Abstract
The number of waitlisted lung transplant candidates exceeds the availability of donor organs. Barriers to utilization of donor lungs include suboptimal lung allograft function, long ischemic times due to geographical distance between donor and recipient, and a wide array of other logistical and medical challenges. Ex vivo lung perfusion (EVLP) is a modality that allows donor lungs to be evaluated in a closed circuit outside of the body and extends lung donor assessment prior to final acceptance for transplantation. EVLP was first utilized successfully in 2001 in Lund, Sweden. Since its initial use, EVLP has facilitated hundreds of lung transplants that would not have otherwise happened. EVLP technology continues to evolve and improve, and currently there are multiple commercially available systems, and more under investigation worldwide. Although barriers to universal utilization of EVLP exist, the possibility for more widespread adaptation of this technology abounds. Not only does EVLP have diagnostic capabilities as an organ monitoring device but also the therapeutic potential to improve lung allograft quality when specific issues are encountered. Expanded treatment potential includes the use of immunomodulatory treatment to reduce primary graft dysfunction, as well as targeted antimicrobial therapy to treat infection. In this review, we will highlight the historical development, the current state of utilization/capability, and the future promise of this technology.
Supplementary Information
The online version contains supplementary material available at 10.1007/s41030-022-00185-w.
Keywords: Ex vivo lung transplant, EVLP, Donor lung utilization, Donor lung conditioning, Cost-effectiveness, Lung transplant outcomes, Lung transplant volume
Key Summary Points
| Ex vivo lung perfusion (EVLP) is a rapidly developing and increasingly utilized technology to increase the lung donor pool for transplantation. |
| EVLP has evolved into a device for logistical optimization of the lung transplant process and increases the tolerability of cold ischemic time through its use. |
| Monitoring of the lung(s) on EVLP allows for more thorough evaluation of the lung(s) and increases confidence in donor lung utilization. |
| Issues such as atelectasis and pulmonary edema may be improved through the use of EVLP. Future opportunities for treatment of donor lung infection and immunomodulation exist on the EVLP platform. |
| Rapid and more universal adoption of EVLP remains limited by resource utilization. |
Digital Features
This article is published with digital features, including a video, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.19189520.
Introduction
Lung transplantation is the ultimate treatment for patients with various forms of end-stage lung disease. However, a large discrepancy between the number of patients awaiting transplantation and the number of suitable donor lungs has always existed. Despite a mismatch in supply and demand, utilization rates of donor lungs remain around 20% [1]. Often donor lungs are discarded over concerns regarding quality, time, or logistical constraints from organ procurement to transplantation, and the potential for future graft dysfunction [2]. This scarcity of appropriate donor lungs leads to a mortality rate of up to 30% of waitlisted patients [3]. Opportunities to increase the number of donor lungs available include the use of extended donor criteria (ECD) and donation after circulatory death (DCD) [4]. Ex vivo lung perfusion (EVLP) is a technology to optimize allograft assessment and function and in these less conventional situations to expand the donor pool for patients on the waiting list.
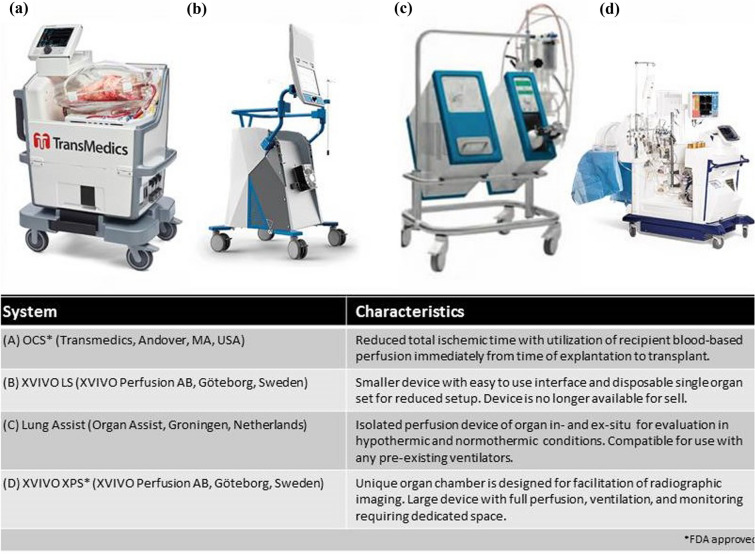
EVLP is a modality that allows donor lungs to be evaluated in a closed circuit outside of the body and extends lung donor assessment prior to final acceptance for transplantation [5]. Three EVLP protocols are currently in use worldwide emerging from Lund, Toronto, and the Organ Care System Lung [6]. The Lund protocol is the original protocol adapted further into the Toronto protocol, which is now the most commonly used. The third protocol includes the use of a transportable device that uniquely eliminates the need to keep lungs in static cold storage prior to transplant and effectively reduces the cold ischemic time [7]. There are currently four commercially available EVLP devices using one or a hybrid of the three standard protocols: Lung Assist™ by Organ Assist®, XVIVO Perfusion System (XPS)™ by XVIVO®, Vivoline LS1™ by Vivoline Medical®, and OCS™ by TransMedics® [9–11] (Fig. 1).
Fig. 1.
Commercially available EVLP systems
Each EVLP system consists of perfusion and ventilation in an enclosed and controlled unit to monitor function and maintain asepsis of the lungs. Lungs are ventilated through an endotracheal tube. A vascular circuit consists of outflow from the left atrium through a reservoir, pump, oxygenator, heater-cooler unit, and a leukocyte filter before entering back through the pulmonary artery [8]. The protocols can vary in perfusate, rate of flow, target left atrial pressure, and ventilatory settings [6].
While the lungs are on the circuit, a variety of assessments can be performed to evaluate organ quality. Depending on the system, this can include gross physical examination, radiographic imaging, bronchoscopy/airway inspection, pressure measurements to include lung compliance, and gas exchange. These dynamic assessments allow the treating team to monitor complications such as pulmonary edema, atelectasis, as well as identify suspicious tumors or mechanical issues such as iatrogenic procurement injury that may ultimately compromise the graft’s successful transplantation [12]. EVLP, in some cases, provides a mechanism to improve suboptimal donor lung quality through mechanical recruitment of atelectatic segments, therapeutic aspiration of secretions via bronchoscopy, and intravascular administration of anti-inflammatory and antibiotic therapies [13]. These benefits may significantly increase the number of lungs suitable for transplantation, thereby contributing to increased transplant volume. Though yet to be shown, the rehabilitation and utilization of even a small percentage of suboptimal donor lungs deemed otherwise unacceptable for transplant, may result in reduced waitlist mortality.
In this review, we present a brief overview of EVLP followed by an analysis of advantages and disadvantages in the current lung transplant landscape. We will then look to the future and evaluate potential uses for EVLP moving forward. This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors. The lung transplant recipient involved in the case study provided consent for the details of his clinical course to be disclosed in this manuscript.
History of EVLP
EVLP has been tested in a myriad of animal models including mice, guinea pigs, rabbits, dogs, and pigs as early as 1970 [14]. While animal models initially served as a cost-effective means for “proof-of-concept” pre-clinical model of EVLP, small organ size limited translatability to human use [15]. Given porcine lungs are similar to human lungs in size, physiology, and gene sequence making, it has become the preferred animal model [16]. The close relationship between porcine and human lungs allowed researchers to test the same equipment for the EVLP circuit that went on to be used in human clinical trials [15].
