Abstract
Significance.
Findings regarding changes in substance use since COVID-19 have been mixed, potentially due to differences in methods used to assess change. Thus, we compared changes in substance use per retrospective self-report at one time-point (March-May 2020) versus prospective, longitudinal self-report across 2 time-points (Sept-Dec 2019; March-May 2020), and identified predictors of discordance.
Methods.
We analyzed data from a longitudinal study of 1,082 young adults from 6 metropolitan areas. Across cigarettes, e-cigarettes, marijuana, and alcohol, participants were categorized as Increasers (increased based on both methods), Decreasers/Stable (decreased/same per both methods), Over-reporters (decreased/same per longitudinal data/increased via retrospective report), or Under-reporters (increased per longitudinal data/decreased/same via retrospective report). We identified predictors (e.g., sociodemographics, pre-pandemic substance use levels) of Under-reporting.
Results.
In this sample (Mage=24.77; 45.7% male, 32.1% sexual minority, 4.0% Black, 12.4% Asian, 12.6% Hispanic), longitudinal data indicated that the proportions of cigarette, e-cigarette, marijuana, and alcohol users who increased their use were 43.3%, 41.7%, 52.6%, and 55.6%, respectively. Examining concordance/discordance groups, Under-reporters accounted for between 17.7% (alcohol) and 26.8% (e-cigarette) of users; over-reporters comprised among the smallest proportions of each group (17.4% for alcohol to 22.2% for marijuana). Multivariable regression indicated that predictors of Under-reporting were less pre-pandemic use across substances; being older for e-cigarettes; and being older, male, and Asian for alcohol.
Conclusions.
Findings highlight methodological variability as a potential reason for mixed findings regarding pandemic-related substance use change and underscore the need for rigorously designed research to accurately assess the population impact of COVID-19 and other historical events.
Keywords: COVID-19, substance use, retrospective report, longitudinal change, young adults
INTRODUCTION
COVID-19 was characterized as a global pandemic on March 11, 2020; by the end of March 2020, over half of US states mandated stay-at-home orders.1,2 Public health efforts to mitigate the spread of COVID-19 led to social and economic stressors potentially related to mental health problems3 and coping-related substance use.4
Research regarding substance use change during COVID-19 has been mixed with some studies suggesting increases in substance use (i.e., tobacco, alcohol, marijuana)5 and others suggesting stability.6 With regard to specific substances, some studies suggest increases in tobacco (cigarettes,7 e-cigarettes,8 overall tobacco9), alcohol,7,10–13 and marijuana,10,12–14 some suggest decreases in tobacco (cigarettes,12,13 e-cigarettes10,15) and marijuana,16 and others suggest stable use of tobacco,17 alcohol,6 and marijuana.7
Differences in the assessment of substance use change across studies may explain inconsistencies. Whereas some research used prospective, longitudinal data to characterize change (before to during COVID-19),11,13 a large proportion relied on retrospective cross-sectional survey data.6,7,9,10,12,14,15,17 Because shorter recall periods of substance use produce more reliable estimates relative to longer periods (which often result in under-reporting use),18–22 data from the latter approach may yield unreliable pre-COVID-19 use estimates.
To shed light on the implications of using retrospective recall to assess COVID-19 related substance use change and reasons for inconsistencies in the literature, the current study compared changes in substance use based on individual retrospective self-report at one time-period (March-May 2020) versus prospective, longitudinal self-report across 2 time-periods (Sept-Dec 2019; March-May 2020), and identified predictors of discordance.
METHODS
Study Overview
This study analyzed data from a 2-year, 5-wave longitudinal study of 3,006 young adults (aged 18–34 at Wave 1 [W1]) in 6 metropolitan statistical areas (MSAs; Atlanta, Boston, Minneapolis, Oklahoma City, San Diego, Seattle), described elsewhere.23 Participants were recruited via social media in Fall 2018, using purposive, quota-based sampling to target tobacco/e-cigarette users.23 We analyzed data from W3 (Fall 2019) and W4, which launched in February 2020 but was interrupted in mid-March to add COVID-related items. The W4 sample was 2,159 (71.2% of W1 N=3,006); the number completing W4 after COVID-related items were added was 1,082 (69.4% of the 1,559 contacted after W4 was interrupted). See Figure 1 for details.
