Abstract
The development of vaccines against COVID-19 has given hope to populations. Public acceptability of vaccination is a major driver in containing the disease. However, in marginalized and stigmatized populations, uncertainty and unwillingness may be a challenge. This study aimed to analyze the factors associated with uncertainty and unwillingness to vaccinate against COVID-19 in men who have sex with men (MSM) living in France. The data used came from Rapport au Sexe (ERAS) 2021, a voluntary, cross-sectional, anonymous, self-administered, online survey conducted from 26 February to 11 April 2021. Among the 15,426 respondents included in the analysis, 60.5% were willing to vaccinate (these included persons already vaccinated), 17.5% were not, and 22% were uncertain. Factors independently associated with uncertainty and unwillingness were lower education level, low health literacy level, financial hardship, being under 30 years of age, and living in a rural area. HIV-positive MSM were less likely to report vaccination uncertainty and unwillingness than HIV-negative MSM and those with unknown serostatus. Although more impacted by COVID-19, socioeconomically vulnerable MSM were the sub-group most unwilling to vaccinate. To improve acceptability of COVID-19 vaccination in MSM, policy makers and researchers must increase access to and understanding of medical information by considering the general public’s health literacy when developing information sources. Moreover, a dedicated global care approach, which ensures these populations can be reached, is necessary.
Keywords: vaccine-hesitancy, uncertainty, unwillingness, COVID-19 vaccine, men who have sex with men, health literacy, social inequalities
1. Introduction
In December 2019, an unusually high number of cases of viral pneumonia were reported in Wuhan, China. The rapid spread of the associated virus SARS-CoV-2, and the consequent infection COVID-19, quickly became a concern for global health authorities. The WHO declared a pandemic on 11 March 2020. The lack of a cure or vaccine at the time, and the high transmissibility of the infection led to protective measures, such as national lockdowns and curfews. Meanwhile, scientists put all their efforts into developing a COVID-19 vaccine. For the first time in modern medical history, mRNA-based vaccines were rapidly developed in less than a year. By the end of 2020, studies had shown the safety and efficacy of the Moderna and Pfizer/BioNtech mRNA vaccines [1,2]. Furthermore, the AstraZeneca vaccine (ChAdOx1 nCoV-19 vaccine-AZD1222) using viral vector technology had shown positive safety and efficacy results [3]. A study confirmed the effectiveness of these COVID-19 vaccines [4].
In France, the vaccination strategy began on 27 December 2020; it consisted of phased vaccination, first prioritizing the elderly and/or those weakened by morbidity factors, in order to protect people most likely to develop a serious form of the disease. Priority was also given to health professionals. Only from 12 May 2021 was vaccination extended to people under 50 years old.
Vaccination is a crucial driver in containing the COVID-19 pandemic. However, unwillingness to be vaccinated is widespread worldwide [5]. In June 2020, intention to vaccinate against COVID-19 differed greatly between countries. France, Poland, and Russia had the lowest rates worldwide (58.9%, 56.3%, and 54.9%, respectively) [6]. Previous studies showed gender differences in unwillingness to be vaccinated against COVID-19, with significant unwillingness in women [7,8]. Several factors have been associated with uncertainty or unwillingness, including age, education level, socioeconomic status, perceived seriousness of COVID-19, and sexual orientation [6,7,9,10,11]. For example, in Puerto Rico, gay self-identity was associated with greater intention to be vaccinated [9].
Marginalization and systematic discrimination of sexual minorities led to inequalities of all kinds. The COVID-19 health crisis has had a greater impact on sexual minorities than the general population, particularly men who have sex with men (MSM) [12]. It has highlighted pre-existing vulnerabilities specific to MSM in terms of health, isolation, socioeconomics, and mental health [12,13,14,15,16]. These vulnerabilities may have exacerbated stigma and internalized homonegativity (feelings of guilt, inferiority, and low self-esteem), two factors associated with low utilization of care and poor preventive behaviors [17,18].
In addition, the rapid development of COVID-19 vaccines, and the divergent medical information regarding these vaccines and the pandemic, may have triggered or reinforced COVID-19 vaccine hesitancy in people with low health literacy [19,20]. While several studies have documented factors associated with intention to vaccinate in the general population, few have focused on sexual minorities [21,22]. Knowing that the binary consideration of gender and the omission of sexual orientation in access to care could be a source of inequality, we must make efforts to build an inclusive environment for equity. This study aimed to investigate factors associated with intention to vaccinate against COVID-19 in the MSM population in France.
2. Materials and Methods
2.1. Study Design and Participants
We used data from Rapport au Sexe 2021, a large, cross-sectional online survey of MSM in France conducted between 26 February and 11 April 2021. Respondents who self-identified as homosexual or bisexual or have had sex with a man in their lifetime are considered MSM. The survey was anonymous, self-administered, and voluntary. Participants were recruited through different digital media. Banners were posted directly on gay dating websites, gay geolocation dating applications, gay affinity news sites, and social media networks (Facebook). They were also posted via programmatic platforms targeting men aged 18 years old and over and on browsing pages containing keywords related to homosexuality and male dating. By clicking on these banners, people were directed to the survey site, where information about its objectives was presented as well as the conditions of participation and data confidentiality. By clicking on a button containing the text “I have read and understood the information above”, the participant provided informed consent and was directed to the online questionnaire. No IP address was collected. No financial incentive was given. The only inclusion criterion was being aged 18 years and older.
2.2. Data Collection
2.2.1. Outcome: Intention to Vaccinate against COVID-19
Intention to vaccinate against COVID-19 was measured using the following question: “Do you intend to be vaccinated against Coronavirus? Yes/I have already been vaccinated against the Coronavirus in the last few weeks/I do not know/No”. Respondents were then classified into three groups: willing (already vaccinated or intended to), uncertain (were unsure about vaccination), or unwilling (did not want to be vaccinated).
