Abstract
Introduction
Myocardial ischemia/reperfusion (I/R) injury is a leading cause of cardiac dysfunction. Circular RNAs (circRNAs) are involved in the pathogenesis of myocardial I/R injury. However, the functions and underlying mechanisms are unclear. The present study determined the role of circ-RHOJ.1 in regulating myocardial cell proliferation and apoptosis after I/R injury.
Material and methods
Myocardial cells isolated from Sprague-Dawley rats were identified with an immunofluorescence assay using cardiac troponin T antibody. Expression of circ-RHOJ.1, miR-124-3p and neuregulin-1 (NRG1) mRNA was assessed with real-time quantitative polymerase chain reaction. NRG1 protein expression was evaluated with western blot and immunofluorescence assays. Dual-luciferase reporter assay was performed to confirm interaction between miR-124-3p and circ-RHOJ.1, and miR-124-3p and NRG1. Effects of circ-RHOJ.1 overexpression or miR-124-3p inhibition on cell proliferation and apoptosis were evaluated using cell counting kit (CCK)-8 assay and flow cytometry. Cytokines levels were analyzed with an enzyme-linked immunosorbent assay.
Results
Myocardial cells were successfully isolated and had down-regulated expression of circ-RHOJ.1 and NRG1, and up-regulated expression of miR-124-3p after I/R injury. circ-RHOJ.1 acted as a sponge for miR-124-3p, and NRG1 served as a target gene of miR-124-3p. circ-RHOJ.1 overexpression or miR-124-3p inhibition increased interleukin (IL)-10 levels and reduced IL-2, IL-6, and tumor necrosis factor-α levels in myocardial cells after I/R injury. Functional assay results illustrated that circ-RHOJ.1 overexpression or miR-124-3p inhibition enhanced proliferation and inhibited apoptosis of myocardial cells after I/R injury.
Conclusions
Circ-RHOJ.1 served as a molecular marker of myocardial I/R injury via regulation of miR-124-3p and NRG1 expression.
Keywords: circ-RHOJ, 1, miR-124-3p, neuregulin 1, myocardial ischemia/reperfusion injury, proliferation, apoptosis
Introduction
Myocardial ischemia/reperfusion (I/R) injury results in tissue injury within a short time period, and restoration of blood flow results in more serious myocardial ischemic injury [1, 2]. Myocardial I/R injury commonly occurs during cardiac surgery, coronary artery bypass graft surgery and viscera recanalization after blood supply infarction. It prevents the myocardium from being repaired via reperfusion and has become a major clinical problem [3]. Myocardial I/R injury is often accompanied with a systemic inflammatory reaction and tissue injury through the generation of oxygen-free radicals, calcium overload, myocardial energy metabolic disorders, apoptosis, activation of neutrophils and release of inflammatory factors [4]. Therefore, the process of myocardial I/R injury is associated with deteriorating inflammation reaction. The rescue approaches for myocardial I/R injury have been extensively studied [5] and further investigations are desirable to discover new strategies and targets to reduce myocardial I/R injury.
Non-coding RNAs (ncRNAs) mainly include microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs) [6, 7]. Emerging evidence has shown that ncRNAs are important regulators in a variety of diseases [8]. In recent years, circRNAs have attracted great attention. CircRNAs are formed via the head-to-tail splicing of several exons of the target gene and usually manifest as covalently closed loop structures without 5¢ caps and 3¢ tails because of the process specificity [9]. At present, several circRNAs have been shown to be differentially expressed in various diseases such as cancers, cardiovascular diseases, and neurologic diseases [10]. Recently, the dysregulated expression of circRNAs has also been identified in myocardial I/R injury [11].
MiRNAs, a class of short RNA molecules with 20–22 nucleotides, may modulate the expression of target genes by binding to the 3¢-untranslated regions (3¢-UTRs) [12]. Abnormal expression of miRNAs has been reported in several diseases such as neurodegenerative disorders, cancers and inflammation-related disorders [13]. MiR-124-3p was demonstrated to play an important role in I/R injury [14]. However, the molecular functions and mechanisms of miR-124-3p in myocardial I/R injury are incompletely understood. CircRNAs could serve as miRNA sponges and regulate the expression level of miRNAs [15]. Using the CircNet prediction tool, we found that miR-124-3p can potentially interact with circ-RHOJ.1 in the cardiovascular system. RHOJ belongs to the small G protein superfamily and is mainly expressed in vascular endothelial cells [16]. Several studies have shown that RHOJ played an important role in pathophysiological processes of certain cardiovascular diseases [17]. Recent studies further demonstrated that RHOJ promoted hypoxia-induced endothelial-to-mesenchymal transition [18]. Hence, we hypothesized that circ-RHOJ.1 may regulate the expression of miR-124-3p by acting as a sponge in myocardial I/R injury.
In the present study, we explored the role of circ-RHOJ.1 in regulating myocardial cell proliferation and apoptosis after I/R injury. The regulatory signaling pathways of circ-RHOJ.1 were further examined by in vitro mechanistic studies. The present study may provide novel insights into the role of circRNAs in regulating I/R injury.
Material and methods
Animals
A total of 15 healthy Sprague-Dawley (SD) rats (3 days old, weighing 5–8 g, 7 male and 8 female) were provided by the Guangdong Medical Laboratory Animal Center (License number, SCXK (Military) 2013-0002; Certification, 44007200053222). Rats were allowed to habituate for 7 days to reduce the stress according to the national standard before the experiment (food and water ad libitum, humidity of 50–60%, temperature of 20–25°C, light period from 7:00 AM to 7:00 PM). All the animal protocols in the present study were approved by Southern Medical University.
Isolation of rat myocardial cells
Animals were anesthetized with 5% isoflurane and were killed by cervical dislocation. Hearts were excised from neonatal rats under aseptic conditions and the ventricular muscles were sheared. The fragments were digested into single cells using 0.06% trypsin (HyClone). The cells were filtered using 180 mesh sieves. After centrifugation (800 ×g for 5 min), the cells were maintained in Dulbecco’s modified Eagle’s medium (Cat. No. SH30022.01B; DMEM; HyClone,) supplemented with 10% fetal bovine serum (Cat. No. SH30087.01; FBS; HyClone), 1% penicillin/streptomycin (Cat. No. SH30010; HyClone), and 0.1 mmol/mL of BrdU (Sigma) in 95% air and 5% CO2 at 37°C.
