Abstract
Objective
In the COVID-19 pandemic, the SARS-CoV-2 virus has infected millions of people worldwide. Mortality primarily results from the inflammation state and its complications. High-dose melatonin has been established as an anti-inflammatory agent. This study evaluated high-dose melatonin as an adjuvant therapy in critically ill patients with SARS-CoV-2 infection.
Methods
We conducted a double-blinded, randomized clinical trial of 21 mg of melatonin per day compared with a placebo in 67 patients with COVID-19. We enrolled patients older than 18 years of age with documented SARS-CoV-2 infection, who were admitted to the intensive care unit and underwent invasive mechanical ventilation. Administration of melatonin and placebo through a nasogastric tube continued for 5 days. The main outcomes were mortality rate, duration of mechanical ventilation, changes in oxygenation indices, and C-reactive protein (CRP) levels.
Results
No significant differences were observed in mortality and duration of mechanical ventilation between the control and intervention groups. After 5 days of the intervention, the mean (±standard deviation) CRP and platelet count were 47.28 (±38.86) mg/L and 195.73 (±87.13) × 1000/μL, respectively, in the intervention group and 75.52 (±48.02) mg/L and 149.62 (±68.03) × 1000/μL, respectively, in the control group (P < 0.05).
Conclusion
High-dose melatonin in intubated patients with COVID-19 was associated with a decrease in CRP levels. However, this treatment did not apparently affect patient outcomes.
Keywords: Adjuvant therapy, COVID-19, Intubated, Melatonin, Mortality
الملخص
أهداف البحث
أصابت جائحة كوفيد-19 الملايين من الناس في جميع أنحاء العالم. ترجع الوفيات أساسا لحالة الالتهاب ومضاعفاته. من المعروف أن جرعة عالية من الميلاتونين تعتبر عاملا مضادا للالتهابات. قيمت هذه الدراسة جرعة عالية من الميلاتونين كعلاج مساعد في الحالات الحرجة للمرضى المصابين بعدوى كوفيد-19.
طرق البحث
أجرينا تجربة سريرية عشوائية مزدوجة التعمية لجرعة 21 ملغ من الميلاتونين في اليوم مقارنة مع دواء وهمي بين 67 مريضا كوفيد-19. تم التسجيل للمرضى الأكبر من 18 عاما والمصابين بعدوى كوفيد-19 الموثقة والذين تم إدخالهم إلى وحدة العناية المركزة وخضعوا لتهوية ميكانيكية. استمر إعطاء الميلاتونين والعلاج الوهمي لمدة خمسة أيام من خلال أنبوب أنفي معدي. كانت النتائج الرئيسية معدل الوفيات، ومدة التهوية الميكانيكية، والتغيرات في مؤشرات الأوكسجين، ومستويات البروتين المتفاعل سي.
النتائج
لم يكن هناك فرق جوهري في الوفيات ومدة التهوية الميكانيكية بين مجموعات التحكم والتدخل. بعد 5 أيام من التدخل، المتوسط (± الانحراف المعياري) لـلبروتين المتفاعل سي و عدد الصفائح الدموية كان 47.28 (± 38.86) ملغم / لتر و 195.73 (± 87.13) × 1000 / ميكرولتر في مجموعة التدخل و 75.52 (± 48.02) ملغم / لتر و 149.62 (± 68.03) × 1000 / ميكرولتر في مجموعة التحكم على التوالي.
الاستنتاجات
ارتبط تناول جرعات عالية من الميلاتونين في مرضى كوفيد-19 بالتناقص فى مستويات البروتين المتفاعل سي. ومع ذلك، فإن تأثيره على نتائج المرضى لم يكن ملحوظا.
