Abstract
Perinatal maternal anxiety and depression negatively affect intrauterine fetal development, birth outcome, breastfeeding initiation, duration, and milk composition. Antenatal classes potentially reduce the anxiety of pregnant women and may thus contribute to healthy infant development. The study investigates the relationship between participation in online or in-person antenatal classes and levels of anxiety and depression in Polish women during the COVID-19 pandemic. The study group included 1774 adult, non-smoking pregnant women. We compared the state anxiety (STAI-State) and depression levels (EPDS) in women who (i) attended antenatal classes in-person, (ii) attended online classes, and (iii) did not attend any of them. The statistical analyses included a GLM model and trend analysis, while controlling for maternal trait anxiety, age, pregnancy complications, trimester of pregnancy, previous pregnancies, and COVID-19 infections. We observed statistically significant differences in the level of anxiety (and depression). Women who did attend antenatal classes in person had the lowest levels of anxiety and depression. Considering the importance of maternal mental well-being on fetal development, birth outcome, and breastfeeding, in-person participation in antenatal classes should be recommended to pregnant women.
Keywords: breastfeeding, infant development, maternal mental health, pregnancy during the COVID-19 pandemic
1. Introduction
Pregnancy and the perinatal period including breastfeeding is a challenging time for many women who experience numerous physiological and sociological changes. The most common reasons for worries include in utero fetal health, possible delivery complications, and potential problems associated with maternal care [1]. Factors such as maternal age, pregnancy planning, traumatic experiences during previous pregnancy or delivery, medical complications during current pregnancy, as well as previous mental disorders not associated with pregnancy including anxiety and depression might predispose women to high prenatal anxiety [2,3].
Increased maternal anxiety, as well as prenatal depression induce negative consequences for pregnancy outcomes including risk of miscarriage, preterm delivery, C-section, and low infant birth weight [3,4,5]. Studies show that maternal anxiety during the perinatal period also affected breastfeeding. High maternal anxiety is related to lower breastfeeding intention and exclusivity [6], decreased rate of breastfeeding [7], and shorter duration and earlier termination of breastfeeding [8]. Moreover, maternal distress and anxiety is also associated with breast milk composition, negatively affecting its nutritional and immunoactive properties. High maternal stress decreases milk energy density and fat content and changes fatty acid profile [9,10]. It also decreases levels of milk secretory immunoglobulin A and lactoferrin [10,11,12].
Antenatal classes, which aim to transfer practical knowledge about labor, puerperium, breastfeeding, and early parental care, have the potential to decrease maternal anxiety and thus reduce potential risks for breastfeeding and infant development [13,14,15,16]. Studies on antenatal education have shown that participation in classes improves the general mood and well-being of pregnant women, therefore, they can endure labor pain more effectively [15]. Moreover, women attending antenatal classes during pregnancy cope better with pregnancy-related stress during the perinatal period compared to those who received only routine medical care [17]. Participating in antenatal education also decreases risk of breastfeeding cessation during the first month after parturition [16,18] and increases maternal confidence [19] and breastfeeding self-efficacy [20,21].
In addition to an educational role, antenatal classes also fulfill a crucial psychosocial role. The possibility of exchanging information and experiences between parents, under the guidance of a specialist, provides support to the future mother and helps her cope with the upcoming changes. It is worth mentioning the role of the child’s father, who can also participate in these activities. The perspective of sharing a mother’s dilemmas with a partner in a supportive environment allows her to experience the time of pregnancy, childbirth, and breastfeeding in an atmosphere of mutual respect and understanding [13,14], and contributes to her better physical and mental well-being. In accordance, support from partners significantly influences women’s decision to initiate and continue breastfeeding [22,23], and father’s participation in antenatal education is associated with an improved rate of any breastfeeding at six weeks after parturition [24].
Health policies for pregnant women differ between countries. Despite many advantages, participation in antenatal classes is not obligatory in Poland. Due to the limited opportunities (a small number of free public institutions offering classes), pregnant women frequently decide to participate in paid classes, which involves additional costs. Unfortunately, not every pregnant woman can afford such an expense [14,15,16,17].
The COVID-19 pandemic is currently one of the most serious public health problems worldwide with various psycho-emotional disturbances for pregnant women [25]. Pregnancy, childbirth, and breastfeeding during the pandemic represent an additional burden and challenge for women, associated with intensified fear about the health and life of the baby, the course of labor and the entire hospitalization [26], and safety of breastfeeding in the face of possible infection. A study in Ireland found that, since the outbreak of the pandemic, more than 50% of pregnant women always worry about their health, and as many as 35% have changed their daily habits. Due to the fear of potential infection and introduced restrictions, women avoided social contact, did not use public transport, and were more willing to work and do their shopping remotely [27].
Recently, some parts of antenatal and perinatal maternity care have moved to the internet or were done by phone. Previous research found that care in the form of phone calls reduces pregnant women’s feelings of anxiety by an average 5.8 points compared to women who did not receive this form of education and counseling (tele-education: 24.25 ± 4.90, no tele-education: 30.04 ± 8.48; p < 0.001) [28]. However, there is a lack of knowledge if online antenatal classes are as helpful for parents as in-person classes. This study aimed to compare levels of anxiety and depression during pregnancy between (a) participants of online antenatal classes, (b) participants of in-person classes, and (c) pregnant women who did not participate in any kind of antenatal education during the COVID-19 pandemic.