Establishment of I/R myocardial cell model
The establishment of the I/R myocardial cell model was based on previous studies [19]. After 2–3 days of myocardial cell culture in normoxic DMEM with 10% FBS, the cells were transferred to a hypoxic incubator in a humidified atmosphere that contained 95% N2 – 5% CO2 for 3 h of hypoxia, and then subsequently reoxygenated for 24 h before further experimentation. For the sham group, incubated in normoxic conditions (95% air – 5% CO2), the total experimental time course for the other groups was followed.
Oligonucleotide transfection
MiR-124-3p mimic and inhibitor as well as negative control (NC) miRNAs were obtained from Gene Pharma (Shanghai, China). The myocardial cells were transfected with miR-124-3p mimic, inhibitor, or respective NC miRNAs using Lipofectamine RNAiMAX (Cat. No. 13778075; Invitrogen) according to the manufacturer’s protocol.
Vector construction and transduction
Full lengths of NRG1 and circ-RHOJ.1 cDNA were produced by polymerase chain reaction (PCR) assay using PrimerSTAR Max DNA Polymerase Mix (Takara, Japan). The primers used were as follows: NRG1-KpnI-F: 5¢-cggggtaccgccaccATGGAGATTTATTCCCCAGACATGTC-3¢, NRG1-XhoI-R: 5¢-ccgctcgagTTATACAGCAATAGGGTCTTGGTTAGCG-3¢; circ-RHOJ.1-EcoRI-F: 5¢-ccggaattcGAGGACTACAACCAGCTGAGGCCAC-3¢, circ-RHOJ.1-NotI-R: 5¢-ataagaatgcggccgcCGCTTTTGCGAGCTTCACACCATG-3¢. The PCR products were sub-cloned into pcDNA3.1+ vector (Invitrogen) to establish recombinant plasmids (pcDNA-NRG1 and pcDNA-circ-RHOJ.1). Myocardial cells were transfected with pcDNA-NRG1 or pcDNA-circ-RHOJ.1 using Lipofectamine RNAiMAX reagent (Cat. No. 13778075; Invitrogen) as per the manufacturer’s instructions.
Immunofluorescence (IF) assay
The treated myocardial cells were fixed with 4% paraformaldehyde (Cat. No. P6148; Sigma, IL) for 15 min and incubated with 0.5% Triton X-100 (Cat. No. 122H0766; Sigma) for 20 min at room temperature. After blocking with 10% normal goat serum (Thermo fisher Scientific) at 37°C for 30 min, the slides were incubated with primary antibodies, including anti-cardiac troponin T antibody (Cat. No. ab8295, 1 : 200, Abcam) and anti-NGR1 antibody (Cat. No. bs-1463R, 1 : 200; Bioss) at 4°C overnight. The slides were treated with fluorescently conjugated secondary antibodies for 1 h at room temperature. Nuclei were stained with 4¢-6-diamidino-2-phenylindole (DAPI; Life Technologies). The results were obtained using a fluorescence microscope (Leica, DMI6000B, magnification at 100× and 400×).
Cell counting kit-8 (CCK-8) assay
The treated myocardial cells were seeded into 96-well plates at a density of 1 × 103 cells/ml and incubated with 10 ml of CCK-8 regent (Cat. No. C0037; Beyotime, China) at 37°C for 3 h. Cell viability was assessed using a microplate reader at 450 nm wavelength (Thermo Fisher Scientific, Multiscan). The inhibition ratio (%) was calculated as follows: (1 – OD values of experimental group/OD values of control group) × 100%.
Cell apoptosis analysis
Cell apoptosis was detected with Annexin V-fluorescein isothiocyanate (FITC) and propidium iodide (PI) apoptosis detection kit (keygen, KGA106). The treated myocardial cells were harvested and washed twice with pre-cold phosphate-buffered saline (PBS). Cells were fixed with 70% ethanol for 4 h and incubated with annexin V-FITC and (PI) for 15 min at room temperature. The results were analyzed with flow cytometry (BD Biosciences, Franklin Lakes, NJ) at an excitation of 575 nm. Annexin V(+)/PI(−) and Annexin V(+)/PI(+) represented the cells in early and late apoptosis or necrosis, respectively.
Enzyme-linked immunosorbent assay (ELISA)
For the determination of interleukin (IL)-10, IL-2, IL-6, and tumor necrosis factor (TNF)-α concentrations, the treated myocardial cells were subjected to ELISA analysis using respective ELISA kits as per the instructions of manufacturers. The ELISA kits for detecting IL-10, IL-2, IL-2 and TNF-α were purchased from NeoBioscience (Shenzhen, China).
RNA extraction and real-time quantitative PCR (qRT-PCR) assay
Total RNA was extracted using TRIzol reagent (Cat. No. 9109; Takara, Japan) from the treated myocardial cells. cDNA was synthesized with the Reverse Transcription kit (Takara, Japan). The amplification of circ-RHOJ.1, NRG1, and miR-124-3p was performed using SYBR GREEN PCR Master Mix (Applied Biosystems). The relative expression levels were analyzed using the 2–ΔΔCt method. The sequences of primers used are shown in Table I.
Table I.
Sequences of primers in this study
| Gene | Primer sequences |
|---|---|
| GAPDH | Forward: 5’-TATGATGATATCAAGAGGGTAGT-3’ Reverse: 5’-TGTATCCAAACTCATTGTCATAC-3’ |
| NRG1 | Forward: 5’-CCTGCAAACTGCTCCTAAAC-3’ Reverse: 5’-GAGTTCCTCCGCTTCCATAA-3’ |
| circ-RHOJ.1 | Forward: 5’-GCCCGTTTGCTGTATATGAA-3’ Reverse: 5’-GGTTGTAGTCCTCCGCTT-3’ |
| 18srRNA | Forward: 5’-CCTGGATACCGCAGCTAGGA-3’ Reverse: 5’-GCGGCGCAATACGAATGCCCC-3’ |
| miR-124-3p | Forward: 5’-ACACTCCAGCTGGGTAAGGCACGCGGTGAAT-3’ Reverse: 5’-CTCAACTGGTGTCGTGGA-3’ |
| U6 | Forward: 5’-CTCGCTTCGGCAGCACA-3’ Reverse: 5’-AACGCTTCACGAATTTGCGT-3’ |
Western blot assay
Proteins were extracted using radioimmunoprecipitation assay (RIPA) buffer (Beyotime). The concentrations of proteins were determined with bicinchoninic acid (BCA) kit (Thermo Scientific). Proteins (40 µg) were isolated with 8% sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS-PAGE) and transferred onto polyvinyl difluoride (PVDF) membranes (Cat. No. IPVH00010; MILLIPORE). The membranes were blocked with 5% skimmed milk (BD Biosciences) and treated with primary antibodies against glyceraldehyde-3-phosphate dehydrogenase (GAPDH; 1 : 1000, KC-5G5) and NRG1 (Cat. No. ab180808; 1 : 10000, Abcam) overnight at 4°C. The membranes were incubated with horseradish peroxidase-conjugated secondary antibodies (1 : 2000, Southern Biotech, 4050-05) for 2 h and treated with enhanced chemiluminescent reagents (Cat. No. WBKLS0500; MILLIPORE). The signals were examined with medical X-ray films (XBT-1, Eastman Kodak Company, NY, USA).
