 and searched for risk factors associated with an adverse outcome (Table 1). Summarizing all studies reporting on more than 50 patients with HM with COVID-19, the overall hospitalization rate ranged from 56.4% to 73.8%, the intensive care unit (ICU) admission rate was 9.8% to 24.1%, mechanical ventilation was applied to 13.8% to 29.2%, and 14.1% to 51.5% of all patients died.8-42
Table 1.
COVID-19 in patients with hematologic malignancy: summary of studies of COVID-19 in >50 patients with hematologic malignancy
| Reference | Investigator | Patient population | Study design | Clinical severity (%) | Mortality (%) | Risk factors for severe COVID-19 |
|---|---|---|---|---|---|---|
| 9 | NCATS' National COVID Cohort Collaborative | 63 413 cancer patients with COVID-19 • 10.5% patients with HM |
Retrospective cohort | • Age ≥ 65 • Male sex • Southern or western US residence • Recent cytotoxic therapy |
||
| 8 | European Haematology Association Survey (EPICOVIDEHA) | 3 801 patients with HM with COVID-19 | Survey | Hospitalization (73.1) ICU (18.1) |
HM patients died (31.2) | • Age • Active malignancy • Chronic cardiac disease • Liver disease • Renal impairment • Smoking history • ICU stay |
| 10 | COVID-19 and Cancer Consortium Registry (CCC19) | 4 966 cancer patients with COVID-19 (10.5% patients with HM) | Registry | Hospitalization (57.8) | Cancer patients died (14) | • Older age • Male sex • Obesity • Cardiovascular and pulmonary comorbidities • Renal disease • Diabetes mellitus • Non-Hispanic Black race • Hispanic ethnicity • ECOG PS • Recent cytotoxic chemotherapy • Hematologic malignancy |
| 11 | Republic of Turkey, Ministry of Health database | 740 patients with HM with COVID-19 | Retrospective cohort | Hospital admission (61.1), ICU admission (18.9), Mechanical ventilation (13.8) | HM patients died (13.7) | |
| 15 | Italian Hematology Alliance on COVID-19 | 536 patients with HM with COVID-19 | Retrospective cohort | HM patients died (36.9%) | • Older age • Progressive disease status • AML • Indolent NHL • Aggressive NHL • Plasma cell neoplasms • Severe/critical COVID-19 |
|
| 12 | Argentine Society of Hematology | 419 patients with HM with COVID-19 | Survey | Hospital admission (64.9), ICU (24.1) | HM patients died (20.7) | • Comorbidities • Disease status • Previous chemotherapy |
| 13 | Republic of Turkey, Ministry of Health database | 497 patients with HM with COVID-19 • 6.9% SCT recipients |
Retrospective cohort | Mechanical ventilation (16.7) • MV in HCT recipients (15.6) |
HM patients died (12.1) • HCT recipients died (15.5) |
|
| 14 | European Society for Blood and Marrow Transplantation (EBMT) and the Spanish Group of Hematopoietic Stem Cell Transplantation (GETH) | 382 SCT recipients with COVID-19 | Prospective survey | SCT recipients died (28) | • Older age • Need for ICU • Moderate/high immunodeficiency |
|
| 16 | Spanish transplant group and cell therapy (GETH) | 367 patients with HM with COVID-19 • 33.5% SCT recipients |
Retrospective cohort | • Hospitalization (56.4) • Oxygen support (40.8) • ICU (9.8) |
HM patients died 28.6% (105) | • Age > 70 y • Uncontrolled hematologic disease • Neutropenia • CRP > 20 mg/dL |
| 17 | Turkish Society of Hematology, Infectious Complications and Supportive Care Working Party | 340 patients with HM with COVID-19 | Retrospective cohort | Hospitalization (73.8) | HM patients died (26.5) | • Disease status • Decreased life expectancy related to primary HM • ICU admission • Type of COVID-19 treatment |
| 18 | NHS England | 10 926 COVID-related deaths • 3.1% patients with HM |
Analytic platform OpenSAFELY | HM patients died (3.1) | • Male • Greater age and deprivation • Diabetes • Severe asthma • Ethnicity |
|
| 19 | SEMI-COVID-19 Registry in Spain | 2 111 immunosuppressed patients with COVID-19 • 15.7% patients with HM |
Retrospective cohort | HM patients died (41.9) | ||
| 20 | National Israeli Study | 313 patients with HM with COVID-19 | Retrospective cohort | Hospitalization (56.9) | HM patients died (19.1) | • Severe COVID-19 • Age ≥ 70 |
| 21 | Center for International Blood and Marrow Transplant Research (CIBMTR) | 318 SCT recipients with COVID-19 • 57.9% allogeneic • 42.1% autologous |
Retrospective cohort | Mechanical ventilation (14.2) | SCT recipients died (20.8) | Allogeneic cohort: • Age ≥ 50 • Male sex • COVID-19 < 12 mo after SCT Autologous cohort: • Lymphoma |
| 22 | Tertiary level medical institute in North India | 242 patients with HM with COVID-19 | Retrospective cohort of electronic database system | Mechanical ventilation (21.1) | HM patients died (19.8) | • Severity of COVID-19 • Secondary infection • Invasive MV |
| 23 | UK Coronavirus Cancer Monitoring Project (UKCCMP) | 1 044 cancer patients with COVID-19 • 21.5% patients with HM |
Prospective cohort | Cancer patients died (30.6) | • Age • Sex • HM with recent chemotherapy |
|
| 24 | Electronic health record data collected by the IBM Watson Health Explorys from 360 US hospitals | 306 640 patients with HM • 0.07% with COVID-19 |
Retrospective case-control of electronic records | • Leukemia • NHL • Lung cancer |
||
| 25 | Cancer centers in France | 425 cancer patients with COVID-19 • 38.2% patients with HM |
Observational prospective | Cancer patients died (27.9) | • Male sex • Metastatic disease • History of inflammatory or autoimmune disease • Receiving immunosuppressive treatments • Lymphopenia ≤ 0.7 G/L |
|
| 26 | 11 centers across India | 130 HM with COVID-19 | Retrospective cohort | Oxygen support (51.5), Mechanical ventilation (29.2) |
HM patients died (20) | • Age ≥ 60 • Severe COVID • Disease status |
| 27 | Italian north-eastern Veneto Region | 1 090 cancer patients with COVID-19 • 124 HM with COVID-19 |
Retrospective population-based study | • Prevalent-active disease • Recent chemotherapy and radiotherapy |
||
| 28 | Guy's Cancer Centre and King's College Hospital in London | 306 cancer patients • 11.4% patients with HM |
Retrospective cohort | HM patients died (31.6) | • Male sex • Asian ethnicity • Hematologic malignancy • Cancer diagnosis > 2 y |
|
| 29 | 2 hematologic departments located in Lombardy, Italy | 102 HM with COVID-19 | HM patients died (39.2) | • Active hematologic treatment • Oxygen supplementation |
||
| 30 | single hematology center in the Czech Republic | 96 HM with COVID-19 | HM patients died (15.6) | • Age ≥ 60 | ||
| 31 | King’s College Hospital | 80 HM with COVID-19 | Retrospective cohort | HM patients died (35) | ||
| 11 | Republic of Turkey, Ministry of Health database | 77 HM with COVID-19 | Retrospective cohort | Mechanical ventilation (20.8) | HM patients died (20.8) | |
| 34 | Memorial Sloan-Kettering Cancer Center | 309 cancer patients with COVID-19 • 23.9% patients with HM |
Hospital admission (47.6) | Cancer patients died (10) | • Active hematologic or lung malignancy • Lymphopenia • Baseline neutropenia |
|
| 35 | London North West University Healthcare NHS Trust | 69 patients with HM with COVID-19 | Retrospective cohort | HM patients died (31.9) | ||
| 32 | Memorial Sloan-Kettering Cancer Center | 77 cellular therapy recipients with COVID-19 | Retrospective cohort | Cellular therapy recipients died (36.4) | ||
| 36 | Regional network of 7 hospitals | 66 HM with COVID-19 | Retrospective cohort | HM patients died (51.5) | ||
| 37 | Danish hematology departments | 66 HM with COVID-19 | ICU (21.2) | HM patients died (24.2) | • Older patients • Severe/critical COVID-19 • Comorbidity • High ECOG PS • Purine analog treatment • Acute leukemia/MDS |
|
| 38 | 4 hospitals in Europe: Spain, Northern-Italy and the Netherlands | 59 HM with COVID-19 | Retrospective cohort | HM patients died (33.9) | • | |
| 39 | Institute of Immunity and Transplantation, University College London | 55 HM with COVID-19 | Retrospective cohort | CPAP (34.5), endotracheal intubation (10.9) | HM patients died (34.5) | • CRP • Age • Ethnicity |
| 40 | New York Hospital System | 218 cancer patients with COVID-19 • 24.8% patients with HM |
Retrospective cohort | Cancer patients died (28) • HM patients died (37) |
• Older age • Multiple comorbidities • ICU support • D-dimer • Lactate dehydrogenase • Lactate |
|
| 41 | NHS Hospitals in England | 179 cancer patients with COVID-19 • 29.1% patients with HM |
Retrospective cohort | Cancer patients died (36.9) • HM patients died (48.1) |
• Age | |
| 42 | Gustave Roussy in France | 51 HM with COVID-19 | • Hypogammaglobulinemia • SARS-CoV-2 viremia |
AML, acute myeloid leukemia; CPAP, continuous positive airway pressure; CRP, C-reactive protein; ECOG PS, Eastern Cooperative Oncology Group Performance Status; MDS, myelodysplastic syndrome; MV, mechanical ventilation; NCATS, National Center for Advancing Translational Sciences; NHL, non-Hodgkin lymphoma; NHS, National Health Service; SCT, stem cell transplantion; SEMI, Sociedad Espanola de Medicina interna; US, United States.
