This review traces the separate discoveries of dendritic cells, cross-priming, and help for cytotoxic T cell responses. The authors document the gradual convergence of these discoveries into the current models of cell-mediated immunity, spotlighting unanswered questions and future directions.
Abstract
Last year was the 10th anniversary of Ralph Steinman’s Nobel Prize awarded for his discovery of dendritic cells (DCs), while next year brings the 50th anniversary of that discovery. Current models of anti-viral and anti-tumor immunity rest solidly on Steinman’s discovery of DCs, but also rely on two seemingly unrelated phenomena, also reported in the mid-1970s: the discoveries of “help” for cytolytic T cell responses by Cantor and Boyse in 1974 and “cross-priming” by Bevan in 1976. Decades of subsequent work, controversy, and conceptual changes have gradually merged these three discoveries into current models of cell-mediated immunity against viruses and tumors.
Introduction
Current models of anti-viral or anti-tumor immunity incorporate many interactions between various types of cells and many participating surface or signaling molecules and downstream pathways. The main effector cells are CD8 T cells recognizing antigens specific to viruses or tumors. These cells are primed by type I classical dendritic cells (cDC1s) that capture material from virally infected cells or tumor cells and present their antigens on MHC class I (MHC-I) molecules. These DCs can be “licensed” for effective priming by CD4 T cells that recognize antigen on MHC class II (MHC-II) molecules presented by the same cDC1. Recent work has confirmed or slightly advanced many details of this model, but it may be surprising that the essential features of these models were discovered nearly 50 yr ago.
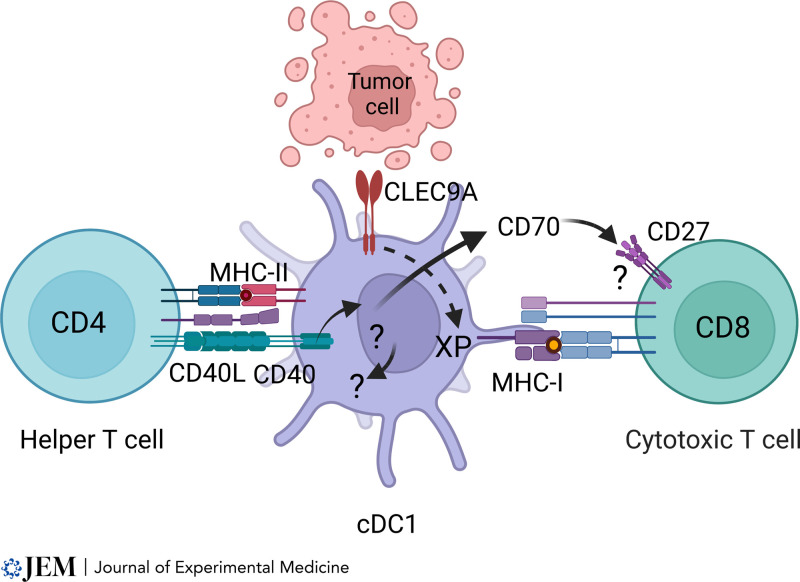
There are three essential features in today’s current model (Laidlaw et al., 2016; Borst et al., 2018; Murphy and Murphy, 2022; Fig. 1). First, T cell priming is performed by a specialized APC belonging to DC lineages, which is separate from other types of APCs such macrophages, monocyte-derived DCs, or B cells. Second, CD8 T cell priming requires a specialized pathway of antigen processing in which exogenous antigens are captured and processed for loading MHC-I molecules, known as cross-presentation. Third, CD4 T cells “help” the priming of CD8 T cells by stimulating CD40 signaling in cDC1s that present cognate antigens on MHC-II molecules.
Figure 1.
A developing scheme for CD4 T cell–mediated help for CTL responses. The cDC1 subset of cDCs can serve as an autonomous platform for priming both CD4 and CD8 T cells. The cDC1 captures and process cell-associated antigens for presentation by MHC-II molecules and cross-presentation (XP) for MHC-I molecules. CD4 T cell engagement induces surface expression of its CD40 ligand, stimulating CD40 signaling in cDC1 cells. This signaling enhances priming of CD8 T cells through mechanisms that remain incompletely defined, including induction of CD70 and potentially other costimulatory ligands, as well as DC-intrinsic effects.
It is of some historical interest that these ideas all originated from independent discoveries made between 1973 and 1976, all published in JEM. In 1973, Steinman and Cohn reported the discovery of a new immune lineage they called “dendritic cells” (Steinman and Cohn, 1973). This discovery led to DCs eventually being recognized not only as distinct from macrophages, but also as comprising diverse subsets with distinct immune functions. In 1975, Cantor and Boyse reported the cooperation between different types of T cells in generating cytolytic T cell responses (Cantor and Boyse, 1975a). A long thread of subsequent studies on “help” led to today’s current appreciation of “DC licensing” via CD40 signaling that enhances CD8 T cell responses. In 1976, Bevan reported the phenomenon of in vivo “cross-priming” (Bevan, 1976) at a time when the nature of T cell recognition of antigen was poorly understood. As the field of antigen processing developed, the idea of processing exogenously derived antigens for presentation on MHC-I molecules remained controversial for decades, but is now firmly established as essential for many anti-viral responses and most anti-tumor immunity.
From today’s technically advanced viewpoint, it may be difficult to appreciate the importance of these original observations. Steinman’s original report of DCs is mostly descriptive, lacking the kind of functional data that is required for most reports today (Steinman and Cohn, 1973). The discovery of help for cytolytic T cell (CTL) responses by Cantor and Boyse uses archaic terminology, hindering ready accessibility (Cantor and Boyse, 1975a). Bevan’s cross-priming discovery relies on mouse genetics, somewhat unfamiliar to today’s students compared with more recent techniques (Bevan, 1976). These studies were published a decade before there was a solid understanding of how T cells recognize antigens (Shimonkevitz et al., 1984; Townsend et al., 1985). Moreover, the discovery of help for CTLs and cross-priming relied heavily on congenic mouse strains that allowed attribution of responses to specific elements of the H-2 locus (Snell, 1958; Snell and Jackson, 1958). As we will see, the first demonstration of cross-priming required use of specific congenic lines B10 and B10.D2 (Snell and Jackson, 1958), as well as BALB/c and BALB.B congenic strains (Freedman and Lilly, 1975). As such, these discoveries relied extensively on previous work by George Snell and others on tumor transplantation that generated these critical reagents. Here, we review the origins of these discoveries and trace their development and gradual fusion to form current models of cell-mediated immunity.
Origins of DCs as drivers of adaptive immunity
DCs as a distinct lineage
The discovery of DCs as a distinct type of immune cell originates from a paper published in the JEM in 1973 (Steinman and Cohn, 1973). This report was a morphological description of DCs without functional evidence of their importance, unlike current expectations of complete “stories” (Snyder, 2013). But this was only the first of a long series of studies by Steinman and colleagues, building a picture of DCs as a distinct immune lineage having critical and unique functions in adaptive immunity (Steinman et al., 1974; Steinman and Cohn, 1974; Steinman et al., 1975; Steinman et al., 1979; Nussenzweig and Steinman, 1980; Steinman et al., 1980), for which Steinman was awarded the 2011 Nobel Prize.
The discovery of DCs may have been partially motivated by earlier work that suggested the idea of “persistence of immunogenicity” in macrophages reported by Unanue in JEM (Unanue and Askonas, 1968) and elsewhere (Unanue, 1969; Unanue et al., 1969). Unanue’s studies originated the concept of antigen processing and stimulated interest in the fate of proteinaceous antigens following immunization. In the year before their discovery of DCs, Steinman and Cohn carried out work in an attempt to follow up this proposal by examining the fate of proteins such as horseradish peroxidase after phagocytosis by macrophages (Steinman and Cohn, 1972a; Steinman and Cohn, 1972b). Although their results were “difficult to equate” with the “persistence of protein antigens” (Steinman and Cohn, 1972b), they nonetheless may have motivated their examination of cells capable of capturing and processing antigens.
Subsequent work showed that DCs were distinct from other known lymphocytes or phagocytes (Steinman and Cohn, 1974), uncovered their rapid turnover and bone marrow origin (Steinman et al., 1974), identified their presence in mouse spleen (Steinman et al., 1975), showed their potency in primary mixed lymphocyte reactions (Steinman and Witmer, 1978), documented their high expression of MHC-II molecules (Steinman et al., 1979), and demonstrated their activity in the syngeneic mixed leukocyte reaction (Nussenzweig and Steinman, 1980). However, like the “persistence of immunogenicity,” the importance of DCs was also not appreciated universally at first. As recounted by William Paul, the early use of the mixed lymphocyte reaction to show DC’s capacity to expand T cells (Steinman and Witmer, 1978) led to uncertainty among some contemporary immunologists as to “the proper interpretation of the mixed leukocyte reaction data” (Paul, 2011). However, several years later, DCs were shown to be powerful APCs for T cells as well (Nussenzweig et al., 1980). Nonetheless, similarities between DCs and other myeloid lineages continued to be the basis for lingering reluctance in accepting DCs as a distinct lineage devoted to T cell priming (Hume, 2008).
DCs as a heterogeneous group of cells
By the 1990s, DCs were recognized to comprise subtypes distinguished by distinct surface markers (Suss and Shortman, 1996; Kronin et al., 1996; Vremec et al., 1992; Wu et al., 1996; Shortman et al., 1995). The field today distinguishes cDCs studied by Steinman from plasmacytoid DCs (pDCs; Cella et al., 1999; Siegal et al., 1999). At least in murine models, it seems well established that only cDCs directly participate in presentation of antigens to T cells, while pDCs modify responses by secreting cytokines in response to the detection of viral infection (Swiecki and Colonna, 2015). The first monoclonal antibody to selectively identify cDCs, 33D1 (Nussenzweig and Steinman, 1982), was soon joined by NLDC-145, which recognizes DEC-205 (Jiang et al., 1995). CD8α+ was found to mark a subset of thymic-derived DCs (Shortman et al., 1995), and splenic cDCs subsets were distinguished on the basis of non-overlapping patterns of CD4 and CD8 expression (Shortman and Liu, 2002). Current surface markers used to distinguish murine cDCs include CD24, XCR1, CD172, and CD103 (Naik et al., 2007).
More recent work on DC development and function has been covered in several reviews (Liu and Nussenzweig, 2010; Merad et al., 2013; Murphy et al., 2016; Shortman and Heath, 2010; Durai and Murphy, 2016; Yin et al., 2021). Some notable findings include the demonstration that distinct DC subsets exhibit inherently different efficiencies for processing antigens for presentation by MHC-I and MHC-II molecules (Dudziak et al., 2007; Lehmann et al., 2017). cDC1s are preferentially specialized for MHC-I antigen processing and cDC2s for MHC-II antigen processing. However, the form of antigen, such as whether it is delivered as a soluble protein or in a cell-associated form, can also influence the efficiency of antigen presentation by DCs. Thus, studies have shown that cDC1 can process and present cell-associated antigens by MHC-II molecules (Kamphorst et al., 2010; Iyoda et al., 2002). This was confirmed using genetic systems that allow for the elimination of cDC1 in vivo (Hildner et al., 2008; Durai et al., 2019) or selective gene inactivation in cDC1 (Ferris et al., 2020). Currently, there is much activity aimed at understanding the different roles of DC subsets in directing effective immune responses to different types of pathogens (Anderson et al., 2018).
Origins of cross-priming and cross-presentation
By the mid-1960s, lymphocyte function was divided into antibody-dependent humoral immunity and cell-mediated immunity (Cooper et al., 1966). For cell-mediated immunity, an early in vitro assay of lymphocyte function measured the release of C14-thymidine from labeled target cells (Vainio et al., 1964), but an improved method based on Cr51 labeling soon became universal (Brunner et al., 1968). Zinkernagel and Doherty used this assay to uncover the remarkable finding that in vitro killing of virally infected target cells by CTLs primed in vivo against lymphocytic choriomeningitis was “restricted by the H-2 gene complex” (Zinkernagel and Doherty, 1974). Their results sparked a series of studies by Bevan that directly led to discovery of cross-priming (Bevan, 1976), later renamed cross-presentation (Carbone and Bevan, 1990).
