Abstract
BACKGROUND:
Despite the rapid growth of assisted living (AL) and frequent hospitalizations among AL residents, little is known about their patterns of post-acute care transitions and outcomes. This study examined the post-acute care transitions among AL residents and their association with outcomes in the first 30 and 60 days after hospital discharge.
METHODS:
This study used data form 2018 national Medicare enrollment and claims datasets, the Minimum Data Set (MDS), and Medicare Provider Analysis and Review (MedPAR) of 104,497 unique Medicare beneficiaries residing in ALs in the U.S. Post-acute care referrals, based on hospital discharge status, to skilled nursing facilities (SNF), home with home health care (HHC), home without HHC, and other settings. Outcomes included 30-day and 60-day hospital readmissions, emergency department (ED) visits, long-stay care nursing home placement, and mortality. Multinomial logistic regression analysis and logistic regression analysis were conducted.
RESULTS:
The most common post-acute care referral was to SNF (40%), followed by home without HHC (28%), home with HHC (17%), and others (15%). Compared to discharge home without HHC, discharge to SNF was associated with lower likelihood of ED visits (Odds Ratio=0.597, p<0.01) and hospital readmissions (OR=0.856, p<0.001), and higher likelihood of long-stay nursing home placement (OR=11.224, p<0.01) and mortality (OR=2.025, p<0.01). Discharge home with HHC was associated with higher likelihood of hospital readmissions (OR=1.148, p<0.01) and lower likelihood of long-stay nursing home placement (OR=0.737, p<0.05) than discharge home without HHC. The results were similar within the first 30 days as well as 60 days after hospital discharge.
CONCLUSIONS:
AL residents who are discharged to different post-acute care settings tend to differ in 30-day and 60-day outcomes. At hospital discharge, clinicians and discharge planners should be provided information about the exact type and availability of services at AL to make the most appropriate discharge referrals for AL residents.
Keywords: assisted living, facility, post-acute care, home health care, skilled nursing facility, Medicare
BACKGROUND
Assisted living (AL) is an important residential care setting in the United States with an estimate of 811,500 older adults residing in 28,900 AL communities in 2016.1, 2 ALs provide housing, meals, some personal care and non-skilled health-related services to older adults who need supportive care.3 Over time, AL has evolved from a residential provider for relatively healthy older adults to a hybrid residential and care provider3 that has been admitting an increasing number of older adults with substantial care needs, such as Alzheimer’s disease and related dementias (ADRD) and functional limitations.4, 5 Many of the AL residents are 85 years and over (52%),6 have prevalent multimorbidity (74%), polypharmacy (51%), functional and cognitive impairments (limitations in activities of daily living [ADL] 64%, ADRD 42%), depressive symptoms (28%), pain (20%),6–10 and unstable health status.11
Hospitalizations and 30-day readmissions are common in the AL population.12–14 This is not only because hospitalization itself is a predictor of AL use,15 but also because of AL residents’ advanced age, comorbidities, and prevalent cognitive and functional impairments, which increase hospitalization risk.16, 17 Therefore, it is critical to better understand post-acute care trajectories in this population, and their association with health outcomes, and to identify both un-modifiable as well as modifiable factors.18
AL residents face unique situations and challenges in the post-acute care transitions. First, AL residents have greater risk for certain outcomes in the post-acute care period, such hospital readmissions,19, 20 indicating that AL residents may need more intensive post-acute care support than the general older population in the community. By virtue of staying in a structured residential setting, AL residents may have greater access to certain services (e.g., meal preparation, social interaction, and group guided exercise) than community-dwelling older adults. Yet, earlier research has suggested that ALs may not be equipped to provide sufficient support for the residents after hospital discharge,21 questioning the adequacy of post-acute care support ALs can provide to residents. Moreover, there is a possibility that ALs may be cautious and/or unable to assume responsibility for post-acute care and be incentivized to advocate other referrals for their residents rather than have them discharged back to the AL. It is unclear whether hospitals take these unique dynamics into account when making discharge referral decisions for AL residents.
Common post-acute care transitions among Medicare beneficiaries include skilled nursing facilities (SNF), home with home health care (HHC), and home without HHC.22 Previous studies have examined the use23 and outcomes24 of different post-acute care referrals among community-dwelling older adults. Indeed, much debate exists regarding whether and how transitions to post-acute care providers such as SNF and HHC may render better outcomes for patients.18, 24–26 In spite of the vulnerability and increased risk of hospitalization among AL residents, our knowledge is limited about these referrals among AL residents and their relationship to subsequent patient outcomes. No published study has used national data to examine the post-acute care transitions of Medicare beneficiaries residing in ALs and their subsequent outcomes.
Focusing on Medicare beneficiaries residing in ALs who had an acute hospitalization, this study had three objectives: 1) examine patterns of their post-acute care referrals; 2) identify factors associated with different post-acute care referrals, and 3) examine the association between post-acute care referrals and outcomes in the first 30 and 60 days after hospital discharge. We hypothesized that AL residents who were older and having a greater number of medical conditions were more likely to be referred to SNF and HHC after hospital discharge than going home without HHC, and that being discharged to SNF would be related to the highest risk for hospital readmissions, ED visits, long-stay nursing home placement and death in the first 30 and 60 days after hospital discharge, followed by HHC and then home without HHC.
METHODS
Data Sources
We used multiple sources of data from CY2018 including the Medicare Provider Analysis and Review (MedPAR), the Minimum Data Set (MDS), the Master Beneficiary Summary File (MBSF), Medicare outpatient claims, the Area Health Resource File (AHRF) of a national cohort of Medicare beneficiaries who resided in ALs (described below), a national inventory of AL communities, and the Provider of Services (POS) files of the discharging hospitals.
Study Sample
We used a previously validated methodology to identify Medicare beneficiaries in AL communities.27 Using the 9-digit zip codes associated with the physical address of each AL, we obtained Medicare beneficiary identification numbers from the Medicare enrollment database and identified beneficiaries who resided in AL.28 For this study, we separately identified CY2018 AL residents who were fee-for-service (FFS) Medicare beneficiaries and those enrolled in Medicare Advantage (MA) plans, because Medicare claims data are only available for the FFS beneficiaries. We limited our study cohort to residents age 55+ because younger individuals do not represent the typical AL population. AL residents were linked to the Medicare data at the individual level. We then identified AL residents who had an unplanned general acute care hospitalization in CY2018 and who were not in a nursing home within 30 days prior to the index hospital admission. We identified 72,421 Medicare FFS residents and 32,076 who were enrolled in MA, residing in 17,380 ALs. The final sample included 104,497 unique AL residents.
