Abstract
Hepatic encephalopathy (HE) is a reversible syndrome of impaired brain function and represents one of the many complications of portal hypertension and decompensated liver disease. Although ammonia is clearly implicated in the pathogenesis of HE, the pathogenesis of HE is multifactorial with numerous mechanisms that results in functional impairment of neuronal cells. The initial management of HE focuses on supportive care and stabilization which includes providing appropriate nutritional support. Thereafter, focus should be on identifying and treating the precipitating factors. There are many therapeutic agents available for the management of HE, most of which are directed towards lowering the gut nitrogen load and thus the serum ammonia level. This review aims to provide an update on the conventional and emerging treatment options for HE.
Keywords: Hepatic encephalopathy, Lactulose, Rifaximin, Fecal microbiota transplant, Zinc, L-ornithine L-aspartate
Core Tip: Hepatic encephalopathy (HE) is a reversible syndrome of impaired brain function and represents one of the many complications of portal hypertension and decompensated liver disease. This review provides an update on the conventional and emerging treatment options for HE. The different conventional and emerging therapeutic options available to date are detailed in the manuscript. We have elaborated all the data available in the literature about the use of fecal microbiota transplant in the treatment of HE.
INTRODUCTION
Hepatic encephalopathy (HE) is a reversible syndrome of impaired brain function and represents one of the many complications of portal hypertension and decompensated liver disease. It is estimated to be present in 50% to 70% of patients with liver cirrhosis[1]. It is a debilitating disease that affects the quality of life of both the patients and their caregivers and contributes to significant health care resource utilization making it an economic burden on health care facilities[2]. In 2009, 23000 patients were admitted for HE, with an average length of stay of 8.5 d exhausting $ 63108 per case[2]. The pathogenesis of HE is multifactorial with numerous mechanisms that results in functional impairment of neuronal cells, none of which are clearly understood[3].
Ammonia, which is a gut-derived nitrogenous toxin produced by the bacterial metabolism of urea from dietary proteins, has been considered the primary pathophysiologic mechanism of HE. It is normally metabolized by the liver and cleared mostly by the kidney and to a lesser extent in the muscle. In patients with cirrhosis and portal hypertension, the hepatic metabolism of ammonia is impaired and there is shunting of ammonia-rich portal blood to the systemic circulation without detoxification. In the brain, ammonia crosses the blood-brain barrier and is metabolized in the astrocytes by glutamine synthetase, which converts ammonia and glutamate to glutamine. Accumulation of glutamine in astrocytes creates an osmotic gradient, resulting in astrocyte swelling and generation of reactive oxygen species, thereby contributing to the cerebral dysfunction. Ammonia also binds to gamma-aminobutyric acid (GABA) receptors on astrocytes, leads to neurosteroids activation, which further contribute to the occurrence of HE. Moreover, the dysbiosis and increased gut permeability seen in cirrhotic patients causes an increase in the production of multiple inflammatory cytokines, which leads to increased blood-brain barrier permeability and cerebral edema[3-5].
Although ammonia is clearly implicated in the pathogenesis of HE, additional factors include inhibition of neurotransmission in the central nervous system via GABA receptors and alteration in other CNS neurotransmitters and circulating amino acids .The precipitating factors for HE include liver failure causing decreased metabolism of ammonia, hypoxia and increased ammonia load due to gastrointestinal bleeding, sepsis, alterations in gut flora, hepatocyte necrosis, neuroinflammation, and structural and functional changes in the brain due to other disease process, presence of spontaneous or iatrogenic portosystemic shunt, and other conditions such as hypokalemia, hyponatremia and use of sedatives.
HE has varying degrees of severity and is commonly divided according to the West Haven criteria into covert HE (CHE) and overt HE (OHE). CHE can be either minimal HE (MHE) or grade I HE, while OHE includes grade II-IV[3,6]. OHE is a spectrum of neuropsychological abnormalities that can usually be detected by bedside clinical tests in contrast to CHE, where specific psychometric tests are needed to discern them because of quasi-normal mental status of the patient at bedside. OHE is present in 30%-45% of patients, with a yearly cumulative risk of development in 20% of patients with cirrhosis. Around 60%-80% of patients diagnosed with liver cirrhosis have evidence of cognitive dysfunction or MHE[7].
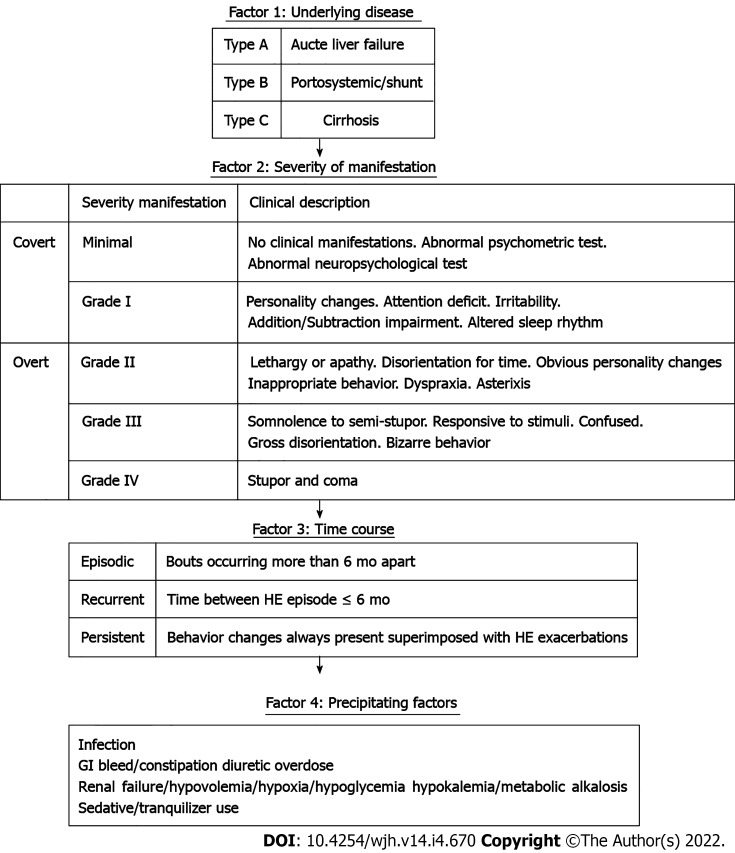
The 2014 American Association for the Study of Liver Diseases (AASLD) and the European Association for the Study of the Liver clinical practice guidelines for HE management[8] recommend classifying HE based on 4 factors detailed in Figure 1: (1) Underlying disease (Type A: HE due to acute liver failure, type B: HE due to portosystemic shunts and type C: HE due to cirrhosis); (2) Severity; (3) Time course; and (4) Precipitating factors.
Figure 1.
Classification of hepatic encephalopathy based on 4 factors. Portions of this figure are adapted from the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver clinical practice guidelines for hepatic encephalopathy management.
The initial management of HE focuses on supportive care and stabilization which includes providing appropriate nutritional support to maintain an energy intake of 35-40 kcal/kg/d, with a protein intake of 1.2-1.5 g/kg/d, correction of precipitating causes which include dehydration and electrolyte abnormalities such as hypokalemia and metabolic alkalosis[9,10]. Thereafter, focus should be on identifying and treating the precipitating factors underlined in Figure 1. There are many therapeutic agents available for the management of HE, most of them are directed towards lowering the gut nitrogen load and thus the serum ammonia levels. This review aims to provide an update on the conventional and emerging treatment options for HE.
