Abstract
Simple Summary
Molecular aberrations in the phosphatidylinositol 3-kinase (PI3K) pathway are often observed in breast cancer and represent a key regulator of many cellular processes, promoting tumor cell growth and survival. The first clinical trials leading to the development of pan-PI3K inhibitors showed certain preclinical activity; nevertheless, the toxicity profile limited further analysis of this drugs’ class. To improve the antitumor effect and therapeutic index, additional clinical trials have been performed to develop the PI3K isoform-specific inhibitors and new schedule combinations with a good toxicity profile. However, further efforts are needed to discover other potentially actionable genetic alterations that remain a challenge to reach the goal of personalized and precision medicine.
Abstract
Breast cancer is the leading cause of death in the female population and despite significant efforts made in diagnostic approaches and treatment strategies adopted for advanced breast cancer, the disease still remains incurable. Therefore, development of more effective systemic treatments constitutes a crucial need. Recently, several clinical trials were performed to find innovative predictive biomarkers and to improve the outcome of metastatic breast cancer through innovative therapeutic algorithms. In the pathogenesis of breast cancer, the phosphatidylinositol 3-kinase (PI3K)-protein kinase B (PKB/AKT)-mammalian target of rapamycin (mTOR) axis is a key regulator of cell proliferation, growth, survival, metabolism, and motility, making it an interest and therapeutic target. Nevertheless, the PI3K/AKT/mTOR cascade includes a complex network of biological events, needing more sophisticated approaches for their use in cancer treatment. In this review, we described the rationale for targeting the PI3K pathway, the development of PI3K inhibitors and the future treatment directions of different breast cancer subtypes in the metastatic setting.
Keywords: PI3K inhibitors, subtype breast cancer, biomarkers, liquid biopsy, next-generation sequencing, real-time PCR, target therapy, clinical trial, precision medicine
1. Introduction
Breast cancer (BC) has been divided into four subgroups according to the different expressions of hormone and human epidermal growth factor (HER2) receptors: luminal A, luminal B, HER2 enriched, and basal-like. Each subtype is characterized by different clinical manifestations and prognosis [1,2,3,4]. The most advanced genomic assays have expanded BC molecular sequencing, shedding light on the detection of further genetic alterations and new potentially predictive and prognostic biomarkers [5].
Genetic dysregulation in the phosphoinositide 3-kinase (PI3K) pathway is frequently observed in BC. Alterations in the PI3K/AKT/mTOR pathway can either increase or abolish PI3K activity. Moreover, mutations in the tumor suppressing system, such as in the genes encoding for phosphatase and tensin homolog (PTEN) and inositol polyphosphate 4-phosphatase (INPP4B), can determine not only cancer growth, progression, survival, metabolism, protein synthesis and angiogenesis but also the risk of resistance to endocrine therapy and chemotherapy [6]. Therefore, a better understanding of the PI3K axis in BC in the metastatic settings is crucial, in order to better target the different molecular subtypes.
PI3Ks represents a group of heterodimeric lipid kinases at plasma and intracellular membranes characterized by catalytic (p110) and regulatory (p85) subunits. PI3K is divided into three classes with different biochemical properties and specificity. Class I PI3Ks, the most involved in BC, are divided by PI3Ks class IA, class IB, and class IC. The activation of the specific receptor—by the extracellular ligand—stimulates PI3K to catalyze phosphorylation of phosphatidylinositol 4,5-bisphosphate (PIP2) to phosphatidylinositol 3,4,5-triphosphate (PIP3), recruiting two central mediators of the PI3K cascade, the protein kinase B (AKT) and the phosphoinositide-dependent kinase 1 (PDK1). Then, the phosphorylation of AKT by PDK1 determines a series of different downstream signals mediated by the activation of mammalian target of rapamycin (mTOR), promoting the metabolic and proliferative setting of the cell. The tumor suppressors PTEN and INPP4B are negative regulators of AKT as they catalyze the dephosphorylation of PIP3 to PIP2, limiting the activation of the PI3K signaling axis [7,8,9] (Figure 1).
Figure 1.
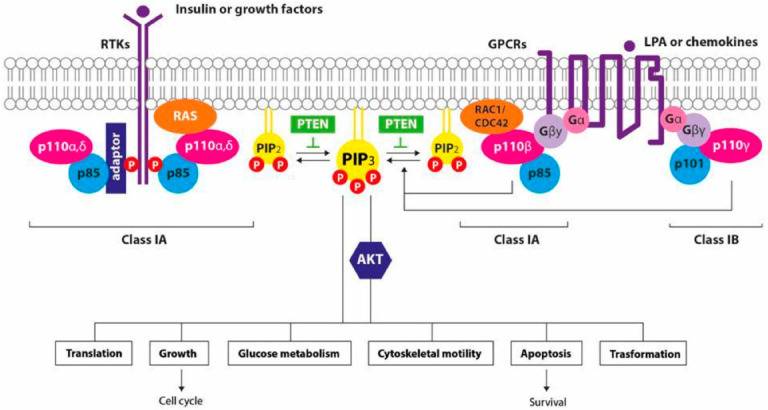
Signaling by PI3K isoforms in summary: growth factors bind their receptors on cell surface and activate the receptor tyrosine kinase (TK) or the G-protein coupled receptor (GPCR), promoting the recruitment of class I PI3Ks. The phosphorylation of PIP2 into PIP3 stimulates the downstream activation of both AKT-dependent and -independent signaling pathways. PTEN acts as regulator, removing the 3′ phosphate from PIP3 inactivating the signal perpetuated by class I PI3K [9].
PIK3CA is the main genomic aberration found in hormone receptor positive (HR+) BC, the mutation occurs in the encoding region of the p110α catalytic subunit of PI3K [4]. Other mutations involved in the PI3K cascade have a pathogenic role, even if less frequently found, as loss-of-function of PTEN (2–4%), activating mutations in AKT (2–3%) and in PI3K regulatory subunit α (1–2%). Similar alterations were found in HER2 positive (HER2+) BC. On the contrary, PTEN loss of expression and PIK3CA mutations can be found in triple negative breast cancer (TNBC) in about 30–50% and <10% of cases, respectively, conferring an unfavorable prognosis and resistance to standard of care (SOC) therapies [10].
The clinical implications of these mutations, however, still need to be clarified considering the controversial findings in the field of PIK3CA in BC [11,12,13]. Although a number of PI3K/AKT/mTOR axis inhibitors have been studied in pre-clinical settings, only a few reached the approval for the treatment of human cancer. In this review, we will provide an overview on the development and the most recent clinical findings of the different PI3K inhibitors in different breast cancer subtypes for the treatment of advanced BC.
2. Pan-PI3K Inhibitors
Activating mutations in PIK3CA, the gene encoding for the p110α catalytic subunits of PI3K, are associated with the growth and survival of cancer cells that play a role in cell survival, proliferation, differentiation, and glucose transport [4,14,15,16]. Dysregulation of the PI3K-pathway may also contribute to resistance to a variety of anticancer agents [17,18]. First-generation PI3K inhibitors (PI3Ki), also known as pan-inhibitors of PI3K, target all four catalytic isoforms of class I PI3Ks (α, β, γ, and δ) [19,20]. These inhibitors encompass a broad spectrum of activities, and this broader inhibition leads to a higher risk of adverse events (AEs) and off-target toxicity, which have limited their use at therapeutic doses and caused treatment discontinuation [10,21,22].
2.1. Pan-PI3K Inhibitors in HR+/HER2− Breast Cancer Subtypes
In luminal BC subtype PIK3CA activating mutations occur in roughly 40% of cases and, in this setting, the pan-PI3Ki mostly include buparlisib (BKM120) and pictilisib (GDC-094) (Table 1).
Table 1.
Summary of phases II-III trials with PI3K-inhibitors in HR-positive/HER2-negative metastatic breast cancer.
| Trials | Phase | Patient Population | Targeted Therapy | Treatment | mPFS (Months) |
mOS (Months) |
ORr (%) |
|
|---|---|---|---|---|---|---|---|---|
| ITT | Mutated PIK3CA | ITT | ITT | |||||
| BELLE-2 (Baselga)[23] NCT01610284 |
III | HR+/HER2− LABC or MBC, resistant to AI | pan-PI3K inhibitor | Buparlisib + Fulvestrant | 6.9 (HR 0.78) |
7.0 (HR 0.58) |
NA | 11.8 |
| Placebo + Fulvestrant | 5.0 | 3.2 | NA | 7.7 | ||||
| BELLE-3 (Di Leo)[18] NCT01633060 |
III | HR+/HER2− LABC or MBC, resistant to mTOR | Buparlisib + Fulvestrant | 3.9 (HR 0.67) |
4.2 (HR 0.46) |
NA | 8 | |
| Placebo + Fulvestrant |
1.8 | 1.6 | NA | 2 | ||||
| BELLE-4 (Martin)[21] NCT01572727 |
II-III | HER2− LABC or MBC |
Buparlisib + Paclitaxel | 8.0 (HR 1.18) |
9.1 (HR 1.17) |
NA | 22.6 | |
| Placebo + Paclitaxel | 9.2 | 9.2 | NA | 27.1 | ||||
| FERGI (Krop)[24] NCT01437566 |
II | HR+/HER2− LABC or MBC, resistant to AI (only PIK3CA | Pictilisib + Fulvestrant | 6.6 (HR 0.74) |
6.5 (HR 0.73) |
NA | 7.9 | |
| Placebo + Fulvestrant |
5.1 | 5.1 | NA | 6.3 | ||||
| PEGGY (Vuylsteke) [25] NCT01740336 |
II | HR+/HER2− LABC or MBC first/second line CT |
Pictilisib + Paclitaxel | 8.2 (HR 0.83) |
7.3 (HR 1.06) |
NA | 22 | |
| Placebo + Paclitaxel | 7.8 | 5.8 | NA | 19.6 | ||||
Abbreviation: HR+: hormone receptor positive, HER2−: human epidermal growth factor receptor 2 negative, ABC: advanced breast cancer, LABC: locally advanced breast cancer; MBC: metastatic breast cancer, AI: aromatase inhibitors, ITT: intention-to-treat, mPFS: median progression free survival (months), mOS: median overall survival (months), ORr: overall response rate, NA: not available, CT: chemotherapy.