Figure 1. Participant recruitment flowchart.
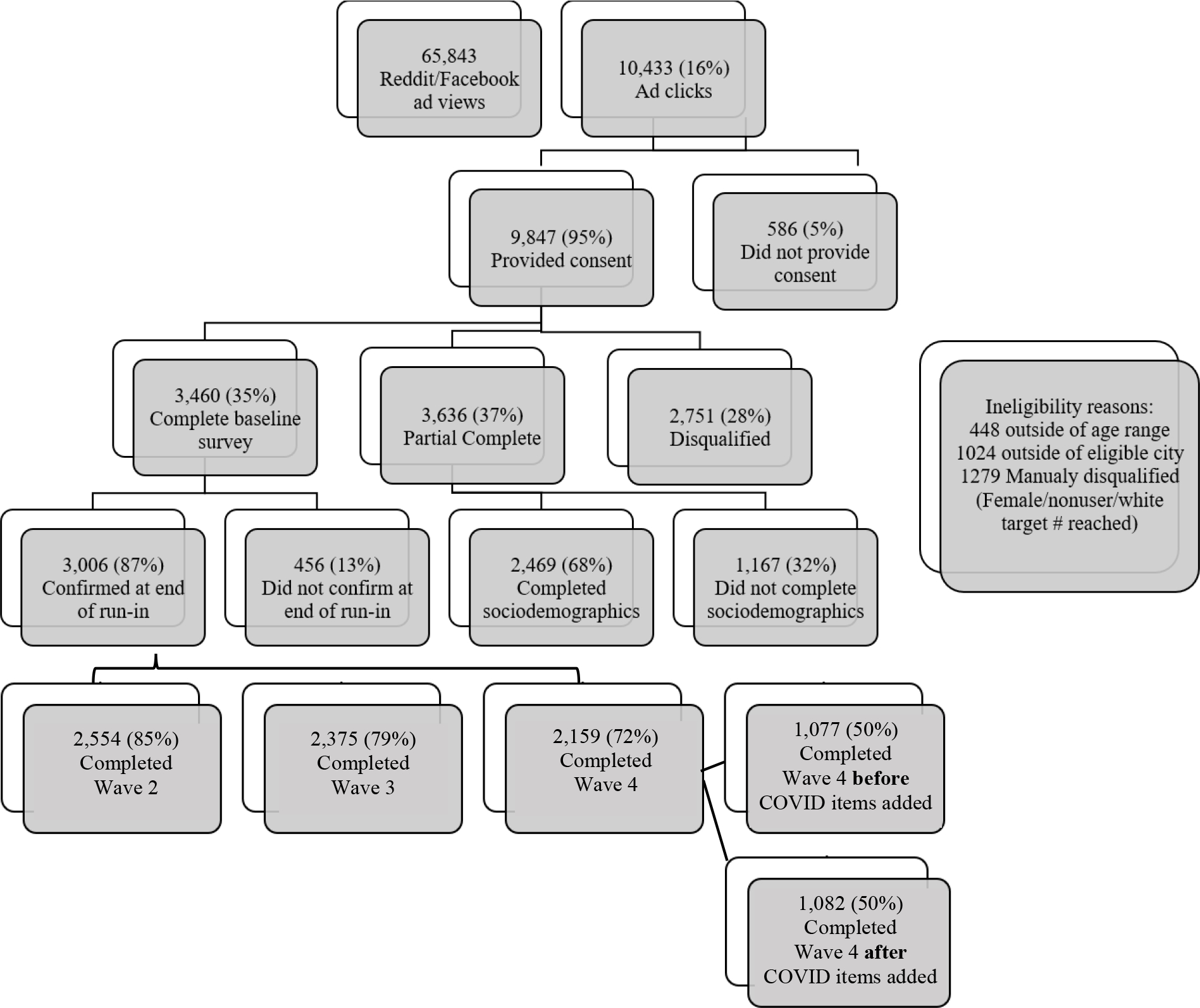
Note: See reference23 for details on recruitment. This study analyzed data from W3 (Fall 2019) and W4, which was launched in Feb 2020 but was interrupted in mid-March to add COVID-19 related items. The W4 sample was 2,159 (71.2% of the baseline sample of 3,006); the number of participants who completed W4 after COVID-related items were added was 1,082 (69.4% of the 1,559 contacted after W4 was interrupted to add these items). W4 completers versus non-completers were older, more likely female, Asian [vs. other race], and college educated, and reported less frequent baseline use of cigarettes, e-cigarettes, and marijuana.