Origins from studies of alloimmunization
The process we now call cross-presentation originated from a series of studies examining the in vitro behavior of CTLs induced in vivo against alloantigens, in contrast to the in vivo priming against lymphocytic choriomeningitis infections used by Zinkernagel and Doherty (1974). CTLs induced in vivo by alloantigens were monospecific for recognition of H-2 gene products (Bevan, 1975a). Further, these studies showed that differences in minor histocompatibility (H) alleles (alleles not encoded in the H-2 locus) could induce CTL responses that were H-2 restricted (Bevan, 1975b). These studies used mouse strains of different backgrounds, such as B10.D2 and BALB/c, harboring different minor H-2 alleles but sharing the same H-2 region. Immunization of BALB/c (H-2d) mice with spleen cells from B10.D2 (H-2d) mice generated CTLs restricted by H-2d, but that were reactive only to antigens derived from the B10 background. This suggested that CTLs recognized antigens “created by an H-2 coded modification of the products of non-H-2 coded genes—probably minor histocompatibility genes” (Bevan, 1975b) in agreement with the recently discovered H-2 restriction.
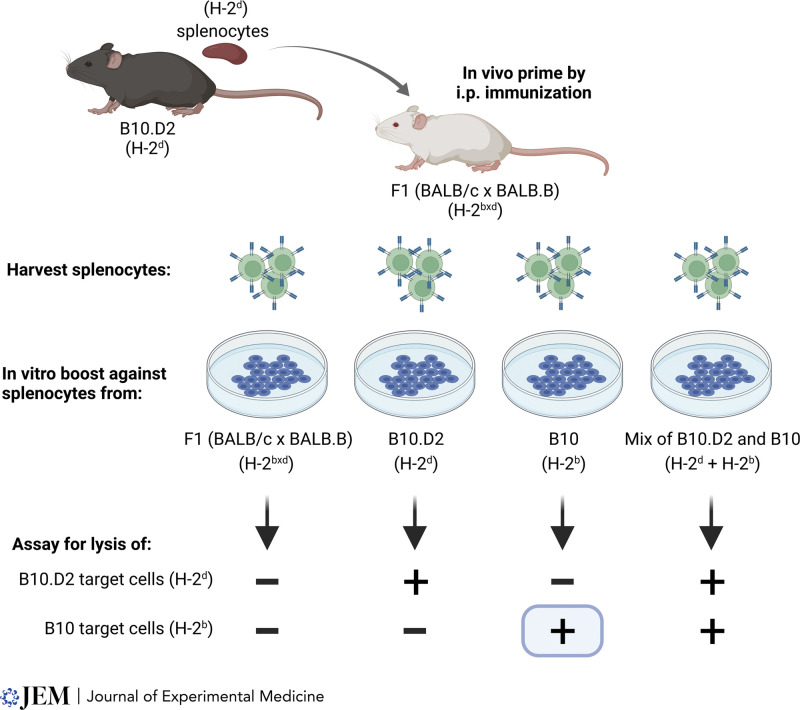
The first experimental evidence for cross-priming arose from somewhat more complicated experiments using F1 mice of mixed H-2 composition (Fig. 2). CTLs were analyzed from F1 (BALB/c x BALB.B; H-2dxb) mice that were immunized with cells from B10.D2 (H-2d) mice (Bevan, 1976). CTLs primed in this way were able to lyse targets from B10.D2 (H-2d) mice, as expected, since these cells were the original immunizing antigen. But somewhat unexpectedly, these CTLs also lysed target cells derived from B10 (H-2b) mice, which were syngeneic to the host and of a different H-2 allele from the original immunizing antigen. This cross-priming referred to induction of an H-2b–restricted response from immunization with H-2d cells, seemingly inconsistent with H-2 restriction. These results were soon confirmed (Matzinger and Bevan, 1977). One interpretation was that “H-2 restriction does not hold during” the priming stage of CTL induction (Matzinger and Bevan, 1977). However, an alternative interpretation was suggested in 1977 that “a host antigen-presenting cells is involved.” Continuing, Bevan explained that “B10 cells injected into an F1 (C x C.B) are disrupted, and the minor H antigens are picked up by F1 presenting cells which carry both H-2b and H-2d.” This process is, essentially, as we describe cross-presentation today. This was a remarkable insight, given that the nature of T cell antigen recognition was still a mystery.
Figure 2.
Cross-priming for a secondary cytotoxic response to minor H antigens. Splenocytes from B10.D2 mice were used to immunize F1 (BALB/c x BALB.B) mice to induce CTL specific for minor H-2 antigens differing between the B10 and BALB/c backgrounds. After in vivo priming, lymphocytes from immunized F1 mice were boosted in vitro against irradiated splenocytes from F1 (BALB/c x BALB.B) mice, B10.D2 mice, B10 mice, or an equal mixture of splenocytes from B10.D2 and B10 mice. CTL activity was then assayed against target cells from B10.D2 or B10 mice. Cytolysis of B10.D2 targets is consistent with priming by direction of the immunizing B10.D2 cell and does not require an explanation by cross-presentation. In contrast, cytolysis of B10 targets cannot be explained by direct priming by the immunizing cells, suggesting that minor antigens from the B10 background were recognized in vivo by CTLs in the context of the host H-2b allele. This was cross-priming. Adapted from Bevan (1976).
Bevan’s original report of cross-priming cited previous literature that was interpreted as consistent with cross-priming in vivo (Snell et al., 1957; Martinez et al., 1959; Gasser and Silvers, 1972). Snell’s studies of H antigens relied on production and analysis of inbred recombinant lines, called congenic resistant lines, tested for susceptibility or resistance to tumors (typically a radiation-induced leukemia) that were derived from other strains. For the majority of congenic resistant lines analyzed, tumor resistance was linked to the H-2 locus. Non–H-2 loci could also mediate resistance, although this was typically weaker and occasionally allowed tumors to overwhelm the H locus barrier. To improve the assay’s discrimination for weaker H antigens, Snell developed a new method of typing inbred strains of mice for H antigens (Snell et al., 1957). This involved the introduction of a prior immunization of mice with a normal tissue (thymus) from another strain, followed by a challenge with that strain’s leukemia. Use of this method allowed for better discrimination of weaker histocompatibility differences, now called minor H antigens. Cross-priming against minor H alleles could explain the basis for this enhanced sensitivity. Notably, Snell himself directed subsequent work confirming in vivo cross-priming, as reported by Murasko (1978). In that study, BALB/c (H-2d) mice grafted first with B10 (H-2b) tail skin acquired effector cells capable of rejecting a second-set graft of H-2 compatible B10.D2 (H-2d) skin. This second-set rejection indicates that CTLs from the BALB/C host recognized minor H antigens from the B10 background presented by H-2d alleles, suggesting they were originally induced by BALB/c host APCs through cross-priming.
Subsequent studies of cross-priming
In the decade following its discovery, cross-presentation was not a topic of intense activity, as greater interest focused on the nature of antigen recognition by T cells. However, as early as 1980, a requirement for antigen processing for CTL responses against minor H-2 was suggested by the inability of glutaraldehyde-fixed allogeneic donor cells to induce robust CTL responses to minor H-2 antigens (Korngold and Sprent, 1980). The subsequent years had rapid progress in the molecular basis for antigen recognition. First, antigens presented by MHC-II molecules were discovered to be inhibited by chloroquine (Ziegler and Unanue, 1982) and shown to be small peptides derived from the antigen (Shimonkevitz et al., 1983; Shimonkevitz et al., 1984; Babbitt et al., 1985). Later, antigens presented by MHC-I molecules were shown also to be small peptides (Townsend et al., 1984; Townsend et al., 1985; Townsend et al., 1986), culminating with the structure of the MHC-I molecule and its peptide ligand (Bjorkman et al., 1987b; Bjorkman et al., 1987a).
Between 1976 and 1990, follow-up studies examined suppression of CTL activity by cross-presented antigens, again suggesting that host APCs “reprocess and present these minor H antigens in conjunction with both H-2 A and H-2 B” (Fink et al., 1983). In 1987, Bevan wrote that a “plausible way to take cellular antigens that are exogenous and to present them as endogenous, class I–associated antigens is via specialized APCs that phagocytose large cellular debris and shuttle the resulting peptide degradation products to their endogenous class I presenting system. Such a phagocytic cell may or may not express class II molecules” (Bevan, 1987).
The clarity of this explanation was not universally appreciated. The prevailing notion that emerged during this time was that MHC-I and MHC-II antigen processing pathways were dedicated solely to either cell-intrinsic or exogenously derived antigens, respectively, with the suggestion that MHC-I “processing may occur in a region of the transitional Golgi specialized for dealing with improperly folded proteins synthesized by the cell” (Germain, 1986). Evidence from in vitro recognition of infected target cells supported an intracellular origin for antigen in loading MHC-I (Morrison et al., 1986). Further, fusogenic activity of a virus was required for its loading onto MHC-I in vitro (Yewdell et al., 1988), which was interpreted as consistent with a purely cell-intrinsic pathway. Importantly, both of these studies were interrogated in only target cells and not professional APCs. By contrast, Bevan reasoned, “if the only cell capable of presenting antigen to class I–restricted T cells is the infected cell itself, then sensitization would have to occur peripherally in the case of a virus that did not productively infect cells in the lymphoid organs” (Bevan, 1987). In short, without cross-priming, CTL responses would need to be primed directly by infected somatic cells, and not by “professional APCs.”
Revived interest and confirmation
During the early 1990s, interest in cross-presentation was revived as numerous reports confirmed that cross-presentation could occur in vivo under various conditions, while a few studies disagreed. For a third time, Bevan demonstrated in vivo cross-priming, this time using splenocytes pulsed with exogenous proteins as immunogens and conditions similar to his original experiments (Carbone and Bevan, 1990), and also introduced the term cross-presentation for this process. Cross-presentation was soon confirmed by several groups, which showed CTLs can be primed in vivo in response to immunization with protein-pulsed DCs (Inaba et al., 1990) or soluble proteins (Rock et al., 1990), and by proteins delivered using liposomes (Reddy et al., 1992; Collins et al., 1992; Pfeifer et al., 1993). Additionally, cross-presentation was demonstrated to occur in macrophages in vitro (Kovacsovics-Bankowski et al., 1993), although the APC responsible for CTL priming in vivo remained unclear. Some evidence arguing against a need for cross-presentation by professional APCs arose from the demonstration that fibroblasts harboring antigens could induce MHC-restricted CTL responses (Kündig et al., 1995). However, later work would show that CTL responses are not induced directly by virally infected cells and instead rely on bone marrow (BM)–derived cells for this function (Sigal et al., 1999).
The physiologic role of cross-presentation and the identity of the APC responsible for it began to emerge in the next decade. A role for cross-presentation in generating CTL responses to tumors was implied by transference of MHC-I–restricted tumor antigens to BM-derived APCs (Huang et al., 1994). Cross-presentation of exogenous self-antigens was shown to induce deletion of auto-reactive CD8 T cells (Kurts et al., 1997). The capture of apoptotic cells by DCs, but not by macrophages, triggered cross-presentation for the induction of CTL responses in vivo (Albert et al., 1998). Bevan developed a method of delivering antigen in a cell-associated form that is incapable of direct presentation by using β2m−/− cells that were osmotically loaded with OVA as an immunogen (den Haan et al., 2000). With this method, a previously identified DC subset, CD8α+ DCs (Crowley et al., 1989; Ardavin and Shortman, 1992; Vremec et al., 1992), but not CD8α− DCs, were shown to be capable of capturing and presenting cell-associated antigens to CD8 T cells in vivo. This was confirmed and extended to soluble protein cross-presentation as well (Pooley et al., 2001). Finally, CD11c-expressing DCs were demonstrated to be sufficient for in vivo cross-presentation in mice engineered to express MHC-I molecules only on DCs (Kurts et al., 2001).
Some evidence has suggested that human pDCs may be capable of cross-presentation in vitro (Hoeffel et al., 2007; Di Pucchio et al., 2008; Segura et al., 2013). Similar evidence was provided for murine pDCs as well (Mouries et al., 2008; Kool et al., 2011). One study showed in vivo priming using antibody-targeting to pDCs with a readout based on activation of transgenic CD4 T cells (Sapoznikov et al., 2007), not relevant to cross-presentation. Another study examined responses to soluble OVA with a readout based on OT-1 CD8 T cells (Shinohara et al., 2006). While these particular experimental settings suggest the capacity for cross-presentation by pDCs, the physiologic relevance to antiviral or antitumor responses was unclear (Colonna and Cella, 2007). Indeed, pDCs were unable to induce endogenous CTL responses unless the antigen was delivered via an anti-SiglecH antibody, despite activation of toll-like receptors (Zhang et al., 2006). Finally, pDCs appear insufficient for autonomous CTL priming, since selective cDC1 lineage ablation abrogates CTL priming to viruses and tumors (Hildner et al., 2008; Durai et al., 2019).