The first clinical application of EVLP in humans took place in 2001 at the University Hospital of Lund, Sweden. Steen and his colleagues originally intended for EVLP to be used as an assessment tool for lungs procured from a DCD donor [17]. During this first attempt, lungs were on the circuit for a brief time of 65 min but allowed for bronchoscopy and radiography to be completed [18]. Extending their success, the Lund group went on to show utility of EVLP in improving suboptimal/marginal lungs and completed the first transplant of lungs not meeting traditional donor criteria (ECD) in 2005 [19, 20].
The Toronto Lung Transplant Program took EVLP a step further by allowing an extended perfusion time of up to 12 h in a pre-clinical model [21]. This now meant that not only could lungs undergoing EVLP be evaluated closely over a longer time period, but also potentially reconditioned prior to transplantation. Building on the success of this technique, the initial clinical trial data reported the successful transplantation of 20 out of 23 marginal lungs after a period of 4 h of perfusion with improved gas exchange [22]. The study primarily highlighted that the use of EVLP overcame the historically significant higher rate of primary graft dysfunction (PGD) in marginal lungs in comparison to conventional donor lungs. In fact, there was a tendency of reduced rates of PGD at 72 h after transplant in the EVLP group. After successful use of EVLP by the Lund and Toronto groups, other centers worldwide began to experiment with their own EVLP circuits, although many lungs at these centers ultimately were not utilized [23]. However, use of the Lund and Toronto protocols over time increased conversion rates of utilization up to 90% for marginal lungs [13].
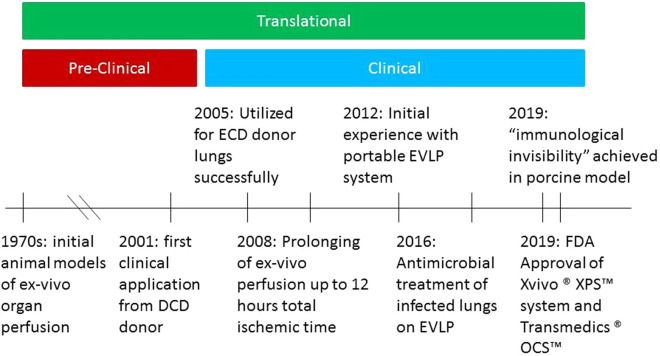
Advancements in technology have made EVLP more accessible and efficient since initial use (Fig. 2). The first models of EVLP in Lund and Toronto were operated manually and were performed in Plexiglass boxes [24]. As stated above, there are now four commercialized semi-automatic devices available each based on the original protocols, or in one case, a blend of them (Fig. 1). A major milestone in EVLP was the successful development of the first portable EVLP system, The Organ Care System™ (OCS™) Lung, a blending of Lund and Toronto protocols, eliminating the need for static cold preservation during transportation from the donor directly to a recipient. Results of the OCS™ Lung clinical trial (INSPIRE) were reported in 2018 [25]. Uniquely, recipient derived blood is used during the OCS™ EVLP process. Physiologic donor lung preservation with the OCS Lung was shown to be non-inferior to conventional lung transplant, with no significant difference in PGD, 30-day mortality, and 1-year survival. While this advancement revealed the safety and effectiveness of sparing prolonged cold ischemia, the direct effect of a portable versus static EVLP system remains unknown. Of note, a subsequent study of the OCS™ Lung showed nearly 87% conversion rate of ECD lungs [26].
Fig. 2.
Major developments in timeline of EVLP
As highlighted above, the goal of EVLP has been to increase the number of viable donor lungs and ultimately, a yet to be seen, decrease in mortality on the lung transplant waitlist. EVLP initially provided a platform for evaluation of the lungs for a short period of time after DCD to assess their viability for transplant. As techniques have improved and technology evolved, it has become possible to perfuse lungs ex vivo for longer periods of time to objectively assess lung quality and intervene to improve organ function. As we will detail later, EVLP can be further expected to evolve into an organ “repair” tool [27] (Fig. 2).
Application of EVLP in Lung Transplant
The practical application of EVLP is best understood within the context of a standard lung transplant. There is heterogeneity in the organ allocation process around the world. In the United States, organ allocation is done by the organ procurement organization (OPO) local to the donor hospital. Each OPO has its criteria for evaluation and donor management which requires juggling the needs of multiple organ systems. Lungs are generally allocated within a certain geographical radius by blood type, height range, and lung allocation (patient acuity) score. Should an organ meet a recipient center’s requirements (detailed below), lung(s) are accepted pending direct visual inspection at the time of procurement. When available, the lungs are evaluated by chest imaging, bronchoscopy, and serial blood gas analyses prior to procurement. Gross visual evaluation is done after the opening of the thoracic cage. Sometimes, physiologic testing of individual segments of the lung can be done by regional blood gas analysis at time of procurement. Upon acceptance in the operating room, the lungs are deflated and dissected away from the central airways and heart. This is followed by antegrade perfusion by a cooled acellular solution to help rapidly halt metabolism and clear donor blood which may contain damaging agents. Often corticosteroids and intravenous vasodilators (nitroglycerin/prostanoids) are used to help preserve vascular function and limit the inflammatory response to ischemia. Retrograde perfusion is done to exclude and remove pulmonary thrombi. The organ is preserved in the acellular, cooled solution for rapid transport to the center where a recipient awaits. After a recipient’s native lungs have been explanted, the donor organ is anastomosed, reperfused, and rewarmed by the recipient’s circulating blood. After adequate gas exchange and hemostasis is achieved, the thoracic cavity is closed and the patient is returned to the intensive care unit for monitoring [28].
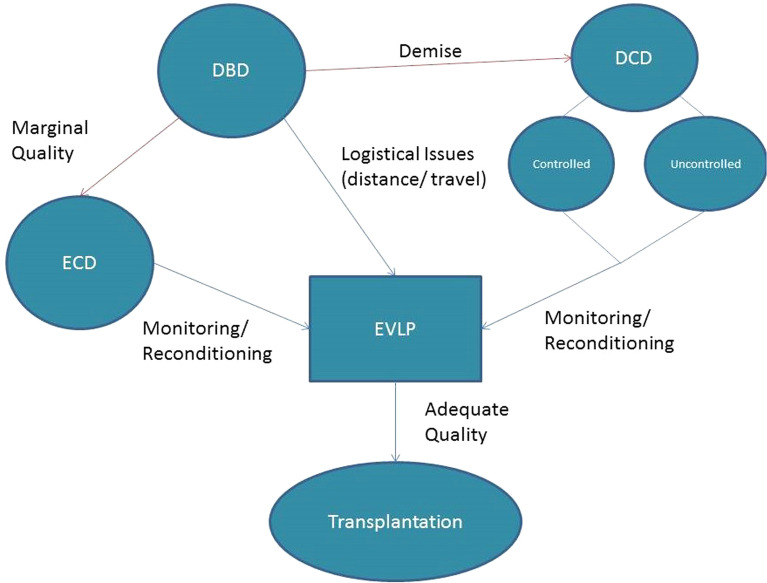
As we will show, EVLP can be used to overcome some of the key logistical challenges involved in the conventional lung transplant process (Fig. 3).
Fig. 3.
