Abstract
Laryngeal tuberculosis is rare despite its close anatomical and physiological proximity to the lungs. It constitutes less than 1% of extrapulmonary tuberculosis. The symptoms of laryngeal tuberculosis are non-specific and mimic other laryngeal pathologies. The recent evolving and atypical endoscopic laryngeal features cause a diagnostic dilemma and delay in treatment. In this report, we presented three patients with distinct age and medical history, and hoarseness. Flexible videolaryngoscopy showed similar findings in the three cases, with irregular mucosa involving the entire length of the vocal fold, unilaterally in two cases and bilaterally in one. Mucosal waves were typically absent on laryngostroboscopy examination. The routine workup for pulmonary tuberculosis was unremarkable. The usage of Mycobacterium tuberculosis complex (MTBC) and rifampicin resistance (Xpert MTB/RIF) assay that detects Mycobacterium tuberculosis in the tissue biopsy specimens has helped in the rapid diagnosis of primary laryngeal tuberculosis and timely commencement of anti-tuberculous therapy. The clinical course and response to treatment were diverse in which two cases showed good response whilst the third developed disseminated tuberculosis despite optimal therapy.
Keywords: Dysphonia, hoarseness, laryngeal tuberculosis, mycobacterium, stroboscopy, case report
Introduction
Primary laryngeal tuberculosis (PLTB) without pulmonary involvement is rare and merely constitutes <1% of extrapulmonary tuberculosis cases (1). It is postulated that PLTB occurs as a result of the direct invasion of the larynx by inhaled mycobacteria, rather than ascending infection from the lower airways (1). Other possible routes of laryngeal infection are via hematogenous or lymphatic spread. The morphological appearance of PLTB was described as ulcerative, polypoid, granulomatous, and nonspecific lesions (2). However, in the authors’ experience, patients with early PLTB presenting with endoscopic findings of irregular mucosa of the true vocal fold has never been described in the literature. Hereby the authors present three PLTB cases together with their laryngoscopic images which depicted similar findings but with contrasting clinical outcomes.
Case Presentation
Case 1: A 31-year-old female presented with worsening hoarseness accompanied by voice fatigue and irritative dry cough for one month. Otherwise, she had no shortness of breath, dysphagia, laryngopharyngeal reflux (LPR) or constitutional symptoms. She was not immunocompromised and had no history of close contact with patients who had pulmonary tuberculosis (PTB). On examination, she had hoarseness at a GRBAS score of G2R1B2A1S1 (G, overall dysphonia; R, roughness; B, breathiness; A, asthenia; and S, strain), the main component being breathiness. The maximum phonation time (MPT) was seven seconds. There was no stridor or signs of respiratory distress. Videoendoscopy and laryngostroboscopy (Pentax Medical, Japan & US) examination showed irregular mucosa involving the entire length of the right vocal fold with absent mucosal wave (Figure 1). Otherwise, the mobility of both vocal folds was normal and symmetrical, and the glottic airway was patent. Infective and inflammatory markers such as total white cell count (TWC) and total erythrocyte sedimentation rate (ESR) were normal. Other routine tuberculosis workups such as sputum for acid-fast bacilli (AFB) smear, chest radiograph and Mantoux test (Tuberculin skin test) were unremarkable. Direct laryngoscopy and examination under general anaesthesia (EUA) revealed irregular mucosa with some cobblestone appearance of the right vocal fold. Endolaryngeal microsurgery (ELMS) and subepithelial incisional biopsy of the right vocal fold lesion with a precision technique was performed using microlaryngeal instruments (Figure 2). The lesion was found confined to the epithelial layer of the vocal fold, sparing the vocal ligament. The incised mucosa was friable and it was sent for a rapid molecular biological diagnostic test to detect Mycobacterium tuberculosis complex (MTBC) and rifampicin resistance (Xpert MTB/RIF assay). The result that was ready in 24 hours revealed positive for MTBC and negative for rifampicin resistance. Anti-tuberculous therapy was commenced immediately. Histopathologic examination (HPE) of the specimen, which was completed two weeks later, reported chronic granulomatous inflammation with negative Ziehl-Neelsen stain. Her hoarseness improved significantly during the two-month follow-up. Repeat laryngostroboscopy showed a return of mucosal wave and resolved mucosal lesion over the affected vocal fold (Figure 3). She continued to improve and completed the anti-tuberculous treatment.
