Abstract
Objective:
To examine the association between severe maternal morbidity (SMM) and infant health using the additional infant costs and length of stay (LOS) as markers of added clinical complexity.
Study Design:
Secondary data analysis using California linked birth certificate-patient discharge data for 2009–2011 (N=1,260,457). Regression models were used to estimate the association between SMM and infant costs and LOS.
Results:
The 16,687 SMM-exposed infants experienced a $6,550 (33%) increase in costs and a 0.7 (18%) day increase in LOS. Preterm infants had ($11,258 (18%) added costs and 1.3 days (8.1%) longer LOS) than term infants ($2,539 (38%) added costs and 0.5 days (22%) longer LOS).
Conclusions:
SMM was associated with increased infant costs and LOS, suggesting that SMM may have adverse health effects for infants, including term infants. The relatively larger effect on costs indicates an increase in treatment intensity (clinical severity) greater than additional LOS.
INTRODUCTION
Severe maternal morbidity (SMM) has been defined by the Centers for Disease Control and Prevention (CDC) as the “unexpected outcomes of labor and delivery that result in significant short or long-term consequences to a woman’s health” (1, 2). SMM has been steadily increasing in recent years and now annually affects more than 50,000 (about 1.5%) women who give birth each year in the United States (3). Maternal complications often affect the health of their infants, but the effects of SMM on infant health are poorly understood. Given that many maternal conditions that precede or lead to the experience of SMM will start prior to delivery, these adverse maternal outcomes may influence the health of the infant through increases in the prevalence of such conditions as hypoxic ischemic encephalopathy or infection. In addition, SMM may result from pre-existing maternal medical conditions such as hypertension or diabetes, which may affect infant growth or development in utero. Finally, other social determinants of health such as household income, educational attainment, and employment may act both to increase the risk of a mother developing SMM and to negatively alter the infant’s health independent of the direct clinical course. These factors can potentially affect the rates of preterm delivery, complications, or increased severity of illness regardless of gestation.
However, there are currently little data on the effects of SMM on infant outcomes. Our literature search only identified one prior study that directly examined the association between SMM and infant health (4). The researchers used all births in Ontario from 2002 to 2017 and found that CDC-defined SMM was associated increased infant mortality and sepsis. It is plausible that the associations between SMM and infant health extend beyond mortality and sepsis; SMM is associated with much higher rates of preterm birth, which is a pathway to infant complications that lead to increased neonatal hospital costs and lengths of stay (LOS) (5). We hypothesized that SMM would be associated with increased costs and LOS for the infant’s delivery hospitalization, recognizing that increases in costs and LOS are markers of additional clinical complexity.
In this paper we used maternal-infant linked, population-based data from California to study the association between SMM and infant costs and length of stay. In addition to the overall associations, we also examined if these effects differed between preterm and term infants, and how they varied when the definition of SMM was restricted to a more focused measure that excludes cases where the only indicator of SMM was a maternal blood transfusion (1, 2). This restricted CDC measure identifies more severe SMM, and hence may have a different impact on infant health than SMM that occurs secondary to maternal blood transfusions.
METHODS
We used a previously described administrative dataset of the birth certificates linked to the maternal and infant hospital discharge records for all in-hospital deliveries that occurred in California non-Federal hospitals between 2009 and 2011 (6). This dataset was designed to examine the maternal and infant hospital costs of all in-hospital deliveries, including transfers and readmissions. Briefly, the California Office of Statewide Planning and Development (OSHPD)Vital Statistics-Patient Discharge Data contain maternal and infant hospital discharge records probabilistically linked with birth, infant death, and fetal death certificates to provide linked information for mother/baby pairs (7). These data include maternal antepartum hospital records for the nine months prior to delivery (or in-hospital fetal death), maternal and infant hospital discharge records for the delivery admission, maternal readmissions, and any infant or maternal transfers. For the primary analysis we only included SMM identified during the maternal delivery hospitalization, with a sensitivity analysis that included SMM identified only through maternal hospital readmission up to 42 days after post-partum discharge to provide a definition of SMM consistent with the only other study of the infant effects of SMM. This study was approved by the Institutional Review Boards at Stanford University, the Children’s Hospital of Pennsylvania and the California Department of Health. Part of both the DUA and the ethics/IRB approval from the California Department of Health explicitly prohibit any sharing of the data; thus the data are not available from the authors and anyone wanting the data must go through the data approval process with the California Department of Health in order to gain access to the data used for this study. The study was performed in accordance with the Declaration of Helsinki.
