Abstract
Substantial racial/ethnic and gender disparities in COVID-19 mortality have been previously documented. However, few studies have investigated the impact of individual socioeconomic position (SEP) on these disparities. Objectives: To determine the joint effects of SEP, race/ethnicity, and gender on the burden of COVID-19 mortality. A secondary objective was to determine whether differences in opportunities for remote work were correlated with COVID-19 death rates for sociodemographic groups. Design: Annual mortality study which used a special government tabulation of 2020 COVID-19-related deaths stratified by decedents’ SEP (measured by educational attainment), gender, and race/ethnicity. Setting: United States in 2020. Participants: COVID-19 decedents aged 25 to 64 years old (n = 69,001). Exposures: Socioeconomic position (low, intermediate, and high), race/ethnicity (Hispanic, Black, Asian, Indigenous, multiracial, and non-Hispanic white), and gender (women and men). Detailed census data on occupations held by adults in 2020 in each of the 36 sociodemographic groups studied were used to quantify the possibility of remote work for each group. Main Outcomes and Measures: Age-adjusted COVID-19 death rates for 36 sociodemographic groups. Disparities were quantified by relative risks and 95% confidence intervals. High-SEP adults were the (low-risk) referent group for all relative risk calculations. Results: A higher proportion of Hispanics, Blacks, and Indigenous people were in a low SEP in 2020, compared with whites. COVID-19 mortality was five times higher for low vs. high-SEP adults (72.2 vs. 14.6 deaths per 100,000, RR = 4.94, 95% CI 4.82–5.05). The joint detriments of low SEP, Hispanic ethnicity, and male gender resulted in a COVID-19 death rate which was over 27 times higher (178.0 vs. 6.5 deaths/100,000, RR = 27.4, 95% CI 25.9–28.9) for low-SEP Hispanic men vs. high-SEP white women. In regression modeling, percent of the labor force in never remote jobs explained 72% of the variance in COVID-19 death rates. Conclusions and Relevance: SARS-CoV-2 infection control efforts should prioritize low-SEP adults (i.e., the working class), particularly the majority with “never remote” jobs characterized by inflexible and unsafe working conditions (i.e., blue collar, service, and retail sales workers).
Keywords: COVID-19, mortality, social class, race/ethnicity, gender
1. Background
COVID-19 is a viral infectious disease with a simple etiology (infection with the novel coronavirus SARS-CoV-2) and a complex clinical course which encompasses pathological derangement of multiple organ systems (e.g., respiratory [1], vascular [2], neurological [3], endocrine [4], and reproductive [5]), both an acute (days to weeks) and chronic (months to >1 year) clinical phase [6,7], and as yet unknown long-term clinical sequelae. Human-to-human transmission of SARS-CoV-2 occurs via exhalation of viral-laden aerosols by an infected person, suspension of these viral-laden aerosols in ambient air for extended periods of time, travel on expiratory plumes, and inhalation by susceptible persons at both near-field and far-field distances [8,9,10]. Put simply, the social environments which can lead to SARS-CoV-2 infection are those in which people are breathing other people’s breath [11,12].
For individuals, the accumulation of economic and social capital gives rise to a privileged socioeconomic position, which grants power relative to others in society [13]. This power manifests itself through control over economic resources (including labor and the means of production) and in a high social status that opens access to less tangible privileges via well-resourced social networks [14]. Numerous studies have verified the better health and lower mortality experienced by those with socioeconomic power and privilege [15,16,17,18,19,20]. Conversely, populations with low socioeconomic resources (i.e., the poor and working class) have historically experienced disproportionate exposure risks and burden of disease [21,22,23].
In the case of COVID-19, socioeconomic resources and privileges create the flexibility and space for the deployment of multiple strategies to reduce and prevent exposure to the highly infectious airborne novel coronavirus SARS-CoV-2. People in privileged socioeconomic positions live in larger homes with fewer people and in less densely populated neighborhoods (whether horizontally spacious in the suburbs or vertically spacious in metropolitan downtown areas), and rarely use public transportation. Additionally, the upper and professional classes have ready access to both high-quality outpatient health care and the best tertiary care hospital centers [24]. College education and related forms of social capital facilitate navigation of a complex health care system [25].
The vast majority of low-SEP adults are employed in blue collar, service, or retail sales jobs (i.e., working-class jobs) which require onsite attendance and prolonged close contact with others. In addition, working conditions vary by gender [26] and race/ethnicity as well as SEP [19,27]. The most physically hazardous occupations are highly segregated by gender and performed largely by men (e.g., meatpacking). At the same time, under racialized capitalism, whites enjoy advantages of occupational status even within narrowly defined job categories, compared with Hispanic, Black, and Indigenous workers with comparable educational credentials [27,28,29]. Moreover, elevated infection risks are amplified across multiple social environmental scales for working-class adults [30], who may reside in poorly ventilated housing [31], commute in a crowded carpool, and labor in a crowded, poorly ventilated worksite.
Our study is a national investigation of the joint effects of socioeconomic position (SEP), gender, and race/ethnicity on COVID-19 mortality in working-age adults, and it takes advantage of an ad hoc death certificate tabulation released by the U.S. National Center for Health Statistics (NCHS) in February 2021 [32,33]. These data permitted the calculation of age-adjusted COVID-19 mortality rates stratified simultaneously by socioeconomic position, race/ethnicity, and gender.
We hypothesized that there were (1) significant SEP disparities in COVID-19 mortality in working-age adults; (2) significant SEP disparities in every racial/ethnic group; and (3) within-SEP strata gender and racial/ethnic differences in opportunities for remote work that would be correlated with within- and between-SEP strata gender and racial/ethnic disparities in COVID-19 mortality.
2. Data and Methods
2.1. Population at Risk
Our target population included adults aged 25 to 64 years who were U.S. residents during 2020. We included six racial/ethnic groups: whites, Hispanics, Blacks, Asians, Indigenous, and multirace. The Indigenous group included American Indians, Alaska Natives, Native Hawaiians, and other Pacific Islanders, who were grouped together because of small numbers of deaths in some age-social class strata.
Reductionist narratives of race and cultural, moral, and biological inferiority [34,35] persist in public health and medicine when race is cited as an explanatory variable for negative health outcomes in the absence of social and historical contexts. In opposition to these biased approaches, we take an explicitly anti-essentialist stance [36] on the meaning of race and ethnicity [37] in the epidemiology of COVID-19. We recognize race not as a genetic or physiological risk factor, but rather as a social construct [38] that is embedded within a nexus of social oppression, exploitation, and conflict. This nexus amplifies exposure risks that result in higher burdens of morbidity and mortality among racial and ethnic minority populations.
