Abstract
Background
During professional identity formation, medical students integrate their newly developing professional identities with their longstanding personal identities. Longitudinal mentorship has been shown to aid students in this process. Lack of clear relationship expectations among students and faculty is a barrier to effective longitudinal mentorship relationships.
Methods
A cross-sectional, survey-based study collected information about experiences from both students (mentees) and faculty (mentors). Surveys focused on collecting participants’ attitudes and expectations regarding ideal and actual mentorship experiences. Descriptive statistics and Fisher's exact test analyses were used to compare the responses within and between students and faculty.
Results
A total of 234 faculty and 181 medical students completed the survey. There were 187 faculty respondents (79.9%) who had previously mentored students. Faculty who had versus had not previously mentored students differed significantly in their responses on the importance of mentors discussing aspects of their personal lives (71.1% vs. 54.3%, respectively, p = 0.0491), a quality valued by the majority of student respondents. As students progressed through medical school, they expressed increasing needs for personal mentorship and conversations regarding work/life integration and wellness (M1: 12.2%, M2: 18.8%, M3: 29.3%, M4: 51.7%). A minority of students (27% of M3 and 14.8% of M4 students) reported meeting faculty mentors through their clinical year experiences.
Conclusions
Faculty mentoring experience may improve student-faculty value alignment, which may in turn help to address student-identified needs pertaining to personal development and professional identity formation in medical school. By contrasting student-identified mentorship expectations with those of faculty at various stages of mentorship experience, this study lays the groundwork for the formation of more effective longitudinal mentorship programs.
Keywords: MeSH terms: mentoring, education, medical, program development, program evaluation, burnout, professional identity formation
Introduction
In 2010, the Carnegie Foundation for the Advancement of Teaching, which in 1910 published the Flexner Report, published a second call for reform in the North American medical education system. This publication was released in response to “forces of change” that were challenging medical education, acknowledging that our contemporary contexts require updated recommendations since the time of Flexner. 1 The authors of that report identified professional identity formation (PIF) as one of four emerging challenges for medical students and an urgent focus of reform efforts. In particular, they noted that over the past several decades, the clinical productivity demands on faculty have steadily increased, compressing or even eliminating time for teaching. 2 Recognizing that formation of professional identity is mainly social and relational in nature, many have argued for institutions to be proactive in establishing programs that support longitudinal mentorship between faculty and medical students.2–4 Notably, invested student-faculty relationships have been shown to be particularly beneficial to medical students’ PIF by modeling how students may integrate their growing professional roles with their longstanding personal identities.5,6
Amidst the rigor of clinical and academic medicine, invested longitudinal mentoring relationships are difficult to sustain. Multiple systematic reviews, meta-analyses, and studies have established the bidirectional personal and professional wellness benefits of these relationships to both faculty and students.7–13 In addition to improving PIF, longitudinal mentoring's benefits to students include improved confidence in specialty selection, increased overall career guidance and satisfaction, greater academic productivity, and improved networking in their fields of interest.8,9 For faculty, reported benefits of serving as a mentor include improved job satisfaction, organizational commitments, job performance, decreased turnover intent, and increased overall career success.7,11 Facilitating invested longitudinal mentorship relationships between students and faculty presents an important opportunity for wellness and career development initiatives that would benefit both students and faculty.
In order to improve longitudinal mentorship relationships, two important points of intervention have been identified: mentorship programmatic structure and faculty development.9,10,14 Regardless of the approach, one theme emerges that characterizes successful longitudinal mentorship: a focus on communicating clear mentorship expectations between faculty and students.15,16 A systematic review investigating the role of expectations in mentoring found that the most successful mentors, as identified by students, prioritized outlining clear mentor-mentee expectations early in the course of the relationship. 16 Unclear expectations contribute to poorer duration and quality of mentoring relationships, as judged by mentees. 17
Regardless of how an institution pursues aligning mentor-mentee expectations, understanding a baseline of student-faculty expectation alignment and how medical students’ mentorship needs change as they progress through medical school is critical to ensure that student needs are addressed dynamically and appropriately. The purpose of this study is to better understand how medical students’ mentorship needs may change throughout the course of their undergraduate medical education and assess faculty alignment with student expectations in order to inform the creation of longitudinal mentoring programming and identify opportunities for faculty development.
