Abstract
Simple Summary
Despite improvements in standardized screening methods and the development of promising therapies for colorectal cancer (CRC), survival rates are still low. Drug repurposing offers an affordable solution to achieve new indications for previously approved drugs that could play a protagonist or adjuvant role in the treatment of CRC. In this review, we summarize the current data supporting drug repurposing as a feasible option for patients with CRC.
Abstract
Colorectal cancer (CRC) is the third most common cancer in the world. Despite improvement in standardized screening methods and the development of promising therapies, the 5-year survival rates are as low as 10% in the metastatic setting. The increasing life expectancy of the general population, higher rates of obesity, poor diet, and comorbidities contribute to the increasing trends in incidence. Drug repurposing offers an affordable solution to achieve new indications for previously approved drugs that could play a protagonist or adjuvant role in the treatment of CRC with the advantage of treating underlying comorbidities and decreasing chemotherapy toxicity. This review elaborates on the current data that supports drug repurposing as a feasible option for patients with CRC with a focus on the evidence and mechanism of action promising repurposed candidates that are widely used, including but not limited to anti-malarial, anti-helminthic, anti-inflammatory, anti-hypertensive, anti-hyperlipidemic, and anti-diabetic agents.
Keywords: colorectal cancer, therapy resistance, drug repurposing, in silico drug screens
1. Introduction
Colorectal cancer (CRC) is the third most prevalent cancer in the world, with more than 100,000 new cases and 50,000 deaths occurring in the United States during 2021 [1]. It is the third most common cancer in both sexes and the second most common cancer-related mortality cause [2]. It is projected that there will be an overall doubling of CRC cases in the following decades [3], with an estimated worldwide increase to 2.5 million new cases in 2035 [4]. In countries with a high human development index, the incidence and mortality rates of CRC have decreased predominantly in older adults, while in lower- and middle-income countries, mortality is increasing [2]. There is a growing incidence of CRC in younger groups, likely attributed to a high prevalence of certain risk factors such as poor diet, low physical activity, and higher rates of obesity [2].
Most CRCs arise from neoplastic polyps as stem cells progressively acquire genetic and epigenetic alterations [4]. Chromosomal instability, mismatch repair deficiency, and CpG hypermethylation underline the pathogenesis of CRC [5]. Significant molecular heterogeneity with altered mismatch repair mechanisms leading to microsatellite instability in BRAF-mutated sessile serrated adenomatous polyps and adenocarcinomas increase after 85 years of age [6]. Sporadic CRC accounts for 70% of new cases, usually following a specific succession of mutations in the adenomatous polyposis coli (APC) gene, followed by KRAS, TP53, and DCC mutations [7]. Familial cases correspond to approximately 25% of cases, and 5% occur in well-defined hereditary CRC syndromes such as familial adenomatous polyposis and Lynch syndrome [7].
The stage of the CRC at the time of diagnosis is crucial in determining survival. While the 5-year survival is approximately 90% for patients with stage I disease, in stage IV it decreases to less than 10%, highlighting the importance of early detection [8]. For localized early-stage CRC, surgery is the standard therapy [5]. In patients with stage II CRC with a high risk of recurrence after surgery or stage III disease (lymph node metastases), adjuvant chemotherapy using oxaliplatin and irinotecan in addition to 5-fluorouracil (5FU) or Capecitabine is used [9]. Targeted therapies, including monocolonal antibodies against VEGF (bevacizumab) or EGFR (cetuximab or panitumumab) are used in the metastatic setting in combination with chemotherapy depending on RAS mutational status and tumor location (left vs. right) [9,10]. In addition, immunotherapy has proven to be an effective treatment modality in the setting of microsatellite instability (MSI) high CRC [10]. For patients with unresectable lesions, treatment is a combination of maximum tumoral cytoreduction and chemotherapy [11]. Despite the advances in treatment, advanced disease remains to be associated with poor survival and resistance to cytotoxic and targeted chemotherapies is still occurring [12].
2. Repurposing Approved Drugs in Colon Cancer
Drug repurposing or repositioning involves using approved drugs for conditions different from their original indication [13,14,15]. Several drugs have acquired additional use in the past years and have been reintroduced into practice fueled by this phenomenon. For instance, thalidomide, discontinued from its original use as an antiemetic, is currently used for multiple myeloma [16] and moderate to severe erythema nodosum leprosum [17]. Another example is Sildenafil which preserves both its primary indication for erectile dysfunction [18] and repurposed indication as a treatment option for idiopathic pulmonary hypertension [19].
Drug repurposing has regained a significant role as a convenient, fast, and relatively safe drug development strategy. New drug development usually takes around 10–15 years on average [20], with a success rate reported from 2 to 10% [21,22]. According to the U.S. Food and Drug Administration (FDA), as of 2018, the compound percentage of drugs reaching stage 4 clinical trials was around 6% [23]. Drug repurposing offers significantly shorter development times and lower investments described as 160 million times lower, particularly costs regarding safety testing, molecular characterization, safety profiling, and initial marketing. It leverages known genetic, pharmacodynamic, pharmacokinetic, and adverse effect profiles, usually bypassing stage 1 clinical trials [24]. Therefore, this approach represents a more cost-efficient, expedited, and less risky strategy than traditional drug development [21].
Many successful reintroductions and alternative indications second repurposing as a feasible option in many areas of medicine. Aspirin, for example, has acquired a wide range of indications, ranging from acutely therapeutic to prolonged preventative ones [14,25]. The cardiovascular field further illustrates this diversity with the recent supportive evidence of SGLT-2 inhibitors, initially approved for hyperglycemia management, for heart failure management regardless of the patients’ ejection fraction and notwithstanding their diabetes status [26,27,28,29]. Therapeutics for Alzheimer’s disease have been highly reliant on this strategy. Since memantine in 2003, no new drugs had been approved until the FDA granted the recent fast track concession for aducanumab in 2021 [14,30]. As of 2017, approximately 27 FDA-approved drugs were being evaluated for Alzheimer’s disease in stages 1–3 clinical trials [14].
Oncology has also gained benefits from drug repurposing. Estimation is that 5% of the anticancer drugs entering phase 1 clinical trials are eventually approved [31]. Certain calcium channels blockers such as felodipine and amlodipine besylate undermine filopodia stability in cancer cells, decreasing the likelihood of progression, invasion, and metastasis [32]. Metformin, classically an antidiabetic drug, has been described to decrease tumor growth. Although metabolic reprogramming halting oxidative phosphorylation and multi-targeted mTOR inhibition have hypothesized metformin’s antitumoral activity, precise mechanisms remain obscure [21,33,34].
The benefits of drug repurposing are evident after their serendipitous discovery and raise interest in predictive tools to optimize outcomes. Many approaches group together into either experimental or computational models [24,35]. The former usually involves either in vitro analysis measuring affinity and interaction stability, also called binding assays, or combined in vitro/in vivo models using compound libraries to test for cellular lineage changes, known as the phenotypic model. The phenotypic approach aims to reproduce diseases in an experimental cellular environment and relies on known compound libraries to test and characterize cellular responses [24]. Alternatively, known compounds have been assessed using in silico models stemming from structure-based principles: direct molecular docking, inverse molecular docking, and receptor-based pharmacophore searching [36]. Drug-based strategies use established drug information such as pharmacodynamics, biochemical, adverse effect profiles, and genomic data to determine potential alternative uses. Transcriptomics data are especially valuable to depict deviant cellular responses to diverse pathologic states, notably those with solid genetic pathomechanisms. Conversely, knowledge-based strategies use well-characterized molecular disease mechanisms to depict candidates for drug repurposing [35].
Large genetic and disease datasets are becoming publicly available, and computational tools for processing massive data are evolving accordingly. Computational-based drug repurposing uses data mining, machine learning, and network analysis to distill large datasets involving disease-specific transcriptomics, proteomics, drug efficacy, responses, and even clinical variables [35]. This information provides insight into complex biologic processes such as epigenetic regulation in cancer cells. Furthermore, drug repurposing approaches may be used for epigenetic reprogramming of cancer cells to increase susceptibility via differential transcriptome expressions. A study characterized 45 FDA-approved drugs yielding synergistic activity with histone deacetylating agents and methylation inhibitors. Additionally, they characterized 85 FDA-approved medications that antagonized the action of these drug families, thwarting favorable responses in colon cancer cells. Altogether, these findings illustrate the benefits and complexity of drug repurposing to design personalized and highly effective treatment plans that account for previously unknown drug interactions [37] (Table 1).
Table 1.
Summary table of the drugs that have been repurposed to be used in colon cancer.