GUT FLORA MODIFYING AGENTS
Nonabsorbable disaccharides
The nonabsorbable disaccharides lactulose and lactitol are considered the first-line therapeutic agents for treating HE. They are shown to significantly improve cognition and quality of life in patients with MHE, with lactitol having fewer side effects compared to lactulose[11,12].
It reduces intestinal ammonia production and absorption by four main mechanisms[13-15]: (1) The catabolism of lactulose by bacterial flora in the colon decreases the pH. The acidic pH leads to the formation of nonabsorbable NH4+ from NH3. The trapping of NH4+ (impermeable to membranes) in the colon reduces the plasma ammonia concentration; (2) It causes a laxative effect by increasing intraluminal osmolality as well as gas formation leading to a reduction in gastrointestinal transit time; thus, reducing the time for ammonia absorption and increasing the fecal nitrogen excretion; (3) It promotes an increase in ammonia uptake by colonic bacteria as a nitrogen source for protein synthesis and decrease in the formation of potentially toxic short-chain fatty acids; and (4) The acidic pH caused by lactulose modifies the colonic flora by displacing the urease- producing bacteria involved in ammonia synthesis with non-urease-producing Lactobacillus.
A systematic review published by the Cochrane collaboration in 2016 included 38 randomized controlled trials (RCTs) with a total of 1826 patients and compared lactulose vs placebo. Results were promising and showed a positive effect of non-absorbable disaccharides on mortality [relative risk (RR) = 0.59, 95% confidence interval (CI): 0.40-0.87] and HE (RR = 0.58, 95%CI: 0.50-0.69)[16].
Lactulose (or lactitol in some countries) is often used as the first-line treatment for OHE, at a dose of 30-45 mL (20-30 g) of lactulose syrup every 1-2 h until at least two soft bowel movements are produced. Subsequently, the dosing is of lactulose is titrated to two to four times a day to achieve and maintain two to three bowel movements per day[8]. An approximately equivalent dose of lactitol is 67-100 g lactitol powder diluted in 100 mL of water. Lactulose and lactitol may be given as enemas, if patients are unable to take them orally, as 1-3 L of a 20 percent solution.
Antibiotics
Antibiotics with activity targeting urease producing gut bacteria have an ammonia lowering effect. These antibiotics include rifaximin, neomycin, vancomycin and metronidazole.
Rifaximin: Rifaximin has low systemic absorption, wide antimicrobial spectrum, and low occurrence of side effects[17]. The dose of rifaximin is 550 mg orally twice daily or 400 mg orally three times daily. It is typically used as a combination therapy with lactulose to treat acute encephalopathy and prevent recurrent HE when response to lactulose monotherapy is not inadequate. A randomized trial where 299 patients with cirrhosis and documented HE who were in remission at the start of the trial were administered 550 mg of rifaximin twice daily vs placebo for a total of 6 mo found that rifaximin was more effective than placebo in preventing recurrent episodes of HE[18]. Another randomized trial comparing the combination of rifaximin and lactulose with lactulose alone in 120 patients hospitalized with OHE showed that patients who received the combination therapy were more likely to have complete resolution of HE and lower mortality[19].
A recent systematic review of five randomized and five observational studies involving 2276 patients by Wang et al[20] comparing combination therapy (rifaximin + lactulose) vs lactulose alone showed that combination therapy significantly increased clinical efficacy compared with lactulose alone in HE patients [risk difference (RD) = 0.19, 95%CI: 0.09-0.29, P = 0.0002] with a number needed to treat (NNT) of 5 in primary analysis. Combination therapy also significantly reduced the mortality in HE patients compared with lactulose alone (RD = 0.11, 95%CI: -0.19 to -0.03, P = 0.009) with an NNT of 9 in primary analysis. Rifaximin has a place mostly in prevention of recurrence of HE when lactulose alone fails; however, recent studies showed that combination therapy with lactulose might be more beneficial[20].
Neomycin: Neomycin acts by inhibiting the activity of glutaminase, consequently decreasing ammonia production from glutamine in the intestinal mucosa. Although widely used for the treatment of HE in the past, neomycin has a significant side effect profile including ototoxicity, nephrotoxicity, and enterocolitis. The AASLD guidelines[8] recommend neomycin as an alternative for the treatment of OHE[21].
Vancomycin and metronidazole: Vancomycin and metronidazole have also been studied alone or in conjunction with lactulose. In one study[22] involving 12 patients with cirrhosis and encephalopathy who were given 2 g of vancomycin, all 12 patients showed a remarkable clinical improvement after treatment. Another study[23] showed that 19 patients with varying grades of encephalopathy that were treated with 1 wk of metronidazole had significant improvement in mental status scores and asterixis, similar to neomycin. Therefore, the authors concluded that metronidazole may be as effective as neomycin. The serious side effect of metronidazole (neurotoxicity) and vancomycin (bacterial resistance) has limited the use of these agents. Hence, long term treatment with these agents is not recommended.
Probiotics
Probiotics are formulations of microorganisms that modify gut flora to acid resistant, non-urease producing flora, resulting in diminished ammonia production and absorption. Prebiotics include compounds such as lactulose and fermentable fiber which promote the growth of beneficial gut flora. The most beneficial species of gut flora in the treatment of HE appears to be Lactobacilli and bifidobacterial[24]. Most commercial probiotic products are derived from food sources, especially cultured milk products. The Cochrane review of 21 trials with 1420 participants that compared probiotics in any dosage with placebo, or with any other treatment in people with HE, concluded that compared with placebo, probiotics probably improve recovery and may reduce recurrences of OHE, quality of life, and plasma ammonia concentrations. Probiotics, however, have no effect on mortality or significant clinical outcomes when probiotics were compared with lactulose[25]. Probiotic groups had reduced plasma ammonia concentrations compared with the placebo/no intervention groups, but not when compared with lactulose groups. Additional studies are needed before probiotics can routinely be recommended for the treatment or prevention of HE.
Fecal microbiota transplant
Cirrhosis is a leading cause of HE. Compared to healthy individual, the fecal microbiome of cirrhotic patients has prevalent pathogenic bacteria such as Enterobacteriaceae and Streptococcaceae and reduced beneficial bacteria such as Lachnospiraceae and Ruminococcaceae[26]. When the human gut microbiome was compared in patients before and after developing a HE episode, it was found that that there was a significant change in microbial abundance[27]. Subsequent studies conducted on this topic included investigating the fecal microbiome in this subgroup of patients and evaluating if fecal microbiota transplant (FMT) in patients with HE might treat or prevent further episodes of HE and improve cognitive outcomes.
A summary of the pertinent published studies and abstracts investigating the use of FMT in patients with HE till this date is shown in Tables 1 and 2. There was a total of 4 RCTs,1 case series and 1 case report included in this analysis.
Table 1.
Table summarizing characteristics of all studies involving fecal microbiota transplant in cirrhotic patients
|
Ref.
|
Study
|
Intervention
|
Route of FMT administration
|
n
|
Mean MELD score
|
Follow-up
|
|
| Bajaj et al[29], 2019 | Phase I | Treatment arm | FMT + SOC | Enema | 10 | 12.5 | 5 mo |
| Control arm | SOC | 10 | 12.5 | 5 mo | |||
| Bajaj et al[28], 2017 | Phase I | Treatment arm | FMT | Enema | 10 | 13.2 | 5 mo |
| Control arm | SOC | 10 | 12 | 5 mo | |||
| Woodhouse et al[33], 2019 | Phase III | Treatment arm | FMT + Lactulose | NJ tube | 13 | 12.88 | 3 mo |
| Control arm | SOC | 5 | 12.88 | 3 mo | |||
| Bloom et al[81], 2019 | Phase II | Treatment arm | FMT | Oral | 7 | 13.9 | 1 mo |
| Control arm | SOC | 3 | NA | 1 mo | |||
| Mehta et al[30], 2018 | Case series | FMT | Colonoscopy | 10 | 18 | 20 d | |
| Kao et al[32], 2016 | Case report | FMT | Colonoscopy | 1 | 10 | 7 d | |
FMT: Fecal microbiota transplant; SOC: Standard of care; MELD: Model for end-stage liver disease.