Cases were selected if the birth certificate was successfully linked to both the maternal delivery record and the infant birth hospital discharge abstract,. The OSHPD annual hospital financial data for 2009–2011 were used to construct cost-to-charge ratios for each hospital and then to convert hospital charges recorded in the maternal and infant hospital discharge records to estimate the costs of each maternal and infant encounter (8). Data on the mean professional/physicians fees for each Diagnosis Related Group (DRG) and payer source (Medicaid or private insurance) were matched to the DRGs of each hospital discharge to estimate professional fees, with separate adjustment factors for Medicaid and private insurance (9). The Bureau of Labor Statistics Producer Price Index was used to adjust costs to December 2017 values (10, 11).
These data excluded cases when reported charges were missing and cases that were missing birthweight or gestational age (6). The main reason cases were excluded was missing hospital charge data, of which 98% were excluded because they included one or more stays at a hospital operated by the Kaiser Permanente health system which does not report hospital charges. Cases were retained only if cost and LOS information were available for both the mother and infant. The final sample included 1,246,859 study cases. The cohort identificiation flow diagram is shown in appendix Figure A-1.
We used the CDC definition of SMM; the complete list of the conditions and the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes used to define them are shown in Appendix Table A-1 (1, 2). While the CDC definition of SMM includes cases where SMM is identified within 42 days of delivery, given that we are focused on how SMM affects infant health, we restricted the primary identification of SMM to the mother’s delivery and included the full definition that includes readmissions to allow a sensitivity analyses. A limitation of the CDC definition of SMM is that the most common indicator of SMM (now accounting for more than half of cases), is receipt of a blood transfusion without any other condition captured by the SMM definition, regardless of the number of units administered because such data are not generally available (12, 13). Most patients in this category only receive 1 or 2 units of blood products and are not at high-risk for serious complications. The CDC has subsequently provided a second, more focused definition of SMM that excludes cases where the only indicator for SMM was a transfusion. Thus, we also created separate indicators for each case of SMM to separately identify transfusion-only SMM and all other indicators for SMM, non-transfusion (ntSMM), consistent with the CDC guidance and prior research (14–16). Some of the cases identified as ntSMM also received a transfusion in addition to one or more other indications for SMM.
To address the skewness of the distributions of costs and LOS, we used generalized linear models with a gamma distribution and a log link to estimate associations between SMM and infant costs and LOS, controlling for race/ethnicity, cesarean delivery, preterm delivery, type of insurance, parity, maternal age and BMI, multiple births, an obstetric comorbidity index (see Appendix Table A-2 for full definition), gestational age, infant sex, and serious congenital anomalies (17). The costs and LOS are until hospital discharge (including transfers) or death, and the costs are the total infant costs (hospital and physician). Because preterm birth is associated with SMM and baseline costs and LOS for preterm infants are much higher than for term infants (5, 6), we re-estimated models separately for term (≥37 weeks’ gestation) and preterm (<37 weeks’ gestation) infants to see if the effects of SMM extend beyond preterm infants. The “margins” command in Stata was used to generate estimates of the dollar or day effects of SMM.
Given that some previous studies have found that controlling for the hospital where the delivery occurs affects the likelihood of SMM (essentially that hospital quality can affect the likelihood of SMM) (18–20), we estimated models that included hospital-specific fixed effects. This method effectively controls for differences in hospital quality. Unfortunately, several of these models did not converge, almost certainly due to the rarity of SMM in many of the hospitals with low patient volumes for delivery. We compared the results of the models with and without fixed-effects for the subset of models that did converge and found the results were the similar to the models without hospital fixed-efects. This is consistent with a recently published study looking at disparities using the same California data that we used that found much smaller effects of controlling for hospital quality in California than the previous reports have found using New York City data (21, 22).
The main results are reported using SMM occurring during the delivery hospitalization on the premise that if the mother develops a SMM-related diagnosis after she has been discharged from the delivery hospitalization that this is unlikely to affect the infant. However, since the previous Canadian study examining the effects of SMM on infant mortality and sepsis did include readmission SMM, we also re-estimated our main regression models including SMM during readmissions after discharge from birth hospitalization (reported in Appendix Table A-7). We also conducted a sensitivity analysis to see if controlling for repeat pregnancy by the same mother (about 10% of the total sample) affected the results.