Cellular and molecular dissection
A period of intense investigation followed these confirmations of cross-presentation (Cruz et al., 2017), largely by analyzing BM-derived DCs (BMDCs) generated in vitro with GM-CSF (Markowicz and Engleman, 1990; Sallusto et al., 1995). Conclusions derived from this system supported both vacuolar and cytosolic pathways involving phagosomes (Houde et al., 2003), phagosome-ER fusion (Guermonprez et al., 2003), and Cathepsin S for generating peptides for a transporter associated with antigen processing–independent vacuolar pathway (Shen et al., 2004). An in vitro role for GAP junctions was suggested for cytosolic delivery of antigens from antigen-bearing cells (Neijssen et al., 2005). Genetic analysis implicated several proteins involved in lysosome and phagosome function, including NOX2 (Savina et al., 2006), Rab27a (Jancic et al., 2007), Rac2 (Savina et al., 2009), IRAP (Segura et al., 2009), Rab3b/c (Zou et al., 2009), Rab34 (Alloatti et al., 2015), and Sec61 (Zehner et al., 2015). In vitro over-expression of the transcription factor EB inhibited cross-presentation by BMDCs (Samie and Cresswell, 2015). However, the involvement of these factors in regulating in vivo cross-presentation remains to be tested (Alloatti et al., 2016; Theisen and Murphy., 2017; Murphy and Murphy, 2022).
Some studies indicated differences in how BMDCs and cDC1 carry out cross-presentation (Briseno et al., 2016; Kretzer et al., 2016). In vivo cross-presentation relies primarily on Batf3-dependent cDC1s (Hildner et al., 2008). Roles for in vivo cross-presentation have been shown for the IFN-γ–induced GTPase (Igtp; Bougneres et al., 2009), the vesicular trafficking protein Sec22b (Cebrian et al., 2011), Ras-related GTP-binding protein RAB43 (Kretzer et al., 2016), and the BEACH domain–containing protein WDFY4 (Theisen et al., 2018). DCs from Igtp−/− mice lack lipid bodies, structures composed of neutral lipids arising from the ER, and in vivo cross-presentation of cell-associated antigens is reduced about fourfold in Igtp−/− mice (Bougneres et al., 2009). Sec22b is a SNARE protein that regulates vesicular trafficking and is highly expressed in cDCs (Cebrian et al., 2011). Sec22b−/− mice exhibit reduced in vivo cross-presentation and impaired tumor rejection (Alloatti et al., 2017). However, conditional deletion of Sec22b induced by a CD11c-Cre transgene was reported to not impair in vivo cross-presentation (Wu et al., 2017), but this discrepancy has not yet been resolved. Rab43−/− mice showed about a fourfold reduction in cross-presentation in vivo, and the RAB43 protein was localized to cis-Golgi and an unidentified vesicular compartment (Kretzer et al., 2016). WDFY4 was identified in a CRISPR/Cas9 screen for cross-presentation by primary cDC1 generated in vitro by Flt3L treated BM (Theisen et al., 2018). Wdfy4−/− mice show normal cDC1 development and normal processing of MHC-II restricted antigens, but exhibited loss of in vivo cross-presentation. This defect in Wdfy4−/− mice was accompanied by the inability to make CTL responses against several viruses and tumors and a complete loss of tumor rejection. Notably, BMDCs derived from Wdfy4−/− mice showed no defect in cross-presentation in vitro.
Origins of help for CTL responses
The form of help we now recognize as CD4 T cells licensing cDC1 for CTL priming was very likely the same as the in vitro phenomenon reported by Cantor and Boyse (1975b), despite the use of Ly-1 (CD5) as a marker for the helper cell, rather than CD4 used today. Conducted well before antigen recognition by T cells was understood, this demonstration of T–T interaction may have grown from earlier ideas of T–B cooperation related to the hapten carrier effect discovered at Mill Hill a few years earlier (Mitchell and Miller, 1968). We trace this idea from these origins to its current state.
Early observations of T–T cooperation
The 1960s saw the identification of a distinct subset of lymphocytes, and the first documentation of the interactions between them. B–T cell cooperation was recognized from the discovery of the hapten-carrier effect in antibody responses (Mitchell and Miller, 1968; Boak et al., 1971). The discovery of help for CTL responses relied on newly available antibodies generated by Boyse against T cell surface proteins Ly-1 (CD5), Ly-2 (CD8α), and Ly-3 (CD8β; Boyse et al., 1968). These antibodies allowed segregation of T cells into functional subclasses (Shiku et al., 1975). Cantor and Asofsky had previously described two populations of cells in graft-versus-host responses in mice that “produced no detectable reactions when injected separately” but were “able to produce significant GVH reactions when combined” (Cantor and Asofsky, 1970). Both populations were later found to be thymus-derived lymphocytes or T cells (Cantor and Asofsky, 1972). The discovery of help for CTL responses was founded on the demonstration that killer activity was mediated by the Ly-23+ T cells and that helper activity was exhibited by Ly-1+ T cells and that this differentiation occurred prior to antigen encounter (Cantor and Boyse, 1975b). Then, using an in vitro mixed lymphocyte culture, Ly-1+ T cells were shown to amplify killer activity of Ly-23+ T cells, but without themselves acquiring killer activity (Cantor and Boyse, 1975a). Studies between 1977 and 1983 transformed this original terminology into the CD4 and CD8 classification used today (Chess, 2006).
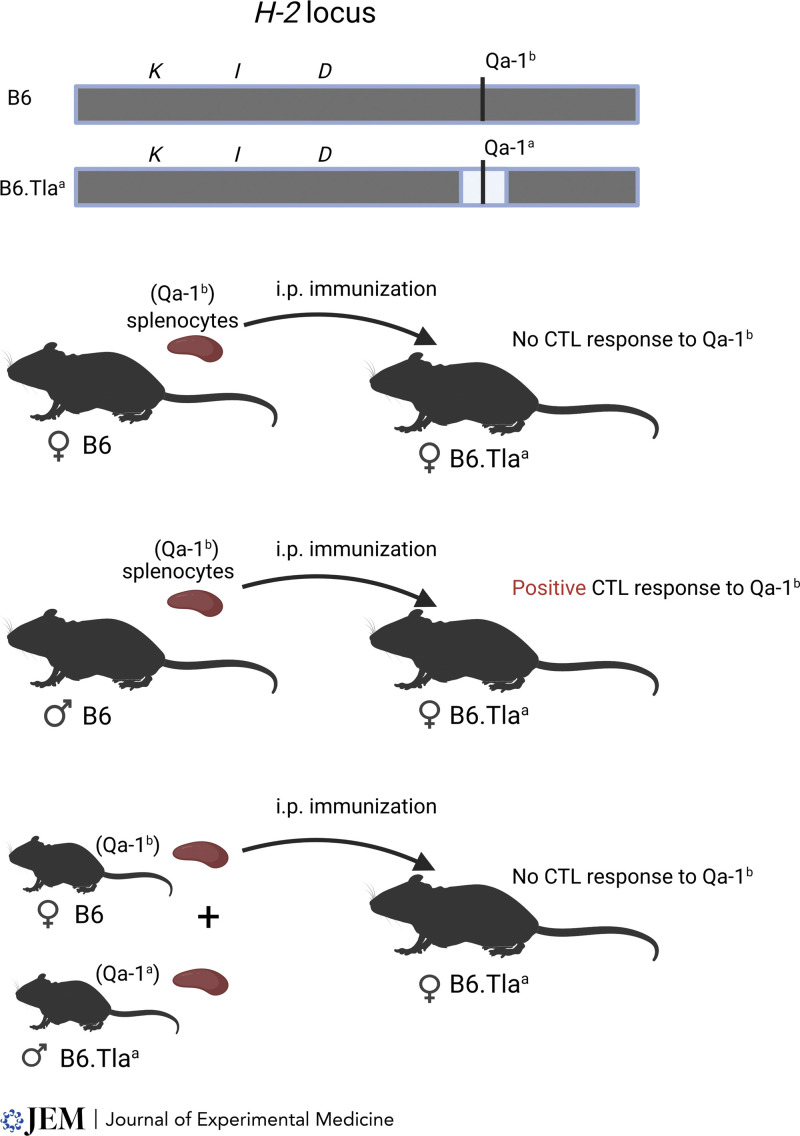
Other evidence of T–T cooperation was suggested subsequently by several in vivo experiments. These studies used mouse strains with H-2 haplotypes having distinct I regions and K/D regions of known permissiveness for CTL responses to vaccinia virus (Zinkernagel et al., 1978), male H-Y antigen (von Boehmer et al., 1978, or the Qa-1 alloantigen (Keene and Forman, 1982). Each study argued that strong CTL responses required a combination of permissive K or D allele with a permissive I region, which was interpreted as supporting a model of helper and CTL cooperation. Although these studies were not without some degree of ambiguity, Keene and Foreman suggested explicitly that the helper and CTL determinants should be expressed on the same cell (Keene and Forman, 1982), supporting linked recognition as a basis for help in CTL responses (Fig. 3).
Figure 3.
Linked recognition of helper activity is required for the in vivo generation of cytotoxic T lymphocytes. A congenic pair of B6 mice were generated differing only at the Qa-1 locus. Original B6 mice express the Qa-1b allele, while the B6.Tlaa congenic partner expresses the Qa-1aa allele. Immunization of female B6.Tlaa mice with splenocytes from B6 female mice fails to induce a Qa-1b specific CTL response. In contrast, immunization using splenocytes from B-6 male does generate the Qa-1b specific CTL. Male cells carry the additional H-Y antigen that serves as a helper determinant. The requirement for linked recognition was indicated by the inability to generate CTLs using a mixed immunization with B6 female splenocytes and male B6.Tlaa splenocytes. This suggested that the H-Y helper determinant and Qa-1b CTL determinant need to be presented on the same cell. Adapted from Keene and Forman (1982).
A three-cell-type model of linked recognition
Subsequent work by Mitchison and O’Malley provided evidence for a three-cell-type model of linked recognition, involving a pre-CTL, helper T cell (TH cell), and APC (Mitchison and O’Malley, 1987). In elegant fashion, adoptive transfers of alloreactive CTLs or helpers of different H-2 specificity were used in concert with appropriate H-2 recombinant mice to show that direct T–T cell cognate interactions were not required for help. The authors concluded that “an APC copresenting two epitopes may create a microenvironment that succeeds in bringing together two types of T cells.” Independent confirmation was provided when allogeneic responses to the class I H antigen Qa1 and the minor H antigen H-Y were also found to require help, without which a tolerant state was acquired (Guerder and Matzinger, 1992). However, how such a “microenvironment” would mediate help was unclear. For example, help might arise from co-localization of helper and killer precursors, allowing for efficient delivery of helper-derived cytokines, such as IL-2 to CTLs (Fearon et al., 1990). Alternately, at this time it was recognized that T cells can receive co-stimulatory signals from APCs (Lafferty and Cunningham, 1975). Thus, T helpers may activate APCs (Beller and Unanue, 1980; Walker et al., 1982) as a means of help. On this latter foundation, Matzinger proposed the alternate mechanism that help is “routed” through and by the APC, rather than being delivered directly from helper to CTL (Guerder and Matzinger, 1992).
CD40 stimulation activates DCs
CD40 was identified in 1986 through antibodies that induced B cell proliferation (Clark and Ledbetter, 1986), but was soon found to be expressed on human tonsillar DCs as well (Hart and McKenzie, 1988). CD40 stimulation was later shown to increase expression of MHC-I and -II molecules and costimulatory molecules CD80 and CD86 on DCs (Sallusto and Lanzavecchia, 1994; Caux et al., 1994). Importantly, Cella showed that CD40 stimulation of DCs enhanced their capacity to induce T cell proliferation and cytokine production (Cella et al., 1996). CD40 ligand (CD40L), identified by expression cloning (Armitage et al., 1992), was found to be expressed on activated TH cells (Noelle et al., 1992; Lederman et al., 1992). In this period, the CD40–CD40L signaling axis was actively studied in the context of B–T cell cooperation (Armitage et al., 1992).
Three simultaneous reports provided evidence that CD4 T cell help for CTL responses in mice was mediated by stimulating CD40 signaling in an APC (Schoenberger et al., 1998; Ridge et al., 1998; Bennett et al., 1998). The approaches used included the depletion of CD4 T cells to abrogate help, provision of CD40 signaling using anti-CD40 antibodies, and analysis of CTL responses in mice with germline deficiencies in CD40 and CD40L. Together, these studies supported the three-cell-type model with the addition that CD40 signaling delivered help to CTLs by activating CD40 signaling in an APC. Reliance on germline deficiencies precluded precise identification of the cellular site of CD40 signaling, although B cells were explicitly excluded (Schoenberger et al., 1998). Another study implicated DCs as the target of anti-CD40 stimulation as a substitute for help, but the DCs used in this setting were uncharacterized (Ridge et al., 1998). Heath and colleagues suggested that the target of CD40 signaling was the “cross-priming APC,” but direct evidence for its identity was not possible at that time (Bennett et al., 1998).