Table 2.
Table summarizing the findings of all studies involving fecal microbiota transplant in cirrhotic patients
|
Ref.
|
MELD or MELD delta (last visit-baseline)
|
SAE
|
No. of hospitalized patients
|
Ammonia level (mean µ/dL )
|
HE episodes
|
Cognitive assessment (s): Encephaloapp stroop test (low is good) (t = time, Δt: Change in time)
|
Cognitive assessment (points): PHES score (high is good) (p = points, Δp: Change in points)
|
| Bajaj et al[29], 2019 | 2.8 + (-4.5) | 1 | 0 at median 1 yr | NA | 0 at median 1 yr | Day 0: 245; day 20: 200; t > 1 yr: 225 | Day 0: -7; day 20: -4; P > 1 yr: -6 |
| 2.78 + (-4.7) | 3 | 10 at median 1 yr | NA | 1.5 at median 1 yr | Day 0: 260; day 20: 250; t > 1 yr: 250 | Day 0: -8; day 20: -8; P > 1 yr: -11 | |
| Bajaj et al[28], 2017 | 0.1 + (-2) | 2 | 1 | NA | 0 at 0.4 yr | Day 0: 247; day 0-20: 29.1 ± 27.9 | Day 0: -7.4; day 0-20: (-3.1) ± (-2.1) |
| -0.2 + (-2.7) | 8 | 9 | NA | 6 at 0.4 yr | Day 0: 282; day 0-20: (-43.5) ± (-95.7) | Day 0: -8.6; day 0-20: 0.0 ± 3.1 | |
| Woodhouse et al[33], 2019 | No significant change | 4 | 4 at day 30 | Day 0: 71; day 30: 51 | NA | NA | NA |
| No significant change | 1 | 1 at day 30 | Day 0: 54; day 30: 73 | NA | NA | NA | |
| Bloom et al[81], 2019 | 14.3 ± 3.3 | 1 | NA | No significant change | NA | Day 0: 56; day 30: 22 | Day 7: 2.6; day 30: 3.9 |
| NA | NA | NA | No significant change | NA | NA | NA | |
| Mehta et al[30], 2018 | 15 | 4 | 2 by 20 wk | Day 0: 96; day 20: 74 | 3 by 20 wk | NA | NA |
| Kao et al[32], 2016 | NA | 0 | 1 | Day 0: 75; day 20: 45 | 0 | Day 0: 250.9; day 7: 203.4 | NA |
MELD: Model for end-stage liver disease; HE: Hepatic encephalopathy; NA: Not available.
In the phase I study conducted in 2017[28] and subsequently in 2019[29], the number of hospitalizations as well as HE episodes was significantly lower in the patients that underwent FMT. Another study[30] showed that 2/10 patients required hospitalization and 3/10 developed an encephalopathy episode after FMT at 20 wk. FMT also appeared to be safe and well tolerated[31].
Cognition was assessed using EncephalApp Stroop test in 4 studies[28,29,32]. Psychometric Hepatic Encephalopathy Score (PHES) was utilized in three studies[28,29]. Improvement in the time taken to complete the EncephalApp Stroop test and improvement in the PHES score was demonstrated in these studies. There was a remarkable improvement in PHES total score (P = 0.003) and EncephalApp Stroop (P = 0.01) in the FMT group compared to baseline[28], possibly indicating that FMT might also reverse cognitive impairment in patients with HE.
The PHES and EncephalApp-Stroop test are validated tests for HE-related cognitive function tests and improvement in these tests in patients who underwent FMT is promising. FMT has also been shown to influence lowering serum ammonia levels in three studies[30,32,33]. Although FMT looks promising, additional larger RCTs are needed to validate the results.
NUTRITION, DIETARY MODIFICATION AND SUPPLEMENTATION
Zinc
It has been demonstrated that zinc deficiency is common in patients with liver cirrhosis[34] and lower serum zinc level has also been a precipitating factor for HE[35]. Zinc deficiency results in decreased activity of muscle glutamine synthetase, an important enzyme in reducing serum ammonia levels making zinc an important factor in ammonia detoxification[36].
Chavez-Tapia et al[37] published a metanalysis that included four RCTs of 233 patients evaluating the effect of oral zinc supplementation vs placebo or standard therapy over HE. Three studies showed an improvement in performance on number connection test in the zinc group compared to placebo or standard therapy. This improvement suggests a beneficial effect of oral zinc in encephalopathic patients. However, there was no beneficial effect on HE recurrence. Shen et al[38] also published a metanalysis that included four RCTs of 247 patient’s and concluded that a combination treatment of zinc and lactulose over 3-6 mo significantly improved performance in the number connection test compared to lactulose alone. The effect of short-term (10 d) oral zinc supplementation (zinc sulfate 600 mg/d) on HE, was assessed in a double-blind, crossover trial involving fifteen cirrhotic patients with stable, chronic HE. Serum zinc was significantly raised after oral zinc administration and reached the levels observed in cirrhotics without HE. Despite this, the study failed to confirm that short-term oral zinc supplementation improves chronic HE[39]. Zinc supplementation cannot be recommended for treatment of HE in the absence of larger sample size study.
Branched-chain amino acids
In cirrhotic patients, it has been clarified that there is an imbalance between aromatic amino acids (AAA) and branch-chain amino acids (BCAA) where serum concentrations of AAA are increased and BCAA are decreased. These alterations are thought to increase brain levels of aromatic amino acid precursors for monoamine neurotransmitters which contribute to altered neuronal excitability and development of HE[40].
In 2017, the Cochrane collaboration published a systemic review of 827 patients in 16 RCTs in which use of oral (eight trials) or intravenous BCAAs (seven trials) was compared with placebo, diet, lactulose, or neomycin. BCAAs were found to have a beneficial effect on manifestations of HE. More specifically, when excluding trials on lactulose or neomycin, BCAA had a beneficial effect on HE. However, when analyzing trials with a lactulose or neomycin control, it was found that there was no statistically significant benefit of BCAA over lactulose or neomycin. Gastrointestinal discomfort was the main adverse reaction observed while using BCAA with no serious adverse events reported and this intervention did not seem to influence mortality and quality of life[41]. In summary, it was found that oral, but not intravenous, BCAAs may have beneficial effects. BCAA supplementation may be considered in severely protein-intolerant patients as no benefit was observed in protein-tolerant patients.
