Abstract
We conducted a systematic review and meta-analysis of randomized clinical trials and pilot trial studies to compare the effectiveness of intermittent fasting (IF) and continuous calorie restriction (CCR) in overweight and obese people. The parameters included body mass index (BMI), body weight, and other metabolism-related indicators. A systematic search in PubMed, Embase, Cochrane Library, and Web of Science was conducted up to January 2022. Standardized mean differences (SMDs) with 95% confidence intervals (CIs) were used to measure the effectiveness. Publication bias was assessed using Egger’s test. The stability of the results was evaluated using sensitivity analyses. The significance of body weight change (SMD = −0.21, 95% CI (−0.40, −0.02) p = 0.028) was more significant after IF than CCR. There was no significant difference in BMI (SMD = 0.02, 95% CI (−0.16, 0.20) p = 0.848) between IF and CCR. These findings suggest that IF may be superior to CCR for weight loss in some respects.
Keywords: intermittent fasting, calorie restriction, energy control, BMI, body weight, meta-analysis
1. Introduction
Compared to 173 million obese people in 2014, 257 million adults worldwide (6% of men and 9% of women) are predicted to be living with severe obesity, showing a rapid increase in the number of obese people [1]. Obesity is now replacing malnutrition and infectious diseases as the most critical cause of suboptimal health. Obesity has been linked to diabetes, coronary heart disease, cancer, metabolic syndrome, and sleep-disordered breathing [2]. In addition, obesity can also cause the elevation of oxidative stress, inflammatory state, and hypoxia, which leads to the dysfunction of perivascular adipose tissue (PVAT) [3,4].
Metabolic syndrome is also a growing concern characterized by pathological metabolism of protein, fat, carbohydrates, and other substances; it is a risk factor for diabetes, cardiovascular, and cerebrovascular diseases [5]. The amount and quality of many types of cells found in adipose tissue, including adipose stem cells (ASC), is altered as a result of obesity. These changes in the function and nature of ASC impair adipose tissue remodeling and adipose tissue function, leading to metabolic disorders [6]. The common causes of these diseases are insulin resistance and hyperinsulinemia secondary to obesity, especially central obesity [7].
Most obese people rarely choose to exercise because of work stress or psychological reasons; they are more enthusiastic about dietary intervention. Dietary adjustment is the heart of obesity treatment. Weight loss diets include various permutations of energy restriction, macronutrients, and food and dietary intake patterns [8]. In recent years, various dietary adjustment methods have become increasingly popular. Current guidelines recommend continuous calorie restriction (CCR; about 500 or 750 kcal of energy deficiency per day, or 30% of baseline energy requirements limits) and comprehensive lifestyle interventions as the cornerstone of obesity treatments [9]. On average, this method produces moderate weight loss (5–10% ≥ 1 year) [9].
Because traditional CCR methods are relatively ineffective in achieving and sustaining weight loss, there has been growing interest in identifying alternative dietary weight-loss strategies that limit the energy intake to specific periods of the day or extend the gap between meals (i.e., intermittent calorie restriction, ICR) [10]. Intermittent fasting (IF) comes in many forms and includes regular breaks. A common form of IF includes fasting once or twice a week for up to 24 h, followed by discretionary food intake for the remainder of the day, known variously as periodic long-term fasting, ICR, intermittent energy restriction (IER) [11], time-restricted eating (TRE, i.e., eating only for 8 h and then fasting for another 16 h a day), and alternate-day fasting (ADF) [12]. However, it is not yet certain whether TRE has the same health effects as other forms of IF [10,13]; therefore, we omitted TRE in this study.
Continuous fasting has become widespread in daily life, and intermittent fasting has become increasingly popular. Intermittent fasting is a dietary pattern alternating between normal energy and energy restriction (or complete fasting) and has attracted substantial attention from scholars [14]. IF reduces body mass and improves glucose and lipid metabolism. Its benefits include reducing the risk of diabetes, cardiovascular disease, and stroke, inhibiting tumor growth, and preventing Alzheimer’s disease and Parkinson’s disease [15].
A study discovered that IF might be comparable to, but not superior to, CCR for weight loss and metabolic illness prevention [10]. However, another study suggested that IF is a more effective strategy in managing the body weight, fat mass, and waist circumference of individuals with metabolic syndrome [16]. These authors found that, compared with CCR, IF decreased the levels of high-sensitivity C-reactive protein and prothrombin and thromboplastin times. A review suggested that IF might be superior to CCR because it helps conserve lean body mass at the expense of fat mass [17]. A growing body of evidence suggests that IF has more benefits and can be more effective than CCR. Nevertheless, IF versus CCR on weight loss in overweight and obese people remains controversial.
At present, there are a variety of obesity evaluation indicators in the home and abroad; the most commonly used are: body mass index (BMI in kg/m2), body fat rate (body fat percentage, BF%), waist circumference (WC), body weight (BW), etc. Among them, BMI is widely used to evaluate generalized obesity. The BF% is widely applied to evaluate the proportion of body fat, WC is widely used to evaluate valence abdominal obesity, and BW is mainly used to evaluate abdominal obesity and health risk. Therefore, our research mainly looked at the BMI, BW, WC, etc.
Because of the growing concern regarding obesity and the diseases it causes, a literature review was carried out to compare these weight-loss strategies. Therefore, our study aimed to compare IF and CCR regarding effectiveness for weight loss in people with obesity or metabolic syndrome.
2. Materials and Methods
Our meta-analysis was based on the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines [18].
2.1. Data Sources and Search Strategy
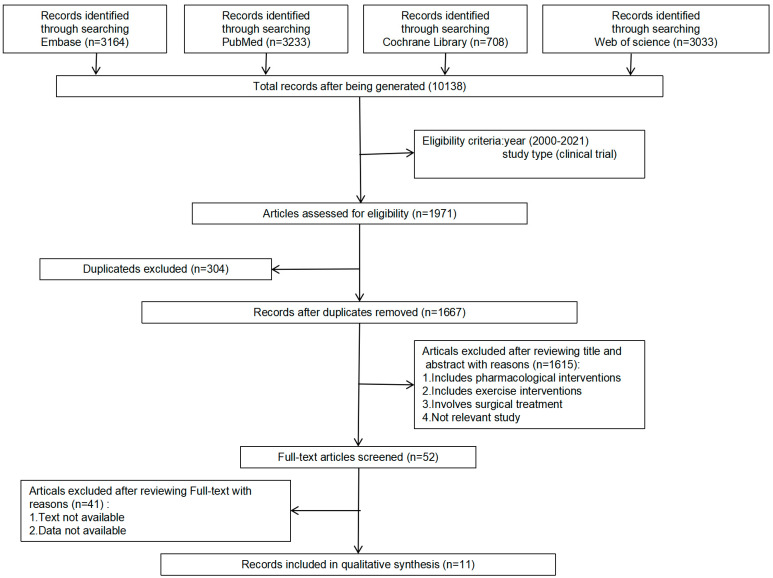
Four significant websites were used to compile our data (PubMed, Embase, Cochrane Library, and Web of Science). The search terms used for the studies were two sets of keywords and their main subtitles, including calorie restriction (“intermittent calorie restriction”, “intermittent energy restriction”, “intermittent fasting”, and “alternate day fasting”) and BMI (“body mass index”, “body weight”, “weight loss”, “weight gain”, “fat mass”, “obesity”, “overweight”, “insulin-resistance”, and “insulin sensitivity”). The date range was 1 January 2000, to 1 February 2022. More details are shown in Figure 1.
Figure 1.
Flow chart of literature search.
2.2. Study Selection and Criteria
Studies were eligible if they met the following criteria: (1) studies of adults (≥18 years old) with overweight or obesity based on BMI (≥25 kg/m2); (2) studies comparing nutritional interventions for weight loss based on IF; (3) studies comparing nutritional interventions for weight loss based on CCR; (4) studies describing body weight loss and modifications of body composition; (5) studies published in English; (6) subjects of original articles ≥10.
Exclusion criteria were as follows: (1) studies with unreliable designs or substantial statistical errors; (2) only one type of diet regimen included; (3) inability to access the full text.
2.3. Data Extraction and Quality Assessment
Two independent reviewers reviewed all the studies and extracted the data in a standardized format. The articles in the database were retrieved based on the data measured at the end of each study, and we extracted the most complete and recent data based on the articles from the same population. The information collected was as follows: first author, publication year, country, study design, participants, study duration, age, BMI, body weight, fat mass, waist, fasting blood glucose, and interventions. The data were converted to unified units as needed. We did not include interventions such as exercise and drugs to avoid affecting the effectiveness of our evaluation.
We compared IF with CCR, without restriction on the treatment history. The outcomes were as follows: change in BMI between baseline and the end of intervention, and change in body weight between baseline and the end of the intervention.
For randomized clinical trials, we used the Cochrane methodology to assess the quality [19] (Supplementary Figures S1 and S2).