Among the most common risk factors for an adverse outcome were, in the order of their frequency, age, comorbidities, active HM, type of HM, ICU stay, mechanical ventilation, and severe COVID-19.8,11-16,20,22,26,29,30,37,39,42 In a pooled meta-analysis, the estimated risk of death was 34% (95% confidence interval [CI], 28-39; N = 3240) in patients with HM with COVID-19.
The analysis of individual patient trajectories demonstrated shifting age and sex profiles of hospitalized patients and large-scale fluctuations in patient mortality with the ongoing progression of the pandemic.43 The results suggest that in HM patient vaccination, more frequent testing with identification of less-symptomatic patients and usage of COVID-19–directed interventions may have improved outcome.44
The SARS-CoV-2 viral load as assessed by cycle threshold (CT) values from reverse transcriptase-polymerase chain reaction (RT-PCR) assays is significantly higher in patients with HM (CT = 25.0) than in patients without HM (CT = 29.2; P = .0039). This seems to apply particularly to those who had received chemotherapy or targeted therapies.45 In a retrospective observational study of patients with HM, median time to RT-PCR negativity for SARS-CoV-2 was 17 days (range, 7-49 days).26 Several case reports of immunocompromised patients indicate that prolonged viral shedding may lead to genomic evolution of the virus with emergence of new variants.46-48
Following SARS-CoV-2 infection, Abdul-Jawad et al49 demonstrated that patients with HM had delayed or negligible seroconversion, prolonged shedding, and sustained immune dysregulation compared with patients with solid cancer. RNA persistence (as detected by nasopharyngeal swab tests) beyond 20 days was seen in 60% of patients with HM compared with only 35% of patients with solid cancer. Thus, although patients with solid cancer, including those with advanced disease, do not seem at higher risk of SARS-CoV-2–associated immune dysregulation compared with the general population, patients with HM show complex immunologic consequences of SARS-CoV-2 exposure.
An immunologic characterization with systematic quantification of different cell types corresponding to patients with COVID-19 showed significantly decreased percentages of classical monocytes, immune-regulatory natural killer cells, double-positive T cells, and B cells for patients with HM compared with patients with COVID-19 without HM.50,51 These data emphasize the significant alterations in the relative distribution of specific innate and adaptive cell types in patients with HM, possibly compromising an initial response to COVID-19.
A prospective study monitored the kinetic of immune response to SARS-CoV-2 in 45 patients with HM. Antibody levels (Ab) to the SARS-CoV-2 nucleocapsid (N) and spike (S) protein were measured at +1, +3, and +6 months after nasal swabs became PCR negative.52 Mean anti-N and anti-S Ab levels were similar between patients with HM and controls and shared the same behavior, with anti-N Ab levels declining at +6 months and anti-S Ab levels remaining stable. However, seroconversion rates both for anti-N and anti-S Abs and at all time points were significant lower in patients with HM than in controls. All rituximab-pretreated patients failed to produce anti-N and anti-S Abs.
A small case series of 25 patients with HM confirmed the short lasting protection with declination of antibody titers from 4 months after COVID-19.53
The Hematology Alliance on COVID‐19 (ITA-HEMA-COV) project (NCT04352556) investigated patterns of seroconversion in a large case series of 237 SARS-CoV-2–infected patients with HM.54 Overall, 69% of patients had detectable immunoglobulin G (IgG) SARS-CoV-2 serum antibodies. In a multivariable logistic regression analysis, chemoimmunotherapy (odds ratio, 3·42; 95% CI, 1·04-11·21; P = .04] was associated with a lower rate of seroconversion, indicating that treatment-mediated immune dysfunction represents a main driver of impaired immunogenicity. Smaller case series confirmed the impaired immune response to SARS-CoV-2 in patients with HM and reported a range of seroconversion of 16.6% to 84%.53,55
Evaluating cellular immune response, Bilich et al56 demonstrated impaired preexisting and newly generated CD4 T-cell responses to SARS-CoV-2 in patients with HM. In this study, patients with HM presented with reduced prevalence of preexisting SARS-CoV-2 cross-reactive CD4+ T-cell responses and signs of T-cell exhaustion compared with patients with solid cancer or healthy volunteers. The intensity, expandability, and diversity of SARS-CoV-2 T-cell responses were profoundly reduced and a potential determinant for a dismal outcome of COVID-19 in patients with HM.
Lacking T-cell immunity even in the setting of humoral response was demonstrated in the prospective monocentric study of specific viral immune responses induced by SARS-CoV-2 (COV-CREM) evaluating 39 SARS-CoV-2–infected patients with cancer, including 11 patients with HM.57 Only 36.4% of patients with HM exhibited T-cell responses against at least 1 of the SARS-CoV-2 proteins (S, M, or N). Of note, 2 patients without peripheral SARS-CoV-2–specific T cells had prolonged virus RNA detection after symptom resolution. The lack of T cell responses suggests that patients with HM fail to mount a protective T cell response. Therefore, a specific immunoglobulin monitoring alone may not be sufficient to characterize anti–SARS-CoV-2 immunity.
Higher rates of SARS-CoV-2–specific T cells (77%) were reported in an observational study of 100 patients with HM who were hospitalized for COVID-19. Flow cytometric and serologic analyses demonstrated that their B-cell response was impaired, and levels of SARS-CoV-2–specific antibodies were reduced compared with patients with solid cancer.58 Higher numbers of CD8 T cells correlated with an improved survival, including patients treated with anti-CD20 antibodies.
Vaccination
In 2020, several effective vaccines against SARS-CoV-2 have become available.59-62 More than 4 billion persons have been vaccinated since then. There is a clear consensus that these vaccinations are helpful to prevent hospitalizations and deaths after SARS-CoV-2 infections for all variants known to date.63
COVID-19 vaccination is particularly recommended in immunocompromised patients. However, there is only limited information on vaccine safety and efficacy for patients with HM, as most trials (eg, the registrational trials for mRNA-1273 [Moderna COVID-19 vaccine] and ChAdOx1 nCoV-19/AZD1222 [University of Oxford, AstraZeneca COVID-19 vaccine] have excluded patients with cancer).60,61 The phase 3 trial of BNT162b2 (Pfizer-BioNTech COVID-19 vaccine) and of Ad26.COV2.S (Janssen/Johnson & Johnson COVID-19 vaccine) enrolled only 4% and 0.5% of patients with cancer, respectively.59,62
It is important to note that many anticancer therapies are immunosuppressive. In particular, anti-CD20 antibodies may result in a prolonged depletion of normal B cells. This inevitably impairs the humoral response, and patients may fail to respond not only to influenza vaccines but also to other common vaccines.64
Patients with HM display the most pronounced impairment of SARS-CoV-2 cross-reactive CD4 T cells in parallel with highest expression of programmed cell death protein 1 on CD4 T cells.56 As opposed to anti-CD20 antibody treatment, programmed cell death protein 1 blockade (immune checkpoint treatment) may therefore enhance vaccination response.
That treatment modality may impact the vaccination response was shown by an evaluation of seroconversion rates against SARS-CoV-2 spike protein after US Food and Drug Administration (FDA)-approved COVID-19 vaccines.65 Although patients with solid tumors had adequate immune response in 98%, this response was only 85% in patients with HM and was particularly impaired in patients having received immunosuppressive therapies such as anti-CD20 therapies (70%) and stem cell transplantation (73%). As previously speculated, patients receiving immune checkpoint inhibitor therapy demonstrated high seroconversion rates after vaccination (97%). Patients with prior COVID-19 infection demonstrated higher antispike IgG titers after vaccination.
A report on quantitative serologic responses and early clinical outcome in a cohort of 885 patients with HM who had received 1 and 2 doses of BNT162b2 demonstrated that both anti-CD20 therapies and treatment with Bruton's tyrosine kinase inhibitor (BTKi), ruxolitinib, and venetoclax were associated with strongly reduced or absent antibody responses.66 Patients on kinase inhibitor treatments or after an hematopoietic stem-cell transplantation or systemic chemotherapy more than 6 months before the first dose of vaccine had good antibody responses (Table 2). Severe breakthrough infections were reported in 9 (1%) of 885 fully vaccinated patients (6 required supplemental oxygen and 3e died of COVID-19 pneumonitis). Six (67%) patients with breakthrough infection did not seroconvert after the second SARS-CoV-2 immunization.