2.1.1. Buparlisib
Buparlisib (BKM120) is an orally selective pan-PI3Ki that inhibits all four class I PI3K isoforms (p110α, β, γ, and δ), as well as somatically mutated p110α, with no activity against the class III PI3K, or mammalian target of rapamycin (mTOR). In cellular assays and in vivo models of human cancers, buparlisib showed significant dose-dependent tumor growth inhibition, potent antiproliferative and proapoptotic activities [26,27]. Miller et al. reported that the hyperactivation of the PI3K pathway, or PTEN loss expression, promoted antioestrogen resistance in HR+/HER2− MBC, inducing ER-transcriptional independent activity and growth of BC cells [24,25]. Therefore, buparlisib plus fulvestrant has been successfully evaluated in a phase I study in postmenopausal women with HR+ MBC, previously treated with endocrine therapy [28]. PIK3CA mutations proved to be a biomarker of poor prognosis, such as PgR negativity, TP53 mutations, and loss of PTEN expression. Conversely, mutations in AKT1 and ESR1 did not prevent tumor response. Treatment-related adverse events (AEs) were generally mild and included hepatic toxicity, rash and hyperglycemia [29,30].
The phase III BELLE-2 clinical trial investigated the efficacy and safety of buparlisib plus fulvestrant in HR+/HER2− post-menopausal MBC patients, who were progressive during/after treatment with aromatase inhibitors (AI) and had received up to one prior line of chemotherapy [23]. Patients were randomized to receive fulvestrant plus buparlisib or placebo and stratified according to PI3K status in tumor tissue by Sanger sequencing, and visceral disease status. The trial met its primary endpoint demonstrating a relatively modest benefit in progression-free survival (PFS) (6.9 versus 5.0 months compared to placebo; HR 0.78 CI 0.67–0.89; p < 0.001). Many patients, in the buparlisib arm, discontinued the study early (1.9 months) due to adverse events (higher transaminase levels, hyperglycemia, rash, and mood disturbances) probably influencing the potential benefits of combination therapy. In the exploratory analysis on PIK3CA mutations identified in circulating tumor DNA (ctDNA), the combination treatment was associated with an improvement in PFS compared with fulvestrant alone only in patients with PIK3CA mutations. In contrast, prespecified analyses of PIK3CA mutation and/or loss of PTEN expression by Sanger sequencing in archival tissue samples did not show increased PFS with buparlisib, potentially suggesting a tumor evolution from initial diagnosis and treatment beginning.
Likewise, BELLE-3 trial explored the ability of fulvestrant plus buparlisib to restore endocrine sensitivity, compared to fulvestrant alone, in patients with luminal MBC subtype previously treated with ET and mTOR inhibitors [31]. The trial showed that the combination therapy was associated with better PFS (median 3.9 months versus 1.8 months; HR 0.67 CI 0.53–0.84; p < 0.001), particularly in patients with real-time polymerase chain reaction (RT-PCR) or ctDNA PIK3CA mutations. In ctDNA-detected PI3K alterations the median PFS was 4.2 months versus 1.6 months (HR 0.46 CI 0.29–0.73; p = 0.00031) while it was 4.7 months versus 1.4 months (HR 0.39 CI 0.23–0.65; p < 0.001) in the group tested by RT-PCR. On the contrary, in the BELLE-2 trial, patients with PIK3CA mutations tested in tumor tissue, PFS was not different between treatments. The discrepancy between the two studies could be explained by the different sensitivity of the test used for PIK3CA assessment, or by the absence of stratification, based on ctDNA at randomization and subsequently added as a secondary endpoint.
Additionally, Baselga et al., in the combined analysis from BELLE-2 and BELLE-3 trials, observed that assessing PIK3CA-mutational status in ctDNA resulted in larger clinical benefits compared with tissue samples PCR [32,33]. The safety profile of buparlisib was consistent in BELLE-3 and BELLE-2. Psychiatric complications, related to the ability of buparlisib to penetrate the blood-brain barrier [34], such as depression, anxiety, and suicidal ideation, were reported in 2% of patients enrolled in the BELLE-3 trial, in contrast with the absence of suicidal ideation in BELLE-2 study.
In phase II/III clinical trial BELLE-4 [35], the combination of paclitaxel plus buparlisib in MBC as first-line treatment was tested, showing that the addition of buparlisib to paclitaxel did not improve median PFS when compared to paclitaxel alone (8.0 months versus 9.2 months in buparlisib and placebo group, respectively; HR 1.18 CI 0.82–1.68). Furthermore, the HRs, in the group of patients with PI3K mutations, PTEN loss expression and PI3K wild type, were similar to the overall enrolled population. Buparlisib treatment was associated with a higher frequency of serious AEs (30.2% in the buparlisib arm versus 20.9% in the placebo group) and more than 40% of patients, in the combination arm, experienced diarrhea (55%), rash (43%), hyperglycemia, and nausea (41%).
2.1.2. Pictilisib
Pictilisib (GDC-094) is an oral class I PI3K pan-inhibitor. In vitro experiments showed preliminary antitumor activity (equipotent inhibition of the p110α and -δPI3K isoforms and less potent inhibition of p110β and -γ isoforms) and, in human tumor xenograft murine models, pictilisib demonstrated a strong inhibitory effect on the growth of human U87MG glioblastoma and IGROV1 ovarian cancer [36].
In the dose-escalation phase I clinical trial, Sarker et al. [37] evaluated the preliminary clinical activity of pictilisib in sixty unselected and heavily pretreated patients with advanced solid tumors. A low response rate, consisting of one partial response (PR) and one stable disease (SD), was observed. The toxicity profile of pictilisib was similar to buparlisib and the most frequent grade 3/4 AEs were rash, hyperglycemia, and pneumonitis. In this study pictilisib-related hyperglycemia was limited to grade 1–2; grade > 3 hyperglycemia occurred only in one patient. Mood alterations were not significant due to the low central nervous system (CNS) penetration of pictilisib compared to Buparlisib.
According to previous results by Schmid et al., in a phase II, open-label, randomized trial [38], the addiction of pictilisib to anastrozole determined a synergic effect and was associated with increased inhibition of tumor cell proliferation over anastrozole alone in postmenopausal women with luminal-B early BC.
In the two-part, randomized, double-blind, placebo-controlled phase II clinical trial FERGI, [39] investigating the benefit of adding pictilisib to fulvestrant in postmenopausal patients with HR+/HER2− MBC resistant to AI, no difference in median PFS was found in the combination treatment arm, regardless of PI3KCA mutation status. The median PFS was 6.6 months and 5.1 months in the experimental arm and control arm, respectively (HR 0.74 CI 0.52–1.06; p = 0.096) in ITT-population and 6.5 months and 5.1 months, respectively (HR 0.73 95% CI 0.42–1.28; p = 0.268) in women with PIK3CA-mutations. Pictilisib treatment was affected by drug toxicity, potentially limiting its efficacy. Rash, diarrhea, increase transaminase level, hyperglycemia, pneumonitis, bronchopneumonia, pleural effusions, and fatigue were the most common AEs in the pictilisib arm and in approximately 60% of cases grade 3 or worse adverse events were observed, with serious AEs occurring in up to 16% of participants.
Another phase II randomized placebo-controlled clinical trial, PEGGY [40], failed to meet the primary endpoint. This study, similar to BELLE 4, was conducted to evaluate the benefit of adding PI3K-inhibitors to paclitaxel vs. paclitaxel alone in pre-and post-menopausal HR-positive/HER2-negative advanced BC patients. Genetic alterations in the PIK3CA gene were assessed in about 35% and 32% of patients in both arms, respectively. At the interim analyses, no significant differences in terms of PFS and overall response (ORR) were observed, irrespective of PIK3CA mutation status. Indeed, the addition of pictilisib to paclitaxel did not improve median PFS in the entire (8.2 months vs. 7.8 months; HR 0.95 CI 0.62–1.46; p = 0.83) and in the PI3K pathway-activated study population (7.3 months vs. 5.8 months; HR 1.06 CI 0.52–2.12; p = 0.88). Toxicity due to pictilisib administration included maculopapular rash, hypertension, and hyperglycemia, and experimental treatment was also associated with higher grade ≥ 3 AEs, dose reduction, and discontinuation.
2.2. Pan-PI3K Inhibitors in HER2+ Breast Cancer Subtypes
Although the anti-HER2 agents demonstrated strong efficacy in patients with HER2 + BC, de novo or acquired resistance to HER2-target therapies represents a wide field of research. About 25% of HER2 + BC harbor PIK3CA mutations confer resistance to anti-HER2 therapy and poorer prognosis [41,42,43,44,45,46]. Preclinical studies showed that HER2-signalling is extremely deregulated and is largely mediated by p110α rather than one of the other class-I PI3K isoforms, providing a robust rationale to target the PI3K pathway [47,48,49]. The tolerability and activity of buparlisib in combination with trastuzumab were investigated in a phase Ib/II dose-escalation trial in PIK3CA unselected HER2-positive BC, progressive to trastuzumab. The recommended dose of buparlisib was reached at 100 mg/day plus weekly intravenous trastuzumab but, even if evidence of clinical activity was observed, the study did not meet the pre-established primary endpoint such as objective response > 25% [50,51].
Furthermore, Guerin et al. studied buparlisib in combination with lapatinib, the orally dual anti-HER2/HER1 tyrosine kinase inhibitor, in the phase Ib/II trial PIKHER2, in HER2-positive trastuzumab-resistant MBC patients, independently to PIK3CA mutational status [52]. Twenty-four patients were treated at five different dose regimens; the selected dose was 80 mg/daily for buparlisib and 1000 mg/daily for lapatinib. Main drug-related adverse events leading to discontinuation of treatment were gastrointestinal disorders, skin rash, depression and anxiety. The disease control rate was 79% (95% CI 57–92%) including 4% of CR and a 29% of clinical benefit rate (CBR) (95% CI 12–51%).