2.4. Data Synthesis and Analysis
The comparison between IF and CCR was analyzed using the random-effects model, which used mean values and standard deviations. Continuous variables were analyzed using standard mean difference (SMD) and 95% confidence intervals (CIs). We utilized Cochran’s (chi-square) test to measure heterogeneity and the I2 statistic to determine the extent of consistency: an I2 of over 75% indicates a high level of inconsistency, I2 of above 50% is moderate, and I2 of below 25% is low [20]. To estimate pooled effect sizes, random effects models were used. A two-sided p-value of less than 0.05 was considered statistically significant. Publication bias was assessed using Begg’s test [21] and Egger’s test [22].
We conducted influence analysis to determine the impact of a single study on the overall results. Subgroup analysis was performed according to the intermittent fasting regimen, age, and area. All statistical analyses were carried out using RevMan (Version 5.3) and Stata Software (Version 12.0).
3. Results
3.1. Literature Search
The details of the search are shown in Figure 1. A total of 10,138 potential reports were identified from PubMed, Embase, Cochrane Library, and Web of Science. Based on the year of publication and the type of study, we included 1971 articles. After re-examination, 304 duplicated studies were deleted. After reviewing the titles and abstracts, 1615 nonconforming studies were excluded. After reviewing the full texts, 41 studies that did not meet the requirements were excluded. Finally, eleven studies met the selection criteria [23,24,25,26,27,28,29,30,31,32,33].
3.2. Study Characteristics
We included 11 articles with 705 patients. The studies’ characteristics are displayed in Table 1 and Table 2. The 11 studies were primarily randomized controlled trials. The BMIs of all participants were more than 25 kg/m2, and some of the patients were diagnosed with type 2 diabetes mellitus or metabolic syndrome. Eight studies compared IF with CCR [23,25,26,27,28,29,31,33], two compared ADF with CCR [30,32], one compared CCR with twice-weekly fasting (i.e., on any two non-consecutive days of the week, girls only ate 500 kcal per day and boys only ate 600 kcal per day. On the other five days, the subjects ate normally, but did not overeat or diet) [24]. ICR, ADF, and twice-weekly fasting are all forms of IF. All studies included data on BMI and weight. All dietary intervention methods met the standard criteria, and data measurements were ensured to minimize errors. The studies included regular follow-up to ensure accuracy. All subjects were above 30 years old.
Table 1.
Characteristics of included studies.
| Author | Year | Country | N | Study Design | Participants | Study Duration | Interventions | Age, y | Body Weight, kg | BMI, kg/m2 | Waist, cm | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Carter et al. | 2016 | Australia | 63 | a pragmatic pilot trial | adults with overweight or obesity | 12 weeks | IER vs. CER | IER | 61 ± 7.5 | 99 ± 16 | 35 ± 4.8 | - |
| CER | 62 ± 9.1 | 99 ± 15 | 36 ± 5.2 | - | ||||||||
| Conley et al. | 2018 | Australia | 24 | a randomised pilot stugy | obese war veterans | 6 months | twice-weekly vs. CCR | twice-weekly | 68 ± 2.7 | 99.1 ± 7.9 | 33.4 ± 1.8 | 114.2 ± 5.2 |
| CCR | 67.1 ± 3.9 | 107.3 ± 17.1 | 36.2 ± 4.3 | 122.5 ± 10.4 | ||||||||
| Sundfor et al. | 2018 | Norway | 112 | RCT | adults with metabolic syndrome | 6 months | IER vs. CER | IER | 49.9 ± 10.1 | 108.6 ± 16.3 | 35.1 ± 3.9 | 116 ± 10 |
| CER | 47.5 ± 11.6 | 107.5 ± 16.1 | 35.3 ± 3.5 | 116 ± 10 | ||||||||
| Schübel et al. | 2018 | Germany | 150 | RCT | overweight or obese nonsmokers | 48 weeks | ICR vs. CCR | ICR | 49.4 ± 9.0 | 96.4 ± 15.8 | 32.0 ± 3.8 | - |
| CCR | 50.0 ± 8.0 | 92.5 ± 15.7 | 31.2 ± 4.0 | - | ||||||||
| Byrne et al. | 2018 | Australia | 51 | RCT | men with obesity | 16 weeks | ICR vs. CCR | ICR | 39.9 ± 9.2 | 109.8 ± 14.1 | 39.7 ± 6.8 | - |
| CCR | 39.3 ± 6.6 | 111.6 ± 10.0 | 38.9 ± 5.2 | - | ||||||||
| Carter et al. | 2019 | Australia | 137 | RCT | adults with type 2 diabetes | 12 months | IER vs. CER | IER | 61 ± 9.0 | 100 ± 19 | 35 ± 5.8 | - |
| CER | 61 ± 9.2 | 102 ± 17 | 37 ± 5.7 | - | ||||||||
| Jimenez et al. | 2019 | Spain | 42 | RCT | adults with overweight or obesity | 6 weeks | ICR vs. CCR | ICR | 46.32 ± 8.03 | 92.21 ± 13.82 | 32.83 ± 3.73 | 106.24 ± 11.89 |
| CCR | 47.88 ± 7.67 | 97.99 ± 18.05 | 35.92 ± 5.32 | 110.49 ± 14.17 | ||||||||
| Parvaresh et al. | 2019 | Iran | 70 | RCT | adults with metabolic syndrome | 8 weeks | ADF vs. CCR | ADF | 44.6 ± 9.08 | 86.7 ± 10.65 | 31.1 ± 3.35 | 101 ± 9.41 |
| CCR | 46.4 ± 7.94 | 84.2 ± 12.21 | 31.6 ± 3.82 | 103 ± 12.92 | ||||||||
| Steger et al. | 2021 | USA | 35 | RCT | adults with overweight or obesity | 12 weeks | IER vs. CER | IER | 43.4 ± 11 | 87.4 ± 11.5 | 31.1 ± 2.4 | 94.2 ± 8.8 |
| CER | 48 ± 10 | 91.0 ± 9.7 | 31.4 ± 2.5 | 95.9 ± 9.3 | ||||||||
| Maroofi et al. | 2020 | Iran | 88 | RCT | subjects with overweight or obesity and mild-to-moderate HTG | 8 weeks | ICR vs. CCR | ICR | 44.0 ± 8.6 | 83.9 ± 13.7 | 31.6 ± 3.9 | 100.6 ± 9.8 |
| CCR | 45.2 ± 11.7 | 90.1 ± 19.3 | 32.4 ± 4.6 | 104.7 ± 11.0 | ||||||||
| Razavi et al. | 2021 | Iran | 80 | RCT | adults with metabolic syndrome | 4 months | ADF vs. CCR | ADF | 41.3 ± 8.65 | 89.4 ± 7.72 | 31.3 ± 3.12 | 106 ± 9.71 |
| CCR | 43.1 ± 9.26 | 87.1 ± 8.17 | 31.2 ± 3.95 | 104 ± 10.2 |
Data presented as means ± standard error of the mean. RCT, randomized clinical trials. HTG, hypertriglyceridemia. IER, intermittent energy restriction. CER, continuous energy restriction. ICR, intermittent calorie restriction. CCR, continuous calorie restriction. ADF, alternate-day fasting. BMI, body mass index.
Table 2.
Characteristics of included studies.