Measures
Outcomes: Substance Use Change and Concordance/Discordance.
Two sets of assessments were used to operationalize concordant versus discordant reports from prospective versus retrospective reports. First, at W3 and W4, participants reported frequency of past 30 day use of cigarettes, e-cigarettes, marijuana, and alcohol. Among those reporting any past-month use at W4 (cigarettes: n=233, e-cigarettes: n=288, marijuana: n=414, alcohol: n=818), we subtracted number of days used at W3 from W4 reports. We then categorized users as: 1) increasers (>0 days change) versus 2) decreasers/stable (≤0 days change); we collapsed decreasers/stable for parsimony, interpretability, and to focus on the high-risk behavior of increased use.
Second, at W4, participants were asked, “Compared to before COVID-19, are you doing more or less of the following: using tobacco (other than e-cigarettes)? vaping (nicotine)? using marijuana? drinking alcohol? much more, somewhat more, no different, somewhat less, much less, not applicable, refuse” – then categorized as: 1) increasers (i.e., much more, somewhat more) versus 2) decreasers/stable (i.e., somewhat less, much less, no different).
Participants were categorized as: 1) Increasers (concordant); 2) Decreasers/Stable (concordant); 3) Over-reporters (decreased/same per W3-W4 substance use but increased per W4 self-report); or 4) Under-reporters (increased per W3-W4 scores but decreased/same per W4 self-report). We excluded W4 nonusers, as ~50% of these participants across substances indicated N/A for the retrospective assessment.
Sociodemographics.
At W1, age, sex, sexual orientation, race, ethnicity, education level, marital status/living with partner, and children in the home were assessed.
Data Analysis
Analyses were conducted using SPSS 26. We characterized our sample using descriptive statistics and conducted multivariable regressions examining predictors of being an “Under-reporter” for each substance. Each model included sociodemographics (excluding education, employment, marital status, and children in the home, due to multicollinearity with age) and W3 substance use.
RESULTS
Table 1 presents participant characteristics. Supplementary Table 1 provides an overview of differences between W4 past-month users versus non-users for each substance. The percentage of participants who increased use based on prospective change scores ranged from 41.7% (e-cigarettes) to 55.6% (alcohol), whereas those who increased use based on retrospective self-report change scores ranged from 31.2% (e-cigarettes) to 53.8% (alcohol; Table 2).
Table 1.
