Abstract
Post-translational modification (PTM) is an essential mechanism for enhancing the functional diversity of proteins and adjusting their signaling networks. The reversible conjugation of ubiquitin (Ub) and ubiquitin-like proteins (Ubls) to cellular proteins is among the most prevalent PTM, which modulates various cellular and physiological processes by altering the activity, stability, localization, trafficking, or interaction networks of its target molecules. The Ub/Ubl modification is tightly regulated as a multi-step enzymatic process by enzymes specific to this family. There is growing evidence that the dysregulation of Ub/Ubl modifications is associated with various diseases, providing new targets for drug development. In this review, we summarize the recent progress in understanding the roles and therapeutic targets of the Ub and Ubl systems in the onset and progression of human diseases, including cancer, neurodegenerative disorders, and heart diseases.
Keywords: post-translational modification, ubiquitin, ubiquitin-like proteins, ubiquitin-proteasome system, disease association and progression
1. Introduction
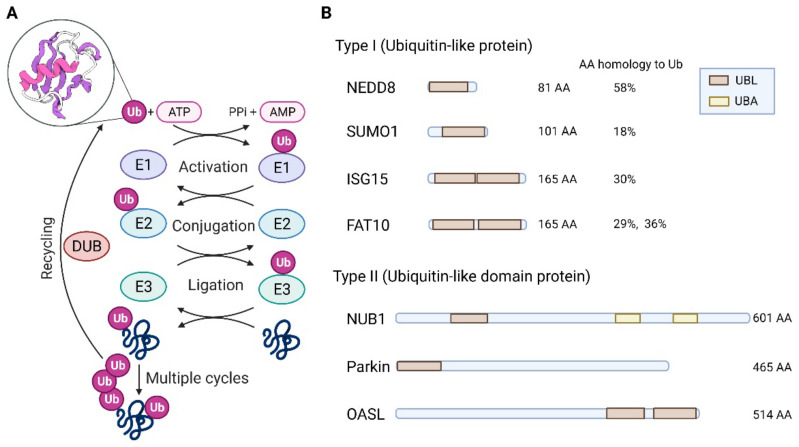
Post-translational modification (PTM) is a key mechanism that precisely regulates protein activity to determine cellular metabolism or fitness in response to genetic and environmental changes. PTMs mediated by ubiquitin (Ub) and various ubiquitin-like proteins (Ubls) can alter the functions, locations, and levels of their specific targets [1]. These modifiers are covalently bound to their targets via an enzymatic cascade involving three enzymes, E1 (activating enzyme), E2 (conjugating enzyme), and E3 (ligase). E1 enzymes activate Ub/Ubl by catalyzing C-terminal adenylation of Ub/Ubl with the aid of adenosine triphosphate (ATP) to form a covalent thioester bond. E2 enzymes then accept the activated Ub/Ubl via a transthioesterification reaction. Finally, the Ub/Ubl-loaded E2 enzyme, either alone or with the help of a partner E3 enzyme, transfers Ub/Ubl to a specific target lysine residue, creating an amide (or isopeptide) bond between Ub/Ubl and the substrate. Deubiquitinating enzymes (DUBs) and Ub/Ubl-specific proteases (ULPs) are responsible for Ub deconjugation, editing, and recycling (Figure 1A).
Figure 1.
Biochemical and Structural Features of Ubiquitin & Ubiquitin-like Proteins. (A) Main steps in the substrate modification process by Ub. The β-grasp globular fold structure of Ub is shown in the circle. (B) Examples of structural domains within human type I and type II Ub family members. DUB, de-ubiquitinating enzymes; FAT10, HLA-F-adjacent transcript 10; ISG15, Interferon-stimulated gene 15; NEDD8, Neural precursor cell-expressed developmentally down-regulated gene 8; NUB1, NEDD8 ultimate buster 1; OASL, 2′-5′-oligoadenylate synthetase-like protein; SUMO1, small ubiquitin-like modifier 1; Ub, ubiquitin; UBL, ubiquitin-like domain; UBA, ubiquitin-associated domain. Figure 1A adapted from “ubiquitination”, by BioRender.com (accessed on 1 March 2022). Retrieved from https://app.biorender.com/biorender-templates. Agreement number is OU23V77K75.
Since Ub was first discovered in 1975, bioinformatic, genetic, and biochemical studies have revealed diverse sets of Ubls. Ub family proteins are structurally similar to ubiquitin (i.e., β-grasp globular fold structure) [2] and are divided into two classes: ubiquitin-like proteins (type I) and ubiquitin-like domain proteins (type II) (Figure 1B). Ubls (type I) have a characteristic sequence motif consisting of one or two glycine residues at the C-terminus, through which covalent attachment occurs. Almost all Ubls are conjugated to other proteins, except for at least one protein (e.g., ATG8, which attaches to lipids). The ubiquitin-like domain protein (type II) lacks a C-terminal diglycine motif and cannot be conjugated to a target. Instead, it can function as a protein-protein interaction domain. Ten Ubl orthologs that function as protein modifiers in humans have been identified [3]: ATG8, ATG12, FAT10, FUBI, HUB1, ISG15, NEDD8, SUMO, UFM1, and URM1. Although Ubls are structurally related to Ub, their biochemical roles are distinct because they are associated with DNA repair, nuclear transport, proteolysis, translation, autophagy, and immune responses.
In this review, we outline the role of Ub/Ubl modifications in disease-associated mechanisms, focusing on ubiquitination and SUMOylation. We also discuss current small-molecule drugs targeting these PTMs as therapeutic strategies for complex diseases, such as cancer, neurodegenerative disorders, and heart disease.
2. Ub/Ubl Modifications in Disease Pathogenesis and Treatment
2.1. Ubiquitin-Proteasome System
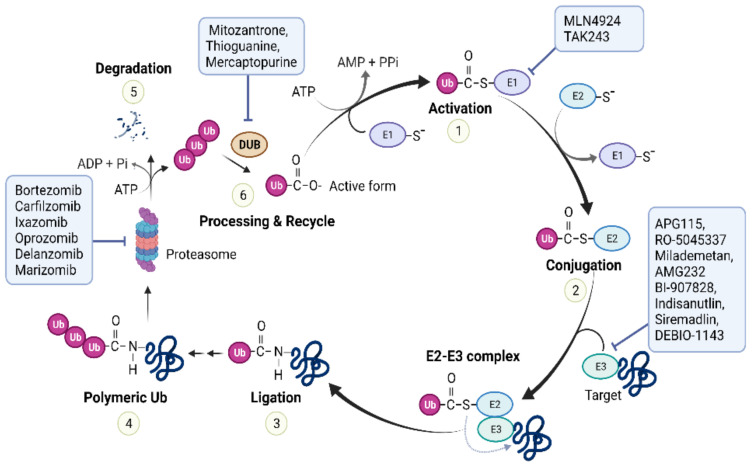
Ubiquitin-proteasome system (UPS)-mediated proteolysis involves two significant steps: (i) attachment of Ub to target proteins via ubiquitination, and (ii) degradation of Ub-proteins by the proteasome (Figure 2). The Ub molecule has seven acceptor lysines, each of which can participate in subsequent ubiquitination to generate multiple mono-Ub proteins or a poly-Ub chain. Different Ub linkages result in different conformations of the Ub chain and produce diverse molecular signals in cells [4]. Proteins homogenously linked to poly-Ub are mainly delivered to and degraded by the 26S proteasome (20S proteasome+19S regulatory particles), where Ub is recycled. The UPS is primarily responsible for the full or partial processing of most intracellular proteins (more than 80%) or stress response transcription factors (e.g., nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) or hypoxia-inducible factor). Maladaptive UPSs with problems including impairment of the ubiquitination process, insufficient substrate delivery to the proteasome, or loss of proteasome activity may contribute to the progressive disruption of cellular proteostasis. In addition to proteolysis, ubiquitination is involved in non-proteolytic events, such as autophagy, inflammation, DNA repair, multi-protein complex assembly, and regulation of enzymatic activity. Abnormalities in this system have been implicated in the pathogenesis of numerous human diseases, and pharmacological manipulation of the UPS appears to alter the outcome of many diseases [5]. Therefore, the UPS is an important therapeutic target.
Figure 2.
The ubiquitin-proteasome system (UPS). In step 1, ubiquitin is activated by a ubiquitin activating enzyme (E1). In step 2, activated ubiquitin (Ub) is transferred to a ubiquitin conjugating enzyme (E2). In step 3, ubiquitin is transferred from E2 to a specific target (substrate) lysine to form a covalent bond. This process is catalyzed by E3 ubiquitin ligase. In step 4, repeated ubiquitin conjugation generates a poly-ubiquitin chain. In step 5, the ubiquitinated target (e.g., canonical K48 linkage) is recognized, unfolded, and digested by the 26S proteasome. In step 6, Deubiquitinating (DUB) enzymes remove covalently linked ubiquitin moieties from ubiquitin-ubiquitin and ubiquitin-protein conjugates. These enzymes also process ubiquitin precursors to generate free (un-anchored) ubiquitin pools. The free ubiquitin can be further reused. Inhibitors of various UPS components are being developed clinically for the treatment of cancer and neurodegenerative diseases.
2.1.1. Abnormal Ub Pathways in Cancer
In cancer cells, an abnormal UPS contributes to cell cycle progression, faulty DNA repair, apoptosis, angiogenesis, receptor downregulation, and gene transcription through the degradation of oncogenes or tumor suppressors. Notable examples include the downregulation of cell cycle-related and tumor suppressor proteins, such as p53 and cyclin-dependent kinase inhibitor 1 B (p27), and the upregulation of oncogenic proteins, such as the transcription factor NF-κB.
To date, only two Ub E1 enzymes have been identified: ubiquitin-like modifier-activating enzyme 1 (UBA1) and ubiquitin-like modifier-activating enzyme 6 (UBA6). These enzymes are essential for supporting cellular stress, including DNA damage and protein toxicity, in cancer cells. Bioinformatics approaches have identified E1 enzymes associated with the pathogenesis of human cancer [6]. The aberrant expression of UBA1, the predominant isoform of the two E1 enzymes, is associated with the pathogenesis of lung cancer [7] and cutaneous squamous cell carcinoma [8]. E1 enzyme activity is also known to increase in malignant hematologic cells [9].
The human genome encodes 38 Ub E2 enzymes. Elevated levels of E2-conjugating enzymes, which are associated with lower patient survival rates, have frequently been observed in various cancer specimens. For example, the upregulation of the ubiquitin-conjugating enzyme E2 L3 (UBE2L3) has been detected in non-small cell lung cancer (NSCLC) tissues compared to non-cancerous tissues. High expression of UBE2L3 is associated with advanced tumor stages and adverse outcomes [10]. Mechanistically, UBE2L3 catalyzes the ubiquitination and proteasomal degradation of p27 by interacting with the S-phase kinase-associated protein 2 (Skp2), a p27-specific E3 ligase.
The human UPS comprises more than 700 E3 ligases and DUBs, and the abnormal expression of these enzymes and the presence of functional mutations are associated with cancer progression. Mouse double-minute 2 homolog (MDM2), a major negative regulator of p53, and the p27 destabilizer Skp2 are well-studied E3 ligases because of their potential to cause human cancer. Ubiquitin-specific protease 7 (USP7) is the most widely studied DUB that modulates p53 function through Ub clearance. USP7 directly regulates p53 stability or downregulates p53 by stabilizing MDM2. USP7 is highly expressed in various malignancies [11].
Examples of UPS defects associated with cancer are summarized in Table 1.
Table 1.
