Abstract
Background:
Potentially disruptive medical, surgical, and social events–such as pneumonia, hip fracture, and widowhood–may accelerate the trajectory of decline and impact caregiving needs in older adults, especially among people with dementia. Prior research has focused primarily on nursing home residents with dementia. We sought to assess the incidence of potentially disruptive events in community-dwelling people with and without dementia.
Methods:
Retrospective cohort study of participants aged 65+ enrolled in the Health and Retirement Study between 2010–2018 (n=9,346), including a subset who were married/partnered at baseline (n=5,105). Dementia was defined with a previously validated algorithm. We calculated age-adjusted and gender-stratified incidence per 1000 person-years and incidence rate ratios of: 1) hospitalization for pneumonia; 2) hip fracture and; 3) widowhood in people with and without dementia.
Results:
People with dementia (PWD) (n=596) were older (mean age 84 vs. 75) and a higher proportion were female (67% vs 57%) than people without dementia (PWoD) (n=8,750). Age-adjusted incidence rates (per 1000 person-years) of pneumonia were higher in PWD (113.1; 95% CI 94.3, 131.9) compared to PWoD (62.1; 95% CI 54.7, 69.5), as were hip fractures (12.3; 95% CI 9.1, 15.6 for PWD compared to 8.1; 95% CI 6.9, 9.2 in PWoD). Point estimates of widowhood incidence were slightly higher for PWD (25.3; 95% CI 20.1, 30.5) compared to PWoD (21.9; 95% CI 20.3, 23.5), but differences were not statistically significant. The association of dementia with hip fracture—but not pneumonia or widowhood—was modified by gender (male incidence rate ratio (IRR) 2.24, 95% CI 1.34, 3.75 versus female IRR 1.31 95% CI 0.92,1.86); interaction term p=0.02).
Conclusions:
Compared to PWoD, community-dwelling PWD had higher rates of pneumonia and hip fracture, but not widowhood. Knowing how often PWD experience these events can aid in anticipatory guidance and care planning for this growing population.
Keywords: Dementia, hip fracture, pneumonia, widowhood
Introduction
Dementia afflicts 5.6 million Americans and costs upwards of $200 billion/year.1 The existing paradigm is that the course of dementia follows a slow and steady decline of increasing functional and cognitive impairment.2,3 Alternatively, there are data that suggest that for some the course of dementia is punctuated by major medical and social events that accelerate the trajectory of decline and increase risk of mortality to a greater extent than in people without dementia (PWoD).3–5 These events may be disruptive to both the people with dementia (PWD) and their caregivers, requiring burdensome and exhausting hospitalizations and reformulations of caregiving and/or living arrangements following the event.
There are numerous examples of events that could be considered disruptive, and one could argue that any medical, surgical, or social events that results in hospitalization, transfer to long-term care, or change in living situation could qualify. From among the many possible events, we identified exemplar events that met the following criteria: (1) associated with poor outcomes in older adults in prior literature; (2) represented distinct domains, specifically, medical, surgical, and social; and (3) were measurable in the Health and Retirement Study-Medicare linked dataset. Our final selection of events included hospitalization for pneumonia (medical), hip fractures (surgical), and widowhood (social). Hospitalization for pneumonia is a medical event that is one of the leading causes of morbidity and mortality for older adults, and, has been shown to be associated with potentially burdensome interventions, such as parental antibiotics and feeding tube placement, in nursing home residents.6,7 Hip fractures are traumatic injuries and surgical events associated with high levels of geriatric and palliative care needs and functional decline before and after the event.8,9 Widowhood is a social event with consequences on health, financial, and socioemotional experience of the surviving spouse.10,11
Even for events as important to the geriatric population as pneumonia, hip fracture, and widowhood, basic information about the frequency of these events in PWD is lacking. Despite the fact that 80% of PWD in the U.S. reside in the community with a range of dementia severity12, most studies of hip fracture and pneumonia incidence and outcomes in PWD are limited to hospital or nursing home based samples of people with severe dementia.13–16 Other studies have found higher rates of both overall and potentially avoidable hospitalizations among PWD in the U.S., but have not specifically examined hip fracture or pneumonia.17,18 The few population-based studies of incidence rates of hip fracture and pneumonia in community-dwelling PWD have mainly been carried out in Europe and Asia.19,20 Studies of widowhood have primarily been limited to cognitively intact adults and have not documented the incidence of widowhood in people with and without dementia.21
Although previous studies have examined events such as hip fracture, pneumonia, and widowhood in isolation, few studies have considered disruptive events as conceptually similar in their likelihood to lead to a shift in health status and other outcomes. As part of a larger study that will assess trajectories following disruptive events in community-dwelling people with and without dementia, the objective of this initial study was to quantify the frequency of our selected disruptive events in these groups. We hypothesized that the cognitive, physical, and functional declines that characterize dementia make PWD more susceptible to serious falls, infections, or aspiration that lead to hip fractures and pneumonia.7,22 With limited evidence on the incidence of widowhood to guide us, we considered the widowhood analyses exploratory. However, based on research demonstrating that caregiving for PWD is associated with high rates of caregiver strain and may be associated with accelerated aging and death, our exploratory hypothesis was that widowhood rates would be higher in PWD.23 Finally, because prior research indicated there may be gender differences in the incidence of these disruptive events (e.g., higher incidence of hip fractures in women),24 we explored gender differences in incidence rates between groups by stratifying results by gender. Of note, we chose to use the term “disruptive event”, instead of “sentinel event” which has sometimes been used to describe these types of events in dementia, to avoid confusion with the more common use of “sentinel event” in patient safety.25
Methods
Data Sources and Participants
We used data from the Health and Retirement Study (HRS), a longitudinal, nationally-representative study of older adults begun in 1992. Interviews are conducted every two years via telephone in most cases, with face-to-face interviews conducted for most participants 80 and older, those too ill to participate in a telephone interview, or those unable to access a phone. Response rates for core interviews range from 85–90%. The HRS uses a national area probability sample of U.S. households, with supplemental oversamples of Black and Hispanic participants. HRS design and data collection procedures are available elsewhere.26
Our cohort included all HRS participants with a completed 2010 core interview (n=22,033). We selected 2010 because it balances data recency with adequate follow-up time and enough events to estimate incidence rates with precision. This time frame also allowed us to avoid excluding Medicare Advantage (MA) enrollees in our analysis, since Medicare required reporting of MA inpatient visits starting in 2008. We excluded individuals younger than 65 (n=11,521), nursing home residents at baseline (n=449), individuals who did not agree to have their data linked to Medicare claims (n=585), individuals without continuous Part A enrollment 2010–2018 (n=18), and those missing a baseline dementia status (n=114), for a final sample of 9,346. The widowhood cohort was a subset of the larger cohort and included participants who were married or partnered and currently living with a spouse in 2010 (n=5,105). We followed participants through 2018 - the most recent year of Medicare-linked data available from HRS.