Key Variables
Post-Acute Care Referral
Post-acute care referral was assessed by the discharge status of the index hospital stay in MedPAR. Our focus was on the following care referrals: SNF (including inpatient rehabilitation facility), home without HHC (referred to as ‘home’ hereafter), and home with HHC (referred to as ‘HHC’ hereafter). Other referrals included inpatient care (e.g., other general acute care hospitals, federal hospitals, psychiatric hospitals, long-term care hospitals, hospital-based Medicare approved swing beds, and critical assess hospitals), non-skilled long-term care (e.g., intermediate care or Medicaid-certified nursing facilities), hospice (home- or facility-based), death, leaving against medical advice and discharge back to corrective facilities.
Outcomes
Outcomes included hospital readmission, emergency department (ED) visit, long-stay nursing home placement, and mortality. Each outcome was operationalized as two binary variables, i.e., 30-day occurrence and 60-day occurrence (yes/no), as described below.
Hospital readmission was identified from MedPAR and observed in the first 30 or 60 days after discharge from the index hospitalization.
ED visit was identified from Medicare outpatient claims with a focus on visits that did not result in hospitalization. Because Medicare outpatient claims were only available for the FFS beneficiaries, this outcome (ED visit) was only counted among FFS beneficiaries.
Long-stay nursing home placement was identified as admission to nursing homes that lasted for 100 days or longer, based on the MDS.
Mortality (death) was identified based on the MBSF-validated death date.
Covariates
We included covariates at the individual, AL, hospital, county, and state levels that may influence post-acute care referrals and outcomes.
Individual covariates included resident age, gender, race, dual eligibility, Medicare Advantage (MA) enrollment, information about the index hospitalization (i.e., length of stay and binary indicator [<3 days / ≥3 days] diagnosis-related groups (DRG) category [medical/surgical], and DRG weight), specific diagnoses of chronic conditions (e.g., ADRD, chronic kidney disease, chronic obstructive pulmonary disease, heart failure, diabetes, and arthritis [yes/no for each]), total number of chronic conditions.
AL covariates included AL bed-size, proportion of dually eligible residents, and average resident age obtained from the national inventory of AL communities and aggregated resident-level data specific to each AL.
Hospital covariates included ownership (non-profit, for-profit, other), teaching status (major, limited, graduate, no affiliation), number of beds, and location (rural/urban) of the discharging hospital obtained from the POS file.
County covariates included the numbers of hospital beds, nursing home beds, and HHC agencies per 1000 population age 65+ obtained from AHRF.
State covariates included state dummies.
Statistical Analysis
Descriptive statistics were used to summarize sample characteristics as means (standard deviations [S.D.]) or median (interquartile range) for continuous variables and frequency (%, [N]) for categorical variables. To identify factors associated with different post-acute care referrals, we conducted multinomial logistic regression analysis of post-acute care referrals as a function of the individual, AL, hospital, and county characteristics as well as state dummies as described above. To examine the associations between post-acute care referral and outcomes, we excluded individuals referred to the “other” post-acute care referral category. We then fit separate logistic regression models for each outcome (readmission, long-stay nursing home placement, ED visit [FFS beneficiaries only], and mortality; each observed in 30 days and 60 days; totaling eight models) as a function of post-acute care referral and the same individual-, AL-, hospital-, county-level controls, and state dummies. Standard errors were clustered at the level of discharging hospital. Statistical analyses were conducted using Stata 14 (Stata Corp, College Station, TX). This study has been approved by the Institutional Review Board of the University.
RESULTS
Upon discharge from an acute hospitalization, the most common post-acute care referral was SNF (40%), followed by home (28%), HHC (17%), and other referrals such as non-skilled long-term care and hospice care (15%) (Figure 1). The analytical sample included AL residents who were discharged to SNF, home, and HHC (N=89,342), excluding those with other referrals (e.g., non-skilled long-term care and hospice care). The sample had an average age of 83, were mostly female (65%), non-Hispanic white (89%) with some having dual Medicare-Medicaid eligibility (21%) and MA enrollment (31%). Overall, AL residents in the sample had multiple chronic conditions (sample mean=13), among which the most common were hypertension (65%), arthritis (56%), ischemic heart disease (49%), anxiety/depression (48%), chronic kidney disease (40%), heart failure (38%), diabetes (34%), chronic obstructive pulmonary disease (33%), and ADRD (31%). The index hospitalization was mostly for medical (79%) rather than surgical reasons. The length of stay of the index hospitalization was mostly three days or longer (75%) with an average of five days (Table 1).
Figure 1.
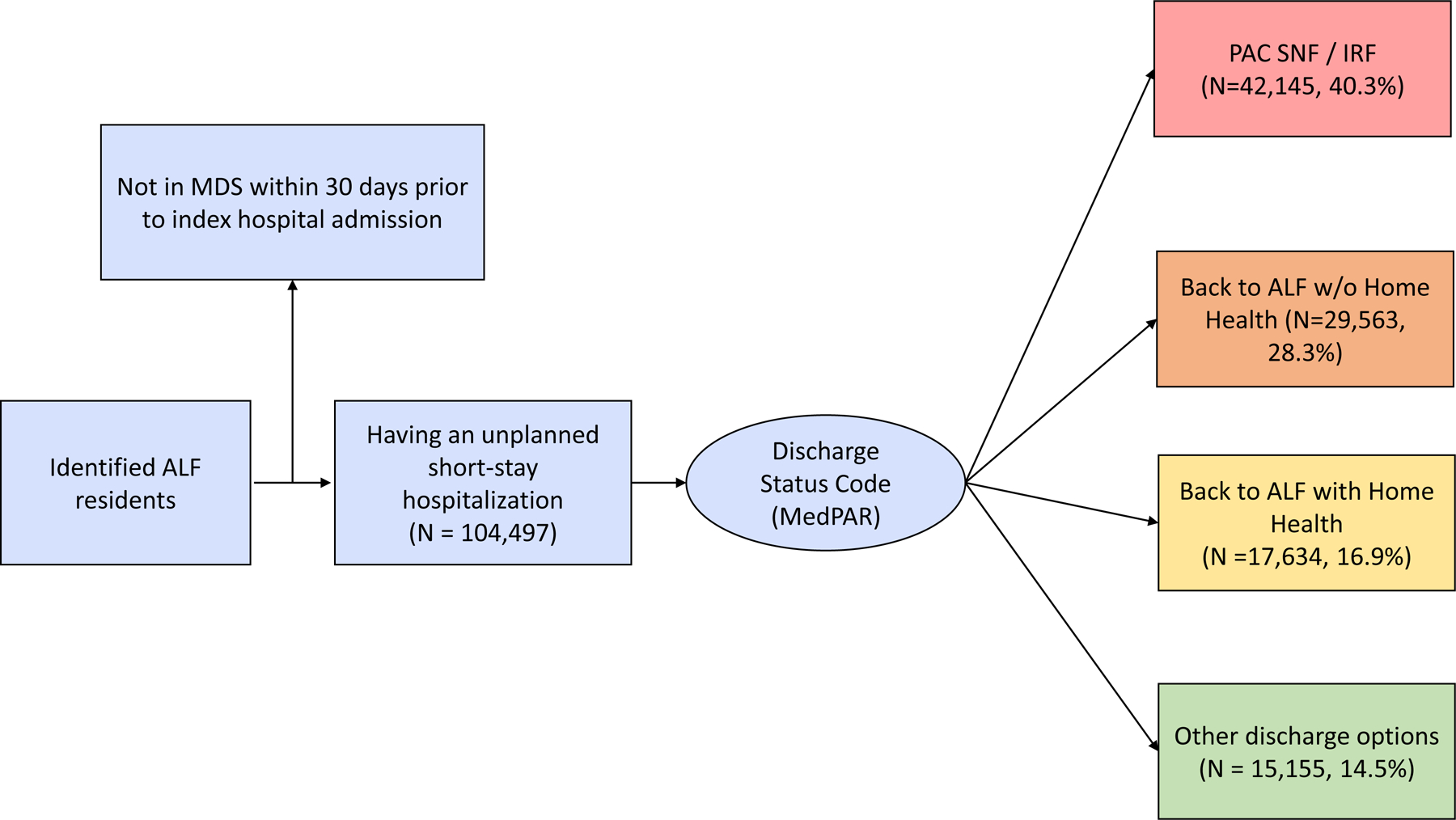
Discharge Transitions After An Acute Care Hospital Stay In Assisted Living
Table 1.
