Abstract
Background
Pelvic floor muscle training is recommended as first line treatment for urinary incontinence in women based on three proposed theorized mechanisms: ‘Enhanced Pelvic Floor Muscle Strength,’ ‘Maximized Awareness of Timing,’ and ‘Strengthened Core Muscles’. The purpose of this scoping review was to systematically map evidence for and against theorized mechanisms through which pelvic floor muscle training interventions work to reduce urinary incontinence in women.
Methods
The scoping review is based upon a comprehensive search of relevant literature published from 1990 to 2020 in PubMed, CINAHL, PsycINFO, ClinialTrials.gov, reference lists from review articles, and hand searches of articles by known researchers in the field. We included English-language, peer-reviewed articles on pelvic floor muscle training as an intervention for adult women if they provided empirical evidence to testing the theorized intervention mechanisms. Two independent reviewers screened articles for inclusion and extracted data to describe details of each study (author, year, country, design, sampling), measures of pelvic floor muscle strength and urinary incontinence, statistical analysis of linkage between changes in the measures, and pelvic floor muscle training regimens. Data were summarized to facilitate the integration of diverse evidence to draw conclusions on supporting or refuting the three proposed theorized mechanisms for managing urinary incontinence in women.
Results
Of the 278 articles identified with the search, 13 (4.7%) met inclusion criteria. There was weak to no evidence for the mechanism of enhanced pelvic floor muscle strength, equivocal support for maximized awareness of timing, and no evidence for strengthened core muscles.
Conclusions
This review revealed extremely limited data supporting the proposed theorized mechanisms underlying pelvic floor muscle training programs to manage urinary incontinence in women. Such evidence is needed to help women and clinicians understand how, why and when a woman benefits from pelvic floor muscle training. Future studies should specifically state and report statistical analysis that relates the theorized mechanisms to the training outcomes observed.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12905-022-01742-w.
Keywords: Urinary incontinence, Kegel, Knack skill, Pelvic muscle exercises, Physical therapy, Transversus abdominis
Background
Urinary incontinence (UI) is defined as the report of any involuntary leakage of urine [1]. The global prevalence of UI is between 5 to 69% during a woman’s lifetime, with higher prevalence in older age groups [2, 3]. Pelvic floor muscle training (PFMT) is recommended as the first line treatment for the most common forms of incontinence: stress, urge, or mixed urinary incontinence (SUI, UUI, or MUI) [4]. PFMT programs vary but can be prescribed as taught and supervised by a health professional, conducted for the purpose of preventing or treating UI and other pelvic floor disorders [5]. Generally, referrals to PFMT programs (typically as supervised by physical therapists or physiotherapists), are routinely made by obstetricians, midwives, gynecologists, urologists, urogynecologists, nurse practitioner continence specialists, in addition to general health care providers.
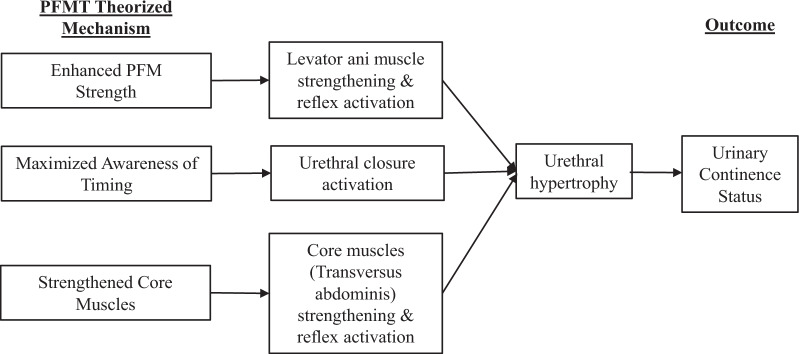
Three proposed theorized mechanisms guide current PFMT approaches [6] (Fig. 1). We named the theorized mechanisms according to the focus and goal of each. The first and dominant mechanism is “Enhanced Pelvic Floor Muscle Strength,” pertaining to increasing the cross-sectional area of the key support muscle underlying the urethra. This mechanism targets the levator ani muscle and is operationalized as repetitive contractions to exercise the levator ani muscle. The names of the PFMT programs that use this theorized mechanism are (most commonly) “Kegel’s exercises” or pelvic floor muscle (PFM) exercises.
Fig. 1.
Theorized Mechanisms of PFMT. PFMT, pelvic floor muscle training; PFM, pelvic floor muscle
The second mechanism is “Maximized Awareness of Timing” pertaining to enhanced personal control over improving urethral closure pressure momentarily in a moment of need [7]. This mechanism targets the urethral striated muscle, is operationalized as first identifying triggers for leakage so that anticipatory timing of PFM contraction in that moment can occur and as a PFMT program it has been named ‘the Knack’, ‘stress strategy’, and ‘perineal lock’. A timely contraction as an overarching descriptor for training emphasizes the knack of knowing when to contract across everyday life events.
The third mechanism is “Strengthened Core Muscles.” This mechanism is derived from the supposition that contraction of core abdominal muscles elicits a co-contraction of the PFM reflexively [8]. ‘Strengthened Core Muscles’ targets the transversus abdominis (TrA) muscle, and PFMT programs reliant on this theorized mechanism are typically referred to as core muscle training.
It is unclear how much evidence is available to support these theorized mechanisms. Reductions in UI in at least some study participants [4, 9] are a desired and logical outcome of these interventions but do not provide direct evidence of mechanisms. If data on mechanisms were available, it could be used to refine interventions and explain why some women do not benefit from certain treatments. For example, suppose there is empirical evidence showing that TrA strength increases after intervention and is highly associated with reductions in UI. Women who do not show increases in TrA strength would be expected not to show improved UI.
Reasons why a mismatch to theory occurred could be further investigated to refine the intervention. A mismatch to theory may be applicable only to certain subpopulations. For instance, it is now known that a partial or complete tear of critical PFM fibers away from their attachment at the pelvic bone occurs under certain childbirth-related conditions [10, 11]. The condition is chronic [12]. As a biological variable that directly affects ability to strengthen or even activate the PFM, a muscle detachment tear represents a logical moderating variable on hypothesized relationships between either maximizing strength or maximizing awareness as mechanisms underlying PFMT success. In this example, the likely assumption exposed is that all women have the biological capacity to contract the PFM, when in reality there is a categorical variable of PFM tear that logically interferes. Evidence for or against the mechanism is thus muddied if the moderator is not included.
Therefore to demonstrate these gaps, a scoping review of the literature was conducted to summarize evidence on the theorized mechanisms underlying PFMT for UI in women. Mechanisms that were investigated included enhanced PFM strength, maximized awareness of timing, and strengthened core muscles. The following research questions were formulated: What is known from statistical analyses in the literature about associations between changes in PFM strength and UI? What is known about PFM tear as a moderator of these associations?
Methods
Protocol and registration
This review of the literature was performed following the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (Additional file 1: PRISMA-ScR) guidelines [13]. This review was not registered. Institutional Review Board approval was not applicable.
Information sources and searches
We performed separate literature searches for each theorized mechanism because each required specific search terms. We searched PubMed for evidence pertaining to all three mechanisms. For enhanced PFM strength mechanism, as the earliest and most long-standing theorized mechanism, we added a search of PsycINFO and CINAHL as the historically gold standard databases for psychological, nursing, and behavioral approaches. For these search engines, search limiters were set to be adults age 18 or older, female, and articles in English published 1990 and after. The reason of choosing publications from 1990 was Wells (1990) conducted a similar state of the literature as reviewed, revealing 22 articles dating from 1952 to 1988 [14].
We then used hand search strategies to screen articles cited by systematic reviews of interventions, such as Cochrane reviews, and seminal PFMT articles written by researchers well-known in the field. We also searched ClinicalTrials.gov to find additional clinical trials that applied PFMT interventions to treat UI in women and then searched MEDLINE/PubMed using the National Clinical Trial number to identify the publications. The final search results were exported into EndNote, and duplicates were removed by the first author.
