Abstract
Background/Aims
We investigated the effect of metabolic dysfunction-associated fatty liver disease (MAFLD) on future mortality and cardiovascular disease (CVD) using a prospective community-based cohort study.
Methods
Individuals from two community-based cohorts who were 40 to 70 years old were prospectively followed for 16 years. MAFLD was defined as a high fatty liver index (FLI ≥60) plus one of the following conditions overweight/obesity (body mass index ≥23 kg/m2), type 2 diabetes mellitus, or ≥2 metabolic risk abnormalities. Nonalcoholic fatty liver disease (NAFLD) was defined as FLI ≥60 without any secondary cause of hepatic steatosis.
Results
Among 8,919 subjects (age 52.2±8.9 years, 47.7% of males), 1,509 (16.9%) had MAFLD. During the median follow-up of 15.7 years, MAFLD independently predicted overall mortality after adjustment for confounders (hazard ratio [HR], 1.33; 95% confidence interval [CI], 1.05 to 1.69) but NAFLD did not (HR, 1.20; 95% CI, 0.94 to 1.53). MAFLD also predicted CVD after adjustment for age, sex, and body mass index (HR, 1.35; 95% CI, 1.13 to 1.62), which lost its statistical significance by further adjustments. Stratified analysis indicated that metabolic dysfunction contributed to mortality (HR, 1.51; 95% CI, 1.21 to 1.89) and CVD (HR, 1.27; 95% CI, 1.02 to 1.59). Among metabolic dysfunctions used for defining MAFLD, type 2 diabetes mellitus in MAFLD increased the risk of both mortality (HR, 2.07; 95% CI, 1.52 to 2.81) and CVD (HR, 1.42; 95% CI, 1.09 to 1.85).
Conclusions
MAFLD independently increased overall mortality. Heterogeneity in mortality and CVD risk of subjects with MAFLD may be determined by the accompanying metabolic dysfunctions.
Keywords: Metabolic dysfunction-associated fatty liver disease, Nonalcoholic fatty liver disease, Mortality, Cardiovascular disease
INTRODUCTION
An international consensus of experts recently proposed the clinical use of metabolic dysfunction-associated fatty liver disease (MAFLD) instead of nonalcoholic fatty liver disease (NAFLD) to emphasize the pathogenic association of fatty liver disease with metabolic dysfunction.1,2 MAFLD is diagnosed based on hepatic steatosis and one of three additional criteria (overweight/obesity, presence of type 2 diabetes mellitus, or metabolic dysfunction).1,2 Thus, MAFLD may be diagnosed even if there are other coexisting risk factors for chronic liver diseases, such as excessive alcohol drinking or chronic viral hepatitis.1,2 A study in Asia reported the prevalence of MAFLD was 45.7% among those with chronic hepatitis B virus infections.3
Many previous studies examined liver-related and non-liver-related outcomes in patients with NAFLD, classically defined as fatty liver disease without any secondary cause of hepatic steatosis.4 There is evidence that NAFLD is a significant predictor of fatal and non-fatal cardiovascular disease (CVD) events5 and liver-related mortality,6 although some researchers have questioned these reported relationships.6,7 Considering the different diagnostic criteria for NAFLD4 and MAFLD,1,2 the updated diagnostic criteria for MAFLD should be used to evaluate the clinical outcomes of these patients and to better determine their long-term prognostic value. To our knowledge, only one study has examined hard clinical outcomes of MAFLD such as mortality and CVD.8
To address this issue, the present study examined two prospective community-based cohorts that represent rural and urban areas of Korea, respectively.9 After 16 years of follow-up, we recorded mortality and CVD events in subjects with and without MAFLD and compared the mortality and rate of CVD events in MAFLD patients and NAFLD patients who were defined using different diagnostic criteria.1,4,10
MATERIALS AND METHODS
1. Study participants
The Ansung-Ansan cohort study is an ongoing prospective, community-based cohort study that was previously described in detail.9 Data from 2001–2002 to 2017–2018 were analyzed in this study (Supplementary Methods). Eligible participants were 40 to 70 years old at baseline and lived in the Ansan (n=5,018) or Ansung (n=5,020) community. After excluding subjects with any previous cancer (n=102), CVD (n=249), or both (n=1), or missing data (n=767), 8,919 participants (4,644 from Ansung and 4,275 from Ansan) were included. This study was conducted in accordance with the Declaration of Helsinki, and the study protocol was approved by the ethics committee of the Korean Center for Disease Control and the Institutional Review Board of Ajou University School of Medicine (IRB number: AJIRB-BMR-SMP-17-477). All participants provided written informed consent.
2. Definitions of outcomes
A CVD event was defined as any acute myocardial infarction, coronary artery disease, or cerebrovascular disease that occurred during the follow-up period. Participants were considered to have coronary artery disease if they received coronary bypass surgery, coronary angioplasty, or insertion of a coronary stent, or if they had angina pectoris. Data on CVD events were obtained from the participants’ reports and were corroborated by in-depth interviews and interviews repeated at each biennial follow-up.
Mortality data were only available for the Ansung cohort. Researchers contacted all participants who did not attend the follow-up examination by telephone or a personal visit, and all deaths were reported by participants’ families. Information about deaths, including the date, place, and cause, was obtained through interviews with families and reference to death certificates. The interview or death certificate was used to classify a death as cancer-related, CVD-related, or liver-related.
3. Assessment of MAFLD, NAFLD, and fibrosis
Hepatic steatosis was defined as the presence of a fatty liver index (FLI) of ≥60 using a validated prediction model.11 MAFLD was diagnosed when a study subject had hepatic steatosis and any one of the following: type 2 diabetes mellitus, body mass index (BMI) ≥23 kg/m2, or at least two metabolic abnormalities,1 and NAFLD was defined as hepatic steatosis without other etiologies of chronic liver disease. Advanced fibrosis is defined as a fibrosis-4 index score ≥2.67.12,13 Further details on the definitions are described in Supplementary Methods.