2. Materials and Methods
2.1. Project Description
The presented study is a part of the ongoing, longitudinal Corona Mums Project conducted since May 2020 among women during the pregnancy and postpartum period. The project’s recruitment and information were advertised via Polish social media groups (mainly via Facebook) for pregnant women including Mleko Mamy +, Położna radzi, and Rodzimy razem (all in Polish). We also advertised the study on the project fan page: https://www.facebook.com/mamawkoronieUJ/ (accessed on 19 June 2020), on the radio broadcasts (Radio Rodzina, ESKA, and Radio Kraków), and in the newspapers (Gazeta Wyborcza and Dziennik Polski) and magazines about motherhood (Mamo to ja). The study included an online questionnaire, collecting information about demographics (place of residence, socio-economic status, etc.), mental health assessments, course of pregnancy (including possibility and form of participation in antenatal classes), infection with COVID-19 (self-reported), and complications of pregnancy (such as anemia, diabetes, and preeclampsia). A large part of this questionnaire, except questions about COVID-19 infection and antenatal education, was used in a previous study conducted in lactating women [10,29]. The research was anonymous, and to avoid duplicate responses filling in questionnaires twice from a device with the same ID was blocked.
The study protocol was approved by the Bioethics Committee of the Jagiellonian University (date: 16.12.2020 r., decision number: 1072.6120.359.2020). Informed, written consent was obtained from all participants of the study.
2.2. Study Group
The study group included 1774 women from Poland, aged 19–43 (mean age = 30.26 years; SD = 3.76), non-smokers, who were in the second or third trimester of pregnancy during the COVID-19 pandemic. All participants filled in the online questionnaire (complete information regarding all measured values) between May 2020 and March 2021. Due to the relatively small number of pregnant women in the first trimester (N = 242) and their low interest in participating in antenatal classes (the majority of them had not decided whether to participate), we decided to exclude women in the early stage of pregnancy from the analysis.
2.3. Participation in Antenatal Classes, Anxiety, and Depression
Pregnant women were asked if they participated in antenatal classes and could choose one of three options: (a) yes, I did participate in the classes in-person; (b) yes, I did participate in the online classes; or (c) no, I did not participate in any form of the classes.
State anxiety (STAI-State) and trait anxiety (STAI-Trait) was assessed based on the Polish version of the State-Trait Anxiety Inventory (STAI) [30]. This questionnaire is based on a 4-point Likert scale and includes 40 questions [31].
The Polish version of the Edinburgh Postnatal Depression Scale (EPDS) was used to estimate the prevalence of depressive symptoms during pregnancy [32]. Even though this questionnaire is intended for the postpartum period, it is widely used as a tool to assess depression antenatally. Moreover, due to the longitudinal character of the study with a prepartum and postpartum assessment, it was chosen as the most comprehensive one for repeated measurements. This questionnaire includes 10 items assessing the feelings of self-blame, anxiety, panic attacks, and suicidal thoughts during the previous week [32]. The Polish translation for the both questionnaires is characterized by high validity and reliability (The Cronbach’s alphas: STAI-State: 0.90; STAI-Trait: 0.88; and EPDS: 0.91) [30,32]. The scores based on questionnaires received in our study were not used for diagnostic purposes.
2.4. Statistical Analysis
We used general linear modeling (GLM model) to investigate if different forms of participation in antenatal classes (3 categories) are related to anxiety (STAI-State) and depression (EPDS) while controlling for maternal trait anxiety, age, pregnancy complications (yes/no), trimester of pregnancy (second trimester/third trimester), previous pregnancies (primipara/multipara), and COVID-19 infections (yes/no). Post hoc pairwise comparisons were conducted using Bonferroni correction. Additionally, we employed planned contrast analysis and tested linear trends in the intensity of the depression and anxiety symptoms in women from different study subgroups. A probability value of p < 0.05 indicated statistically significant results. The analyses were performed in SPSS software, version 27 (Chicago, IL, USA).
3. Results
Out of 1774 pregnant women participating in the study, 858 (48.5%) were primiparous and 916 were multiparous. Pregnancy complications occurred in 421 (23.7%) women, 122 were diagnosed with COVID-19 (6.9%), and 673 (37.9%) women were in the second trimester. Among all surveyed women, 633 women (35.7%) participated in antenatal classes in-person, 427 women (24.1%) in online classes, and 714 women (40.2%) did not participate in any classes. Descriptive statistics for each group can be found in Table 1.
Table 1.
Descriptive statistics of the variables in the study groups.