Figure 1.
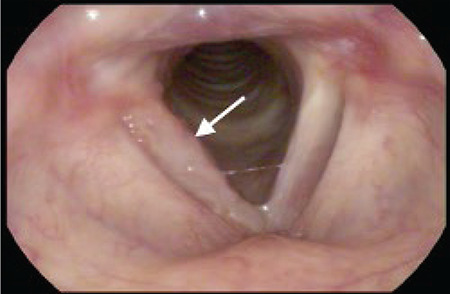
Endoscopic image of Case 1 shows irregular mucosa lesions along the entire length of the right vocal fold with cobblestone appearance (arrow)
Figure 2.
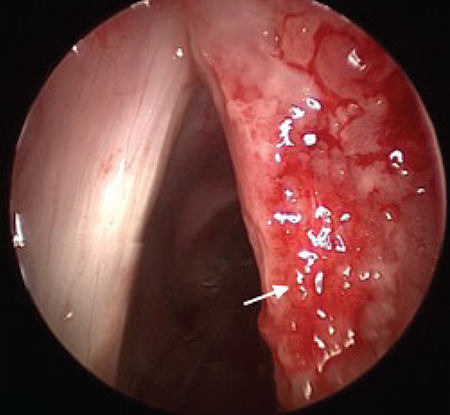
Subepithelial incisional biopsy of the right vocal fold (arrow) was performed under direct laryngoscopy via ELMS, preserving the vocal ligament
ELMS: Endolaryngeal microsurgery
Figure 3.
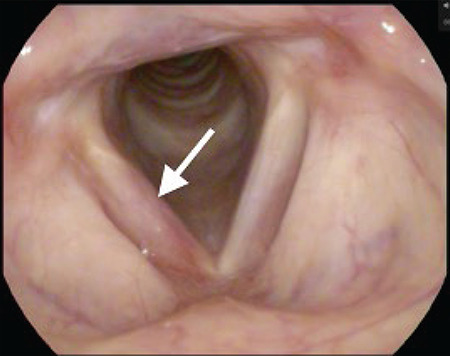
Endoscopic image of Case 1 shows resolved mucosal lesion over the affected vocal fold (arrow) after two months of anti-tuberculous therapy
Case 2: A 70-year-old male, a chronic ex-smoker with underlying hypertension, diabetes mellitus, presented with persistent hoarseness for one-month and preceding dry cough. For the past two years he had LPR symptoms that were treated medically. There was no constitutional symptom or history of contact with PTB patients. On examination, he was identified to have dysphonia with a score of G3R3B0A1S2, with a main component of roughness. MPT was 16 seconds. There was no stridor or palpable cervical lymphadenopathy. Videoendoscopy and laryngostroboscopy revealed findings almost similar to those of Case 1, in which there was irregular mucosa involving the entire length of the right vocal fold with absent mucosal wave (Figure 4). The vocal folds were mobile and the glottic airway was patent. TWC and ESR were not raised and other PTB investigations such as chest radiograph, sputum examination and Mantoux test were unremarkable. Direct laryngoscopy and EUA revealed irregular mucosa with slough on the right vocal fold. Incisional biopsy was taken via ELMS with a precision technique, preserving the vocal ligament (Figure 5). Xpert MTB/RIF assay revealed positive detection of MTBC without rifampicin resistance. He was started on anti-tuberculous therapy right away, but unfortunately developed intolerance to the medication, complicated with acute kidney injury and hepatitis. HPE revealed chronic granulomatous inflammation with necrotic tissue and Langhans type multinucleated giant cells seen (Figure 6). There was no AFB seen on Ziehl-Neelsen stain. Human immunodeficiency virus (HIV) and viral hepatitis screening tests were negative. Two months later the disease progressed and disseminated as he developed PTB with pneumothorax and TB meningitis. He had an acute cardiac event while nursed in the intensive care unit and required tracheostomy due to prolonged ventilation with poor neurological recovery. He was eventually discharged home and dependent on long-term positive pressure ventilation via tracheostomy, making his condition not suitable for reassessment using laryngostroboscopy.