Sample Characteristics of Assisted Living Medicare Beneficiary Residents with A Discharge from Short-Stay Hospitalization
| Characteristics | Home (N=29563, 28.3%) |
HHC (N=17634, 16.9%) |
SNF (N=42145, 40.3%) |
Total (N=89,342) |
|---|---|---|---|---|
| Outcomes | ||||
| Having 30-day ED visit1 | 4.6% | 4.7% | 2.9% | 3.8% |
| Having 60-day ED visits1 | 7.2% | 7.3% | 5.2% | 6.3% |
| Having 30-day readmission | 15.0% | 17.3% | 14.3% | 15.1% |
| Having 60-day readmission | 22.0% | 24.7% | 22.1% | 22.6% |
| Having 30-day LTC admission | 0.7% | 0.5% | 8.1% | 4.1% |
| Having 60-day LTC admission | 1.0% | 0.7% | 9.2% | 4.8% |
| Having 30-day mortality | 2.3% | 3.0% | 6.0% | 4.2% |
| Having 60-day mortality | 4.1% | 5.7% | 10.1% | 7.2% |
| Age - Mean (SD) | 79.9 (12.7) | 83.7 (10.3) | 84.6 (9.8) | 82.8 (11.1) |
| Pct. <65 | 11.1% | 4.9% | 4.1% | 6.6% |
| 65–74 | 19.1% | 13.9% | 11.9% | 14.7% |
| 75–84 | 24.8% | 24.5% | 24.0% | 24.4% |
| 85–94 | 38.6% | 46.5% | 48.5% | 44.8% |
| 95 and over | 6.5% | 10.1% | 11.5% | 9.6% |
| Gender - Female | 60.4% | 65.4% | 67.4% | 64.7% |
| Race | ||||
| Non-Hispanic White | 85.7% | 90.4% | 91.0% | 89.1% |
| Non-Hispanic Black | 6.8% | 4.1% | 4.3% | 5.1% |
| Hispanic | 4.4% | 3.1% | 2.6% | 3.3% |
| Asian/Pacific Islander | 1.9% | 1.4% | 1.2% | 1.4% |
| Other | 1.2% | 1.0% | 0.9% | 1.0% |
| Dual eligibility | 23.3% | 16.9% | 21.8% | 21.3% |
| Index admission Length of Stay, Mean (SD) | 3.9 (5.2) | 4.4 (4.2) | 6.0 (5.4) | 5.0 (5.2) |
| Index Admission LOS >= 3 days | 55.1% | 68.3% | 92.6% | 75.4% |
| DRG weights, Mean (SD) | 1.3 (0.9) | 1.4 (0.9) | 1.6 (1.1) | 1.5 (1.0) |
| DRG type | ||||
| Medical | 84.9% | 84.1% | 73.1% | 79.2% |
| Surgical | 14.4% | 14.4% | 25.9% | 19.8% |
| Missing | 0.8% | 1.5% | 1.0% | 1.0% |
| Medicare Advantage enrollees | 31.3% | 32.5% | 29.8% | 30.8% |
| Number of Chronic Conditions (Medicare fee-for-service only)2 | ||||
| Mean (SD) | 13.0 (7.57) | 13.3 (7.32) | 13.7 (7.08) | 13.4 (7.30) |
| <=10 | 15.1% | 11.2% | 11.2% | 12.5% |
| 11–19 | 37.5% | 38.9% | 41.3% | 39.6% |
| >=20 | 16.2% | 17.5% | 17.7% | 17.1% |
| Alzheimer’s Disease and Related Dementias2 | 26.0% | 29.7% | 35.9% | 31.4% |
| Acute Myocardial Infarction2 | 6.5% | 7.5% | 6.9% | 6.9% |
| Atrial Fibrillation2 | 21.7% | 25.5% | 24.2% | 23.6% |
| Chronic Kidney Disease2 | 38.0% | 40.5% | 41.1% | 39.9% |
| Chronic Obstructive Pulmonary Disease2 | 31.9% | 33.2% | 32.6% | 32.5% |
| Heart Failure2 | 35.1% | 39.1% | 39.0% | 37.8% |
| Diabetes2 | 33.4% | 34.1% | 34.5% | 34.0% |
| Ischemic Heart Disease2 | 47.4% | 49.6% | 50.8% | 49.4% |
| Osteoporosis2 | 24.8% | 29.3% | 32.4% | 29.3% |
| Rheumatoid Arthritis/Osteoarthritis2 | 52.7% | 55.7% | 58.7% | 56.1% |
| Asthma2 | 17.4% | 17.3% | 16.0% | 16.7% |
| Hypertension2 | 62.8% | 63.7% | 66.7% | 64.8% |
| Sensory - Deafness and Hearing Impairment2 | 18.5% | 20.7% | 21.7% | 20.5% |
| Mobility Impairments2 | 7.3% | 9.0% | 9.5% | 8.6% |
| Multiple Sclerosis and Transverse Myelitis2 | 1.0% | 1.1% | 1.0% | 1.0% |
| Obesity2 | 21.4% | 20.2% | 19.8% | 20.4% |
| Sensory - Blindness and Visual Impairment2 | 2.8% | 3.5% | 3.4% | 3.2% |
| Cancer2,3 | 14.7% | 16.1% | 15.9% | 15.5% |
| Anxiety/Depression2 | 45.8% | 46.3% | 49.2% | 47.5% |
| Mental Illness4 | 17.6% | 14.2% | 17.0% | 16.7% |
| Hip/Pelvic Fracture in 20182 | 1.6% | 2.5% | 10.2% | 5.9% |
| Stroke/Transient Ischemic Attack in 20182 | 9.3% | 10.6% | 12.3% | 11.0% |
| Pressure Ulcers and Chronic Ulcers in 20182 | 10.3% | 15.3% | 18.5% | 15.1% |
| Drug Use Disorder2 | 8.7% | 6.7% | 6.5% | 7.3% |
Notes:
The information about ED visits was only available for Medicare Fee-For-Service beneficiaries;
The information about chronic conditions and specific diagnoses was only available for Medicare Fee-For-Service beneficiaries;
Cancer includes breast cancer, colorectal cancer, endometrial cancer, lung cancer, and prostate cancer;
Mental illness includes bipolar disorder, personality disorders, schizophrenia, schizophrenia and other psychotic disorders;
HHC = home health care; SNF = skilled nursing facility
Differences were noted among AL residents with different post-acute care referrals (Table 2). Compared with home, post-acute care referrals to SNF and HHC were more likely to occur for AL residents who are older (Relative Risk Ratio [RRR] of older age groups in SNF vs. home and HHC vs. home comparisons ranged from 1.116 to 2.645, all p<0.01), dual-eligible (SNF vs. home: RRR=1.186, p<0.01), MA enrollees (SNF vs. home: RRR=1.644; HHC vs. home: RRR=1.487; all p<0.01), having a longer hospital stay (≥ 3 days versus < 3 days; SNF vs. home: RRR=10.178, p<0.01; HHC vs. home: RRR=1.843, p<0.01), having surgical DRG (SNF vs. home: RRR=1.809, p<0.01), having certain diagnoses (e.g., ADRD; HHC vs. home: RRR=1.142; SNF vs. home: RRR=1.441; all p<0.01) and less likely for AL residents from under-represented racial/ethnic groups (e.g., non-Hispanic Black vs. non-Hispanic white in SNF vs. home [RRR=0.845, p<0.01] and HHC vs. home comparisons [RRR=0.908, all p<0.1]).