Enhanced PFM strength search details
The search for the enhanced PFM strength mechanism was completed in July 2020 excepting for the search in ClinicalTrials.gov, which was completed in December 2020. The literature was searched using various combinations of both Medical Subject Headings and/or related keywords. Specific search strings were: (pelvic floor muscle strength OR levator ani muscle OR Kegel muscle OR pelvic floor muscles) AND (pelvic floor muscle training OR Kegel exercises OR pelvic muscle exercises) AND urinary incontinence. The search strategy for PubMed using the above search strings as well as details of clinical trials search from ClinicalTrials.gov can be found in Additional file 2: Supplementary A.
Maximized awareness of timing search details
The search for the maximized awareness of timing mechanism was completed in PubMed in August 2020, excepting the ClinicalTrials.gov search completed in December 2020. This search included maximized awareness as either the singularly focused mechanism of PFMT or as a mechanism in addition to enhanced PFM strength as another proposed theorized mechanism and accompanying part in operationalizing the full PFMT reported. Search strings were stress urinary incontinence AND (knack OR stress strategy OR perineal lock OR single Kegel OR precontraction OR perineal co-contraction OR voluntary pelvic muscle contraction OR pelvic clutch OR bracing OR counter bracing OR quick Kegel OR perineal blockage).
Strengthened core muscles search details
The search for the strengthened core muscles mechanism was completed in PubMed in August 2020 and ClincialTrials.gov in December 2020. The search strings were (transverse abdominis training OR transverse abdominis exercises OR transversus abdominis training OR transversus abdominis exercises OR transversus abdominis muscle contraction) AND urinary incontinence.
Eligibility criteria
Inclusion criteria common across the three searches were: peer-reviewed, original research, full-length articles; English-language; published in 1990 and later; PFMT as an intervention for adult women; and reported data on purported mechanisms. For the latter, we included articles that reported data on associations between increased PFM strength and incontinence reduction for the enhanced PFM strength mechanism; mechanism data of PFM volitional activation, urethral closure and striated muscle bulk for maximized awareness of timing mechanism; and mechanism data of co-contraction of PFM and TrA muscles as indicative of strengthened core muscles mechanism.
Common exclusion criteria were: book chapters, review articles, commentaries, dissertations, published abstracts, newspapers, magazines, animal studies, and studies or men or children (under 18 years of age).
Selection of sources of evidence
Lists of potential articles were combined and de-duplicated. In the first stage of review, the first author screened abstracts and titles and retained only those that met inclusion criteria. In the second stage of review, the first author reviewed full texts and retained only those that met inclusion criteria. Disagreements were rare and were resolved through discussion.
We included all articles that met inclusion criteria. Nearly all included articles did not have a stated purpose of testing the mechanism of action of the intervention. Thus, it seemed inappropriate to employ traditional approaches to complete risk of bias in ratings. Rigorously performed trials specific to their specified trial outcomes for the intervention would have rated poorly when considering the purpose of this review—linking analysis of purported mechanism to intervention outcomes.
Data charting process
The first and second authors independently reviewed full texts. The first author extracted relevant data from each eligible article and the second author verified the data extraction. Authors completed all data extraction using Microsoft Excel spreadsheets. Each column was a piece of data to be extracted and each row listed an article. The data extraction form was designed by the first author and revised as needed during the data extraction process.
Data items
Data extracted from the studies included: authors, year of publication, country, statement regarding how sample size was established, sample characteristics, measures used for quantifying the purported theorized mechanism, measures used for quantifying incontinence, description of the PFMT regimen used, and PFM tears. We tabulated statistical parameters reflecting the linkage between purported mechanisms and intervention outcomes, such as correlation, odds ratios, and regression coefficients.
Heterogeneity of PFMT regimens, measurement instruments, and mechanism reports prohibited meta-analysis; thus, a scoping review was performed. We grouped the articles by the three individual theorized mechanisms, summarized sample characteristics, statistical analysis methods, the associations between changes in PFM strength and UI and interventions success.
Because our research questions emphasized robust testing of theorized mechanisms as described in the selected articles, data were also extracted on measures of PFM strength. Extraction categories were (a) the measure’s common or generic name, (b) type (subjective, objective), (c) purpose, and (d) psychometrics.
Results
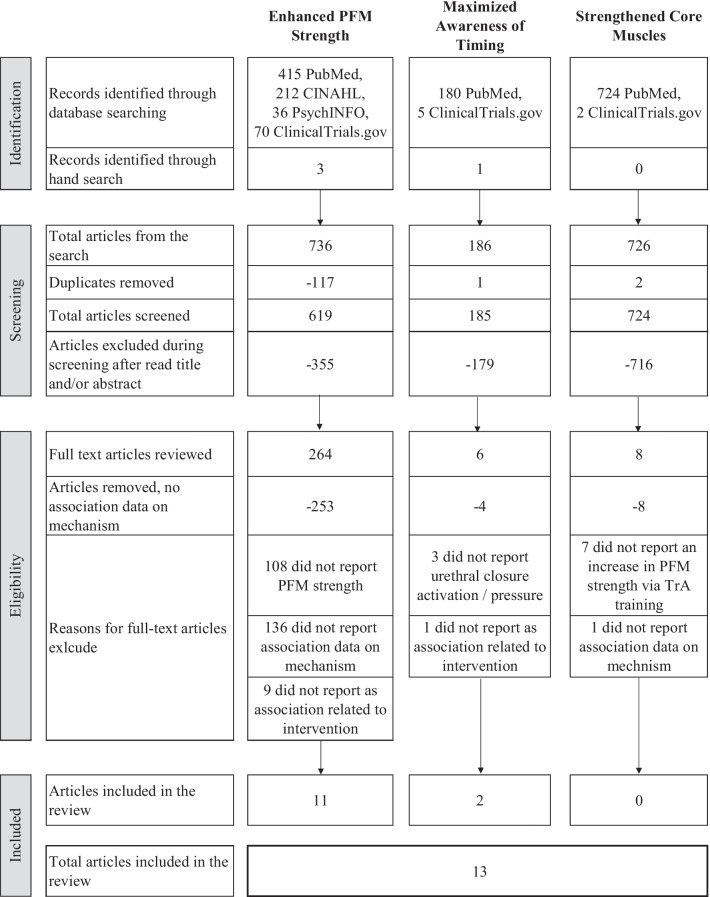
Figure 2 shows the flow of articles from the three searches (one for each purported mechanism). Of 278 full articles reviewed, only 13 (4.7%) were identified as meeting inclusion criteria for providing any statistical analysis testing the linkage between purported mechanism and intervention outcomes. The results by each of the three mechanisms are described below.
Fig. 2.
Modified PRISMA flow diagram showing disposition of articles from the three searches. PRISMA, Preferred Reporting Items for Systematic reviews and Meta-Analysis; PFM, pelvic floor muscle; TrA, transversus abdominis
Mechanism 1. Enhanced PFM strength
As shown in Table 1, the 11 retained articles [15–25] were conducted in Norway, the USA, Turkey, Sweden, Taiwan, Japan, China, and Belgium and included a wide range of populations. Sample sizes assigned to PFMT ranged from 35 to 215. Four studies included control groups—three were no UI treatments and one was bladder training. Mean ages ranged from 26 to 77 years. Samples included pregnant women during the 20th to 34th week of pregnancy [16], postpartum women [24], middle aged and elderly parous women [17, 25], and women older than 70 years [19]. Most samples were characterized with SUI or SUI predominant if representing MUI. Studies included both subjective and objective measures of PFM strength and UI. All studies reported group level increases in PFM strength following intervention, and all but one [15] reported group improvements in UI (Table 2).
Table 1.