In contrast, another study argued against the APC as the target of CD40 signaling. In examining CTL responses to H-Y antigen, Tanchot and colleagues found that CD40 signaling was important for memory, but not the primary CTL response (Bourgeois et al., 2002). Moreover, while providing evidence for a three-cell-type model, this study argued that CD40 signaling acted directly within CTL, but not the APC. The experimental basis for this claim relied on adoptive transfers of H-Y–bearing APC from WT or CD40−/− mice, introduced into recipient mice harboring CD4 and TCR-transgenic H-Y specific CD8 T cells. No difference between responses was seen in mice receiving APCs from WT or CD40-deficient APCs, a negative result interpreted as excluding a requirement for CD40 expression by APCs in mediating help. However, as discussed above, H-Y antigens from CD40−/− APCs can still be cross-presented by the CD40-sufficient host APCs. Nonetheless, subsequent studies using infectious model systems argue against these results, supporting the requirement for CD40 signaling in the APC as the primary mechanism for help in CD8 T cell memory (Lee et al., 2003; Sun and Bevan, 2004). However, the structure of these studies did not directly test the effect of selective CD40 deficiency on CD8 T cells. For example, CD40-deficient CD8 T cells were only tested in Listeria infection in a setting that was independent of CD40-mediated help (Sun and Bevan, 2004).
Identification of the APC mediating CD4 T cell help
In vitro analysis (Smith et al., 2004) and intravital imaging (Eickhoff et al., 2015; Hor et al., 2015) suggested that the relevant target of CD4 help for CTL responses is the cDC1 subset, which is uniquely responsible for priming CD8 T cells to tumors (Hildner et al., 2008; Theisen et al., 2018), but did not demonstrate the involvement of CD40 signaling in vivo. Direct in vivo evidence for the requirement of CD40 expression on cDC1 for help-dependent rejection of tumors was recently obtained using a cDC1-specific Cre deleter mouse strain, Xcr1Cre, crossed to CD40fl/fl or MHC-IIfl/fl mouse strains (Ferris et al., 2020). Mice with cDC1-specific inactivation of CD40 failed to reject tumors normally rejected by WT mice, in a system where tumor rejection requires both CD8 priming and CD4 help (Ferris et al., 2020). In the same system, cDC1-specific inactivation of MHC-II expression severely reduced the expansion of endogenous tumor-specific CD8 T cells and impaired tumor rejection. These results support a role for CD40 signaling activated by CD4 T cells in cDC1 to provide help for CD8 T cells during tumor challenge.
One target of CD40 signaling proposed as providing help for CTL responses involves the CD70/CD27 signaling axis (Taraban et al., 2004; French et al., 2007; Feau et al., 2012; Ahrends et al., 2017; Borst et al., 2018). Several studies have used CD70 blockade by antibody (French et al., 2007; Feau et al., 2012; Keller et al., 2008; Ahrends et al., 2016) or examined CD70 or CD27 germline deficiencies (Munitic et al., 2013; Hendriks et al., 2000) to demonstrate a role for CD70 expression on cDC1 for enhancing CTL responses. However, these studies could not pinpoint the cellular action of CD40 and CD70. Toward this goal, another study examined Batf3−/− Cd70−/− mixed BM chimeras to test the role of CD70 on cDC1 (Oba et al., 2020), but did not examine responses of endogenous T cells to tumors. No study has yet tested the specific requirement for cDC1-specific CD70 expression using a conditional deletion system in vivo. Thus, it remains unclear whether induction of CD70 on cDC1 is fully responsible for mediating CD40-dependent help for CTL responses.
The road ahead in DCs, cross-presentation, and help
Current work in DCs is very broad and comprises open questions related to subset heterogeneity, functional specialization, and developmental pathways. Other questions related to alterations of DC in response to pathologic processes and the degree of individual variability within the human population. Within the area of functional specialization, the mechanism by which different DC subsets support alternative T helper cell responses remains undefined. For example, protection against Toxoplamsa gondii in mice requires the cDC1 subset presumably based on its superior IL-12 production (Mashayekhi et al., 2011). However, the molecular basis for this remains unclear (Kim et al., 2020). Similarly, cDC2 appears specialized for driving TH17 (Satpathy et al., 2013) and TH2 cell responses (Kumamoto et al., 2013; Gao et al., 2013; Williams et al., 2013) against various pathogens, but again the underlying mechanisms are unknown. Alternative explanations include those relying on cytokine bias, for example, with cDC2 acting as neutral agents in early CD4 T cell priming, thereby avoiding an early commitment toward a TH1 cell outcome. However, other explanations could involve differential localization within lymphoid tissues or differences in antigen processing. This field is in its early stages since reagents for complete cDC2-specific lineage ablation or gene inactivation are lacking.
Much of the literature on cross-presentation relies on analysis of BMDCs developed in vitro using GM-CSF, but the physiologic relevance of this system has recently been challenged (Helft et al., 2015). Many gene candidates for participation in cross-presentation that derive from these studies have yet to be tested for their impact on in vivo cross-presentation. The cDC1 lineage appears primarily responsible for in vivo cross-presentation, but analysis of its cellular pathway for cross-presentation is incompletely defined. Unique surface receptors expressed by cDC1, such as CLEC9A, may contribute to its capture and processing cell-associated antigen (Sancho et al., 2009), but these do not appear to be autonomously sufficient for this activity. The intracellular protein WDFY4 is a stringent requirement for in vivo cross-presentation. However, WDFY4 is expressed by cDC1 and cDC2, and again does not explain cDC1-specific cross-presentation. WDFY4 itself remains an enigma, with virtually nothing known regarding its cellular function. Future work will be required to identify the molecular pathways that connect receptors such as CLEC9A to the intracellular trafficking pathways within cDC1 that deliver their cargo to MHC-I loading compartments.
While CD40 is clearly a control hub in mediating CD4 help for CTL responses, the underlying cellular mechanism in cDC1 remains obscure. For example, the target genes induced by CD40 signaling in cDC1 remain largely unidentified, and which of these targets contributes to CTL responses remains incompletely defined. The induction of any one gene, such as Cd70, may not fully explain the complete effect of cDC1 licensing on CTL responses. Further, while CD40 signaling in cDC1 appears important for help, other factors may include the induction of cytokines and chemokines by cDC1 or CD4 T cells (Mackey et al., 1998; Castellino et al., 2006), or the amplification of other signals in cDC1 (Greyer et al., 2016; Schulz et al., 2000), or the enhanced survival or accumulation of these cells (Bjorck et al., 1997; Miga et al., 2001). Also, CD4 T cells may not be the exclusive cells responsible for licensing cDC1. Indeed, deletion of MHC-II on cDC1, which prevents cognate interactions with CD4 T cells, had less impact on CTL priming than did the deletion of CD40 on cDC1 (Ferris et al., 2020). This result may suggest that alternative cells, such as NK T cells that react with lipids presented by CD1 molecules, may also license cDC1 (Fujii et al., 2002). Alternately, CD4 T cells may function in a non-cognate manner to provide generalized cDC1 licensing in some settings (Pasqual et al., 2018).
In the 1970s, the connection between the discovery of DCs, cross-priming, and help for CTL responses was not fully appreciated, but these are now recognized as being connected elements embodied in the three-cell-type model (Mitchison and O’Malley, 1987). Decades of subsequent investigation have left this model conceptually intact, but it is now being seen with increasing resolution of detail. Nonetheless, the picture is not complete, and important aspects of this model are in need of further refinement.
Acknowledgments
The authors thank Theresa L. Murphy for editing. We thank Francis Carbone, William Heath, Jonathan Sprent, Philippa Marrack, Donna Murasko, Michael Bevan, and Emil Unanue for helpful discussions. This publication is solely the responsibility of the authors and does not represent the official view of the National Institutes of Health. Figures were created with BioRender.com.
This work was supported by the National Institutes of Health (R01AI150297, R01CA248919, and R21AI164142 to K.M. Murphy, and F30CA247262 to R. Wu).
Author contributions: R. Wu and K.M. Murphy wrote the manuscript.
References
- Ahrends, T., Babala N., Xiao Y., Yagita H., van Eenennaam H., and Borst J.. 2016. CD27 agonism plus PD-1 blockade recapitulates CD4+ T-cell help in therapeutic anticancer vaccination. Cancer Res. 76:2921–2931. 10.1158/0008-5472.CAN-15-3130 [DOI] [PubMed] [Google Scholar]
- Ahrends, T., Spanjaard A., Pilzecker B., Babala N., Bovens A., Xiao Y., Jacobs H., and Borst J.. 2017. CD4(+) T cell help confers a cytotoxic T cell effector program including coinhibitory receptor downregulation and increased tissue invasiveness. Immunity. 47:848–861.e5. 10.1016/j.immuni.2017.10.009 [DOI] [PubMed] [Google Scholar]
- Albert, M.L., Sauter B., and Bhardwaj N.. 1998. Dendritic cells acquire antigen from apoptotic cells and induce class I-restricted CTLs. Nature. 392:86–89. 10.1038/32183 [DOI] [PubMed] [Google Scholar]
- Alloatti, A., Kotsias F., Magalhaes J.G., and Amigorena S.. 2016. Dendritic cell maturation and cross-presentation: Timing matters. Immunol. Rev. 272:97–108. 10.1111/imr.12432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alloatti, A., Kotsias F., Pauwels A.M., Carpier J.M., Jouve M., Timmerman E., Pace L., Vargas P., Maurin M., Gehrmann U., et al. 2015. Toll-like receptor 4 engagement on dendritic cells restrains phago-lysosome fusion and promotes cross-presentation of antigens. Immunity. 43:1087–1100. 10.1016/j.immuni.2015.11.006 [DOI] [PubMed] [Google Scholar]
- Alloatti, A., Rookhuizen D.C., Joannas L., Carpier J.M., Iborra S., Magalhaes J.G., Yatim N., Kozik P., Sancho D., Albert M.L., and Amigorena S.. 2017. Critical role for Sec22b-dependent antigen cross-presentation in antitumor immunity. J. Exp. Med. 214:2231–2241. 10.1084/jem.20170229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson, D.A., III, Murphy K.M., and Briseno C.G.. 2018. Development, diversity, and function of dendritic cells in mouse and human. Cold Spring Harb. Perspect. Biol. 10:a028613. 10.1101/cshperspect.a028613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ardavin, C., and Shortman K.. 1992. Cell surface marker analysis of mouse thymic dendritic cells. Eur. J. Immunol. 22:859–862. 10.1002/eji.1830220334 [DOI] [PubMed] [Google Scholar]
- Armitage, R.J., Fanslow W.C., Strockbine L., Sato T.A., Clifford K.N., Macduff B.M., Anderson D.M., Gimpel S.D., Davis-Smith T., and Maliszewski C.R.. 1992. Molecular and biological characterization of a murine ligand for CD40. Nature. 357:80–82. 10.1038/357080a0 [DOI] [PubMed] [Google Scholar]
- Babbitt, B.P., Allen P.M., Matsueda G., Haber E., and Unanue E.R.. 1985. Binding of immunogenic peptides to Ia histocompatibility molecules. Nature. 317:359–361. 10.1038/317359a0 [DOI] [PubMed] [Google Scholar]
