Abstract
Food insecurity (FI) is one of the major causes of malnutrition and is associated with a range of negative health outcomes in low and middle-income countries. The burden of FI in southern Africa is unknown, although FI continues to be a major public health problem across sub-Saharan Africa as a whole. Therefore, this review sought to identify empirical studies that related FI to health outcomes among adults in southern Africa. Altogether, 14 publications using diverse measures of FI were reviewed. The majority of the studies measured FI using modified versions of the United States Department of Agriculture Household Food Security Survey Module. A wide range in prevalence and severity of FI was reported (18–91%), depending on the measurement tool and population under investigation. Furthermore, FI was mostly associated with hypertension, diabetes, anxiety, depression and increased risk of human immunodeficiency virus (HIV) acquisition. Based on the findings, future research is needed, especially in countries with as yet no empirical studies on the subject, to identify and standardize measures of FI suitable for the southern African context and to inform public health policies and appropriate interventions aiming to alleviate FI and potentially improve health outcomes in the region.
Keywords: food insecurity, health outcomes, measurement, southern Africa
1. Introduction
Food insecurity (FI) continues to be one of the major causes of malnutrition in low and middle income countries (LMICs) [1]. The definition of FI is either as lack of nutritionally adequate and safe food or as limited ability to acquire food in socially acceptable ways [2]. It encompasses four hierarchical dimensions: availability, accessibility, utilization and stability [3,4]. “Availability” refers to sufficient quantities of quality food for an active and healthy life [4] and includes food production and distribution [5]. “Accessibility” refers to economic or physical resources for acquiring food [4] and includes affordability and preference [6]. “Utilization” refers to the intake of sufficient and safe food and includes the physical, social and human resources to transform food into meals [4], as well as societal values [6]. The dimension “stability” recognizes that FI can be transitory and cyclic or chronic [4] because of climate change, conflict, job loss, disease and other factors that can disrupt any one of the first three dimensions [7].
According to a report by FAO et al. [8] (p. 4), about 256.1 million people (20% of the total population) in Africa are undernourished; of these, 239.1 million live in sub-Saharan Africa. Within the sub-Saharan African region, the southern African countries continue to have the lowest burden of undernourishment (5.3 million), while eastern Africa has the highest burden in terms of numbers (133.1 million). In southern Africa, the latest UN World Food Programme (WFP)’s Hunger Map [9] puts South Africa, Namibia and Mauritius in the best position, with a prevalence of undernourishment between 5% and 14.9%, while Madagascar emerges as the country with the highest prevalence (>35%); no WFP data are available for Zimbabwe and Zambia. According to the report by FAO et al. [8] (p. 51), climate change, conflict and economic slowdowns and downturns are the major causes of FI in the region and its sub-regions. Poverty, socioeconomic disparities, social exclusion and rapid population growth also play a significant part in the rise in FI. At the household level, most research from LMICs gives poor extension services (e.g., lack of dissemination of relevant information needed to boost food production, particularly on farming methods and techniques including adequate funding and introduction of improved varieties of crops and breeds of animals), climate change, large family size, poverty (due to low income or unemployment) [10] and instability in government policies or poor governance as the major causes of FI [10,11]. Other causes include: lack of or inadequate access to productive resources, fluctuations in food availability and access, high food prices, diseases and pest infestations [10,12].
Research evidence from LMICs has found an association between FI and negative health outcomes. In children, FI has been associated with decreased academic performance, decreased emotional and intellectual development, delayed development of motor skills, poor general health, iron deficiency anaemia [13], underweight and obesity [1] and stunting [14]. In adults, it has been associated with diabetes, hypertension [15,16], anxiety, depression and suicide ideation [17,18] and other negative health outcomes [16,19], including intimate partner violence perpetration [20,21]. In Africa, a systematic review by Trudell et al. [22] found that FI was associated with poor mental health, depending on specific characteristics of study population. The authors of the review called for further research to include populations at risk to better understand the factors that could mediate the found relationship in order to inform policies and appropriate interventions [22]. Furthermore, in another review carried out in sub-Saharan Africa on the relationship between FI and key risk factors for diet-sensitive non-communicable diseases (NCDs), Nkambule et al. [23] found that FI was associated with dyslipidaemia, hypertension and overweight, especially among women. In the review, Nkambule and colleagues argued for the need to address FI as an integral component of diet-sensitive NCDs prevention programmes [23].
There is a dearth of systematic reviews on FI and health outcomes in southern Africa. For instance, a systematic review by Haines et al. [24] on risk factors for depression in people living with HIV (PLHIV) found that FI was one of the key risk factors, and thus FI needed to be considered when developing appropriate interventions to improve antiretroviral therapy (ART) outcomes [24].
Given the potential implications of FI for health outcomes, it becomes crucial to fully understand the major dimensions of FI as well as to know which instrument is most appropriate to measure FI and its dimensions [2]. Many researchers rely on the United States Department of Agriculture (USDA) Household Food Security Survey Module (HFSSM) for data on household FI. The HFSSM is an 18-item, self-report household measure of uncertain, insufficient or inadequate food access, availability and utilization, which assesses the food security (FS) situation of adults and children in a household over the past 12 months [2,7]. One limitation of this instrument is that it was designed to capture mostly financial constraints, poor resources and compromised eating patterns and consumption [7]. According to Webb et al. [7], however, the HFSSM, with some modification, is a valid instrument and has been widely used in countries across America. Based on the USDA instrument and the Latin American and Caribbean Food Security Scale (ELCSA), the FAO has developed and validated the Food Insecurity Experience Scale (FIES) for global use [25].
The burden of FI including its major determinants in some countries of the southern African region is not well known, and there is also a lack of systematic reviews. Therefore, this paper sought to review studies that empirically examined the relationship between FI and health outcomes among adults in southern Africa. The following question was sought: in which countries of the sub-region were the studies carried out and what were the most frequent health outcomes related with food insecurity?
2. Materials and Methods
2.1. Search Strategy
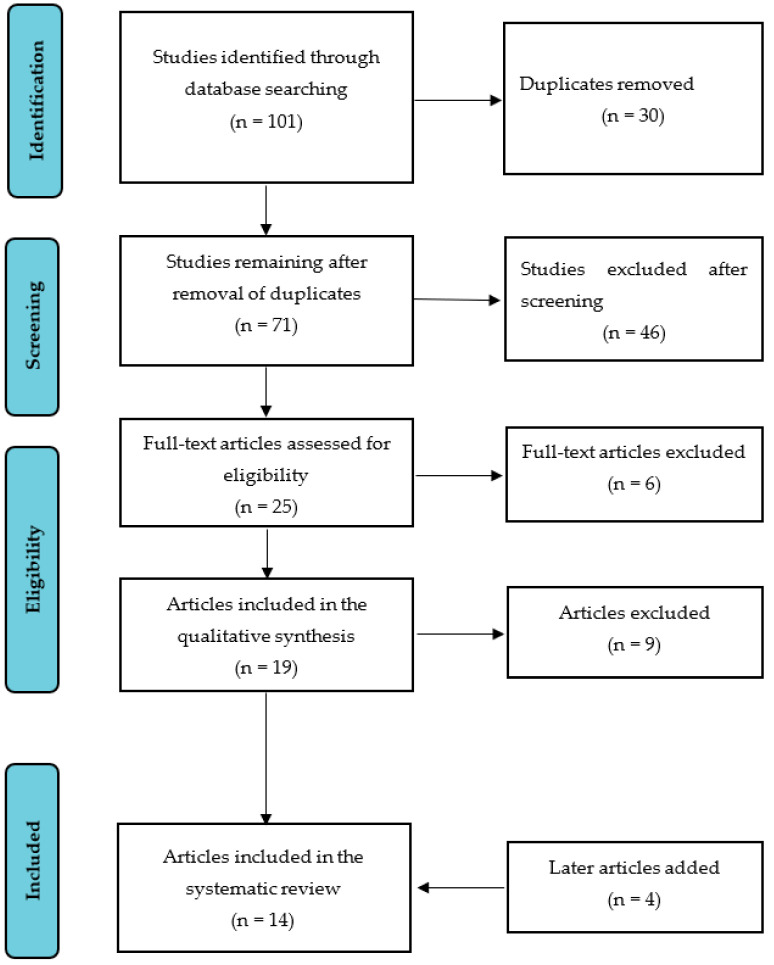
A systematic literature search was conducted using the Web of Science, PubMed and Google Scholar. The review was conducted and reported following the Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) statement [26]. A PRISMA flow chart is presented in Figure 1. The review covered studies published from January 2001 to October 2021 in order to include studies carried out in the last two decades on FI and health outcomes. Studies were included if they were published in full-text English language, were empirical studies conducted in southern African countries and addressed the relationship between household FI and health outcomes. Search terms included “food insecurity OR food security OR household food insecurity AND health outcomes”, “food insecurity OR food security OR household food insecurity AND health-related outcomes” and “food insecurity OR food security OR household food insecurity AND health”. We excluded conference papers as well as conceptual, theory-building, review articles or articles that did not focus on household food insecurity.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) flow chart of the literature search and selection process.