Description of study samples and urinary incontinence type
| Author, year and country | Study design | Sample | UI type | |||||
|---|---|---|---|---|---|---|---|---|
| n Assigned PFMT | Age M ± SD, (age range) | Condition | n, Comparators | Urge | Stress | Mixed | ||
| Mechanism 1. Enhanced PFM strength | ||||||||
| Bø (2003), Norway | Secondary analysis of RCT | 52 | 45.5, (24–64) | X | ||||
| Burns et al. (1993), USA | RCT | 83 | 63.0 ± 6.0, 63.0 ± 5.0, (≥ 50) | 40 controls | X | X | ||
| Dinc et al. (2009), Turkey | RCT | 35 | 26.05 ± 4.8, 27.7 ± 7.2 | 20th-34th week of pregnancy | 33 controls | X | X | |
| Dougherty et al. (1993), USA | Pre and post-intervention study | 65 | 51.3 ± 10.6, (35–75) | Mid-age and elderly Parous | X | |||
| Hahn et al. (1993), Sweden | Case-controlled study | 170 | 51.3 ± 0.98, (27–84) | 27 awaiting surgery | X | |||
| Hung et al. (2012), Taiwan | Prospective cohort study | 68 | 50.5 ± 6.0 | X | X | |||
| Kim et al. (2007), Japan | RCT, crossover follow up trial | 70 (35 in each group) | 76.6 ± 5.0, 76.6 ± 3.8 | Elderly | X | |||
| Nystrom et al. (2018), Sweden | Pre and post-intervention study | 61 | 44.7 ± 9.7, (27–72) | X | ||||
| Segal et al. (2016), USA | Prospective cohort study | 215 | 54.4 ± 12.7 | Mid-age and elderly parous | X | |||
| Sun et al. (2018), China | Prospective cohort study | 133 | 33.63 ± 3.98, 42.66 ± 11.35 | Postpartum | X | |||
| Theofrastous et al. (2002), USA | RCT | 69 | 60.6 ± 10.0, (45–79) | 68, bladder training | X | X | ||
| Mechanism 2. Maximized awareness of timing | ||||||||
| Cammu et al. (2000)a, Belgium | 10-Year follow-up | 45 | 61.0 ± 10.0 | X | ||||
| Junginger et al. (2014), Germany | Prospective cohort study | 55 | Not reported | X | X | X | ||
Blank cells = information was not appliable or not available. Articles retained from search results (n = 13 including 11 for enhanced PFM strength mechanism and 2 for maximized awareness of timing mechanism). This table focuses on tabulation in readiness of integration of information for critical analysis of the general quality of studies on PFMT to treat UI, while also testing for theorized mechanism/s of effect
UI, urinary incontinence; PFMT, pelvic floor muscle training; PFM, pelvic floor muscle; M, mean; SD, standard deviation; RCT, randomized controlled trial
aA 10-year PFMT follow up article was also found in the main PFMT strengthening theory literature search, but it was not included in the analysis of results for the main PFMT strengthening theory since it did not report PFM strength and had no statistical analysis of correlation between changes in PFM strength and incontinence
Table 2.
Description of pelvic floor muscle strength and urinary incontinence measures used
| Author and year | PFM strength | UI | ||||
|---|---|---|---|---|---|---|
| Subjective | Objective | Direction of change over time | Subjective | Objective | Direction of change over time | |
| Mechanism 1. Enhanced PFM strength | ||||||
| Bø (2003) | Vaginal balloon catheter | ↑ | Leakage index | Pad test | Not reported | |
| Burns et al. (1993) | EMG | ↑a | 24-h urinary diary | ↓ | ||
| Dinc et al. (2009) | Perineometer | ↑ | 3-day urinary diary | 1-h pad test | ↓ | |
| Dougherty et al. (1993) | Intravaginal balloon device | ↑ | 24-h urinary diary | 24-h pad test | ↓ | |
| Hahn et al. (1993) | Vaginal palpation | ↑ | Pad test | ↓ | ||
| Hung et al. (2012) | Modified Oxford scale | ↑ | Severity Index score | ↓ | ||
| Kim et al. (2007) | Dynamometer | ↑ | Modified ICIQ questions | ↓ | ||
| Nystrom et al. (2018) | A self-rated PFM strength question | ↑ | PGI-I | ↓ | ||
| Segal et al. (2016) | Vaginal EMG | ↑ | Self-reported UI improvement | ↓ | ||
| Sun et al. (2018) | Vaginal manometer | ↑ | 1-h pad test | ↓ | ||
| Theofrastous et al. (2002) | Balloon devices | ↑ | Urinary diary | 48-h pad test | ↓ | |
| Mechanism 2. Maximized awareness of timing | ||||||
| Cammu et al. (2000)b | Vaginal palpationc | ↑ Timely precontraction skill | Self-assessment | ↓ | ||
| Junginger et al. (2014) | Vaginal palpationd | Perineal ultrasounde | ↑ Timely precontraction skill | Posttreatment improvement scales, analog scales for satisfaction, frequency of precontraction | ↓ | |
Blank cells = Information was not appliable or not available. Articles retained from search results (n = 13 including 11 for enhanced PFM strength mechanism and 2 for maximized awareness of timing mechanism). This table focuses on tabulation in readiness of integration of information for critical analysis of the general quality of studies on PFMT to treat UI, while also testing for theorized mechanism/s of effect. All pad tests for UI were performed under provocative maneuver to ask participants to, such as cough, pick, set up and down, run or walk, jump, step, bounce, rise, lay down sit-ups, or stand
PFM, pelvic floor muscle; UI, urinary incontinence; PFMT, pelvic floor muscle training; EMG, electromyography; ICIQ, International Consultation on Incontinence Questionnaire; PGI-I, Patient Global Impression of Improvement Questionnaire
aPelvic muscle electromyography scores measured as quick and sustained contractions only increased in PFMT + biofeedback group, not in the PFMT only group
bA 10-year PFMT follow up article was also found in the main PFMT strengthening theory literature search, but it was not included in the analysis of results for the main PFMT strengthening theory since it did not report PFM strength and had no statistical analysis of correlation between changes in PFM strength and incontinence
cVaginal palpation to correct PFM contraction
dVaginal palpation to evaluate pelvic floor dysfunction
ePerineal ultrasound to evaluate pelvic floor dysfunction and for bladder-neck effective PFM contraction
The majority of the 11 studies provided indirect evidence of the association between improved PFM strength and UI (Table 3). Only two studies provided direct evidence of the correlation as part of the primary aims [15, 21], all others provided evidence as supplementary information.
Table 3.
Statistical analysis of linkage between changes in pelvic floor muscle strength and urinary incontinence
| Author and year | Evidence | Statistical tests of associations between changes in PFM strength and UI with treatment | Association findings by type of measures | ||||
|---|---|---|---|---|---|---|---|
| Direct | Indirect | Subjective PFM strength and UI | Objective PFM strength, subjective UI | Subjective PFM strength, objective UI | Objective PFM strength and UI | ||
| Mechanism 1. Enhanced PFM strength | |||||||
| Bø (2003) | X | 0.23 (p = 0.05), 0.34 (p < 0.01) (Spearman’s rho) | Moderate | Weak | |||
| Burns et al. (1993) | X | 0.26 (p < 0.005), 0.22 (p < 0.03) (Pearson’s r) | Weak | ||||
| Dinc et al. (2009) | X | − 0.17 (p = 0.34) and 0.06 (p = 0.75) (Pearson’s r) | NS | NS | |||
| Dougherty et al. (1993) | X | No value | NS | NS | |||
| Hahn et al. (1993) | X | No value (Pitman’s permutation test, p < 0.05) | Value not reported | ||||
| Hung et al. (2012) | X | 0.265 (Spearman’s rho, p = 0.043); 0.238 (standardized coefficients, p = 0.014) | Weak | Weak | |||
| Kim et al. (2007) | X | No value; 4.545 (p = 0.10), 3.100a (p = 0.21) (Cochran Q) | NS | ||||
| Nystrom et al. (2018) | X | 35.54 (4.96–254.61) (OR, 95% CI; p < .0.001) | Moderate to large | ||||
| Segal et al. (2016) | X | No value (Spearman’s rho) | NS | ||||
| Sun et al. (2018) | X | 1.042 (1.010–1.070) (OR, 95% CI) | Weak | ||||
| Theofrastous et al. (2002) | X | 0.32 (Pearson’s r, p = 0.04), other NS (p > 0.30)b | Moderate to NS | ||||
| Mechanism 2. Maximized awareness of timing | |||||||
| Cammu et al. (2000)c | X | NSd | NS | ||||
| Junginger et al. (2014) | X | − 0.36 (Spearman’s rho, p = 0.006)); 71% women routinely used Knack had less UI (p = 0.021)e | Moderate | ||||
Blank cells = information was not appliable or not available. Only measures and changes that related to statistical analysis of correlation between the changes in PFM strength and incontinence were included in the table
PFM, pelvic floor muscle; UI, urinary incontinence; OR, odds ratio; NS, non significant; CI, confidence interval
aAt 3 months for treatment group and at 12 months for both treatment and control groups
bNon significant correlations were found between increased PFM strength with reduction in incontinence episode per week and in pad weight, significant correlation = 0.32 for the correlation between an increase in maximum sustained vaginal pressure and reduction in incontinence episodes per week in women with stress incontinence
cA 10-year PFMT follow up article was also found in the main PFMT strengthening theory literature search, but it was not included in the analysis of results for the main PFMT strengthening theory since it did not report PFM strength and had no statistical analysis of correlation between changes in PFM strength and incontinence
dNS due to few participants—more often use Knack, the greater improvement; 3 leaked urine during stress test
e71% women routinely used Knack had less UI; improvement of symptoms was not associated with length of follow up and did not decrease over time
In a majority of studies, analysis of the relationship was based on correlation coefficients including Spearman’s rho, Pitman’s permutation test, or Pearson’s r. Few used logistic regression analysis (odds ratios [OR]), Cochran’s Q, or multiple linear regression analysis (standardized coefficients).