Table 2.
Factors Associated with Post-Acute Care Discharge Transitions
| Relative Risk Ratios1 (S.E.) | p-value2 | ||
|---|---|---|---|
| HHC vs. Home3 | SNF vs. Home4 | (SNF vs. HHC) | |
| Reference group | Home | HHC | |
| Individual-level variables | |||
| Age (ref: 65–75) | |||
| <65 | 0.750*** (0.038) | 0.634*** (0.028) | 0.003 |
| 75–84 | 1.116*** (0.040) | 1.415*** (0.045) | 0.000 |
| 85–94 | 1.283*** (0.046) | 1.897*** (0.063) | 0.000 |
| >=95 | 1.581*** (0.076) | 2.645*** (0.118) | 0.000 |
| Gender (ref: Male) | |||
| Female | 1.126*** (0.026) | 1.145*** (0.023) | 0.448 |
| Race (ref: Non-Hispanic White) | |||
| Non-Hispanic Black | 0.908* (0.048) | 0.845*** (0.038) | 0.192 |
| Hispanic | 0.779*** (0.068) | 0.603*** (0.055) | 0.001 |
| Asian/Pacific Islander | 0.921 (0.091) | 0.767*** (0.061) | 0.088 |
| Other | 1.047 (0.098) | 0.994 (0.087) | 0.599 |
| Dual eligibility (ref: Non-dual) | 1.042 (0.039) | 1.186*** (0.040) | 0.000 |
| MA enrollees (ref: FFS enrollees) | 1.487*** (0.086) | 1.644*** (0.083) | 0.098 |
| Index Admission LOS >= 3 days (ref: <3 days) | 1.843*** (0.043) | 10.178*** (0.303) | 0.000 |
| DRG type (ref: Medical) | |||
| Surgical | 0.976 (0.040) | 1.809*** (0.061) | 0.000 |
| DRG weights | 1.115*** (0.020) | 1.148*** (0.018) | 0.027 |
| Number of Chronic Conditions (ref: <=10) | |||
| 11–19 | 1.020 (0.046) | 1.053 (0.041) | 0.475 |
| >=20 | 1.060 (0.069) | 1.024 (0.059) | 0.588 |
| Presence of Chronic Conditions (Medicare fee-for-service only) | |||
| Alzheimer’s Disease and Related Dementias | 1.142*** (0.031) | 1.441*** (0.034) | 0.000 |
| Acute Myocardial Infarction | 1.050 (0.042) | 0.942 (0.034) | 0.006 |
| Atrial Fibrillation | 1.022 (0.028) | 0.917*** (0.023) | 0.000 |
| Chronic Kidney Disease | 1.033 (0.029) | 1.004 (0.023) | 0.288 |
| Chronic Obstructive Pulmonary Disease | 1.031 (0.029) | 0.935*** (0.023) | 0.000 |
| Heart Failure | 1.067** (0.031) | 0.986 (0.024) | 0.004 |
| Diabetes | 1.073*** (0.029) | 1.005 (0.024) | 0.010 |
| Ischemic Heart Disease | 0.921** (0.030) | 0.896*** (0.024) | 0.367 |
| Osteoporosis | 1.025 (0.028) | 1.071*** (0.026) | 0.098 |
| Rheumatoid Arthritis/Osteoarthritis | 1.021 (0.036) | 1.067** (0.032) | 0.198 |
| Asthma | 0.983 (0.030) | 0.902*** (0.024) | 0.004 |
| Hypertension | 1.011 (0.056) | 1.076 (0.052) | 0.280 |
| Sensory - Deafness and Hearing Impairment | 0.970 (0.028) | 0.965 (0.023) | 0.827 |
| Mobility Impairments | 1.246*** (0.047) | 1.282*** (0.045) | 0.438 |
| Multiple Sclerosis and Transverse Myelitis | 1.163 (0.113) | 1.096 (0.095) | 0.527 |
| Obesity | 0.974 (0.029) | 1.019 (0.025) | 0.102 |
| Sensory - Blindness and Visual Impairment | 1.142** (0.070) | 1.074 (0.061) | 0.249 |
| Cancer | 0.993 (0.029) | 0.937** (0.024) | 0.043 |
| Anxiety/Depression | 1.060** (0.032) | 1.069** (0.029) | 0.781 |
| Mental Illness | 0.915*** (0.032) | 1.069** (0.032) | 0.000 |
| Hip/Pelvic Fracture in 2018 | 1.314*** (0.095) | 4.154*** (0.229) | 0.000 |
| Stroke / Transient Ischemic Attack in 2018 | 1.161*** (0.041) | 1.504*** (0.044) | 0.000 |
| Pressure Ulcers and Chronic Ulcers in 2018 | 1.500*** (0.047) | 1.767*** (0.049) | 0.000 |
| Drug Use Disorder | 0.964 (0.042) | 0.917** (0.035) | 0.252 |
| AL-level variables | |||
| AL beds | 1.000 (0.000) | 1.001*** (0.000) | 0.000 |
| Proportion of duals in AL | 1.008 (0.070) | 2.669*** (0.165) | 0.000 |
| Average age in AL | 1.029*** (0.003) | 1.050*** (0.002) | 0.000 |
| Hospital-level variables | |||
| Hospital Ownership (ref: for-profit) | |||