Examples of cancer-related UPS enzymes. The relevant cancer type information for each gene referenced OMIM (https://www.ncbi.nlm.nih.gov/omim) (accessed on 7 March 2022) or The Cancer Genome Atlas data.
| Gene Name | Function in Cancer | Deregulation | Cancer Type | |
|---|---|---|---|---|
| E1 | UBA1 | Oncogene | ↑ | LNC [7], SCC [8], MM [9], PM in LC, TC [TCGA] |
| E2 | UBE2A | Oncogene | Mutation, ↑ | HCC [12] CML [13], PM in RCC, CC, HNC [TCGA] |
| UBE2C | Proto-oncogene | ↑ | BC, PC, CRC, OC, Lymphoma [14], PM in RCC, LC, PC [TCGA] | |
| UBE2D | Oncogene | ↑ | PM in RCC [TCGA] | |
| UBE2L | Oncogene | ↑ | NSCLC [10], PM in BC, OC [TCGA] | |
| UBE2N | Oncogene | ↑ | BC, PC, CRC, OC, Lymphoma [14], PM in LC [TCGA] | |
| UBE2S | Oncogene | ↑ | PM in RCC, LC, EC [TCGA] | |
| UBE2T | Oncogene | ↑ | PM in RCC, LC, OC [TCGA] | |
| E3 | APC3 (CDC27) | Tumor suppressor | Mutation, ↑ | PC [15], PM in RCC, CRC, LC, LNC [TCGA] |
| BRCA1 | Tumor suppressor | Mutation | Familial BC, OC [OMIM 113705] | |
| CBL | Proto-oncogene | Mutation | Leukemia [OMIM 165360] | |
| FBW7 | Tumor suppressor | Mutation | BRC, CRC, EC [16], PM in RCC [TCGA] | |
| MDM2 | Oncogene | ↑ | PM in EC, CC [TCGA] | |
| SKP2 | Oncogene | ↑ | PM in RCC, Melanoma, OC [TCGA] | |
| PAKN2 | Tumor suppressor | Mutation | LNC, OC [OMIM 602544] | |
| VHL | Tumor suppressor | Mutation | RCC [OMIM 608537], PM in LC, BC, SC [TCGA] | |
| DUB | BAP1 | Tumor suppressor | Mutation | BC, LC, RCC [OMIM 603089], PM in RCC [TCGA] |
| CYLD | Tumor suppressor/Oncogene | Mutation | Familial cylindromatosis, Trichoepithelioma [OMIM 605018] | |
| FANCL | Tumor suppressor | Mutation | Fanconi leukemia [OMIM 608111], PM in RCC, LC, UC [TCGA] | |
| TNFAIP3 | Tumor suppressor/Oncogene | Mutation, ↑ | BC, Lymphomas [OMIM 191163], PM in RCC [TCGA] | |
| USP4 | Oncogene | Mutation, ↑ | LNC [OMIM 603486], PM in RCC, LNC [TCGA] | |
| USP7 | Tumor suppressor/Oncogene | ↑ | OC [17], Glioma [18], PM in RCC [TCGA] | |
| USP14 | Oncogene | ↑ | PM in LC, HNC, OC [TCGA] | |
| USP28 | Oncogene | ↑ | BC [19], CRC [20] | |
| USP42 | Oncogene | ↑ | GC [21] |
Abbreviations: BC, breast cancer; BRC, bladder cancer; CC, cervical cancer; CML, chronic myelogenous leukemia; CRC, colorectal cancer; EC, endometrial cancer; GC, gastric cancer; HCC, hepatocellular carcinoma; HNC, head and neck cancer; LC, liver cancer; LNC, Lung cancer; NSCLC, Non-small cell lung cancer; MM, multiple melanoma; OC, ovarian cancer; PC, pancreatic cancer; RCC, renal cell carcinoma; SC, stomach cancer; SCC, squamous cell carcinoma; TC, thyroid cancer; UC, urothelial cancer; ↑, Upregulation; PM, Prognostic marker; TCGA, The Cancer Genome Atlas.
2.1.2. UPS Inhibitors Used to Treat Cancer
The clinical success of cancer treatments targeting proteasome inhibitors has demonstrated that UPS is a therapeutic strategy. In recent years, extensive studies of E1 activating enzymes as targets of pharmacological inhibition have identified potential novel targets. Targeting common pathways, such as E1 enzymes or the proteasome, may lead to non-specific effects, but can be applied to therapeutic and safety windows that will be useful for short-term therapy. Inhibiting single E3 Ub ligases or specific proteasome-associated DUB enzymes is another strategy for modulating the UPS, which is expected to increase specificity and lower toxicity.
Proteasome inhibitors: Proteasome inhibitor (PI)-induced tumor suppression is a classical strategy for cancer treatment. Bortezomib, a prototype PI drug, is effective against malignancies with high UPS dependence, such as multiple myeloma (MM) and mantle cell lymphoma. To date, three PI drugs are available on the market: Bortexomib (a first-in-class PI), Carfilzomib (a second-in-class PI), and Ixazomib (a first oral PI). Second-generation PIs have been clinically developed, including the oral active agents Oprozomib, Delanzomib, and Marizomib, which have different pharmacokinetic properties. Phase I/II trials demonstrated the efficacy of Oprozomib monotherapy in patients with MM, but have raised pharmacokinetic profile and safety issues that need improvement [22]. The feasibility of Delanzomib has been demonstrated in early-stage clinical studies of MM and solid tumor [23]. However, clinical development of Delanzomib for MM therapy has been halted because of its significant toxicity [24]. Marizomib is more lipophilic and less neurotoxic drugs. In phase III trial, Marizomib is being assessed for the treatment of malignant glioblastoma in combination with temozolomide and radiotherapy (NCT03345095). MM has been studied as a top priority target for PI drugs because of its ability to produce large amounts of IgG from plasma cells. The high protein turnover in myeloma cells and the preferential susceptibility of malignant cells compared to normal cells result in a favorable therapeutic window for PIs in this disease [25]. The main challenges associated with PI drugs are acquired resistance and low efficacy due to poor pharmacokinetic/pharmacodynamic profiles.
E1 inhibitors: Inhibitors of the ubiquitination initiator E1 enzymes comprise a new class of cancer therapeutics [26]. Compared with PIs, E1 inhibitors are expected to induce broader and more effective biological effects, because they interfere with proteasome degradation and Ub-dependent signaling pathways, such as DNA repair and NF-κB signaling. The success of MLN4924 (Pevonedistat), an inhibitor of the E1 enzyme responsible for Neddylation in cancer [27], has led to the development of other E1 enzyme inhibitors involved in Ub/Ubl modification. MLN4924 is currently being studied in phase III trials for patients with leukemia (NCT04090736, NCT03268954). Among them, TAK-243 (MLN7243) is a first-in-class UAE (ubiquitin-activating enzyme) inhibitor. This agent potently inhibits two key Ub E1 enzymes UBA1 and UBA6 in vitro and is effective in preclinical models of solid and hematological tumors [28]. The TAK-243 inhibitor has been registered in a phase I clinical trial in patients with leukemia (NCT03816319). The research is scheduled to begin this year (2022). Another phase I clinical trial of TAK-243 for advanced solid tumors (NCT02045095) was also conducted, but was terminated for sponsorship reasons.
E3 ligase inhibitors: Because E3 ligase is an important factor in determining substrate specificity in ubiquitination, cancer researchers have been interested in regulating this enzyme. For example, MDM2 and HDM2 (the human counterpart of MDM2) have been extensively validated as potential anticancer drug targets [29]. Several MDM2 inhibitors, including Milademetan (NCT05012397, NCT04979442), APG115 (NCT03781986, NCT04358393), Idasanutlin (NCT04029688, NCT02633059), AMG232 (NCT04190550, NCT03031730), BI-907828 (NCT03449381, NCT05218499), and Siremadlin (NCT05155709, NCT05180695), are currently under clinical investigation for cancer. However, features of E3, such as the lack of a canonically active site for E3 ligase, extensive protein-protein interactions with other proteins, and a multi-domain structure, limit the development of high-potency inhibitors. Protein-targeted chimeras (PROTAC), which chemically link proteins with E3 to induce targeted degradation through the UPS, is a new technology that generates proteolytic agents. PROTAC has drawn considerable attention for research in recent years and is expected to be developed as a cancer treatment in the future [30].
DUB inhibitors: The activation (or inhibition of degradation) of DUB, which acts as a tumor suppressor, as well as the inhibition of DUB, which acts as an oncoprotein, may also be promising cancer treatment strategies [31]. Efforts to develop chemical probes and drugs have reported more than 50 DUB inhibitors, and significant advances have been made in the development of tools for biochemical analysis of DUB [32]. However, only a few DUB inhibitors, such as VLX1570, have entered clinical trials (phase I), but were terminated prematurely due to severe toxicity [33]. Mitoxantrone, a US Food and Drug Administration (FDA)-approved drug that can inhibit DUB ubiquitin-specific peptidase 11 (NCT02724163, NCT05313958), and potential DUB ubiquitin-specific peptidase 14 inhibitors, such as 6-mercaptopurine (NCT00866918, NCT00482833) and 6-thioguanine (NCT05276284, NCT00549848), are currently in clinical trials to treat several types of cancers, including leukemia.
The UPS-targeted drugs under clinical investigation for the treatment of cancer are summarized in Table 2.
Table 2.
List of anticancer drugs targeting UPS. Drugs under FDA/EMA approval or clinical investigation are summarized. For more detailed clinical information, see ClinicalTrials.gov. All accessed on 1 March 2022.
Abbreviations: DUB, de-ubiquitinating enzymes; E1, ubiquitin-activating enzyme; E2, ubiquitin-conjugating enzyme; E3, ubiquitin ligase; FDA, The United States Food and Drug Administration; PI, proteasome inhibitor.
2.1.3. Abnormal Ub Pathway in Neurodegenerative Diseases
Many neurodegenerative disorders (ND), such as Alzheimer’s disease (AD), Parkinson’s disease (PD), amyotrophic lateral sclerosis (ALS), and Huntington’s disease (HD), present distinct clinical symptoms depending on the localization of the brain pathology. However, they exhibit common neuropathological characteristics, such as the accumulation of misfolded or aggregated proteins. Abnormalities in the Ub-dependent proteolytic pathways have been associated with neurotoxic aggregate formation and consequent neurodegeneration [37]. There is growing evidence that UPS-associated enzymes play a role in neurodegenerative mechanisms, including the aggregation and accumulation of proteins, autophagy, oxidative stress, apoptosis, and aberrant glutamine transduction. The altered expression or presence of mutations in the UPS components reported in patients with ND are summarized in Table 3.
Table 3.
Examples of neurodegenerative disease-related UPS components. The disease information for each gene referenced OMIM (https://www.ncbi.nlm.nih.gov/omim). (All accessed on 1 March 2022).
| Gene Name | Deregulation Type | Disease | |
|---|---|---|---|
| Ub precursor | UBB | Missreading, misframed mutations | AD [OMIM 191339] |
| E3 | CHIP | ↑ | AD [38] |
| FBXO7 | Loss-of-function mutations | PD [OMIM 605648] | |
| HACE1 | ↓ | HD [39] | |
| HRD1 | ↓ | AD [40] | |
| LRSAM1 | Loss-of-function mutations | PD [OMIM 610933] | |
| NEDD4-1 | ↑ | AD, PD, ALS [41] | |
| PRKN (PARK2) | Loss-of-function mutations | PD [OMIM 602544] | |
| RNF182 | ↑ | AD [42] | |
| TRAF6 | ↑ | PD [43], HD [44] | |
| UBE3A | Loss-of-function mutations | AS [OMIM 601623] | |
| DUB | UCHL1 (PARK5) | ↓, Loss-of-function mutations | AD, PD [OMIM 191342] |
| USP13 | ↑ | PD [45] |
Abbreviations: AD, Alzheimer’s disease; AS, angelman syndrome; ALS, amyotrophic lateral sclerosis; DUB, de-ubiquitinating enzymes; E3, ubiquitin ligase; HD, Huntington’s disease; PD, Parkinson’s disease; ↑, Upregulation; ↓, Downregulation.
Alzheimer’s disease (AD): UPS dysfunction is caused by Ub mutations associated with AD and other tauopathies. One such protein is a transcriptional frameshift mutant form of Ub (Ubb+1), in which the C-terminal Gly76 is replaced by a tyrosine with a 20-residue extension [46]. Ubb+1 has been found to specifically accumulate in neurofibrillary tangles and neuritic plaques in the brain tissues of patients with AD [46]. Lack of C-terminal Gly76 renders Ubb+1 unable to ubiquitinate other proteins and instead terminates poly Ub chains, rendering it resistant to DUB [47]. Additionally, the overexpression of Ubb+1 triggers mitochondrial impairment and cell death in neurons, suggesting that Ubb+1 contributes to AD progression [48]. The importance of Ub E3 ligases in AD pathogenesis has been increasingly recognized. For example, Nedd4-1 (neural precursor cell expressed developmentally downregulated protein 4-1), a HECT (Homologous to the E6-AP Carboxyl Terminus) family of E3 ligases, targets several ND-related proteins, including the insulin/insulin growth factor 1 receptor (IGF-1R) [49]. In AD patients, IGF-1 signaling is significantly impaired, and the overall expression of IGF-1R is downregulated [50]. More recent studies have demonstrated that Nedd4-1 promotes the ubiquitination of alpha-amino-3-hydroxy-5-methyl-4-isoxazoleproprionic acid receptor (AMPAR), the primary mediator of synaptic transmission, in response to amyloid β (Aβ). This process triggers AMPAR internalization, accompanied by loss-of-surface AMPAR, resulting in synaptic weakening [51]. The reduction in AMPAR protein levels is one of the molecular features of the early stages of AD [52]. Upregulation of Nedd4-1 has been reported in human AD, PD, and HD brains, and in spinal cords of patients with ALS [41]. There have been no reports of pathogenic mutations at the genetic level. Another HACT domain E3 ligase, UBE3A, plays a key role in synaptic function [53]. Loss-of-function mutations in the UBE3A gene cause neurodevelopmental disorders, such as Angelman syndrome [54]. Unsurprisingly, downregulation of UBE3A has been found in a mouse model of AD, Tg2576. UBE3A deficiency is associated with Aβ metabolism and synaptotoxicity in mice [53,55].