| Reference | Drug | Original Indication | Possible Mode(s) of Action | Effect(s) |
|---|---|---|---|---|
| [38,39] | ACEIs/ARBs | Hypertension | Decreased chronic inflammation and oxidative stress | Reduced risk of adenomatous colon polyps |
| [40] | Nebivolol | Hypertension and other indications | Inhibition of mitochondrial respiration by decreasing the activity of Complex I of the respiratory chain | Suppressed the growth of colon cancer cells |
| [41,42,43,44] | Aspirin | Antiplatelet | Inhibition of COX-2, c-MYC transcription factor, and the antiplatelet mechanism of action | Decreased cancer metastasis and immune evasion |
| [45,46] | Celecoxib | Anti-inflammatory | Effect on p53 by regulating the expression of p21 and CyclinD1 in a COX-2-independent manner Upregulation of BCCIP Increased radiosensitivity in HCT116 cell line |
Decreased incidence of adenomatous polyps. |
| [47,48] | Lovastatin | Antilipidemic | Inhibition of MACC1 | Restricted cancer progression and metastasis formation |
| [49,50,51,52,53] | Metformin | Antihyperglycemic | Inhibition of mTOR Modulation of oxidative stress and nuclear factor-κB inflammatory responses |
Apoptosis in CRC cell lines |
| [54,55] | Dapagliflozin | Antihyperglycemic | Effect on cellular interaction with Collagen types I and IV Increased Erk phosphorylation |
Decreased adhesion and proliferation of colon cancer cells |
| [56,57] | Mebendazole | Anti-helminthic | Inhibition of MYC | Cytotoxic activity against different colon cancer cell lines |
| [58,59] | Niclosamide | Anti-helminthic | Downregulation of the Wnt/β-catenin cascade | Decreased proliferation in multiple human CRC cell lines |
| [60] | Tenofovir | Anti-retroviral (anti-HIV drug) | Decreased Bcl-2 and cyclin D1 expression | Inhibition of proliferation, oxidative stress, and inflammation |
| [61,62] | Zidovudine | Anti-retroviral (anti-HIV drug) | Increased expression of the p53-Puma/Bax/Noxa pathways Activation of the p53-p21 pathway |
Apoptosis Cell cycle arrest |
| [63] | Efavirenz | Anti-retroviral (anti-HIV drug) | Activation of the phosphorylation of p53 | Cytotoxic activity against different colon cancer cell lines |
| [64] | Indinavir | Anti-retroviral (anti-HIV drug) | Proteasome-independent block of angiogenesis and matrix metalloproteinases | Suppressed growth |
| [64,65] | Saquinavir | Anti-retroviral (anti-HIV drug) | Proteasome-independent block of angiogenesis and matrix metalloproteinases Inhibition of proteolytic degradation and accumulation of p21 |
Apoptosis Suppressed growth |
| [66,67,68] | Ritonavir | Anti-retroviral (anti-HIV drug) | Inhibition proteolytic degradation and accumulation of p21 Decreased production of TNF-α, IL-6, IL-8, and VEGF Increased expression of heme oxygenase-1 |
Apoptosis Suppressed angiogenesis |
| [69] | Raltegravir | Anti-retroviral (anti-HIV drug) | Blockage of fascin-1 | Suppressed invasion |
| [70,71] | Doxycycline | Antibiotic | Inhibition of matrix metalloproteinases Activation of caspase-3, -8, and -9 Release of cytochrome c and Bax translocation |
Apoptosis Suppressed proliferation and invasive potential |
| [72,73,74,75] | Clarithromycin | Antibiotic | Inhibition of autophagy by targeting hERG1 | Suppressed angiogenesis Suppressed growth of colon cancer cells |
| [76,77,78] | Azithromycin | Antibiotic | Inhibition of autophagy by upregulating p62 and LC-3B | Apoptosis |
| [79] | Gemifloxacin | Antibiotic | Inhibition of NF-κB activation Inhibition of TNF-α, IL-6, IL-8, and VEGF |
Suppressed cell migration and invasion |
| [80,81] | Artesunate | Antimalarial | Downregulation of β-catenin | Apoptosis Cytotoxicity |
| [82] | Mefloquine | Antimalarial | Inhibition of NF-κB activation | Apoptosis Growth arrest |
| [83] | Valproate | Antipsychotic | Histone hyperacetylation Relief of HDAC-mediated transcriptional repression |
Reduced viability Enhanced cytotoxicity |
| [84,85] | Fluoxetine | Antidepressant | Inhibition of NF-κB activation and IKK phosphorylation Cell-cycle arrest at G0/G1 Enhanced p27 expression Reduced VEGF expression |
Suppressed colitis-associated tumorigenesis Suppressed dysplasia and angiogenesis |
| [86,87,88] | Sirolimus | Prevention of kidney transplant rejection | CHOP-dependent DR5 induction on 4E-BP1 dephosphorylation Suppressed FBXW7 loss-driven EMT |
Apoptosis Decreased angiogenesis Suppressed proliferation and invasion of colon cancer cells |
| [89] | Butyrate | Probiotic | Inhibition of miR-92a | Suppressed proliferation of colon cancer cells |
2.1. Anti-Hypertensives and Anti-Arrhythmic Drugs
Angiotensin I converting enzyme inhibitors (ACEIs) and angiotensin II receptor blockers (ARBs) are commonly used drugs that have life-prolonging effects on patients treated for several diseases including but not limited to hypertension and heart failure [90]. An in vivo study by Kubota et al. suggested that both ACEIs and ARBs suppress colitis-induced CRC by decreasing chronic inflammation and oxidative stress in obese mice [38]. In another study by Kedika et al., patients who had one or more histologically confirmed adenomatous polyps on an index colonoscopy and received lisinopril—an ACEI—had a 41% reduction in the risk of developing similar polyps over the next 3–5 years [39].
Beta blockers (BB) are class II antiarrhythmic drugs used primarily to treat cardiovascular diseases and many other conditions [91]. In a study by Tapioles et al., Nebivolol was shown to selectively inhibit mitochondrial respiration in an HCT-116 colon cancer cell line by decreasing the activity of complex I of the respiratory chain and restraining the growth of colon cancer cells, hinting towards a repurposing potential for this drug in colon cancer [40]. Furthermore, Engineer et al. demonstrated that the combination of ACEI/ARB with BB was associated with increased survival, decreased hospitalization, and decreased tumor progression in advanced CRC [92].
2.2. Nonsteroidal Anti-Inflammatory Drugs
Nonsteroidal anti-inflammatory drugs (NSAIDs) employ their anti-inflammatory, analgesic, and antipyretic properties by inhibiting the cyclooxygenase (COX) enzymes [93]. COX-2 overexpression is a major risk factor for the development of CRC [94]. The therapeutic effect of aspirin in CRC can be explained by inhibition of COX-2 as well as the c-MYC transcription factor [41,42]. Furthermore, aspirin blocks platelet activity which is implicated in cancer metastasis and immune evasion [43]. However, Chan et al. argued that aspirin must be used for more than 10 years to achieve a statistically significant reduction in COX-2 positive cancer [44].
Celecoxib works by selectively and reversibly inhibiting COX-2, and thus acts to decrease inflammation and pain without affecting platelets [95]. Many studies concluded that celecoxib increases radiosensitization of CRC cells [96,97]. Celecoxib also affects p53 by regulating the expression of p21 and CyclinD1 in a COX-2-independent manner, by upregulating BCCIP, increasing radiosensitivity in the HCT116 CRC cell line [45]. A randomized controlled trial by Bertagnolli et al. showed that celecoxib was effective for the secondary prevention of colorectal adenomas and decreased the cumulative incidence of adenomas after 3 years from 60.7% in the placebo arm to 43.2% in patients receiving 200 mg of celecoxib twice daily [46].
2.3. Anti-Hyperlipidemic Drugs
Statins markedly inhibit HMG-CoA reductase, the enzyme that controls the rate-limiting step in the cholesterol synthesis pathway in the liver [98]. Remarkably, in a large study including 1953 patients with CRC and 2015 controls, the use of statins for at least 5 years was associated with a significantly reduced relative risk of developing CRC (odds ratio (OR) = 0.50; 95% confidence interval (CI), 0.40–0.63) [99]. In vivo, lovastatin was shown to restrict cancer progression and metastasis formation by inhibiting MACC1 [47]. In a large meta-analysis including a total of 31 studies and involving more than 1.6 million subjects, statins were shown to have a moderate protective effect against developing CRC [48].
2.4. Anti-Diabetic Drugs
Metformin, an oral anti-diabetic medication used for type 2 diabetes mellitus, is a biguanide drug that increases insulin sensitivity, decreases intestinal absorption of glucose, and decreases its production by the liver [100]. Previous studies have shown a protective effect of metformin in CRC risk and prognosis [101,102]. The current understanding is that metformin inhibits the mammalian target of rapamycin (mTOR) pathway which plays a central role in CRC cell growth and proliferation [49]. Furthermore, metformin downregulates IGF receptor activation through decreasing insulin and insulin growth factor, resulting in decreased proliferation in colorectal neoplasia [103,104]. Inhibition of mTOR is achieved through inhibition of mitochondrial mammalian respiratory chain complex I followed by activation of liver kinase B1 and downstream target Adenosine monophosphate-activated protein kinase (AMPK) [50,51]. Other research has shown that metformin, through modulation of oxidative stress and nuclear factor-κB (NF-κB) inflammatory responses would induce apoptosis in CRC cell lines [52,53]. Metformin may also increase sensitivity of cancer cell lines to chemotherapeutic agents such as 5-Fluorouracil, irinotecan, and paclitaxel [105,106,107].
Dapagliflozin, another oral antihyperglycemic medication used for type 2 diabetes mellitus works by inhibiting the sodium/glucose cotransporter 2 (SGLT2) in the proximal tubules of the kidney [108]. Dapagliflozin decreases the adhesion of CRC cells by affecting cellular interaction with Collagen types I and IV through activating ADAM10, which subsequently causes a loss in the full-length DDR1 [54]. DDR1 binding to Collagens I and IV is necessary to stimulate cell–collagen interactions [109]. Dapagliflozin also decreases colon cell proliferation by increasing Erk phosphorylation in the HCT116 human colon cancer cell line [55]. In a case report by Okada et al., SGLT2 inhibition in combination with the EGFR inhibitor, cetuximab, reduced both tumor size and carcinoembryonic antigen (CEA) levels in CRC with liver metastasis [110].
2.5. Anti-Helminthic Drugs
Mebendazole is a broad spectrum benzimidazole that inhibits microtubule synthesis by blocking tubulin polymerization [111]. Mebendazole has cytotoxic activity against different CRC cell lines such as HCT-116, RKO, HT-29, HT-8, and SW626 [56,112]. Nygren and Larsson reported that mebendazole induced remission of metastatic lesions in a patient with refractory metastatic CRC [113]. Another study carried out on mice with a constitutional mutation in the Adenomatous polyposis coli (APC) gene showed that the combination of mebendazole and sulindac (an NSAID) decreased both the number and size of intestinal microadenomas by inhibiting MYC and COX-2 pathways, angiogenesis, and the release of pro-tumorigenic cytokines [57].
Niclosamide is a salicylamide derivative that acts by uncoupling oxidative phosphorylation and regulating different signaling pathways [114]. Niclosamide downregulated the Wnt/β-catenin cascade, which is aberrantly activated in 80% of sporadic CRC [115], in both in vitro and in vivo studies [58] and resulted in decreased proliferation in multiple human CRC cell lines such as HCT-116, Caco2, and HT-29 [59], possibly via the induction of autophagy [116]. Furthermore, a recent study by Kang et al. demonstrated that niclosamide could be combined with metformin to synergistically inhibit APC-mutant CRC by suppressing Wnt and YAP [117].
2.6. Anti-Retroviral Drugs
Tenofovir is a nucleoside antiretroviral drug that acts by inhibiting the reverse transcriptase enzyme [118]. Tenofovir also inhibits the activity of human telomerase [119], a crucial enzyme for tumorigenesis and cancer proliferation, whose inhibition represents a promising therapeutic strategy in cancer treatment [120,121]. Sherif et al. demonstrated that rats receiving tenofovir at a dose of 50 mg/kg for 24 weeks had diminished colorectal cell proliferation attributed to decreased Bcl-2 and cyclin D1 expression [60]. Zidovudine, also known as azidothymidine, is another nucleoside reverse transcriptase inhibitor (NRTI) used in the treatment of human immunodeficiency virus (HIV) [122]. Brown et al. demonstrated Zidovudine’s telomerase inhibition activity in the HT-29 colon cancer cell line [61]. Furthermore, Fang et al. showed that the antitumor activity of zidovudine in colon cancer cells is mediated by increased expression of the p53-Puma/Bax/Noxa pathways favoring apoptosis, and activation of the p53-p21 pathway promoting cell cycle arrest [62]. Efavirenz is a non-nucleoside reverse transcriptase inhibitor (NNRTI) used in the treatment of HIV that is selectively cytotoxic to different tumor cell lines, including colorectal carcinoma, by activating the phosphorylation of p53 [63].