الكلمات المفتاحية: كوفيد-19, الميلاتونين, تنبيب, معدل الوفيات, العلاج المساعد
Introduction
The SARS-CoV-2 virus, which causes COVID-19, has led to more than 5.7 million deaths and 370 million infections globally.1 This infection presents differently among cases, and may range from asymptomatic, flu-like symptoms in most patients to severe conditions or death.2,3 The pathogenesis of the infection is not fully known; however, most scientists believe that cytokine storms and severe inflammatory responses are associated with organ damage and patient death. In the past 3 years, several clinical trials have been conducted to decrease severe inflammation and its subsequent complications in patients with COVID-19.4 Scientists have recommended several immunomodulatory agents, such as corticosteroids, anti-interleukins, and granulocyte macrophage colony stimulating factor inhibitors. Although these agents are lifesaving, they sometimes result in adverse reactions such as flare-up of latent infections (e.g., tuberculosis, hepatitis B, or strongyloidiasis), or fungal and bacterial superinfections.5, 6, 7, 8
Melatonin is a potent free radical scavenger. This hormone up-regulates anti-oxidative enzymes (e.g., glutathione peroxidase or superoxide dismutase) and down-regulates pro-oxidative enzymes. Melatonin decreases the expression of inflammatory cytokines, such as interleukins 1, 6 and 8 and tumor necrosis factor-alpha (TNF-α), and increases the levels of the anti-inflammatory cytokine interleukin 109. No reports have documented fungal and bacterial superinfection or reactivation of latent infection after melatonin use. El Frargy and colleagues have reported that the administration of melatonin as adjuvant therapy in septic newborns is associated with improved clinical outcomes.10 Melatonin might be beneficial for prophylaxis or treatment of patients with COVID-19.11 Although melatonin does not have direct antiviral activity, animal studies have shown that it decreases viremia, viral load, and mortality rates in rats infected with influenza virus.12 However, melatonin has a synergic effect with some antiviral drugs, such as ribavirin, in animal models of influenza. Moreover, it decreases renal damage due to the oxidative stress caused by lopinavir/ritonavir combination treatment.13
Research in 2015, during the Ebola outbreak, has suggested that melatonin decreases Ebola symptoms and increases patient survival.9 Although mechanical ventilation is lifesaving in patients with respiratory failure, this modality is associated with increased oxidant generation and pulmonary injury.12 Melatonin has several protective effects against ventilator-associated injury14; therefore, its administration in intubated patients with COVID-19 might be beneficial. Therefore, the current study aimed to evaluate the effects of melatonin on critically ill patients with COVID-19 who underwent invasive mechanical ventilation. To our knowledge, this is the first trial of high-dose oral melatonin in severe COVID-19 cases.
Materials and Methods
Study design
This study was a single-center, double-blinded, randomized controlled trial conducted from June to September 2020 at the Tehran University of Medical Sciences, Iran. The trial was registered with the Iranian registry of clinical trials (IRCT20210225050495N1).
Study population
Patients with COVID-19 who were admitted to the intensive care unit (ICU) and had undergone invasive ventilation were included in a prospective, interventional study. The diagnosis of COVID-19 was confirmed by polymerase chain reaction testing and chest imaging. An age below 18 years, hepatic failure (Child-Pugh class C), and intolerance of nasogastric feeding were all exclusion criteria. The patients' legal guardians were adequately informed regarding the study, and their consent was obtained.
Randomization and treatment
During the first 24 h of intubation, the patients were randomly allocated to one of two treatment arms in a 1:1 ratio through permuted block randomization. A biostatistician oversaw the randomization techniques. The intervention group received 21 mg melatonin daily (i.e., seven crushed tablets of 3 mg melatonin, Razak, Tehran, Iran) through a nasogastric tube for five nights. If patients were extubated before five nights, drug administration was stopped. The matched placebo was given to the control group. The medications were administered in a double-blinded manner, and the placebo tablet had the same size and shape as the melatonin tablet. All patients received the standard care recommended by the national Iranian COVID-19 treatment guidelines: remdesivir (200 mg on the first day and 100 mg daily for 4 days thereafter), corticosteroids, anticoagulant (prophylactic dose), and sometimes tocilizumab. They also received supportive care in the intensive care unit.
Data collection
The following were recorded on the first day of ICU hospitalization: demographic data, Glasgow Coma Scale (GCS) score; Acute Physiology and Chronic Health Evaluation (APACHE) score; hemodynamic parameters such as pulse rate and mean arterial pressure; urine output; and laboratory parameters such as arterial blood gas, blood urea nitrogen, creatinine (Cr), C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), white blood cell (WBC) count, alanine aminotransferase (ALT), aspartate aminotransferase (AST), and alkaline phosphatase.