| Nonprofit/Public | 1.044 (0.050) | 0.876*** (0.040) | 0.000 |
| Other | 1.140** (0.076) | 0.890** (0.053) | 0.000 |
| Teaching Status (ref: Major) | |||
| Limited | 1.119** (0.064) | 1.043 (0.049) | 0.194 |
| Graduate | 0.999 (0.089) | 1.026 (0.072) | 0.709 |
| No Affiliation | 1.038 (0.055) | 0.977 (0.044) | 0.211 |
| Hospital Beds | 1.000 (0.000) | 1.000 (0.000) | 0.393 |
| Location (ref: Urban) | |||
| Rural | 0.982 (0.072) | 0.858** (0.054) | 0.035 |
| County-level variables | |||
| Hospital beds per 1000 people 65+ | 0.996*** (0.001) | 0.995*** (0.001) | 0.753 |
| Nursing home beds per 1000 people 65+ | 0.997 (0.002) | 1.007*** (0.002) | 0.000 |
| Home health agencies per 1000 people 65+ | 0.911 (0.078) | 0.940 (0.068) | 0.674 |
| State dummies | Not shown | Not shown | Not shown |
| Observations | 87,856 | 87,856 | 87,856 |
| Clustered SE | Yes | Yes | |
Note:
Relative risk ratios estimated in multinomial logistic regression models between post-acute care referral (reference group = home without HHC) and outcomes;
p-values generated in another set of multinomial logistic regression models between post-acute care referral (reference group = home with HHC) and outcomes;
HHC=Home health care;
SNF= skilled nursing facilities; standard errors are clustered at the level of the discharging hospital (in parentheses);
p<0.01,
p<0.05,
p<0.1;
HHC = home health care; SNF = skilled nursing facility
AL-level characteristics such as older average age was associated with higher relative risk of post-acute care referrals to SNF and HHC. Greater AL concentration of dually-eligible residents was associated with higher relative risk of post-acute care referrals to SNF than home (RRR=2.669, p<0.01). Characteristics of the discharging hospital such as rural location (RRR=0.858, p<0.01) and non-profit or public ownership (RRR=0.876, p<0.01) were associated with lower likelihood of post-acute care referrals to SNF as compared to home. Local supply of health care services such as the concentration of hospital beds (SNF vs. home: RRR=0.995, p<0.01; HHC vs. home: RRR=0.996, p<0.01) and nursing home beds (SNF vs. home: RRR=1.007, p<0.01) were related to post-acute care referrals in AL. Differences existed between referrals to HHC and SNF (p-values in Table 2), where older AL residents and dual eligible beneficiaries were more likely to be referred to SNF than HHC.
Adjusted logistic regression analyses (Supplementary Table S1 and Figure 2) between post-acute care referrals and outcomes showed that compared to discharge home, discharge to SNF was associated with lower likelihood of 30-day ED visit (OR=0.597, p<0.01), lower likelihood of 30-day hospital readmission (OR=0.856, p<0.01), higher likelihood of 30-day long-stay nursing home placement (OR=11.224, p<0.01), and higher likelihood of 30-day mortality (OR=2.025, p<0.01). Discharge to HHC was associated with higher likelihood of 30-day hospital readmission (OR=1.148, p<0.01) and lower likelihood of 30-day long-stay nursing home placement (OR=0.737, p<0.05), and no difference in ED visits and 30-day mortality relative to discharge home.
Figure 2.
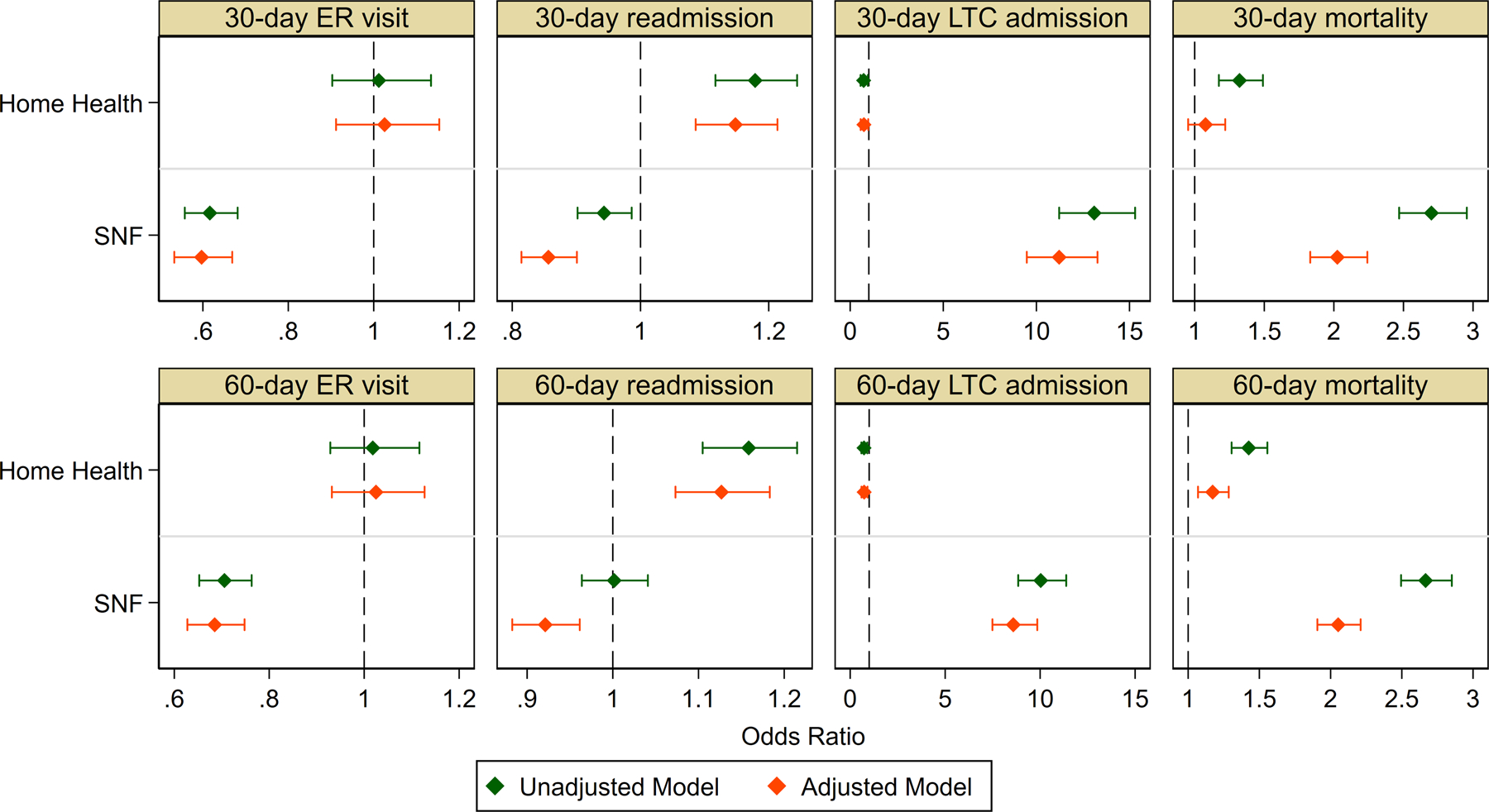
Effect Sizes of the Relationships Between Post-Acute Care Transitions and 30-Day and 60-Day Outcomes
Results for 60-day outcomes were consistent with those for 30-day outcomes. Figure 2 illustrates the effect sizes of the association between post-acute care transitions and outcomes. The full models of these analyses are detailed in Supplementary Tables (S1–S2).