Acetyl-L-carnitine
Carnitine is a metabolite in the degradation pathway of the essential amino acid lysine and is a substance natural to the body. Acetyl-L-carnitine (ALC) is readily formed in cells by the enzymatic addition of an acetyl group to carnitine. The major difference between ALC and carnitine is that ALC is more easily absorbed from the gut, and more readily crosses the blood-brain barrier. Carnitine is a carrier for short chain fatty acids across the mitochondrial membrane and is thought to have neuroprotective properties. A systematic review[42] concluded that ALC was effective in improving serum ammonia level (weighted mean difference 25.90, 95%CI: 20.89-30.91, P < 0.05) and number connection test completion time (weighted mean difference: 16.62, 95%CI: 9.88-23.36, P < 0.05), and thus a promising treatment for HE. However, in 2019, the Cochrane collaboration published a systemic review of 398 patients in 5 clinical trials that compared ALC plus standard care (e.g., antibiotics, lactulose) vs placebo or standard care in participants with cirrhosis with covert or OHE. The review showed that ALC reduces serum ammonium levels compared with placebo however no information was found about all-cause mortality, serious adverse events, or days of hospitalization. No clear differences were found between ALC and placebo regarding quality of life, fatigue, and non-serious adverse event[43]. In summary, further RCTs are needed to assess ALC vs placebo.
CENTRAL NERVOUS SYSTEM ACTING AGENTS
Flumazenil
Flumazenil is a short acting benzodiazepine receptor antagonist that was described in multiple trials to benefit patients with HE by antagonizing and eliciting a negative allosteric modulatory effect on the central benzodiazepine receptors[44-46]. The Cochrane collaboration published in 2017 a systematic review[47] of 14 RCT that included 867 patients comparing flumazenil vs placebo. The duration of follow-up was less than 1 d in the majority of the RCT and it was shown that flumazenil was associated with a beneficial effect on HE but with no beneficial effect on mortality, serious adverse events, or health-related quality of life. Although flumazenil yielded short term improvement, all except one of the RCT were described as having high-risk bias. Flumazenil is not recommended for routine clinical use, though it may be considered for select patients who have received benzodiazepine therapy.
Dopamine agonists
Bromocriptine, a dopamine receptor agonist, has been studied as a potential treatment for HE. In one study, 6 patients with cirrhosis and severe HE unresponsive to standard therapy were given oral bromocriptine up to 15 mg daily. All patients showed significant improvement clinically as well as improvement in cerebral blood flow and cerebral glucose consumption which led the authors to conclude that bromocriptine is a useful treatment for chronic HE when conventional therapy fails[48]. A recent metanalysis of 5 trials including levodopa and bromocriptine reported no beneficial effects on HE and mortality[49]. The available clinical data are insufficient to assess the benefit of dopamine agonists; however, they might be useful in patients not responding to first line therapies[48,50].
AMMONIA SCAVENGING AGENTS
L-ornithine L-aspartate
L-ornithine L-aspartate (LOLA) is a combination of two endogenous amino acids. In patients with cirrhosis, the activities of carbamoyl phosphate synthetase and glutamine synthetase are impaired. Ornithine activates both the enzymes, ornithine and aspartate increase ammonia removal via stimulation of glutamine synthesis. LOLA has thus been shown to have ammonia lowering actions via stimulation of urea synthesis by residual periportal hepatocytes and ammonia removal by glutamine synthesis in skeletal muscle[51].
The first published analysis considered[52] five double-blind, placebo-controlled RCTs in 246 patients with cirrhosis (Child-Pugh status A or B) and compared intravenous infusions of 20-40 mg of LOLA over 4-8 h for a 7-d period to placebo. LOLA treatment showed a 3.22-fold greater chance of resolution of OHE and significant reduction of post-prandial serum ammonia after 7 d of therapy compared to placebo. Subsequently, a high quality meta-analysis of three randomized trials that included 212 patients with cirrhosis[53], a meta-analysis of 8 RCTs with 646 patients with cirrhosis[54], and a meta-analysis of 15 RCTs with 1023 patients[55] showed that LOLA was significantly more effective than placebo in patient with OHE. In another met analysis[56], LOLA was shown to significantly reduce serum ammonia level (MD = 17.50, 95%CI: -27.73 to -7.26), regardless of its formulation, compared to placebo. When compared to other ammonia lower agents, LOLA was noted to cause decreases in serum ammonia levels compared to lactulose[57], and improvement of psychometric test scores compared to rifaximin and probiotics[58,59].
A very recent metanalysis published by the Cochrane collaboration[55] in 2018 of 36 RCTs encompassing 2377 patients showed that LOLA had beneficial effect on HE compared with placebo. In patients with MHE, LOLA was found to be comparable to lactulose and rifaximin for both reversal of deficits in psychometric test scores and for slowing of progression from MHE to OHE[51]. Treatment with LOLA is beneficial compared with placebo, but trials comparing LOLA with lactulose are needed. Overall, LOLA has been evaluated to be a safe, effective, and well-tolerated. It is routinely given to patients with HE outside of the United States.
Ornithine phenylacetate, phenylbutyrate and sodium benzoate
L-ornithine combined with phenylacetate as L-ornithine phenylacetate (OPA) lowers ammonia level by L ornithine stimulating synthesis of glutamine from ammonia in skeletal muscle and phenylacetate binding to glutamine and excreting the compound as phenylacetylglutamine through the kidneys in the urine[60]. A study performed by Stravitz et al[61] included 47 patients with acute liver injury/acute liver failure and ammonia level above 60 μM showed that this therapy is safe and well-tolerated in patients with acute liver failure. A metanalysis published by the Cochrane database in 2019[62] failed to show beneficial or harmful effects of OPA vs placebo. Up to this date, there is no clear clinical evidence linking OPA to HE.
Phenylbutyrate (PB), a prodrug of phenylacetate is rapidly oxidized to phenylacetate and acts in the same way[63]. A phase II trial of 178 patients[64] compared glycerol PB (GPB) to placebo and concluded that GPB decreased the frequency of HE events as well as the ammonia levels in patients with cirrhosis and HE and had a comparable safety profile to placebo. However, larger RCTs are needed to confirm these results.
Sodium benzoate is generally used in food and beverage preservative. It conjugates with glycine in the liver and the kidney to form hippuric acid which carries waste nitrogen and is then excreted by the kidneys[13,65]. This low-priced adjunctive agent has shown promising results but cannot be used as first-line therapy until additional randomized trials are conducted. It can be considered as an alternative in patients with good creatinine clearance who are unable to tolerate standard of care regimen or have failed to improve despite the standard regimen[65,66]. A small RCT performed in 1992 by Sushma et al[67], however, compared sodium benzoate to lactulose and concluded that that sodium benzoate is as safe and effective as lactulose.
Spherical carbon microsphere adsorbent (AST-120)
This is an orally administered, engineered carbon microsphere. Compared to activated charcoal, it possesses a better adsorptive capacity for certain organic compounds. It binds to ammonia in the gastrointestinal lumen and facilitate its excretion[62,68]. In rats, it has shown to lower serum ammonia levels and normalize brain water content[68].
Polyethylene glycol 3350-electrolyte solution
Prior to the introduction of lactulose as a therapeutic option for HE, laxative agents were used, suggesting that catharsis might be an effective treatment of HE. However, since the adoption of lactulose for the treatment of HE, studies of cathartic methods have largely been abandoned until recently when a growing interest has developed over a safe, commonly used, and highly effective laxative: Polyethylene glycol 3350-electrolyte solution (PEG)[69]. Multiple RCTs[69-71] studied the effect of PEG vs lactulose for the treatment of HE. These studies showed that PEG led to a more rapid improvement of the HE scoring algorithm score in 24 h and shortened the hospital say. Larger trials are needed to confirm these results before recommending PEG as a routine treatment for patients with cirrhosis and encephalopathy.
Molecular absorbent recirculating system
Molecular absorbent recirculating system (MARS) is an extracorporeal hepatic support system that integrates the mechanisms of dialysis, ultrafiltration, and adsorption. It utilizes an albumin dialysate across a semi-permeable high-fluid membrane to remove protein-bound and water-soluble toxins[72]. MARS was first approved by the United States Food and Drug Administration in 2005 for use in drug overdoses and an additional approval was granted in 2012 for use in HE due to decompensated chronic liver disease[73].