| Variables | Attending Antenatal Classes | Mean | SD |
|---|---|---|---|
| Age (years) | In-person classes | 30.22 | 3.66 |
| Online classes | 29.71 | 3.53 | |
| No classes | 30.61 | 3.94 | |
| STAI-State | In-person classes | 42.2 | 10.61 |
| Online classes | 44.62 | 10.24 | |
| No classes | 46.18 | 11.23 | |
| STAI-Trait | In-person classes | 43.69 | 8.47 |
| Online classes | 44.76 | 8.21 | |
| No classes | 46.17 | 8.49 | |
| EPDS | In-person classes | 7.41 | 4.96 |
| Online classes | 8.28 | 4.95 | |
| No classes | 8.96 | 5.35 | |
| N | % | ||
| Pregnancy complications | |||
| Yes | In-person classes | 247 | 13.9 |
| Online classes | 106 | 6 | |
| No classes | 68 | 3.8 | |
| No | In-person classes | 212 | 12 |
| Online classes | 427 | 24.1 | |
| No classes | 714 | 40.2 | |
| COVID-19 infection | |||
| Yes | In-person classes | 52 | 2.9 |
| Online classes | 23 | 1.3 | |
| No classes | 47 | 2.7 | |
| No | In-person classes | 581 | 32.7 |
| Online classes | 404 | 22.8 | |
| No classes | 667 | 37.6 | |
| Trimester of pregnancy | |||
| Second | In-person classes | 263 | 14.8 |
| Online classes | 116 | 6.5 | |
| No classes | 294 | 16.6 | |
| Third | In-person classes | 370 | 20.9 |
| Online classes | 311 | 17.5 | |
| No classes | 420 | 23.7 | |
| Primiparous | |||
| Yes | In-person classes | 370 | 20.9 |
| Online classes | 298 | 16.8 | |
| No classes | 190 | 10.7 | |
| No | In-person classes | 263 | 14.8 |
| Online classes | 129 | 7.3 | |
| No classes | 524 | 29.5 |
Both the models for anxiety (F15,1771 = 118.98; p < 0.001) and depression (F14,1771 = 3.58; p < 0.001) were statistically significant. After controlling for the confounding factors (maternal age, pregnancy complications, STAI-Trait, COVID-19 infection) the analysis showed significant differences in the levels of state anxiety and depression. The associations between studied factors and the STAI-State and EPDS values are presented in Table 2. The lowest STAI-State and EPDS scores were noted in women who attended in-person classes (STAI: mean = 42.20, SD = 10.61; EPDS: mean = 7.41, SD = 4.96), the intermediate in participants of online classes (STAI: mean = 44.62, SD = 10.24; EPDS: mean = 8.28, SD = 4.95), and the highest in those who did not attend birthing school at all (STAI: mean = 46.18, SD = 11.23; EPDS: mean = 8.96, SD = 5.35).
Table 2.
The association between studied factors and the reported levels of STAI-State and EPDS. Statistically significant results are in bold.
| Anxiety (STAI-State) | Depression (EPDS) | |||||
|---|---|---|---|---|---|---|
| Factors | Mean ± SD | ηp2 | p | Mean ± SD | ηp2 | p |
| Pregnancy complications | 0.004 | 0.011 | 0.004 | 0.011 | ||
| Yes | 43.84 ± 10.80 | 7.02 ± 3.94 | ||||
| No | 46.28 ± 10.71 | 8.06 ± 5.15 | ||||
| COVID-19 infection | 0.001 | 0.291 | 0.001 | 0.341 | ||
| Yes | 43.44 ± 9.25 | 7.78 ± 4.86 | ||||
| No | 44.44 ± 10.99 | 8.27 ± 5.17) | ||||
| Trimester of pregnancy | 0 | 0.413 | 0.003 | 0.032 | ||
| Third | 43.59 ± 10.71 | 7.98 ± 5.08 | ||||
| Second | 44.93 ± 11.01 | 8.43 ± 5.21 | ||||
| Parity | 0.002 | 0.07 | 0.001 | 0.34 | ||
| Primiparas | 43.34 ± 10.81 | 7.95 ± 5.08 | ||||
| Multiparas | 45.36 ± 10.92 | 8.27 ± 5.21 | ||||
| β | β | |||||
| Maternal age | −0.59 | 0.002 | 0.067 | 0.74 | 0.003 | 0.041 |
| STAI-Trait | 1.43 | 0.48 | <0.001 | |||
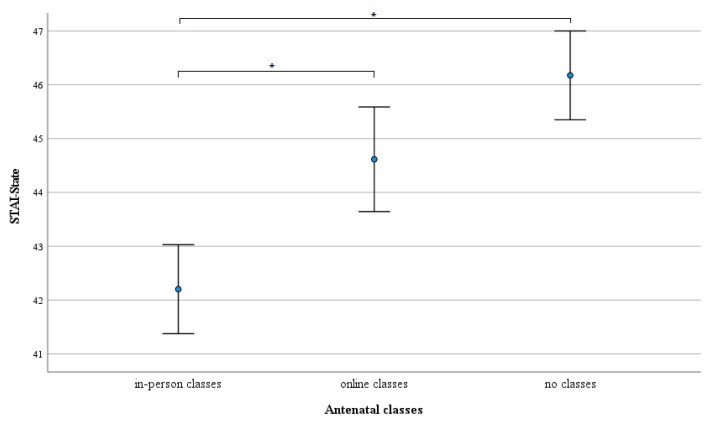
Post hoc pairwise comparisons with the Bonferroni correction showed statistically significant differences in STAI-State between women attending in-person classes and those who attended the online classes (p = 0.002), as well as women who did not attend antenatal classes (p < 0.001). The difference in STAI-State reported by women who took online classes and those not attending antenatal classes were not statistically significant (p = 0.429) (Figure 1).
Figure 1.
Differences in mean levels of state anxiety (dots) between in-person antenatal classes participants, online antenatal classes participants, and non-participants of any kind of antenatal classes adjusted for maternal age, pregnancy complications, COVID-19 infection, and STAI-Trait. Whiskers show 95% CI, * p < 0.05.
