Abstract
It has been found that soluble epoxide hydrolase (sEH; encoded by the EPHX2 gene) in the metabolism of polyunsaturated fatty acids (PUFAs) plays a key role in inflammation, which, in turn, plays a part in the pathogenesis of neuropsychiatric disorders. Meanwhile, epoxy fatty acids such as epoxyeicosatrienoic acids (EETs), epoxyeicosatetraenoic acids (EEQs), and epoxyeicosapentaenoic acids (EDPs) have been found to exert neuroprotective effects in animal models of neuropsychiatric disorders through potent anti-inflammatory actions. Soluble expoxide hydrolase, an enzyme present in all living organisms, metabolizes epoxy fatty acids into the corresponding dihydroxy fatty acids, which are less active than the precursors. In this regard, preclinical findings using sEH inhibitors or Ephx2 knock-out (KO) mice have indicated that the inhibition or deficiency of sEH can have beneficial effects in several models of neuropsychiatric disorders. Thus, this review discusses the current findings of the role of sEH in neuropsychiatric disorders, including depression, autism spectrum disorder (ASD), schizophrenia, Parkinson’s disease (PD), and stroke, as well as the potential mechanisms underlying the therapeutic effects of sEH inhibitors.
Keywords: autism spectrum disorder, depression, inflammation, Parkinson’s disease, schizophrenia, soluble epoxide hydrolase, stroke
1. Introduction
Neuropsychiatric disorders, including depression, autism spectrum disorder (ASD), schizophrenia, and Parkinson’s disease (PD), are common brain diseases characterized by cognitive deficits, psychiatric symptoms, and somatoform symptoms [1]. Meanwhile, psychiatric disorders such as depression, ASD, and schizophrenia are cumulatively common and show a remarkable increase of prevalence in young people [2,3]. Moreover, according to the 2019 Global Burden of Diseases, Injuries, and Risk Factors Study (GBD), psychiatric disorders are among the leading causes of the global health-related burden [4]. This burden was generally high across the entire lifespan for both genders and across many locations [5].
In 2020, as COVID-19 spread throughout the world, the increasing SARS-CoV-2 infection rates and decreasing human mobility contributed to a significant increase in the prevalence of neuropsychiatric disorders [6]. Neurological disorders, including PD, Alzheimer’s disease, and stroke, have also become a major public health challenge, due to the decreased quality of life and increased burden for millions of patients and their caregivers [7]. Although several approved drugs have been used to eliminate some symptoms in patients with neuropsychiatric disorders, the development of new therapeutic drugs for such disorders must occur to meet the medical needs of individuals [8,9,10,11,12].
In general, fatty acids are the major products of lipid metabolism [13]. Additionally, polyunsaturated fatty acids (PUFAs) are essential dietary fats that include more than one double bond and are classified based on the number of carbon atoms located between the first double bond of the carbon chain and the terminal methyl end [14,15]. In particular, PUFAs in the n-3 and n-6 (omega-3 and omega-6) families play a prominent role in biological function as components of cell membranes, membrane fluidity regulation, membrane-associated proteins, and neurotransmission [16]. Increasing evidence has shown that inadequate diets or metabolic deficiencies can cause low levels of n-3 PUFAs, which are related to the etiologies of various neuropsychiatric disorders such as PD, schizophrenia, depression, and attention deficit hyperactivity disorder [14,17,18,19].
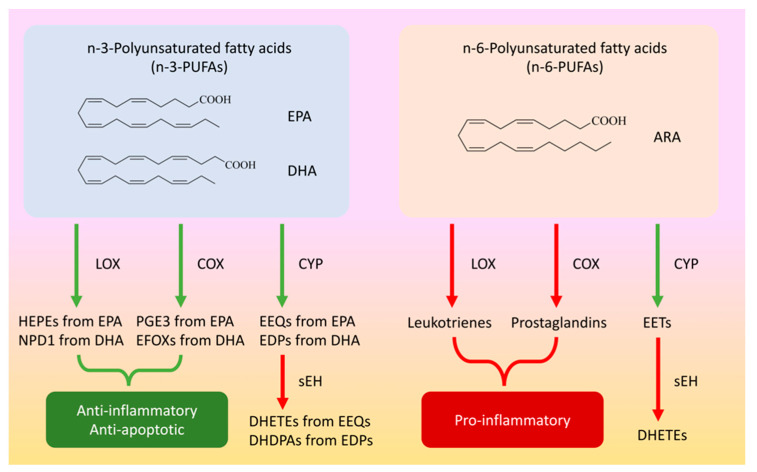
The biologically important long-chain PUFAs include docosahexaenoic acid (DHA or 22:6 n-3) (see Figure 1), which represents approximately 40% of central PUFAs. Such acids contribute to neural cell signaling, membrane fatty acid chain fluidity, ion permeability, and protein function [20,21]. At the cerebral level of the n-6 family, roughly 50% of PUFAs are represented by arachidonic acid (ARA, 20:4 n-6) (see Figure 1), which plays a role in signaling, memory, and learning modulation [22,23]. Another important lipid is eicosapentaenoic acid (EPA, 20:5 n-3) (see Figure 1), whose concentration is significantly lower in the central nervous system. It also stands out for its anti-inflammatory properties, which can have neuroprotective impacts on the brain [24,25].
Figure 1.
Metabolism of eicosapentaenoic acid (EPA), docosohexaenoic acid (DHA), and arachidonic acid (ARA). Eicosapentaenoic acid (EPA) is converted into hydroxyeicosapentaenoic acids (HEPEs) and prostaglandin E3 (PGE3) through the lipoxygenase (LOX) and cyclooxygenase (COX) pathways, respectively. Docosohexaenoic acid (DHA) is also converted into neuroprotectin D1 (NPD1) and electrophile oxo-derivatives (EFOXs) through the LOX and COX pathways, respectively. The compounds HEPEs, NPD1, PGE3, and EFOXs act as anti-inflammatory and anti-apoptotic mediators, while EPA and DHA are converted into epoxyeicosatetraenoic acids (EEQs) and epoxydocosapentaenoic acids (EDPs) through the cytochrome P450 (CYP) pathway, respectively. Moreover, these epoxide fatty acids are metabolized into their corresponding diols (DHETEs and DHDPAs) by soluble epoxide hydrolase (sEH), while arachidonic acid (ARA) is converted into leukotrienes and prostaglandins by the LOX and COX pathways, respectively. Finally, ARA is converted into epoxyeicosatrienoic acids (EETs) by the CYP pathway, and these EETs are metabolized into their corresponding diols (DHETs) by sEH. In this case, epoxy fatty acids (EEQs, EDPs, and EETs) have anti-inflammatory effects.
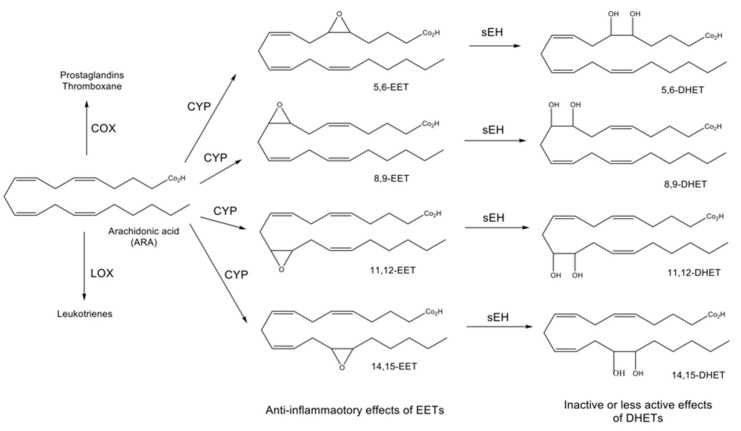
Specifically, PUFAs are metabolized into bioactive derivatives by main enzymes such as cyclooxygenases (COXs), lipoxygenases (LOXs), and cytochrome P450s (CYPs) (see Figure 1) [26,27,28], whereas EPA is converted into hydroxyeicosapentaenoic acids (HEPEs) and prostaglandin E3 (PGE3) through the LOX and COX pathways, respectively. Moreover, neuroprotectin D1 (NPD1) and electrophile oxo-derivatives (EFOXs) are synthesized from DHA through the LOX and COX pathways, respectively. These mediators such as HEPEs, PGE3, NPD1, and EFOXs act as anti-apoptotic protein activators and suppress inflammatory gene expression (see Figure 1) [14]. EPA and DHA are also converted into epoxyeicosatetraenoic acids (EEQs) and epoxydocosapentaenoic acids (EDPs) through the CYP pathway, respectively. These epoxide fatty acids are then metabolized into their corresponding diols (DHETEs and DHDPAs) by soluble epoxide hydrolase (sEH: coded by the EPHX2 gene). For example, 19,20-epoxydocosapentaenoic acid (19,20-EDP) synthesized from DHA through the CYP pathway is metabolized into 19,20-dihydroxydocosapentaenoic acid (19,20-DHDPA) by sEH [29,30]. ARA is also metabolized by the COX and LOX pathways to create a class of compounds known as leukotrienes and prostaglandins, which are important signaling molecules that control pro-inflammatory actions (see Figure 1 and Figure 2) [26,27,31]. Furthermore, the CYP pathway generates epoxyeicosatrienoic acids (EETs) from ARA, and EETs are metabolized into dihydroxyeicosatrienoic acids (DHETs) by sEH (see Figure 1 and Figure 2) [26,27,32].
Figure 2.
Roles of CYP and sEH in the arachidonic acid (ARA) cascade. In addition to the COX and LOX pathways, ARA is metabolized into four epoxyeicosatrienoic acids (EETs) through the cytochrome P450 (CYP) pathway. EETs are then metabolized into the corresponding dihydroxyeicosatetraenoic acids (DHETs) by soluble epoxide hydrolase (sEH). EETs have anti-inflammatory effects, while DHETs are inactive or have fewer active effects.