4. Assessment of metabolic parameters
Details are described in Supplementary Methods.
5. Statistical analysis
Data are presented as means±standard deviations or medians (interquartile ranges) for continuous variables and as numbers (percentages) for discrete variables. Cox proportional hazards models were used to assess whether MAFLD or NAFLD was an independent predictor of mortality and incident CVD (model 1: unadjusted; model 2: adjusted for age, sex, and BMI; model 3: adjusted for chronic kidney disease and smoking in addition to all model 2 factors; and model 4: adjusted for hypertension, dyslipidemia, diabetes mellitus, and high-sensitivity C-reactive protein [hs-CRP] in addition to all model 3 factors; model 5: adjusted for excess alcohol consumption and a history of viral hepatitis in addition to all model 4 factors). For sensitivity analyses, participants were categorized into four subgroups based on the presence of hepatic steatosis and/or metabolic dysfunction, or the type of metabolic dysfunction for those with MAFLD. A difference was considered significant when the p-value was <0.05. Further details are described in Supplementary Methods.
RESULTS
1. Baseline characteristics of study subjects
We examined 8,919 subjects, 4,644 from Ansung and 4,275 from Ansan (Table 1). At baseline, the mean age was 52.2±8.9 years and 4,250 subjects (47.7%) were men. Among them, 1,521 subjects (17.1%) had hepatic steatosis (FLI ≥60), 7,168 (80.4%) had one or more metabolic dysfunction. A total of 1,509 (16.9%) had MAFLD. Subjects with MAFLD had higher prevalence of diabetes mellitus, hypertension, and dyslipidemia; a higher rate of obesity; and higher levels of total cholesterol, triglycerides, aspartate aminotransferase, alanine aminotransferase, and gamma glutamyl transpeptidase (p<0.001 for all). A higher proportion of subjects with MAFLD consumed excess alcohol and had a history of viral hepatitis. The baseline characteristics of subjects with NAFLD (n=1,145, 12.8%) and without NAFLD (n=7,774) are shown in Supplementary Table 1. When study subjects were divided according to the presence or absence of NAFLD, subjects with MAFLD were more obese and had worse metabolic profiles compared to subjects without MAFLD (Supplementary Table 1). Advanced fibrosis was detected in 6.3% and 5.7% of subjects with MAFLD and NAFLD, respectively (Supplementary Table 2).
Table 1.
Baseline Clinical Characteristics According to MAFLD Status
| Characteristics | Total | MAFLD (–) | MAFLD (+) | p-value |
|---|---|---|---|---|
| No. of participants | 8,919 | 7,410 | 1,509 | |
| Age, yr | 52.2±8.9 | 52.2±8.9 | 52.4±8.6 | 0.384 |
| Male sex | 4,250 (47.7) | 3,231 (43.6) | 1,019 (67.5) | <0.001 |
| BMI, kg/m2 | 24.4 (22.4–26.5) | 23.9 (22.0–25.7) | 27.6 (25.8–29.6) | <0.001 |
| Waist circumference, cm | 82.8 (76.3–89.0) | 81.0 (75.3–86.0) | 92.0 (88.0–96.7) | <0.001 |
| HbA1c, % | 5.4 (5.1–5.7) | 5.4 (5.1–5.6) | 5.6 (5.3–6.1) | <0.001 |
| Total cholesterol, mg/dL | 190.9 (168.0–216.0) | 188.1 (166.0–212.0) | 206 (180.0–232.0) | <0.001 |
| Triglycerides, mg/dL | 131.3 (95.5–187.8) | 120.0 (90.0–161.0) | 236.0 (177.4–322.0) | <0.001 |
| HDL-C, mg/dL | 45.0 (38.7–52.0) | 46.0 (39.5–53.2) | 41.0 (35.5–47.0) | <0.001 |
| AST, U/L | 25.0 (21.0–30.6) | 24.6 (20.7–29.0) | 30.0 (24.6–40.0) | <0.001 |
| ALT, U/L | 22.0 (16.1–30.0) | 20.4 (16.0–26.7) | 34.1 (25.0–50.0) | <0.001 |
| GGT, U/L | 20.0 (13.1–36.2) | 17.1 (12.1–28.1) | 52.2 (31.2–93.0) | <0.001 |
| Platelet, 109/L | 266.2±64.2 | 265.6±63.0 | 269.4±69.6 | 0.049 |
| eGFR, mL/min/1.73 m2 | 90.9 (78.8–104.7) | 91.1 (79.1–105.2) | 88.3 (76.9–102.8) | <0.001 |
| Systolic blood pressure, mm Hg | 115.3 (104.7–128.0) | 113.3 (103.3–126.0) | 122.0 (112.0–134.7) | <0.001 |
| Diastolic blood pressure, mm Hg | 74.0 (68.7–81.3) | 73.3 (67.3–80.7) | 79.3 (72.7–87.3) | <0.001 |
| HOMA-IR | 1.5 (1.1–2.1) | 1.4 (1.0–1.9) | 2.0 (1.3–2.8) | <0.001 |
| hs-CRP, mg/dL | 0.14 (0.06–0.25) | 0.13 (0.06–0.22) | 0.21 (0.11–0.34) | <0.001 |
| Diabetes mellitus | 1,040 (11.7) | 665 (9.0) | 375 (24.9) | <0.001 |
| Hypertension | 1,959 (22.0) | 1,397 (18.9) | 562 (37.2) | <0.001 |
| Dyslipidemia | 2,665 (29.9) | 1,596 (21.5) | 1,069 (70.8) | <0.001 |
| Chronic kidney disease | 192 (2.2) | 147 (2.0) | 45 (3.0) | 0.015 |
| Excess alcohol consumption* | 608 (8.2) | 305 (20.2) | 913 (10.2) | <0.001 |
| History of viral hepatitis | 296 (4.0) | 84 (5.6) | 380 (4.3) | 0.006 |
| Smoking | <0.001 | |||
| Never | 5,343 (59.9) | 4,711 (63.6) | 632 (41.9) | |
| Past | 1,358 (15.2) | 1,026 (13.8) | 332 (22.0) | |
| Active | 2,218 (24.9) | 1,673 (22.6) | 545 (36.1) |
Data are presented as the mean±SD, number (%), or median (interquartile range). Hepatic steatosis was defined as fatty liver index ≥60 for the diagnosis of MAFLD.