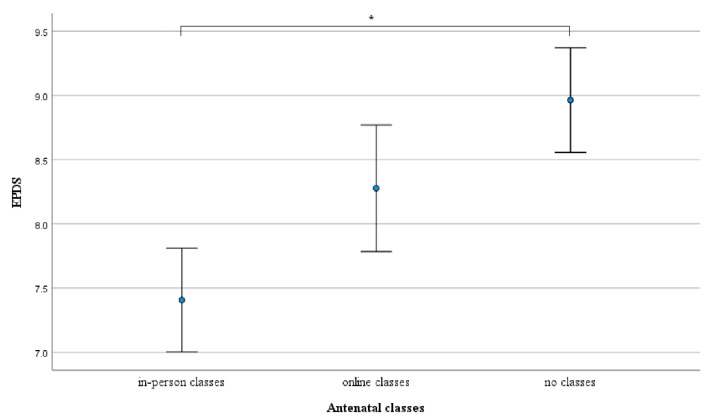
The difference in EPDS Scores between women who attended in-person classes and those women who did not take antenatal classes was statistically significant (p < 0.001). Nonetheless, no statistically significant differences were found between women taking in-person classes and online classes (p = 0.085), and between women attending online classes and women who did not participate in antenatal courses (p = 0.214) (Figure 2).
Figure 2.
Differences in mean levels of depression (dots) between in-person antenatal classes participants, online antenatal classes participants, and non-participants of any kind of antenatal classes adjusted for maternal age, pregnancy complications, and COVID infections. Whiskers show 95% CI, * p < 0.05.
The observed trends in the increase in both STAI-State (F1;1771 = 17.089; p < 0.001) and EPDS Score (F1;1771 = 6.963; p < 0.01) associated with non-participating vs. participating different forms of classes were statistically significant, demonstrating the significant differences between the highest scores among non-participants and the lowest scores among in-person participants of antenatal classes. Referring to other variables, we did not observe a significant effect of COVID-19 infection, parity, maternal age, and pregnancy trimester on STAI-State. Pregnancy complications and STAI-Trait were associated with increased STAI-State (Table 2). The whole model, including antenatal classes participation, accounted for nearly 51% of the variability in STAI-State.
Similarly, COVID-19 infection and parity had no effect on EPDS score. In contrast, pregnancy complications, maternal age, and the pregnancy trimester were associated with the EPDS score. The whole model, including antenatal classes participation, accounted for 3% of the variability in EPDS score.
4. Discussion
The analysis revealed that pregnant women who attended in-person antenatal classes had significantly lower levels of anxiety compared to women who attended online antenatal classes or did not attend these classes. In addition, pregnant women who attended in-person classes had a lower score of EPDS compared to those not participating in classes. The increased trait of anxiety and presence of pregnancy complications were both associated with increased levels of prenatal anxiety, while maternal age, presence of pregnancy complications, and trimester of pregnancy heightened the risk of prenatal depression. Neither COVID-19 infection nor parity had any effect on anxiety levels and risk of depression.
The spread of the SARS-CoV-2 virus and the increased mortality associated with contracting COVID-19 led to the implementation of severe restrictions involving isolation and social distancing in many countries around the world. Pregnant women usually face increased anxiety and risk of depression due to physiological changes, worries about the child’s prenatal development and health, course of delivery, and the postpartum period. During the pandemics, women have been exposed to additional worries associated with limited access to medical care and the potential impact of COVID-19 infection on the unborn child. After delivery, infected women are frequently separated from their newborns due to hospital regulations, which further increases maternal anxiety, hinders mother–infant bonding, and decreases the chance for successful breastfeeding initiation.
Many pregnant women facing worries and problems during pregnancy look for information about childbearing, healthcare, and support from specialists and other mothers while participating in antenatal classes [27,33]. Previous studies showed that participation in antenatal classes is beneficial for pregnant women’s well-being by reducing anxiety and the risk of postnatal depression [15,16,34], especially when these classes included respiratory exercises, mindfulness practices, and learning to cope with anxiety [15,35]. However, due to the pandemic restrictions that were introduced in many countries, including Poland, since March 2020, pregnant women could not or decided not to attend antenatal classes in-person. Instead, nearly one in four gravidas participating in our project decided to attend online classes that were perceived as easily accessible and safe by means of not increasing the risk of infection. Online classes were also recommended in other countries and became an increasingly popular form of antenatal care [36].
A previous study suggested that online antenatal classes can also reduce prenatal anxiety, however, the authors did not compare those results to in-person classes, but solely to no classes at all [37,38,39]. Thus the effectiveness of online classes, when compared to in-person participation, remains questionable. Taking into consideration the increasing popularity of online antenatal classes and the importance of maternal psychological well-being for a child’s prenatal and postnatal development and breastfeeding, determination of the effectiveness of online classes seems to be essential [40]. Our research answers this need by demonstrating that in-person participation in antenatal classes is superior to online classes when it comes to reducing maternal anxiety level.