Since DHETs dramatically reduce biologic activity, sEH inhibitors have been extensively used to prolong the anti-inflammatory function of EETs in the ARA cascade [33,34]. Such inhibitors have also been shown to decrease sEH activity, with little to no toxicity in animal models [35,36]. Meanwhile, inflammatory cytokines and chemokines are found in various neurobiological pathways which are related to neuropsychiatric disorders [37]. Overall, it is likely that sEH plays a role in the pathogenesis of psychiatric and neurological disorders. Thus, this review discusses the role of sEH in neuropsychiatric disorders such as depression, autism spectrum disorder (ASD), schizophrenia, Parkinson’s disease (PD), and stroke as well as the potential mechanisms underlying the therapeutic effects of sEH inhibitors.
2. Depression
According to the 2021 Global Health Data Exchange, depression is one of the most common psychiatric disorders in the world, with an estimated 3.8% of the population affected, including 5.0% of adults and 5.7% of adults 60 years and older [38]. Current antidepressants such as selective serotonin reuptake inhibitors or serotonin–norepinephrine reuptake inhibitors can take several weeks before they are effective. Since approximately one-third of patients with depression do not respond to current antidepressants, new antidepressants must be developed for such treatment-resistant patients [27,39,40]. Moreover, numerous studies have suggested a strong association between inflammatory processes and the pathophysiology of depression [41,42,43,44,45,46,47].
The cytochrome P450 epoxygenase CYP2J2 converts ARA into four regioisomeric EETs (see Figure 2), while systemic overexpression of human CYP2J2 reduces the increased plasma levels of inflammatory cytokines and decreased levels of the anti-inflammatory mediator interleukin-10 (IL-10) after injection of tumor necrosis factor-α (TNF-α) [48]. In addition, the increase of inflammatory protein in TNF-α treated human bronchi is suppressed by 14,15-EET [49]. These findings suggest that the decrease of EETs metabolized by sEH can aggravate inflammation in the brain. Hence, regarding inflammation in depression, sEH is likely to play a crucial role [27,39].
In a related study, the expression of sEH protein in the brain was higher in a sample of susceptible mice after chronic social defeat stress (CSDS) compared to the control mice [50]. Other findings from the study were as follows. First, the expression of sEH protein was higher in the postmortem brain samples of patients with depression compared to those of the controls [50]. Second, pretreatment with the sEH inhibitor TPPU [1-(1-propionylpiperidin-4-yl)-3-(4-(trifluoromethoxy) phenyl) urea] prevented the onset of depression-like behaviors after CSDS. Third, the sample of Ephx2 KO mice did not show depression-like behaviors after CSDS, suggesting stress resilience [50]. Interestingly, fecal microbiota transplantation from CSDS-susceptible mice with depression-like phenotype produced such a phenotype in antibiotic-treated Ephx2 KO mice, indicating that the administration of “depression-related microbes” can contribute to the conversion of resilient Ephx2 KO mice into KO mice with depression-like phenotype [51]. Altogether, these results suggest that sEH plays a key role in the pathophysiology of depression and that sEH inhibitors can be potential therapeutic or prophylactic drugs for depression [27,39,50].
The downregulation of hepatic sEH in mice caused a reduction in sucrose preference and coat deterioration compared with the control group [52]. Moreover, patients with depression showed higher levels of sEH protein in the parietal cortex and liver compared to those in the control group [53]. Thus, it is likely that the brain–liver axis plays a role in depression [52,53,54].
Immunoreactivity of sEH was also detected in astrocytes throughout the brain [55], whereas sEH activity in the astrocytes of the medial prefrontal cortex (PFC) of CSDS-susceptible mice was negatively correlated with depression-like behaviors [56]. Moreover, a recent study showed that sEH in the central nucleus of the amygdala regulates anxiety-related behaviors [57], while TPPU produced antidepressant-like effects in the lipopolysaccharide (LPS)-induced inflammation model of depression and in the CSDS model [50]. However, the antidepressant-like effects of TPPU were blocked by the tropomyosin receptor kinase B (TrkB) antagonist, indicating that brain-derived neurotrophic factor (BDNF)-TrkB signaling plays a certain role in the antidepressant-like effects of TPPU [58,59].
In other research, pretreatment with TPPU attenuated the increase of pro-inflammatory cytokine IL-1β and rescued neuronal and dendritic spine loss in the hippocampus by increasing the expression of the N-methyl-D-aspartate receptor, the extracellular-signal-regulated kinase (ERK)1/2, and the CREB (cAMP response element binding protein) [60]. In the LiCl-pilocarpine-induced post-status epilepticus rat model, TPPU attenuated spontaneous recurrent seizures and epilepsy-associated depression-like behaviors through anti-inflammatory effects [61], while co-treatment with TPPU, EPA, and DHA was more effective in preventing IL-1β, IL-6, and TNF-α-induced decreased neurogenesis and increased apoptosis [62]. Furthermore, the serum levels of sEH-derived fatty acid diols increased in depressed patients with type 2 diabetes mellitus, while depressive symptom severity was associated with the oxylipin profile [63], suggesting higher activity of sEH in these patients. In sum, increased activity of sEH most likely plays a role in the pathogenesis of depression and suggests that sEH inhibitors are potential antidepressants [27,39,64,65,66,67].
3. ASD and Schizophrenia
Accumulating evidence has suggested that maternal immune activation (MIA) such as maternal infection can increase the risk of neuropsychiatric disorders (e.g., ASD and schizophrenia) in offspring [68,69,70,71,72,73,74,75]. A meta-analysis also showed a strong relationship between maternal infection during pregnancy and the increased risk of ASD in offspring [76]. It was also pointed out that the COVID-19 pandemic may increase the risk of ASD and schizophrenia in offspring after maternal infection of SARS-CoV-2 [77,78,79].
Meanwhile, MIA using poly(I:C) has been widely used as animal models of ASD and schizophrenia [80,81]. For example, using rodents, there were higher levels of sEH and decreased levels of epoxy fatty acids (i.e., 10,11-EDP, 5,6-EET, 8,9-EET, 11,12-EET) in the PFC of juvenile offspring after MIA, indicating increased activity of sEH in the PFC of juvenile offspring after MIA [82]. The expression of EPHX2 mRNA in induced pluripotent stem cell-derived neurospheres was higher among schizophrenia patients than the controls [82]. There was also a higher expression of EPHX2 mRNA in the postmortem brain samples of ASD patients than that of the controls [82]. Additionally, the levels of sEH in the parietal cortex from schizophrenia patients were higher than those of the controls [50,53]. Collectively, neuroinflammation by the increased expression of sEH most likely plays a role in the pathogenesis of ASD and schizophrenia.
In related research, repeated treatment with TPPU in juvenile offspring from prenatal days P28 to P56 prevented cognitive deficits and loss of parvalbumin (PV)-immunoreactivity in the medial PFC of adult offspring, especially after MIA [82]. Additionally, treatment with TPPU in pregnant mothers from E5 to P21 prevented cognitive deficits, social interaction deficits, and PV-immunoreactivity in the medial PFC of juvenile offspring after MIA. Altogether, increased activity of sEH in the brain can contribute to ASD (or schizophrenia)-like behavioral abnormalities in offspring after MIA.
Epidemiological studies have suggested that exposure to herbicides (i.e., glyphosate) during pregnancy might increase the risk of ASD in offspring. For instance, a population-based case study in California (USA) reported that the risk of ASD was associated with the use of glyphosate (odds ratio = 1.16) [83]. It was also found that maternal glyphosate exposure during pregnancy and lactation caused ASD-like behavioral abnormalities, an increase of expression of sEH in the PFC, hippocampus, and striatum of juvenile offspring, and a decrease of PV-immunoreactivity in the prelimbic of the medial PFC of juvenile mice [84,85]. In addition, the levels of 8,9-EET in the blood and brain regions (i.e., PFC, hippocampus, and striatum) of juvenile offspring after maternal glyphosate exposure were lower than those of the control groups, indicating increased expression of sEH in the brain regions [84]. Moreover, oral administration of TPPU to pregnant mothers from E5 to P21 prevented ASD-like behaviors such as social interaction deficits and increased grooming time in the juvenile offspring after maternal glyphosate exposure. Collectively, increased sEH in the brain seems to play a role in the pathogenesis of ASD after maternal glyphosate exposure [84,85,86].
Finally, the potent sEH inhibitor AS2586114 improved schizophrenia-like behavioral abnormalities (e.g., hyperlocomotion and pre-pulse inhibition deficits) in a sample of phencyclidine (PCP)-treated mice, suggesting that sEH inhibitor might have antipsychotic-like activity [87]. Furthermore, TPPU in drinking water during the juvenile and adolescent stages of offspring can also prevent the onset of cognitive deficits and a reduction of PV-immunoreactivity in the medial PFC of adult offspring after MIA [82]. Repeated treatment with TPPU from pregnancy to weaning can also prevent the onset of cognitive deficits in juvenile offspring after MIA or maternal glyphosate exposure [82,84]. Overall, these findings indicate that sEH plays a key role in the development of ASD and schizophrenia in offspring after MIA and that sEH inhibitors can have prophylactic or therapeutic impacts on neuropsychiatric disorders [10,88,89].