Table 2.
COVID-19 vaccines in patients with hematologic malignancy: summary of studies evaluating the efficacy of COVID-19 vaccines in >10 patients with hematologic malignancy
| Reference | Patient population | Vaccine type/ vaccine regimen | Endpoint | Results |
|---|---|---|---|---|
| 65 | 200 cancer patients | FDA-approved COVID-19 vaccines | Seroconversion | |
| Overall | 94% | |||
| Type of vaccine | ||||
| BNT162b2 | 95% | |||
| mRNA-1273 | 94% | |||
| Ad26.COV2.S | 85% | |||
| Type of cancer therapy | ||||
| Anti-CD20 | 70% | |||
| Stem cell transplant | 73% | |||
| CAR-T cell | 0 | |||
| Hormonal | 100% | |||
| Immune checkpoint inhibitor | 97% | |||
| 71 | 80 HM patients | Double-dose BNT162b2 | Seroconversion | |
| Type of treatment | ||||
| CAR-T cell | 36% | |||
| Allogeneic stem cell transplant | 75% | |||
| ELISpot positivity | ||||
| Type of treatment | ||||
| CAR-T cell | 50% | |||
| Allogeneic stem cell transplant | 19% | |||
| 72 | 32 HM patients | Double-dose BNT162b2 and Ad26-COV2.S boost | Seroconversion | |
| Overall | 31% | |||
| Type of HM | ||||
| CLL or lymphoma | 16.7% | |||
| 73 | 270 HM patients | Double-dose mRNA-1273 | Seroconversion | |
| Overall | 76.3% | |||
| Treatment status | ||||
| Off-therapy >6 mo | 91.7% | |||
| On-therapy/off-therapy <6 mo | 63.7% | |||
| Treatment-naïve | 96.7% | |||
| Type of treatment | ||||
| BTK | 86.2% | |||
| IMIDs | 100% | |||
| Anti-CD20 alone | 18.5% | |||
| CHI ±anti-CD20 | 27.8% | |||
| Cellular response | ||||
| Overall | 79% | |||
| Treatment status | ||||
| Off-therapy >6 mo | 85.7% | |||
| On-therapy/off-therapy < 6 mo | 78% | |||
| Treatment-naïve | 86.7% | |||
| Type of treatment | ||||
| BTK | 81.5% | |||
| IMIDs | 92.3% | |||
| Anti-CD20 alone | 80% | |||
| CHI ±anti-CD20 | 50% | |||
| 69 | 49 HM patients | Booster BNT162b2 or mRNA-1273 | Seroconversion | |
| Overall | 65% | |||
| Treatment status | ||||
| Off-treatment >24 mo | 92.9% | |||
| Completed anti-CD20 | 42.9% | |||
| Prior anti-CD20 <7 mo | 71.4% | |||
| BTK | 61.1% | |||
| 81 | 100 HM patients | Double-dose BNT162b2 or mRNA-1273 | Seroconversion | |
| Overall | 49% | |||
| Treatment status | ||||
| Anti-CD20 <12 mo prior | 26% | |||
| After booster dose | 41.7% | |||
| 75 | 160 HM patients | FDA-approved COVID-19 vaccines | Seroconversion Overall | 39.4% |
| Treatment status | ||||
| B-cell/plasma cell-depleting mAb | 29% | |||
| Active disease | 27% | |||
| In remission | 49% | |||
| Watch & wait | 67% | |||
| CHI >12 mo prior | 69% | |||
| CHI < 12 mo prior | 24% | |||
| 70 | 239 HM patients | Double-dose BNT162b2 | Seroconversion | |
| Overall | 47% | |||
| Cellular response | Cellular response | |||
| Overall | 53% | |||
| 83 | 123 HM patients | BNT162b2 | Seroconversion | |
| 1 dose | 43.4% | |||
| Double-dose | 71.4% | |||
| 76 | 58 HM patients | Single dose BNT162b2 or AZD1222 | Neutralizing antibodies | |
| ≥30% | 14% | |||
| ≥50% | 5% | |||
| 77 | 102 HM patients | Single dose BNT162b2 or mRNA-1273 | Seroconversion | |
| Overall | 61.8% | |||
| Treatment | ||||
| Anti-CD20 <12 mo | 5.9% | |||
| Anti-CD20 >12 mo | 63.6% | |||
| 66 | 857 HM patients | Single-dose and double-dose BNT162b2 | Median anti-S IgG level (AU/mL) | |
| Overall | 6 961 | |||
| Age | ||||
| >60 y | 1 140 | |||
| Treatment | ||||
| Treatment-naïve | 5 761 | |||
| Ruxolitinib | 10 | |||
| BTKi | 0 | |||
| Anti-CD20 | 17 | |||
| Hydroxycarbamide | 1 825 | |||
| IMID | 679 | |||
| TKIs | 10 537 | |||
| Anagrelide/interferon | 6 927 | |||
| Auto SCT | 6 203 | |||
| Allogeneic SCT | 6 304 | |||
| 78 | 315 HM patients | Double-dose BNT162b2 | Seroconversion | |
| Overall | 75% | |||
| HM subtype | ||||
| Aggressive NHL | 71% | |||
| Indolent NHL | 60% | |||
| Hodgkin lymphoma | 94% | |||
| Multiple myeloma | 76% | |||
| CLL | 47% | |||
| Acute leukemia | 80% | |||
| MDS | 94% | |||
| MPN | 84% | |||
| CML | 91% | |||
| 82 | 1 445 HM patients | Double-dose BNT162b2 or mRNA-1273 | Seroconversion | |
| Overall | 75% | |||
| HM subtype | ||||
| ALL | 88.2% | |||
| AML | 91.2% | |||
| Burkitt lymphoma | 100% | |||
| CLL | 64.2% | |||
| CML | 97.1% | |||
| Diffuse large B cell lymphoma | 78.8% | |||
| Follicular lymphoma | 77.6% | |||
| Hairy cell leukemia | 100% | |||
| Hodgkin lymphoma | 98.5% | |||
| Mantle cell lymphoma | 44.4% | |||
| Marginal zone lymphoma | 61.8% | |||
| MDS/MPN | 97.1% | |||
| Multiple myeloma | 95.1% | |||
| Primary CNS lymphoma | 50% | |||
| Primary mediastinal large B-NHL | 100% | |||
| Smoldering myeloma | 100% | |||
| T cell lymphoma | 84.6% | |||
| Waldenstrom macroglobulinemia | 74.2% | |||
| 79 | 585 cancer patients | Double-dose BNT162b2 or AZD1222 | Seroconversion | |
| Overall | 78% | |||
| Cancer subtype | ||||
| HM | 59% | |||
| Solid cancer | 85% | |||
| 85 | 132 HM patients | BNT162b2 | Neutralizing SARS-CoV-2 antibodies inhibition titer | |
| Median | 32.5% | |||
| ≥30% | 50.8% | |||
| ≥50% | 43.9% |
AML, acute myeloid leukemia; CAR-T, chimeric antigen receptor; CHI, chemoimmunotherapy; CLL, chronic lymphocytic leukemia; CML, chronic myeloid leukemia; ELISpot, enzyme-linked immunospot; IMIDs, immunomodulatory imide drugs; MDS, myelodysplastic syndrome; MPN, myeloproliferative disease; NHL, non-Hodgkin lymphoma; SCT, stem cell transplantion; TKI, tyrosine kinase inhibitor.
Several other prospective studies confirmed the low antibody response after SARS-CoV-2 vaccination in patients with HM (Table 2), particularly in patients pretreated with rituximab. These studies also reported cases of breakthrough infections in partially or completely vaccinated patients.65-79
A comprehensive workup of SARS-CoV-2 breakthrough infections among partially or completely vaccinated patients with HM was provided by an open web-based registry (EPICOVIDEHA) of the European Hematology Association Infectious Diseases Working Party.67 Most patients with breakthrough infections had lymphoproliferative disorders (>80%), received an active treatment within 3 months before vaccination (68.1%), were males (61.1%), and were >50 years of age (85.5%). Eighty-seven patients (77%) were considered fully vaccinated, and COVID-19 was diagnosed more than 2 weeks after the second vaccination. Overall, 79 (60.4%) patients had a severe or critical infection. Seventy-five patients (66.4%) were admitted to the hospital, with 16 (21.3%) to an ICU, and 10 of 16 required mechanical ventilation. At 30 days after COVID-19 diagnosis, the overall mortality rate was 12.4% (N = 14). No statistical differences were observed between partially or fully vaccinated patients (15.4% vs 11.5%; P = .734) and patients achieving a serologic response vs nonresponders (13.3% vs 15.6%; P = 1). Multivariable analysis showed that the only factor independently related to the risk of death was age.
