Summary
Introduction
COVID-19 pandemic has affected the self-management of patients with chronic disease all over the world. The present study COVID-19 is a review to investigate the chronic patient self-management challenges during the corona epidemic, and providing solutions to solve this problem.
Methods
The relevant literature on chronic patient self-management is investigated (from March 2019 to Jan 2021). Databases including Google Scholar, PubMed, Science Direct, Springer were used to search articles from the Latin articles. Also, keywords in this study included self-management, chronic disease, COVID-19. Finally, 26 relevant articles were used in this study.
Results
Studies assessed the effective role of self-management in control and prevention of complications of chronic diseases and the challenges related to self-management programs during COVID-19, in addition the role of the health team in patients’ self-management during the corona epidemics.
Conclusion
the main challenges for chronic patients during the COVID-19 include decreased healthcare service and regular follow-ups because of physical restrictions; economic problems, change in lifestyle, and lack of rapid compliance with the changes. In this regard, the health team should provide the best healthcare services using the available resources to reduce suffer and pain of the patients.
Keywords: Self-management, Chronic diseases, COVID-19
Introduction
On 11 March 2020, the World Health Organization (WHO) announced the COVID-19 disease as a pandemic. The disease has caused a high mortality rate across the world to date. In the meantime, the risk of morbidity and mortality due to the COVID-19 is high in people with chronic diseases such as diabetes, hypertension, cardiovascular diseases, chronic obstructive pulmonary disease, and weakened immune system compared to the normal population [1-5]. Many efforts have been taken to produce the vaccine and definite treatment of the COVID pandemic in the world. These efforts have led to restricted access to the vaccine. According to academic evidence, specific drugs for COVID are not available. Hence, the best option here is trying to use preventive methods and to take self-management behaviors in chronic patients [1, 6].
According to the declaration of the WHO, 35% of women and 29% of men suffer from chronic diseases such as cardiovascular diseases, chronic pulmonary diseases, or diabetes. Such prevalence of chronic diseases has left abundant negative effects on the workforce of different countries. Self-management is very important to save resources and improve the ability of patients. The results of interventions under the title of Chronic Disease Self-Management Program (CDSMP) made by the Stanford University of America in this country and more than 20 other countries (Canada, Australia, Argentina, England, Denmark, Spain, Coast Arica, and China) 40 years ago show that included individuals have acted successfully in the field of self-management of health [7].
The implementation of health instructions and protocols, such as social distancing and quarantine for reducing the spread of COVID-19 disease and transmission between carriers and healthy individuals has disrupted the treatment and self-management process of chronic patients. For example, the implementation of social distancing and quarantine has result in a significant reduction in regular visits of a patient with specialists to check their health status. Also, the pharmaceutical reserves have been decreased in some regions because of the closure of drug production plants. On the other hand, many patients have lost their insurance coverage because of unemployment caused by the corona pandemic and have encountered problems with treatment costs [8, 9]. Besides, as the sources, equipment, and healthcare forces of states to control the COVID-19 pandemic, the chronic patients have trouble in access to healthcare services [10-12].
Health service providers are vital elements of societies, the health, and security of whom are significant not only for the continuous care of patients but also to control the prevalence of diseases. For example, the description presented by the health service providers of China based on their face-to-face experience on fighting COVID-19 was a responsibility to reduce pain and suffer from the patients and common effort to protect the country against the virus. This is because they believed in this sentence “everyone is responsible for the advent or collapse of his-her country”. Health service providers play a key role in the treatment of COVID-19 patients. The majority of these healthcare providers have little clinical experience working in the units of special infectious diseases. However, when healthcare systems are not ready to fight infectious disease, the health service providers help the system by gaining knowledge and skill and improving their communications in intensive training courses by accepting the risks and injuries caused by this disease. Health service providers need continuous medical training to cope with emergencies and to become ready under conditions like the corona pandemic. Healthcare systems must seek inter-professional, and inter-organizational cooperation to provide high-quality and efficient care because of the variety of organizational culture [13-17].
We aimed to assess the global impact of COVID-19 on self-management in chronic diseases and its challenges and evaluate the role of health care workers to support and improve patient care.
Method
SEARCH STRATEGY
This study is a narrative review conducted in 2019-2020. This study is focused on relevant works of chronic patient self-management during the corona pandemic from March 2019 to Jan 2021. To search Latin articles, databases including Google Scholar, PubMed, Science Direct, and Springer were used. The search strategy consisted of the combination of the following Boolean keywords and operators: (COVID-19 OR “Coronavirus 2” AND “chronic disease” OR “chronic condition” AND (“self-management”). Figure 1 shows the flowchart relating to the process of finding and selecting the studies included in this narrative.
Fig. 1.