4. Parkinson’s Disease
Parkinson’s disease (PD) is a neurodegenerative disease characterized by the deposition of the aggregates of α-synuclein (termed “Lewy bodies”) and the loss of dopaminergic neurons in the substantia nigra (SN), which results in motor dysfunction and non-motor dysfunction [90,91,92]. PD is the second most prevalent neurodegenerative disorder, only after Alzheimer’s disease. It is also predicted that the number of patients with PD will double over the next 20 years [93]. Meanwhile, L-DOPA (the precursor of dopamine) or dopamine (DA) receptor agonists have been used in the treatment of PD [94]. Although these treatments seem to alleviate symptoms, there are no disease-modifying or neuroprotective drugs for PD [95,96,97].
Multiple evidence has supported neuroinflammation-related oxidative stress in the pathogenesis of PD [66,98,99,100]. Related research has shown that activated astrocytes and microglia caused by brain immune response are involved in the development of neuroinflammatory features, leading to the exacerbation of DA neurons in the substantia nigra pars compacta (SNc) [101]. In addition, EETs, regulators of inflammation processes, can produce the neurotrophic role of astrocytes, increase the release of BDNF, reduce glutamatergic toxicity through the astrocytic metabotropic glutamate receptor mGluR5, prevent mitochondrial dysfunction and apoptosis, and protect synaptic function in the brain [100,102,103,104].
MPTP (1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine)-induced neurotoxicity in the striatum and SNc of a sample of rodents has been a well-established preclinical in vivo model to study the pathogenesis of PD [105,106]. Higher expression of the sEH protein in the striatum has also been found in MPTP-treated mice or postmortem brain samples from dementia patients with Lewy bodies [107]. Moreover, the expression of the EPHX2 mRNA in human PARK2 (Parkinson’s disease protein 2) iPSC-derived neurons were significantly higher compared to the control groups [107], while the levels of 8,9-EET in the striatum of MPTP-treated mice were lower than those of the control mice, suggesting higher activity of sEH in the striatum of the MPTP-treated mice [107]. Interestingly, sEH expression was positively correlated to the phosphorylation of α-synuclein in the striatum of the MPTP-treated mice [107]. Since PD may not display symptoms until approximately 80% of the striatal DA has been lost, a biomarker for earlier diagnosis is important for finding treatment options [108]. In this regard, peripheral detection of elevated levels of sEH in the gut, which is possible prior to the losses of dopaminergic neurons, may potentially provide an early biomarker of PD [95,108].
MPTP-induced neurotoxicity in the striatum and SN, including the loss of the DA transporter (DAT), loss of tyrosine hydrolase (TH)-positive cells, and increased endoplasmic reticulum (ER) stress, was attenuated by repeated oral administration of TPPU [107]. Additionally, both AUDA [12-(((tricyclo(3.3.1.13,7)dec-1-ylamino)carbonyl)amino)-dodecanoic acid], another sEH inhibitor, and sEH deficiency significantly protected against MPTP-induced toxicity [109,110]. A recent study found that the natural compound kurarinone, an uncompetitive inhibitor of sEH, can alleviate the MPTP-induced behavioral deficits, dopaminergic neurotoxicity, and neuroinflammation via suppressing the activated microglia, including the nuclear factor kappa B (NF-κB) signaling pathway [111]. Furthermore, the inhibition of sEH can suppress the aggregation of α-synuclein, microglia activation, neuroinflammation, and apoptosis, resulting in the neuroprotection activity in the PD model [112,113]. Altogether, increased sEH and the resulting increase in phosphorylation of α-synuclein may play a role in the pathogenesis of PD and that sEH inhibitors can be potential drugs for PD.
5. Stroke
Stroke, constituting a loss of blood flow to the brain, is the leading cause of disability and death worldwide. In fact, the global prevalence of stroke in 2019 alone was 101.5 million people [114]. Acute episodes, including ischemic strokes, hemorrhagic strokes, traumatic brain injury, and seizures, can cause neuroinflammation in the brain, resulting in the loss of neurons and activation of resident immune cells [92]. Subsequent activation of immune responses can increase pro-inflammatory cytokines [115] and compromise the brain-blood barrier (BBB), further deteriorating neurodegeneration and exacerbating the injury caused by stroke [116].
Despite extensive efforts to discover better therapies for stroke, treatment options are still limited. The primary current treatment for ischemic stroke is thrombolysis with the tissue plasminogen activator (tPA), which was approved by the Food and Drug Administration. However, it must be administered within a relatively short time window before neuronal loss occurs [117]. While the tPA can be effective for patients with ischemic stroke, it can also aggravate hemorrhagic strokes, which include similar clinical symptoms with ischemia [118]. Thus, developing a therapy that focuses on a single agent that targets multiple mechanisms of ischemic brain injury may prove more effective [119].
As for sEH, it catalyzes the metabolism of EETs, which exhibit potentially beneficial actions in stroke via vasodilation, neuroprotection, promotion of angiogenesis, suppression of platelet aggregation, oxidative stress, and post-ischemic inflammation [120]. In related research, hypertension- and diabetes-associated ischemic stroke risk increased through the EPHX2 gene variants in the Turkish population [121]. Moreover, serum oxylipin changes consistent with higher sEH activity played a key role in vascular cognitive impairment, which is associated with the injury of periventricular subcortical white matter [122]. Collectively, sEH inhibition is a potential intervention for stroke patients based on the beneficial properties of EETs.
The inhibition of sEH is also effective for reducing infarct volume, improving memory deficits, and alleviating cognitive impairment and microvasculature augmentation by suppressing neuroinflammation and increasing reparative cytokines and growth factors such as BDNF and doublecortin [123,124,125]. Regarding BDNF, it activates the receptor TrkB to promote the growth and differentiation of nerve cells and to have a neuroprotective effect on the neurons. Thus, a blockade of the BDNF-TrkB signaling pathway by the TrkB inhibitor ANA-12 can abolish the protective effect of sEH gene deletion in the middle cerebral arterial occlusion (MCAO) models of stroke [126], suggesting the role of BDNF-TrkB signaling in the actions of sEH inhibitors.
Finally, administration of TPPU or AUDA significantly promoted M2 polarization of microglial cells, which indicates a shift from pro-inflammatory polarized microglia to microglia that primarily release anti-inflammatory cytokines. This can result in the differentiation of oligodendrocytes, protection against white matter integrity, and remyelination against chronic hypoperfusion [127,128,129,130,131]. Interestingly, treatment with t-AUCB (a sEH inhibitor) after ischemic stroke onset has been shown to exert brain protection in a sample of non-diabetic mice, but not in type 2 diabetes mellitus (DM2) mice, while DM2-induced hyperglycemia can abolish t-AUCB-mediated neuroprotection against stroke [132]. SMTP-7 targeting sEH has also been shown to be effective in treating severe embolic stroke in a sample of monkeys under conditions in which tPA treatment causes hemorrhagic infarct-associated premature death [133,134]. Furthermore, related research has shown that treatment with the sEH inhibitor can decrease the activity of matrix metalloproteases (MMP)-2 and MMP-9, increase the expression of tight junction proteins, reduce activation of NF-κB, and suppress the apoptosis to protect the BBB integrity from ischemia [135,136]. Altogether, these studies suggest that sEH inhibition can have multi-target protective effects and alleviate cognitive impairment after a stroke.
6. Conclusions and Future Perspectives
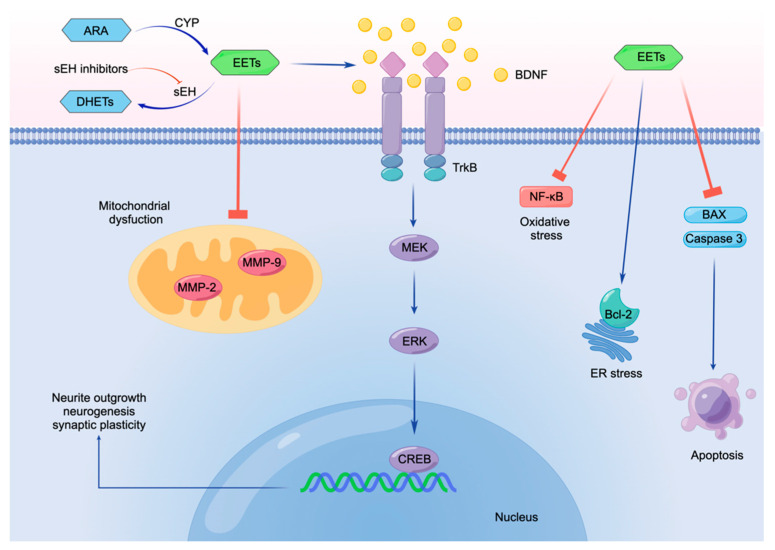
As discussed in this review, sEH inhibitors can exert a neuroprotective effect through potent anti-inflammatory actions, including BDNF-TrkB activation for inflammation-related endoplasmic reticulum stress and mitochondrial dysfunction (Figure 3). For example, EETs suppress the MMP-2 and MMP-9, resulting in the prevention of mitochondrial dysfunction. Furthermore, EETs induce the expression of BDNF which binds to its receptor TrkB, resulting in the MEK–ERK–CREB signaling pathway [45,137]. BDNF–TrkB–MEK–ERK–CREB pathway could contribute to neurite outgrowth, neurogenesis, and synaptic plasticity. Furthermore, EETs could reduce oxidative stress and ER stress through suppression of NF-kB and activation of Bcl-2, respectively. In addition, EETs can protect against apoptosis through suppression of the BAX (Bxcl-2-associated X protein) and caspase-3 (see Figure 3). Thus, it is likely that sEH inhibitors can potentially serve as prophylactic or therapeutic drugs for neuropsychiatric disorders such as depression, ASD, schizophrenia, PD, and stroke.
Figure 3.