Utility of EVLP depending on donor type
Donor Quality
Traditional criteria for lung donors originated in the 1980s [29]. Based on initial criteria, the ideal donor is brain dead with preserved cardiovascular function, young (under age 55), with no acute or chronic lung disease, without significant smoking history, clear radiographically and on bronchoscopy, and geographically close to the recipient. To expand the donor pool, these criteria have been extended to include donors who may meet limited standards. To mitigate the risks of suboptimal lung allograft function in these cases, a lung donor scoring tool to predict outcomes and utilization rate was developed to confer confidence in transplanting these less optimal organs [29, 30]. Likewise, lungs from DCD donors can be successfully utilized, although there are unique challenges such as the unpredictability of time from withdrawal of life support to death (agonal time) as well as the occurrence of atelectasis and de-recruiting after withdrawal [31]. In addition, there may be limited data (bronchoscopy in particular) available prior to the time of procurement for DCDs given restrictions on invasive procedures for non-brain-dead donors in certain situations. These challenges can lead to “dry runs” in which an organ is evaluated in the operating room and deemed not transplantable due to excessive agonal time or poor organ quality [32]. “Dry runs” are resource intense, diverting surgical teams and transport systems away from other healthcare system needs. Retrospective analysis of referring Belgian centers showed that up to 7.4% of lung donors were declined at time of procurement due to concerns about organ quality [33].
Ischemic Time
The duration of time between procurement and implantation into the recipient is defined as the ischemic time—without perfusion. It consists of one or two phases, “cold” ± “warm” ischemia. Traditionally, an organ will only undergo “cold” ischemia during which preservation is targeted by reduction in metabolism using temperature regulation, using 4 °C solution and storage in an ice cooler. This is ideally limited to 4–6 h to ensure adequate function of the lung allograft, though studies suggest up to 9–10 h can be acceptable [34]. Travel distance is limited by cold ischemic time. Normothermic perfusion phase (also called warm ischemic time) describes the duration during which the organ is perfused and ventilated at physiologic temperature, 34–37 °C outside of the body. With the addition of a normothermic perfusion phase, total preservation time can be significantly extended [35].
Logistical Issues
Transplantation is a complex workflow that involves a myriad of healthcare providers and logistical support personnel. Organ procurement organizations (OPO) are regional and coordinate the recovery of multiple organs by distinct transplant teams. Organ procurement teams travel to the donor, the procured organ then is transported from the donor center to the recipient hospital, and inclement weather may result in unsafe travel at any point along the timeline. In most cases, while procurement is occurring, the recipient is undergoing preparation, and in some cases, explantation of the native lungs to minimize ischemic time. Many lung transplant recipients are admitted from home at the time of donor organ availability, thus travel to the transplant hospital and pre-operative preparation may delay the ability to begin the transplant. The need to optimally coordinate and time these processes ultimately affects the success of the transplant. Notable recent data from Australia highlights that up to 26% of all declined donor offers were due to logistical issues [36].
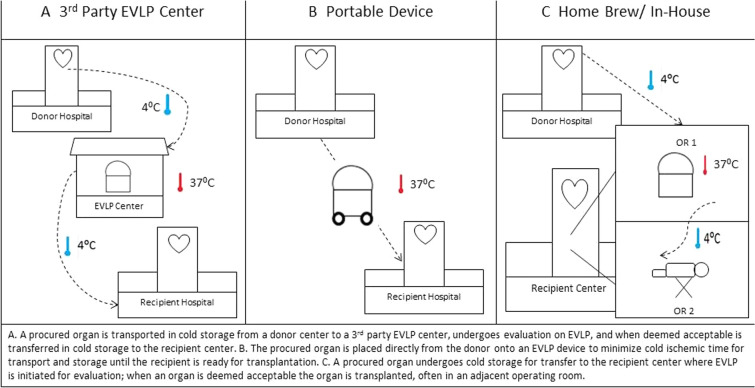
Conventional Lung Transplant vs. Lung Transplant with the Use of EVLP
Most commonly, cold preservation of the organ begins immediately after organ recovery for transport to the recipient hospital. When EVLP is utilized as an intermediate step, the lungs are either (1) placed on a portable EVLP device without cold preservation (OCS™) or placed in cold preservation and then (2) transported to a third-party EVLP facility, or (3) taken to the recipient transplant center and placed on EVLP in an operating room near the recipient. Notably, if a third-party facility is involved, the organ is cooled a second time after the completion of EVLP for transport to the recipient’s facility for transplantation (Fig. 4).
Fig. 4.
Schematic of application of EVLP during lung transplant
With use of the portable EVLP device (OCS™), the donor lungs are not placed on ice, rather directly placed on an ex vivo device to maintain warm perfusion with blood and ventilation. This mobile device is used to transport an organ from the donor center directly to the recipient hospital [7]. At time of removal from the circuit, the lungs are flushed with and immersed in cold acellular solution to allow for time for re-anastomosis (Fig. 4B).
Generally uniform across the platforms, organs are deemed acceptable for transplantation if compliance, airway pressures, and vascular resistance are stable or improving. As prescribed by the Food and Drug Administration for both currently approved systems, the lung(s) must have adequate gas exchange via perfusate gas sampling. The XPS system uses a change in absolute oxygen tension between the arterial and venous access during ventilation with 100% oxygen and a positive end expiratory pressure (PEEP) of 5 cm H20, with two values greater than 350 mmHg to deem an organ acceptable [37]. For the OCS™ Lung, a partial pressure of oxygen (PaO2) to fraction of inspired oxygen (FiO2) (P/F) ratio over 300 mmHg while ventilated using a PEEP of 5 cm H2O and FiO2 of 21% (room air) is required [38]. Radiographic improvement is desirable with recruitment of atelectasis and reduction of pulmonary edema. Lastly, a “collapse” or “deflation” test is performed to ensure normal global deflation (atelectasis) upon disconnection from positive pressure ventilation [22, 25] (See video 1 in the online/HTML version of the manuscript). Recent development of the COMPLETE score and utilization of P/F ratio with inflammatory score (by serial interleukin-6 and -8 measurement) seek to further standardize acceptance criteria across platforms [39].
Key Barriers to the Use of EVLP
The incorporation of EVLP into a lung transplant center’s practice involves an initial investment of time and resources. Fundamentally, the components can be conceptualized in three broad categories: personnel cost, the system (i.e., equipment and supplies) itself, and physical space. Depending on the EVLP system selected, there may be a significant initial capital investment for the equipment itself as well as hands-on training for responsible staff members. Estimated initial cost for commercially available systems range from $10,000 up to approximately $250,000, excluding replacement costs of disposable parts [40]. Additionally, operating room space for an EVLP procedure is necessary if a portable system is not utilized. This involves high level institutional commitment to growth of the lung transplant program [41]. Often, a sporadically used system that is resource intensive is difficult to justify in the hierarchy of institutional needs. For institutions less willing or able to make a large initial capital investment, outsourcing to a dedicated EVLP facility may be more practical (Table 1). In some cases, a center may decide that a combination approach may offer the most flexibility for their program.
Table 1.