Outcomes
Hip Fracture:
Based on previous algorithms27,28, we identified inpatient hospitalizations for hip fracture (femoral neck or intertrochanteric fractures) in the Medicare inpatient claims file using ICD-9 codes before 2015 and ICD-10 thereafter. For ICD-9 codes, we included admissions with code 820.xx and excluded admissions that were considered late effects from a prior hip fracture (733.81, 733.82, 905.3, V540-V549). ICD-10 codes included S72.0XX, S72.1XX, M80.05X, M84.45, M80.85X, M84.65X with letters A, B, or C to indicate an initial encounter. Both ICD-9 and 10 definitions included a period of 100 days to ensure we identified distinct events. We excluded admissions to long-term acute care (LTAC) facilities. While some studies have included both outpatient and inpatient claims to identify hip fractures, and have also included contiguous fractures (e.g. pelvic fractures), we opted against this approach for several reasons: 1) 90–95% of all hip fracture events will be captured in the inpatient file27; 2) Non-operative outpatient management of hip fractures is rare in community-dwelling older adults and usually reserved for those at the very end of life; and 3) We sought a uniform definition of hip fracture based on prior work.4,5,8,9,29
Pneumonia:
Guided by prior algorithms30–32, we defined pneumonia using ICD-9 and ICD-10 diagnostic codes in the Medicare inpatient claims file (see Supplement Table S1 for full list). We included ICD codes in any position in the claims and applied a 30-day period to define a single pneumonia event. While we considered including outpatient files to identify pneumonia, we opted to only include pneumonia that resulted in hospitalization because: 1) we were interested in events that would lead to a substantial disruption in an older person’s life, and reasoned that pneumonia managed in the outpatient setting would not meet those criteria; 2) We wanted to create consistency with our definition of hip fractures; 3) Data on outpatient claims for MA (MA) enrollees have not been validated to our knowledge, thus including outpatient events in our definition would have required excluding MA enrollees. This exclusion would have reduced generalizability since a large proportion (~ 30%) of our sample were enrolled in MA. Admissions to LTAC facilities were excluded.
Widowhood:
We defined widowhood as a new report of a spouse’s death (not gender specific) based on self or proxy response in the biennial HRS interview, which also includes the date of the spouse’s death. This approach has been used previously with HRS data.33
Primary Predictor
Our primary predictor was time-varying dementia status based on the validated Hurd algorithm.34 This algorithm uses cognitive and functional data from the HRS interviews to estimate a predicted probability that the participant has dementia at the time of each biennial interview. We classified participants with a predicted probability of 0.5 or greater as having dementia based on prior studies.35 The distribution of dementia probabilities in our sample demonstrated that vast majority of people were either <0.3 or equal to 1, further justifying this approach.
Other Variables
We described our sample by examining sociodemographic and clinical characteristics at the time of the baseline interview. These included mean age and age by category (65–74/75–84/85+), gender (male/female); race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic/non-Hispanic Other); educational attainment (greater or less than high school education); median household wealth; marital status (married or partnered/divorced or separated/never married/widowed); living situation (lives alone or with spouse only if married/lives with others); Medicaid eligible (yes/no); Medicare Part C (also referred to as Medicare Advantage) enrollee (yes/no); mean number of comorbidities; impairments in activities of daily living (0–1/2+); and smoking status (never/past or current).
Statistical Analysis
We used Poisson regression to estimate incidence rates for each disruptive event by dementia status and incidence rate ratios comparing PWD to PWoD. Multiple episodes of pneumonia and hip fracture were included in the calculation of incidence rates, while widowhood could occur once. Because dementia status could vary over the study period, participants could contribute time to both the dementia and non-dementia calculations. We report rates in number of events per thousand person-years. All analyses were adjusted for age as a continuous variable and stratified by gender. We opted against adjusting for other sociodemographic variables (race, education, wealth, etc) due to their high correlation with dementia, which would reduce our ability to assess the independent effect of dementia on our outcomes.