RESULTS
Table 1 presents the descriptive statistics of the study sample stratified by whether the mother did or did not have SMM. Of the 1,260,457 infants in the sample, 16,687 (1.3%) were cases where the mother experienced SMM during the delivery hospitalization. The meaningful differences between the groups were that infants with SMM exposure were more likely to be Black (8.5% vs 5.2%), to be preterm (24.8% vs. 7.9%), to be a multiple birth (11.6% vs. 2.9%), to be delivered by cesarean (63.0% vs. 34.0%), and to have a diagnosis of sepsis (7.8% vs. 2.7%).
Table 1.
Patient Characteristics by Severe Maternal Morbidity (SMM) Status
| No SMM | Any SMM | P-value | |
|---|---|---|---|
| N | 1,243,770 | 16,687 | |
| Total Cost (hospital and physician) of Infant Unitl Hospital Discharge | $6,152 ($38,180) |
$24,027 ($86,500) |
<.0001 |
| Length of Stay of Infant Until Hospital Discharge | 3.4 (8.1) |
8.6 (17.2) |
<.0001 |
| Male Infant | 637,778 (51.3%) |
8,385 (50.2%) |
0.008 |
| Infant Race/ethnicity | |||
| Asian | 129,805 (10.4%) |
1,609 (9.6%) |
<.001 |
| Black | 65,403 (5.2%) |
1,417 (8.5%) |
<.0001 |
| Hispanic | 609,482 (49.0%) |
8,550 (51.2%) |
<.0001 |
| Non-Hispanic White | 381,515 (30.7%) |
4,332 (26.0%) |
<.0001 |
| Other | 57,565 (4.6%) |
779 (4.7%) |
0.795 |
| Maternal age (y) | |||
| <=19 | 112,577 (9.1%) |
1,792 (10.7%) |
<.0001 |
| 20–29 | 603,695 (48.5%) |
7,336 (44.0%) |
<.0001 |
| 30–34 | 306,667 (24.7%) |
3,833 (23.0%) |
<.0001 |
| 35–39 | 173,843 (14.0%) |
2,684 (16.1%) |
<.0001 |
| >=40 | 46,981 (3.8%) |
1,042 (6.2%) |
<.0001 |
| Unknown age | 7 (0.0%) |
0 (0.0%) |
1.0 |
| Maternal insurance | |||
| Private insurance | 502,311 (40.4%) |
5,7658 (34.6%) |
<.0001 |
| Medicaid | 682,869 (54.9%) |
10,036 (60.1%) |
<.0001 |
| Other insurance | 58,590 (4.7%) |
883 (5.3%) |
0.040 |
| Education Level | |||
| No high school | 102,172 (8.2%) |
1,583 (9.5%) |
<.0001 |
| Some high school | 213,764 (17.2%) |
3,458 (20.7%) |
<.0001 |
| High school/GED | 315,904 (25.4%) |
4,215 (25.3%) |
0.687 |
| Some college | 219,019 (17.6%) |
2,772 (16.6%) |
<.001 |
| College grad or more | 348,909 (28.1%) |
4,041 (24.2%) |
<.0001 |
| Maternal weight | |||
| Underweight | 124,211 (10.0%) |
1,988 (11.9%) |
<.0001 |
| Overweight | 301,787 (24.3%) |
3,931 (23.6%) |
0.035 |
| Obese | 243,070 (19.5%) |
3,391 (20.3%) |
0.012 |
| Unknown weight | 76,576 (6.2%) |
1,304 (7.8%) |
<.0001 |
| Gestational Age | |||
| <28 Weeks | 4,706 (0.4%) |
359 (2.2%) |
<.0001 |
| 28–31 Weeks | 7,433 (0.6%) |
622 (3.7%) |
<.0001 |
| 32–36 Weeks | 85,825 (6.9%) |