Comparison of modalities
| EVLP modality | Initial capital investment | Cost per case | Space requirements | Transplant center staff requirements | Advantages | Disadvantages |
|---|---|---|---|---|---|---|
| Portable system | Significant | Supplies for case, staff pay including travel | Storage when not in use, transport space | Perfusionist(s) travel to procurements | No cold ischemic time, autonomy, may be more cost effective for high volume centers | Requires additional staff member training, availability, and travel to procurement |
| Transplant center system | Significant | Supplies for case, staff pay | Storage when not in use, dedicated operating room when in use | Perfusionist(s) operate device at institution | Autonomy, may be more cost effective for high volume centers, may allow for research protocols | Requires staff member training, availability, and operating room space |
| EVLP facility | None | Negotiated bundled fee per case | None | None | Less up-front cost and commitment, may appeal to small to medium-sized programs | Adds additional travel segment to EVLP facility, adds second cold ischemic time to travel to lung transplant center |
Training of transplant staff members on the selected EVLP system(s), guidelines for donor lung referral, logistics of referral, criteria for acceptance of lung(s) from EVLP, impact on timing of transplant cases, and modification of existing procedures and standards of practice are not standardized. The cost effectiveness of integration of EVLP into transplant center practice is an area of ongoing study [42–44]. EVLP has been shown to be profitable at the institutional level through increased transplant program volume, but each individual EVLP case costs approximately $US 40,000–50,000 more than a traditional transplant. The broader role within healthcare delivery on a state or national level remain difficult to determine. The National Health System in the United Kingdom attempted to assess this question during the DEVELOP-UK trial, showing that cost, on average, was about 35,000 GBP more per patient but the trial was stopped early due to a high need for ECMO in the EVLP arm [45].
Increasing Lung Transplant Volume
Utilization of EVLP can result in augmentation of overall transplant volume and lung utilization rate, both directly and indirectly. Direct growth can be quantified easily by conversion rate of donor lungs that do not meet conventional center criteria for acceptance, but undergo EVLP, and are subsequently accepted as referenced previously. Indirect growth may also result because access to EVLP can alter patterns of donor offer acceptance and willingness to travel to evaluate donor lungs in person given access to EVLP as a back-up modality for suboptimal quality. Even when EVLP is not actually utilized for a case, there is likely behavior change and more aggressive selection of donor lungs because of its availability. Multiple centers throughout the world have reported significant increases in utilization of donor organs after integration of EVLP, up 70% after a decade of experience [41–43, 46, 47]. More aggressive lung donor utilization, in many cases, may translate to decreased waitlist times, though this may be difficult to demonstrate until there is more universal adoption of EVLP [48]. The ability of EVLP to increase the pool of donor lungs remains particularly important at the extremes of the spectrum for recipients, those with low waitlist urgency and those with high waitlist urgency.
In addition to its utility in cases of suboptimal lung allograft quality, EVLP allows for the gift of flexibility during a rather strict timeline. As highlighted previously, organizational constraints imposed by multiple factors can lead to viable organs being declined. The additional time afforded by EVLP can be helpful in a situation where procurement occurs in the absence of a comprehensive evaluation. For example, when bronchoscopy or computed tomography (CT) imaging are not possible prior to acceptance of the DCD donor lungs, this which could lead to discomfort accepting the lungs for direct transplantation without ELVP evaluation [49]. One notable example includes the use of EVLP for to permit adequate time for histologic evaluation of extra-pulmonary malignancy [50].
As stated previously, “dry runs” or last-minute donor lung declines can occur even in the operating room. The availability of EVLP allows other lung transplant programs the opportunity to independently evaluate the lungs for their recipients using their own acceptance criteria [36]. Additionally, broader sharing of organs over larger geographic areas and extended travel times are becoming more common, with some programs extending travel distance to up to 5000 nautical miles [51]. Likewise, sometimes there are recipient issues that can lead to extended ischemic times, such as time to arrival to transplant hospital, clinical instability, need for prospective crossmatch, or technically difficult removal of native lungs. One example, the Foch Hospital (Suresnes, Franc) successfully utilized EVLP to offer three hyperimmunized candidates transplantation after providing adequate time for a prospective crossmatch to be completed [52]. Lastly, operating room or surgical team availability may be limited in some situations where there are multiple competing procedures occurring concurrently. Ultimately, extended warm perfusion has been performed using multiple EVLP systems, and pre-clinical data suggest that EVLP may allow for a ‘resetting’ of adverse physiologic changes that may occur during cold ischemic time, buying time to overcome potential issues as described above [34].
Utilization of EVLP in the United States
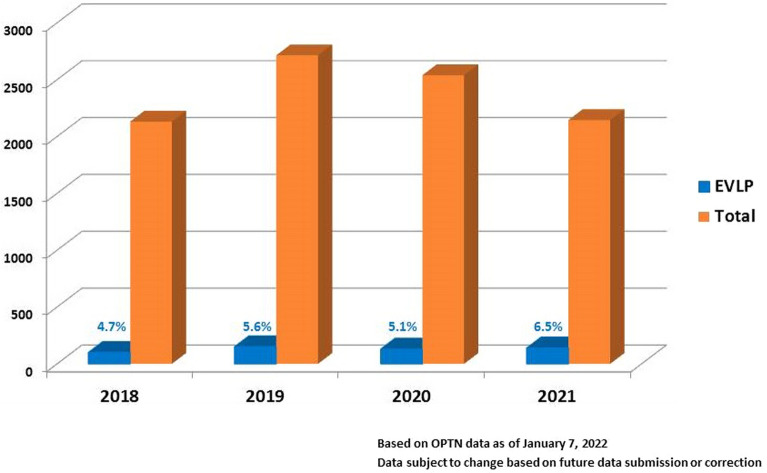
With increasing availability and familiarity with the use of EVLP for lung transplant, utilization has increased some over the past few years in the United States (Fig. 5). Recent inquiry of data from the United Network for Organ Sharing/Organ Procurement and Transplant Network shows the number of organs utilizing EVLP range between 4.7 and 6.5% [53]. As more centers gain access to EVLP effectively increasing the lung donor pool, we can anticipate a rise in lung utilization rate which may be accelerated by standardization of protocols and service development [54].
Fig. 5.
Deceased donor lung transplants performed in the US from 03/2018 to 10/2021 stratified by use of EVLP prior to transplant
Future Utility of EVLP
Much of the current utility of EVLP has been focused on short-term outcomes such as PGD and 30-days post-transplant mortality. Data from individual institutional retrospective studies and post hoc analyses of clinical trials provide evidence of equivalent 12-month allograft and patient survival of after EVLP versus conventional transplantation [13]. However, the utility of EVLP can extend beyond organ evaluation and extension of ischemic time to incorporate more advanced diagnostic and therapeutic modalities.
Allograft Assessment
An area of great growth and potential within EVLP is the capacity for comprehensive, multi-dimensional organ monitoring. Gross inspection, such as by weight, can be predictive of suitability [55]. Additionally, sampling by bronchoscopy may play a potential role in future diagnostic testing, even on a molecular level [27]. Beyond conventional chest radiography, broader imaging modalities such as magnetic resonance imaging and ultrasound techniques are being investigated [56, 57]. Perfusate sample assessment in pre-clinical models has identified extracellular biomarker presence and pro-inflammatory gene expression. Certain monitoring modalities, once validated, could help assess organ response to ischemia, quantify inflammation, and help predict future reperfusion injury and/or alloimmune response [58]. However, feasibility of these types of assessment in the clinical setting still requires further study. As a clearer understanding of normal allograft response to EVLP emerges, so too will the potential for interventions to optimize lung allograft function [59, 60].