| Author | Year | Country | Interventions | Fat Mass, kg | Percentage Fat Mass (%) | TC | TG | FBG | Insulin, IU/L | SBP, mmhg | DBP, mmhg | HOMA-IR | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Carter et al. | 2016 | Australia | IER vs. CER | IER | 38 ± 9.2 | 41 ± 7.9 | - | - | - | - | 134 ± 17 | 84 ± 10 | - |
| CER | 40 ± 10.5 | 42 ± 7.7 | - | - | - | - | 138 ± 15 | 90 ± 11 | - | ||||
| Conley et al. | 2018 | Australia | twice-weekly vs. CCR | twice-weekly | - | - | 3.9 ± 0.9 (mmol/L) | 1.9 ± 0.6 (mmol/L) | - | - | 141.5 ± 13.9 | 84.0 ± 9.5 | - |
| CCR | - | - | 4.3 ± 1.0 (mmol/L) | 2.4 ± 1.7 (mmol/L) | - | - | 149.8 ± 18.3 | 88.1 ± 14.4 | - | ||||
| Sundfor et al. | 2018 | Norway | IER vs. CER | IER | - | - | 4.87 ± 0.90 (mmol/L) | 1.84 ± 0.83 (mmol/L) | 5.8 ± 1.2 (mmol/L) | - | 129 ± 13.4 | 88 ± 8.1 | - |
| CER | - | - | 5.09 ± 0.87 (mmol/L) | 1.55 ± 0.68 (mmol/L) | 5.7 ± 0.7 (mmol/L) | - | 128 ± 13.2 | 86 ± 8.7 | - | ||||
| Schübel et al. | 2018 | Germany | ICR vs. CCR | ICR | - | - | 205.0 ± 30.8 (mg/dL) | 130.0 ± 83.8 (mg/dL) | 92.7 ± 7.5 (mg/dL) | 11.6 ± 5.4 | 139.4 ± 18.7 | 136.0 ± 16.7 | 2.7 ± 1.3 |
| CCR | - | - | 202.9 ± 39.3 (mg/dL) | 121.2 ± 66.3 (mg/dL) | 93.9 ± 7.5 (mg/dL) | 12.6 ± 6.9 | 87.2 ± 9.9 | 87.3 ± 8.7 | 3.0 ± 1.7 | ||||
| Byrne et al. | 2018 | Australia | ICR vs. CCR | ICR | 44.1 ± 11.5 | 39.7 ± 6.8 | - | - | - | - | - | - | - |
| CCR | 43.6 ± 8.5 | 38.9 ± 5.2 | - | - | - | - | - | - | - | ||||
| Carter et al. | 2019 | Australia | IER vs. CER | IER | 40 ± 9.4 | 42 ± 7.3 | 4.6 ± 1.3 (mmol/L) | 1.5 ± 0.7 (mmol/L) | - | 14 ± 20 | - | - | - |
| CER | 42 ± 9.1 | 44 ± 6.6 | 5.0 ± 1.7 (mmol/L) | 1.9 ± 1.4 (mmol/L) | - | 14 ± 21 | - | - | - | ||||
| Jimenez et al. | 2019 | Spain | ICR vs. CCR | ICR | - | 40.76 ± 6.61 | - | - | - | - | - | - | - |
| CCR | - | 44.51 ± 6.40 | - | - | - | - | - | - | - | ||||
| Parvaresh et al. | 2019 | Iran | ADF vs. CCR | ADF | - | - | 177 ± 36.52 (mg/dL) | 199 ± 108.29 (mg/dL) | 102 ± 9.17 (mg/dL) | 13.07 ± 6.34 | 125 ± 9.78 | 84 ± 9.35 | 3.33 ± 1.69 |
| CCR | - | - | 177 ± 37.17 (mg/dL) | 218 ± 115.10 (mg/dL) | 101 ± 7.58 (mg/dL) | 14.28 ± 6.79 | 127 ± 14.03 | 83 ± 6.61 | 3.49 ± 1.86 | ||||
| Steger et al. | 2021 | USA | IER vs. CER | IER | 37.9 ± 6.8 | 45.0 ± 4.7 | - | - | - | - | 119 ± 14 | 70 ± 11 | - |
| CER | 41.5 ± 7.6 | 47.4 ± 6.3 | - | - | - | - | 123 ± 10 | 74 ± 10 | - | ||||