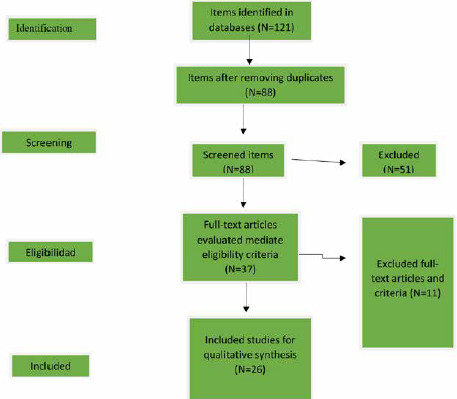
Flowchart of the process of searching and selecting the studies.
ELIGIBILITY CRITERIA
The articles were used in the study based on inclusion criteria including being relevant to the research objective, using structures framework including keywords including self-management, chronic disease, and COVID-19 in the abstract. Also, Latin articles with the availability of full text entered into the study. Figure 1 shows the flowchart of the search and selection process for the included studies. The exclusion criteria included works on diseases other than chronic diseases, repetitive works, and unavailable books.
REMOVING AND ANALYZING DATA
In the initial search based on the said keywords, 121 articles were collected. by studying the abstract and full text, 26 articles were selected based on inclusion and exclusion criteria, and elimination of repetitive and irrelevant cases. Two researchers who independently reviewed the titles have evaluated the data extracted and summaries of the articles found, considering the eligibility criteria. Disagreements were resolved by discussion, or in the event of no agreement by a four reviewers or researcher.
Results
In this study, 26 qualified Latin articles were used. The results obtained from the reviewed studies were classified into 3 major domains
SIGNIFICANCE OF SELF-MANAGEMENT IN CHRONIC DISEASES
8 out of the 26 articles used in the study explained self-management in chronic diseases. Self-management in chronic patients is one of the best solutions to promote health and improve the quality of life (Tab. I). Sharif Ali et al presented a review on analyzing the positive effects of self-management on the emotional, behavioral, and social-mental domains, and the individual skills of diabetes patients [18]. Al Grant et al conducted a systematic and meta-analysis review on chronic patients such as diabetes, cardiovascular, and arthritis patients. In this study, they referred to the role of self-management to improve the quality of life and to reduce using healthcare system resources [19]. Banerji et al mentioned in a review that training self-management by healthcare cadre during the corona pandemic to diabetes patients plays a key role in the achievement of treatment purposes of these patients [20].
Tab. I.
The specifications relevant to the significance of self-management in chronic diseases.
| Row | Author/ place/ year | Purpose | Article type | Target population | Results |
|---|---|---|---|---|---|
| 1 | Tan SS, et al. 2019 [7] | Evaluation of self-management programs in chronic patients | Clinical trial | Chronic patients | Implementation of a self-management program (CDSMP) could increase the ability of patients in self-management |
| 2 | Van de Velde D, et al. 2019 [26] | Analysis of the self-management concept in chronic diseases | Concept analysis | Relevant articles on the self-management concept | The self-management should be considered in healthcare systems as an educational program |
| 3 | Wainwright T, Low M 2020 [27] | Analysis of the reason for participatory self-management and its role in rehabilitation programs of COVID-19 patients | Letter to editor | - | Participatory self-management should be considered as an essential element in the rehabilitation programs of COVID-19 patients |
| 4 | Ghosh A, Gupta R, Misra A 2020 [28] | The effect of telemedicine in diabetes self-management during the COVID epidemic | Review | Relevant articles | Telemedicine is a useful tool for self-management of diabetes patients during the COVID epidemic |
| 5 | Izzedine H, Jhaveri KD, Perazella MA 2020 [29] | Analysis of the treatment options of COVID-19 in kidney patients | Letter to editor | Renal patients with COVID-19 | Pharmacological treatment in kidney patients with COVID-19 should be modified concerning side effects of medicine and effects on kidney function |
| 6 | Plevinsky JM, et al. 2020 [30] | Analysis of the effect of COVID-19 on self-management and treatment follow-up in kids | Original paper | Kids with chronic diseases | Supporting kids with chronic diseases and their families is essential for the healthcare team to enhance their coping with the changes caused by the COVID epidemic, and access to modern medications, such as telemedicine programs |
| 7 | Leonardi M, et al. 2020 [31] | Analysis of the effect of self-management strategies on symptoms of patients with endometriosis during the corona epidemic | Original paper | Endometriosis patients | Effectiveness of using non-pharmacological methods, along with using diet regime, to reduce the symptoms of endometriosis patients |
| 8 | Kaye L, et al. 2020 [32] | Analysis of change in treatment follow-up procedures and self-management of COPD and asthma patients during the corona epidemic | Original paper | Patients with COPD and asthma | Following treatment in COPD and asthma patients in the first weak of corona lead to reduced need to treat the severe pulmonary complications of these patients |
SELF-MANAGEMENT CHALLENGES DURING THE COVID EPIDEMIC
10 out of 26 articles were focused on self-management challenges during the COVID-19 epidemic (Tab. II). According to the nature of chronic diseases and imposing unwanted and unpleasant conditions of the disease such as tolerating continuous pain and stress, and long-term treatment process causes necessity of frequent references to the healthcare systems, attachment of these systems to healthcare team to control the disease, and regular monitoring of self-management program [21]. However, the healthcare systems have reduced access to hospitals and visits for chronic patients during the corona epidemic because of managing the disease. This can make disruption in quality of life, and the treatment process of these patients [22]. For example, Banerji et al have conducted a study and referred to challenges such as a change in lifestyle, on-time unavailability of resources, and health team reducing the awareness of diabetes patients to control the disease and the mental effects of these restrictions [20].
