Abstract
Objective:
Tourette syndrome (TS) and co-occurring mental, behavioral, and developmental disorders (MBDDs) have been shown to affect peer relationships. This study provides nationally representative estimates of diagnosed TS prevalence and the prevalence of parent-reported bullying victimization and perpetration among US children with and without TS.
Methods:
This study included 2016–2017 National Survey of Children’s Health data on children aged 6 to 17 years (N = 51,001) with parent-reported responses about TS diagnosis and their child’s experiences with bullying victimization and perpetration. We calculated weighted prevalence estimates of diagnosed TS and of bullying indicators among children ever diagnosed with TS compared with peers without TS. We conducted a logistic regression analysis to estimate adjusted prevalence ratios of bullying involvement by TS status, controlling for age, sex, and co-occurring MBDDs.
Results:
By parent report, 0.3% of US children had ever received a diagnosis of TS; most children with a TS diagnosis (83.2%) had a co-occurring MBDD. Among children with TS, 56.1% experienced bullying victimization, 20.7% experienced bullying perpetration, and 15.9% experienced both, compared with 21.6%, 6.0%, and 4.1% for children without TS, respectively. After adjusting for age, sex, and co-occurring MBDDs, only the association between TS and bullying victimization remained statistically significant.
Conclusion:
Compared with children without TS, children with TS overall experience more bullying victimization and perpetration. Health care professionals treating children with TS could assess challenges with peer relationships and co-occurring disorders to provide targeted support and referral.
Bullying involvement in childhood has negative consequences for long-term health and well-being.1,2 Bullying involvement can be perpetration, victimization, or both; can be physical (e.g., hitting, tripping, and breaking someone’s belongings), verbal (e.g., name calling and teasing), or relational/social (e.g., excluding from groups and spreading rumors); and can occur both in-person and virtually.1,3 Victimization and perpetration are associated with negative mental, emotional, and behavioral consequences, with those who are both victims and perpetrators at the highest risk for negative outcomes.1,2 Because of the long-lasting consequences of bullying such as poor school performance, anxiety, depression, and delinquent and aggressive behavior, bullying has been recognized as a significant public health concern.1,4
As a group, children with special health care needs are at increased risk of being bullied.1,2 Based on 2016 National Survey of Children’s Health (NSCH) data, children with special health care needs had a 28% higher prevalence of being bullied by others compared with those without special health care needs.5 Similarly, children with a mental, behavioral, or developmental disorder (MBDD) are more likely than children without these disorders to be both bullied and to bully other children.6 Specifically, children with internalizing problems such as anxiety or depression had 47% higher prevalence of being bullied, children with behavior or conduct problems had 41% higher prevalence of being bullied, and children with speech or language problems had a 65% higher prevalence of being bullied, relative to children without each of those disorders. Furthermore, children with speech or other language disorders, attention-deficit/hyperactivity disorder (ADHD), and learning disabilities had a decreased prevalence of bullying perpetration.5
Bullying is also a significant concern for children with Tourette syndrome (TS)7,8 although previous nationally representative studies of bullying among US children have not included estimates specific to TS.5,6 TS is a tic disorder characterized by involuntary motor and phonic tics that persist for at least 1 year.9 Motor tics are repetitive movements such as blinking. Phonic tics include vocalizations like grunting that are usually sudden and rapid. Tics usually begin in early childhood between the ages of 5 and 8 years.9 In a meta-analysis of community-based studies of TS, prevalence estimates of TS among children aged 0 to 19 years ranged from 0.1% to just over 5%, with a summary estimate of 0.77%.10 Variation in reported prevalence estimates may be due to differences in surveillance methods, including ages of individuals included in the sample population. Nationally representative estimates of TS based on the NSCH from 2009 to 2012 have shown that approximately 0.3% of US children aged 6 to 17 years have ever had TS and 0.2% have current TS, based on parent report of a health care provider diagnosis.11,12 Based on previous estimates, a TS diagnosis was more common in boys than girls and in children who are non-Hispanic White compared with other races.11,12
Tourette syndrome is associated with characteristics that are known to put people with TS at risk for bullying involvement.7,8 TS often co-occurs with one or more additional MBDDs such as ADHD, obsessive-compulsive disorder, anxiety, and depression.11,13,14 Tics and the co-occurring disorders can both independently and concurrently affect peer relationships, including problems making friends and being teased.7,8 In addition, distress and impairment is more common among youth with TS and comorbid conditions compared with TS alone.8,14–16 Children with TS are more likely to have social deficits and poor peer relationships compared with their peers without TS.17,18 One indicator of poor social relationships is bullying involvement. Bullying may be a particular problem for children with tics because it may not only affect social functioning but also increase stress, which can exacerbate tics.14 Results from an online survey found that 26% of children with a chronic tic disorder, including TS, experienced peer victimization; bullying was associated with greater tic severity and tic complexity.8 Children with TS may also experience victimization through bullying by teachers.7
Although older iterations of the NSCH included a question about parents’ concerns related to their child being bullied, a specific item about children’s involvement in bullying victimization was not included until the 2016 NSCH.6 A previous question about children’s involvement in bullying perpetration was also revised in 2016 to mirror the format of the new bullying victimization question. Previous analyses of the 2016 NSCH data showed that 22.7% of US children aged 6 to 17 years were reported by their parents to be victims of bullying and 6.4% of children were reported as perpetrators of bullying.5 Our study used a pooled sample of NSCH 2016–2017 data to (1) present updated national prevalence estimates of TS among US children overall and by demographic factors associated with TS and (2) estimate the prevalence of bullying perpetration and victimization among children with TS compared with children without TS.