- Beller, D.I., and Unanue E.R.. 1980. IA antigens and antigen-presenting function of thymic macrophages. J. Immunol. 124:1433–1440. [PubMed] [Google Scholar]
- Bennett, S.R., Carbone F.R., Karamalis F., Flavell R.A., Miller J.F., and Heath W.R.. 1998. Help for cytotoxic-T-cell responses is mediated by CD40 signalling. Nature. 393:478–480. 10.1038/30996 [DOI] [PubMed] [Google Scholar]
- Bevan, M.J. 1975a. Alloimmune cytotoxic T cells: Evidence that they recognize serologically defined antigens and bear clonally restricted receptors. J. Immunol. 114:316–319 [PubMed] [Google Scholar]
- Bevan, M.J. 1975b. Interaction antigens detected by cytotoxic T cells with the major histocompatibility complex as modifier. Nature. 256:419–421. 10.1038/256419a0 [DOI] [PubMed] [Google Scholar]
- Bevan, M.J. 1976. Cross-priming for a secondary cytotoxic response to minor H antigens with H-2 congenic cells which do not cross-react in the cytotoxic assay. J. Exp. Med. 143:1283–1288. 10.1084/jem.143.5.1283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bevan, M.J. 1987. Antigen recognition. Class discrimination in the world of immunology. Nature. 325:192–194. 10.1038/325192b0 [DOI] [PubMed] [Google Scholar]
- Bjorck, P., Banchereau J., and Flores-Romo L.. 1997. CD40 ligation counteracts Fas-induced apoptosis of human dendritic cells. Int. Immunol. 9:365–372. 10.1093/intimm/9.3.365 [DOI] [PubMed] [Google Scholar]
- Bjorkman, P.J., Saper M.A., Samraoui B., Bennett W.S., Strominger J.L., and Wiley D.C.. 1987a. Structure of the human class I histocompatibility antigen, HLA-A2. Nature. 329:506–512. 10.1038/329506a0 [DOI] [PubMed] [Google Scholar]
- Bjorkman, P.J., Saper M.A., Samraoui B., Bennett W.S., Strominger J.L., and Wiley D.C.. 1987b. The foreign antigen binding site and T cell recognition regions of class I histocompatibility antigens. Nature. 329:512–518. 10.1038/329512a0 [DOI] [PubMed] [Google Scholar]
- Boak, J.L., Mitchison N.A., and Pattisson P.H.. 1971. The carrier effect in the secondary response to hapten-protein conjugates. 3. The anatomical distribution of helper cells and antibody-forming-cell-precursors. Eur. J. Immunol. 1:63–65. 10.1002/eji.1830010202 [DOI] [PubMed] [Google Scholar]
- Borst, J., Ahrends T., Babala N., Melief C.J.M., and Kastenmuller W.. 2018. CD4(+) T cell help in cancer immunology and immunotherapy. Nat. Rev. Immunol. 18:635–647. 10.1038/s41577-018-0044-0 [DOI] [PubMed] [Google Scholar]
- Bougneres, L., Helft J., Tiwari S., Vargas P., Chang B.H.-J., Chan L., Campisi L., Lauvau G., Hugues S., Kumar P., et al. 2009. A role for lipid bodies in the cross-presentation of phagocytosed antigens by MHC class I in dendritic cells. Immunity. 31:232–244. 10.1016/j.immuni.2009.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourgeois, C., Rocha B., and Tanchot C.. 2002. A role for CD40 expression on CD8+ T cells in the generation of CD8+ T cell memory. Science. 297:2060–2063. 10.1126/science.1072615 [DOI] [PubMed] [Google Scholar]
- Boyse, E.A., Miyazawa M., Aoki T., and Old L.J.. 1968. Ly-A and Ly-B: Two systems of lymphocyte isoantigens in the mouse. Proc. R Soc. Lond B Biol. Sci. 170:175–193. 10.1098/rspb.1968.0032 [DOI] [PubMed] [Google Scholar]
- Briseno, C.G., Haldar M., Kretzer N.M., Wu X., Theisen D.J., Kc W., Durai V., Grajales-Reyes G.E., Iwata A., Bagadia P., et al. 2016. Distinct transcriptional programs control cross-priming in classical and monocyte-derived dendritic cells. Cell Rep. 15:2462–2474. 10.1016/j.celrep.2016.05.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunner, K.T., Mauel J., Cerottini J.C., and Chapuis B.. 1968. Quantitative assay of the lytic action of immune lymphoid cells on 51-Cr-labelled allogeneic target cells in vitro; inhibition by isoantibody and by drugs. Immunology. 14:181–196. [PMC free article] [PubMed] [Google Scholar]
- Cantor, H., and Asofsky R.. 1970. Synergy among lymphoid cells mediating the graft-versus-host response. II. Synergy in graft-versus-host reactions produced by Balb-c lymphoid cells of differing anatomic origin. J. Exp. Med. 131:235–246. 10.1084/jem.131.2.235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantor, H., and Asofsky R.. 1972. Synergy among lymphoid cells mediating the graft-versus-host response. 3. Evidence for interaction between two types of thymus-derived cells. J. Exp. Med. 135:764–779. 10.1084/jem.135.4.764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantor, H., and Boyse E.A.. 1975a. Functional subclasses of T lymphocytes bearing different Ly antigens. II. Cooperation between subclasses of Ly+ cells in the generation of killer activity. J. Exp. Med. 141:1390–1399. 10.1084/jem.141.6.1390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantor, H., and Boyse E.A.. 1975b. Functional subclasses of T-lymphocytes bearing different Ly antigens. I. The generation of functionally distinct T-cell subclasses is a differentiative process independent of antigen. J. Exp. Med. 141:1376–1389. 10.1084/jem.141.6.1376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carbone, F.R., and Bevan M.J.. 1990. Class I-restricted processing and presentation of exogenous cell-associated antigen in vivo. J. Exp. Med. 171:377–387. 10.1084/jem.171.2.377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castellino, F., Huang A.Y., Altan-Bonnet G., Stoll S., Scheinecker C., and Germain R.N.. 2006. Chemokines enhance immunity by guiding naive CD8+ T cells to sites of CD4+ T cell-dendritic cell interaction. Nature. 440:890–895. 10.1038/nature04651 [DOI] [PubMed] [Google Scholar]
- Caux, C., Massacrier C., Vanbervliet B., Dubois B., Van Kooten C., Durand I., and Banchereau J.. 1994. Activation of human dendritic cells through CD40 cross-linking. J. Exp. Med. 180:1263–1272. 10.1084/jem.180.4.1263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cebrian, I., Visentin G., Blanchard N., Jouve M., Bobard A., Moita C., Enninga J., Moita L.F., Amigorena S., and Savina A.. 2011. Sec22b regulates phagosomal maturation and antigen crosspresentation by dendritic cells. Cell. 147:1355–1368. 10.1016/j.cell.2011.11.021 [DOI] [PubMed] [Google Scholar]
- Cella, M., Jarrossay D., Facchetti F., Alebardi O., Nakajima H., Lanzavecchia A., and Colonna M.. 1999. Plasmacytoid monocytes migrate to inflamed lymph nodes and produce large amounts of type I interferon [see comments]. Nat. Med. 5:919–923. 10.1038/11360 [DOI] [PubMed] [Google Scholar]
- Cella, M., Scheidegger D., Palmer-Lehmann K., Lane P., Lanzavecchia A., and Alber G.. 1996. Ligation of CD40 on dendritic cells triggers production of high levels of interleukin-12 and enhances T cell stimulatory capacity: T-T help via APC activation. J. Exp. Med. 184:747–752. 10.1084/jem.184.2.747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chess, L. 2006. The birth of functionally distinct T cell subsets. J. Immunol. 176:3859–3860. 10.4049/jimmunol.176.7.3859 [DOI] [PubMed] [Google Scholar]
- Clark, E.A., and Ledbetter J.A.. 1986. Activation of human B cells mediated through two distinct cell surface differentiation antigens, Bp35 and Bp50. Proc. Natl Acad. Sci. USA. 83:4494–4498. 10.1073/pnas.83.12.4494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins, D.S., Findlay K., and Harding C.V.. 1992. Processing of exogenous liposome-encapsulated antigens in vivo generates class I MHC-restricted T cell responses. J. Immunol. 148:3336–3341. [PubMed] [Google Scholar]
- Colonna, M., and Cella M.. 2007. Crosspresentation: Plasmacytoid dendritic cells are in the business. Immunity. 27:419–421. 10.1016/j.immuni.2007.08.006 [DOI] [PubMed] [Google Scholar]
- Cooper, M.D., Peterson R.D.A., South M.A., and Good R.A.. 1966. The functions of the thymus system and the bursa system in the chicken. J. Exp. Med. 123:75–102. 10.1084/jem.123.1.75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowley, M., Inaba K., Witmer-Pack M., and Steinman R.M.. 1989. The cell surface of mouse dendritic cells: FACS analyses of dendritic cells from different tissues including thymus. Cell Immunol. 118:108–125. 10.1016/0008-8749(89)90361-4 [DOI] [PubMed] [Google Scholar]
- Cruz, F.M., Colbert J.D., Merino E., Kriegsman B.A., and Rock K.L.. 2017. The biology and underlying mechanisms of cross-presentation of exogenous antigens on MHC-I molecules. Annu. Rev. Immunol. 35:149–176. 10.1146/annurev-immunol-041015-055254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- den Haan, J.M., Lehar S.M., and Bevan M.J.. 2000. CD8(+) but not CD8(-) dendritic cells cross-prime cytotoxic T cells in vivo. J. Exp. Med. 192:1685–1696. 10.1084/jem.192.12.1685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Pucchio, T., Chatterjee B., Smed-Sorensen A., Clayton S., Palazzo A., Montes M., Xue Y., Mellman I., Banchereau J., and Connolly J.E.. 2008. Direct proteasome-independent cross-presentation of viral antigen by plasmacytoid dendritic cells on major histocompatibility complex class I. Nat. Immunol. 9:551–557. 10.1038/ni.1602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dudziak, D., Kamphorst A.O., Heidkamp G.F., Buchholz V.R., Trumpfheller C., Yamazaki S., Cheong C., Liu K., Lee H.W., Park C.G., et al. 2007. Differential antigen processing by dendritic cell subsets in vivo. Science. 315:107–111. 10.1126/science.1136080 [DOI] [PubMed] [Google Scholar]
- Durai, V., Bagadia P., Granja J.M., Satpathy A.T., Kulkarni D.H., Davidson J.T., Wu R., Patel S.J., Iwata A., Liu T.T., et al. 2019. Cryptic activation of an Irf8 enhancer governs cDC1 fate specification. Nat. Immunol. 20:1161–1173. 10.1038/s41590-019-0450-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durai, V., and Murphy K.M.. 2016. Functions of murine dendritic cells. Immunity. 45:719–736. 10.1016/j.immuni.2016.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eickhoff, S., Brewitz A., Gerner M.Y., Klauschen F., Komander K., Hemmi H., Garbi N., Kaisho T., Germain R.N., and Kastenmuller W.. 2015. Robust anti-viral immunity requires multiple distinct T cell-dendritic cell interactions. Cell. 162:1322–1337. 10.1016/j.cell.2015.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fearon, E.R., Pardoll D.M., Itaya T., Golumbek P., Levitsky H.I., Simons J.W., Karasuyama H., Vogelstein B., and Frost P.. 1990. Interleukin-2 production by tumor cells bypasses T helper function in the generation of an antitumor response. Cell. 60:397–403. 10.1016/0092-8674(90)90591-2 [DOI] [PubMed] [Google Scholar]
- Feau, S., Garcia Z., Arens R., Yagita H., Borst J., and Schoenberger S.P.. 2012. The CD4+ T-cell help signal is transmitted from APC to CD8+ T-cells via CD27-CD70 interactions. Nat. Commun. 3:948. 10.1038/ncomms1948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferris, S.T., Durai V., Wu R., Theisen D.J., Ward J.P., Bern M.D., Davidson J.T., Bagadia P., Liu T., Briseno C.G., et al. 2020. cDC1 prime and are licensed by CD4(+) T cells to induce anti-tumour immunity. Nature. 584:624–629. 10.1038/s41586-020-2611-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fink, P.J., Weissman I.L., and Bevan M.J.. 1983. Haplotype-specific suppression of cytotoxic T cell induction by antigen inappropriately presented on T cells. J. Exp. Med. 157:141–154. 10.1084/jem.157.1.141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman, H.A., and Lilly F.. 1975. Properties of cell lines derived from tumors induced by Friend virus in BALB/c and BALB/c-H-2b mice. J. Exp. Med. 142:212–223. 10.1084/jem.142.1.212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- French, R.R., Taraban V.Y., Crowther G.R., Rowley T.F., Gray J.C., Johnson P.W., Tutt A.L., Al Shamkhani A., and Glennie M.J.. 2007. Eradication of lymphoma by CD8 T cells following anti-CD40 monoclonal antibody therapy is critically dependent on CD27 costimulation. Blood. 109:4810–4815. 10.1182/blood-2006-11-057216 [DOI] [PubMed] [Google Scholar]