Methods
Survey context and design
This study was performed at Harvard Medical School (HMS), a major United States medical school which uses an academic advisor framework to facilitate mentoring. Through this system, advisors meet with students to discuss professional and personal development throughout medical school through semi-annual one-on-one meetings. Further career mentorship is administered through personal referral from students’ advisors or through other opportunities that students seek out individually, such as connecting with research mentors or clinical shadowing. In addition to the aforementioned advisor system, a lecture series with invited guest faculty and resident speakers representing different specialties each month provides students with exposure to specialty mentors.
Within this context, we conducted a cross-sectional survey-based study to examine and compare the mentor-mentee relationship expectations and needs of students and faculty. Survey items were designed in consultation with students and faculty advisors in the Office of Student Affairs, each with experience in survey design; face validation of the survey instrument was ensured by faculty advisors in the Office of Student Affairs with expertise in academic mentorship and survey design, in addition to a group of students with demonstrated interest in medical education and advising. 18 Survey questions elicited student and faculty respondents’ demographics, experiences, beliefs, and preferences about current and ideal mentoring relationships. Demographic data for students included their year in medical school, program, dual degree program enrollment (e.g., MD/PhD program), whether they had at least one mentor at the medical school, and number of mentors. Demographic data for faculty included the number of years that they had been on faculty at HMS and the number of students that they had ever previously mentored. Specific questions about mentorship were designed to assess factors that were hypothesized to influence perceptions and expectations regarding how mentoring relationships and needs form and change over time. Survey items were composed of multiple-choice questions and checklist questions which allowed respondents to indicate several areas of importance to mentoring relationships. Individual survey items examined student and faculty preferences regarding the importance of timely communication, honest communication, availability for mentoring, consistent meeting cadence, frequency of meetings, openness to sharing aspects of their personal lives, openness to sharing examples of professional experiences, openness to sharing about career pathways and decisions, supportiveness of mentees’ goals, networking, non-evaluative mentoring, and ability to hold mentees accountable to their goals. In addition, students and faculty indicated how they had met and established their mentoring relationships, frequency of mentoring meetings, topics discussed during meetings, topics for which students desired greater mentorship, and whether students felt adequately supported by their mentors.
Survey implementation
Parallel surveys using the Qualtrics platform were administered to students and faculty at HMS in the fall of 2018. Surveys were distributed to MD candidates in all class years (N = 713) and to select faculty (N = 1393) with expressed interest and/or experience in mentoring, including faculty advisors in the Office of Student Affairs, the Office of Recruitment and Multicultural Affairs, and members of the HMS Academy, which supports the professional development of medical educators. In order to optimize survey response rates, multiple survey reminders and clear confidentiality statements were provided. Participation in the survey was voluntary and all responses were anonymous. Participants retained the right to withdraw at any time by exiting the survey. No incentives were provided for study participation. Data were collected and stored securely within a Qualtrics database. The HMS Academy and Office of Human Research Administration reviewed this study as a quality improvement initiative and deemed that it met criteria for institutional review board exemption.
Statistical analysis
Descriptive statistics reported frequencies of mentoring strengths and opportunities described by students and faculty. Responses of all students and faculty members, students across academic years, and faculty both who had and had not mentored students, were compared using the Fisher's exact test to assess for non-random associations between responses. All analyses were conducted with statistical significance set as α = 0.05.
Results
Participant characteristics and evaluation of current mentorship experiences
A total of 234 faculty surveys were initiated and completed (100%), while 183 student surveys were initiated with 181 completed responses (98.9%). Among student responses, there was representation from all class years (M1: 41 [24.8%], M2: 35 [19.3%], M3: 43 [23.8%], M4+ : 58 [32.1%]). In this study, M4+ refers to medical students in their fourth year and beyond (e.g., those pursuing additional degrees or research during their undergraduate medical trajectory) (Table 1).
Table 1.
Characteristics of student (N = 181) and faculty (N = 234) survey respondents.
| Respondents characteristics | N | % |
|---|---|---|
| Faculty | 234 | − |
| Previous mentoring experience | 187 | 79.9 |
| No previous mentoring experience | 35 | 15.0 |
| Non-response for this item | 12 | 5.1 |
| Medical Students | 181 | − |
| Class year | ||
| M1 | 45 | 25.0 |
| M2 | 35 | 19.4 |
| M3 | 43 | 23.9 |
| M4+ | 58 | 32.2 |
| Curriculum* | ||
| Pathways | 134 | 74.4 |
| New Pathways | 23 | 12.8 |
| Health Sciences and Technology | 23 | 12.8 |
*At the time of student surveying, there were three overlapping curricula with students in the first through third years of medical school in either the Pathways or Health Science and Technology (HST) curricula. Students in the fourth year of medical school were in either the New Pathways or HST curricula.