MAFLD, metabolic dysfunction-associated fatty liver disease; BMI, body mass index; HbA1c, glycated hemoglobin; HDL-C, high-density lipoprotein cholesterol; AST, aspartate aminotransferase; ALT, alanine aminotransferase; GGT, gamma glutamyl transpeptidase; eGFR, estimated glomerular filtration rate; HOMA-IR, homeostasis model assessment of insulin resistance; hs-CRP, high-sensitivity C-reactive protein.
*Excess alcohol consumption was defined as alcohol consumption measuring more than 210 g/wk (male) or 140 g/wk (female).
In the 4,644 subjects from Ansung, 729 subjects (15.7%) died (median follow-up period, 15.7 years; interquartile range, 13.9 to 15.9 years) (Supplementary Table 3). Relative to survivors, deceased subjects were predominantly male (63.9% vs 40.6%) and older (61.5±7.2 years vs 54.3±8.6 years). Diabetes mellitus, hypertension, chronic kidney disease, and smoking were more common among deceased subjects than survivors at baseline (Supplementary Table 3). The prevalence of MAFLD was also significantly higher in deceased subjects than survivors (20.3% vs 17.2%, p=0.044).
2. Effect of MAFLD and NAFLD on mortality
Next, we investigated whether MAFLD and NAFLD were independent risk factors for mortality (Table 2). An unadjusted model indicated that MAFLD significantly increased the risk of mortality (hazard ratio [HR], 1.23; 95% confidence interval [CI], 1.03 to 1.47; model 1). MAFLD also increased the risk of mortality after adjustment for multiple confounders, including age, sex, BMI, chronic kidney disease, and smoking status (HR, 1.53; 95% CI, 1.24 to 1.90; model 3). This association remained significant after additional adjustment for metabolic risk factors including hypertension, dyslipidemia, diabetes mellitus, and hs-CRP (HR, 1.36; 95% CI, 1.08 to 1.73; model 4). MAFLD remained to be a significant risk factor for mortality even after further adjustment for a history of viral hepatitis and excess alcohol consumption (HR, 1.33; 95% CI, 1.05 to 1.69; model 5) (Fig. 1A), and viral hepatitis was also an independent predictor of mortality (HR, 1.75; 95% CI, 1.26 to 2.43) (Supplementary Table 4).
Table 2.
Hazard Ratios for Mortality and Cardiovascular Disease According to MAFLD and NAFLD Status
| Mortality | CVD | ||||||
|---|---|---|---|---|---|---|---|
| Hazard ratio | 95% CI | p-value | Hazard ratio | 95% CI | p-value | ||
| MAFLD | |||||||
| Model 1 | 1.23 | 1.03–1.47 | 0.025 | 1.61 | 1.38–1.86 | <0.001 | |
| Model 2 | 1.57 | 1.27–1.94 | <0.001 | 1.35 | 1.13–1.62 | 0.001 | |
| Model 3 | 1.53 | 1.24–1.90 | <0.001 | 1.31 | 1.10–1.57 | 0.003 | |
| Model 4 | 1.36 | 1.08–1.73 | 0.011 | 1.07 | 0.89–1.30 | 0.474 | |
| Model 5 | 1.33 | 1.05–1.69 | 0.018 | 1.08 | 0.89–1.31 | 0.440 | |
| NAFLD | |||||||
| Model 1 | 1.08 | 0.88–1.32 | 0.456 | 1.56 | 1.32–1.81 | <0.001 | |
| Model 2 | 1.35 | 1.07–1.70 | 0.011 | 1.20 | 0.99–1.45 | 0.059 | |
| Model 3 | 1.32 | 1.05–1.67 | 0.018 | 1.17 | 0.97–1.42 | 0.099 | |
| Model 4 | 1.20 | 0.94–1.53 | 0.155 | 0.99 | 0.82–1.21 | 0.947 | |
Hazard ratios of mortality (n=4,644; 729 [15.7%] were deceased) and CVD (n=8,774; 972 [11.1%] developed CVD) for 16 years of follow-up were evaluated by multivariate Cox analysis. Hepatic steatosis was defined as fatty liver index ≥60 for the diagnosis of MAFLD and NAFLD.
MAFLD, metabolic dysfunction-associated fatty liver disease; NAFLD, nonalcoholic fatty liver disease; CVD, cardiovascular disease; CI, confidence interval; Model 1, without adjustment; Model 2, adjusted for age, sex, and body mass index; Model 3, adjusted for chronic kidney disease and smoking status in addition to model 2; Model 4, adjusted for hypertension, dyslipidemia, diabetes mellitus, and high-sensitivity C-reactive protein in addition to model 3; Model 5, adjusted for viral hepatitis and excess alcohol consumption in addition to model 4.
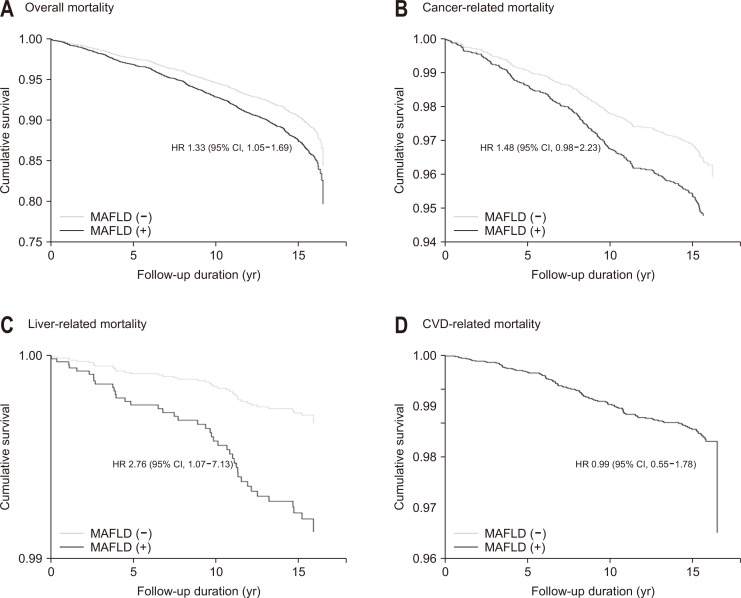
Fig. 1.