The first prospective evaluation of a booster dose was reported in a well-described cohort of patients with cancer (all but 1 with HM) and demonstrated a high booster-induced seroconversion of 56%, even in patients that were previously treated for their malignancy.80 Prior BTKi or anti-CD20 treatment was associated with inferior postbooster seroconversion and anti-S IgG titers. All patients remaining seronegative after the booster vaccination had B-cell malignancies. Of the seronegative patients, booster-induced T-cell responses were detectable in 80% of evaluable patients.
Two observational studies confirmed an improvement of the immune response after a booster dose of COVID-19 vaccine in patients with HM, and 41.7% to 65% of patients seroconverted.69,81 Again, previous treatment with anti-CD20 antibodies had the strongest adverse impact on immunogenicity, whereas most patients treated with BTKi were able to seroconvert after a third booster vaccination.80
When comparing different HM subtypes, patients with chronic lymphocytic leukemia (CLL) and indolent lymphoma had the lowest seroconversion rate after COVID-19 vaccination.78,82 In contrast, the highest seroconversion rates in descending order were reported in patients with smoldering myeloma, hairy cell leukemia, Hodgkin lymphoma, myelodysplastic syndrome, chronic myeloid leukemia, myeloproliferative disorders, acute myeloid leukemia, multiple myeloma, acute lymphoid leukemia, T-cell lymphoma, and aggressive lymphoma.
Predictive markers other than the type of HM (lymphoma or chronic lymphocytic leukemia) were the levels of different cell types in the peripheral blood (T cells, B cells, neutrophils, natural killer cells, and monocytes), IgG count, and clinical and treatment characteristics (male sex, age, and B-cell targeting treatment within 12 months before vaccination).70,78,83,84
Results of several studies indicate that the time from last rituximab infusion (<6 months, <12 months) is associated with lower rates of serologic conversion,66,69,70,73,75,79,81 and hardly any HM patients treated with rituximab within 6 months before vaccination had detectable neutralizing antibodies.85 As up to 80% of anti-CD20–treated patients with HM were able to mount a specific T-cell response,73 it is possible that SARS-CoV2 vaccines may generate a cellular protection even at the time of anti-CD20 antibody induced B-cell depletion.
After a 2-dose vaccination, the antibody persistence was reported to hold up to 6 months in healthy individuals.86 The duration of protection from reinfection and severe disease after booster vaccination is currently the subject of extensive debate. Cellular immunity might provide long-term protection (in contrast to waning humoral immunity), and as recently demonstrated, even T-cell response to the Omicron variant is preserved in most vaccinated individuals, albeit with reduced reactivity in approximately 20% of individuals.87
Of note, vaccination with initial mRNA-1273 or Ad26.CoV2.S vaccination, as well as mRNA-1273 booster compared with BNT162b2, yielded higher titers of antiviral antibodies in patients with HM, unlike the nearly identical efficacy of mRNA vaccines in healthy volunteers.82 Differences in the amount of spike mRNA, differences in the exact coding sequence of the mRNA or lipid composition of the vaccines, and different dosing schedules may alter immunogenicity of the vaccines in patients with HM.80,82
Many countries now offer a fourth dose of COVID-19 vaccine to special risk groups.88 The first case series of solid-organ transplant recipients reports successful second boosting in up to 50% of negative and in 100% of patients with low-positive titer.89 Data on patients with HM have not been reported. However, a second booster vaccination should be offered to all patients with hematologic malignancy.
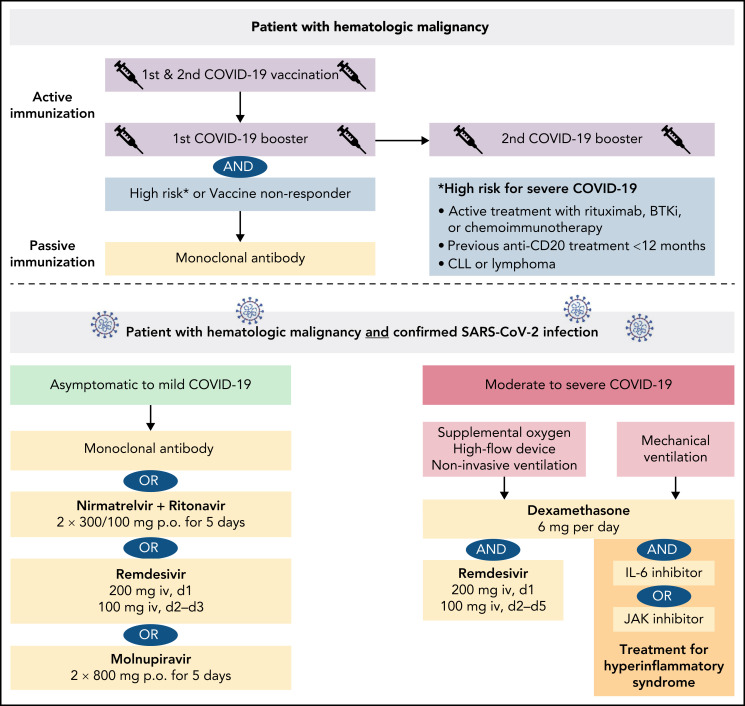
In summary, the vaccine-induced immunity is significantly lower in patients with lymphoid malignancies and patients receiving active B cell–depleting treatment, whereas vaccine-induced immunity in patients with myeloid malignancies or Hodgkin lymphoma is hardly impaired. Hematologic patients with a deficient vaccine response need other protective measures to prevent or minimize the risk of breakthrough infections, as discussed in the following chapter of antiviral therapies (Figure 1).
Figure 1.
Management of a patient with hematologic malignancy during the pandemic.
Antiviral therapies
Because a large subgroup of patients with HM does not respond adequately to COVID-19 vaccination, early therapeutic or prophylactic measures are needed to prevent severe COVID-19. A large variety of options have been tested over the last 2 years. In terms of the current dominating Omicron variant, the antiviral drugs nirmatrelvir-ritonavir, remdesivir, and molnupiravir retain their efficacy against Omicron compared with earlier variants of concern.90-92
Nirmatrelvir/ritonavir
The oral protease inhibitor nirmatrelvir inhibits the SARS-CoV-2 3CL protease that is critical for viral replication.93 Nirmatrelvir is administered in combination with ritonavir, a prodrug to inhibit the metabolism of nirmatrelvir. As a result, relevant CYP3A4 drug interactions should be noted (eg, kinase inhibitor, venetoclax). The evaluation of protease inhibition for COVID-19 in high-risk patients (EPIC-HR) phase 2/3 trial evaluating nirmatrelvir/ritonavir in high-risk patients treated within 3 days of COVID-19–related symptom onset demonstrated a relative risk reduction of 90% for hospitalization or death compared with placebo, and the viral load was lower at day 5 of treatment.94 Nirmatrelvir/ritonavir received emergency use authorization for the treatment of mild-to-moderate COVID-19 in SARS-CoV-2–positive patients at high risk for severe COVID-19.
Remdesivir
The nucleotide analog remdesivir was the first approved drug for the treatment of SARS-CoV-2. A 10-day course of remdesivir was superior to placebo in shortening the time to recovery in hospitalized patients with lower respiratory tract infections but did not reduce mortality.95 The randomised, double-blind, placebo-controlled phase 3 Study GS-US-540-9012 (PINETREE) evaluated the efficacy of a 3-day course of remdesivir in high-risk, nonhospitalized patients with COVID-19, including a small subgroup of immunocompromised patients (4.1%).96 Early remdesivir treatment resulted in an 87% lower risk of hospitalization or death than placebo (hazard ratio, 0.13; 95% CI, 0.03-0.59; P = .008). Remdesivir received emergency use authorization for the treatment of COVID-19 patients with pneumonia requiring supplemental oxygen (low- or high-flow oxygen or other noninvasive ventilation at the start of treatment).
Molnupiravir
Molnupiravir is an oral, small-molecule antiviral prodrug that is active against SARS-CoV-2 by increasing the frequency of viral RNA mutations and impairing SARS-CoV-2 replication.97 MOVe-OUT is a double-blind, placebo-controlled phase 3 trial that evaluated molnupiravir therapy starting within 5 days after onset of symptoms in nonhospitalized, unvaccinated patients with confirmed SARS-CoV-2 (including 2.2% patients with active cancer) and demonstrated a relative risk reduction of hospitalization or death of 30% (relative risk, 0.70; 95% CI: 0.49-0.99).98 Because of the mechanism of action, an increased teratogenicity is of concern, particularly in younger, childbearing, pregnant, and lactating patients. Molnupiravir is indicated for the treatment of COVID-19 in patients with HM who do not require supplemental oxygen to reduce the risk of progression to severe COVID-19.
Convalescent plasma
Virus-neutralizing antibodies contained in convalescent plasma of recovered individuals may be used for the therapy of immunocompromised patients with SARS-CoV-2. Several observational studies have demonstrated reduced symptoms and mortality in patients with COVID-19 after convalescent plasma transfusion.99-101 Although case series showed some effectiveness among immunocompromised patients with HM, large clinical trials did not find evidence for therapeutic effects of convalescent plasma.102-109 Therefore, convalescent plasma therapy represents an option for individual patients with HM but should not be applied routinely.