2.3. Pan-PI3K Inhibitors in Triple Negative Breast Cancer Subtypes
TNBC represents the most aggressive BC with an incidence of 15–20% and a high heterogeneity in the mutational profile. Due to limited possibility of target therapies, standard chemotherapy still represents the milestone of treatment [53]. Approximately 10% of TNBC harbors a germline mutation in BRCA1 or BRCA2 genes and recent evidence has shown that platinum-based therapy offers promising activity both in early and metastatic settings [54,55,56,57,58,59,60]. In TNBC, activating PIK3CA mutations, the majority located in the p110α subunit, are the second most frequent molecular aberrations after TP53 mutations and occur in 7–9% of primary TNBC, with a likely higher rate in advanced TNBC [1]. PIK3CA mutations, with additional inactivating alterations in PTEN [61] and activating mutations in AKT1, globally occur in about 25% of TNBC [62]. In this subtype, dysregulation of the PI3K pathway has been correlated with chemotherapy resistance [63] and loss of PTEN function confers resistance to PDL1-blockade and leads to increased PI3Kβ signaling. Indeed, based on preclinical models, combined therapy with an anti-PDL1 agent and a PI3Kβ inhibitor showed an improvement in cancer growth inhibition [62,64]. However, the role of the PI3K pathway-targeted therapy in TNBC is also unclear. The activation of the PI3K pathway is more linked with the androgen receptor-positive subtype of TNBC and less correlated to TNBC compared to HR-positive and HER2-positive BC [62,65]. In the BELLE-4 trial TNBC patients (about 25% of total) tended to have a worse prognosis with buparlisib versus placebo arm (5.5 versus 9.3 months; HR 1.86 CI 0.91–3.79) and versus HR+ population (9.2 vs. 9.2 months; HR 1.00 CI 0.66–1.529). In this trial, the poorer prognosis in the TNBC subgroup, may be explained by a lower duration of paclitaxel exposure in the buparlisib group suggesting that the toxicity of buparlisib may have compromised the adequate administration of chemotherapy; hence, the authors failed to confirm the PIK3CA mutation’s predictive role in TNBC subtype [35]. In preclinical models, the pan-PI3Ki BKM120 sensitized BRCA-proficient TNBC to PARP inhibitor olaparib: the authors demonstrated that the dual PI3K and PARP inhibition significantly downregulated BRCA1/2 expression and reduced tumor cell growth [66]. Likewise, a second study showed synergic activity of buparlisib combined with olaparib in an MMTV-CreBRCA1f/fp53 +/− mouse model of BC [67]. Additionally, Matulonis UA et al., in a phase I dose-escalation trial, demonstrated anticancer activity in BC (54% of which TNBC) and ovarian cancer and in both germline BRCA (gBRCA)-mutated and gBRCA-wild-type patients [68].
3. PI3K Isoform-Specific Inhibitors
Even if buparlisib met the efficacy endpoint in patients with the PIK3CA mutation, particularly in combination with endocrine therapy, the toxicity profile observed in clinical trials limits its potential use such as to be adopted as SOC and determining the stop of further developments. Likewise, in the light of the similar poor tolerability of pictilisib (GDC-0941) in absence of significant difference in terms of outcomes, also in PIK3CA-mutant cohort, no additional clinical trials have been performed to develop this drug. On the other hand, the introduction of selective inhibitors of specific PI3K isoforms [2] allowed a safer profile and consequently a prolonged adherence at therapeutic doses, even if requiring a stricter selection of patients [10].
3.1. PI3K Isoform-Specific Inhibitors in HR+/HER2− Breast Cancer Subtypes
In HR+/HER2− BC subtype, the most studied PI3K isoform specific inhibitors are alpelisib (BYL719) and taselisib (GDC-0032) (Table 2).
Table 2.
Summary of phases II-III trials with PI3K isoform specific-inhibitors in HR-positive/HER2-negative metastatic breast cancer.
| Trial | Phase | Patient Population | Targeted Therapy | Treatment | mPFS (Months) |
mOS (Months) |
Orr (%) |
|
|---|---|---|---|---|---|---|---|---|
| Wild Type PI3KCA |
Mutated PIK3CA | Mutated PIK3CA | Mutated PIK3CA | |||||
| SOLAR-1 (Andrè) [69,70] NCT02437318 |
III | HR+/HER2− MBC, resistant to AI | PI3Kα inhibitor |
Alpelisib + Fulvestrant | 7.4 (HR 0.85) |
11.0 (HR 0.65) |
39.3 (HR 0.86) |
26.6 |
| Placebo + Fulvestrant |
5.6 | 5.7 | 31.4 | 12.8 | ||||
| SANDPIPER (Baselga)[71] NCT02340221 |
III | HR+/HER2− LABC or MBC, resistant to AI | Taselisib + Fulvestrant | 5.6 (HR 0.69) |
7.4 (HR 0.70) |
NA | 28 | |
| Placebo + Fulvestrant |
4.0 | 5.4 | NA | 11.9 | ||||
| BYLieve (Rugo)[72] NCT03056755 |
II | HR+/HER2− PIK3CA-mutated MBC, after CDKi + ET or CT or ET | Alpelisib + AI +/− LHRHa | - | NA | NA | NA | |
| Alpelisib + Fulvestrant +/− LHRHa | - | 7.5 | NA | 21 | ||||
Abbreviation: HR+: hormone receptor positive, HER2−: human epidermal growth factor receptor 2 negative, LABC: locally advanced breast cancer; MBC: metastatic breast cancer, AI: aromatase inhibitors, ITT: intention-to-treat, mPFS: progression free survival (months), mOS: overall survival (months), ORR: overall response rate, NA: not available, CDKi: CDK 4/6 inhibitor, ET: endocrine therapy, CT: chemotherapy, LHRHa: luteinizing hormone-releasing hormone agonist.
3.1.1. Alpelisib
Alpelisib (BYL719) is the first oral inhibitor to be approved by the US Food and Drug Administration (FDA) and by European Medicines Agency (EMA), specifically designed to target the p110α isoform of wildtype PI3Kα. The specificity determines a 50 times more potent action against PI3Kα than the other isoforms [48,73].
In preclinical models, Alpelisib inhibited the most common hotspot PIK3CAH1047R and PIK3CAE545K mutations at nanomolar concentration (4.6 nM/L) and interfered with PIK3CA-mediated downstream signaling; moreover, it induced a dose-dependent degradation of p110 protein levels in HR+/PIK3CA-mutated BC cell lines [33].
The phase I trial CBYL719X2101 (NCT01219699) included 134 heavily pre-treated patients with PIK3CA alterations across advanced cancer types and demonstrated sensitivity to the single agent alpelisib. At the achieved dose of alpelisib at 400 mg p.o. once daily or 150 mg p.o. twice daily, frequent treatment-related AEs of all grades were showed: hyperglycemia (51%), nausea (50%), skin rash (42.5%), decreased appetite (42%), diarrhea (40%), vomiting (31%), fatigue (30%), and mucositis (20%). A good activity was observed and the median PFS was 5.5 months with an improved benefit among PI3CA mutated BC [74].
A phase Ib study evaluated the MTD, the safety, and the efficacy of the combination of alpelisib plus fulvestrant in 87 heavily pre-treated luminal MBC and with about 60% of patients with PIK3CA alterations. The most frequent grade 3/4 AEs were hyperglycemia and maculopapular rash, and 10% of patients permanently discontinued. The indicated dose was 300 mg once daily. The ORr was 29% among patients with PIK3CA alterations compared to no objective tumor response in the PI3KCA wild-type group. The median PFS was longer (9.1 vs. 4.7 months) among patients with PI3KCA alterations than those with no PI3KCA mutations [75]. These preliminary findings motivated the following phase III SOLAR-1 randomized clinical trial (RTC) on the combination regimen with alpesib and fulvestrant.
The phase III randomized SOLAR-1 trial was conducted to assess the safety and the efficacy of alpelisib plus fulvestrant in contrast with only fulvestrant in man or post-menopausal women with luminal MBC who recurred or progressed on, or after AI treatment [21,69]. Pre-treatment with CDK4/6 inhibitors was permitted, but palliative chemotherapy or fulvestrant or mTOR inhibitors were not accepted as previous treatments. At a median follow-up of 30.8 months, in the PIK3CA-mutated group the median PFS was longer than control arm [11.0 months (95% CI 7.5–14.5) versus 5.7 months (HR 0.65; p < 0.001)]; in tumors with PIK3CA wild-type alpelisib did not show improvement in term of PFS (7.4 versus 5.6 months; HR 0.85 95% CI 0.58–1.25). Even if not statistically significant difference was shown in OS [39.3 months in the experimental arm (95% CI 34.1–44.9) versus 31.4 months (95% CI 26.8–41.3) in the fulvestrant arm (HR 0.86 95% CI 0.64–1.15 one-sided p = 0.15)], the absolute 8-month gain in the experimental arm was clinically relevant. Also, an increase of ORr was registered for patients receiving alpelisib/fulvestrant compared to control arm (26.6% versus 12.8%) showing mainly a PR [70]. Alpelisib demonstrated high incidence of hyperglycemia (64%), diarrhea (58%), nausea (45%), decreased appetite (36%), rash (36%) and maculopapular rash (14%) and higher permanent discontinuation due to AEs occurred in 25% of patients in the experimental group respect to fulvestrant group.
As shown in the SOLAR-1 study, a high concordance of PI3KCA status between primary and metastatic site was documented. Through liquid biopsy by plasma ctDNA, authors found a median PFS for the alpelisib/fulvestrant in the ctDNA-defined PIK3CA-mutant cohort versus the control arm (10.9 months vs. 3.7 months, respectively) the presence of PIK3CA mutations identified in ctDNA resulted in a risk of progression of 45% versus 35% in patients with PIK3CA mutations evaluated in tissue samples [76,77]. Giving the easy access of ctDNA and the results of the trials showing a positive correlation of ctDNA-detected PIK3CA mutations [21,78], US FDA approved the liquid biopsy testing, recommending the possibility to verify the presence of PIK3CA mutations in the tumor tissue when ctDNA testing has resulted negative [33,69].
In an exploratory analysis, the tissue samples were retrospectively tested with FoundationOne CDx 324-gene panel by Next Generation Sequencing (NGS) and a total of 7% of patients presented tumor PIK3CA mutations identified by NGS but not by RT-PCR-based testing and, moreover, showed a benefit from alpelisib [79]; therefore, the FDA has authorized FoundationOne CDx as a companion diagnostic test.
B-YOND is an interesting phase 1b study that included HR+/HER2− premenopausal asian advanced BC patients treated with alpelisib or buparlisib with tamoxifen plus goserelin as first-line therapy. Despite the high percentage of discontinuation due to toxicity, alpelisib plus endocrine therapy may be a valuable resource for premenopausal women with HR+/HER2− MBC [80].
Recruitment for the SOLAR-1 started in 2015 when CDK4/6 inhibitors were not yet approved; therefore, only 6% of patients with PI3CA mutations, randomized in the experimental arm, had previously received cyclines [69].
In the post-cyclin-dependent kinase 4/6 inhibitor setting, the phase II, open label, BYLieve trial (NCT03056755) was designed to assess the efficacy and the safety of alpelisib plus endocrine therapy (fulvestrant or letrozole) in three cohorts defined by immediate previous treatment for patients with HR+, HER2− PIK3CA-mutations MBC. In this trial, 112 patients with centrally confirmed PIK3CA mutations in tumor tissue were enrolled based on their previous treatment (CDKi + AI, CDKi + fulvestrant, or systemic chemotherapy or endocrine therapy): enrollment was completed in prior CDKi + AI and CDKi + fulvestrant SOC cohorts. The cohort of patients with CDKi + AI as immediate prior therapy received oral alpelisib 300 mg/day (continuously) plus fulvestrant: 50% of patients showed no disease progression at 6 months with median PFS resulted in 7 months and ORr of 21% over a median follow-up of 12 months [72].