Protease inhibitors (PI) are also drugs that suppress the action of HIV proteases to inhibit viral growth, infectivity, and replication [123]. Indinavir and Saquinavir are PI that suppress the growth of human tumor cells by blocking angiogenesis and matrix metalloproteinases to inhibit tumor invasion and progression. [64]. Furthermore, Mühl et al. reported that Ritonavir synergizes with butyrate to induce apoptosis of CRC cells [66]. The anticancer effect of Ritonavir is most likely due to the inhibition of proteolytic degradation, which causes the accumulation of p21 [68], the decreased production of TNF-α, IL-6, IL-8, and VEGF [67], and the increased expression of anti-inflammatory heme oxygenase-1 [66].
Integrase inhibitors are the latest class of antiretroviral drugs which were approved for HIV therapy due to their efficacy, tolerability, and safety [124]. Raltegravir is an integrase inhibitor that inhibits the Fascin-1-dependent invasion of colorectal tumor cells in vitro and in vivo [69]. Fascin-1 is an actin cross-linking protein whose elevated expression is associated with aggressive clinical progression, dismal prognosis, increased recurrence, and worse survival outcomes in patients with CRC [125,126].
2.7. Anti-Microbials
Other anti-microbial drugs have been investigated for repurposing in colon cancer treatment including doxycycline, a semi-synthetic antibiotic derivative of tetracycline used in the treatment of a wide variety of infections [127]. Doxycycline has also been shown to inhibit matrix metalloproteinases [128]. Onoda et al. demonstrated that a combination therapy consisting of doxycycline and a COX-2 inhibitor suppressed colon cancer cell proliferation and invasion [71]. Doxycycline reportedly induced apoptosis in a dose-dependent manner through activation of caspases, release of cytochrome C, and translocation of Bax [70].
Another antibiotic with potential in cancer therapeutics is clarithromycin. Clarithromycin is a potent inhibitor of tumor-induced angiogenesis [73] showing increased efficacy when combined with approved anticancer drugs [72,75,129]. It is also implicated in attenuating autophagy in myeloma cells [130]. Targeting autophagy is considered a promising strategy for colon cancer therapy [131,132]. In a study by Petroni et al., clarithromycin was indeed shown to modulate autophagy in human CRC cells and inhibited the growth of tumors by targeting hERG1 [74].
The inhibition of autophagy as a mechanism of anticancer activity is also shared by azithromycin, another macrolide antibiotic [76,77]. Qiao et al. demonstrated that azithromycin had a synergistic antitumor activity with the tumor necrosis factor-related apoptosis-inducing ligand (TRAIL) in colon cancer cells. Azithromycin may also suppress autophagy by upregulating the expression of p62 and LC-3B to ultimately induce colon cancer cell death [78].
Gemifloxacin is a fluoroquinolone used in the setting of community-acquired pneumonia and acute exacerbations of chronic bronchitis [133]. Kan et al. demonstrated that gemifloxacin inhibits the migration and invasion of SW620 and LoVol colon cancer cells and downregulates Snail to reduce epithelial-to-mesenchymal transition (EMT). Gemifloxacin also suppresses the NF-κB pathway and cytokine-mediated cell migration and invasion as shown by decreased levels of tumor necrosis factor alpha (TNF-alpha), interleukin 6 (IL-6), IL-8, and vascular endothelial growth factor (VEGF) [79].
Antimalarials are also being considered for the treatment of colon cancer. Artesunate is an antimalarial agent recommended for the treatment of patients with severe Plasmodium falciparum malaria [134]. In a preclinical model of CRC, artesunate was found to suppress inflammation and oxidative stress [81]. Efferth et al. demonstrated a cytotoxic action of artesunate on tumor cells via both p53-dependent and -independent pathways [135] implicated in downregulation of β-catenin [80]. Mefloquine, another antimalarial drug, was found to induce growth arrest and apoptosis of CRC cells in mice via inhibition of the tumor NF-κB signaling pathway [82].
2.8. Others
Drugs used for neurological conditions are increasingly being considered as therapeutic options in cancer patients [136,137]. Friedmann et al. demonstrated that valproate, a histone deacetylase inhibitor (HDACi), dose-dependently reduced the viability of adenocarcinoma cell lines, particularly when combined with mitomycin C [138]. Additionally, in a study by Mologni et al., valproate was found to enhance bosutinib cytotoxicity in colon cancer cells [139]. This may be explained by increasing histone hyperacetylation of H3 and H4 to enhance antitumor activity and by relieving HDAC-driven transcriptional repression [83,140].
Fluoxetine is a selective serotonin reuptake inhibitor (SSRI) that is used in the treatment of major depressive disorder [141]. In a study examining murine colitis-associated colon cancer, fluoxetine was found to inhibit NF-κB activation and decrease TNF-α-mediated IκB kinase (IKK) and IκBα phosphorylation; thus suppressing dextran sulfate sodium (DSS)-induced colitis and colitis-associated tumorigenesis [84]. Furthermore, Kannen et al. studied the antiproliferative effects of fluoxetine on HT29 colon cancer cells. Fluoxetine increased the percentage of HT29 cells in the G0/G1 phase of the cell cycle and enhanced the expression of p27 protein. Fluoxetine also suppressed the development of dysplasia and vascularization-related dysplasia in colon tissue, and reduced VEGF expression and the number of cells with angiogenic potential, such as CD133, CD34, and CD31-positive cell clusters [85].
Sirolimus, also known as Rapamycin, is an FDA-approved mTOR inhibitor used in the prophylaxis of renal graft rejection [142]. Mussin et al. demonstrated that a combination of sirolimus and metformin synergistically inhibits colon tumor growth both in vitro and in vivo [86]. He et al. revealed that mTOR inhibitors induce apoptosis in colon cancer cells via CHOP-dependent DR5 induction of 4E-BP1 dephosphorylation resulting in decreased tumor proliferation, angiogenesis, and invasion [88]. In addition, Wang et al. demonstrated that sirolimus suppresses the FBXW7-loss-driven EMT through its mTOR inhibition activity, thereby decreasing CRC cell migration and invasion [87].
Finally, it is worth noting that probiotics have also been considered for the treatment of CRC. For instance, Hu et al. found that butyrate decreased the transcription of the pro-proliferative miR-92a in human CRC cells [89]. Furthermore, butyrate can also induce apoptosis of DLD-1 colon cancer cells by synergizing with ritonavir [66].
3. Clinical Trials on Drug Repurposing in Colon Cancer
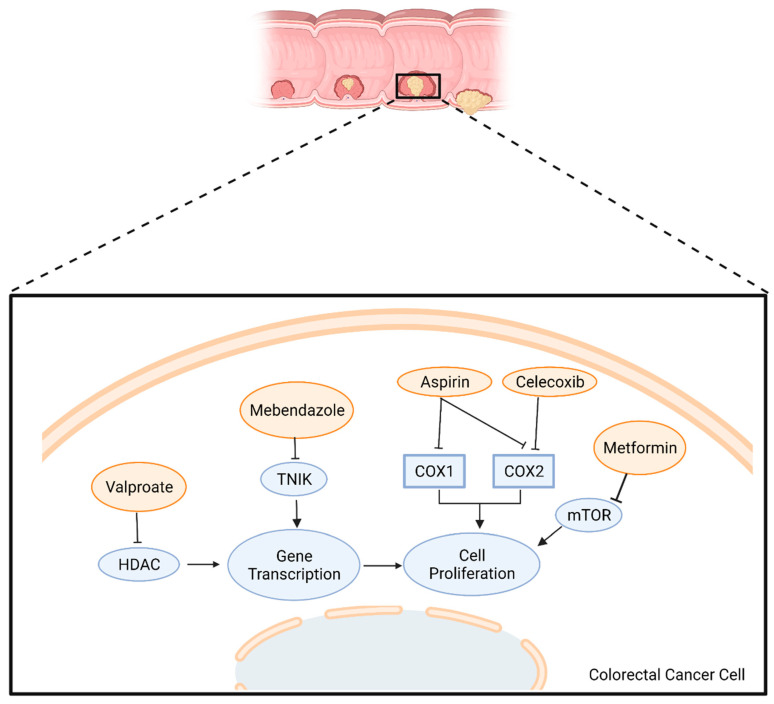
Despite the heterogeneity of potential drugs that can be repurposed, only a few collectively form the most promising treatments for CRC and have been incorporated in clinical trials. A brief overview of the mechanism of action of these drugs is summarized in Figure 1.
Figure 1.
Mode of action of candidate repurposed drugs being tested in clinical trials for patients with CRC. HDAC: Histone Deacetylase; TNIK: TRAF2 And NCK Interacting Kinase; COX: Cyclo-oxygenase; mTOR: mammalian Target of Rapamycin. Adapted from “Round-Cell Background”, by BioRender.com (2022). Retrieved from https://app.biorender.com/biorender-templates accessed on 15 April 2022.
Aspirin is the most represented drug in current clinical trials investigating candidate drugs for repurposing in the treatment of CRC (Table 2). One phase 3 clinical trial involves the use of aspirin as an adjuvant component in stages II and III PIK3CA-mutated colon cancer patients. The trial aims to determine whether the daily consumption of 100 mg of aspirin is effective in reducing recurrence and improving survival compared to placebo (ClinicalTrials.gov; NCT02467582). Two similar phase 3 clinical trials aim to determine the effect of 80 mg daily adjuvant aspirin on survival in stages II and III colon cancer patients compared to placebo (ClinicalTrials.gov; NCT02301286 and NCT03464305). ASPIK French is another phase 3 clinical trial whose goal is to determine local or distant recurrence or second CRC or death from any cause, whichever occurs first, in patients with surgically resected PI3K-mutated colon cancer taking 100 mg of daily aspirin as compared to placebo (ClinicalTrials.gov; NCT02945033). Finally, the ASCOLT phase 3 clinical trial is studying the 5-year disease-free and overall survival in patients with Dukes C or high-risk Dukes B CRC taking 200 mg daily aspirin for 3 years (ClinicalTrials.gov; NCT00565708).
Table 2.