Tab. II.
The specifications of relevant studies of self-management challenges during the COVID-19 pandemic.
| Row | Author/ place/ year | Purpose | Article type | Target population | Results |
|---|---|---|---|---|---|
| 1 | Brigo F, et al. 2020 [8] | Analysisof self-management challenges of epilepsy disease during the corona epidemic | Letter to editor | Telemedicine is an effective tool for the management of epilepsy under severe conditions such as the COVID-19 epidemic | |
| 2 | Hartmann-Boyce J, et al. 2020 [9] | Analysis of risks and management of diabetes during the COVID epidemic using the experiences of past crises | Review | Diabetes patients with COVID-19 | According to the effects of COVID-19 on diabetes, it is necessary to reduce the risks of the crisis with proper management based on past experiences |
| 3 | Huang S, et al. 2020 [11] | Analysis of the effect of using online management on two patients with COVID-19 | Case report | COVID-19 patients | The positive effect of using online management on the improvement of symptoms and self-management of COVID patients |
| 4 | Karasavvidis T, et al. 2020 [12] | Analysis of the effect of using home-oriented management in knee osteoarthritis patients during the COVID epidemic | Systematic review | Patients with knee osteoarthritis | The results show the effectiveness of home-oriented management in knee osteoarthritis patients during the corona epidemic |
| 5 | Elbeddini A, Tayefehchamani Y 2020 [22] | Analysis of the limitations and challenges in COPD patients during the COVID epidemic | Original paper | Copd patients | The challenges and limitations for these patients include limitations in self-management, advanced medication programs, online service providing because of decreased access of patients to healthcare services in person, and lack of specialized guidelines for doctors in the field of changes in disease management during the COVID epidemic |
| 6 | Chang AY, et al. 2020 [33] | Analysis of the effect of COVID-19 on chronic patients | Review | Chronic patients | The complications of COVID-19 in chronic patients may be continued for a long time after acute phase treatment |
| 7 | Goodsall TM, Sangwoo H, Bryant RV 2020 [34] | Analysis of the attitude, health behaviors, and concerns of patients with inflammatory bowel disease during the COVID-19 epidemic | Original paper | Patients with inflammatory bowel disease | Using methods such as telemedicine, non-invasive analysis, education, and informing patients can reduce concerns and cause desirable changes in the health behaviors of these patients during the COVID epidemic |
| 8 | Shimada N, et al. 2020 [35] | Analysis of the effects of COVID-19 on ESKD patients | Review | ESKD patients | Some changes should be made in the treatment methods of ESKD patients with COVID-19 so that they can continue living under corona epidemic conditions |
| 9 | Liu Q, et al. 2020 [16] | Analysis of the experiences of the healthcare team during the COVID-19 epidemic in China | Original paper | Healthcare team | According to the unpleasant consequences of COVID-19 on the physical and mental conditions of the healthcare team. And its impact on the management and medical interventions in the epidemic, comprehensive supports are needed |
| 10 | Korytkowski M, et al. 2020 [36] | Analysis of practical approaches in the management of diabetic patients during the COVID epidemic | Original paper | Diabetic patients | Positive results of using various treatments in the management of diabetic patients, such as positive effect on self-management of these patients |
THE ROLE OF THE HEALTH TEAM IN THE SELF-MANAGEMENT OF PATIENTS DURING THE CORONA EPIDEMIC
Among entered studies, 9 articles were focused on the role of the healthcare team in the self-management of patients during the corona pandemic (Tab. III). The increased number of chronic diseases has made abundant challenges for the healthcare team. As the healthcare team tends to use specialized sources and facilities to support the patients and create high-quality life, providing information and making self-confidence in patients to take proper self-care behavior can be some part of the supportive plan of personnel for self-management of these patients. This can finally improve the quality of life, reduce anxiety and stress, and improve the adaptability and physical performance of patients under special conditions [23]. Hence, according to the outcomes of the COVID-19, the health team should provide programs and facilities for the patients and their families to support the self-management plans of chronic patients [24].