DISCUSSION
This study is the first to examine post-acute care referrals among AL residents in the U.S. using national datasets and the associations between post-acute care referrals and outcomes in the 30 and 60 days after hospital discharge, with three principal findings. First, similar to the overall Medicare population,29 SNF is the most common post-acute care referral in the AL population, followed by home and HHC. Second, referrals to different post-acute care settings were associated with multiple characteristics of the individual, the AL, the discharging hospital, and the region, highlighting the complexity of post-acute care transitions. Third, adjusting for multilevel covariates, post-acute care referrals were associated with differences in outcomes, emphasizing the importance of providing appropriate post-acute care services to AL residents. AL residents discharged to HHC had the highest probability of having hospital readmissions and ED visits, followed by AL residents discharged home, and then by those discharged to SNF.
Findings should be interpreted with consideration of the complexity in hospital discharge decision making, which often involves multiple stakeholders including the patient, his/her caregivers, the hospitalists, discharge planners, post-acute care providers, and the AL.30 The post-acute care referrals are decided based on not only the patient’s needs and preferences, but also the post-acute care that is available at hospital discharge.31, 32 Findings about individual variables associated with post-acute care referrals indicate a general trend that AL residents who are older, having more chronic conditions (e.g., ADRD), and more complex admission diagnoses leading to the index hospitalization, and a longer hospital stay tend to be discharged to more intense post-acute care options (i.e., SNF), which are consistent with studies with community-dwelling older adults.24, 26 There was a consistent decrease in the likelihood of referrals to receive additional post-acute care (HHC and SNF versus home) among under-represented racial/ethnic groups. We also noted increased likelihood of SNF referrals among dually eligible beneficiaries and increased likelihood of HHC referrals among MA enrollees. Together, these findings suggest systematic differences in post-acute care33–36 that may be related to the patient’s ability to finance additional personal care and his/her healthcare plans. Dual-eligible beneficiaries may be unable to afford additional privately paid support that is needed at AL after hospital discharge, and thus have to be referred to SNF. The different reimbursement rates for post-acute care service across healthcare plans (e.g., MA vs. FFS) may also play a role in one’s post-acute care destinations37 and services38 received. Adding to such complexity is that even though AL and nursing home are substantially different in their services3 and target populations (e.g., diagnoses, prognosis, and care needs39), clinicians and discharge planners in the hospital are often unfamiliar with these differences, urging deeper understanding of the residential care landscape among hospital-based professionals to optimize post-acute care referrals and outcomes for AL residents.
Findings about acute care admissions (including hospital readmission and ED visits) among AL residents in this study are consistent with prior studies with community-dwelling older adults, where discharge to SNF is associated with lower risk of readmission and discharge to HHC is associated with higher risk of hospital readmissions and ED visits.24 There are, however, also studies that reported discharge to home (including HHC and home without HHC) to be related to lower risk of hospital readmissions,40 which may be due to the differences in the patient population and categorization of post-acute care referrals. Several potential reasons may exist for why discharge to SNF is associated with lower rates of acute care admissions in AL than discharge home (with or without HHC). The 24/7 monitoring and emergency services available at SNF represent a more intensive level of care than what is typically available in ALs.41 Therefore, at the onset of symptom changes, the on-call clinicians in SNFs may be able to provide emergent care for patients and prevent some of the acute care admissions. Furthermore, because SNFs themselves represent an inpatient level of care, conditions that might require a hospitalization if acquired at home (e.g., a urinary tract infection) may be successfully treated in the SNFs without the need for hospitalization. SNFs also provide more intensive rehabilitation services than ALs, and thus may be able to facilitate greater functional improvement to reduce the risk of acute care admissions, particularly those caused by falls.
This study is descriptive, because we were unable to determine the extent to which differences in patient outcomes across discharge destinations are due to differences in the quality and adequacy of care or patient case-mix. Although we controlled for numerous measures of health status, there are likely a number of unobservable characteristics that may vary across discharge referrals and could influence the risk of outcomes. Therefore, though prior evidence has suggested unmet needs of AL residents after hospital discharge (e.g., medication administration and symptom monitoring19), this study is unable to ascertain the specific reasons of differences in acute care readmissions across the different post-acute care settings.
We noted large effect sizes (OR>10) in the association between post-acute care referral to SNF and long-stay nursing home placement in the first 30 and 60 days after hospital discharge, and that HHC referral being related to the lowest likelihood of long-stay nursing home placement. The lower risk of long-stay nursing home placement related to HHC referral may be that for relatively healthier older adults with fewer ADL limitations, HHC delays long-stay nursing home placement.42 Yet for AL residents with more intensive care needs, HHC – being an intermittent skilled care provider – may be insufficient to meet their needs. Rather, for AL residents who acquired new care needs that the AL cannot provide, long-stay nursing home placement may be more reasonable than staying in AL. Indeed, hospitalizations among vulnerable older adults such as AL residents often trigger the transition to long-stay nursing homes. Also contributing to this finding is the fact that SNFs are often located within the same facilities that also provide long-term care, making it easier for SNF patients to transition to long-stay nursing homes than patients in other post-acute care settings.