Participant characteristics and bivariate comparisons among under-reporters versus other categories per cross-sectional self-report of increase, decrease, same at W4 (versus self-reported levels of use at W3 and W4)
| Cigarette users | E-cigarette users | Marijuana users | Alcohol users | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| Total | Under-reporters | Else | Under-reporters | Else | Under-reporters | Else | Under-reporters | Else | |
|
|
|||||||||
| Variables | N=1,082 (100%) | N=47 (26.4%) | N=131 (73.6%) | N=66 (26.8%) | N=180 (73.2%) | N=78 (21.1%) | N=291 (78.9%) | N=132 (17.7%) | N=613 (82.3%) |
|
| |||||||||
| Sociodemographics | |||||||||
| Age, M (SD) | 24.77 (4.68) | 25.89 (5.36) | 25.26 (4.75) | 25.44 (4.89) | 24.07 (4.82) | 23.85 (4.75) | 24.53 (4.75) | 25.88 (4.94) | 24.58 (4.57) |
| Female, N (%) | 556 (51.4) | 12 (26.1) | 70 (55.1) | 27 (40.9) | 92 (53.2) | 44 (57.9) | 152 (54.1) | 54 (41.5) | 334 (56.1) |
| Sexual minority, N (%) | 347 (32.1) | 10 (21.3) | 50 (38.2) | 21 (31.8) | 67 (37.2) | 28 (35.9) | 124 (42.6) | 33 (25.0) | 210 (34.3) |
| Race, N (%) | |||||||||
| White | 793 (73.3) | 31 (66.0) | 101 (77.1) | 47 (71.2) | 125 (69.4) | 56 (71.8) | 220 (75.6) | 94 (71.2) | 477 (77.8) |
| Black | 43 (4.0) | 1 (2.1) | 5 (3.8) | 3 (1.7) | 3 (4.5) | 6 (7.7) | 10 (3.4) | 6 (4.5) | 19 (3.1) |
| Asian | 134 (12.4) | 10 (21.3) | 9 (6.9) | 9 (13.6) | 24 (13.3) | 11 (14.1) | 29 (10.0) | 14 (10.6) | 64 (10.4) |
| Other | 112 (10.4) | 5 (10.6) | 16 (12.2) | 7 (10.6) | 28 (15.6) | 5 (6.4) | 32 (11.0) | 18 (13.6) | 53 (8.6) |
| Hispanic, N (%) | 136 (12.6) | 15 (31.9) | 20 (15.3) | 10 (15.2) | 25 (13.9) | 6 (7.7) | 35 (12.0) | 22 (16.7) | 65 (10.6) |
| Education ≥bachelor’s degree, N (%) | 822 (76.0) | 32 (68.1) | 80 (61.1) | 40 (60.6) | 120 (66.7) | 54 (69.2) | 202 (69.4) | 105 (79.5) | 485 (79.1) |
| Married/living with partner, N (%) | 422 (39.0) | 24 (51.1) | 55 (42.0) | 31 (47.0) | 80 (44.4) | 31 (39.7) | 120 (41.2) | 55 (41.7) | 247 (40.3) |
| Children in the home, N (%) | 216 (20.0) | 14 (29.8) | 40 (30.5) | 17 (25.8) | 33 (18.3) | 17 (21.8) | 55 (18.9) | 33 (25.0) | 102 (16.6) |
| W3 Substance Use | |||||||||
| Past 30-day cigarette use, M (SD) | 3.02 (7.74) | 4.26 (5.81) | 15.93 (12.18) | 8.64 (11.24) | 6.00 (9.23) | 3.32 (7.97) | 4.17 (8.99) | 3.08 (7.19) | 2.73 (7.24) |
| Past 30-day e-cigarette use, M (SD) | 4.69 (9.74) | 7.53 (11.17) | 10.21 (12.19) | 4.91 (7.75) | 20.14 (11.71) | 6.47 (10.65) | 6.30 (10.59) | 3.58 (8.56) | 4.67 (9.60) |
| Past 30-day marijuana use, M (SD) | 5.54 (9.94) | 8.36 (11.02) | 9.44 (11.69) | 8.88 (10.86) | 9.44 (11.88) | 6.73 (9.67) | 15.65 (12.11) | 5.12 (10.24) | 5.55 (9.56) |
| Past 30-day alcohol use, M (SD) | 5.75 (6.29) | 5.43 (7.39) | 7.06 (7.05) | 6.50 (6.90) | 6.42 (6.66) | 5.86 (5.24) | 7.53 (7.19) | 3.72 (4.64) | 7.86 (6.46) |
Note: Bolded values denote statistical significance (per t-tests and Chi-square).
Table 2.