Examples of some repurposed drugs currently being clinically investigated for the treatment of colon cancer.
| Clinical Trial Number | Phase | Status | Estimated Completion Date | Intervention/Treatment | Patient Population | Patients Enrolled | Primary Outcome Measures | Secondary Outcome Measures |
|---|---|---|---|---|---|---|---|---|
| NCT02467582 | 3 | Active, not recruiting | June 2029 | Aspirin | Stages II and III PIK3CA-mutated CRC previously treated with surgery | 185 | DFS after 6 years | Time to recurrenceOS Cancer-specific survival Adverse events |
| NCT02301286 | 3 | Recruiting | September 2022 | Aspirin | Stages II and III CRC | 1588 | OS | DFS TTF |
| NCT03464305 | 3 | Recruiting | December 2026 | Aspirin | Stages II and III CRC | 400 | 5-year OS | DFS TTF |
| NCT02945033 | 3 | Recruiting | July 2024 | Aspirin | PI3K-mutated CRC | 246 | Recurrence or second CRC or death, whichever occurs first | 5-year OS Adverse events |
| NCT00565708 | 3 | Active, not recruiting | June 2026 | Aspirin | Dukes C and high-risk Dukes B CRCs | 1587 | DFS | OS |
| NCT03026140 | 2 | Recruiting | January 2022 | Nivolumab + Ipilimumab with or without Celecoxib | Stages I to III CRC | 60 | Incidence of adverse events | Immune activating capacity of immunotherapyRelapse-free survival |
| NCT03925662 | 3 | Recruiting | December 2028 | FOLFOX + bevacizumab with or without mebendazole | Stage IV CRC | 40 | ORR | - |
| NCT03359681 | 2 | Recruiting | January 2022 | Metformin | CRC | 48 | Ki67 expression on tumor samples | Cleaved Caspase-3 expression Immunoscore Immunological changes in blood samples In vitro cell growth |
| NCT04873895 | 1 | Recruiting | November 2023 | Axitinib + hydroxychloroquine | Liver-dominant metastatic CRC | 25 | Serious adverse events | ORR in setting of liver metastasis PFS OS |
| NCT03919292 | 1/2 | Recruiting | January 2024 | Neratinib + valproate | Advanced solid tumors including CRC | 113 | Recommended phase 2 dose | Adverse events Antitumor effects PFS |
Abbreviations: CRC: colorectal cancer; DFS: disease-free survival; ORR: objective response rate; OS: overall survival; PFS: progression-free survival; TTF: time-to-treatment-failure; FOLFOX: folinic acid + fluorouracil + oxaliplatin.
NSAIDs are also among the drugs currently under study for repurposing in CRC therapeutics. For instance, the NICHE phase 2 clinical trial involves the administration of celecoxib along with nivolumab and ipilimumab for stages I to III colon cancer in the neoadjuvant setting. The adverse effects will be assessed to determine the regimen’s safety (ClinicalTrials.gov; NCT03026140).
Mebendazole, an anti-helminthic drug, is being tested in a phase 3 clinical trial for its use as an adjuvant component to FOLFOX with Bevacizumab in stage IV CRC patients (ClinicalTrials.gov; NCT03925662). Furthermore, MECORA is a phase 2 clinical trial which aims to examine the effect of metformin in non-diabetic patients with colon cancer where metformin will be administered before and after colon cancer surgery (ClinicalTrials.gov; NCT03359681).
A phase IB clinical trial aims to assess the safety of the antimalarial hydroxychloroquine along with Axitinib and hepatic chemoembolization in subjects with liver dominant metastatic CRC (ClinicalTrials.gov; NCT04873895). Finally, a dose-finding phase 1/2 clinical trial is studying the safety and recommended phase 2 dose (RP2D) of the combination of neratinib and sodium valproate in patients with advanced solid tumors, including RAS-mutated CRC patients (ClinicalTrials.gov; NCT03919292).
4. Conclusions and Future Directions
Despite the advances in oncology, cancer continues to be one of the leading causes of morbidity and mortality worldwide. CRC has the third highest mortality rate of all cancers, with poor survival rates in many groups. Moreover, CRC cases are expected to increase dramatically in the following decades [3]; this is why finding effective treatments for these patients is crucial. Developing new drugs and translating them into clinical practice from phases 1 to 3 is very long and expensive, with only 5% of oncology drugs resulting in FDA approval [33]. For this reason, drug repurposing has gained more interest as a fast and safe way to achieve better outcomes since the pharmacokinetic, pharmacodynamic, and toxicity profiles of these drugs are already established. The investigation of previously approved drugs with other indications for CRC treatment should identify new effective therapies with lower costs and shorter timelines. Many FDA-approved drugs for infectious, cardiovascular, metabolic, and other diseases are currently studied as possible cancer therapies.
It is important to highlight that the heterogeneity of cancer physiology and response to therapy and the multiple resistance mechanisms these cells develop represent an enormous challenge in oncology. The combination of computational frameworks (translational bioinformatics, computational intelligence, and methodological and systems biology) in multidisciplinary teams has successfully sped up clinical trials for repurposing drugs [143]. The emergence of new technologies in this field, such as large-scale multi-omics sequencing, genome-wide positioning systems network (GPSnet) algorithms, and other artificial intelligence algorithms, has helped identify new targets for older drugs [144].
The tools have matured, and novel technological advancements have enabled the identification of drugs that are suitable for repurposing. Pushpakom et al. elegantly highlighted the recent ongoing drug repurposing strategies [145]. In the era of big data, computational-based approaches will be a driving force in this field. These strategies range from mapping drug-binding sites and implicated downstream pathways to developing correlative signatures of transcriptomic and genetic data and their integration with clinical databases [145]. These approaches can help narrow down the list of candidate drugs that can be used for repurposing [146]. Nevertheless, experimental strategies relying on large-scale drug testing using in vitro and in vivo models remain to be an essential bridge to early phase clinical trials [145,147].
However, there are several limitations that might have rendered efforts in drug repurposing unsuccessful. Currently available drugs are approved at specific dosages to treat specific conditions. It is unknown whether these drugs are effective in treating other conditions such as CRC and whether different pharmacodynamic and pharmacokinetic properties are required for their activity in this setting [148]. Clinical trials are crucial to answer these questions; however, funding efforts have remained to be important obstacles as well as regulatory and organizational hurdles [149]. Despite that, not all trials translate into a clinical benefit which has recently been observed during the COVID-19 pandemic where a lot of negative trials have been reported [150]. This may be due to poorly designed trials or due to the fact that in vitro effects observed are simply not always translated into clinical benefit in larger groups of patients [150,151].
In conclusion, the overall impact of repurposing drugs must be studied in terms of survival and other aspects such as toxicity and side effects. Although the success rate is not so high, this is a promising strategy that must be deeply studied to provide new therapies for patients with CRC. Drugs that are currently being tested in clinical trials including but not limited to metformin, mebendazole, aspirin, celecoxib, and valproic acid are promising candidate drugs that might have substantial benefit in the CRC clinic.
Acknowledgments
Figures were created with BioRender.com accessed on 15 April 2022.
Author Contributions
Conceptualization, T.E.Z., M.Y., H.F.B. and N.B.; methodology, T.E.Z., M.Y., D.D.O.-G., M.M., R.N., G.B., H.F.B. and N.B.; validation, H.F.B. and N.B.; data curation, T.E.Z., M.Y., D.D.O.-G., M.M., R.N., G.B. and H.F.B.; writing—original draft preparation, T.E.Z., M.Y., D.D.O.-G., M.M., R.N., G.B. and H.F.B.; writing—review and editing, T.E.Z., H.F.B. and N.B.; visualization, N.B.; supervision, N.B.; project administration, H.F.B.; funding acquisition, H.F.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Siegel R.L., Miller K.D., Fuchs H.E., Jemal A. Cancer Statistics, 2021. CA Cancer J. Clin. 2021;71:7–33. doi: 10.3322/caac.21654. [DOI] [PubMed] [Google Scholar]
- 2.Wild C., Weiderpass E., Stewart B.W. World Cancer Report: Cancer Research for Cancer Prevention. Cancer Control. 2020;199:512. [Google Scholar]
- 3.Guren M.G. The global challenge of colorectal cancer. Lancet Gastroenterol. Hepatol. 2019;4:894–895. doi: 10.1016/S2468-1253(19)30329-2. [DOI] [PubMed] [Google Scholar]
- 4.Dekker E., Tanis P.J., Vleugels J.L.A., Kasi P.M., Wallace M.B. Colorectal cancer. Lancet. 2019;394:1467–1480. doi: 10.1016/S0140-6736(19)32319-0. [DOI] [PubMed] [Google Scholar]
- 5.Recio-Boiles A.C. Colon Cancer. StatPearls; Treasure Island, FL, USA: 2021. [Google Scholar]
- 6.Itatani Y., Kawada K. Treatment of Elderly Patients with Colorectal Cancer. BioMed Res. Int. 2018;2018:2176056. doi: 10.1155/2018/2176056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mármol I., Sánchez-de-Diego C., Pradilla Dieste A., Cerrada E., Rodriguez Yoldi M.J. Colorectal Carcinoma: A General Overview and Future Perspectives in Colorectal Cancer. Int. J. Mol. Sci. 2017;18:197. doi: 10.3390/ijms18010197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van der Jeught K., Xu H.C., Li Y.J., Lu X.B., Ji G. Drug resistance and new therapies in colorectal cancer. World J. Gastroenterol. 2018;24:3834–3848. doi: 10.3748/wjg.v24.i34.3834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Das P.K., Islam F., Lam A.K. The Roles of Cancer Stem Cells and Therapy Resistance in Colorectal Carcinoma. Cells. 2020;9:1392. doi: 10.3390/cells9061392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Golshani G., Zhang Y. Advances in immunotherapy for colorectal cancer: A review. Ther. Adv. Gastroenterol. 2020;13:1756284820917527. doi: 10.1177/1756284820917527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xie Y.H., Chen Y.X., Fang J.Y. Comprehensive review of targeted therapy for colorectal cancer. Signal Transduct. Target. Ther. 2020;5:22. doi: 10.1038/s41392-020-0116-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hammond W.A., Swaika A., Mody K. Pharmacologic resistance in colorectal cancer: A review. Ther. Adv. Med. Oncol. 2016;8:57–84. doi: 10.1177/1758834015614530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Giampieri R., Cantini L., Giglio E., Bittoni A., Lanese A., Crocetti S., Pecci F., Copparoni C., Meletani T., Lenci E., et al. Impact of Polypharmacy for Chronic Ailments in Colon Cancer Patients: A Review Focused on Drug Repurposing. Cancers. 2020;12:2724. doi: 10.3390/cancers12102724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jourdan J.P., Bureau R., Rochais C., Dallemagne P. Drug repositioning: A brief overview. J. Pharm. Pharmacol. 2020;72:1145–1151. doi: 10.1111/jphp.13273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nowak-Sliwinska P., Scapozza L., Ruiz i Altaba A. Drug repurposing in oncology: Compounds, pathways, phenotypes and computational approaches for colorectal cancer. Biochim. Biophys. Acta Rev. Cancer. 2019;1871:434–454. doi: 10.1016/j.bbcan.2019.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kumar S.K., Callander N.S., Adekola K., Anderson L., Baljevic M., Campagnaro E., Castillo J.J., Chandler J.C., Costello C., Efebera Y., et al. Multiple Myeloma, Version 3.2021, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. JNCCN. 2020;18:1685–1717. doi: 10.6004/jnccn.2020.0057. [DOI] [PubMed] [Google Scholar]
- 17.Upputuri B., Pallapati M.S., Tarwater P. Thalidomide in the treatment of erythema nodosum leprosum (ENL) in an outpatient setting: A five-year retrospective analysis from a leprosy referral centre in India. PLoS Neglected Trop. Dis. 2020;14:e0008678. doi: 10.1371/journal.pntd.0008678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fink H.A., Mac Donald R., Rutks I.R., Nelson D.B., Wilt T.J. Sildenafil for male erectile dysfunction: A systematic review and meta-analysis. Arch. Intern. Med. 2002;162:1349–1360. doi: 10.1001/archinte.162.12.1349. [DOI] [PubMed] [Google Scholar]
- 19.Barnett C.F., Machado R.F. Sildenafil in the treatment of pulmonary hypertension. Vasc. Health Risk Manag. 2006;2:411–422. doi: 10.2147/vhrm.2006.2.4.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Institute of Medicine (US) Forum on Drug Discovery, Development, and Translation . Transforming Clinical Research in the United States: Challenges and Opportunities: Workshop Summary. National Academies Press (US); Washington, DC, USA: 2010. [PubMed] [Google Scholar]
- 21.Xue H., Li J., Xie H., Wang Y. Review of Drug Repositioning Approaches and Resources. Int. J. Biol. Sci. 2018;14:1232–1244. doi: 10.7150/ijbs.24612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.U.S. Food and Drug Administration Step 3: Clinical Research. [(accessed on 30 November 2021)]; Available online: https://www.fda.gov/patients/drug-development-process/step-3-clinical-research.