Most articles (n = 7 of 11) reported a statistically significant association of PFM strength change and incontinence change. Only one article [20] reported a moderate to large statistical association between self-reported improvement of PFM strength and PFMT success (defined as improved continence) but the confidence interval was exceptionally large (OR = 35.54, 95% CI 4.96–254.61). All others reported no or only weak or moderate associations.
Of the two articles that stated a primary aim of looking for correlation between purported mechanism and outcome, one reported moderate-to-weak and one reported no significant correlation. One article reported that improvement in maximal PFM strength measured by a vaginal balloon catheter significantly correlated with improvement in urine leakage index (rho = 0.34, p < 0.01) and with UI reduction in pad weights (rho = 0.23, p = 0.05) [15].
The second article reported inconsistent findings of the associations. Although the authors found a moderate correlation (r = 0.32, p = 0.04) between increased maximum sustained vaginal pressure measured via a balloon device and self-reported reduction in weekly incontinence episodes, they did not find significant correlations between increased PFM strength measured by the same balloon device with the self-reported incontinence reduction weekly episodes, or reduction of leakage amount in pad weights [21].
The remaining articles had no stated aim about linking mechanism and outcome. Three studies reported weak correlations between purported mechanism and UI reduction (rho = 0.265, p = 0.043; r = 0.22, p < 0.03 and r = 0.26, p < 0.005; or OR = 1.042, 95% CI 1.010–1.070, respectively) [18, 22, 24]. One article also reported standardized coefficients (= 0.238, p = 0.014) for increased PFM strength correlated with reduction in UI severity index in a multiple regression analysis, controlling for baseline levels [18].
One article did not report the parameter value of a correlation reported as significant [23]. Another four studies did not find any significant correlation between change in PFM strength and change in incontinence [16, 17, 19, 25], with one [19] reporting non-significant Cochran Q-values = 4.545 (p = 0.10) at 3 months for intervention group and 3.100 (p = 0.21) at 12 months follow up for all women after received PFMT treatment between improved (adductor muscle) strength and proportion of cured women.
Details of the PFM strength measures used in these studies and their limitations are described in Table 4 and Additional file 3: Supplementary B. Heterogeneity in instruments and accompaniment measurement limitations are notable, making it impossible to compare results across articles. Similarly, there is enormous variance in exercise regimens of the “Kegel muscle”, as shown in Table 5 and Additional file 3: Supplementary B, even though all purportedly are operating from the shared theoretical mechanism to enhance strength of the muscle supporting the urethra.
Table 4.
Instruments used in the reviewed studies to measure pelvic floor muscle strength
| Measures common name (review article) | What is assessed | Reliability | Validity | |
|---|---|---|---|---|
| Subjective | Vaginal digital examination [23, 26] | Grading contraction, pressure around finger/s (4-point scale) | – | – |
| Modified Oxford scale [18] | Grading contraction, pressure around fingers, Poisson effect (as muscle is contracted, it expands a bulging up) (6-point scale) |
r = 0.27–0.95 (inter-rater) [49–53] r = 0.93 (test–retest) [50] |
Correlation with perineometric pressure 0.79 [50] Contaminated by IAP |
|
| A self-rated PFM strength question [20] | Self-reported improvement of PFM strength | – | – | |
| Objective | Perineometer-like devices [16, 24] | Maximum voluntary vaginal closure pressure (mm Hg) | r = 0.79–0.80 (inter-rater) [54] |
Good agreement with Brink digital exam score [55] Contaminated by IAP |
| Intravaginal balloon-like device [15, 17, 21] | Maximum voluntary vaginal closure pressure (mm Hg) | r = 0.52–0.85 (test–retest) [56] | Contaminated by IAP [57] | |
| Needle EMG: quantitative EMG [22] | Muscle electrical activity from individual motor units (in microvolt units) |
r = 0.89 (range 0.78–0.95) [22] hard to repeat |
Not possible to measure contractile force using EMG [58] Contaminated by IAP |
|
| Surface EMG (vaginally): quantitative EMG [25] | Muscle electrical activities from summated from many motor units (millivolt) | Between-visit ICC ranging 0.76–0.97 [59] |
Measured PFM activity other than vaginal closure pressure |
|
| A handheld dynamometer (mTasMF-01, ANIMA, Japan) [19] | Hip adductor muscle strength | – | Not measure PFM strength | |
| Sagittal dynamic (perineal) ultrasound [27] | Cephalic displacement (in mm) of the bladder neck in a sagittal view available as biofeedback (as opposed to caudal movement observable when she pushes down instead) | r = 0.52–0.96 (intra-rater) [62] | Visual “lift” of the bladder neck with a correct PFM contraction |
—, Information was not available; IAP, intraabdominal pressure; PFM, pelvic floor muscle; EMG, electromyography; ICC, intra-class correlation coefficients
Table 5.