Molecular mechanisms underlying the neuroprotective effect of EETs. EETs suppress the MMP-2 and MMP-9 to prevent mitochondrial dysfunction. EETs induce the expression of BDNF, then stimulate BDNF-TrkB signaling. Subsequently, BDNF-TrkB signaling stimulates the MEK–ERK–CREB signaling pathway, promoting neurite outgrowth, neurogenesis, and synaptic plasticity. Furthermore, EETs reduce oxidative stress and suppress ER stress through suppression of NF-kB and activation of Bcl-2, respectively. Moreover, EETs protect against apoptosis through suppressing the BAX and Caspase-3; MMP-2: matrix metalloproteinase-2; MMP-9: matrix metalloproteinase-9; BDNF: brain derived neurotrophic factor; TrkB: tropomyosin receptor kinase B; MEK: mitogen-activated protein kinase; ERK: extracellular signal-regulated kinase; CREB: cAMP response element binding protein; ER: endoplasmic reticulum; NF-κB: nuclear factor kappa-light-chain-enhancer of activated B cells; Bcl-2: B-cell lymphoma 2; BAX: Bcl-2-associated X protein. Made by Figdraw (www.figdraw.com, accessed on 24 March 2022).
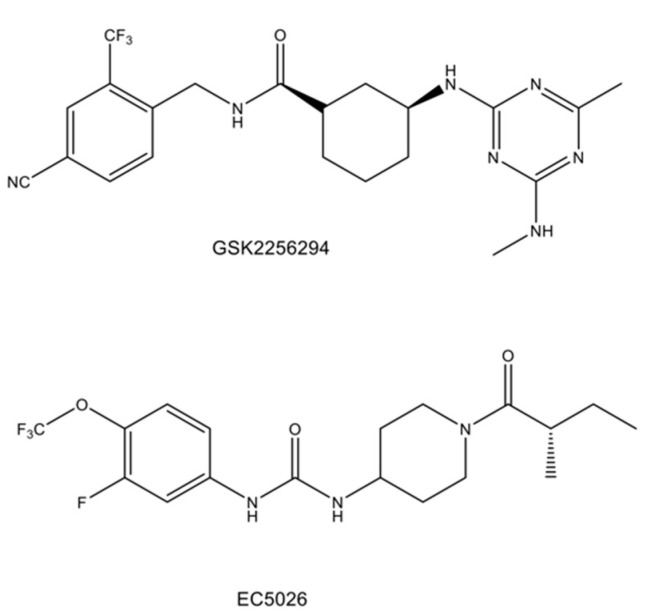
Currently, clinical studies using two sEH inhibitors (i.e., GSK2256294 and EC5026) (see Figure 4) in humans are underway [138]. For instance, a recent randomized, double-blind, placebo-controlled study found that treatment with GSK2256294 for seven days in a sample of subjects with obesity and prediabetes (n = 16) effectively inhibited sEH activity in plasma, muscle, and adipose tissue. Although it reduced F2-isoprostanes (a marker of oxidative stress), it did not improve insulin sensitivity or blood pressure [139]. Moreover, a double-blind, randomized placebo-controlled trial indicated that treatment with GSK2256294 for 10 days in a sample of patients (n = 10) with aneurysmal subarachnoid hemorrhage resulted in a considerable increase in the serum EET/DHET ratio at days 7 and 10 but not in the cerebrospinal fluid (CSF) [140]. Conversely, there was decreased CSF inflammatory cytokines following GSK2256294 treatment, but it did not achieve statistical significance [140]. These clinical studies showed that treatment with GSK2256294 can cause an increase in the EET/DHET ratio of blood and tissue through potent sEH inhibition in humans. Furthermore, although a clinical trial of EC5026 in humans is underway by EicOsis Human Health Inc. (Davis, CA, USA) [138], future randomized, double-blind, placebo-control studies using a large sample size are necessary for determining the efficacy of sEH inhibitors in patients with neuropsychiatric disorders.
Figure 4.
Chemical structure of GSK2256294 and EC5026 for human use.
Acknowledgments
The authors would like to than our collaborators who are listed as the co-authors of our papers in the reference list.
Author Contributions
Conceptualization, J.S. and K.H.; writing—original draft preparation, J.S.; writing—review and editing, K.H.; visualization, K.H.; supervision, K.H.; project administration, K.H.; funding acquisition, K.H. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Funding Statement
This research was funded by Japan Society for the Promotion of Science, grant number 21H02846 (to K.H.), 21H00184 (to K.H.) and 21H05612 (to K.H.).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cheng L., Liu J., Chen Z. The histaminergic system in neuropsychiatric disorders. Biomolecules. 2021;11:1345. doi: 10.3390/biom11091345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bray N.J., O’Donovan M.C. The genetics of neuropsychiatric disorders. Brain Neurosci. Adv. 2018;2:2398212818799271. doi: 10.1177/2398212818799271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kessler R.C., Amminger G.P., Aguilar-Gaxiola S., Alonso J., Lee S., Ustun T.B. Age of onset of mental disorders: A review of recent literature. Curr. Opin. Psychiatry. 2007;20:359. doi: 10.1097/YCO.0b013e32816ebc8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.GBD 2019 Diseases and Injuries Collaborators Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.GBD 2019 Diseases and Injuries Collaborators Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9:137–150. doi: 10.1016/S2215-0366(21)00395-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.COVID-19 Mental Disorders Collaborators Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398:1700–1712. doi: 10.1016/S0140-6736(21)02143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gooch C.L., Pracht E., Borenstein A.R. The burden of neurological disease in the United States: A summary report and call to action. Ann. Neurol. 2017;81:479–484. doi: 10.1002/ana.24897. [DOI] [PubMed] [Google Scholar]
- 8.Hashimoto K., Malchow B., Falkai P., Schmitt A. Glutamate modulators as potential therapeutic drugs in schizophrenia and affective disorders. Eur. Arch. Psychiatry Clin. Neurosci. 2013;263:367–377. doi: 10.1007/s00406-013-0399-y. [DOI] [PubMed] [Google Scholar]
- 9.Hashimoto K. Targeting of NMDA receptors in new treatments for schizophrenia. Expert Opin. Ther. Targets. 2014;18:1049–1063. doi: 10.1517/14728222.2014.934225. [DOI] [PubMed] [Google Scholar]
- 10.Hashimoto K. Recent advances in the early intervention in schizophrenia: Future direction from preclinical findings. Curr. Psychiatry Rep. 2019;21:75. doi: 10.1007/s11920-019-1063-7. [DOI] [PubMed] [Google Scholar]
- 11.LeWitt P.A., Chaudhuri K.R. Unmet needs in Parkinson disease: Motor and non-motor. Park. Relat. Disord. 2020;80((Suppl. 1)):S7–S12. doi: 10.1016/j.parkreldis.2020.09.024. [DOI] [PubMed] [Google Scholar]
- 12.Grosso Jasutkar H., Oh S.E., Mouradian M.M. Therapeutics in the pipeline targeting alpha-synuclein for Parkinson’s disease. Pharmacol. Rev. 2022;74:207–237. doi: 10.1124/pharmrev.120.000133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mongan D., Healy C., Jones H.J., Zammit S., Cannon M., Cotter D.R. Plasma polyunsaturated fatty acids and mental disorders in adolescence and early adulthood: Cross-sectional and longitudinal associations in a general population cohort. Transl. Psychiatry. 2021;11:321. doi: 10.1038/s41398-021-01425-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Healy-Stoffel M., Levant B. N-3 (Omega-3) fatty acids: Effects on brain dopamine systems and potential role in the etiology and treatment of neuropsychiatric disorders. CNS Neurol. Disord. Drug Targets. 2018;17:216–232. doi: 10.2174/1871527317666180412153612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Morgese M.G., Schiavone S., Mhillaj E., Bove M., Tucci P., Trabace L. N-3 PUFA diet enrichment prevents amyloid beta-induced depressive-like phenotype. Pharmacol. Res. 2018;129:526–534. doi: 10.1016/j.phrs.2017.11.034. [DOI] [PubMed] [Google Scholar]
- 16.Dagnino-Subiabre A. Stress and Western diets increase vulnerability to neuropsychiatric disorders: A common mechanism. Nutr. Neurosci. 2021;24:624–634. doi: 10.1080/1028415X.2019.1661651. [DOI] [PubMed] [Google Scholar]
- 17.Tesei A., Crippa A., Ceccarelli S.B., Mauri M., Molteni M., Agostoni C., Nobile M. The potential relevance of docosahexaenoic acid and eicosapentaenoic acid to the etiopathogenesis of childhood neuropsychiatric disorders. Eur. Child Adolesc. Psychiatry. 2017;26:1011–1030. doi: 10.1007/s00787-016-0932-4. [DOI] [PubMed] [Google Scholar]
- 18.Daray F.M., Grendas L.N., Rodante D.E., Errasti A.E., Cases G.G., Moix C.F., Uicich R.E., GimÉNez M.I., Puppo S., Fasolino G.H., et al. Polyunsaturated fatty acids as predictors of future suicide attempt. Prostaglandins Leukot. Essent. Fat. Acids. 2021;165:102247. doi: 10.1016/j.plefa.2021.102247. [DOI] [PubMed] [Google Scholar]
- 19.Di Miceli M., Bosch-Bouju C., Layé S. PUFA and their derivatives in neurotransmission and synapses: A new hallmark of synaptopathies. Proc. Nutr. Soc. 2020;79:388–403. doi: 10.1017/S0029665120000129. [DOI] [PubMed] [Google Scholar]
- 20.Chen W., Chen Y., Wu R., Guo G., Liu Y., Zeng B., Liao X., Wang Y., Wang X. DHA alleviates diet-induced skeletal muscle fiber remodeling via FTO/m6A/DDIT4/PGC1α signaling. BMC Biol. 2022;20:39. doi: 10.1186/s12915-022-01239-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Díaz M., Mesa-Herrera F., Marín R. DHA and its elaborated modulation of antioxidant defenses of the brain: Implications in aging and AD neurodegeneration. Antioxidants. 2021;10:907. doi: 10.3390/antiox10060907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Funk Colin D. Prostaglandins and leukotrienes: Advances in eicosanoid biology. Science. 2001;294:1871–1875. doi: 10.1126/science.294.5548.1871. [DOI] [PubMed] [Google Scholar]