METHODS
Data Source
We pooled data from the 2016 and 2017 National Survey of Children’s Health (NSCH) for these analyses. The NSCH is a web-based or mail-out/mail-back paper questionnaire, sponsored and directed by the Health Resources and Services Administration’s (HRSA) Maternal and Child Health Bureau and administered by the US Census Bureau, that allows for estimates of a variety of child-health indicators from a nationally representative sample of noninstitutionalized US children.19,20 Questionnaires were completed by parents or guardians from June 2016 through January 2017 for the 2016 survey (n = 50,212) and from August 2017 through February 2018 for the 2017 survey (n = 21,599).21 The weighted interview completion rate (ICR) was 69.7% and the weighted overall response rate (ORR) was 40.7% for the 2016 survey. For the 2017 survey, the weighted ICR was 70.9%, and the weighted ORR was 37.4%. One child was randomly selected from each sampled household to be the focus of the questionnaire. Data were weighted by the Census Bureau to account for unequal probability of selection of each household and child within the household and for nonresponse. Weights were adjusted further so that estimates reflected the demographic distribution of noninstitutionalized US children.21 The data from 2 survey years were combined using guidance provided by the Census Bureau on producing multiyear estimates. Additional information about the NSCH is available elsewhere.20
Variables
We calculated the prevalence of Tourette syndrome (TS) overall and by sociodemographic characteristics among children aged 6 to 17 years. We also examined the prevalence of bullying victimization and bullying perpetration, among children with and without TS. The respondent parent or guardian (hereby referred to as the parent) was asked “Has a doctor or other health care provider ever told you that this child has Tourette syndrome?” (hereafter referred to as TS). If yes, the parent was asked whether their child currently had TS, and if so, whether the parent would describe the child’s TS as mild, moderate, or severe. Like previous studies, severity indicators for children with reported current TS were dichotomized for analysis (mild versus moderate or severe).11,15 Questions about the child ever receiving a diagnosis were also asked about other mental, behavioral, and developmental disorders (MBDDs). As in previous studies analyzing MBDDs using the NSCH,22,23 we included the following co-occurring MBDDs in our analyses: attention-deficit/hyperactivity disorder (ADHD), behavioral or conduct problems, anxiety problems, depression, autism spectrum disorder, developmental delay, intellectual disability, learning disability, and speech or language disorder. We categorized ADHD and behavioral or conduct problems as externalizing disorders and anxiety problems and depression as internalizing disorders. Autism spectrum disorder, developmental delays, intellectual disability, learning disability, and speech or other language disorder were categorized as learning/developmental disorders.
Parents reported on their child’s involvement in bullying victimization and perpetration by responding to a question about how well do each of the following phrases describe this child, followed by statements: “This child is bullied, picked on, or excluded by other children” (victimization) and “This child bullies others, picks on them, or excludes them” (perpetration). Parents could respond either “Definitely true,” “Somewhat true,” or “Not true.” We collapsed responses of “Definitely true” and “Somewhat true” for each question related to bullying and created dichotomous variables for bullying victimization and bullying perpetuation (yes vs no), consistent with previous research on bullying using the NSCH.5 We also created variables for any bullying involvement (victimization or perpetration), only victimization (experienced victimization but not perpetration), only perpetration (involved in perpetration but not victimization), and both (experienced victimization and perpetration). Sociodemographic characteristics included in the analyses were child age, sex, ethnicity and race, highest level of household education, urbanicity (rural vs urban areas), and federal poverty level, which was derived using multiple imputation techniques to calculate estimates with correct standard errors.21 Estimates related to geography were calculated using restricted data accessed by the HRSA. Children were categorized as living in a metropolitan statistical area (MSA) or living outside an MSA. The US Census Bureau reviewed this data product for unauthorized disclosure of confidential information and approved the disclosure avoidance practices applied to this release (CBDRB-FY20-POP001–0156).
Data Analyses
Across the 2016 and 2017 NSCH, complete data on whether the child had ever been diagnosed with TS were available for 51,001 children aged 6 to 17 years. We calculated overall weighted prevalence estimates and weighted population estimates of parent reports of children ever diagnosed with TS and current TS. We calculated overall weighted prevalence estimates of severity of current TS, ever diagnosed co-occurring MBDDs, and sociodemographic characteristics. We also calculated weighted prevalence estimates of bullying victimization and bullying perpetration among those who were ever diagnosed with TS compared with their peers without a TS diagnosis, as well as by severity of current TS.