- 23.Deotarse P.J.A., Baile M., Kohle N., Kulkarni A. Drug Repurposing: A Review. Int. J. Pharm. Res. Rev. 2015;4:51–58. [Google Scholar]
- 24.Parvathaneni V., Kulkarni N.S., Muth A., Gupta V. Drug repurposing: A promising tool to accelerate the drug discovery process. Drug Discov. Today. 2019;24:2076–2085. doi: 10.1016/j.drudis.2019.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moffat J.G., Vincent F., Lee J.A., Eder J., Prunotto M. Opportunities and challenges in phenotypic drug discovery: An industry perspective. Nat. Rev. Drug Discov. 2017;16:531–543. doi: 10.1038/nrd.2017.111. [DOI] [PubMed] [Google Scholar]
- 26.Packer M., Anker S.D., Butler J., Filippatos G., Pocock S.J., Carson P., Januzzi J., Verma S., Tsutsui H., Brueckmann M., et al. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. N. Engl. J. Med. 2020;383:1413–1424. doi: 10.1056/NEJMoa2022190. [DOI] [PubMed] [Google Scholar]
- 27.Zannad F., Ferreira J.P., Pocock S.J., Anker S.D., Butler J., Filippatos G., Brueckmann M., Ofstad A.P., Pfarr E., Jamal W., et al. SGLT2 inhibitors in patients with heart failure with reduced ejection fraction: A meta-analysis of the EMPEROR-Reduced and DAPA-HF trials. Lancet. 2020;396:819–829. doi: 10.1016/S0140-6736(20)31824-9. [DOI] [PubMed] [Google Scholar]
- 28.Anker S.D., Butler J., Filippatos G., Ferreira J.P., Bocchi E., Böhm M., Brunner-La Rocca H.P., Choi D.J., Chopra V., Chuquiure-Valenzuela E., et al. Empagliflozin in Heart Failure with a Preserved Ejection Fraction. N. Engl. J. Med. 2021;385:1451–1461. doi: 10.1056/NEJMoa2107038. [DOI] [PubMed] [Google Scholar]
- 29.McMurray J.J.V., Solomon S.D., Inzucchi S.E., Køber L., Kosiborod M.N., Martinez F.A., Ponikowski P., Sabatine M.S., Anand I.S., Bělohlávek J., et al. Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N. Engl. J. Med. 2019;381:1995–2008. doi: 10.1056/NEJMoa1911303. [DOI] [PubMed] [Google Scholar]
- 30.U.S. Food and Drug Administration FDA Grants Accelerated Approval for Alzheimer’s Drug. [(accessed on 30 November 2021)]; Available online: https://www.fda.gov/news-events/press-announcements/fda-grants-accelerated-approval-alzheimers-drug.
- 31.Paul S.M., Mytelka D.S., Dunwiddie C.T., Persinger C.C., Munos B.H., Lindborg S.R., Schacht A.L. How to improve R&D productivity: The pharmaceutical industry’s grand challenge. Nat. Rev. Drug Discov. 2010;9:203–214. doi: 10.1038/nrd3078. [DOI] [PubMed] [Google Scholar]
- 32.Jacquemet G., Baghirov H., Georgiadou M., Sihto H. L-type calcium channels regulate filopodia stability and cancer cell invasion downstream of integrin signalling. Nat. Commun. 2016;7:13297. doi: 10.1038/ncomms13297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang Z., Zhou L., Xie N., Nice E.C., Zhang T., Cui Y., Huang C. Overcoming cancer therapeutic bottleneck by drug repurposing. Signal Transduct. Target. Ther. 2020;5:113. doi: 10.1038/s41392-020-00213-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lord S.R., Cheng W.C., Liu D., Gaude E., Haider S., Metcalf T., Patel N., Teoh E.J., Gleeson F., Bradley K., et al. Integrated Pharmacodynamic Analysis Identifies Two Metabolic Adaption Pathways to Metformin in Breast Cancer. Cell Metab. 2018;28:679–688.e674. doi: 10.1016/j.cmet.2018.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jarada T.N., Rokne J.G., Alhajj R. A review of computational drug repositioning: Strategies, approaches, opportunities, challenges, and directions. J. Cheminform. 2020;12:46. doi: 10.1186/s13321-020-00450-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu X., Zhu F., Ma X.H., Shi Z., Yang S.Y., Wei Y.Q., Chen Y.Z. Predicting targeted polypharmacology for drug repositioning and multi- target drug discovery. Curr. Med. Chem. 2013;20:1646–1661. doi: 10.2174/0929867311320130005. [DOI] [PubMed] [Google Scholar]
- 37.Raynal N.J., Da Costa E.M., Lee J.T., Gharibyan V., Ahmed S., Zhang H., Sato T., Malouf G.G., Issa J.J. Repositioning FDA-Approved Drugs in Combination with Epigenetic Drugs to Reprogram Colon Cancer Epigenome. Mol. Cancer Ther. 2017;16:397–407. doi: 10.1158/1535-7163.MCT-16-0588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kubota M., Shimizu M., Sakai H., Yasuda Y., Ohno T., Kochi T., Tsurumi H., Tanaka T., Moriwaki H. Renin-angiotensin system inhibitors suppress azoxymethane-induced colonic preneoplastic lesions in C57BL/KsJ-db/db obese mice. Biochem. Biophys. Res. Commun. 2011;410:108–113. doi: 10.1016/j.bbrc.2011.05.115. [DOI] [PubMed] [Google Scholar]
- 39.Kedika R., Patel M., Pena Sahdala H.N., Mahgoub A., Cipher D., Siddiqui A.A. Long-term use of angiotensin converting enzyme inhibitors is associated with decreased incidence of advanced adenomatous colon polyps. J. Clin. Gastroenterol. 2011;45:e12–e16. doi: 10.1097/MCG.0b013e3181ea1044. [DOI] [PubMed] [Google Scholar]
- 40.Nuevo-Tapioles C., Santacatterina F., Stamatakis K., Núñez de Arenas C., Gómez de Cedrón M., Formentini L., Cuezva J.M. Coordinate β-adrenergic inhibition of mitochondrial activity and angiogenesis arrest tumor growth. Nat. Commun. 2020;11:3606. doi: 10.1038/s41467-020-17384-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dovizio M., Tacconelli S., Sostres C., Ricciotti E., Patrignani P. Mechanistic and pharmacological issues of aspirin as an anticancer agent. Pharmaceuticals. 2012;5:1346–1371. doi: 10.3390/ph5121346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thun M.J., Jacobs E.J., Patrono C. The role of aspirin in cancer prevention. Nat. Rev. Clin. Oncol. 2012;9:259–267. doi: 10.1038/nrclinonc.2011.199. [DOI] [PubMed] [Google Scholar]
- 43.Kopp H.G., Placke T., Salih H.R. Platelet-derived transforming growth factor-beta down-regulates NKG2D thereby inhibiting natural killer cell antitumor reactivity. Cancer Res. 2009;69:7775–7783. doi: 10.1158/0008-5472.CAN-09-2123. [DOI] [PubMed] [Google Scholar]
- 44.Chan A.T., Ogino S., Fuchs C.S. Aspirin and the risk of colorectal cancer in relation to the expression of COX-2. N. Engl. J. Med. 2007;356:2131–2142. doi: 10.1056/NEJMoa067208. [DOI] [PubMed] [Google Scholar]
- 45.Xu X.T., Hu W.T., Zhou J.Y., Tu Y. Celecoxib enhances the radiosensitivity of HCT116 cells in a COX-2 independent manner by up-regulating BCCIP. Am. J. Transl. Res. 2017;9:1088–1100. [PMC free article] [PubMed] [Google Scholar]
- 46.Bertagnolli M.M., Eagle C.J., Zauber A.G., Redston M., Solomon S.D., Kim K., Tang J., Rosenstein R.B., Wittes J., Corle D., et al. Celecoxib for the prevention of sporadic colorectal adenomas. N. Engl. J. Med. 2006;355:873–884. doi: 10.1056/NEJMoa061355. [DOI] [PubMed] [Google Scholar]
- 47.Juneja M., Kobelt D., Walther W., Voss C., Smith J., Specker E., Neuenschwander M., Gohlke B.O., Dahlmann M., Radetzki S., et al. Statin and rottlerin small-molecule inhibitors restrict colon cancer progression and metastasis via MACC1. PLoS Biol. 2017;15:e2000784. doi: 10.1371/journal.pbio.2000784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Qi J.H., Wei J.N., Zhang Z.J., Dong L., Zhang L., Mao Y.Y., Lei L.J., Hu X.Q., Bai W.Q. [A Meta-analysis on association between statins and colorectal cancer] Zhonghua Liu Xing Bing Xue Za Zhi. 2021;42:343–350. doi: 10.3760/cma.j.cn112338-20200119-00045. [DOI] [PubMed] [Google Scholar]
- 49.Slattery M.L., Herrick J.S., Lundgreen A., Fitzpatrick F.A., Curtin K., Wolff R.K. Genetic variation in a metabolic signaling pathway and colon and rectal cancer risk: mTOR, PTEN, STK11, RPKAA1, PRKAG2, TSC1, TSC2, PI3K and Akt1. Carcinogenesis. 2010;31:1604–1611. doi: 10.1093/carcin/bgq142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vial G., Detaille D., Guigas B. Role of Mitochondria in the Mechanism(s) of Action of Metformin. Front. Endocrinol. 2019;10:294. doi: 10.3389/fendo.2019.00294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zi F., Zi H., Li Y., He J., Shi Q., Cai Z. Metformin and cancer: An existing drug for cancer prevention and therapy. Oncol. Lett. 2018;15:683–690. doi: 10.3892/ol.2017.7412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nguyen T.T., Ung T.T., Li S., Lian S., Xia Y., Park S.Y., Do Jung Y. Metformin inhibits lithocholic acid-induced interleukin 8 upregulation in colorectal cancer cells by suppressing ROS production and NF-kB activity. Sci. Rep. 2019;9:2003. doi: 10.1038/s41598-019-38778-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Saber M.M., Galal M.A., Ain-Shoka A.A., Shouman S.A. Combination of metformin and 5-aminosalicylic acid cooperates to decrease proliferation and induce apoptosis in colorectal cancer cell lines. BMC Cancer. 2016;16:126. doi: 10.1186/s12885-016-2157-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Okada J., Yamada E., Saito T., Yokoo H., Osaki A., Shimoda Y., Ozawa A., Nakajima Y., Pessin J.E., Okada S., et al. Dapagliflozin Inhibits Cell Adhesion to Collagen I and IV and Increases Ectodomain Proteolytic Cleavage of DDR1 by Increasing ADAM10 Activity. Molecules. 2020;25:495. doi: 10.3390/molecules25030495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Saito T., Okada S., Yamada E., Shimoda Y., Osaki A., Tagaya Y., Shibusawa R., Okada J., Yamada M. Effect of dapagliflozin on colon cancer cell [Rapid Communication] Endocr. J. 2015;62:1133–1137. doi: 10.1507/endocrj.EJ15-0396. [DOI] [PubMed] [Google Scholar]