Antimicrobial Treatment
Donor transmission of infection through transplantation is an inherent risk. Prolonged mechanical ventilation, terminal extubation with DCD, and reduced or absent airway reflexes (to include cough clearance) increase the risk of infection of the donor organ. Infection may result in direct cellular injury and reduced gas exchange, as well as propagation of infection and transmission to recipient during the transplant process [61, 62]. Activation of the recipient immune system by harbored organisms can also lead to reduced immune tolerance [63]. Prior to transplant, donor management involves a risk/benefit ratio for any donor intervention to maximize multi-organ donation potential. Antibiotics can have deleterious side effects, such as aminoglycosides with significant risk of precipitating acute kidney injury. Inversely, localized infection or systemic sepsis can adversely affect donor lung quality [64]. EVLP allows for targeted treatment of donor lungs in isolation, including removal from a toxic milieu of endotoxins. Additionally, it can allow for supra-therapeutic drug levels without associated toxicity to other donor or recipient organs [65, 66]. For example, administration of vancomycin is considered therapeutic if a pre-dose serum level of 10 mg/l can be maintained, however peak levels above 30 mg/l increase the risk of nephrotoxicity. Administered during EVLP, a single dose of 15 mg/kg of donor body weight could consistently maintain a perfusate concentration of 300–400 mg/l for up to 12 h, a level significantly higher than the threshold for renal toxicity and allowing maximal efficacy of the time-dependent bactericidal effect of this medication. Broad-spectrum coverage with antibacterial agents during EVLP can reduce bacterial load, endotoxin, and alter pro-inflammatory markers with a significant improvement in gas exchange and pulmonary mechanics. Interestingly, inhaled nitric oxide has been shown to have antimicrobial effects, and has been safely used in a pre-clinical model of EVLP for a continuous 12 h at 200 parts per million without associated risk of side effects such as systemic hypotension and methemoglobinemia [67]. Apart from direct transmission of respiratory infection, blood-borne pathogens also pose a threat to recipients. Viral load reduction of hepatitis C with ultraviolet light application during EVLP, specifically with wavelengths of 200–280 manometers (ultraviolet-C) appears to be useful for disinfection and could serve as a method to reduce donor transmission of hepatitis C [68]. Similar reduction of other viruses to reduce transmission such as hepatitis B and human immunodeficiency virus may also prove feasible and effective, thus leading to increased donor lung utilization.
Optimization of Allograft Function
Ultimately, long-term allograft function and recipient survival is the goal of a successful lung transplant. EVLP promises to be an effective platform for directed therapies for immunomodulation as well. Therapies such as anti-inflammatory alpha 1-antitrypsin administration or allograft B-cell depleting rituximab are investigational at present but may eventually be adopted into broader use [69, 70].
Acute and chronic rejection stem from recipient immune system recognition of a foreign organ and are mitigated using systemic immunosuppression [71]. The pro-inflammatory state immediately after transplant can be associated with long-term rejection [72]. Multi-drug regimens for immunosuppression, however, increase risk of infection and secondary effects can lead to other end organ damage. Though limited, pre-clinical models of isolated treatment during EVLP with cyclosporine and methylprednisolone have shown benefit on physiologic parameters and gas exchange during early graft function [73, 74]. Longer-term data remain to be seen. Vector therapy using modified adenovirus/lentivirus could be utilized to deliver gene therapy directly to the organ to reduce pro-inflammatory signaling without exposing other recipient organ systems [75, 76]. Other targeted immunomodulation, RNA based therapies, have been utilized and can selectively be administered during EVLP [77]. Immunomodulation of the donor lungs during EVLP could reduce recognition and sensitization of the recipient immune system and/or increase tolerance markers resulting in less acute and chronic rejection potentially with lower levels of long-term immunosuppression.
Conclusions
Although use of ex vivo lung perfusion remains in its early phase, multiple studies have demonstrated its feasibility and utility. Increasing use of commercially available and investigational EVLP systems demonstrates the potential of EVLP to further revolutionize lung transplantation. With the passage of time and ongoing investigation, additional advances and potential benefits of EVLP are assured. In the short term, EVLP represents a viable pathway to increase the lung donor pool and potentially reduce transplant waitlist time and mortality. However, this technology holds promise to modulate long-term post-lung transplant outcomes as well. The optimal EVLP system(s) for a particular transplant center depends on individual center practices and resources, thus the availability of distinct EVLP models is critical. Expanded capacity for diagnostic testing to guide lung allograft acceptance and transplantation holds great promise, but perhaps most exciting for the future of EVLP is the emergence of therapeutic options for infection control and immunomodulation. With continued evolution and expanded utility, ex vivo lung perfusion may provide the major leap needed to improve and extend allograft function in lung transplantation. 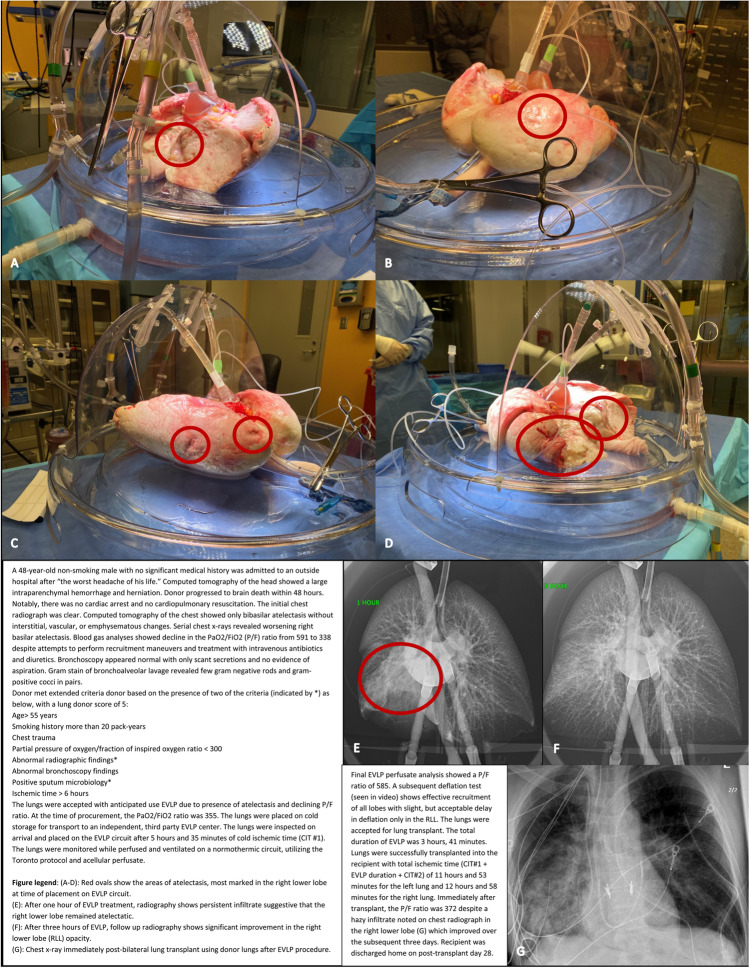
“Deflation” Test. (MP4 35929 KB)
Acknowledgements
Funding
This work was supported in part by Health Resources and Services Administration contract HHSH250-2019-00001C. The content is the responsibility of the authors alone and does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. government. No Rapid Service Fee was received by the journal for the publication of this article.