We used χ2 p values with an alpha of 0.05 to test the association between ever TS and current TS severity with bullying involvement. To further assess the relationship between TS and experience with bullying, we used a stepwise approach to conduct multiple logistic regressions for each of 4 bullying indicators (victimization, perpetration, both victimization and perpetration, and any involvement), comparing children with TS with children without TS. The first model for each indicator produced unadjusted prevalence ratios (PRs). The second model produced PRs adjusted for child sex and age, which were significantly associated with a TS diagnosis. The third model produced adjusted PRs that additionally controlled for the presence of co-occurring disorders. Prevalence proportions with Clopper-Pearson 95% confidence intervals (CIs) and PRs with Wald 95% CIs were calculated for all unadjusted and adjusted estimates. All analyses were conducted in SAS-callable SUDAAN v11.0.1 (RTI International, Cary, NC) to account for the complex survey design and to apply sample weights that adjust for probability of selection, nonresponse, and the underlying demographic distribution of the target population.19,20
RESULTS
Tourette Syndrome Prevalence
The prevalence of ever being diagnosed with Tourette syndrome (TS) based on parent report was 3.0 per 1,000, representing approximately 150,000 US children aged 6 to 17 years (Table 1). The prevalence of current TS was 2.7 per 1,000, representing approximately 135,000 US children aged 6 to 17 years, or 92% of those who had ever been diagnosed with TS (data not shown). The prevalence of ever receiving a TS diagnosis was 2.43 (95% confidence interval [CI], 1.43–4.15) times higher for children aged 12 to 17 years compared with 6 to 11 years and was 2.89 (95% CI, 1.68–4.96) times higher for boys compared with girls. No significant differences in prevalence of ever-diagnosed TS by race/ethnicity, highest level of parent education, federal poverty level, or urbanicity were found. Over half of children with current TS were described as having mild TS (55.6%; 95% CI, 41.7–68.7); 44.4% (95% CI, 31.3–58.3) had moderate or severe TS.
Table 1.
Prevalence of Ever Receiving a Diagnosis of Tourette Syndrome (TS) Among Children Aged 6 to 17 Years by Selected Sociodemographic Characteristics, National Survey of Children’s Health, 2016–2017
| Variable | Unweighted Sample Sizea | Ever TS (Unweighted) | Weighted Prevalence of TS Per 1,000 (95% CI) | Prevalence Ratio (95% CI) |
|---|---|---|---|---|
|
| ||||
| Total surveyed | 51,001 | 186 | 3.0 (2.4–3.9) | – |
| Age, yr | ||||
| 6–11 | 21,469 | 52 | 1.8 (1.1–2.7) | Ref. |
| 12–17 | 29,532 | 134 | 4.3 (3.1–5.8) | 2.43 (1.43–4.15) |
| Sex | ||||
| Male | 26,059 | 138 | 4.4 (3.2–6.0) | 2.89 (1.68–4.96) |
| Female | 24,942 | 48 | 1.5 (0.9–2.4) | Ref. |
| Race/Ethnicity | ||||
| Non-Hispanic White | 35,700 | 150 | 3.8 (2.9–4.9) | Ref. |
| Other | 15,301 | 36 | 2.2 (1.2–3.7) | 0.59 (0.33–1.05) |
| Highest level of parent education | ||||
| High school diploma or less | 7,826 | 35 | 2.8 (1.4–5.1) | 0.89 (0.47–1.71) |
| At least some college or technical | 42,296 | 150 | 3.2 (2.4–4.1) | Ref. |
| FPL | ||||
| <200% | 13,420 | 52 | 2.6 (1.5–4.1) | 0.78 (0.45–1.35) |
| ≥200% | 37,581 | 134 | 3.3 (2.4–4.5) | Ref. |
| MSA statusb | ||||
| Living outside of a MSA | 9,430 | 30 | 3.3 (1.7–5.8) | 1.10 (0.58–2.09) |
| Living in a MSA | 41,650 | 150 | 3.0 (2.2–3.9) | Ref. |
CI, confidence interval; FPL, Federal Poverty Level.
The sum of the sample sizes within each stratum might not equal the total surveyed because some parents did not know or refused to provide an answer to the question about the characteristic. Missing data for federal poverty level were derived using multiple imputation techniques. Missing data for child sex, race, and ethnicity were imputed using hot-deck imputation. Highest level of parent education (missing n = 879).
Residence in or not in a metropolitan statistical area (MSA) was used as a proxy for urbanicity. Children living in an MSA were considered to be living in an urban/suburban area, and children not living in an MSA were considered to be living in a rural area. Estimates related to urbanicity were calculated using restricted data accessed by the Health Resources and Services Administration because some geographic information is suppressed in the public use file to protect respondent confidentiality; unweighted counts have been rounded as part of the disclosure review process and do not sum to the overall n. The US Census Bureau reviewed this data product for unauthorized disclosure of confidential information and approved the disclosure avoidance practices applied to this release (CBDRB-FY20-POP001-0156).
Approximately 5 of 6 (83.2%; 95% CI, 74.3–89.4) children who had ever been diagnosed with TS had also ever been diagnosed with at least one other co-occurring mental, behavioral, and developmental disorder (MBDD) (data not shown). Anxiety problems were the most common individual co-occurring condition with a prevalence of 61.2% (95% CI, 48.6–72.9) among children with TS, followed by attention-deficit/hyperactivity disorder (52.4%; 95% CI, 39.3–65.2), behavioral or conduct problems (34.4%; 95% CI, 22.9–47.5), and learning disability (33.7%; 95% CI, 22.7–46.1) (Fig. 1). Overall, 61.7% (95% CI, 49.5–72.6) of children ever diagnosed with TS have also been diagnosed with one or more internalizing conditions, 58.3% (95% CI, 45.3–70.2) had been diagnosed with one or more externalizing conditions, and 44.5% (95% CI, 32.7–57.0) had been diagnosed with a learning/developmental disorder (not shown in figure).
Figure 1.