GCS status, hemodynamic and laboratory parameters, oxygenation indices, and prescribed medicines were recorded daily. CRP was rechecked on the sixth day of the intervention. At the end of the study, the length of ICU stay, duration of mechanical ventilation, extubation rate, mortality, changes in oxygenation indices, and laboratory tests (i.e., WBC, CRP, ALT, AST, and Cr) were evaluated as outcomes. All patients were observed and followed up during their ICU admission.
Statistical analysis
Data were statistically analyzed in IBM SPSS (IBM Corp.2011. IBM SPSS Statistics for Windows, version 20.0. NY, EUA). The Kolmogorov–Smirnov test was used to assess the normal distribution of continuous variables. Normally and non-normally distributed continuous data were expressed as mean and standard deviation and median (interquartile range). Categorical variables are reported as percentages. The chi-squared or Fisher's exact test evaluated probable associations between categorical variables. Parametric and non-parametric continuous variables were analyzed with independent t and Mann–Whitney tests. A P-value less than 0.05 was considered statistically significant. All analyses were performed in statistical software version 22.
Results
Comparison of baseline characteristics
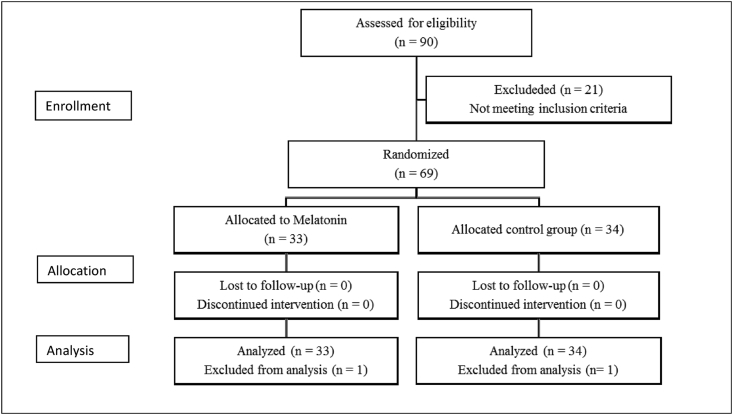
A total of 67 patients who met the inclusion criteria were enrolled in the study. They were randomly divided into two groups. The intervention and control groups comprised 34 and 33 patients, respectively. Overall, 43 patients were men (64%), and 24 were women (36%). In both groups, most patients were men (19 (57.6%) and 24 (70.6%) of the patients in intervention and control groups, respectively). The patients' mean age (±standard deviation) was 65.73 ± 19.47 years and 61.27 ± 18.09 years in the intervention and control groups, respectively. Ten patients were extubated during the study. Seven (27.2%) patients were in the intervention group, and three (9.1%) were in the control group (P = 0.283). All extubated patients survived except for one patient in the intervention group who died from Acinetobacter-associated sepsis (Figure 1). More information regarding the baseline characteristics is presented in Table 1.
Figure 1.
CONSORT flow diagram of the study.
Table 1.
Demographic and clinical characteristics of the study groups on day 1.