Overall and cause-specific mortality and CVD risk by MAFLD status. Cumulative survival rates according to (A) overall, (B) cancer-related, (C) liver-related, and (D) CVD-related mortality in subjects with (black line) and without (gray line) MAFLD for 16 years of follow-up were analyzed using Cox proportional hazards analysis (n=4,644; 729 [15.7%] were deceased; n=244 for cancer-related death; n=114 for CVD-related death; and n=41 for liver-related death). HRs (95% CIs) were calculated after adjustment for age, sex, body mass index, hypertension, dyslipidemia, smoking, diabetes mellitus, chronic kidney disease, high-sensitivity C-reactive protein, excess alcohol consumption, and a history of viral hepatitis (model 5 in Table 3).
MAFLD, metabolic dysfunction-associated fatty liver disease; CVD, cardiovascular disease; HR, hazard ratio; CI, confidence interval.
In contrast, NAFLD did not predict mortality in an unadjusted analysis (model 1 in Table 2), or after adjustment for multiple confounders, including hypertension, dyslipidemia, smoking, and diabetes mellitus (model 4). When a less stringent cutoff point for hepatic steatosis was applied (FLI ≥30), MAFLD marginally, but not significantly, increased the risk mortality (HR, 1.22; 95% CI, 0.99 to 1.50) (model 5 in Supplementary Table 5), but NAFLD did not.
Among the 729 mortalities, cancer, CVD, and liver disease were responsible for 244 (33.4%) (Supplementary Table 6), 114 (15.6%), and 41 deaths (5.6%), respectively. After adjustment for all covariates, MAFLD showed a marginal trend to increase mortality from cancer (HR, 1.48; 95% CI, 0.98 to 2.23) and significantly increased the risk liver disease (HR, 2.76; 95% CI, 1.07 to 7.13), but not from CVD (HR, 0.99; 95% CI, 0.55 to 1.78) (model 5 in Table 3, Fig. 1B-D).
Table 3.
Cause-Specific Mortality According to the MAFLD Status
| Mortality | Hazard ratio | 95% CI | p-value |
|---|---|---|---|
| Overall mortality | |||
| Model 1 | 1.23 | 1.03–1.47 | 0.025 |
| Model 2 | 1.57 | 1.27–1.94 | <0.001 |
| Model 3 | 1.53 | 1.24–1.90 | <0.001 |
| Model 4 | 1.36 | 1.08–1.73 | 0.011 |
| Model 5 | 1.33 | 1.05–1.69 | 0.018 |
| Cancer-related mortality | |||
| Model 1 | 1.21 | 0.89–1.66 | 0.232 |
| Model 2 | 1.63 | 1.13–2.36 | 0.009 |
| Model 3 | 1.59 | 1.10–2.30 | 0.015 |
| Model 4 | 1.52 | 1.01–2.30 | 0.045 |
| Model 5 | 1.48 | 0.98–2.23 | 0.060 |
| CVD-related mortality | |||
| Model 1 | 1.36 | 0.87–2.12 | 0.172 |
| Model 2 | 1.13 | 0.66–1.91 | 0.663 |
| Model 3 | 1.12 | 0.66–1.90 | 0.682 |
| Model 4 | 1.00 | 0.55–1.77 | 0.975 |
| Model 5 | 0.99 | 0.55–1.78 | 0.978 |
| Liver-related mortality | |||
| Model 1 | 1.77 | 0.89–3.52 | 0.107 |
| Model 2 | 3.63 | 1.57–8.43 | 0.003 |
| Model 3 | 3.64 | 1.57–8.45 | 0.003 |
| Model 4 | 3.78 | 1.43–9.95 | 0.007 |
| Model 5 | 2.76 | 1.07–7.13 | 0.036 |
Hazard ratios of cause-specific mortality (n=4,644; 729 [15.7%] were deceased; n=244 for cancer-related death; n=114 for CVD-related death; and n=37 for liver-related death) for 16 years of follow-up were evaluated by multivariate Cox analysis. Hepatic steatosis was defined as fatty liver index ≥60.
MAFLD, metabolic dysfunction-associated fatty liver disease; CI, confidence interval; CVD, cardiovascular disease; Model 1, without adjustment; Model 2, adjusted for age, sex, and body mass index; Model 3, adjusted for chronic kidney disease and smoking status in addition to model 2; Model 4, adjusted for hypertension, dyslipidemia, diabetes mellitus, and high-sensitivity C-reactive protein in addition to model 3; Model 5, adjusted for viral hepatitis and excess alcohol consumption in addition to model 4.
Subsequent sensitivity analysis according to the presence of diabetes mellitus, hypertension, or dyslipidemia, hs-CRP, or BMI which were already included in the definition of MAFLD confirmed that MAFLD consistently increased mortality across different subgroups except for subjects with diabetes mellitus or hypertension (Supplementary Table 7, Supplementary Fig. 1A). NAFLD also increased the risk of mortality among subjects without hypertension, dyslipidemia, or with hs-CRP ≥0.2 mg/dL or BMI <23 kg/m2, but generally to a lesser extent compared to MAFLD.