Descriptive statistics for change scores and discrepancies between W3-W4 prospective and W4 retrospective change scores, N=1,082
| Cigarettes | E-cigarettes | Marijuana | Alcohol | |
|---|---|---|---|---|
|
| ||||
| Continuous Prospective W3-W4 Change Score, M (SD) | 0.51 (8.74) | 1.96 (9.00) | 2.24 (8.12) | 2.20 (5.92) |
| Categorical Prospective W3-W4 Change, N (%) | ||||
| Increased | 94 (43.3) | 110 (41.7) | 203 (52.6) | 430 (55.6) |
| Decreased/Same | 123 (56.7) | 154 (58.3) | 183 (47.4) | 344 (44.4) |
| Categorical Retrospective Self-Report Change, N (%) | ||||
| Increased | 62 (32.5) | 84 (31.2) | 212 (53.5) | 440 (53.8) |
| Decreased/Same | 129 (67.5) | 185 (68.8) | 184 (46.5) | 348 (44.2) |
| Discrepancies in W3-W4 Prospective and Retrospective Change Scores, N (%) | ||||
| Increased W3-W4 and Retrospective Self-Report (Increaser) | 24 (13.5) | 34 (13.8) | 116 (31.4) | 288 (38.7) |
| Decreased/Same W3-W4 and Retrospective Self-Report (Decreaser) | 73 (41.0) | 103 (41.9) | 93 (25.2) | 195 (26.2) |
| Decreased/Same W3-W4 but Increased Retrospective Self-Report (Over-reporter) | 34 (19.1) | 43 (17.5) | 82 (22.2) | 130 (17.4) |
| Increased W3-W4 but Decreased/Same Retrospective Self-Report (Under-reporter) | 47 (26.4) | 66 (26.8) | 78 (21.1) | 132 (17.7) |
Note: Analyses conducted among W4 users of respective substances (N=233 for cigarettes, N=288 for e-cigarettes, N=414 for marijuana, N=818 for alcohol).
Participants using every day of the past 30 days at W3 ranged from 0.9% (alcohol) to 33.7% (e-cigarettes). Among W3 daily users, those also using daily at W4 ranged from 74.0% (cigarettes) to 86.5% (e-cigarettes). W3 daily users who decreased their number of days of W4 use ranged from 13.5% (e-cigarette users) to 26.0% (cigarette users).
Regarding use change concordance/discordance, the largest category was Decreasers/Stable (41.0%, 41.9%, and 31.4%, respectively) for cigarettes, e-cigarettes, and marijuana, and Increasers (38.7%) for alcohol (Table 2). The smallest category was Increasers (13.5% and 13.8%, respectively) for cigarettes and e-cigarettes, Under-reporters (21.1%) for marijuana, and Over-reporters (17.4%) for alcohol. Under-reporters accounted for 26.4% of cigarette users, 26.8% of e-cigarette users, and 17.7% of alcohol users. Over-reporters were among the smallest proportions of each group (17.4% of alcohol users to 22.2% of marijuana users).
Bivariate findings characterizing differences between Under-reporters versus others for each substance are also presented in Table 1. Multivariable regression (Table 3) indicated that predictors of being Under-reporters were: 1) cigarettes: less frequent W3 cigarette use; 2) e-cigarettes: older age and less frequent W3 e-cigarette use; 3) marijuana: less frequent W3 marijuana and alcohol use; and 4) alcohol: older age, male, Asian, and less frequent W3 alcohol use.
Table 3.