3.1.2. Taselisib
Taselisib (GDC-0032) is an oral class I PI3K inhibitor; it is technically a beta-sparing inhibitor selectively inhibiting p110α, δ and γ isoforms with 30-fold lower potency against p110β [81]. Taselisib exhibits greater selectivity for mutant PI3Kα isoform, and it was expected to improve efficacy on PIK3CA-mutant tumors with better toxicity profile as compared with pan-PI3K inhibitors. In preclinical studies, treatment with taselisib described marked tumor suppressing effect on PIK3CA-mutant xenografts models [82].
A phase I dose-finding clinical trial demonstrated clinical activity of taselisib in patients with metastatic solid tumors, specifically in PIK3CA-mutant metastatic BC [83].
After these encouraging results, the SANDPIPER phase III trial showed the superiority of the combination of fulvestrant with taselisib over fulvestrant alone in postmenopausal HR+/PIK3CA-mutated MBC patients and progressive during/following AI [median PFS 7.4 months vs. 5.4 months (HR 0.7 95% CI 0.56–0.89; p = 0.004)], ORr 28% vs. 12%, p < 0.001). Conversely, among 120 participants with PI3KCA-wild type tumors, median PFS did not significantly differ between experimental arm versus control arm (5.6 versus 4.0 months; HR 0.69 95% CI, 0.44–1.08; p = 0.106). Further investigations of taselisib were stopped due to the high incidence of AEs, especially diarrhea (grade 3/4 of 12% versus <1% for hormonal therapy alone) and hyperglycemia (grade 3/4 of 11% for taselisib arm versus <1% for control arm) [71,84].
3.2. PI3K Isoform-Specific Inhibitors in HER2+ Breast Cancer Subtypes
In HER2 + BC, the development resistance to SOC anti-HER2 antibody has been correlated with the constitutive activation of the PI3K pathway [85]. Moreover, in trastuzumab-resistant BC cell lines due to the PTEN loss expression, inhibition of PI3K pathway inhibits cell growth and overcomes trastuzumab resistance [86].
With the purpose of studying the overcoming resistant to trastuzumab by PI3K pathway, new associations were tested. Alpelisib combined to trastuzumab emtansine (TDM-1) in trastuzumab-resistant patients with loss of PTEN function, AKT overexpression or PIK3CA mutation, documented an ORR of 43% in all populations and 30% in TDM1-resistant patients. Although 59% of patients experienced grade 3 toxicity, AEs were globally manageable. These results suggest that some sort of activation of the downstream PI3K pathway might occur, potentially provoking a resistance effect to TDM-1, similar to trastuzumab [87,88].
MEN1611 is a novel orally available α-selective PI3K inhibitor. Preclinical data demonstrated activity either as single agent or in combination with targeted therapies as shown in both xenograft and patient-derived xenograft (PDX) models of BC bearing PI3Kα mutations. In HER2 + BC harboring PIK3CA-mutation, cell lines and PDX models, MEN1611 acted synergistically when combined with trastuzumab, induced depletion protein, and a pro-inflammatory phenotype [89,90].
3.3. PI3K Isoform-Specific Inhibitors in Triple Negative Breast Cancer
The first in human phase I clinical trial studied the PI3KCB/PI3KCD inhibitor (AZD8186) in patients with PTEN-deficient/-mutated or PIK3CB-mutated/-amplified advanced TNBC in combination with abiraterone acetate or vistusertib (AZD2014), a dual mTOR inhibitor. AZD8186 showed significant anti-tumor activity in PTEN-deficient TNBC cell lines, especially when combined with anti-androgens or the dual mTORC1/2 inhibitor [91]. However, AZD8186 has limited efficacy as a single agent, but has improved efficacy when combined with paclitaxel and anti-PD1 in vivo [92].
Since upregulation of the PI3K/AKT/mTOR pathway has been related with resistance to microtubule-targeting drugs [93], alpelisib was combined with taxanes (paclitaxel or nab-paclitaxel) in two phase I/II trials. Both trials were interrupted for high grade toxicity in terms of hyperglycemia, grade 3 acute renal failure, and grade 4 leukopenia, in line with PEGGY and BELLE-4 studies [94,95,96].
Ashgar et al. showed that CDK4/6 and PI3 kinase inhibitor combinations have substantial activity in vitro and in vivo among PIK3CA mutant non-basal TNBC, both in the luminal androgen receptor and in mesenchymal-stem subgroups [97]. In luminal androgen receptor TNBC, high frequency PIK3CA mutations, provide rationale for the potential combination approach and reveal sensitivity to PI3K/mTOR inhibitors and AR targeted therapy [98]. A phase Ib clinical trial assessed the combination of taselisib with palbociclib in metastatic BC including a cohort of TNBC selected for activating PIK3 mutations and showed good treatment tolerability and promising preliminary anti-tumor activity [99].
Another preclinical study showed that blocking both PI3Kα and CDK4/6 has a synergic effect in multiple RB1-wild-type TNBC models, increasing apoptosis, cell-cycle arrest, and cancer immunogenicity. Particularly, the combination of PI3Kα and CDK4/6 inhibition, together with PD-1 and CTLA-4 inhibition, was able to induce the TNBC tumor regression in vivo providing a novel potential therapeutic approach for TNBC [100].
4. PIK3 Inhibitors: New Perspectives
Several clinical trials are ongoing to determinate the activity, efficacy, and toxicity profile of PIK3CA inhibitors in metastatic BC. These are mostly trials evaluating combination of PI3K inhibitors with different targeted agents to drive the treatment of different BC subtypes and to achieve the best possible disease control (Table 3).
Table 3.
Summary of ongoing phases I–III trials with PI3K-inhibitors in metastatic breast cancer according to different molecular subtypes.
| BC Subtypes |
Trials | Phase | Patient Population |
Targeted Therapy |
Treatment | Primary Endpoint |
Secondary Endpoint |
|---|---|---|---|---|---|---|---|
| HR+/ HER2− |
NCT04191499 [101] (INAVO 120) |
II/III | 400 | PI3Kα-inhibitor | Inavolisib (GDC-0077) Palbociclib Fulvestrant |
PFS | ORR BOR DOR CBR OS TTD AE |
|
NCT04355520 [102] |
I/II | 42 | PI3K α/δ-inhibitor | TQ-B3525 Fulvestrant |
DLT | ORR DCR DOR PFS OS |
|
|
NCT05025735 [103] |
II | 25 | PI3Kα-inhibitor | Alpelisib Dapagliflozin Fulvestrant |
Incidence of all grade hyperglycemia | Incidence of grade 3/4 hyperglycemia ORR PFS |
|
| HER2+ |
NCT03006172 [104] |
I | 256 | PI3Kα-inhibitor | Inavolisib (GDC-0077) Fulvestrant Letrozole Palbociclib Metformin Trastuzumab Pertuzumab |
DLTs | AUC Half-Life Cmax Cmin Time to Cmax of Inavolisib Apparent Clearance of Inavolisib ORR CBR DOR PFS |
|
NCT04108858 [105] |
Ib/II | 102 | pan-PI3K—PI3K α/δ-inhibitor | Copanlisib Petruzumab Trastuzumab |
AEs and SAEs DLTs PFS |
PFS OS AEs and SAEs |
|
|
NCT04208178 [106] |
III | 588 | PI3Kα-inhibitor | Alpelisib Pertuzumab Trastuzumab |
DLTs PFS |
OS ORR CBR TTR DOR |
|
|
NCT03767335 (B-PRECISE 01)[107] |
I | 48 | PI3K α/β/γ-inhibitor | MEN1611 Trastuzumab Fulvestrant |
MTD | TEAEs OS PFS |
|
|
NCT05063786 (ALPHABET)1 [9] |
III | 300 | PI3Kα-inhibitor | Alpelisib Trastuzumab Fulvestrant Vinorelbine/ Capecitabine or Eribulin |
PFS | OS OR Safety profile |
|
| HR+/ HER2 and TNBC |
NCT04586335 [108] |
Ib | 350 | PI3Kα-inhibitor | CYH33 Olaparib |
DLT ORR |
AEs DCR Pharmacokinetic measures |
|
NCT03218826 [109] |
I | 58 | PI3Kβ-inhibitor | AZD8186 Docetaxel |
MTD AEs |
ORR CBR Drug—Drug interaction |
|
| TNBC |
NCT04251533 (EPIK B3)[110] |
III | 566 | PI3Kα-inhibitor | Alpelisib Nab-paclitaxel |
PFS ORR |
OS CBR ORr TTR DOR |
|
NCT03961698 (MARIO-3)[111] |
II | 90 | PI3Kγ-inhibitor | IPI-549 (eganelisib) Nab-paclitaxel Atezolizumab |
CR | TEAEs SAEs AEs ORr TTR DOR PFS |
|
|
NCT02637531 [112] |
I | 219 | PI3Kγ-inhibitor | IPI-549 (eganelisib) Nivolumab |
DLT AEs |
AEs and safety laboratory Values Plasma concentrations of IPI-549 ORr CR PR DOR PFS OS |
|
| NCT02646748 [113] | Ib | 159 | PI3Kδ-inhibitor | INCB050465 Pembrolizumab |
Safety and tolerability profile | ORr Change in the number of TILs and the ratio of CD8+ lymphocytes to FOXP3+ cells infiltrating tumor post-treatment versus pretreatment by IHC |
|
| NCT04345913 [114] | I/II | 18 | pan-PI3K-inhibitor / PI3K α/δ-inhibitor | Copanlisib Eribulina |
MTD PFS |
ORR CBR PFS |
|
| TNBC AR+ | NCT02457910 [115] | I/II | 30 | PI3K α/δ/γ- inhibitor |
Taselisib Enzalutamide |
CBR MTD |
PFS Pharmacokinetic profile |
|
NCT03207529 [116] |
I | 28 | PI3Kα-inhibitor | Alpelisib Enzalutamide |
MDT RP2D |
DLT Safety profile |
Abbreviation: AUC: Area Under the Concentration Time-Curve, Cmax: Maximum Plasma Concentration, Cmin: Minimum Plasma Concentration, AEs: adverse events, SAEs: serious adverse events, PFS: progression free survival, OS: overall survival, DLT: dose limiting toxicities, ORr: overall response rate, CBR: clinical benefit rate, TTR: time to response, DOR: duration of response, TEAEs: treatment-emergent adverse events, BOR: best overall response rate, TTD: time to deterioration, MTD: maximum tolerated dose, RP2D: recommended phase II dose, CR: complete response, TILs: Tumor Infiltrating Lymphocytes, IHC: immunohistochemistry.