2.2. Article Selection and Assessment
A total of 101 articles were identified in Web of Science, PubMed and Google Scholar. After duplicates were removed, 71 articles remained to be thoroughly screened. All 71 were retrieved and exported to Zotero reference management software [27] for manual screening, which was undertaken in two steps. In the first step, E.M. removed 46 articles (e.g., conceptual articles and reviews). In the second step, the full text of the remaining 25 articles was assessed for eligibility, and a further six articles were removed (e.g., water insecurity or child malnutrition without data on household FI). The remaining 19 articles were further assessed by G.M., and nine were removed (e.g., FI and medication adherence). Ten articles met the inclusion criteria. An additional search was performed to find empirical studies published between October 2020 and October 2021, which yielded four more articles for inclusion (see Figure 1).
3. Results
This section first presents the characteristics of the studies included in the review and then describes their findings.
3.1. Characteristics of the Included Studies
Fourteen studies published between 2006 and 2021 met the inclusion criteria. Five were conducted in South Africa [17,18,19,28,29], two in Zimbabwe [30,31] and one each in Zambia [32], Tanzania [33], Madagascar [34], Malawi [35], Namibia [36] and Botswana [37]. One study was carried out in Botswana and Swaziland [38]. Three studies used mixed methods, ten used quantitative methodology and one used qualitative methods including in-depth interviews, participant observations and focus group discussions. The sample sizes varied from 53 [31] to 8790 respondents [30] (see Table 1). We found no peer-reviewed studies that were carried out in Mozambique, Democratic Republic of Congo and Angola examining the relationship between FI and health outcomes.
Table 1.
Summary of the 14 studies included in the systematic review.
| Author, Year/Country/Reference | Study Objective | Design, Sample, and Methods of Analysis | Measurement of FI | Prevalence of FI | Factors a Associated with FI |
Associated Health Outcomes | Findings (Overall) |
|---|---|---|---|---|---|---|---|
| Hadley and Patil, 2006/Tanzania/[33] | To examine whether FI is associated with anxiety and depression | Cross-sectional study (survey and ethnography), n = 449, Logistic regression | 15 items from the USDA HFSSM to measure FI in the last 3 months | 36% were food insecure | Poverty, ethnicity, large household size | Maternal anxiety and depression | There was a strong positive association between FI and maternal anxiety and depression |
| Weiser et al., 2007/Botswana and Swaziland/[38] | To examine the association between FI and risky sexual behaviours; to determine whether gender modifies this association | Cross-sectional study, n = 2051 (1255 in Botswana and 796 in Swaziland), Logistic regression | One single question on food insufficiency in the last 12 months | 32% of women were food insecure (Botswana 28%, Swaziland 38%) vs. 22% of men (Botswana 18%, Swaziland 29%) | Poverty, socioeconomic differences, gender inequality and unequal household food allocation | Multiple risky sexual practices among women (selling sex, and engaging in unprotected sex and intergenerational sex) | Food insufficiency was associated with inconsistent condom use with a non-primary partner, sex exchange, intergenerational sexual relationships and lack of sexual control |
| Cole and Tembo, 2011/Zambia/[32] | To examine the association between FI and self-reported mental health | Longitudinal design (surveys and ethnography), n = 280, Multilevel regression model | Modified 7-item scale on coping strategies | 64% were food insecure (17.5% low, 21.1% medium, 25.4% high) | Seasonality, dependency ratio and illness | Poor mental health | There was a positive and significant association between household FI and poor mental health |
| Dewing et al., 2013/South Africa/[18] | To assess the relationship between FI, postnatal depression, hazardous drinking, and suicidality | Cross-sectional study, n = 249, Poisson regression models | 9 items from the HFIAS to measure FI in the last 4 weeks | 59.8% were severely food insecure | Unemployment or very low income, HIV endemic and tuberculosis | 31.7% postnatal depression, 15.7% hazardous drinking, and 7.6% suicide risk | FI was strongly associated with postnatal depression, hazardous drinking and suicide risk |
| Naicker et al., 2015/South Africa/[29] | To assess trends in FS from 2006 to 2012; to determine the main predictors of FI and its associated health outcomes | Cross-sectional studies, n = 188, Logistic regression | Modified 10-item version of the Radimer/Cornell Questionnaire on household FS | In 2006, 85%, in 2009, 91%, and in 2012, 70% of households were food insecure | Low asset ownership, having major residence problems, having a very low income or no full-time employment | Chronic disease (diabetes mellitus, hypertension or heart disease); 13% common mental disorders (anxiety or depression) |
Household FI decreased from 2006 to 2012, though there was a spike in 2009, and FI was translated to poor food diversity |
| McCoy et al., 2015/Zimbabwe/[30] | To examine the association between FI and women’s uptake of services to prevent MTCT | Cross-sectional study, n = 8790, Poisson regression models | 3 items from the HFIAS to measure FI in the last 4 weeks | 51% were food insecure (33% moderately, 18% severely) | Poverty, province of residence, being single, low education and large household size | Increased risk of HIV acquisition | Severe FI is a barrier to uptake of some PMTCT services, contributing to HIV transmission from mother to child |
| Abrahams et al., 2018/South Africa/[17] | To assess factors associated with FI and depression and anxiety | Cross-sectional study, n = 376, Logistic regression | 6 items from the USDA HFSSM to measure FI in the last 6 months | 42% were food insecure | Poverty, unemployment, having three or more children, pregnancy | 21.4% were depressed (MDE); 22.8% had anxiety disorder |
The odds of being food insecure were increased in women with suicidal behaviour (OR = 5.34), depression (4.27) and three or more children (3.79) |
| Muderedzi et al., 2019/Zimbabwe/[31] | To explore the relationship between FI, gender roles and HIV/AIDS | Qualitative study (in-depth interviews and focus group discussions), n = 57, Thematic analysis | Not available | Not available | Extreme poverty, poor governance, lack of food, gender inequality, transactional sex | Increased risk of HIV acquisition | Most women were eager for an HIV-positive result in order to secure food handouts from NGOs to feed their families |
| Koyanagi et al., 2019/South Africa/[19] | To assess the association between FI and mild cognitive impairment (MCI) | Cross-sectional study, n = 3672, Logistic Regression | 2 questions on FI in the last 12 months based on the USDA HFSSM | 31.8% were food insecure (11% moderately, 20.8% severely) | Extreme poverty, race, low education, HIV endemic, high food prices | MCI (8.5%) | Moderate and severe FI was associated with 2.82 and 2.51 times the odds of having MCI |
| Farris et al., 2020/ Madagascar/[34] |
To assess the drivers of food choices and barriers to diet diversity | Cross-sectional study (survey and focus group discussions), n = 137, Descriptive statistics and thematic analysis | 5 questions on FI as described by Rakotosamimanana et al. [39] | Not available | Poverty, high food prices, lack of food and food beliefs | Poor general health, chronic malnutrition, poor academic performance | Though health concerns were consistently reported to be one of the major drivers of food choices, they were not translated into actual dietary choices |
| Wang et al., 2020/Botswana/[37] | To examine the association between FI and HIV infection, and depression and anxiety | Cross-sectional study, n = 180, Poisson regression models | 9 items from the HFIAS to measure FI in the last 4 weeks | 46.67% were food insecure (8.33% had mild FI; 9.44% had moderate FI; 28.89% had severe FI) | Poverty, co-infection of HIV and tuberculosis | Depression and anxiety | FI was associated with higher odds for depression (OR = 2.3) and anxiety (OR = 1.41) irrespective of being HIV-positive or not |
| Mark et al., 2021/Malawi/[35] | To evaluate the association between FI and clinical depression, and the modifying effects of seasonality | Cross-sectional study, n = 175, Logistic regression | 9 items from the HFIAS to measure FI in the last 4 weeks | 49.7% were food insecure | Poverty, having three or more children, seasonality, climate change | Clinical depression | Food-insecure participants had 4.6 times the odds of experiencing clinical depression, and the effect was greater in the dry season (OR = 9.9) than in the rainy season (OR = 2.6) |
| Kazembe et al., 2021/Namibia/[36] | To investigate the association between dietary patterns and non-communicable diseases | Cross-sectional study, n = 863, Factor analysis and logistic regression | 9 items from the HFIAS to measure FI in the last 30 days and the HDDS to examine FI in the last 24 h | 77.2% were food insecure | Poverty, low-income, informal settlements, type of housing, informal work | Increased odds of hypertension, diabetes and CVD | Food-insecure households less often had starch-oil-sugar diets and/or processed foods which are associated with increased odds of hypertension, diabetes and CVD |
| Jesson et al., 2021/South Africa/[28] | To assess the association between FI and depression | Prospective cohort study, n = 422, Logistic regression models | 3 items from the HHS to measure FI in the last 30 days | 18% were food insecure (12% had moderate FI and 6% severe FI) | Poverty, female-headed household, household size, not currently being a student, transactional sex | 42% probable depression, 72% perceived stress, 63% probable anxiety | Participants with probable depression had increased odds (OR = 2.79) of being food insecure |
United States Department of Agriculture (USDA); Household Food Security Survey Module (HFSSM); Household Food Insecurity Access Scale (HFIAS); Household Dietary Diversity Score (HDDS); Household Hunger Scale (HHS); Human immunodeficiency virus (HIV); Acquired immune deficiency syndrome (AIDS); Mild cognitive impairment (MCI); Cardiovascular disease (CVD); Major depressive episodes (MDEs); Prevention of mother-to-child HIV transmission (PMTCT); Non-governmental organizations (NGOs).