Parkinson’s disease (PD): Parkin, a ring-to-ring-type E3, is the first E3 enzyme targeting α-synuclein [56]. Mutations in the gene encoding parkin are now thought to account for approximately 50% of early-onset PD cases and 10–20% of adolescent PD cases [57]. All known mutations in parkin are loss-of-function mutations. Parkin exerts neuroprotective effects by inducing mitophagy, together with PTEN-induced putative phosphatase 1 (PINK1), to clear damaged mitochondria. In addition, the E3 activity of parkin is involved in promoting the expression of the NF-κB pathway, providing further evidence for the neuroprotective role of parkin [58]. Loss of parkin function promotes early-onset PD and potential cancer progression. In addition to parkin, ubiquitin C-terminal hydrolase L1 (UCHL1) is associated with familial PD. For example, the I93M missense mutation in UCHL1 has been linked to a rare autosomal dominant form of familial PD. For example, the I93M missense mutation in the UCHL1 has been linked to a rare, autosomal dominant form of familial PD [59]. Transgenic mice overexpressing the I93M substitution showed significantly induced dopaminergic neuronal loss [60]. Furthermore, the downregulation and extensive oxidation of the UCHL1 protein have been found in idiopathic PD brains [61]. In this study, reduced UCHL1 was also found in the cortex tissues of patients with AD, suggesting a pathological feature common to both AD and PD. Many E3 enzymes are able to ubiquitinate α-synuclein. Among them, Nedd4-1 potently promotes α-synuclein ubiquitination and clearance in cells [62] and in vivo [63]. Moreover, enhanced Nedd4-1 activity indicates a neuroprotective function against α-synuclein-induced toxicity in two animal models of PD, fruit flies and rats [63].
2.1.4. UPS Inhibitors as Treatment for Neurodegenerative Diseases
As a potential treatment strategy for ND, the Ub pathway is also being studied to enhance ubiquitination (e.g., maintaining Ub retention or upregulating E3 ligase activity), enhance proteasome activity, and inhibit polyubiquitin chain trimming. As with cancer, small molecules are currently being developed by targeting different mechanisms, such as the inhibition or activation of specific E3 ligases or DUBs, and the correction of possible misregulations in the UPS. However, most drugs targeting the Ub pathway, including DUB inhibitors used as ND therapies, are still in preclinical development (Table 4).
Table 4.
Selected DUB small molecule inhibitors reported in neurodegenerative disorders.
| Compound ID | Description | Stage |
|---|---|---|
| Pimozide | USP1 inhibitor | Phase II trials (https://clinicaltrials.gov/ct2/show/NCT03272503, accessed on 1 March 2022) |
| IU1, IU1 analogs and derivatives | USP14 inhibitor | Preclinical [64,65,66,67] |
| Cyanopyrrolidine derivatives, LDN57444 | UCHL1 inhibitor | Preclinical [68,69,70] |
| MTX652, MTX114, MF0094 | USP30 inhibitors | Preclinical [71] |
Abbreviations: USP, ubiquitin-specific peptidase; UCHL1, ubiquitin carboxyl-terminal hydrolase L1.
USP14 inhibitors: The inhibition of Ub-specific protease 14 (USP14), a proteasome-associated DUB enzyme that binds to proteasomes, is a strategy to promote efficient proteasomal clearance of ubiquitylated proteins by preventing premature trimming of the Ub chain on the substrate [64]. In cultured cells, selective USP14 inhibitors, such as IU1, promote proteasome-mediated degradation of ND-associated proteins, such as Tau, TAR DNA binding protein 43 (TDP-43), and ataxin-3 [64,65]. In a PD fruit fly model, genetic or pharmacological inhibition of USP14 improved the phenotype of the disease and prolonged lifespan of the organism [66]. However, IU1 treatment reduces autophagy activity in cultured cells and induces the accumulation of HTT proteins with long, pathogenic polyQ repeats [67] showing a preference for autophagy-mediated clearance. Although USP14 inhibition may be substrate-specific, a reduction in the autophagy-lysosome pathway may be a potential neurotoxic mechanism. Further animal model studies are needed to validate the clinical usefulness of USP14 inhibition in the treatment of ND.
UCHL1 inhibitor: Another important DUB enzyme associated with ND pathogenesis is ubiquitin carboxyl-terminal hydrolase isozyme L1 (UCHL1), highly specific to neuron and is one of the most abundant soluble proteins in the brain [72]. UCHL1 binds to the PD-relevant protein α-synuclein, and pharmacological inhibition of UCHL1 in oligodendroglia prevents aggregation of α-synuclein by promoting autophagy [69]. Reducing UCHL1 activity, either by LDN57444 or genetic deletion, alleviates PD-related phenotypes, including reduced climbing ability and loss of dopaminergic neurons, by regulating glucose metabolism in PINK1- or Parkin-deficient mutant flies [70]. To date, LDN57444 is the only reported UCHL1 inhibitor that exhibits chemical instability and off-target toxicity [73]. Over the past few years, Mission Therapeutics, a drug development company targeting UPS in the UK, has developed cyanopyrrolidine derivatives as new inhibitors of UCHL1 and has filed a patent for the results [68]. However, information regarding their inhibitory potency in cells and their biological activities is still very limited.
USP30 inhibitors: The inhibition of Ub carboxyl-terminus hydrolase 30 (USP30), which acts as an antagonist of parkin, is a new strategy to ameliorate mitophagy deficits in PD. The mitochondrial-localized DUB USP30 can selectively induce mitochondrial ubiquitination, making it a particularly attractive drug target. Neuronal USP30 suppression improves mitophagy defects, motor function, and organism survival induced by parkin mutants in the Drosophila PD model [74]. Pharmaceutical companies are working to identify USP30 inhibitors, including phenylalanine derivatives, cyano-pyrrolidines, and phenyl- or naphthyl sulfonamide derivatives. For example, several small-molecule USP30 inhibitors have been developed by Mission Therapeutics and Mitobridge (Astellas Pharma Company), including MTX652, MTX114, and MF0094 [71]. Animal studies, including USP30 knockout studies, are essential for the future development of these therapeutics.
Pimozide: Pimozide has been approved by the US FDA as an antipsychotic drug. This compound was initially screened out as an anticancer drug, targeting its reversible inhibitory activity against the USP1/USP1-associated factor 1 (UAF1) complex [75]. Pimozide re-sensitizes NSCLC resistant to cisplatin, a platinum-based chemotherapeutic drug with sub-micromolar potency [75]. One substrate of the USP1/UAF1 deubiquitinase complex is TANK-binding kinase 1 (TBK1), a key regulator of autophagy [76]. In ND, heterozygous loss-of-function mutations in TBK1 have been identified as the cause of ALS [77]. USP1/UAF1 inhibition may promote TBK1 stabilization. Therefore, Pimozide is currently undergoing a phase II clinical trial in ALS patients in Canada (NCT03272503). Short-term (6 weeks) administration of this drug stabilizes the right hand muscles in patients with ALS [78].
2.2. SUMOylation
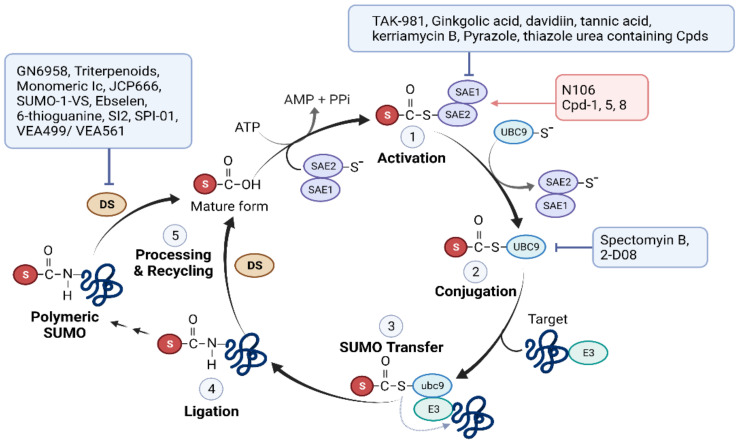
Small ubiquitin-related modifiers (SUMOs) are the most extensively studied UBLs. Similar to ubiquitination, SUMOylation/deSUMOylation requires E1-E2-E3 enzymes and isopeptidases [79]. These enzymes are SUMO-specific and do not overlap with enzymes used for ubiquitination. UBC9, the sole SUMO-specific E2 enzyme in mammals, can directly transfer SUMO to hundreds of SUMO substrates by directly binding to the SUMO consensus motif ψ-K-X-E, where ψ is a hydrophobic amino acid, and X can be located in any amino acid. Covalent binding of SUMO to a substrate often modulates its target function by recruiting other cellular proteins. Most known SUMO E3 enzymes harbor one or more SUMO interaction/binding motifs that mediate non-covalent interactions with SUMO. SUMOylation is a key regulator of gene expression, chromatin remodeling, ion channel activity, signal transduction, and sensing of oxidative stress, as it can alter the localization, activity, protein-protein interactions, and stability of its substrates [79]. The SUMOylation process and drugs targeting the different steps are shown in Figure 3.
Figure 3.
Small molecules targeting the SUMO pathway. In step 1: SUMO E1 (SAE1/SAE2 heterodimer) activates mature SUMO through an ATP-dependent reaction. SAE1 catalyzes adenylation of the C-terminus of SUMO to form a SUMO-AMP intermediate, which then transfers SUMO to SAE2 and forms a thioester bond. In step 2: SUMO is transferred from SAE2 to SUMO E2 (UBC9), which in turn forms a thioester bond. In steps 3 and 4: UBC9 catalyzes the formation of an isopeptide bond between the C-terminal glycine of SUMO and a lysine residue on the substrate. Certain SUMO E3 ligases are often involved in this process. In step 5: SUMO is removed from the lysine residue of the target proteins by a de-SUMOylation enzyme (DS), such as SENP, sentrin-specific protease. SENP also catalyzes SUMO maturation by cleaving the precursor SUMO at C-terminus, exposing two glycine residues required for conjugation.
2.2.1. Dysregulation of the SUMO Pathway in Cancer
In cancer cells, SUMO modifications are involved in carcinogenesis, differentiation, proliferation, metastasis, and apoptosis by regulating the DNA damage response, cell cycle, and cell-to-cell communication. PTMs can contribute to oncogenic or tumor suppressor signaling pathways in a context-dependent manner.
Abnormalities in the SUMOylation machinery in cancer tissues have been detected at the genetic, epigenetic, mRNA, and protein levels. Large-scale data from The Cancer Genome Atlas (TCGA) show that most SUMOylation/deSUMOylation-associated enzymes are upregulated in cancer, indicating an increased utility of SUMO modification in cancer cells. In some cases, their levels are positively correlated with the cancer stage, malignancy, and poor prognosis. For example, unbiased genetic screens have identified SAE1/SAE2, subunits of the SUMO-activating enzyme E1, as a genetic driver of Myc-dependent tumorigenesis [80]. The upregulation of SAE1/SAE2 is correlated with lower survival rates in patients with Myc-high breast cancer [80]. In addition, hyper-SUMOylation, which is associated with SAE1/SAE2 upregulation, is required for the progression of Myc-induced hematological malignancies [81] and small-cell lung cancer with high Myc expression [82]. SNPs in the UBC9 (UBE2I) and PIAS3 genes are associated with higher breast cancer risk and tumor grade [83]. In patients with MM, both gene and protein levels of UBC9 and PIAS1 are elevated and negatively correlated with patient survival [84]. Genetic mutations and the abnormal expression of SUMO deconjugases SENPs have also been reported. According to TCGA data, SENP isoforms are upregulated in most cancers [85]. A genome-wide epigenetic examination of clinical samples revealed promoter hypomethylation of SENP6 in hepatocellular carcinoma (HCC), providing evidence that elevated levels of SENP6 are associated with the promotion of HCC tumorigenesis [86]. The types of cancer for which SUMOylation defects have been reported in patients are summarized in Table 5.
Table 5.
Examples of SUMOylation components associated with cancer.
| Gene Name | Deregulation | Caner Type | |
|---|---|---|---|
| Modifier | SUMO1 | ↑ | PM in OC [TCGA] |
| SUMO2 | ↑ | PM in RC, EC, HCC [TCGA] | |
| SUMO3 | ↑ | PM in EC [TCGA] | |
| SUMO E1 | SAE1 | ↑ | PTC [87] PM in HCC, RC, TC [TCGA] |
| SAE2 | ↑ | BC [80], SCLC [81], PM in HCC, RC [TCGA] | |
| SUMO E2 | UBC9 | ↑ | Melanoma [88], PM in TC, HCC [TCGA] |
| SUMO E3 | PIAS1 | ↑ | PTC [87], PCA [89] |
| PIAS2 | ↓ | PTC [87], PM in TC [TCGA] | |
| PIAS3 | ↑ or ↓, Mutation | PM in RC, HCC [TCGA] | |
| PIAS4 | ↑ | PM in EC, PAC [TCGA] | |
| RANBP2 | ↑, Mutation | CRC [90] | |
| deSUMOylase | SENP1 | ↑ | PM in RC, HCC [TCGA] |
| SENP2 | ↓ or ↑, Mutation | PM in EC [TCGA] | |
| SENP3 | ↑ | PM in PAC [TCGA] | |
| SENP5 | ↑ | PM in RC, EC, HCC [TCGA] | |
| SENP6 | ↑ | PM in RC, TC [TCGA] | |
| SENP7 | Long↑; Short varient↓ | BC [91] | |
| ↑ | PM for HNC [TCGA] |
Abbreviations: BC, breast cancer; CRC, colorectal cancer; EC, endometrial cancer; HCC, hepatocellular carcinoma; HNC, Head and neck cancer; PAC, pancreatic cancer; PCA, prostate cancer; RC, renal cancer; TC, Thyroid cancer; SAE, SUMO-activating enzyme; SCC, squamous cell carcinoma; SENP, SUMO-specific proteases; SCLC, small cell lung cancer; OC, ovarian cancer; PIAS, protein inhibitor of activated STAT; PTC, papillary thyroid cancer; UBC9, ubiquitin-conjugating enzyme 9; ↑, Upregulation; ↓, Downregulation. PM, Prognostic marker; TCGA, The Cancer Genome Atlas.