Twelve percent of participants were missing data on dementia status at any follow-up assessment. Based on the assumption that a person with dementia would continue to have dementia, if a participant was categorized as having dementia we then categorized all future assessments as dementia. Conversely, we assigned missing assessments to the no dementia group if that participant was classified as having no dementia in a later round but were missing dementia status in an earlier round. This reduced missing to 8.7%. For the remaining missing, we excluded interviews with missing data (lost to follow-up). We conducted several sensitivity analyses to examine different approaches to dealing with missing data: 1) carry forward last dementia status for all assessments; 2) classify all missing assessment as dementia; 3) classify all missing assessments as no dementia.
All analyses take into account the complex survey design in HRS. Analyses were conducted in SAS Version 9.4 and Stata Version 17. This study was approved by the UCSF and ISMMS Internal Review Boards
Results
Sample characteristics are in Table 1. At baseline (2010), 596 participants met criteria for dementia and 8,750 did not. PWD were older (mean age 84 vs. 75), were more likely to be female (67% vs. 57%), less often reported being non-Hispanic White (69% versus 84%), and had lower median household wealth ($74,096 vs. $225,869) than PWoD. In the married at baseline subset, 273 met criteria for dementia and 4,382 did not. Differences in characteristics between those with and without dementia in this subset were similar to the entire cohort. Overall, the married at baseline subset were younger, less likely to be male, more likely to report being Non-Hispanic White, and had lower household wealth than the cohort as a whole. The mean follow-up time for the baseline cohort was 4.0 years (SD 2.7) for PWD and 6.9 years (SD 2.3) for PWoD. In the married cohort, the mean follow-up time was 4.1 years (SD 2.7) for PWD and 7.0 years (SD 2.1) for PWoD. Among the baseline cohort, 81 (13.6%) PWD and 451 (5.2%) PWoD were hospitalized for pneumonia, 22 (3.7%) PWD and 90 (1.0%) PWoD had a hip fracture, and 36 (16.9%) PWD and 760 (15.8%) PWoD were widowed.
Table 1.
Participant characteristics at baseline
| Total | Married/Partnered Subset | |||
|---|---|---|---|---|
| Dementia (N=596) | No Dementia (N=8,750) | Dementia (N=273) | No Dementia (N=4,823) | |
| Mean follow-up time, years (SD) | 4.0 (2.7) | 6.9 (2.3) | 4.1 (2.7) | 7.0 (2.1) |
| Mean age (SD) | 84 (6.6) | 75 (5.7) | 81 (7) | 74 (6) |
| Age category, n (%) | ||||
| 65–74 | 75 (13) | 4435 (52) | 39 (17) | 2723 (59) |
| 75–84 | 210 (33) | 3337 (36) | 142 (49) | 1793 (34) |
| 85+ | 311 (54) | 978 (12) | 92 (35) | 307 (7) |
| Female, n(%) | 381 (67) | 5026 (57) | 113 (39) | 2177 (44) |
| Race and Ethnicity, n (%) | ||||
| Non-Hispanic White | 371 (69) | 6785 (84) | 205 (77) | 3972 (88) |
| Non-Hispanic Black | 129 (14) | 1103 (8) | 29 (7) | 416 (5) |
| Hispanic/Non-Hispanic Other | 94 (17) | 861 (8) | 39 (16) | 434 (7) |
| Less than high school education, n(%) | 275 (44) | 2308 (23) | 98 (35) | 961 (17) |
| Median household wealth, US $ (IQR) | 74,096 (1,905– 278,505) | 225,869 (65,960– 569,840) | 176,700 (132,000– 772,118) | 325,563 (58,000–579,000) |
| Current marital status, n (%) | ||||
| Married | 226 (35) | 5246 (58) | 273 (100) | 4,823 (100) |
| Divorced/separated/never married | 70 (15) | 1102 (15) | N/A | N/A |
| Widowed | 200 (51) | 2400 (27) | N/A | N/A |
| Living situation, n (%) | ||||
| Lives alone (or with spouse only in married/partnered subset) | 166 (34) | 2509 (32) | 196 (74) | 3940 (84) |
| Medicare Part C enrollee, n (%) | 180 (29) | 2784 (31) | 85 (32) | 1487 (31) |
| Medicaid dual eligible, n (%) | 174 (28) | 990 (10) | 64 (14) | 246 (4) |
| Number of comorbidities, mean (SD) | 1.9 (1.2) | 1.7 (1.1) | 2.1 (1.2) | 1.6 (1.1) |
| Impairments in activities of daily living, n (%) | ||||
| 0–1 | 314 (54) | 7890 (91) | 128 (59) | 4463 (94) |
| 2+ | 276 (46) | 854 (9) | 145 (41) | 360 (6) |
| Smoking status, n (%) | ||||
| Never smoker | 306 (56) | 3685 (42) | 120 (50) | 1997 (42) |
| Past or current smoker | 282 (44) | 4957 (57) | 148 (50) | 2782 (58) |
Notes. Data Source: Health and Retirement Study, 2010–2018. Estimates are weighted to adjust for complex survey design. SD=standard deviation.