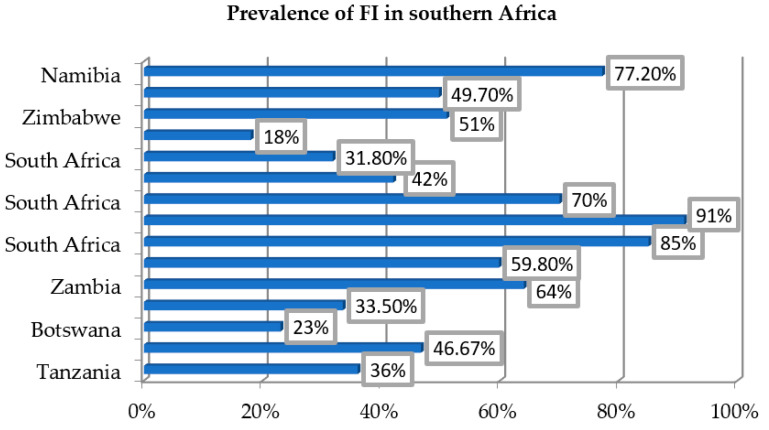
3.2. Prevalence of Food Insecurity
In this review, most of the studies, except Farris et al. [34] and Muderedzi et al. [31], measured FI using validated instruments based on the HFSSM and the Household Food Insecurity Access Scale (HFIAS). The reported prevalence of FI across the countries varied from 18% in Botswana and South Africa [28,38] to 91% in South Africa [29] (see Figure 2).
Figure 2.
The prevalence of FI across southern African countries included in this systematic review.
Koyanagi et al. [19] in a South African study measured FI in the previous 12 months using two questions based on the USDA HFSSM. They found that 31.8% of the participants were food insecure. Of these, 11% had moderate FI and 20.8% had severe FI. Abrahams et al. [17], studying a population of pregnant South African women, examined FI in the last 6 months using six items from the HFSSM, and found that 42% were food insecure. Hadley and Patil [33] studying the situation in rural Tanzania, assessed FI in the last 3 months using 15 items from the USDA HFSSM, and found that 36% were food insecure.
McCoy et al. [30] measured FI in the last 4 weeks in a Zimbabwean population using three items from the HFIAS. They found that 51% were food insecure. Of these, 33% had moderate and 18% had severe FI. Dewing et al. [18], Wang et al. [37] and Mark et al. [35] measured FI in the last 4 weeks using nine items from the HFIAS and found that 59.8%, 46.67% and 49.7%, respectively, of the participants were food insecure. Kazembe et al. [36] assessed FI in the last 30 days using nine items from the HFIAS, as well as FI in the past 24 h using the Household Dietary Diversity Score (HDDS), and found 77.2% of the households were food insecure, but consumed less of unhealthy foods than those who were food secure (i.e., they consumed less of starch-oil-sugar diet and/or processed food).
Cole and Tembo [32] evaluated FI using the modified seven-item scale on coping strategies proposed by Maxwell [40] and found a prevalence of 64%. Of these, 17.5% had low FI, while 21.1% had moderate and 25.4% severe FI. Weiser et al. [38] estimated FI using one single question on food insufficiency in the last 12 months, and found that more women (32%) than men (22%) were food insecure. Naicker et al. [29] examined trends of FS in an urban South African population using a modified ten-item version of the Radimer/Cornell questionnaire. They found that in 2006, 85% of households were food insecure; in 2009, FI increased and peaked at 91%; and in 2012, it decreased to 70%. Jesson et al. [28], also in South Africa, measured FI over the past 30 days using three items from the Household Hunger Scale (HHS), and found that 18% of participants were food insecure.
In these studies, FI was associated with a variety of determinants, with a focus on poverty (due to unemployment, low income, lack of full-time employment or poor governance), high food prices, illness, dependency ratio, having three or more children, gender inequality, seasonality and food unavailability.
3.3. Food Insecurity and Associated Health Outcomes
The studies in the review addressed different dimensions of FI and how various structural factors within households or society affect these and produce different health outcomes. Most of the studies used a cross-sectional design, except the studies by Cole and Tembo [32] (longitudinal design) and Jesson et al. [28] (prospective cohort study).
Farris et al. [34] aimed to assess the drivers of food choices and barriers to diet diversity among a vulnerable population of caregivers in Madagascar. The findings revealed that though health concerns were consistently reported as one of the most important factors when shopping or preparing food items, they were not translated into actual dietary choices. Furthermore, FI was associated with poor general health, chronic malnutrition and poor academic performance in children [34]. Kazembe et al. [36] examined the association between dietary patterns and non-communicable diseases in Windhoek, Namibia. They found that higher levels of consumption of diets consisting largely of a starch, oil and sugar diet and/or processed foods were associated with increased odds of having hypertension, diabetes and cardiovascular disease, but that these products were consumed more by food-secure than by food-insecure households. Naicker et al. [29] evaluated the association between FI and health outcomes in an informal settlement in Johannesburg. They found that 24% of participants were affected by any kind of chronic disease (diabetes mellitus, hypertension or heart disease). Twenty percent of households with a member who had a chronic disease were food insecure. Thirteen percent of respondents in food-insecure households screened positive for common mental health disorders (anxiety or depression) compared with 1% in food-secure households. On the other hand, Koyanagi et al. [19] examined the association between FI and mild cognitive impairment (MCI) among middle-aged and older adults in South Africa. The authors found that FI was strongly associated with MCI, particularly among individuals aged ≥65 years.
The study by Muderedzi et al. [31] explored the relationship between FI, gender roles and human immunodeficiency virus (HIV)/acquired immune deficiency syndrome (AIDS) among caregivers and health care personnel in Binga, one of Zimbabwe’s poorest and most food insecure districts. The findings showed FI, gender roles and HIV/AIDS entwined in a vicious cycle that heightens vulnerability to and worsens the severity of each condition. McCoy et al. [30] examined the association between FI and women’s uptake of services to prevent mother-to-child HIV transmission (MTCT) in Zimbabwe. The findings showed that FI was not associated with maternal or infant antiretroviral therapy (ART)/ARV prophylaxis. However, among HIV-exposed infants, 13.3% were born to women who reported severe household FI, compared with 8.2% of infants whose mothers reported FS. Among pregnant and postpartum women, FI was inversely associated with use of prevention of MTCT (PMTCT). Weiser et al. [38], in turn, examined the association between FI and risky sexual behaviours in Botswana and Swaziland and found food insufficiency, especially among women, was associated with inconsistent condom use with a non-primary partner, selling sex, intergenerational sexual relationships and lack of control in sexual relationships. In contrast, Wang et al. [37] evaluated the association between FI and HIV infection with depression and anxiety among tuberculosis (TB) patients in Gaborone, Botswana. They found that food-insecure participants had 2.3 and 1.4 times the odds of experiencing depression and anxiety, regardless of being HIV-positive or not.
With regard to mental health, Abrahams et al. [17] analysed factors associated with FI and depression among pregnant women from a low-income suburb in Cape Town. They found the odds for FI were increased in women with suicidal behaviour (odds ratio (OR = 5.34)) and depression (OR = 4.27) and in those with three or more children (OR = 3.79). In addition, FI was strongly associated with major depressive episodes (MDEs). Hadley and Patil [33] examined the association between FI and maternal anxiety and depression among four ethnic groups living in two communities of rural Tanzania. The findings showed a strong positive correlation between a caretaker’s FI score and her summed response on the Hopkins Symptom Checklist (HSCL) (p < 0.0001). High maternal age (p = 0.029) and household FI (p < 0.0001) were significant predictors of HSCL scores. The study by Cole and Tembo [32] examined the association between FI and self-reported mental health in rural Zambia. Their findings showed a positive and significant association between FI and poor mental health (r = 0.39, p-value < 0.0001). In addition, FI during the dry season, the time of relative food abundance, had greater effect on mental health than FI during the rainy season. Likewise, Mark et al. [35] examined the association between FI and clinical depression and how seasonality modifies this relationship among post-partum women in the rural Ntcheu District of Central Malawi. They found participants reporting higher levels of FI had 4.6 times the odds of meeting the cut-off for clinical depression compared with those reporting lower levels of FI, and the effect of FI on mental health was greater during the dry season (OR = 9.9) than during the rainy season (OR = 2.6). Dewing et al. [18], in turn, investigated the associations between FI, postnatal depression, hazardous drinking and suicide risk among women in the outskirts of Cape Town. In their study, 79 (31.7%) women met screening criteria for probable depression, and 39 (15.7%) met screening criteria for hazardous drinking. Nineteen (7.6%) women had significant suicidality, seven (2.8%) of whom were classified as high risk. Food insecurity was strongly associated with postnatal depression, hazardous drinking and suicidality. Lastly, Jesson et al. [28] assessed the association between FI and depression among youth living in Durban and Soweto, South Africa. They found those individuals with probable depression had increased odds (OR = 2.79) of being food insecure compared with those who were not depressed.
4. Discussion
4.1. Prevalence of Food Insecurity
The majority of the studies included in this review used quantitative and mixed methods, and the main findings used quantitative methodology. The same pattern in terms of methods was found among empirical studies that examined FI in other regions of sub-Saharan Africa [41,42,43].