Plasmid construction and dual luciferase activity assay
HEK293T cells were provided by the Chinese Academy of Sciences (Shanghai, China) and maintained in DMEM containing 10% FBS and 1% penicillin/streptomycin in 95% air and 5% CO2 at 37°C, and the HEK293T cells were used for the luciferase reporter assay. The binding sites between miR-124-3p and circ-RHOJ.1 were predicted by StarBase V3.0 (starbase.sysu.edu.cn/starbase2/index.php), and the binding sites between miR-124-3p and NGR 3¢-UTR were predicted by TargetScan (http://www.targetscan.org/vert_72/). Wild-type (WT) and mutant (MUT) variants of NRG1 as well as circ-RHOJ.1 were inserted into the luciferase vector psi-CHECK2 (Promega, Madison, USA) to generate reporter plasmids. The primers used were as follows: circ-RHOJ.1-XhoI-F, 5¢-ccgctcgagGAGGACTACAACCAGCTGAGGCCACTC-3¢ and circ-RHOJ.1-NotI-R: 5¢-ataagaatgcggccgcCGCTTTTGCGAGCTTCACACCATGC-3¢; NRG1-XhoI-F: 5¢-ccgctcgagAACCTAAATAAACACATAGATTCACCTG-3¢ and NRG1-NotI-R: 5¢-ataagaatgcggccgcCTGTGGTTGGTTGGTCGTCATATGAG-3¢. HEK293T cells were seeded into 24-well plates and transfected with circ-RHOJ.1 or NRG1 3¢-UTR WT/MUT and miR-124-3p mimic or miR-124-3p inhibitor using Lipofectamine 2000 (Invitrogen, Shanghai, China). After 48 h, the fluorescence intensity was assessed with the Dual Luciferase Assay System (Cat. No. E1910; Promega) according to the manufacturer’s instructions.
Statistical analysis
Data are expressed as mean ± standard deviation (SD). GraphPad (Version 7.0, GraphPad Prism Software, La Jolla, CA, USA) was used to perform statistical analysis with one-way analysis of variance or Student’s t-test. A value of p < 0.05 was considered as significant.
Results
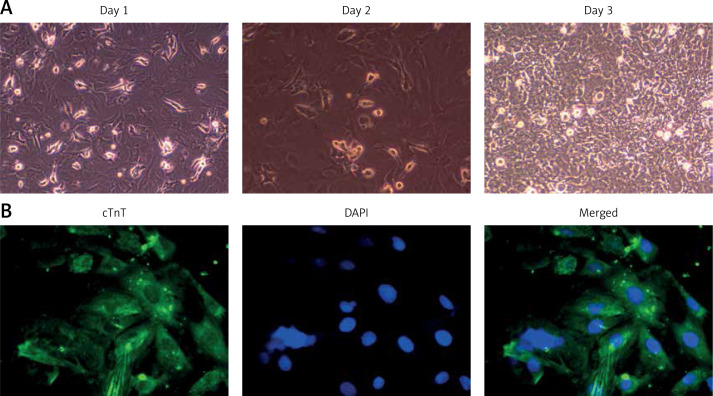
Isolation and identification of rat myocardial cells
Under an inverted microscope, myocardial cells appeared round or oval in shape. After 24 h, most myocardial cells adhered to the surface and gradually extended cellular pseudopods. The morphology of adherent cells was irregular (polygonal- and triangular-shaped cells). After 3 days, the cells formed clusters that were joined by dendrites (Figure 1 A). The results of IF staining showed that cardiac troponin T (cTnT) expression was high and mainly localized in the cytoplasm of the myocardial cells, thereby confirming the staining characteristics of myocardial cells (Figure 1 B).
Figure 1.
Isolation and identification of rat myocardial cells. A – The morphology of the extracted myocardial cells was observed under a microscope on days 1, 2, and 3. Magnification, 100×, scale bars, 50 µm. B – Localization and expression of cTnT was evaluated with immunofluorescence assay in the extracted myocardial cells. cTnT is stained green and nuclei are stained blue (DAPI). Magnification, 400×, scale bars, 10 µm (down)
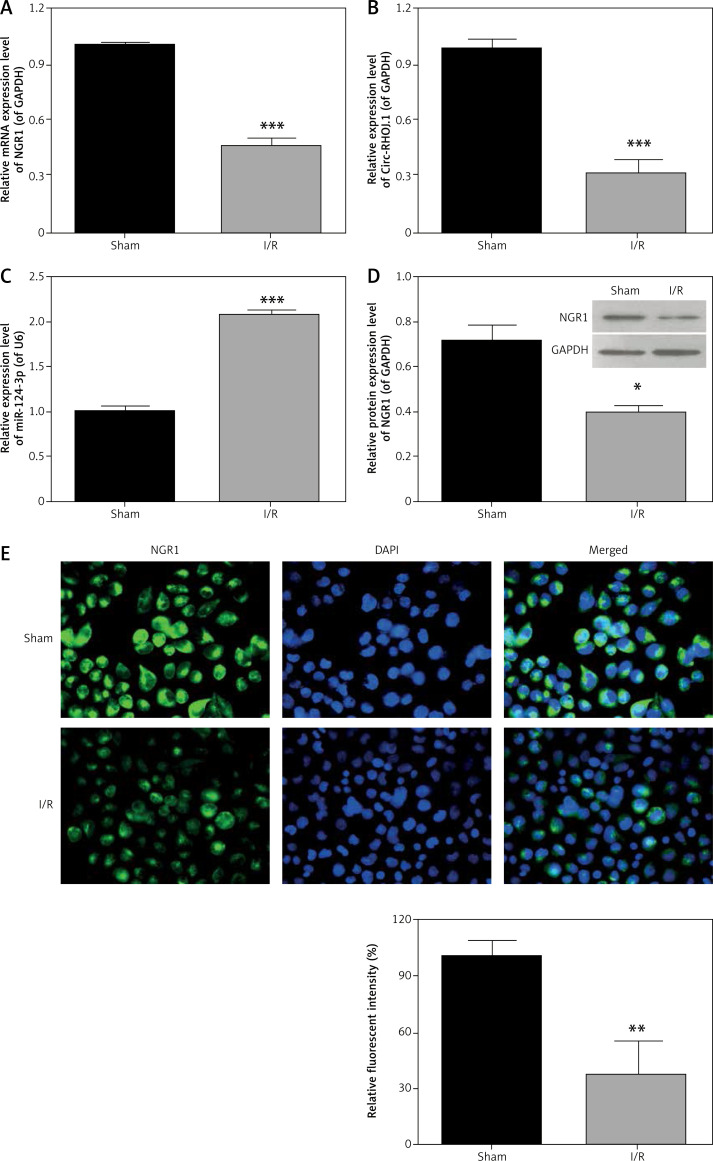
NRG1 and circ-RHOJ.1 expression was down-regulated and miR-124-3p showed up-regulated expression in myocardial cells after I/R injury
To evaluate the effects of NRG1, circ-RHOJ.1, and miR-124-3p expression on myocardial cells after I/R injury, we analyzed the expression levels of these molecules in sham and I/R groups. In comparison with the sham group, the I/R group showed a significant decrease in the expression levels of NRG1 and circ-RHOJ.1 and a significant increase in miR-124-3p expression level in the myocardial cells after I/R injury (Figures 2 A–C). Consistently, the protein expression level of NRG1 was significantly downregulated in myocardial cells after I/R injury as compared with the cells from the sham group (Figure 2 D). The results of IF assay further revealed that NRG1 expression was dramatically reduced in the I/R group as compared with the sham group (Figure 2 E).