2.2. Measurement of Socioeconomic Position
As observed nearly 40 years ago, the association between low socioeconomic resources and adverse health outcomes is robust regardless of the specific measures employed in individual studies [22]. Educational attainment is frequently used in the United States as a measure of socioeconomic position because it is more widely collected and recorded than occupation or annual income [39]. Furthermore, educational attainment is a more stable indicator of SEP over time, and is far less likely to be missing or unknown for women than occupation. The National Center for Health Statistics (NCHS) added educational attainment to the 1989 revision of the model death certificate specifically as “as a more reliable measure of socioeconomic status than occupation” [40]. Furthermore, Krieger et al. (1997) prefer the term “socioeconomic position” (as opposed to “socioeconomic status”) for measures which capture actual resources (e.g., a college degree) vs. relative prestige [39]. We used educational attainment data to define three ordinal strata of SEP, with consideration of credentialism as an important mechanism by which education conveys health benefits in society [39]. Low-SEP adults had no education beyond high school. The vast majority of adults aged 25–64 years in this group had graduated from high school. Intermediate-SEP adults had at least one year of college attendance, but did not have a 4-year college degree (bachelor’s degree). This stratum included those with associate’s degrees, and other technical/vocational certifications (e.g., licensed practical nurses). High-SEP adults had at minimum a bachelor’s degree. This stratum included everyone with advanced degrees. We chose not to further stratify “very low SEP” (i.e., those without a high school diploma) or “very high SEP” (i.e., those with Master’s and Doctoral degrees) because of the need to maintain sufficient cell size counts to support our plan to further divide each SEP stratum 36 times for the purpose of age adjustment.
2.3. COVID-19 Deaths
COVID-19-involved deaths included all deaths for which COVID-19 (ICD-10 code U07.1) was listed as the underlying or a contributing cause of death on the death certificate. We analyzed provisional death counts for 2020 stratified by four sociodemographic variables: (1) educational attainment (no college, some college, and college graduate); (2) race and ethnicity (white non-Hispanic, Hispanic, Black non-Hispanic, Asian non-Hispanic, American Indian/Alaska Native non-Hispanic, Native Hawaiian and other Pacific Islander non-Hispanic, more than one race non-Hispanic, and unknown); (3) gender (male, female, and unknown); and (4) age group (25–39 years, 40–54 years, and 55–64 years) [32,33].
2.4. Population Denominators
We used the 2020 Annual Social and Economic Supplement (ASEC) to the Current Population Survey (CPS) to calculate national population estimates stratified by educational attainment, race/ethnicity, gender, and age to exactly match the strata available in the COVID-19 death dataset [41]. Public-use CPS datasets include statistical weights to calculate national population estimates from the household-based sample [42]. We used special alternative weights that compensated for lower 2020 response rates in the CPS which were found to be differential by respondent income [42,43].
2.5. Death Rate Calculations
We first calculated age-specific death rates (deaths/population) for three age strata (25–39 years, 40–54 years, and 55–64 years) by SEP for the following groups: (a) all adults combined; (b) men and women; (c) six racial/ethnic groups, and (d) 12 groups defined by both gender and race/ethnicity. Next, we verified that SEP patterns of mortality were similar across age for all population groups. Then, we calculated age-adjusted mortality rates for ages 25–64 combined, using the direct method with the U.S. 2020 population as the standard.
2.6. Socioeconomic Position and Occupation Distributions
For the 36 sociodemographic groups aged 25 to 64 years (3 SEP strata × 2 gender strata × 6 race/ethnicity strata), we used the 2020 CPS ASEC [41] to identify the percent of adults with reported occupation in the following mutually exclusive categories: (1) blue collar, (2) service, (3) retail sales, (4) health professionals, and (5) white collar (excluding health professionals and retail sales). Further details and specific examples of common job titles in each of these categories can be found in Table S1.
We rated each job title in the CPS on its potential for remote work (i.e., work from home). All blue collar, service, and retail sales jobs were classified as “never remote” jobs. All other jobs were classified as “sometimes remote” (health professionals) or “feasibly remote” (all other white collar jobs).
2.7. Analytic Methods
We calculated SEP rate ratios (RRs) of the age-adjusted death rates for the entire study population, by gender, by race/ethnicity, and finally by gender and race/ethnicity simultaneously. High-SEP individuals (college graduates) were the referent group for all comparisons. Then, we calculated disparity RRs that compared COVID-19 mortality in 35 sociodemographic groups with a single low-risk referent group (high-SEP white women). Finally, we regressed the population-weighted log-transformed age-adjusted COVID-19 mortality rates against the percent of workers employed in never remote jobs for the 36 sociodemographic groups described above.
3. Results
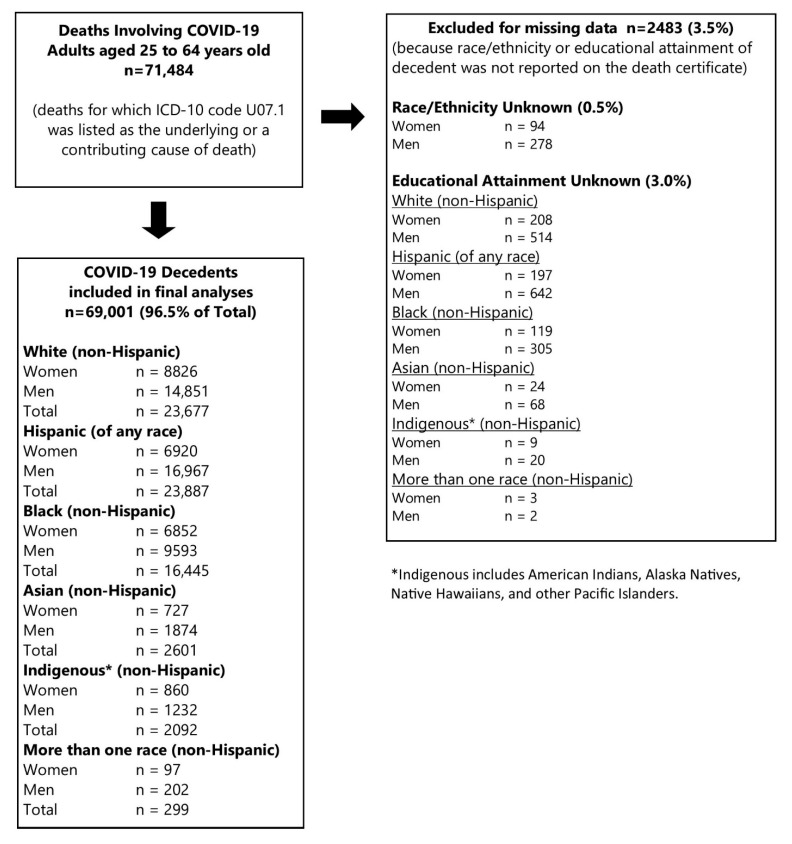
There were 71,484 COVID-19-involved deaths among adults aged 25 to 64 years old during calendar year 2020 (Figure 1), as reported to NCHS by the end of February 2021. There were very few missing data; 2483 deaths (3.5%) were excluded for missing race/ethnicity (0.5%) or educational attainment (3.0%). The final analytic dataset included 96.5% of the total deaths (n = 69,001) (Figure 1).