- 56.Nygren P., Fryknäs M., Agerup B., Larsson R. Repositioning of the anthelmintic drug mebendazole for the treatment for colon cancer. J. Cancer Res. Clin. Oncol. 2013;139:2133–2140. doi: 10.1007/s00432-013-1539-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Williamson T., Bai R.Y., Staedtke V., Huso D., Riggins G.J. Mebendazole and a non-steroidal anti-inflammatory combine to reduce tumor initiation in a colon cancer preclinical model. Oncotarget. 2016;7:68571–68584. doi: 10.18632/oncotarget.11851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Sack U., Walther W., Scudiero D., Selby M., Kobelt D., Lemm M., Fichtner I., Schlag P.M., Shoemaker R.H., Stein U. Novel effect of antihelminthic Niclosamide on S100A4-mediated metastatic progression in colon cancer. J. Natl. Cancer Inst. 2011;103:1018–1036. doi: 10.1093/jnci/djr190. [DOI] [PubMed] [Google Scholar]
- 59.Osada T., Chen M., Yang X.Y., Spasojevic I., Vandeusen J.B., Hsu D., Clary B.M., Clay T.M., Chen W., Morse M.A., et al. Antihelminth compound niclosamide downregulates Wnt signaling and elicits antitumor responses in tumors with activating APC mutations. Cancer Res. 2011;71:4172–4182. doi: 10.1158/0008-5472.CAN-10-3978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sherif D.A., Makled M.N., Suddek G.M. The HIV reverse transcriptase inhibitor Tenofovir suppressed DMH/HFD-induced colorectal cancer in Wistar rats. Fundam. Clin. Pharmacol. 2021;35:940–954. doi: 10.1111/fcp.12679. [DOI] [PubMed] [Google Scholar]
- 61.Brown T., Sigurdson E., Rogatko A., Broccoli D. Telomerase inhibition using azidothymidine in the HT-29 colon cancer cell line. Ann. Surg. Oncol. 2003;10:910–915. doi: 10.1245/ASO.2003.03.032. [DOI] [PubMed] [Google Scholar]
- 62.Fang X., Hu T., Yin H., Yang J., Tang W., Hu S., Xu X. Differences in telomerase activity and the effects of AZT in aneuploid and euploid cells in colon cancer. Int. J. Oncol. 2017;51:525–532. doi: 10.3892/ijo.2017.4043. [DOI] [PubMed] [Google Scholar]
- 63.Hecht M., Harrer T., Büttner M., Schwegler M., Erber S., Fietkau R., Distel L.V. Cytotoxic effect of efavirenz is selective against cancer cells and associated with the cannabinoid system. AIDS. 2013;27:2031–2040. doi: 10.1097/QAD.0b013e3283625444. [DOI] [PubMed] [Google Scholar]
- 64.Toschi E., Sgadari C., Malavasi L., Bacigalupo I., Chiozzini C., Carlei D., Compagnoni D., Bellino S., Bugarini R., Falchi M., et al. Human immunodeficiency virus protease inhibitors reduce the growth of human tumors via a proteasome-independent block of angiogenesis and matrix metalloproteinases. Int. J. Cancer. 2011;128:82–93. doi: 10.1002/ijc.25550. [DOI] [PubMed] [Google Scholar]
- 65.Pajonk F., Himmelsbach J., Riess K., Sommer A., McBride W.H. The human immunodeficiency virus (HIV)-1 protease inhibitor saquinavir inhibits proteasome function and causes apoptosis and radiosensitization in non-HIV-associated human cancer cells. Cancer Res. 2002;62:5230–5235. [PubMed] [Google Scholar]
- 66.Mühl H., Paulukat J., Höfler S., Hellmuth M., Franzen R., Pfeilschifter J. The HIV protease inhibitor ritonavir synergizes with butyrate for induction of apoptotic cell death and mediates expression of heme oxygenase-1 in DLD-1 colon carcinoma cells. Br. J. Pharmacol. 2004;143:890–898. doi: 10.1038/sj.bjp.0706023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Pati S., Pelser C.B., Dufraine J., Bryant J.L., Reitz M.S., Jr., Weichold F.F. Antitumorigenic effects of HIV protease inhibitor ritonavir: Inhibition of Kaposi sarcoma. Blood. 2002;99:3771–3779. doi: 10.1182/blood.V99.10.3771. [DOI] [PubMed] [Google Scholar]
- 68.Gaedicke S., Firat-Geier E., Constantiniu O., Lucchiari-Hartz M., Freudenberg M., Galanos C., Niedermann G. Antitumor effect of the human immunodeficiency virus protease inhibitor ritonavir: Induction of tumor-cell apoptosis associated with perturbation of proteasomal proteolysis. Cancer Res. 2002;62:6901–6908. [PubMed] [Google Scholar]
- 69.Alburquerque-González B., Bernabé-García Á., Bernabé-García M., Ruiz-Sanz J., López-Calderón F.F., Gonnelli L., Banci L., Peña-García J., Luque I., Nicolás F.J., et al. The FDA-Approved Antiviral Raltegravir Inhibits Fascin1-Dependent Invasion of Colorectal Tumor Cells In Vitro and In Vivo. Cancers. 2021;13:861. doi: 10.3390/cancers13040861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Onoda T., Ono T., Dhar D.K., Yamanoi A., Nagasue N. Tetracycline analogues (doxycycline and COL-3) induce caspase-dependent and -independent apoptosis in human colon cancer cells. Int. J. Cancer. 2006;118:1309–1315. doi: 10.1002/ijc.21447. [DOI] [PubMed] [Google Scholar]
- 71.Onoda T., Ono T., Dhar D.K., Yamanoi A., Fujii T., Nagasue N. Doxycycline inhibits cell proliferation and invasive potential: Combination therapy with cyclooxygenase-2 inhibitor in human colorectal cancer cells. J. Lab. Clin. Med. 2004;143:207–216. doi: 10.1016/j.lab.2003.12.012. [DOI] [PubMed] [Google Scholar]
- 72.Carella A.M., Beltrami G., Pica G., Carella A., Catania G. Clarithromycin potentiates tyrosine kinase inhibitor treatment in patients with resistant chronic myeloid leukemia. Leuk. Lymphoma. 2012;53:1409–1411. doi: 10.3109/10428194.2012.656105. [DOI] [PubMed] [Google Scholar]
- 73.Yatsunami J., Turuta N., Wakamatsu K., Hara N., Hayashi S. Clarithromycin is a potent inhibitor of tumor-induced angiogenesis. Res. Exp. Med. 1997;197:189–197. doi: 10.1007/s004330050068. [DOI] [PubMed] [Google Scholar]
- 74.Petroni G., Bagni G., Iorio J., Duranti C., Lottini T., Stefanini M., Kragol G., Becchetti A., Arcangeli A. Clarithromycin inhibits autophagy in colorectal cancer by regulating the hERG1 potassium channel interaction with PI3K. Cell Death Dis. 2020;11:161. doi: 10.1038/s41419-020-2349-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Schafranek L., Leclercq T.M., White D.L., Hughes T.P. Clarithromycin enhances dasatinib-induced cell death in chronic myeloid leukemia cells, by inhibition of late stage autophagy. Leuk. Lymphoma. 2013;54:198–201. doi: 10.3109/10428194.2012.698737. [DOI] [PubMed] [Google Scholar]
- 76.Tanaka H., Hino H., Moriya S., Kazama H., Miyazaki M., Takano N., Hiramoto M., Tsukahara K., Miyazawa K. Comparison of autophagy inducibility in various tyrosine kinase inhibitors and their enhanced cytotoxicity via inhibition of autophagy in cancer cells in combined treatment with azithromycin. Biochem. Biophys. Rep. 2020;22:100750. doi: 10.1016/j.bbrep.2020.100750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Toriyama K., Takano N., Kokuba H., Kazama H., Moriya S., Hiramoto M., Abe S., Miyazawa K. Azithromycin enhances the cytotoxicity of DNA-damaging drugs via lysosomal membrane permeabilization in lung cancer cells. Cancer Sci. 2021;112:3324–3337. doi: 10.1111/cas.14992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Qiao X., Wang X., Shang Y., Li Y., Chen S.Z. Azithromycin enhances anticancer activity of TRAIL by inhibiting autophagy and up-regulating the protein levels of DR4/5 in colon cancer cells in vitro and in vivo. Cancer Commun. 2018;38:43. doi: 10.1186/s40880-018-0309-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kan J.Y., Hsu Y.L., Chen Y.H., Chen T.C., Wang J.Y., Kuo P.L. Gemifloxacin, a fluoroquinolone antimicrobial drug, inhibits migration and invasion of human colon cancer cells. Biomed Res. Int. 2013;2013:159786. doi: 10.1155/2013/159786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Verma S., Das P., Kumar V.L. Chemoprevention by artesunate in a preclinical model of colorectal cancer involves down regulation of β-catenin, suppression of angiogenesis, cellular proliferation and induction of apoptosis. Chem. Biol. Interact. 2017;278:84–91. doi: 10.1016/j.cbi.2017.10.011. [DOI] [PubMed] [Google Scholar]
- 81.Kumar V.L., Verma S., Das P. Artesunate suppresses inflammation and oxidative stress in a rat model of colorectal cancer. Drug Dev. Res. 2019;80:1089–1097. doi: 10.1002/ddr.21590. [DOI] [PubMed] [Google Scholar]
- 82.Xu X., Wang J., Han K., Li S., Xu F., Yang Y. Antimalarial drug mefloquine inhibits nuclear factor kappa B signaling and induces apoptosis in colorectal cancer cells. Cancer Sci. 2018;109:1220–1229. doi: 10.1111/cas.13540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Patel M.M., Patel B.M. Repurposing of sodium valproate in colon cancer associated with diabetes mellitus: Role of HDAC inhibition. Eur. J. Pharm. Sci. 2018;121:188–199. doi: 10.1016/j.ejps.2018.05.026. [DOI] [PubMed] [Google Scholar]
- 84.Koh S.J., Kim J.M., Kim I.K., Kim N., Jung H.C., Song I.S., Kim J.S. Fluoxetine inhibits NF-κB signaling in intestinal epithelial cells and ameliorates experimental colitis and colitis-associated colon cancer in mice. Am. J. Physiol. Gastrointest Liver Physiol. 2011;301:G9–G19. doi: 10.1152/ajpgi.00267.2010. [DOI] [PubMed] [Google Scholar]