Figure 2.
Expression of circ-RHOJ.1, miR-124-3p, and NRG1 in myocardial cells after I/R injury. Expression levels of NRG1 (A), circ-RHOJ.1 (B), and miR-124-3p (C) were assessed with qRT-PCR assay in sham group and I/R group, ***p < 0.001 versus sham group. D – Western blot assay was carried out to measure NRG1 expression in sham group and I/R group. GAPDH was used as a reference. Relative protein expression level of NRG1 was analyzed based on the protein gray values, *p < 0.05 versus sham group. E – Immunofluorescence assay was used to analyze NRG1 expression in sham group and I/R group. Green indicates NGR1 and blue (DAPI) indicates nuclei. Magnification, 400×, scale bars, 10 µm. All the data are presented as mean ± SD (n = 3)
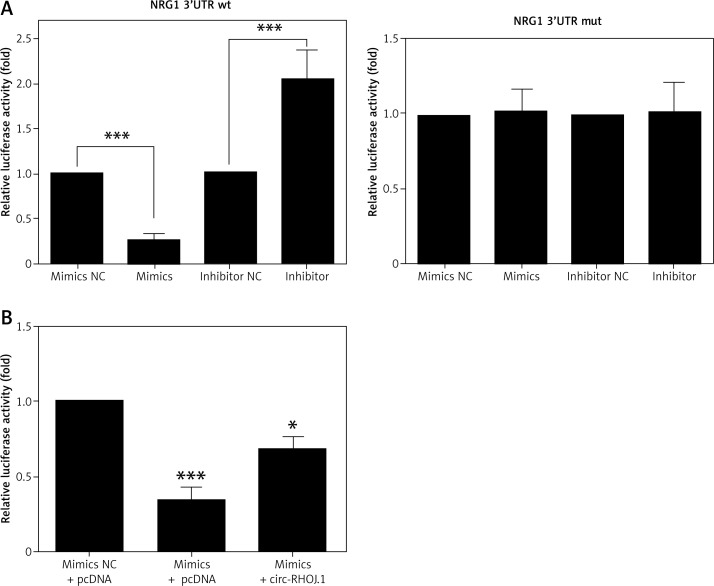
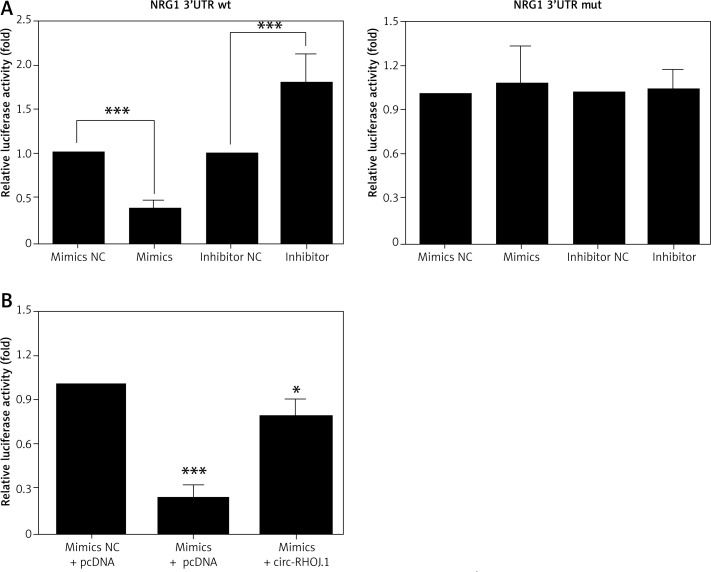
NRG1 was a target gene of miR-124-3p
To investigate whether NRG1 is a target gene of miR-124-3p, we explored the upstream sequence of NRG1 based on the University of California Santa Cruz Genomics Institute (https://genome.ucsc.edu/goldenPath/help/hgTracksHelp.html) and identified the binding sites of NRG1 gene promoter and miR-124-3p using STARBASE 2.0. We generated WT and MUT NRG1 3¢-UTR luciferase reporter plasmids and found that the luciferase activity of the WT 3¢-UTR was significantly inhibited after miR-124-3p mimics treatment as compared with control group, while the luciferase activity of the WT 3¢-UTR was significantly increased after miR-124-3p inhibitor treatment (Figure 3 A). Similar findings were also observed in the myocardial cells (Figure 4 A).
Figure 3.
NRG1 is a target gene of miR-124-3p and circ-RHOJ.1 serves as a sponge for miR-124-3p. A – HEK293T cells were co-transfected with psi-CHECK2 or luciferase plasmids containing the wild-type or mutated NRG1 3’-UTR or NC and miR-124-3p, NC inhibitor, or miR-124-3p inhibitor for 24 h. The relative luciferase intensities were measured with dual luciferase reporter assay, **p < 0.01; ***p < 0.001. B – HEK293T cells were co-transfected with psi-CHECK2 or luciferase plasmids containing the circ-RHOJ.1 and pcDNA or negative control (NC) and miR-124-3p, for 24 h. Dual luciferase reporter assay was carried out to verify the interaction between circ-RHOJ.1 and miR-124-3p, *p < 0.05; **p < 0.01 versus mimics NC + pcDNA group; p < 0.05 versus mimics + pcDNA group. All the data are presented as mean ± SD (n = 3)
Figure 4.