| Variables | Melatonin group Day 1 |
Control group Day 1 |
P-value Day 1 |
|---|---|---|---|
| Age (years) | 61.27 ± 18.09 | 65.35 ± 19.30 | 0.376 |
| Sex (male) | 19 (57.6) | 24 (70.6) | 0.316 |
| BMI ([kg/cm]2) | 26.66 + 5.32 | 25.52 + 4.71 | 0.46 |
| WBC (×1000/μL) | 11.41 ± 4.24 | 12.66 ± 4.37 | 0.241 |
| Neutrophil (×1000/μL) | 9630 ± 3810 | 11,010 ± 4170 | 0.199 |
| Lymph (×1000/μL) | 880 ± 530 | 1050 ± 420 | 0.173 |
| Neutrophil/lymph | 14.18 ± 7.10 | 11.91 ± 5.73 | 0.190 |
| Platelet (×1000/μL) | 221.36 ± 123.03 | 208.88 ± 87.94 | |
| Urea (mg/dL) | 70.94 ± 43.99 | 50.12 ± 23.30 | 0.019 |
| Cr (mg/dL) | 1.25 ± 0.54 | 1.14 ± 0.46 | 0.401 |
| ALT (U/L) | 65.03 ± 60.75 | 62.20 ± 67.21 | 0.871 |
| AST (U/L) | 58.21 ± 35.48 | 56.37 ± 50.44 | 0.871 |
| CRP (mg/L) | 62.73 ± 67.04 | 64.55 ± 55.15 | 0.913 |
| ESR (mm/h) | 47.66 ± 27.59 | 55.40 ± 38.80 | 0.507 |
| APACHE score | 19.6 ± 3.35 | 18.9 ± 4.43 | 0.682 |
| GCS | 7.62 ± 3.95 | 7.93 ± 3.19 | 0.721 |
BMI: Body mass index, WBC: white blood cells, Lymph: lymphocytes, Cr: serum creatinine, ALT: alanine aminotransferase, AST: aspartate aminotransferase, CRP: C-reactive protein, ESR: erythrocyte sedimentation rate, APACHE: Acute Physiology and Chronic Health Evaluation, GCS: Glasgow Coma Scale.
Comparison of outcomes between the intervention and placebo groups
On day 1 (Table 1), no significant differences were observed between the melatonin and placebo groups in CBC, CRP, and liver enzymes (Table 1). However, on day 6, significant differences were found between the melatonin and placebo groups in terms of CRP and platelets. The CRP titer in the melatonin and control groups was 47.28 ± 38.86 and 75.52 ± 48.02, respectively (P = 0.042). In addition, the platelet count in the melatonin and control groups significantly differed (195.73 ± 87.13 and 149.62 ± 68.03; P = 0.048). No significant differences were observed between groups in the other variables (Table 2, Table 3).
Table 2.
Demographic and clinical characteristics of the study groups: day 6.
| Variables | Melatonin group Day 6 |
Control group Day 6 |
P-value Day 6 |
|---|---|---|---|
| WBC (×1000/μL) | 12.44 ± 5.17 | 13.68 ± 6.29 | 0.491 |
| Neutrophil (×1000/μL) | 12,840 ± 9640 | 11,980 ± 5670 | 0.770 |
| Lymph (×1000/μL) | 910 ± 410 | 1320 ± 950 | 0.077 |
| Neutrophil/lymph | 15.86 ± 11.70 | 11.97 ± 5.44 | 0.267 |
| Platelet (×1000/μL) | 195.73 ± 87.13 | 149.62 ± 68.03 | 0.048 |
| Urea (mg/dL) | 86.73 ± 68.67 | 105.13 ± 68.27 | 0.337 |
| Cr (mg/dL) | 1.14 ± 0.46 | 1.25 ± 0.54 | 0.401 |
| ALT (U/L) | 44.30 ± 30.33 | 51.88 ± 53.93 | 0.559 |
| AST (U/L) | 96.03 ± 188.76 | 70.10 ± 118.83 | 0.598 |
| CRP (mg/L) | 47.28 ± 38.86 | 75.52 ± 48.02 | 0.042 |
| ESR (mm/h) | 85.57 ± 38.35 | 60.71 ± 29.28 | 0.163 |
WBC: white blood cells, Lymph: lymphocytes, Cr: serum creatinine, ALT: alanine aminotransferase, AST: aspartate aminotransferase, CRP: C-reactive protein, ESR: erythrocyte sedimentation rate.
Table 3.
Comparison of duration of in-hospital mortality, extubation rate, and duration of mechanical ventilation.
| Variable | Melatonin group | Control group | P-value |
|---|---|---|---|
| Extubation rate (patients) | 7 (21.2%) | 3 (9.1%) | 0.283 |
| Duration of mechanical ventilation, time to extubation (days) | 27 (18–35) | 37 (22–45) | 0.091 |
| In-patient mortality (patients) | 28 (84.8%) | 30 (90.9%) | 0.451 |
Numerical values are reported as median (interquartile range), and nominal factors are reported as number (%).