3,160 (18.9%) |
<.0001 |
| 37–39 Weeks | 763,572 (61.4%) |
8,755 (52.5%) |
<.0001 |
| Multiple birth | 35,720 (2.9%) |
1,929 (11.6%) |
<.0001 |
| Parity = 1 | 480,271 (38.6%) |
6,825 (40.9%) |
<.0001 |
| Unknown parity | 393 (0.0%) |
13 (0.1%) |
0.003 |
| Primary cesarean birth | 422,431 (34.0%) |
10,505 (63.0%) |
<.0001 |
| Repeat cesarean birth | 198,111 (15.9%) |
3,681 (22.1%) |
<.0001 |
| Delivery SMM (transfusion only) | · | 10,210 (61.12%) |
|
| Delivery SMM (all other) | · | 6,477 (38.8%) |
|
| Infant Complications | |||
| Sepsis | 33,191 (2.7%) |
1,298 (7.8%) |
<.0001 |
| Any infection | 34,932 (2.8%) |
1,382 (8.3%) |
<.0001 |
| Hypoxic Ischemic Encephalopathy | 674 (0.1%) |
71 (0.4%) |
<.0001 |
| Modified Bateman Index* | 0.2 (0.7) |
1.0 (1.7) |
<.0001 |
| Congenital Anomaly Groups | |||
| Cardiac | 3,066 (0.2%) |
95 (0.6%) |
<.0001 |
| Coronary Heart Disease | 2,549 (0.2%) |
85 (0.5%) |
<.0001 |
| Chromosomal Syndromes | 1,241 (0.1%) |
41 (0.2%) |
<.0001 |
| Central Nervous System | 1,753 (0.1%) |
79 (0.5%) |
<.0001 |
| Gastrointestinal | 8,196 (0.7%) |
255 (1.5%) |
<.0001 |
| Genitourinary | 5,127 (0.4%) |
125 (0.7%) |
<.0001 |
| Pulmonary | 1,902 (0.2%) |
68 (0.4%) |
<.0001 |
| Skeletal | 101 (0.0%) |
2 (0.0%) |
0.396 |
| Skin | 52 (0.0%) |
1 (0.0%) |
0.507 |
| Other anomaly | 1,452 (0.1%) |
89 (0.5%) |
<.0001 |
| Any anomaly | 96,955 (7.8%) |
2,216 (13.3%) |
<.0001 |
Bateman obstetric comorbidity score modified to exclude variables directly included in the model or part of the definition of SMM; see Appendix Table for full definition of Bateman Index.
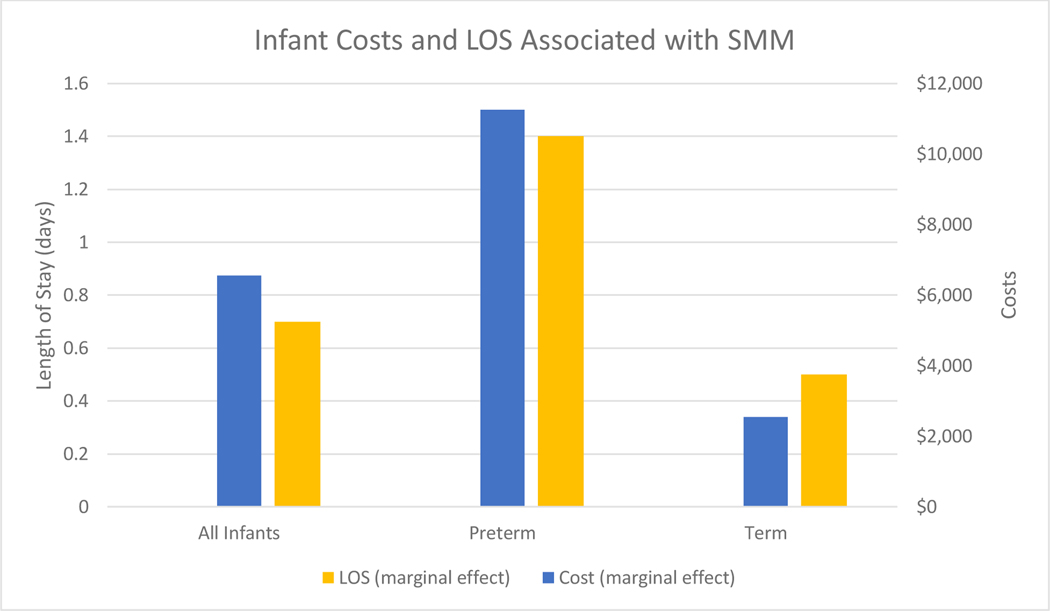
Figure 1 shows estimated infant costs and LOS (marginal effects (ME)) associated with SMM during the delivery hospitalization, beyond what would be expected without SMM; Table 2 reports the parameter estimates (percentage effects), the standard errors, and the exact value of these marginal effects (full regression results in Appendix Tables A-3 and A-4). Across all infants, costs were $6,550 higher (32.8%) with SMM and LOS was 0.7 days (18.1%) longer. Among preterm infants, SMM was associated with $11,258 (18.2%) higher costs and 1.3 days (8.1%) longer LOS. Among term infants, SMM was associated with $2,539 (37.9%) higher costs and 0.5 days (21.9%) longer LOS. For all groups, the relative increase in costs was around twice as large as the increase in LOS, indicating that these infants had an increase in their treatment intensity in addition to longer stays in the hospital, almost certainly associated with increased severity of illness.