NRG1 is a target gene of miR-124-3p and circ-RHOJ.1 serves as a sponge for miR-124-3p. A – Myocardial cells were co-transfected with psi-CHECK2 or luciferase plasmids containing the wild-type or mutated NRG1 3’-UTR or NC and miR-124-3p, NC inhibitor, or miR-124-3p inhibitor for 24 h. The relative luciferase intensities were measured with dual luciferase reporter assay, ***p < 0.001. B – Myocardial cells were co-transfected with psi-CHECK2 or luciferase plasmids containing the circ-RHOJ.1 and pcDNA or negative control (NC) and miR-124-3p, for 24 h. Dual luciferase reporter assay was carried out to verify the interaction between circ-RHOJ.1 and miR-124-3p, *p < 0.05; ***p < 0.001 versus mimics NC + pcDNA group; &p < 0.05 versus mimics + pcDNA group. All the data were presented as mean ± SD (n = 3)
Circ-RHOJ.1 served as a sponge for miR-124-3p
One of the important mechanistic actions of circRNAs was acting as a competing endogenous RNA (ceRNA) for miRNAs. Thus, we predicted the possible binding sites between circ-RHOJ.1 and miR-124-3p using bioinformatic software (STARBASE 2.0: starbase.sysu.edu.cn). The results of dual-luciferase reporter assay demonstrated that circ-RHOJ.1 may interact with miR-124-3p by acting as a ceRNA (Figure 3 B). Consistent findings were also observed in the myocardial cells (Figure 4 B).
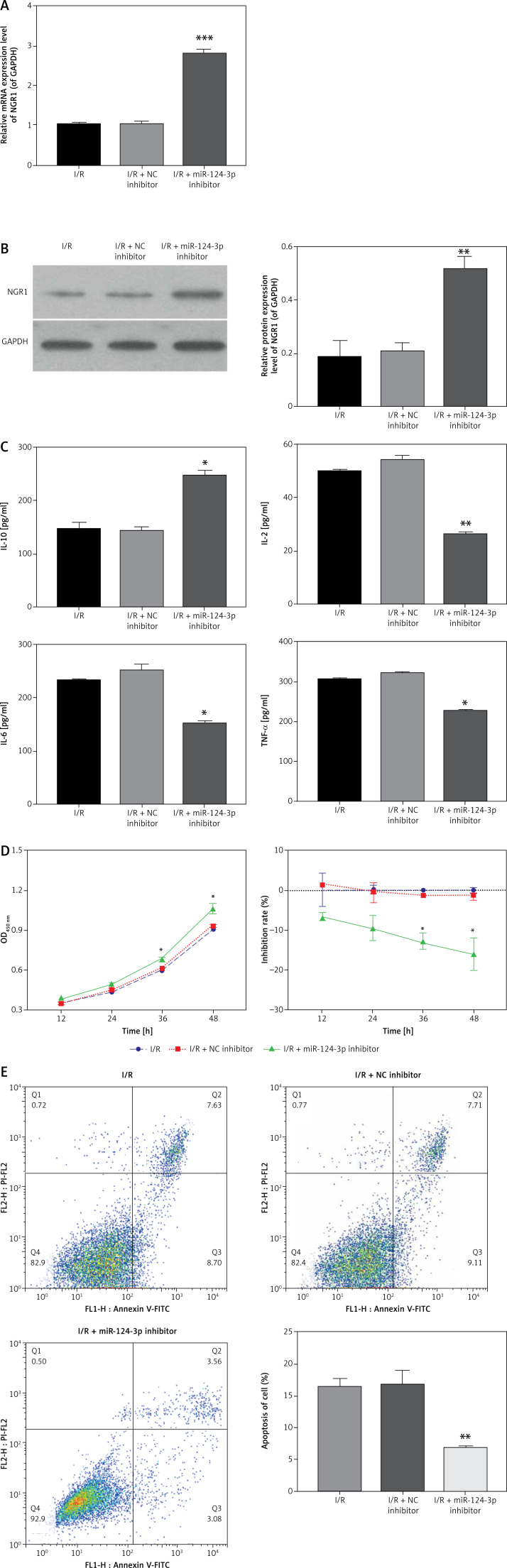
MiR-124-3p inhibitor enhanced the proliferation and inflammatory response and inhibited apoptosis of myocardial cells after I/R injury
To explore the biological role of miR-124-3p in myocardial cells after I/R injury, cells were treated with miR-124-3p inhibitor or NC inhibitor after I/R injury. NRG1 expression markedly increased in cells treated with miR-124-3p inhibitor as compared with those treated with NC inhibitor (Figures 5 A, B). We examined the effects of miR-124-3p inhibitor on levels of cytokines including IL-10, IL-2, IL-6, and TNF-α, and myocardial cells after I/R injury showed a decrease in the IL-10 concentration and an increase in the concentrations of IL-2, IL-6, and TNF-α (Figure 6). Cells were treated with miR-124-3p inhibitor after I/R injury, and IL-10 expression was significantly increased and concentrations of IL-2, IL-6, and TNF-α were significantly reduced in the miR-124-3p inhibitor transfection group as compared with the NC inhibitor group (Figure 5 C). We detected the effects of these treatments on cell proliferation and found that miR-124-3p inhibitor treatment significantly increased the proliferative ability of myocardial cells after I/R injury as compared with NC inhibitor treatment (Figure 5 D). In addition, flow cytometer assay results showed that the apoptotic rate in myocardial cells was significantly reduced following miR-124-3p inhibitor treatment as compared with NC inhibitor treatment (Figure 5 E).