- 23.Orr S.K., Bazinet R.P. The emerging role of docosahexaenoic acid in neuroinflammation. Curr. Opin. Investig. Drugs. 2008;9:735–743. [PubMed] [Google Scholar]
- 24.Borsini A., Stangl D., Jeffries A.R., Pariante C.M., Thuret S. The role of omega-3 fatty acids in preventing glucocorticoid-induced reduction in human hippocampal neurogenesis and increase in apoptosis. Transl. Psychiatry. 2020;10:219. doi: 10.1038/s41398-020-00908-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Giacobbe J., Benoiton B., Zunszain P., Pariante C.M., Borsini A. The anti-inflammatory role of omega-3 polyunsaturated fatty acids metabolites in pre-clinical models of psychiatric, neurodegenerative, and neurological disorders. Front. Psychiatry. 2020;11:122. doi: 10.3389/fpsyt.2020.00122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Morisseau C., Hammock B.D. Impact of soluble epoxide hydrolase and epoxyeicosanoids on human health. Annu. Rev. Pharmacol. Toxicol. 2013;53:37–58. doi: 10.1146/annurev-pharmtox-011112-140244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hashimoto K. Role of soluble epoxide hydrolase in metabolism of PUFAs in psychiatric and neurological disorders. Front. Pharmacol. 2019;10:36. doi: 10.3389/fphar.2019.00036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Imig J.D., Cervenka L., Neckar J. Epoxylipids and soluble epoxide hydrolase in heart diseases. Biochem. Pharmacol. 2022;195:114866. doi: 10.1016/j.bcp.2021.114866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Capozzi M.E., Hammer S.S., McCollum G.W., Penn J.S. Epoxygenated fatty acids inhibit retinal vascular inflammation. Sci. Rep. 2016;6:39211. doi: 10.1038/srep39211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yanai R., Mulki L., Hasegawa E., Takeuchi K., Sweigard H., Suzuki J., Gaissert P., Vavvas D.G., Sonoda K.H., Rothe M., et al. Cytochrome P450-generated metabolites derived from ω-3 fatty acids attenuate neovascularization. Proc. Natl. Acad. Sci. USA. 2014;111:9603–9608. doi: 10.1073/pnas.1401191111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang B., Wu L., Chen J., Dong L., Chen C., Wen Z., Hu J., Fleming I., Wang D.W. Metabolism pathways of arachidonic acids: Mechanisms and potential therapeutic targets. Signal Transduct. Target. Ther. 2021;6:94. doi: 10.1038/s41392-020-00443-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dos Santos L.R., Fleming I. Role of cytochrome P450-derived, polyunsaturated fatty acid mediators in diabetes and the metabolic syndrome. Prostaglandins Other Lipid Mediat. 2020;148:106407. doi: 10.1016/j.prostaglandins.2019.106407. [DOI] [PubMed] [Google Scholar]
- 33.Hiesinger K., Wagner K.M., Hammock B.D., Proschak E., Hwang S.H. Development of multitarget agents possessing soluble epoxide hydrolase inhibitory activity. Prostaglandins Other Lipid Mediat. 2019;140:31–39. doi: 10.1016/j.prostaglandins.2018.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hildreth K., Kodani S.D., Hammock B.D., Zhao L. Cytochrome P450-derived linoleic acid metabolites EpOMEs and DiHOMEs: A review of recent studies. J. Nutr. Biochem. 2020;86:108484. doi: 10.1016/j.jnutbio.2020.108484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jones R.D., Liao J., Tong X., Xu D., Sun L., Li H., Yang G.Y. Epoxy-oxylipins and soluble epoxide hydrolase metabolic pathway as targets for NSAID-induced gastroenteropathy and inflammation-associated carcinogenesis. Front. Pharmacol. 2019;10:731. doi: 10.3389/fphar.2019.00731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sun C.P., Zhang X.Y., Morisseau C., Hwang S.H., Zhang Z.J., Hammock B.D., Ma X.C. Discovery of soluble epoxide hydrolase inhibitors from chemical synthesis and natural products. J. Med. Chem. 2021;64:184–215. doi: 10.1021/acs.jmedchem.0c01507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Abdoli A., Taghipour A., Pirestani M., Mofazzal Jahromi M.A., Roustazadeh A., Mir H., Ardakani H.M., Kenarkoohi A., Falahi S., Karimi M. Infections, inflammation, and risk of neuropsychiatric disorders: The neglected role of “co-infection”. Heliyon. 2020;6:e05645. doi: 10.1016/j.heliyon.2020.e05645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Institute of Health Metrics and Evaluation, Global Health Datta Exchange. [(accessed on 1 May 2021)]. Available online: http://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2019-permalink/d780dffbe8a381b25e1416884959e88b.
- 39.Hashimoto K. Soluble epoxide hydrolase: A new therapeutic target for depression. Expert Opin. Ther. Targets. 2016;20:1149–1151. doi: 10.1080/14728222.2016.1226284. [DOI] [PubMed] [Google Scholar]
- 40.Hashimoto K. Molecular mechanisms of the rapid-acting and long-lasting antidepressant actions of (R)-ketamine. Biochem. Pharmacol. 2020;177:113935. doi: 10.1016/j.bcp.2020.113935. [DOI] [PubMed] [Google Scholar]
- 41.Hashimoto K. Inflammatory biomarkers as differential predictors of antidepressant response. Int. J. Mol. Sci. 2015;16:7796–7801. doi: 10.3390/ijms16047796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhang J.C., Yao W., Hashimoto K. Brain-derived neurotrophic factor (BDNF)-TrkB signaling in inflammation-related depression and potential therapeutic targets. Curr. Neuropharmacol. 2016;14:721–731. doi: 10.2174/1570159X14666160119094646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Troubat R., Barone P., Leman S., Desmidt T., Cressant A., Atanasova B., Brizard B., El Hage W., Surget A., Belzung C., et al. Neuroinflammation and depression: A review. Eur. J. Neurosci. 2021;53:151–171. doi: 10.1111/ejn.14720. [DOI] [PubMed] [Google Scholar]
- 44.Carlessi A.S., Borba L.A., Zugno A.I., Quevedo J., Réus G.Z. Gut microbiota–brain axis in depression: The role of neuroinflammation. Eur. J. Neurosci. 2021;53:222–235. doi: 10.1111/ejn.14631. [DOI] [PubMed] [Google Scholar]
- 45.Wei Y., Chang L., Hashimoto K. Molecular mechanisms underlying the antidepressant actions of arketamine: Beyond the NMDA receptor. Mol. Psychiatry. 2021;27:559–573. doi: 10.1038/s41380-021-01121-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chang L., Wei Y., Hashimoto K. Brain-gut-microbiota axis in depression: A historical overview and future directions. Brain Res. Bull. 2022;182:44–56. doi: 10.1016/j.brainresbull.2022.02.004. [DOI] [PubMed] [Google Scholar]
- 47.Wei Y., Wang T., Liao L., Fan X., Chang L., Hashimoto K. Brain-spleen axis in health and diseases: A review and future perspective. Brain Res. Bull. 2022;182:130–140. doi: 10.1016/j.brainresbull.2022.02.008. [DOI] [PubMed] [Google Scholar]
- 48.Zhao G., Tu L., Li X., Yang S., Chen C., Xu X., Wang P., Wang D.W. Delivery of AAV2-CYP2J2 protects remnant kidney in the 5/6-nephrectomized rat via inhibition of apoptosis and fibrosis. Hum. Gene Ther. 2012;23:688–699. doi: 10.1089/hum.2011.135. [DOI] [PubMed] [Google Scholar]
- 49.Morin C., Sirois M., Echave V., Gomes M.M., Rousseau E. EET displays anti-inflammatory effects in TNF-α–stimulated human bronchi. Am. J. Respir. Cell Mol. Biol. 2008;38:192–201. doi: 10.1165/rcmb.2007-0232OC. [DOI] [PubMed] [Google Scholar]
- 50.Ren Q., Ma M., Ishima T., Morisseau C., Yang J., Wagner K.M., Zhang J.C., Yang C., Yao W., Dong C., et al. Gene deficiency and pharmacological inhibition of soluble epoxide hydrolase confers resilience to repeated social defeat stress. Proc. Natl. Acad. Sci. USA. 2016;113:E1944–E1952. doi: 10.1073/pnas.1601532113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang S., Ishima T., Qu Y., Shan J., Chang L., Wei Y., Zhang J., Pu Y., Fujita Y., Tan Y., et al. Ingestion of Faecalibaculum rodentium causes depression-like phenotypes in resilient Ephx2 knock-out mice: A role of brain-gut-microbiota axis via the subdiaphragmatic vagus nerve. J. Affect. Disord. 2021;292:565–573. doi: 10.1016/j.jad.2021.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Qin X.H., Wu Z., Dong J.H., Zeng Y.N., Xiong W.C., Liu C., Wang M.Y., Zhu M.Z., Chen W.J., Zhang Y., et al. Liver soluble epoxide hydrolase regulates behavioral and cellular effects of chronic stress. Cell Rep. 2019;29:3223–3234.e6. doi: 10.1016/j.celrep.2019.11.006. [DOI] [PubMed] [Google Scholar]