Age-adjusted incidence rate estimates of all three disruptive events were higher in PWD compared to those without (Table 2, Figure 1). The incidence rate of pneumonia in PWD was 113.1 (95% CI 94.3,131.9) per 1000 person-years, which was almost double that of PWoD 62.1 (95% CI 54.7 69.5), IRR 1.82 (95% CI 1.53, 2.17). The hip fracture rate was 12.3 (95% CI 9.1, 15.6) per 1000 person-years in PWD compared to 8.1 (95% CI 6.9, 9.2) in PWoD, IRR 1.53 (95% CI 1.09, 2.4). Widowhood incidence rate was slightly higher in PWD (25.3 per 1000 person-years, 95% CI 20.1, 30.5) compared to PWoD (21.9 per 1000 person-years, 95% CI 20.3, 23.5), though differences were not statistically significant (IRR 1.15, 95% CI 0.93, 1.44). Values of incidence rates and IRR’s were similar in sensitivity analyses, with slight attenuation in values when missing values were changed to having dementia (Table 3).
Table 2.
Age-adjusted incidence rate per 1000 person-years and incidence rate ratio of pneumonia, hip fracture, and widowhood in people with and without dementia (N=9,346)
| No Dementia | Dementia | ||
|---|---|---|---|
| Incidence Rate Per 1000 Person-Years (95% CI) |
Incidence Rate Per 1000 Person-Years (95% CI) |
Incidence Rate Ratio1 (95% CI) |
|
| Pneumonia (all) | 62.1 (54.7, 69.5) | 113.1 (94.3, 131.9) | 1.82 (1.53, 2.17) |
| Male | 75.6 (63.6, 87.6) | 148.4 (117.1, 179.8) | 1.96 (1.57, 2.45) |
| Female | 51.5 (44.3, 58.7) | 91.8 (68.7, 114.9) | 1.78 (1.39, 2.30) |
| Hip fracture (all) | 8.1 (6.9, 9.2) | 12.3 (9.1, 15.6) | 1.53 (1.09, 2.14) |
| Male | 4.7 (3.5, 5.8) | 10.4 (5.9, 15.0) | 2.24 (1.34, 3.75) |
| Female | 10.5 (8.9, 12.1) | 13.7 (10.0, 17.5) | 1.31 (0.92, 1.86) |
| Widowhood (all) | 21.9 (20.3, 23.5) | 25.3 (20.1, 30.5) | 1.15 (0.93, 1.44) |
| Male | 12.6 (10.9, 14.4) | 12.6 (7.8, 17.4) | 1.00 (0.66, 1.13) |
| Female | 32.7 (30.1, 35) | 38.1 (29.3, 47.0) | 1.17 (0.91, 1.49) |
Notes. Data Source: Health and Retirement Study, 2010–2018. Estimates are weighted to adjust for complex survey design.
Reference group is people without dementia. Abbreviations: CI=Confidence interval
Figure 1.
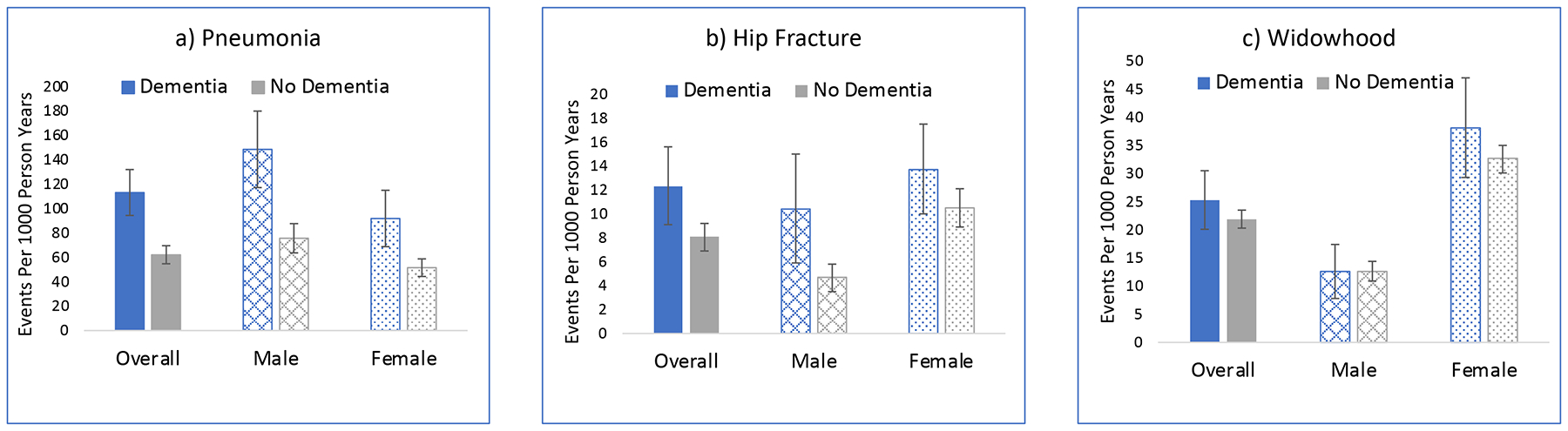
Age-adjusted incidence rates for: a) pneumonia; b) hip fracture; and c) widowhood in Health and Retirement Study participants, 2010–2018 (N=9,346). Bars indicate 95% confidence intervals.
Table 3.