Prenatal depression results in a number of health issues for children and mothers. For children, it increases the risk of premature birth and fetal growth restrictions [41]. For mothers, it is associated with complications during pregnancy and parturition, “postpartum blues”, and postpartum depression [34,42,43,44]. Prenatal and postnatal depression is also associated with a lower rate of breastfeeding [45], and exclusive breastfeeding duration [40]. Previous studies have shown that the risk for prenatal depression during the COVID-19 pandemic is doubled compared to pre-pandemic levels [46]. In our study, we observed a reduced EPDS score among pregnant women who attended antenatal classes in-person, compared to non-attenders. We also found that the intensity of depression symptoms in online participants did not differ significantly from the non-participants. This observation stands in contrast to the results of a quasi-experimental study from Taiwan, where e-health, web-based antenatal education was associated with lower pregnancy stress and higher self-efficacy than standard education delivered to pregnant women in-person [47,48]. However, it has to be acknowledged that, in the case of this study, routine education was delivered individually. Such a solution excludes the positive effect of peer support from other pregnant women, who co-participate in antenatal classes in Poland. Lack of peer social support may thus explain differences in results between Tsai et al. [49] and our study.
The observed differences in the level of anxiety and depression symptoms between non-participants and participants of different forms of education might have several explanations. First, it is possible that more anxious women were stricter in social distancing, and they preferred staying at home, not participating in antenatal education or choosing online classes. Indeed, studies demonstrate that people with high anxiety and COVID-19 infection fear were predisposed toward more self-care and avoidance behavior [27,42,44,45,46,47]. The strong effect of trait anxiety found in our study suggests that this explanation is plausible. A study with repeated surveying of each participant could aid in testing this hypothesis.
It is also probable that online classes were not as effective as the on-site classes in teaching relaxation. As a consequence, online participants could have encountered problems utilizing relaxation methods in practice, especially as even participants of traditional classes sometimes report problems implementing these methods [15].
Finally, antenatal classes also play a psychological function of peer support. During in-person antenatal classes, women can meet other future mothers and bond with them. Finding support among other antenatal class participants improves well-being and is beneficial to women’s mental health after delivery [48]. Social support was found to be one of the principal factors in decreasing maternal anxiety and depression during the postnatal period. It is also associated with increased birth weight [37,41], and higher levels of immunoactive factors in breast milk [29]. Social distancing and online participation in antenatal classes do not facilitate making new bonds. Although there is a general lack of knowledge about establishing emotional connections among online antenatal classes attendees, university students after online classes reported a sense of loneliness, low social support, and problems with maintaining social networks [47,50,51].
It is unfortunate that during the sanitary restrictions, when most activities are transferred to the virtual world, there are some indications that online classes do not improve the mental well-being of pregnant women as much as in-person classes would. Low maternal psychological well-being during pregnancy may result in higher levels of anxiety and increased depressive symptoms. Thus, it can be associated with less favorable developmental conditions during the prenatal period [3,4,5]. Postnatally, it may result in lower maternal–infant bonding and a lower chance for breastfeeding initiations and a shorter breastfeeding duration. In that perspective, attending in-person antenatal classes associated with lower maternal anxiety and depression symptoms whenever possible would be more beneficial for a child’s development than attending the online substitute.
Our results should be interpreted in light of some limitations. Firstly, although results of our analyses were statistically significant, the overall observed effect size was not large, which can indicate a relatively low difference in anxiety and depression symptoms between participants of various forms of antenatal education. Secondly, we did not collect data on the quality of the classes the participants attended, either online or in person. Hence, in future studies, attendees’ opinions and the received social support should be included in the questionnaire to adequately assess the quality of online antenatal classes. Another limitation is the risk of self-selection and external selection resulting from the level of education of participants or access to online resources. Unfortunately, we do not have information on how many pregnant women participating in the study had symptoms of depression or anxiety before pregnancy. The lack of this information is the next limitation of our study. A final limitation worth mentioning is including women who delivered only a complete set of data. In our study, women who did not complete a significant portion of the questionnaire were excluded from the analysis. Thus, the 1774 participants whose results were statistically analyzed have complete information on all measured values. The use of the complete cases approach may also introduce errors depending on the mechanism of missing data.
5. Conclusions
Maternal prenatal anxiety and depression have a significant impact on breastfeeding and child development during prenatal and postnatal periods. The opportunity to attend antenatal classes is vital in terms of reducing anxiety and depression symptoms and maintaining a positive sense of well-being in pregnant women.
In our research, we observed increased levels of state anxiety in women who did not attend antenatal classes compared to those attending online and in-person classes. Women who did not attend antenatal classes had the highest levels of anxiety and depression. To reduce maternal anxiety and the risk of depression, participating in online and in-person antenatal classes is preferable to not attending.
Due to the better mental well-being of pregnant women attending in-person classes compared to online classes, it should be recommended to use this form of antenatal classes whenever health risks do not outweigh the benefits associated with it.
It is also worth considering the preparation of appropriate psychological support programs that could be presented in social media and traditional media, increasing social awareness of the studied issue.
Acknowledgments
We thank Magdalena Mijas for her significant contribution to the Corona Mums Project.