2.2.2. SUMO Pathway Inhibitors Used to Treat Cancer
Several SUMOylation inhibitors with anticancer potential have been reported [92]. Examples of SUMOylation inhibitors are listed in Table 6 and Figure 3.
Table 6.
Selected inhibitors target in SUMO pathway.
| Compound ID | Description | Stage | |
|---|---|---|---|
| E1 | TAK-981 (Subasumstat) | The first-in-Class SAE Inhibitor | Phase I/II trials (https://clinicaltrials.gov/ct2/show/NCT03648372, accessed on 1 March 2022) |
| Ginkgolic acid, davidiin, tannic acid, kerriamycin B, Pyrazole, and thiazole urea containing Cpds | SAE inhibitor | Preclinical [93,94,95,96,112] | |
| E2 | 2-D08, Spectomyin B | UBC9 inhibitor | Preclinical [101,102,103,104,105,106] |
| SENP | GN6958, Triterpenoids, Monomeric Ic | SENP1 inhibitor | Preclinical [108,110,111] |
| JCP666 and its analogues | SENP1/2 inhibitor | Preclinical [113] | |
| SUMO-1-VS, Ebselen and 6-thioguanine | SENP2 inhibitor | Preclinical [114,115] | |
| SI2 | SENP1/2/3 inhibitor | Preclinical [109] | |
| SPI-01 | SENP1/2/7 inhibitor | Preclinical [109] | |
| VEA499/VEA561 | SENP1/2/6/7 inhibitor | Preclinical [113] |
Abbreviations: Cpd, compounds; SAE, SUMO-activating enzyme; UBC9, ubiquitin-conjugating enzyme 9; SENP, SUMO-specific proteases.
SUMO E1 (SAE) inhibitors: Several natural compounds, including ginkgolic acid [93], davidiin [94], tannic acid [95], and kerriamycin B [96], have been shown to inhibit SUMO E1. However, owing to the multifaceted pleiotropic effects of natural product-oriented SUMOylation inhibitors, much attention is being paid to the development of synthetic inhibitors with higher SUMO E1 complex specificity. For example, ML-792, a nanomolar potency small-molecule inhibitor of SUMO E1, has been developed. This compound forms a conjugate with SUMO, subsequently binds to SAE2, the catalytic subunit of SUMO E1, and inhibits its activity [97]. The selective cytotoxicity of ML-792 is elevated in cells overexpressing c-Myc [97]. TAK-981 is a mechanism-based inhibitor derived from ML-792, designed to improve the retention period of the TAK-981-SUMO adduct in vivo [98]. This agent inhibits SUMOylation (i.e., loss of SUMO2/3-protein conjugates) for approximately 15 to 20 h in human lymphoma xenograft mice treated with 10 mg/kg [99]. To date, TAK-981 (Subasumstat) is the only compound that directly targets SUMO E1 and SUMOylation, and has successfully entered clinical investigations in cancer patients. In vivo preclinical studies demonstrate TAK-81′s synergistic effects in combination with other immunomodulatory agents for cancer treatment [99]. Phase I/II studies are ongoing for the treatment of patients with solid tumors and lymphomas (monotherapy: NCT03648372; in combination with immunotherapy drugs: NCT04065555, NCT04074330, NCT04381650, and NCT04776018).
UBC9 inhibitors: UBC9 is the only conjugating enzyme in the SUMOylation process and is upregulated in various types of tumors [100], making it an attractive drug target. However, as in the case of Ub E2, efficient drug design to inhibit UBC9 is difficult due to its rigid structure, the absence of drug-processable pockets, and the presence of many protein-protein interaction sites. Several UBC9 inhibitors, such as 2-D08 [101] and spectomycin B1 (natural product) [102], show some promise in vitro because of their anticancer effects. For example, 2-D08 inhibits the migration of pancreatic cancer cells by regulating the oncogenic or pathogenic activities of K-Ras [103]. 2-D08 inhibitor promotes excessive ROS-mediated intrinsic mitochondrial apoptosis of acute myeloid leukemia (AML) cells [104]. Recent studies have indicated the potential benefits of 2-D08 inhibitors in the treatment of cancer combined with chemotherapy. Co-treatment with 2-D08 and etoposide, a clinically used chemotherapeutic drug, enhances the sensitivity of tumor cells to etoposide in vivo [105]. In many cases, despite the profound efficacy of 2-D08 found in vitro, its antitumor activity in vivo is unclear, which may be due to its low solubility and bioavailability [106]. Spectomycin B1 also validated its ability to bind directly to UBC9 and inhibit the formation of the UBC9-SUMO complex in the low-micromolar range. Antagonizing UBC9 by spectomycin B1 treatment prevents estrogen-dependent proliferation in MCF7 human breast cancer cells [102]. These results suggest the potential antitumor activity of spectomycin B1 against hormone-dependent breast cancer. However, these two agents have not been used in clinical studies. The development of other UBC9 chemical inhibitors using a small-molecule microarray approach is underway [107].
SENP inhibitors: The development of SENP-directed inhibitors began relatively early on. Although isoform inhibitors can improve drug efficacy and safety compared to pan-SENP inhibitors, the design of isotype-selective inhibitors is difficult because of their isopeptidase cleavage chemistry, protein structure, and the presence of similar amino acid sequences within the catalytic site [85]. Currently, SENP inhibitors mainly target SENP1, which is the most commonly analyzed inhibitor in clinical samples, and is a therapeutic target in ex vivo clinical studies (NCT03798587 and NCT04167605). SENP1 inhibitors have specifically been reported for the treatment of prostate cancer. For example, GN6958 [108] and SI2 [109] show SENP1-specific inhibitory activity in the micromolar range and exhibit antitumor activity in prostate cancer cells. Other reported SENP1 inhibitors are triterpenoids [110] and monomeric Ic [111]. These two natural products have demonstrated preclinical efficacy in vitro and in prostate cancer xenograft models. Approximately ten more peptides or compounds have been reported as SENP inhibitors without further efficacy studies. No SENP inhibitors have been clinically studied.
2.2.3. Role of SUMOylation in Neurodegenerative Disease Pathogenesis
Dysregulation of SUMOylation is likely involved in ND, because SUMO targets multiple proteins involved in neural development and function [116]. Studies have shown that protein SUMOylation directly regulates neurogenesis and plays a role in recovery from brain damage caused by cerebral ischemia, a causative factor of ND. Cerebral ischemia in mice and humans results in significant increases in SUMOylated proteins in the region surrounding cerebral lesions [117,118]. This PTM also plays a protective role against cellular stresses, such as glucose and oxygen starvation in neurons [119]. It is important to note that SUMO frequently co-localizes with neural inclusions, and SUMO modifications can enhance or prevent the formation of pathogenic protein aggregates in many cases of ND (Table 7). In addition, genetic mutations and altered expression of the SUMO machinery have been found in patients with ND. For example, an analysis of the genomic DNA of patients with late-onset AD revealed that polymorphisms in the UBC9 gene are significantly associated with the disease [120]. The downregulation of SENP3 mRNA expression [121] and SUMO2 levels [122] in the brain tissues of patients with AD is another example of the relationship between abnormal SUMOylation and AD pathological mechanisms.
Table 7.
Neurodegenerative disease-related key protein regulated by SUMO.
| Substrate | Substrate’s Function | Functional Impact | Disease |
|---|---|---|---|
| APP | Aβ generation | Negative regulation of Aβ aggregates levels | AD [123] |
| Tau | Microtubule stabilization | Induction of tau hyper-phosphorylation & inhibition of tau degradation | AD [124] |
| HTT | Microtubule-mediated transport and vesicle function | Increased cytotoxicity by specifically stabilizing mutant HTT via Rhes | HD [125] |
| α-Synuclein | PD pathogenesis | Maintanance of α-synuclein in a soluble form | PD [126] |
| DJ-1 | Anti-oxidative stress and transcriptional regulation | Essential for DJ-1 solubility and its function | PD [127] |
| Parkin | E3 Ub ligase | Induction of Parkin’s self-ubiquitination & nuclear translocation | PD [128] |
Abbreviations: Aβ, amyloid-β; AD, Alzheimer’s disease; APP, Amyloid-β precursor protein; HD, Huntington’s disease; HTT, Huntingtin; PD, Parkinson’s disease.
2.2.4. Therapeutics Targeting the SUMO Pathway in Neurodegenerative Diseases
Despite the importance of SUMOylation in neurodegeneration, functional studies have yielded inconsistent results, and appropriate animal models for studying SUMO in many NDs have not yet been established. Nevertheless, given the importance of proteolysis, SUMOylation inhibitors are gaining attention in ND therapy, and recent studies have suggested their potential as therapeutics. For example, ginkgolic acid, a natural compound with SUMO E1 inhibitory activity, reduces the levels of the mutant form of huntingtin and activates autophagy flux in cultured HD striatal cells [129]. 2-D08, a specific inhibitor of UBC9, exhibits concentration-dependent protective efficacy over the range between 10 to 100 µM against amyloid β protein neurotoxicity in cultured cells [130]. Computational modeling further showed that 2-D08 could bind to the 42 amino acid form of Aβ1–42 monomer with high affinity, thereby eliminating the pathological form of amyloid β.
There have also been reports of drug-like small molecules that enhance SUMOylation in ND. Krajnak and Dahl identified three small-molecule SUMOylation activators that directly targeted SUMO E1, and confirmed their neuroprotective efficacy in cultured cells. [131]. Given the findings of a study on cerebral ischemia, a temporary increase in SUMOylation at the border of the ischemic tissue is expected to have a therapeutic effect [132]. Studies using mouse neural stem cells (NSCs) have provided further evidence that upregulated SUMOylation is an essential component of ischemic tolerance. Activation of SUMOylation through UBC9 overexpression in NSCs confers a higher predisposition to differentiate into neurons in the brains of stroke mice. Further studies are needed to investigate whether pharmacological manipulation of SUMOylation can improve the outcomes of NSC-based therapy [133]. Currently, no SUMO-specific drugs are in clinical trials for patients with ND.
2.2.5. Dysregulation of SUMOylation in Heart Disease
SUMO modification is essential for the development, functioning, and pathogenesis of heart disease. In murine models, reduced SUMOylation activity, such as SUMO1 deficiency or SENP2 overexpression, can lead to fatal congenital heart disease [134,135]. SUMO1 knockdown induces contractile dysfunction and structural abnormalities in mice [136], whereas mouse hearts overexpressing SUMO2 or SENP5 develop extensive cardiac muscle dysfunction [137,138]. Similar to the other diseases described above, abnormalities in the SUMO machinery components have been found in humans, including heart failure, cardiomyopathy, and myocardial infarction (Table 8). There are no reports of genetic mutations in the SUMOylation component associated with heart disease. Similar to those in other organs, critical cardiac proteins, including sarcoplasmic reticulum Ca2+-ATPase pump (SERCA2a), responsible for stress adaptation and cardiac function, are physically and functionally linked to SUMOylation [139,140].
Table 8.
Heart disease related SUMO components.
| Component | Expression | Regulation Pathway | Disease | |
|---|---|---|---|---|
| Modifier | SUMO1 | ↓ | Heart development, cardiac pathology | CHD, HF [134,136] |
| SUMO2/3 conjugates | ↑ | Cardiac pathology | HF [137] | |
| E2 | UBC9 | ↑ | Authophagy | MI, CM [141,142] |
| Deconjugase | SENP1 | ↑ | Mithocondrial function | HF, MI/R [143,144] |
| SENP2 | ↑ | Heart development and function | CHD [134] | |
| SENP5 | ↑ | Mithocondrial function | HF [138] |
Abbreviations: CHD, Congenital heart disease; CM, cardiomyopathy; HF, Heart failure; MI/R, Myocardial Ischemia/Reperfusion injury; MI, Myocardial infarction; ↑, Upregulation; ↓, Downregulation.
2.2.6. Therapeutics Targeting the SUMO Pathway
Although clinical studies involving drugs targeting this pathway are not yet underway, SUMOylation has recently emerged as an exciting PTM that positively contributes to cardiac function and protein maintenance. For example, SUMO enhances the activity and protein stability of SERCA2a, a heart failure disease-modifying protein [145]. In murine and porcine models of heart failure, recovery of SUMO1 expression via gene transfer significantly improved cardiac contractility and hemodynamic parameters by restoring SERCA2a activity and SUMOylation. SUMO1 overexpression and gene transfer also restored SERCA2a downregulation and SERCA2a SUMOylation, resulting in significantly improved cardiac contractility and hemodynamic parameters [134,146]. More importantly, mouse studies suggest the potential of compound N106, an activator of SERCA2a SUMOylation that targets the SUMO E1 enzyme, as a therapy for heart failure [147]. Additionally, the cardioprotective effect of luteolin, a flavonoid with anticancer potential, has been reported to occur through SERCA2a SUMOylation [148]. These studies indicate that SUMOylation is a promising target for heart failure therapy.