Discussion
Melatonin is a sleep hormone with a broad range of characteristics, such as anti-inflammatory, antioxidant, and antiviral activity. Given the wide range of its effects, melatonin is advised for treating sleep disorders and various medical conditions (e.g., rheumatologic conditions, respiratory illness, renal diseases, and viral infection).15, 16, 17, 18, 19 The COVID-19 pandemic has burdened the health system, and the presence of effective treatments or vaccines is inevitable.19,20
The pathogenesis of COVID-19 poses a dilemma; most experts believe that a heightened immune response against SARS-CoV-2 may be the essential factor responsible for cytokine storms, and the subsequent damage to the lungs and other organs. This severe immune reaction can result in ICU admission and death.21, 22, 23
Clinicians must sometimes use immunomodulatory agents (e.g., corticosteroids, anti-interleukins, and Granulocyte Macrophage Colony Stimulating factor (GCF) inhibitors) to modulate excessive immune responses; however, the risk of adverse effects, such as reactivation and superinfection of pathogens, is not negligible.5,6,8,24 Regarding melatonin's anti-inflammatory effects in decreasing inflammatory cytokines,25,26 the present study was designed to investigate the effects of high dose of melatonin on patient outcomes. We enrolled intubated patients because respiratory apnea may be induced by high doses of melatonin.27 A systematic review (studies from 28 countries) has indicated that the mortality of intubated patients with COVID-19 is 43%, and the mean duration of intubation is 10.12 days.28,29 Our study indicated a lower mortality rate and intubation period in both intervention and control groups (Table 3). The intervention group had fewer deaths and shorter intubation periods (i.e., two cases and 10 days, respectively) than the control group. The lack of a significant difference in this regard might have been due to the small sample size and enrollment of patients in deteriorated condition with low survival probability in our study. Despite the scarcity of research on patients with COVID-19 extubation, evidence has demonstrated that in severe SARS-CoV-2 infection, the risks of respiratory failure, organ damage, and intubation are elevated, and fewer than 50% of intubated COVID-19 cases lead to extubation.29,30 In this study, the extubation rate in the intervention group was twice that of the control group, but this difference was non-significant (Table 3). A high dose of melatonin on the first intubation day decreased inflammation (CRP) and organ failure. Therefore, the patients might have had a high chance of being extubated.
CRP is an acute phase mediator produced in liver tissue; in normal conditions, its serum level is less than 10 mg/dL. Conditions including infection, chronic inflammation, cardiovascular diseases, and necrosis can lead to tissue damage, thus triggering CRP formation, which in turn improves opsonization and phagocytosis, and helps heal these injuries.30 In severe SARS-CoV-2 infection, several inflammatory mediators increase (e.g., interleukins, GCS-F, CRP, ferritin, and TNF-α), thus potentially causing organ failure and death. CRP levels are associated with the severity of COVID-19 infection, even on the first admission day. Therefore, CRP can be used to predict death risk, and decreasing CRP levels indicate improving conditions.30, 31, 32, 33 In a recent study, the difference in CRP levels between groups on day 6 was significant; however, on the first day, it was not (Table 1, Table 2). Administering a high dose of melatonin in the first 5 days of intubation might decrease inflammation and CRP. Therefore, a high dose of melatonin may be an effective adjuvant treatment in critical COVID-19 cases.
The platelet count is an easily accessed test that has been used in different prognostic systems; a decreased platelet count is a parameter in the Sequential Organ Failure Assessment (SOFA) score and Multiple Organ Dysfunction Score (MODS) to predict ICU patient outcomes.34 In addition, in severe SARS-CoV-2 infection, the platelet count decreases. The possible mechanism of thrombocytopenia involves direct invasion of the bone marrow by the virus, destruction of precursor cells in the bone marrow through cytokine storms and immune complexes, platelet consumption due to disseminated intravascular coagulation, and microthrombosis after lung damage.35,36 Subsequently, thrombotic complications and bleeding may result in death.37,38 Our study revealed that on day 6, the final level of CRP in the intervention group was significantly lower than that in the control group.