| Maroofi et al. | 2020 | Iran | ICR vs. CCR | ICR | - | 37.5 ± 4.6 | 178.6 ± 30.3 (mg/dL) | 180.5 ± 115 (mg/dL) | - | 18.2 ± 8.1 | - | - | 3.5 ± 3 |
| CCR | - | 35.9 ± 5.8 | 190.1 ± 38.1 (mg/dL) | 165.0 ± 126 (mg/dL) | - | 22.0 ± 9.7 | - | - | 3.7 ± 3 | ||||
| Razavi et al. | 2021 | Iran | ADF vs. CCR | ADF | 37.1 ± 9.25 | - | - | - | - | - | 134 ± 9 | 86 ± 4 | - |
| CCR | 34.2 ± 9.80 | - | - | - | - | - | 137 ± 10 | 85 ± 5 | - |
Data presented as means ± standard error of the mean. IER, intermittent energy restriction. CER, continuous energy restriction. ICR, intermittent calorie restriction. CCR, continuous calorie restriction. ADF, alternate-day fasting. TC, total cholesterol. TG, triacylglycerol. FBG, fasting blood glucose. SBP, systolic blood pressure. DBP, diastolic blood pressure.
3.3. Meta-Analysis
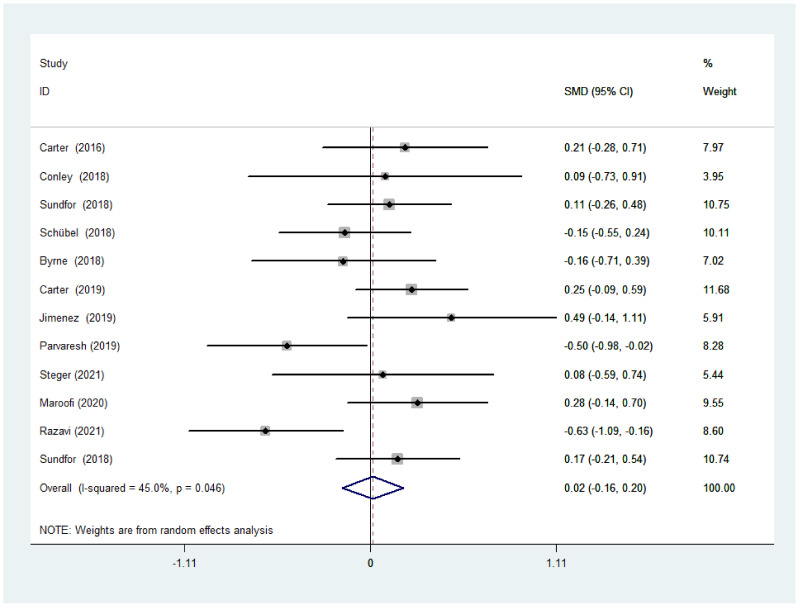
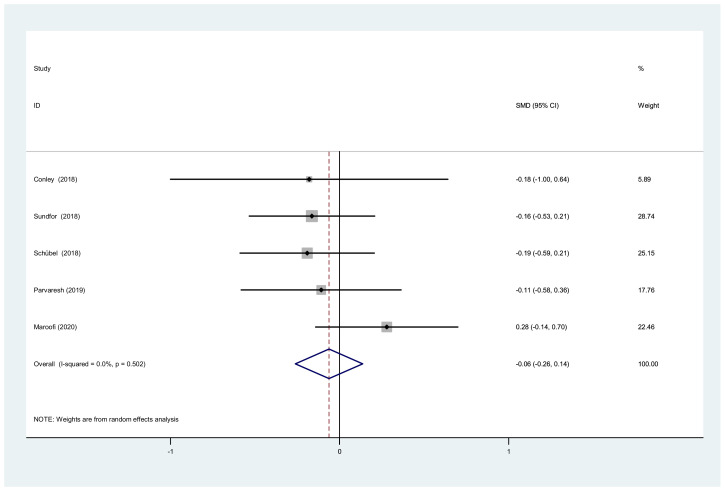
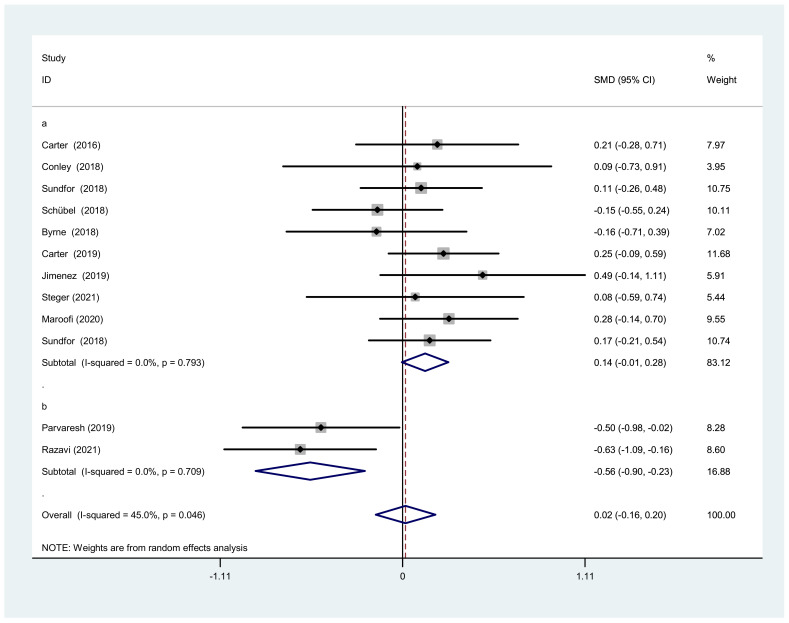
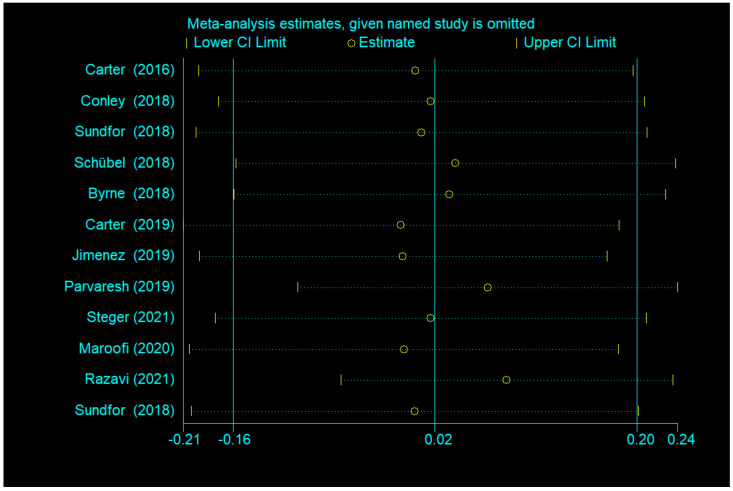
3.3.1. BMI after IF versus CCR
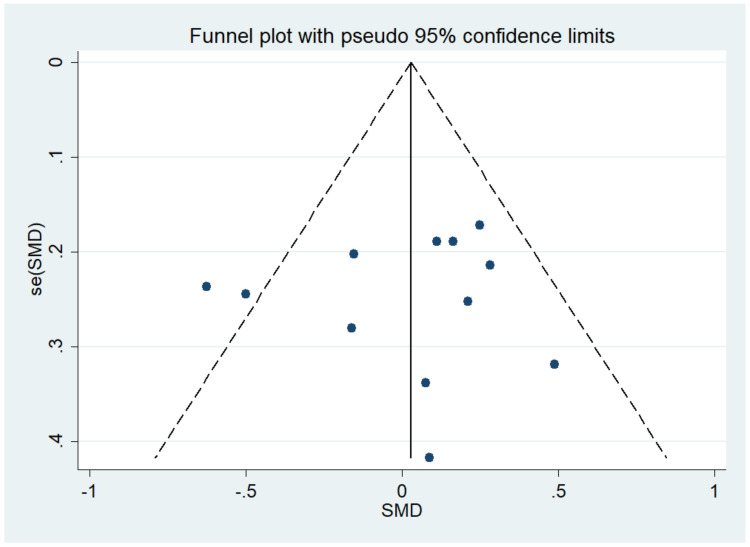
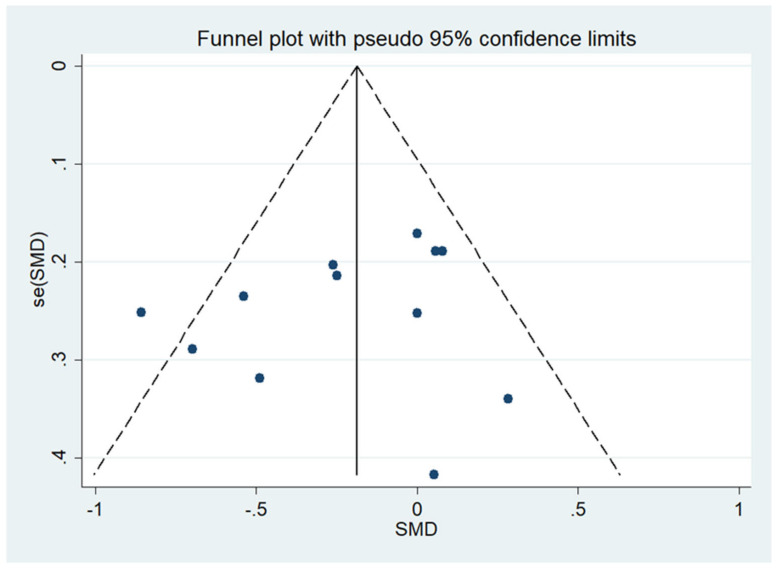
There was no significant difference between IF and CCR for BMI (SMD = 0.02, 95% CI (−0.16, 0.20) p = 0.848; Figure 2). The SMD showed no significant heterogeneity using the random-effect model (I2 = 45.0%, p = 0.046). Publication bias was insignificant (Supplementary Figure S1; Egger’s test: p = 0.730). The funnel plot is shown in Figure 3.
Figure 2.
The weighted mean difference in BMI (kg/m2) between the IF and CCR (SD: standard deviation; CI: confidence interval).
Figure 3.
The funnel plot of the publication bias of BMI.
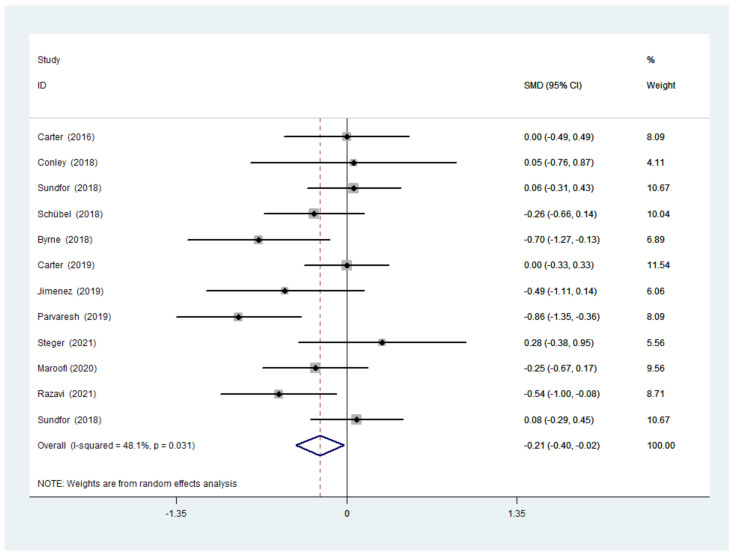
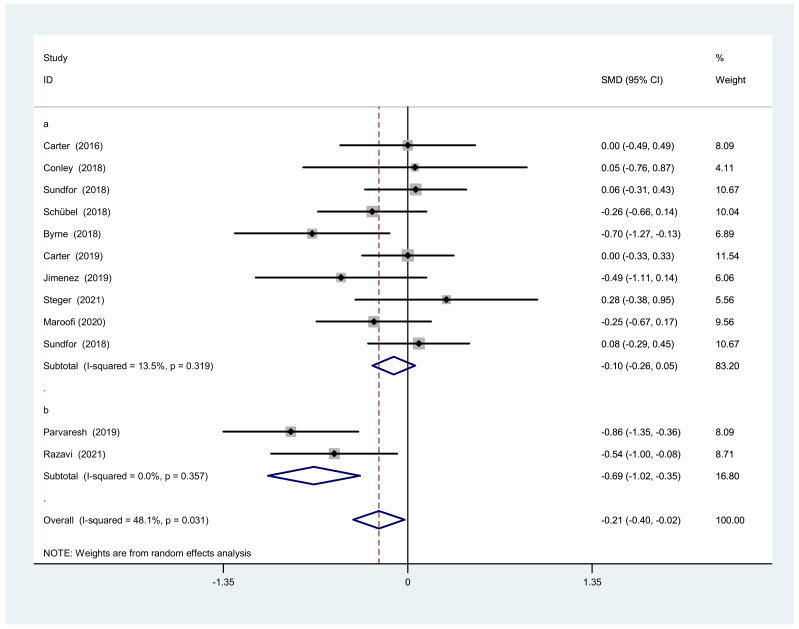
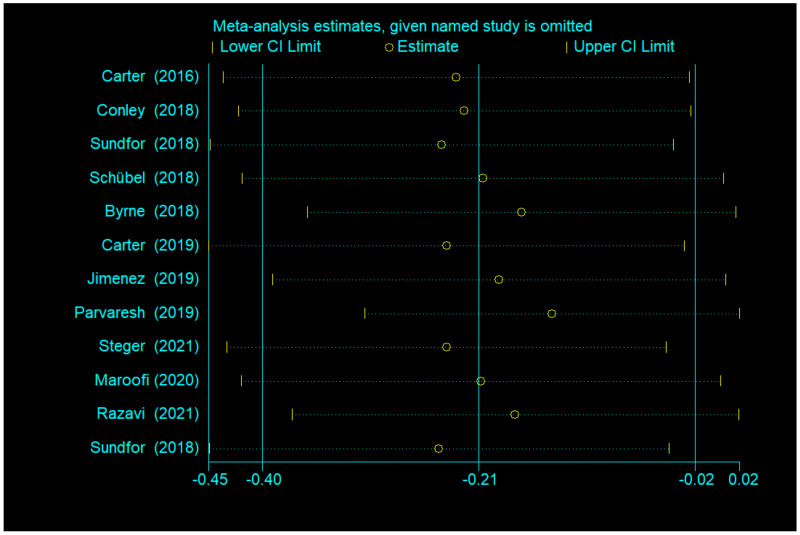
3.3.2. Body Weight after IF Versus CCR
There was a significant difference between IF and CCR for weight (SMD = −0.21, 95% CI (−0.40, −0.02) p = 0.028; Figure 4). The SMD showed no significant heterogeneity using a random-effect model (I2 = 48.1%, p = 0.031). Publication bias was insignificant (Supplementary Figure S1; Egger’s test: p = 0.401). The funnel plot is shown in Figure 5.
Figure 4.
The weighted mean difference in body weight (kg) between the IF and CCR (SD: standard deviation; CI: confidence interval).
Figure 5.
The funnel plot of the publication bias of body weight.