Figure 1:
Marginal Increase in Infant Costs and Length of Stay Associated with Severe Maternal Morbidity
Table 2.
Regression estimates of additional infant costs and lengths of stay associated with severe maternal morbidity occurring during the birth hospitalization
| All Infants | Preterm | Term | |
|---|---|---|---|
| Additional Costs | 0.328 (0.0186) |
0.182 (0.0286) |
0.377 (0.0219) |
| $6,550 | $11,258 | $2,539 | |
| Additional Length of Stay | 0.181 (0.0072) |
0.081 (0.0150) |
0.219 (0.0082) |
| 0.7 days | 1.3 days | 0.5 days |
All significant at P<0.0001
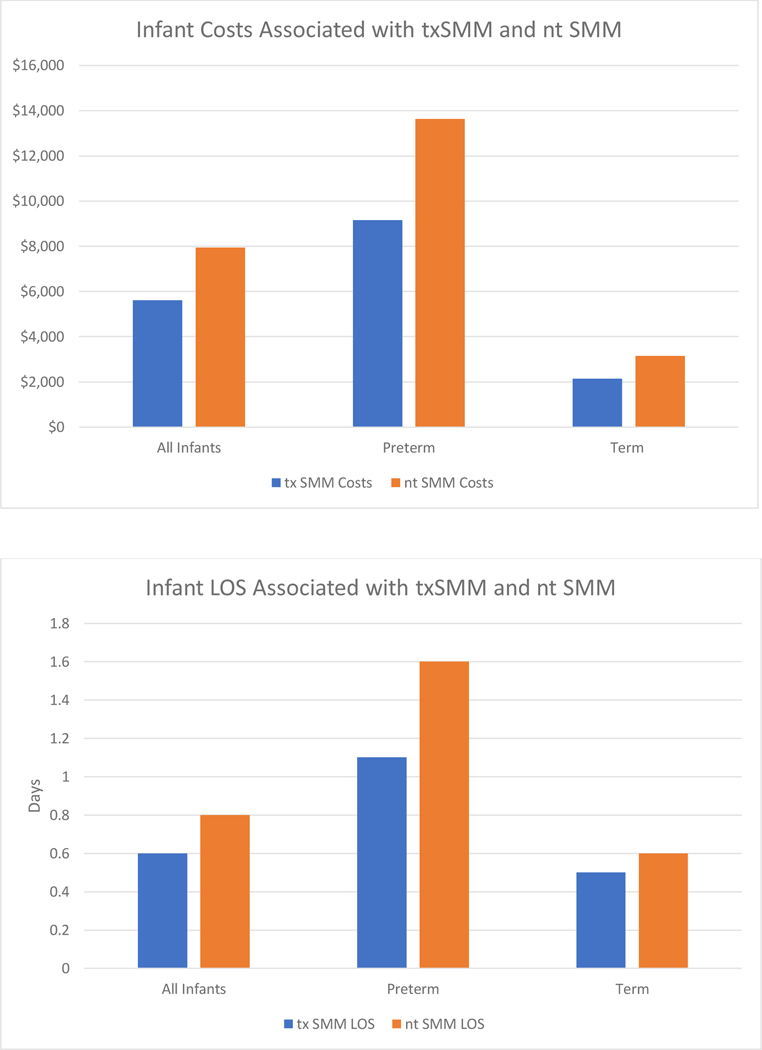
We repeated these analyses splitting SMM into transfusion-only SMM and ntSMM. Figure 2 shows the marginal effects; the top panel shows the marginal effects for costs and the bottom panel shows them for LOS. Table 3 reports the parameter estimates (percentage effects), the standard errors, and the exact value of these marginal effects (full regression results in Appendix Tables A-5 and A-6)). These results show that the effects for SMM on costs and LOS are always larger for ntSMM than for transfusion-only SMM ($5,606 and 0.6 days for transfusion only SMM vs. $7,941 and 0.8 days for ntSMM, with a similar pattern for the preterm and term subsets. Consistent with the overall effects, the absolute effects are larger for the preterm infants and the relative effects are larger for the term infants. These effects were similar when SMM occurring only during a maternal hospital readmission were included in the cohort, and when we adjusted for maternal repeat deliveries in the cohort.
Figure 2:
Marginal Increase in Infant Costs and Length of Stay Associated with Severe Maternal Morbidity, by Transfusion Only SMM (txSMM) vs. non-Transfusion SMM (ntSMM)
Table 3.