Dexamethasone
Early use of oral or IV dexamethasone (at a dose of 6 mg once daily) for up to 10 days in hospitalized patients with COVID-19 resulted in a lower mortality among patients on respiratory support (oxygen or mechanical ventilation) as evaluated with the Randomised Evaluation of COVID-19 Therapy Study (RECOVERY).110 Dexamethasone is indicated in the treatment of COVID-19 in adults who require supplemental oxygen therapy.
Monoclonal antibodies
Monoclonal antibodies directed to the S protein can neutralize the ability of the virus to bind and fuse with the target host cell. The neutralizing reactivity of FDA-approved and investigational therapeutic monoclonal antibodies against Omicron and other variants of concern was evaluated recently.91,111 In summary, several monoclonal antibodies (etesevimab-bamlanivimab, imdevimab-casirivimab) lose their neutralizing activity and are not effective against Omicron. Substantial inhibitory activity was demonstrated for tixagevimab-cilgavimab (although with reduced neutralizing capacity compared with Beta or Gamma) and for sotrovimab, albeit to a much lesser extent. Extended studies including antigenic characterization of the emerging Omicron sublineages demonstrated that in 17 of 19 neutralizing monoclonal antibodies tested (including sotrovimab), BA.2 exhibited marked resistance.112 Only the recently authorized monoclonal antibody bebtelovimab could adequately cover all sublineages of the Omicron variant.
Sotrovimab
The neutralizing antibody sotrovimab binds to the receptor-binding motif that engages the ACE2 receptor and demonstrated activity against several variants of concern including Alpha, Beta, Gamma, Delta, and Lambda.113 The COVID-19 Monoclonal Antibody Efficacy Trial–Intent to Care Early (COMET-ICE) demonstrated that sotrovimab reduces the risk of severe COVID-19 in high-risk ambulatory patients with mild-to-moderate COVID-19 (relative risk reduction, 85%; 97.24% CI, 44-96; P = .002).114 Following these results, sotrovimab has been approved for the treatment of COVID-19 in patients who do not require oxygen supplementation but are at increased risk of progressing to severe COVID-19. Sotrovimab retained activity against Omicron BA.1 sublineages, but its activity against BA.2 has remarkably dropped.112 Following these findings, the FDA has limited use of sotrovimab to regions where the Omicron BA.2 subvariant is not the dominant subvariant.
Tixagevimab and cilgavimab
The phase 3 double-blind, placebo-controlled trial for pre-exposure prophylaxis of COVID-19 in (PROVENT) (#NCT04723394) evaluated AZD7442, a combination of 2 long-acting antibodies, tixagevimab and cilgavimab, to prevent symptomatic COVID-19 including patients with a poor vaccine response. The data have not been published, but a press release stated that tixagevimab/cilgavimab reduced the risk of developing symptomatic COVID-19 by 83% compared with placebo.115 The combination is authorized for the emergency use as pre-exposure prophylaxis for prevention of COVID-19 in moderately to severely immunocompromised patients or for whom an active COVID-19 vaccination is not possible.116 This includes patients with active HM, patients with HM receiving immunosuppressive therapy, and transplant recipients. The FDA has amended its Emergency Use Authorization to increase the recommended dose of each drug from 150 to 300 mg. The revision was based on in vitro data showing that tixagevimab/cilgavimab retain a greater degree of neutralizing activity against the BA.2 Omicron variant (5.4-fold reduction vs the ancestral virus).117 The duration of protection is estimated to be 9 to 12 months and, in contrast to other monoclonal antibodies, this antibody-cocktail is given by intramuscular administration.
Bebtelovimab
The FDA has granted emergency approval for LY-CoV1404 (bebtelovimab), as the antibody retains potent neutralizing activity against both Omicron sublineages BA.1 and BA.2 in pseudovirus neutralization studies.112 However, clinical data evaluating bebtelovimab alone or in combination in patients with mild to moderate COVID-19 are still pending (#NCT04634409).
Impact of Omicron SARS-COV-2 variant
Epidemiologic data from Africa showed a decoupling of hospitalizations and deaths from infections while Omicron was circulating.118 The first population-based study of patients with CLL with COVID-19 from eastern Denmark evaluated the severity and outcome before and after Omicron predominance.119 High ICU admission rates before Omicron emergence might reflect the protection by booster vaccination and improved care for patients with COVID-19 such as full implementation of early antiviral treatment with monoclonal antibodies and treatment with remdesivir of hospitalized patients. Albeit the numbers of patients reported are small, the survival rate decreased with the emergence of ο BA.2 sublineage, indicating an impaired efficacy of sotrovimab against Omicron available at that time.
Psychologic distress
Patients with HM often report increased psychologic stress levels, as they are part of a population at increased risk of contracting COVID-19. Evaluation of the psychologic status of outpatients with HM receiving infusional therapies or other antineoplastic treatments demonstrated an increased level of anxiety and depression. Up to 36% of patients with HM fulfilled the criteria for a posttraumatic stress disorder.120 Women and younger patients were found to be more vulnerable to anxiety and posttraumatic disorders. Concerns about the impact of COVID-19 on cancer management were significantly associated with fear of cancer recurrence among responder in remission.121 Other stressors were social distancing and limited social interactions induced by the pandemic.122
Summary: management of patients with hematologic malignancy during the SARS-COV-2 pandemic
For patients with HM, the current SARS-CoV-2 pandemic represents a particular challenge for at least 2 reasons. First, their immune system may be impaired by the interaction of cancer cells with different immune cell subsets, inducing a state of anergy. Second, the antineoplastic therapies themselves, and in particular anti-CD20 antibodies or chemotherapies, act as potent immunosuppressive agents. As a consequence, patients with HM have an increased risk for a severe course of COVID-19, with a hospitalization rate of more than 50% and a case fatality rate of approximately 30%. Advanced age, comorbidities, and type of HM seem to be additional risk factors.
Patients with HM show short-lasting protection after SARS-CoV-2 infection with detection of specific antibodies for less than 4 months and signs of T-cell exhaustion, indicating a lack of long-term immunity and an increased risk of reinfection.
Active immunization by vaccination remains an important element of protection for these patients. As the recent SARS-CoV-2 variants of concerns have increased their transmissibility, a first and second booster vaccination should be given to all patients with HM regardless of serologic results.
As the protection by COVID-19 vaccines is significantly reduced in patients with lymphoid malignancies or patients receiving B cell–directed treatments, preventive passive immunization with monoclonal antibodies (pre-exposure prophylaxis) is another milestone in containment of the pandemic and should be offered to all such patients with HM and to vaccine nonresponders.
Antiviral drugs and monoclonal antibodies for early treatment of COVID-19 have become available and should be given to all SARS-CoV-2–infected patients with HM to prevent severe or fatal courses. The treatment selection is based on efficacy against the current dominating SARS-CoV-2 variants, potential contraindications, drug interactions, and availability in different health care systems.
Moreover, we feel that it is important to establish specific programs and registries at a national and global level for patients with HM during this historic pandemic because they represent a particularly vulnerable group of patients with regard to COVID-19 in our society.
Supplementary Material
Authorship
Contribution: P.L. performed a systematic review and wrote an initial draft; M.H. conceived, reviewed, and edited the manuscript; and both authors approved the final version.
Conflict-of-interest disclosure: P.L. research funding, travel grants and honoraria by AbbVie, F. Hoffmann-LaRoche, Janssen-Cilag and AstraZeneca. M.H. consultant or advisory board member, honoraria and research support by AbbVie, Amgen, Celgene, F. Hoffmann-LaRoche, Gilead, Janssen-Cilag, and Mundipharma.
Correspondence: Petra Langerbeins, Department I of Internal Medicine, Center for Integrated Oncology Aachen Bonn Cologne Duesseldorf, German CLL Study Group, CECAD Cluster of Excellence, University of Cologne, Kerpener Str 62, 50937 Cologne, Germany; e-mail: petra.langerbeins@uk-koeln.de.