3.3.3. TC, TG and Waist Circumference after IF versus CCR
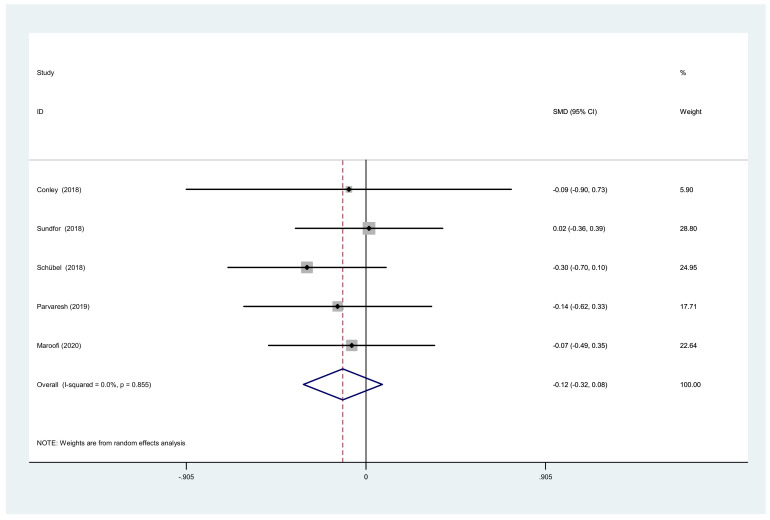
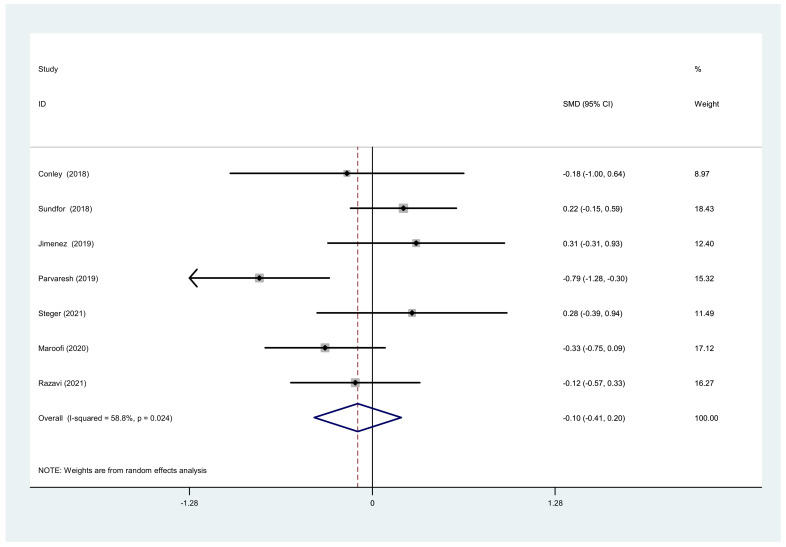
We also analyzed the total cholesterol, triacylglycerol, and waist circumference. There was a significant difference between IF and CCR for the total cholesterol (SMD = −0.06, 95% CI (−0.26, 0.14) p = 0.538; Figure 6). The SMD showed no heterogeneity using a random-effect model (I2 = 0%, p = 0.502). There was a significant difference between IF and CCR for triacylglycerol (SMD = −0.12, 95% CI (−0.32, 0.08) p = 0.252; Figure 7). The SMD showed no heterogeneity using a random-effect model (I2 = 0%, p = 0.855). There was a significant difference between IF and CCR for waist circumference (SMD = −0.10, 95% CI (−0.41, 0.20) p = 0.508; Figure 8). The SMD showed no heterogeneity using a random-effect model (I2 = 58.8%, p = 0.024).
Figure 6.
Forest plot of meta-analysis on comparing TC changes after IF and CCR interventions.
Figure 7.
Forest plot of meta-analysis on comparing TG changes after IF and CCR interventions.
Figure 8.
Forest plot of meta-analysis on comparing waist changes after IF and CCR interventions.
3.4. Subgroup Analysis
3.4.1. Subgroup Analysis of BMI
We conducted a subgroup analysis because of the moderate heterogeneity of BMI change in the overall analysis. We found that the different IF forms accounted for the heterogeneity between IF and CCR. Therefore, all studies were divided into modified ADF and normal IF. Two studies with modified ADF showed significant differences between IF and CCR (SMD = −0.56, 95% CI: −0.90 to −0.23, I2 = 0%, p = 0.709), while the remaining studies with normal IF showed no significance (SMD = 0.14, 95% CI: −0.01 to 0.28, I2 = 0.0%, p = 0.059) (Figure 9). Because both sets of heterogeneity were zero, we deduced that the form of IF was the source of heterogeneity.
Figure 9.
Forest plot of BMI changes after IF and CCR interventions based on fasting days. (a) Normal intermittent fasting (calorie restriction is usually two days per week). (b) Modified alternate-day fasting (a very lowcalorie diet (75% energy restriction) during the three fast days).
We carried out other subgroup analyses classified by age (≥60 y, <60 y), area (Oceania, Europe, Western Asia, North America), and physical condition (obesity or overweight, obesity or overweight with disease) (Table 3). These factors showed no significant differences or reductions in heterogeneity. More information is needed for further analysis.
Table 3.
Subgroups analyses of comparison of IF and CCR based on BMI changes.
| Groups | Participants | Random Effect SMD (95% CI) | I2 (%) | p for Heterogeneity | |
|---|---|---|---|---|---|
| Over all | 12 | 905 | 0.02 (−0.16, 0.20) | 45 | 0.046 |
| Subgroup analysis | |||||
| Age | |||||
| ≥60 y | 3 | 223 | 0.22 (−0.04, 0.49) | 0 | 0.937 |
| <60 y | 9 | 682 | −0.04 (−0.27, 0.18) | 53.2 | 0.029 |
| Area | |||||
| Oceania | 4 | 274 | 0.15 (−0.09, 0.39) | 0 | 0.651 |
| Europe | 4 | 364 | 0.10 (−0.11, 0.31) | 5.5 | 0.366 |
| Western Asia | 3 | 232 | −0.27 (−0.85, 0.31) | 79.4 | 0.008 |
| North America | 1 | 35 | 0.08 (−0.59, 0.74) | ||
| Physical condition | |||||
| Obesity or overweight with disease | 6 | 593 | 0.05 (−0.18, 0.27) | 0 | 0.568 |
| Obesity or overweight | 6 | 312 | −0.03 (−0.32, 0.27) | 68.9 | 0.007 |
3.4.2. Subgroup Analysis of Body Weight
Because of the moderate heterogeneity of body weight change in the overall analysis, we conducted a subgroup analysis. We performed the same analysis as the BMI sub-group research. Two studies of modified ADF fasting showed that IF was more effective than CCR (SMD = −0.69, 95% CI: −1.02 to −0.23, I2 = 0%, p = 0.357). Nine studies of normal IF showed no significant difference between IF and CCR (SMD = −0.10, 95% CI: −0.26 to 0.05, I2 = 13.5%, p = 0.319) (Figure 10).
Figure 10.
Forest plot of body weight changes after IF and CCR interventions based on fasting days. (a) Normal intermittent fasting (calorie restriction is usually two days per week). (b) Modified alternate-day fasting (a very low-calorie diet (75% energy restriction) during the three fast days).
We carried out other subgroup analyses classified by age (≥60 y, <60 y), area (Oceania, Europe, Western Asia, North America), and physical condition (obesity or overweight, obesity or overweight with disease) (Table 4). No statistical significance was found for these factors.
Table 4.
Subgroups analyses of comparison of IF and CCR based on body weight changes.
| Groups | Participants | Random Effect SMD (95% CI) | I2 (%) | p for Heterogeneity | |
|---|---|---|---|---|---|
| Over all | 12 | 905 | −0.21 (−0.40, −0.02) | 48.1 | 0.031 |
| Subgroup analysis | |||||
| Age | |||||
| ≥60 y | 3 | 223 | 0.01 (−0.26, 0.27) | 0 | 0.993 |
| <60 y | 9 | 682 | −0.28 (−0.52, −0.05) | 56.6 | 0.018 |
| Area | |||||
| Oceania | 4 | 274 | −0.15 (−0.48, 0.18) | 38.9 | 0.178 |
| Europe | 4 | 364 | −0.09 (−0.32, 0.14) | 18.5 | 0.298 |
| Western Asia | 3 | 232 | −0.53 (−0.87, −0.19) | 41.1 | 0.183 |
| North America | 1 | 35 | 0.28 (−0.38, 0.95) | ||
| Physical condition | |||||
| Obesity or overweight with disease | 6 | 593 | −0.21 (−0.48, 0.06) | 27.3 | 0.23 |
| Obesity or overweight | 6 | 312 | −0.22 (−0.50, 0.06) | 64.8 | 0.014 |
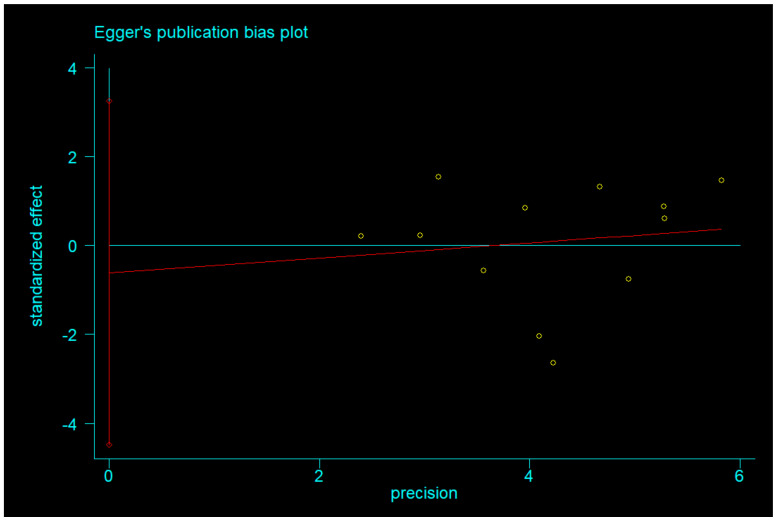
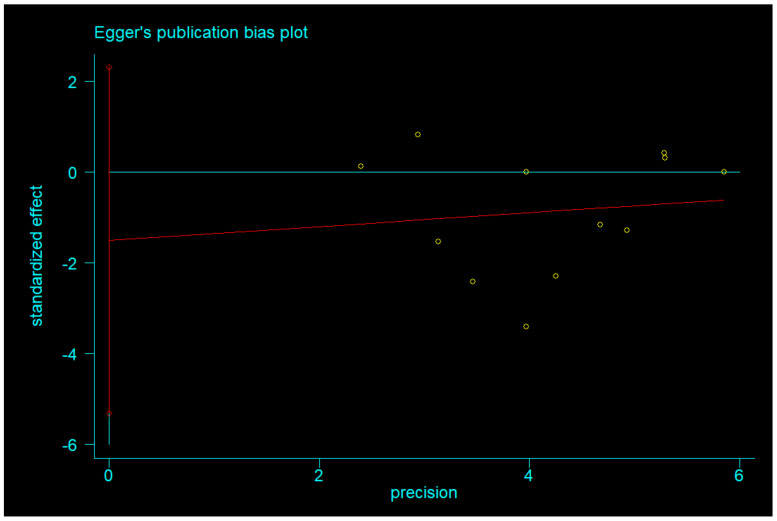
3.4.3. Publication Bias and Sensitivity Analysis
Egger’s test was used to measure publication bias (p = 0.730 for BMI and p = 0.401 for body weight). Meta-analysis of articles included in this study revealed no publication bias (Figure 11 and Figure 12). The stability of our meta-analysis was demonstrated by the sensitivity analysis (Figure 13 and Figure 14).