Figure 5.
miR-124-3p inhibitor enhances the proliferation and inflammatory response and inhibits apoptosis of myocardial cells after I/R injury. A, B – Relative mRNA and protein expression levels of NRG1 were examined with qRT-PCR and western blot assays in myocardial cells after I/R injury, respectively. **p < 0.01, ***p < 0.001 versus I/R + NC inhibitor group. C – The concentrations of IL-10, IL-2, IL-6, and TNF-α were analyzed with ELISA assay in miR-124-3p inhibitor-treated myocardial cells after I/R injury, *p < 0.05, **p < 0.01 vs. I/R + NC inhibitor group D – CCK-8 assay was used to examine the effect of miR-124-3p inhibitor on the viability of myocardial cells after I/R injury, *p < 0.05 versus I/R + NC inhibitor group. E – The effect of miR-124-3p inhibitor on the apoptosis rate of myocardial cells after I/R injury was determined with flow cytometry, **p < 0.01 versus I/R + NC inhibitor group. All the data are presented as mean ± SD (n = 3)
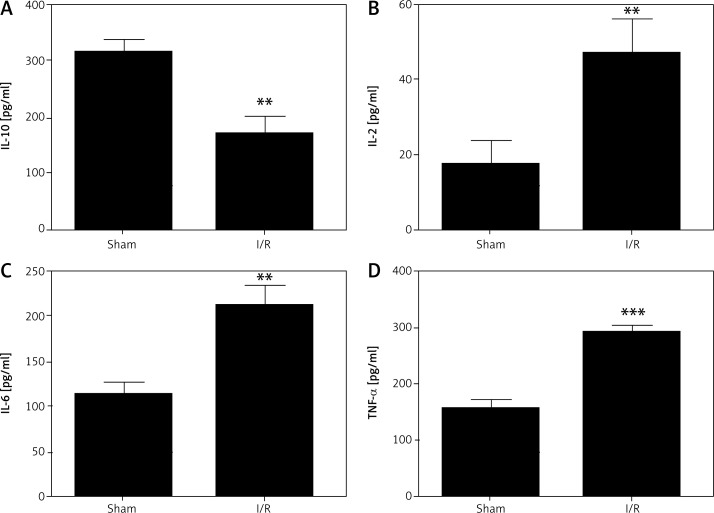
Figure 6.
Effects of myocardial I/R injury on the concentrations of cytokines. The concentrations of IL-10, IL-2, IL-6, and TNF-α were analyzed with ELISA in myocardial cells after I/R injury. **P < 0.01 and **p < 0.001. All the data were presented as mean ± SD (n = 3)
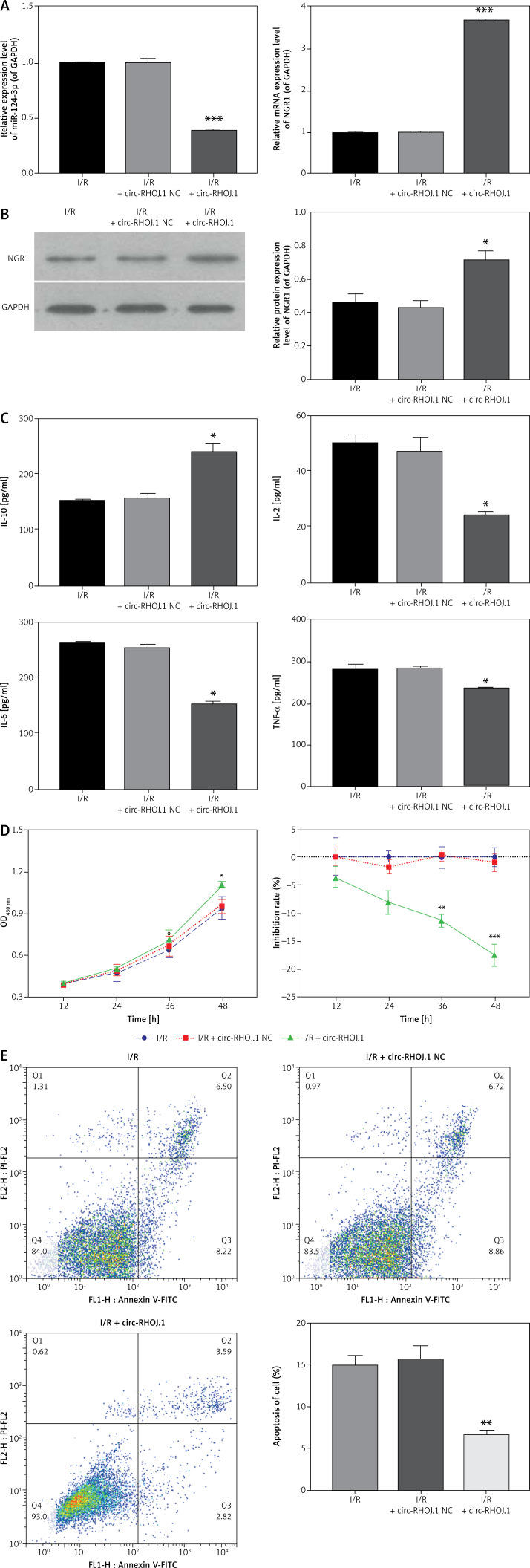
Overexpression of circ-RHOJ.1 accelerated the proliferation and inflammatory response and suppressed apoptosis of myocardial cells after I/R injury
To explore the biological role of circ-RHOJ.1 after I/R injury, we overexpressed circ-RHOJ.1 in myocardial cells after I/R injury through the transfection of circ-RHOJ.1 plasmid. The results revealed that the overexpression of circ-RHOJ.1 significantly downregulated the expression of miR-124-3p and upregulated the expression of NRG1 in myocardial cells after I/R injury (Figures 7 A, B). IL-10 expression was increased and IL-2, IL-6, and TNF-α expression was markedly decreased in the cells overexpressing circ-RHOJ.1 as compared with those treated with NC (Figure 7 C). The effects of circ-RHOJ.1 on cell proliferation and apoptosis were assessed with CCK-8 assay and flow cytometry, respectively. CCK-8 results indicated that the overexpression of circ-RHOJ.1 significantly promoted cell proliferation as compared with control cells (Figure 7 D). Flow cytometry results also showed that the overexpression of circ-RHOJ.1 significantly inhibited the apoptosis of myocardial cells after I/R injury (Figure 7 E).
Figure 7.