Figure 1.
Study Inclusion of Deaths Involving COVID-19 in Adults Aged 25–64 Years Old, United States, 1 January 2020 to 31 December 2020.
3.1. Socioeconomic Position Distribution of the Population at Risk
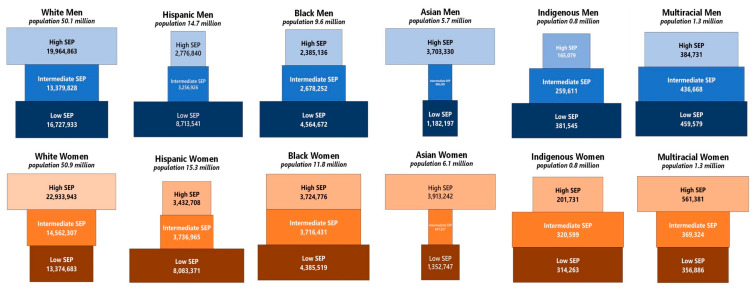
There were 168.4 million adults aged 25 to 64 years old in the U.S. in 2020. Figure 2 presents SEP population pyramids for each of the 12 gender-race/ethnicity groups. In each pyramid, high-SEP adults are represented in the top tier, intermediate-SEP adults in the middle tier, and low-SEP adults (i.e., the working class) in the bottom tier. White men and women comprised approximately 60.2% of the total population at risk for COVID-19 mortality in working-age adults, and high SEP comprised the largest class among whites. Hispanics were predominantly of low SEP. Low SEP also predominated among Black and Indigenous men.
Figure 2.
Socioeconomic Position (SEP) Population Pyramids * among Adults 25–64 Years Old (n = 168.4 million), United States 2020. Note: * The width of each bar is proportional to the size of the social class stratum within each race/ethnicity-gender group. Indigenous includes American Indians, Alaska Natives, Native Hawaiians, and other Pacific Islanders.
3.2. Socioeconomic Position and COVID-19 Mortality: Total Population
The age-adjusted COVID-19 mortality rate among high-SEP adults aged 25–64 years was 14.6 deaths per 100,000 (Table 1). The death rate was twice as high among intermediate-SEP adults (30.4 deaths/100,000; RR = 2.08, 95% CI 2.02–2.14) and five times as high among low-SEP working-class adults (72.2 deaths/100,000; RR = 4.94, 95% CI 4.82–5.05). The majority (68%, n = 46,966) of COVID-19 decedents were in a low SEP, and only 12% (n = 8421) had a high SEP.
Table 1.
Socioeconomic Position (SEP) Disparities in Reported COVID-19 Mortality Overall and by Gender and Race/Ethnicity among Adults 25–64 Years Old in the United States, 2020.
| Demographic Groups | Low SEP | Intermediate SEP | High SEP |
|---|---|---|---|
| Population at risk | 59.9 million | 44.4 million | 64.1 million |
| Total Study Population | |||
| COVID-19 deaths | 46,966 | 13,614 | 8421 |
| Age-adjusted mortality rate | 72.2/100,000 | 30.4/100,000 | 14.6/100,000 |
| SEP rate ratio (95% CI) | 4.94 (4.82–5.05) | 2.08 (2.02–2.14) | 1.0 (referent) |
| By Reported Gender | |||
| Women | |||
| COVID-19 deaths | 15,708 | 5535 | 3039 |
| Age-adjusted mortality rate | 50.4/100,000 | 22.8/100,000 | 10.0/100,000 |
| SEP rate ratio (95% CI) | 5.06 (4.87–5.26) | 2.29 (2.19–2.39) | 1.0 (referent) |
| Men | |||
| COVID-19 deaths | 31,258 | 8079 | 5382 |
| Age-adjusted mortality rate | 92.1/100,000 | 39.5/100,000 | 19.8/100,000 |
| SEP rate ratio (95% CI) | 4.65 (4.52–4.79) | 1.99 (1.93–2.06) | 1.0 (referent) |
| By Reported Race/Ethnicity | |||
| White, non-Hispanic | |||
| COVID-19 deaths | 14,587 | 5344 | 3746 |
| Age-adjusted mortality rate | 40.6/100,000 | 17.8/100,000 | 9.3/100,000 |
| SEP rate ratio (95% CI) | 4.37 (4.21–4.53) | 1.92 (1.84–2.00) | 1.0 (referent) |
| Hispanic | |||
| COVID-19 deaths | 19,174 | 3173 | 1540 |
| Age-adjusted mortality rate | 125.0/100,000 | 57.0/100,000 | 32.9/100,000 |
| SEP rate ratio (95% CI) | 3.80 (3.61–4.00) | 1.73 (1.63–1.84) | 1.0 (referent) |
| Black, non-Hispanic | |||
| COVID-19 deaths | 10,544 | 3912 | 1989 |
| Age-adjusted mortality rate | 105.9/100,000 | 59.0/100,000 | 33.8/100,000 |
| SEP rate ratio (95% CI) | 3.14 (2.99–3.29) | 1.75 (1.66–1.84) | 1.0 (referent) |
| Asian, non-Hispanic | |||
| COVID-19 deaths | 1149 | 497 | 955 |
| Age-adjusted mortality rate | 38.5/100,000 | 32.1/100,000 | 17.7/100,000 |
| SEP rate ratio (95% CI) | 2.18 (2.00–2.38) | 1.82 (1.63–2.03) | 1.0 (referent) |
| Indigenous, non-Hispanic | |||
| COVID-19 deaths | 1353 | 602 | 137 |
| Age-adjusted mortality rate | 182.1/100,000 | 113.4/100,000 | 37.2/100,000 |
| SEP rate ratio (95% CI) | 4.90 (4.11–5.84) | 3.05 (2.53–3.67) | 1.0 (referent) |
| Multirace/Other, non-Hispanic | |||
| COVID-19 deaths | 159 | 86 | 54 |
| Age-adjusted mortality rate | 20.0/100,000 | 12.9/100,000 | 8.7/100,000 |
| SEP rate ratio (95% CI) | 2.32 (1.70–3.15) | 1.49 (1.06–2.10) | 1.0 (referent) |
3.3. Socioeconomic Position and COVID-19 Mortality by Gender
Women experienced lower COVID-19 death rates than men (high-SEP women: 10.0 deaths/100,000 vs. 19.8 deaths/100,000 in high-SEP men), but a slightly higher disparity for low vs. high SEP (RR = 5.06, 95% CI 4.87–5.26 in women vs. RR = 4.65, 95% CI 4.52–4.79 in men). Numerically, both the age-adjusted death rate (92.1/100,000) and the number of deaths (n = 31,258) were highest for low-SEP men (Table 1).