- 85.Kannen V., Hintzsche H., Zanette D.L., Silva W.A., Garcia S.B., Waaga-Gasser A.M., Stopper H. Antiproliferative effects of fluoxetine on colon cancer cells and in a colonic carcinogen mouse model. PLoS ONE. 2012;7:e50043. doi: 10.1371/journal.pone.0050043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mussin N., Oh S.C., Lee K.W., Park M.Y., Seo S., Yi N.J., Kim H., Yoon K.C., Ahn S.W., Kim H.S., et al. Sirolimus and Metformin Synergistically Inhibits Colon Cancer In Vitro and In Vivo. J. Korean Med. Sci. 2017;32:1385–1395. doi: 10.3346/jkms.2017.32.9.1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wang Y., Liu Y., Lu J., Zhang P., Xu Y., Wang Z., Mao J.H., Wei G. Rapamycin inhibits FBXW7 loss-induced epithelial-mesenchymal transition and cancer stem cell-like characteristics in colorectal cancer cells. Biochem. Biophys. Res. Commun. 2013;434:352–356. doi: 10.1016/j.bbrc.2013.03.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.He K., Zheng X., Li M., Zhang L., Yu J. mTOR inhibitors induce apoptosis in colon cancer cells via CHOP-dependent DR5 induction on 4E-BP1 dephosphorylation. Oncogene. 2016;35:148–157. doi: 10.1038/onc.2015.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hu S., Liu L., Chang E.B., Wang J.Y., Raufman J.P. Butyrate inhibits pro-proliferative miR-92a by diminishing c-Myc-induced miR-17-92a cluster transcription in human colon cancer cells. Mol. Cancer. 2015;14:180. doi: 10.1186/s12943-015-0450-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hradec J. Pharmacological therapy for chronic heart failure. Vnitr. Lek. 2018;64:853–859. doi: 10.36290/vnl.2018.117. [DOI] [PubMed] [Google Scholar]
- 91.Do Vale G.T., Ceron C.S., Gonzaga N.A., Simplicio J.A., Padovan J.C. Three Generations of β-blockers: History, Class Differences and Clinical Applicability. Curr. Hypertens. Rev. 2019;15:22–31. doi: 10.2174/1573402114666180918102735. [DOI] [PubMed] [Google Scholar]
- 92.Engineer D.R., Burney B.O., Hayes T.G., Garcia J.M. Exposure to ACEI/ARB and β-Blockers Is Associated with Improved Survival and Decreased Tumor Progression and Hospitalizations in Patients with Advanced Colon Cancer. Transl. Oncol. 2013;6:539–545. doi: 10.1593/tlo.13346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bacchi S., Palumbo P., Sponta A., Coppolino M.F. Clinical pharmacology of non-steroidal anti-inflammatory drugs: A review. Antiinflamm. Antiallergy Agents Med. Chem. 2012;11:52–64. doi: 10.2174/187152312803476255. [DOI] [PubMed] [Google Scholar]
- 94.Sheng J., Sun H., Yu F.B., Li B., Zhang Y., Zhu Y.T. The Role of Cyclooxygenase-2 in Colorectal Cancer. Int. J. Med. Sci. 2020;17:1095–1101. doi: 10.7150/ijms.44439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.McAdam B.F., Catella-Lawson F., Mardini I.A., Kapoor S., Lawson J.A., FitzGerald G.A. Systemic biosynthesis of prostacyclin by cyclooxygenase (COX)-2: The human pharmacology of a selective inhibitor of COX-2. Proc. Natl. Acad. Sci. USA. 1999;96:272–277. doi: 10.1073/pnas.96.1.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Pal I., Dey K.K., Chaurasia M., Parida S., Das S., Rajesh Y., Sharma K., Chowdhury T., Mandal M. Cooperative effect of BI-69A11 and celecoxib enhances radiosensitization by modulating DNA damage repair in colon carcinoma. Tumour Biol. 2016;37:6389–6402. doi: 10.1007/s13277-015-4399-6. [DOI] [PubMed] [Google Scholar]
- 97.Dulai P.S., Singh S., Marquez E., Khera R., Prokop L.J., Limburg P.J., Gupta S., Murad M.H. Chemoprevention of colorectal cancer in individuals with previous colorectal neoplasia: Systematic review and network meta-analysis. BMJ. 2016;355:i6188. doi: 10.1136/bmj.i6188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bansal A.B., Cassagnol M. StatPearls. StatPearls Publishing; Treasure Island, FL, USA: 2021. HMG-CoA Reductase Inhibitors. [PubMed] [Google Scholar]
- 99.Poynter J.N., Gruber S.B., Higgins P.D., Almog R., Bonner J.D., Rennert H.S., Low M., Greenson J.K., Rennert G. Statins and the risk of colorectal cancer. N. Engl. J. Med. 2005;352:2184–2192. doi: 10.1056/NEJMoa043792. [DOI] [PubMed] [Google Scholar]
- 100.Buse J.B., Wexler D.J., Tsapas A., Rossing P., Mingrone G., Mathieu C., D’Alessio D.A., Davies M.J. 2019 Update to: Management of Hyperglycemia in Type 2 Diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) Diabetes Care. 2020;43:487–493. doi: 10.2337/dci19-0066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Berkovic M.C., Mikulic D., Bilic-Curcic I., Mrzljak A. How far along are we in revealing the connection between metformin and colorectal cancer? World J. Gastroenterol. 2021;27:1362–1368. doi: 10.3748/wjg.v27.i14.1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Cunha Júnior A.D., Bragagnoli A.C., Costa F.O., Carvalheira J.B.C. Repurposing metformin for the treatment of gastrointestinal cancer. World J. Gastroenterol. 2021;27:1883–1904. doi: 10.3748/wjg.v27.i17.1883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Pollak M. Insulin, insulin-like growth factors and neoplasia. Best Pract. Res. Clin. Endocrinol. Metab. 2008;22:625–638. doi: 10.1016/j.beem.2008.08.004. [DOI] [PubMed] [Google Scholar]
- 104.Pollak M. The insulin and insulin-like growth factor receptor family in neoplasia: An update. Nat. Rev. Cancer. 2012;12:159–169. doi: 10.1038/nrc3215. [DOI] [PubMed] [Google Scholar]
- 105.Khader E.I., Ismail W.W., Mhaidat N.M., Alqudah M.A. Effect of metformin on irinotecan-induced cell cycle arrest in colorectal cancer cell lines HCT116 and SW480. Int. J. Health Sci. 2021;15:34–41. [PMC free article] [PubMed] [Google Scholar]
- 106.Kim S.H., Kim S.C., Ku J.L. Metformin increases chemo-sensitivity via gene downregulation encoding DNA replication proteins in 5-Fu resistant colorectal cancer cells. Oncotarget. 2017;8:56546–56557. doi: 10.18632/oncotarget.17798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Rocha G.Z., Dias M.M., Ropelle E.R., Osório-Costa F., Rossato F.A., Vercesi A.E., Saad M.J., Carvalheira J.B. Metformin amplifies chemotherapy-induced AMPK activation and antitumoral growth. Clin. Cancer Res. 2011;17:3993–4005. doi: 10.1158/1078-0432.CCR-10-2243. [DOI] [PubMed] [Google Scholar]
- 108.Ganesan K., Rana M.B.M., Sultan S. StatPearls. 2021 January ed. StatPearls Publishing; Treasure Island, FL, USA: 2021. Oral Hypoglycemic Medications. [PubMed] [Google Scholar]
- 109.Kothiwale S., Borza C.M., Lowe E.W., Pozzi A., Meiler J. Discoidin domain receptor 1 (DDR1) kinase as target for structure-based drug discovery. Drug Discov. Today. 2015;20:255–261. doi: 10.1016/j.drudis.2014.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Okada J., Matsumoto S., Kaira K., Saito T., Yamada E., Yokoo H., Katoh R., Kusano M., Okada S., Yamada M. Sodium Glucose Cotransporter 2 Inhibition Combined With Cetuximab Significantly Reduced Tumor Size and Carcinoembryonic Antigen Level in Colon Cancer Metastatic to Liver. Clin. Colorectal. Cancer. 2018;17:e45–e48. doi: 10.1016/j.clcc.2017.09.005. [DOI] [PubMed] [Google Scholar]
- 111.Lacey E. Mode of action of benzimidazoles. Parasitol. Today. 1990;6:112–115. doi: 10.1016/0169-4758(90)90227-U. [DOI] [PubMed] [Google Scholar]
- 112.Laudisi F., Marônek M., Di Grazia A., Monteleone G., Stolfi C. Repositioning of Anthelmintic Drugs for the Treatment of Cancers of the Digestive System. Int. J. Mol. Sci. 2020;21:4957. doi: 10.3390/ijms21144957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Nygren P., Larsson R. Drug repositioning from bench to bedside: Tumour remission by the antihelmintic drug mebendazole in refractory metastatic colon cancer. Acta Oncol. 2014;53:427–428. doi: 10.3109/0284186X.2013.844359. [DOI] [PubMed] [Google Scholar]
- 114.Chen W., Mook R.A., Premont R.T., Wang J. Niclosamide: Beyond an antihelminthic drug. Cell. Signal. 2018;41:89–96. doi: 10.1016/j.cellsig.2017.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Segditsas S., Tomlinson I. Colorectal cancer and genetic alterations in the Wnt pathway. Oncogene. 2006;25:7531–7537. doi: 10.1038/sj.onc.1210059. [DOI] [PubMed] [Google Scholar]