Regarding mortality, we want to emphasize that the higher mortality risk noted among AL residents referred to SNF likely reflects unobserved differences in the case mix of AL residents referred to SNF as opposed to other settings. This includes unmeasured factors, such as frailty, which isn’t available in the current datasets but is a predominant predictor of mortality among community-dwelling older adults.43
Findings have important clinical and policy implications for AL and post-acute care. Part of the challenge in providing the right type and amount of post-acute care for AL residents lies in the complexity and variation of services provided within AL. AL communities with more licensed staff have lower rates of hospitalization and long-stay nursing home placement.44, 45 Yet most AL communities in the U.S. do not provide medical or skilled nursing services.46 Further, the majority (83.3%) of AL staff are unlicensed personnel (e.g., personal care aides) and only 16% are licensed personnel (e.g., registered nurses [6.1% and licensed practical nurses [9.9%]).2 The need for more skilled post-acute care among AL residents after hospital discharge may not be met on site19 and necessitates additional support. Moreover, because AL communities are regulated at the state level, much variation exists in the availability and type of services provided in the AL.46 Due to the unfamiliarity with AL settings, complexity and variation in AL services,5, 47 clinicians who discharge AL residents from the hospital are often unaware of the specific type and amount of support patients will have once they return to AL and thus find it challenging to make informed decisions. Information regarding the level of support available in the AL is critical yet often unavailable to hospitalists and discharge planners when they are trying to decide on the most suitable post-acute care referral for AL residents. In light of recent reforms that may affect post-acute care providers’ ability and willingness to offer certain care to patients,25 more work is needed to ensure that those who are the most vulnerable (e.g., racial/ethnic minorities and persons with ADRD) have access to the right type of post-acute care.
This study has several limitations. First, we measured post-acute care referrals, not the actual use of post-acute care that may be different from the referral. Second, though we controlled for a comprehensive set of individual-, hospital-, AL- and regional variables, there may be residual confounding, e.g., in variation in disease severity, functionality, caregivers and AL policies.
CONCLUSION
Post-acute care referrals for AL residents in the U.S. are related to multi-level variables that speak to both the needs of the patient and the availability of care. AL residents with different post-acute care referrals tend to differ in 30-day and 60-day outcomes. At hospital discharge, clinicians and discharge planners should be provided information about the exact type and availability of services at AL to make the most appropriate discharge referrals for AL residents.
Supplementary Material
Supplementary Table S1. Relationship between Post-Acute Care Discharge Transitions and 30-day Outcomes
Supplementary Table S2. Relationship between Post-Acute Care Discharge Transitions and 60-day Outcomes
Key Points:
In assisted living (AL) communities in the U.S., skilled nursing facility is the most common post-acute care referral, followed by home without home health care (HHC) and home with HHC.
Post-acute care referrals made for AL residents in the U.S. are related to multi-level variables that speak to both the needs of the patient and the availability of care.
AL residents who are discharged to different post-acute care referrals tend to differ in 30-day and 60-day outcomes.
Why does this matter?
Because the AL is the fastest growing residential care provider in the United States, it is important for clinicians and discharge planners to be provided information about the exact type and availability of services at AL to make the most appropriate discharge referrals for AL residents.
Funding Statement:
This study was conducted with the support of the following funders: Agency for Healthcare Research and Quality (AHRQ) (1R01HS026893 [HTG]). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Sponsor’s Role
This study was conducted with the support of the following funders: Agency for Healthcare Research and Quality (AHRQ) (1R01HS026893-01 [HTG]). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Conflict of Interest
The authors declare no conflicts of interest, financial, personal, or other related to this manuscript.
References
- [1].Grabowski DC, Stevenson DG, Cornell PY. Assisted living expansion and the market for nursing home care. Health Serv Res. 2012;47: 2296–2315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Harris-Kojetin LSM, Lendon JP, Rome V, Valverde R, Caffrey C. Long-term Care Providers and Services Users in the United States, 2015–2016. In: Statistics NCfH, ed. National Center for Health Statistics, 2019. [PubMed] [Google Scholar]
- [3].Zimmerman S, Gruber-Baldini AL, Sloane PD, et al. Assisted living and nursing homes: Apples and oranges? The Gerontologist. 2003;43: 107–117. [DOI] [PubMed] [Google Scholar]
- [4].Thomas KS, Zhang W, Cornell PY, Smith L, Kaskie B, Carder PC. State Variability in the Prevalence and Healthcare Utilization of Assisted Living Residents with Dementia. J Am Geriatr Soc. 2020;68: 1504–1511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Han K, Trinkoff AM, Storr CL, Lerner N, Yang BK. Variation Across U.S. Assisted Living Facilities: Admissions, Resident Care Needs, and Staffing. J Nurs Scholarsh. 2017;49: 24–32. [DOI] [PubMed] [Google Scholar]
- [6].Caffrey C, Sengupta M. Variation in Residential Care Community Resident Characteristics, by Size of Community: United States, 2016. NCHS Data Brief. 2018: 1–8. [PubMed] [Google Scholar]
- [7].Wang J, Kearney JA, Jia H, Shang J. Mental health disorders in elderly people receiving home care: Prevalence and correlates in the national U.S. population. Nurs Res. 2016;65: 107–116. [DOI] [PubMed] [Google Scholar]
- [8].Caffrey C, Sengupta M, Park-Lee E, Moss A, Rosenoff E, Harris-Kojetin L. Residents living in residential care facilities: United States, 2010. NCHS data brief. 2012: 1. [PubMed] [Google Scholar]
- [9].Resnick B, Boltz M, Galik E, et al. Pain Assessment, Management, and Impact Among Older Adults in Assisted Living. Pain Manag Nurs. 2019;20: 192–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Resnick B, Galik E, Boltz M, et al. Polypharmacy in Assisted Living and Impact on Clinical Outcomes. Consult Pharm. 2018;33: 321–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Kistler CE, Zimmerman S, Ward KT, Reed D, Golin C, Lewis CL. Health of Older Adults in Assisted Living and Implications for Preventive Care. Gerontologist. 2017;57: 949–954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Zimmerman S, Sloane PD, Eckert JK, et al. How good is assisted living? Findings and implications from an outcomes study. J Gerontol B Psychol Sci Soc Sci. 2005;60: S195–204. [DOI] [PubMed] [Google Scholar]