- 53.Zhang J., Tan Y., Chang L., Hammock B.D., Hashimoto K. Increased expression of soluble epoxide hydrolase in the brain and liver from patients with major psychiatric disorders: A role of brain–liver axis. J. Affect. Disord. 2020;270:131–134. doi: 10.1016/j.jad.2020.03.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yang B., Ren Q., Zhang J.C., Chen Q.X., Hashimoto K. Altered expression of BDNF, BDNF pro-peptide and their precursor proBDNF in brain and liver tissues from psychiatric disorders: Rethinking the brain-liver axis. Transl. Psychiatry. 2017;7:e1128. doi: 10.1038/tp.2017.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Marowsky A., Burgener J., Falck J.R., Fritschy J.M., Arand M. Distribution of soluble and microsomal epoxide hydrolase in the mouse brain and its contribution to cerebral epoxyeicosatrienoic acid metabolism. Neuroscience. 2009;163:646–661. doi: 10.1016/j.neuroscience.2009.06.033. [DOI] [PubMed] [Google Scholar]
- 56.Xiong W., Cao X., Zeng Y., Qin X., Zhu M., Ren J., Wu Z., Huang Q., Zhang Y., Wang M., et al. Astrocytic epoxyeicosatrienoic acid signaling in the medial prefrontal cortex modulates depressive-like behaviors. J. Neurosci. 2019;39:4606. doi: 10.1523/JNEUROSCI.3069-18.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ren J., Lu C.L., Huang J., Fan J., Guo F., Mo J.W., Huang W.Y., Kong P.L., Li X.W., Sun L.R., et al. A distinct metabolically defined central nucleus circuit bidirectionally controls anxiety-related behaviors. J. Neurosci. 2022;42:2356–2370. doi: 10.1523/JNEUROSCI.1578-21.2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wu Q., Cai H., Song J., Chang Q. The effects of sEH inhibitor on depression-like behavior and neurogenesis in male mice. J. Neurosci. Res. 2017;95:2483–2492. doi: 10.1002/jnr.24080. [DOI] [PubMed] [Google Scholar]
- 59.Wu Q., Song J., Meng D., Chang Q. TPPU, a sEH inhibitor, attenuates corticosterone-induced PC12 cell injury by modulation of BDNF-TrkB pathway. J. Mol. Neurosci. 2019;67:364–372. doi: 10.1007/s12031-018-1230-z. [DOI] [PubMed] [Google Scholar]
- 60.Peng W., Shen Y., Wang Q., Ding J., Wang X. TPPU Pre-treatment rescues dendritic spine loss and alleviates depressive behaviours during the latent period in the lithium chloride-pilocarpine-induced status epilepticus rat model. Brain Sci. 2021;11:1465. doi: 10.3390/brainsci11111465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Shen Y., Peng W., Chen Q., Hammock B.D., Liu J., Li D., Yang J., Ding J., Wang X. Anti-inflammatory treatment with a soluble epoxide hydrolase inhibitor attenuates seizures and epilepsy-associated depression in the LiCl-pilocarpine post-status epilepticus rat model. Brain Behav. Immun. 2019;81:535–544. doi: 10.1016/j.bbi.2019.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Borsini A., Nicolaou A., Camacho-Muñoz D., Kendall A.C., Di Benedetto M.G., Giacobbe J., Su K.P., Pariante C.M. Omega-3 polyunsaturated fatty acids protect against inflammation through production of LOX and CYP450 lipid mediators: Relevance for major depression and for human hippocampal neurogenesis. Mol. Psychiatry. 2021;26:6773–6788. doi: 10.1038/s41380-021-01160-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Anita N.Z., Forkan N., Kamal R., Nguyen M.M., Yu D., Major-Orfao C., Wong S.K., Lanctôt K.L., Herrmann N., Oh P.I., et al. Serum soluble epoxide hydrolase related oxylipins and major depression in patients with type 2 diabetes. Psychoneuroendocrinology. 2021;126:105149. doi: 10.1016/j.psyneuen.2021.105149. [DOI] [PubMed] [Google Scholar]
- 64.Swardfager W., Hennebelle M., Yu D., Hammock B.D., Levitt A.J., Hashimoto K., Taha A.Y. Metabolic/inflammatory/vascular comorbidity in psychiatric disorders; soluble epoxide hydrolase (sEH) as a possible new target. Neurosci. Biobehav. Rev. 2018;87:56–66. doi: 10.1016/j.neubiorev.2018.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ren Q. Soluble epoxide hydrolase inhibitor: A novel potential therapeutic or prophylactic drug for psychiatric disorders. Front. Pharmacol. 2019;10:420. doi: 10.3389/fphar.2019.00420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Atone J., Wagner K., Hashimoto K., Hammock B.D. Cytochrome P450 derived epoxidized fatty acids as a therapeutic tool against neuroinflammatory diseases. Prostaglandins Other Lipid Mediat. 2020;147:106385. doi: 10.1016/j.prostaglandins.2019.106385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Borsini A. The role of soluble epoxide hydrolase and its inhibitors in depression. Brain Behav. Immun. Health. 2021;16:100325. doi: 10.1016/j.bbih.2021.100325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bilbo S.D., Block C.L., Bolton J.L., Hanamsagar R., Tran P.K. Beyond infection—Maternal immune activation by environmental factors, microglial development, and relevance for autism spectrum disorders. Exp. Neurol. 2018;299:241–251. doi: 10.1016/j.expneurol.2017.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Brown A.S., Meyer U. maternal immune activation and neuropsychiatric illness: A translational research perspective. Am. J. Psychiatry. 2018;175:1073–1083. doi: 10.1176/appi.ajp.2018.17121311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lombardo M.V., Moon H.M., Su J., Palmer T.D., Courchesne E., Pramparo T. Maternal immune activation dysregulation of the fetal brain transcriptome and relevance to the pathophysiology of autism spectrum disorder. Mol. Psychiatry. 2018;23:1001–1013. doi: 10.1038/mp.2017.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Solek C.M., Farooqi N., Verly M., Lim T.K., Ruthazer E.S. Maternal immune activation in neurodevelopmental disorders. Dev. Dyn. 2018;247:588–619. doi: 10.1002/dvdy.24612. [DOI] [PubMed] [Google Scholar]
- 72.Conway F., Brown A.S. Maternal immune activation and related factors in the risk of offspring psychiatric disorders. Front. Psychiatry. 2019;10:430. doi: 10.3389/fpsyt.2019.00430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Siniscalco D., Schultz S., Brigida A.L., Antonucci N. Inflammation and neuro-immune dysregulations in autism spectrum disorders. Pharmaceuticals. 2018;11:56. doi: 10.3390/ph11020056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Matta S.M., Hill-Yardin E.L., Crack P.J. The influence of neuroinflammation in autism spectrum disorder. Brain Behav. Immun. 2019;79:75–90. doi: 10.1016/j.bbi.2019.04.037. [DOI] [PubMed] [Google Scholar]
- 75.Gevezova M., Sarafian V., Anderson G., Maes M. Inflammation and mitochondrial dysfunction in autism spectrum disorder. CNS Neurol. Disord. Drug Targets. 2020;19:320–333. doi: 10.2174/1871527319666200628015039. [DOI] [PubMed] [Google Scholar]
- 76.Jiang H.Y., Xu L.l., Shao L., Xia R.M., Yu Z.H., Ling Z.X., Yang F., Deng M., Ruan B. Maternal infection during pregnancy and risk of autism spectrum disorders: A systematic review and meta-analysis. Brain Behav. Immun. 2016;58:165–172. doi: 10.1016/j.bbi.2016.06.005. [DOI] [PubMed] [Google Scholar]
- 77.Hashimoto K. Risk of neuropsychiatric disorders in offspring of COVID-19-infected pregnant women and nutritional intervention. Eur. Arch. Psychiatry Clin. Neurosci. 2021;271:387–389. doi: 10.1007/s00406-020-01148-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lins B. Maternal immune activation as a risk factor for psychiatric illness in the context of the SARS-CoV-2 pandemic. Brain Behav. Immun. Health. 2021;16:100297. doi: 10.1016/j.bbih.2021.100297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hashimoto Y., Suzuki T., Hashimoto K. Mechanisms of action of fluvoxamine for COVID-19: A historical review. Mol. Psychiatry. 2022:1–10. doi: 10.1038/s41380-021-01432-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Guma E., Plitman E., Chakravarty M.M. The role of maternal immune activation in altering the neurodevelopmental trajectories of offspring: A translational review of neuroimaging studies with implications for autism spectrum disorder and schizophrenia. Neurosci. Biobehav. Rev. 2019;104:141–157. doi: 10.1016/j.neubiorev.2019.06.020. [DOI] [PubMed] [Google Scholar]
- 81.Haddad F.L., Patel S.V., Schmid S. Maternal immune activation by poly(I:C) as a preclinical model for neurodevelopmental disorders: A focus on autism and schizophrenia. Neurosci. Biobehav. Rev. 2020;113:546–567. doi: 10.1016/j.neubiorev.2020.04.012. [DOI] [PubMed] [Google Scholar]