Tab. III.
The specifications of studies relevant to the role of the healthcare team in the self-management of patients during the COVID pandemic.
| Row | Author/ place/ year | Purpose | Article type | Target population | Results |
|---|---|---|---|---|---|
| 1 | Arlt W, et al. 2020 [37] | Analysis of the role of the healthcare team in the improvement of clinical conditions of patients with adrenal insufficiency | Original paper | Patients with adrenal insufficiency | The efforts of the healthcare team to improve self-management of patients using methods such as training, empowerment, and providing equipment, and required medicine of these patients in the epidemic |
| 2 | Xu H, et al. 2020 [38] | Analysis of the effect of telemedicine via WeChat applications for monitoring and management of COVID patients during the home quarantine | Retrospective cohort | COVID-19 patients | Using telemedicine based on We-Chat application by the healthcare team to reduce the prevalence of COVID in the society |
| 3 | Bajwah S, et al. 2020 [39] | Analysis of the role of the healthcare team for management and meeting supportive needs of COVID-19 patients | Original paper | COVID-19 patients | The healthcare team should use available resources to provide the best care to decrease the suffering and mortality of patients |
| 4 | Garg SK, et al. 2020 [40] | Analysis of the challenges and opportunities for management of patients with type 1 diabetes during the COVID epidemic | Original paper | Patients with type 1 diabetes | The healthcare team should use telemedicine as an effective approach for the management of patients with type 1 diabetes |
| 5 | Bhutani M, et al. 2020 [41] | Analysis of the effect of implementing educational programs to improve performance of health team for self-management of patients with COPD during the corona epidemic | Original paper | Healthcare team | The results can be used in similar environments to empower the healthcare team to improve the self-management of COPD patients during the COVID-19 epidemic |
| 6 | Ballard M, et al. 2020 [42] | Analysis of the priority of healthcare team functions during the COVID epidemic | Original paper | Healthcare team | The performances of the healthcare team should be in line with the goals and protocols determined in the health system, along with matching all health departments for proper management of COVID-19 |
| 7 | Bhaumik S, et al. 2020 [43] | Analysis of the responsibilities of the healthcare team during the COVID epidemic | Review | Healthcare team | Change in functions and responsibilities of the healthcare team during the corona epidemic compared to other epidemics showed that the responsibility of the healthcare team has been increased |
| 8 | Goldfarb N, et al. 2021 [44] | Analysis of the relevant factors of increase in professional promises of nurses during the COVID-19 epidemic | Original paper | Nurses | Factors such as increasing awareness, group work, mental support, and increased self-efficacy of personnel play a key role in increasing professional promises of nurses as the main member of the healthcare team in the COVD-19 epidemic |
Discussion
The present study was conducted to analyze the status of self-management of chronic patients n the COVID-19. According to the results of reviewed articles, they were classified into 3 major groups.
SIGNIFICANCE OF SELF-MANAGEMENT IN CHRONIC DISEASES
The role of self-management interventions has been increasing in the field of providing healthcare services for chronic patients. The results of a systematic review conducted by Panagioti et al. showed that self-management interventions in patients can improve health consequences and decrease the amount of using healthcare services. According to recent studies, it could be found that the definition of health has become more dynamic, and self-management is one of the key concepts in this field [25]. Self-management interventions applied from various methods and programs such as physical activity, educational interventions, and fitness programs among chronic patients have caused high ability of them for management of the disease [26].
Self-management is the best method for caring for chronic patients refers to the active participation of the patient in the management of disease and controlling the lifestyle [27]. Besides, self-management encompasses behaviors including food diet behaviors, pharmacological treatment, monitoring symptoms, sleeping, physical activity, fitness, growing the skills, setting goals, problem-solving, reducing stress, and using operating plans. Chronic patients use self-management as a part of their life, which can enhance the quality of life and can make patients feel healthy [24]. The most important consequences of self-management include an adaptation of chronic patients to the health problems related to their disease. This is because; the patients can diagnose the symptoms of the disease by self-management and awareness of relevant problems, and take effective measures to control them [28]. This can prevent more disabilities and development of the health of these individuals; because self-management in chronic diseases is not just focused on treatment and rehabilitation. It should be noted that achievement to desirable self-management is dependent on facilitating the health services, and meeting communicative barriers between the healthcare team and the patient. Also, it is dependent on providing more cooperation between patients and the healthcare team [29]. This issue has been changed into a challenge for the healthcare team and the patients, and the results have affected the self-management strategies [30-32].