2.2.2. Independent Variables
The following socioeconomic and demographic characteristics were collected: age, place of birth, area of residence, having a steady relationship with a man, education level, occupational situation, perceived financial situation, and health literacy. Perceived financial situation was measured with the question “Would you say that financially…” (‘you are comfortable’; ‘you get by’; ‘you have to be careful’; ‘you find it difficult to make ends meet’; and ‘you can’t make ends meet without incurring debt’). Response categories were merged to form a three-level variable: comfortable (which covered ‘comfortable’ and ‘you get by’; need to be careful; difficulty and debt).
Health literacy was evaluated using the Health Literacy Questionnaire (HLQ) scale ‘having sufficient information to manage my health’ [23,24]. This scale contains four items, each scored on a 4-point Likert scale. The total score is calculated as the average of the four item scores, and ranges from 1 to 4. Participants were categorized into two groups: low (score ≤ 2.8 1st quartile) and adequate (score > 2.8) health literacy.
Respondents also reported their vaccination history (hepatitis A and hepatitis B) and their HIV status. Furthermore, COVID-19-related information was collected, such as COVID-19-like symptoms or signs (yes/no) and diagnosed with COVID-19 (yes/no). In addition to these individual factors, respondents could report the reasons for their unwillingness to be vaccinated from a list of suggestions (COVID-19 vaccines are unsafe and side effects are not really known, doubts about vaccine effectiveness, COVID-19 is not a very dangerous disease, vaccine hesitant in general, not liking injections, other reasons).
2.3. Statistical Analysis
We performed univariate analyses to describe respondents’ characteristics. Median and interquartile range (IQR) were computed for continuous variables. Categorical variables were expressed as proportions. Chi-squared tests were used to compare categorical data.
To identify factors associated with intention to vaccinate against COVID-19, multinomial logistic models were used. A backward procedure was employed to select statistically significant factors in the multivariate models (entry threshold, p < 0.20). Only factors with a p < 0.05 were kept in the final multivariate model. Statistical analyses were performed using Stata software version 15 (StataCorp, College Station, TX, USA).
3. Results
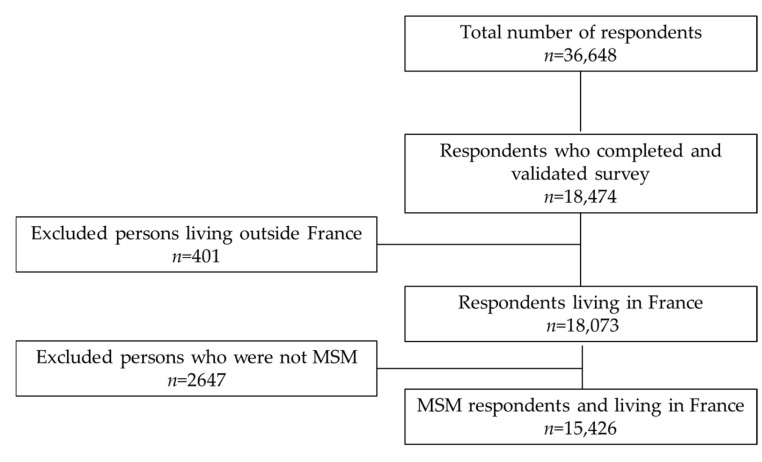
Of the 36,648 people who started the questionnaire, 18,474 (50%) completed and validated it (Figure 1). Respondents who discontinued the questionnaire were younger on average than those who completed it (32.2 vs. 34.7 years). They had lower than the upper secondary school certificate (39.8 vs. 32.1) and were more heterosexual or refused to self-identify (54.8 vs. 21.3) than respondents completed questionnaire. Among the latter, 3048 were excluded because they lived outside France (401) or were not MSM (2647). The majority of the sample (80%) had connected to the survey via social networks.
Figure 1.
Participant flow chart.
Most of the respondents were born in France (94.6%), lived in an urban area (82.8%), and had a third-level education level (68.2%). Just under a third (31.1%) had a low level of health literacy, and 14% perceived their financial situation as difficult. With regard to COVID-19, 42.5% of respondents reported having COVID-19-like symptoms or signs, and 9.7% had been diagnosed with the disease. At the time of the study (February to April 2021), 60.5% of respondents were already COVID-19 vaccinated or intended to vaccinate, 17.5% did not intend to vaccinate, and 22% were uncertain about vaccinating (Table 1).
Table 1.
Participants’ characteristics (n = 15,426).