Figure 11.
Egger’s publication bias plot of BMI.
Figure 12.
Egger’s publication bias plot of body weight.
Figure 13.
Impact analysis of a single study based on BMI.
Figure 14.
Impact analysis of a single study based on body weight.
4. Discussion
We performed a systematic review and meta-analysis comparing IF and CCR regimens regarding BMI and body weight reduction. IF is beneficial for weight loss, and the effect was significant. If dietary intervention is well studied, it will substantially impact society. Our findings are consistent with those of Enríquez Guerrero et al. [34].
Calorie restriction involves reduced caloric intake of about 25–30% without eliminating essential nutrients [35]; this approach prolongs health and life in rodent and primate models [36,37]. The mechanisms of these benefits are related to the inhibition of anabolism, improvement of mitochondrial energy metabolism, and the conversion of substrate utilization. These processes are related to the reduced dependence on glucose metabolism and increased fatty acid oxidation [35]. IF is an effective dietary intervention because it improves the lipid profile and reduces body weight [38]. IF has a positive effect on glycolipid metabolism in obese individuals. A study showed that eight consecutive weeks of ADF in obese adults led to a 6.8% reduction in blood glucose levels after fasting and a 22.6% reduction in insulin concentrations [12]. ADF improved insulin signaling and altered the proportion of α and β cells in obese mouse pancreases by reducing β cell apoptosis, increasing Akt (serine/threonine) phosphorylation, and improving diet-induced obesity islet tissue remodeling and β cell function [39]. IF improved glucose homeostasis through autophagy in a rodent model; TRE promoted the expression of glycolytic genes (Hk2, PFK, and PK) in obese mice and inhibited the expression of gluconeogenesis (G6pc, Pck1, and Fbp1), thereby promoting glucose uptake in peripheral tissues, and inhibited gluconeogenesis, ultimately reducing the blood glucose levels [40]. IF regulates glucose homeostasis by the intestinal flora [41]. ADF improves blood lipid levels whilst reducing the body mass and body weight, related to the depletion of liver glycogen reserves during fasting; triglyceride levels indicated that free fatty acids are released into liver cells to produce ketone energy [42]. IF (1 day of fasting followed by 2 days of feeding) promotes browning of white adipose tissue; the possible mechanisms include the activation of type II cell signaling through increasing the secretion of IL-5, stimulation of M2 macrophages, and reduction of M1/M2 macrophage ratios [43].
In addition to its positive effects of fasting, side effects are inevitable, such as muscle pain, sleep disturbances, headaches, and hunger, occurring mainly in the first few days of fasting [44]. In the group with longer fasting periods, baseline values for emotional well-being (EWB) and physical well-being (PWB) were lower [44]. These side effects of fasting do not occur for all people because of different physical fitness levels, including personal health, physiological mechanisms, lifestyle, etc.
Identifying long-term effective dietary interventions is critical to reducing the range of diseases caused by obesity [45]. Many people lead sedentary lifestyles because of office work, and exercise may be challenging. Therefore, dietary interventions are becoming more popular.
Elevated BMI is correlated with disease prevalence, suggesting that reducing BMI will reduce the disease burden. Epidemiological studies showed that elevated BMI could cause cardiovascular disease, diabetes mellitus, chronic kidney disease [46,47], cancers [48], and musculoskeletal disorders [49,50]. In the studies we considered, all subjects had BMIs greater than 25 kg/m2. Our meta-analysis found that IF and CCR improved BMI, and weights decreased significantly. While our analysis showed no difference between the two interventions for improvement in BMI, we can draw some inferences from the analysis. Of the eleven studies, seven showed a relatively significant decrease in BMI with CCR [23,24,25,28,29,31,33], and four showed a relatively significant decrease with IF [26,27,30,32]; however, the differences in these comparisons were relatively small. In the analysis of BMI, heterogeneity was 45% (moderate). The source of heterogeneity was different fasting days of IF. Therefore, we suspect that the weight loss effect is more significant when the number of fasting days in a week is greater than two.
We considered age as a possible source of heterogeneity. The heterogeneity of three studies, including subjects older than 60, was zero. Age is correlated with BMI to some extent [51]; as people age, their BMI increases. We speculate that CCR may be more appropriate in older people, especially the elderly. Their autoimmunity is relatively low, they require food to replenish energy, and their ability to endure hunger is relatively weak. Because their bodies have poor metabolic capacity, extremely low-calorie restriction throughout the day can be harmful. Therefore, persistent calorie restriction is a safer dietary intervention for them. This view was also mentioned in a review [52]. Studies showed that ADF did not produce superior adherence to daily calorie restriction [53]. In previous studies on other forms of IF, abandonment was reported in up to 40% of participants [54]. Therefore, future studies should determine the appropriate dietary intervention method according to the population and individual wishes.
We also analyzed changes in body weight. As articulated in the results, the differences in weight between the two interventions showed significance. The analysis showed that IF was more effective for weight loss. This finding suggests that IF requires further study and in-depth exploration. The weight loss effect of IF has been demonstrated in clinical trials. A strict IF of 4 to 24 weeks reduced subject body mass by 4–10% [55]. Other scholars pointed out that the role of IF in weight loss is not significantly different from that of a calorie-restricted diet, consistent with our analysis; however, IF was better at maintaining lean body mass [17].
11 May was declared World Obesity Day by the World Health Organization. Today, obesity is no longer merely a threat to individual health; it is also a social problem that has attracted worldwide attention for over 30 years, as overweight and obesity continues to grow. All sectors of society should work together to create a healthy environment that supports the active adoption of healthy lifestyles.
IF and CCR have powerful weight loss effects. Although weight and fat mass decreased in most studies, it is crucial to consider protocol adherence and exit rates. Sundfør et al. showed that IF subjects were hungrier than CCR subjects, and their willingness to persist decreased [56]. However, IF also offers some benefits. There are several studies on the effects of IF on cardiovascular disease in humans. A rat study found that IF improved glycemic control and protected the myocardium from ischemia-induced cell damage and inflammation more than daily CR [57]. These findings suggest that IF has substantial clinical significance, and it is a dietary intervention method that deserves in-depth research.
Our meta-analysis has some limitations. Firstly, the sample sizes of some of the included studies were small, leading to heterogeneity. More largescale studies are necessary to enhance the accuracy of our meta-analysis. Second, the follow-up time varied widely, and some did not follow-up.
In our study, it seems that ADF produces better results. More research is therefore needed to assess the mechanism of intermittent fasting regimens, and the safety of each type of them is also to be valued to finally determine applicable dietary interventions for specific groups of people.
In summary, we found that IF was more effective than CCR for weight loss; however, there was no difference in BMI improvement. Although the data are insufficient, our study shows that IF is superior to CCR in metabolism in obese people. We hope that there will be more long-term studies of dietary interventions and further investigation on cognitive function, which may reduce the economic burdens caused by obesity. Studies need to compare IF and CCR with controlled patient characters to confirm the effectiveness of these weight-loss methods and to determine whether IF is more appropriate for specific populations.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu14091781/s1, Figure S1. Risk of bias graph: review authors’ judgements about each risk of bias item presented as percentages across all included studies. Figure S2. Risk of bias summary: review authors’ judgements about each risk of bias item for each included study.