An interesting study has suggested the importance of SUMOylation in cardiac protein quality control. Increased UBC9 expression enhances proteasome function and reduces protein aggregate levels in cell cultures and murine models of protein toxicity [149]. Given the results of ND study, targeting the ability of SUMOylation to regulate toxic proteins and interact with the UPS will be another novel therapeutic strategy. The identification and functional studies of SUMO-targeted ubiquitin ligases and SUMO deubiquitinases are currently ongoing [150].
3. Conclusions
Ub and Ubl are essential molecules for cellular homeostasis and function, and their modification processes are often poorly regulated in diseased states. Recently, ubiquitination and SUMOylation have attracted attention as novel therapeutic targets for complex diseases, such as cancer, neurodegenerative disorders, and heart disease. Many clinical investigations are underway on Ub- and SUMO-specific drugs. Synergistic effects of these drugs can be expected in clinical settings, because ubiquitination and SUMOylation not only modify the target protein, but are also associated with communication with other major PTMs, including phosphorylation and acetylation. Further studies on the disease-specific substrates of Ub/Ubl, the detailed molecular basis of modulating their modification process, and their physical and functional relationships with other PTMs will increase the likelihood of developing Ub/Ubl modulators as next-generation treatments for complex human diseases.
Author Contributions
Conceptualization, C.K., A.L. and J.-T.H.; writing—original draft preparation, C.K., A.L. and J.-T.H.; writing—review and editing, C.K., A.L. and J.-T.H.; funding acquisition, C.K. and J.-T.H. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was supported by the Research Program (no. E0210601-02) of the Korea Food Research Institute and Cooperative Research Program for Agriculture Science and Technology Development (Project No. PJ01573502) of the Rural Development Administration.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cappadocia L., Lima C.D. Ubiquitin-like Protein Conjugation: Structures, Chemistry, and Mechanism. Chem. Rev. 2018;118:889–918. doi: 10.1021/acs.chemrev.6b00737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hochstrasser M. Evolution and function of ubiquitin-like protein-conjugation systems. Nat. Cell Biol. 2000;2:E153–E157. doi: 10.1038/35019643. [DOI] [PubMed] [Google Scholar]
- 3.Kerscher O., Felberbaum R., Hochstrasser M. Modification of proteins by ubiquitin and ubiquitin-like proteins. Annu. Rev. Cell Dev. Biol. 2006;22:159–180. doi: 10.1146/annurev.cellbio.22.010605.093503. [DOI] [PubMed] [Google Scholar]
- 4.Park C.W., Ryu K.Y. Cellular ubiquitin pool dynamics and homeostasis. BMB Rep. 2014;47:475–482. doi: 10.5483/BMBRep.2014.47.9.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Popovic D., Vucic D., Dikic I. Ubiquitination in disease pathogenesis and treatment. Nat. Med. 2014;20:1242–1253. doi: 10.1038/nm.3739. [DOI] [PubMed] [Google Scholar]
- 6.Schulman B.A., Harper J.W. Ubiquitin-like protein activation by E1 enzymes: The apex for downstream signalling pathways. Nat. Rev. Mol. Cell Biol. 2009;10:319–331. doi: 10.1038/nrm2673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ruosaari S., Hienonen-Kempas T., Puustinen A., Sarhadi V.K., Hollmén J., Knuutila S., Saharinen J., Wikman H., Anttila S. Pathways affected by asbestos exposure in normal and tumour tissue of lung cancer patients. BMC Med. Genom. 2008;1:55. doi: 10.1186/1755-8794-1-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McHugh A., Fernandes K., South A.P., Mellerio J.E., Salas-Alanís J.C., Proby C.M., Leigh I.M., Saville M.K. Preclinical comparison of proteasome and ubiquitin E1 enzyme inhibitors in cutaneous squamous cell carcinoma: The identification of mechanisms of differential sensitivity. Oncotarget. 2018;9:20265–20281. doi: 10.18632/oncotarget.24750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xu G.W., Ali M., Wood T.E., Wong D., Maclean N., Wang X., Gronda M., Skrtic M., Li X., Hurren R., et al. The ubiquitin-activating enzyme E1 as a therapeutic target for the treatment of leukemia and multiple myeloma. Blood. 2010;115:2251–2259. doi: 10.1182/blood-2009-07-231191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ma X., Zhao J., Yang F., Liu H., Qi W. Ubiquitin conjugating enzyme E2 L3 promoted tumor growth of NSCLC through accelerating p27kip1 ubiquitination and degradation. Oncotarget. 2017;8:84193–84203. doi: 10.18632/oncotarget.20449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lu J., Zhao H., Yu C., Kang Y., Yang X. Targeting Ubiquitin-Specific Protease 7 (USP7) in Cancer: A New Insight to Overcome Drug Resistance. Front. Pharmacol. 2021;12:648491. doi: 10.3389/fphar.2021.648491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shen J.D., Fu S.Z., Ju L.L., Wang Y.F., Dai F., Liu Z.X., Ji H.Z., Shao J.G., Bian Z.L. High expression of ubiquitin-conjugating enzyme E2A predicts poor prognosis in hepatocellular carcinoma. Oncol. Lett. 2018;15:7362–7368. doi: 10.3892/ol.2018.8189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Luo H., Qin Y., Reu F., Ye S., Dai Y., Huang J., Wang F., Zhang D., Pan L., Zhu H., et al. Microarray-based analysis and clinical validation identify ubiquitin-conjugating enzyme E2E1 (UBE2E1) as a prognostic factor in acute myeloid leukemia. J. Hematol. Oncol. 2016;9:125. doi: 10.1186/s13045-016-0356-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gallo L.H., Ko J., Donoghue D.J. The importance of regulatory ubiquitination in cancer and metastasis. Cell Cycle. 2017;16:634–648. doi: 10.1080/15384101.2017.1288326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yu M., Hong W., Ruan S., Guan R., Tu L., Huang B., Hou B., Jian Z., Ma L., Jin H. Genome-wide profiling of prognostic alternative splicing pattern in pancreatic cancer. Front. Oncol. 2019;9:773. doi: 10.3389/fonc.2019.00773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Davis R.J., Welcker M., Clurman B.E. Tumor suppression by the Fbw7 ubiquitin ligase: Mechanisms and opportunities. Cancer Cell. 2014;26:455–464. doi: 10.1016/j.ccell.2014.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ma M., Yu N. Ubiquitin-specific protease 7 expression is a prognostic factor in epithelial ovarian cancer and correlates with lymph node metastasis. OncoTargets Ther. 2016;9:1559–1569. doi: 10.2147/OTT.S100050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cheng C., Niu C., Yang Y., Wang Y., Lu M. Expression of HAUSP in gliomas correlates with disease progression and survival of patients. Oncol. Rep. 2013;29:1730–1736. doi: 10.3892/or.2013.2342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wu Y., Wang Y., Yang X.H., Kang T., Zhao Y., Wang C., Evers B.M., Zhou B.P. The Deubiquitinase USP28 Stabilizes LSD1 and Confers Stem-Cell-like Traits to Breast Cancer Cells. Cell Rep. 2013;5:224–236. doi: 10.1016/j.celrep.2013.08.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Diefenbacher M.E., Popov N., Blake S.M., Schülein-Völk C., Nye E., Spencer-Dene B., Jaenicke L.A., Eilers M., Behrens A. The deubiquitinase USP28 controls intestinal homeostasis and promotes colorectal cancer. J. Clin. Investig. 2014;124:3407–3418. doi: 10.1172/JCI73733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hou K., Zhu Z., Wang Y., Zhang C., Yu S., Zhu Q., Yan B. Overexpression and Biological Function of Ubiquitin-Specific Protease 42 in Gastric Cancer. PLoS ONE. 2016;11:e0152997. doi: 10.1371/journal.pone.0152997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shah J., Usmani S., Stadtmauer E.A., Rifkin R.M., Berenson J.R., Berdeja J.G., Lyons R.M., Klippel Z., Chang Y.L., Niesvizky R. Oprozomib, pomalidomide, and Dexamethasone in Patients with Relapsed and/or Refractory Multiple Myeloma. Clin. Lymphoma Myeloma Leuk. 2019;19:570–578.e1. doi: 10.1016/j.clml.2019.05.017. [DOI] [PubMed] [Google Scholar]
- 23.Gallerani E., Zucchetti M., Brunelli D., Marangon E., Noberasco C., Hess D., Delmonte A., Martinelli G., Böhm S., Driessen C., et al. A first in human phase I study of the proteasome inhibitor CEP-18770 in patients with advanced solid tumours and multiple myeloma. Eur. J. Cancer. 2013;49:290–296. doi: 10.1016/j.ejca.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 24.Vogl D.T., Martin T.G., Vij R., Hari P., Mikhael J.R., Siegel D., Wu K.L., Delforge M., Gasparetto C. Phase I/II study of the novel proteasome inhibitor delanzomib (CEP-18770) for relapsed and refractory multiple myeloma. Leuk. Lymphoma. 2017;58:1872–1879. doi: 10.1080/10428194.2016.1263842. [DOI] [PubMed] [Google Scholar]
- 25.Nunes A.T., Annunziata C.M. Proteasome inhibitors: Structure and function. Semin. Oncol. 2017;6:377–380. doi: 10.1053/j.seminoncol.2018.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barghout S.H., Schimmer A.D. E1 Enzymes as Therapeutic Targets in Cancer. Pharmacol. Rev. 2021;73:1–58. doi: 10.1124/pharmrev.120.000053. [DOI] [PubMed] [Google Scholar]
- 27.Soucy T.A., Smith P.G., Milhollen M.A., Berger A.J., Gavin J.M., Adhikari S., Brownell J.E., Burke K.E., Cardin D.P., Critchley S. An inhibitor of NEDD8-activating enzyme as a new approach to treat cancer. Nature. 2009;458:732–736. doi: 10.1038/nature07884. [DOI] [PubMed] [Google Scholar]
- 28.Hyer M.L., Milhollen M.A., Ciavarri J., Fleming P., Traore T., Sappal D., Huck J., Shi J., Gavin J., Brownell J., et al. A small-molecule inhibitor of the ubiquitin activating enzyme for cancer treatment. Nat. Med. 2018;24:186–193. doi: 10.1038/nm.4474. [DOI] [PubMed] [Google Scholar]
- 29.Konopleva M., Martinelli G., Daver N., Papayannidis C., Wei A., Higgins B., Ott M., Mascarenhas J., Andreeff M. MDM2 inhibition: An important step forward in cancer therapy. Leukemia. 2020;34:2858–2874. doi: 10.1038/s41375-020-0949-z. [DOI] [PubMed] [Google Scholar]
- 30.Békés M., Langley D.R., Crews C.M. PROTAC targeted protein degraders: The past is prologue. Nat. Rev. Drug Discov. 2022;21:181–200. doi: 10.1038/s41573-021-00371-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Harrigan J.A., Jacq X., Martin N.M., Jackson S.P. Deubiquitylating enzymes and drug discovery: Emerging opportunities. Nat. Rev. Drug Discov. 2018;17:57–78. doi: 10.1038/nrd.2017.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Antao A.M., Tyagi A., Kim K.S., Ramakrishna S. Advances in Deubiquitinating Enzyme Inhibition and Applications in Cancer Therapeutics. Cancers. 2020;12:1579. doi: 10.3390/cancers12061579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rowinsky E.K., Paner A., Berdeja J.G., Paba-Prada C., Venugopal P., Porkka K., Gullbo J., Linder S., Loskog A., Richardson P.G., et al. Phase 1 study of the protein deubiquitinase inhibitor VLX1570 in patients with relapsed and/or refractory multiple myeloma. Investig. New Drugs. 2020;38:1448–1453. doi: 10.1007/s10637-020-00915-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kane R.C., Bross P.F., Farrell A.T., Pazdur R. Velcade: U.S. FDA approval for the treatment of multiple myeloma progressing on prior therapy. Oncologist. 2003;8:508–513. doi: 10.1634/theoncologist.8-6-508. [DOI] [PubMed] [Google Scholar]