Details of pelvic floor muscle training regimens
| Author and year | PFMT at home dose | PFMT in clinic dose | Graded training | Duration | PFMT delivery | Methods for compliance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| # Sessions/day | # Contractions/session | Minutes/session | # Sessions/week | # Contractions/session | Minutes/session | Individual | Group | Supervised | Unsupervised | Device assisted training | ||||
| Mechanism 1. Enhanced PFM strength | ||||||||||||||
| Bø (2003) | 3 | 3 sets of 8–12 per daya | 1 | 6 mo | X | X | X | X | Meet wkly for intensive group | |||||
| Burns et al. (1993) | 4 sets of 20 (10 quick + 10 sustained), then ↑ 10 per set to 200 | 1 | 25–35 | X | 8 wkb | X | X | X | Biofeedback (1 of 2 groups) | Call and exercise reminder cards | ||||
| Dinc et al. (2009) | 2–3 | 3 sets of 10–15 | X | 12–28 wk | X | X | ||||||||
| Dougherty et al. (1993) | 3/wk | 15–45 | X | 16 wk | X | X | Audio recording | Call and written records wkly | ||||||
| Hahn et al. (1993) | 6–8 | Maximal, during jumping and coughing | 1 × 4–5 wks then monthly for measures | 1–18 mo (mean 4.7 ± 0.2) | X | X | ||||||||
| Hung et al. (2012) | ≥ 3 | 6 high-intensity (hold 10 s and rest 10 s) | 4 mo | X | X | |||||||||
| Kim et al. (2007) | ≥ 2 for follow up | 2–3 sets | 30 for follow up | 2 then monthlyc | 20a | 60 | 12 wkd | X | X | X | X | Fitness exercises | ||
| Nystrom et al. (2018) | 3 | 6 basic + 6 advance | X | 3 mo | X | X | App-based + Knack | |||||||
| Segal et al. (2016) | 2 | 1–7 | 1/two wks | 3 | X | 16 wk | X | X | FemiScan trainer device | |||||
| Sun et al. (2018) | 3 | 10 slow + 3–4 fasta | 20 | 2 | 20 | 6–8 wk | X | X | X | Biofeedback + electrical stimulatione | ||||
| Theofrastous et al. (2002) | 2 | 5 quick + 10–20 sustained | 1 × 4 wks | 30 | X | 12 wk | X | X | X | Biofeedback | ||||
| Mechanism 2. Maximized awareness of timing | ||||||||||||||
| Cammu et al. (2000)f | As frequently as possible + Knack | 2 | 20 | 30 | X | 10 wk | X | X | X | |||||
| Junginger et al. (2014) | Engage precontraction into daily life | Median 2 (1–6) for study period | ?g | 15–90 (total 60–240) | 4–6 wkh | X | X | X | Perineal ultrasound | |||||
Blank cells = information was not appliable or not available. Articles retained from search results (n = 13 including 11 for enhanced PFM strength mechanism and 2 for maximized awareness of timing mechanism). This table focuses on tabulation in readiness of integration of information for critical analysis of the general quality of studies on PFMT to treat urinary incontinence, while also testing for theorized mechanism/s of effect
PFMT, pelvic floor muscle training; PFM, pelvic floor muscle; mo, month; wk, week; TrA, transversus abdominis
aPerformed in supine, sitting, and standing positions with legs apart
bFollow up at 3 months and 6 months
cAdded 2 times 60-min exercise sessions plus fitness exercises for 12 weeks and then monthly for 12 months
dFollow up at 12 months
eFor women with two times incontinence after completed basic training or with week strength for active training
fA 10-year PFMT follow up article was also found in the main PFMT strengthening theory literature search, but it was not included in the analysis of results for the main PFMT strengthening theory since it did not report PFM strength and had no statistical analysis of correlation between changes in PFM strength and incontinence
gTrA precontraction + Knack + urge strategies, number of contractions was not clear from the article
hFollow up at 1 to 16 months (median 7, mean 7.6)
Mechanism 2. Maximized awareness of timing
The two studies included in the review had small sample sizes and applied maximized awareness of timing as well as enhanced PFM strength in operationalizing the PFMT programs (Tables 1, 2). One [26] studied 45 women with SUI and used vaginal palpation to correct PFM contractions. Another one [27] studied 55 women who had MUI, SUI or overactive bladder and used both vaginal palpation and perineal ultrasound to evaluate pelvic floor dysfunction and perineal ultrasound was also used to ensure bladder neck effective PFM contractions. Neither reported PFM strength. Both studies described that women gained PFM skill in voluntarily contracting the PFM or improved PFM function and also found self-reported improvement of UI and success for some women.
Both articles provided indirect evidence for the theorized mechanism of maximized awareness of timing (Table 3) based on different measures (Tables 2, 4). In both articles [26, 27], frequency of application of maximized awareness was described as being related to success in terms of improved continence and treatment satisfaction. However, that relationship was not significant in one article [26] and only weakly moderate in another [27]. The latter found maximized awareness frequency of use was only minimally correlated with patient satisfaction with PFMT (rho = − 0.36, p = 0.006).
Both studies involved using the Knack in daily life to treat UI although the PFMT regimens were different. Details of the Knack combined with PFMT regimen used in the two studies are described in Table 5 and Additional file 3: Supplementary B.
Mechanism 3. Strengthened core muscles
As shown in Fig. 2, all articles were excluded during full text review because they did not have analytic data linking mechanism and PFMT outcome. Thus, there were no articles reporting data on the purported mechanism of strengthened core muscle.
PFM tear as a moderating variable
No studies evaluated PFM tears.
Discussion
The overall findings from this review are concerning. Results show that the state of the science has a near complete lack of evidence to support or refute the three purported mechanisms through which PFMT interventions are believed to work (Fig. 1). Analytic parameters used to examine the association varied in the reviewed studies. Almost all of the studies reported no or weak associations.
Respectively, less than 5%, less than 1% and 0% of articles provided confirmation for enhanced PFM strength, maximized awareness of timing, or strengthened core muscles as the purported mechanism of PFMT interventions. Thus, the overall finding is that because theorized mechanisms are not properly investigated, these mechanisms are largely assumed to be operating, rather than empirically shown to be responsible for intervention effects. Assumptions about how interventions are efficacious/effective need further testing. Our findings are comparable to a similar state of the literature as reviewed by Wells (1990) revealing 22 articles dating from 1952 to 1988, and concluding “the research data is limited in … quality of design, and extent of reporting” [14].
Although the mechanism of urgency differs from SUI, findings from our review may raise awareness for how the treatments for urgency work. Urge suppression strategy (Quick squeezing) is considered effective to reduce the feeling of urgency by quick contracting PFM and relaxing the bladder (diminish bladder detrusor muscle activation). To study the association between changes in PFM strength or how fast the PFM will be activated and change of the occurrence rates of urgency might provide some information to discover the underlying mechanisms of using the quick squeezing strategy to diminish urgency. Additional moderating variables, such as women with conditions such as diabetes and age should be considered along with the moderating variable of a tear highlighted in this review, since all of these conditions may influence the effectiveness of the quick squeezing.
Lack of empirical support for theorized mechanisms
Most studies were underpowered for the association analysis. The studies with larger study samples reported weak significant associations, while the largest [25] and smallest [16] samples did not find significant associations. Future studies need to be designed so they are appropriately powered to directly test the association between changes in factors considered as the mechanism of interest and change in UI outcomes within and across subgroups. Future studies should include reporting of not only the average effect of the treatment, but also responders to PFMT, and associations related to purported mechanisms while controlling factors, such as sample size and age.
A majority of the reviewed studies used correlation coefficients that estimate the monotonic association between the changes in PFM strength and UI. No studies evaluated variations in the strength of the association between strength/skill and UI according to age, clinical condition, etc.
We emphasize that evaluating potential moderating variables can help determine which individuals are best able to achieve the mechanistic goals. For example, since PFM function declines with age [28], the age of the sample could affect the association between strength or skill and changes in UI. Certainly striated muscle in older women can be strength trained [29], but these muscles may never reach the strength of younger women because of the age-related loss of large diameter motoneurons and their associated large diameter muscle fibers. Future studies should apply scatterplots to graph the association between changes of PFMT strength and UI and multiple analytic parameters such as correlation coefficients and multiple regression models controlling covariates to examine the association.
Study measures to test theorized mechanism were highly variable, subject to examiner influences, and of questionable and varying validity. These review findings are aligned with findings from another review [30] reporting lack of validity and reproducibility when using the Oxford Grading scale to measure PFM strength. For example, PFM strength measures were contaminated by intraabdominal pressure when measuring during effort at PFM contraction.
There is a lack of reliable measures of PFM strength at all within in-clinic practices. One previous review found that most PFMT studies failed to measure the treatment outcomes [14]. For instance, work on the issue of crosstalk from changes in intraabdominal pressure on measurements of PFM strength is decades long but while newer instruments have solved the problem through clever design, these improved instruments are not readily available in the clinic setting. This example, as well as many others that could be provided, highlight that without accurate, reproducible and reliable measures, lead one to the conclusion that it is presently simply not possible to evaluate the theorized underlying mechanisms.
PFMT regimens were highly variable, interfering with synthesis across studies. This heterogeneity makes it impossible to deduce which regimen(s) produce(s) the strongest evidence for a purported mechanism to treat UI. Regimens varied enormously with, astoundingly, no two studies from the literature reporting the same regimen despite commonality in underlying purported mechanism for building the PFMT program.
It has been previously reported that although almost all studies use either therapist supervision, intensive exercises, gradually increasing training load, or device-assisted training to ensure a woman contracts the correct muscles, almost all studies rate compliance to PFMT, but no one training regimen stands out from all the rest in terms of efficacy [31]. Three studies [18, 20, 21] had PFMT regimens with exercise at least three times per day with a minimum of two non-consecutive days per week, with one set of 8 to 12 maximum contractions reported significant associations. These PFMT regimens are consistent with the resistance training recommended by the American College of Sports Medicine [32]. Further studies should evaluate the theorized mechanisms of PFMT interventions and may design their PFMT interventions following the recommendation.
