Abstract
Ultrasound imaging is a key investigatory step in the evaluation of chronic kidney disease and kidney transplantation. It uses nonionizing radiation, is noninvasive, and generates real-time images, making it the ideal initial radiographic test for patients with abnormal kidney function. Ultrasound enables the assessment of both structural (form and size) and functional (perfusion and patency) aspects of kidneys, both of which are especially important as the disease progresses. Ultrasound and its derivatives have been studied for their diagnostic and prognostic significance in chronic kidney disease and kidney transplantation. Ultrasound is rapidly growing more widely accessible and is now available even in handheld formats that allow for bedside ultrasound examinations. Given the trend toward ubiquity, the current use of kidney ultrasound demands a full understanding of its breadth as it and its variants become available. We described the current applications and future directions of ultrasound imaging and its variants in the context of chronic kidney disease and transplantation in this review.
Index Words: Chronic kidney disease, Doppler, elastography, kidney transplantation, ultrasound
Ultrasound (US) imaging is a critical diagnostic tool for assessing human kidneys. A US transducer works by transmitting radiofrequency sound waves into the body. These waves interact with tissues and tissue interfaces, changing them and returning them to the transducer as echoes. Its piezoelectric crystals vibrate in response, converting the echoes into electrical signals, which are then processed using complex algorithms to provide cross-sectional images of the body’s underlying tissue layers. US does not use ionizing radiation and is noninvasive, meaning that it does not require any penetration of the skin. In both acute care and ambulatory settings, US imaging can reveal information on kidney morphology, physical features, function, and probable anomalies. US is used as the first-line imaging modality for previously undiagnosed native and transplanted, abnormal kidney function.1,2 Several studies have argued for the formal incorporation of sonography into training and clinical practice, citing its increasing utility and accessibility in nephrology.3, 4, 5, 6, 7 Taken together, advances in beamforming, image acquisition, and image processing make portable US a reality while lowering costs by several orders of magnitude. One of these advances is point-of-care US. It is a US examination performed by nephrologists at the patient’s bedside, often treated as an extension of physical examination.8,9 Point-of-care US has become more accessible and widespread with increasingly portable, even handheld, US equipment.4 To successfully use US as an adjunct to clinical decision making, a thorough understanding of the technology and its variants is required, particularly in the context of chronic kidney disease (CKD) and kidney transplantation.
This review discusses US and its derivatives as well as their clinical applications. Brightness mode (B-mode), color Doppler, power Doppler, and spectral Doppler US are all types of US often used in disease evaluation. Additional types, including contrast-enhanced US and US-based elastography, have seen tremendous research efforts and may be worth considering for routine clinical use. This review focuses on the most common types for which published literature on CKD and kidney transplantation is accessible. This article summarizes the mechanism of action for each variation, reviews the type of data obtained, and synthesizes pertinent research demonstrating its therapeutic utility in CKD and transplantation.
B-Mode Imaging
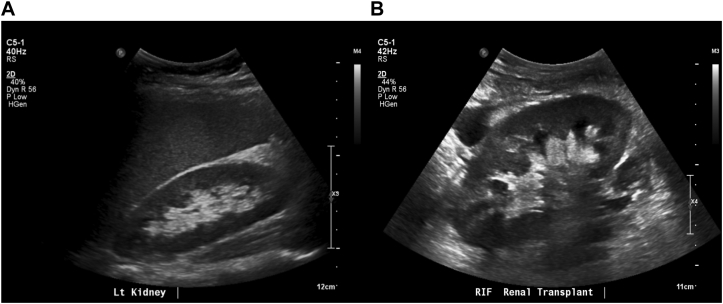
B-mode US is a 2-dimensional, cross-sectional depiction of anatomy in grayscale.10 A pixel’s depth in the image represents a tissue’s distance from the transducer, and its intensity represents echogenicity, which is the ability of the tissue to reflect the US signal.10 Tissue interfaces and microstructures influence echogenicity, capturing underlying tissue variations.10 Lower imaging frequencies allow the imaging of deeper tissues, such as native kidneys in the abdominal cavity’s back wall. The trade-off for penetration depth is that frequency is inversely linked to spatial resolution; lower frequencies have worse resolution (Fig 1). A transplanted kidney, located in the recipient’s iliac fossa, is closer to the abdominal skin surface, allowing higher frequencies (Fig 1).
Figure 1.
Exemplary clinical images of (A) a native kidney in longitudinal view with the liver and (B) a transplanted kidney in longitudinal view in the right iliac fossa.
The anthropomorphic measurements provided by B-mode US include the length and volume of kidneys. Kidney length is defined as the maximum distance from pole to pole, measured in a longitudinal view, with a normal range of 10-12 cm.11 The left kidney is longer than the right, with median lengths of 11.2 and 10.9 cm, respectively.12 Widjaja et al13 used US imaging to quantify the native kidney lengths of 69 adults and compared them with single kidney function using radionuclide imaging. They found the length to have a moderate positive correlation (r2 = 0.48) with the estimated glomerular filtration rate (eGFR) of the native single kidneys, although Zanoli et al14 discovered that the correlation between length and eGFR varied based on the eGFR equation. Measured in a longitudinal view from the kidney’s midpole boundary to the base of the medullary pyramids, cortical thickness is a common metric. The normal cortical thickness is 7-10 mm; reduced cortical thickness may indicate progressive kidney disease or decreased eGFR.11,15,16
With respect to volume, the normal range in men is 110-190 mL and in women is 90-150 mL.17 It is possible to measure volume by simplifying the kidney’s shape as spherical or ellipsoid and measuring several distances. Better still is to contour the kidney in each US frame and sum the contoured area. Manual contouring is the gold standard for US-based volume estimation; however, it is very time consuming and labor intensive. Studies by Zanoli et al14 and Sanusi et al18 reported favorable relationships between kidney volume and 24-hour creatinine clearance as well as eGFR estimated using various equations. Volume interpretation requires caution as Kim et al19 found that 2-dimensional, US-based volumes underestimated computed tomography volumes by 15%.