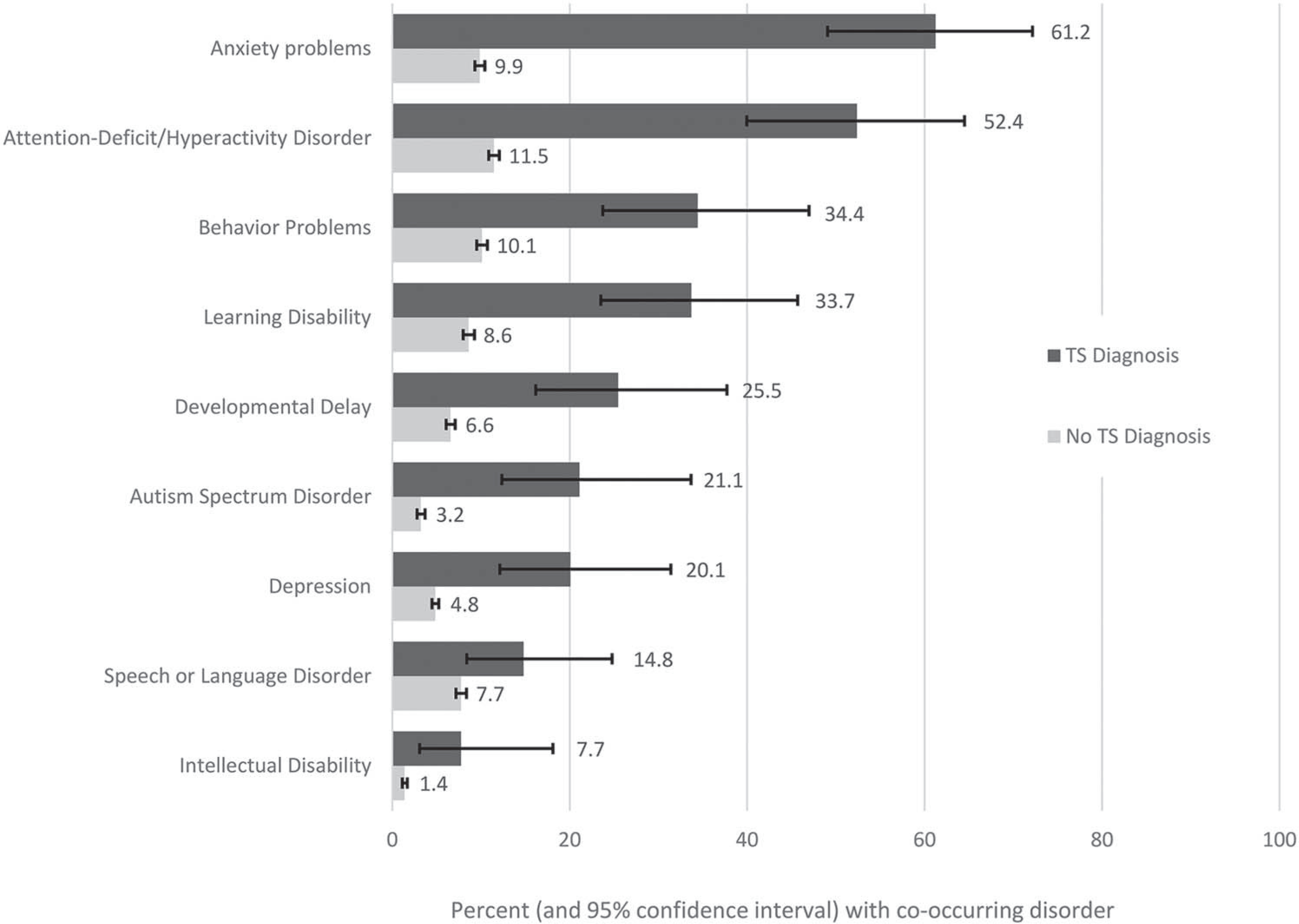
Prevalence of co-occurring mental, behavioral, and developmental disorders by Tourette syndrome (TS) status among children aged 6 to 17 years, National Survey of Children’s Health, 2016–2017.
Tourette Syndrome and Bullying
The overall prevalence of bullying victimization was greater among children who have ever been diagnosed with TS (56.1%) compared with 21.6% among those without TS (p < 0.001; Table 2). Similarly, bullying perpetration was higher among those ever diagnosed with TS (20.7%), compared with 6.0% among those without TS (p = 0.04). The prevalence of any bullying involvement among children with TS was 60.8% compared with 23.5% among children without TS (p < 0.001). The prevalence of being both victim and perpetrator was 15.9% among children ever diagnosed with TS and 4.1% among children without TS (p = 0.08). Children with moderate or severe TS had a higher prevalence of being both a bullying victim and a bullying perpetrator compared with children with mild TS (34.0% vs 4.1%, p = 0.05). Similar patterns were found when comparing prevalence of only victimization among children with and without a TS diagnosis; specifically, children with a TS diagnosis had a higher prevalence of only victimization (40.0% vs 17.4%; p < 0.001), relative to their counterparts without TS.
Table 2.