Author Contributions
Conceptualization, A.C. and U.M.M.; methodology, A.C., U.M.M., D.P.D., A.G. and A.Z.; formal analysis, A.C., D.P.D. and A.G.; investigation, A.C.; data curation, A.A.; writing—original draft preparation, A.C., U.M.M., A.Z. and A.A.; writing—review and editing, A.C., U.M.M., A.G., M.K. and A.Z.; visualization, A.C. and M.K.; project administration, A.C. and U.M.M.; and funding acquisition, U.M.M. and A.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Priority Research Area qLife under the program “Excellence Initiative—Research University” at the Jagiellonian University in Krakow (grant number 06/IDUB/2019/94) and supported by Jagiellonian University in Krakow (grant number N43/DBS/000170).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Bioethics Committee of the Jagiellonian University (date: 16.12.2020 r., decision number: 1072.6120.359.2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy restrictions.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Deklava L., Lubina K., Circenis K., Sudraba V., Millere I. Causes of Anxiety during Pregnancy. Procedia-Soc. Behav. Sci. 2015;205:623–626. doi: 10.1016/j.sbspro.2015.09.097. [DOI] [Google Scholar]
- 2.Schetter C.D., Niles A.N., Guardino C.M., Khaled M., Kramer M.S. Demographic, Medical, and Psychosocial Predictors of Pregnancy Anxiety. Paediatr. Périnat. Epidemiol. 2016;30:421–429. doi: 10.1111/ppe.12300. [DOI] [PubMed] [Google Scholar]
- 3.Rubertsson C., Hellström J., Cross M., Sydsjö G. Anxiety in early pregnancy: Prevalence and contributing factors. Arch. Women’s Ment. Health. 2014;17:221–228. doi: 10.1007/s00737-013-0409-0. [DOI] [PubMed] [Google Scholar]
- 4.Evans J., Heron J., Patel R.R., Wiles N. Depressive symptoms during pregnancy and low birth weight at term. Br. J. Psychiatry. 2007;191:84–85. doi: 10.1192/bjp.bp.105.016568. [DOI] [PubMed] [Google Scholar]
- 5.Koelewijn J.M., Sluijs A.M., Vrijkotte T.G.M. Possible relationship between general and pregnancy-related anxiety during the first half of pregnancy and the birth process: A prospective cohort study. BMJ Open. 2017;7:e013413. doi: 10.1136/bmjopen-2016-013413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fallon V., Groves R., Halford J.C.G., Bennett K.M., Harrold J.A. Postpartum Anxiety and Infant-Feeding Outcomes. J. Hum. Lact. 2016;32:740–758. doi: 10.1177/0890334416662241. [DOI] [PubMed] [Google Scholar]
- 7.English S., Wright I., Ashburn V., Ford G., Caramaschi D. Prenatal anxiety, breastfeeding and child growth and puberty: Linking evolutionary models with human cohort studies. Ann. Hum. Biol. 2020;47:106–115. doi: 10.1080/03014460.2020.1751286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ritchie-Ewing G., Mitchell A.M., Christian L.M. Associations of Maternal Beliefs and Distress in Pregnancy and Postpartum with Breastfeeding Initiation and Early Cessation. J. Hum. Lact. 2019;35:49–58. doi: 10.1177/0890334418767832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kortesniemi M., Slupsky C.M., Aatsinki A.-K., Sinkkonen J., Karlsson L., Linderborg K.M., Yang B., Karlsson H., Kailanto H.-M. Human milk metabolome is associated with symptoms of maternal psychological distress and milk cortisol. Food Chem. 2021;356:129628. doi: 10.1016/j.foodchem.2021.129628. [DOI] [PubMed] [Google Scholar]
- 10.Ziomkiewicz A., Apanasewicz A., Danel D.P., Babiszewska M., Piosek M., Orczyk-Pawiłowicz M. Maternal Distress and Social Support Are Linked to Human Milk Immune Properties. Nutrients. 2021;13:1857. doi: 10.3390/nu13061857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kawano A., Emori Y. The Relationship Between Maternal Postpartum Psychological State and Breast Milk Secretory Immunoglobulin A Level. J. Am. Psychiatr. Nurses Assoc. 2015;21:23–30. doi: 10.1177/1078390314566882. [DOI] [PubMed] [Google Scholar]
- 12.Groer M., Davis M., Steele K. Associations between Human Milk SIgA and Maternal Immune, Infectious, Endocrine, and Stress Variables. J. Hum. Lact. 2004;20:153–158. doi: 10.1177/0890334404264104. [DOI] [PubMed] [Google Scholar]
- 13.Hassanzadeh R., Abbas-Alizadeh F., Meedya S., Mohammad-Alizadeh-Charandabi S., Mirghafourvand M. Fear of childbirth, anxiety and depression in three groups of primiparous pregnant women not attending, irregularly attending and regularly attending childbirth preparation classes. BMC Women’s Health. 2020;20:180. doi: 10.1186/s12905-020-01048-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barimani M., Frykedal K.F., Rosander M., Berlin A. Childbirth and parenting preparation in antenatal classes. Midwifery. 2018;57:1–7. doi: 10.1016/j.midw.2017.10.021. [DOI] [PubMed] [Google Scholar]
- 15.Krysa J., Iwanowicz-Palus G.J., Bień A.M., Rzońca E., Zarajczyk M. Antenatal classes as a form of preparation for parenthood: Analysis of benefits of participating in prenatal education. Pol. J. Public Health. 2016;126:192–196. doi: 10.1515/pjph-2016-0040. [DOI] [Google Scholar]