Figure 4.

Endoscopic image of Case 2 shows irregular mucosa lesions along the entire length of the right vocal fold with erythema (arrow)
Figure 5.
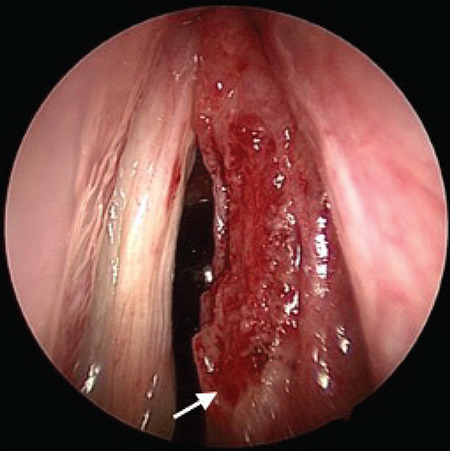
Direct laryngoscopic image shows subepithelial incisional biopsy of the right vocal fold lesion was performed, preserving the vocal ligament
Figure 6.
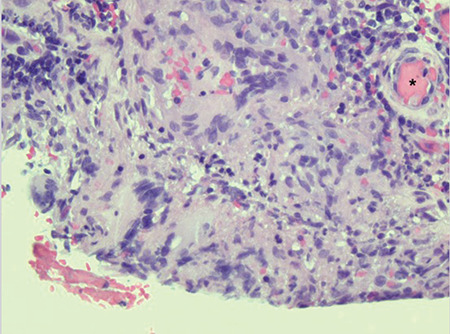
Histopathologic image shows granuloma composed of a collection of epithelioid histiocytes rimmed by lymphocytes and plasma cells with Langhans type multinucleated giant cells (asterisk) (H&E, x400)
H&E: Hematoxylin and eosin stain
Case 3: A 73-year-old male with underlying diabetes mellitus and hypertension, presented with a two-year history of hoarseness worsened over the past six months, associated with poor voice projection. There was no constitutional symptom or history of contact with PTB patients. Examination revealed dysphonia G2R2B0A1S1, with a main component of roughness. MPT was two seconds. There was no stridor or palpable cervical lymph node. Videoendoscopy showed thickened whitish mucosal lesion over the entire length of both vocal folds, without abnormal perpendicular vessels seen. Laryngostroboscopy examination showed an absent mucosal wave bilaterally. Chest radiograph and Mantoux test results were normal. ESR and TWC were not raised. Direct laryngoscopy and EUA showed irregular mucosa and slough on both vocal folds, with cobblestone appearance on its posterior third (Figure 7). Vocal fold lesions were biopsied via ELMS, preserving the vocal ligament. Xpert MTB/RIF assay of the specimen revealed positive detection of MTBC, and treatment was initiated within 24 hours. The result of the histopathologic examination of the biopsy specimen revealed chronic granulomatous inflammation with caseous necrosis. Numerous AFBs were seen on the Ziehl-Neelsen stain (Figure 8). He showed good response to anti-tuberculous therapy. The hoarseness had improved at the one-month follow-up visit. Repeat laryngostroboscopy showed a return of mucosal wave over both vocal folds. Presently he is followed up at another hospital because of logistic reasons.
Figure 7.
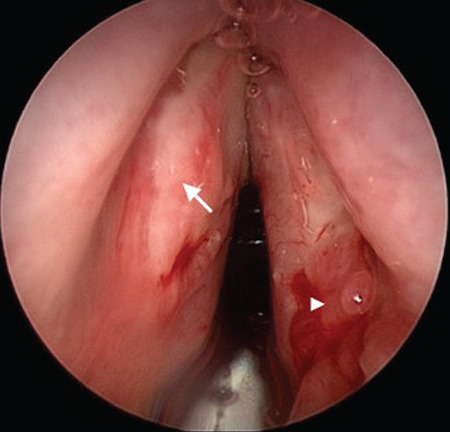
Direct laryngoscopy image of Case 3 shows whitish thickened mucosal lesion over the entire length of left vocal fold (arrow) and cobblestone appearance at the right posterior third (arrowhead)
Figure 8.