3. Effect of MAFLD and NAFLD on CVD
We evaluated the incidence of CVD in 8,774 subjects after excluding individuals who were lost to follow-up (n=175); the median follow-up period for these subjects was 15.6 years (interquartile range, 9.6 to 15.8 years). Among them, 972 (11.1%) developed incident CVD. MAFLD predicted cardiovascular events after adjustment for age, sex, and BMI (HR, 1.35; 95% CI, 1.13 to 1.62) (model 2 in Table 2). However, this association was no longer significant after further adjustment for hypertension, dyslipidemia, and diabetes mellitus (models 4-5 in Table 2). Similarly, NAFLD did not independently predict CVD (models 2-4 in Table 2). MAFLD increased the risk of CVD in subjects without diabetes mellitus, hypertension, or dyslipidemia, or with hs-CRP ≥0.2 mg/dL or BMI ≥23 kg/m2; NAFLD predicted CVD only in subjects without hypertension or with hs-CRP ≥0.2 mg/dL (Supplementary Table 7, Supplementary Fig. 1B). When hepatic steatosis was defined by a less stringent cutoff (FLI ≥30), MAFLD independently predicted CVD (HR, 1.28; 95% CI, 1.07 to 1.53) (model 5 in Supplementary Table 5), but NAFLD did not.
4. Subgroup analysis of the effect of MAFLD on mortality and CVD
We next examined which component of MAFLD was most responsible for increased risks of mortality and CVD by stratification of study subjects into four subgroups based on hepatic steatosis and/or metabolic dysfunction: (1) no hepatic steatosis and no metabolic dysfunction (n=1,739; normal control); (2) metabolic dysfunction without hepatic steatosis (n=5,659); (3) hepatic steatosis without metabolic dysfunction (n=12); and (4) hepatic steatosis with metabolic dysfunction (n=1,509).
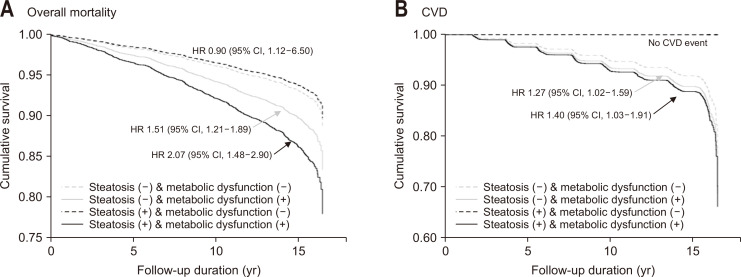
The results of the fully adjusted model, that is, with adjustment for age, sex, BMI, chronic kidney disease, smoking status, hypertension, dyslipidemia, diabetes mellitus, hs-CRP, viral hepatitis and excess alcohol consumption, indicated that metabolic dysfunction independently increased the risk of mortality (HR, 1.51; 95% CI, 1.21 to 1.89) and CVD (HR, 1.27; 95% CI, 1.02 to 1.59) in subjects without hepatic steatosis (Fig. 2). Subjects with hepatic steatosis and metabolic dysfunction (i.e., MAFLD) had an approximately two-fold higher risk of mortality relative to the reference group without both conditions (HR, 2.07; 95% CI, 1.48 to 2.90).
Fig. 2.
Overall mortality and CVD events by MAFLD status. Cumulative survival rates for (A) for overall mortality or (B) incident CVD by the existence of either hepatic steatosis and/or metabolic dysfunction for 16 years of follow-up were analyzed using Cox proportional hazards analysis–(1) no hepatic steatosis and no metabolic dysfunction (n=1,739; normal control; dashed gray line), (2) no hepatic steatosis but metabolic dysfunction (n=5,659; solid gray line), (3) hepatic steatosis without metabolic dysfunction (n=12; dashed black line), and (4) hepatic steatosis with metabolic dysfunction (n=1,509; MAFLD; solid black line). No CVD events occurred in (3) hepatic steatosis without metabolic dysfunction. HRs (95% CIs) were calculated after adjustment for age, sex, body mass index, hypertension, dyslipidemia, smoking, diabetes mellitus, chronic kidney disease, high-sensitivity C-reactive protein, excess alcohol consumption, and a history of viral hepatitis.
CVD, cardiovascular disease; MAFLD, metabolic dysfunction-associated fatty liver disease; HR, hazard ratio; CI, confidence interval.
We also compared the outcomes among three subgroups of patients with MAFLD who had different types of metabolic dysfunction (Table 4): MAFLD1 (BMI ≥23 kg/m2 without diabetes; n=1,102); MAFLD2 (BMI <23 kg/m2 with at least two metabolic abnormalities but not diabetes; n=32); and MAFLD3 (type 2 diabetes mellitus; n=375). Model 5 indicated that the MAFLD3 subgroup had a significantly increased risk of mortality (HR, 2.07; 95% CI, 1.52 to 2.81) and CVD (HR, 1.42; 95% CI, 1.09 to 1.85) and that the MAFLD2 subgroup had increased risk of mortality (HR, 2.34; 95% CI, 1.18 to 4.65) but not CVD. The MAFLD1 subgroup did not show an increased risk of mortality or CVD. Therefore, the analysis of these three subgroups of MAFLD patients indicated that those with diabetes (MAFLD3) had the highest risks of mortality and CVD.
Table 4.