SELF-MANAGEMENT CHALLENGES DURING THE COVID EPIDEMIC
According to the risk of COVID-19 prevalence in Canada in the in-person visits of patients to doctors' offices, online medical and health services are provided for the patients. For example, online triaging services are provided for COPD patients. Some limitations like cognitive and hearing disorders of patients, unavailability of technology, the lingual barriers, and problems of working with the system have reduced the quality of virtual healthcare compared to in-person healthcare. This problem is highly manifested in aged patients with COPD. Besides, quarantine and social distancing by the governments to reduce the prevalence of the virus has resulted in dysfunction in the management of patients with chronic neural disorders like epilepsy despite reducing the pulmonary infections caused by the disease. This is because; the patients suffer from anxiety and depression caused by decreased times of in-person visits with their doctors [22].
The restrictions have resulted in self-management behaviors such as nutrition, physical activity, and controlling chronic patients during the treatment process. This is because; these patients need special treatment and regular visits to various specialists to control their disease because of complicated clinical conditions. Hence, decreased access to healthcare services, medicine, and changes in their lifestyle can result in abundant problems for them [9, 33, 34]. Therefore, the healthcare team needs to control and support self-management programs due to the worry of these patients about the negative effects of the conditions on their health status and based on the significance of monitoring their health status [34, 35].
THE ROLE OF THE HEALTHCARE TEAM IN THE SELF-MANAGEMENT OF PATIENTS DURING THE CORONA PANDEMIC
During the corona pandemic, the healthcare team has to decrease in-person visits with chronic patients (especially diabetes patients) with COVID-19 and tries to train self-management to these patients. These patients have welcomed this method recently. However, it should be mentioned that some hospitals have caused the risk of high blood sugar by applying restrictive strategies in the activities of diabetic patients. The healthcare team, especially those with diabetic patients or newly diagnosed hyperglycemia with COVID-19, has to set their management strategies in such a way that the needs of patients are met and the personnel has been also protected [36].
Arlt et al. have mentioned that the healthcare team should pay attention to 3 elements including training, equipment, and empowerment to support chronic patient self-management.
In the field of training: the patients should be trained sufficiently about coping with the changes in their health status, such as conditions caused by the corona pandemic in their life. Through this, the patients can be prepared to pass the crisis.
Equipment: equipment aims to provide the needs of these patients such as medicine and medical equipment, which should be under careful supervision.
Empowerment: empowerment means making patients ready to encounter critical conditions and take urgent interventions when needed. Also, the healthcare team tries to enhance the self-confidence and ability of the patients to take the self-management process properly [37].
The main limitations in this study include a few numbers of studies in this field because of the newness of the disease. Also, it could be mentioned that reviewed articles were Latin because no similar study existed in Persian. Hence, it would be better for further studies to emphasize chronic patient self-management during the COVID-19 pandemic.
Conclusions
In general, the healthcare team should identify the restrictions, problems, and concerns of self-management of patients, and evaluate the solutions and effective interventions to meet and control the barriers. They should also provide the best options to facilitate self-management of chronic patients during the corona pandemic. Besides, the health centers should be urgently equipped with relevant technologies of virtual healthcare including online and offline electronic consulting, providing educational sources through the website of the universities and social media, phone follow up, presenting educational papers, providing non-pharmacological methods like relaxation, and effective breathing practices to reduce anxiety. Multiple studies have proved the effectiveness of using technology (telemedicine) for the self-management of chronic patients during the COVID 19.
Acknowledgements
Funding sources: this research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
We would like to express our gratitude to Shiraz University of Medical Sciences Vice Chancellor for Research, Education and Research for approving this project.
Figures and tables
Footnotes
Conflict of interest statement
The authors declare no conflict of interest.
Authors’ contributions
Conceptualization: TGH. Data curation: JS. Funding acquisition: None. Visualization: EAK. Writing-original draft: MGG, JS. Writing-review & editing: TGH.