REFERENCES
- 1.Kidd M, Richter A, Best A, et al. S-variant SARS-CoV-2 lineage B1.1.7 is associated with significantly higher viral loads in samples tested by ThermoFisher TaqPath polymerase chain reaction. J Infect Dis. 2021;223(10):1666-1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Volz E, Mishra S, Chand M, et al. ; COVID-19 Genomics UK (COG-UK) consortium . Assessing transmissibility of SARS-CoV-2 lineage B.1.1.7 in England. Nature. 2021;593(7858):266-269. [DOI] [PubMed] [Google Scholar]
- 3.Zhou D, Dejnirattisai W, Supasa P, et al. Evidence of escape of SARS-CoV-2 variant B.1.351 from natural and vaccine-induced sera. Cell. 2021;184(9):2348-2361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Faria NR, Mellan TA, Whittaker C, et al. Genomics and epidemiology of the P.1 SARS-CoV-2 lineage in Manaus, Brazil. Science. 2021;372(6544):815-821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sheikh A, McMenamin J, Taylor B, Robertson C; Public Health Scotland and the EAVE II Collaborators . SARS-CoV-2 Delta VOC in Scotland: demographics, risk of hospital admission, and vaccine effectiveness. Lancet. 2021;397(10293):2461-2462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kandeel M, Mohamed MEM, Abd El-Lateef HM, Venugopala KN, El-Beltagi HS. Omicron variant genome evolution and phylogenetics. J Med Virol. 2021;94(4):1627-1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.He W, Chen L, Chen L, et al. COVID-19 in persons with haematological cancers. Leukemia. 2020;34(6):1637-1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pagano L, Salmanton-García J, Marchesi F, et al. ; EPICOVIDEHA working group . COVID-19 infection in adult patients with hematological malignancies: a European Hematology Association Survey (EPICOVIDEHA). J Hematol Oncol. 2021;14(1):168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sharafeldin N, Bates B, Song Q, et al. Outcomes of COVID-19 in patients with cancer: report from the national COVID cohort collaborative (N3C). J Clin Oncol. 2021;39(20):2232-2246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grivas P, Khaki AR, Wise-Draper TM, et al. Association of clinical factors and recent anticancer therapy with COVID-19 severity among patients with cancer: a report from the COVID-19 and Cancer Consortium. Ann Oncol. 2021;32(6):787-800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yigenoglu TN, Ata N, Altuntas F, et al. The outcome of COVID-19 in patients with hematological malignancy. J Med Virol. 2021;93(2):1099-1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Basquiera AL, García MJ, Martinez Rolón J, et al. Clinical characteristics and evolution of hematological patients and COVID-19 in Argentina: a report from the Argentine Society of Hematology. Medicina (B Aires). 2021;81(4):536-545. [PubMed] [Google Scholar]
- 13.Altuntas F, Ata N, Yigenoglu TN, et al. ; Turkish Ministry of Health, Hematology Scientific Working Group . COVID-19 in hematopoietic cell transplant recipients. Bone Marrow Transplant. 2021;56(4): 952-955. [DOI] [PubMed] [Google Scholar]
- 14.Ljungman P, de la Camara R, Mikulska M, et al. COVID-19 and stem cell transplantation; results from an EBMT and GETH multicenter prospective survey. Leukemia. 2021;35(10):2885-2894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Passamonti F, Cattaneo C, Arcaini L, et al. ; ITA-HEMA-COV Investigators . Clinical characteristics and risk factors associated with COVID-19 severity in patients with haematological malignancies in Italy: a retrospective, multicentre, cohort study. Lancet Haematol. 2020;7(10):e737-e745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Piñana JL, Martino R, García-García I, et al. ; Infectious Complications Subcommittee of the Spanish Hematopoietic Stem Cell Transplantation and Cell Therapy Group (GETH) . Risk factors and outcome of COVID-19 in patients with hematological malignancies. Exp Hematol Oncol. 2020; 9(1):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Civriz Bozdağ S, Cengiz Seval G, Yönal Hindilerden İ, et al. Clinical characteristics and outcome of COVID-19 in Turkish hematological malignancy patients. Turk J Haematol. 2021;39(1):43-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584(7821):430-436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Suárez-García I, Perales-Fraile I, González-García A, et al. ; SEMI-COVID-19 Network . In-hospital mortality among immunosuppressed patients with COVID-19: analysis from a national cohort in Spain. PLoS One. 2021;16(8):e0255524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Levy I, Lavi A, Zimran E, et al. COVID-19 among patients with hematological malignancies: a national Israeli retrospective analysis with special emphasis on treatment and outcome. Leuk Lymphoma. 2021;62(14):3384-3393. [DOI] [PubMed] [Google Scholar]
- 21.Sharma A, Bhatt NS, St Martin A, et al. Clinical characteristics and outcomes of COVID-19 in haematopoietic stem-cell transplantation recipients: an observational cohort study. Lancet Haematol. 2021;8(3):e185-e193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gupta A, Desai N. Clinical profile and outcome of COVID-19 in haematological malignancies: experience from tertiary care centre in India. Ann Hematol. 2021;101(1):1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee LYW, Cazier JB, Starkey T, et al. ; UK Coronavirus Cancer Monitoring Project Team . COVID-19 prevalence and mortality in patients with cancer and the effect of primary tumour subtype and patient demographics: a prospective cohort study. Lancet Oncol. 2020;21(10):1309-1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang Q, Berger NA, Xu R. Analyses of risk, racial disparity, and outcomes among US patients with cancer and COVID-19 infection. JAMA Oncol. 2021;7(2):220-227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Assaad S, Zrounba P, Cropet C, Blay JY; ONCOVID-19 study Consortium . Mortality of patients with solid and haematological cancers presenting with symptoms of COVID-19 with vs without detectable SARS-COV-2: a French nationwide prospective cohort study. Br J Cancer. 2021;125(5):658-671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Borah P, Mirgh S, Sharma SK, et al. ; AIIMS Hematology Alumni Group . Effect of age, comorbidity and remission status on outcome of COVID-19 in patients with hematological malignancies. Blood Cells Mol Dis. 2021;87:102525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zorzi M, Guzzinati S, Avossa F, Fedeli U, Calcinotto A, Rugge M. SARS-CoV-2 infection in cancer patients: a population-based study. Front Oncol. 2021;11:730131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Russell B, Moss CL, Shah V, et al. ; Guy’s Cancer Real World Evidence . Risk of COVID-19 death in cancer patients: an analysis from Guy’s Cancer Centre and King’s College Hospital in London. Br J Cancer. 2021;125(7):939-947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cattaneo C, Daffini R, Pagani C, et al. Clinical characteristics and risk factors for mortality in hematologic patients affected by COVID-19. Cancer. 2020;126(23): 5069-5076. [DOI] [PubMed] [Google Scholar]
- 30.Čerňan M, Szotkowski T, Obr A, et al. COVID-19 in 96 patients with hematologic disease: the first single-center experience from the Czech Republic. Clin Lymphoma Myeloma Leuk. 2021;21(9):606-612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shah GL, DeWolf S, Lee YJ, et al. Favorable outcomes of COVID-19 in recipients of hematopoietic cell transplantation. J Clin Invest. 2020;130(12):6656-6667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shah V, Ko Ko T, Zuckerman M, et al. Poor outcome and prolonged persistence of SARS-CoV-2 RNA in COVID-19 patients with haematological malignancies; King’s College Hospital experience. Br J Haematol. 2020;190(5):e279-e282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tığlıoğlu P, Albayrak M, Tığlıoğlu M, et al. The outcome of COVID-19 in patients with hematological malignancy. J Med Virol. 2021;93(2):1099–1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jee J, Foote MB, Lumish M, et al. Chemotherapy and COVID-19 outcomes in patients with cancer. J Clin Oncol. 2020; 38(30):3538-3546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hinton R, Nesr G, Garnett C, et al. Improvement in mortality of hospitalized patients with hematological malignancies in the 2nd wave of COVID-19 in the UK: experience of a large London NHS trust. Leuk Lymphoma. 2021;63(1):227-230. [DOI] [PubMed] [Google Scholar]
- 36.Booth S, Willan J, Wong H, et al. Regional outcomes of severe acute respiratory syndrome coronavirus 2 infection in hospitalised patients with haematological malignancy. Eur J Haematol. 2020;105(4):476-483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Glenthøj A, Jakobsen LH, Sengeløv H, et al. SARS-CoV-2 infection among patients with haematological disorders: severity and one-month outcome in 66 Danish patients in a nationwide cohort study. Eur J Haematol. 2021;106(1):72-81. [DOI] [PubMed] [Google Scholar]
- 38.van Doesum J, Chinea A, Pagliaro M, et al. Clinical characteristics and outcome of SARS-CoV-2-infected patients with haematological diseases: a retrospective case study in four hospitals in Italy, Spain and the Netherlands. Leukemia. 2020;34(9):2536-2538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fox TA, Troy-Barnes E, Kirkwood AA, et al. Clinical outcomes and risk factors for severe COVID-19 in patients with haematological disorders receiving chemo- or immunotherapy. Br J Haematol. 2020; 191(2):194-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mehta V, Goel S, Kabarriti R, et al. Case fatality rate of cancer patients with COVID-19 in a New York Hospital System. Cancer Discov. 2020;10(7):935-941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bhogal T, Khan UT, Lee R, et al. Haematological malignancy and nosocomial transmission are associated with an increased risk of death from COVID-19: results of a multi-center UK cohort. Leuk Lymphoma. 2021;62(7): 1682-1691. [DOI] [PubMed] [Google Scholar]