Hazard Ratios for Mortality and Cardiovascular Disease According to Metabolic Dysfunction Subcategories of MAFLD
| Non-MAFLD | MAFLD | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BMI ≥23 kg/m2 without diabetes (MAFLD1) | BMI <23 kg/m2 with ≥2 metabolic risk abnormalities but not diabetes (MAFLD2) | Diabetes (MAFLD3) | |||||||||||
| HR | HR | 95% CI | p-value | HR | 95% CI | p-value | HR | 95% CI | p-value | ||||
| Mortality | |||||||||||||
| Model 1 | 1.00 (reference) | 0.87 | 0.69–1.10 | 0.246 | 4.18 | 2.16–8.07 | <0.001 | 2.14 | 1.65–2.79 | <0.001 | |||
| Model 2 | 1.00 (reference) | 1.24 | 0.95–1.62 | 0.119 | 2.51 | 1.29–4.86 | 0.006 | 2.04 | 1.53–2.72 | <0.001 | |||
| Model 3 | 1.00 (reference) | 1.20 | 0.92–1.58 | 0.179 | 2.40 | 1.23–4.65 | 0.010 | 2.02 | 1.52–2.69 | <0.001 | |||
| Model 4 | 1.00 (reference) | 1.26 | 0.95–1.67 | 0.112 | 2.30 | 1.16–4.57 | 0.017 | 2.11 | 1.55–2.87 | <0.001 | |||
| Model 5 | 1.00 (reference) | 1.23 | 0.93–1.64 | 0.150 | 2.34 | 1.18–4.65 | 0.015 | 2.07 | 1.52–2.81 | <0.001 | |||
| CVD | |||||||||||||
| Model 1 | 1.00 (reference) | 1.40 | 1.17–1.66 | <0.001 | 0.51 | 0.07–3.59 | 0.495 | 2.38 | 1.88–3.01 | <0.001 | |||
| Model 2 | 1.00 (reference) | 1.23 | 1.01–1.51 | 0.043 | 0.48 | 0.07–3.44 | 0.467 | 1.73 | 1.34–2.23 | <0.001 | |||
| Model 3 | 1.00 (reference) | 1.20 | 0.98–1.47 | 0.086 | 0.46 | 0.06–3.24 | 0.432 | 1.69 | 1.31–2.19 | <0.001 | |||
| Model 4 | 1.00 (reference) | 1.04 | 0.84–1.29 | 0.709 | 0.29 | 0.04–2.09 | 0.220 | 1.41 | 1.08–1.84 | 0.012 | |||
| Model 5 | 1.00 (reference) | 1.05 | 0.84–1.29 | 0.684 | 0.30 | 0.04–2.13 | 0.228 | 1.42 | 1.09–1.85 | 0.010 | |||
Hazard ratios (HRs) of mortality (n=4,644; 729 [15.7%] were deceased) and CVD (n=8,774; 972 [11.1%] developed CVD) for 16 years of follow-up were evaluated by multivariate Cox analysis. Hepatic steatosis was defined as fatty liver index ≥60 for the diagnosis of MAFLD and NAFLD.
MAFLD, metabolic dysfunction-associated fatty liver disease; BMI, body mass index; CI, confidence interval; CVD, cardiovascular disease; Model 1, without adjustment; Model 2: adjusted for age, sex, and BMI; Model 3: adjusted for chronic kidney disease and smoking status in addition to model 2; Model 4, adjusted for hypertension, dyslipidemia, and high-sensitivity C-reactive protein in addition to model 3; Model 5, adjusted for viral hepatitis and excess alcohol consumption in addition to model 4.
DISCUSSION
Using an ongoing prospective, community-based cohort study, we found that individuals with MAFLD at baseline had a significantly higher overall mortality during the median follow-up of 15.7 years compared to those without MAFLD, and that the impact of MAFLD on overall mortality was greater than that of NAFLD, which corresponded to the claim-based result.8 In particular, MAFLD at baseline increased the risk of death primarily due to cancer and liver disease.
In the present study, individuals with hepatic steatosis alone did not increase the risk of mortality while individuals with both hepatic steatosis and metabolic dysfunction showed a significantly higher mortality compared to the reference group without hepatic steatosis and metabolic dysfunction. MAFLD is a more pathological phenotype than NAFLD, and patients with MAFLD have higher incidences of comorbidities such as diabetes mellitus, hypertension, and advanced fibrosis.14 The inconsistent data on the effect of hepatic steatosis in the risk of mortality7,15 might be due to the fact that hepatic steatosis alone (without metabolic dysfunction) is insufficient to increase the risk of mortality or CVD events. On the contrary, the presence of metabolic dysfunction alone did independently increase the risk of mortality and CVD events compared to the reference group in the current study, which might attenuate the effect of MAFLD on the risk of CVD. Coexistence of metabolic dysfunction and hepatic steatosis did not further increase the risk of CVD compared to metabolic dysfunction alone, in agreement with the previous studies.16 These findings suggest that metabolic dysfunction contributes to the development of CVD in subjects with MAFLD. Subsequent comparison of MAFLD subgroups according to the different types of metabolic dysfunction suggested that only type 2 diabetes mellitus independently contributes to the development of CVD in MAFLD subjects. This supports the view that diabetes mellitus has a stronger impact on the development of CVD than overweight/obesity (BMI ≥23 kg/m2) and other metabolic abnormalities.17,18
We found that MAFLD had a marginal significance for the risk of death due to cancer, but did not increase the risk of incident CVD. A recent Swedish study reported that excess mortality in patients with biopsy-proven NAFLD was predominantly from extrahepatic cancer and cirrhosis, with only modest contributions from CVD and hepatocellular carcinoma.19 Furthermore, in contrast to what is found in Western population, cancer-related mortality is occasionally greater than CVD-related mortality in Asian populations.7,20 CVD events are significantly less common in Asians than in other ethnic groups, even though metabolic risk factors were found not to vary among ethnic groups.21 This is because each NAFLD-associated risk variant has a different effect on CVD and other metabolic phenotypes,22 and the frequency of genetic variants varies among ethnic groups.23,24 Together, these findings suggest that ethnic differences might affect the association between MAFLD and CVD incidence and CVD-related death.
There is a major concern that, compared to NAFLD, MAFLD includes a more heterogeneous group of patients, in that it does not distinguish alcoholic from nonalcoholic patients, non-obese (i.e., overweight) from obese patients, and patients with NAFLD alone from those with additional liver diseases, and is therefore not representative of the underlying pathophysiologic mechanisms of fatty liver disease.25 The current study confirmed that individuals with MAFLD were heterogeneous in the sense that rates of mortality and CVD in these subjects varied according to the accompanying metabolic dysfunctions. Furthermore, given that metabolic dysfunction26 and NAFLD-induced metabolic abnormalities18 may change over time, MAFLD status might have also changed over time in the current study. To improve the practical utility of MAFLD from a public health standpoint, further work in diverse populations is needed to establish the optimal combination of metabolic dysfunctions that should be included in the definition of MAFLD.