Abbreviations: M4+ refers to medical students in their fourth year and beyond (e.g., those who had pursued additional degrees or research during their undergraduate medical training).
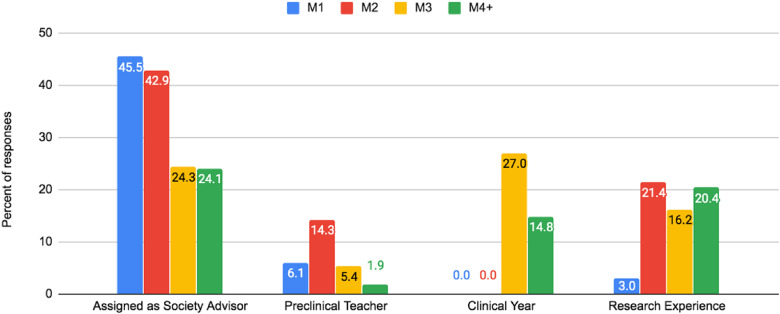
There were 187 faculty respondents (79.9%) who had previously mentored students, while the remaining 47 (20.1%) had never previously mentored students. A majority of students (81.2%) reported that they had had at least one mentor in medical school. Nearly half of first-year medical students (45.4%) and second-year medical students (42.9%) identified their assigned academic advisor as their primary mentor, in contrast to 24.3% of third-year medical students and 24.1% of fourth-year or higher medical students (Figure 1). Only 10 third-year (27.0%) and 8 fourth-year or higher (14.8%) medical students reported meeting any faculty mentors through their clinical year experiences.
Figure 1.
How medical students meet their faculty mentors during undergraduate medical training. Students respondents chose from multiple-choice options to indicate how they met their mentors. The responses of students were stratified based on their class year in medical school. First and second-year medical students tended to meet their faculty mentors based on assignment as an advisor. Less than one-third of third- and fourth-year students indicated meeting their faculty mentor through clinical experiences. Abbreviations: M4 + refers to medical students in their fourth year and beyond (e.g., those pursuing additional degrees or research during their undergraduate medical training).
Mentorship needs expressed by students
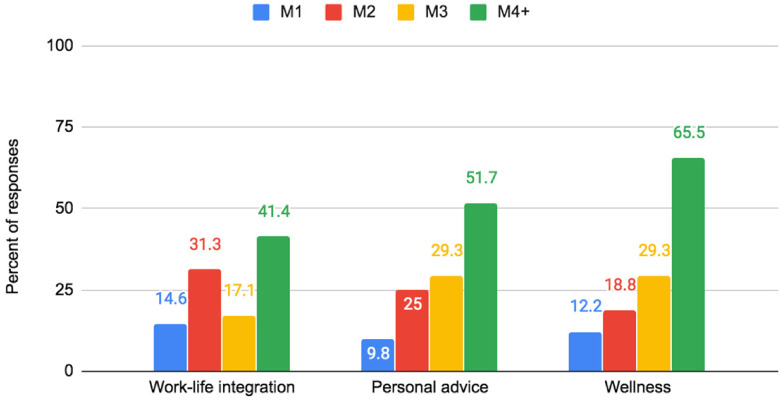
Students discussed career advising with mentors more frequently as they progressed through medical school (M1: 58.5%, M2: 70.0%, M3: 76.7%, M4+ : 87.3%). Research and networking were other common topics discussed in mentoring conversations. However, as students progressed through medical school, they expressed an increasing need for personal mentorship, conversations regarding work/life integration, and discussions about wellness that they felt were not being met in their current mentorship relationships (M1: 12.2%, M2: 18.8%, M3: 29.3%, M4+: 51.7%) (Figure 2). Overall, 14.4% of students reported that they did not feel adequately supported by their mentors in medical school.
Figure 2.