Sensitivity analysis using different approaches to missing assessment data on dementia status
| Pneumonia | Hip Fracture | Widowhood | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Dementia | No Dementia | Dementia | No Dementia | Dementia | No Dementia | ||||
| Incidence rate per 1000 person-years (95% CI) |
Incidence rate per 1000 person-years (95% CI) |
Incidence Rate Ratio (95% CI) |
Incidence rate per 1000 person-years (95% CI) |
Incidence rate per 1000 person-years (95% CI) |
Incidence Rate Ratio (95% CI) |
Incidence rate per 1000 person-years (95% CI) |
Incidence rate per 1000 person-years (95% CI) |
Incidence Rate Ratio (95% CI) |
|
| Last dementia status carried forward | 114.5 (95.4, 133.6) |
65.2 (57.4, 72.9) |
1.76 (1.48, 2.09) |
12.4 (9.2, 15.7) |
8.0 (7.0, 9.1) |
1.6 (1.1, 2.2) |
25.6 (20.4, 30.8) |
21.2 (19.6, 22.7) |
1.2 (1.0, 1.5) |
| Change all missing to dementia | 109.1 (92.8, 125.4) |
63.4 (55.9, 71.0) |
1.72 (1.49, 1.99) |
10.9 (8.5, 13.3) |
8.2 (7.0, 9.3) |
1.3 (1.0, 1.8) |
18.5 (15.1, 22.0) |
22.2 (20.6, 23.9) |
0.8 (0.7, 1.0) |
| Change all missing to no dementia | 114.7 (95.6, 133.8) |
65.2 (57.4, 72.9) |
1.76 (1.48, 2.09) |
12.5 (9.2, 15.7) |
8.0 (7.0, 9.1) |
1.6 (1.1, 2.2) |
25.7 (20.5, 31.0) |
21.2 (19.6, 22.7) |
1.2 (1.0, 1.5) |
Notes. Data source: Health and Retirement Study, 2010–2018. All analyses age-adjusted and weighted to account for complex survey design. Abbreviations: CI=confidence interval
Gender differences in the incidence rates of the disruptive events were noted. Men had higher rates of pneumonia, while women had higher rates of hip fracture and widowhood in both the dementia and no dementia groups (Table 2). Males had a higher IRR for hip fracture (IRR 2.24, 95% CI 1.34, 3.75) compared to females (IRR 1.31, 95% CI 0.92, 1.86) and the interaction term for gender and dementia was statistically significant (p=0.02). The interaction term was not statistically significant for pneumonia (p=0.2) and widowhood (p=0.7).
Discussion
In this study of a nationally-representative sample of community-dwelling older adults in the United States, about 1 in 10 PWD were hospitalized for pneumonia, 1 in 100 were hospitalized with a hip fracture, and 1 in 40 were widowed annually. As a point of comparison, just under 1 in 50 adults 65 and older were hospitalized for COVID-19 between March 2020 and September 2021.36 Compared to PWoD, these rates were 80% higher for pneumonia and 40% higher for hip fracture. Although not statistically significant, point estimates for widowhood were 15% higher among PWD. Gender modified the association between dementia and hip fracture (higher ratios among males than females).
Our findings provide initial evidence that for a substantial proportion of community dwelling PWD, the clinical course is not one of gradual physical and cognitive decline2,3 –but is staggered, punctuated by potentially disruptive medical and social events that have the potential to markedly alter prognoses and care needs. As we expected, pneumonia and hip fractures were more common among PWD than PWoD. The higher hip fracture rates among men with dementia but not women with dementia (compared to those without dementia) is likely explained by the higher prevalence of osteoporosis in women compared to men.37 Osteoporotic women are more likely to sustain fractures following less severe falls and this may attenuate differences between women with and without dementia. Men, conversely, are less often affected by osteoporosis, and thus will only experience a hip fracture in the event of a severe fall, which are more common in PWD.38 We did not find evidence for increased widowhood by dementia status. While this may be due to a small sample size and insufficient power, further research that measures the spousal caregiver stress experience is required to adequately examine this issue.
These findings fill a gap in our knowledge about how frequently these disruptive events occur in community-dwelling PWD in the U.S. and are also novel in considering these potentially disruptive medical, surgical, and social events congruently, rather than in isolation. Most U.S. based studies examining pneumonia and hip fractures have sampled from nursing home or hospital-based populations have focused on assessing prevalence and outcomes, not incidence.7,39 Findings from the few international studies that have examined incidence of these events in community-based populations are generally consistent with our findings.19,20,40–43 While recent studies of widowhood have examined the association between widowhood and risk of incident dementia44,45, our study flips this equation to examine the association between dementia and risk of widowhood. By considering both medical/surgical and social potentially disruptive events as conceptually linked, we expand our examination of such events beyond a medically-focused paradigm to a paradigm that incorporates the social sphere, which may have equal or greater consequences on one’s health.46
Information on the absolute and relative frequency of these events will be useful for clinicians, healthcare systems, and policymakers. Clinicians can use these data as the basis for anticipatory guidance to PWD and caregivers about the likely course of illness to help inform financial and care planning, as well as help surrogates prepare for the complex medical decision making that may be required for PWD in the setting of what we have identified as not-uncommon acute disruptive events. Healthcare systems require these types of data to better manage their patient populations – particularly as reimbursement shifts from fee-for-service to value-based payments.47 Planning for and managing high-need high-cost patient populations as exemplified by PWD experiencing disruptive events, is a key component of successful value- based care.48 Policymakers can use these data for resource planning, risk adjustment and quality reporting, and development of payment models. Economic analyses that consider dementia as a gradually progressive disease with predictable expenditures are likely to underestimate the true yearly costs of this disease. Metrics for pneumonia and hip fracture care under the Centers for Medicare and Medicaid Services value-based and public reporting programs do not consider the contributions of dementia to patient outcomes.49 Our data support the development of new measures that account for these interactions. Finally, payment models should be informed by our data when establishing case rates for PWD.