Unadjusted Percentages of Bullying Indicators by Tourette Syndrome (TS) Status and Severity Among Children Aged 6 to 17 Years, National Survey of Children’s Health, 2016–2017
| Ever TS |
Current TS Severity |
|||||||
|---|---|---|---|---|---|---|---|---|
| Yes | Noa | χ2 p | Prevalence Ratio (95% CI) | Moderate/Severe | Milda | χ2 p | Prevalence Ratio (95% CI) | |
|
| ||||||||
| Victimization | 56.1 (43.1–68.4) | 21.6 (20.8–22.4) | <0.001 | 2.60 (2.08–3.24) | 69.5 (46.1–87.3) | 50.3 (33.5–67.0) | 0.16 | 1.38 (0.90–2.13) |
| Perpetration | 20.7b (9.5–36.4) | 6.0 (5.5–6.5) | 0.04 | 3.47 (1.87–6.44) | 34.3b (12.2–63.0) | 13.1b (4.0–29.2) | 0.16 | 2.62 (0.83–8.23) |
| Both victimization and perpetration | 15.9b (5.9–32.0) | 4.1 (3.7–4.6) | 0.08 | 3.85 (1.79–8.29) | 34.0b (12.0–62.8) | 4.1b (1.1–10.3) | 0.05 | 8.31 (2.55–27.07) |
| Any involvement | 60.8 (48.2–72.5) | 23.5 (22.6–24.3) | <0.001 | 2.59 (2.13–3.16) | 69.8 (46.4–87.5) | 59.3 (42.5–74.6) | 0.42 | 1.18 (0.80–1.73) |
| Only victimization | 40.0 (28.0–52.9) | 17.4 (16.7–18.2) | <0.001 | 2.30 (1.70–3.11) | 35.1 (16.4–58.0) | 46.2 (29.7–63.3) | 0.42 | 0.76 (0.39–1.50) |
| Only perpetration | 4.8c (0.8–14.7) | 1.8 (1.6–2.1) | 0.33 | 2.64 (0.77–9.12) | 0.3c (0.0–7.0) | 9.0c (1.4–27.2) | 0.14 | 0.03 (0.00–0.32) |
CI, confidence interval; RSE, relative standard error.
Referent group for the prevalence ratios shown in this table.
RSE is between 30% and 50% and should be interpreted with caution.
RSE is larger than 50%; estimate is unreliable and should not be used except for inferential statistics (e.g., comparison with other estimates).
The unadjusted prevalence ratio (PR) of bullying victimization among children with TS compared with children without TS was 2.60 (95% CI, 2.08–3.24), and the PR was similar for the model adjusting for child age and sex (PR = 2.62, 95% CI, 2.10–3.26; Table 3). The PR for bullying victimization from the fully adjusted model that controlled for child age, sex, and presence of co-occurring MBDDs was 1.61 (95% CI, 1.13–2.29). For bullying perpetration, the unadjusted PR comparing children with TS with children without TS was 3.47 (95% CI, 1.87–6.44). The PR was similar for the model adjusting only for child sex and age (PR = 3.47, 95% CI, 1.86–6.48), but adding the presence of co-occurring disorders to the fully adjusted model brought the PR to 1.72 with a CI that includes 1.00 (95% CI, 0.73–4.05), suggesting that the association between TS status and bullying perpetration may be explained by the presence of co-occurring disorders. Similarly, the crude model for both victimization and perpetration yielded a PR of 3.85 (95% CI, 1.79–8.29). After adjusting for age and sex, the ratio remained at 3.86 (95% CI, 1.79–8.31), but further adjusting for co-occurring disorders yielded a PR of 1.61 (0.54–4.80) with a CI including 1.00, once again suggesting that the association between TS status and both bullying perpetration and victimization may be explained by the presence of co-occurring disorders. For any bullying involvement, the crude and age and sex adjusted models yielded similar estimates (PR = 2.59, 95% CI, 2.13–3.16 vs PR = 2.61, 95% CI, 2.15–3.17, respectively). The fully adjusted PR for any bullying involvement for children with TS compared with those without TS was 1.68 (95% CI, 1.23–2.30). Of note, numerous co-occurring disorders were also associated with bullying victimization (all examined except intellectual disability) and bullying perpetration (depression and behavioral problems; Table 3).
Table 3.
Adjusted Associations Between Bullying Indicators and Tourette Syndrome (TS) Status, Sociodemographic Characteristics, and Co-occurring Mental, Behavioral, and Developmental Disorders in Children Aged 6 to 17 Years, National Survey of Children’s Health, 2016–2017
| Bullying Victimization Prevalence Ratio (95% CI) |
Bullying Perpetration Prevalence Ratio (95% CI) |
Both Victimization and Perpetration Prevalence Ratio (95% CI) |
Any Bullying Involvement Prevalence Ratio (95% CI) |
|||||
|---|---|---|---|---|---|---|---|---|
| Partially Adjusted Modela | Fully Adjusted Modelb | Partially Adjusted Modela | Fully Adjusted Modelb | Partially Adjusted Modela | Fully Adjusted Modelb | Partially Adjusted Modela | Fully Adjusted Modelb | |
|
| ||||||||
| Ever TS (crude) | 2.60 (2.08–3.24) | 3.47 (1.87–6.44) | 3.85 (1.79–8.29) | 2.59 (2.13–3.16) | ||||
| Ever TS | 2.62 (2.10–3.26) | 1.61 (1.13–2.29) | 3.47 (1.86–6.48) | 1.72 (0.73–4.05) | 3.86 (1.79–8.31) | 1.61 (0.54–4.80) | 2.61 (2.15–3.17) | 1.68 (1.23–2.30) |
| Sex (male vs female) | 1.00 (0.92–1.08) | 0.89 (0.82–0.96) | 1.31 (1.11–1.55) | 1.06 (0.90–1.25) | 1.32 (1.07–1.62) | 1.06 (0.87–1.30) | 1.02 (0.95–1.10) | 0.90 (0.84–0.97) |
| Age, yr (12–17 vs 6–11) | 0.93 (0.86–1.01) | 0.86 (0.79–0.92) | 0.74 (0.63–0.87) | 0.70 (0.59–0.83) | 0.74 (0.60–0.90) | 0.67 (0.54–0.83) | 0.92 (0.85–0.99) | 0.85 (0.79–0.91) |
| Externalizing disorders | ||||||||