| n | % | |
|---|---|---|
| Age, median [IQR] (years) | 33 [25–44] | |
| 18–24 | 3828 | 24.8 |
| 25–29 | 2557 | 16.6 |
| 30–44 | 5238 | 34 |
| ≥45 | 3803 | 24.7 |
| Place of birth | ||
| Outside France | 834 | 5.4 |
| France | 14,592 | 94.6 |
| Area of residence | ||
| Rural | 2653 | 17.2 |
| Urban | 12,773 | 82.8 |
| Education level | ||
| Lower than upper secondary school certificate | 2328 | 15.1 |
| Upper secondary school certificate | 2583 | 16.7 |
| Third-level | 10,515 | 68.2 |
| Health literacy | ||
| Low | 4804 | 31.1 |
| Adequate | 10,622 | 68.9 |
| In a steady relationship with a man | ||
| No (Single/separated/other) | 8207 | 46.8 |
| Yes (Married/cohabitation/civil partnership) | 7219 | 53.2 |
| Occupation | ||
| Employee, self-employed | 10,164 | 65.9 |
| Unemployed, not active or retired | 2324 | 15.1 |
| Student | 2938 | 19 |
| Perceived financial situation | ||
| Comfortable | 8978 | 58.2 |
| Need to be careful | 4294 | 27.8 |
| Difficulty and debt | 2154 | 14 |
| Biomedical status | ||
| HIV negative and PrEP user | 1504 | 9.7 |
| HIV negative | 10,002 | 64.8 |
| HIV positive | 1023 | 6.6 |
| Unknown HIV status | 2897 | 18.8 |
| Had COVID-19-type symptoms | ||
| No | 8877 | 57.5 |
| Yes | 6549 | 42.5 |
| Diagnosed with COVID-19 | ||
| No | 13,937 | 90.3 |
| Yes | 1489 | 9.7 |
| Vaccination history (vaccinated against Hepatitis A or B) | ||
| No | 5279 | 34.2 |
| Yes | 10,147 | 65.8 |
| Intention to vaccinate against COVID-19 | ||
| Willing (already vaccinated and intended) | 9335 | 60.5 |
| Uncertain | 3399 | 22 |
| Unwilling | 2692 | 17.5 |
Factors Associated with Uncertainty and Unwillingness to Receive the COVID-19 Vaccine
In univariate analyses, uncertainty and unwillingness were associated with age, occupation, area of residence (i.e., urban versus rural) and vaccination for hepatitis A and B diseases (Table 2).
Table 2.
Univariate analyses of factors associated with intention to vaccinate against COVID-19 (n = 15,426).
| Intention to Get Vaccinations against COVID-19 | |||||||
|---|---|---|---|---|---|---|---|
| Willing n = 9335 |
Uncertainly n = 3399 |
Unwillingness n = 2692 |
|||||
| n | % | n | % | n | % | p-Value | |
| Age (years) | *** | ||||||
| 18–24 | 2008 | 52.5 | 1029 | 26.9 | 791 | 20.7 | |
| 25–29 | 1391 | 54.4 | 595 | 23.3 | 571 | 22.3 | |
| 30–44 | 3077 | 58.7 | 1218 | 23.3 | 943 | 18 | |
| ≥45 | 2859 | 75.2 | 557 | 14.6 | 387 | 10.2 | |
| Place of birth | *** | ||||||
| Outside France | 595 | 71.3 | 149 | 17.9 | 90 | 10.8 | |
| France | 8740 | 59.9 | 3250 | 22.3 | 2602 | 17.8 | |
| Area of residence | *** | ||||||
| Rural | 1287 | 48.5 | 686 | 25.9 | 680 | 25.6 | |
| Urban | 8048 | 63 | 2713 | 21.2 | 2012 | 15.8 | |
| Education level | *** | ||||||
| Lower than upper secondary school certificate | 1010 | 43.4 | 627 | 26.9 | 691 | 29.7 | |
| Upper secondary school certificate | 1228 | 47.5 | 716 | 27.7 | 639 | 24.7 | |
| Third-level | 7097 | 67.5 | 2056 | 19.6 | 1362 | 13 | |
| Health literacy | *** | ||||||
| Low | 2679 | 55.8 | 1179 | 24.5 | 946 | 19.7 | |
| Adequate | 6656 | 62.7 | 2220 | 20.9 | 1746 | 16.4 | |
| In a steady relationship with a man | *** | ||||||
| No (Single/separated/other) | 4724 | 57.6 | 1903 | 23.2 | 1580 | 19.3 | |
| Yes (Married/cohabitation/civil partnership) | 4611 | 63.9 | 1496 | 20.7 | 1112 | 15.4 | |
| Occupation | *** | ||||||
| Employee, self-employed | 6316 | 62.1 | 2155 | 21.2 | 1693 | 16.7 | |
| Unemployed, not active or retired | 1304 | 56.1 | 506 | 21.8 | 514 | 22.1 | |
| Student | 1715 | 58.4 | 738 | 25.1 | 485 | 16.5 | |
| Perceived financial situation | *** | ||||||
| Comfortable | 6021 | 67.1 | 1771 | 19.7 | 1186 | 13.2 | |
| Need to be careful | 2328 | 54.2 | 1065 | 24.8 | 901 | 21 | |
| Difficulty and debt | 986 | 45.8 | 563 | 26.1 | 605 | 28.1 | |
| Biomedical status | *** | ||||||
| HIV negative and PrEP user | 1134 | 75.4 | 250 | 16.6 | 120 | 8 | |
| HIV negative | 5946 | 59.4 | 2253 | 22.5 | 1803 | 18 | |
| HIV positive | 801 | 78.3 | 134 | 13.1 | 88 | 8.6 | |
| Unknown HIV status | 1454 | 50.2 | 762 | 26.3 | 681 | 23.5 | |
| Vaccination history (vaccinated against Hepatitis A or B) | *** | ||||||
| No | 2739 | 51.9 | 1353 | 25.6 | 1187 | 22.5 | |
| Yes | 6596 | 65 | 2046 | 20.2 | 1505 | 14.8 | |
| Had symptoms or signs of COVID-19 | *** | ||||||
| No | 5290 | 59.6 | 1944 | 21.9 | 1643 | 18.5 | |
| Yes | 4045 | 61.8 | 1455 | 22.2 | 1049 | 16 | |
| Diagnosed with COVID-19 | *** | ||||||
| No | 8351 | 59.9 | 3105 | 22.3 | 2481 | 17.8 | |
| Yes | 984 | 66.1 | 294 | 19.7 | 211 | 14.2 | |
*** p-value < 0.001.
MSM aged 25–29 years old were more likely to report unwillingness to vaccinate (22.3%) than other age groups (18–24 years: 20.7%, 30–44 years: 18%, and ≥45 years: 10.2%, p < 0.001). Unemployed, inactive, and retired MSM were also more likely to be unwilling to vaccinate. In addition, the relationships between education level, health literacy, financial situation, and intention to vaccinate revealed a socioeconomic gradient. More specifically, MSM with a lower level of education (i.e., <third-level), a lower level of health literacy, and those perceiving their financial situation as difficult, were all more likely to be unwilling to vaccinate or uncertain about it. COVID-19 diagnosis and having had COVID-19-like symptoms were both negatively associated with uncertainty and unwillingness to vaccinate. Finally, HIV-negative MSM using PrEP and HIV-positive MSM were less likely to report uncertainty and unwillingness to vaccinate than HIV-negative MSM or those with unknown serostatus.