Nephrologists can use these parameters to understand the state of kidney disease. A kidney length of ≤8 cm is related to kidney failure.20 If the kidney loses its length or volume, this is attributed to atrophy or fibrosis.8 A unilateral decrease may specifically indicate hypoperfusion, such as in renal artery stenosis,8 whereas bilateral hypotrophic kidneys with decreased volumes may indicate advanced disease, such as in kidney failure. Fluid retention, inflammation, protein deposition, and acute tubular necrosis or neoplasms are linked to increased kidney volume.8
Renal echogenicity is frequently used as a kidney health biomarker. The echogenicity of renal parenchyma is assessed by comparing it with a reference tissue, such as the liver, which should be less echogenic.11,21 Moghazi et al22 retrospectively evaluated the correlation between cortical echogenicity and histopathologic parameters, finding a strong correlation with severe disease and increased relative echogenicity. Similarly, Page et al23 found a link between glomerular sclerosis detected using biopsy and cortical echogenicity. Echogenicity must be carefully considered because it depends on the US machine setup, image acquisition factors, or hydration status. Additionally, occult liver disease may increase the liver’s echogenicity, causing a misleading negative comparison with the renal cortex. The echogenicity of the cortex and medulla are easily compared. The inability to distinguish between them is known as the loss of corticomedullary differentiation.24 This observation is nonspecific in both native and transplanted kidneys.24 Infection, autosomal recessive kidney disease, renal vein thrombosis, and rejection are all conditions that may present with the loss of corticomedullary differentiation.25,26.
B-mode imaging lies in point-of-care adoption. The feasibility and usability of these morphologic and echogenic properties are considerably boosted by accessible US imaging. Further research on understanding how easily nephrologists can acquire clinically meaningful images is required, as is research on existing technical challenges to further adoption.
Doppler Imaging
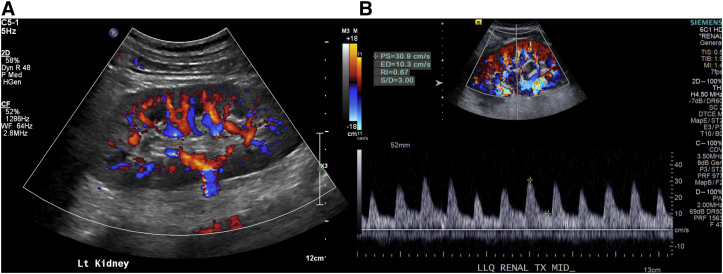
Doppler imaging is used to assess renal vascular flow and patency. When a pulsed US wave encounters a moving medium, the resultant echo undergoes a frequency shift.10 In the human body, this moving medium is commonly blood inside vessels. The frequency decreases as the medium moves away from the transducer and increases as it moves toward it.10 Derived from these shifts is flow velocity.10 The types of Doppler US can be color Doppler, power Doppler, or spectral Doppler imaging. In Fig 2, color Doppler imaging overlays the color map of flow velocity onto a B-mode image also showing directionality. Power Doppler imaging employs a color map that sacrifices directionality for increased sensitivity to detect blood flow. Spectral Doppler imaging produces a “waveform” of velocities across time and can be employed in continuous or pulsed wave patterns. Continuous waves measure high velocities but cannot localize them because they employ different crystals to send and receive radiofrequency waves at the same time. Pulsed waves can localize velocities but are subject to aliasing.
Figure 2.
Sample images of color Doppler imaging used to assess a kidney’s vasculature. (B) A renal resistive index of 0.67 was calculated from the spectral information obtained.
Doppler US is widely used to assess transplanted kidneys, although it is difficult to be performed in native kidneys because of the depth of the organ. It can be used to detect renal vascular disorders such as stenosis or thrombosis. For example, increased peak systolic velocities surpassing 200 cm/sec, a 3.5:1 peak systolic velocity ratio between the renal artery and the vascular tributary proximal to it, and aliasing are all signs of the renin angiotensin system.27 The use of pulsed-wave spectral Doppler imaging is required. A systematic review found that peak systolic velocity had the highest sensitivity (85%) and specificity (92%) compared with other US parameters in the diagnosis of this devastating complication.28 With increasing kidney size and reversed parenchymal vascular flow, the absence of venous flow from renal vein thromboses is instructive. Doppler US can also be used after biopsy to evaluate postprocedure complications, such as intrarenal arteriovenous fistula, which occurs up to 18% of the time.29 Power Doppler imaging is useful in the diagnosis of kidney ischemia or infarction because its greater sensitivity helps in the detection of minor vascular alterations such as capillary bed changes.30
The renal resistive index (RRI) can be derived from Doppler US. This is a unitless, surrogate measure of intrarenal parenchymal pathology, defined as the ratio of the difference between peak systolic velocity and end-diastolic velocity to the peak systolic velocity. It is measured in arcuate or interlobar arteries. When RRI is ≤0.7, it reassures the nephrologist of the absence of severe kidney damage.31 In the native kidney setting, a controversy arises when elevated RRI and histopathologic markers are associated. Some studies have linked increased RRI with glomerulosclerosis progression, glomerular disease, arteriolosclerosis, and interstitial fibrosis, whereas others have found no correlation.32, 33, 34, 35, 36 Elevated RRI may have prognostic value because it has been associated with worsening kidney function,37,38 cardiovascular risk scores.,37 and progressive diabetic nephropathy.39 In kidney transplantation, renal vein and renal artery thromboses have been associated with low RRI values in the immediate postoperative period.40 Wang et al reported that donor kidneys from deceased individuals have higher RRIs (0.73 ± 0.10) than control kidneys from living donors (0.66 ± 0.11). RRI is yet to be proven as a predictive factor for kidney transplant outcomes, including long-term allograft survival.41
Some researchers have contended that variation in RRI is related to extrarenal variables rather than inherent structural changes in the kidney, both in native and transplanted contexts. RRI is affected by age, heart rate, blood pressure, systemic vascular resistance, and hydration.42 O’Neill43 presented a mathematical approach to the interpretation of RRI, suggesting that it is more easily impacted by pulse pressure, renal capillary wedge pressure, and vascular compliance. Rather than intrarenal changes, the author argued that it reflects systemic hemodynamics.43 Others have suggested that increases in posttransplantation RRI are linked to the organ’s new vascular environment in the recipient.44 Seiler et al45 showed that RRI may not be specific to kidneys. They reported a correlation between RRI and increased common carotid thickness but not kidney-specific markers.45 However, as Grün et al46 reported in their investigation of variations in resistive indices between the spleen and the kidney, the use of 2 indices may reduce extrarenal influence and enhance kidney specificity. Overall, these studies suggest caution while interpreting RRI as a kidney-specific pathology indication.