- 42.Michot JM, Hueso T, Ibrahimi N, et al. Severe COVID-19 in patients with hematological cancers presenting with viremia. Ann Oncol. 2021;32(10):1297-1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lefrancq N, Paireau J, Hozé N, et al. Evolution of outcomes for patients hospitalised during the first 9 months of the SARS-CoV-2 pandemic in France: a retrospective national surveillance data analysis. Lancet Reg Health Eur. 2021;5:100087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Roeker LE, Eyre TA, Thompson MC, et al. COVID-19 in patients with CLL: improved survival outcomes and update on management strategies. Blood. 2021; 138(18):1768-1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Westblade LF, Brar G, Pinheiro LC, et al. SARS-CoV-2 viral load predicts mortality in patients with and without cancer who are hospitalized with COVID-19. Cancer Cell. 2020;38(5):661-671.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lynch M, Macori G, Fanning S, et al. Genomic evolution of SARS-CoV-2 virus in immunocompromised patient, Ireland. Emerg Infect Dis. 2021;27(9):2499-2501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Choi B, Choudhary MC, Regan J, et al. Persistence and evolution of SARS-CoV-2 in an immunocompromised host. N Engl J Med. 2020;383(23):2291-2293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tarhini H, Recoing A, Bridier-Nahmias A, et al. Long-term severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infectiousness among three immunocompromised patients: from prolonged viral shedding to SARS-CoV-2 superinfection. J Infect Dis. 2021;223(9):1522-1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Abdul-Jawad S, Baù L, Alaguthurai T, et al. Acute immune signatures and their legacies in severe acute respiratory syndrome coronavirus-2 infected cancer patients. Cancer Cell. 2021;39(2):257-275.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Maia C, Martín-Sánchez E, Garcés JJ, et al. Immunologic characterization of COVID-19 patients with hematological cancer. Haematologica. 2020;106(5):1457-1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kalicińska E, Szymczak D, Andrasiak I, et al. Lymphocyte subsets in haematological patients with COVID-19: multicentre prospective study. Transl Oncol. 2021; 14(1):100943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cattaneo C, Cancelli V, Imberti L, et al. Production and persistence of specific antibodies in COVID-19 patients with hematologic malignancies: role of rituximab. Blood Cancer J. 2021;11(9):151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Candoni A, Pizzano U, Fabris M, Curcio F, Fanin R. Seroconversion and kinetic of anti SARS-COV-2 antibodies in 25 patients with hematological malignancies who recovered from SARS-COV-2 infection. Hematol Oncol. 2021;39(3):428-431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Passamonti F, Romano A, Salvini M, et al. ; ITA-HEMA-COV Investigators . COVID-19 elicits an impaired antibody response against SARS-CoV-2 in patients with haematological malignancies. Br J Haematol. 2021;195(3):371-377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bird PW, Badhwar V, Kennedy B, Ladani S, Tang JW. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) seroconversion in hematology-oncology patients. J Med Virol. 2021;93(7): 4585-4591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bilich T, Roerden M, Maringer Y, et al. Preexisting and post-COVID-19 immune responses to SARS-CoV-2 in patients with cancer. Cancer Discov. 2021;11(8): 1982-1995. [DOI] [PubMed] [Google Scholar]
- 57.Mansi L, Spehner L, Daguindau E, et al. Study of the SARS-CoV-2-specific immune T-cell responses in COVID-19-positive cancer patients. Eur J Cancer. 2021;150:1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bange EM, Han NA, Wileyto P, et al. CD8+ T cells contribute to survival in patients with COVID-19 and hematologic cancer. Nat Med. 2021;27(7):1280-1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Polack FP, Thomas SJ, Kitchin N, et al. ; C4591001 Clinical Trial Group . Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med. 2020;383(27): 2603-2615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Baden LR, El Sahly HM, Essink B, et al. ; COVE Study Group . Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med. 2021;384(5):403-416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Voysey M, Clemens SAC, Madhi SA, et al. ; Oxford COVID Vaccine Trial Group . Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: an interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet. 2021;397(10269):99-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sadoff J, Gray G, Vandebosch A, et al. ; ENSEMBLE Study Group . Safety and efficacy of single-dose Ad26.COV2.S vaccine against Covid-19. N Engl J Med. 2021;384(23):2187-2201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zheng C, Shao W, Chen X, Zhang B, Wang G, Zhang W. Real-world effectiveness of COVID-19 vaccines: a literature review and meta-analysis. Int J Infect Dis. 2021;114:252-260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Yri OE, Torfoss D, Hungnes O, et al. Rituximab blocks protective serologic response to influenza A (H1N1) 2009 vaccination in lymphoma patients during or within 6 months after treatment. Blood. 2011;118(26):6769-6771. [DOI] [PubMed] [Google Scholar]
- 65.Thakkar A, Gonzalez-Lugo JD, Goradia N, et al. Seroconversion rates following COVID-19 vaccination among patients with cancer. Cancer Cell. 2021;39(8):1081-1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Maneikis K, Šablauskas K, Ringelevičiūtė U, et al. Immunogenicity of the BNT162b2 COVID-19 mRNA vaccine and early clinical outcomes in patients with haematological malignancies in Lithuania: a national prospective cohort study. Lancet Haematol. 2021;8(8):e583-e592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pagano L, Salmanton-García J, Marchesi F, et al. COVID-19 in vaccinated adult patients with hematological malignancies. preliminary results from EPICOVIDEHA. Blood. 2022;139(10):1588–1592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Peeters M, Verbruggen L, Teuwen L, et al. Reduced humoral immune response after BNT162b2 coronavirus disease 2019 messenger RNA vaccination in cancer patients under antineoplastic treatment. ESMO Open. 2021;6(5):100274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Greenberger LM, Saltzman LA, Senefeld JW, Johnson PW, DeGennaro LJ, Nichols GL. Anti-spike antibody response to SARS-CoV-2 booster vaccination in patients with B cell-derived hematologic malignancies. Cancer Cell. 2021;39(10):1297-1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Malard F, Gaugler B, Gozlan J, et al. Weak immunogenicity of SARS-CoV-2 vaccine in patients with hematologic malignancies. Blood Cancer J. 2021;11(8):142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ram R, Hagin D, Kikozashvilli N, et al. Safety and immunogenicity of the BNT162b2 mRNA COVID-19 vaccine in patients after allogeneic HCT or CD19-based CART therapy: a single-center prospective cohort study. Transplant Cell Ther. 2021;27(9):788-794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Reimann P, Ulmer H, Mutschlechner B, et al. Efficacy and safety of heterologous booster vaccination with Ad26.COV2.S after BNT162b2 mRNA COVID-19 vaccine in haemato-oncological patients with no antibody response. Br J Haematol. 2021;196(3):577-584. [DOI] [PubMed] [Google Scholar]
- 73.Jiménez M, Roldan E, Fernández-Naval C, et al. Cellular and humoral immunogenicity of the mRNA-1273 SARS-CoV-2 vaccine in patients with hematologic malignancies. Blood Adv. 2022;6(3):774-784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ariamanesh M, Porouhan P, PeyroShabany B, et al. Immunogenicity and safety of the inactivated SARS-CoV-2 vaccine (BBIBP-CorV) in patients with malignancy. Cancer Invest. 2022;40(1):26-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ollila TA, Lu S, Masel R, et al. Antibody response to COVID-19 vaccination in adults with hematologic malignant disease. JAMA Oncol. 2021;7(11):1714-1716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gavriatopoulou M, Terpos E, Kastritis E, et al. Low neutralizing antibody responses in WM, CLL and NHL patients after the first dose of the BNT162b2 and AZD1222 vaccine. Clin Exp Med. 2022;22(2): 319-323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Re D, Barrière J, Chamorey E, et al. Low rate of seroconversion after mRNA anti-SARS-CoV-2 vaccination in patients with hematological malignancies. Leuk Lymphoma. 2021;62(13):3308-3310. [DOI] [PubMed] [Google Scholar]