Binary logistic regression analyses identifying correlates of under-reporting increases in substance use per retrospective self-report of increase, decrease, or same (versus self-reported levels of use at W3 and W4)
| Under-reported increases in cigarette use (yes vs. no) | Under-reported increases in e-cigarette use (yes vs. no) | Under-reported increases in marijuana use (yes vs. no) | Under-reported increases in alcohol use (yes vs. no) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||
| Sociodemographics | OR | CI | p | OR | CI | p | OR | CI | p | OR | CI | p |
|
| ||||||||||||
| Age | 1.07 | 0.98, 1.17 | .157 | 1.08 | 1.01, 1.17 | .048 | 0.97 | 0.92, 1.03 | .355 | 1.05 | 1.01, 1.10 | .025 |
| Female | 0.46 | 0.18, 1.13 | .091 | 0.66 | 0.31, 1.40 | .281 | 1.07 | 0.61, 1.87 | .807 | 0.55 | 0.36, 0.84 | .006 |
| Sexual minority | 0.81 | 0.29, 2.23 | .682 | 0.91 | 0.40, 2.07 | .817 | 0.72 | 0.40, 1.29 | .263 | 0.64 | 0.39, 1.03 | .065 |
| Race (ref: White) | ||||||||||||
| Black | 0.34 | 0.03, 4.11 | .398 | 0.74 | 0.13, 4.33 | .735 | 1.65 | 0.50, 5.48 | .415 | 1.11 | 0.41, 2.96 | .840 |
| Asian | 2.94 | 0.91, 9.45 | .071 | 0.57 | 0.20, 1.59 | .281 | 1.07 | 0.47, 2.43 | .878 | 0.85 | 0.43, 1.68 | .632 |
| Other | 0.81 | 0.20, 3.25 | .768 | 0.76 | 0.26, 2.26 | .619 | 0.67 | 0.24, 1.92 | .458 | 2.10 | 1.09, 4.04 | .026 |
| Hispanic | 2.20 | 0.80, 6.06 | .128 | 0.86 | 0.32, 2.34 | .772 | 0.50 | 0.19, 1.36 | .177 | 1.01 | 0.56, 1.82 | .987 |
| W3 Substance Use | ||||||||||||
| Past 30-day cigarette use | 0.87 | 0.82, 0.93 | <.001 | 1.01 | 0.98, 1.05 | .510 | 1.02 | 0.98, 1.06 | .293 | 1.02 | 0.99, 1.05 | .224 |
| Past 30-day e-cigarette use | 0.98 | 0.94, 1.02 | .272 | 0.88 | 0.84, 0.91 | <.001 | 1.02 | 0.99, 1.05 | .207 | 0.99 | 0.96, 1.01 | .315 |
| Past 30-day marijuana use | 1.02 | 0.98, 1.06 | .269 | 1.01 | 0.98, 1.04 | .586 | 0.92 | 0.90, 0.95 | <.001 | 1.01 | 0.99, 1.03 | .365 |
| Past 30-day alcohol use | 0.98 | 0.92, 1.05 | .572 | 0.98 | 0.93, 1.04 | .533 | 0.94 | 0.90, 0.99 | .022 | 0.83 | 0.79, 0.88 | <.001 |
|
| ||||||||||||
| Nagelkerke R-square | .423 | .433 | .204 | .193 | ||||||||
Notes: Bolded values denote statistical significance.
Analyses conducted among W4 users of respective substances (N=233 for cigarettes, N=288 for e-cigarettes, N=414 for marijuana, N=818 for alcohol).
Sensitivity Analyses:
We also operationalized W3-W4 change based on frequency of past 30 day cigarette and e-cigarette use, respectively, multiplied by times used per day to create overall cigarette and e-cigarette use variables; the use per day items were not included for marijuana and alcohol. Participants were then designated into the Increasers, Decreasers/Stable, Over-reporters, or Under-reporters categorizations, which remained largely unchanged (i.e., generally within 5% differences in category size). In analyses using these categorizations, bivariate associations were similar, and multivariable regression consistently indicated that predictors of being cigarette and e-cigarette Under-reporters were less frequent W3 use, respectively.
DISCUSSION
Longitudinal data indicated that proportions of cigarette, e-cigarette, marijuana, and alcohol users who increased use were 43.3%, 41.7%, 52.6%, and 55.6%, respectively – highlighting the population impact of COVID-19 on substance use. The proportion who under-reported change per retrospective report ranged from 17% to 26%, with under-reporting particularly prominent among cigarette and e-cigarette users; over-reporters represented the smallest group of participants across all substances. Results underscore the importance of considering assessment methods when interpreting findings18–22 and call into question findings based on retrospective reports that provide lower estimates of increased substance use.6–10,14,15,17 To more accurately assess change and identify the temporal associations among variables, using longitudinal, as opposed to cross-sectional research is necessary.24
Being an Under-reporter was associated with lower levels of W3 substance use, which may reflect ceiling effects. Daily users at W3 and W4 would have been accurately categorized as Decreasers/stable, despite being high-risk overall (At W4, daily users represented 7% of cigarette users, 41.3% of e-cigarette users, 21.5% of marijuana users, and 1.7% of alcohol users). Moreover, less frequent users would be subject to recall bias, given the potential variability in their behavior over time.