In the current review, the prevalence of FI across the countries varied from 18% in Botswana and South Africa [28,38] to 91% in another study from South Africa [29]. The major factors associated with FI were: poverty, illnesses (mostly HIV and tuberculosis), high food prices, dependency ratio, having three or more children, gender inequality, seasonality and food unavailability. The variations in FI across the countries may be due to the measuring instruments, the specific characteristics of the study populations and the time period used for data collection [44]. Nonetheless, most of the studies used reliable and valid instruments for measuring FI, in most cases, modified versions of the USDA HFSSM and the HFIAS [45,46,47].
Food insecurity in Africa is largely associated with poverty [48]. Many factors can contribute to poverty, but flawed economic policies and institutions suffering from corruption, poor governance and political conflicts [49,50] as well as poor land utilization are considered the primary causes of poverty in Africa [49]. Hence, effective interventions from governments, the private sector and international institutions such as the World Bank and International Monetary Fund are needed to stimulate decent work and build inclusive economic growth [49,50]. In addition, low per capita income and rapid population growth make it extremely difficult to have savings and invest in Africa, a condition that perpetuates low productivity and low income [50].
Moreover, the majority of poor urban households purchase the bulk of their food rather than produce it themselves, and therefore, household income and food prices are critical determinants of FI in cities [48]. Food insecurity tends to exacerbate with illness, high food prices observed in cities, dependency ratio and having three or more children, as highlighted in this review. For instance, various studies indicate that the COVID-19 pandemic has caused a rise in FI [51] through food shortages and high food prices, job losses and decrease in livelihoods [52,53]. In a unique way, the COVID-19 pandemic highlighted the fragilities of health systems and food systems not only in LMICs [54,55], but also in high income countries [56,57]. A study by Rosenberg et al. [58] on the impact of the COVID-19 pandemic on labour markets and economies of 16 southern African countries found that the COVID-19 pandemic was associated with increased job loss risk specifically in Angola, South Africa and Zimbabwe. These studies suggested the need to provide social and economic support to the most vulnerable groups [59,60,61] as well as the need to rethink future actions towards global food security, since COVID-19 greatly affected all its four pillars [56,59]. Furthermore, FI in urban areas is largely an outcome of income poverty often accompanied by lack of secure employment, but also includes living conditions and inconsistent access to water, sanitation, electricity and other resources that shape households’ food utilization capacity [62].
On the other hand, there is a body of evidence about the relationship between household FI and gender inequality in Africa and other LMICs, and this suggests that socioeconomic interventions are needed to empower women and close the FI gap between female- and male-headed households [63,64]. In contrast to the cities, in rural areas, factors such as seasonality and climate change can have a huge impact, as most households rely on their own food production. Smallholder farmers cannot afford the cost of fertilizers, high quality seeds and planting materials, especially the cost of irrigation, nor can they afford quality education, and therefore, depend on rainfall, which is becoming increasingly unreliable because of climate change [65].
With regard to factors associated with FI, similar results have been reported for Africa and elsewhere, particularly in LMICs [66,67,68]. Besides poverty, climate change [66,67], rapid population growth [11], poor governance and political conflicts [11,68] have been highlighted as relevant determinants of FI. For instance, climate change may affect food systems and FI in a number of ways ranging from direct effects on food production (e.g., variations in rainfall patterns leading to droughts or floods, vacillations in temperatures and variation in the length of growing seasons) to changes in markets, food prices, increased poverty and food supply chain infrastructure [6,67]. The quality of governance (e.g., government effectiveness, political stability, rule of law, accountability) and targeted policies are critical for fostering an adequate environment, which is vital to all economic processes and investments, especially those related to enhancing national food and nutrition security, social protection and the pace of economic growth [11].
4.2. Food Insecurity and Associated Health Outcomes
The studies included in this review examined the relationship between FI and health outcomes in adults. For instance, FI in South Africa was associated with MCI [19], depression and anxiety [17,28], postnatal depression, hazardous drinking and suicide risk [18], chronic diseases (diabetes mellitus, hypertension and CVD) [29] and perceived stress [28].
Koyanagi and colleagues [19] found that the odds of having MCI were 3.87 times higher in individuals aged ≥65 years with severe FI than their food-secure counterparts. Their findings are supported by other studies [69,70]. The mechanisms linking FI to MCI are not clear, but it is believed that stress derived from FI can increase the risk of cognitive decline [71]. Moreover, FI often compromises diet quality, and poor diet has been associated with higher risk of cognitive decline [72,73].
Abrahams et al. [17] found that the odds of experiencing depression were five times greater in food-insecure compared with food-secure women. They also found that the odds of being food insecure were 4.3 times greater in depressed women compared with women who were not depressed. In fact, many studies conducted in LMICs suggest that FI and common mental illnesses are related in a vicious cycle, but the strength of this association depends on various factors, including the specific characteristics of the study population, the measuring instrument used and the time period for data collection. For instance, in Ecuador, self-reported depression in mothers increased the odds of being food insecure by almost three times [16], and in Korea it was by four times [74]. On the other hand, the study by Cole and Tembo [32] in rural Zambia revealed that FI during the dry season had greater effects on mental health than FI during the rainy season. Along the same lines, Mark et al. [35], in rural Malawi, found FI during the dry season to be associated with greater odds of experiencing clinical depression (OR = 9.9) than FI during the rainy season (OR = 2.6). One plausible explanation is that, because the dry season is supposed to be the time of relative food abundance and FS, therefore, when households fail to harvest an adequate amount of food, they are forced to rely on various coping strategies, and this becomes the source of worry and anxiety [32,35]. Likewise, the rainy season is associated with disease outbreak, which brings uncertainty about physical health and future food production [32].
Overall, across investigated countries, FI was associated with chronic malnutrition, poor general health and poor academic performance [34], anxiety and depression [33,37], poor mental health [32] and increased odds of hypertension, diabetes and CVD [36]. Many studies have shown that food-insecure children have difficulty in achieving academic success [75], and FI has been associated with poor cognitive and emotional development [76]. Other findings include those by Farris and colleagues [34] who found that, though health concerns were consistently reported as relevant when buying food, they were not translated into actual food choices. For instance, green leafy vegetables were not viewed as nutrient-dense because of their relatively lower cost and confusion over energy-dense vs. nutrient-dense food [34]. Hence, educational initiatives are needed to educate the population about the nutritional value and benefits of consuming green leafy vegetables.
Kazembe et al. [36] found that “starch–oil–sugars” and “meat–fish–dairy” dietary patterns were associated with hypertension, diabetes and CVDs, but that these products were less consumed by food-insecure households. This is an unusual finding that food-insecure households were found to consume less of unhealthy foods than their counterpart who were food secure (i.e., they consumed less of the starch–oil–sugar diet and/or processed food). The authors of the study explained their findings, pointing out that, on one hand, there was a lack of processed foods in informal markets and, on the other, food-insecure households could not afford products such as meat, and only managed to buy them for festive occasions. Another explanation is the role of food transfers (e.g., grains, vegetables and wild foods) in mitigating FI and combating NCDs in informal settlements, as highlighted by the authors. The HDDS instrument, which was used by Kazembe et al. [36], captures the types of food the households have consumed in the last 24 h, hence it is possible that it captures chance findings, and the findings depend on the season when the instrument is administered. The availability of food transfers for food-insecure households in informal settlements is dependent on the season. Moreover, this instrument is recognized in Namibia as inadequate for capturing, for instance, the consumption of wild foods (which are very healthy), as is common in informal settlements [77,78]. With regard to the negative health outcomes revealed, there is a body of evidence that a dietary pattern characterized by high intake of vegetables, fruit and complex carbohydrates and low intake of processed meat and refined carbohydrates may have a protective effect against hypertension, type 2 diabetes, CVDs and other NCDs [79]. These findings require further investigation, as it has been reported elsewhere that food-insecure households are more likely to buy cheap and unhealthy food (e.g., highly processed foods with large amount of sugar, sodium and oils), and therefore have increased risk for NCDs [15,80].
According to Davison et al. [81], the mechanisms linking FI to mental illnesses include biological mechanisms, by which micronutrient deficiency impacts mental health, and psychological mechanisms, by which stress, worry and anxiety that derive from FI may cause maladaptive responses, leading to suicidal ideation and behaviour. Furthermore, suicidal behaviour, as with other mental illnesses, may lead to increased health expenses, unemployment, social withdrawal and other consequences that worsen each of these conditions [82].
In Zimbabwe, FI was associated with increased risk of HIV acquisition [30,31], and severe FI was considered a barrier to uptake PMTCT services [30]. Muderedzi et al. [31] illustrate the relationship between FI, gender roles and HIV/AIDS acquisition as a vicious cycle. These authors found that the four dimensions of FS were missing in Tonga communities because of extreme poverty. For this reason, women, even if aware of the related health issues, often adopted sexual (as well as non-sexual) coping strategies to obtain food for their families. Most women in their study had taken numerous HIV tests and were eager to get an HIV-positive result because several NGOs in the area provide food aid to HIV-positive people. These women often stated that HIV came with food, and that the need for food was far more important than getting HIV. In addition, the authors stated that Tonga cultural factors (e.g., polygamous marriage systems, widow inheritance and sexual cleansing) are important factors in the spread of HIV [31].