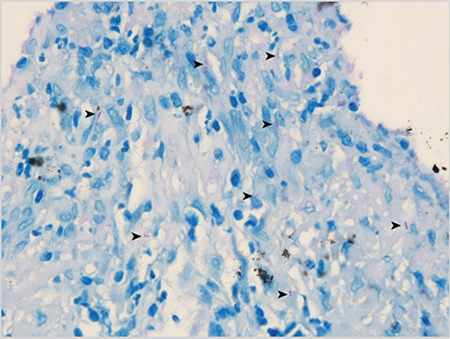
Histopathology image shows acid-fast bacilli (arrowhead) on Ziehl-Neelsen stain (x600)
Discussion
Laryngeal tuberculosis is the most common granulomatous disease of the larynx (1). The incidence of PLTB has increased following the resurgence of tuberculosis globally with a changing trend of clinical manifestations. Primary laryngeal tuberculosis is prevalent in the fifth to sixth decades of life with male predominance. Hoarseness (80%–100%) and odynophagia/dysphagia (55%–100%) are the most common presentations whilst dry cough (11%–45%) and constitutional symptoms are uncommon (3).
The risk factors for PLTB include HIV infection, diabetes mellitus, immunosuppressive therapies, tobacco smoking, alcoholism, drug abuse, malnutrition and poor socioeconomic status (4). In the present case series, the main risk factor was diabetes mellitus, however it was well controlled with medications. None of the three patients had a history of close contact with TB patients or of excessive alcohol use, and their HIV statuses were negative.
PLTB frequently involves the true vocal folds (3, 5, 6). However, the morphological description varies with the preponderance of single exophytic or ulcerative lesion at the vocal fold (67%–73%) (2). Hematogenous spread is associated with polypoid and non-specific lesions. The atypical manifestations that mimic neoplasm, laryngitis and polyp often result in misdiagnosis (3). To the extent of the authors’ experience and knowledge, PLTB presenting as an isolated irregular mucosa at the true vocal fold has not been previously described in the literature. In these cases, videoendoscopy and laryngostroboscopy demonstrate reduced or absent mucosal waves at vocal fold with a non-vibrating segment indicating submucosal invasion, which mimic a malignant tumor (7). Therefore, laryngeal biopsy is crucial to ascertain the diagnosis (5, 6). The intraoperative findings of our cases under direct laryngoscopy showed irregular mucosa lesions involving the entire length of the vocal fold, with cobblestone appearance on the posterior third of the vocal fold and ventricle. The incised mucosa was friable with slough seen, which is not typical of a glottic malignant lesion. Chronic inflammatory disorders such as laryngeal tuberculosis therefore must be excluded in such cases since tuberculosis is endemic in this region. Subepithelial incisional biopsy of the vocal fold lesion was performed using microlaryngeal instruments, preserving the vocal ligament underneath. The specimens were sent for histopathological examination and tuberculous investigations including Mycobacterium culture and Xpert MTB/RIF assay.
The routine workup for PTB, such as chest radiography, sputum examination, Mantoux test and serum ESR is unremarkable in PLTB, as demonstrated in our cases. Conventional chest radiograph remains as the initial imaging modality for pulmonary TB screening. Computed tomography of the thorax is not a routine investigation for PLTB if the chest X-ray shows normal findings (8). PLTB was diagnosed essentially based on tissue biopsy specimens that were sent for histopathological examination and mycobacterial culture. However, only 34% of HPE results of PLTB demonstrated chronic granulomatous inflammation with caseous necrosis, which is pathognomonic of TB (3). In two out of three of our cases, the Ziehl-Neelsen stain on histopathology specimen was negative (Table 1). This finding is consistent with the literature where 40%–100% of the PLTB tissue biopsies were negative for AFB on Ziehl-Neelsen stain due to its paucibacillary nature (9). Standard mycobacterium culture has moderate sensitivity and specificity for extrapulmonary TB and it takes up to six weeks for MTBC to grow (10). In all three of our cases, the diagnosis was inconclusive at the initial stage due to the atypical endoscopic laryngeal features and negative PTB investigations. The treatment could be initiated only when confirmatory result was obtained from HPE or mycobacterial culture. In our center, the finalized HPE report turnaround time is usually two weeks. However, the result of positive Xpert MTB/RIF assay that detects MTB DNA in the biopsy tissue within hours has helped for the rapid definitive diagnosis of PLTB. As a result, it helped to avoid delays in diagnosis and enabled timely commencement of the anti-tuberculous therapy.