Widowhood likely has critical implications for community-dwelling PWD that will require further study. Spouses are often the primary, and frequently the only, caregiver for community-dwelling PWD.50 Thus, the death of a spouse may mean that alternate caregiving arrangements (e.g., moving in with adult children, hiring an in-home caregiver, or moving to facilities or settings with higher levels of care (e.g., assisted living, nursing homes) will need to be arranged. These arrangements may occur under potentially stressful circumstances and at significant financial cost to families and/or government payors, such as Medicaid, which most often covers the cost of in-home and facility-based long-term care.51 Since, as our results show, PWD already have much lower household wealth than PWoD, it is critical that future research address the financial impacts of widowhood for PWD, not only for individuals and families, but also for long-term care payors.
This study has limitations. First, the algorithm to determine dementia status is not as rigorous as a formal clinical diagnosis, and misclassification may have occurred.35 Misclassification may also have occurred because dementia status was only assessed at two-year time intervals, and it is possible that some people who developed dementia in the intervening time would be classified as not having dementia. However, this would likely have the effect of diminishing differences between the two groups, so if anything, differences are greater than what we observe. Furthermore, the algorithm-based approach does not allow for determinations of the severity of dementia, and there may be differences in incidence rates between people with mild versus moderate to severe dementia. Second, there was a relatively high proportion of participants missing data necessary to ascertain dementia status. However, sensitivity analyses demonstrated robust consistency in our estimates. Slight attenuations in differences when assigning those with missing data to the dementia group are to be expected, since most of those individuals will not have dementia and will therefore have lower incidence of events. Third, although about 85% of HRS respondents agree to have their data linked to Medicare, we cannot rule out selection bias from including only those HRS respondents with a Medicare linkage. Fourth, although studies show that 90% of MA hospitalizations are captured in Medicare claims data52, we may be missing some hip fractures and pneumonia cases among MA enrollees. However, we believe it is important to include MA enrollees in our analysis, considering that they recently comprise 30–40% of all Medicare enrollees. Fifth, our pneumonia events only included those that resulted in hospitalization and should not be construed as representing the rate of all community-acquired pneumonia cases. Finally, we do not yet know if the events examined in this study are disproportionately disruptive for PWD and whether findings of higher incidence and impact extend to other events, such as myocardial infarction and stroke.
In conclusion, this initial study provides data on the incidence of three potentially disruptive medical, surgical, and social events in community-dwelling people with dementia relative to people without dementia. These data fill a gap in our basic understanding of the frequency of these events, which can begin to inform anticipatory guidance discussions with patients and families and the development of services and supports to better support PWD and their caregivers. Forthcoming studies will assess the impacts of disruptive events on the trajectories of people with dementia, as well as the social and economic impacts of these events on caregivers and families.
Supplementary Material
Supplement Table S1. List of ICD-9 and ICD-10 codes used to identify pneumonia
Key Points.
Potentially disruptive medical, surgical, and social events may accelerate the trajectory of decline and impact caregiving needs in people with dementia.
The incidence of potentially disruptive events has not been previously examined in community-dwelling people with dementia, who comprise the majority of the dementia population.
We found that compared to people without dementia, people with dementia had higher age-adjusted incidence rates of pneumonia and hip fracture, while differences in widowhood rates were not statistically significant.
Why Does This Matter?
Knowing how often community-dwelling people with dementia experience potentially disruptive events can aid in anticipatory guidance and care planning for this growing population.
Acknowledgements
The authors would like to thank Brian Nguyen for his administrative support of this project, as well as other investigators on the DEVELOP AD research team for their helpful advice and feedback on this project.
Disclosures:
This project was supported by the National Institute on Aging (P01AG066605). Dr. Hunt was supported by the National Center for Advancing Translational Sciences (KL2TR001870). Dr. Smith was supported by the National Institute on Aging (K24AG068312). Dr. Morrison was supported by P30AG028741 and R33AG065726 from the National Institute on Aging and by the National Palliative Care Research Center. The Health and Retirement Study is sponsored by the National Institute on Aging (U01AG009740) and the Social Security Administration.
Sponsor’s Role:
The sponsor had no role in the design, methods, subject recruitment, data collection, analysis or preparation of paper.
Footnotes
Conflict of Interest Statement: The authors have no conflicts to disclose.