The present study had several limitations. First, mortality data were only available for the Ansung cohort. Nonetheless, we found that MAFLD significantly increased the risk of mortality even with a reduced number of subjects. Second, we used the FLI to define hepatic steatosis, although histological or radiological methods are more accurate. However, extensive data on the diagnostic and prognostic performance of the FLI indicate that it is an acceptable surrogate marker of hepatic steatosis for epidemiological studies.1,11,27-30 Conflicting reports on the optimal FLI cutoffs to define hepatic steatosis in Asians should be taken into account.29 In fact, if we had adopted FLI ≥30 to define hepatic steatosis, the prevalence of MAFLD and NAFLD would be 44.3% (3,947/8,919) and 36.8% (3,282/8,919), respectively. In this study, we analyzed the effect of MAFLD on the outcomes using FLI ≥30 as well as FLI ≥60. Third, we could not assess whether MAFLD or NAFLD affects the incidence or prognosis of certain type of cancer. Fourth, our data on CVD events were obtained by self-reports, and could therefore be affected by recall bias. For this reason, we conducted in-depth interviews to confirm CVD events, and excluded subjects with any history of CVD at baseline to eliminate residual confounding. Nonetheless, we used community-based prospective cohorts, extensively evaluated the metabolic risk factors, including insulin resistance and systemic inflammation, and successfully demonstrated that MAFLD was independently associated with mortality. The lack of an association of CVD with MAFLD after adjustment for diverse metabolic risk factors suggests that the association between MAFLD and CVD observed in unadjusted analysis was mainly due to metabolic dysfunction that accompanied MAFLD.
In conclusion, MAFLD independently increased overall mortality in a prospective, community-based cohort study during the median follow-up of 15.7 years. In particular, incident CVD events were mainly determined by the type of accompanying metabolic dysfunctions. Considering the heterogeneity in clinical outcomes of MAFLD according to the type of metabolic dysfunctions included in the current definition of MAFLD, further research to refine the definition of MAFLD is warranted to improve the predictability of the adverse outcomes in diverse populations. The present results also provide a basis for stimulating further research into the role of MAFLD in predicting long-term clinical outcomes including CVD and mortality.
SUPPLEMENTARY MATERIALS
Supplementary materials can be accessed at https://doi.org/10.5009/gnl210167.
ACKNOWLEDGEMENTS
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea Government (MEST) (2021R1A2C2005820, 2021M3A9E4021818, and 2021R1C1C1009875), the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI) funded by the Ministry of Health & Welfare, Republic of Korea (HI21C0538), the Research Program funded by the Korea Centers for Disease Control and Prevention (2001-347-6111-221, 2002-347-6111-221, 2003-347-6111-221, 2004-E71001-00, 2005-E71001-00, 2006-E71005-00, 2006-E71006-00, 2007-E71001-00, 2007-E71003-00, 2008-E71001-00, 2008-E71005-00, 2009-E71002-00, 2009-E71007-00, 2010-E71001-00, 2010-E71004-00, 2011-E71004-00, 2011-E71008-00, 2012-E71008-00, 2012-E71005-00, 2013-E71007-00, 2013-E71005-00, 2014-E71005-00, 2014-E71003-00, 2015-P71002-00, 2015-P71001-00, 2016-E71002-00, 2016-E71003-00, 2017-E71002-00, 2017-E71001-00, 2018-E7102-00, 2018-E7101-00).
The data are available from the corresponding author on reasonable request.
Footnotes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTIONS
Guarantor of article: N.H.C. Conception or design: J.H.M., W.K., B.K.K., N.H.C. Acquisition, analysis, or interpretation of data: J.H.M., W.K., B.K.K., N.H.C. Drafting the work or revising: J.H.M., W.K., B.K.K. Final approval of the manuscript: all authors.
REFERENCES
- 1.Eslam M, Newsome PN, Sarin SK, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020;73:202–209. doi: 10.1016/j.jhep.2020.03.039. [DOI] [PubMed] [Google Scholar]
- 2.Eslam M, Sarin SK, Wong VW, et al. The Asian Pacific Association for the Study of the Liver clinical practice guidelines for the diagnosis and management of metabolic associated fatty liver disease. Hepatol Int. 2020;14:889–919. doi: 10.1007/s12072-020-10094-2. [DOI] [PubMed] [Google Scholar]
- 3.Mak LY, Yuen MF, Seto WK. Letter regarding "A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement". J Hepatol. 2020;73:1573–1574. doi: 10.1016/j.jhep.2020.07.008. [DOI] [PubMed] [Google Scholar]
- 4.European Association for the Study of the Liver (EASL); European Association for the Study of Diabetes (EASD); European Association for the Study of Obesity (EASO), author EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64:1388–1402. doi: 10.1016/j.jhep.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 5.Targher G, Byrne CD, Lonardo A, Zoppini G, Barbui C. Non-alcoholic fatty liver disease and risk of incident cardiovascular disease: a meta-analysis. J Hepatol. 2016;65:589–600. doi: 10.1016/j.jhep.2016.05.013. [DOI] [PubMed] [Google Scholar]
- 6.Angulo P, Kleiner DE, Dam-Larsen S, et al. Liver fibrosis, but no other histologic features, is associated with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology. 2015;149:389–397. doi: 10.1053/j.gastro.2015.04.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim D, Kim WR, Kim HJ, Therneau TM. Association between noninvasive fibrosis markers and mortality among adults with nonalcoholic fatty liver disease in the United States. Hepatology. 2013;57:1357–1365. doi: 10.1002/hep.26156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee H, Lee YH, Kim SU, Kim HC. Metabolic dysfunction-associated fatty liver disease and incident cardiovascular disease risk: a nationwide cohort study. Clin Gastroenterol Hepatol. 2021;19:2138–2147. doi: 10.1016/j.cgh.2020.12.022. [DOI] [PubMed] [Google Scholar]