Along the same lines, Weiser et al. [38] found that FI was associated with risky sexual practices among women in Botswana and Swaziland. These findings suggest that FS could play an important role in limiting the spread of HIV/AIDS in sub-Saharan Africa. Furthermore, income generation programmes together with educational initiatives and interventions on food supplementation and food production could alleviate gender disparities that drive risky sexual practices, and therefore reduce HIV/AIDS acquisition among high-risk populations [38]. Most of the studies reporting associations between FI and HIV in Africa have focused on the effects of FI on ART and have found that approaches aiming to enhance the FS of people living with HIV (PLHIVs) may be effective for improving HIV outcomes [83,84,85]. For instance, Benzekri et al. [83] aimed to assess the retention on ART and to identify the predictors of loss to follow-up (LTFU) among PLHIVs in Senegal. They found that severe FI (OR = 2.55) was the strongest predictor of LTFU, and therefore, implementing strategies to enhance FS for PLHIV may be effective for reducing LTFU and strengthening the HIV care cascade in Africa. Similar results have been found in Democratic Republic of Congo [84] and Mozambique [85,86]. A systematic study by Singer et al. [87] in Africa, Europe, Canada, USA and South America found that FI was an important barrier to ART adherence, and food assistance appeared to be a promising intervention strategy to improve ART outcomes among PLHIV. Thus, household FS or food assistance programmes should be an essential component of HIV/AIDS strategies to improve ART outcomes [87,88]. On the other hand, a study by Nagata et al. [89] using nationally representative data on US young adults aged 24–32 years has found that food-insecure young women had greater odds of self-reported sexually transmitted infections (STIs), particularly chlamydia and HIV, exchanging sex for money and having multiple concurrent sex partners in the past 12 months compared with food-secure ones. In both young men and women, FI was associated with greater odds of substance use. These findings have public health and clinical implications regarding alleviation of FI and improved health outcomes.
It is noteworthy that for Mozambique and Democratic Republic of Congo, no studies were found examining the association between FI and health outcomes although FI is a living reality for many households [90,91,92,93,94]. In Mozambique and Democratic Republic of Congo, the studies found addressed the effects of FI or food assistance programmes on ART, as indicated in the previous paragraph [84,85,86,87]. In Angola, one study examined malnutrition in children under 2 years old and its associated factors [95]. Unfortunately, some potential determinants of child malnutrition (e.g., household FI, sanitation, primary care) were not measured, and diarrhoea (PR 1.39 [95% CI: 1.01–1.87]) was associated with stunting (32% [95% CI: 28.7–35.5]). Nonetheless, Humbwavali and colleagues [95] recognized that they identified few risk factors for child malnutrition, and suggested that a combination of life course factors related to pregnancy and birth, and collective exposures (e.g., household FI, sanitation, primary care, infectious diseases) could be causing child malnutrition in Angola. In addition, the authors argued that probably because of pre-existing nutritional deficits, these children were more vulnerable to infections that led to diarrhoea or these children had repeated episodes of diarrhoea that led to stunting. In any case, these conditions were entwined in a vicious circle which strengthened each condition [95]. Thus, joint and coordinated efforts between governments, private sector, non-government organizations and communities are needed to improve child malnutrition in the region in particular and in Africa as a whole [95,96,97,98,99]. On the other hand, a recent case-control study by Robbiati et al. [100] found an association between severe FI and diabetes among adults in the capital city of Angola. Therefore, the authors called for further longitudinal studies to assess the pathways linking food insecurity and diabetes in that setting.
4.3. Areas for Further Research
This review has shown that FI is an important societal and public health problem in southern Africa, and it has been measured using different instruments, but mostly the USDA HFSSM and the HFIAS. Food insecurity has been associated with a variety of factors, mainly poverty, illness, high food prices, dependency ratio, gender inequality, seasonality and food unavailability. Crush and Frayne [48] argue that FI in Africa is largely the result of poverty and that many factors may contribute to poverty. In other research, flawed economic policies and institutions (e.g., corruption, poor governance, political conflicts and poor land utilization) are considered the primary causes of poverty in Africa [49,50]. Therefore, future studies that investigate the role by structural and institutional policy on FI are warranted. In addition, the studies included in this review indicate that FI has detrimental consequences for the physical and mental wellbeing of those affected; in adults, FI has been associated with poor mental health, anxiety and depression, type II diabetes, hypertension and other negative health outcomes. These findings suggest an urgent need for research that can also provide a deeper understanding of the determinants of FI in southern African countries for which empirical research is still not available (e.g., Mozambique, Democratic Republic of Congo). Such research will help to disentangle mechanistic pathways of the relationship between FI and physical and psychological health outcomes across the region.
4.4. Strengths and Limitations
This review provides one of the first assessments of empirical studies that examined FI and its relationship with health outcomes in southern Africa. Broad search terms were used to identify as many articles as possible on the topic. Moreover, the selection process was conducted in two stages to increase the number of included papers. Nonetheless, the review has some limitations that need to be acknowledged. It relied exclusively on peer-reviewed studies published in English in databases. Therefore, it is very likely that other publications addressing FI and health outcomes written in other languages do exist, but that they were not included.
5. Conclusions
This review investigated empirical evidence of the relationship between FI and health outcomes in southern Africa and found 14 studies carried out in South Africa, Zimbabwe, Zambia, Tanzania, Madagascar, Malawi, Namibia, Botswana and Swaziland. No studies were found on this subject in Mozambique and Democratic Republic of Congo. The majority of the identified studies used quantitative methodology, which is in line with reviews conducted in other regions of sub-Saharan Africa. A variety of instruments were used to collect information about FI, with most studies using the USDA HFSSM and the HFIAS. Food insecurity in this sub-region was associated with a number of factors, but poverty, illness, high food prices, dependency ratio, having three or more children, gender inequality, seasonality and food unavailability were consistently found to be the main drivers of FI. Furthermore, FI was associated with poor mental health, anxiety and depression, type II diabetes, hypertension, CVD and increased risk of HIV acquisition through biological, psychological and behavioural mechanisms. These findings suggest that future research is needed to identify and standardize measures of FI suitable for the southern African context and inform public health policies and design appropriate interventions to alleviate household FI and improve health outcomes. This is crucial for countries such as Mozambique and Democratic Republic of Congo for which no current studies exist that address the relationship between food insecurity and health outcomes.
Author Contributions
Conceptualization, E.M.A.M. and G.M.; methodology, E.M.A.M., E.M.S. and G.M.; validation, E.M.A.M., E.M.S., G.M. and S.V.; formal analysis, E.M.A.M., E.M.S. and G.M.; investigation, E.M.A.M. and G.M.; data curation, E.M.A.M., E.M.S. and G.M.; writing—original draft preparation, E.M.S., writing—review and editing, E.M.A.M., E.M.S., G.M., S.V. and O.A.U.; visualization, E.M.S. All authors have read and agreed to the published version of the manuscript.
Funding
This study was funded by SIDA, ISP 2018/28:6 Mozambique; SIDA Decision No.: 2017/11862 Subprogram 1.2.1. Food Technology and Food Safety; and PhD grant (Elias Militao) Project 8-71101-3283.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The review used existing research data.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tydeman-Edwards R., Van Rooyen F.C., Walsh C.M. Obesity, Undernutrition and the Double Burden of Malnutrition in the Urban and Rural Southern Free State, South Africa. Heliyon. 2018;4:e00983. doi: 10.1016/j.heliyon.2018.e00983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bickel G.W., Nord M., Price C., Hamilton W., Cook J. Guide to Measuring Household Food Security: Revised March, 2000. USDA Food and Nutrition Service; Alexandria, VA, USA: 2000. p. 82. [Google Scholar]
- 3.Gross R., Schoeneberger H.G., Pfeifer H., Preuss H.J.A. The Four Dimensions of Food and Nutrition Security: Definitions and Concepts. European Union; Bonn, Germany: Inwent; Bonn, Germany: FAO; Bonn, Germany: 2000. p. 17. [Google Scholar]
- 4.McKay F.H., Haines B.C., Dunn M. Measuring and Understanding Food Insecurity in Australia: A Systematic Review. Int. J. Environ. Res. Public Health. 2019;16:476. doi: 10.3390/ijerph16030476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ray D.E., Schaffer H.D. Food Accessibility. Agricultural Policy Analysis Center; Knoxville, TN, USA: 2013. p. 2. [Google Scholar]
- 6.Gregory P.J., Ingram J.S.I., Brklacich M. Climate Change and Food Security. Philos. Trans. R. Soc. B Biol. Sci. 2005;360:2139–2148. doi: 10.1098/rstb.2005.1745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Webb P., Coates J., Frongillo E.A., Rogers B.L., Swindale A., Bilinsky P. Measuring Household Food Insecurity: Why It’s So Important and Yet So Difficult to Do. J. Nutr. 2006;136:1404S–1408S. doi: 10.1093/jn/136.5.1404S. [DOI] [PubMed] [Google Scholar]
- 8.FAO. ECA. AUC . 2019 Africa Regional Overview of Food Security and Nutrition. FAO; Accra, Ghana: 2020. p. 104. [Google Scholar]
- 9.WFP 2020 Hunger Map. [(accessed on 2 November 2021)]. Available online: https://www.wfp.org/publications/hunger-map-2020.