3.4. Socioeconomic Position and COVID-19 Mortality by Race and Hispanic Ethnicity
In all six racial/ethnic groups, there was a monotonic association between SEP and COVID-19 mortality, with the lowest age-adjusted death rates in high-SEP adults, and the highest rates in low-SEP adults (Table 1). SEP disparity RRs ranged from 2.18 (95% CI 2.00–2.38) among Asians to RR = 4.90 (95% CI 4.11–5.84) among Indigenous adults. Within each stratum of SEP, death rates were highest for Indigenous, Hispanic, and Black adults, and lowest for multiracial, Asian, and white adults.
3.5. Disparities in COVID-19 Mortality: Independent and Joint Effects of Socioeconomic Position, Gender, and Race/Ethnicity
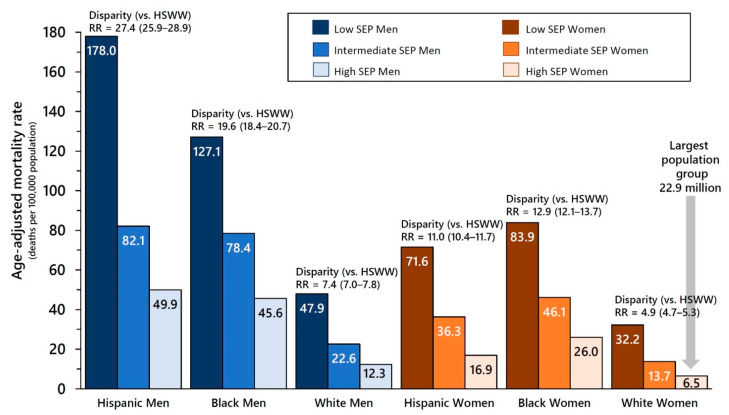
The independent effects of SEP, gender, and race/ethnicity on COVID-19 mortality are evident in Figure 3 for Hispanics, Blacks, and whites, who together comprised 90.5% of the total population at risk. Across all six groups defined by gender and race/ethnicity, there was a strong and statistically significant association of SEP with age-adjusted COVID-19 mortality (see Table S2 for all RRs and 95% CI). Similarly, across all nine groups defined by SEP and race/ethnicity, age-adjusted death rates were always higher for men than for women. However, there was effect modification by gender when stratifying by SEP. Within each of the three SEP strata, the highest death rates were suffered by Hispanics among men, and by Blacks among women.
Figure 3.
COVID-19 Death Rates by Socioeconomic Position (SEP), Gender, and Race/Ethnicity with High-SEP White Women (HSWW) as the Referent Group for Disparity Rate Ratios ** among Adults 25–64 Years Old, United States 1 January 2020 to 31 December 2020. Note: ** The disparity rate ratios (RR) are calculated separately for each sociodemographic group and compare age-adjusted COVID-19 death rates to the referent group (high-SEP white women (HSWW)). Results are presented for the three largest population groups (whites, Hispanics, and Blacks). All rate ratios and full results for Asians, Indigenous adults (American Indians, Alaska Natives, Native Hawaiians, and other Pacific Islanders) and multiracial adults are shown in Table S2.
Finally, disparity RRs which capture the joint effects of SEP, gender, and race/ethnicity on COVID-19 mortality in working-age adults confirm that high-SEP white women were at lowest risk for COVID-19 mortality (6.5 deaths/100,000). The joint detriments of low (i.e., working class) SEP, Hispanic ethnicity, and male gender resulted in a COVID-19 age-adjusted death rate which was over 27 times higher (178.0 deaths/100,000, RR = 27.4, 95% CI 25.9–28.9) compared with high-SEP white women (Figure 3). While in all SEP strata Hispanic and Black women experienced lower death rates than Hispanic and Black men, respectively, they still suffered higher death rates than white men. Full results for all 36 sociodemographic groups are available in Table S2.
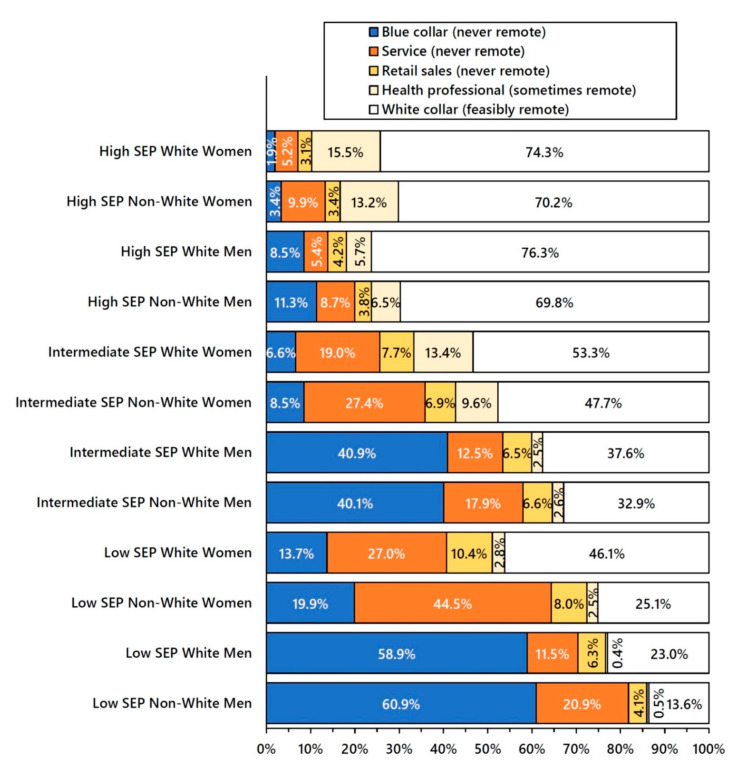
3.6. Working-Class Jobs and Never Remote Work by Socioeconomic Position, Gender, and Race/Ethnicity
As predicted, the majority of high-SEP adults had white collar jobs, and those of intermediate SEP were employed in a mixture of blue collar, service, retail sales, and white collar jobs, with no category in the majority (Figure 4). Conversely, the majority of low-SEP adults were employed in working-class jobs (blue collar, service, and retail sales) with no potential for remote work. However, majority employment in working-class jobs varied from 51.1% of low-SEP white women to 85.9% of low-SEP non-white men. In all SEP strata, non-whites were more likely to be employed in service jobs than whites, and men were much more likely to be employed in blue collar jobs than women.