- 82.Ma M., Ren Q., Yang J., Zhang K., Xiong Z., Ishima T., Pu Y., Hwang S.H., Toyoshima M., Iwayama Y., et al. Key role of soluble epoxide hydrolase in the neurodevelopmental disorders of offspring after maternal immune activation. Proc. Natl. Acad. Sci. USA. 2019;116:7083–7088. doi: 10.1073/pnas.1819234116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.von Ehrenstein O.S., Ling C., Cui X., Cockburn M., Park A.S., Yu F., Wu J., Ritz B. Prenatal and infant exposure to ambient pesticides and autism spectrum disorder in children: Population based case-control study. BMJ. 2019;364:l962. doi: 10.1136/bmj.l962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Pu Y., Yang J., Chang L., Qu Y., Wang S., Zhang K., Xiong Z., Zhang J., Tan Y., Wang X., et al. Maternal glyphosate exposure causes autism-like behaviors in offspring through increased expression of soluble epoxide hydrolase. Proc. Natl. Acad. Sci. USA. 2020;117:11753–11759. doi: 10.1073/pnas.1922287117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pu Y., Ma L., Shan J., Wan X., Hammock B.D., Hashimoto K. Autism-like behaviors in male juvenile offspring after maternal glyphosate exposure. Clin. Psychopharmacol. Neurosci. 2021;19:554–558. doi: 10.9758/cpn.2021.19.3.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hashimoto K., Hammock B.D. Reply to Reeves and Dunn: Risk for autism in offspring after maternal glyphosate exposure. Proc. Natl. Acad. Sci. USA. 2021;118:e2016496118. doi: 10.1073/pnas.2016496118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ma M., Ren Q., Fujita Y., Ishima T., Zhang J.C., Hashimoto K. Effects of AS2586114, a soluble epoxide hydrolase inhibitor, on hyperlocomotion and prepulse inhibition deficits in mice after administration of phencyclidine. Pharmacol. Biochem. Behav. 2013;110:98–103. doi: 10.1016/j.pbb.2013.06.005. [DOI] [PubMed] [Google Scholar]
- 88.Iyer M.R., Kundu B., Wood C.M. Soluble epoxide hydrolase inhibitors: An overview and patent review from the last decade. Expert Opin. Ther. Pat. 2022;12:1–19. doi: 10.1080/13543776.2022.2054329. [DOI] [PubMed] [Google Scholar]
- 89.Hashimoto K. Understanding the link between maternal infections and neurodevelopmental disorders in offspring: The role of abnormalities in metabolism of polyunsaturated fatty acids. Brain Behav. Immun. 2019;81:4–5. doi: 10.1016/j.bbi.2019.07.010. [DOI] [PubMed] [Google Scholar]
- 90.Kalia L.V., Lang A.E. Parkinson’s disease. Lancet. 2015;386:896–912. doi: 10.1016/S0140-6736(14)61393-3. [DOI] [PubMed] [Google Scholar]
- 91.Ascherio A., Schwarzschild M.A. The epidemiology of Parkinson’s disease: Risk factors and prevention. Lancet Neurol. 2016;15:1257–1272. doi: 10.1016/S1474-4422(16)30230-7. [DOI] [PubMed] [Google Scholar]
- 92.Kodani S.D., Morisseau C. Role of epoxy-fatty acids and epoxide hydrolases in the pathology of neuro-inflammation. Biochimie. 2019;159:59–65. doi: 10.1016/j.biochi.2019.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Chen J.J. Parkinson’s disease: Health-related quality of life, economic cost, and implications of early treatment. Am. J. Manag. Care. 2010;16:S87–S93. [PubMed] [Google Scholar]
- 94.Zarriello S., Tuazon J.P., Corey S., Schimmel S., Rajani M., Gorsky A., Incontri D., Hammock B.D., Borlongan C.V. Humble beginnings with big goals: Small molecule soluble epoxide hydrolase inhibitors for treating CNS disorders. Prog. Neurobiol. 2019;172:23–39. doi: 10.1016/j.pneurobio.2018.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Borlongan C.V. Fatty acid chemical mediator provides insights into the pathology and treatment of Parkinson’s disease. Proc. Natl. Acad. Sci. USA. 2018;115:6322–6324. doi: 10.1073/pnas.1807276115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Dehay B., Bourdenx M., Gorry P., Przedborski S., Vila M., Hunot S., Singleton A., Olanow C.W., Merchant K.M., Bezard E. Targeting α-synuclein for treatment of Parkinson’s disease: Mechanistic and therapeutic considerations. Lancet Neurol. 2015;14:855–866. doi: 10.1016/S1474-4422(15)00006-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Bloem B.R., Okun M.S., Klein C. Parkinson’s disease. Lancet. 2021;397:2284–2303. doi: 10.1016/S0140-6736(21)00218-X. [DOI] [PubMed] [Google Scholar]
- 98.Hirsch E.C., Hunot S. Neuroinflammation in Parkinson’s disease: A target for neuroprotection? Lancet Neurol. 2009;8:382–397. doi: 10.1016/S1474-4422(09)70062-6. [DOI] [PubMed] [Google Scholar]
- 99.Hirsch E.C., Standaert D.G. Ten unresolved questions about neuroinflammation in Parkinson’s disease. Mov. Disord. 2021;36:16–24. doi: 10.1002/mds.28075. [DOI] [PubMed] [Google Scholar]
- 100.Pallàs M., Vázquez S., Sanfeliu C., Galdeano C., Griñán-Ferré C. Soluble epoxide hydrolase inhibition to face neuroinflammation in Parkinson’s disease: A new therapeutic strategy. Biomolecules. 2020;10:703. doi: 10.3390/biom10050703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wang Q., Liu Y., Zhou J. Neuroinflammation in Parkinson’s disease and its potential as therapeutic target. Transl. Neurodegener. 2015;4:19. doi: 10.1186/s40035-015-0042-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Liu L., Chen C., Gong W., Li Y., Edin M.L., Zeldin D.C., Wang D.W. Epoxyeicosatrienoic acids attenuate reactive oxygen species level, mitochondrial dysfunction, caspase activation, and apoptosis in carcinoma cells treated with arsenic trioxide. J. Pharmacol. Exp. Ther. 2011;339:451. doi: 10.1124/jpet.111.180505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Yuan L., Liu J., Dong R., Zhu J., Tao C., Zheng R., Zhu S. 14,15-epoxyeicosatrienoic acid promotes production of brain derived neurotrophic factor from astrocytes and exerts neuroprotective effects during ischaemic injury. Neuropathol. App. Neurobiol. 2016;42:607–620. doi: 10.1111/nan.12291. [DOI] [PubMed] [Google Scholar]
- 104.Kuo Y.M., Hsu P.C., Hung C.C., Hu Y.Y., Huang Y.J., Gan Y.L., Lin C.H., Shie F.S., Chang W.K., Kao L.S. Soluble epoxide hydrolase inhibition attenuates excitotoxicity involving 14,15-epoxyeicosatrienoic acid–mediated astrocytic survival and plasticity to preserve glutamate homeostasis. Mol. Neurobiol. 2019;56:8451–8474. doi: 10.1007/s12035-019-01669-8. [DOI] [PubMed] [Google Scholar]
- 105.Sedelis M., Schwarting R.K.W., Huston J.P. Behavioral phenotyping of the MPTP mouse model of Parkinson’s disease. Behav. Brain Res. 2001;125:109–125. doi: 10.1016/S0166-4328(01)00309-6. [DOI] [PubMed] [Google Scholar]
- 106.Jackson-Lewis V., Przedborski S. Protocol for the MPTP mouse model of Parkinson’s disease. Nat. Protoc. 2007;2:141–151. doi: 10.1038/nprot.2006.342. [DOI] [PubMed] [Google Scholar]
- 107.Ren Q., Ma M., Yang J., Nonaka R., Yamaguchi A., Ishikawa K., Kobayashi K., Murayama S., Hwang S.H., Saiki S., et al. Soluble epoxide hydrolase plays a key role in the pathogenesis of Parkinson’s disease. Proc. Natl. Acad. Sci. USA. 2018;115:E5815–E5823. doi: 10.1073/pnas.1802179115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Marsden C.D. Parkinson’s disease. Lancet. 1990;335:948–949. doi: 10.1016/0140-6736(90)91006-V. [DOI] [PubMed] [Google Scholar]
- 109.Qin X., Wu Q., Lin L., Sun A., Liu S., Li X., Cao X., Gao T., Luo P., Zhu X., et al. Soluble epoxide hydrolase deficiency or inhibition attenuates MPTP-induced Parkinsonism. Mol. Neurobiol. 2015;52:187–195. doi: 10.1007/s12035-014-8833-3. [DOI] [PubMed] [Google Scholar]
- 110.Huang H.J., Wang Y.T., Lin H.C., Lee Y.H., Lin A.M.Y. Soluble epoxide hydrolase inhibition attenuates MPTP-induced neurotoxicity in the nigrostriatal dopaminergic system: Involvement of α-synuclein aggregation and ER stress. Mol. Neurobiol. 2018;55:138–144. doi: 10.1007/s12035-017-0726-9. [DOI] [PubMed] [Google Scholar]
- 111.Sun C.P., Zhou J.J., Yu Z.L., Huo X.K., Zhang J., Morisseau C., Hammock B.D., Ma X.C. Kurarinone alleviated Parkinson’s disease via stabilization of epoxyeicosatrienoic acids in animal model. Proc. Natl. Acad. Sci. USA. 2022;119:e2118818119. doi: 10.1073/pnas.2118818119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Lakkappa N., Krishnamurthy P.T., Pandareesh M.D., Hammock B.D., Hwang S.H. Soluble epoxide hydrolase inhibitor, APAU, protects dopaminergic neurons against rotenone induced neurotoxicity: Implications for Parkinson’s disease. Neurotoxicology. 2019;70:135–145. doi: 10.1016/j.neuro.2018.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Lakkappa N., Krishnamurthy P.T., Yamjala K., Hwang S.H., Hammock B.D., Babu B. Evaluation of antiparkinson activity of PTUPB by measuring dopamine and its metabolites in Drosophila melanogaster: LC–MS/MS method development. J. Pharm. Biomed. Anal. 2018;149:457–464. doi: 10.1016/j.jpba.2017.11.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Virani S.S., Alonso A., Aparicio H.J., Benjamin E.J., Bittencourt M.S., Callaway C.W., Carson A.P., Chamberlain A.M., Cheng S., Delling F.N., et al. Heart Disease and Stroke Statistics-2021 update: A report from the American Heart Association. Circulation. 2021;143:e254–e743. doi: 10.1161/CIR.0000000000000950. [DOI] [PubMed] [Google Scholar]