4.1. PI3K Inhibitors in HR+ HER2− Breast Cancer Subtypes
Inavolisib (GDC-0077) is an oral experimental drug targeting and inhibiting the PI3K p110a catalytic subunit (NCY 03006172). Based on preclinical studies that proved synergy between CDK4/6 inhibitors and PI3K inhibitors, a phase I open label dose-escalation study tested GDC-0077 as a single agent or in combination with letrozole/fulvestrant and Palbociclib for the treatment of locally advanced or metastatic PIK3CA-mutant BC. Worthy of mention is the metformin-addition arm to prevent PIK3I-induced hyperglycemia. The trial showed that GDC-0077 plus CDK4/6I and endocrine therapy could be combined at maximum doses [104]. Hence, the combination therapy is being evaluated in the INAVO120 trial, a phase III, randomized, double blind, placebo-controlled study (NCT04191499) that enrolled endocrine resistant patients with PIK3CA-mutant/HR+/HER2−, locally advanced or MBC. The trial is designed to verify the progression free survival and safety of Inavolisib plus palbocilib and fulvestrant [101].
An ongoing multicentre, open-label, phase Ib study (NCT04355520) is evaluating the safety and efficacy of TQ-B3525, a novel selective oral PI3K α/δ inhibitor. The drug is combined with fulvestrant SOC in subjects with HR+/HER2− and PIK3CA mutation [102].
Moreover, a single arm open label pilot trial is ongoing to assess the combination of dapagliflozin, a sodium/glucose cotransporter-2 (SGLT-2)-inhibitor used to treat diabetes mellitus, with alpelisib + fulvestrant in patients with HR+/HER2− metastatic BC. The aim of this study is to determine if the addition of dapagliflozin to alpelisib and fulvestrant combination could lead to a significant reduction of all-grade hyperglycemia [103].
4.2. PI3K Inhibitors in HER2 + Breast Cancer Subtypes
The combination of copanlisib, trastuzumab, and pertuzumab is currently tested in a phase Ib/II study for HER2+ stage IV BC with PIK3CA or PTEN mutation. Copanlisib is an intravenously administered PI3K inhibitor typically used to treat relapsed and refractory follicular lymphoma, but the addition of copanlisib to trastuzumab and pertuzumab in HER2 + BC therapy could increase the duration of response as compared to the standard treatment, overcoming the resistance due to the hyperactivation of PI3K signaling downstream of HER2. Incidence of AEs, dose limiting toxicities and PFS are the primary endpoints evaluated in this trial [105,117].
In the same setting of disease and in the same patient population a multicenter randomized, double-blind, placebo-controlled phase III study (NCT04208178) is evaluating alpelisib in combination with trastuzumab and pertuzumab as maintenance treatment after induction therapy with a taxane. The study is divided into multiple sections: part 1 is the open-label, safety run-in part of the study, designed to confirm the recommended phase III dose (RP3D) of alpelisib in combination with the monoclonal antibodies [106].
B-PRECISE-01 trial (NCT03767335) tests MEN 1611, a molecule targeting the p110 α and, to a lesser extent, β and γ isoforms. The primary outcome of this open-label, dose-escalation, phase Ib study is to verify the maximum tolerated dose while treatment emergent adverse events (TEAEs); PFS and OS are the secondary endpoints. MEN 1611 is investigated in association with trastuzumab in patients affected by Her2+ metastatic BC after progression from HER2 based therapy. In the same trial, fulvestrant is added in post-menopausal women with hormone-sensitive disease [107].
In the international, multicenter, open-label, controlled phase III RCT ALPHABET TRIAL (NCT05063786), the combination of alpelisib with trastuzumab +/− fulvestrant will be tested. Patients with HER2 + BC and documented PIK3CA mutation, previously treated with TDM-1, will be enrolled. The control arm with chemotherapy according to investigator RCT (vinorelbine, capecitabine or eribulin) makes this study particularly interesting [118].
4.3. PI3K Inhibitors in Triple Negative Breast Cancer Subtypes
The purpose of EPICK-B3 (NCT04251533) is to determine whether treatment with alpelisib in combination with nab-paclitaxel is safe and effective in subjects with advanced TNBC. This RCT is divided into different parts: part A, that is a randomized, double-blind, placebo-controlled study for patients with PIK3CA mutation regardless of PTEN status; part B1, that is a single-arm, open-label study for patients with PTEN loss expression without PIK3CA mutation. If preliminary efficacy is demonstrated, study part B2 will explore alpelisib + nab-paclitaxel in the same patient population as part B1 in a randomized, double-blind trial [96,110].
Still in the TNBC, Mario-3 (Macrophage Reprogramming in Immuno-Oncology) trial (NCT03961698) is studying a “triple combination”, which includes the addition of a new investigational drug called eganelisib (IPI-549) to the FDA-approved combination treatment with nab-paclitaxel and atezolizumab. IPI-549 is an oral, selective inhibitor of PI3Kγ. that works by reprogramming M2 macrophages or myeloid derived suppressor cells (MDSCs) within the tumor microenvironment from a pro-tumor function to an anti-tumor function. These effects allowed decreasing immune-suppression and increasing immune-activation, leading to the activation and proliferation of T cells that can attack cancer cells [119,120]. The evaluation of CR according to RECIST v1.1 criteria is the primary endpoint of MARIO-3, while safety, ORr, time to CR (TTCR), time to response (TTR), duration of CR (DOCR), duration of response (DOR), and PFS are the secondary endpoints [111].
Two additional trials evaluate novel combinations of PI3Ki with immunotherapy: one trial analyzes the association of PI3Kγ inhibitor with nivolumab (NCT02637531), and another one evaluates the combination of PI3Kδ inhibitor with pembrolizumab (NCT02646748) [53,112,113].
Moreover, the phase I/II trial studies the side effects and best dose of copanlisib and its activity and efficacy when given together with eribulin in treating patients with TNBC (NCT04345913) [114].
Patients with luminal androgen receptor TNBC deserve a special mention. For this peculiar population a phase Ib/II trial (NCT02457910) is testing the side effects and best dose of taselisib when given together with enzalutamide, a potent androgen receptor (AR) currently used for the treatment of patients with metastatic castration-resistant prostate cancer [115].
Another phase I clinical trial is studying the association of the α-specific PI3-kinase inhibitor alpelisib with enzalutamide in PTEN loss function and AR+ TNBC (NCT03207529). However, enzalutamide, in a phase II study, has already demonstrated clinical activity and good tolerability in patients with advanced AR+ TNBC [21,116].
A promising combination strategy is represented by PARP/PI3K dual inhibitors. This combination synergically acts to block the growth of cancer cells: PI3K inhibition leads to downregulation of BRCA1/2 proteins which increase the degree of Homologous Recombination Repair (HRR) deficiency. Therefore, the purpose of an ongoing phase I trial (NCT04586335) is to assess the safety, tolerability, and preliminary efficacy of CYH33, a novel highly potent and selective oral inhibitor of PI3Kα, in combination with olaparib in BC and other solid tumors like ovarian, endometrial, or prostate cancer [108].
AZD8186 is a PI3Kβ inhibitor tested in a phase I trial (NCT03218826) in combination with docetaxel. This is essentially a dose escalation study in which patients with HR+/HER2− advanced BC or metastatic TNBC and PTEN or PIK3CB mutation are enrolled. The primary objectives are to determine MDT or RP2D and to assess the safety and tolerability of AZD8186 when administrated in combination with docetaxel. The possible mechanisms of acquired resistance to PI3Kβ inhibition will be also evaluated: sequencing data from pre- and post-treatment specimens of patients that initially responded to PI3Kβ inhibitor AZD8186 will be compared to identify newly acquired mutations or deoxyribonucleic acid copy number alterations [109].
The results from these several trials could give us a better perspective on how PI3K inhibition impacts on TNBC patients’ management.
5. Conclusions
As previously mentioned, PI3K/AKT/mTOR signaling pathway is highly involved in cell differentiation, proliferation, energetic and glucose metabolism, apoptosis, motility, and angiogenesis. The high frequency of genetic aberrations in this pathway can result in tumorigenesis and cancer progression, as well as intrinsic and acquired resistance to available anti-tumor treatments for BC. PI3K mutations can be detected by tumor tissue and/or ctDNA in all BC subtypes and provide the rationale for the development of inhibitors targeting PI3K axis. The first pan-PI3K inhibitors combined with ET showed efficacy in PIK3CA-mutated patients, and their lack of selectivity determined high toxicity profile and limitation of the use in clinical practice. The subsequent development of the PI3K isoform-specific inhibitors with better tolerability profile in part overcame these concerns and provided new treatment chances for luminal PIK3CA mutations MBC, progressed after ET. The p110α-specific alpelisib was recently included in the arsenal of the treatments of HR+ MBC patients. However, the use of this agent in clinical practice requires better management of side effects, and a more suitable selection of patient population. In order to optimize the efficacy of these drugs, further clinical trials are needed to identify novel predictive biomarkers, and to elucidates the possible mechanism of intrinsic and acquired resistance. Moreover, clinical studies on new combinations of the PI3K isoform-specific inhibitors with ET, chemotherapy, CDK 4/6 inhibitors, immune checkpoint inhibitors, or novel target agents are still ongoing and could enhance the clinical benefit due to the possible synergistic action of an innovative treatment tailored to the specific BC subtypes and driven by PIK3CA aberrations. Another challenge will be to identify future new associations that do not increase the intrinsic toxicity of the PI3k inhibitor and associate with those of the companion molecules. Actually, no evidence of new methods has been developed to overcome the additive toxicity induced by combination therapies; possible studies on polymorphisms could identify genomic markers of predictivity to specific drug-related toxicities. Finally, genetic profiling of BC patients could lead to a better case selection, particularly for patients with poorer prognosis.
Acknowledgments
We thank Francesca Grillo for her graphic assistance.