However, the platelet count was significantly higher than that in the control group (Table 2). This finding might have been due to decreased inflammation after melatonin administration, thereby improving the platelet count. According to the present study, the difference in platelet counts between the intervention and control group (on day 6) was significant. Inflammatory process changes on day 6 (decreased CRP levels and increased platelet counts) occurred in parallel with amelioration of COVID-19.35, 36, 37, 38, 39, 40 Thus, administering high-dose melatonin in critically ill patients with COVID-19 who have undergone invasive mechanical ventilation might decrease the inflammatory response and improve patient outcomes. The small sample size and inaccessibility to parenteral dosage forms of melatonin are limitations of this study. Therefore, further studies with larger sample sizes and intravenous high-dose melatonin are recommended. To our knowledge, this is the first clinical trial administering high-dose melatonin in critically ill patients with COVID-19.
Conclusion
Administration of high-dose melatonin in critically ill patients with COVID-19 who have undergone invasive mechanical ventilation might decrease the inflammatory response.
Source of funding
This study was supported by a grant (grant number: 4710) from the Deputy of Research, Tehran University of Medical Sciences.
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
This trial was approved by the Ethics Committee of Tehran University of Medical Sciences under number IR.TUMS.REC.1399.159, ethical date (2020-04-07).
Authors contributions
NA, YA, HH, NF, FM, ZR, and MA: participated in the acquisition, analysis, or interpretation of data. NA, MD, HH, and SA: designed the study and participated in data analysis. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Acknowledgment
We thank Fatemeh Taghizadeh, Arezoo Khosravani, Somayeh Roshangaran, Somayeh Hassani, and the staff of the ICU at Baharloo Hospital.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91:157. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fauci A.S., Lane H.C., Redfield R.R. Covid-19—navigating the uncharted. Mass Medical Soc. 2020:1268–1269. doi: 10.1056/NEJMe2002387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mahase E., Kmietowicz Z. British Medical Journal Publishing Group; 2020. Covid-19: doctors are told not to perform CPR on patients in cardiac arrest. [DOI] [PubMed] [Google Scholar]
- 4.Li C., He Q., Qian H., Liu J. Overview of the pathogenesis of COVID-19. Exp Ther Med. 2021;22:1–10. doi: 10.3892/etm.2021.10444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garg D., Muthu V., Sehgal I.S., Ramachandran R., Kaur H., Bhalla A., et al. Coronavirus disease (Covid-19) associated mucormycosis (CAM): case report and systematic review of literature. Mycopathologia. 2021;186:289–298. doi: 10.1007/s11046-021-00528-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moorthy A., Gaikwad R., Krishna S., Hegde R., Tripathi K., Kale P.G., et al. SARS-CoV-2, uncontrolled diabetes, and corticosteroids—an unholy trinity in invasive fungal infections of the maxillofacial region? A retrospective, multi-centric analysis. J Maxillofac Oral Surg. 2021;20:418–425. doi: 10.1007/s12663-021-01532-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu J., Wang T., Cai Q., Sun L., Huang D., Zhou G., et al. Longitudinal Changes of liver function and hepatitis B reactivation in COVID-19 patients with pre-existing chronic HBV infection. Hepatol Res. 2020;50(11):1211–1221. doi: 10.1111/hepr.13553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Charan J., Dutta S., Kaur R., Bhardwaj P., Sharma P., Ambwani S., et al. Tocilizumab in COVID-19: a study of adverse drug events reported in the WHO database. Expet Opin Drug Saf. 2021;20:1125–1136. doi: 10.1080/14740338.2021.1946513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anderson G., Maes M., Markus R.P., Rodriguez M. Ebola virus: melatonin as a readily available treatment option. J Med Virol. 2015;87:537–543. doi: 10.1002/jmv.24130. [DOI] [PubMed] [Google Scholar]