Topics not discussed in mentorship relationships that students wished were discussed. Student respondents chose from multiple-choice options to indicate topics that are not discussed in mentorship relationships that they wish were discussed. The responses of students were stratified based on their class year in medical school. The most common topics that students wished were discussed were wellness, personal advice, and work-life integration. Abbreviations: M4+ refers to medical students in their fourth year and beyond.
Qualities of a good mentor as identified by students and faculty
When asked about mentoring on professional topics, students and faculty did not differ significantly in their responses to the importance of mentors sharing examples of professional experience (84.5% students vs. 83.2% faculty, p = 0.2521), sharing about career pathways and decisions (88.4% students vs. 85.8% faculty, p = 0.1001), or offering networking opportunities (69.6% students vs. 68.5% faculty, p = 0.4629). However, students and faculty differed in their responses when commenting on the value of a mentor's openness to sharing aspects of their personal life. In stratified analysis, 71.1% of faculty who had previously mentored students versus 54.3% of those without previous mentoring experience agreed that mentors’ openness to discussing aspects of their personal life was a quality of a good mentor (p = 0.0491) (Table 2). Agreement with the value of openness to discussing personal lives among faculty who had previously mentored students was similar to the student agreement rate of 70.2% for this survey item.
Table 2.
Comparison of faculty descriptions of the qualities of good mentors based on faculty experience with mentoring medical students.
| Item | Faculty with previous mentoring experience (n = 187*) | Faculty without previous mentoring experience (n = 35*) | P Value |
|---|---|---|---|
| Timely communication | 131 (70.1) | 23 (65.7) | 0.5554 |
| Availability for meeting | 158 (84.5) | 31 (88.6) | 0.7939 |
| Openness to sharing aspects of their personal life | 133 (71.1) | 19 (54.3) | 0.0491 |
| Openness to sharing examples of professional experience | 163 (87.2) | 30 (85.7) | 0.7822 |
| Openness to sharing about career pathways/decision | 168 (89.8) | 31 (88.6) | 0.7591 |
| Supportive of individual goals | 168 (89.8) | 31 (88.6) | 0.7591 |
| Offering networking opportunities | 135 (72.2) | 24 (68.6) | 0.6827 |
| Non-evaluative and confidential | 141 (75.4) | 23 (65.7) | 0.213 |
| Ability to hold mentee accountable | 56 (29.9) | 16 (45.7) | 0.0791 |
* 12 Faculty respondents did not indicate whether or not they had previous mentoring experience and were excluded from analysis. Faculty were permitted to select several characteristics as important qualities of good mentors.
Discussion
In the process of PIF, medical students’ integrate their longstanding personal identities with their newly forming professional identities. Longitudinal mentorship has been shown to be particularly beneficial to students throughout this process.2–5 Given the pace of medical training and the significant responsibilities of clinical practice, many factors may contribute to the breakdown of a mentorship relationship; principal among these factors are unclear mentor and mentee expectations. 17 Several institutions have published their experiences implementing programs that support long-term mentorship for medical students.5,19–21 Although many of these programs have achieved great success at their home institutions, the number and variety of mentorship models in existence illustrate the medical education community's continued exploration of effective programmatic structures for longitudinal mentorship in undergraduate medical education.5,22–24 Program objectives of published models range from continuous monitoring of students’ academic performance to fostering interest in specific specialties; mentorship roles in these programs vary across a spectrum from one-on-one academic mentoring to personal mentorship to role modeling behaviors for entire groups of medical students.22,25 Better understanding of student and faculty mentorship relationship expectations and how these expectations may change throughout student's undergraduate medical education may help inform the creation of longitudinal mentorship programs and identify areas for faculty development.
In our study, a majority of students sampled (81.2%) reported that they had at least one mentor in medical school. Importantly, in spite of there being a formal academic advisory system in place, through which every student is assigned and meets regularly with their advisor, nearly 20% of students did not feel that they had a mentor in medical school. It is known that relationships organized through formal programs are qualitatively different from spontaneous mentoring in areas of task orientation, trust, mutual commitment, breadth, depth, duration, and structure. 14 Given that each student at our institution has an assigned advisor, the fact that 1 in 5 students reported that they did not have a mentor demonstrates student understanding of the distinction between an advisor and a mentor, and identifies an unmet need.