Author Contributions
Conceptualization: A.F. and P.F.; Critical Review of Literature: P.F., M.M. and T.D.; Writing-Original Draft Preparation: A.F., P.F., M.M. and T.D.; Writing-Review and Editing: P.F. and A.F.; supervision: A.F. Validation: All authors; P.F., M.M., T.D., I.P., L.C., G.T. (Giordana Tiberi), F.P., S.D., A.O., G.T. (Giampaolo Tortora), G.S., A.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
All authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bray F., Ferlay J. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Heer E., Harper A. Global burden and trends in premenopausal and postmenopausal breast cancer: A population-based study. Lancet Glob. Health. 2020;8:e1027–e1037. doi: 10.1016/S2214-109X(20)30215-1. [DOI] [PubMed] [Google Scholar]
- 3.Perou C.M., Sørli T. Molecular portraits of human breast tumours. Nature. 2000;406:747–752. doi: 10.1038/35021093. [DOI] [PubMed] [Google Scholar]
- 4.Cancer Genome Atlas Network Comprehensive molecular portraits of human breast tumors. Nature. 2012;490:61–70. doi: 10.1038/nature11412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kawaji H., Kubo M. Comprehensive molecular profiling broadens treatment options for breast cancer patients. Cancer Med. 2021;10:529–539. doi: 10.1002/cam4.3619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guerrero-Zotano A., Mayer I.A. PI3K/AKT/mTOR: Role in breast cancer progression, drug resistance, and treatment. Cancer Metastasis Rev. 2016;35:515–524. doi: 10.1007/s10555-016-9637-x. [DOI] [PubMed] [Google Scholar]
- 7.Fruman D., Chiu H. The PI3K pathway in human disease. Cell. 2017;170:605–635. doi: 10.1016/j.cell.2017.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Engelman J., Luo J. The evolution of phosphatidylinositol 3-kinases as regulators of growth and metabolism. Nat. Rev. Genet. 2006;7:606–619. doi: 10.1038/nrg1879. [DOI] [PubMed] [Google Scholar]
- 9.Thorpe L., Yuzugullu H. PI3K in cancer: Divergent roles of isoforms, modes of activation, and therapeutic targeting. Nat. Rev. Cancer. 2015;15:7–24. doi: 10.1038/nrc3860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ellis H., Ma C.X. PI3K Inhibitors in Breast Cancer Therapy. Curr. Oncol. Rep. 2019;21:110. doi: 10.1007/s11912-019-0846-7. [DOI] [PubMed] [Google Scholar]
- 11.Saal L., Holm K. PIK3CA Mutations Correlate with Hormone Receptors, Node Metastasis, and ERBB2, and Are Mutually Exclusive with PTEN Loss in Human Breast Carcinoma. Cancer Res. 2005;65:2554–2559. doi: 10.1158/0008-5472-CAN-04-3913. [DOI] [PubMed] [Google Scholar]
- 12.Loi S., Michiels S., Lambrechts D., Fumagalli D., Claes B., Kellokumpu-Lehtinen P.L., Sotiriou C. Somatic Mutation Profiling and Associations With Prognosis and Trastuzumab Benefit in Early Breast Cancer. J. Natl. Cancer Inst. 2013;105:960–967. doi: 10.1093/jnci/djt121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.López-Knowles E., O’Toole S.A., McNeil C.M., Millar E.K., Qiu M.R., Crea P., Sutherland R.L. PI3K pathway activation in breast cancer is associated with the basal-like phenotype and cancer-specific mortality. Int. J. Cancer. 2009;126:1121–1131. doi: 10.1002/ijc.24831. [DOI] [PubMed] [Google Scholar]
- 14.Fabi A., Metro G., Di Benedetto A., Nisticò C., Vici P., Melucci E., Antoniani B. Clinical significance of PTEN and p-Akt co-expression in HER2-positive metastatic breast cancer patients treated with trastuzumab-based therapies. Oncology. 2010;78:141–149. doi: 10.1159/000312656. [DOI] [PubMed] [Google Scholar]
- 15.Bader A.G., Kang S. Oncogenic PI3K deregulates transcription and translation. Nat. Rev. Cancer. 2005;5:921–929. doi: 10.1038/nrc1753. [DOI] [PubMed] [Google Scholar]
- 16.Vivanco I., Sawyers C.L. The phosphatidylinositol 3-Kinase AKT pathway in human cancer. Nat. Rev. Cancer. 2002;2:489–501. doi: 10.1038/nrc839. [DOI] [PubMed] [Google Scholar]
- 17.Fekete M., Santiskulvong C. Effect of PI3K/Akt pathway inhibition-mediated G1 arrest on chemosensitization in ovarian cancer cells. Anticancer Res. 2012;32:445–452. [PubMed] [Google Scholar]
- 18.Carden C.P., Stewart A. The association of PI3 kinase signaling and chemoresistance in advanced ovarian cancer. Mol. Cancer Ther. 2012;11:1609–1617. doi: 10.1158/1535-7163.MCT-11-0996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garces A.E., Stocks M.J. PI3K Clinical Candidates and Recent Inhibitor Design Strategies: A Medicinal Chemistry Perspective. Med. Chem. 2019;62:4815–4850. doi: 10.1021/acs.jmedchem.8b01492. [DOI] [PubMed] [Google Scholar]
- 20.Yang J., Nie J. Targeting PI3K in cancer: Mechanisms and advances in clinical trials. Mol. Cancer. 2019;18:26. doi: 10.1186/s12943-019-0954-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Verret B., Cortes J. Efficacy of PI3K inhibitors in advanced breast cancer. Ann. Oncol. 2019;30:12–20. doi: 10.1093/annonc/mdz381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Janku F., Yap T.A. Targeting the PI3K pathway in cancer: Are we making headway? Nat. Rev. Clin. Oncol. 2018;15:273–291. doi: 10.1038/nrclinonc.2018.28. [DOI] [PubMed] [Google Scholar]
- 23.Baselga J., Im S.A., Iwata H., Cortés J., De Laurentiis M., Jiang Z., Campone M. Buparlisib plus fulvestrant versus placebo plus fulvestrant in postmenopausal, hormone receptor-positive, HER2-negative, advanced breast cancer (BELLE-2): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2017;18:904–916. doi: 10.1016/S1470-2045(17)30376-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Miller T., Hennessy W. Hyperactivation of phosphatidylinositol-3 kinase promotes escape from hormone dependence in estrogen receptor-positive human breast cancer. J. Clin. Investig. 2010;120:2406–2413. doi: 10.1172/JCI41680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miller T., Rexer W. Mutations in the phosphatidylinositol 3-kinase pathway: Role in tumor progression and therapeutic implications in breast cancer. Breast Cancer Res. 2011;13:224. doi: 10.1186/bcr3039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maira S.M., Pecchi S. Identification and characterization of NVP-BKM120, an orally available pan-class I PI3-kinase inhibitor. Mol. Cancer Ther. 2012;11:317–328. doi: 10.1158/1535-7163.MCT-11-0474. [DOI] [PubMed] [Google Scholar]
- 27.Sanchez C.G., Ma C.X. Preclinical modeling of combined phosphatidylinositol-3-kinase inhibition with endocrine therapy for estrogen receptor-positive breast cancer. Breast Cancer Res. 2011;13:R21. doi: 10.1186/bcr2833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ma C.X., Luo J. A phase I trial of BKM120 (Buparlisib) in combination with fulvestrant in postmenopausal women with estrogen receptor-positive metastatic breast cancer. Clin. Cancer Res. 2016;22:1583–1591. doi: 10.1158/1078-0432.CCR-15-1745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bendell J.C., Rodon J. Phase I, dose-escalation study of BKM120, an oral pan-Class I PI3K inhibitor, in patients with advanced solid tumors. J. Clin. Oncol. 2012;30:282–290. doi: 10.1200/JCO.2011.36.1360. [DOI] [PubMed] [Google Scholar]
- 30.Mayer I.A., Abramson V.G. Stand up to cancer phase Ib study of pan-phosphoinositide-3-kinase inhibitor buparlisib with letrozole in estrogen receptor-positive/human epidermal growth factor receptor 2-negative metastatic breast cancer. J. Clin. Oncol. 2014;32:1202–1209. doi: 10.1200/JCO.2013.54.0518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Di Leo A., Johnston S. Buparlisib plus fulvestrant in postme nopausal women with hormone-receptor-positive, HER2-negative, advanced breast cancer progressing on or after mTOR inhibition (BELLE-3): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2018;19:87–100. doi: 10.1016/S1470-2045(17)30688-5. [DOI] [PubMed] [Google Scholar]
- 32.Baselga J., Sellami D. Abstract A050: PIK3CA mutation status in tumor tissue and ctDNA as a biomarker for PFS in patients with HRþ, HER2- ABC treated with buparlisib or placebo plus fulvestrant: Results from the BELLE-2 and BELLE-3 randomized studies. Mol. Cancer Ther. 2018;17((Suppl. 1)):A050. [Google Scholar]
- 33.Chang D.Y., Ma W.L. Role of Alpelisib in the Treatment of PIK3CA-Mutated Breast Cancer: Patient Selection and Clinical Perspectives (Review) Ther. Clin. Risk Manag. 2021;17:193–207. doi: 10.2147/TCRM.S251668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nanni P., Nicoletti G. Multiorgan metastasis of human HER-2+ breast cancer in Rag2−/−;Il2rg−/− mice and treatment with PI3K inhibitor. PLoS ONE. 2012;7:e39626. doi: 10.1371/journal.pone.0039626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Martín M., Chan A., Dirix L., O’Shaughnessy J., Hegg R., Manikhas A., Delaloge S. A randomized adaptive phase II/III study of buparlisib, a pan-class I PI3K inhibitor, combined with paclitaxel for the treatment of HER2- advanced breast cancer (BELLE-4) Ann. Oncol. 2017;28:313–320. doi: 10.1093/annonc/mdw562. [DOI] [PubMed] [Google Scholar]
- 36.Folkes A., Ahmadi. K. The identification of 2-(1Hindazol-4-yl)-6-(4-methanesulfonyl-piperazin-1-ylmethyl)-4-morpholin-4-yl-thieno[3, 2-d]pyrimidine (GDC-0941) as a potent, selective, orally bioavailable inhibitor of class I PI3 kinase for the treatment of cancer. J. Med. Chem. 2008;51:5522–5532. doi: 10.1021/jm800295d. [DOI] [PubMed] [Google Scholar]