| Attention-deficit/hyperactivity disorder | 1.28 (1.13–1.44) | 0.99 (0.81–1.23) | 1.17 (0.92–1.47) | 1.22 (1.08–1.37) | ||||
| Behavior problems | 1.82 (1.62–2.05) | 5.59 (4.49–6.97) | 4.61 (3.56–5.97) | 2.14 (1.93–2.38) | ||||
| Internalizing disorders | ||||||||
| Anxiety problems | 1.51 (1.34–1.70) | 1.12 (0.86–1.46) | 1.02 (0.75–1.37) | 1.53 (1.37–1.71) | ||||
| Depression | 1.75 (1.53–2.01) | 1.81 (1.32–2.48) | 2.40 (1.63–3.52) | 1.69 (1.48–1.93) | ||||
| Developmental disorders | ||||||||
| Autism spectrum disorder | 1.33 (1.02–1.73) | 1.29 (0.77–2.17) | 1.71 (0.93–3.16) | 1.23 (0.94–1.62) | ||||
| Developmental delay | 1.42 (1.20–1.69) | 0.91 (0.66–1.25) | 0.95 (0.64–1.41) | 1.38 (1.17–1.62) | ||||
| Intellectual disability | 0.84 (0.54–1.29) | 0.85 (0.46–1.56) | 0.74 (0.34–1.61) | 0.86 (0.55–1.35) | ||||
| Learning disability | 1.26 (1.09–1.46) | 1.06 (0.81–1.38) | 1.10 (0.80–1.51) | 1.24 (1.08–1.43) | ||||
| Speech or language disorder | 1.13 (0.98–1.30) | 0.79 (0.58–1.08) | 0.78 (0.53–1.14) | 1.11 (0.96–1.27) | ||||
CI, confidence interval.
Adjusting for sex and age.
Adjusting for sex, age, and co-occurring mental, behavioral, and developmental disorders (externalizing, internalizing, and developmental disorders).
DISCUSSION
The prevalence of parent-reported lifetime receipt of a Tourette syndrome (TS) diagnosis was about 1 in 330 children aged 6 to 17 years (3.0 per 1,000) in 2016 to 2017. This estimate is similar to results from a previous nationally representative survey from 2011 to 2012 which calculated the prevalence of ever being diagnosed with TS as 1 in 360 (2.8 per 1,000) children aged 6 to 17 years.13 These estimates are less than half of population estimates of TS using diagnostic criteria in community studies (7.7 per 1,000),10 suggesting that a sizeable number of children who meet criteria for TS may have not received a diagnosis. Consistent with previous studies,11,12 TS was more common among boys, and over half of current TS diagnoses were described as mild in this study population.
The current findings indicate that overall, children ever diagnosed with TS are more often involved in bullying, both as victims and as perpetrators. Approximately 3 in 5 children ever diagnosed with TS (61%) were reported by their parents to be involved in bullying. Furthermore, among children ever diagnosed with TS, approximately 1 in 2 was involved in bullying as a victim and 1 in 5 as a perpetrator; 1 in 6 was both victim and perpetrator. The prevalence of bullying victimization was 2.6 times higher among children with TS compared with children without TS based on unadjusted estimates, and the prevalence of bullying perpetration was more than 3 times higher for children with TS than children without TS. Although experiences with only victimization and only perpetration were less common, the patterns were similar between children with and without TS.
The higher prevalence of any bullying involvement among children with TS could be associated with a number of factors that affect children with TS, including lower social competence, noticeability of tics, and high frequency of co-occurring disorders including anxiety and conduct problems.16,24–27 These factors can negatively influence social interactions by children with TS and thus may make children more likely to act out toward others and also more prone to victimization, for example, by experiencing bullying from teachers or other students who are frustrated with disruptive tics.28,29
In this study, most children with TS (83%) had a co-occurring mental, behavioral, and developmental disorder (MBDD), many of which were independently associated with bullying behaviors, consistent with previous findings.11 This overlap is expected; behavioral or emotional symptoms such as aggression and anxiety can reflect the MBDD diagnosis as well as the experience of bullying, and the connection of MBDD with bullying involvement has been documented.6 The association between TS status and bullying victimization and any bullying involvement remained after adjusting for child sex, age, and presence of other co-occurring disorders. However, the association between TS status and bullying perpetration as well as TS status and both victimization and perpetration resulted in a prevalence ratio with a confidence interval that included 1.00 once adjustments for demographic factors and co-occurring disorders were made. This finding may indicate that the data from the study sample lacked sufficient power to detect a difference in bullying perpetration and both bullying victimization and perpetration between children with and without TS when demographics and co-occurring disorders are considered or that bullying perpetration among children with TS may be associated with co-occurring disorders rather than TS. Given that children with TS experience co-occurring MBDDs more frequently than children without TS (Fig. 1), the relationship of these disorders to bullying perpetration is important to note when considering the effect of bullying on children with TS.