Typically, mentorship relationships develop voluntarily on the part of the student in contrast to relationships with academic advisors, which occur through assignment. Prior studies have posited that students voluntarily develop mentorship relationships most frequently with attendings or preceptors whom they meet in their clinical years.14,26 Of the students we surveyed, however, only 27.0% of third-year students and 14.8% of students in their fourth year or beyond reported having met a mentor during their primary clinical year (Figure 1). Thus, the majority of students in our sample did not develop mentorship relationships during their clinical experiences, and these experiences therefore cannot be considered reliable drivers of voluntary mentorship relationships. Additionally, to reap the full benefits of longitudinal mentorship, opportunities should be made available to students in all class years, with intentional inclusion of first-year students for whom most curricula provide only modest clinical exposure.
Prior studies have established that honoring mentee experiences and goals as well as clarifying mentor role expectations contribute to the quality and durability of mentorship relationships.27–30 In order to identify unmet needs, we asked students about topics that are not discussed in mentorship relationships that they wish were addressed. Student respondents identified three under-addressed fields: work-life integration, personal advice, and wellness. These responses indicate that these are currently unmet student needs in the domain of PIF. This need appears to be increasingly more pronounced as students progress through medical school, demonstrating a need to tailor mentoring programming to the developmental needs of students at different phases of training (Figure 2).
To facilitate the formation of longitudinal mentorship relationships, we investigated the alignment of mentor-mentee relationship expectations. We found that previous faculty mentorship experience was positively associated with sharing student values regarding the importance of personal disclosure as a quality of a good mentoring relationship. Given that students in our study reported increasing interest in discussing personal development topics as they progressed through medical school, this association suggests that mentor-mentee alignment could be enhanced by providing year-specific mentoring education to novice faculty mentors, especially those who plan to mentor more senior students.
Our findings should be interpreted in light of several limitations. Although the overall sample size was appropriate (N = 234 for faculty; N = 181 for students) for a non-population based study, the results are from a single urban academic institution that may not be representative of all student and faculty experiences in medical schools with different class sizes in different geographic regions, which may limit the generalizability of the study. We also were unable to compare responders to non-responders on a few key indicators, including whether students who did not complete the survey felt adequately supported with existing mentorship resources at our institution.
Strengths of this study include representation of medical students among all class years in order to understand how mentorship needs and preferences differ among class years in medical school. There was also inclusion of faculty who had previously mentored students and those who had not in order to appreciate differences that may be associated with mentorship experience. Finally, survey questions investigated many different dimensions of mentorship including research, networking, goal setting, and personal advice, which highlight the salience of students’ identifying personal mentorship as a particularly important area of unmet need.
In addition to the known benefits of mentorship for both mentors and mentees,7,8,14,16,31 our study demonstrates encouraging evidence that mentorship experience may improve student-faculty value alignment, which may in turn help to address student-identified needs pertaining to personal development in medical school. This finding provides an actionable starting point for faculty development efforts to improve the quality of medical student mentorship. By clarifying student and faculty mentorship expectations, this study lays the groundwork for quality improvement in longitudinal mentoring programming.
Conclusion
While in the past, longitudinal mentorship may have occurred informally, a meaningful proportion of students in our study reported either having no mentor in medical school or feeling inadequately supported by their mentors. In particular, students identified unmet needs in discussing work/life integration, wellness, and other personal matters; these needs were reported more frequently as students progressed through medical school. Among faculty, we found that those who had previously mentored at least one student were significantly more likely to report personal disclosure as an important quality of good mentors. Our study demonstrates that mentorship experience may improve student-faculty value alignment. This alignment was focused specifically in the dimension of personal mentorship, the main area of unmet mentorship need identified by students. This study lays the groundwork for faculty development efforts or longitudinal mentorship programming structures that prioritize student-faculty mentorship expectations alignment in service of appropriately addressing unmet medical student mentorship needs throughout the course of students’ undergraduate medical education.
Footnotes
Ethical Approval: This study was reviewed by the Academy at Harvard Medical School and Harvard Office of Human Research Administration. It was determined to meet the criteria for institutional review board exemption (IRB no. 18-1525).
- Jonathan J. Kusner is a first-year resident physician in the Department of Medicine, Duke University Hospital, Durham, NC.
- Jie Jane Chen is a second-year resident physician in the Department of Radiation Oncology, University of California, San Francisco, San Francisco, CA.
- Fidencio Saldaña is Dean for Students at Harvard Medical School and a clinical cardiologist in the Department of Medicine at the Brigham and Women's Hospital, Boston, MA.