The RELIEF trial that compared standard therapy vs MARS in 189 patients with acute on chronic liver failure showed that the patients treated with MARS had a significant improvement in symptoms of HE (38.2% vs 62.5%, respectively). Specifically, patients with HE treated with MARS improved from grade III-IV to grade 0-I. The study was statistically significant (P = 0.07)[74].
MARS is an expensive therapy necessitating specific skill set and expertise to operate. It is offered only in a few institutions in the United States and Europe. Survival benefit has not been demonstrated. Larger RCTs are essential to rationalize its usage at a greater scale.
VASCULAR/INTERVENTIONAL MANAGEMENT
Embolization of portosystemic shunts
Patients who fail medical management are referred to as having refractory HE. These patients may harbor large spontaneous portosystemic shunts (SPSS), mainly splenorenal shunt, leading to sustained HE episodes. A few studies have investigated embolization of these shunts in selected patients and have noticed beneficial results in the treatment of HE episodes. In a multicenter study of 37 patients with diagnosed refractory HE and SPSS, 18 patients managed to remain free of HE for about 2 years, there was also an overall improvement in autonomy and a decrease in the number of hospitalizations[75]. In another retrospective study[76] involving 20 patients who were eligible for embolization of SPSS, all the patients had immediate improvement by day 7, and 67% of the patients were free from HE related hospitalization over 1 year. Therefore, SPSS embolization may be a treatment option in a select group of patients with refractory HE.
Although HE is not an indication for liver transplant, liver transplantation remains the definitive treatment for reversal of the complications related to cirrhosis. Studies have shown that patients become free of HE following transplantation; follow up studies have also shown that HE may become irreversible despite liver transplant[77-80].
CONCLUSION
Management of HE, since its initial description, has seen great advancement. However, there still exists a wide discrepancy in delivery of care and patient outcomes. Our understanding of the underlying pathophysiologic mechanisms is still limited. Further research into the pathogenesis of the disease may lead to development of more definitive as well as targeted treatment options.
Footnotes
Conflict-of-interest statement: We have no affiliations with any organization or entity with any financial or non-financial interest in the subject matter pertaining to this manuscript.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: April 17, 2021
First decision: July 27, 2021
Article in press: March 25, 2022
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Perazzo JC, Argentina S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
Contributor Information
Gilles Jadd Hoilat, Department of Medicine, SUNY Upstate Medical University, Syracuse, NY 13210, United States. hoilatg@upstate.edu.
Fathima Keshia Suhail, Department of Medicine, SUNY Upstate Medical University, Syracuse, NY 13210, United States.
Talal Adhami, Department of Gastroenterology, Cleveland Clinic Foundation, Cleveland, OH 44195, United States.
Savio John, Department of Gastroenterology, SUNY Upstate Medical University, Syracuse, NY 13210, United States.
References
- 1.Bustamante J, Rimola A, Ventura PJ, Navasa M, Cirera I, Reggiardo V, Rodés J. Prognostic significance of hepatic encephalopathy in patients with cirrhosis. J Hepatol. 1999;30:890–895. doi: 10.1016/s0168-8278(99)80144-5. [DOI] [PubMed] [Google Scholar]
- 2.Stepanova M, Mishra A, Venkatesan C, Younossi ZM. In-hospital mortality and economic burden associated with hepatic encephalopathy in the United States from 2005 to 2009. Clin Gastroenterol Hepatol. 2012;10:1034–41.e1. doi: 10.1016/j.cgh.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 3.Elwir S, Rahimi RS. Hepatic Encephalopathy: An Update on the Pathophysiology and Therapeutic Options. J Clin Transl Hepatol. 2017;5:142–151. doi: 10.14218/JCTH.2016.00069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tapper EB, Jiang ZG, Patwardhan VR. Refining the ammonia hypothesis: a physiology-driven approach to the treatment of hepatic encephalopathy. Mayo Clin Proc. 2015;90:646–658. doi: 10.1016/j.mayocp.2015.03.003. [DOI] [PubMed] [Google Scholar]
- 5.Wijdicks EF. Hepatic Encephalopathy. N Engl J Med. 2016;375:1660–1670. doi: 10.1056/NEJMra1600561. [DOI] [PubMed] [Google Scholar]
- 6.Patidar KR, Bajaj JS. Covert and Overt Hepatic Encephalopathy: Diagnosis and Management. Clin Gastroenterol Hepatol. 2015;13:2048–2061. doi: 10.1016/j.cgh.2015.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bajaj JS. Review article: the modern management of hepatic encephalopathy. Aliment Pharmacol Ther. 2010;31:537–547. doi: 10.1111/j.1365-2036.2009.04211.x. [DOI] [PubMed] [Google Scholar]
- 8.Vilstrup H, Amodio P, Bajaj J, Cordoba J, Ferenci P, Mullen KD, Weissenborn K, Wong P. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology. 2014;60:715–735. doi: 10.1002/hep.27210. [DOI] [PubMed] [Google Scholar]
- 9.Córdoba J, López-Hellín J, Planas M, Sabín P, Sanpedro F, Castro F, Esteban R, Guardia J. Normal protein diet for episodic hepatic encephalopathy: results of a randomized study. J Hepatol. 2004;41:38–43. doi: 10.1016/j.jhep.2004.03.023. [DOI] [PubMed] [Google Scholar]
- 10.Morgan TR, Moritz TE, Mendenhall CL, Haas R. Protein consumption and hepatic encephalopathy in alcoholic hepatitis. VA Cooperative Study Group #275. J Am Coll Nutr. 1995;14:152–158. doi: 10.1080/07315724.1995.10718487. [DOI] [PubMed] [Google Scholar]
- 11.Conn HO, Leevy CM, Vlahcevic ZR, Rodgers JB, Maddrey WC, Seeff L, Levy LL. Comparison of lactulose and neomycin in the treatment of chronic portal-systemic encephalopathy. A double blind controlled trial. Gastroenterology. 1977;72:573–583. [PubMed] [Google Scholar]
- 12.Sharma P, Sharma BC. Disaccharides in the treatment of hepatic encephalopathy. Metab Brain Dis. 2013;28:313–320. doi: 10.1007/s11011-013-9392-4. [DOI] [PubMed] [Google Scholar]
- 13.Schiano TD. Treatment options for hepatic encephalopathy. Pharmacotherapy. 2010;30:16S–21S. doi: 10.1592/phco.30.pt2.16S. [DOI] [PubMed] [Google Scholar]
- 14.Mukherjee S, John S. Lactulose. 2021 Jul 19. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. [Google Scholar]