Author Contributions
Q.Z. designed the work and wrote the manuscript. Q.Z. and C.Z. collected the data and conducted data analysis. H.W., D.L., Z.M., X.G., Y.L., Y.F. and M.C. reviewed and edited the manuscript. J.D. had full access over all data in the study and is ultimately responsible for the decision to submit and publish the final version. All authors contributed to the article and approved the submitted version. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by two grants (to J.D.) from the National Natural Science Foundation of China (No. 31872791) and Natural Science Foundation of Shandong Province of China (No. ZR2019MC046).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cignarella F., Cantoni C., Ghezzi L., Salter A., Dorsett Y., Chen L., Phillips D., Weinstock G.M., Fontana L., Cross A.H., et al. Intermittent Fasting Confers Protection in CNS Autoimmunity by Altering the Gut Microbiota. Cell Metab. 2018;27:1222–1235.e1226. doi: 10.1016/j.cmet.2018.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kopelman P.G. Obesity as a medical problem. Nature. 2000;404:635–643. doi: 10.1038/35007508. [DOI] [PubMed] [Google Scholar]
- 3.Stanek A., Brożyna-Tkaczyk K., Myśliński W. The Role of Obesity-Induced Perivascular Adipose Tissue (PVAT) Dysfunction in Vascular Homeostasis. Nutrients. 2021;13:3843. doi: 10.3390/nu13113843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xia N., Li H. The role of perivascular adipose tissue in obesity-induced vascular dysfunction. Br. J. Pharmacol. 2017;174:3425–3442. doi: 10.1111/bph.13650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eckel R.H., Grundy S.M., Zimmet P.Z. The metabolic syndrome. Lancet. 2005;365:1415–1428. doi: 10.1016/S0140-6736(05)66378-7. [DOI] [PubMed] [Google Scholar]
- 6.Shin S., El-Sabbagh A.S., Lukas B.E., Tanneberger S.J., Jiang Y. Adipose stem cells in obesity: Challenges and opportunities. Biosci. Rep. 2020;40:BSR20194076. doi: 10.1042/BSR20194076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Samson S.L., Garber A.J. Metabolic syndrome. Endocrinol. Metab. Clin. N. Am. 2014;43:1–23. doi: 10.1016/j.ecl.2013.09.009. [DOI] [PubMed] [Google Scholar]
- 8.Chao A.M., Quigley K.M., Wadden T.A. Dietary interventions for obesity: Clinical and mechanistic findings. J. Clin. Investig. 2021;131:e140065. doi: 10.1172/JCI140065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jensen M.D., Ryan D.H., Apovian C.M., Ard J.D., Comuzzie A.G., Donato K.A., Hu F.B., Hubbard V.S., Jakicic J.M., Kushner R.F., et al. Tomaselli, 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J. Am. Coll. Cardiol. 2014;63:2985–3023. doi: 10.1016/j.jacc.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 10.Rynders C.A., Thomas E.A., Zaman A., Pan Z., Catenacci V.A., Melanson E.L. Effectiveness of Intermittent Fasting and Time-Restricted Feeding Compared to Continuous Energy Restriction for Weight Loss. Nutrients. 2019;11:2442. doi: 10.3390/nu11102442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.St-Onge M.P., Ard J., Baskin M.L., Chiuve S.E., Johnson H.M., Kris-Etherton P., Varady K. Meal Timing and Frequency: Implications for Cardiovascular Disease Prevention: A Scientific Statement From the American Heart Association. Circulation. 2017;135:e96–e121. doi: 10.1161/CIR.0000000000000476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Varady K.A., Bhutani S., Church E.C., Klempel M.C. Short-term modified alternate-day fasting: A novel dietary strategy for weight loss and cardioprotection in obese adults. Am. J. Clin. Nutr. 2009;90:1138–1143. doi: 10.3945/ajcn.2009.28380. [DOI] [PubMed] [Google Scholar]
- 13.Longo V.D., Panda S. Fasting, Circadian Rhythms, and Time-Restricted Feeding in Healthy Lifespan. Cell Metab. 2016;23:1048–1059. doi: 10.1016/j.cmet.2016.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Anton S.D., Moehl K., Donahoo W.T., Marosi K., Lee S.A., Mainous A.G., 3rd, Leeuwenburgh C., Mattson M.P. Flipping the Metabolic Switch: Understanding and Applying the Health Benefits of Fasting. Obesity. 2018;26:254–268. doi: 10.1002/oby.22065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de Cabo R., Mattson M.P. Effects of Intermittent Fasting on Health, Aging, and Disease. N. Engl. J. Med. 2019;381:2541–2551. doi: 10.1056/NEJMra1905136. [DOI] [PubMed] [Google Scholar]
- 16.Schübel R., Graf M.E., Nattenmüller J., Nabers D., Sookthai D., Gruner L.F., Johnson T., Schlett C.L., von Stackelberg O., Kirsten R., et al. The effects of intermittent calorie restriction on metabolic health: Rationale and study design of the HELENA Trial. Contemp. Clin. Trials. 2016;51:28–33. doi: 10.1016/j.cct.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 17.Varady K.A. Intermittent versus daily calorie restriction: Which diet regimen is more effective for weight loss? Obes. Rev. 2011;12:e593–e601. doi: 10.1111/j.1467-789X.2011.00873.x. [DOI] [PubMed] [Google Scholar]
- 18.Moher D., Shamseer L., Clarke M., Ghersi D., Liberati A., Petticrew M., Shekelle P., Stewart L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015;4:1. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Higgins J.P., Altman D.G., Gøtzsche P.C., Jüni P., Moher D., Oxman A.D., Savovic J., Schulz K.F., Weeks L., Sterne J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bowden J., Tierney J.F., Copas A.J., Burdett S. Quantifying, displaying and accounting for heterogeneity in the meta-analysis of RCTs using standard and generalised Q statistics. BMC Med. Res. Methodol. 2011;11:41. doi: 10.1186/1471-2288-11-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Begg C.B., Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. doi: 10.2307/2533446. [DOI] [PubMed] [Google Scholar]
- 22.Egger M., Smith G.D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carter S., Clifton P.M., Keogh J.B. The effect of intermittent compared with continuous energy restriction on glycaemic control in patients with type 2 diabetes: 24-month follow-up of a randomised noninferiority trial. Diabetes Res. Clin. Pract. 2019;151:11–19. doi: 10.1016/j.diabres.2019.03.022. [DOI] [PubMed] [Google Scholar]
- 24.Conley M., Fevre L.L., Haywood C., Proietto J. Is two days of intermittent energy restriction per week a feasible weight loss approach in obese males? A randomised pilot study. Nutr. Diet. 2018;75:65–72. doi: 10.1111/1747-0080.12372. [DOI] [PubMed] [Google Scholar]
- 25.Sundfør T.M., Svendsen M., Tonstad S. Effect of intermittent versus continuous energy restriction on weight loss, maintenance and cardiometabolic risk: A randomized 1-year trial. Nutr. Metab. Cardiovasc. Dis. NMCD. 2018;28:698–706. doi: 10.1016/j.numecd.2018.03.009. [DOI] [PubMed] [Google Scholar]
- 26.Schübel R., Nattenmüller J., Sookthai D., Nonnenmacher T., Graf M.E., Riedl L., Schlett C.L., von Stackelberg O., Johnson T., Nabers D., et al. Effects of intermittent and continuous calorie restriction on body weight and metabolism over 50 wk: A randomized controlled trial. Am. J. Clin. Nutr. 2018;108:933–945. doi: 10.1093/ajcn/nqy196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Byrne N.M., Sainsbury A., King N.A., Hills A.P., Wood R.E. Intermittent energy restriction improves weight loss efficiency in obese men: The MATADOR study. Int. J. Obes. 2018;42:129–138. doi: 10.1038/ijo.2017.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carter S., Clifton P.M., Keogh J.B. The effects of intermittent compared to continuous energy restriction on glycaemic control in type 2 diabetes; a pragmatic pilot trial. Diabetes Res. Clin. Pract. 2016;122:106–112. doi: 10.1016/j.diabres.2016.10.010. [DOI] [PubMed] [Google Scholar]
- 29.Jimenez A.M., Oliva S.L., Vilar E.G., de Cuevillas B., Moreno M.D.C.M., de Prado J.G., Diaz E.A., Martin I.S.M. The Mediterranean diet pattern with intermittent semi-fasting may facilitate weight loss: Randomised controlled trial. Mediterr. J. Nutr. Metab. 2019;12:153–161. doi: 10.3233/MNM-180257. [DOI] [Google Scholar]
- 30.Parvaresh A., Razavi R., Abbasi B., Yaghoobloo K., Hassanzadeh A., Mohammadifard N., Safavi S.M., Hadi A., Clark C.C.T. Modified alternate-day fasting vs. calorie restriction in the treatment of patients with metabolic syndrome: A randomized clinical trial. Complement. Ther. Med. 2019;47:102187. doi: 10.1016/j.ctim.2019.08.021. [DOI] [PubMed] [Google Scholar]