- 35.Katsnelson A. Next-generation proteasome inhibitor approved in multiple myeloma. Nat. Biotechnol. 2012;30:1011–1102. doi: 10.1038/nbt1112-1011. [DOI] [PubMed] [Google Scholar]
- 36.Shirley M. Ixazomib: First Global Approval. Drugs. 2016;76:405–411. doi: 10.1007/s40265-016-0548-5. [DOI] [PubMed] [Google Scholar]
- 37.Schmidt M.F., Gan Z.Y., Komander D., Dewson G. Ubiquitin signalling in neurodegeneration: Mechanisms and therapeutic opportunities. Cell Death Differ. 2021;28:570–590. doi: 10.1038/s41418-020-00706-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Petrucelli L., Dickson D., Kehoe K., Taylor J., Snyder H., Grover A., De Lucia M., McGowan E., Lewis J., Prihar G., et al. CHIP and Hsp70 regulate tau ubiquitination, degradation and aggregation. Hum. Mol. Genet. 2004;13:703–714. doi: 10.1093/hmg/ddh083. [DOI] [PubMed] [Google Scholar]
- 39.Rotblat B., Southwell A.L., Ehrnhoefer D.E., Skotte N.H., Metzler M., Franciosi S., Leprivier G., Somasekharan S.P., Barokas A., Deng Y., et al. HACE1 reduces oxidative stress and mutant Huntingtin toxicity by promoting the NRF2 response. Proc. Natl. Acad. Sci. USA. 2014;111:3032–3037. doi: 10.1073/pnas.1314421111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kaneko M., Koike H., Saito R., Kitamura Y., Okuma Y., Nomura Y. Loss of HRD1-mediated protein degradation causes amyloid precursor protein accumulation and amyloid-beta generation. J. Neurosci. 2010;30:3924–3932. doi: 10.1523/JNEUROSCI.2422-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kwak Y.-D., Wang B., Li J.J., Wang R., Deng Q., Diao S., Chen Y., Xu R., Masliah E., Xu H., et al. Upregulation of the E3 ligase NEDD4-1 by Oxidative Stress Degrades IGF-1 Receptor Protein in Neurodegeneration. J. Neurosci. 2012;32:10971–10981. doi: 10.1523/JNEUROSCI.1836-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liu Q.Y., Lei J.X., Sikorska M., Liu R. A novel brain-enriched E3 ubiquitin ligase RNF182 is up regulated in the brains of Alzheimer’s patients and targets ATP6V0C for degradation. Mol. Neurodegener. 2008;3:4. doi: 10.1186/1750-1326-3-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chung J.Y., Park H.R., Lee S.J., Lee S.H., Kim J.S., Jung Y.S., Hwang S.H., Ha N.C., Seol W.G., Lee J., et al. Elevated TRAF2/6 expression in Parkinson’s disease is caused by the loss of Parkin E3 ligase activity. Lab. Investig. 2013;93:663–676. doi: 10.1038/labinvest.2013.60. [DOI] [PubMed] [Google Scholar]
- 44.Zucchelli S., Marcuzzi F., Codrich M., Agostoni E., Vilotti S., Biagioli M., Pinto M., Carnemolla A., Santoro C., Gustincich S., et al. Tumor necrosis factor receptor-associated factor 6 (TRAF6) associates with huntingtin protein and promotes its atypical ubiquitination to enhance aggregate formation. J. Biol. Chem. 2011;286:25108–25117. doi: 10.1074/jbc.M110.187591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Liu X., Hebron M., Shi W., Lonskaya I., Moussa C.E. Ubiquitin specific protease-13 independently regulates parkin ubiquitination and alpha-synuclein clearance in alpha-synucleinopathies. Hum. Mol. Genet. 2019;28:548–560. doi: 10.1093/hmg/ddy365. [DOI] [PubMed] [Google Scholar]
- 46.Van Leeuwen F.W., de Kleijn D.P., van den Hurk H.H., Neubauer A., Sonnemans M.A., Sluijs J.A., Köycü S., Ramdjielal R.D., Salehi A., Martens G.J., et al. Frameshift mutants of beta amyloid precursor protein and ubiquitin-B in Alzheimer’s and Down’s patients. Science. 1998;279:242–247. doi: 10.1126/science.279.5348.242. [DOI] [PubMed] [Google Scholar]
- 47.Krutauz D., Reis N., Nakasone M.A., Siman P., Zhang D., Kirkpatrick D.S., Gygi S.P., Brik A., Fushman D., Glickman M.H. Extended ubiquitin species are protein-based DUB inhibitors. Nat. Chem. Biol. 2014;10:664–670. doi: 10.1038/nchembio.1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tan Z., Sun X., Fy H., Hw O., Hilgenberg L.G.W., Hol E.M., van Leeuwen F.W., Smith M.A., O’Dowd D.K., Schreiber S.S. Mutant ubiquitin found in Alzheimer’s disease causes neuritic beading of mitochondria in association with neuronal degeneration. Cell Death Differ. 2007;14:1721–1732. doi: 10.1038/sj.cdd.4402180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Huang X., Chen J., Cao W., Yang L., Chen Q., He J., Yi Q., Huang H., Zhang E., Cai Z. The many substrates and functions of NEDD4-1. Cell Death Dis. 2019;10:1–12. doi: 10.1038/s41419-019-2142-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rivera E.J., Goldin A., Fulmer N., Tavares R., Wands J.R., de la Monte S.M. Insulin and insulin-like growth factor expression and function deteriorate with progression of Alzheimer’s disease: Link to brain reductions in acetylcholine. J. Alzheimer’s Dis. 2005;8:247–268. doi: 10.3233/JAD-2005-8304. [DOI] [PubMed] [Google Scholar]
- 51.Rodrigues E.M., Scudder S.L., Goo M.S., Patrick G.N. Aβ-Induced Synaptic Alterations Require the E3 Ubiquitin Ligase Nedd4-1. J. Neurosci. 2016;36:1590–1595. doi: 10.1523/JNEUROSCI.2964-15.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Carter T.L., Rissman R.A., Mishizen-Eberz A.J., Wolfe B.B., Hamilton R.L., Gandy S., Armstrong D.M. Differential preservation of AMPA receptor subunits in the hippocampi of Alzheimer’s disease patients according to Braak stage. Exp. Neurol. 2004;187:299–309. doi: 10.1016/j.expneurol.2003.12.010. [DOI] [PubMed] [Google Scholar]
- 53.Olabarria M., Pasini S., Corona C., Robador P., Song C., Patel H., Lefort R. Dysfunction of the ubiquitin ligase E3A Ube3A/E6-AP contributes to synaptic pathology in Alzheimer’s disease. Commun. Biol. 2019;2:111. doi: 10.1038/s42003-019-0350-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Maranga C., Fernandes T.G., Bekman E., Da Rocha S.T. Angelman syndrome: A journey through the brain. FEBS J. 2020;287:2154–2175. doi: 10.1111/febs.15258. [DOI] [PubMed] [Google Scholar]
- 55.Singh B.K., Vatsa N., Kumar V., Shekhar S., Sharma A., Jana N.R. Ube3a deficiency inhibits amyloid plaque formation in APPswe/PS1δE9 mouse model of Alzheimer’s disease. Hum. Mol. Genet. 2017;26:4042–4054. doi: 10.1093/hmg/ddx295. [DOI] [PubMed] [Google Scholar]
- 56.Shimura H., Schlossmacher M.G., Hattori N., Frosch M.P., Trockenbacher A., Schneider R., Mizuno Y., Kosik K.S., Selkoe D.J. Ubiquitination of a new form of α-synuclein by parkin from human brain: Implications for Parkinson’s disease. Science. 2001;293:263–269. doi: 10.1126/science.1060627. [DOI] [PubMed] [Google Scholar]
- 57.Dawson T.M., Dawson V.L. The role of parkin in familial and sporadic Parkinson’s disease. Mov. Disord. 2010;25:S32–S39. doi: 10.1002/mds.22798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Clark E.H., Vázquez de la Torre A., Hoshikawa T., Briston T. Targeting mitophagy in Parkinson’s disease. J. Biol. Chem. 2021;296:100209. doi: 10.1074/jbc.REV120.014294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Leroy E., Boyer R., Auburger G., Leube B., Ulm G., Mezey E., Harta G., Brownstein M.J., Jonnalagada S., Chernova T., et al. The ubiquitin pathway in Parkinson’s disease. Nature. 1998;395:451–452. doi: 10.1038/26652. [DOI] [PubMed] [Google Scholar]
- 60.Setsuie R., Wang Y.L., Mochizuki H., Osaka H., Hayakawa H., Ichihara N., Li H., Furuta A., Sano Y., Sun Y.J., et al. Dopaminergic neuronal loss in transgenic mice expressing the Parkinson’s disease-associated UCH-L1 I93M mutant. Neurochem. Int. 2007;50:119–129. doi: 10.1016/j.neuint.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 61.Choi J., Levey A.I., Weintraub S.T., Rees H.D., Gearing M., Chin L.S., Li L. Oxidative modifications and down-regulation of ubiquitin carboxyl-terminal hydrolase L1 associated with idiopathic Parkinson’s and Alzheimer’s diseases. J. Biol. Chem. 2004;279:13256–13264. doi: 10.1074/jbc.M314124200. [DOI] [PubMed] [Google Scholar]
- 62.Tofaris G.K., Kim H.T., Hourez R., Jung J.W., Kim K.P., Goldberg A.L. Ubiquitin ligase Nedd4 promotes alpha-synuclein degradation by the endosomal-lysosomal pathway. Proc. Natl. Acad. Sci. USA. 2011;108:17004–17009. doi: 10.1073/pnas.1109356108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Davies S.E., Hallett P.J., Moens T., Smith G., Mangano E., Kim H.T., Goldberg A.L., Liu J.L., Isacson O., Tofaris G.K. Enhanced ubiquitin-dependent degradation by Nedd4 protects against α-synuclein accumulation and toxicity in animal models of Parkinson’s disease. Neurobiol. Dis. 2014;64:79–87. doi: 10.1016/j.nbd.2013.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lee B.H., Lee M.J., Park S., Oh D.C., Elsasser S., Chen P.C., Gartner C., Dimova N., Hanna J., Gygi S.P., et al. Enhancement of proteasome activity by a small-molecule inhibitor of USP14. Nature. 2010;467:179–184. doi: 10.1038/nature09299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Boselli M., Lee B.H., Robert J., Prado M.A., Min S.W., Cheng C., Silva M.C., Seong C., Elsasser S., Hatle K.M., et al. An Inhibitor of the Proteasomal Deubiquitinating Enzyme USP14 Induces Tau Elimination in Cultured Neurons. J. Biol. Chem. 2017;292:19209–19225. doi: 10.1074/jbc.M117.815126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chakraborty J., von Stockum S., Marchesan E., Caicci F., Ferrari V., Rakovic A., Klein C., Antonini A., Bubacco L., Ziviani E. USP14 inhibition corrects an in vivo model of impaired mitophagy. EMBO Mol. Med. 2018;10:e9014. doi: 10.15252/emmm.201809014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kim E., Park S., Lee J.H., Mun J.Y., Choi W.H., Yun Y., Lee J., Kim J.H., Kang M.J., Lee M.J. Dual Function of USP14 Deubiquitinase in Cellular Proteasomal Activity and Autophagic Flux. Cell Rep. 2018;24:732–743. doi: 10.1016/j.celrep.2018.06.058. [DOI] [PubMed] [Google Scholar]
- 68.Kemp M., Stockley M., Jones A. Cyanopyrrolidines as Dub Inhibitors for the Treatment of Cancer. WO 2017009650 (A1) 2017 January 19;
- 69.Pukass K., Richter-Landsberg C. Inhibition of UCH-L1 in oligodendroglial cells results in microtubule stabilization and prevents alpha-synuclein aggregate formation by activating the autophagic pathway: Implications for multiple system atrophy. Front. Cell. Neurosci. 2015;9:163. doi: 10.3389/fncel.2015.00163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ham S.J., Lee D., Xu W.J., Cho E., Choi S., Min S., Park S., Chung J. Loss of UCHL1 rescues the defects related to Parkinson’s disease by suppressing glycolysis. Sci. Adv. 2021;7:eabg4574. doi: 10.1126/sciadv.abg4574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kluge A.F., Lagu B.R., Maiti P., Jaleel M., Webb M., Malhotra J., Mallat A., Srinivas P.A., Thompson J.E. Novel highly selective inhibitors of ubiquitin specific protease 30 (USP30) accelerate mitophagy. Bioorg. Med. Chem. Lett. 2018;28:2655–2659. doi: 10.1016/j.bmcl.2018.05.013. [DOI] [PubMed] [Google Scholar]
- 72.Cartier A.E., Djakovic S.N., Salehi A., Wilson S.M., Masliah E., Patrick G.N. Regulation of synaptic structure by ubiquitin C-terminal hydrolase L1. J. Neurosci. 2009;29:7857–7868. doi: 10.1523/JNEUROSCI.1817-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hussain S., Bedekovics T., Chesi M., Bergsagel P.L., Galardy P.J. UCHL1 is a biomarker of aggressive multiple myeloma required for disease progression. Oncotarget. 2015;6:40704–40718. doi: 10.18632/oncotarget.5727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bingol B., Tea J.S., Phu L., Reichelt M., Bakalarski C.E., Song Q., Foreman O., Kirkpatrick D.S., Sheng M. The mitochondrial deubiquitinase USP30 opposes parkin-mediated mitophagy. Nature. 2014;510:370–375. doi: 10.1038/nature13418. [DOI] [PubMed] [Google Scholar]