- 15.Aldridge DR, Tranah EJ, Shawcross DL. Pathogenesis of hepatic encephalopathy: role of ammonia and systemic inflammation. J Clin Exp Hepatol. 2015;5:S7–S20. doi: 10.1016/j.jceh.2014.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gluud LL, Vilstrup H, Morgan MY. Non-absorbable disaccharides vs placebo/no intervention and lactulose vs lactitol for the prevention and treatment of hepatic encephalopathy in people with cirrhosis. Cochrane Database Syst Rev. 2016:CD003044. doi: 10.1002/14651858.CD003044.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zeneroli ML, Avallone R, Corsi L, Venturini I, Baraldi C, Baraldi M. Management of hepatic encephalopathy: role of rifaximin. Chemotherapy. 2005;51 Suppl 1:90–95. doi: 10.1159/000081994. [DOI] [PubMed] [Google Scholar]
- 18.Bass NM, Mullen KD, Sanyal A, Poordad F, Neff G, Leevy CB, Sigal S, Sheikh MY, Beavers K, Frederick T, Teperman L, Hillebrand D, Huang S, Merchant K, Shaw A, Bortey E, Forbes WP. Rifaximin treatment in hepatic encephalopathy. N Engl J Med. 2010;362:1071–1081. doi: 10.1056/NEJMoa0907893. [DOI] [PubMed] [Google Scholar]
- 19.Sharma BC, Sharma P, Lunia MK, Srivastava S, Goyal R, Sarin SK. A randomized, double-blind, controlled trial comparing rifaximin plus lactulose with lactulose alone in treatment of overt hepatic encephalopathy. Am J Gastroenterol. 2013;108:1458–1463. doi: 10.1038/ajg.2013.219. [DOI] [PubMed] [Google Scholar]
- 20.Wang Z, Chu P, Wang W. Combination of rifaximin and lactulose improves clinical efficacy and mortality in patients with hepatic encephalopathy. Drug Des Devel Ther. 2019;13:1–11. doi: 10.2147/DDDT.S172324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.American Association for the Study of Liver Diseases; European Association for the Study of the Liver. Hepatic encephalopathy in chronic liver disease: 2014 practice guideline by the European Association for the Study of the Liver and the American Association for the Study of Liver Diseases. J Hepatol. 2014;61:642–659. doi: 10.1016/j.jhep.2014.05.042. [DOI] [PubMed] [Google Scholar]
- 22.Tarao K, Ikeda T, Hayashi K, Sakurai A, Okada T, Ito T, Karube H, Nomoto T, Mizuno T, Shindo K. Successful use of vancomycin hydrochloride in the treatment of lactulose resistant chronic hepatic encephalopathy. Gut. 1990;31:702–706. doi: 10.1136/gut.31.6.702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Morgan MH, Read AE, Speller DC. Treatment of hepatic encephalopathy with metronidazole. Gut. 1982;23:1–7. doi: 10.1136/gut.23.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Khungar V, Poordad F. Hepatic encephalopathy. Clin Liver Dis. 2012;16:301–320. doi: 10.1016/j.cld.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 25.Dalal R, McGee RG, Riordan SM, Webster AC. Probiotics for people with hepatic encephalopathy. Cochrane Database Syst Rev. 2017;2:CD008716. doi: 10.1002/14651858.CD008716.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen Y, Yang F, Lu H, Wang B, Chen Y, Lei D, Wang Y, Zhu B, Li L. Characterization of fecal microbial communities in patients with liver cirrhosis. Hepatology. 2011;54:562–572. doi: 10.1002/hep.24423. [DOI] [PubMed] [Google Scholar]
- 27.Bajaj JS, Heuman DM, Hylemon PB, Sanyal AJ, White MB, Monteith P, Noble NA, Unser AB, Daita K, Fisher AR, Sikaroodi M, Gillevet PM. Altered profile of human gut microbiome is associated with cirrhosis and its complications. J Hepatol. 2014;60:940–947. doi: 10.1016/j.jhep.2013.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bajaj JS, Kassam Z, Fagan A, Gavis EA, Liu E, Cox IJ, Kheradman R, Heuman D, Wang J, Gurry T, Williams R, Sikaroodi M, Fuchs M, Alm E, John B, Thacker LR, Riva A, Smith M, Taylor-Robinson SD, Gillevet PM. Fecal microbiota transplant from a rational stool donor improves hepatic encephalopathy: A randomized clinical trial. Hepatology. 2017;66:1727–1738. doi: 10.1002/hep.29306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bajaj JS, Salzman NH, Acharya C, Sterling RK, White MB, Gavis EA, Fagan A, Hayward M, Holtz ML, Matherly S, Lee H, Osman M, Siddiqui MS, Fuchs M, Puri P, Sikaroodi M, Gillevet PM. Fecal Microbial Transplant Capsules Are Safe in Hepatic Encephalopathy: A Phase 1, Randomized, Placebo-Controlled Trial. Hepatology. 2019;70:1690–1703. doi: 10.1002/hep.30690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mehta R, Kabrawala M, Nandwani S, Kalra P, Patel C, Desai P, Parekh K. Preliminary experience with single fecal microbiota transplant for treatment of recurrent overt hepatic encephalopathy-A case series. Indian J Gastroenterol. 2018;37:559–562. doi: 10.1007/s12664-018-0906-1. [DOI] [PubMed] [Google Scholar]
- 31.Taylor A, Lee D, Allard M, Poland B, Greg Slatter J. Phase 1 Concentration-QTc and Cardiac Safety Analysis of the MDM2 Antagonist KRT-232 in Patients With Advanced Solid Tumors, Multiple Myeloma, or Acute Myeloid Leukemia. Clin Pharmacol Drug Dev. 2021;10:918–926. doi: 10.1002/cpdd.903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kao D, Roach B, Park H, Hotte N, Madsen K, Bain V, Tandon P. Fecal microbiota transplantation in the management of hepatic encephalopathy. Hepatology. 2016;63:339–340. doi: 10.1002/hep.28121. [DOI] [PubMed] [Google Scholar]
- 33.Woodhouse CA, Patel VC, Goldenberg S, Sanchez-Fueyo A, China L, O'Brien A, Flach C, Douiri A, Shawcross D. PROFIT, a PROspective, randomised placebo controlled feasibility trial of Faecal mIcrobiota Transplantation in cirrhosis: study protocol for a single-blinded trial. BMJ Open. 2019;9:e023518. doi: 10.1136/bmjopen-2018-023518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Katayama K, Kawaguchi T, Shiraishi K, Ito T, Suzuki K, Koreeda C, Ohtake T, Iwasa M, Tokumoto Y, Endo R, Kawamura N, Shiraki M, Hanai T, Habu D, Tsuruta S, Sakai H, Miwa Y, Kawada N, Kato A, Takei Y, Mine T, Kohgo Y, Seki T, Sata M, Ito Y, Fukui K, Nishiguchi S, Moriwaki H. The Prevalence and Implication of Zinc Deficiency in Patients With Chronic Liver Disease. J Clin Med Res. 2018;10:437–444. doi: 10.14740/jocmr3374w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Loomba V, Pawar G, Dhar KL, Setia MS. Serum zinc levels in hepatic encephalopathy. Indian J Gastroenterol. 1995;14:51–53. [PubMed] [Google Scholar]
- 36.Rahelić D, Kujundzić M, Romić Z, Brkić K, Petrovecki M. Serum concentration of zinc, copper, manganese and magnesium in patients with liver cirrhosis. Coll Antropol. 2006;30:523–528. [PubMed] [Google Scholar]