- 16.Artieta-Pinedo I., Paz-Pascual C., Grandes G., Remiro-Fernandezdegamboa G., Odriozola-Hermosilla I., Bacigalupe A., Payo J. The Benefits of Antenatal Education for the Childbirth Process in Spain. Nurs. Res. 2010;59:194–202. doi: 10.1097/NNR.0b013e3181dbbb4e. [DOI] [PubMed] [Google Scholar]
- 17.Lee L.Y.K., Holroyd E. Evaluating the effect of childbirth education class: A mixed-method study. Int. Nurs. Rev. 2009;56:361–368. doi: 10.1111/j.1466-7657.2008.00701.x. [DOI] [PubMed] [Google Scholar]
- 18.Henderson J., Redshaw M. Midwifery factors associated with successful breastfeeding. Child Care Health Dev. 2011;37:744–753. doi: 10.1111/j.1365-2214.2010.01177.x. [DOI] [PubMed] [Google Scholar]
- 19.Kronborg H., Maimburg R.D., Væth M. Antenatal training to improve breast feeding: A randomized trial. Midwifery. 2012;28:784–790. doi: 10.1016/j.midw.2011.08.016. [DOI] [PubMed] [Google Scholar]
- 20.Wong M.S., Mou H., Chien W.T. Effectiveness of educational and supportive intervention for primiparous women on breastfeeding related outcomes and breastfeeding self-efficacy: A systematic review and meta-analysis. Int. J. Nurs. Stud. 2021;117:103874. doi: 10.1016/j.ijnurstu.2021.103874. [DOI] [PubMed] [Google Scholar]
- 21.Bilgin N.C., Ak B., Ayhan F., Kocyigit F., Yorgun S., Topcuoglu M.A. Effect of childbirth education on the perceptions of childbirth and breastfeeding self-efficacy and the obstetric outcomes of nulliparous women. Health Care Women Int. 2020;41:188–204. doi: 10.1080/07399332.2019.1672171. [DOI] [PubMed] [Google Scholar]
- 22.Davidson E.L., Ollerton R. Partner behaviours improving breastfeeding outcomes: An integrative review. Women Birth. 2020;33:e15–e23. doi: 10.1016/j.wombi.2019.05.010. [DOI] [PubMed] [Google Scholar]
- 23.Chang Y.-S., Li K.M.C., Li K.Y.C., Beake S., Lok K.Y.W., Bick D. Relatively speaking? Partners’ and family members’ views and experiences of supporting breastfeeding: A systematic review of qualitative evidence. Philos. Trans. R. Soc. B Biol. Sci. 2021;376:20200033. doi: 10.1098/rstb.2020.0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maycock B., Binns C.W., Dhaliwal S., Tohotoa J., Hauck Y., Burns S., Howat P. Education and Support for Fathers Improves Breastfeeding Rates: A Randomized Controlled Trial. J. Hum. Lact. 2013;29:484–490. doi: 10.1177/0890334413484387. [DOI] [PubMed] [Google Scholar]
- 25.Wieckiewicz M., Danel D., Pondel M., Smardz J., Martynowicz H., Wieczorek T., Mazur G., Pudlo R., Wieckiewicz G. Identification of risk groups for mental disorders, headache and oral behaviors in adults during the COVID-19 pandemic. Sci. Rep. 2021;11:10964. doi: 10.1038/s41598-021-90566-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Studniczek A., Kossakowska K. Ciąża i poród w czasach pandemii COVID-19: Wybrane aspekty psychologiczne. Kwart. Nauk. Fides Ratio. 2020;43:274–284. doi: 10.34766/fetr.v43i3.417. [DOI] [Google Scholar]
- 27.Corbett G.A., Milne S.J., Hehir M.P., Lindow S.W., O’Connell M.P. Health anxiety and behavioural changes of pregnant women during the COVID-19 pandemic. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020;249:96–97. doi: 10.1016/j.ejogrb.2020.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Derya Y.A., Altiparmak S., Akça E., Gökbulut N., Yilmaz A.N. Pregnancy and birth planning during COVID-19: The effects of tele-education offered to pregnant women on prenatal distress and pregnancy-related anxiety. Midwifery. 2021;92:102877. doi: 10.1016/j.midw.2020.102877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ziomkiewicz A., Babiszewska M., Apanasewicz A., Piosek M., Wychowaniec P., Cierniak A., Barbarska O., Szołtysik M., Danel D., Wichary S. Psychosocial stress and cortisol stress reactivity predict breast milk composition. Sci. Rep. 2021;11:11576. doi: 10.1038/s41598-021-90980-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sosnowski T., Wrześniewski K., Jaworowska A., Fecenec D. STAI—Inwentarz Stanu I Cechy Leku. Psychological Test Laboratory of the PPA; Warsaw, Poland: 2011. (In Polish) [Google Scholar]
- 31.Spielberger C.D. APA PsycTests. American Psychological Association; Washington, DC, USA: 1983. State-Trait Anxiety Inventory for Adults. [DOI] [Google Scholar]
- 32.Kossakowska K. Edynburska Skala Depresji Poporodowej–właściwości psychometryczne i charakterystyka. Acta Univ. Lodz. Folia Psych. 2013;17:39–50. (In Polish) [Google Scholar]
- 33.Cox J.L., Holden J.M., Sagovsky R. Detection of Postnatal Depression. Br. J. Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 34.Kajdy A., Feduniw S., Ajdacka U., Modzelewski J., Baranowska B., Sys D., Pokropek A., Pawlicka P., Kaźmierczak M., Rabijewski M., et al. Risk factors for anxiety and depression among pregnant women during the COVID-19 pandemic: A web-based cross-sectional survey. Medicine. 2020;99:e21279. doi: 10.1097/MD.0000000000021279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kowalska J., Olszowa D., Markowska D., Teplik M., Rymaszewska J. Physical activity and childbirth classes during a pregnancy and the level of perceived stress and depressive symptoms in women after childbirth. Psychiatr. Pol. 2014;48:889–900. doi: 10.12740/PP/24984. [DOI] [PubMed] [Google Scholar]