References
- [1].Wu YC, Chen CS, Chan YJ. The outbreak of COVID-19: an overview. J Chin Med Assoc 2020;83:217. https://doi.org10.1097/JCMA.0000000000000270 10.1097/JCMA.0000000000000270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Honarvar MR, Roshandel G, Shirzad-Aski H, Tabarraei A, Tahamtan A, Ghelichi-Ghojogh M, Fazel A, Arefnia S, Jafari N, Mansoury M, Jafari A, Rajabi A. Epidemiological and clinical characteristics of the COVID-19 epidemic and associated factors for mortality in Golestan province, Iran: a retrospective cohort study. JPMH 2021;62:E298-304. https://doi.org/10.15167/2421-4248/jpmh2021.62.2.1910 10.15167/2421-4248/jpmh2021.62.2.1910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Mosazadeh H, Charkazi A, Ahmadi-Livani M, Nori A, Foroughi A, Rahimi A, Ghelichi-Ghojogh M, allah Kalteh E, Pahlavanzadeh B, Ozouni-Davaji RB, Rajabi A. Association of fear of COVID-19 and preventive behaviors (PB) against COVID-19 in Iran. Psychiatria 2021;18:169-75. https://doi.org/10.5603/PSYCH.a2021.0016 10.5603/PSYCH.a2021.0016 [DOI] [Google Scholar]
- [4].Mirahmadizadeh A, Rezaei F, Jokari K, Moftakhar L, Hemmati A, Dehghani SS, Hassani AH, Lotfi M, Jafari A, Ghelichi-Ghojogh M. Correlation between environmental factors and COVID-19 indices: a global level ecological study. Environ Sci Pollut Res Int 2021:1-11. https://doi.org/10.1007/s11356-021-16876-x 10.1007/s11356-021-16876-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Azarbakhsh H, Jokari K, Moftakhar L, Ghelichi-Ghojogh M, Karimyan A, Salmanzadeh S, Zeitooni MP, Khezri R, Valipour A. Epidemiological characteristics of patients with COVID-19 in Southwest of Iran from February 19 to June 20, 2020. Med J Islam Repub Iran 2021;35:875-9. 10.47176/mjiri.35.116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].De Hert M, Mazereel V, Detraux J, Van Assche K. Prioritizing COVID-19 vaccination for people with severe mental illness. World J Psychiatry 2021;20:54. http://doi.org/10.1002/wps.20826 10.1002/wps.20826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Tan SS, Pisano MM, Boone AL, Baker G, Pers YM, Pilotto A, Valsecchi V, Zora S, Zhang X, Fierloos I, Raat H. Evaluation design of EFFICHRONIC: the chronic disease self-management programme (CDSMP) intervention for citizens with a low socioeconomic position. Int J Environ Res Public Health 2019;16:1883. https://doi.org/10.3390/ijerph16111883 10.3390/ijerph16111883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Brigo F, Bonavita S, Leocani L, Tedeschi G, Lavorgna L. Telemedicine and the challenge of epilepsy management at the time of COVID-19 pandemic. Epilepsy Behav 2020;110. https://doi.org/10.1016/j.yebeh.2020.107164 10.1016/j.yebeh.2020.107164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Hartmann-Boyce J, Morris E, Goyder C, Kinton J, Perring J, Nunan D, Mahtani K, Buse JB, Del Prato S, Ji L, Roussel R. Diabetes and COVID-19: risks, management, and learnings from other national disasters. Diabetes Care 2020;43:1695-703. https://doi.org/10.2337/dc20-1192 10.2337/dc20-1192 [DOI] [PubMed] [Google Scholar]
- [10].Grabowski D, Overgaard M, Meldgaard J, Johansen LB, Willaing I. Disrupted self-management and adaption to new diabetes routines: a qualitative study of how people with diabetes managed their illness during the COVID-19 lockdown. Diabetology 2021;2:1-5. https://doi.org/10.3390/diabetology2010001 10.3390/diabetology2010001 [DOI] [Google Scholar]
- [11].Huang S, Xiao Y, Yan L, Deng J, He M, Lu J, Ke S. Implications for online management: two cases with COVID-19. Telemed J E Health 2020;26:487-94. https://doi.org/10.1089/tmj.2020.0066 10.1089/tmj.2020.0066 [DOI] [PubMed] [Google Scholar]
- [12].Karasavvidis T, Hirschmann MT, Kort NP, Terzidis I, Totlis T. Home-based management of knee osteoarthritis during COVID-19 pandemic: literature review and evidence-based recommendations. J Exp Orthop 2020;7:1-7. https://doi.org/10.1186/s40634-020-00271-5 10.1186/s40634-020-00271-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Feldman M, Lacey Krylova V, Farrow P, Donovan L, Zandamela E, Rebelo J, Rodrigues M, Bulo A, Ferraz C, Rodrigues H, Roca-Feltrer A. Community health worker knowledge, attitudes and practices towards COVID-19: learnings from an online cross-sectional survey using a digital health platform, UpSCALE, in Mozambique. PloS one 2021;16:e0244924. https://doi.org/10.1371/journal.pone.0244924 10.1371/journal.pone.0244924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Gupta SK, Lakshmi PV, Kaur M, Rastogi A. Role of self-care in COVID-19 pandemic for people living with comorbidities of diabetes and hypertension. J Family Med Prim Care 2020;9:5495. http://doi.org/10.4103/jfmpc.jfmpc_1684_20 10.4103/jfmpc.jfmpc_1684_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Chudasama YV, Gillies CL, Zaccardi F, Coles B, Davies MJ, Seidu S, Khunti K. Impact of COVID-19 on routine care for chronic diseases: a global survey of views from healthcare professionals. Diabetes Metab Syndr 2020;14:965-7. https://doi.org/10.1016/j.dsx.2020.06.042 10.1016/j.dsx.2020.06.