In the multivariate analysis, the factors independently associated with uncertainty and unwillingness to vaccinate were the same (Table 3). More specifically, MSM 29 years old and under (18–24 years: Ora = 1.34, 95%CI [1.15–1.56]; 25-29 years: Ora = 1.41, 95%CI [1.24–1.61]), those residing in rural areas (Ora = 1.71, 95%CI [1.52–1.91]), and persons born in France (Ora = 1.67, 95%CI [1.32–2.12]) were more likely to be unwilling to vaccinate against COVID-19. Furthermore, participants with less than third-level education (Ora = 2.11, 95%CI [1.87–2.38] and Ora = 3.09, 95%CI [2.72–3.51], for upper secondary school certificate and lower, respectively), those with low health literacy (Ora = 1.19, 95%CI [1.08–1.32]), and persons who just got by financially (Ora = 1.65, 95%CI [1.49–1.84]) or had a difficult financial situation (Ora = 2.31, 95%CI [2.02–2.63]) were all more likely to be unwilling to vaccinate against COVID-19. The effect sizes of less than third-level education (Ora = 2.12, 95%CI [1.88–2.39] vs. Ora = 3.09, 95%CI [2.72–3.51]) and having a difficult financial situation (Ora = 1.61, 95%CI [1.42–1.83] vs Ora = 2.31, 95%CI [2.02–2.63]) were lower for persons who were uncertain than those who were unwilling. MSM HIV negative using PrEP and HIV positive MSM were less uncertain and less unwilling to vaccinate against COVID-19.
Table 3.
Multivariate analyses using multinomial logistic models of factors associated with intention to vaccinate against COVID-19 (n = 15,426).
| Uncertainly vs. Acceptance | Unwillingness vs. Acceptance | |||
|---|---|---|---|---|
| ORa | 95%CI | ORa | 95%CI | |
| Age (years) | ||||
| 18–24 | 1.26 | 1.09–1.45 | 1.34 | 1.15–1.56 |
| 25–29 | 1.10 | 0.98–1.24 | 1.41 | 1.24–1.61 |
| 30–44 | 1 | 1 | ||
| ≥45 | 0.44 | 0.39–0.50 | 0.36 | 0.31–0.42 |
| Place of birth | ||||
| Outside France | 1 | 1 | ||
| France | 1.33 | 1.10–1.61 | 1.67 | 1.32–2.12 |
| Area of residence | ||||
| Rural | 1.40 | 1.26–1.56 | 1.71 | 1.52–1.91 |
| Urban | 1 | 1 | ||
| Education level | ||||
| Lower than upper secondary school certificate | 2.12 | 1.88–2.39 | 3.09 | 2.72–3.51 |
| Upper secondary school certificate | 1.78 | 1.60–1.99 | 2.11 | 1.87–2.38 |
| Third-level | 1 | 1 | ||
| Health literacy | ||||
| Low | 1.21 | 1.11–1.32 | 1.19 | 1.08–1.32 |
| Adequate | 1 | 1 | ||
| In a steady relationship with a man | ||||
| No (Single/separated/other) | 1 | 1 | ||
| Yes (Married/cohabitant/civil partnership) | 0.86 | 0.79–0.94 | 0.79 | 0.72–0.87 |
| Occupation | ||||
| Employee, self-employed | 1 | 1 | ||
| Unemployed, not active or retired | 0.98 | 0.86–1.11 | 1.08 | 0.95–1.23 |
| Student | 0.83 | 0.72–0.96 | 0.66 | 0.56–0.77 |
| Perceived financial situation | ||||
| Comfortable | 1 | 1 | ||
| Need to be careful | 1.39 | 1.26–1.52 | 1.65 | 1.49–1.84 |
| Difficulty and debt | 1.61 | 1.42–1.83 | 2.31 | 2.02–2.63 |
| HIV status | ||||
| HIV negative and PrEP user | 0.74 | 0.62–0.89 | 0.45 | 0.36–0.57 |
| HIV negative | 0.98 | 0.88–1.10 | 0.93 | 0.83–1.05 |
| HIV positive | 0.57 | 0.46–0.71 | 0.44 | 0.34–0.58 |
| Unknown HIV status | 1 | 1 | ||
| Vaccination history (vaccinated against Hepatitis A or B or HPV) | ||||
| No | 1 | 1 | ||
| Yes | 0.74 | 0.67–0.80 | 0.67 | 0.61–0.74 |
| Had symptoms or signs of COVID-19 | ||||
| No | 1 | 1 | ||
| Yes | 0.93 | 0.85–1.01 | 0.81 | 0.74–0.89 |
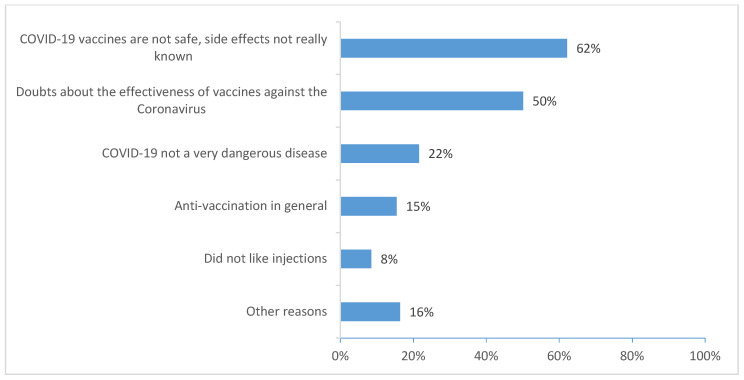
The reasons MSM reported for their unwillingness to vaccinate against COVID-19 were related to the safety and unknown adverse effects of vaccines (62%), doubts about their effectiveness (51%), perceiving COVID-19 not to be dangerous (24%), and being against vaccination in general (16%) (Figure 2).