Skill of maximizing awareness of timing developed during PFM strength training
Despite weak correlation or no correlation between changes in strength and incontinence, continence status improved. What could the underlying mechanism be for this effect? One might speculate that if a woman can maintain a certain degree of urethral closure pressure; she may be able to maintain continence if not too physically active. Thus, increasing PFM strength may not be necessary if women already have adequate PFM strength (the degree has not been identified to date). Being able to reliably recruit the urethral closure muscles to increase urethral closure pressure during those times of need when a woman anticipates urine leakage may suffice to manage leakage. Unfortunately, studies did not consider or evaluate this or any other alternative mechanisms.
Though PFM strengthening per se is not a goal of PFMT for timely contraction, it is possible that by learning the skill and habit of consciously activating the PFM at a moment of risk for leakage, the muscle over time may gain strength related to the new habit of timely contraction.
Voluntary PFM contraction during coughing can be trained and the reaction time of the contraction was improved via a 12-week PFMT program [33] or a 2-week cognitive rehabilitation (dual-task method) [34]. This might have led to urethral striated muscle hypertrophy, but we found no study that tested for the association of maximized awareness of timely contraction skill and either increased PFM strength or increased volitional urethral closure pressure.
There is evidence that urethral closure pressure may be enhanced in the moment of effort to contract the PFM [7, 35], and that urethral sphincteric hypertrophy which occurred with PFM strength training may be bolstered by maximized awareness of timely contraction training [36]. An earlier study [37] also demonstrated that even with complete bilateral tears of the “Kegel” muscles, activation of the urethral striated muscle was demonstrable in most women, though with less of a urethral closure pressure rise compared to women with intact PFM muscles. Pragmatically, women’s ability to feel and volitionally contract the small urethral striated muscle in isolation of the larger PFM has not been well demonstrated.
Potential impact of a PFM tear on theorized mechanisms
None of the articles evaluated birth-related nonrepairable tears of the critical urethral support provided by the pubovisceral portion of the levator ani muscle (also referred to as Kegel muscle, pubococcygeal muscles, generally PFM). Such tears were suspected as early as 1943 [38] and irrefutable evidence suggests they are permanent [12].
Suggested psychometrically sound methods to diagnose PFM tear include various clinical appraisal estimates using one or more fingers for palpatory assessment, MRI, and three- or four-dimensional (3D or 4D) ultrasound for imaging assessment [38–46]. Importantly, though PFMT targets this very muscle whether women had a tear was not assessed in any of the articles. For these women, PFMT may strengthen the urethral striated muscle as an alternative mechanism explaining its effects on UI.
More evidence is needed, particularly given that 5% to 15% of women who have delivered vaginally have at least a partial tear of the pubovisceral muscle origin at the pubic bone [12, 41, 47]. In addition, our previous study found that postpartum women with PFM tears were more likely to have lower urethral closure pressure during Kegel exercises [48]. More research is needed to account for the effect of PFM tear(s) on theorized mechanisms as well as its effects of PFMT on reducing UI.
Strengths and limitations
There are both strengths and weaknesses to our approach. The weaknesses include the fact that the databases searched were selected based on best match per guidance from a professional librarian specializing in instruction; however, the search was not fully exhaustive. Restriction to the English language may have excluded studies that might otherwise have offered unique and important data. Similarly, the exclusion of the grey literature may have meant we missed some articles.
This study focused on examining the PFMT literature for its robustness regarding the theoretical mechanisms underlying formation of the programs. Our findings of major gaps should not be misinterpreted as denigrating PFMT for it is well established that PFMT, in its many forms, can work for many women. Rather, our results call for research that is dedicated to better understanding theorized mechanisms to improve efficacy—in other words, we need greater understanding of why PFMT works.
Our literature review differs from others in the field of PFMT in its organization and focus on theoretical mechanisms. Our authorship includes experts in both PFMT mechanisms and interventions for pelvic floor disorders. Questions raised by the findings and implications for additional research lead to the suggestion that future investigators (1) report the theory base of their specific PFMT program, and (2) measure the constructs implied by the theory (e.g., PFM strength change) with psychometrically sound instruments.
Once this work is accomplished, cost-effective and time efficient treatment can become more of the norm. It may be time for an adaptive or even smart trial design to be used to identify how best to personalize PFMT in order to optimize a women’s outcomes by applying the theory-driven PFMT program most appropriate to her unique situation.
Conclusions
Explicit theories for guiding PFMT research and practice are available in the literature, but statistical analyses for testing these purported theoretical mechanistic links with PFMT outcomes, to explain why some women respond and others do not, are largely absent. Future studies should explicitly state the theoretical basis guiding the work, which components of the theory are being tested, and the statistical analysis used to confirm the mechanism underlying the intervention-outcomes relationship, with attention paid to important potentially moderating variables, such as whether the levator ani is intact, age, and other important demographics. Only then can a better understanding of the mechanisms underlying PFMT for improving continence status be obtained.
Supplementary Information
Additional file 1. Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews checklist.
Additional file 2. Search strategies in PubMed and ClinicalTrials.gov for enhanced pelvic floor muscle strength mechanism.
Additional file 3.Measurement issues and pelvic floor muscle training regimens.
Acknowledgements
The authors would like to thank the authors and publishers of the original studies. Authors presented partial results from this review (PFM strengthening theory) at the American Urogynecologic Society and the International Urogynecological Associations Joint Scientific Meeting on September 24-28, 2019, in Nashville, TN.
Abbreviations
- UI
Urinary incontinence
- PFMT
Pelvic floor muscle training
- SUI
Stress urinary incontinence
- UUI
Urge urinary incontinence
- MUI
Mixed urinary incontinence
- PFM
Pelvic floor muscles
- TrA
Transversus abdominis
- PRISMA-ScR
Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews
- CINAHL
Cumulative Index to Nursing and Allied Health Literature
Author contributions
YS, JSC, JAAM, and JMM made substantial contributions to project development and manuscript writing/editing; YS, JSC, and JMM conducted and revised the literature search, assessed the studies, extracts, and analyzed and interpreted the data. All authors have participated in writing and revising the manuscript. All authors read and approved the final manuscript.
Funding
Dr. Sheng received support as a postdoctoral fellow under 5T32CA117865 Interdisciplinary Training in Behavioral Oncology (V. Champion, PI) and as a Dean’s Enhancing Diversity in Nursing Science Postdoctoral Scholar. Dr. Ashton-Miller was supported by PHS grants 1 RC2 DK122379-01 and P30 AG 024824. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Availability of data materials
The datasets used and/or analyzed during the current study are available from the corresponding authors on reasonable request.
Declarations
Ethics approval and consent to participate
Ethics approval was not needed for this review.
Consent to publish
Not applicable.