Figure 4.
Remote Work Occupations * by Socioeconomic Position (SEP), Gender, and Race/Ethnicity # among Adults 25–64 Years Old, United States 2020. Note: * The denominators for occupation percentages include only persons who were in the labor force with a reported occupation in the Current Population Survey (CPS), the representative sample from which national population estimates were derived. Service occupations include health care support, protective service, food service, housekeeping, building and grounds, and personal care service workers. Registered nurses and licensed practical nurses are classified as health professionals. Transportation workers, including airline pilots and flight attendants, are classified as blue collar. White collar feasibly remote is comprised of managers, professionals, technical workers, non-retail sales workers, and office support and administrative workers. # Non-white includes Hispanic, Black, Asian, Indigenous, and multiracial adults.
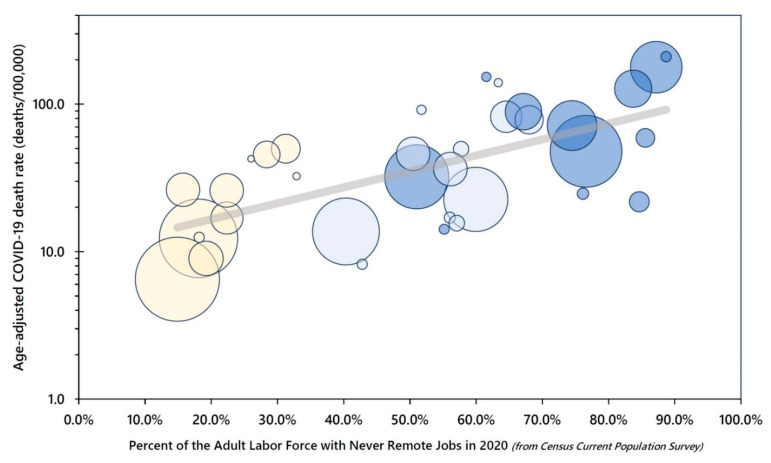
A population-weighted regression of the natural log-transformed age-adjusted 2020 COVID-19 death rates revealed a good fit of an exponential model in which the percent of adults employed in never remote jobs during 2020 explained 72% of the variance in the age-adjusted death rates across the 36 population groups defined by socioeconomic position, gender, and race/ethnicity (Figure 5).
Figure 5.
COVID-19 Mortality by Never Remote (Blue Collar/Service/Retail) Jobs among Adults 25 to 64 Years Old, United States 2020. Note: Each bubble represents a socioeconomic position (SEP)-gender-racial/ethnic group, with bubble size proportional to population size. Dark blue = low SEP, light blue = intermediate SEP, and yellow = high SEP.
4. Discussion
People with high socioeconomic positions retain a far greater degree of discretionary control over their professions, work lives, and daily schedules than workers of low SEP. For many, a college degree and professional status permits a measure of autonomy and flexibility in meeting job requirements [44]. In contrast, the working class (in blue collar, service, and retail sales occupations) are subjected to authoritarian control [45] and inflexible requirements of work [17,27,44,46]. Moreover, the worksites in which the working class perform their wage labor are often replete with physical, chemical, and biological hazards which directly and negatively impact workers’ health and well-being [44,47,48,49]. The results of our census data analyses confirm that educational attainment is highly correlated with occupational segregation, with the majority of low-SEP adults in working-class jobs (i.e., blue collar, service, and retail sales) across all gender-race/ethnicity groups.
In the United States, individual socioeconomic position results from an intrinsically racialized set of economic and social status relationships [50,51,52]. The legacies of colonialism, slavery, and other forms of structural racism shape local labor markets, housing opportunities, and other material aspects of workers’ lives [19,53]. Consequently, compared with whites, a given level of educational attainment usually provides fewer economic benefits to Blacks and other minorities [19,53].
Our results support the hypothesis that hazardous conditions of work were a primary driver of joint socioeconomic, gender, and racial/ethnic disparities in COVID-19 mortality. During the first year of the COVID-19 pandemic in the United States, low-SEP adults aged 25–64 years old were five times as likely as high-SEP adults to die from COVID-19, and intermediate-SEP adults were twice as likely as high-SEP adults to die. High-SEP whites aged 25 to 64 years were largely shielded from COVID-19 mortality during the first year of the pandemic. They comprised more than one-quarter of the study population, but accounted for only 5% of the COVID-19 deaths. High-SEP white women, the numerically largest population group (n = 22.9 million), accounted for only 2% of COVID-19 decedents in working-age adults. In contrast, Hispanic and Black low-SEP (i.e., working-class) men comprised only 8% of the 25–64 years old population, but they were 29% of the premature COVID-19 decedents. Non-white low-SEP men were most likely to be employed in never remote occupations (i.e., blue collar, service, and retail sales) compared with every other sociodemographic group.
Our results are consistent with those of a smaller study of excess mortality by occupation in California during the period March–October 2020 [54], and with a small study of worksite COVID-19 transmission in Asian countries which found the most commonly affected occupations were health care, drivers, sales, cleaners, and public safety [55]. A major report on social inequalities in COVID-19 in the United Kingdom found social class patterns of COVID-19 mortality that were very similar to what we observed for the U.S. [31]. However, the magnitude of the socioeconomic mortality disparities was much lower in the U.K.
4.1. COVID-19 Case Fatality
Axiomatically, mortality rates (deaths/population) are a function of two underlying phenomena: the incidence of disease in a specified population (cases/population) and the case fatality rate (deaths/cases) of the disease. We hypothesize that disparities in both case fatality and incidence have contributed to the strong and highly significant mortality disparities observed in our study. Access to high-quality evidence-based medical care is not universal in the U.S. [56]. Barriers to accessing timely and appropriate COVID-19 medical care include lack of health insurance, inadequate health insurance (e.g., high deductible/co-pay plans), lack of or inadequate paid sick leave [57], geographic location, transportation access/costs/timeliness, lack of respite dependent care, threat of job loss, immigration status, racism and discrimination, and distrust of health care and government institutions [58]. An analysis of place of death of U.S. COVID-19 decedents found that 22% of 30–49 year olds and 14% of 50–64 year olds died either outside a hospital or in the emergency department (OH/ED) [59]. Minimizing COVID-19 case fatality requires that individuals have access to timely diagnosis and high-quality hospital medical care before they become critically ill.