This study is subject to a few limitations. First, all data are parent-reported and may be subject to recall or social desirability bias. Parent-reported diagnoses have not been validated against medical records. Parent report of TS severity may be more related to child functioning than tic noticeability,24 which may influence the interpretation of our findings. Parents may not be present during their child’s bullying involvement and may need to rely on reports from other sources; children may not always report their bullying involvement, and responses may be subject to misclassification because children and parents may differ in their perception of what constitutes bullying involvement.30 Another limitation is that the National Survey of Children’s Health data contain a relatively small sample of children with TS (n = 186) and do not include data for children diagnosed with other persistent tic disorders. Thus, the analyses may be underpowered to detect small-to-moderate differences in bullying indicators, and the findings are specific to TS. In addition, minor changes were made to the bullying items from the 2016 to the 2017 survey. In 2016, the stem question asked, “How well do each of the following phrases describe this child?” (Definitely true, Somewhat True, and Not true). The stem question was modified in 2017: “How true are each of the following statements about this child?” (while keeping the same response options). Although the change was minor, we cannot rule out the possibility of unmeasured effects on bullying item responses because of the slight wording change across survey years.
A final limitation was that the sample size was insufficient to explore characteristics of children with TS who were only perpetrators. Children who are bullying perpetrators without concurrent victimization may use aggression instrumentally, as a way to gain social status.1 These children generally rate higher on social skills and lower on psychopathology.1 In our study, children with TS, particularly mild TS, had notable rates of perpetration only, but the cell sizes were small and resulted in unstable estimates, and co-occurring disorders in this group could not be explored. Future research may be needed to explore this issue in detail because children who use bullying in lieu of prosocial strategies to gain status may need different intervention strategies than children who use bullying while also being victimized.1
Despite these limitations, this study provides nationally representative estimates on the prevalence of TS among US children aged 6 to 17 years and suggests that a substantial percentage of children with TS are affected by bullying behaviors. The results from this paper can be used by health care professionals working with families of children with TS. For example, health care professionals treating children with TS could assess challenges with peer relationships and co-occurring disorders to provide targeted support and referral. Published guidelines for treating TS include assessing for co-occurring disorders and social functioning.14,31 As bullying involvement may contribute to problems with social functioning, increased awareness of the high prevalence of victimization and bullying among children with TS might aid in the treatment of TS by health care professionals. Strategies that may prevent or protect children with TS from bullying include psychoeducation to improve understanding about tics among peers as well as teachers, resilience building, and social skills development.7
Several federal agencies are leading bullying prevention initiatives to address this public health problem. The Centers for Disease Control and Prevention has developed a comprehensive technical package to prevent youth violence, including bullying and associated risk factors.4 The key strategies in this package, such as parenting programs to promote family environments that support healthy development, universal school-based program to strengthen youth’s skills, and reducing exposure to risks to create protective community environments, highlight the importance of family and community environments to support healthy development.4 The approaches for these key strategies are linked to potential outcomes that can affect children at risk for bullying involvement.4 As described in the technical package, parenting programs can improve prosocial behavior and decrease disruptive behavior problems; universal school-based programs can decrease bullying, support academic proficiency, and improve school climate; and protective community environments can decrease youth violence.4 These approaches have many other positive outcomes and can be included in cross-cutting efforts to promote healthy development.4
In addition, in recognition of the fact that bullying within a community is an indicator of that community’s overall health, federal partners have developed several resources to aid state and local leaders in decision-making and resource allocation related to bullying prevention, including online training courses, community action toolkits, and stakeholder-specific prevention guides. The StopBullying.gov website represents interagency efforts established to develop and share research, guidance, and resources at the national, state, and local levels to significantly reduce the prevalence of youth peer-to-peer bullying.4,32 Promising practices are emerging, such as integrating bullying prevention with other approaches to school-based interventions or services that address a range of learning, mental health, and emotional-behavioral health concerns.32 Bullying in youth with disabilities and special health care needs is included in the interagency efforts, but given limited evidence and the increased risk and special challenges among this population, future research and evaluations could identify additional evidence-based strategies to address bullying specifically among children with mental, behavioral, or developmental disorders, including TS.32
Footnotes
Disclosure: The authors declare no conflict of interest.
Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the official policies of the US Department of Health and Human Services, the Centers for Disease Control and Prevention, or the Health Resources and Services Administration, nor does mention of the department or agency names imply endorsement by the US government.