- 75.Chen J., Dexheimer T.S., Ai Y., Liang Q., Villamil M.A., Inglese J., Maloney D.J., Jadhav A., Simeonov A., Zhuang Z. Selective and cell-active inhibitors of the USP1/UAF1 deubiquitinase complex reverse cisplatin resistance in non-small cell lung cancer cells. Chem. Biol. 2011;18:1390–1400. doi: 10.1016/j.chembiol.2011.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zhongxia Y., Hui S., Mutian J., Jintao Z., Wenwen W., Qi L., Lining Z., Wei Z. USP1–UAF1 deubiquitinase complex stabilizes TBK1 and enhances antiviral responses. J. Exp. Med. 2017;214:3553–3563. doi: 10.1084/jem.20170180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Freischmidt A., Wieland T., Richter B., Ruf W., Schaeffer V., Muller K., Marroquin N., Nordin F., Hubers A., Weydt P., et al. Haploinsufficiency of TBK1 causes familial ALS and fronto-temporal dementia. Nat. Neurosci. 2015;18:631–636. doi: 10.1038/nn.4000. [DOI] [PubMed] [Google Scholar]
- 78.Patten S.A., Aggad D., Martinez J., Tremblay E., Petrillo J., Armstrong G.A., La Fontaine A., Maios C., Liao M., Ciura S., et al. Neuroleptics as therapeutic compounds stabilizing neuromuscular transmission in amyotrophic lateral sclerosis. JCI Insight. 2017;2:e97152. doi: 10.1172/jci.insight.97152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Celen A.B., Sahin U. Sumoylation on its 25th anniversary: Mechanisms, pathology, and emerging concepts. FEBS J. 2020;287:3110–3140. doi: 10.1111/febs.15319. [DOI] [PubMed] [Google Scholar]
- 80.Kessler J.D., Kahle K.T., Sun T., Meerbrey K.L., Schlabach M.R., Schmitt E.M., Skinner S.O., Xu Q., Li M.Z., Hartman Z.C., et al. A SUMOylation-dependent transcriptional subprogram is required for Myc-driven tumorigenesis. Science. 2012;335:348–353. doi: 10.1126/science.1212728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hoellein A., Fallahi M., Schoeffmann S., Steidle S., Schaub F.X., Rudelius M., Laitinen I., Nilsson L., Goga A., Peschel C., et al. Myc-induced SUMOylation is a therapeutic vulnerability for B-cell lymphoma. Blood. 2014;124:2081–2090. doi: 10.1182/blood-2014-06-584524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Liu X., Xu Y., Pang Z., Guo F., Qin Q., Yin T., Sang Y., Feng C., Li X., Jiang L., et al. Knockdown of SUMO-activating enzyme subunit 2 (SAE2) suppresses cancer malignancy and enhances chemotherapy sensitivity in small cell lung cancer. J. Hematol. Oncol. 2015;8:67. doi: 10.1186/s13045-015-0164-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Dünnebier T., Bermejo J.L., Haas S., Fischer H.P., Pierl C.B., Justenhoven C., Brauch H., Baisch C., Gilbert M., Harth V., et al. Polymorphisms in the UBC9 and PIAS3 genes of the SUMO-conjugating system and breast cancer risk. Breast Cancer Res. Treat. 2010;121:185–194. doi: 10.1007/s10549-009-0530-y. [DOI] [PubMed] [Google Scholar]
- 84.Driscoll J.J., Pelluru D., Lefkimmiatis K., Fulciniti M., Prabhala R.H., Greipp P.R., Barlogie B., Tai Y.T., Anderson K.C., Shaughnessy J.D., Jr., et al. The sumoylation pathway is dysregulated in multiple myeloma and is associated with adverse patient outcome. Blood. 2010;115:2827–2834. doi: 10.1182/blood-2009-03-211045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tokarz P., Woźniak K. SENP Proteases as Potential Targets for Cancer Therapy. Cancers. 2021;13:2059. doi: 10.3390/cancers13092059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Stefanska B., Cheishvili D., Suderman M., Arakelian A., Huang J., Hallett M., Han Z.G., Al-Mahtab M., Akbar S.M., Khan W.A., et al. Genome-wide study of hypomethylated and induced genes in patients with liver cancer unravels novel anticancer targets. Clin. Cancer Res. 2014;20:3118–3132. doi: 10.1158/1078-0432.CCR-13-0283. [DOI] [PubMed] [Google Scholar]
- 87.Tuccilli C., Baldini E., Sorrenti S., Di Gioia C., Bosco D., Ascoli V., Mian C., Barollo S., Rendina R., Coccaro C., et al. Papillary Thyroid Cancer Is Characterized by Altered Expression of Genes Involved in The Sumoylation Process. J. Biol. Regul. Homeost. Agents. 2015;29:655–662. [PubMed] [Google Scholar]
- 88.Moschos S.J., Smith A.P., Mandic M., Athanassiou C., Watson-Hurst K., Jukic D.M., Edington H.D., Kirkwood J.M., Becker D. SAGE and antibody array analysis of melanoma-infiltrated lymph nodes: Identification of Ubc9 as an important molecule in advanced-stage melanomas. Oncogene. 2007;26:4216–4225. doi: 10.1038/sj.onc.1210216. [DOI] [PubMed] [Google Scholar]
- 89.Hoefer J., Schäfer G., Klocker H., Erb H.H., Mills I.G., Hengst L., Puhr M., Culig Z. PIAS1 is increased in human prostate cancer and enhances proliferation through inhibition of p21. Am. J. Pathol. 2012;180:2097–2107. doi: 10.1016/j.ajpath.2012.01.026. [DOI] [PubMed] [Google Scholar]
- 90.Vecchione L., Gambino V., Raaijmakers J., Schlicker A., Fumagalli A., Russo M., Villanueva A., Beerling E., Bartolini A., Mollevi D.G., et al. A Vulnerability of a Subset of Colon Cancers with Potential Clinical Utility. Cell. 2016;165:317–330. doi: 10.1016/j.cell.2016.02.059. [DOI] [PubMed] [Google Scholar]
- 91.Bawa-Khalfe T., Lu L.S., Zuo Y., Huang C., Dere R., Lin F.M., Yeh E.T. Differential expression of SUMO-specific protease 7 variants regulates epithelial-mesenchymal transition. Proc. Natl. Acad. Sci. USA. 2012;109:17466–17471. doi: 10.1073/pnas.1209378109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Brackett C.M., Blagg B.S.J. Current Status of SUMOylation Inhibitors. Curr. Med. Chem. 2021;28:3892–3912. doi: 10.2174/0929867327666200810135039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Fukuda I., Ito A., Hirai G., Nishimura S., Kawasaki H., Saitoh H., Kimura K., Sodeoka M., Yoshida M. Ginkgolic acid inhibits protein SUMOylation by blocking formation of the E1-SUMO intermediate. Chem. Biol. 2009;16:133–140. doi: 10.1016/j.chembiol.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 94.Takemoto M., Kawamural Y., Hirohama M., Yamaguchi Y., Handa H., Saitoh H., Nakao Y., Kawada M., Khalid K., Koshino H., et al. Inhibition of protein SUMOylation by davidiin, an ellagitannin from Davidia involucrata. J. Antibiot. 2014;67:335–338. doi: 10.1038/ja.2013.142. [DOI] [PubMed] [Google Scholar]
- 95.Suzawa M., Miranda D.A., Ramos K.A., Ang K.K., Faivre E.J., Wilson C.G., Caboni L., Arkin M.R., Kim Y.S., Fletterick R.J., et al. A gene-expression screen identifies a non-toxic sumoylation inhibitor that mimics SUMO-less human LRH-1 in liver. eLife. 2015;4:e09003. doi: 10.7554/eLife.09003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Fukuda I., Ito A., Uramoto M., Saitoh H., Kawasaki H., Osada H., Yoshida M. Kerriamycin B inhibits protein SUMOylation. J. Antibiot. 2009;62:221–224. doi: 10.1038/ja.2009.10. [DOI] [PubMed] [Google Scholar]
- 97.He X., Riceberg J., Soucy T., Koenig E., Minissale J., Gallery M., Bernard H., Yang X., Liao H., Rabino C., et al. Probing the roles of SUMOylation in cancer cell biology by using a selective SAE inhibitor. Nat. Chem. Biol. 2017;13:1164–1171. doi: 10.1038/nchembio.2463. [DOI] [PubMed] [Google Scholar]
- 98.Langston S.P., Grossman S., England D., Afroze R., Bence N., Bowman D., Bump N., Chau R., Chuang B.C., Claiborne C., et al. Discovery of TAK-981, a First-in-Class Inhibitor of SUMO-Activating Enzyme for the Treatment of Cancer. J. Med. Chem. 2021;64:2501–2520. doi: 10.1021/acs.jmedchem.0c01491. [DOI] [PubMed] [Google Scholar]
- 99.Lightcap E.S., Yu P., Grossman S., Song K., Khattar M., Xega K., He X., Gavin J.M., Imaichi H., Garnsey J.J., et al. A small-molecule SUMOylation inhibitor activates antitumor immune responses and potentiates immune therapies in preclinical models. Sci. Transl. Med. 2021;13:eaba7791. doi: 10.1126/scitranslmed.aba7791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Seeler J.S., Dejean A. SUMO and the robustness of cancer. Nat. Rev. Cancer. 2017;17:184–197. doi: 10.1038/nrc.2016.143. [DOI] [PubMed] [Google Scholar]
- 101.Kim Y.S., Keyser S.G., Schneekloth J.S., Jr. Synthesis of 2′,3′,4′-trihydroxyflavone (2-D08), an inhibitor of protein sumoylation. Bioorg. Med. Chem. Lett. 2014;24:1094–1097. doi: 10.1016/j.bmcl.2014.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Hirohama M., Kumar A., Fukuda I., Matsuoka S., Igarashi Y., Saitoh H., Takagi M., Shin-ya K., Honda K., Kondoh Y., et al. Spectomycin B1 as a novel SUMOylation inhibitor that directly binds to SUMO E2. ACS Chem. Biol. 2013;8:2635–2642. doi: 10.1021/cb400630z. [DOI] [PubMed] [Google Scholar]
- 103.Choi B.H., Philips M.R., Chen Y., Lu L., Dai W. K-Ras Lys-42 is crucial for its signaling, cell migration, and invasion. J. Biol. Chem. 2018;293:17574–17581. doi: 10.1074/jbc.RA118.003723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Zhou P., Chen X., Li M., Tan J., Zhang Y., Yuan W., Zhou J., Wang G. 2-D08 as a SUMOylation inhibitor induced ROS accumulation mediates apoptosis of acute myeloid leukemia cells possibly through the deSUMOylation of NOX2. Biochem. Biophys. Res. Commun. 2019;513:1063–1069. doi: 10.1016/j.bbrc.2019.04.079. [DOI] [PubMed] [Google Scholar]
- 105.Zhou L., Zheng L., Hu K., Wang X., Zhang R., Zou Y., Zhong L., Wang S., Wu Y., Kang T. SUMOylation stabilizes hSSB1 and enhances the recruitment of NBS1 to DNA damage sites. Signal Transduct. Target. Ther. 2020;5:80. doi: 10.1038/s41392-020-0172-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Baik H., Boulanger M., Hosseini M., Kowalczyk J., Zaghdoudi S., Salem T., Sarry J.E., Hicheri Y., Cartron G., Piechaczyk M., et al. Targeting the SUMO pathway primes all-trans retinoic acid-induced differentiation of non-promyelocytic acute myeloid leukemias. Cancer Res. 2018;78:2601–2613. doi: 10.1158/0008-5472.CAN-17-3361. [DOI] [PubMed] [Google Scholar]
- 107.Zlotkowski K., Hewitt W.M., Sinniah R.S., Tropea J.E., Needle D., Lountos G.T., Barchi J.J., Jr., Waugh D.S., Schneekloth J.S., Jr. A Small-Molecule Microarray Approach for the Identification of E2 Enzyme Inhibitors in Ubiquitin-Like Conjugation Pathways. SLAS Discov. Adv. Life Sci. 2017;22:760–766. doi: 10.1177/2472555216683937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Uno M., Koma Y., Ban H.S., Nakamura H. Discovery of 1-[4-(N-benzylamino)phenyl]-3-phenylurea derivatives as non-peptidic selective SUMO-sentrin specific protease (SENP)1 inhibitors. Bioorg. Med. Chem. Lett. 2012;22:5169–5173. doi: 10.1016/j.bmcl.2012.06.084. [DOI] [PubMed] [Google Scholar]
- 109.Wen D., Xu Z., Xia L., Liu X., Tu Y., Lei H., Wang W., Wang T., Song L., Ma C., et al. Important role of SUMOylation of Spliceosome factors in prostate cancer cells. J. Proteome Res. 2014;13:3571–3582. doi: 10.1021/pr4012848. [DOI] [PubMed] [Google Scholar]
- 110.Huang W., He T., Chai C., Yang Y., Zheng Y., Zhou P., Qiao X., Zhang B., Liu Z., Wang J., et al. Triptolide inhibits the proliferation of prostate cancer cells and down-regulates SUMO-specific protease 1 expression. PLoS ONE. 2012;7:e37693. doi: 10.1371/journal.pone.0037693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Wu J., Lei H., Zhang J., Chen X., Tang C., Wang W., Xu H., Xiao W., Gu W., Wu Y. Momordin Ic, a new natural SENP1 inhibitor, inhibits prostate cancer cell proliferation. Oncotarget. 2016;7:58995–59005. doi: 10.18632/oncotarget.10636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Kumar A., Ito A., Hirohama M., Yoshida M., Zhang K.Y. Identification of new SUMO activating enzyme 1 inhibitors using virtual screening and scaffold hopping. Bioorg. Med. Chem. Lett. 2016;26:1218–1223. doi: 10.1016/j.bmcl.2016.01.030. [DOI] [PubMed] [Google Scholar]