Older participants were more likely to under-report increases in e-cigarette and alcohol use, whereas male and Asian participants were more likely to under-report increases in alcohol use. Findings are consistent with literature indicating that older young-adult men use tobacco and alcohol at higher rates,25,26 which is associated with greater difficulty with retrospective recall,22 and identifying as Asian is associated with under-reporting use to conform to cultural values.27 Findings also have implications for research examining longitudinal associations among the use of various tobacco products (e.g., gateway effects of e-cigarettes), or among predictors and use. Research relying on retrospective reports of change may yield different findings than research utilizing longitudinal data, perhaps due to a broad range of factors (e.g., social desirability, inaccurate recall, or other biases) and may also lead to inaccurate interpretations of temporal associations or causality.
Limitations include generalizability to other young adults in these MSAs or the US. Use prevalence should not be interpreted as nationally representative, given the purposive sampling design.23 Additionally, participants who were older, female, Asian (vs. other race), more educated, and reported less frequent substance use were more likely to complete the W4 survey, also limiting generalizability. As noted, we did not include assessments of frequency of use per day for marijuana and alcohol, preventing us from running sensitivity analyses for these substances.
Findings highlight measurement (i.e., cross-sectional retrospective versus longitudinal prospective reporting) as a potential reason for mixed findings regarding pandemic-related substance use change and underscore the need for rigorously designed research to accurately assess the population impact of COVID-19 and other historical events. It is critical to accurately understand substance use changes to identify risk/protective factors of such change to inform policy and intervention. Researchers must consider the potential for bias and inaccuracies in data to ensure appropriate interpretation and caution in generalizing.
Supplementary Material
Funding Sources
This work was supported by the US National Cancer Institute (R01CA215155–01A1; PI: Berg). Dr. Berg is also supported by other US National Cancer Institute funding (R01CA179422–01; PI: Berg; R01CA239178–01A1; MPIs: Berg, Levine), the US National Institutes of Health/Fogarty International Center (1R01TW010664–01; MPIs: Berg, Kegler), and the US National Institute of Environmental Health Sciences/Fogarty International Center (D43ES030927–01; MPIs: Berg, Marsit, Sturua).
Footnotes
Declaration of Interests
The authors declare no conflicts of interests.
Ethical Approvals
Institutional Review Board approvals were obtained from Emory University.
REFERENCES
- 1.Elassar A This is where each state is during its phased reopening. http://www.cnn.com/interactive/2020/us/states-reopen-coronavirus-trnd/. Published 2020. Accessed.