Regression estimates of additional infant costs and lengths of stay associated with major subtypes of severe maternal morbidity occurring during the birth hospitalization
| Additional Costs | All Infants | Preterm | Term |
|---|---|---|---|
| Transfusion-only SMM | 0.281 (0.0092) |
0.148 (0.0248) |
0.318 (0.0101) |
| $5606 | $9,1490 | $2,144 | |
| Non-transfusion SMM | 0.398 (0.0115) |
0.220 (0.0266) |
0.473 (0.0133) |
| $7,941 | $13,629 | $3,150 | |
| Additional LOS | |||
| Transfusion-only SMM | 0.167 (0.0048) |
0.067 (0.0156) |
0.198 (0.0051) |
| 0.6 days | 1.1 days | 0.5 days | |
| Non-transfusion SMM | 0.203 (0.0060) |
0.097 (0.0167) |
0.256 (0.0067) |
| 0.8 days | 1.6 days | 0.6 days |
All significant at P<0.0001
DISCUSSION
This analysis provides empirical evidence that severe maternal morbidity is assoiciated with infant health even after adjusting for gestational age and other potential confounders. We found that SMM was associated with increased infant costs and length of stay during the birth hospitalization. The associations between SMM and infant costs and LOS were observed among both term and preterm infants. Thus, the cost and LOS effects of SMM are not just due to the fact that SMM is associated with higher rates of preterm delivery (5). The cost effects we found were about twice as large as the LOS effects, which indicates that the increase in treatment intensity (likely owing to higher clinical severity) was greater than the added infant LOS associated with SMM. We also found that the effects of SMM were largest among infants born to patients with non-transfusion SMM, which represents the most severe forms of SMM.
This study builds upon the sparse existing evidence that SMM is associated with infant health. One previous study of this relationship found associations between SMM and infant mortality and sepsis (4). This study used the standard CDC definition of SMM, which includes maternal readmissions up to 42 days after delivery, while our study restricted SMM to those cases identified during the delivery hospitalization in order to focus on infant outcomes. Readmission SMM composes about 12% of all SMM cases (23), so the distinction is important. As Appendix Table A-7 shows, the results using the expanded definition of SMM are virtually identical to those with our more restrictive definition of infant SMM exposure, which is what one would expect given the implausible temporal relationship between readmission SMM and the costs and LOS of the infants delivery hospitalization.
There are a wide range of infant outcomes that SMM could potentially influence. For this study, we chose to look at infant costs and length of stay (LOS) as they are sensitive all-cause indicators of the need for additional treatment; when infants experience complications it can increase both the intensity of treatment and the length of hospitalization. This study provides initial evidence of the close relationship between the health of an obstetric patient and their infant. The fact that SMM not only affects obstetric patients, but may also adversely affect at least some of the infants of patients who experience SMM adds to the already compelling need for efforts to address SMM. Most cases of SMM are potentially preventable (24), and prevention may not only result in better health and cost savings for obstetric care, but may also improve outcomes and reduce costs for infant care. Currently, there is growing attention to the issues of maternal morbidity and mortality, but a lack of data has contributed to limited attention to the full potential benefits of improving maternal health, including how SMM may affect infants. Clinical and policy efforts addressing obstetric care access, quality and outcomes may also affect neonatal and infant health, further highlighting the dyadic nature of pregnancy complications. While these data do not allow assertainment of causation, the associations merit further investigation and add urgency to clinical and policy efforts to reduce SMM. Indeed, prevention of SMM represents an opportunity for true “perinatal medicine” as was envisioned as high quality care for the maternal-infant dyad.
The estimated additional infant costs per case of SMM of $6,550 to the 16,687 infants exposed to delivery SMM in this study sample could comprise added costs of $109 million, and the additional treatment for these infants may have required an additional 11,700 hospital days. If one assumes that the 80% of deliveries included in this study are broadly representative of all California deliveries, the total impacts of SMM on infant health care are $137 million in added costs and over 14,600 additional hospital days over 3 years. As a rough projection, California accounts for 1/8th of US deliveries and average US hospital costs are about 70% of California average (25), resulting in a national estimate of $255 million in additional annual infant costs associated with SMM and 39,000 additional annual hospital days. These additional costs are of similar magnitude to the additional maternal costs associated with SMM, essentially doubling any estimate of the potential savings associated with preventing SMM, when accounting for effects on the mother-infant dyad (26).