- 113.Albrow V.E., Ponder E.L., Fasci D., Békés M., Deu E., Salvesen G.S., Bogyo M. Development of small molecule inhibitors and probes of human SUMO deconjugating proteases. Chem. Biol. 2011;18:722–732. doi: 10.1016/j.chembiol.2011.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Hemelaar J., Borodovsky A., Kessler B.M., Reverter D., Cook J., Kolli N., Gan-Erdene T., Wilkinson K.D., Gill G., Lima C.D., et al. Specific and covalent targeting of conjugating and deconjugating enzymes of ubiquitin-like proteins. Mol. Cell. Biol. 2014;24:84–95. doi: 10.1128/MCB.24.1.84-95.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Bernstock J.D., Ye D., Smith J.A., Lee Y.J., Gessler F.A., Yasgar A., Kouznetsova J., Jadhav A., Wang Z., Pluchino S., et al. Quantitative high-throughput screening identifies cytoprotective molecules that enhance SUMO conjugation via the inhibition of SUMO-specific protease (SENP)2. FASEB J. 2018;32:1677–1691. doi: 10.1096/fj.201700711R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Yau T.Y., Molina O., Courey A.J. SUMOylation in development and neurodegeneration. Development. 2020;147:dev175703. doi: 10.1242/dev.175703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Yang W., Sheng H., Warner D.S., Paschen W. Transient global cerebral ischemia induces a massive increase in protein sumoylation. J. Cereb. Blood Flow Metab. 2008;28:269–279. doi: 10.1038/sj.jcbfm.9600523. [DOI] [PubMed] [Google Scholar]
- 118.Bernstock J.D., Ye D.G., Griffin A., Lee Y.-J., Lynch J., Latour L.L., Friedman G.K., Maric D., Hallenbeck J.M. Cerebral ischemia increases small ubiquitin-like modifier conjugation within human penumbral tissue: Radiological-pathological correlation. Front. Neurol. 2018;8:738. doi: 10.3389/fneur.2017.00738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Lee Y.J., Castri P., Bembry J., Maric D., Auh S., Hallenbeck J.M. SUMOylation participates in induction of ischemic tolerance. J. Neurochem. 2009;109:257–267. doi: 10.1111/j.1471-4159.2009.05957.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Ahn K., Song J.H., Kim D.K., Park M.H., Jo S.A., Koh Y.H. Ubc9 gene polymorphisms and late-onset Alzheimer’s disease in the Korean population: A genetic association study. Neurosci. Lett. 2009;465:272–275. doi: 10.1016/j.neulet.2009.09.017. [DOI] [PubMed] [Google Scholar]
- 121.Weeraratna A.T., Kalehua A., Deleon I., Bertak D., Maher G., Wade M.S., Lustig A., Becker K.G., Wood W., 3rd, Walker D.G., et al. Alterations in immunological and neurological gene expression patterns in Alzheimer’s disease tissues. Exp. Cell Res. 2007;313:450–461. doi: 10.1016/j.yexcr.2006.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Lee L., Dale E., Staniszewski A., Zhang H., Saeed F., Sakurai M., Fa M., Orozco I., Michelassi F., Akpan N., et al. Regulation of synaptic plasticity and cognition by SUMO in normal physiology and Alzheimer’s disease. Sci. Rep. 2014;4:7190. doi: 10.1038/srep07190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Zhang Y.Q., Sarge K.D. Sumoylation of amyloid precursor protein negatively regulates Abeta aggregate levels. Biochem. Biophys. Res. Commun. 2008;374:673–678. doi: 10.1016/j.bbrc.2008.07.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Luo H.B., Xia Y.Y., Shu X.J., Liu Z.C., Feng Y., Liu X.H., Yu G., Yin G., Xiong Y.S., Zeng K., et al. SUMOylation at K340 inhibits tau degradation through deregulating its phosphorylation and ubiquitination. Proc. Natl. Acad. Sci. USA. 2014;111:16586–16591. doi: 10.1073/pnas.1417548111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Steffan J.S., Agrawal N., Pallos J., Rockabrand E., Trotman L.C., Slepko N., Illes K., Lukacsovich T., Zhu Y.Z., Cattaneo E., et al. SUMO modification of Huntingtin and Huntington’s disease pathology. Science. 2004;304:100–104. doi: 10.1126/science.1092194. [DOI] [PubMed] [Google Scholar]
- 126.Krumova P., Meulmeester E., Garrido M., Tirard M., Hsiao H.H., Bossis G., Urlaub H., Zweckstetter M., Kügler S., Melchior F., et al. Sumoylation inhibits alpha-synuclein aggregation and toxicity. J. Cell Biol. 2011;194:49–60. doi: 10.1083/jcb.201010117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Baulac S., Lu H., Strahle J., Yang T., Goldberg M.S., Shen J., Schlossmacher M.G., Lemere C.A., Lu Q., Xia W. Increased DJ-1 expression under oxidative stress and in Alzheimer’s disease brains. Mol. Neurodegener. 2009;4:12. doi: 10.1186/1750-1326-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Ulrich H.D. Mutual interactions between the SUMO and ubiquitin systems: A plea of no contest. Trends Cell Biol. 2005;15:525–532. doi: 10.1016/j.tcb.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 129.Ramírez-Jarquín U.N., Sharma M., Zhou W., Shahani N., Subramaniam S. Deletion of SUMO1 attenuates behavioral and anatomical deficits by regulating autophagic activities in Huntington disease. Proc. Natl. Acad. Sci. USA. 2022;119:e2107187119. doi: 10.1073/pnas.2107187119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Marsh D.T., Das S., Ridell J., Smid S.D. Structure-activity relationships for flavone interactions with amyloid beta reveal a novel anti-aggregatory and neuroprotective effect of 2′,3′,4′-trihydroxyflavone (2-D08) Bioorg. Med. Chem. 2017;25:3827–3834. doi: 10.1016/j.bmc.2017.05.041. [DOI] [PubMed] [Google Scholar]
- 131.Krajnak K., Dahl R. Small molecule SUMOylation activators are novel neuroprotective agents. Bioorg. Med. Chem. Lett. 2018;28:405–409. doi: 10.1016/j.bmcl.2017.12.028. [DOI] [PubMed] [Google Scholar]
- 132.Yang W., Sheng H., Homi H.M., Warner D.S., Paschen W. Cerebral ischemia/stroke and small ubiquitin-like modifier (SUMO) conjugation—A new target for therapeutic intervention? J. Neurochem. 2008;106:989–999. doi: 10.1111/j.1471-4159.2008.05404.x. [DOI] [PubMed] [Google Scholar]
- 133.Bernstock J.D., Peruzzotti-Jametti L., Leonardi T., Vicario N., Ye D., Lee Y.J., Maric D., Johnson K.R., Mou Y., Van Den Bosch A., et al. SUMOylation promotes survival and integration of neural stem cell grafts in ischemic stroke. EBioMedicine. 2019;42:214–224. doi: 10.1016/j.ebiom.2019.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Wang J., Chen L., Wen S., Zhu H., Yu W., Moskowitz I.P., Shaw G.M., Finnell R.H., Schwartz R.J. Defective sumoylation pathway directs congenital heart disease. Birth Defects Res. Part A Clin. Mol. Teratol. 2011;91:468–476. doi: 10.1002/bdra.20816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Kim E.Y., Chen L., Ma Y., Yu W., Chang J., Moskowitz I.P., Wang J. Enhanced desumoylation in murine hearts by overexpressed SENP2 leads to congenital heart defects and cardiac dysfunction. J. Mol. Cell. Cardiol. 2012;52:638–649. doi: 10.1016/j.yjmcc.2011.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Kho C., Lee A., Jeong D., Oh J.G., Chaanine A.H., Kizana E., Park W.J., Hajjar R.J. SUMO1-dependent modulation of SERCA2a in heart failure. Nature. 2011;477:601–605. doi: 10.1038/nature10407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Kim E.Y., Zhang Y., Ye B., Segura A.M., Beketaev I., Xi Y.T., Yu W., Chang J., Li F.Q., Wang J. Involvement of activated SUMO-2 conjugation in cardiomyopathy. Biochim. Biophys. Acta BBA Mol. Basis Dis. 2015;1852:1388–1399. doi: 10.1016/j.bbadis.2015.03.013. [DOI] [PubMed] [Google Scholar]
- 138.Kim E.Y., Zhang Y., Beketaev I., Segura A.M., Yu W., Xi Y.T., Chang J., Wang J. SENP5, a SUMO isopeptidase, induces apoptosis and cardiomyopathy. J. Mol. Cell. Cardiol. 2015;78:154–164. doi: 10.1016/j.yjmcc.2014.08.003. [DOI] [PubMed] [Google Scholar]
- 139.Zhao W., Zhang X., Rong J. SUMOylation as a Therapeutic Target for Myocardial Infarction. Front. Cardiovasc. Med. 2021;8:701583. doi: 10.3389/fcvm.2021.701583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Du C., Chen X., Su Q., Lu W., Wang Q., Yuan H., Zhang Z., Wang X., Wu H., Qi Y. The Function of SUMOylation and Its Critical Roles in Cardiovascular Diseases and Potential Clinical Implications. Int. J. Mol. Sci. 2021;22:10618. doi: 10.3390/ijms221910618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Gupta M.K., Gulick J., Liu R., Wang X., Molkentin J.D., Robbins J. Sumo E2 enzyme UBC9 is required for efficient protein quality control in cardiomyocytes. Circ. Res. 2014;115:721–729. doi: 10.1161/CIRCRESAHA.115.304760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Xiao Q., Chen X.H., Jiang R.C., Chen S.Y., Chen K.F., Zhu X., Zhang X.L., Huang J.J., Qin Y., Zhang G.P., et al. Ubc9 Attenuates Myocardial Ischemic Injury Through Accelerating Autophagic Flux. Front. Pharmacol. 2020;11:561306. doi: 10.3389/fphar.2020.561306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Gu J., Fan Y., Liu X., Zhou L., Cheng J., Cai R., Xue S. SENP1 Protects against Myocardial Ischaemia/reperfusion Injury via a HIF1α-dependent Pathway. Cardiovasc. Res. 2014;104:83–92. doi: 10.1093/cvr/cvu177. [DOI] [PubMed] [Google Scholar]
- 144.Cai R., Gu J., Sun H., Liu X., Mei W., Qi Y., Xue S., Ren S., Rabinowitz J.E., Wang Y., et al. Induction of SENP1 in myocardium contributes to abnormities of mitochondria and cardiomyopathy. Mol. Cell. Cardiol. 2015;79:115–122. doi: 10.1016/j.yjmcc.2014.11.014. [DOI] [PubMed] [Google Scholar]
- 145.Del Monte F., Harding S.E., Schmidt U., Matsui T., Kang Z.B., Dec G.W., Gwathmey J.K., Rosenzweig A., Hajjar R.J. Restoration of contractile function in isolated cardiomyocytes from failing human hearts by gene transfer of SERCA2a. Circulation. 1999;100:2308–2311. doi: 10.1161/01.CIR.100.23.2308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Tilemann L., Lee A., Ishikawa K., Aguero J., Rapti K., Santos-Gallego C., Kohlbrenner E., Fish K.M., Kho C., Hajjar R.J. SUMO-1 gene transfer improves cardiac function in a large-animal model of heart failure. Sci. Transl. Med. 2013;5:211ra159. doi: 10.1126/scitranslmed.3006487. [DOI] [PubMed] [Google Scholar]
- 147.Kho C., Lee A., Jeong D., Oh J.G., Gorski P.A., Fish K., Sanchez R., DeVita R.J., Christensen G., Dahl R., et al. Small-molecule activation of SERCA2a SUMOylation for the treatment of heart failure. Nat. Commun. 2015;6:7229. doi: 10.1038/ncomms8229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Hu W., Xu T., Wu P., Pan D., Chen J., Chen J., Zhang B., Zhu H., Li D. Luteolin improves cardiac dysfunction in heart failure rats by regulating sarcoplasmic reticulum Ca2+-ATPase 2a. Sci. Rep. 2017;7:41017. doi: 10.1038/srep41017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Gupta M.K., McLendon P.M., Gulick J., James J., Khalili K., Robbins J. UBC9-mediated sumoylation favorably impacts cardiac function in compromised hearts. Circ. Res. 2016;118:1894–1905. doi: 10.1161/CIRCRESAHA.115.308268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Liebelt F., Vertegaal A.C. Ubiquitin-dependent and independent roles of SUMO in proteostasis. Am. J. Physiol. Cell Physiol. 2016;311:C284–C296. doi: 10.1152/ajpcell.00091.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]