- 37.Chavez-Tapia NC, Cesar-Arce A, Barrientos-Gutiérrez T, Villegas-López FA, Méndez-Sanchez N, Uribe M. A systematic review and meta-analysis of the use of oral zinc in the treatment of hepatic encephalopathy. Nutr J. 2013;12:74. doi: 10.1186/1475-2891-12-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shen YC, Chang YH, Fang CJ, Lin YS. Zinc supplementation in patients with cirrhosis and hepatic encephalopathy: a systematic review and meta-analysis. Nutr J. 2019;18:34. doi: 10.1186/s12937-019-0461-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Riggio O, Ariosto F, Merli M, Caschera M, Zullo A, Balducci G, Ziparo V, Pedretti G, Fiaccadori F, Bottari E. Short-term oral zinc supplementation does not improve chronic hepatic encephalopathy. Results of a double-blind crossover trial. Dig Dis Sci. 1991;36:1204–1208. doi: 10.1007/BF01307509. [DOI] [PubMed] [Google Scholar]
- 40.Tajiri K, Shimizu Y. Branched-chain amino acids in liver diseases. World J Gastroenterol. 2013;19:7620–7629. doi: 10.3748/wjg.v19.i43.7620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gluud LL, Dam G, Les I, Marchesini G, Borre M, Aagaard NK, Vilstrup H. Branched-chain amino acids for people with hepatic encephalopathy. Cochrane Database Syst Rev. 2017;5:CD001939. doi: 10.1002/14651858.CD001939.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jiang Q, Jiang G, Shi KQ, Cai H, Wang YX, Zheng MH. Oral acetyl-L-carnitine treatment in hepatic encephalopathy: view of evidence-based medicine. Ann Hepatol. 2013;12:803–809. [PubMed] [Google Scholar]
- 43.Martí-Carvajal AJ, Gluud C, Arevalo-Rodriguez I, Martí-Amarista CE. Acetyl-L-carnitine for patients with hepatic encephalopathy. Cochrane Database Syst Rev. 2019;1:CD011451. doi: 10.1002/14651858.CD011451.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Barbaro G, Di Lorenzo G, Soldini M, Giancaspro G, Bellomo G, Belloni G, Grisorio B, Annese M, Bacca D, Francavilla R, Barbarini G. Flumazenil for hepatic encephalopathy grade III and IVa in patients with cirrhosis: an Italian multicenter double-blind, placebo-controlled, cross-over study. Hepatology. 1998;28:374–378. doi: 10.1002/hep.510280212. [DOI] [PubMed] [Google Scholar]
- 45.Goulenok C, Bernard B, Cadranel JF, Thabut D, Di Martino V, Opolon P, Poynard T. Flumazenil vs. placebo in hepatic encephalopathy in patients with cirrhosis: a meta-analysis. Aliment Pharmacol Ther. 2002;16:361–372. doi: 10.1046/j.1365-2036.2002.01191.x. [DOI] [PubMed] [Google Scholar]
- 46.Laccetti M, Manes G, Uomo G, Lioniello M, Rabitti PG, Balzano A. Flumazenil in the treatment of acute hepatic encephalopathy in cirrhotic patients: a double blind randomized placebo controlled study. Dig Liver Dis. 2000;32:335–338. doi: 10.1016/s1590-8658(00)80027-4. [DOI] [PubMed] [Google Scholar]
- 47.Goh ET, Andersen ML, Morgan MY, Gluud LL. Flumazenil vs placebo or no intervention for people with cirrhosis and hepatic encephalopathy. Cochrane Database Syst Rev. 2017;8:CD002798. doi: 10.1002/14651858.CD002798.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Morgan MY, Jakobovits AW, James IM, Sherlock S. Successful use of bromocriptine in the treatment of chronic hepatic encephalopathy. Gastroenterology. 1980;78:663–670. [PubMed] [Google Scholar]
- 49.Junker AE, Als-Nielsen B, Gluud C, Gluud LL. Dopamine agents for hepatic encephalopathy. Cochrane Database Syst Rev. 2014:CD003047. doi: 10.1002/14651858.CD003047.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Uribe M, Farca A, Márquez MA, Garcĭa-Ramos G, Guevara L. Treatment of chronic portal systemic encephalopathy with bromocriptine: a double-blind controlled trial. Gastroenterology. 1979;76:1347–1351. [PubMed] [Google Scholar]
- 51.Butterworth RF, McPhail MJW. L-Ornithine L-Aspartate (LOLA) for Hepatic Encephalopathy in Cirrhosis: Results of Randomized Controlled Trials and Meta-Analyses. Drugs. 2019;79:31–37. doi: 10.1007/s40265-018-1024-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Delcker A, Turowski B, Mihm U, Raab P, Rusch O, Pilatus U, Zeuzem S, Zanella FE. Proton MR spectroscopy of neurometabolites in hepatic encephalopathy during L-ornithine-L-aspartate treatment--results of a pilot study. Metab Brain Dis. 2002;17:103–111. doi: 10.1023/a:1015468112686. [DOI] [PubMed] [Google Scholar]
- 53.Jiang Q, Jiang XH, Zheng MH, Chen YP. L-Ornithine-l-aspartate in the management of hepatic encephalopathy: a meta-analysis. J Gastroenterol Hepatol. 2009;24:9–14. doi: 10.1111/j.1440-1746.2008.05582.x. [DOI] [PubMed] [Google Scholar]
- 54.Bai M, Yang Z, Qi X, Fan D, Han G. l-ornithine-l-aspartate for hepatic encephalopathy in patients with cirrhosis: a meta-analysis of randomized controlled trials. J Gastroenterol Hepatol. 2013;28:783–792. doi: 10.1111/jgh.12142. [DOI] [PubMed] [Google Scholar]
- 55.Goh ET, Stokes CS, Sidhu SS, Vilstrup H, Gluud LL, Morgan MY. L-ornithine L-aspartate for prevention and treatment of hepatic encephalopathy in people with cirrhosis. Cochrane Database Syst Rev. 2018;5:CD012410. doi: 10.1002/14651858.CD012410.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Butterworth RF, Kircheis G, Hilger N, McPhail MJW. Efficacy of l-Ornithine l-Aspartate for the Treatment of Hepatic Encephalopathy and Hyperammonemia in Cirrhosis: Systematic Review and Meta-Analysis of Randomized Controlled Trials. J Clin Exp Hepatol. 2018;8:301–313. doi: 10.1016/j.jceh.2018.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Poo JL, Góngora J, Sánchez-Avila F, Aguilar-Castillo S, García-Ramos G, Fernández-Zertuche M, Rodríguez-Fragoso L, Uribe M. Efficacy of oral L-ornithine-L-aspartate in cirrhotic patients with hyperammonemic hepatic encephalopathy. Results of a randomized, lactulose-controlled study. Ann Hepatol. 2006;5:281–288. [PubMed] [Google Scholar]
- 58.Mittal VV, Sharma BC, Sharma P, Sarin SK. A randomized controlled trial comparing lactulose, probiotics, and L-ornithine L-aspartate in treatment of minimal hepatic encephalopathy. Eur J Gastroenterol Hepatol. 2011;23:725–732. doi: 10.1097/MEG.0b013e32834696f5. [DOI] [PubMed] [Google Scholar]
- 59.Alvares-da-Silva MR, de Araujo A, Vicenzi JR, da Silva GV, Oliveira FB, Schacher F, Oliboni L, Magnus A, Kruel LP, Prieb R, Fernandes LN. Oral l-ornithine-l-aspartate in minimal hepatic encephalopathy: A randomized, double-blind, placebo-controlled trial. Hepatol Res. 2014;44:956–963. doi: 10.1111/hepr.12235. [DOI] [PubMed] [Google Scholar]
- 60.Jalan R, Wright G, Davies NA, Hodges SJ. L-Ornithine phenylacetate (OP): a novel treatment for hyperammonemia and hepatic encephalopathy. Med Hypotheses. 2007;69:1064–1069. doi: 10.1016/j.mehy.2006.12.061. [DOI] [PubMed] [Google Scholar]