Competing interests
YS and JMM have no conflict of interest. JSC reports personal fees from RoundGlass Inc. and Kappa Santé. JAAM reports institutional research grants from Hologic, Procter & Gamble and Materna Medical.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21(1):5–26. doi: 10.1007/s00192-009-0976-9. [DOI] [PubMed] [Google Scholar]
- 2.Buckley BS, Lapitan MCM. Prevalence of urinary incontinence in men, women, and children—current evidence: findings of the Fourth International Consultation on Incontinence. Urology. 2010;76(2):265–270. doi: 10.1016/j.urology.2009.11.078. [DOI] [PubMed] [Google Scholar]
- 3.Milsom I, Gyhagen M. The prevalence of urinary incontinence. Climacteric. 2019;22(3):217–222. doi: 10.1080/13697137.2018.1543263. [DOI] [PubMed] [Google Scholar]
- 4.Dumoulin C, Cacciari LP, Hay-Smith EJC. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev. 2018;10(10):CD005654. doi: 10.1002/14651858.CD005654.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lamin E, Parrillo LM, Newman DK, Smith AL. Pelvic floor muscle training: underutilization in the USA. Curr Urol Rep. 2016;17(2):10. doi: 10.1007/s11934-015-0572-0. [DOI] [PubMed] [Google Scholar]
- 6.Bø K. Pelvic floor muscle training is effective in treatment of female stress urinary incontinence, but how does it work? Int Urogynecol J. 2004;15(2):76–84. doi: 10.1007/s00192-004-1125-0. [DOI] [PubMed] [Google Scholar]
- 7.Miller JM, Ashton-Miller JA, DeLancey JO. A pelvic muscle precontraction can reduce cough-related urine loss in selected women with mild SUI. J Am Geriatr Soc. 1998;46(7):870–874. doi: 10.1111/j.1532-5415.1998.tb02721.x. [DOI] [PubMed] [Google Scholar]
- 8.Sapsford RR, Hodges PW, Richardson CA, Cooper DH, Markwell SJ, Jull GA. Co-activation of the abdominal and pelvic floor muscles during voluntary exercises. Neurourol Urodyn. 2001;20(1):31–42. doi: 10.1002/1520-6777(2001)20:1<31::aid-nau5>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 9.Neumann PB, Grimmer KA, Deenadayalan Y. Pelvic floor muscle training and adjunctive therapies for the treatment of stress urinary incontinence in women: a systematic review. BMC Womens Health. 2006;6(1):11. doi: 10.1186/1472-6874-6-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ashton-Miller JA, Delancey JO. On the biomechanics of vaginal birth and common sequelae. Annu Rev Biomed Eng. 2009;11:163–176. doi: 10.1146/annurev-bioeng-061008-124823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dietz HP, Shek C. Levator avulsion and grading of pelvic floor muscle strength. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(5):633–636. doi: 10.1007/s00192-007-0491-9. [DOI] [PubMed] [Google Scholar]
- 12.Miller JM, Low LK, Zielinski R, Smith AR, DeLancey JO, Brandon C. Evaluating maternal recovery from labor and delivery: bone and levator ani injuries. Am J Obstet Gynecol. 2015;213(2):188.e1–e11. doi: 10.1016/j.ajog.2015.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 14.Wells TJ. Pelvic (floor) muscle exercise. J Am Geriatr Soc. 1990;38(3):333–337. doi: 10.1111/j.1532-5415.1990.tb03515.x. [DOI] [PubMed] [Google Scholar]
- 15.Bø K. Pelvic floor muscle strength and response to pelvic floor muscle training for stress urinary incontinence. Neurourol Urodyn. 2003;22(7):654–658. doi: 10.1002/nau.10153. [DOI] [PubMed] [Google Scholar]
- 16.Dinc A, Kizilkaya Beji N, Yalcin O. Effect of pelvic floor muscle exercises in the treatment of urinary incontinence during pregnancy and the postpartum period. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(10):1223–1231. doi: 10.1007/s00192-009-0929-3. [DOI] [PubMed] [Google Scholar]
- 17.Dougherty M, Bishop K, Mooney R, Gimotty P, Williams B. Graded pelvic muscle exercise: effect on stress urinary incontinence. J Reprod Med. 1993;38(9):684–91. [PubMed] [Google Scholar]
- 18.Hung HC, Chih SY, Lin HH, Tsauo JY. Exercise adherence to pelvic floor muscle strengthening is not a significant predictor of symptom reduction for women with urinary incontinence. Arch Phys Med Rehabil. 2012;93(10):1795–1800. doi: 10.1016/j.apmr.2012.03.010. [DOI] [PubMed] [Google Scholar]
- 19.Kim H, Suzuki T, Yoshida Y, Yoshida H. Effectiveness of multidimensional exercises for the treatment of stress urinary incontinence in elderly community-dwelling Japanese women: a randomized, controlled, crossover trial. J Am Geriatr Soc. 2007;55(12):1932–1939. doi: 10.1111/j.1532-5415.2007.01447.x. [DOI] [PubMed] [Google Scholar]
- 20.Nystrom E, Antonio FI, Brito LGO, Ferreira CHJ, Nystrom E. Treatment of stress urinary incontinence with a mobile app: factors associated with success. Physiother Theory Pract. 2018;29(9):1325–1333. doi: 10.1007/s00192-017-3514-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Theofrastous JP, Wyman JF, Bump RC, McClish DK, Elser DM, Bland DR, et al. Effects of pelvic floor muscle training on strength and predictors of response in the treatment of urinary incontinence. Neurourol Urodyn. 2002;21(5):486–490. doi: 10.1002/nau.10021. [DOI] [PubMed] [Google Scholar]
- 22.Burns PA, Pranikoff K, Nochajski TH, Hadley EC, Levy KJ, Ory MG. A comparison of effectiveness of biofeedback and pelvic muscle exercise treatment of stress incontinence in older community-dwelling women. J Gerontol. 1993;48(4):M167–M174. doi: 10.1093/geronj/48.4.m167. [DOI] [PubMed] [Google Scholar]
- 23.Hahn I, Milsom I, Fall M, Ekelund P. Long-term results of pelvic floor training in female stress urinary incontinence. Br J Urol. 1993;72:421–427. doi: 10.1111/j.1464-410x.1993.tb16170.x. [DOI] [PubMed] [Google Scholar]
- 24.Sun Z-J, Zhu L, Liang M-L, Xu T, Lang J-H. Comparison of outcomes between postpartum and non-postpartum women with stress urinary incontinence treated with conservative therapy: a prospective cohort study. Neurourol Urodyn. 2018;37:1426–1433. doi: 10.1002/nau.23464. [DOI] [PubMed] [Google Scholar]
- 25.Segal S, Morse A, Sangal P, Hirsch N, Kohli N. Efficacy of FemiScan pelvic floor therapy for the treatment of urinary incontinence. Female Pelvic Med Reconstr Surg. 2016;22(6):433–437. doi: 10.1097/SPV.0000000000000307. [DOI] [PubMed] [Google Scholar]
- 26.Cammu H, Van Nylen M, Amy JJ. A 10-year follow-up after Kegel pelvic floor muscle exercises for genuine stress incontinence. BJU Int. 2000;85(6):655–658. doi: 10.1046/j.1464-410x.2000.00506.x. [DOI] [PubMed] [Google Scholar]
- 27.Junginger B, Seibt E, Baessler K. Bladder-neck effective, integrative pelvic floor rehabilitation program: follow-up investigation. Eur J Obstet Gynecol Reprod Biol. 2014;174:150–153. doi: 10.1016/j.ejogrb.2013.12.022. [DOI] [PubMed] [Google Scholar]
- 28.Pfisterer MHD, Griffiths DJ, Schaefer P, Resnick NM. The effect of age on lower urinary tract function: a study in women. J Am Geriatr Soc. 2006;54(3):405–12. doi: 10.1111/j.1532-5415.2005.00613.x. [DOI] [PubMed] [Google Scholar]
- 29.Claflin DR, Larkin LM, Cederna PS, Horowitz JF, Alexander NB, Cole NM, et al. Effects of high-and low-velocity resistance training on the contractile properties of skeletal muscle fibers from young and older humans. J Appl Physiol. 2011;111(4):1021–1030. doi: 10.1152/japplphysiol.01119.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rocha F, Carvalho J, Jorge Natal R, Viana R. Evaluation of the pelvic floor muscles training in older women with urinary incontinence: a systematic review. Porto Biomed J. 2018;3(2):e9. doi: 10.1016/j.pbj.0000000000000009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dumoulin C, Glazener C, Jenkinson D. Determining the optimal pelvic floor muscle training regimen for women with stress urinary incontinence. Neurourol Urodyn. 2011;30(5):746–753. doi: 10.1002/nau.21104. [DOI] [PubMed] [Google Scholar]
- 32.Westcott W. ACSM strength training guidelines: role in body composition and health enhancement. ACSMs Health Fit J. 2009;13(4):14. [Google Scholar]
- 33.Madill SJ, Pontbriand-Drolet S, Tang A, Dumoulin C. Effects of PFM rehabilitation on PFM function and morphology in older women. Neurourol Urodyn. 2013;32(8):1086–1095. doi: 10.1002/nau.22370. [DOI] [PubMed] [Google Scholar]