4.2. Study Limitations and Public Health Data Gaps
It is likely that COVID-19 deaths in the U.S. have been undercounted (i.e., cause of death has been misclassified), and this misclassification is likely to be differential by socioeconomic position, resulting in a bias toward the null in our estimates of socioeconomic disparities. Misclassification occurs when there is insufficient medical information available at the time of death. Lack of access to medical care and out-of-hospital mortality can result in the use of non-specific cause of death coding on death certificates. We have previously shown that the percent of all non-injury deaths coded to “symptoms, signs, and ill-defined conditions” increased from 2019 to 2020 among working-age adults [59].
A simple step toward improving COVID-19 surveillance data, which could be implemented immediately across a wide range of data systems, is to add one yes/no question to all individual adult patient encounter medical records: “Has this person completed one or more years of college?” A “no” response on this single data item would identify low-SEP adults (i.e., the working class). A follow-up question for those who replied “yes” (“Does this person have a 4-year college degree?”) would easily differentiate intermediate- vs. high-SEP adults.
5. Conclusions
The most urgent implication of our study points to immediate actions needed to protect low-SEP adults, particularly blue collar, service, and retail sales workers, from infection with the SARS-CoV-2 virus. Expert recommendations include strengthening federal and state labor laws [60], empowering OSHA [49], adopting the Total Worker Health Framework [61], and direct actions for unions to organize for greater protections for worker safety [48].
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph19095479/s1, Table S1: Top Five Occupations of Adults 25–64 years old in 2020, by Socioeconomic Position, Gender, and Race/Ethnicity. Table S2: Disparities in COVID-19-Related Mortality by Socioeconomic Position, Race/Ethnicity, and Gender Among Adults 25–64 Year Old in the United States, 1 January 2020 to 31 December 2020.
Author Contributions
E.B.P. conceived of this study and performed preliminary analyses. E.B.P., J.M.M., R.B.G. and J.L.S. contributed to final analyses, figures, and tables. E.B.P. and J.M.M. wrote the first draft. All authors edited and revised the final manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
This study was exempt from IRB review because it utilized only publicly available anonymized secondary datasets.
Informed Consent Statement
Not applicable.
Data Availability Statement
The publicly available datasets analyzed in this study are referenced in the Methods section of this paper.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Johnson K.D., Harris C., Cain J.K., Hummer C., Goyal H., Perisetti A. Pulmonary and Extra-Pulmonary Clinical Manifestations of COVID-19. Front. Med. 2020;7:526. doi: 10.3389/fmed.2020.00526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Greenberg A., Pemmasani G., Yandrapalli S., Frishman W.H. Cardiovascular and Cerebrovascular Complications with COVID-19. Cardiol. Rev. 2021;29:143–149. doi: 10.1097/CRD.0000000000000385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zheng K.I., Feng G., Liu W.Y., Targher G., Byrne C.D., Zheng M.H. Extrapulmonary complications of COVID-19: A multisystem disease? J. Med. Virol. 2021;93:323–335. doi: 10.1002/jmv.26294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.White-Dzuro G., Gibson L.E., Zazzeron L., White-Dzuro C., Sullivan Z., Diiorio D.A., Low S.A., Chang M.G., Bittner E.A. Multisystem effects of COVID-19: A concise review for practitioners. Postgrad. Med. 2021;133:20–27. doi: 10.1080/00325481.2020.1823094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nassau D.E., Best J.C., Kresch E., Gonzalez D.C., Khodamoradi K., Ramasamy R. Impact of the SARS-CoV-2 virus on male reproductive health. BJU Int. 2021;129:145–150. doi: 10.1111/bju.15573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sudre C.H., Murray B., Varsavsky T., Graham M.S., Penfold R.S., Bowyer R.C., Pujol J.C., Klaser K., Antonelli M., Canas L.S., et al. Attributes and predictors of long COVID. Nat. Med. 2021;27:626–631. doi: 10.1038/s41591-021-01292-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Michelen M., Manoharan L., Elkheir N., Cheng V., Dagens A., Hastie C., O’Hara M., Suett J., Dahmash D., Bugaeva P., et al. Characterising long COVID: A living systematic review. BMJ Glob. Health. 2021;6:e005427. doi: 10.1136/bmjgh-2021-005427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang C.C., Prather K.A., Sznitman J., Jimenez J.L., Lakdawala S.S., Tufekci Z., Marr L.C. Airborne transmission of respiratory viruses. Science. 2021;373:6558. doi: 10.1126/science.abd9149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greenhalgh T., Jimenez J.L., Prather K.A., Tufekci Z., Fisman D., Schooley R. Ten scientific reasons in support of airborne transmission of SARS-CoV-2. Lancet. 2021;397:1603–1605. doi: 10.1016/S0140-6736(21)00869-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tang J.W., Marr L.C., Milton D.K. Aerosols should not be defined by distance travelled. J. Hosp. Infect. 2021;115:131–132. doi: 10.1016/j.jhin.2021.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coleman K.K., Tay D.J.W., Sen Tan K., Ong S.W.X., Son T.T., Koh M.H., Chin Y.Q., Nasir H., Mak T.M., Chu J.J.H., et al. Viral Load of SARS-CoV-2 in Respiratory Aerosols Emitted by COVID-19 Patients while Breathing, Talking, and Singing. Clin. Infect. Dis. 2021:ciab691. doi: 10.1093/cid/ciab691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morawska L., Allen J., Bahnfleth W., Bluyssen P.M., Boerstra A., Buonanno G., Cao J., Dancer S.J., Floto A., Franchimon F., et al. A paradigm shift to combat indoor respiratory infection. Science. 2021;372:689–691. doi: 10.1126/science.abg2025. [DOI] [PubMed] [Google Scholar]
- 13.Wright E.O. Class Counts: Comparative Studies in Class Analysis. Cambridge University Press; New York, NY, USA: 1997. [Google Scholar]
- 14.Oliver M.N., Muntaner C. Researching Health Inequities Among African Americans: The Imperative to Understand Social Class. Int. J. Health Serv. 2005;35:485–498. doi: 10.2190/PPQX-47DY-KW0X-78Y8. [DOI] [PubMed] [Google Scholar]
- 15.Krieger N., Rowley D.L., Herman A.A., Avery B., Phillips M.T. Racism, sexism, and social class: Implications for studies of health, disease, and well-being. Am. J. Prev. Med. 1993;9((Suppl. 6)):82–122. doi: 10.1016/S0749-3797(18)30666-4. [DOI] [PubMed] [Google Scholar]