Overexpression of circ-RHOJ.1 accelerates the proliferation and inflammatory response and suppresses apoptosis of myocardial cells after I/R injury. A – NRG1 and miR-124-3p expression was evaluated with qRT-PCR assay in circ-RHOJ.1-overexpressing myocardial cells after I/R injury. ***P < 0.001 versus I/R + circ-RHOJ.1 NC group. B – NRG1 expression was measured with western blot assay, and the relative protein expression level of NRG1 was calculated, ***p < 0.001 versus I/R + circ-RHOJ.1 NC group. C – Concentrations of IL-10, IL-2, IL-6, and TNF-α were analyzed with ELISA in circ-RHOJ.1-treated myocardial cells after I/R injury. *P < 0.05, **p < 0.01 versus I/R + NC inhibitor group D – CCK-8 assay was performed to confirm the effect of circ-RHOJ.1 on the viability of myocardial cells after I/R injury, *p < 0.05 versus I/R + circ-RHOJ.1 NC group. E – Effect of circ-RHOJ.1 on the apoptosis rate of myocardial cells after I/R injury, as examined with flow cytometry. **P < 0.01 versus I/R + circ-RHOJ.1 NC group. All the data are presented as mean ± SD (n = 3)
Discussion
Ischemia is the pathological manifestation of insufficient blood supply caused by a blood supply disorder [20]. Diseases caused by tissue ischemia are known as ischemic diseases, which are common in a variety of tissues and organs. Timely myocardial reperfusion therapy such as thrombolysis and percutaneous coronary intervention (PCI) may reconstruct the coronary artery and reduce the area of myocardial necrosis. This serves as a key treatment strategy for acute myocardial infarction (AMI) [20]. However, recent studies have found that the sudden opening of coronary arteries and the recovery of blood flow may lead to abnormal vascular endothelial cell function and activation of relevant inflammatory factors that may aggravate the injury of ischemic myocardium and lead to reperfusion injury [21]. About 40–50% of cases of necrotic myocardium were shown to be related to reperfusion injury [22]. Therefore, reduction in reperfusion injury has become one of the most important goals of AMI prevention and treatment. Both cTnT and cardiac troponin I (cTnTI) are identified as biochemical markers of myocardial injury [23]. In our study, we found that cTnT expression was high in the isolated myocardial cells, suggestive of the successful isolation of rat myocardial cells.
The expression profiles of abnormal circRNAs were shown to be closely associated with the initiation and progression of various human diseases, including cancer, diabetes, atherosclerotic vascular diseases and systemic diseases [24]. CircRNAs were shown to be involved in myocardial I/R injury. For instance, autophagy-related circular RNA could attenuate myocardial I/R injury through the inhibition of autophagy [11]. In addition, circRNAs were differentially expressed in a liver I/R injury model [25] and silencing of circ_008018 expression resulted in protective effects against cerebral I/R injury through regulating miR-99a expression [26]. In our study, we demonstrated that circ-RHOJ.1 expression was significantly downregulated in myocardial cells after I/R injury and circ-RHOJ.1 could accelerate proliferation and inhibit apoptosis of myocardial cells after I/R injury. Recent studies have also shown that miR-124-3p had significant effects on I/R injury [14]. In our study, similar results were obtained regarding the effects of miR-124-3p in myocardial I/R injury.
MiRNA response elements (MREs) are also considered as circRNAs, indicating that circRNAs may serve as miRNA sponges and reduce their levels to restore the function of their targeted genes [27]. In our study, we proved that circ-RHOJ.1 negatively regulates miR-124-3p expression by serving as a sponge and that NRG1 is a target gene of miR-124-3p. NRG1, a member of the epidermal growth factor family, could induce the growth and differentiation of skeletal muscle cells and play a crucial role in heart protection [28]. As miR-124-3p suppressed the NRG1 expression via targeting the 3¢-UTR, restoration of circ-RHOJ.1 induced miR-124-3p suppression, which could subsequently lead to the activation of NRG1 after myocardial I/R injury. Therefore, the circ-RHOJ.1/miR-124-3p/NRG1 axis may participate in myocardial I/R injury.
The inflammatory response is a crucial process in myocardial I/R injury, and the inflammatory response may involve the release of a variety of cytokines such as TNF-α, IL-6, IL-10, and IL-2 [29, 30]. Previous studies have confirmed that TNF-α could induce myocardial I/R through inflammatory responses [31]. In our study, we demonstrated that circ-RHOJ.1 overexpression or miR-124-3p inhibitor significantly increased the IL-10 level and significantly reduced IL-2, IL-6, and TNF-α levels in myocardial cells after I/R injury. Previous studies have shown that interferon regulatory factor 9 serves as a pivotal mediator in hepatic I/R injury by increasing the levels of pro-inflammatory cytokines and chemokines (TNF-α and IL-6) and decreasing levels of the anti-inflammatory cytokine IL-10 [32]. Therefore, we suggest that circ-RHOJ.1 and miR-124-3p may act as crucial mediators in myocardial I/R injury by inhibiting the inflammatory response.
In the current study, several limitations should be addressed. Based on the prediction results, the interaction between circ-RHOJ.1 and miR-124-3p was confirmed in our study. However, the targets of circ-RHOJ.1 may not be limited to miR-124-3p, and other targets of circ-RHOJ.1 may be explored in future studies. In addition, miR-124-5p co-exists simultaneously in similar amounts with miR-124-3p, and miR-124-5p is also known for its role in certain cardiac diseases [33], though miR-124-5p was not predicted to interact with circ-RHOJ.1. Hence, further investigations may be needed to determine the role of miR-124-5p in regulating inflammatory responses in I/R injury. Moreover, the use of human cardiomyocytes may provide more direct evidence for circ-RHOJ.1 in I/R injury. The present study also lacks in vivo animal studies as well as clinical sample examination to further consolidate the role of circ-CHOJ.1 in the pathophysiology of I/R injury.
In conclusion, our data showed the downregulation of circ-RHOJ.1 and NRG1 and the up-regulation of miR-124-3p in myocardial cells after I/R injury. Further mechanistic studies revealed that circ-RHOJ.1 enhanced proliferation and inhibited apoptosis and inflammatory responses of myocardial cells after I/R injury by targeting miR-124-3p/NRG1. The role of circ-RHOJ.1 in regulating I/R injury may require further confirmation by in vivo animal studies and clinical investigations. The present study may advance our understanding of circRNAs-mediated I/R injury.
Acknowledgments
The work was supported by grants from the Science and Technology project of Shenzhen city of China (JCYJ20180302173849459, JCYJ20170307161535847 and JCYJ20170413114916687), Sanming Project of Medicine in Shenzhen of China (No. SZSM201512047), the Research Project (Doctoral Innovation Program) of the Health Planning system of Shenzhen city (SZBC2017007).
Conflict of interest
The authors declare no conflict of interest.