Our study does have some limitations. Since we only had hospital discharge and birth certificate data we could only look at association between SMM and infant costs and LOS; we did not have the ability to identify which infants suffered adverse effects from the maternal condition or what these complications were. Further research is needed to understand the biological and clinical pathways that are driving the additional infant costs and LOS associated with maternal SMM (5). We also acknowledge that for term infants, a small proportion of the additional costs and LOS may be related to healthy infants waiting for maternal discharge, but given that the cost effects were much larger than the LOS effects, this was not a major driver of our findings. While we limited our definition of SMM to cases that occurred during the delivery hospitalization, the data in the hospital discharge abstracts do not include any time stamps for the diagnoses so it is likely that some of the cases of SMM had clinical pathways such that they would not have had any effect on infant health. To the extent that this occurred, which we are unable to assess in these data, it would bias our estimates downward, as we are assessing the impact of SMM on infant health without interventions. Further, our regression models control for gestational age at delivery, which will bias our estimates downward to the extent that SMM causes earlier delivery.
The data used for this study are older, based on hospitalizations during 2009–2011. The data used in this study are the most recent US-based data available that can address this issue. To our knowledge, this study dataset is the only one available in the U.S. that contains linked data (birth certificates linked to hospital discharge abstracts for mothers and infants, including transfers) that also has accurate cost estimates. Maternal-infant linkage with transfers, which are not available in standard datasets, provides the capability for linked data on maternal and infant outcomes of pregnancy, which is essential to study the association of SMM with infant outcomes. These data are available for a very limited number of states and, to our knowledge, the California data we used are the only ones with valid cost estimates, where the charge data have been converted to estimated costs with careful screening to eliminate outlier values that are inconsistent with the care provided (6). As a result, the findings of this study do need to be validated with more recent data as it becomes available. We believe that these data are still relevant to today’s population and highlight an important yet unstudied at-risk population to examine in light of the rising SMM rates in the US. Finally, future studies may examine this association in greater depth from a maternal-infant dyad perspective and also from a broader facility, neighborhood, community, or policy perspective (27).
CONCLUSION
Severe maternal complications of childbirth are associated with increased costs and hospital length of stay for infants born to patients who suffer SMM. Cost-effectively improving the health of both obstetric and neonatal patients may require efforts and programs that target upstream clinical and social risks for SMM.
Supplementary Material
Acknowledgments
Funding/Support: Partial support provided by NIH/NICHD R01s HD084819 and HD099197
Role of Funder/Sponsor (if any): The NICHD had no role in the design and conduct of the study.
Abbreviations:
- SMM
Severe maternal morbidity
- CDC
Centers for Disease Control and Prevention
- LOS
Length of Stay
- DRG
Diagnosis Related Group
- ME
Marginal effects
Footnotes
Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States Government.
Conflict of Interest Disclosures (includes financial disclosures) : The authors have no conflicts of interest relevant to this article to disclose.
References
- 1.Centers for Disease Control and Prevention. Severe maternal morbidity in the United States [Internet]. [updated 2017 Nov 27; cited 2018 Oct 2]. Available from: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/severematernalmorbidity.html
- 2.Centers for Disease Control and Prevention. Severe maternal morbidity indicators and corresponding ICD codes during delivery hospitalizations [Internet]. [updated 2018 Aug 21; cited 2018 Oct 2]. Available from: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/smm/severe-morbidity-ICD.htm
- 3.Centers for Disease Control and Prevention. Maternal mortality [Internet]. [cited 2020 Jul 8]. Available from: https://www.cdc.gov/nchs/maternal-mortality/index.htm
- 4.Aoyama K, Park AL, Davidson AJF, Ray JG. Severe maternal morbidity and infant mortality in Canada. Pediatrics. 2020;146(3). [DOI] [PubMed] [Google Scholar]
- 5.Kilpatrick SJ, Abreo A, Gould J, Greene N, Main EK. Confirmed severe maternal morbidity is associated with high rate of preterm delivery. Am J Obstet Gynecol. 2016;215(2):233.e1–7. [DOI] [PubMed] [Google Scholar]