References
- 1.Alzheimer’s Association. Alzheimer’s Disease Facts and Figures. Alzheimer’s & dementia : the journal of the Alzheimer’s Association. 2021;17(3). [DOI] [PubMed] [Google Scholar]
- 2.Lunney JR, Lynn J, Hogan C. Profiles of older medicare decedents. Journal of the American Geriatrics Society. 2002;50(6):1108–1112. [DOI] [PubMed] [Google Scholar]
- 3.Gill TM, Gahbauer EA, Han L, Allore HG. Trajectories of disability in the last year of life. The New England journal of medicine. 2010;362(13):1173–1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morrison RS, Siu AL. Mortality from pneumonia and hip fractures in patients with advanced dementia. JAMA : the journal of the American Medical Association. 2000;284(19):2447–2448. [PubMed] [Google Scholar]
- 5.Morrison RS, Siu AL. Survival in end-stage dementia following acute illness. JAMA : the journal of the American Medical Association. 2000;284(1):47–52. [DOI] [PubMed] [Google Scholar]
- 6.Arnold FW, Reyes Vega AM, Salunkhe V, et al. Older Adults Hospitalized for Pneumonia in the United States: Incidence, Epidemiology, and Outcomes. Journal of the American Geriatrics Society. 2020;68(5):1007–1014. [DOI] [PubMed] [Google Scholar]
- 7.Mitchell SL, Teno JM, Kiely DK, et al. The clinical course of advanced dementia. The New England journal of medicine. 2009;361(16):1529–1538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cenzer IS, Tang V, Boscardin WJ, et al. One-Year Mortality After Hip Fracture: Development and Validation of a Prognostic Index. Journal of the American Geriatrics Society. 2016;64(9):1863–1868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ritchie CS, Kelley AS, Stijacic Cenzer I, Smith AK, Wallhagen ML, Covinsky KE. High Levels of Geriatric Palliative Care Needs in Hip Fracture Patients Before the Hip Fracture. Journal of pain and symptom management. 2016;52(4):533–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ornstein KA, Garrido MM, Siu AL, Bollens-Lund E, Rahman OK, Kelley AS. An Examination of Downstream Effects of Bereavement on Healthcare Utilization for Surviving Spouses in a National Sample of Older Adults. Pharmacoeconomics. 2019;37(4):585–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vable AM, Subramanian SV, Rist PM, Glymour MM. Does the “widowhood effect” precede spousal bereavement? Results from a nationally representative sample of older adults. The American journal of geriatric psychiatry : official journal of the American Association for Geriatric Psychiatry. 2015;23(3):283–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harrison KL, Ritchie CS, Patel K, et al. Care Settings and Clinical Characteristics of Older Adults with Moderately Severe Dementia. Journal of the American Geriatrics Society. 2019;67(9):1907–1912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zomer TP, VDM T, VANG-L AB, DEG SC, VDS JT, Verhoef L. Incidence of pneumonia in nursing home residents with dementia in the Netherlands: an estimation based on three differently designed studies. Epidemiol Infect. 2017;145(11):2400–2408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gruber-Baldini AL, Zimmerman S, Morrison RS, et al. Cognitive impairment in hip fracture patients: timing of detection and longitudinal follow-up. Journal of the American Geriatrics Society. 2003;51(9):1227–1236. [DOI] [PubMed] [Google Scholar]
- 15.Mitchell R, Harvey L, Brodaty H, Draper B, Close J. One-year mortality after hip fracture in older individuals: the effects of delirium and dementia. Archives of gerontology and geriatrics. 2017;72:135–141. [DOI] [PubMed] [Google Scholar]
- 16.Neuman MD, Silber JH, Magaziner JS, Passarella MA, Mehta S, Werner RM. Survival and functional outcomes after hip fracture among nursing home residents. JAMA internal medicine. 2014;174(8):1273–1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Phelan EA, Borson S, Grothaus L, Balch S, Larson EB. Association of incident dementia with hospitalizations. Jama. 2012;307(2):165–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Anderson TS, Marcantonio ER, McCarthy EP, Herzig SJ. National Trends in Potentially Preventable Hospitalizations of Older Adults with Dementia. Journal of the American Geriatrics Society. 2020;68(10):2240–2248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tolppanen AM, Lavikainen P, Soininen H, Hartikainen S. Incident hip fractures among community dwelling persons with Alzheimer’s disease in a Finnish nationwide register-based cohort. PloS one. 2013;8(3):e59124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang HK, Hung CM, Lin SH, et al. Increased risk of hip fractures in patients with dementia: a nationwide population-based study. BMC Neurol. 2014;14:175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stroebe M, Schut H, Stroebe W. Health outcomes of bereavement. Lancet. 2007;370(9603):1960–1973. [DOI] [PubMed] [Google Scholar]
- 22.McKhann GM, Knopman DS, Chertkow H, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s & dementia : the journal of the Alzheimer’s Association. 2011;7(3):263–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dassel KB, Carr DC. Does Dementia Caregiving Accelerate Frailty? Findings From the Health and Retirement Study. The Gerontologist. 2016;56(3):444–450. [DOI] [PubMed] [Google Scholar]
- 24.Smith AK, Walter LC, Miao Y, Boscardin WJ, Covinsky KE. Disability during the last two years of life. JAMA internal medicine. 2013;173(16):1506–1513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.The Joint Commission. Sentinel Event Policy and Procedures. https://www.jointcommission.org/resources/patient-safety-topics/sentinel-event/sentinel-event-policy-and-procedures/. Accessed August 18, 2021, 2021.