- 37.Sarker D., Ang J.E. First-in-human phase I study of pictilisib (GDC-0941), a potent pan-class I phosphatidylinositol-3-kinase (PI3K) inhibitor, in patients with advanced solid tumors. Clin. Cancer Res. 2015;21:77–86. doi: 10.1158/1078-0432.CCR-14-0947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schmid P., Pinder S.E. Phase II randomized preoperative window-of-opportunity study of the PI3K inhibitor pictilisib plus anastrozole compared with anastrozole alone in patients with estrogen receptor-positive breast cancer. J. Clin. Oncol. 2016;34:1987–1994. doi: 10.1200/JCO.2015.63.9179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Krop I.E., Mayer I.A. Pictilisib for oestrogen receptor-positive, aromatase inhibitor-resistant, advanced or metastatic breast cancer (FERGI): A randomised, double-blind, placebo-controlled, phase 2 trial. Lancet Oncol. 2016;17:811–821. doi: 10.1016/S1470-2045(16)00106-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vuylsteke P., Huizing M. Pictilisib PI3Kinase inhibitor (a phosphatidylinositol 3-kinase [PI3K] inhibitor) plus paclitaxel for the treatment of hormone receptor-positive, HER2-negative, locally recurrent, or metastatic breast cancer: Interim analysis of the multicentre, placebo-controlled, phase II randomised PEGGY study. Ann. Oncol. 2016;27:2059–2066. doi: 10.1093/annonc/mdw320. [DOI] [PubMed] [Google Scholar]
- 41.Bahrami A., Khazaei M. The therapeutic potential of PI3K/AKT/ mTOR inhibitors in breast cancer: Rationale and progress. J. Cell Biochem. 2018;119:213–222. doi: 10.1002/jcb.26136. [DOI] [PubMed] [Google Scholar]
- 42.Berns K., Horlings H.M. A functional genetic approach identifies the PI3K pathway as a major determinant of trastuzumab resistance in breast cancer. Cancer Cell. 2007;12:395–402. doi: 10.1016/j.ccr.2007.08.030. [DOI] [PubMed] [Google Scholar]
- 43.Pernas S., Tolaney S.M. HER2-positive breast cancer: New therapeutic frontiers and overcoming resistance. Ther. Adv. Med. Oncol. 2019;11:1758835919833519. doi: 10.1177/1758835919833519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Baselga J., Cortes J. Biomarker analyses in CLEOPATRA: A phase III, placebo-controlled study of pertuzumab in human epidermal growth factor receptor 2-positive, firstline metastatic breast cancer. J. Clin. Oncol. 2014;32:3753–3761. doi: 10.1200/JCO.2013.54.5384. [DOI] [PubMed] [Google Scholar]
- 45.Baselga J., Lewis G. Relationship between tumor biomarkers and efficacy in EMILIA, a phase III study of trastuzumab emtansine in HER2-positive metastatic breast cancer. Clin. Cancer Res. 2016;22:3755–3763. doi: 10.1158/1078-0432.CCR-15-2499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chandarlapaty S., Sakr R.A. Frequent mutational activation of the PI3K-AKT pathway in trastuzumab-resistant breast cancer. Clin. Cancer Res. 2012;18:6784–6791. doi: 10.1158/1078-0432.CCR-12-1785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wilks S. Potential of overcoming resistance to HER2-targeted therapies through the PI3K/Akt/mTOR pathway. Breast. 2015;24:548–555. doi: 10.1016/j.breast.2015.06.002. [DOI] [PubMed] [Google Scholar]
- 48.Li H., Prever L. Targeting PI3K/AKT/mTOR Signaling Pathway in Breast Cancer (Review) Cancers. 2021;13:3517. doi: 10.3390/cancers13143517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hanker A.B., Pfefferl A.D. Mutant PIK3CA accelerates HER2-driven transgenic mammary tumors and induces resistance to combinations of anti-HER2 therapies. Proc. Natl. Acad. Sci. USA. 2013;110:14372–14377. doi: 10.1073/pnas.1303204110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Saura C., Bendell J. Phase Ib study of buparlisib plus trastuzumab in patients with HER2-positive advanced or metastatic breast cancer that has progressed on Trastuzumab-based therapy. Clin. Cancer Res. 2014;20:1935–1945. doi: 10.1158/1078-0432.CCR-13-1070. [DOI] [PubMed] [Google Scholar]
- 51.Pistilli B., Pluard T. Phase II study of buparlisib (BKM120) and trastuzumab in patients with HER2+ locally advanced or metastatic breast cancer resistant to trastuzumab-based therapy. Breast Cancer Res. Treat. 2018;168:357–364. doi: 10.1007/s10549-017-4596-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Guerin M., Rezai K. PIKHER2: A phase IB study evaluating buparlisib in combination with lapatinib in trastuzumabresistant HER2-positive advanced breast cancer. Eur. J. Cancer. 2017;86:28–36. doi: 10.1016/j.ejca.2017.08.025. [DOI] [PubMed] [Google Scholar]
- 53.Zhang Z., Richmond A. The Role of PI3K Inhibition in the Treatment of Breast Cancer, Alone or Combined with Immune Checkpoint Inhibitors. Front. Mol. Biosci. 2021;8:648663. doi: 10.3389/fmolb.2021.648663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Poggio F., Bruzzone M. Platinum-based neoadjuvant chemotherapy in triple-negative breast cancer: A systematic review and meta-analysis. Ann. Oncol. 2018;29:1497–1508. doi: 10.1093/annonc/mdy127. [DOI] [PubMed] [Google Scholar]
- 55.Byrski T., Dent R. Results of a phase II open-label, non-randomized trial of cisplatin chemotherapy in patients with BRCA1-positive metastatic breast cancer. Breast Cancer Res. 2012;14:R110. doi: 10.1186/bcr3231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tutt A., Tovey H. Carboplatin in BRCA1/2-mutated and triple-negative breast cancer BRCAness subgroups: The TNT Trial. Nat. Med. 2018;24:628–637. doi: 10.1038/s41591-018-0009-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Robson M., Im S.A. Olaparib for metastatic breast cancer in patients with a germline BRCA mutation. N. Engl. J. Med. 2017;377:523–533. doi: 10.1056/NEJMoa1706450. [DOI] [PubMed] [Google Scholar]
- 58.Litton J.K., Rugo H.S. Talazoparib in patients with advanced breast cancer and a germline BRCA mutation. N. Engl. J. Med. 2018;379:753–763. doi: 10.1056/NEJMoa1802905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Turner N.C., Telli M.L. Final results of a phase 2 study of talazoparib (TALA) following platinum or multiple cytotoxic regimens in advanced breast cancer patients (pts) with germline BRCA1/2 mutations (ABRAZO) J. Clin. Oncol. 2017;35((Suppl. 15)):1007. doi: 10.1200/JCO.2017.35.15_suppl.1007. [DOI] [Google Scholar]
- 60.Andrè F., Zielinski C.C. Optimal strategies for the treatment of metastatic triple-negative breast cancer with currently approved agents. Ann. Oncol. 2012;23:vi46–vi51. doi: 10.1093/annonc/mds195. [DOI] [PubMed] [Google Scholar]
- 61.Shah S.P., Roth A. The clonal and mutational evolution spectrum of primary triple-negative breast cancers. Nature. 2012;486:395–399. doi: 10.1038/nature10933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pascual J., Turner N.C. Targeting the PI3-kinase pathway in triple negative breast cancer. Ann. Oncol. 2019;30:1051–1060. doi: 10.1093/annonc/mdz133. [DOI] [PubMed] [Google Scholar]
- 63.Drullinsky P.R., Hurvitz S.A. Mechanistic basis for PI3K inhibitor antitumor activity and adverse reactions in advanced breast cancer. Breast Cancer Res. Treat. 2020;181:233–248. doi: 10.1007/s10549-020-05618-1. [DOI] [PubMed] [Google Scholar]
- 64.Peng W., Chen J.Q. Loss of PTEN promotes resistance to T cell-mediated immunotherapy. Cancer Discov. 2016;6:202–216. doi: 10.1158/2159-8290.CD-15-0283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.LoRusso P. Inhibition of the PI3K/AKT/mTOR pathway in solid tumors. J. Clin. Oncol. 2016;34:3803–3815. doi: 10.1200/JCO.2014.59.0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ibrahim Y.H., Garcia G. PI3K inhibition impairs BRCA1/2 expression and sensitizes BRCA-proficient triple-negative breast cancer to PARP inhibition. Cancer Discov. 2012;2:1036–1047. doi: 10.1158/2159-8290.CD-11-0348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Juvekar A., Burga L.N. Combining a PI3K inhibitor with a PARP inhibitor provides an effective therapy for BRCA1-related breast cancer. Cancer Discov. 2012;2:1048–1063. doi: 10.1158/2159-8290.CD-11-0336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Matulonis U.A., Wulf G.M. Phase I dose escalation study of the PI3kinase pathway inhibitor BKM120 and the oral poly (ADP ribose) polymerase (PARP) inhibitor olaparib for the treatment of highgrade serous ovarian and breast cancer. Ann. Oncol. 2017;28:512–518. doi: 10.1093/annonc/mdw672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.André F., Ciruelos E. Alpelisib for PIK3CA-Mutated, Hormone Receptor–Positive Advanced Breast Cancer. N. Engl. J. Med. 2019;380:1929–1940. doi: 10.1056/NEJMoa1813904. [DOI] [PubMed] [Google Scholar]
- 70.André F., Ciruelos E.M. Overall survival (os) results from SOLAR-1, a phase III study of alpelisib (ALP) + fulvestrant (FUL) for hormone receptor-positive (HR+), human epidermal growth factor receptor 2-negative (HER2−) advanced breast cancer (ABC) Ann. Oncol. 2020;31((Suppl. 4)):S1150–S1151.76. doi: 10.1016/j.annonc.2020.08.2246. [DOI] [PubMed] [Google Scholar]
- 71.Baselga J., Dent S.F. Phase III study of taselisib (GDC-0032) + fulvestrant (FULV) v FULV in patients (pts) with estrogen receptor (ER)-positive, PIK3CA-mutant (MUT), locally advanced or metastatic breast cancer (MBC): Primary analysis from SANDPIPER. J. Clin. Oncol. 2018;36((Suppl. 18)):LBA1006. doi: 10.1200/JCO.2018.36.18_suppl.LBA1006. [DOI] [Google Scholar]
- 72.Rugo H.S., Lerebours F. Alpelisib (ALP) + fulvestrant (FUL) in patients (pts) with PIK3CA-mutated (mut) hormone receptor-positive (HR+), human epidermal growth factor receptor 2-negative (HER2−) advanced breast cancer (ABC) previously treated with cyclin-dependent kinase 4/6 inhibitor (CDKi) + aromatase inhibitor (AI): BYLieve study results. J. Clin. Oncol. 2020;38:1006. [Google Scholar]
- 73.Mavratzas A., Marmé F. Alpelisib in the treatment of metastatic HR+ breast cancer with PIK3CA mutations. Future Oncol. 2021;17:13–36. doi: 10.2217/fon-2020-0464. [DOI] [PubMed] [Google Scholar]