Doppler US-acquired values are subject to external factors, such as the imaging plane, operator technique, and transducer location, making valid, accurate, and repeatable measurements difficult. Future research should consider extrarenal hemodynamic variables that may affect RRI values. Given the difficulty in conducting high-quality Doppler imaging studies without experienced personnel, the use of Doppler US at the bedside may be best suited for determining vascular patency or its absence.
Contrast-Enhanced US
A technique known as contrast-enhanced US is used to investigate blood flow and perfusion in greater detail.47 A contrast medium—a nontoxic, biologically inert microbubble with a diameter <10 μm—is injected into the systemic circulation.47 The contrast medium dissolves on its own within minutes of being injected and has no effect on kidney function or the systemic circulation in any other manner. Although contrast-enhanced US is less expensive than color Doppler imaging, it provides a more accurate assessment of the microvasculature and perfusion in narrow blood arteries, where color Doppler imaging may require significant operator expertise or blood flow may be too slow.48
Contrast-enhanced US enables improved visualization of perfusion and the provision of absolute, quantitative values through the observation of destruction and replenishment of the contrast medium, which is characterized using time-intensity curves.48 These curves can be used to compute perfusion characteristics, such as time to peak, rising time, area under the curve, peak intensity, and mean transit time. The contrast agents are typically injected intravenously as either a bolus or an infusion.47 With the use of bolus injections, it is possible to image the contrast agent as it enters and exits the image, with the imaging period ranging between 3 and 5 minutes per bolus injection.47 Infusion provides for extended imaging times (up to 15 minutes), but it does not allow the imaging of the agent leaving the image.47 Contrast-enhanced US can be used to assess ischemic diseases, including infarction and necrosis, as well as the states of relative hypervascularization, such as malignant kidney lesions.49,50.
Ma et al51 investigated the role of contrast-enhanced US in 33 patients with CKD and diabetes. They discovered that the total area under the time-intensity curve was only moderately correlated with eGFR and that patients with early- and late-stage CKD had significantly different rising time and time-to-peak parameters.51 These parameters mirror the hemodynamic environment, showing slower kidney perfusion in advanced disease.51 Dong et al52 demonstrated, using a bolus injection in 41 patients with suspected CKD stages 1-3, that the area under the curve and the derived peak intensity, but not the time to peak, were significantly different from those in healthy controls even though the set of parameters was different from that used by Ma et al.51 The use of a derived peak intensity of <12 dB was the best predictor of the onset of CKD, achieving an accuracy of 79%, a sensitivity of 76%, and a specificity of 81%.52 Girometti et al53 used contrast-enhanced US to evaluate acute diseases such as kidney infarction. Using contrast-enhanced US, they found a significantly higher (P = 0.0002) detection rate of infarction than with the use of color Doppler imaging.53 Finally, Chang et al50 used contrast-enhanced US to evaluate indeterminate kidney lesions in patients with and without CKD. Across all patients, contrast-enhanced US achieved high sensitivity (96%) and moderate specificity (50%) for malignancy detection, whereas the sensitivity dropped to 90% and specificity increased to 55% only in those with CKD.50 However, this was based on a radiologist’s interpretation of contrast-enhanced US images rather than any specific perfusion parameter. In contrast to these studies, Jeong et al54 discovered no relationship between perfusion parameters and kidney function.
Several publications have shown that contrast-enhanced US parameters can be used to identify abnormal kidney function in patients who have undergone transplantation. Fischer et al55 published 1 of the earliest studies that found that the arrival time of the contrast medium from the renal artery to the cortex was significantly delayed in patients with acute rejection compared with that in controls. Although Yang et al56 successfully used contrast-enhanced US to differentiate between acute and chronic transplanted abnormal kidney function, the researchers were unable to differentiate between rejection subtypes. Contrast-enhanced US had a sensitivity of 86%, a specificity of 90%, and an area under the curve of 0.94 in a systematic review of posttransplantation complications, such as rejection or vascular pathologies, in 542 patients.57
Currently, there is paucity of research on contrast-enhanced US in the kidney. Additional contrast agents, specialized US machines, and general lack of competence in using contrast-enhanced US are all factors. Furthermore, the requirement for contrast agent injections distinguishes this variant as the only invasive US variant, complicating its adoption even further. More research is needed to determine the efficacy of contrast-enhanced US in the detection of early intrinsic kidney disease pathologies and early kidney transplant abnormalities such as rejection.
Elastography
Regardless of the primary diagnosis, kidney disease frequently follows a common histologic pathway that includes inflammation, sclerosis, atrophy, maladaptive hemodynamic and nonhemodynamic responses, and fibrosis. These various states might have a local or global effect on the kidney. Kidney biopsy is the gold standard for the assessment of its pathology; however, it carries with it the potential complications of an invasive procedure. Can US be used instead of biopsy for noninvasive evaluation of disease conditions because it is noninvasive? Elastography, a type of US imaging, is a possible alternative.
Elastography is used to measure tissue elasticity, allowing for subsurface “palpation.”58,59 This US variation’s mechanism of action involves the transmission of acoustic energy into the body to cause transient displacements.58,59 This can be generated by the transducer or an external source.58,59. This energy causes a transient displacement of the tissue.58,59 The US transducer can be used to detect deformations because the displacement is slower than the speed of the US pulse waves.58,59 These deformations determine the tissue’s elasticity. Elasticity can be measured either in a relative (to other tissues in the same image) or absolute (in standardized units and compared with a reference) manner.58,59. The outputs of elastography include shear wave velocity (measured in m/s), Young modulus (measured in kPa), or elastograms (Fig 3).58,59
Figure 3.
Sample image of shear wave elastography used to assess a kidney’s parenchymal stiffness. (A) A confidence map is used to obtain high-quality measurements. (B) The elastogram demonstrates differences in regional stiffness within the tissue.