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Liu Q, Luo D, Haase JE, Guo Q, Wang XQ, Liu S, Xia L, Liu Z, Yang J, Yang BX. The experiences of health-care providers during the COVID-19 crisis in China: a qualitative study. Lancet Glob Health 2020;8:e790-8. https://doi.org/10.1016/S2214-109X(20)30204-7 10.1016/S2214-109X(20)30204-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Meza O, Pérez-Chiqués E, Campos SA, Varela Castro S. Against the COVID-19 pandemic: analyzing role changes of healthcare street-level bureaucrats in Mexico. J Comp Policy Anal: Res Pract 2021;23:109-19. https://doi.org/10.1080/13876988.2020.1846993 10.1080/13876988.2020.1846993 [DOI] [Google Scholar]
- [18].Sherifali D, Berard LD, Gucciardi E, MacDonald B, MacNeill G. Self-management education and support. Can J Diabetes 2018;42:S36-41. https://doi.org/10.1016/j.jcjd.2017.10.006 10.1016/j.jcjd.2017.10.006 [DOI] [PubMed] [Google Scholar]
- [19].Allegrante JP, Wells MT, Peterson JC. Interventions to support behavioral self-management of chronic diseases. Annu Rev Public Health 2019;40:127-46. https://doi.org/10.1146/annurev-publhealth-040218-044008 10.1146/annurev-publhealth-040218-044008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Banerjee M, Chakraborty S, Pal R. Diabetes self-management amid COVID-19 pandemic. Diabetes Metab Syndr 2020;14:351-4. https://doi.org/10.1016/j.dsx.2020.04.013 10.1016/j.dsx.2020.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Paschos K. The management of chronic diseases is a major challenge for modern health systems: an integration of concepts and strategies concerning patients, doctors and health care. Sci Chron 2020;25:38-53. [Google Scholar]
- [22].Elbeddini A, Tayefehchamani Y. Amid COVID-19 pandemic: challenges with access to care for COPD patients. Res Social Adm Pharm 2021;17:1934-7. https://doi.org/10.1016/j.sapharm.2020.06.002 10.1016/j.sapharm.2020.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Kelly C, Spencer S, Grundy S, Lynes D, Evans DJ. Self-management for non-cystic fibrosis bronchiectasis. Cochrane Database Syst Rev 2017;2017(1). https://doi.org/10.1002/14651858.CD012528 10.1002/14651858.CD012528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Bayless AK, Wyatt TH, Raynor H. Obese-asthma phenotype self-management: a literature review. J Pediatr Nurs 2021;60:154-63. https://doi.org/10.1542/peds.2017-1284H 10.1542/peds.2017-1284H [DOI] [PubMed] [Google Scholar]
- [25].Panagioti M, Richardson G, Small N, Murray E, Rogers A, Kennedy A, Newman S, Bower P. Self-management support interventions to reduce health care utilisation without compromising outcomes: a systematic review and meta-analysis. BMC Health Serv Res 2014;14:1-4. https://doi.org/10.1186/1472-6963-14-356 10.1186/1472-6963-14-356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Van de Velde D, De Zutter F, Satink T, Costa U, Janquart S, Senn D, De Vriendt P. Delineating the concept of self-management in chronic conditions: a concept analysis. BMJ Open 2019;9:e027775. https://doi.org/10.1136/bmjopen-2018-027775 10.1136/bmjopen-2018-027775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Wainwright T, Low M. Beyond acute care: Why collaborative self-management should be an essential part of rehabilitation pathways for COVID-19 patients. J Rehabil Med 2020;52. https://doi.org/10.2340/16501977-2685 10.2340/16501977-2685 [DOI] [PubMed] [Google Scholar]
- [28].Ghosh A, Gupta R, Misra A. Telemedicine for diabetes care in India during COVID19 pandemic and national lockdown period: guidelines for physicians. Diabetes Metab Syndr 2020;14:273-6. https://doi.org/10.1016/j.dsx.2020.04.001 10.1016/j.dsx.2020.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Izzedine H, Jhaveri KD, Perazella MA. COVID-19 therapeutic options for patients with kidney disease. Kidney Int 2020;97:1297-8. https://doi.org/10.1016/j.kint.2020.03.015 10.1016/j.kint.2020.03.