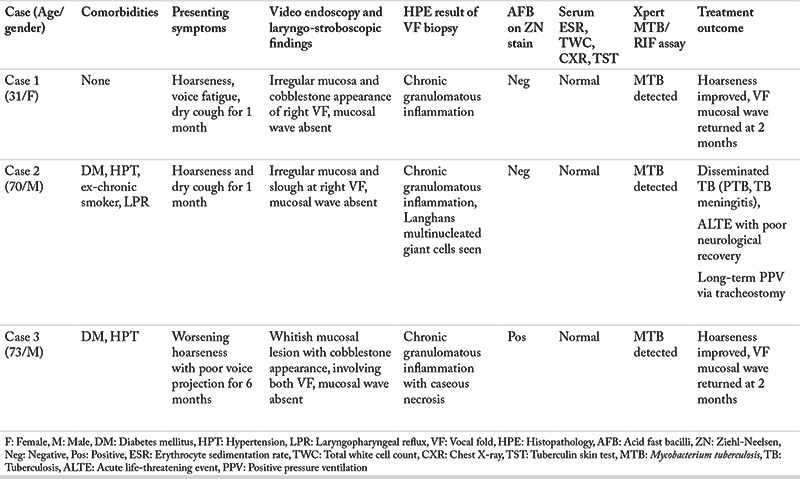
Table 1. Summary of patient characteristics, presenting symptoms, video laryngostroboscopic findings, investigation results and treatment outcomes.
The Xpert MTB/RIF assay is an automated cartridge-based nucleic acid amplification test for the rapid identification of MTB DNA and rifampicin resistance. The result would be ready in less than two hours using real-time polymerase chain reaction (11). The rapid identification of a drug resistant variant is extremely beneficial as the conventional drug susceptibility test takes longer than two months (12). It was reported that the Xpert MTB/RIF assay has 81.3% sensitivity and 99.8% specificity in detecting MTB in extrapulmonary specimens (12). Current WHO guidelines recommend using Xpert MTB/RIF as a replacement test for specific non-respiratory tissue specimens to diagnose extrapulmonary TB. To the authors’ knowledge, there is no study on the diagnostic accuracy of Xpert MTB/RIF in PLTB to date, probably due to this rare clinical entity.
PLTB responds well to anti-tuberculous therapy within 18 weeks (7). However, long-term follow-up is recommended to monitor possible laryngeal and extralaryngeal complications. PLTB may progress into disseminated TB that carries a poor prognosis, as demonstrated in our second case.
Conclusion
In view of the emergence of PLTB with atypical clinical manifestations, otolaryngologists in endemic regions should be more vigilant when treating patients presenting with hoarseness and subtle laryngeal endoscopic findings. PLTB must be considered as a differential diagnosis in a patient with unilateral irregular vocal fold lesion. Employing the Xpert MTB/RIF assay would be exceedingly beneficial in the early detection of the disease with good diagnostic accuracy, which, in turn, contributes to achieve a favorable outcome.
Main Points
• Primary laryngeal tuberculosis is becoming more common with hoarseness as the chief complaint.
• Irregular vocal fold mucosal lesion, either unilateral or bilateral, can be the early and the only clinical manifestation of primary laryngeal tuberculosis.
• The vocal fold mucosal waves in primary laryngeal tuberculosis were typically absent on laryngostroboscopy examination.
• Biopsy of the vocal fold lesion with precision technique is crucial to confirm the diagnosis.
• Xpert MTB/RIF assay that detects Mycobacterium tuberculosis in the tissue biopsy specimens enables the rapid diagnosis of primary laryngeal tuberculosis.
• The vocal fold mucosal lesions can be potentially resolved with return of the mucosal wave by timely commencement of antituberculous therapy.