Figure 2.
Reasons for unwillingness to vaccinate against COVID-19 (ERAS 2021 n = 2692).
4. Discussion
People who are more socially disadvantaged are at a disproportionately greater risk of COVID-19 as well as developing severe forms and dying [25]. The current COVID-19 period has seen sexual minorities, particularly MSM, face a deterioration of their socioeconomic status [12]. The rapid availability of vaccines against COVID-19 has given hope to different populations everywhere. This availability has however been accompanied by growing public vaccine refusal and hesitancy.
In our study, 60% of MSM had already vaccinated against COVID-19 or intended to do so. This rate is very close to those found for the French general population by Lazarus et al. (58.9%) in June 2020, and Neumann-Böhme et al. (62%) in April 2020 [6,26]. A study conducted between April and May 2020 in 5018 participants from the French general population reported that 76% intended to vaccinate (39.9% “probably” and 36.1% “certainly”) [7]. However, in April 2021, the French national survey Coviprev reported a slightly high COVID-19 vaccination uptake rate (68%) [27]. These marginal differences in intention to vaccinate might be related to the different timing of the surveys and also to differences in survey methodology. The ERAS 2021 survey was conducted after vaccinations had begun. They may also be related to the fact that adverse effects after vaccination created a great deal of controversy with the subsequent reluctance by some to vaccinate. A previous study showed that intention to vaccinate against COVID-19 varied according to survey date [7].
Our study showed that the factors associated with uncertainty were the same as those associated with unwillingness. Age and vaccination history were negatively associated with COVID-19 vaccine uncertainty and unwillingness. Older MSM and those previously vaccinated for hepatitis A and/or hepatitis B were less hesitant about vaccination. These results are consistent with findings in previous studies [6,7,28]. One possible explanation is that the possibility to vaccinate was extended to people in France under 50 years of age after this survey was implemented. Unlike Alleaume et al., in our study, living with a partner was associated with a greater likelihood of COVID-19 vaccine uncertainty and unwillingness. Our result regarding the role of social density—measured by several indicators, including area of residence (metropolitan versus urban)—on the likelihood of vaccination, reflects previous research studying the impact on vaccination against COVID-19 or influenza [29]. In addition, this could also be related to reasons of social gradient and isolation. People living in rural areas may be less concerned about the issue and may perceive the disease to be less severe than people in urban areas.
HIV-negative MSM using PrEP and HIV-positive MSM were less likely to be uncertain about vaccination or unwilling to vaccinate. Between February and April 2021, HIV-positive individuals were one of the high-risk populations given vaccination priority in France. Governmental recommendations may therefore have played a role in intention to vaccinate in HIV-positive MSM. For MSM using PrEP, their positive attitude about COVID-19 vaccination might be related to their risk behaviors and lifestyle. The reasons to vaccinate are to protect oneself and to have a positive impact on others within one’s community [29]. In addition, having had COVID-19-like symptoms was negatively associated with vaccine refusal. Being confronted with the reality of the disease may influence the acceptance of the COVID-19 vaccine.
Our results stress the existence of a socioeconomic gradient regarding the intention to vaccinate against COVID-19. Less that third-level education, perceived financial hardship, and low health literacy were associated with a greater likelihood of vaccine hesitancy and unwillingness. With respect to education level and health literacy, our results are consistent with recent studies on intention to vaccinate against COVID-19, as reported in a systematic review [28,30,31]. Difficulties in understanding scientific information—especially complex COVID-19-related information—is a barrier to informed decision-making. Our results reflected those from other studies showing that the two most-cited reasons for unwillingness to vaccinate against the disease were that “COVID-19 vaccines are not safe, side effects not really known (62%)” and “doubts about the effectiveness of COVID-19 vaccines” (50%) [5]. These reasons reflect a poor understanding of health information because current COVID-19 vaccines are considered safe and effective despite moderate side effects [1,2,3]. In terms of financial position, people with financial difficulties often do not have sufficient access to prevention and care services. Other studies have shown that low income is associated with unwillingness to vaccinate against COVID-19 [5,7].
Policy makers and institutions implementing immunization programs face major challenges, including making scientific information accessible, clear, and easy to understand for better adherence by the most vulnerable populations. In addition, providing outreach for population who are the most hesitant about vaccination should be considered, especially for disadvantaged populations. The scientific literature has shown that several actions are favorable to encourage disadvantaged people to be vaccinated. This is the case, for example, of public vaccination of high-profile individuals and community leaders [32]. In addition, mobile vaccination unit programs make it possible to go directly to the vulnerable populations in order to combat misinformation, to convince them and to get them vaccinated [33]. In France, a mobile unit for COVID-19 vaccination has given satisfactory results [34]. Other actions such as the translation of information documents into several languages and the writing plain language have been implemented within the national public health agency in France.