- Jennifer E. Potter is Advisory Dean and Director of the William Bosworth Castle Society at Harvard Medical School and Director of the Women's Health Center at Beth Israel Deaconess Medical Center, Boston, MA.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received financial support from the Harvard Medical School Dean's Innovation Award in Diversity and Inclusion for the open-access publication of this article.
Informed Consent: Not applicable, because this article does not contain any studies with human or animal subjects.
Trial Registration: Not applicable, because this article does not contain any clinical trials.
ORCID iDs: Jonathan J. Kusner https://orcid.org/0000-0003-1466-4345
Jie Jane Chen https://orcid.org/0000-0002-5380-4825
References
- 1.Cooke M, Irby DM, Brien BCO. Educating Physicians A Call for Reform of Medical School and Residency. 1st ed. San Francisco, CA: Jossey-Bass; 2010. [Google Scholar]
- 2.Irby DM, Cooke M, Brien BCO. Calls for reform of medical education by the teaching : 1910 and 2010. Acad Med. 2010;85(2):220-227. doi: 10.1097/ACM.0b013e3181c88449 [DOI] [PubMed] [Google Scholar]
- 3.Goldie J. The formation of professional identity in medical students: considerations for educators. Med Teach. 2012;34(9):e641-e648. 10.3109/0142159X.2012.687476 [DOI] [PubMed] [Google Scholar]
- 4.Wald HS, Anthony D, Hutchinson TA, Liben S, Smilovitch M, Donato AA. Professional identity formation in medical education for humanistic, resilient physicians: pedagogic strategies for bridging theory to practice. Acad Med. 2015;90(6):753-760. doi: 10.1097/ACM.0000000000000725 [DOI] [PubMed] [Google Scholar]
- 5.Kalén S, Ponzer S, Seeberger A, Kiessling A, Silén C. Longitudinal mentorship to support the development of medical students’ future professional role: a qualitative study. BMC Med Educ. 2015;15(1):1-10. doi: 10.1186/s12909-015-0383-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen J, Kusner J, Saldaña F, Potter J. Development of a novel mentorship platform to foster relational mentoring, empowered vulnerability, and professional identity formation in undergraduate medical education. Acad Med. 2021;96(11):1580-1585. 10.1097/ACM.000 [DOI] [PubMed] [Google Scholar]
- 7.Ghosh R, Reio TG. Career benefits associated with mentoring for mentors: a meta-analysis. J Vocat Behav. 2013;83(1):106-116. doi: 10.1016/j.jvb.2013.03.011 [DOI] [Google Scholar]
- 8.Sambunjak D, Sharon ES, Marusic A. Mentoring in academic medicine. A Systematic Review. JAMA - J Am Med Assoc. 2006;296(9):1103-1115. doi: 10.1111/j.1741-6787.2007.00099.x [DOI] [PubMed] [Google Scholar]
- 9.Henry-Noel N, Bishop M, Gwede CK, Petkova E, Szumacher E. Mentorship in medicine and other health professions. J Cancer Educ. 2019;34(4):629 − 6637. doi: 10.1007/s13187-018-1360-6 [DOI] [PubMed] [Google Scholar]
- 10.Der Lin C, Lin BYJ, Lin CC, Lee CC. Redesigning a clinical mentoring program for improved outcomes in the clinical training of clerks. Med Educ Online. 2015;20(1):1-7. doi: 10.3402/meo.v20.28327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choi AMK, Moon JE, Steinecke A, Prescott JE. Developing a culture of mentorship to strengthen academic medical centers. Acad Med. 2019;94(5):630-633. doi: 10.1097/ACM.0000000000002498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haidet P, Stein HF. The role of the student-teacher relationship in the formation of physicians: the hidden curriculum as process. J Gen Intern Med. 2006;21(SUPPL. 1):16-20. doi: 10.1111/j.1525-1497.2006.00304.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mann MP. Faculty mentors for medical students: a critical review. Med Teach. 1992;14(4):311-319. doi: 10.3109/01421599209018849 [DOI] [PubMed] [Google Scholar]
- 14.Rose GL, Rukstalis MR, Schuckit MA. Informal mentoring between faculty and medical students. Acad Med. 2005;80(4):344-348. doi: 10.1097/00001888-200504000-00007 [DOI] [PubMed] [Google Scholar]