- 26.Ofstedal MB, Weir D, Chen K, Wagner J. Updates to HRS Sample Weights. Ann Arbor, MI: Survey Research Center University of Michigan;2011. [Google Scholar]
- 27.Rigler SK, Ellerbeck E, Whittle J, Mahnken J, Cook-Wiens G, Shireman TI. Comparing methods to identify hip fracture in a nursing home population using Medicare claims. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2011;22(1):57–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Berry SD, Zullo AR, McConeghy K, Lee Y, Daiello L, Kiel DP. Defining hip fracture with claims data: outpatient and provider claims matter. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2017;28(7):2233–2237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smith AK, Cenzer IS, John Boscardin W, Ritchie CS, Wallhagen ML, Covinsky KE. Increase in Disability Prevalence Before Hip Fracture. Journal of the American Geriatrics Society. 2015;63(10):2029–2035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lave JR, Fine MJ, Sankey SS, Hanusa BH, Weissfeld LA, Kapoor WN. Hospitalized pneumonia. Outcomes, treatment patterns, and costs in urban and rural areas. J Gen Intern Med. 1996;11(7):415–421. [DOI] [PubMed] [Google Scholar]
- 31.Brereton CJ, Lennon D, Browning S, Dunn E, Ferguson JK, Davis JS. Is gentamicin safe and effective for severe community-acquired pneumonia? An 8-year retrospective cohort study. Int J Antimicrob Agents. 2018;51(6):862–866. [DOI] [PubMed] [Google Scholar]
- 32.Zhang D, Petigara T, Yang X. Clinical and economic burden of pneumococcal disease in US adults aged 19–64 years with chronic or immunocompromising diseases: an observational database study. BMC Infect Dis. 2018;18(1):436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kotwal AA, Abdoler E, Diaz-Ramirez LG, et al. ‘Til Death Do Us Part: End-of-Life Experiences of Married Couples in a Nationally Representative Survey. Journal of the American Geriatrics Society. 2018;66(12):2360–2366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hurd MD, Martorell P, Delavande A, Mullen KJ, Langa KM. Monetary costs of dementia in the United States. The New England journal of medicine. 2013;368(14):1326–1334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Power MC, Gianattasio KZ, Ciarleglio A. Implications of the Use of Algorithmic Diagnoses or Medicare Claims to Ascertain Dementia. Neuroepidemiology. 2020;54(6):462–471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Center for Disease Control. Laboratory Confirmed COVID-19-Associated Hospitalizations. https://gis.cdc.gov/grasp/covidnet/covid19_3.html. Accessed August 23, 2021.
- 37.Alswat KA. Gender Disparities in Osteoporosis. Journal of clinical medicine research. 2017;9(5):382–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.van Doorn C, Gruber-Baldini AL, Zimmerman S, et al. Dementia as a risk factor for falls and fall injuries among nursing home residents. Journal of the American Geriatrics Society. 2003;51(9):1213–1218. [DOI] [PubMed] [Google Scholar]
- 39.Gruber-Baldini AL, Hosseini M, Orwig D, et al. Cognitive Differences between Men and Women who Fracture their Hip and Impact on Six-Month Survival. Journal of the American Geriatrics Society. 2017;65(3):e64–e69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jantzen C, Madsen CM, Lauritzen JB, Jørgensen HL. Temporal trends in hip fracture incidence, mortality, and morbidity in Denmark from 1999 to 2012. Acta Orthop. 2018;89(2):170–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tolppanen AM, Taipale H, Tanskanen A, Tiihonen J, Hartikainen S. Comparison of predictors of hip fracture and mortality after hip fracture in community-dwellers with and without Alzheimer’s disease - exposure-matched cohort study. BMC geriatrics. 2016;16(1):204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stubbs B, Perara G, Koyanagi A, et al. Risk of Hospitalized Falls and Hip Fractures in 22,103 Older Adults Receiving Mental Health Care vs 161,603 Controls: A Large Cohort Study. Journal of the American Medical Directors Association. 2020;21(12):1893–1899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lai SW, Chen YL, Lin CL, Liao KF. Alzheimer’s disease correlates with greater risk of hip fracture in older people: a cohort in Taiwan. Journal of the American Geriatrics Society. 2013;61(7):1231–1232. [DOI] [PubMed] [Google Scholar]
- 44.Liu H, Zhang Y, Burgard SA, Needham BL. Marital status and cognitive impairment in the United States: evidence from the National Health and Aging Trends Study. Ann Epidemiol. 2019;38:28–34.e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Singham T, Bell G, Saunders R, Stott J. Widowhood and cognitive decline in adults aged 50 and over: A systematic review and meta-analysis. Ageing Res Rev. 2021;71:101461. [DOI] [PubMed] [Google Scholar]
- 46.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA : the journal of the American Medical Association. 2004;291(10):1238–1245. [DOI] [PubMed] [Google Scholar]
- 47.Johnston KJ, Hockenberry JM, Joynt Maddox KE. Building a Better Clinician Value-Based Payment Program in Medicare. JAMA : the journal of the American Medical Association. 2021;325(2):129–130. [DOI] [PubMed] [Google Scholar]
- 48.National Academy of Medicine. Effective care for high-need patients. Opportunities for improving outcomes, value, and health. Washington DC: National Academy of Sciences; 2017. [PubMed] [Google Scholar]
- 49.Center for Medicare and Medicaid Services. CMS Measures Management System Blueprint Version 17.0. In:2021.
- 50.Ornstein KA, Wolff JL, Bollens-Lund E, Rahman OK, Kelley AS. Spousal Caregivers Are Caregiving Alone In The Last Years Of Life. Health affairs (Project Hope). 2019;38(6):964–972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kelley AS, McGarry K, Gorges R, Skinner JS. The burden of health care costs for patients with dementia in the last 5 years of life. Annals of internal medicine. 2015;163(10):729–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Huckfeldt PJ, Escarce JJ, Rabideau B, Karaca-Mandic P, Sood N. Less Intense Postacute Care, Better Outcomes For Enrollees In Medicare Advantage Than Those In Fee-For-Service. Health affairs (Project Hope). 2017;36(1):91–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplement Table S1. List of ICD-9 and ICD-10 codes used to identify pneumonia