The variants of elastography include strain elastography (also known as quasistatic or qualitative elastography), transient elastography, acoustic radiation force impulse imaging, shear wave elastography, and shear wave absolute vibroelastography.58,59 External compression is applied to the tissue in strain elastography, with pulse-echo data collected before and after compression.58,59. Only a qualitative elastogram is produced because the amount of compression is not measured. Transient elastography improves on this by providing 1-dimensional quantitative measurement (a point). The acoustic radiation force impulse imaging technology further advances this by applying small acoustic radiation forces to induce displacements at a focal point or at multiple points. With the use of multiple points, a 2-dimensional elastogram within a region of interest can be obtained.58,59 Shear wave elastography uses shear waves that propagate laterally relative to the transducer and concentrate within regions of interest, causing displacements. Shear wave absolute vibroelastography employs an external low-frequency excitation source, allowing for 3-dimensional quantitative mapping of elasticity at greater depths.58,59 The key differences between these variants include qualitative versus quantitative outputs, imaging depths at which measurements can be obtained, the dimensionality of the measures (a single point, a small region of interest, or an entire volume), and the source of the excitatory stress (internal vs external).58,59 Because image acquisition protocols and data analysis approaches differ, it is difficult to compare the results of these technologies.
Elastography in the kidney has several potential applications. Consider fibrosis, a hallmark of CKD and chronic transplant rejection.60 As fibrosis accrues, there is an increase in collagen deposition and extracellular matrix at the microscopic level, in turn potentially impacting the overall stiffness of the kidney. Measuring this stiffness may have diagnostic and prognostic potential in clinical decision making.
According to Menzilcioglu et al,61 the use of strain imaging with a cutoff value of 0.93 (88% sensitivity and 95% specificity) can help detect CKD. Bob et al62 used acoustic radiation force impulse imaging to discover that patients with advanced CKD had significantly lower elasticity values than those with early-stage disease. Some groups found no significant difference in stiffness measured using acoustic radiation force impulse imaging between CKD stages.63 Similarly, shear wave elastography has had mixed results. Unlike Bob et al,62 Hassan et al64 found greater stiffness in patients with CKD stage 3 and 4 than in healthy participants. Although Leong et al65 reported that shear wave elastography is superior to kidney length and cortical thickness as the US markers of CKD, their cutoff value for healthy versus diseased native kidneys was 4.31 kPa. As of now, no in situ reference values for native kidneys have been developed.
Because of its superficial placement, a transplanted kidney is ideal for elastography. Gao et al66 found that “normalized strain” (defined as the ratio of cortical strain to the strain in the surrounding structures) was substantially linked with the biopsy-proven degree of fibrosis. Wang et al67 employed acoustic radiation force impulse imaging to measure the cortical stiffness within transplanted kidneys, reporting a mean (±standard deviation) of 3.19 (±1.01) m/s. The researchers discovered substantial relationships with RRIs evaluated throughout the renal vasculature tree.67 They hypothesized that complicated hemodynamics affect stiffness. Stock et al68 also discovered a moderately positive correlation between acoustic radiation force impulse imaging measures and the degree of biopsy-determined fibrosis, lending credence to the use of elastography as a fibrosis marker. However, using acoustic radiation force impulse imaging, Syversveen et al69 reported no correlation between shear wave velocity (SWV) measurements and fibrosis, showing that transducer force discrepancies caused the differences in stiffness.
In one of the earliest studies on shear wave elastography for transplanted kidneys, Grenier et al demonstrated that renal cortical stiffness measured using shear wave elastography was not correlated with any individual Banff score component or grade of interstitial fibrosis but was correlated with the summation of chronic lesions scores.70 Early et al found a significant association between median medullary stiffness and fibrosis, reporting that a unit increase in medullary stiffness increased the likelihood of having fibrosis by 20%.71 The use of medullary stiffness differs from other studies that reported total parenchymal stiffness or cortical stiffness more commonly. By combining advanced work in shear wave elastography measurements with machine learning, Urban et al72 were able to differentiate between patients with fibrosis and inflammation and those without fibrosis and inflammation. Finally, Schneider et al59 demonstrated the feasibility of the shear wave absolute vibroelastography technology in a pilot study on transplant recipients. Volumetric elastography may provide more thorough stiffness measurements than existing 2-dimensional techniques.
Overall, despite its importance, the field of kidney elastography is still in its early stages. Peride et al73 identified significant variability of kidney elastography in the literature. This variability can be attributed to a myriad of factors. Because of signal attenuation, the elastographic imaging of deep organs, such as native kidney, is also challenging. Blood and urinary pressures may also affect elastography.74 Given the anisotropic nature of kidneys, the orientation of the excitation source relative to the nephrons may result in different stiffness values depending on whether the source is parallel or perpendicular to the nephrons. Hydration status is understudied for its role in elastography, although a recent study found its impact to be significant.75 Furthermore, microstructural changes beyond interstitial fibrosis, such as glomerular hypertrophy and sclerosis, may be confounders that are not accounted for. The impact of cardiac and respiratory cycles on elastographic measurements is also unclear. Fundamentally, as Sigrist et al76 highlighted, elastography measurements rely on critical underlying assumptions about the tissue. In other words, these techniques assume that the tissues are linear, isotropic, and incompressible; such modeling may not accurately capture the nuance of the kidney.74As our understanding of the complexities of US and kidney elastography improves, detailed reporting of these potential confounders in future studies may help to reduce variability. Noninvasive fibrosis biomarkers may become available soon.
Challenges and Opportunities in Kidney US
Kidney US has several limitations. In all derivatives, image acquisition and interpretation fall under operator dependencies and remain barriers to its use. Clinically acceptable images, which may be technically complex to achieve, require considerable expertise. Subjective interpretation of images persists, resulting in interrater variability. Manual measurements of the length and volume entail manual labor and may introduce intrarater and interrater variability. Artificial intelligence may mitigate these issues. It may enhance nephrologists’ ability to acquire and interpret images, regardless of their baseline skill. Additionally, thorough interpretation has not yet been fully integrated into medical education, necessitating additional training and effort. The modification of fellowships, residencies, and medical undergraduate programs to incorporate US training will require significant program support, the availability of machines and qualified instructors, and mechanisms for assessing competency. There is a clear interest in this training because several US curricula have been outlined across the stages of medical training.4,6,77,78
New technologies may also offer unforeseen opportunities. Chen et al79 demonstrated the use of superresolution ultrasound imaging in the detection of alterations in the renal microvasculature in a murine model of acute kidney injury. They demonstrated the ability to achieve a resolution of 50 μm and observed changes in the microvascular density and tortuosity; these metrics would be difficult to obtain with conventional techniques.79 As another example, Hossain et al80 created a novel variant of acoustic radiation force impulse imaging and explored how the inherent anisotropic nature of kidneys is emphasized by employing this variant and how it serves as a biomarker, a promising avenue of research. In a seminal article, Hysi et al81 used photoacoustic imaging, an emerging variant of US that leverages laser pulses, to directly image fibrosis. They demonstrated this US variant’s ability to directly image collagen with phenomenal accuracy in rat, porcine, and ex vivo human kidneys.81 Although it requires in vivo validation and clinical translation, this study represents a noninvasive kidney fibrosis measurement milestone.