- 16.Kokkinen L., Muntaner C., Koskinen A., Väänänen A. Occupational class, capitalist class advantage and mortality among working-age men. J. Epidemiol. Community Health. 2020;74:3–6. doi: 10.1136/jech-2019-212952. [DOI] [PubMed] [Google Scholar]
- 17.Muntaner C., Solar O., Vanroelen C., Martínez J.M., Vergara M., Santana V., Castedo A., Kim I.-H., Benach J. Unemployment, informal work, precarious employment, child labor, slavery, and health inequalities: Pathways and mechanisms. Int. J. Health Serv. 2010;40:281–295. doi: 10.2190/HS.40.2.h. [DOI] [PubMed] [Google Scholar]
- 18.Graham H. Unequal Lives: Health and Socioeconomic Inequalities. Open University Press; Berkshire, UK: 2007. [Google Scholar]
- 19.Krieger N. Workers are people too: Societal aspects of occupational health disparities—An ecosocial perspective. Am. J. Ind. Med. 2010;53:104–115. doi: 10.1002/ajim.20759. [DOI] [PubMed] [Google Scholar]
- 20.Krieger N., Fee E. Measuring Social Inequalities in Health in the United States: A Historical Review, 1900–1950. In: Krieger N., editor. Embodying Inequality: Epidemiologic Perspectives. Baywood Publishing Company, Inc.; Amityville, NY, USA: 2005. pp. 5–78. [Google Scholar]
- 21.Pickett K.E., Wilkinson R.G. Income inequality and health: A causal review. Soc. Sci. Med. 2015;128:316–326. doi: 10.1016/j.socscimed.2014.12.031. [DOI] [PubMed] [Google Scholar]
- 22.Syme S., Berkman L. Social class, susceptibility and sickness. Am. J. Epidemiol. 1976;104:1–8. doi: 10.1093/oxfordjournals.aje.a112268. [DOI] [PubMed] [Google Scholar]
- 23.Winkleby M.A., Fortmann S.P., Barrett D.C. Social class disparities in risk factors for disease: Eight-year prevalence patterns by level of education. Prev. Med. 1990;19:1–12. doi: 10.1016/0091-7435(90)90001-Z. [DOI] [PubMed] [Google Scholar]
- 24.Whiteis D.G. Third world medicine in first world cities: Capital accumulation, uneven development and public health. Soc. Sci. Med. 1998;47:795–808. doi: 10.1016/S0277-9536(98)00137-3. [DOI] [PubMed] [Google Scholar]
- 25.Singh-Manoux A., Marmot M. Role of socialization in explaining social inequalities in health. Soc. Sci. Med. 2005;60:2129–2133. doi: 10.1016/j.socscimed.2004.08.070. [DOI] [PubMed] [Google Scholar]
- 26.Williams D.R. The health of men: Structured inequalities and opportunities. Am. J. Public Health. 2003;93:724–731. doi: 10.2105/AJPH.93.5.724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Landsbergis P.A., Grzywacz J.G., LaMontagne A.D. Work organization, job insecurity, and occupational health disparities. Am. J. Ind. Med. 2014;57:495–515. doi: 10.1002/ajim.22126. [DOI] [PubMed] [Google Scholar]
- 28.Quinn M.M., Sembajwe G., Stoddard A.M., Kriebel D., Krieger N., Sorensen G., Hartman C., Naishadham D., ScD E.M.B. Social disparities in the burden of occupational exposures: Results of a cross-sectional study. Am. J. Ind. Med. 2007;50:861–875. doi: 10.1002/ajim.20529. [DOI] [PubMed] [Google Scholar]
- 29.Williams D.R. Race, socioeconomic status, and health: The added effects of racism and discrimination. Ann. N. Y. Acad. Sci. 1999;896:173–188. doi: 10.1111/j.1749-6632.1999.tb08114.x. [DOI] [PubMed] [Google Scholar]
- 30.Whitacre R., Oni-Orisan A., Gaber N., Martinez C., Buchbinder L., Herd D., Holmes S.M. COVID-19 and the political geography of racialisation: Ethnographic cases in San Francisco, Los Angeles and Detroit. Glob. Public Health. 2021;16:1396–1410. doi: 10.1080/17441692.2021.1908395. [DOI] [PubMed] [Google Scholar]
- 31.Marmot M., Allen J., Goldblatt P., Herd E., Morrison J. The Pandemic, Socioeconomic and Health Inequalities in England. University College London Institute of Health Equity; London, UK: 2020. Build Back Fairer: The COVID-19 Marmot Review. Available online: https://www.instituteofhealthequity.org/resources-reports/build-back-fairer-the-covid-19-marmot-review. [Google Scholar]
- 32.National Center for Health Statistics . Ad Hoc Deaths by Educational Attainment, 2019–2020 [Dataset] National Center for Health Statistics; Hyattsville, MD, USA: 2021. Available online: https://data.cdc.gov/NCHS/AH-Deaths-by-Educational-Attainment-2019-2020/4ueh-89p9. [Google Scholar]
- 33.National Center for Health Statistics . Technical Notes: Provisional Death Counts for Coronavirus Disease (COVID-19) National Center for Health Statistics; Hyattsville MD, USA: 2020. Available online: https://www.cdc.gov/nchs/nvss/vsrr/covid19/tech_notes.htm. [Google Scholar]
- 34.LaVeist T.A. On the study of race, racism, and health: A shift from description to explanation. Int. J. Health Serv. 2000;30:217–219. doi: 10.2190/LKDF-UJQ5-W1KU-GLR1. [DOI] [PubMed] [Google Scholar]
- 35.Burden-Stelly C., Modern U.S. Racial Capitalism: Some Theoretical Insights. Mon. Rev. 2020;72:201–203. [Google Scholar]
- 36.Chowkwanyun M., Reed A.L. Racial Health Disparities and Covid-19—Caution and Context. N. Engl. J. Med. 2020;383:201–203. doi: 10.1056/NEJMp2012910. [DOI] [PubMed] [Google Scholar]
- 37.Smedley A., Smedley B.D. Race as biology is fiction, racism as a social problem is real: Anthropological and historical perspectives on the social construction of race. Am. Psychol. 2005;60:16–26. doi: 10.1037/0003-066X.60.1.16. [DOI] [PubMed] [Google Scholar]
- 38.Williams D.R., Lavizzo-Mourey R., Warren R.C. The concept of race and health status in America. Public Health Rep. 1994;109:26–41. [PMC free article] [PubMed] [Google Scholar]
- 39.Krieger N., Williams D.R., Moss N.E. Measuring Social Class in US Public Health Research: Concepts, Methodologies, and Guidelines. Annu. Rev. Public Health. 1997;18:341–378. doi: 10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
- 40.Tolson G., Barnes J., Gay G., Kowaleski K.L. The 1989 Revision of the U.S. Standard Certificates and Reports. Volume 28. National Center for Health Statistics; Hyattsville MD, USA: 1991. pp. 1–34. Available online: https://www.cdc.gov/nchs/data/series/sr_04/sr04_028.pdf. [PubMed] [Google Scholar]
- 41.Sarah F., Miriam K., Renae R., Steven Ruggles J., Robert W., Westberry M. Integrated Public Use Microdata Series, Current Population Survey: Version 9.0 [Dataset] IPUMS; Minneapolis, MN, USA: 2021. [DOI] [Google Scholar]
- 42.Bureau of the Census 2020 Annual Social and Economic (ASEC) Supplement Technical Documentation. 2021 Available online: https://www2.census.gov/programs-surveys/cps/techdocs/cpsmar20.pdf.