- Fujii, S.-i., Shimizu K., Kronenberg M., and Steinman R.M.. 2002. Prolonged IFN-gamma-producing NKT response induced with alpha-galactosylceramide-loaded DCs. Nat. Immunol. 3:867–874. 10.1038/ni827 [DOI] [PubMed] [Google Scholar]
- Gao, Y., Nish S.A., Jiang R., Hou L., Licona-Limón P., Weinstein J.S., Zhao H., and Medzhitov R.. 2013. Control of T helper 2 responses by transcription factor IRF4-dependent dendritic cells. Immunity. 39:722–732. 10.1016/j.immuni.2013.08.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasser, D.L., and Silvers W.K.. 1972. Genetics and immunology of sex-linked antigens. Adv. Immunol. 15:215–247. 10.1016/s0065-2776(08)60686-0 [DOI] [PubMed] [Google Scholar]
- Germain, R.N. 1986. Immunology. The ins and outs of antigen processing and presentation. Nature. 322:687–689. 10.1038/322687a0 [DOI] [PubMed] [Google Scholar]
- Greyer, M., Whitney P.G., Stock A.T., Davey G.M., Tebartz C., Bachem A., Mintern J.D., Strugnell R.A., Turner S.J., Gebhardt T., et al. 2016. T cell help amplifies innate signals in CD8(+) DCs for optimal CD8(+) T cell priming. Cell Rep. 14:586–597. 10.1016/j.celrep.2015.12.058 [DOI] [PubMed] [Google Scholar]
- Guerder, S., and Matzinger P.. 1992. A fail-safe mechanism for maintaining self-tolerance. J. Exp. Med. 176:553–564. 10.1084/jem.176.2.553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guermonprez, P., Saveanu L., Kleijmeer M., Davoust J., Van Endert P., and Amigorena S.. 2003. ER-phagosome fusion defines an MHC class I cross-presentation compartment in dendritic cells. Nature. 425:397–402. 10.1038/nature01911 [DOI] [PubMed] [Google Scholar]
- Hart, D.N., and McKenzie J.L.. 1988. Isolation and characterization of human tonsil dendritic cells. J. Exp. Med. 168:157–170. 10.1084/jem.168.1.157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helft, J., Böttcher J., Chakravarty P., Zelenay S., Huotari J., Schraml B.U., Goubau D., and Reis e Sousa C.. 2015. GM-CSF mouse bone marrow cultures comprise a heterogeneous population of CD11c(+)MHCII(+) macrophages and dendritic cells. Immunity. 42:1197–1211. 10.1016/j.immuni.2015.05.018 [DOI] [PubMed] [Google Scholar]
- Hendriks, J., Gravestein L.A., Tesselaar K., van Lier R.A., Schumacher T.N., and Borst J.. 2000. CD27 is required for generation and long-term maintenance of T cell immunity. Nat. Immunol. 1:433–440. 10.1038/80877 [DOI] [PubMed] [Google Scholar]
- Hildner, K., Edelson B.T., Purtha W.E., Diamond M., Matsushita H., Kohyama M., Calderon B., Schraml B.U., Unanue E.R., Diamond M.S., et al. 2008. Batf3 deficiency reveals a critical role for CD8alpha+ dendritic cells in cytotoxic T cell immunity. Science. 322:1097–1100. 10.1126/science.1164206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoeffel, G., Ripoche A.C., Matheoud D., Nascimbeni M., Escriou N., Lebon P., Heshmati F., Guillet J.G., Gannage M., Caillat-Zucman S., et al. 2007. Antigen crosspresentation by human plasmacytoid dendritic cells. Immunity. 27:481–492. 10.1016/j.immuni.2007.07.021 [DOI] [PubMed] [Google Scholar]
- Hor, J.L., Whitney P.G., Zaid A., Brooks A.G., Heath W.R., and Mueller S.N.. 2015. Spatiotemporally distinct interactions with dendritic cell subsets facilitates CD4+ and CD8+ T cell activation to localized viral infection. Immunity. 43:554–565. 10.1016/j.immuni.2015.07.020 [DOI] [PubMed] [Google Scholar]
- Houde, M., Bertholet S., Gagnon E., Brunet S., Goyette G., Laplante A., Princiotta M.F., Thibault P., Sacks D., and Desjardins M.. 2003. Phagosomes are competent organelles for antigen cross-presentation. Nature. 425:402–406. 10.1038/nature01912 [DOI] [PubMed] [Google Scholar]
- Huang, A.Y., Golumbek P., Ahmadzadeh M., Jaffee E., Pardoll D., and Levitsky H.. 1994. Role of bone marrow-derived cells in presenting MHC class I-restricted tumor antigens. Science. 264:961–965. 10.1126/science.7513904 [DOI] [PubMed] [Google Scholar]
- Hume, D.A. 2008. Differentiation and heterogeneity in the mononuclear phagocyte system. Mucosal Immunol. 1:432–441. 10.1038/mi.2008.36 [DOI] [PubMed] [Google Scholar]
- Inaba, K., Metlay J.P., Crowley M.T., and Steinman R.M.. 1990. Dendritic cells pulsed with protein antigens in vitro can prime antigen-specific, MHC-restricted T cells in situ. J. Exp. Med. 172:631–640. 10.1084/jem.172.2.631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iyoda, T., Shimoyama S., Liu K., Omatsu Y., Akiyama Y., Maeda Y., Takahara K., Steinman R.M., and Inaba K.. 2002. The CD8+ dendritic cell subset selectively endocytoses dying cells in culture and in vivo. J. Exp. Med. 195:1289–1302. 10.1084/jem.20020161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jancic, C., Savina A., Wasmeier C., Tolmachova T., El-Benna J., Dang P.M.-C., Pascolo S., Gougerot-Pocidalo M.-A., Raposo G., Seabra M.C., and Amigorena S.. 2007. Rab27a regulates phagosomal pH and NADPH oxidase recruitment to dendritic cell phagosomes. Nat. Cell Biol. 9:367–378. 10.1038/ncb1552 [DOI] [PubMed] [Google Scholar]
- Jiang, W., Swiggard W.J., Heufler C., Peng M., Mirza A., Steinman R.M., and Nussenzweig M.C.. 1995. The receptor DEC-205 expressed by dendritic cells and thymic epithelial cells is involved in antigen processing. Nature. 375:151–155. 10.1038/375151a0 [DOI] [PubMed] [Google Scholar]
- Kamphorst, A.O., Guermonprez P., Dudziak D., and Nussenzweig M.C.. 2010. Route of antigen uptake differentially impacts presentation by dendritic cells and activated monocytes. J. Immunol. 185:3426–3435. 10.4049/jimmunol.1001205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keene, J.A., and Forman J.. 1982. Helper activity is required for the in vivo generation of cytotoxic T lymphocytes. J. Exp. Med. 155:768–782. 10.1084/jem.155.3.768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller, A.M., Schildknecht A., Xiao Y., van den Broek M., and Borst J.. 2008. Expression of costimulatory ligand CD70 on steady-state dendritic cells breaks CD8+ T cell tolerance and permits effective immunity. Immunity. 29:934–946. 10.1016/j.immuni.2008.10.009 [DOI] [PubMed] [Google Scholar]
- `Kim, S., Bagadia P., Anderson D.A. III, Liu T.T., Huang X., Theisen D.J., O’Connor K.W., Ohara R.A., Iwata A., Murphy T.L., and Murphy K.M.. 2020. High amount of transcription factor IRF8 engages AP1-IRF composite elements in enhancers to direct type 1 conventional dendritic cell identity. Immunity. 53:1–16. 10.1016/j.immuni.2020.07.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kool, M., Geurtsvankessel C., Muskens F., Madeira F.B., van Nimwegen M., Kuipers H., Thielemans K., Hoogsteden H.C., Hammad H., and Lambrecht B.N.. 2011. Facilitated antigen uptake and timed exposure to TLR ligands dictate the antigen-presenting potential of plasmacytoid DCs. J. Leukoc. Biol. 90:1177–1190. 10.1189/jlb.0610342 [DOI] [PubMed] [Google Scholar]
- Korngold, R., and Sprent J.. 1980. Selection of cytotoxic T-cell precursors specific for minor histocompatibility determinants. I. Negative selection across H-2 barriers induced with disrupted cells but not with glutaraldehyde-treated cells: Evidence for antigen processing. J. Exp. Med. 151:314–327. 10.1084/jem.151.2.314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacsovics-Bankowski, M., Clark K., Benacerraf B., and Rock K.L.. 1993. Efficient major histocompatibility complex class I presentation of exogenous antigen upon phagocytosis by macrophages. Proc. Natl. Acad. Sci. USA. 90:4942–4946. 10.1073/pnas.90.11.4942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kretzer, N.M., Theisen D.J., Tussiwand R., Briseno C.G., Grajales-Reyes G.E., Wu X., Durai V., Albring J., Bagadia P., Murphy T.L., and Murphy K.M.. 2016. RAB43 facilitates cross-presentation of cell-associated antigens by CD8α+ dendritic cells. J. Exp. Med. 213:2871–2883. 10.1084/jem.20160597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kronin, V., Winkel K., Süss G., Kelso A., Heath W., Kirberg J., von Boehmer H., and Shortman K.. 1996. A subclass of dendritic cells regulates the response of naive CD8 T cells by limiting their IL-2 production. J. Immunol. 157:3819–3827. [PubMed] [Google Scholar]
- Kumamoto, Y., Linehan M., Weinstein J.S., Laidlaw B.J., Craft J.E., and Iwasaki A.. 2013. CD301b+ dermal dendritic cells drive T helper 2 cell-mediated immunity. Immunity. 39:733–743. 10.1016/j.immuni.2013.08.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kündig, T.M., Bachmann M.F., DiPaolo C., Simard J.J.L., Battegay M., Lother H., Gessner A., Kühlcke K., Ohashi P.S., Hengartner H., and Zinkernagel R.M.. 1995. Fibroblasts as efficient antigen-presenting cells in lymphoid organs. Science. 268:1343–1347. 10.1126/science.7761853 [DOI] [PubMed] [Google Scholar]
- Kurts, C., Cannarile M., Klebba I., and Brocker T.. 2001. Dendritic cells are sufficient to cross-present self-antigens to CD8 T cells in vivo. J. Immunol. 166:1439–1442. 10.4049/jimmunol.166.3.1439 [DOI] [PubMed] [Google Scholar]
- Kurts, C., Kosaka H., Carbone F.R., Miller J.F., and Heath W.R.. 1997. Class I-restricted cross-presentation of exogenous self-antigens leads to deletion of autoreactive CD8(+) T cells. J. Exp. Med. 186:239–245. 10.1084/jem.186.2.239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lafferty, K.J., and Cunningham A.J.. 1975. A new analysis of allogeneic interactions. Aust. J. Exp. Biol. Med. Sci. 53:27–42. 10.1038/icb.1975.3 [DOI] [PubMed] [Google Scholar]
- Laidlaw, B.J., Craft J.E., and Kaech S.M.. 2016. The multifaceted role of CD4(+) T cells in CD8(+) T cell memory. Nat. Rev. Immunol. 16:102–111. 10.1038/nri.2015.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lederman, S., Yellin M.J., Inghirami G., Lee J.J., Knowles D.M., and Chess L.. 1992. Molecular interactions mediating T-B lymphocyte collaboration in human lymphoid follicles. Roles of T cell-B-cell-activating molecule (5c8 antigen) and CD40 in contact-dependent help. J. Immunol. 149:3817–3826. [PubMed] [Google Scholar]
- Lee, B.O., Hartson L., and Randall T.D.. 2003. CD40-deficient, influenza-specific CD8 memory T cells develop and function normally in a CD40-sufficient environment. J. Exp. Med. 198:1759–1764. 10.1084/jem.20031440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehmann, C.H.K., Baranska A., Heidkamp G.F., Heger L., Neubert K., Luhr J.J., Hoffmann A., Reimer K.C., Bruckner C., Beck S., et al. 2017. DC subset-specific induction of T cell responses upon antigen uptake via Fcγ receptors in vivo. J. Exp. Med. 214:1509–1528. 10.1084/jem.20160951 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, K., and Nussenzweig M.C.. 2010. Origin and development of dendritic cells. Immunol. Rev. 234:45–54. 10.1111/j.0105-2896.2009.00879.x [DOI] [PubMed] [Google Scholar]
- Mackey, M.F., Gunn J.R., Maliszewsky C., Kikutani H., Noelle R.J., and Barth R.J. Jr.. 1998. Dendritic cells require maturation via CD40 to generate protective antitumor immunity. J. Immunol. 161:2094–2098. [PubMed] [Google Scholar]
- Markowicz, S., and Engleman E.G.. 1990. Granulocyte-macrophage colony-stimulating factor promotes differentiation and survival of human peripheral blood dendritic cells in vitro. J. Clin. Invest. 85:955–961. 10.1172/JCI114525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez, C., Shapiro F., and Good R.A.. 1959. Absence of gene interaction in mouse hybrids, revealed by studies of immunological tolerance and homotransplantation. Proc. Soc. Exp. Biol. Med. 101:658–660. 10.3181/00379727-101-25051 [DOI] [PubMed] [Google Scholar]