Medical Writing/Editorial Assistance
No individual or private service was hired in the medical writing or editorial assessment. During the peer-review process, United Therapeutics was offered an opportunity to comment on the article. Changes resulting from comments received were made by the authors based on their scientific and editorial merit. Lung Bioengineering did provide the digital media for the case study.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors participated in the conception, drafting, editing, and submission of this manuscript and associated supplementary material.
Disclosure
A. Whitney Brown received an honorarium from Lung Bioengineering in 2021 for participating in an educational video on ex vivo lung perfusion. Kareem Ahmad received an honorarium from Triangle Insights in 2021 for participating in an interview on experience with the use of ex vivo lung perfusion with Lung Bioengineering. Jennifer Pluhacek has nothing to disclose.
Compliance with Ethics Guidelines
The lung transplant recipient involved in the case study provided consent for the details of his clinical course to be disclosed in this manuscript.
References
- 1.Smith S, Trivedi JR, Fox M, Van Berkel VH. Donor lung utilization for transplantation in the United States. J Heart Lung Transplant. 2020;39(4, Supplement):S374. doi: 10.1016/j.healun.2020.01.471. [DOI] [Google Scholar]
- 2.Reeb J, Keshavjee S, Cypel M. Expanding the lung donor pool: advancements and emerging pathways. Curr Opin Organ Transplant. 2015;20(5):498–505. doi: 10.1097/MOT.0000000000000233. [DOI] [PubMed] [Google Scholar]
- 3.Canadian Institute for Health Information. Annual statistics on organ replacement in Canada: dialysis, transplantation and donation, 2008 to 2017. Canada. 2018.
- 4.Van Raemdonck D, Neyrinck A, Verleden GM, et al. Lung donor selection and management. Proc Am Thorac Soc. 2009;6(1):28–38. doi: 10.1513/pats.200808-098GO. [DOI] [PubMed] [Google Scholar]
- 5.Steen S, Liao Q, Wierup RPN, et al. Sjöberg Transplantation of lungs from non-heart-beating donors after functional assessment ex vivo. Ann Thorac Surg. 2003;76:244–252. doi: 10.1016/S0003-4975(03)00191-7. [DOI] [PubMed] [Google Scholar]
- 6.Nakajima D, Date H. Ex vivo lung perfusion in lung transplantation. Gen Thorac Cardiovasc Surg. 2021;69(4):625–630. doi: 10.1007/s11748-021-01609-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schmack B, Weymann A, Mohite P, et al. Contemporary review of the organ care system in lung transplantation: potential advantages of a portable ex-vivo lung perfusion system. Expert Rev Med Devices. 2016;13(11):1035–1041. doi: 10.1080/17434440.2016.1243464. [DOI] [PubMed] [Google Scholar]
- 8.Schraufnagel DP, Steffen RJ, Vargo PR, et al. Devices for ex vivo heart and lung perfusion. Expert Rev Med Devices. 2018;15(3):183–191. doi: 10.1080/17434440.2018.1430568. [DOI] [PubMed] [Google Scholar]
- 9.Warnecke G, Moradiellos J, Tudorache I, et al. Normothermic perfusion of donor lungs for preservation and assessment with the organ care system lung before bilateral transplantation: a pilot study of 12 patients. Lancet. 2012;380:1851–1858. doi: 10.1016/S0140-6736(12)61344-0. [DOI] [PubMed] [Google Scholar]
- 10.Zhang ZL, van Suylen V, van Zanden JE, et al. First experience with ex vivo lung perfusion for initially discarded donor lungs in the Netherlands: a single-centre study. Eur J Cardiothorac Surg. 2018 doi: 10.1093/ejcts/ezy373. [DOI] [PubMed] [Google Scholar]
- 11.Cypel M, Yeung JC, Machuca T, et al. Experience with the first 50 ex vivo lung perfusions in clinical transplantation. J Thorac Cardiovasc Surg. 2012;144(5):1200–1206. doi: 10.1016/j.jtcvs.2012.08.009. [DOI] [PubMed] [Google Scholar]
- 12.Van Raemdonck D, Neyrinck A, Cypel M, et al. Ex vivo lung perfusion. Transplant Int. 2015;28:643–656. doi: 10.1111/tri.12317. [DOI] [PubMed] [Google Scholar]
- 13.Luo Q, Zhu L, Wang Y, et al. The conversional efficacy of ex vivo lung perfusion and clinical outcomes in patients undergoing transplantation of donor lungs by ex vivo lung perfusion: a meta-analysis. Ann Transplant. 2019;27(24):647–660. doi: 10.12659/AOT.919242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jirsch DW, Fisk RL, Couves CM. Ex vivo evaluation of stored lungs. Ann Thorac Surg. 1970;10(2):163–168. doi: 10.1016/S0003-4975(10)65582-8. [DOI] [PubMed] [Google Scholar]
- 15.Nelson K, Bobba C, Ghadiali S, et al. Animal models of ex vivo lung perfusion as a platform for transplantation research. World J Exp Med. 2014;4(2):7–15. doi: 10.5493/wjem.v4.i2.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kalka K, Keldenich Z, Carstens H, et al. Porcine slaughterhouse lungs for ex vivo lung perfusion—a pilot project. Am J Transl Res. 2020;12(10):6455–6463. [PMC free article] [PubMed] [Google Scholar]
- 17.Roman MA, Nair S, Tsui S, et al. Ex vivo lung perfusion: a comprehensive review of the development and exploration of future trends. Transplantation. 2013;96(6):509–518. doi: 10.1097/TP.0b013e318295eeb7. [DOI] [PubMed] [Google Scholar]
- 18.Steen S, Sjöberg T, Pierre L, et al. Transplantation of lungs from a non-heart-beating donor. Lancet. 2001;357(9259):825–829. doi: 10.1016/S0140-6736(00)04195-7. [DOI] [PubMed] [Google Scholar]
- 19.Wierup P, Haraldsson A, Nilsson F, et al. Ex vivo evaluation of nonacceptable donor lungs. Ann Thorac Surg. 2006;81(2):460–466. doi: 10.1016/j.athoracsur.2005.08.015. [DOI] [PubMed] [Google Scholar]
- 20.Steen S, Ingemansson R, Eriksson L, et al. First human transplantation of a nonacceptable donor lung after reconditioning ex vivo. Ann Thorac Surg. 2007;83(6):2191–2194. doi: 10.1016/j.athoracsur.2007.01.033. [DOI] [PubMed] [Google Scholar]
- 21.Cypel M, Yeung JC, Hirayama S, et al. Technique for prolonged normothermic ex vivo lung perfusion. J Heart Lung Transplant. 2008;27(12):1319–1325. doi: 10.1016/j.healun.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 22.Cypel M, Yeung JC, Liu M, et al. Normothermic ex vivo lung perfusion in clinical lung transplantation. N Engl J Med. 2011;364(15):1431–1440. doi: 10.1056/NEJMoa1014597. [DOI] [PubMed] [Google Scholar]
- 23.Possoz J, Neyrinck A, Van Raemdonck D. Ex vivo lung perfusion prior to transplantation: an overview of current clinical practice worldwide. J Thorac Dis. 2019;11(4):1635–1650. doi: 10.21037/jtd.2019.04.33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Briot R, Gennai S, Maignan M, et al. Ex vivo lung graft perfusion. Anaesth Crit Care Pain Med. 2016;35(2):123–131. doi: 10.1016/j.accpm.2015.09.006. [DOI] [PubMed] [Google Scholar]