- [13].Zimmerman S, Guo W, Mao Y, Li Y, Temkin-Greener H. Health Care Needs in Assisted Living: Survey Data May Underestimate Chronic Conditions. J Am Med Dir Assoc 2021;22: 471–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Temkin-Greener H, Mao Y, McGarry B, Zimmerman S, Li Y Healthcare Use and Outcomes in Assisted Living Communities: Race, Ethnicity, and Dual Eligibility [In Press]. Med Care Res Rev. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Chyr LC, Drabo EF, Fabius CD. Patterns and Predictors of Transitions Across Residential Care Settings and Nursing Homes Among Community-Dwelling Older Adults in the United States. Gerontologist. 2020;60: 1495–1503. [DOI] [PubMed] [Google Scholar]
- [16].Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. New England Journal of Medicine. 2009;360: 1418–1428. [DOI] [PubMed] [Google Scholar]
- [17].O’Connor M Hospitalization among Medicare-reimbursed skilled home health recipients. Home Health Care Management & Practice. 2012;24: 27–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Huckfeldt PJ, Mehrotra A, Hussey PS. The Relative Importance of Post-Acute Care and Readmissions for Post-Discharge Spending. Health Serv Res. 2016;51: 1919–1938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Wang J, Ying M, Temkin-Greener H, et al. Care-partner support and hospitalization in assisted living during transitional home health care [In Press]. J Am Geriatr Soc. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Bartley MM, Quigg SM, Chandra A, Takahashi PY. Health Outcomes From Assisted Living Facilities: A Cohort Study of a Primary Care Practice. J Am Med Dir Assoc. 2018;19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Wang J, Ying M, Temkin-Greener H, et al. Care-Partner Support and Hospitalization in Assisted Living During Transitional Home Health Care. J Am Geriatr Soc. 2021;69: 1231–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Medicare Payment Advisory Commission. Report to the Congress: Medicare payment policy (March 2021). Washington, DC, 2021. [Google Scholar]
- [23].Werner RM, Konetzka RT. Trends in Post–Acute Care Use Among Medicare Beneficiaries: 2000 to 2015. JAMA. 2018;319: 1616–1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Werner RM, Coe NB, Qi M, Konetzka RT. Patient Outcomes After Hospital Discharge to Home With Home Health Care vs to a Skilled Nursing Facility. JAMA Intern Med. 2019;179: 617–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Burke RE, Cumbler E, Coleman EA, Levy C. Post-acute care reform: Implications and opportunities for hospitalists. J Hosp Med. 2017;12: 46–51. [DOI] [PubMed] [Google Scholar]
- [26].Wang J, Dietrich MS, Bell SP, Maxwell CA, Simmons SF, Kripalani S. Changes in vulnerability among older patients with cardiovascular disease in the first 90 days after hospital discharge: A secondary analysis of a cohort study. BMJ Open. 2019;9: e024766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Temkin-Greener H, Mao Y, McGarry B, Zimmerman S, Li Y. Health Care Use and Outcomes in Assisted Living Communities: Race, Ethnicity, and Dual Eligibility. Med Care Res Rev. 2021: 10775587211050189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Temkin-Greener HMY, McGarry B, Li Y. Using Medicare Enrollment to Identify Medicare Beneficiaries Residing in Assisted Living. [In Review]. 2021. [DOI] [PMC free article] [PubMed]
- [29].Medicare Payment Advisory Commission. A data book: Health Care Spending and the Medicare Program. Washington, DC, 2019, pp. 110–112. [Google Scholar]
- [30].Morrow-Howell N, Proctor E. Discharge destinations of Medicare patients receiving discharge planning: who goes where? Med Care. 1994;32: 486–497. [DOI] [PubMed] [Google Scholar]
- [31].Bowles KH, Holmes JH, Ratcliffe SJ, Liberatore M, Nydick R, Naylor MD. Factors identified by experts to support decision making for post acute referral. Nurs Res. 2009;58: 115–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Bowles KH, Foust JB, Naylor MD. Hospital discharge referral decision making: a multidisciplinary perspective. Appl Nurs Res. 2003;16: 134–143. [DOI] [PubMed] [Google Scholar]
- [33].Holmes GM, Freburger JK, Ku LJ. Decomposing racial and ethnic disparities in the use of postacute rehabilitation care. Health Serv Res. 2012;47: 1158–1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Freburger JK, Holmes GM, Ku LJ, Cutchin MP, Heatwole-Shank K, Edwards LJ. Disparities in postacute rehabilitation care for stroke: an analysis of the state inpatient databases. Arch Phys Med Rehabil. 2011;92: 1220–1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Li Y, Glance LG, Yin J, Mukamel DB. Racial disparities in rehospitalization among medicare patients in skilled nursing facilities. Am J Public Health. 2011;101: 875–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Temkin-Greener H, Campbell L, Cai X, Hasselberg MJ, Li Y. Are Post-Acute Patients with Behavioral Health Disorders Admitted to Lower-Quality Nursing Homes? The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2018;26: 643–654. [DOI] [PubMed] [Google Scholar]
- [37].Schwartz ML, Kosar CM, Mroz TM, Kumar A, Rahman M. Quality of Home Health Agencies Serving Traditional Medicare vs Medicare Advantage Beneficiaries. JAMA Network Open. 2019;2: e1910622–e1910622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Skopec L, Huckfeldt PJ, Wissoker D, et al. Home Health And Postacute Care Use In Medicare Advantage And Traditional Medicare. Health Aff (Millwood). 2020;39: 837–842. [DOI] [PubMed] [Google Scholar]
- [39].Unroe KT, Bernard B, Stump TE, Tu W, Callahan CM. Variation in Hospice Services by Location of Care: Nursing Home Versus Assisted Living Facility Versus Home. J Am Geriatr Soc. 2017;65: 1490–1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Keswani A, Tasi MC, Fields A, Lovy AJ, Moucha CS, Bozic KJ. Discharge Destination After Total Joint Arthroplasty: An Analysis of Postdischarge Outcomes, Placement Risk Factors, and Recent Trends. J Arthroplasty. 2016;31: 1155–1162. [DOI] [PubMed] [Google Scholar]
- [41].Kisling-Rundgren A, Paul DP 3rd, Coustasse A. Costs, Staffing, and Services of Assisted Living in the United States: A Literature Review. Health Care Manag (Frederick). 2016;35: 156–163. [DOI] [PubMed] [Google Scholar]
- [42].Young Y, Kalamaras J, Kelly L, Hornick D, Yucel R. Is Aging in Place Delaying Nursing Home Admission? J Am Med Dir Assoc. 2015;16: 900.e901–900.e906. [DOI] [PubMed] [Google Scholar]
- [43].Morley JE, Vellas B, van Kan GA, et al. Frailty consensus: A call to action. Journal of the American Medical Directors Association. 2013;14: 392–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Stearns SC, Park J, Zimmerman S, Gruber-Baldini AL, Konrad TR, Sloane PD. Determinants and effects of nurse staffing intensity and skill mix in residential care/assisted living settings. Gerontologist. 2007;47: 662–671. [DOI] [PubMed] [Google Scholar]
- [45].Maxwell CJ, Soo A, Hogan DB, et al. Predictors of Nursing Home Placement from Assisted Living Settings in Canada. Canadian journal on aging = La revue canadienne du vieillissement. 2013;32: 333–348. [DOI] [PubMed] [Google Scholar]
- [46].Dys S, Smith L, Tunalilar O, Carder P. Revisiting the Role of Physicians in Assisted Living and Residential Care Settings. Gerontol Geriatr Med. 2020;6: 2333721420979840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Rome V, Harris-Kojetin L, Carder P. Variation in Licensed Nurse Staffing Characteristics by State Requirements in Residential Care. Res Gerontol Nurs. 2019;12: 27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1. Relationship between Post-Acute Care Discharge Transitions and 30-day Outcomes
Supplementary Table S2. Relationship between Post-Acute Care Discharge Transitions and 60-day Outcomes