- 10.El Frargy M., El-Sharkawy H., Attia G. Use of Melatonin as an adjuvant therapy in neonatal sepsis. J Neonatal Perinat Med. 2015;8:227–232. doi: 10.3233/NPM-15814072. [DOI] [PubMed] [Google Scholar]
- 11.Reiter R.J., Abreu-Gonzalez P., Marik P.E., Dominguez-Rodriguez A. Therapeutic algorithm for use of melatonin in patients with COVID-19. Front Med. 2020;7:226. doi: 10.3389/fmed.2020.00226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shneider A., Kudriavtsev A., Vakhrusheva A. Can melatonin reduce the severity of COVID-19 pandemic? Int Rev Immunol. 2020;39:153–162. doi: 10.1080/08830185.2020.1756284. [DOI] [PubMed] [Google Scholar]
- 13.Adikwu E., Brambaifa N., Obianime W.A. Melatonin and alpha lipoic acid restore electrolytes and kidney morphology of lopinavir/ritonavir-treated rats. J Nephropharmacology. 2019;9:e06. [Google Scholar]
- 14.Gitto E., Karbownik M., Reiter R.J., Tan D.X., Cuzzocrea S., Chiurazzi P., et al. Effects of melatonin treatment in septic newborns. Pediatr Res. 2001;50:756–760. doi: 10.1203/00006450-200112000-00021. [DOI] [PubMed] [Google Scholar]
- 15.Huang C.C., Chiou C.H., Liu S.C., Hu S.L., Su C.M., Tsai C.H., et al. Melatonin attenuates TNF-α and IL-1β expression in synovial fibroblasts and diminishes cartilage degradation: implications for the treatment of rheumatoid arthritis. J Pineal Res. 2019;66 doi: 10.1111/jpi.12560. [DOI] [PubMed] [Google Scholar]
- 16.Anderson G., Reiter R.J. Melatonin: roles in influenza, Covid-19, and other viral infections. Rev Med Virol. 2020;30 doi: 10.1002/rmv.2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ling Y., Li Z.-Z., Zhang J.-F., Zheng X.-W., Lei Z.-Q., Chen R.-Y., et al. MicroRNA-494 inhibition alleviates acute lung injury through Nrf2 signaling pathway via NQO1 in sepsis-associated acute respiratory distress syndrome. Life Sci. 2018;210:1–8. doi: 10.1016/j.lfs.2018.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 18.da Cunha Pedrosa A.M., Weinlich R., Mognol G.P., Robbs B.K., de Biaso Viola J.P., Campa A., et al. Melatonin protects CD4+ T cells from activation-induced cell death by blocking NFAT-mediated CD95 ligand upregulation. J Immunol. 2010;184:3487–3494. doi: 10.4049/jimmunol.0902961. [DOI] [PubMed] [Google Scholar]
- 19.Sun C.K., Lee F.Y., Kao Y.H., Chiang H.J., Sung P.H., Tsai T.H., et al. Systemic combined melatonin–mitochondria treatment improves acute respiratory distress syndrome in the rat. J Pineal Res. 2015;58:137–150. doi: 10.1111/jpi.12199. [DOI] [PubMed] [Google Scholar]
- 20.Darab M.G., Keshavarz K., Sadeghi E., Shahmohamadi J., Kavosi Z. The economic burden of coronavirus disease 2019 (COVID-19): evidence from Iran. BMC Health Serv Res. 2021;21:1–7. doi: 10.1186/s12913-021-06126-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen G., Wu D., Guo W., Cao Y., Huang D., Wang H., et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020;130:2620–2629. doi: 10.1172/JCI137244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cao X. COVID-19: immunopathology and its implications for therapy. Nat Rev Immunol. 2020;20:269–270. doi: 10.1038/s41577-020-0308-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Merad M., Martin J.C. Pathological inflammation in patients with COVID-19: a key role for monocytes and macrophages. Nat Rev Immunol. 2020;20:355–362. doi: 10.1038/s41577-020-0331-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu J., Wang T., Cai Q., Sun L., Huang D., Zhou G., et al. Longitudinal changes of liver function and hepatitis B reactivation in COVID-19 patients with pre-existing chronic hepatitis B virus infection. Hepatol Res. 2020;50:1211–1221. doi: 10.1111/hepr.13553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Habtemariam S., Daglia M., Sureda A., Selamoglu Z., Fuat Gulhan M., Mohammad Nabavi S. Melatonin and respiratory diseases: a review. Curr Top Med Chem. 2017;17:467–488. doi: 10.2174/1568026616666160824120338. [DOI] [PubMed] [Google Scholar]