- 15.Straus SE, Johnson MO, Marquez C, Feldman MD. Characteristics of successful and failed mentoring relationships: a qualitative study across two academic health centers. Acad Med. 2013;88(1):82-89. doi: 10.1097/ACM.0b013e31827647a0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huskins WC, Silet K, Weber-Main AM, et al. Identifying and aligning expectations in a mentoring relationship. Clin Transl Sci. 2011;4(6):439-447. doi: 10.1111/j.1752-8062.2011.00356.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Spencer R, Drew AL, Walsh J, Kanchewa SS. Girls (and boys) just want to have fun: a mixed-methods examination of the role of gender in youth mentoring relationship duration and quality. J Prim Prev. 2018;39(1):17-35. doi: 10.1007/s10935-017-0494-3 [DOI] [PubMed] [Google Scholar]
- 18.Scott KW, Callahan DG, Chen JJet al. Fostering student-faculty partnerships for continuous curricular improvement in undergraduate medical educa. [DOI] [PubMed]
- 19.Indyk D, Deen D, Fornari A, Santos MT, Lu WH, Rucker L. The influence of longitudinal mentoring on medical student selection of primary care residencies. BMC Med Educ. 2011;11(27):1–7. 10.1186/1472-6920-11-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sheu L, Hauer KE, Schreiner K, Van Schaik SM, Chang A, O’Brien BC. “A friendly place to grow as an educator”: a qualitative study of community and relationships among medical student coaches. Acad Med. 2020;95(2):293-300. doi: 10.1097/ACM.0000000000002900 [DOI] [PubMed] [Google Scholar]
- 21.Aagaard EM, Hauer KE. A cross-sectional descriptive study of mentoring relationships formed by medical students. J Gen Intern Med. 2003;18(4):298-302. doi: 10.1046/j.1525-1497.2003.20334.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Frei E, Stamm M, Buddeberg-Fischer B. Mentoring programs for medical students - A review of the PubMed literature 2000-2008. BMC Med Educ. 2010;10(32):1–14. 10.1186/1472-6920-10-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Melnyk BM. Mentoring in academic medicine. A systematic review. Worldviews Evidence-Based Nurs. 2007;4(3):170-171. doi: 10.1111/j.1741-6787.2007.00099.x [DOI] [Google Scholar]
- 24.Buddeberg-Fischer B, Herta KD. Formal mentoring programmes for medical students and doctors - A review of the medline literature. Med Teach. 2006;28(3):248-257. doi: 10.1080/01421590500313043 [DOI] [PubMed] [Google Scholar]
- 25.Nimmons D, Giny S, Rosenthal J. Medical student mentoring programs: current insights. Adv Med Educ Pract. 2019;10(1):113−123. doi: 10.2147/amep.s154974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tekian A, Jalovecky MJ, Hruska L. The impact of mentoring and advising at-risk underrepresented minority students on medical school performance. Acad Med. 2001;76(12):1264. doi: 10.1097/00001888-200112000-00024 [DOI] [PubMed] [Google Scholar]
- 27.van Eps MA, Cooke M, Creedy DK, Walker R. Student evaluations of a year-long mentorship program: a quality improvement initiative. Nurse Educ Today. 2006;26(6):519-524. doi: 10.1016/j.nedt.2006.01.009 [DOI] [PubMed] [Google Scholar]
- 28.Elcigil A, Sari HY. Students’ opinions about and expectations of effective nursing clinical mentors. J Nurs Educ. 2008;47(3):118-123. doi: 10.3928/01484834-20080301-07 [DOI] [PubMed] [Google Scholar]
- 29.Pinho SDC, Coetzee M, Schreuder D. Formal mentoring: mentee and mentor expectations and perceived challenges. SA J Hum Resour Manag. 2005;4(1):20-26. doi: 10.4102/sajhrm.v3i3.72 [DOI] [Google Scholar]
- 30.Sambunjak D, Straus SE, Marusic A. A systematic review of qualitative research on the meaning and characteristics of mentoring in academic medicine. J Gen Intern Med. 2010;25(1):72-78. doi: 10.1007/s11606-009-1165-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thorndyke L, Gusic M, Milner R. Functional mentoring: a practical approach with multilevel outcomes. J Contin Educ Health Prof. 2008;28(3):157-164. doi: 10.1002/chp.178 [DOI] [PubMed] [Google Scholar]