REFERENCES
- 1.National Academies of Sciences Engineering and Medicine. Preventing Bullying Through Science, Policy, and Practice. Washington, DC: The National Academies Press; 2016. [PubMed] [Google Scholar]
- 2.National Research Council. Building Capacity to Reduce Bullying: Workshop Summary. Washington, DC: The National Academies Press; 2014. [PubMed] [Google Scholar]
- 3.Gladden RM, Vivolo-Kantor AM, Hamburger ME, et al. Bullying Surveillance Among Youths: Uniform Definitions for Public Health and Recommended Data Elements, Version 1.0. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention and U.S. Department of Education; 2014. [Google Scholar]
- 4.David-Ferdon C, Vivolo-Kantor AM, Dahlberg LL, et al. A Comprehensive Technical Package for the Prevention of Youth Violence and Associated Risk Behaviors. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2016. [Google Scholar]
- 5.Lebrun-Harris LA, Sherman LJ, Limber SP, et al. Bullying victimization and perpetration among U.S. children and adolescents: 2016 National Survey of Children’s Health. J Child Fam Stud. 2019;28:2543–2557. [Google Scholar]
- 6.Van Cleave J, Davis MM. Bullying and peer victimization among children with special health care needs. Pediatrics. 2006;118: e1212–e1219. [DOI] [PubMed] [Google Scholar]
- 7.Mingbunjerdsuk D, Zinner SH. Coping with tics in school and with peers. Curr Dev Disord Rep. 2020;7:227–236. [Google Scholar]
- 8.Zinner SH, Conelea CA, Glew GM, et al. Peer victimization in youth with Tourette syndrome and other chronic tic disorders. Child Psychiatry Hum Dev. 2012;43:124–136. [DOI] [PubMed] [Google Scholar]
- 9.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). 5th ed. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 10.Knight T, Steeves T, Day L, et al. Prevalence of tic disorders: a systematic review and meta-analysis. Pediatr Neurol. 2012;47:77–90. [DOI] [PubMed] [Google Scholar]
- 11.Bitsko RH, Holbrook JR, Visser SN, et al. A national profile of Tourette syndrome, 2011–2012. J Dev Behav Pediatr. 2014;35: 317–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. Prevalence of diagnosed Tourette syndrome in persons aged 6–17 years—United States, 2007. MMWR Morb Mortal Wkly Rep. 2009;58:581–585. [PubMed] [Google Scholar]
- 13.Freeman RD, Fast DK, Burd L, et al. An international perspective on Tourette syndrome: selected findings from 3500 individuals in 22 countries. Dev Med Child Neurol. 2000;42:436–447. [DOI] [PubMed] [Google Scholar]
- 14.Murphy TK, Lewin AB, Storch EA, et al. American Academy of Child and Adolescent Psychiatry Committee on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with tic disorders. J Am Acad Child Adolesc Psychiatry. 2013;52:1341–1359. [DOI] [PubMed] [Google Scholar]
- 15.Claussen AH, Bitsko RH, Holbrook JR, et al. Impact of Tourette syndrome on school measures in a nationally representative sample. J Dev Behav Pediatr. 2018;39:335–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Debes N, Hjalgrim H, Skov L. The presence of attention-deficit hyperactivity disorder (ADHD) and obsessive-compulsive disorder worsen psychosocial and educational problems in Tourette syndrome. J Child Neurol. 2010;24:171–181. [DOI] [PubMed] [Google Scholar]
- 17.Stokes A, Bawden HN, Camfield PR, et al. Peer problems in Tourette’s disorder. Pediatrics. 1991;87:936–942. [PubMed] [Google Scholar]
- 18.McGuire JF, Hanks C, Lewin AB, et al. Social deficits in children with chronic tic disorders: phenomenology, clinical correlates and quality of life. Compr Psychiatry. 2013;54:1023–1031. [DOI] [PubMed] [Google Scholar]
- 19.Health Resources and Services Administration Maternal and Child Health Bureau. National Survey of Children’s Health. Available at: https://mchb.hrsa.gov/data/national-surveys. Published 2018. Accessed March 27, 2020.
- 20.Ghandour RM, Jones JR, Lebrun-Harris LA, et al. The design and implementation of the 2016 National Survey of Children’s Health. Matern Child Health J. 2018;22:1093–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.U.S. Census Bureau. National Survey of Children’s Health Methodology and Data User FAQs. Available at: https://www.census.gov/programs-surveys/nsch/technical-documentation/methodology.html. Published 2019. Accessed April 22, 2020.
- 22.Claussen AH, Robinson LR, Kaminski JW, et al. Factors associated with self-regulation in a nationally representative sample of children ages 3–5 years: United States, 2016. Matern Child Health J. 2021;25:27–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cree RA, Bitsko RH, Robinson LR, et al. Health care, family, and community factors associated with mental, behavioral, and developmental disorders and poverty among children aged 2–8 years—United States, 2016. MMWR Morb Mortal Wkly Rep. 2018; 67:1377–1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wolicki SB, Bitsko RH, Danielson ML, et al. Children with Tourette syndrome in the United States: parent-reported diagnosis, co-occurring disorders, severity, and influence of activities on tics. J Dev Behav Pediatr. 2019;40:407–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eapen V, Cavanna AE, Robertson MM. Comorbidities, social impact, and quality of life in Tourette syndrome. Front Psychiatry. 2016;7:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gutierrez-Colina AM, LaMotte J, Eaton C, et al. The role of self-competence in health-related quality of life and behavioral functioning of children with Tourette syndrome. J Dev Behav Pediatr. 2015;36:743–751. [DOI] [PubMed] [Google Scholar]
- 27.Bitsko RH, Danielson ML, Leeb RT, et al. Indicators of social competence and social participation among U.S. children with Tourette syndrome. J Child Neurol. 2020;35:612–620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grace R, Russell C. Tourette’s syndrome and the school experience: a qualitative study of children’s and parents’ perspectives. Australas J Spec Educ. 2016;29:40–59. [Google Scholar]
- 29.Packer LE. Tic-related school problems: impact on functioning, accommodations, and interventions. Behav Modif. 2005;29:876–899. [DOI] [PubMed] [Google Scholar]
- 30.Holt MK, Kaufman Kantor G, Finkelhor D. Parent/child concordance about bullying involvement and family characteristics related to bullying and peer victimization. J Sch Violence. 2008;8:42–63. [Google Scholar]
- 31.Pringsheim T, Okun MS, Müller-Vahl K, et al. Practice guideline recommendations summary: treatment of tics in people with Tourette syndrome and chronic tic disorders. Neurology. 2019;92: 896–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.U.S. Department of Health and Human Services. Available at: https://www.stopbullying.gov/. Published 2020. Accessed March 27, 2020.