- 10.Anugwa I., Agwu A. Perceived Causes of Household Food Insecurity and Policy Implications for Food Production in Kano State, Nigeria. J. Appl. Sci. 2019;19:513–519. doi: 10.3923/jas.2019.513.519. [DOI] [Google Scholar]
- 11.Ogunniyi A.I., Mavrotas G., Olagunju K.O., Fadare O., Adedoyin R. Governance Quality, Remittances and Their Implications for Food and Nutrition Security in Sub-Saharan Africa. World Dev. 2020;127:104752. doi: 10.1016/j.worlddev.2019.104752. [DOI] [Google Scholar]
- 12.Tantu A.T., Gamebo T.D., Sheno B.K., Kabalo M.Y. Household Food Insecurity and Associated Factors among Households in Wolaita Sodo Town, 2015. Agric. Food Secur. 2017;6:19. doi: 10.1186/s40066-017-0098-4. [DOI] [Google Scholar]
- 13.Chinyoka K. Impact of Poor Nutrition on the Academic Performance of Grade Seven Learners: A Case of Zimbabwe. Int. J. Learn. Dev. 2014;4:73–84. doi: 10.5296/ijld.v4i3.6169. [DOI] [Google Scholar]
- 14.Gassara G., Chen J. Household Food Insecurity, Dietary Diversity, and Stunting in Sub-Saharan Africa: A Systematic Review. Nutrients. 2021;13:4401. doi: 10.3390/nu13124401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pérez-Escamilla R., Villalpando S., Shamah-Levy T., Méndez-Gómez Humarán I. Household Food Insecurity, Diabetes and Hypertension among Mexican Adults: Results from Ensanut 2012. Salud Pública Méx. 2014;56:62–70. doi: 10.21149/spm.v56s1.5167. [DOI] [PubMed] [Google Scholar]
- 16.Weigel M.M., Armijos R.X., Racines M., Cevallos W., Castro N.P. Association of Household Food Insecurity with the Mental and Physical Health of Low-Income Urban Ecuadorian Women with Children. J. Environ. Public Health. 2016;2016:5256084. doi: 10.1155/2016/5256084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abrahams Z., Lund C., Field S., Honikman S. Factors Associated with Household Food Insecurity and Depression in Pregnant South African Women from a Low Socio-Economic Setting: A Cross-Sectional Study. Soc. Psychiatry Psychiatr. Epidemiol. 2018;53:363–372. doi: 10.1007/s00127-018-1497-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dewing S., Tomlinson M., le Roux I.M., Chopra M., Tsai A.C. Food Insecurity and Its Association with Co-Occurring Postnatal Depression, Hazardous Drinking, and Suicidality among Women in Peri-Urban South Africa. J. Affect. Disord. 2013;150:460–465. doi: 10.1016/j.jad.2013.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koyanagi A., Veronese N., Stubbs B., Vancampfort D., Stickley A., Oh H., Shin J., Jackson S., Smith L., Lara E. Food Insecurity Is Associated with Mild Cognitive Impairment among Middle-Aged and Older Adults in South Africa: Findings from a Nationally Representative Survey. Nutrients. 2019;11:749. doi: 10.3390/nu11040749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abrahams Z., Boisits S., Schneider M., Prince M., Lund C. The Relationship between Common Mental Disorders (CMDs), Food Insecurity and Domestic Violence in Pregnant Women during the COVID-19 Lockdown in Cape Town, South Africa. Soc. Psychiatry Psychiatr. Epidemiol. 2021;57:37–46. doi: 10.1007/s00127-021-02140-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hatcher A.M., Stöckl H., McBride R.-S., Khumalo M., Christofides N. Pathways From Food Insecurity to Intimate Partner Violence Perpetration Among Peri-Urban Men in South Africa. Am. J. Prev. Med. 2019;56:765–772. doi: 10.1016/j.amepre.2018.12.013. [DOI] [PubMed] [Google Scholar]
- 22.Trudell J.P., Burnet M.L., Ziegler B.R., Luginaah I. The Impact of Food Insecurity on Mental Health in Africa: A Systematic Review. Soc. Sci. Med. 2021;278:113953. doi: 10.1016/j.socscimed.2021.113953. [DOI] [PubMed] [Google Scholar]
- 23.Nkambule S.J., Moodley I., Kuupiel D., Mashamba-Thompson T.P. Association between Food Insecurity and Key Metabolic Risk Factors for Diet-Sensitive Non-Communicable Diseases in Sub-Saharan Africa: A Systematic Review and Meta-Analysis. Sci. Rep. 2021;11:5178. doi: 10.1038/s41598-021-84344-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Haines C., Loades M.E., Coetzee B.J., Higson-Sweeney N. Which HIV-Infected Youth Are at Risk of Developing Depression and What Treatments Help? A Systematic Review Focusing on Southern Africa. Int. J. Adolesc. Med. Health. 2021;33:20190037. doi: 10.1515/ijamh-2019-0037. [DOI] [PubMed] [Google Scholar]
- 25.Ballard T.J., Kepple A.W., Cafiero C., Schmidhuber J. Better Measurement of Food Insecurity in the Context of Enhancing Nutrition. Ernahrungs Umsch. 2014;61:38–41. doi: 10.4455/eu.2014.007. [DOI] [Google Scholar]
- 26.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. J. Clin. Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 27.CDS Zotero; Version 5.0.96.3; USA. [(accessed on 2 November 2021)]. Available online: https://www.zotero.org/support/
- 28.Jesson J., Dietrich J., Beksinska M., Closson K., Nduna M., Smit J., Brockman M., Ndung’u T., Gray G., Kaida A. Food Insecurity and Depression: A Cross-sectional Study of a Multi-site Urban Youth Cohort in Durban and Soweto, South Africa. Trop. Med. Int. Health. 2021;26:687–700. doi: 10.1111/tmi.13572. [DOI] [PubMed] [Google Scholar]
- 29.Naicker N., Mathee A., Teare J. Food Insecurity in Households in Informal Settlements in Urban South Africa. S. Afr. Med. J. 2015;105:268. doi: 10.7196/SAMJ.8927. [DOI] [PubMed] [Google Scholar]
- 30.McCoy S.I., Buzdugan R., Mushavi A., Mahomva A., Cowan F.M., Padian N.S. Food Insecurity Is a Barrier to Prevention of Mother-to-Child HIV Transmission Services in Zimbabwe: A Cross-Sectional Study. BMC Public Health. 2015;15:420. doi: 10.1186/s12889-015-1764-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Muderedzi J., Eide A.H., Braathen S.H., Stray-Pedersen B. Exploring the Relationship Between Food Insecurity, Gender Roles and HIV/AIDS Among Tonga Carers of Disabled Children of Binga in Zimbabwe. Sex. Cult. 2019;23:1131–1146. doi: 10.1007/s12119-019-09610-w. [DOI] [Google Scholar]
- 32.Cole S.M., Tembo G. The Effect of Food Insecurity on Mental Health: Panel Evidence from Rural Zambia. Soc. Sci. Med. 2011;73:1071–1079. doi: 10.1016/j.socscimed.2011.07.012. [DOI] [PubMed] [Google Scholar]
- 33.Hadley C., Patil C.L. Food Insecurity in Rural Tanzania Is Associated with Maternal Anxiety and Depression. Am. J. Hum. Biol. 2006;18:359–368. doi: 10.1002/ajhb.20505. [DOI] [PubMed] [Google Scholar]
- 34.Farris A.R., Misyak S., O’Keefe K., VanSicklin L., Porton I. Understanding the Drivers of Food Choice and Barriers to Diet Diversity in Madagascar. J. Hunger Environ. Nutr. 2020;15:388–400. doi: 10.1080/19320248.2019.1566110. [DOI] [Google Scholar]
- 35.Mark T.E., Latulipe R.J., Anto-Ocrah M., Mlongoti G., Adler D., Lanning J.W. Seasonality, Food Insecurity, and Clinical Depression in Post-Partum Women in a Rural Malawi Setting. Matern. Child Health J. 2021;25:751–758. doi: 10.1007/s10995-020-03045-8. [DOI] [PubMed] [Google Scholar]
- 36.Kazembe L.N., Nickanor N., Crush J. Food Insecurity, Dietary Patterns, and Non-Communicable Diseases (NCDs) in Windhoek, Namibia. J. Hunger Environ. Nutr. 2021 doi: 10.1080/19320248.2021.1901822. [DOI] [Google Scholar]
- 37.Wang Q., Dima M., Ho-Foster A., Molebatsi K., Modongo C., Zetola N.M., Shin S.S. The Association of Household Food Insecurity and HIV Infection with Common Mental Disorders among Newly Diagnosed Tuberculosis Patients in Botswana. Public Health Nutr. 2020;25:913–921. doi: 10.1017/S1368980020004139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Weiser S.D., Leiter K., Bangsberg D.R., Butler L.M., Korte F.P., Hlanze Z., Phaladze N., Iacopino V., Heisler M. Food Insufficiency Is Associated with High-Risk Sexual Behavior among Women in Botswana and Swaziland. PLoS Med. 2007;4:e260. doi: 10.1371/journal.pmed.0040260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rakotosamimanana V., Arvisenet G., Valentin D. Studying the Nutritional Beliefs and Food Practices of Malagasy School Children Parents. A Contribution to the Understanding of Malnutrition in Madagascar. Appetite. 2014;81:67–75. doi: 10.1016/j.appet.2014.05.032. [DOI] [PubMed] [Google Scholar]