Conclusion
In conclusion, US and its derivatives have a broad range of potential for improving the management of kidney disease by nephrologists. US can and continues to deliver clinically useful information in a noninvasive, real-time manner, with applications ranging from simple size measurements using B-mode imaging to perfusion and vasculature assessments in Doppler and contrast-enhanced US to the assessment of stiffness and elastic properties using US elastography. With the advancement of technology in the field, low-cost, high-quality, portable US scanning to provide multiparametric quantification may eliminate tests that are orders of magnitude more expensive and eliminate traditional, invasive biopsies. A nephrologist’s arsenal needs US now and in the future.
Article Information
Authors’ Full Names and Academic Degrees
Rohit K. Singla, MASc, Matthew Kadatz, MSc, MD, Robert Rohling, PhD, and Christopher Nguan, MD.
Support
The authors acknowledge funding from the Vanier Canada Graduate Scholarship, National Sciences and Engineering Research Council of Canada, and Kidney Foundation of Canada.
Financial Disclosure
Drs Rohling and Nguan are directors of SonicIncytes, an elastography imaging company that uses shear wave absolute vibroelastography. Dr Rohling is a coinvestigator on grants supported by Philips Healthcare, Clarius Mobile Health Corp, and Change Healthcare. Dr Nguan is the president of Cosmic Medical, a nonprofit organization for respiratory devices. Dr Nguan receives research funding from Roche and Pfizer. The remaining authors declare that they have no relevant financial interests.
Acknowledgments
The authors thank Kaitlin Hardy and Matthew Willis for their assistance with the manuscript.
Peer Review
Received August 18, 2021. Evaluated by 3 external peer reviewers, with direct editorial input from an Associate Editor and the Editor-in-Chief. Accepted in revised form February 14, 2022.
Footnotes
Complete author and article information provided before references.
References
- 1.Remer E.M., Papanicolaou N., Casalino D.D., et al. ACR appropriateness criteria® on renal failure. Am J Med. 2014;127(11):1041–1048. doi: 10.1016/j.amjmed.2014.05.014. [DOI] [PubMed] [Google Scholar]
- 2.Taffel M.T., Nikolaidis P., Beland M.D., et al. ACR appropriateness criteria® renal transplant dysfunction. J Am Coll Radiol. 2017;14(5):S272–S281. doi: 10.1016/j.jacr.2017.02.034. [DOI] [PubMed] [Google Scholar]
- 3.O’Neill W.C. Sonographic evaluation of renal failure. Am J Kidney Dis. 2000;35(6):1021–1038. doi: 10.1016/s0272-6386(00)70036-9. [DOI] [PubMed] [Google Scholar]
- 4.Koratala A., Segal M.S., Kazory A. Integrating point-of-care ultrasonography into nephrology fellowship training: a model curriculum. Am J Kidney Dis. 2019;74(1):1–5. doi: 10.1053/j.ajkd.2019.02.002. [DOI] [PubMed] [Google Scholar]
- 5.Niyyar V.D., O’Neill W.C. Point-of-care ultrasound in the practice of nephrology. Kidney Int. 2018;93(5):1052–1059. doi: 10.1016/j.kint.2017.11.032. [DOI] [PubMed] [Google Scholar]
- 6.Koratala A., Olaoye O.A., Bhasin-Chhabra B., Kazory A. A blueprint for an integrated point-of-care ultrasound curriculum for nephrology trainees. Kidney360. 2021;2(10):1669–1676. doi: 10.34067/KID.0005082021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berns J.S., O’Neill W.C. Performance of procedures by nephrologists and nephrology fellows at US nephrology training programs. Clin J Am Soc Nephrol. 2008;3(4):941–947. doi: 10.2215/CJN.00490108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Narula J., Chandrashekhar Y., Braunwald E. Time to add a fifth pillar to bedside physical examination: inspection, palpation, percussion, auscultation, and insonation. JAMA Cardiol. 2018;3(4):346–350. doi: 10.1001/jamacardio.2018.0001. [DOI] [PubMed] [Google Scholar]
- 9.Rad A.H., Badeli H. Point-of-care ultrasonography: is it time nephrologists were equipped with the 21st century’s stethoscope? Iran J Kidney Dis. 2017;11(4):259–262. [PubMed] [Google Scholar]
- 10.Szabo T.L. In: Diagnostic Ultrasound Imaging: Inside Out. 2nd ed. Szabo T.L., editor. Elsevier Science & Technology; 2014. Chapter 9 - Scattering from tissue and tissue characterization; pp. 295–363. [Google Scholar]
- 11.Koratala A., Bhattacharya D., Kazory A. Point of care renal ultrasonography for the busy nephrologist: a pictorial review. World J Nephrol. 2019;8(3):44–58. doi: 10.5527/wjn.v8.i3.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Emamian S.A., Nielsen M.B., Pedersen J.F., Ytte L. Kidney dimensions at sonography: correlation with age, sex, and habitus in 665 adult volunteers. AJR Am J Roentgenol. 1993;160(1):83–86. doi: 10.2214/ajr.160.1.8416654. [DOI] [PubMed] [Google Scholar]
- 13.Widjaja E., Oxtoby J.W., Hale T.L., Jones P.W., Harden P.N., McCall I.W. Ultrasound measured renal length versus low dose CT volume in predicting single kidney glomerular filtration rate. Br J Radiol. 2004;77(921):759–764. doi: 10.1259/bjr/24988054. [DOI] [PubMed] [Google Scholar]
- 14.Zanoli L., Romano G., Romano M., et al. Renal function and ultrasound imaging in elderly subjects. Sci World J. 2014;2014:7. doi: 10.1155/2014/830649. 830649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Korkmaz M., Aras B., Güneyli S., Yılmaz M. Clinical significance of renal cortical thickness in patients with chronic kidney disease. Ultrasonography. 2018;37(1):50–54. doi: 10.14366/usg.17012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beland M.D., Walle N.L., Machan J.T., Cronan J.J. Renal cortical thickness measured at ultrasound: is it better than renal length as an indicator of renal function in chronic kidney disease? AJR Am J Roentgenol. 2010;195(2):W146–W149. doi: 10.2214/AJR.09.4104. [DOI] [PubMed] [Google Scholar]