- 78.Herzog Tzarfati K, Gutwein O, Apel A, et al. BNT162b2 COVID-19 vaccine is significantly less effective in patients with hematologic malignancies. Am J Hematol. 2021;96(10):1195-1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Fendler A, Shepherd STC, Au L, et al. ; Crick COVID19 consortium . Adaptive immunity and neutralizing antibodies against SARS-CoV-2 variants of concern following vaccination in patients with cancer: the CAPTURE study. Nat Cancer. 2021;2: 1321-1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Shapiro LC, Thakkar A, Campbell ST, et al. Efficacy of booster doses in augmenting waning immune responses to COVID-19 vaccine in patients with cancer. Cancer Cell. 2022;40(1):3–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kohn M, Delord M, Chbat M, et al. A third anti-SARS-Cov2 mRNA dose does not overcome the pejorative impact of anti-CD20 therapy and/or low immunoglobulin levels in patients with lymphoma or chronic lymphocytic leukemia [published online ahead of print]. Haematologica. 2021. doi: 10.3324/haematol.2021.280026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Greenberger LM, Saltzman LA, Senefeld JW, Johnson PW, DeGennaro LJ, Nichols GL. Antibody response to SARS-CoV-2 vaccines in patients with hematologic malignancies. Cancer Cell. 2021;39(8):1031-1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Benda M, Mutschlechner B, Ulmer H, et al. Serological SARS-CoV-2 antibody response, potential predictive markers and safety of BNT162b2 mRNA COVID-19 vaccine in haematological and oncological patients. Br J Haematol. 2021;195(4):523-531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tamariz-Amador LE, Battaglia AM, Maia C, et al. ; The Asociación Vasco-Navarra de Hematología y Hemoterapia (ASOVASNA) Cooperative Group . Immune biomarkers to predict SARS-CoV-2 vaccine effectiveness in patients with hematological malignancies. Blood Cancer J. 2021;11(12):202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Terpos E, Gavriatopoulou M, Fotiou D, et al. Poor neutralizing antibody responses in 132 patients with CLL, NHL and HL after vaccination against SARS-CoV-2: a prospective study. Cancers (Basel). 2021;13(17):4480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Doria-Rose N, Suthar MS, Makowski M, et al. ; mRNA-1273 Study Group . Antibody persistence through 6 months after the second dose of mRNA-1273 vaccine for Covid-19. N Engl J Med. 2021;384(23):2259-2261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Naranbhai V, Nathan A, Kaseke C, et al. T cell reactivity to the SARS-CoV-2 Omicron variant is preserved in most but not all individuals. Cell. 2022;185(6): 1041-1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Burki TK. Fourth dose of COVID-19 vaccines in Israel. Lancet Respir Med. 2022; 10(2):e19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Alejo JL, Mitchell J, Chiang TP, et al. Antibody response to a fourth dose of a SARS-CoV-2 vaccine in solid organ transplant recipients: a case series. Transplantation. 2021;105(12):e280-e281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Li P, Wang Y, Lavrijsen M, et al. SARS-CoV-2 Omicron variant is highly sensitive to molnupiravir, nirmatrelvir, and the combination. Cell Res. 2022;32(3):322-324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Takashita E, Kinoshita N, Yamayoshi S, et al. Efficacy of antibodies and antiviral drugs against Covid-19 Omicron variant. N Engl J Med. 2022;386(10):995-998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Vangeel L, Chiu W, De Jonghe S, et al. Remdesivir, molnupiravir and nirmatrelvir remain active against SARS-CoV-2 Omicron and other variants of concern. Antiviral Res. 2022;198:105252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Owen DR, Allerton CMN, Anderson AS, et al. An oral SARS-CoV-2 Mpro inhibitor clinical candidate for the treatment of COVID-19. Science. 2021;374(6575): 1586-1593. [DOI] [PubMed] [Google Scholar]
- 94.Hammond J, Leister-Tebbe H, Gardner A, et al. ; EPIC-HR Investigators . Oral nirmatrelvir for high-risk, nonhospitalized adults with Covid-19. N Engl J Med. 2022;386(15):1397-1408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Beigel JH, Tomashek KM, Dodd LE, et al. ; ACTT-1 Study Group Members . Remdesivir for the treatment of Covid-19: final report. N Engl J Med. 2020;383(19):1813-1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Gottlieb RL, Vaca CE, Paredes R, et al. ; GS-US-540-9012 (PINETREE) Investigators . Early remdesivir to prevent progression to severe Covid-19 in outpatients. N Engl J Med. 2022;386(4):305-315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kabinger F, Stiller C, Schmitzová J, et al. Mechanism of molnupiravir-induced SARS-CoV-2 mutagenesis. Nat Struct Mol Biol. 2021;28(9):740-746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Jayk Bernal A, Gomes da Silva MM, Musungaie DB, et al. Molnupiravir for oral treatment of Covid-19 in nonhospitalized patients. N Engl J Med. 2022;386(6):509–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hegerova L, Gooley TA, Sweerus KA, et al. Use of convalescent plasma in hospitalized patients with COVID-19: case series. Blood. 2020;136(6):759-762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Zeng QL, Yu ZJ, Gou JJ, et al. Effect of convalescent plasma therapy on viral shedding and survival in patients with coronavirus disease 2019. J Infect Dis. 2020;222(1):38-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.O’Brien MP, Forleo-Neto E, Musser BJ, et al. ; Covid-19 Phase 3 Prevention Trial Team . Subcutaneous REGEN-COV antibody combination to prevent Covid-19. N Engl J Med. 2021;385(13):1184-1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Baang JH, Smith C, Mirabelli C, et al. Prolonged severe acute respiratory syndrome coronavirus 2 replication in an immunocompromised patient. J Infect Dis. 2021;223(1):23-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Biernat MM, Kolasińska A, Kwiatkowski J, et al. Early administration of convalescent plasma improves survival in patients with hematological malignancies and COVID-19. Viruses. 2021;13(3):436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Weinbergerova B, Mayer J, Kabut T, et al. Successful early treatment combining remdesivir with high-titer convalescent plasma among COVID-19-infected hematological patients. Hematol Oncol. 2021; 39(5):715-720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Hueso T, Pouderoux C, Péré H, et al. Convalescent plasma therapy for B-cell-depleted patients with protracted COVID-19. Blood. 2020;136(20):2290-2295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Jeyaraman P, Agrawal N, Bhargava R, et al. ; Delhi Hematology Group . Convalescent plasma therapy for severe Covid-19 in patients with hematological malignancies. Transfus Apheresis Sci. 2021;60(3):103075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Camprubí D, Gaya A, Marcos MA, et al. Persistent replication of SARS-CoV-2 in a severely immunocompromised patient treated with several courses of remdesivir. Int J Infect Dis. 2021;104:379-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Lanza F, Agostini V, Monaco F, Passamonti F, Seghatchian J. Therapeutic use of convalescent plasma in COVID-19 infected patients with concomitant hematological disorders. Clin Hematol Int. 2021;3(3): 77-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Tremblay D, Seah C, Schneider T, et al. ; Mount Sinai Health System Convalescent Plasma Team . Convalescent plasma for the treatment of severe COVID-19 infection in cancer patients. Cancer Med. 2020;9(22):8571-8578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Horby P, Lim WS, Emberson JR, et al. ; RECOVERY Collaborative Group . Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2021;384(8):693-704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.VanBlargan LA, Errico JM, Halfmann PJ, et al. An infectious SARS-CoV-2 B.1.1.529 Omicron virus escapes neutralization by therapeutic monoclonal antibodies. Nat Med. 2022;28(3):490-495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Iketani S, Liu L, Guo Y, et al. Antibody evasion properties of SARS-CoV-2 Omicron sublineages. Nature. 2022;604(7906): 553-556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Wang P, Nair MS, Liu L, et al. Antibody resistance of SARS-CoV-2 variants B.1.351 and B.1.1.7. Nature. 2021;593(7857): 130-135. [DOI] [PubMed] [Google Scholar]
- 114.Gupta A, Gonzalez-Rojas Y, Juarez E, et al. ; COMET-ICE Investigators . Early treatment for Covid-19 with SARS-CoV-2 neutralizing antibody sotrovimab. N Engl J Med. 2021;385(21):1941-1950. [DOI] [PubMed] [Google Scholar]
- 115.Mahase E. Covid-19: AstraZeneca says its antibody drug AZD7442 is effective for preventing and reducing severe illness. BMJ. 2021;375(2860):n2860. [DOI] [PubMed] [Google Scholar]
- 116.Tixagevimab and Cilgavimab (Evusheld) for Pre-Exposure Prophylaxis of COVID-19 . Tixagevimab and cilgavimab (evusheld) for pre-exposure prophylaxis of COVID-19. JAMA. 2022;327(4):384-385. [DOI] [PubMed] [Google Scholar]
- 117.COVID-19 updates: booster immunization in persons who are immunocompromised. Med Lett Drugs Ther. 2022;64(1646):47-48. [PubMed] [Google Scholar]
- 118.Madhi SA, Kwatra G, Myers JE, et al. Population immunity and Covid-19 severity with Omicron variant in South Africa. N Engl J Med. 2022;386(14):1314-1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Niemann CU, da Cunha-Bang C, Helleberg M, Ostrowski SR, Brieghel C. Patients with CLL have lower risk of death from COVID-19 in the omicron era [published online ahead of print 19 May 2022]. Blood. doi: 10.1182/blood.2022016147. [DOI] [PMC free article] [PubMed]
- 120.Levy I, Sharf G, Norman S, Tadmor T. The impact of COVID-19 on patients with hematological malignancies: the mixed-method analysis of an Israeli national survey. Support Care Cancer. 2021;29(12):7591-7599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zomerdijk N, Jongenelis M, Short CE, Smith A, Turner J, Huntley K. Prevalence and correlates of psychological distress, unmet supportive care needs, and fear of cancer recurrence among haematological cancer patients during the COVID-19 pandemic. Support Care Cancer. 2021;29(12):7755-7764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Romito F, Dellino M, Loseto G, et al. psychological distress in outpatients with lymphoma during the COVID-19 pandemic. Front Oncol. 2020;10:1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.