- 40.Maxwell D.G. Measuring Food Insecurity: The Frequency and Severity of “Coping Strategies”. Food Policy. 1996;21:291–303. doi: 10.1016/0306-9192(96)00005-X. [DOI] [Google Scholar]
- 41.Hadley C., Tegegn A., Tessema F., Cowan J.A., Asefa M., Galea S. Food Insecurity, Stressful Life Events and Symptoms of Anxiety and Depression in East Africa: Evidence from the Gilgel Gibe Growth and Development Study. J. Epidemiol. Community Health. 2008;62:980–986. doi: 10.1136/jech.2007.068460. [DOI] [PubMed] [Google Scholar]
- 42.Nagata J.M., Magerenge R.O., Young S.L., Oguta J.O., Weiser S.D., Cohen C.R. Social Determinants, Lived Experiences, and Consequences of Household Food Insecurity among Persons Living with HIV/AIDS on the Shore of Lake Victoria, Kenya. AIDS Care. 2012;24:728–736. doi: 10.1080/09540121.2011.630358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tesfaye M., Kaestel P., Olsen M.F., Girma T., Yilma D., Abdissa A., Ritz C., Prince M., Friis H., Hanlon C. Food Insecurity, Mental Health and Quality of Life among People Living with HIV Commencing Antiretroviral Treatment in Ethiopia: A Cross-Sectional Study. Health Qual. Life Outcomes. 2016;14:37. doi: 10.1186/s12955-016-0440-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Smith M.D., Kassa W., Winters P. Assessing Food Insecurity in Latin America and the Caribbean Using FAO’s Food Insecurity Experience Scale. Food Policy. 2017;71:48–61. doi: 10.1016/j.foodpol.2017.07.005. [DOI] [Google Scholar]
- 45.Gebreyesus S.H., Lunde T., Mariam D.H., Woldehanna T., Lindtjørn B. Is the Adapted Household Food Insecurity Access Scale (HFIAS) Developed Internationally to Measure Food Insecurity Valid in Urban and Rural Households of Ethiopia? BMC Nutr. 2015;1:2. doi: 10.1186/2055-0928-1-2. [DOI] [Google Scholar]
- 46.Leroy J.L., Ruel M., Frongillo E.A., Harris J., Ballard T.J. Measuring the Food Access Dimension of Food Security: A Critical Review and Mapping of Indicators. Food Nutr. Bull. 2015;36:167–195. doi: 10.1177/0379572115587274. [DOI] [PubMed] [Google Scholar]
- 47.Tutunchi H., Ebrahimi-Mameghani M., Asghari-Jafarabadi M., Farrin N., Tabrizi S., Vaghef-Mehrabany E., Ostadrahimi A. Is the Modified Household Food Security Survey (HFSS) Questionnaire a Practical Tool for Screening Food Insecurity? Evidence from Northwest of Iran. BMC Public Health. 2020;20:883. doi: 10.1186/s12889-020-09014-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Crush J.S., Frayne G.B. Urban Food Insecurity and the New International Food Security Agenda. Dev. S. Afr. 2011;28:527–544. doi: 10.1080/0376835X.2011.605571. [DOI] [Google Scholar]
- 49.Addae-Korankye A. Causes of Poverty in Africa: A Review of Literature. Am. Int. J. Soc. Sci. 2014;3:147–153. [Google Scholar]
- 50.Kabuya F.I. Fundamental Causes of Poverty in Sub-Saharan Africa. IOSR J. Humanit. Soc. Sci. 2015;20:78–81. [Google Scholar]
- 51.Laborde D., Herforth A., Headey D., de Pee S. COVID-19 Pandemic Leads to Greater Depth of Unaffordability of Healthy and Nutrient-Adequate Diets in Low- and Middle-Income Countries. Nat. Food. 2021;2:473–475. doi: 10.1038/s43016-021-00323-8. [DOI] [PubMed] [Google Scholar]
- 52.Dasgupta S., Robinson E.J.Z. Food Insecurity, Safety Nets, and Coping Strategies during the COVID-19 Pandemic: Multi-Country Evidence from Sub-Saharan Africa. Int. J. Environ. Res. Public Health. 2021;18:9997. doi: 10.3390/ijerph18199997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Clapp J., Moseley W.G. This Food Crisis Is Different: COVID-19 and the Fragility of the Neoliberal Food Security Order. J. Peasant Stud. 2020;47:1393–1417. doi: 10.1080/03066150.2020.1823838. [DOI] [Google Scholar]
- 54.Erokhin V., Gao T. Impacts of COVID-19 on Trade and Economic Aspects of Food Security: Evidence from 45 Developing Countries. Int. J. Environ. Res. Public Health. 2020;17:5775. doi: 10.3390/ijerph17165775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mugabe V.A., Gudo E.S., Inlamea O.F., Kitron U., Ribeiro G.S. Natural Disasters, Population Displacement and Health Emergencies: Multiple Public Health Threats in Mozambique. BMJ Glob. Health. 2021;6:e006778. doi: 10.1136/bmjgh-2021-006778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Toffolutti V., Stuckler D., McKee M. Is the COVID-19 Pandemic Turning into a European Food Crisis? Eur. J. Public Health. 2020;30:626–627. doi: 10.1093/eurpub/ckaa101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Niles M.T., Bertmann F., Belarmino E.H., Wentworth T., Biehl E., Neff R. The Early Food Insecurity Impacts of COVID-19. Nutrients. 2020;12:2096. doi: 10.3390/nu12072096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rosenberg J., Strauss I., Isaacs G. COVID-19 Impact on SADC Labour Markets: Evidence from High-frequency Data and Other Sources. Afr. Dev. Rev. 2021;33:S177–S193. doi: 10.1111/1467-8268.12528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Laborde D., Martin W., Swinnen J., Vos R. COVID-19 Risks to Global Food Security. Science. 2020;369:500–502. doi: 10.1126/science.abc4765. [DOI] [PubMed] [Google Scholar]
- 60.Crush J., Si Z. COVID-19 Containment and Food Security in the Global South. J. Agric. Food Syst. Community Dev. 2020;9:149–151. doi: 10.5304/jafscd.2020.094.026. [DOI] [Google Scholar]
- 61.Tripathi H.G., Smith H.E., Sait S.M., Sallu S.M., Whitfield S., Jankielsohn A., Kunin W.E., Mazibuko N., Nyhodo B. Impacts of COVID-19 on Diverse Farm Systems in Tanzania and South Africa. Sustainability. 2021;13:9863. doi: 10.3390/su13179863. [DOI] [Google Scholar]
- 62.Anand S., Jagadeesh K., Adelina C., Koduganti J. Urban Food Insecurity and Its Determinants: A Baseline Study of Bengaluru. Environ. Urban. 2019;31:421–442. doi: 10.1177/0956247819861899. [DOI] [Google Scholar]
- 63.Jung N.M., De Bairros F.S., Pattussi M.P., Pauli S., Neutzling M.B. Gender Differences in the Prevalence of Household Food Insecurity: A Systematic Review and Meta-Analysis. Public Health Nutr. 2017;20:902–916. doi: 10.1017/S1368980016002925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.McCordic C., Riley L., Raimundo I. Household Food Security in Maputo: The Role of Gendered Access to Education and Employment. Dev. S. Afr. 2021;38:816–827. doi: 10.1080/0376835X.2021.1932423. [DOI] [Google Scholar]
- 65.Onyutha C. African Food Insecurity in a Changing Climate: The Roles of Science and Policy. Food Energy Secur. 2019;8:e00160. doi: 10.1002/fes3.160. [DOI] [Google Scholar]
- 66.Alam M.M., Siwar C., Murad W., bin Toriman M.E. Impacts of Climate Change on Agriculture and Food Security Issues in Malaysia: An Empirical Study on Farm Level Assessment. World Appl. Sci. J. 2011;14:431–442. doi: 10.31219/osf.io/mdqpz. [DOI] [Google Scholar]
- 67.Sam A.G., Abidoye B.O., Mashaba S. Climate Change and Household Welfare in Sub-Saharan Africa: Empirical Evidence from Swaziland. Food Secur. 2021;13:439–455. doi: 10.1007/s12571-020-01113-z. [DOI] [Google Scholar]
- 68.Ujunwa A., Okoyeuzu C., Kalu E.U. Armed Conflict and Food Security in West Africa: Socioeconomic Perspective. Int. J. Soc. Econ. 2019;46:182–198. doi: 10.1108/IJSE-11-2017-0538. [DOI] [Google Scholar]
- 69.Frith E., Loprinzi P.D. Food Insecurity and Cognitive Function in Older Adults: Brief Report. Clin. Nutr. 2018;37:1765–1768. doi: 10.1016/j.clnu.2017.07.001. [DOI] [PubMed] [Google Scholar]
- 70.Wong J.C., Scott T., Wilde P., Li Y.-G., Tucker K.L., Gao X. Food Insecurity Is Associated with Subsequent Cognitive Decline in the Boston Puerto Rican Health Study. J. Nutr. 2016;146:1740–1745. doi: 10.3945/jn.115.228700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pruessner J.C., Dedovic K., Pruessner M., Lord C., Buss C., Collins L., Dagher A., Lupien S.J. Stress Regulation in the Central Nervous System: Evidence from Structural and Functional Neuroimaging Studies in Human Populations—2008 Curt Richter Award Winner. Psychoneuroendocrinology. 2010;35:179–191. doi: 10.1016/j.psyneuen.2009.02.016. [DOI] [PubMed] [Google Scholar]