- 74.Juric D., Rodon J. Phosphatidylinositol 3-kinase α-selective inhibition with alpelisib (BYL719) in PIK3CA-altered solid tumors: Results from the first-in-human study. J. Clin. Oncol. 2018;36:1291–1299. doi: 10.1200/JCO.2017.72.7107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Juric D., Janku F. Alpelisib Plus Fulvestrant in PIK3CA-altered and PIK3CA-wild-Type Estrogen Receptor-Positive Advanced Breast Cancer. JAMA Oncol. 2019;5:e184475. doi: 10.1001/jamaoncol.2018.4475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bertucci F., Finetti P. Comparative genomic analysis of primary tumors and metastases in breast cancer. Oncotarget. 2016;7:27208–27219. doi: 10.18632/oncotarget.8349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Jeselsohn R., Yelensky R. Emergence of constitutively active estrogen receptor-α mutations in pretreated advanced estrogen receptor-positive breast cancer. Clin. Cancer Res. 2014;20:1757–1767. doi: 10.1158/1078-0432.CCR-13-2332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Higgins M.J., Jelovac D. Detection of tumor PIK3CA status in metastatic breast cancer using peripheral blood. Clin. Cancer Res. 2012;18:3462–3469. doi: 10.1158/1078-0432.CCR-11-2696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Juric D., Andre F. Abstract P4-10-04: Clinical outcomes of alpelisib in hormone receptor-positive, human epidermal growth factor receptor-2-negative advanced breast cancer by next-generation sequencing-detected PIK3CA alteration status and phosphatase and tensin homolog loss: Biomarker analysis from the SOLAR-1 study. Cancer Res. 2020;80((Suppl. 4)):P4-10-04. [Google Scholar]
- 80.Lu Y.S., Lee K.S. A phase Ib study of alpelisib or buparlisib combined with tamoxifen plus goserelin in premenopausal women with HR-positive HER2-negative advanced breast cancer. Clin. Cancer Res. 2020;27:408–417. doi: 10.1158/1078-0432.CCR-20-1008. [DOI] [PubMed] [Google Scholar]
- 81.Juric D., Krop I.K. Abstract LB-64: GDC-0032, a beta isoform-sparing PI3K inhibitor: Results of a first-in-human phase Ia dose escalation study. Cancer Res. 2013;73:LB-64. [Google Scholar]
- 82.Olivero A., Heffron T. Discovery of GDC-0032: A beta-sparing PI3K inhibitor active against PIK3CA mutant tumors. Cancer Res. 2013;73:DDT02-01. [Google Scholar]
- 83.Juric D., Krop I. Phase I dose-escalation study of taselisib, an oral PI3K inhibitor, in patients with advanced solid tumors. Cancer Discov. 2017;7:704–715. doi: 10.1158/2159-8290.CD-16-1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ndubaku C.O., Heffron T.P. Discovery of 2-{3-[2-(1-isopropyl-3-methyl-1H-1,2-4-triazol-5-yl)-5,6-dihydrobenzo[f]imidazo[1,2-d][1,4]oxazepin-9-yl]-1H-pyrazol-1-yl}-2-methylpropanamide (GDC-032): A b-sparing phosphoinositide 3-kinase inhibitor with high unbound exposure and robust in vivo antitumor activity. J. Med. Chem. 2013;56:4597–4610. doi: 10.1021/jm4003632. [DOI] [PubMed] [Google Scholar]
- 85.Pohlmann P.R., Mayer I.A. Resistance to Trastuzumab in Breast Cancer. Clin. Cancer Res. 2009;15:7479–7491. doi: 10.1158/1078-0432.CCR-09-0636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Junttila T.T., Akita R.W. Ligand-independent HER2/HER3/PI3K complex is disrupted by trastuzumab and is effectively inhibited by the PI3K inhibitor GDC-0941. Cancer Cell. 2009;15:429–440. doi: 10.1016/j.ccr.2009.03.020. [DOI] [PubMed] [Google Scholar]
- 87.Jain S., Shah A.N. Phase I study of alpelisib (BYL-719) and trastuzumab emtansine (T-DM1) in HER2-positive metastatic breast cancer (MBC) after trastuzumab and taxane therapy. Breast Cancer Res. Treat. 2018;171:371–381. doi: 10.1007/s10549-018-4792-0. [DOI] [PubMed] [Google Scholar]
- 88.Barok M., Tanner M. Trastuzumab-DM1 causes tumour growth inhibition by mitotic catastrophe in trastuzumab-resistant breast cancer cells in vivo. Breast Cancer Res. 2011;13:R46. doi: 10.1186/bcr2868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Merlino G., Fiascarelli A. Abstract 2160: MEN1611, a novel α-selective PI3K inhibitor in solid tumors. Cancer Res. 2018;78((Suppl. 13)):2160. [Google Scholar]
- 90.Fiascarelli A., Merlino G. Characterization of the mechanism of action and efficacy of MEN1611 (PA799), a novel PI3K inhibitor, in breast cancer preclinical models. Ann Oncol. 2019;30((Suppl. 5)):v781–v782. doi: 10.1093/annonc/mdz268.065. [DOI] [Google Scholar]
- 91.Hansen A.R., Shapiro G. A first in human phase I study of AZD8186, a potent and selective inhibitor of PI3K in patients with advanced solid tumours as monotherapy and in combination with the dual mTORC1/2 inhibitor vistusertib (AZD2014) or abiraterone acetate. J. Clin. Oncol. 2017;35:2570. doi: 10.1200/JCO.2017.35.15_suppl.2570. [DOI] [Google Scholar]
- 92.Owusu-Brackett N., Zhao M. Targeting PI3K alone and in combination with chemotherapy or immunotherapy in tumors with PTEN loss. Oncotarget. 2020;11:969–981. doi: 10.18632/oncotarget.27503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Liu Z., Zhu G. The upregulation of PI3K/Akt and MAP kinase pathways is associated with resistance of microtubule-targeting drugs in prostate cancer. J. Cell. Biochem. 2015;116:1341–1349. doi: 10.1002/jcb.25091. [DOI] [PubMed] [Google Scholar]
- 94.Rodon J., Curigliano G. A Phase Ib, open-label, dose-finding study of alpelisib in combination with paclitaxel in patients with advanced solid tumors. Oncotarget. 2018;9:31709–31718. doi: 10.18632/oncotarget.25854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Sharma P., Abramson V.G. Safety and efficacy results from Phase I study of BYL719 plus nab-paclitaxel in HER-2 negative metastatic breast cancer. Cancer Res. 2017;77((Suppl. 4)):P6-11-08. [Google Scholar]
- 96.Sharma P., Abramson V.G. Clinical and biomarker results from phase I/II study of PI3K inhibitor BYL 719 (alpelisib) plus nab-paclitaxel in HER2-negative metastatic breast cancer. J. Clin. Oncol. 2018;36:1018. doi: 10.1200/JCO.2018.36.15_suppl.1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Asghar U.S., Barr A.R. Single-cell dynamics determines response to CDK4/6 inhibition in triple-negative breast cancer. Clin. Cancer Res. 2017;23:5561–5572. doi: 10.1158/1078-0432.CCR-17-0369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lehmann B.D., Bauer J.A. PIK3CA mutations in androgen receptor-positive triple negative breast cancer confer sensitivity to the combination of PI3K and androgen receptor inhibitors. Breast Cancer Res. 2014;16:406. doi: 10.1186/s13058-014-0406-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lopez J.S., Miralles M.S. PIPA: A phase Ib study of selective ß-isoform sparing phosphatidylinositol 3-kinase (PI3K) inhibitor taselisib (T) plus palbociclib (P) in patients (pts) with advanced solid cancers—Safety, tolerability, pharmacokinetic (PK), and pharmacodynamic (PD) analysis of the doublet combination. J. Clin. Oncol. 2019;37((Suppl. 15)):3087–3308. [Google Scholar]
- 100.Teo Z.L., Versaci S. Combined CDK4/6 and PI3Kα Inhibition Is Synergistic and Immunogenic in Triple-Negative Breast Cancer. Cancer Res. 2017;77:6340–6352. doi: 10.1158/0008-5472.CAN-17-2210. [DOI] [PubMed] [Google Scholar]
- 101. [(accessed on 8 February 2022)]; Available online: https://clinicaltrials.gov/ct2/show/study/NCT04191499.
- 102. [(accessed on 15 February 2022)]; Available online: https://clinicaltrials.gov/ct2/show/NCT04355520.
- 103. [(accessed on 15 February 2022)]; Available online: https://clinicaltrials.gov/ct2/show/NCT05025735.
- 104. [(accessed on 8 February 2022)]; Available online: https://clinicaltrials.gov/ct2/show/NCT03006172.
- 105. [(accessed on 15 February 2022)]; Available online: https://clinicaltrials.gov/ct2/show/study/NCT04108858.
- 106. [(accessed on 15 February 2022)]; Available online: https://clinicaltrials.gov/ct2/show/study/NCT04208178.
- 107. [(accessed on 15 February 2022)]; Available online: https://clinicaltrials.gov/ct2/show/NCT03767335.
- 108. [(accessed on 16 February 2022)]; Available online: https://www.clinicaltrials.gov/ct2/show/NCT04586335.
- 109. [(accessed on 16 February 2022)]; Available online: https://clinicaltrials.gov/ct2/show/study/NCT03218826.
- 110. [(accessed on 15 February 2022)]; Available online: https://www.clinicaltrials.gov/ct2/show/NCT04251533.
- 111. [(accessed on 16 February 2022)]; Available online: https://clinicaltrials.gov/ct2/show/NCT03961698.
- 112. [(accessed on 16 February 2022)]; Available online: https://clinicaltrials.gov/ct2/show/NCT02637531.
- 113. [(accessed on 16 February 2022)]; Available online: https://clinicaltrials.gov/ct2/show/NCT02646748.
- 114. [(accessed on 16 February 2022)]; Available online: https://clinicaltrials.gov/ct2/show/study/NCT04345913.
- 115. [(accessed on 16 February 2022)]; Available online: https://clinicaltrials.gov/ct2/show/record/NCT02457910.
- 116. [(accessed on 16 February 2022)]; Available online: https://clinicaltrials.gov/ct2/show/NCT03207529.
- 117.Eltantawy A., Vallejos X. Copanlisib: An Intravenous Phosphatidylinositol 3-Kinase (PI3K) Inhibitor for the Treatment of Relapsed Follicular Lymphoma. Ann. Pharmacother. 2019;53:954–958. doi: 10.1177/1060028019833992. [DOI] [PubMed] [Google Scholar]
- 118. [(accessed on 15 February 2022)]; Available online: https://clinicaltrials.gov/ct2/show/NCT05063786.
- 119.Kaneda M., Messer K. PI3Kγ is a molecular switch that controls immune suppression. Nature. 2016;539:437–442. doi: 10.1038/nature19834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.De Henau O., Rausch M. Overcoming resistance to checkpoint blockade therapy by targeting PI3Kγ in myeloid cells. Nature. 2016;539:443–447. doi: 10.1038/nature20554. [DOI] [PMC free article] [PubMed] [Google Scholar]