- 61.Stravitz RT, Gottfried M, Durkalski V, Fontana RJ, Hanje AJ, Koch D, Hameed B, Ganger D, Subramanian RM, Bukofzer S, Ravis WR, Clasen K, Sherker A, Little L, Lee WM Acute Liver Failure Study Group. Safety, tolerability, and pharmacokinetics of l-ornithine phenylacetate in patients with acute liver injury/failure and hyperammonemia. Hepatology. 2018;67:1003–1013. doi: 10.1002/hep.29621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zacharias HD, Zacharias AP, Gluud LL, Morgan MY. Pharmacotherapies that specifically target ammonia for the prevention and treatment of hepatic encephalopathy in adults with cirrhosis. Cochrane Database Syst Rev. 2019;6:CD012334. doi: 10.1002/14651858.CD012334.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.van Straten G, van Dalen D, Mesu SJ, Rothuizen J, Teske E, Spee B, Favier RP, van Geijlswijk IM. Efficacy of orally administered sodium benzoate and sodium phenylbutyrate in dogs with congenital portosystemic shunts. J Vet Intern Med. 2019;33:1331–1335. doi: 10.1111/jvim.15477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rockey DC, Vierling JM, Mantry P, Ghabril M, Brown RS Jr, Alexeeva O, Zupanets IA, Grinevich V, Baranovsky A, Dudar L, Fadieienko G, Kharchenko N, Klaryts'ka I, Morozov V, Grewal P, McCashland T, Reddy KG, Reddy KR, Syplyviy V, Bass NM, Dickinson K, Norris C, Coakley D, Mokhtarani M, Scharschmidt BF HALT-HE Study Group. Randomized, double-blind, controlled study of glycerol phenylbutyrate in hepatic encephalopathy. Hepatology. 2014;59:1073–1083. doi: 10.1002/hep.26611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Misel ML, Gish RG, Patton H, Mendler M. Sodium benzoate for treatment of hepatic encephalopathy. Gastroenterol Hepatol (N Y) 2013;9:219–227. [PMC free article] [PubMed] [Google Scholar]
- 66.Al Sibae MR, McGuire BM. Current trends in the treatment of hepatic encephalopathy. Ther Clin Risk Manag. 2009;5:617–626. doi: 10.2147/tcrm.s4443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sushma S, Dasarathy S, Tandon RK, Jain S, Gupta S, Bhist MS. Sodium benzoate in the treatment of acute hepatic encephalopathy: a double-blind randomized trial. Hepatology. 1992;16:138–144. doi: 10.1002/hep.1840160123. [DOI] [PubMed] [Google Scholar]
- 68.Bosoi CR, Parent-Robitaille C, Anderson K, Tremblay M, Rose CF. AST-120 (spherical carbon adsorbent) lowers ammonia levels and attenuates brain edema in bile duct-ligated rats. Hepatology. 2011;53:1995–2002. doi: 10.1002/hep.24273. [DOI] [PubMed] [Google Scholar]
- 69.Naderian M, Akbari H, Saeedi M, Sohrabpour AA. Polyethylene Glycol and Lactulose vs Lactulose Alone in the Treatment of Hepatic Encephalopathy in Patients with Cirrhosis: A Non-Inferiority Randomized Controlled Trial. Middle East J Dig Dis. 2017;9:12–19. doi: 10.15171/mejdd.2016.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rahimi RS, Singal AG, Cuthbert JA, Rockey DC. Lactulose vs polyethylene glycol 3350--electrolyte solution for treatment of overt hepatic encephalopathy: the HELP randomized clinical trial. JAMA Intern Med. 2014;174:1727–1733. doi: 10.1001/jamainternmed.2014.4746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shehata HH, Elfert AA, Abdin AA, Soliman SM, Elkhouly RA, Hawash NI, Soliman HH. Randomized controlled trial of polyethylene glycol vs lactulose for the treatment of overt hepatic encephalopathy. Eur J Gastroenterol Hepatol. 2018;30:1476–1481. doi: 10.1097/MEG.0000000000001267. [DOI] [PubMed] [Google Scholar]
- 72.Yarrarapu SNS, Sanghavi D. Molecular Absorbent Recirculating System. 2021 Jul 31. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan- [PubMed] [Google Scholar]
- 73.Hanish SI, Stein DM, Scalea JR, Essien EO, Thurman P, Hutson WR, Bartlett ST, Barth RN, Scalea TM. Molecular Adsorbent Recirculating System Effectively Replaces Hepatic Function in Severe Acute Liver Failure. Ann Surg. 2017;266:677–684. doi: 10.1097/SLA.0000000000002361. [DOI] [PubMed] [Google Scholar]
- 74.Bañares R, Nevens F, Larsen FS, Jalan R, Albillos A, Dollinger M, Saliba F, Sauerbruch T, Klammt S, Ockenga J, Pares A, Wendon J, Brünnler T, Kramer L, Mathurin P, de la Mata M, Gasbarrini A, Müllhaupt B, Wilmer A, Laleman W, Eefsen M, Sen S, Zipprich A, Tenorio T, Pavesi M, Schmidt HH, Mitzner S, Williams R, Arroyo V RELIEF study group. Extracorporeal albumin dialysis with the molecular adsorbent recirculating system in acute-on-chronic liver failure: the RELIEF trial. Hepatology. 2013;57:1153–1162. doi: 10.1002/hep.26185. [DOI] [PubMed] [Google Scholar]
- 75.Laleman W, Simon-Talero M, Maleux G, Perez M, Ameloot K, Soriano G, Villalba J, Garcia-Pagan JC, Barrufet M, Jalan R, Brookes J, Thalassinos E, Burroughs AK, Cordoba J, Nevens F EASL-CLIF-Consortium. Embolization of large spontaneous portosystemic shunts for refractory hepatic encephalopathy: a multicenter survey on safety and efficacy. Hepatology. 2013;57:2448–2457. doi: 10.1002/hep.26314. [DOI] [PubMed] [Google Scholar]
- 76.Lynn AM, Singh S, Congly SE, Khemani D, Johnson DH, Wiesner RH, Kamath PS, Andrews JC, Leise MD. Embolization of portosystemic shunts for treatment of medically refractory hepatic encephalopathy. Liver Transpl. 2016;22:723–731. doi: 10.1002/lt.24440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Atluri DK, Asgeri M, Mullen KD. Reversibility of hepatic encephalopathy after liver transplantation. Metab Brain Dis. 2010;25:111–113. doi: 10.1007/s11011-010-9178-x. [DOI] [PubMed] [Google Scholar]
- 78.García-Martínez R, Simón-Talero M, Córdoba J. Prognostic assessment in patients with hepatic encephalopathy. Dis Markers. 2011;31:171–179. doi: 10.3233/DMA-2011-0840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Frederick RT. Extent of reversibility of hepatic encephalopathy following liver transplantation. Clin Liver Dis. 2012;16:147–158. doi: 10.1016/j.cld.2011.12.004. [DOI] [PubMed] [Google Scholar]
- 80.Garcia-Martinez R, Rovira A, Alonso J, Jacas C, Simón-Talero M, Chavarria L, Vargas V, Córdoba J. Hepatic encephalopathy is associated with posttransplant cognitive function and brain volume. Liver Transpl. 2011;17:38–46. doi: 10.1002/lt.22197. [DOI] [PubMed] [Google Scholar]
- 81.Bloom PP, Donlan J, Torres Soto M, Bloom JA, Scherrer AB, Xavier RJ, Hohmann E, Chung RT. Oral fecal microbiota transplant capsules improve cognition in patients with recurrent hepatic encephalopathy in a donor-specific fashion. Hepatology. 2019;70:268A–269A. [Google Scholar]