- 26.Sánchez-López A.L., Ortiz G.G., Pacheco-Moises F.P., Mireles-Ramírez M.A., Bitzer-Quintero O.K., Delgado-Lara D.L., et al. Efficacy of melatonin on serum pro-inflammatory cytokines and oxidative stress markers in relapsing remitting multiple sclerosis. Arch Med Res. 2018;49:391–398. doi: 10.1016/j.arcmed.2018.12.004. [DOI] [PubMed] [Google Scholar]
- 27.Chung C. An upsurge in melatonin overdose. Hong Kong J Emerg Med. 2001;8:150–152. [Google Scholar]
- 28.Chang R., Elhusseiny K.M., Yeh Y.-C., Sun W.-Z. COVID-19 ICU and mechanical ventilation patient characteristics and outcomes—a systematic review and meta-analysis. PLoS One. 2021;16 doi: 10.1371/journal.pone.0246318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ionescu F., Zimmer M.S., Petrescu I., Castillo E., Bozyk P., Abbas A., et al. Extubation failure in critically ill COVID-19 patients: risk factors and impact on in-hospital mortality. J Intensive Care Med. 2021;36:1018–1024. doi: 10.1177/08850666211020281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ahnach M., Zbiri S., Nejjari S., Ousti F., Elkettani C. C-reactive protein as an early predictor of COVID-19 severity. J Med Biochem. 2020;39:500. doi: 10.5937/jomb0-27554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huang I., Pranata R., Lim M.A., Oehadian A., Alisjahbana B. C-reactive protein, procalcitonin, D-dimer, and ferritin in severe coronavirus disease-2019: a meta-analysis. Ther Adv Respir Dis. 2020;14 doi: 10.1177/1753466620937175. 1753466620937175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ali N. Elevated level of C-reactive protein may be an early marker to predict risk for severity of COVID-19. J Med Virol. 2020 doi: 10.1002/jmv.26097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Li H., Xiang X., Ren H., Xu L., Zhao L., Chen X., et al. Serum Amyloid A is a biomarker of severe Coronavirus Disease and poor prognosis. J Infect. 2020;80:646–655. doi: 10.1016/j.jinf.2020.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tajarernmuang P., Phrommintikul A., Limsukon A., Pothirat C., Chittawatanarat K. The role of mean platelet volume as a predictor of mortality in critically ill patients: a systematic review and meta-analysis. Crit Care Res Pract. 2016;2016 doi: 10.1155/2016/4370834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xu P., Zhou Q., Xu J. Mechanism of thrombocytopenia in COVID-19 patients. Ann Hematol. 2020;99:1205–1208. doi: 10.1007/s00277-020-04019-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bhattacharjee S., Banerjee M. Immune thrombocytopenia secondary to COVID-19: a systematic review. SN Compr Clin Med. 2020;2:2048–2058. doi: 10.1007/s42399-020-00521-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mei H., Luo L., Hu Y. Springer; 2020. Thrombocytopenia and thrombosis in hospitalized patients with COVID-19; pp. 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wool G.D., Miller J.L. The impact of COVID-19 disease on platelets and coagulation. Pathobiology. 2021;88:15–27. doi: 10.1159/000512007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Henry B.M., De Oliveira M.H.S., Benoit S., Plebani M., Lippi G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): a meta-analysis. Clin Chem Lab Med. 2020;58:1021–1028. doi: 10.1515/cclm-2020-0369. [DOI] [PubMed] [Google Scholar]
- 40.Mehrpouri M. Hematological abnormalities in patients with COVID-19: an emerging approach to differentiate between severe COVID-19; compared with non-severe forms of the disease. Acta Med Iran. 2021;59 [Google Scholar]