- 9.Kim Y, Han BG KoGES group, author. Cohort profile: the Korean Genome and Epidemiology Study (KoGES) consortium. Int J Epidemiol. 2017;46:e20. doi: 10.1093/ije/dyv316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67:328–357. doi: 10.1002/hep.29367. [DOI] [PubMed] [Google Scholar]
- 11.Bedogni G, Bellentani S, Miglioli L, et al. The fatty liver index: a simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol. 2006;6:33. doi: 10.1186/1471-230X-6-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McPherson S, Hardy T, Dufour JF, et al. Age as a confounding factor for the accurate non-invasive diagnosis of advanced NAFLD fibrosis. Am J Gastroenterol. 2017;112:740–751. doi: 10.1038/ajg.2016.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McPherson S, Stewart SF, Henderson E, Burt AD, Day CP. Simple non-invasive fibrosis scoring systems can reliably exclude advanced fibrosis in patients with non-alcoholic fatty liver disease. Gut. 2010;59:1265–1269. doi: 10.1136/gut.2010.216077. [DOI] [PubMed] [Google Scholar]
- 14.Yamamura S, Eslam M, Kawaguchi T, et al. MAFLD identifies patients with significant hepatic fibrosis better than NAFLD. Liver Int. 2020;40:3018–3030. doi: 10.1111/liv.14675. [DOI] [PubMed] [Google Scholar]
- 15.Liu Y, Zhong GC, Tan HY, Hao FB, Hu JJ. Nonalcoholic fatty liver disease and mortality from all causes, cardiovascular disease, and cancer: a meta-analysis. Sci Rep. 2019;9:11124. doi: 10.1038/s41598-019-47687-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koo BK, Allison MA, Criqui MH, Denenberg JO, Wright CM. The association between liver fat and systemic calcified atherosclerosis. J Vasc Surg. 2020;71:204–211. doi: 10.1016/j.jvs.2019.03.044. [DOI] [PubMed] [Google Scholar]
- 17.Haffner SM, Lehto S, Rönnemaa T, Pyörälä K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med. 1998;339:229–234. doi: 10.1056/NEJM199807233390404. [DOI] [PubMed] [Google Scholar]
- 18.Adams LA, Lymp JF, St Sauver J, et al. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology. 2005;129:113–121. doi: 10.1053/j.gastro.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 19.Simon TG, Roelstraete B, Khalili H, Hagström H, Ludvigsson JF. Mortality in biopsy-confirmed nonalcoholic fatty liver disease: results from a nationwide cohort. Gut. 2021;70:1375–1382. doi: 10.1136/gutjnl-2020-322786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hwang YC, Ahn HY, Park SW, Park CY. Nonalcoholic fatty liver disease associates with increased overall mortality and death from cancer, cardiovascular disease, and liver disease in women but not men. Clin Gastroenterol Hepatol. 2018;16:1131–1137. doi: 10.1016/j.cgh.2017.11.026. [DOI] [PubMed] [Google Scholar]
- 21.DeFilippis AP, Young R, McEvoy JW, et al. Risk score overestimation: the impact of individual cardiovascular risk factors and preventive therapies on the performance of the American Heart Association-American College of Cardiology-Atherosclerotic Cardiovascular Disease risk score in a modern multi-ethnic cohort. Eur Heart J. 2017;38:598–608. doi: 10.1093/eurheartj/ehw301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Simons N, Isaacs A, Koek GH, Kuč S, Schaper NC, Brouwers MCGJ. PNPLA3, TM6SF2, and MBOAT7 genotypes and coronary artery disease. Gastroenterology. 2017;152:912–913. doi: 10.1053/j.gastro.2016.12.020. [DOI] [PubMed] [Google Scholar]
- 23.Mancina RM, Dongiovanni P, Petta S, et al. The MBOAT7-TMC4 variant rs641738 increases risk of nonalcoholic fatty liver disease in individuals of European descent. Gastroenterology. 2016;150:1219–1230. doi: 10.1053/j.gastro.2016.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Koo BK, Joo SK, Kim D, et al. Additive effects of PNPLA3 and TM6SF2 on the histological severity of non-alcoholic fatty liver disease. J Gastroenterol Hepatol. 2018;33:1277–1285. doi: 10.1111/jgh.14056. [DOI] [PubMed] [Google Scholar]
- 25.Younossi ZM, Rinella ME, Sanyal AJ, et al. From NAFLD to MAFLD: implications of a premature change in terminology. Hepatology. 2021;73:1194–1198. doi: 10.1002/hep.31420. [DOI] [PubMed] [Google Scholar]
- 26.Cho YK, Kang YM, Yoo JH, et al. Implications of the dynamic nature of metabolic health status and obesity on risk of incident cardiovascular events and mortality: a nationwide population-based cohort study. Metabolism. 2019;97:50–56. doi: 10.1016/j.metabol.2019.05.002. [DOI] [PubMed] [Google Scholar]
- 27.Wong VW, Chan WK, Chitturi S, et al. Asia-Pacific working party on non-alcoholic fatty liver disease guidelines 2017-part 1: definition, risk factors and assessment. J Gastroenterol Hepatol. 2018;33:70–85. doi: 10.1111/jgh.13857. [DOI] [PubMed] [Google Scholar]
- 28.Khang AR, Lee HW, Yi D, Kang YH, Son SM. The fatty liver index, a simple and useful predictor of metabolic syndrome: analysis of the Korea National Health and Nutrition Examination Survey 2010-2011. Diabetes Metab Syndr Obes. 2019;12:181–190. doi: 10.2147/DMSO.S189544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huang X, Xu M, Chen Y, et al. Validation of the fatty liver index for nonalcoholic fatty liver disease in middle-aged and elderly Chinese. Medicine (Baltimore) 2015;94:e1682. doi: 10.1097/MD.0000000000001682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xu Z, Li H, Tian S, et al. Blood biomarkers for the diagnosis of hepatic steatosis in metabolic dysfunction-associated fatty liver disease. J Hepatol. 2020;73:1264–1265. doi: 10.1016/j.jhep.2020.06.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.