- 115.Chamorro Á., Meisel A., Planas A.M., Urra X., van de Beek D., Veltkamp R. The immunology of acute stroke. Nat. Rev. Neurol. 2012;8:401–410. doi: 10.1038/nrneurol.2012.98. [DOI] [PubMed] [Google Scholar]
- 116.Emsley H.C.A., Smith C.J., Gavin C.M., Georgiou R.F., Vail A., Barberan E.M., Hallenbeck J.M., del Zoppo G.J., Rothwell N.J., Tyrrell P.J., et al. An early and sustained peripheral inflammatory response in acute ischaemic stroke: Relationships with infection and atherosclerosis. J. Neuroimmunol. 2003;139:93–101. doi: 10.1016/S0165-5728(03)00134-6. [DOI] [PubMed] [Google Scholar]
- 117.Adeoye O., Hornung R., Khatri P., Kleindorfer D. Recombinant tissue-type plasminogen activator use for ischemic stroke in the United States. Stroke. 2011;42:1952–1955. doi: 10.1161/STROKEAHA.110.612358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Nor A.M., Ford G.A. Misdiagnosis of stroke. Expert Rev. Neurother. 2007;7:989–1001. doi: 10.1586/14737175.7.8.989. [DOI] [PubMed] [Google Scholar]
- 119.Iliff J.J., Alkayed N.J. Soluble epoxide hydrolase inhibition: Targeting multiple mechanisms of ischemic brain injury with a single agent. Future Neurol. 2009;4:179–199. doi: 10.2217/14796708.4.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Zhang W., Iliff J.J., Campbell C.J., Wang R.K., Hurn P.D., Alkayed N.J. Role of soluble epoxide hydrolase in the sex-specific vascular response to cerebral ischemia. J. Cereb. Blood Flow Metab. 2009;29:1475–1481. doi: 10.1038/jcbfm.2009.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Demirdöğen B.C., Miçooğulları Y., Özçelik A.T., Adalı O. Missense genetic polymorphisms of microsomal (EPHX1) and soluble epoxide hydrolase (EPHX2) and their relation to the risk of large artery atherosclerotic ischemic stroke in a Turkish population. Neuropsychiatr. Dis. Treat. 2020;16:3251. doi: 10.2147/NDT.S233992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Yu D., Hennebelle M., Sahlas D.J., Ramirez J., Gao F., Masellis M., Cogo-Moreira H., Swartz R.H., Herrmann N., Chan P.C., et al. Soluble epoxide hydrolase-derived linoleic acid oxylipins in serum are associated with periventricular white matter hyperintensities and vascular cognitive impairment. Transl. Stroke Res. 2019;10:522–533. doi: 10.1007/s12975-018-0672-5. [DOI] [PubMed] [Google Scholar]
- 123.Matin N., Fisher C., Lansdell T.A., Hammock B.D., Yang J., Jackson W.F., Dorrance A.M. Soluble epoxide hydrolase inhibition improves cognitive function and parenchymal artery dilation in a hypertensive model of chronic cerebral hypoperfusion. Microcirculation. 2021;28:e12653. doi: 10.1111/micc.12653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Hao J., Chen Y., Yao E., Liu X. Soluble epoxide hydrolase inhibition alleviated cognitive impairments via NRG1/ErbB4 signaling after chronic cerebral hypoperfusion induced by bilateral carotid artery stenosis in mice. Brain Res. 2018;1699:89–99. doi: 10.1016/j.brainres.2018.07.002. [DOI] [PubMed] [Google Scholar]
- 125.Tu R., Armstrong J., Lee K.S.S., Hammock B.D., Sapirstein A., Koehler R.C. Soluble epoxide hydrolase inhibition decreases reperfusion injury after focal cerebral ischemia. Sci. Rep. 2018;8:5279. doi: 10.1038/s41598-018-23504-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Chang L.H., Lin H.C., Huang S.S., Chen I.C., Chu K.W., Chih C.L., Liang Y.W., Lee Y.C., Chen Y.Y., Lee Y.H., et al. Blockade of soluble epoxide hydrolase attenuates post-ischemic neuronal hyperexcitation and confers resilience against stroke with TrkB activation. Sci. Rep. 2018;8:118. doi: 10.1038/s41598-017-18558-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Taguchi N., Nakayama S., Tanaka M. Single administration of soluble epoxide hydrolase inhibitor suppresses neuroinflammation and improves neuronal damage after cardiac arrest in mice. Neurosci. Res. 2016;111:56–63. doi: 10.1016/j.neures.2016.05.002. [DOI] [PubMed] [Google Scholar]
- 128.Wang J., Fujiyoshi T., Kosaka Y., Raybuck J.D., Lattal K.M., Ikeda M., Herson P.S., Koerner I.P. Inhibition of soluble epoxide hydrolase after cardiac arrest/cardiopulmonary resuscitation induces a neuroprotective phenotype in activated microglia and improves neuronal survival. J. Cereb. Blood Flow Metab. 2013;33:1574–1581. doi: 10.1038/jcbfm.2013.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Chen Y., Tian H., Yao E., Tian Y., Zhang H., Xu L., Yu Z., Fang Y., Wang W., Du P., et al. Soluble epoxide hydrolase inhibition promotes white matter integrity and long-term functional recovery after chronic hypoperfusion in mice. Sci. Rep. 2017;7:7758. doi: 10.1038/s41598-017-08227-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Yeh C.F., Chuang T.Y., Hung Y.W., Lan M.Y., Tsai C.H., Huang H.X., Lin Y.Y. Soluble epoxide hydrolase inhibition enhances anti-inflammatory and antioxidative processes, modulates microglia polarization, and promotes recovery after ischemic stroke. Neuropsychiatr. Dis. Treat. 2019;15:2927. doi: 10.2147/NDT.S210403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Yeh C.F., Chuang T.Y., Hung Y.W., Lan M.Y., Tsai C.H., Huang H.X., Lin Y.Y. Inhibition of soluble epoxide hydrolase regulates monocyte/macrophage polarization and improves neurological outcome in a rat model of ischemic stroke. Neuroreport. 2019;30:567–572. doi: 10.1097/WNR.0000000000001248. [DOI] [PubMed] [Google Scholar]
- 132.Davis C.M., Zhang W.H., Allen E.M., Bah T.M., Shangraw R.E., Alkayed N.J. Soluble epoxide hydrolase blockade after stroke onset protects normal but not diabetic mice. Int. J. Mol. Sci. 2021;22:5419. doi: 10.3390/ijms22115419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Hasumi K., Suzuki E. Impact of SMTP targeting plasminogen and soluble epoxide hydrolase on thrombolysis, inflammation, and ischemic stroke. Int. J. Mol. Sci. 2021;2:954. doi: 10.3390/ijms22020954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Suzuki E., Nishimura N., Yoshikawa T., Kunikiyo Y., Hasegawa K., Hasumi K. Efficacy of SMTP-7, a small-molecule anti-inflammatory thrombolytic, in embolic stroke in monkeys. Pharmacol. Res. Perspect. 2018;6:e00448. doi: 10.1002/prp2.448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Zhang L., Xu S., Wu X., Muse F.M., Chen J., Cao Y., Yan J., Cheng Z., Yi X., Han Z. Protective effects of the soluble epoxide hydrolase inhibitor 1-trifluoromethoxyphenyl-3-(1-propionylpiperidin-4-yl) urea in a rat model of permanent middle cerebral artery occlusion. Front. Pharmacol. 2020;11:182. doi: 10.3389/fphar.2020.00182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Yi X., Xu C., Huang P., Zhang L., Qing T., Li J., Wang C., Zeng T., Lu J., Han Z. 1-trifluoromethoxyphenyl-3-(1-propionylpiperidin-4-yl) urea protects the blood-brain barrier against ischemic injury by upregulating tight junction protein expression, mitigating apoptosis and inflammation in vivo and in vitro model. Front. Pharmacol. 2020;11:1197. doi: 10.3389/fphar.2020.01197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Yao W., Cao Q., Luo S., He L., Yang C., Chen J., Qi Q., Hashimoto K., Zhang J.C. Microglial ERK-NRBP1-CREB-BDNF signaling in sustained antidepressant actions of (R)-ketamine. Mol. Psychiatry. 2021 doi: 10.1038/s41380-021-01377-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Hammock B.D., McReynolds C.B., Wagner K., Buckpitt A., Cortes-Puch I., Croston G., Lee K.S.S., Yang J., Schmidt W.K., Hwang S.H. Movement to the clinic of soluble epoxide hydrolase inhibitor EC5026 as an analgesic for neuropathic pain and for use as a nonaddictive opioid alternative. J. Med. Chem. 2021;64:1856–1872. doi: 10.1021/acs.jmedchem.0c01886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Luther J.M., Ray J., Wei D., Koethe J.R., Hannah L., DeMatteo A., Manning R., Terker A.S., Peng D., Nian H., et al. GSK2256294 decreases sEH (soluble epoxide hydrolase) activity in plasma, muscle, and adipose and reduces F2-isoprostanes but does not alter insulin sensitivity in humans. Hypertension. 2021;78:1092–1102. doi: 10.1161/HYPERTENSIONAHA.121.17659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Martini R.P., Siler D., Cetas J., Alkayed N.J., Allen E., Treggiari M.M. A double-blind, randomized, placebo-controlled trial of soluble epoxide hydrolase inhibition in patients with aneurysmal subarachnoid hemorrhage. Neurocrit. Care. 2021 doi: 10.1007/s12028-021-01398-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.