- 72.Fenech M. Vitamins Associated with Brain Aging, Mild Cognitive Impairment, and Alzheimer Disease: Biomarkers, Epidemiological and Experimental Evidence, Plausible Mechanisms, and Knowledge Gaps. Adv. Nutr. Int. Rev. J. 2017;8:958–970. doi: 10.3945/an.117.015610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Gao X., Scott T., Falcon L.M., Wilde P.E., Tucker K.L. Food Insecurity and Cognitive Function in Puerto Rican Adults. Am. J. Clin. Nutr. 2009;89:1197–1203. doi: 10.3945/ajcn.2008.26941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chung H.-K., Kim O., Kwak S., Cho Y., Lee K., Shin M.-J. Household Food Insecurity Is Associated with Adverse Mental Health Indicators and Lower Quality of Life among Koreans: Results from the Korea National Health and Nutrition Examination Survey 2012–2013. Nutrients. 2016;8:819. doi: 10.3390/nu8120819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Alaimo K., Olson C.M., Frongillo E.A. Food Insufficiency and American School-Aged Children’s Cognitive, Academic, and Psychosocial Development. Pediatrics. 2001;108:44–53. doi: 10.1542/peds.108.1.44. [DOI] [PubMed] [Google Scholar]
- 76.Chilton M., Rose D. A Rights-Based Approach to Food Insecurity in the United States. Am. J. Public Health. 2009;99:1203–1211. doi: 10.2105/AJPH.2007.130229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kazembe L.N., Nickanor N., Crush J. Informalized Containment: Food Markets and the Governance of the Informal Food Sector in Windhoek, Namibia. Environ. Urban. 2019;31:461–480. doi: 10.1177/0956247819867091. [DOI] [Google Scholar]
- 78.Nickanor N.M. Ph.D. Thesis. University of Cape Town; Cape Town, South Africa: 2014. Food Deserts and Household Food Insecurity in the Informal Settlements of Windhoek, Namibia. [Google Scholar]
- 79.McEvoy C.T., Cardwell C.R., Woodside J.V., Young I.S., Hunter S.J., McKinley M.C. A Posteriori Dietary Patterns Are Related to Risk of Type 2 Diabetes: Findings from a Systematic Review and Meta-Analysis. J. Acad. Nutr. Diet. 2014;114:1759–1775. doi: 10.1016/j.jand.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 80.Livingstone K.M., McNaughton S.A. Dietary Patterns by Reduced Rank Regression Are Associated with Obesity and Hypertension in Australian Adults. Br. J. Nutr. 2017;117:248–259. doi: 10.1017/S0007114516004505. [DOI] [PubMed] [Google Scholar]
- 81.Davison K.M., Marshall-Fabien G.L., Tecson A. Association of Moderate and Severe Food Insecurity with Suicidal Ideation in Adults: National Survey Data from Three Canadian Provinces. Soc. Psychiatry Psychiatr. Epidemiol. 2015;50:963–972. doi: 10.1007/s00127-015-1018-1. [DOI] [PubMed] [Google Scholar]
- 82.Pellowski J.A., Barnett W., Kuo C.C., Koen N., Zar H.J., Stein D.J. Investigating Tangible and Mental Resources as Predictors of Perceived Household Food Insecurity during Pregnancy among Women in a South African Birth Cohort Study. Soc. Sci. Med. 2017;187:76–84. doi: 10.1016/j.socscimed.2017.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Benzekri N.A., Sambou J.F., Ndong S., Diallo M.B., Tamba I.T., Faye D., Sall I., Diatta J.P., Faye K., Cisse O., et al. The Impact of Food Insecurity on HIV Outcomes in Senegal, West Africa: A Prospective Longitudinal Study. BMC Public Health. 2021;21:451. doi: 10.1186/s12889-021-10444-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Musumari P.M., Wouters E., Kayembe P.K., Kiumbu Nzita M., Mbikayi S.M., Suguimoto S.P., Techasrivichien T., Lukhele B.W., El-saaidi C., Piot P., et al. Food Insecurity Is Associated with Increased Risk of Non-Adherence to Antiretroviral Therapy among HIV-Infected Adults in the Democratic Republic of Congo: A Cross-Sectional Study. PLoS ONE. 2014;9:e85327. doi: 10.1371/journal.pone.0085327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Blanco A.J., Micek M.A., Frenkel L.M., Montoya P., Karagianis M., Matunha L., Johnson W., Gloyd S., Pfeiffer J. Loss to Follow-Up Among HIV-Exposed Children in an HIV Clinic in Beira, Mozambique. SAGE Open. 2015;5:215824401559084. doi: 10.1177/2158244015590841. [DOI] [Google Scholar]
- 86.Pires P., Marega A., Craegh J. Food Insecurity and ART Non Adherence, Nampula, Mozambique. Int. J. Res. 2015;2:92–98. [Google Scholar]
- 87.Singer A.W., Weiser S.D., McCoy S.I. Does Food Insecurity Undermine Adherence to Antiretroviral Therapy? A Systematic Review. AIDS Behav. 2015;19:1510–1526. doi: 10.1007/s10461-014-0873-1. [DOI] [PubMed] [Google Scholar]
- 88.Oluma A., Abadiga M., Mosisa G., Etafa W., Fekadu G. Food Insecurity among People Living with HIV/AIDS on ART Follower at Public Hospitals of Western Ethiopia. Int. J. Food Sci. 2020;2020:e8825453. doi: 10.1155/2020/8825453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Nagata J.M., Palar K., Gooding H.C., Garber A.K., Tabler J.L., Whittle H.J., Bibbins-Domingo K., Weiser S.D. Food Insecurity, Sexual Risk, and Substance Use in Young Adults. J. Adolesc. Health. 2021;68:169–177. doi: 10.1016/j.jadohealth.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.MIC Estratégia Nacional de Fortificação de Alimentos (2016–2021) [(accessed on 1 November 2021)]. Available online: https://pt.scribd.com/document/428418816/Estrategia-Nacional-de-Fortificacao-de-Alimentos.
- 91.Macassa G., Salvador E.M., Francisco J.D.C. Food Insecurity in Mozambique: What Do We Know? And What Can Be Done? Volume 59. Gävle Univ. Press; Gävle, Sweden: 2018. p. 16. [Google Scholar]
- 92.McCordic C., Abrahamo E. Family Structure and Severe Food Insecurity in Maputo and Matola, Mozambique. Sustainability. 2019;11:267. doi: 10.3390/su11010267. [DOI] [Google Scholar]
- 93.Doocy S., Emerson J., Colantouni E., Strong J., Mansen K.A., Caulfield L.E., Klemm R., Brye L., Funna S., Nzanzu J.-P., et al. Improving Household Food Security in Eastern Democratic Republic of the Congo: A Comparative Analysis of Four Interventions. Food Secur. 2018;10:649–660. doi: 10.1007/s12571-018-0808-1. [DOI] [Google Scholar]
- 94.Bapolisi W.A., Ferrari G., Bisimwa G., Merten S. Gendered Determinants of Food Insecurity in Ongoing Regional Conflicts, North and South Kivu, the Democratic Republic of Congo. Agric. Food Secur. 2021;10:13. doi: 10.1186/s40066-021-00285-x. [DOI] [Google Scholar]
- 95.Humbwavali J.B., Giugliani C., Nunes L.N., Dalcastagnê S.V., Duncan B.B. Malnutrition and Its Associated Factors: A Cross-Sectional Study with Children under 2 Years in a Suburban Area in Angola. BMC Public Health. 2019;19:220. doi: 10.1186/s12889-019-6543-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Cardoso J., Allwright L., Salvucci V. Characteristics and Determinants of Child Malnutrition in Mozambique, 2003–2011. 147th ed. Volume 2016. UNU-WIDER; Helsinki, Finland: 2016. WIDER Working Paper. [Google Scholar]
- 97.Desyibelew H.D., Dadi A.F. Burden and Determinants of Malnutrition among Pregnant Women in Africa: A Systematic Review and Meta-Analysis. PLoS ONE. 2019;14:e0221712. doi: 10.1371/journal.pone.0221712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Akombi B.J., Agho K.E., Hall J.J., Wali N., Renzaho A.M.N., Merom D. Stunting, Wasting and Underweight in Sub-Saharan Africa: A Systematic Review. Int. J. Environ. Res. Public Health. 2017;14:863. doi: 10.3390/ijerph14080863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Klingberg S., Draper C.E., Micklesfield L.K., Benjamin-Neelon S.E., van Sluijs E.M.F. Childhood Obesity Prevention in Africa: A Systematic Review of Intervention Effectiveness and Implementation. Int. J. Environ. Res. Public Health. 2019;16:1212. doi: 10.3390/ijerph16071212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Robbiati C., Armando A., da Conceição N., Putoto G., Cavallin F. Association between Diabetes and Food Insecurity in an Urban Setting in Angola: A Case–Control Study. Sci. Rep. 2022;12:1084. doi: 10.1038/s41598-022-04888-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The review used existing research data.