- 36.Lönnberg G., Jonas W., Unternaehrer E., Bränström R., Nissen E., Niemi M. Effects of a mindfulness based childbirth and parenting program on pregnant women’s perceived stress and risk of perinatal depression–Results from a randomized controlled trial. J. Affect. Disord. 2020;262:133–142. doi: 10.1016/j.jad.2019.10.048. [DOI] [PubMed] [Google Scholar]
- 37.Anderson E., Brigden A., Davies A., Shepherd E., Ingram J. Pregnant women’s experiences of social distancing behavioural guidelines during the COVID-19 pandemic ‘lockdown’ in the UK, a qualitative interview study. BMC Public Health. 2021;21:1202. doi: 10.1186/s12889-021-11202-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bonciani M., Corazza I., De Rosis S. The COVID-19 emergency as an opportunity to co-produce an innovative approach to health services provision: The women’s antenatal classes move on the web. Ital. J. Mark. 2022;2022:59–85. doi: 10.1007/s43039-021-00045-6. [DOI] [Google Scholar]
- 39.Rofiasari L., Noprianty R., Yusita I., Mulyani Y., Suryanah A. Assistance for Pregnant Women Class in Providing Antenatal Care Motivation as an Effort to Improve Maternal and Fetal Health in the Pandemic COVID-19. J. Peduli Masy. 2020;2:197–204. doi: 10.37287/jpm.v2i4.251. [DOI] [Google Scholar]
- 40.Shahid A., Johnson R. Evaluation of an online antenatal course. Understanding pregnancy, labour, birth and your baby’ by the Solihull Approach. Evid. Based Midwifery. 2018;16:101–106. [Google Scholar]
- 41.Grussu P., Quatraro R.M., Jorizzo G.J. Supporting perinatal women in the context of the COVID-19 emergency: Can web-based antenatal education classes make it possible? J. Reprod. Infant Psychol. 2020;38:471–473. doi: 10.1080/02646838.2020.1834261. [DOI] [PubMed] [Google Scholar]
- 42.Kaźmierczak M., Sołdyńska M., Gierszewska M., Gebuza G., Mieczkowska E. Assessment of fear in women before childbirth. Public Health Nurs. 2017;7:69–75. doi: 10.17219/pzp/64034. [DOI] [Google Scholar]
- 43.Grigoriadis S., VonderPorten E.H., Mamisashvili L., Tomlinson G., Dennis C.-L., Koren G., Steiner M., Mousmanis P., Cheung A., Radford K., et al. The Impact of Maternal Depression During Pregnancy on Perinatal Outcomes: A Systematic Review and Meta-Analysis. J. Clin. Psychiatry. 2013;74:e321–e341. doi: 10.4088/JCP.12r07968. [DOI] [PubMed] [Google Scholar]
- 44.Fairlie T.G., Gillman M.W., Rich-Edwards J. High Pregnancy-Related Anxiety and Prenatal Depressive Symptoms as Predictors of Intention to Breastfeed and Breastfeeding Initiation. J. Women’s Health. 2009;18:945–953. doi: 10.1089/jwh.2008.0998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dias C.C., Figueiredo B. Breastfeeding and depression: A systematic review of the literature. J. Affect. Disord. 2015;171:142–154. doi: 10.1016/j.jad.2014.09.022. [DOI] [PubMed] [Google Scholar]
- 46.Rosa A.O.-L., Chuquichambi E.G., Ingram G.P.D. Keep your (social) distance: Pathogen concerns and social perception in the time of COVID-19. Pers. Individ. Differ. 2020;166:110200. doi: 10.1016/j.paid.2020.110200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mohammadpour M., Ghorbani V., Khoramnia S., Ahmadi S.M., Ghvami M., Maleki M. Anxiety, Self-Compassion, Gender Differences and COVID-19: Predicting Self-Care Behaviors and Fear of COVID-19 Based on Anxiety and Self-Compassion with an Emphasis on Gender Differences. Iran. J. Psychiatry. 2020;15:213–219. doi: 10.18502/ijps.v15i3.3813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Durankuş F., Aksu E. Effects of the COVID-19 pandemic on anxiety and depressive symptoms in pregnant women: A preliminary study. J. Matern.-Fetal Neonatal Med. 2020;35:205–211. doi: 10.1080/14767058.2020.1763946. [DOI] [PubMed] [Google Scholar]
- 49.Tsai Y.-J., Hsu Y.-Y., Hou T.-W., Chang C.-H. Effects of a Web-Based Antenatal Care System on Maternal Stress and Self-Efficacy During Pregnancy: A Study in Taiwan. J. Midwifery Women’s Health. 2018;63:205–213. doi: 10.1111/jmwh.12685. [DOI] [PubMed] [Google Scholar]
- 50.Nolan M.L., Mason V., Snow S., Messenger W., Catling J., Upton P. Making Friends at Antenatal Classes: A Qualitative Exploration of Friendship Across the Transition to Motherhood. J. Perinat. Educ. 2012;21:178–185. doi: 10.1891/1058-1243.21.3.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Elmer T., Mepham K., Stadtfeld C. Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS ONE. 2020;15:e0236337. doi: 10.1371/journal.pone.0236337. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy restrictions.