- 116.Wang J., Ren X.R., Piao H., Zhao S., Osada T., Premont R.T., Mook R.A., Morse M.A., Lyerly H.K., Chen W. Niclosamide-induced Wnt signaling inhibition in colorectal cancer is mediated by autophagy. Biochem. J. 2019;476:535–546. doi: 10.1042/BCJ20180385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Kang H.E., Seo Y., Yun J.S., Song S.H., Han D., Cho E.S., Cho S.B., Jeon Y., Lee H., Kim H.S., et al. Metformin and Niclosamide Synergistically Suppress Wnt and YAP in APC-Mutated Colorectal Cancer. Cancers. 2021;13:3437. doi: 10.3390/cancers13143437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Wassner C., Bradley N., Lee Y. A Review and Clinical Understanding of Tenofovir: Tenofovir Disoproxil Fumarate versus Tenofovir Alafenamide. J. Int. Assoc. Provid. AIDS Care. 2020;19:2325958220919231. doi: 10.1177/2325958220919231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Hukezalie K.R., Thumati N.R., Côté H.C., Wong J.M. In vitro and ex vivo inhibition of human telomerase by anti-HIV nucleoside reverse transcriptase inhibitors (NRTIs) but not by non-NRTIs. PLoS ONE. 2012;7:e47505. doi: 10.1371/journal.pone.0047505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Jafri M.A., Ansari S.A., Alqahtani M.H., Shay J.W. Roles of telomeres and telomerase in cancer, and advances in telomerase-targeted therapies. Genome Med. 2016;8:69. doi: 10.1186/s13073-016-0324-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Sanford S.L., Welfer G.A., Freudenthal B.D., Opresko P.L. Mechanisms of telomerase inhibition by oxidized and therapeutic dNTPs. Nat. Commun. 2020;11:5288. doi: 10.1038/s41467-020-19115-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Kinloch-De Loës S., Hirschel B.J., Hoen B., Cooper D.A., Tindall B., Carr A., Saurat J.H., Clumeck N., Lazzarin A., Mathiesen L. A controlled trial of zidovudine in primary human immunodeficiency virus infection. N. Engl. J. Med. 1995;333:408–413. doi: 10.1056/NEJM199508173330702. [DOI] [PubMed] [Google Scholar]
- 123.Flexner C. HIV-protease inhibitors. N. Engl. J. Med. 1998;338:1281–1292. doi: 10.1056/NEJM199804303381808. [DOI] [PubMed] [Google Scholar]
- 124.Blanco J.L., Whitlock G., Milinkovic A., Moyle G. HIV integrase inhibitors: A new era in the treatment of HIV. Expert Opin. Pharmacother. 2015;16:1313–1324. doi: 10.1517/14656566.2015.1044436. [DOI] [PubMed] [Google Scholar]
- 125.Shi S., Zheng H.C., Zhang Z.G. Roles of Fascin mRNA expression in colorectal cancer: Meta-analysis and bioinformatics analysis. Mol. Clin. Oncol. 2020;13:119–128. doi: 10.3892/mco.2020.2069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Tampakis A., Tampaki E.C., Nonni A., Kostakis I.D., Posabella A., Kontzoglou K., von Flue M., Felekouras E., Kouraklis G., Nikiteas N. High fascin-1 expression in colorectal cancer identifies patients at high risk for early disease recurrence and associated mortality. BMC Cancer. 2021;21:153. doi: 10.1186/s12885-021-07842-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Cunha B.A., Sibley C.M., Ristuccia A.M. Doxycycline. Ther. Drug Monit. 1982;4:115–135. doi: 10.1097/00007691-198206000-00001. [DOI] [PubMed] [Google Scholar]
- 128.Jung J.J., Razavian M., Kim H.Y., Ye Y., Golestani R., Toczek J., Zhang J., Sadeghi M.M. Matrix metalloproteinase inhibitor, doxycycline and progression of calcific aortic valve disease in hyperlipidemic mice. Sci. Rep. 2016;6:32659. doi: 10.1038/srep32659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Komatsu S., Moriya S., Che X.F., Yokoyama T., Kohno N., Miyazawa K. Combined treatment with SAHA, bortezomib, and clarithromycin for concomitant targeting of aggresome formation and intracellular proteolytic pathways enhances ER stress-mediated cell death in breast cancer cells. Biochem. Biophys. Res. Commun. 2013;437:41–47. doi: 10.1016/j.bbrc.2013.06.032. [DOI] [PubMed] [Google Scholar]
- 130.Nakamura M., Kikukawa Y., Takeya M., Mitsuya H., Hata H. Clarithromycin attenuates autophagy in myeloma cells. Int. J. Oncol. 2010;37:815–820. [PubMed] [Google Scholar]
- 131.Mokarram P., Albokashy M., Zarghooni M., Moosavi M.A., Sepehri Z., Chen Q.M., Hudecki A., Sargazi A., Alizadeh J., Moghadam A.R., et al. New frontiers in the treatment of colorectal cancer: Autophagy and the unfolded protein response as promising targets. Autophagy. 2017;13:781–819. doi: 10.1080/15548627.2017.1290751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Burada F., Nicoli E.R., Ciurea M.E., Uscatu D.C., Ioana M., Gheonea D.I. Autophagy in colorectal cancer: An important switch from physiology to pathology. World J. Gastrointest. Oncol. 2015;7:271–284. doi: 10.4251/wjgo.v7.i11.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Zhanel G.G., Fontaine S., Adam H., Schurek K., Mayer M., Noreddin A.M., Gin A.S., Rubinstein E., Hoban D.J. A Review of New Fluoroquinolones: Focus on their Use in Respiratory Tract Infections. Treat. Respir. Med. 2006;5:437–465. doi: 10.2165/00151829-200605060-00009. [DOI] [PubMed] [Google Scholar]
- 134.Barradell L.B., Fitton A. Artesunate. A review of its pharmacology and therapeutic efficacy in the treatment of malaria. Drugs. 1995;50:714–741. doi: 10.2165/00003495-199550040-00009. [DOI] [PubMed] [Google Scholar]
- 135.Efferth T., Sauerbrey A., Olbrich A., Gebhart E., Rauch P., Weber H.O., Hengstler J.G., Halatsch M.E., Volm M., Tew K.D., et al. Molecular modes of action of artesunate in tumor cell lines. Mol. Pharmacol. 2003;64:382–394. doi: 10.1124/mol.64.2.382. [DOI] [PubMed] [Google Scholar]
- 136.Bai L., Xu Z., Huang C., Sui Y., Guan X., Shi L. Psychotropic medication utilisation in adult cancer patients in China: A cross-sectional study based on national health insurance database. Lancet Reg. Health West. Pac. 2020;5:100060. doi: 10.1016/j.lanwpc.2020.100060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Ng C.G., Boks M.P., Smeets H.M., Zainal N.Z., de Wit N.J. Prescription patterns for psychotropic drugs in cancer patients; a large population study in the Netherlands. Psychooncology. 2013;22:762–767. doi: 10.1002/pon.3056. [DOI] [PubMed] [Google Scholar]
- 138.Friedmann I., Atmaca A., Chow K.U., Jager E., Weidmann E. Synergistic effects of valproic acid and mitomycin C in adenocarcinoma cell lines and fresh tumor cells of patients with colon cancer. J. Chemother. 2006;18:415–420. doi: 10.1179/joc.2006.18.4.415. [DOI] [PubMed] [Google Scholar]
- 139.Mologni L., Cleris L., Magistroni V., Piazza R., Boschelli F., Formelli F., Gambacorti-Passerini C. Valproic acid enhances bosutinib cytotoxicity in colon cancer cells. Int. J. Cancer. 2009;124:1990–1996. doi: 10.1002/ijc.24158. [DOI] [PubMed] [Google Scholar]
- 140.Göttlicher M., Minucci S., Zhu P., Krämer O.H., Schimpf A., Giavara S., Sleeman J.P., Lo Coco F., Nervi C., Pelicci P.G., et al. Valproic acid defines a novel class of HDAC inhibitors inducing differentiation of transformed cells. EMBO J. 2001;20:6969–6978. doi: 10.1093/emboj/20.24.6969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Benfield P., Heel R.C., Lewis S.P. Fluoxetine. A review of its pharmacodynamic and pharmacokinetic properties, and therapeutic efficacy in depressive illness. Drugs. 1986;32:481–508. doi: 10.2165/00003495-198632060-00002. [DOI] [PubMed] [Google Scholar]
- 142.Sehgal S.N. Sirolimus: Its discovery, biological properties, and mechanism of action. Transplant. Proc. 2003;35:7S–14S. doi: 10.1016/S0041-1345(03)00211-2. [DOI] [PubMed] [Google Scholar]
- 143.Hernández-Lemus E., Martínez-García M. Pathway-Based Drug-Repurposing Schemes in Cancer: The Role of Translational Bioinformatics. Front. Oncol. 2020;10:605680. doi: 10.3389/fonc.2020.605680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Fu L., Jin W., Zhang J., Zhu L., Lu J., Zhen Y., Zhang L., Ouyang L., Liu B., Yu H. Repurposing non-oncology small-molecule drugs to improve cancer therapy: Current situation and future directions. Acta Pharm. Sin. B. 2021;12:532–557. doi: 10.1016/j.apsb.2021.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Pushpakom S., Iorio F., Eyers P.A., Escott K.J., Hopper S., Wells A., Doig A., Guilliams T., Latimer J., McNamee C., et al. Drug repurposing: Progress, challenges and recommendations. Nat. Rev. Drug Discov. 2019;18:41–58. doi: 10.1038/nrd.2018.168. [DOI] [PubMed] [Google Scholar]
- 146.Wu P., Feng Q., Kerchberger V.E., Nelson S.D., Chen Q., Li B., Edwards T.L., Cox N.J., Phillips E.J., Stein C.M., et al. Integrating gene expression and clinical data to identify drug repurposing candidates for hyperlipidemia and hypertension. Nat. Commun. 2022;13:46. doi: 10.1038/s41467-021-27751-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Zhang L., Chen C., Fu J., Lilley B., Berlinicke C., Hansen B., Ding D., Wang G., Wang T., Shou D., et al. Large-scale phenotypic drug screen identifies neuroprotectants in zebrafish and mouse models of retinitis pigmentosa. eLife. 2021;10:e57245. doi: 10.7554/eLife.57245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Oprea T.I., Bauman J.E., Bologa C.G., Buranda T., Chigaev A., Edwards B.S., Jarvik J.W., Gresham H.D., Haynes M.K., Hjelle B., et al. Drug Repurposing from an Academic Perspective. Drug Discov. Today Ther. Strateg. 2011;8:61–69. doi: 10.1016/j.ddstr.2011.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Neuberger A., Oraiopoulos N., Drakeman D.L. Renovation as innovation: Is repurposing the future of drug discovery research? Drug Discov. Today. 2019;24:1–3. doi: 10.1016/j.drudis.2018.06.012. [DOI] [PubMed] [Google Scholar]
- 150.Martinez M.A. Lack of Effectiveness of Repurposed Drugs for COVID-19 Treatment. Front. Immunol. 2021;12:635371. doi: 10.3389/fimmu.2021.635371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Abdullah M.I., de Wolf E., Jawad M.J., Richardson A. The poor design of clinical trials of statins in oncology may explain their failure—Lessons for drug repurposing. Cancer Treat Rev. 2018;69:84–89. doi: 10.1016/j.ctrv.2018.06.010. [DOI] [PubMed] [Google Scholar]