This study has limitations. A low response rate (50% of questionnaires completed and validated), often including heterosexuals not concerned by the study. The methodology of an online survey did not reach MSM who do not use the web. However, given the importance of the internet and social networks in MSM lifestyles, an online survey remains the most relevant and cost-effective methodology for reaching this hard-to-reach population [35]. Sexual, declarative, voluntary surveys—such as ERAS—tend to over-represent men with the strongest gay self-identity [36]. Therefore, our results cannot be generalized to the entire population of MSM living in France for lack of representativeness of the sample. Indeed, the absence of both a sample frame and controls during the inclusion process means that our results cannot be extrapolated to the entire MSM population [37]. Having said that, recruitment via social networks allowed us to diversify the sociodemographic and affinity profiles, and to include MSM who were more distant from the gay community, and persons more economically disadvantaged. Moreover, the timing of the survey (February to April 2021) may have led to an underestimation of overall vaccination acceptance because of misinformation and anti-vaccination campaigns which were prevalent on social networks. These elements may have made it more difficult for people to decide to vaccinate. Furthermore, the suspension of the AstraZeneca vaccine during the survey period may have increased vaccine-hesitancy. However, it should be noted that our vaccine willingness and hesitancy rates were close to those reported in the Coviprev survey [27]. The use of self-perceived measures such as HL could lead to bias. However, the HL had good reliability. Finally, the ERAS survey was not developed specifically to assess vaccine-hesitancy and therefore did not assess all factors that may influence uncertainty and unwillingness, such as perceived current health status, perceived susceptibility of contracting COVID-19, perceived severity of the disease, and perceived benefits of and perceived barriers to vaccination. However, the factors observed in this specific population are consistent with the literature.
5. Conclusions
Uncertainty and unwillingness to be vaccinated is a major problem for vaccination programs. For a global pandemic, such as the COVID-19 crisis, rapid herd immunity must be achieved through mass vaccination. In order to increase vaccination coverage, it is necessary to understand the factors associated with vaccine-hesitancy. More impacted by COVID-19, socioeconomically vulnerable persons in our study were the MSM most reluctant to vaccinate. Vaccine prevalence was lower in vulnerable populations than in the general French population (74.9% with at least one dose vs. 89.3% in the general population, and 72.7% with two doses vaccination vs. 87.3% in the general population) [38]. For a virus that continues to evolve, a 60% vaccination rate for MSM remains low.
Our results will allow decision makers to do targeted work to convince the hesitant and reach out to the most disadvantaged populations (socioeconomically vulnerable MSM and those with a low health literacy level) are often the furthest from the healthcare system. In addition, our results will help improve recall campaigns. To improve acceptability of COVID-19 vaccination in MSM, policy makers and researchers must improve access to and understanding of medical information, by considering health literacy when developing information sources. Moreover, a dedicated global care approach, which ensures these populations can be reached is necessary.
Acknowledgments
The authors thank all the survey participants who gave their time to complete the ERAS 2021-study questionnaire, and Jude Sweeney (Milan, Italy) for the English revision and copyediting of this manuscript.
Author Contributions
Conceptualization, A.V. and N.L.; methodology, Y.M.O., A.V. and N.L.; software, Y.M.O.; validation, Y.M.O., A.V. and N.L.; formal analysis, Y.M.O.; investigation, A.V.; resources, A.V.; data curation, Y.M.O.; writing—original draft preparation, Y.M.O.; writing—review and editing, Y.M.O., S.V. (Sophie Vaux), S.V. (Stéphanie Vandentorren), I.B., K.C., N.L. and A.V.; visualization, Y.M.O.; supervision, A.V.; project administration, A.V.; funding acquisition, A.V. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of the French Institute of Medical Research and Health (IRB0003888, IORG0003254, FWA00005831).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. By clicking on a button containing the text “I have read and understood the information above” the participant provided informed consent and was directed to the online questionnaire. No IP address was collected.
Data Availability Statement
The datasets used and/or analyzed during the current study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by the National Agency for Research on AIDS and Viral Hepatitis (ANRS).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Baden L.R., El Sahly H.M., Essink B., Kotloff K., Frey S., Novak R., Diemert D., Spector S.A., Rouphael N., Creech C.B., et al. Efficacy and Safety of the MRNA-1273 SARS-CoV-2 Vaccine. N. Engl. J. Med. 2021;384:403–416. doi: 10.1056/NEJMoa2035389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Polack F.P., Thomas S.J., Kitchin N., Absalon J., Gurtman A., Lockhart S., Perez J.L., Pérez Marc G., Moreira E.D., Zerbini C., et al. Safety and Efficacy of the BNT162b2 MRNA COVID-19 Vaccine. N. Engl. J. Med. 2020;383:2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Voysey M., Clemens S.A.C., Madhi S.A., Weckx L.Y., Folegatti P.M., Aley P.K., Angus B., Baillie V.L., Barnabas S.L., Bhorat Q.E., et al. Safety and Efficacy of the ChAdOx1 NCoV-19 Vaccine (AZD1222) against SARS-CoV-2: An Interim Analysis of Four Randomised Controlled Trials in Brazil, South Africa, and the UK. Lancet. 2021;397:99–111. doi: 10.1016/S0140-6736(20)32661-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jabłońska K., Aballéa S., Toumi M. The Real-Life Impact of Vaccination on COVID-19 Mortality in Europe and Israel. Public Health. 2021;198:230–237. doi: 10.1016/j.puhe.2021.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin C., Tu P., Beitsch L.M. Confidence and Receptivity for COVID-19 Vaccines: A Rapid Systematic Review. Vaccines. 2021;9:16. doi: 10.3390/vaccines9010016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lazarus J.V., Ratzan S.C., Palayew A., Gostin L.O., Larson H.J., Rabin K., Kimball S., El-Mohandes A. A Global Survey of Potential Acceptance of a COVID-19 Vaccine. Nat. Med. 2021;27:225–228. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alleaume C., Verger P., Dib F., Ward J.K., Launay O., Peretti-Watel P. Intention to Get Vaccinated against COVID-19 among the General Population in France: Associated Factors and Gender Disparities. Hum. Vaccines Immunother. 2021;17:3421–3432. doi: 10.1080/21645515.2021.1893069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nguyen K.H., Nguyen K., Corlin L., Allen J.D., Chung M. Changes in COVID-19 Vaccination Receipt and Intention to Vaccinate by Socioeconomic Characteristics and Geographic Area, United States, January 6–March 29, 2021. Ann. Med. 2021;53:1419–1428. doi: 10.1080/07853890.2021.1957998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Melin K., Zhang C., Zapata J.P., Rivera Y.M., Fernandez K., Shacham E., Malavé-Rivera S.M., Rodriguez-Diaz C.E. Factors Associated with Intention to Receive Vaccination against COVID-19 in Puerto Rico: An Online Survey of Adults. Int. J. Environ. Res. Public Health. 2021;18:7743. doi: 10.3390/ijerph18157743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ruiz J.B., Bell R.A. Predictors of Intention to Vaccinate against COVID-19: Results of a Nationwide Survey. Vaccine. 2021;39:1080–1086. doi: 10.1016/j.vaccine.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schwarzinger M., Watson V., Arwidson P., Alla F., Luchini S. COVID-19 Vaccine Hesitancy in a Representative Working-Age Population in France: A Survey Experiment Based on Vaccine Characteristics. Lancet Public Health. 2021;6:e210–e221. doi: 10.1016/S2468-2667(21)00012-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Velter A., Champenois K., Castro D., Lydie N. Perceived Impact of the COVID-19 Pandemic on Men Who Have Sex with Men in France. Eras COVID-19 Survey, 30 June-15 July 2020.(Dépistage Du VIH: Nouvelles Expérimentations, Données de Surveillance et Impact de La COVID.) [French] Bull. Epidemiol. Hebd. 2020;33:666–672. [Google Scholar]
- 13.Santos G.-M., Ackerman B., Rao A., Wallach S., Ayala G., Lamontage E., Garner A., Holloway I.W., Arreola S., Silenzio V. Economic, Mental Health, HIV Prevention and HIV Treatment Impacts of COVID-19 and the COVID-19 Response on a Global Sample of Cisgender Gay Men and Other Men Who Have Sex with Men. AIDS Behav. 2021;25:311–321. doi: 10.1007/s10461-020-02969-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Camargo E.L.S., de Oliveira B.I.A., Siffoni I.F., de Sousa A.R., Teixeira J.R.B., Mendes I.A.C., de Sousa Á.F.L. Low Psychological Well-Being in Men Who Have Sex with Men (MSM) During the Shelter-in-Place Orders to Prevent the COVID-19 Spread: Results from a Nationwide Study. Sex. Res. Soc. Policy. 2021;19:391–400. doi: 10.1007/s13178-021-00550-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Torres T.S., Hoagland B., Bezerra D.R., Garner A., Jalil E.M., Coelho L.E., Benedetti M., Pimenta C., Grinsztejn B., Veloso V.G. Impact of COVID-19 Pandemic on Sexual Minority Populations in Brazil: An Analysis of Social/Racial Disparities in Maintaining Social Distancing and a Description of Sexual Behavior. AIDS Behav. 2021;25:73–84. doi: 10.1007/s10461-020-02984-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gibb J.K., DuBois L.Z., Williams S., McKerracher L., Juster R.-P., Fields J. Sexual and Gender Minority Health Vulnerabilities during the COVID-19 Health Crisis. Am. J. Hum. Biol. Off. J. Hum. Biol. Counc. 2020;32:e23499. doi: 10.1002/ajhb.23499. [DOI] [PubMed] [Google Scholar]
- 17.Pachankis J., Hatzenbuehler M., Berg R., Fernández-Dávila P., Mirandola M., Marcus U., Weatherburn P., Schmidt A. An Intersectional Analysis of Sexual Minority Men’s HIV Risk When Migrating to or within Europe. Eur. J. Public Health. 2018;28:cky213.790. doi: 10.1093/eurpub/cky212.790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ross M.W., Berg R.C., Schmidt A.J., Hospers H.J., Breveglieri M., Furegato M., Weatherburn P. Internalised Homonegativity Predicts HIV-Associated Risk Behavior in European Men Who Have Sex with Men in a 38-Country Cross-Sectional Study: Some Public Health Implications of Homophobia. BMJ Open. 2013;3:e001928. doi: 10.1136/bmjopen-2012-001928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Montagni I., Ouazzani-Touhami K., Mebarki A., Texier N., Schück S., Tzourio C. Acceptance of a COVID-19 Vaccine Is Associated with Ability to Detect Fake News and Health Literacy. J. Public Health Oxf. Engl. 2021;43:695–702. doi: 10.1093/pubmed/fdab028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Turhan Z., Dilcen H.Y., Dolu İ. The Mediating Role of Health Literacy on the Relationship between Health Care System Distrust and Vaccine Hesitancy during COVID-19 Pandemic. Curr. Psychol. 2021:1–10. doi: 10.1007/s12144-021-02105-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lin Y.-J., Chang Y.-P., Chou W.-J., Yen C.-F. Explicit and Intrinsic Intention to Receive COVID-19 Vaccination among Heterosexuals and Sexual Minorities in Taiwan. Int. J. Environ. Res. Public. Health. 2021;18:7260. doi: 10.3390/ijerph18147260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Teixeira da Silva D., Biello K., Lin W.Y., Valente P.K., Mayer K.H., Hightow-Weidman L., Bauermeister J.A. COVID-19 Vaccine Acceptance among an Online Sample of Sexual and Gender Minority Men and Transgender Women. Vaccines. 2021;9:204. doi: 10.3390/vaccines9030204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Osborne R.H., Batterham R.W., Elsworth G.R., Hawkins M., Buchbinder R. The Grounded Psychometric Development and Initial Validation of the Health Literacy Questionnaire (HLQ) BMC Public Health. 2013;13:658. doi: 10.1186/1471-2458-13-658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Debussche X., Lenclume V., Balcou-Debussche M., Alakian D., Sokolowsky C., Ballet D., Elsworth G.R., Osborne R.H., Huiart L. Characterisation of Health Literacy Strengths and Weaknesses among People at Metabolic and Cardiovascular Risk: Validity Testing of the Health Literacy Questionnaire. SAGE Open Med. 2018;6:2050312118801250. doi: 10.1177/2050312118801250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Public Health England Disparities in the Risk and Outcomes of COVID-19. Public Health England; London, UK: 2020. [Google Scholar]
- 26.Neumann-Böhme S., Varghese N.E., Sabat I., Barros P.P., Brouwer W., van Exel J., Schreyögg J., Stargardt T. Once We Have It, Will We Use It? A European Survey on Willingness to Be Vaccinated against COVID-19. Eur. J. Health Econ. 2020;21:977–982. doi: 10.1007/s10198-020-01208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.CoviPrev: Une Enquête Pour Suivre L’évolution des Comportements et de la Santé Mentale Pendant L’épidémie de COVID-19. [(accessed on 2 November 2021)]. Available online: https://www.santepubliquefrance.fr/etudes-et-enquetes/coviprev-une-enquête-pour-suivre-l’évolution-des-comportements-et-de-la-sante-mentale-pendant-l-epidemie-de-covid-19.