- 25.Warnecke G, Van Raemdonck D, Smith MA, et al. Normothermic ex-vivo preservation with the portable Organ Care System Lung device for bilateral lung transplantation (INSPIRE): a randomised, open-label, non-inferiority, phase 3 study. Lancet Respir Med. 2018;6(5):357–367. doi: 10.1016/S2213-2600(18)30136-X. [DOI] [PubMed] [Google Scholar]
- 26.Loor G, Warnecke G, Villavicencio MA, Smith MA, et al. Portable normothermic ex-vivo lung perfusion, ventilation, and functional assessment with the Organ Care System on donor lung use for transplantation from extended-criteria donors (EXPAND): a single-arm, pivotal trial. Lancet Respir Med. 2019;7(11):975–984. doi: 10.1016/S2213-2600(19)30200-0. [DOI] [PubMed] [Google Scholar]
- 27.Hsin M, Au T. Ex vivo lung perfusion: a potential platform for molecular diagnosis and ex vivo organ repair. J Thorac Dis. 2018;10(Suppl 16):S1871–S1883. doi: 10.21037/jtd.2018.04.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Aigner C, Klepetko W. Bilateral lung transplantation. Oper Tech Thorac Card Surg. 2012;17:181–193. doi: 10.1053/j.optechstcvs.2012.09.001. [DOI] [Google Scholar]
- 29.Chaney J, Suzuki Y, Cantu E, 3rd, van Berkel V. Lung donor selection criteria. J Thorac Dis. 2014;6(8):1032–1038. doi: 10.3978/j.issn.2072-1439.2014.03.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smits JM, van der Bij W, Van Raemdonck D, et al. Defining an extended criteria donor lung: an empirical approach based on the Eurotransplant experience. Transpl Int. 2011;24:393–400. doi: 10.1111/j.1432-2277.2010.01207.x. [DOI] [PubMed] [Google Scholar]
- 31.Lardinois D, Banysch M, Korom S, et al. Extended donor lungs: eleven years experience in a consecutive series. Eur J Cardiothorac Surg. 2005;27:762–767. doi: 10.1016/j.ejcts.2005.01.019. [DOI] [PubMed] [Google Scholar]
- 32.Snell GI, Levvey BJ, Levin K, et al. Donation after brain death versus donation after circulatory death: lung donor management issues. Semin Respir Crit Care Med. 2018;39(2):138–147. doi: 10.1055/s-0037-1615820. [DOI] [PubMed] [Google Scholar]
- 33.Martens A, Van Raemdonck DE, Smits J, et al. A retrospective database analysis to evaluate the potential of ex vivo lung perfusion to recruit declined lung donors. Transpl Int. 2017;30(10):1002–1010. doi: 10.1111/tri.12990. [DOI] [PubMed] [Google Scholar]
- 34.Gammie JS, Stukus DR, Pham SM, et al. Effect of ischemic time on survival in clinical lung transplantation. Ann Thorac Surg. 1999;68(6):2015–2019. doi: 10.1016/S0003-4975(99)00903-0. [DOI] [PubMed] [Google Scholar]
- 35.Hsin MKY, Iskander I, Nakajima D, et al. Extension of donor lung preservation with hypothermic storage after normothermic ex vivo lung perfusion. J Heart Lung Transplant. 2016;35:130–136. doi: 10.1016/j.healun.2015.05.017. [DOI] [PubMed] [Google Scholar]
- 36.Okahara S, Levvey B, McDonald M, D'Costa R, Opdam H, Pilcher DV, Snell GI. A retrospective review of declined lung donors: estimating the potential of ex vivo lung perfusion. Ann Thorac Surg. 2021;112(2):443–449. doi: 10.1016/j.athoracsur.2020.08.042. [DOI] [PubMed] [Google Scholar]
- 37.XVIVO Perfusion AB. XVIVO Perfusion System (XPSTM) with STEEN SolutionTM Professional Labeling. Göteborg, Sweden. 2019. https://www.accessdata.fda.gov/cdrh_docs/pdf18/P180014d.pdf
- 38.TransMedics, Inc. TransMedics® Organ Care System™ Clinical User Guide: OCS™ Lung System. Andover, MA. 2019. https://www.accessdata.fda.gov/cdrh_docs/pdf16/P160013S002C.pdf
- 39.Sage AT, Richard-Greenblatt M, Zhong K, et al. Prediction of donor related lung injury in clinical lung transplantation using a validated ex vivo lung perfusion inflammation score. J Heart Lung Transplant. 2021;40(7):687–695. doi: 10.1016/j.healun.2021.03.002. [DOI] [PubMed] [Google Scholar]
- 40.Senior M. Beating the organ clock. Nat Biotechnol. 2018;36:488–492. doi: 10.1038/nbt.4157. [DOI] [PubMed] [Google Scholar]
- 41.Murala JS, Whited WM, Banga A, et al. Ex vivo lung perfusion: how we do it. Indian J Thorac Cardiovasc Surg. 2021;1:1–12. doi: 10.1007/s12055-021-01215-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cypel M, Yeung JC, Donahoe L, et al. Normothermic ex vivo lung perfusion: Does the indication impact organ utilization and patient outcomes after transplantation? J Thorac Cardiovasc Surg. 2019;S0022–5223(19):31732–31735. doi: 10.1016/j.jtcvs.2019.06.123. [DOI] [PubMed] [Google Scholar]
- 43.McMeekin N, Chrysos AE, Vale L, et al. Incorporating ex-vivo lung perfusion into the UK adult lung transplant service: an economic evaluation and decision analytic model. BMC Health Serv Res. 2019;19:326. doi: 10.1186/s12913-019-4154-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hopkins PM, Chamber D, Smith I, et al. Cost effectiveness of ex vivo lung perfusion warrants analysis of long-term recipient outcome and donor organ utilization rate. JHLT. 2015;4:S174. [Google Scholar]
- 45.Fisher A, Andreasson A, Chrysos A, et al. An observational study of donor ex vivo lung perfusion in UK lung transplantation: DEVELOP-UK. Health Technol Assess. 2016;20(85):1–276. doi: 10.3310/hta20850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nilsson T, Wallinder A, Henriksen I, et al. Lung transplantation after ex vivo lung perfusion in two Scandinavian centres. Eur J Cardiothorac Surg. 2019;55(4):766–772. doi: 10.1093/ejcts/ezy354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Valenza F, Rosso L, Coppola S, et al. Ex vivo lung perfusion to improve donor lung function and increase the number of organs available for transplantation. Transpl Int. 2014;27(6):553–561. doi: 10.1111/tri.12295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wey A, Valapour M, Skeans MA, et al. Heart and lung organ offer acceptance practices of transplant programs are associated with waitlist mortality and organ yield. Am J Transplant. 2018;18(8):2061–2067. doi: 10.1111/ajt.14885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chancellor WZ, Charles EJ, Mehaffey JH, et al. Expanding the donor lung pool: how many donations after circulatory death organs are we missing? J Surg Res. 2018;223:58–63. doi: 10.1016/j.jss.2017.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Palleschi AI, Rosso L, Ruggeri G, et al. Overcoming the limits of reconditioning: seventeen hours of EVLP with successful transplantation from uncontrolled circulatory death donor. Transplantation. 2021;105(12):2620–2624. doi: 10.1097/TP.0000000000003646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fitch ZW, Doberne J, Reynolds JM, et al. Expanding donor availability in lung transplantation: a case report of 5000 miles traveled. Am J Transplant. 2021;21(6):2269–2272. doi: 10.1111/ajt.16556. [DOI] [PubMed] [Google Scholar]