- 17.Cheong B., Muthupillai R., Rubin M.F., Flamm S.D. Normal values for renal length and volume as measured by magnetic resonance imaging. Clin J Am Soc Nephrol. 2007;2(1):38–45. doi: 10.2215/CJN.00930306. [DOI] [PubMed] [Google Scholar]
- 18.Sanusi A.A., Arogundade F.A., Famurewa O.C., et al. Relationship of ultrasonographically determined kidney volume with measured GFR, calculated creatinine clearance and other parameters in chronic kidney disease (CKD) Nephrol Dial Transplant. 2009;24(5):1690–1694. doi: 10.1093/ndt/gfp055. [DOI] [PubMed] [Google Scholar]
- 19.Kim H.C., Yang D.M., Lee S.H., Cho Y.D. Usefulness of renal volume measurements obtained by a 3-dimensional sonographic transducer with matrix electronic arrays. J Ultrasound Med. 2008;27(12):1673–1681. doi: 10.7863/jum.2008.27.12.1673. [DOI] [PubMed] [Google Scholar]
- 20.Fiorini F., Barozzi L. The role of ultrasonography in the study of medical nephropathy. J Ultrasound. 2007;10(4):161–167. doi: 10.1016/j.jus.2007.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Manley J.A., O’Neill W.C. How echogenic is echogenic? Quantitative acoustics of the renal cortex. Am J Kidney Dis. 2001;37(4):706–711. doi: 10.1016/s0272-6386(01)80118-9. [DOI] [PubMed] [Google Scholar]
- 22.Moghazi S., Jones E., Schroepple J., et al. Correlation of renal histopathology with sonographic findings. Kidney Int. 2005;67(4):1515–1520. doi: 10.1111/j.1523-1755.2005.00230.x. [DOI] [PubMed] [Google Scholar]
- 23.Page J.E., Morgan S.H., Eastwood J.B., et al. Ultrasound findings in renal parenchymal disease: comparison with histological appearances. Clin Radiol. 1994;49(12):867–870. doi: 10.1016/s0009-9260(05)82877-6. [DOI] [PubMed] [Google Scholar]
- 24.Faubel S., Patel N.U., Lockhart M.E., Cadnapaphornchai M.A. Renal relevant radiology: use of ultrasonography in patients with AKI. Clin J Am Soc Nephrol. 2014;9(2):382–394. doi: 10.2215/CJN.04840513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Browne R.F.J., Tuite D.J. Imaging of the renal transplant: comparison of MRI with duplex sonography. Abdom Imaging. 2006;31(4):461–482. doi: 10.1007/s00261-005-0394-5. [DOI] [PubMed] [Google Scholar]
- 26.Gulati M., Cheng J., Loo J.T., Skalski M., Malhi H., Duddalwar V. Pictorial review: renal ultrasound. Clin Imaging. 2018;51(September–October 2018):133–154. doi: 10.1016/j.clinimag.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 27.Al-Katib S., Shetty M., Jafri S.M., Jafri S.Z. Radiologic assessment of native renal vasculature: a multimodality review. Radiographics. 2017;37(1):136–156. doi: 10.1148/rg.2017160060. [DOI] [PubMed] [Google Scholar]
- 28.Williams G.J., Macaskill P., Chan S.F., et al. Comparative accuracy of renal duplex sonographic parameters in the diagnosis of renal artery stenosis: paired and unpaired analysis. AJR Am J Roentgenol. 2007;188(3):798–811. doi: 10.2214/AJR.06.0355. [DOI] [PubMed] [Google Scholar]
- 29.Whittier W.L. Complications of the percutaneous kidney biopsy. Adv Chronic Kidney Dis. 2012;19(3):179–187. doi: 10.1053/j.ackd.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 30.Chen P., Maklad N., Redwine M. Color and power Doppler imaging of the kidneys. World J Urol. 1998;16(1):41–45. doi: 10.1007/s003450050024. [DOI] [PubMed] [Google Scholar]
- 31.Platt J.F., Ellis J.H., Rubin J.M., DiPietro M.A., Sedman A.B. Intrarenal arterial Doppler sonography in patients with nonobstructive renal disease: correlation of resistive index with biopsy findings. AJR Am J Roentgenol. 1990;154(6):1223–1227. doi: 10.2214/ajr.154.6.2110732. [DOI] [PubMed] [Google Scholar]
- 32.Gigante A., Barbano B., Di Mario F., et al. Renal parenchymal resistance in patients with biopsy proven glomerulonephritis: correlation with histological findings. Int J Immunopathol Pharmacol. 2016;29(3):469–474. doi: 10.1177/0394632016645590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sugiura T., Nakamori A., Wada A., Fukuhara Y. Evaluation of tubulointerstitial injury by Doppler ultrasonography in glomerular diseases. Clin Nephrol. 2004;61(2):119–126. doi: 10.5414/cnp61119. [DOI] [PubMed] [Google Scholar]
- 34.Ikee R., Kobayashi S., Hemmi N., et al. Correlation between the resistive index by Doppler ultrasound and kidney function and histology. Am J Kidney Dis. 2005;46(4):603–609. doi: 10.1053/j.ajkd.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 35.Kirkpantur A., Yilmaz R., Baydar D.E., et al. Utility of the Doppler ultrasound parameter, resistive index, in renal transplant histopathology. Transplant Proc. 2008;40(1):104–106. doi: 10.1016/j.transproceed.2007.11.032. [DOI] [PubMed] [Google Scholar]
- 36.Garcia-Covarrubias L., Martinez A., Morales-Buenrostro L.E., et al. Parameters of Doppler ultrasound at five days posttransplantation as predictors of histology and renal function at one year. Transplant Proc. 2010;42(1):262–265. doi: 10.1016/j.transproceed.2009.11.027. [DOI] [PubMed] [Google Scholar]
- 37.Heine G.H., Reichart B., Ulrich C., Köhler H., Girndt M. Do ultrasound renal resistance indices reflect systemic rather than renal vascular damage in chronic kidney disease? Nephrol Dial Transplant. 2007;22(1):163–170. doi: 10.1093/ndt/gfl484. [DOI] [PubMed] [Google Scholar]