- Mashayekhi, M., Sandau M.M., Dunay I.R., Frickel E.M., Khan A., Goldszmid R.S., Sher A., Ploegh H.L., Murphy T.L., Sibley L.D., and Murphy K.M.. 2011. CD8α(+) dendritic cells are the critical source of interleukin-12 that controls acute infection by toxoplasma gondii tachyzoites. Immunity. 35:249–259. 10.1016/j.immuni.2011.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matzinger, P., and Bevan M.J.. 1977. Induction of H-2-restricted cytotoxic T cells: In vivo induction has the appearance of being unrestricted. Cell Immunol. 33:92–100. 10.1016/0008-8749(77)90137-x [DOI] [PubMed] [Google Scholar]
- Merad, M., Sathe P., Helft J., Miller J., and Mortha A.. 2013. The dendritic cell lineage: Ontogeny and function of dendritic cells and their subsets in the steady state and the inflamed setting. Annu. Rev. Immunol. 31:563–604. 10.1146/annurev-immunol-020711-074950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miga, A.J., Masters S.R., Durell B.G., Gonzalez M., Jenkins M.K., Maliszewski C., Kikutani H., Wade W.F., and Noelle R.J.. 2001. Dendritic cell longevity and T cell persistence is controlled by CD154-CD40 interactions. Eur. J. Immunol. 31:959–965. [DOI] [PubMed] [Google Scholar]
- Mitchell, G.F., and Miller J.F.A.P.. 1968. Cell to cell interaction in the immune response. II. The source of hemolysin-forming cells in irradiated mice given bone marrow and thymus or thoracic duct lymphocytes. J. Exp. Med. 128:821–837. 10.1084/jem.128.4.821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchison, N.A., and O’Malley C.. 1987. Three-cell-type clusters of T cells with antigen-presenting cells best explain the epitope linkage and noncognate requirements of the in vivo cytolytic response. Eur. J. Immunol. 17:1579–1583. 10.1002/eji.1830171109 [DOI] [PubMed] [Google Scholar]
- Morrison, L.A., Lukacher A.E., Braciale V.L., Fan D.P., and Braciale T.J.. 1986. Differences in antigen presentation to MHC class I-and class II-restricted influenza virus-specific cytolytic T lymphocyte clones. J. Exp. Med. 163:903–921. 10.1084/jem.163.4.903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouries, J., Moron G., Schlecht G., Escriou N., Dadaglio G., and Leclerc C.. 2008. Plasmacytoid dendritic cells efficiently cross-prime naive T cells in vivo after TLR activation. Blood. 112:3713–3722. 10.1182/blood-2008-03-146290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munitic, I., Kuka M., Allam A., Scoville J.P., and Ashwell J.D.. 2013. CD70 deficiency impairs effector CD8 T cell generation and viral clearance but is dispensable for the recall response to lymphocytic choriomeningitis virus. J. Immunol. 190:1169–1179. 10.4049/jimmunol.1202353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murasko, D.M. 1978. Apparent lack of H-2 restriction of allograft rejection. J. Immunol. 121:958–961 [PubMed] [Google Scholar]
- Murphy, T.L., Grajales-Reyes G.E., Wu X., Tussiwand R., Briseno C.G., Iwata A., Kretzer N.M., Durai V., and Murphy K.M.. 2016. Transcriptional control of dendritic cell development. Annu. Rev. Immunol. 34:93–119. 10.1146/annurev-immunol-032713-120204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy, T.L., and Murphy K.M.. 2022. Dendritic cells in cancer immunology. Cell Mol Immunol. 19:3–13. 10.1038/s41423-021-00741-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naik, S.H., Sathe P., Park H.Y., Metcalf D., Proietto A.I., Dakic A., Carotta S., O’Keeffe M., Bahlo M., Papenfuss A., et al. 2007. Development of plasmacytoid and conventional dendritic cell subtypes from single precursor cells derived in vitro and in vivo. Nat. Immunol. 8:1217–1226. 10.1038/ni1522 [DOI] [PubMed] [Google Scholar]
- Neijssen, J., Herberts C., Drijfhout J.W., Reits E., Janssen L., and Neefjes J.. 2005. Cross-presentation by intercellular peptide transfer through gap junctions. Nature. 434:83–88. 10.1038/nature03290 [DOI] [PubMed] [Google Scholar]
- Noelle, R.J., Roy M., Shepherd D.M., Stamenkovic I., Ledbetter J.A., and Aruffo A.. 1992. A 39-kDa protein on activated helper T cells binds CD40 and transduces the signal for cognate activation of B cells. Proc. Natl. Acad. Sci. USA. 89:6550–6554. 10.1073/pnas.89.14.6550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nussenzweig, M.C., and Steinman R.M.. 1980. Contribution of dendritic cells to stimulation of the murine syngeneic mixed leukocyte reaction. J. Exp. Med. 151:1196–1212. 10.1084/jem.151.5.1196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nussenzweig, M.C., and Steinman R.M.. 1982. The cell surface of mouse lymphoid dendritic cells. Immunol. Today. 3:65–68. 10.1016/S0167-5699(82)80036-4 [DOI] [PubMed] [Google Scholar]
- Nussenzweig, M.C., Steinman R.M., Gutchinov B., and Cohn Z.A.. 1980. Dendritic cells are accessory cells for the development of anti-trinitrophenyl cytotoxic T lymphocytes. J. Exp. Med. 152:1070–1084. 10.1084/jem.152.4.1070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oba, T., Hoki T., Yamauchi T., Keler T., Marsh H.C., Cao X., and Ito F.. 2020. A critical role of CD40 and CD70 signaling in conventional type 1 dendritic cells in expansion and antitumor efficacy of adoptively transferred tumor-specific T cells. J. Immunol. 205:1867–1877. 10.4049/jimmunol.2000347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasqual, G., Chudnovskiy A., Tas J.M.J., Agudelo M., Schweitzer L.D., Cui A., Hacohen N., and Victora G.D.. 2018. Monitoring T cell-dendritic cell interactions in vivo by intercellular enzymatic labelling. Nature. 553:496–500. 10.1038/nature25442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul, W.E. 2011. Bridging innate and adaptive immunity. Cell. 147:1212–1215. 10.1016/j.cell.2011.11.036 [DOI] [PubMed] [Google Scholar]
- Pfeifer, J.D., Wick M.J., Roberts R.L., Findlay K., Normark S.J., and Harding C.V.. 1993. Phagocytic processing of bacterial antigens for class I MHC presentation to T cells. Nature. 361:359–362. 10.1038/361359a0 [DOI] [PubMed] [Google Scholar]
- Pooley, J.L., Heath W.R., and Shortman K.. 2001. Cutting edge: Intravenous soluble antigen is presented to CD4 T cells by CD8- dendritic cells, but cross-presented to CD8 T cells by CD8+ dendritic cells. J. Immunol. 166:5327–5330. 10.4049/jimmunol.166.9.5327 [DOI] [PubMed] [Google Scholar]
- Reddy, R., Zhou F., Nair S., Huang L., and Rouse B.T.. 1992. In vivo cytotoxic T lymphocyte induction with soluble proteins administered in liposomes. J. Immunol. 148:1585–1589. [PubMed] [Google Scholar]
- Ridge, J.P., Di Rosa F., and Matzinger P.. 1998. A conditioned dendritic cell can be a temporal bridge between a CD4+ T-helper and a T-killer cell. Nature. 393:474–478. 10.1038/30989 [DOI] [PubMed] [Google Scholar]
- Rock, K.L., Gamble S., and Rothstein L.. 1990. Presentation of exogenous antigen with class I major histocompatibility complex molecules. Science. 249:918–921. 10.1126/science.2392683 [DOI] [PubMed] [Google Scholar]
- Sallusto, F., Cella M., Danieli C., and Lanzavecchia A.. 1995. Dendritic cells use macropinocytosis and the mannose receptor to concentrate macromolecules in the major histocompatibility complex class II compartment: Downregulation by cytokines and bacterial products. J. Exp. Med. 182:389–400. 10.1084/jem.182.2.389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallusto, F., and Lanzavecchia A.. 1994. Efficient presentation of soluble antigen by cultured human dendritic cells is maintained by granulocyte/macrophage colony-stimulating factor plus interleukin 4 and downregulated by tumor necrosis factor alpha. J. Exp. Med. 179:1109–1118. 10.1084/jem.179.4.1109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samie, M., and Cresswell P.. 2015. The transcription factor TFEB acts as a molecular switch that regulates exogenous antigen-presentation pathways. Nat. Immunol. 16:729–736. 10.1038/ni.3196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sancho, D., Joffre O.P., Keller A.M., Rogers N.C., Martínez D., Hernanz-Falcón P., Rosewell I., and Reis e Sousa C.. 2009. Identification of a dendritic cell receptor that couples sensing of necrosis to immunity. Nature. 458:899–903. 10.1038/nature07750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sapoznikov, A., Fischer J.A., Zaft T., Krauthgamer R., Dzionek A., and Jung S.. 2007. Organ-dependent in vivo priming of naive CD4+, but not CD8+, T cells by plasmacytoid dendritic cells. J. Exp. Med. 204:1923–1933. 10.1084/jem.20062373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satpathy, A.T., Briseno C.G., Lee J.S., Ng D., Manieri N.A., Kc W., Wu X., Thomas S.R., Lee W.L., Turkoz M., et al. 2013. Notch2-dependent classical dendritic cells orchestrate intestinal immunity to attaching-and-effacing bacterial pathogens. Nat. Immunol. 14:937–948. 10.1038/ni.2679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savina, A., Jancic C., Hugues S., Guermonprez P., Vargas P., Moura I.C., Lennon-Dumenil A.M., Seabra M.C., Raposo G., and Amigorena S.. 2006. NOX2 controls phagosomal pH to regulate antigen processing during crosspresentation by dendritic cells. Cell. 126:205–218. 10.1016/j.cell.2006.05.035 [DOI] [PubMed] [Google Scholar]
- Savina, A., Peres A., Cebrian I., Carmo N., Moita C., Hacohen N., Moita L.F., and Amigorena S.. 2009. The small GTPase Rac2 controls phagosomal alkalinization and antigen crosspresentation selectively in CD8(+) dendritic cells. Immunity. 30:544–555. 10.1016/j.immuni.2009.01.013 [DOI] [PubMed] [Google Scholar]
- Schoenberger, S.P., Toes R.E., van der Voort E.I., Offringa R., and Melief C.J.. 1998. T-cell help for cytotoxic T lymphocytes is mediated by CD40-CD40L interactions. Nature. 393:480–483. 10.1038/31002 [DOI] [PubMed] [Google Scholar]
- Schulz, O., Edwards A.D., Schito M., Aliberti J., Manickasingham S., Sher A., and Reis e Sousa C.. 2000. CD40 triggering of heterodimeric IL-12 p70 production by dendritic cells in vivo requires a microbial priming signal. Immunity. 13:453–462. 10.1016/s1074-7613(00)00045-5 [DOI] [PubMed] [Google Scholar]
- Segura, E., Albiston A.L., Wicks I.P., Chai S.Y., and Villadangos J.A.. 2009. Different cross-presentation pathways in steady-state and inflammatory dendritic cells. Proc. Natl. Acad. Sci. USA. 106:20377–20381. 10.1073/pnas.0910295106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segura, E., Durand M., and Amigorena S.. 2013. Similar antigen cross-presentation capacity and phagocytic functions in all freshly isolated human lymphoid organ-resident dendritic cells. J. Exp. Med. 210:1035–1047. 10.1084/jem.20121103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen, L., Sigal L.J., Boes M., and Rock K.L.. 2004. Important role of cathepsin S in generating peptides for TAP-independent MHC class I crosspresentation in vivo. Immunity. 21:155–165. 10.1016/j.immuni.2004.07.004 [DOI] [PubMed] [Google Scholar]
- Shiku, H., Kisielow P., Bean M.A., Takahashi T., Boyse E.A., Oettgen H.F., and Old L.J.. 1975. Expression of T-cell differentiation antigens on effector cells in cell-mediated cytotoxicity in vitro. Evidence for functional heterogeneity related to the surface phenotype of T cells. J. Exp. Med. 141:227–241. 10.1084/jem.141.1.227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimonkevitz, R., Colon S., Kappler J.W., Marrack P., and Grey H.M.. 1984. Antigen recognition by H-2-restricted T cells. II. A tryptic ovalbumin peptide that substitutes for processed antigen. J. Immunol. 133:2067–2074. [PubMed] [Google Scholar]