- 28.Al-Amer R., Maneze D., Everett B., Montayre J., Villarosa A.R., Dwekat E., Salamonson Y. COVID-19 Vaccination Intention in the First Year of the Pandemic: A Systematic Review. J. Clin. Nurs. 2022;31:62–86. doi: 10.1111/jocn.15951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jung H., Albarracín D. Concerns for Others Increase the Likelihood of Vaccination against Influenza and COVID-19 More in Sparsely Rather than Densely Populated Areas. Proc. Natl. Acad. Sci. USA. 2021;118:e2007538118. doi: 10.1073/pnas.2007538118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dodd R.H., Cvejic E., Bonner C., Pickles K., McCaffery K.J., Ayre J., Batcup C., Copp T., Cornell S., Dakin T., et al. Willingness to Vaccinate against COVID-19 in Australia. Lancet Infect. Dis. 2021;21:318–319. doi: 10.1016/S1473-3099(20)30559-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sherman S.M., Smith L.E., Sim J., Amlôt R., Cutts M., Dasch H., Rubin G.J., Sevdalis N. COVID-19 Vaccination Intention in the UK: Results from the COVID-19 Vaccination Acceptability Study (CoVAccS), a Nationally Representative Cross-Sectional Survey. Hum. Vaccines Immunother. 2021;17:1612–1621. doi: 10.1080/21645515.2020.1846397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ala A., Wilder J., Jonassaint N.L., Coffin C.S., Brady C., Reynolds A., Schilsky M.L. COVID-19 and the Uncovering of Health Care Disparities in the United States, United Kingdom and Canada: Call to Action. Hepatol. Commun. 2021;5:1791–1800. doi: 10.1002/hep4.1790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Alcendor D.J., Juarez P.D., Matthews-Juarez P., Simon S., Nash C., Lewis K., Smoot D. Meharry Medical College Mobile Vaccination Program: Implications for Increasing COVID-19 Vaccine Uptake among Minority Communities in Middle Tennessee. Vaccines. 2022;10:211. doi: 10.3390/vaccines10020211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ribera-Cano A., Dupont M., Houzé-Cerfon C.-H., Houzé-Cerfon V., Hart A., Hertelendy A.J., Ciottone G., Bounes V. Evaluation of a Prototype Decontamination Mobile Unit (UMDEO) for COVID-19 Vaccination: A Cross-Sectional Survey in France. Vaccine. 2021;39:7441–7445. doi: 10.1016/j.vaccine.2021.10.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Prah P., Hickson F., Bonell C., McDaid L.M., Johnson A.M., Wayal S., Clifton S., Sonnenberg P., Nardone A., Erens B., et al. Men Who Have Sex with Men in Great Britain: Comparing Methods and Estimates from Probability and Convenience Sample Surveys. Sex. Transm. Infect. 2016;92:455–463. doi: 10.1136/sextrans-2015-052389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Velter A., Saboni L., Bouyssou A., Bernillon P., Sommen C., Semaille C. Echantillons de Convenance Par Internet et Par La Presse—Enquête Presse Gays et Lesbiennes 2011. Bull. Sociol. Methodol. Méthodologie Sociol. 2015;126:46–66. doi: 10.1177/0759106315572568. [DOI] [Google Scholar]
- 37.Beyrer C., Baral S.D., van Griensven F., Goodreau S.M., Chariyalertsak S., Wirtz A.L., Brookmeyer R. Global Epidemiology of HIV Infection in Men Who Have Sex with Men. Lancet Lond. Engl. 2012;380:367–377. doi: 10.1016/S0140-6736(12)60821-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Point Epidémiologique COVID-19 du 21 Octobre 2021—Augmentation de L’incidence du SARS-CoV-2: La Plus Grande Vigilance Doit être Apportée Dans un Contexte de Circulation des Virus Hivernaux. [(accessed on 5 November 2021)]. Available online: https://www.santepubliquefrance.fr/presse/2021/point-epidemiologique-covid-19-du-21-octobre-2021-augmentation-de-l-incidence-du-sars-cov-2-la-plus-grande-vigilance-doit-etre-apportee-dans-un.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available on request from the corresponding author.