- 2.Kates J, Michaud J, Tolbert J. Stay-at-home orders to fight COVID-19 in the Unites States: The risks of a scattershot approach. KFF. 2020. [Google Scholar]
- 3.Marroquin B, Vine V, Morgan R. Mental health during the COVID-19 pandemic: Effects of stay-at-home policies, social distancing behavior, and social resources. Psychiatry Research. 2020;293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mota P Avoiding a new epidemic during a pandemic: The importance of assessing the risk of substance use disorders in the COVID-19 era. Psychiatry Res. 2020;290:113142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Czeisler M, Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic - United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(32):1049–1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Knell G, Robertson MC, Dooley EE, Burford K, Mendez KS. Health behavior changes during COVID-19 pandemic and subsequent “Stay-at-Home” orders. Int J Environ Res Public Health. 2020;17(17). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vanderbruggen N, Matthys F, Van Laere S, et al. Self-Reported Alcohol, Tobacco, and Cannabis Use during COVID-19 Lockdown Measures: Results from a Web-Based Survey. Eur Addict Res. 2020;26(6):309–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yach D Tobacco Use Patterns in Five Countries During the COVID-19 Lockdown. Nicotine Tob Res. 2020;22(9):1671–1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kowitt SD, Cornacchione Ross J, Jarman KL, et al. Tobacco Quit Intentions and Behaviors among Cigar Smokers in the United States in Response to COVID-19. Int J Environ Res Public Health. 2020;17(15). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dumas TM, Ellis W, Litt DM. What Does Adolescent Substance Use Look Like During the COVID-19 Pandemic? Examining Changes in Frequency, Social Contexts, and Pandemic-Related Predictors. J Adolesc Health. 2020;67(3):354–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pollard MS, Tucker JS, Green HD Jr. Changes in Adult Alcohol Use and Consequences During the COVID-19 Pandemic in the US. JAMA Netw Open. 2020;3(9):e2022942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sharma P, Ebbert JO, Rosedahl JK, Philpot LM. Changes in substance use among young adults during a respiratory disease pandemic. SAGE Open Med. 2020;8:2050312120965321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Romm K, Patterson B, Crawford ND, Posner H, West CD, Wedding D, Horn K, & Berg CJ. Changes in young adult substance use during COVID-19 as a function of ACEs, depression, prior substance use and resilience. Substance ABuse. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Laar MW, Oomen PE, van Miltenburg CJA, Vercoulen E, Freeman TP, Hall WD. Cannabis and COVID-19: Reasons for Concern. Front Psychiatry. 2020;11:601653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stokes AC. Declines in Electronic Cigarette Use Among US Youth in the Era of COVID-19-A Critical Opportunity to Stop Youth Vaping in Its Tracks. JAMA Netw Open. 2020;3(12):e2028221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Starks TJ, Jones SS, Sauermilch D, et al. Evaluating the impact of COVID-19: A cohort comparison study of drug use and risky sexual behavior among sexual minority men in the U.S.A. Drug Alcohol Depend. 2020;216:108260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tzu-Hsuan Chen D The psychosocial impact of the COVID-19 pandemic on changes in smoking behavior: Evidence from a nationwide survey in the UK. Tob Prev Cessat. 2020;6:59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Napper LE, Fisher DG, Reynolds GL, Johnson ME. HIV risk behavior self-report reliability at different recall periods. AIDS Behav. 2010;14(1):152–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Martin GW, Pearlman S, Li S. The test-retest reliability of the frequency of multiple drug use in young drug users entering treatment. J Subst Abuse. 1998;10(3):275–290. [DOI] [PubMed] [Google Scholar]
- 20.Blair E, & Burton S Cognitive processes used by survey respondents to answer behavioral frequency questions. The Journal of Consumer Research. 1987;14:280–288. [Google Scholar]
- 21.Brown N Encording, representing, and estimating event frequencies: A multiple strategy perspective. In: Betsh T, ed. Frequency Processing & Cognition. Oxford: Oxford University Press; 2002:37–53. [Google Scholar]
- 22.Monk RL, Heim D, Qureshi A, Price A. “I have no clue what I drunk last night” using Smartphone technology to compare in-vivo and retrospective self-reports of alcohol consumption. PLoS One. 2015;10(5):e0126209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berg CJ, Duan X, Getachew B, et al. Young adult e-cigarette use and retail exposure in 6 US metropolitan areas. Tobacco Regulatory Science. 2020;7(1):59–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hajat C PR, Selya A, Stein E. Critical analysis of common methodology flaws in e-cigarette surveys. Qeios. 2021. [Google Scholar]
- 25.Vasilenko SA, Evans-Polce RJ, Lanza ST. Age trends in rates of substance use disorders across ages 18–90: Differences by gender and race/ethnicity. Drug Alcohol Depend. 2017;180:260–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Reports of the Surgeon General. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General Atlanta (GA): Centers for Disease Control and Prevention (US); 2014. [PubMed] [Google Scholar]
- 27.Moloney M, Hunt G, Evans K. Asian American identity and drug consumption: from acculturation to normalization. J Ethn Subst Abuse. 2008;7(4):376–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