- Shimonkevitz, R., Kappler J., Marrack P., and Grey H.. 1983. Antigen recognition by H-2-restricted T cells. I. Cell-free antigen processing. J. Exp. Med. 158:303–316. 10.1084/jem.158.2.303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinohara, M.L., Lu L., Bu J., Werneck M.B.F., Kobayashi K.S., Glimcher L.H., and Cantor H.. 2006. Osteopontin expression is essential for interferon-alpha production by plasmacytoid dendritic cells. Nat. Immunol. 7:498–506. 10.1038/ni1327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shortman, K., and Heath W.R.. 2010. The CD8+ dendritic cell subset. Immunol. Rev. 234:18–31. 10.1111/j.0105-2896.2009.00870.x [DOI] [PubMed] [Google Scholar]
- Shortman, K., and Liu Y.J.. 2002. Mouse and human dendritic cell subtypes. Nat. Rev. Immunol. 2:151–161. 10.1038/nri746 [DOI] [PubMed] [Google Scholar]
- Shortman, K., Wu L., Ardavin C., Vremec D., Stozik F., Winkel K., and Suss G.. 1995. Thymic dendritic cells: Surface phenotype, developmental origin and function. Adv. Exp. Med. Biol. 378:21–29. 10.1007/978-1-4615-1971-3_5 [DOI] [PubMed] [Google Scholar]
- Siegal, F.P., Kadowaki N., Shodell M., Fitzgerald-Bocarsly P.A., Shah K., Ho S., Antonenko S., and Liu Y.J.. 1999. The nature of the principal type 1 interferon-producing cells in human blood. Science. 284:1835–1837. 10.1126/science.284.5421.1835 [DOI] [PubMed] [Google Scholar]
- Sigal, L.J., Crotty S., Andino R., and Rock K.L.. 1999. Cytotoxic T-cell immunity to virus-infected non-haematopoietic cells requires presentation of exogenous antigen. Nature. 398:77–80. 10.1038/18038 [DOI] [PubMed] [Google Scholar]
- Smith, C.M., Wilson N.S., Waithman J., Villadangos J.A., Carbone F.R., Heath W.R., and Belz G.T.. 2004. Cognate CD4(+) T cell licensing of dendritic cells in CD8(+) T cell immunity. Nat. Immunol. 5:1143–1148. 10.1038/ni1129 [DOI] [PubMed] [Google Scholar]
- Snell, G.D. 1958. Histocompatibility genes of the mouse. I. Demonstration of weak histocompatibility differences by immunization and controlled tumor dosage. J. Natl. Cancer Inst. 20:787–824. [PubMed] [Google Scholar]
- Snell, G.D., and Jackson R.B.. 1958. Histocompatibility genes of the mouse. II. Production and analysis of isogenic resistant lines. J. Natl. Cancer Inst. 21:843–877. [PubMed] [Google Scholar]
- Snell, G.D., Wheeler N., and Aaron M.. 1957. A new method of typing inbred strains of mice for histocompatibility antigens. Transplant. Bull. 4:18–21. [PubMed] [Google Scholar]
- Snyder, S.H. 2013. Science interminable: Blame Ben? Proc. Natl. Acad. Sci. USA. 110:2428–2429. 10.1073/pnas.201300924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinman, R.M., Adams J.C., and Cohn Z.A.. 1975. Identification of a novel cell type in peripheral lymphoid organs of mice. IV. Identification and distribution in mouse spleen. J. Exp. Med. 141:804–820. [PMC free article] [PubMed] [Google Scholar]
- Steinman, R.M., and Cohn Z.A.. 1972a. The interaction of particulate horseradish peroxidase (HRP)-anti HRP immune complexes with mouse peritoneal macrophages in vitro. J. Cell Biol. 55:616–634. 10.1083/jcb.55.3.616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinman, R.M., and Cohn Z.A.. 1972b. The interaction of soluble horseradish peroxidase with mouse peritoneal macrophages in vitro. J. Cell Biol. 55:186–204. 10.1083/jcb.55.1.186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinman, R.M., and Cohn Z.A.. 1973. Identification of a novel cell type in peripheral lymphoid organs of mice. I. Morphology, quantitation, tissue distribution. J. Exp. Med. 137:1142–1162. 10.1084/jem.137.5.1142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinman, R.M., and Cohn Z.A.. 1974. Identification of a novel cell type in peripheral lymphoid organs of mice. II. Functional properties in vitro. J. Exp. Med. 139:380–397. 10.1084/jem.139.2.380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinman, R.M., Kaplan G., Witmer M.D., and Cohn Z.A.. 1979. Identification of a novel cell type in peripheral lymphoid organs of mice. V. Purification of spleen dendritic cells, new surface markers, and maintenance in vitro. J. Exp. Med. 149:1–16. 10.1084/jem.149.1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinman, R.M., Lustig D.S., and Cohn Z.A.. 1974. Identification of a novel cell type in peripheral lymphoid organs of mice. 3. Functional properties in vivo. J. Exp. Med. 139:1431–1445. 10.1084/jem.139.6.1431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinman, R.M., and Witmer M.D.. 1978. Lymphoid dendritic cells are potent stimulators of the primary mixed leukocyte reaction in mice. Proc. Natl. Acad. Sci. USA. 75:5132–5136. 10.1073/pnas.75.10.5132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinman, R.M., Witmer M.D., Nussenzweig M.C., Chen L.L., Schlesinger S., and Cohn Z.A.. 1980. Dendritic cells of the mouse: Identification and characterization. J. Invest Dermatol. 75:14–16. 10.1111/1523-1747.ep12521052 [DOI] [PubMed] [Google Scholar]
- Sun, J.C., and Bevan M.J.. 2004. Cutting edge: Long-lived CD8 memory and protective immunity in the absence of CD40 expression on CD8 T cells. J. Immunol. 172:3385–3389. 10.4049/jimmunol.172.6.3385 [DOI] [PubMed] [Google Scholar]
- Suss, G., and Shortman K.. 1996. A subclass of dendritic cells kills CD4 T cells via Fas/Fas-ligand-induced apoptosis. J. Exp. Med. 183:1789–1796. 10.1084/jem.183.4.1789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swiecki, M., and Colonna M.. 2015. The multifaceted biology of plasmacytoid dendritic cells. Nat. Rev. Immunol. 15:471–485. 10.1038/nri3865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taraban, V.Y., Rowley T.F., and Al Shamkhani A.. 2004. Cutting edge: A critical role for CD70 in CD8 T cell priming by CD40-licensed APCs. J. Immunol. 173:6542–6546. 10.4049/jimmunol.173.11.6542 [DOI] [PubMed] [Google Scholar]
- Theisen, D., and Murphy K.. 2017. The role of cDC1s in vivo: CD8 T cell priming through cross-presentation. F1000Res. 6:98. 10.12688/f1000research.9997.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theisen, D.J., Davidson J.T., Briseno C.G., Gargaro M., Lauron E.J., Wang Q., Desai P., Durai V., Bagadia P., Brickner J.R., et al. 2018. WDFY4 is required for cross-presentation in response to viral and tumor antigens. Science. 362:694–699. 10.1126/science.aat5030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsend, A.R., Gotch F.M., and Davey J.. 1985. Cytotoxic T cells recognize fragments of the influenza nucleoprotein. Cell. 42:457–467. 10.1016/0092-8674(85)90103-5 [DOI] [PubMed] [Google Scholar]
- Townsend, A.R., McMichael A.J., Carter N.P., Huddleston J.A., and Brownlee G.G.. 1984. Cytotoxic T cell recognition of the influenza nucleoprotein and hemagglutinin expressed in transfected mouse L cells. Cell. 39:13–25. 10.1016/0092-8674(84)90187-9 [DOI] [PubMed] [Google Scholar]
- Townsend, A.R., Rothbard J., Gotch F.M., Bahadur G., Wraith D., and McMichael A.J.. 1986. The epitopes of influenza nucleoprotein recognized by cytotoxic T lymphocytes can be defined with short synthetic peptides. Cell. 44:959–968. 10.1016/0092-8674(86)90019-x [DOI] [PubMed] [Google Scholar]
- Unanue, E.R. 1969. The immune response of mice to keyhole limpet hemocyanin bound to macrophages. J. Immunol. 102:893–898. [PubMed] [Google Scholar]
- Unanue, E.R., and Askonas B.A.. 1968. Persistence of immunogenicity of antigen after uptake by macrophages. J. Exp. Med. 127:915–926. 10.1084/jem.127.5.915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unanue, E.R., Cerottini J.C., and Bedford M.. 1969. Persistence of antigen on the surface of macrophages. Nature. 222:1193–1195. 10.1038/2221193a0 [DOI] [PubMed] [Google Scholar]
- Vainio, T., Koskimies O., Perlmann P., Perlmann H., and Klein G.. 1964. In vitro cytotoxic effect of lymphoid cells from mice immunized with allogeneic tissue. Nature. 204:453–455. 10.1038/204453a0 [DOI] [PubMed] [Google Scholar]
- von Boehmer, H., Haas W., and Jerne N.K.. 1978. Major histocompatibility complex-linked immune-responsiveness is acquired by lymphocytes of low-responder mice differentiating in thymus of high-responder mice. Proc. Natl. Acad. Sci. USA. 75:2439–2442. 10.1073/pnas.75.5.2439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vremec, D., Zorbas M., Scollay R., Saunders D.J., Ardavin C.F., Wu L., and Shortman K.. 1992. The surface phenotype of dendritic cells purified from mouse thymus and spleen: Investigation of the CD8 expression by a subpopulation of dendritic cells. J. Exp. Med. 176:47–58. 10.1084/jem.176.1.47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker, E.B., Lanier L.L., and Warner N.L.. 1982. Concomitant induction of the cell surface expression of Ia determinants and accessory cell function by a murine macrophage tumor cell line. J. Exp. Med. 155:629–634. 10.1084/jem.155.2.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams, J.W., Tjota M.Y., Clay B.S., Lugt B.V., Bandukwala H.S., Hrusch C.L., Decker D.C., Blaine K.M., Fixsen B.R., Singh H., et al. 2013. Transcription factor IRF4 drives dendritic cells to promote Th2 differentiation. Nat. Commun. 4:2990. 10.1038/ncomms3990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, L., Li C.L., and Shortman K.. 1996. Thymic dendritic cell precursors: Relationship to the T lymphocyte lineage and phenotype of the dendritic cell progeny. J. Exp. Med. 184:903–911. 10.1084/jem.184.3.903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu, S.J., Niknafs Y.S., Kim S.H., Oravecz-Wilson K., Zajac C., Toubai T., Sun Y., Prasad J., Peltier D., Fujiwara H., et al. 2017. A critical analysis of the role of SNARE protein SEC22B in antigen cross-presentation. Cell Rep. 19:2645–2656. 10.1016/j.celrep.2017.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yewdell, J.W., Bennink J.R., and Hosaka Y.. 1988. Cells process exogenous proteins for recognition by cytotoxic T lymphocytes. Science. 239:637–640. 10.1126/science.3257585 [DOI] [PubMed] [Google Scholar]
- Yin, X., Chen S., and Eisenbarth S.C.. 2021. Dendritic cell regulation of T helper cells. Annu. Rev. Immunol. 39:759–790. 10.1146/annurev-immunol-101819-025146 [DOI] [PubMed] [Google Scholar]
- Zehner, M., Marschall A.L., Bos E., Schloetel J.G., Kreer C., Fehrenschild D., Limmer A., Ossendorp F., Lang T., Koster A.J., et al. 2015. The translocon protein Sec61 mediates antigen transport from endosomes in the cytosol for cross-presentation to CD8(+) T cells. Immunity. 42:850–863. 10.1016/j.immuni.2015.04.008 [DOI] [PubMed] [Google Scholar]
- Zhang, J., Raper A., Sugita N., Hingorani R., Salio M., Palmowski M.J., Cerundolo V., and Crocker P.R.. 2006. Characterization of Siglec-H as a novel endocytic receptor expressed on murine plasmacytoid dendritic cell precursors. Blood. 107:3600–3608. 10.1182/blood-2005-09-3842 [DOI] [PubMed] [Google Scholar]
- Ziegler, H.K., and Unanue E.R.. 1982. Decrease in macrophage antigen catabolism caused by ammonia and chloroquine is associated with inhibition of antigen presentation to T cells. Proc. Natl. Acad. Sci. USA. 79:175–178. 10.1073/pnas.79.1.175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinkernagel, R.M., Callahan G.N., Althage A., Cooper S., Streilein J.W., and Klein J.. 1978. The lymphoreticular system in triggering virus plus self-specific cytotoxic T cells: Evidence for T help. J. Exp. Med. 147:897–911. 10.1084/jem.147.3.897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinkernagel, R.M., and Doherty P.C.. 1974. Restriction of in vitro T cell-mediated cytotoxicity in lymphocytic choriomeningitis within a syngeneic or semiallogeneic system. Nature. 248:701–702. 10.1038/248701a0 [DOI] [PubMed] [Google Scholar]
- Zou, L., Zhou J., Zhang J., Li J., Liu N., Chai L., Li N., Liu T., Li L., Xie Z., et al. 2009. The GTPase Rab3b/3c-positive recycling vesicles are involved in cross-presentation in dendritic cells. Proc. Natl. Acad. Sci. USA. 106:15801–15806. 10.1073/pnas.0905684106 [DOI] [PMC free article] [PubMed] [Google Scholar]