- 43.Rothbaum J., Bee A. Coronavirus Infects Surveys, Too: Survey Nonresponse Bias and the Coronavirus Pandemic. United States Census Bureau; Washington, DC, USA: 2021. Available online: https://www.census.gov/library/working-papers/2020/demo/SEHSD-WP2020-10.html. [Google Scholar]
- 44.Kaikkonen R., Rahkonen O., Lallukka T., Lahelma E. Physical and psychosocial working conditions as explanations for occupational class inequalities in self-rated health. Eur. J. Public Health. 2009;19:458–463. doi: 10.1093/eurpub/ckp095. [DOI] [PubMed] [Google Scholar]
- 45.Krieger N., Waterman P.D., Hartman C., Bates L.M., Stoddard A.M., Quinn M.M., Sorensen G., Barbeau E.M. Social hazards on the job: Workplace abuse, sexual harassment, and racial discrimination--a study of Black, Latino, and White low-income women and men workers in the United States. Int. J. Health Serv. 2006;36:51–85. doi: 10.2190/3EMB-YKRH-EDJ2-0H19. [DOI] [PubMed] [Google Scholar]
- 46.Muntaner C. Digital Platforms, Gig Economy, Precarious Employment, and the Invisible Hand of Social Class. Int. J. Health Serv. 2018;48:597–600. doi: 10.1177/0020731418801413. [DOI] [PubMed] [Google Scholar]
- 47.Fielding-Miller R.K., Sundaram M.E., Brouwer K. Social determinants of COVID-19 mortality at the county level. PLoS ONE. 2020;15:e0240151. doi: 10.1371/journal.pone.0240151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.AFL-CIO . Death on the Job: The Toll of Neglect: A National and State-by-State Profile of Worker Safety and Health in the United States. AFL-CIO; Washington, DC, USA: 2021. Available online: https://aflcio.org/reports/death-job-toll-neglect-2020. [Google Scholar]
- 49.Michaels D., Wagner G.R. Halting Workplace COVID-19 Transmission: An Urgent Proposal to Protect American Workers. The Century Foundation; New York, NY, USA: 2020. Available online: https://tcf.org/content/report/halting-workplace-covid-19-transmission-urgent-proposal-protect-american-workers/ [Google Scholar]
- 50.Marable M. How Capitalism Underdeveloped Black America. South End Press; Boston, MA, USA: 1983. [Google Scholar]
- 51.Laster Pirtle W.N. Racial Capitalism: A Fundamental Cause of Novel Coronavirus (COVID-19) Pandemic Inequities in the United States. Health Educ. Behav. 2020;47:504–508. doi: 10.1177/1090198120922942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.McClure E.S., Vasudevan P., Bailey Z., Patel S., Robinson W.R. Racial Capitalism Within Public Health-How Occupational Settings Drive COVID-19 Disparities. Am. J. Epidemiol. 2020;189:1244–1253. doi: 10.1093/aje/kwaa126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Williams D.R., Mohammed S.A., Leavell J., Collins C. Race, socioeconomic status, and health: Complexities, ongoing challenges, and research opportunities. Ann. N. Y. Acad. Sci. 2010;1186:69–101. doi: 10.1111/j.1749-6632.2009.05339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chen Y.-H., Glymour M., Riley A., Balmes A., Duchowny K., Harrison R., Matthay E., Bibbins-Domingo K. Excess mortality associated with the COVID-19 pandemic among Californians 18–65 years of age, by occupational sector and occupation: March through October 2020. PLoS ONE. 2021;16:e0252454. doi: 10.1371/journal.pone.0252454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lan F.Y., Wei C.F., Hsu Y.T., Christiani D.C., Kales S.N. Work-related COVID-19 transmission in six Asian countries/areas: A follow-up study. PLoS ONE. 2020;15:e0233588. doi: 10.1371/journal.pone.0233588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fiscella K., Sanders M.R. Racial and Ethnic Disparities in the Quality of Health Care. Annu. Rev. Public Health. 2016;37:375–394. doi: 10.1146/annurev-publhealth-032315-021439. [DOI] [PubMed] [Google Scholar]
- 57.Mays V.M., Cochran S.D., Sprague A., Heymann J. Social Justice Is Not the COVID-19 Vaccine Alone: It Is Addressing Structural Racism Through Social Policies That Shape Health. Am. J. Public Health. 2021;111:S75–S79. doi: 10.2105/AJPH.2021.306442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gehlbach D., Vázquez E., Ortiz G., Li E., Sánchez C.B., Rodríguez S., Pozar M., Cheney A.M. COVID-19 Testing and Vaccine Hesitancy in Latinx Farm-Working Communities in The Eastern Coachella Valley. Res. Sq. 2021:1–17. doi: 10.21203/rs.3.rs-587686/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pathak E.B., Garcia R.B., Menard J.M., Salemi J.L. Out-of-Hospital COVID-19 Deaths: Consequences for Quality of Medical Care and Accuracy of Cause of Death Coding. Am. J. Public Health. 2021;111:S101–S106. doi: 10.2105/AJPH.2021.306428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.McNicholas C., Rhinehart L., Poydock M., Shierholz H., Perez D. Why Unions are Good for Workers—Especially in a Crisis Like COVID-19. Economic Policy Institute; Washington, DC, USA: 2020. Available online: https://files.epi.org/pdf/204014.pdf. [Google Scholar]
- 61.Dennerlein J.T., Burke L., Sabbath E.L., Williams J.A.R., Peters S., Wallace L., Karapanos M., Sorensen G. An Integrative Total Worker Health Framework for Keeping Workers Safe and Healthy during the COVID-19 Pandemic. Hum. Factors. 2020;62:689–696. doi: 10.1177/0018720820932699. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The publicly available datasets analyzed in this study are referenced in the Methods section of this paper.