Footnotes
Informed Consent: The patients signed informed consent regarding publishing their data and photographs.
Peer-review: Externally peer-reviewed.
Authorship Contributions
Surgical and Medical Practices: L.S.G., T.K.J., M.A., M.M.B., Concept: L.S.G., T.K.J., M.A., M.M.B., Design: L.S.G., M.A., M.M.B., Data Collection and/or Processing: L.S.G., T.K.J., Analysis and/or Interpretation: L.S.G., T.K.J., M.A., M.M.B., Literature DSearch: L.S.G., T.K.J., M.A., M.M.B., Writing: L.S.G., T.K.J., M.A., M.M.B.
Conflict of Interest: There is no conflict of interest to disclose.
Financial Disclosure: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Saldanha M, Sima NH, Bhat VS, Kamath SD, Aroor R. Present scenario of laryngeal tuberculosis. Int J Otorhinolaryngol Head Neck Surg. 2018;4:242–6. [Google Scholar]
- 2.Lim JY, Kim KM, Choi EC, Kim YH, Kim HS, Choi HS. Current clinical propensity of laryngeal tuberculosis: review of 60 cases. Eur Arch Otorhinolaryngol. 2006;263:838–42. doi: 10.1007/s00405-006-0063-5. [DOI] [PubMed] [Google Scholar]
- 3.Ponni S, Venkatesan SK, Saxena SK, Suryanarayanan G. Primary laryngeal tuberculosis-changing trends and masquerading presentations: a retrospective study. Int J Otorhinolaryngol Head Neck Surg. 2019;5:634. [Google Scholar]
- 4.Jindal SK, Jindal A, Agarwal R. Upper respiratory tract tuberculosis. Microbiol Spectr. 2016;4:35–40. doi: 10.1128/microbiolspec.TNMI7-0009-2016. [DOI] [PubMed] [Google Scholar]
- 5.El Ayoubi F, Chariba I, El Ayoubi A, Chariba S, Essakalli L. Primary tuberculosis of the larynx. Eur Ann Otorhinolaryngol Head Neck Dis. 2014;131:361–4. doi: 10.1016/j.anorl.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 6.Swain SK, Behera IC, Sahu MC. Primary laryngeal tuberculosis: our experiences at a tertiary care teaching hospital in Eastern India. J Voice. 2019;33:812.e9–14. doi: 10.1016/j.jvoice.2018.04.010. [DOI] [PubMed] [Google Scholar]
- 7.Ling L, Zhou SH, Wang SQ. Changing trends in the clinical features of laryngeal tuberculosis: a report of 19 cases. Int J Infect Dis. 2010;14:e230–5. doi: 10.1016/j.ijid.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 8.Nachiappan AC, Rahbar K, Shi X, Guy ES, Mortani Barbosa EJ Jr, Shroff GS, et al. Pulmonary tuberculosis: role of radiology in diagnosis and management. Radiographics. 2017;37:52–72. doi: 10.1148/rg.2017160032. [DOI] [PubMed] [Google Scholar]
- 9.Agarwal R, Gupta L, Singh M, Yashaswini N, Saxena A, Khurana N, et al. Primary laryngeal tuberculosis: a series of 15 cases. Head Neck Pathol. 2019;13:339–43. doi: 10.1007/s12105-018-0970-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Qian X, Albers AE, Nguyen DTM, Dong Y, Zhang Y, Schreiber F, et al. Head and neck tuberculosis: literature review and metaanalysis. Tuberculosis. 2019;116:S78–88. doi: 10.1016/j.tube.2019.04.014. [DOI] [PubMed] [Google Scholar]
- 11.Sachdeva K, Shrivastava T. CBNAAT: a boon for early diagnosis of tuberculosis-head and neck. Indian J Otolaryngol Head Neck Surg. 2018;70:572–7. doi: 10.1007/s12070-018-1364-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mehta PK, Raj A, Singh N, Khuller GK. Diagnosis of extrapulmonary tuberculosis by PCR. FEMS Immunol Med Microbiol. 2012;66:20–36. doi: 10.1111/j.1574-695X.2012.00987.x. [DOI] [PubMed] [Google Scholar]