- 38.Bigé N., Lévy P.P., Callard P., et al. Renal arterial resistive index is associated with severe histological changes and poor renal outcome during chronic kidney disease. BMC Nephrol. 2012;13(1):1–9. doi: 10.1186/1471-2369-13-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Milovanceva-Popovska M., Dzikova S. Progression of diabetic nephropathy: value of intrarenal resistive index (RI) Prilozi. 2007;28(1):69–79. [PubMed] [Google Scholar]
- 40.Nezami N., Tarzamni M.K., Argani H., Nourifar M. Doppler ultrasonographic indices after renal transplantation as renal function predictors. Transplant Proc. 2008;40(1):94–99. doi: 10.1016/j.transproceed.2007.11.036. [DOI] [PubMed] [Google Scholar]
- 41.McArthur C., Geddes C.C., Baxter G.M. Early measurement of pulsatility and resistive indexes: correlation with long-term renal transplant function. Radiology. 2011;259(1):278–285. doi: 10.1148/radiol.10101329. [DOI] [PubMed] [Google Scholar]
- 42.Platt J.F. Imaging: refining noninvasive ultrasound evaluation of the kidneys. Nat Rev Nephrol. 2012;8(10):557–558. doi: 10.1038/nrneph.2012.192. [DOI] [PubMed] [Google Scholar]
- 43.O’Neill W.C. Renal resistive index: a case of mistaken identity. Hypertension. 2014;64(5):915–917. doi: 10.1161/HYPERTENSIONAHA.114.04183. [DOI] [PubMed] [Google Scholar]
- 44.de Freminville J.B., Vernier L.M., Roumy J., et al. Impact on renal resistive index of diabetes in renal transplant donors and recipients: a retrospective analysis of 1827 kidney transplant recipients. J Clin Hypertens (Greenwich) 2019;21(3):382–389. doi: 10.1111/jch.13492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Seiler S., Colbus S.M., Lucisano G., et al. Ultrasound renal resistive index is not an organ-specific predictor of allograft outcome. Nephrol Dial Transplant. 2012;27(8):3315–3320. doi: 10.1093/ndt/gfr805. [DOI] [PubMed] [Google Scholar]
- 46.Grün O.S., Herath E., Weihrauch A., et al. Does the measurement of the difference of resistive indexes in spleen and kidney allow a selective assessment of chronic kidney injury? Radiology. 2012;264(3):894–902. doi: 10.1148/radiol.12111533. [DOI] [PubMed] [Google Scholar]
- 47.Chang E.H. An introduction to contrast-enhanced ultrasound for nephrologists. Nephron. 2018;138(3):176–185. doi: 10.1159/000484635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zeisbrich M., Kihm L.P., Drüschler F., Zeier M., Schwenger V. When is contrast-enhanced sonography preferable over conventional ultrasound combined with Doppler imaging in renal transplantation? Clin Kidney J. 2015;8(5):606–614. doi: 10.1093/ckj/sfv070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tenant S.C., Gutteridge C.M. The clinical use of contrast-enhanced ultrasound in the kidney. Ultrasound. 2016;24(2):94–103. doi: 10.1177/1742271X15627185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chang E.H., Chong W.K., Kasoji S.K., et al. Diagnostic accuracy of contrast-enhanced ultrasound for characterization of kidney lesions in patients with and without chronic kidney disease. BMC Nephrol. 2017;18(1):1–13. doi: 10.1186/s12882-017-0681-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ma F., Cang Y., Zhao B., et al. Contrast-enhanced ultrasound with SonoVue could accurately assess the renal microvascular perfusion in diabetic kidney damage. Nephrol Dial Transplant. 2012;27(7):2891–2898. doi: 10.1093/ndt/gfr789. [DOI] [PubMed] [Google Scholar]
- 52.Dong Y., Wang W.P., Cao J., Fan P., Lin X. Early assessment of chronic kidney dysfunction using contrast-enhanced ultrasound: a pilot study. Br J Radiol. 2014;87(1042):20140350. doi: 10.1259/bjr.20140350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Girometti R., Stocca T., Serena E., Granata A., Bertolotto M. Impact of contrast-enhanced ultrasound in patients with renal function impairment. World J Radiol. 2017;9(1):10–16. doi: 10.4329/wjr.v9.i1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jeong S., Park S.B., Kim S.H., Hwang J.H., Shin J. Clinical significance of contrast-enhanced ultrasound in chronic kidney disease: a pilot study. J Ultrasound. 2019;22(4):453–460. doi: 10.1007/s40477-019-00409-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fischer T., Dieckhöfer J., Mühler M., et al. The use of contrast-enhanced US in renal transplant: first results and potential clinical benefit. Eur Radiol. 2005;15(5):E109–E116. doi: 10.1007/s10406-005-0173-y. [DOI] [PubMed] [Google Scholar]
- 56.Yang C., Wu S., Yang P., et al. Prediction of renal allograft chronic rejection using a model based on contrast-enhanced ultrasonography. Microcirculation. 2019;26(6) doi: 10.1111/micc.12544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hai Y., Chong W., Liu J.B., Forsberg F., Eisenbrey J. The diagnostic value of contrast-enhanced ultrasound for monitoring complications after kidney transplantation—a systematic review and meta-analysis. Acad Radiol. 2021;28(8):1086–1093. doi: 10.1016/j.acra.2020.05.009. [DOI] [PubMed] [Google Scholar]
- 58.Abeysekera J. University of British Columbia; Vancouver, Canada: 2016. Three-Dimensional Ultrasound Elasticity Imaging. Dissertation. [Google Scholar]
- 59.Schneider C. University of British Columbia; Vancouver, Canada: 2017. Ultrasound Elastography for Intra-Operative Use and Renal Tissue Imaging. Dissertation. [Google Scholar]
- 60.Whittier W.L., Lewis E.J. In: National Kidney Foundation Primer on Kidney Diseases. 6th ed. Gilbert S.J., Weiner D.E., Gipson D.S., Perazella M.A., Tonelli M., editors. Elsevier Saunders; 2014. Pathophysiology of chronic kidney disease; pp. 448–457. [Google Scholar]