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Plevinsky JM, Young MA, Carmody JK, Durkin LK, Gamwell KL, Klages KL, Ghosh S, Hommel KA. The impact of COVID-19 on pediatric adherence and self-management. J Pediatr Psychol 2020;45:977-82. https://doi.org/10.1093/jpepsy/jsaa079 10.1093/jpepsy/jsaa079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Leonardi M, Horne AW, Vincent K, Sinclair J, Sherman KA, Ciccia D, Condous G, Johnson NP, Armour M. Self-management strategies to consider to combat endometriosis symptoms during the COVID-19 pandemic. Hum Reprod Open 2020;2020:hoaa028. https://doi.org/10.1093/hropen/hoaa028 10.1093/hropen/hoaa028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Kaye L, Theye B, Smeenk I, Gondalia R, Barrett MA, Stempel DA. Changes in medication adherence among patients with asthma and COPD during the COVID-19 pandemic. J Allergy Clin Immunol Pract 2020;8:2384-5. https://doi.org/10.1016/j.jaip.2020.04.053 10.1016/j.jaip.2020.04.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Chang AY, Cullen MR, Harrington RA, Barry M. The impact of novel coronavirus COVID-19 on noncommunicable disease patients and health systems: a review. J Intern Med 2021;289:450-62. https://doi.org/10.1111/joim.13184 10.1111/joim.13184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Goodsall TM, Han S, Bryant RV. Understanding attitudes, concerns, and health behaviors of patients with inflammatory bowel disease during the coronavirus disease 2019 pandemic. J Gastroenterol Hepatol 2021;36:1550-5. https://doi.org/10.1111/jgh.15299 10.1111/jgh.15299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Shimada N, Shimada H, Itaya Y, Tomino Y. Novel coronavirus disease in patients with end-stage kidney disease. Ther Apher Dial 2021;25:544-50. https://doi.org/10.1111/1744-9987.13599 10.1111/1744-9987.13599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Korytkowski M, Antinori-Lent K, Drincic A, Hirsch IB, McDonnell ME, Rushakoff R, Muniyappa R. A pragmatic approach to inpatient diabetes management during the COVID-19 pandemic. J Clin Endocrinol Metab 2020;105:3076-87. https://doi.org/10.1210/clinem/dgaa342 10.1210/clinem/dgaa342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Arlt W, Baldeweg SE, Pearce SH, Simpson HL. Endocrinology in the time of COVID-19: management of adrenal insufficiency. Eur J Endocrinol 2020;183:G25-32. https://doi.org/10.1530/EJE-20-0361 10.1530/EJE-20-0361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Xu H, Huang S, Qiu C, Liu S, Deng J, Jiao B, Tan X, Ai L, Xiao Y, Belliato M, Yan L. Monitoring and Management of Home-Quarantined Patients with COVID-19 using a WeChat-based telemedicine system: retrospective cohort study. J Med Internet Res 2020;22:e19514. https://doi.org/10.2196/19514 10.2196/19514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Bajwah S, Wilcock A, Towers R, Costantini M, Bausewein C, Simon ST, Bendstrup E, Prentice W, Johnson MJ, Currow DC, Kreuter M. Managing the supportive care needs of those affected by COVID-19. Eur Respir J 2020;55:2000815. https://doi.org/10.1183/13993003.00815-2020 10.1183/13993003.00815-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Garg SK, Rodbard D, Hirsch IB, Forlenza GP. Managing new-onset type 1 diabetes during the COVID-19 pandemic: challenges and opportunities. Diabetes Technol Ther 2020;22:431-9. https://doi.org/10.1089/dia.2020.0161 10.1089/dia.2020.0161 [DOI] [PubMed] [Google Scholar]
- [41].Bhutani M, Hernandez P, Bourbeau J, Dechman G, Penz E, Aceron R, Beauchamp M, Wald J, Stickland M, Olsen SR, Goodridge D. Addressing therapeutic questions to help Canadian health care professionals optimize COPD management for their patients during the COVID-19 pandemic. Can. J. Respir Crit Care Sleep Med 2020;4:77-80. https://doi.org/10.1080/24745332.2020.1754712 10.1080/24745332.2020.1754712 [DOI] [Google Scholar]
- [42].Ballard M, Bancroft E, Nesbit J, Johnson A, Holeman I, Foth J, Rogers D, Yang J, Nardella J, Olsen H, Raghavan M. Prioritising the role of community health workers in the COVID-19 response. BMJ Global Health 2020;5:e002550. https://doi.org/10.1136/bmjgh-2020-002550 10.1136/bmjgh-2020-002550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Bhaumik S, Moola S, Tyagi J, Nambiar D, Kakoti M. Community health workers for pandemic response: a rapid evidence synthesis. BMJ Global Health 2020;5:e002769. https://doi.org/10.1136/bmjgh-2020-002769 10.1136/bmjgh-2020-002769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Goldfarb N, Grinstein-Cohen O, Shamian J, Schwartz D, Zilber R, Hazan-Hazoref R, Goldberg S, Cohen O. Nurses’ perceptions of the role of health organisations in building professional commitment: Insights from an israeli cross-sectional study during the COVID-19 pandemic. J Nurs Manag 2021;:1102-1110. https://doi.org/10.1111/jonm.13248 10.1111/jonm.13248 [DOI] [PubMed] [Google Scholar]