References
- 1.He S, Wang X, Chen A. Myocardial ischemia/reperfusion injury: the role of adaptor proteins Crk. Perfusion 2017; 32: 345-9. [DOI] [PubMed] [Google Scholar]
- 2.Fang R, Zhang LL, Zhang LZ, Li W, Li M, Wen K. Sphingosine 1-phosphate postconditioning protects against myocardial ischemia/reperfusion injury in rats via mitochondrial signaling and Akt-Gsk3beta phosphorylation. Arch Med Res 2017; 48: 147-55. [DOI] [PubMed] [Google Scholar]
- 3.Carden DL, Granger DN. Pathophysiology of ischaemia-reperfusion injury. J Pathol 2000; 190: 255-66. [DOI] [PubMed] [Google Scholar]
- 4.Boag SE, Andreano E, Spyridopoulos I. Lymphocyte communication in myocardial ischemia/reperfusion injury. Antioxid Redox Signal 2017; 26: 660-75. [DOI] [PubMed] [Google Scholar]
- 5.Shu L, Zhang W, Huang C, Huang G, Su G. Troxerutin protects against myocardial ischemia/reperfusion injury via Pi3k/Akt pathway in rats. Cell Physiol Biochem 2017; 44: 1939-48. [DOI] [PubMed] [Google Scholar]
- 6.Strmsek Z, Kunej T. MicroRNA silencing by DNA methylation in human cancer: a literature analysis. Noncoding RNA 2015; 1: 44-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhao J, Chen Y, Liu F, Yin M. Overexpression of miRNA-143 inhibits colon cancer cell proliferation by inhibiting glucose uptake. Arch Med Res 2018; 49: 497-503. [DOI] [PubMed] [Google Scholar]
- 8.Comai L, Zhang B. MicroRNAs: key gene regulators with versatile functions. Plant Mol Biol 2012; 80: 1. [DOI] [PubMed] [Google Scholar]
- 9.Wang PL, Bao Y, Yee MC, et al. Circular RNA is expressed across the eukaryotic tree of life. PLoS One 2014; 9: e90859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Greene J, Baird AM, Brady L, et al. Circular RNAs: biogenesis, function and role in human diseases. Front Mol Biosci 2017; 4: 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhou LY, Zhai M, Huang Y, et al. The circular RNA ACR attenuates myocardial ischemia/reperfusion injury by suppressing autophagy via modulation of the Pink1/FAM65B pathway. Cell Death Differ 201p; 26: 1299-315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bartel DP. MicroRNAs: genomics, biogenesis, mechanism, and function. Cell 2004; 116: 281-97. [DOI] [PubMed] [Google Scholar]
- 13.Qiu L, Tan EK, Zeng L. microRNAs and Neurodegenerative diseases. Adv Exp Med Biol 2015; 888: 85-105. [DOI] [PubMed] [Google Scholar]
- 14.Leung LY, Chan CP, Leung YK, et al. Comparison of miR-124-3p and miR-16 for early diagnosis of hemorrhagic and ischemic stroke. Clin Chim Acta 2014; 433: 139-44. [DOI] [PubMed] [Google Scholar]
- 15.Rong D, Sun H, Li Z, et al. An emerging function of circRNA-miRNAs-mRNA axis in human diseases. Oncotarget 2017; 8: 73271-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim C, Yang H, Fukushima Y, et al. Vascular RhoJ is an effective and selective target for tumor angiogenesis and vascular disruption. Cancer Cell 2014; 25: 102-17. [DOI] [PubMed] [Google Scholar]
- 17.Wilson E, Leszczynska K, Poulter NS, et al. RhoJ interacts with the GIT-PIX complex and regulates focal adhesion disassembly. J Cell Sci 2014; 127: 3039-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu L, Chen J, Sun L, Xu Y. RhoJ promotes hypoxia induced endothelial-to-mesenchymal transition by activating WDR5 expression. J Cell Biochem 2018; 119: 3384-93. [DOI] [PubMed] [Google Scholar]
- 19.Zhu HL, Wei X, Qu SL, et al. Ischemic postconditioning protects cardiomyocytes against ischemia/reperfusion injury by inducing MIP2. Exp Mol Med 2011; 43: 437-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kalogeris T, Baines CP, Krenz M, Korthuis RJ. Ischemia/reperfusion. Compr Physiol 2016; 7: 113-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ibanez B, Heusch G, Ovize M, Van de Werf F. Evolving therapies for myocardial ischemia/reperfusion injury. J Am Coll Cardiol 2015; 65: 1454-71. [DOI] [PubMed] [Google Scholar]
- 22.Zaha VG, Qi D, Su KN, et al. AMPK is critical for mitochondrial function during reperfusion after myocardial ischemia. J Mol Cell Cardiol 2016; 91: 104-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yang R, Fang W, Liang J, et al. RhoJ Apelin/APJ axis improves angiotensin II-induced endothelial cell senescence through AMPK/SIRT1 signaling pathway. Arch Med Sci 2018; 14: 725-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Qu S, Yang X, Li X, et al. Circular RNA: a new star of noncoding RNAs. Cancer Lett 2015; 365: 141-8. [DOI] [PubMed] [Google Scholar]
- 25.Ye Z, Kong Q, Han J, Deng J, Wu M, Deng H. Circular RNAs are differentially expressed in liver ischemia/reperfusion injury model. J Cell Biochem 2018; 119: 7397-405. [DOI] [PubMed] [Google Scholar]
- 26.Yang X, Ji H, Yao Y, et al. Downregulation of circ_008018 protects against cerebral ischemia-reperfusion injury by targeting miR-99a. Biochem Biophys Res Commun 2018; 499: 758-64. [DOI] [PubMed] [Google Scholar]
- 27.Ke X, Ke B, Wang X, Wu S, Yang R, Hu C. Additive effects of atorvastatin combined with sitagliptin on rats with myocardial infarction: a pilot study. Arch Med Sci 2017; 13: 956-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhou Q, Wang L, Wang X, et al. Effect of neuregulin-1 on heart function and inflammatory mediators in rats with sepsis. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue 2018; 30: 140-4. [DOI] [PubMed] [Google Scholar]
- 29.Ling H, Chen H, Wei M, Meng X, Yu Y, Xie K. The effect of autophagy on inflammation cytokines in renal ischemia/reperfusion injury. Inflammation 2016; 39: 347-56. [DOI] [PubMed] [Google Scholar]
- 30.Shi J, Dai W, Kloner RA. Therapeutic hypothermia reduces the inflammatory response following ischemia/reperfusion injury in rat hearts. Ther Hypothermia Temp Manag 2017; 7: 162-70. [DOI] [PubMed] [Google Scholar]
- 31.Hu X, Ma R, Lu J, et al. IL-23 promotes myocardial I/R injury by increasing the inflammatory responses and oxidative stress reactions. Cell Physiol Biochem 2016; 38: 2163-72. [DOI] [PubMed] [Google Scholar]
- 32.Wang PX, Zhang R, Huang L, et al. Interferon regulatory factor 9 is a key mediator of hepatic ischemia/reperfusion injury. J Hepatol 2015; 62: 111-20. [DOI] [PubMed] [Google Scholar]
- 33.Zheng D, Cai A, Xu R, et al. Effects and potential mechanism of atorvastatin treatment on Lp-PLA2 in rats with dyslipidemia. Arch Med Sci 2018; 14: 629-34. [DOI] [PMC free article] [PubMed] [Google Scholar]