- 34.Villot A, Deffieux X, Billecocq S, Auclair L, Amarenco G, Thubert T. Influence of cognitive rehabilitation on pelvic floor muscle contraction: a randomized controlled trial. Neurourol Urodyn. 2017;36(6):1636–1644. doi: 10.1002/nau.23169. [DOI] [PubMed] [Google Scholar]
- 35.Miller JM, Sampselle C, Ashton-Miller J, Hong GR, DeLancey JO. Clarification and confirmation of the Knack maneuver: the effect of volitional pelvic floor muscle contraction to preempt expected stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(6):773–782. doi: 10.1007/s00192-007-0525-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Madill SJ, Pontbriand-Drolet S, Tang A, Dumoulin C. Changes in urethral sphincter size following rehabilitation in older women with stress urinary incontinence. Int Urogynecol J. 2015;26(2):277–283. doi: 10.1007/s00192-014-2507-6. [DOI] [PubMed] [Google Scholar]
- 37.Miller JM, Umek WH, Delancey JOL, Ashton-Miller JA. Can women without visible pubococcygeal muscle in MR images still increase urethral closure pressures? Am J Obstet Gynecol. 2004;191(1):171–175. doi: 10.1016/j.ajog.2004.03.082. [DOI] [PubMed] [Google Scholar]
- 38.Gainey HL. Postpartum observation of pelvic tissue damage. Am J Obstet Gynecol. 1943;45:457–466. doi: 10.1016/s0002-9378(16)37836-x. [DOI] [PubMed] [Google Scholar]
- 39.Sheng Y, Low LK, Liu X, Ashton-Miller JA, Miller JM. Association of index finger palpatory assessment of pubovisceral muscle body integrity with MRI-documented tear. Neurourol Urodyn. 2019;38(4):1120–1128. doi: 10.1002/nau.23967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gainey HL. Postpartum observation of pelvic tissue damage: further studies. Am J Obstet Gynecol. 1955;70:800–807. doi: 10.1016/s0002-9378(16)37836-x. [DOI] [PubMed] [Google Scholar]
- 41.DeLancey JOL, Kearney R, Chou Q, Speights S, Binno S. The appearance of levator ani muscle abnormalities in magnetic resonance images after vaginal delivery. Obstet Gynecol. 2003;101(1):46–53. doi: 10.1016/s0029-7844(02)02465-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dietz HP, Steensma AB. The prevalence of major abnormalities of the levator ani in urogynaecological patients. BJOG. 2006;113(2):225–230. doi: 10.1111/j.1471-0528.2006.00819.x. [DOI] [PubMed] [Google Scholar]
- 43.Kearney R, Miller JM, Delancey JO. Interrater reliability and physical examination of the pubovisceral portion of the levator ani muscle, validity comparisons using MR imaging. Neurourol Urodyn. 2006;25(1):50–54. doi: 10.1002/nau.20181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dietz HP, Shek C. Validity and reproducibility of the digital detection of levator trauma. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(8):1097–1101. doi: 10.1007/s00192-008-0575-1. [DOI] [PubMed] [Google Scholar]
- 45.Morgan DM, Umek W, Stein T, Hsu Y, Guire K, DeLancey JOL. Interrater reliability of assessing levator ani muscle defects with magnetic resonance images. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(7):773–778. doi: 10.1007/s00192-006-0224-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lammers K, Kluivers KB, Vierhout ME, Prokop M, Fütterer JJ. Inter- and intraobserver reliability for diagnosing levator ani changes on magnetic resonance imaging. Ultrasound Obstet Gynecol. 2013;42(3):347–352. doi: 10.1002/uog.12462. [DOI] [PubMed] [Google Scholar]
- 47.Schwertner-Tiepelmann N, Thakar R, Sultan AH, Tunn R. Obstetric levator ani muscle injuries: current status. Ultrasound Obstet Gynecol. 2012;39(4):372–383. doi: 10.1002/uog.11080. [DOI] [PubMed] [Google Scholar]
- 48.Sheng Y, Liu X, Low LK, Ashton-Miller JA, Miller JM. Association of pubovisceral muscle tear with functional capacity of urethral closure: evaluating maternal recovery from labor and delivery. Am J Obstet Gynecol. 2020;222(6):598.e1–e7. doi: 10.1016/j.ajog.2019.11.1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Navarro Brazález B, Torres Lacomba M, de la Villa P, Sánchez Sánchez B, Prieto Gómez V, Asúnsolo Del Barco Á, et al. The evaluation of pelvic floor muscle strength in women with pelvic floor dysfunction: a reliability and correlation study. Neurourol Urodyn. 2018;37(1):269–277. doi: 10.1002/nau.23287. [DOI] [PubMed] [Google Scholar]
- 50.Laycock J, Jerwood D. Pelvic floor muscle assessment: the PERFECT scheme. Physiotherapy. 2001;87(12):631–642. [Google Scholar]
- 51.Devreese A, Staes F, De Weerdt W, Feys H, Van Assche A, Penninckx F, et al. Clinical evaluation of pelvic floor muscle function in continent and incontinent women. Neurourol Urodyn. 2004;23(3):190–197. doi: 10.1002/nau.20018. [DOI] [PubMed] [Google Scholar]
- 52.Bø K, Finckenhagen HB. Vaginal palpation of pelvic floor muscle strength: inter-test reproducibility and comparison between palpation and vaginal squeeze pressure. Acta Obstet Gynecol Scand. 2001;80(10):883–887. doi: 10.1034/j.1600-0412.2001.801003.x. [DOI] [PubMed] [Google Scholar]
- 53.Ferreira CH, Barbosa PB, de Oliveira SF, Antônio FI, Franco MM, Bø K. Inter-rater reliability study of the modified Oxford Grading Scale and the Peritron manometer. Physiotherapy. 2011;97(2):132–138. doi: 10.1016/j.physio.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 54.Ribeiro Jdos S, Guirro EC, Franco Mde M, Duarte TB, Pomini JM, Ferreira CH. Inter-rater reliability study of the Peritron™ perineometer in pregnant women. Physiother Theory Pract. 2016;32(3):209–217. doi: 10.3109/09593985.2015.1129654. [DOI] [PubMed] [Google Scholar]
- 55.Isherwood PJ, Rane A. Comparative assessment of pelvic floor strength using a perineometer and digital examination. BJOG. 2000;107(8):1007–1011. doi: 10.1111/j.1471-0528.2000.tb10404.x. [DOI] [PubMed] [Google Scholar]
- 56.Dougherty M, Abrams R, McKey PL. An instrument to assess the dynamic characteristics of the circumvaginal musculature. Nurs Res. 1986;35(4):202–206. [PubMed] [Google Scholar]
- 57.Bø K, Kvarstein B, Hagen RR, Larsen S. Pelvic floor muscle exercise for the treatment of female stress urinary incontinence: II—validity of vaginal pressure measurements of pelvic floor muscle strength and the necessity of supplementary methods for control of correct contraction. Neurourol Urodyn. 1990;9(5):479–87. [Google Scholar]
- 58.Thelen DG, Schultz AB, Fassois SD, Ashton-Miller JA. Identification of dynamic myoelectric signal-to-force models during isometric lumbar muscle contractions. J Biomech. 1994;27(7):907–919. doi: 10.1016/0021-9290(94)90263-1. [DOI] [PubMed] [Google Scholar]
- 59.Thorp JM, Jr, Bowes WA, Jr, Droegemueller W, Wicker H. Assessment of perineal floor function: electromyography with acrylic plug surface electrodes in nulliparous women. Obstet Gynecol. 1991;78(1):89–92. [PubMed] [Google Scholar]
- 60.Fowler C, Benson J, Craggs M, Vodusek D, Yang C, Podnar S. Clinical neurophysiology. In: Abrams P, Cardozo L, Khoury S, Wein A, editors. Incontinence. Plymouth: Plymbridge Distributors Ltd.; 2002. pp. 389–424. [Google Scholar]
- 61.Peschers UM, Gingelmaier A, Jundt K, Leib B, Dimpfl T. Evaluation of pelvic floor muscle strength using four different techniques. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(1):27–30. doi: 10.1007/s001920170090. [DOI] [PubMed] [Google Scholar]
- 62.Armstrong SM, Miller JM, Benson K, Jain S, Panagopoulos K, DeLancey JOL, et al. Revisiting reliability of quantified perineal ultrasound: Bland and Altman analysis of a new protocol for the rectangular coordinate method. Neurourol Urodyn. 2006;25(7):731–738. doi: 10.1002/nau.20299. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews checklist.
Additional file 2. Search strategies in PubMed and ClinicalTrials.gov for enhanced pelvic floor muscle strength mechanism.
Additional file 3.Measurement issues and pelvic floor muscle training regimens.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding authors on reasonable request.