- 6.Phibbs CS, Schmitt SK, Cooper M, Gould JB, Lee HC, Profit J, et al. Birth hospitalization costs and days of care for mothers and neonates in California, 2009–2011. J Pediatr. 2019;204:118–25.e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Herrchen B, Gould JB, Nesbitt TS. Vital statistics linked birth/infant death and hospital discharge record linkage for epidemiological studies. Comput Biomed Res. 1997;30:290–305. [DOI] [PubMed] [Google Scholar]
- 8.California Office of Statewide Health Planning and Development. Hospital annual financial data 2017. [Internet]. [cited 2016 Aug 25]. Available from: https://www.oshpd.ca.gov/HID/Hospital-Financial.asp
- 9.Peterson C, Xu L, Florence C, Grosse SD, Annest JL. Professional fee ratios for US hospital discharge data. Med Care. 2015;53:840–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Crawford M, Church J, Akin B, eds. Bureau of Labor Statistics. 2017. Producer Price Index [Internet]. [cited 2018 Apr 23]. Available from: https://www.bls.gov/bls/news-release/ppi.htm#2017
- 11.Dunn A, Grosse SD, Zuvekas SH. Adjusting health expenditures for inflation: a review of measures for health services research in the United States. Health Serv Res. 2018;53(1):175–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grobman WA, Bailit JL, Rice MM, Wapner RJ, Reddy UM, Varner MW, et al. Frequency of and factors associated with severe maternal morbidity. Obstet Gynecol. 2014;123:804–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Callaghan WM, Creanga AA, Kuklina EV. Severe maternal morbidity among delivery and postpartum hospitalizations in the United States. Obstet Gynecol. 2012;120:1029–36. [DOI] [PubMed] [Google Scholar]
- 14.Leonard SA, Main EK, Scott KA, Profit J, Carmichael SL. Racial and ethnic disparities in severe maternal morbidity prevalence and trends. Ann Epidemiol. 2019;33:30–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leonard SA, Kennedy CJ, Carmichael SL, Lyell DJ, Main EK. An expanded bbstetric comorbidity scoring system for predicting severe maternal morbidity. Obstet Gynecol. 2020;136:440–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Main EK, Leonard SA, Menard MK. Association of maternal comorbidity with severe maternal morbidity: a cohort study of California mothers delivering between 1997 and 2014. Ann Intern Med. 2020;173(11 Suppl):S11–S8. [DOI] [PubMed] [Google Scholar]
- 17.Bateman BT, Mhyre JM, Hernandez-Diaz S, Huybrechts KF, Fischer MA, Creanga AA, et al. Development of a comorbidity index for use in obstetric patients. Obstet Gynecol. 2013;122:957–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Howell EA, Janevic T, Hebert PL, Egorova NN, Balbierz A, Zeitlin J. Differences in morbidity and mortality rates in black, white, and Hispanic very preterm infants among New York City hospitals. JAMA Pediatr. 2018;172:269–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Howell EA, Janevic T, Blum J, Zeitlin J, Egorova NN, Balbierz A, et al. Double disadvantage in delivery hospital for Black and Hispanic women and high-risk infants. Matern Child Health J. 2020;24:687–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Howell EA, Egorova NN, Janevic T, Brodman M, Balbierz A, Zeitlin J, et al. Race and ethnicity, medical insurance, and within-hospital severe maternal morbidity disparities. Obstet Gynecol. 2020;135:285–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mujahid MS, Kan P, Leonard SA, Hailu EM, Wall-Wieler E, Abrams B, et al. Birth hospital and racial and ethnic differences in severe maternal morbidity in the state of California. Am J Obstet Gynecol. 2021;224(2):219.e1–219.e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Howell EA, Egorova NN, Balbierz A, Zeitlin J, Hebert PL. Site of delivery contribution to black-white severe maternal morbidity disparity. Am J Obstet Gynecol. 2016;215:143–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Girsen AI, Sie L, Carmichael SL, Lee HC, Foeller ME, Druzin ML, et al. Rate and causes of severe maternal morbidity at readmission: California births in 2008–2012. J Perinatol. 2020;40(1):25–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Petersen EE, Davis NL, Goodman D, Cox S, Mayes N, Johnston E, et al. Vital signs: pregnancy-related deaths, United States, 2011–2015, and strategies for prevention, 13 states, 2013–2017. MMWR Morb Mortal Wkly Rep. 2019;68:423–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaiser Family Foundation. Hospital adjusted expenses per inpatient day by ownership [Internet]. [cited 2016 Dec 13]. Available from: http://kff.org/other/state-indicator/expenses-per-inpatient-day-by-ownership/?currentTimeframe=0
- 26.Phibbs CM, Kozhimannil KB, Leonard S, Lorch SA, Main EK, Schmitt SK, et al. A comprehensive analysis of the costs of severe maternal morbidity. Womens Health Issues (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Janevic T, Zeitlin J, Egorova N, Hebert PL, Balbierz A, Howell EA. Neighborhood racial and economic polarization, hospital of delivery, and severe maternal morbidity. Health Aff (Millwood). 2020;39:768–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.