- 52.De Wolf J, Puyo P, Bonnette P, et al. Logistic ex vivo lung perfusion for hyperimmunized patients. Ann Thorac Surg. 2016;102(3):e205–e206. doi: 10.1016/j.athoracsur.2016.01.081. [DOI] [PubMed] [Google Scholar]
- 53.Based on Organ Procurement and Transplantation Network data as of 1/7/2022. OPTN.transplant.hrsa.gov/datarequest
- 54.Gilmour J, Griffiths C, Pither T, et al. Normothermic machine perfusion of donor-lungs ex-vivo: promoting clinical adoption. Curr Opin Organ Transplant. 2020;25(3):285–292. doi: 10.1097/MOT.0000000000000765. [DOI] [PubMed] [Google Scholar]
- 55.Okamoto T, Niikawa H, Wheeler D, et al. Significance of lung weight in cellular ex vivo lung perfusion. J Surg Res. 2021;260:190–199. doi: 10.1016/j.jss.2020.11.069. [DOI] [PubMed] [Google Scholar]
- 56.Renne J, Gutberlet M, Voskrebenzev A, et al. Multiparametric MRI for organ quality assessment in a porcine Ex-vivo lung perfusion system. PLoS ONE. 2018;13(12):e0209103. doi: 10.1371/journal.pone.0209103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ayyat KS, Okamoto T, Niikawa H, et al. A CLUE for better assessment of donor lungs: novel technique in clinical ex vivo lung perfusion. J Heart Lung Transplant. 2020; S1053–2498(20)31665-X [DOI] [PubMed]
- 58.Iske J, Hinze CA, Salman J, et al. The potential of ex vivo lung perfusion on improving organ quality and ameliorating ischemia reperfusion injury. Am J Transplant. 2021;21(12):3831–3839. doi: 10.1111/ajt.16784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Caldarone L, Mariscal A, Sage A, et al. Neutrophil extracellular traps in ex vivo lung perfusion perfusate predict the clinical outcome of lung transplant recipients. Eur Respir J. 2019;53(4):1801736. doi: 10.1183/13993003.01736-2018. [DOI] [PubMed] [Google Scholar]
- 60.Kanou T, Nakahira K, Choi AM, et al. Cell-free DNA in human ex vivo lung perfusate as a potential biomarker to predict the risk of primary graft dysfunction in lung transplantation. J Thorac Cardiovasc Surg. 2020;S0022–5223(20):32354. doi: 10.1016/j.jtcvs.2020.08.008. [DOI] [PubMed] [Google Scholar]
- 61.Bunsow E, Los-Arcos I, Martin-Gómez MT, Bello I, et al. Donor-derived bacterial infections in lung transplant recipients in the era of multidrug resistance. J Infect. 2020;80(2):190–196. doi: 10.1016/j.jinf.2019.12.006. [DOI] [PubMed] [Google Scholar]
- 62.Snell G, Hiho S, Levvey B, et al. Consequences of donor-derived passengers (pathogens, cells, biological molecules and proteins) on clinical outcomes. J Heart Lung Transplant. 2019;38(9):902–906. doi: 10.1016/j.healun.2019.06.019. [DOI] [PubMed] [Google Scholar]
- 63.Tanaka S, Gauthier JM, et al. Bacterial products in donor airways prevent the induction of lung transplant tolerance. Am J Transplant. 2021;21(1):353–361. doi: 10.1111/ajt.16256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mehaffey JH, Charles EJ, Sharma AK, et al. Ex vivo lung perfusion rehabilitates sepsis-induced lung injury. Ann Thorac Surg. 2017;103(6):1723–1729. doi: 10.1016/j.athoracsur.2017.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Nakajima D, Cypel M, Bonato R, et al. Ex vivo perfusion treatment of infection in human donor lungs. Am J Transplant. 2016;16(4):1229–1237. doi: 10.1111/ajt.13562. [DOI] [PubMed] [Google Scholar]
- 66.Zinne N, Krueger M, Hoeltig D, et al. Treatment of infected lungs by ex vivo perfusion with high dose antibiotics and autotransplantation: a pilot study in pigs. PLoS ONE. 2018;13(3):e0193168. doi: 10.1371/journal.pone.0193168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Michaelsen VS, et al. Safety of continuous 12-hour delivery of antimicrobial doses of inhaled nitric oxide during ex vivo lung perfusion. J Thorac Cardiovasc Surg. 2020 doi: 10.1016/j.jtcvs.2020.11.150. [DOI] [PubMed] [Google Scholar]
- 68.Galasso M, Feld JJ, Watanabe Y, et al. Inactivating hepatitis C virus in donor lungs using light therapies during normothermic ex vivo lung perfusion. Nat Commun. 2019;10(1):481. doi: 10.1038/s41467-018-08261-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lin H, Chen M, Tian F, Tikkanen J, et al. α1-Anti-trypsin improves function of porcine donor lungs during ex-vivo lung perfusion. J Heart Lung Transplant. 2018;37(5):656–666. doi: 10.1016/j.healun.2017.09.019. [DOI] [PubMed] [Google Scholar]
- 70.Ku TJY, et al. Ex-vivo delivery of monoclonal antibody (Rituximab) to treat human donor lungs prior to transplantation. EBioMedicine. 2020;60:102994. doi: 10.1016/j.ebiom.2020.102994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ivulich S, Westall G, Dooley M, Snell G. The evolution of lung transplant immunosuppression. Drugs. 2018;78(10):965–982. doi: 10.1007/s40265-018-0930-6. [DOI] [PubMed] [Google Scholar]
- 72.Hall DJ, Baz M, Daniels MJ, et al. Immediate postoperative inflammatory response predicts long-term outcome in lung-transplant recipients. Interact Cardiovasc Thorac Surg. 2012;15(4):603–607. doi: 10.1093/icvts/ivs330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Haam S, Noda K, Philips BJ, et al. Cyclosporin A administration during ex vivo lung perfusion preserves lung grafts in rat transplant model. Transplantation. 2020;104(9):e252–e259. doi: 10.1097/TP.0000000000003237. [DOI] [PubMed] [Google Scholar]
- 74.van Zanden JE, Leuvenink HGD, Verschuuren EAM, et al. Ex vivo perfusion with methylprednisolone attenuates brain death-induced lung injury in rats. Transplant Direct. 2021;7(4):e682. doi: 10.1097/TXD.0000000000001141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yeung JC, Wagnetz D, Cypel M, et al. Ex vivo adenoviral vector gene delivery results in decreased vector-associated inflammation pre- and post-lung transplantation in the pig. Mol Ther. 2012;20(6):1204–1211. doi: 10.1038/mt.2012.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Figueiredo C, Carvalho Oliveira M, Chen-Wacker C, et al. Immunoengineering of the vascular endothelium to silence MHC expression during normothermic ex vivo lung perfusion. Hum Gene Ther. 2019;30(4):485–496. doi: 10.1089/hum.2018.117. [DOI] [PubMed] [Google Scholar]
- 77.Brüggenwirth IMA, Martins PN. RNA interference therapeutics in organ transplantation: the dawn of a new era. Am J Transplant. 2020;20(4):931–941. doi: 10.1111/ajt.15689. [DOI] [PubMed] [Google Scholar]