- 31.Steger F.L., Donnelly J.E., Hull H.R., Li X., Hu J., Sullivan D.K. Intermittent and continuous energy restriction result in similar weight loss, weight loss maintenance, and body composition changes in a 6 month randomized pilot study. Clin. Obes. 2021;11:e12430. doi: 10.1111/cob.12430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Razavi R., Parvaresh A., Abbasi B., Yaghoobloo K., Hassanzadeh A., Mohammadifard N., Clark C.C.T., Safavi S.M. The alternate-day fasting diet is a more effective approach than a calorie restriction diet on weight loss and hs-CRP levels. Int. J. Vitam. Nutr. Res. 2021;91:242–250. doi: 10.1024/0300-9831/a000623. [DOI] [PubMed] [Google Scholar]
- 33.Maroofi M., Nasrollahzadeh J. Effect of intermittent versus continuous calorie restriction on body weight and cardiometabolic risk markers in subjects with overweight or obesity and mild-to-moderate hypertriglyceridemia: A randomized trial. Lipids Health Dis. 2020;19:216. doi: 10.1186/s12944-020-01399-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guerrero A.E., Martín I.S.M., Vilar E.G., Martín M.A.C. Effectiveness of an intermittent fasting diet versus continuous energy restriction on anthropometric measurements, body composition and lipid profile in overweight and obese adults: A meta-analysis. Eur. J. Clin. Nutr. 2021;75:1024–1039. doi: 10.1038/s41430-020-00821-1. [DOI] [PubMed] [Google Scholar]
- 35.Pignatti C., D’Adamo S., Stefanelli C., Flamigni F., Cetrullo S. Nutrients and Pathways that Regulate Health Span and Life Span. Geriatrics. 2020;5:95. doi: 10.3390/geriatrics5040095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Davis T.A., Bales C.W., Beauchene R.E. Differential effects of dietary caloric and protein restriction in the aging rat. Exp. Gerontol. 1983;18:427–435. doi: 10.1016/0531-5565(83)90021-9. [DOI] [PubMed] [Google Scholar]
- 37.Masoro E.J., Iwasaki K., Gleiser C.A., McMahan C.A., Seo E.J., Yu B.P. Dietary modulation of the progression of nephropathy in aging rats: An evaluation of the importance of protein. Am. J. Clin. Nutr. 1989;49:1217–1227. doi: 10.1093/ajcn/49.6.1217. [DOI] [PubMed] [Google Scholar]
- 38.Santos H.O., Macedo R.C.O. Impact of intermittent fasting on the lipid profile: Assessment associated with diet and weight loss. Clin. Nutr. ESPEN. 2018;24:14–21. doi: 10.1016/j.clnesp.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 39.Marinho T.S., Borges C.C., Aguila M.B., Mandarim-de-Lacerda C.A. Intermittent fasting benefits on alpha- and beta-cell arrangement in diet-induced obese mice pancreatic islet. J. Diabetes Its Complicat. 2020;34:107497. doi: 10.1016/j.jdiacomp.2019.107497. [DOI] [PubMed] [Google Scholar]
- 40.Martinez-Lopez N., Tarabra E., Toledo M., Garcia-Macia M., Sahu S., Coletto L., Batista-Gonzalez A., Barzilai N., Pessin J.E., Schwartz G.J., et al. System-wide Benefits of Intermeal Fasting by Autophagy. Cell Metab. 2017;26:856–871.e855. doi: 10.1016/j.cmet.2017.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Beli E., Yan Y., Moldovan L., Vieira C.P., Gao R., Duan Y., Prasad R., Bhatwadekar A., White F.A., Townsend S.D., et al. Restructuring of the Gut Microbiome by Intermittent Fasting Prevents Retinopathy and Prolongs Survival in db/db Mice. Diabetes. 2018;67:1867–1879. doi: 10.2337/db18-0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ng G.Y., Kang S.W., Kim J., Alli-Shaik A., Baik S.H., Jo D.G., Hande M.P., Sobey C.G., Gunaratne J., Fann D.Y., et al. Genome-Wide Transcriptome Analysis Reveals Intermittent Fasting-Induced Metabolic Rewiring in the Liver. Dose-Response. 2019;17:1559325819876780. doi: 10.1177/1559325819876780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kim K.H., Kim Y.H., Son J.E., Lee J.H., Kim S., Choe M.S., Moon J.H., Zhong J., Fu K., Lenglin F., et al. Intermittent fasting promotes adipose thermogenesis and metabolic homeostasis via VEGF-mediated alternative activation of macrophage. Cell Res. 2017;27:1309–1326. doi: 10.1038/cr.2017.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.de Toledo F.W., Grundler F., Bergouignan A., Drinda S., Michalsen A. Safety, health improvement and well-being during a 4 to 21-day fasting period in an observational study including 1422 subjects. PLoS ONE. 2019;14:e0209353. doi: 10.1371/journal.pone.0209353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tobias D.K., Chen M., Manson J.E., Ludwig D.S., Willett W., Hu F.B. Effect of low-fat diet interventions versus other diet interventions on long-term weight change in adults: A systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2015;3:968–979. doi: 10.1016/S2213-8587(15)00367-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Singh G.M., Danaei G., Farzadfar F., Stevens G.A., Woodward M., Wormser D., Kaptoge S., Whitlock G., Qiao Q., Lewington S., et al. The age-specific quantitative effects of metabolic risk factors on cardiovascular diseases and diabetes: A pooled analysis. PLoS ONE. 2013;8:e65174. doi: 10.1371/journal.pone.0065174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wormser D., Kaptoge S., di Angelantonio E., Wood A.M., Pennells L., Thompson A., Sarwar N., Kizer J.R., Lawlor D.A., Nordestgaard B.G., et al. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: Collaborative analysis of 58 prospective studies. Lancet. 2011;377:1085–1095. doi: 10.1016/S0140-6736(11)60105-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lauby-Secretan B., Scoccianti C., Loomis D., Grosse Y., Bianchini F., Straif K. Body Fatness and Cancer—Viewpoint of the IARC Working Group. N. Engl. J. Med. 2016;375:794–798. doi: 10.1056/NEJMsr1606602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jiang L., Rong J., Wang Y., Hu F., Bao C., Li X., Zhao Y. The relationship between body mass index and hip osteoarthritis: A systematic review and meta-analysis. Jt. Bone Spine. 2011;78:150–155. doi: 10.1016/j.jbspin.2010.04.011. [DOI] [PubMed] [Google Scholar]
- 50.Jiang L., Tian W., Wang Y., Rong J., Bao C., Liu Y., Zhao Y., Wang C. Body mass index and susceptibility to knee osteoarthritis: A systematic review and meta-analysis. Jt. Bone Spine. 2012;79:291–297. doi: 10.1016/j.jbspin.2011.05.015. [DOI] [PubMed] [Google Scholar]
- 51.Kocur P., Tomczak M., Wiernicka M., Goliwąs M., Lewandowski J., Łochyński D. Relationship between age, BMI, head posture and superficial neck muscle stiffness and elasticity in adult women. Sci. Rep. 2019;9:8515. doi: 10.1038/s41598-019-44837-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sung M.M., Dyck J.R. Age-related cardiovascular disease and the beneficial effects of calorie restriction. Heart Fail. Rev. 2012;17:707–719. doi: 10.1007/s10741-011-9293-8. [DOI] [PubMed] [Google Scholar]
- 53.Trepanowski J.F., Kroeger C.M., Barnosky A., Klempel M.C., Bhutani S., Hoddy K.K., Gabel K., Freels S., Rigdon J., Rood J., et al. Effect of Alternate-Day Fasting on Weight Loss, Weight Maintenance, and Cardioprotection Among Metabolically Healthy Obese Adults: A Randomized Clinical Trial. JAMA Intern. Med. 2017;177:930–938. doi: 10.1001/jamainternmed.2017.0936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Antoni R., Johnston K.L., Collins A.L., Robertson M.D. Investigation into the acute effects of total and partial energy restriction on postprandial metabolism among overweight/obese participants. Br. J. Nutr. 2016;115:951–959. doi: 10.1017/S0007114515005346. [DOI] [PubMed] [Google Scholar]
- 55.Freire R. Scientific evidence of diets for weight loss: Different macronutrient composition, intermittent fasting, and popular diets. Nutrition. 2020;69:110549. doi: 10.1016/j.nut.2019.07.001. [DOI] [PubMed] [Google Scholar]
- 56.Sundfør T.M., Tonstad S., Svendsen M. Effects of intermittent versus continuous energy restriction for weight loss on diet quality and eating behavior. A randomized trial. Eur. J. Clin. Nutr. 2019;73:1006–1014. doi: 10.1038/s41430-018-0370-0. [DOI] [PubMed] [Google Scholar]
- 57.Wan R., Ahmet I., Brown M., Cheng A., Kamimura N., Talan M., Mattson M.P. Cardioprotective effect of intermittent fasting is associated with an elevation of adiponectin levels in rats. J. Nutr. Biochem. 2010;21:413–417. doi: 10.1016/j.jnutbio.2009.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article.