- 61.Menzilcioglu M.S., Duymus M., Citil S., et al. Strain wave elastography for evaluation of renal parenchyma in chronic kidney disease. Br J Radiol. 2015;88(1050):20140714. doi: 10.1259/bjr.20140714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bob F., Grosu I., Sporea I., et al. Ultrasound-based shear wave elastography in the assessment of patients with diabetic kidney disease. Ultrasound Med Biol. 2017;43(10):2159–2166. doi: 10.1016/j.ultrasmedbio.2017.04.019. [DOI] [PubMed] [Google Scholar]
- 63.Wang L., Xia P., Lv K., et al. Assessment of renal tissue elasticity by acoustic radiation force impulse quantification with histopathological correlation: preliminary experience in chronic kidney disease. Eur Radiol. 2014;24(7):1694–1699. doi: 10.1007/s00330-014-3162-5. [DOI] [PubMed] [Google Scholar]
- 64.Hassan K., Loberant N., Abbas N., Fadi H., Shadia H., Khazim K. Shear wave elastography imaging for assessing the chronic pathologic changes in advanced diabetic kidney disease. Ther Clin Risk Manag. 2016;12:1615–1622. doi: 10.2147/TCRM.S118465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Leong S.S., Wong J.H., Md Shah M.N., Vijayananthan A., Jalalonmuhali M., Ng K.H. Shear wave elastography in the evaluation of renal parenchymal stiffness in patients with chronic kidney disease. Br J Radiol. 2018;91(1089):20180235. doi: 10.1259/bjr.20180235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gao J., Weitzel W., Rubin J.M., et al. Renal transplant elasticity ultrasound imaging: correlation between normalized strain and renal cortical fibrosis. Ultrasound Med Biol. 2013;39(9):1536–1542. doi: 10.1016/j.ultrasmedbio.2013.04.007. [DOI] [PubMed] [Google Scholar]
- 67.Wang H.K., Lai Y.C., Lin Y.H., Chiou H.J., Chou Y.H. Acoustic radiation force impulse imaging of the transplant kidney: correlation between cortical stiffness and arterial resistance in early post-transplant period. Transplant Proc. 2017;49(5):1001–1004. doi: 10.1016/j.transproceed.2017.03.045. [DOI] [PubMed] [Google Scholar]
- 68.Stock K.F., Klein B.S., Vo Cong M.T., et al. ARFI-based tissue elasticity quantification in comparison to histology for the diagnosis of renal transplant fibrosis. Clin Hemorheol Microcirc. 2010;46(2-3):139–148. doi: 10.3233/CH-2010-1340. [DOI] [PubMed] [Google Scholar]
- 69.Syversveen T., Midtvedt K., Berstad A.E., Brabrand K., Strøm E.H., Abildgaard A. Tissue elasticity estimated by acoustic radiation force impulse quantification depends on the applied transducer force: an experimental study in kidney transplant patients. Eur Radiol. 2012;22(10):2130–2137. doi: 10.1007/s00330-012-2476-4. [DOI] [PubMed] [Google Scholar]
- 70.Grenier N., Poulain S., Lepreux S., et al. Quantitative elastography of renal transplants using supersonic shear imaging: a pilot study. Eur Radiol. 2012;22(10):2138–2146. doi: 10.1007/s00330-012-2471-9. [DOI] [PubMed] [Google Scholar]
- 71.Early H.M., Cheang E.C., Aguilera J.M., et al. Utility of shear wave elastography for assessing allograft fibrosis in renal transplant recipients: a pilot study. J Ultrasound Med. 2017;37(6):1455–1465. doi: 10.1002/jum.14487. [DOI] [PubMed] [Google Scholar]
- 72.Urban M.W., Vasconcelos L., Kijanka P. Using multiparametric ultrasound-based elastographic characterization for evaluation of renal transplants. J Acoust Soc Am. 2019;146(4) 2863-2863. [Google Scholar]
- 73.Peride I., Rădulescu D., Niculae A., Ene V., Bratu O.G., Checheriță I.A. Value of ultrasound elastography in the diagnosis of native kidney fibrosis. Med Ultrason. 2016;18(3):362–369. doi: 10.11152/mu.2013.2066.183.per. [DOI] [PubMed] [Google Scholar]
- 74.Gennisson J.L., Grenier N., Combe C., Tanter M. Supersonic shear wave elastography of in vivo pig kidney: influence of blood pressure, urinary pressure and tissue anisotropy. Ultrasound Med Biol. 2012;38(9):1559–1567. doi: 10.1016/j.ultrasmedbio.2012.04.013. [DOI] [PubMed] [Google Scholar]
- 75.Gao J., Thai A., Lee J., Fowlkes J.B. Ultrasound shear wave elastography and Doppler sonography to assess the effect of hydration on human kidneys: a preliminary observation. Ultrasound Med Biol. 2020;46(5):1179–1188. doi: 10.1016/j.ultrasmedbio.2020.01.011. [DOI] [PubMed] [Google Scholar]
- 76.Sigrist R.M., Liau J., Kaffas A.E., Chammas M.C., Willmann J.K. Ultrasound elastography: review of techniques and clinical applications. Theranostics. 2017;7(5):1303–1329. doi: 10.7150/thno.18650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ma I.W., Steinmetz P., Weerdenburg K., et al. The Canadian medical student ultrasound curriculum. J Ultrasound Med. 2020;39(7):1279–1287. doi: 10.1002/jum.15218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Reisinger N., Koratala A., Goral S. Use of point-of-care ultrasound to assess CKD. Am J Kidney Dis. 2021;77(1):A16–A19. doi: 10.1053/j.ajkd.2020.06.021. [DOI] [PubMed] [Google Scholar]
- 79.Chen Q., Yu J., Rush B.M., Stocker S.D., Tan R.J., Kim K. Ultrasound super-resolution imaging provides a noninvasive assessment of renal microvasculature changes during mouse acute kidney injury. Kidney Int. 2020;98(2):355–365. doi: 10.1016/j.kint.2020.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hossain M.M., Detwiler R.K., Chang E.H., et al. Mechanical anisotropy assessment in kidney cortex using ARFI peak displacement: preclinical validation and pilot in vivo clinical results in kidney allografts. IEEE Trans Ultrason Ferroelectr Freq Control. 2019;66(3):551–562. doi: 10.1109/TUFFC.2018.2865203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hysi E., He X., Fadhel M.N., et al. Photoacoustic imaging of kidney fibrosis for assessing pretransplant organ quality. JCI Insight. 2020;5(10) doi: 10.1172/jci.insight.136995. [DOI] [PMC free article] [PubMed] [Google Scholar]