Abstract
Background & Aims
The COVID-19 pandemic has affected clinical services globally, including colorectal cancer (CRC) screening and diagnostic testing. We investigated the pandemic’s impact on fecal immunochemical test (FIT) screening, colonoscopy utilization, and colorectal neoplasia detection across 21 medical centers in a large integrated health care organization.
Methods
We performed a retrospective cohort study in Kaiser Permanente Northern California patients ages 18 to 89 years in 2019 and 2020 and measured changes in the numbers of mailed, completed, and positive FITs; colonoscopies; and cases of colorectal neoplasia detected by colonoscopy in 2020 vs 2019.
Results
FIT kit mailings ceased in mid-March through April 2020 but then rebounded and there was an 8.7% increase in kits mailed compared with 2019. With the later mailing of FIT kits, there were 9.0% fewer FITs completed and 10.1% fewer positive tests in 2020 vs 2019. Colonoscopy volumes declined 79.4% in April 2020 compared with April 2019 but recovered to near pre-pandemic volumes in September through December, resulting in a 26.9% decline in total colonoscopies performed in 2020. The number of patients diagnosed by colonoscopy with CRC and advanced adenoma declined by 8.7% and 26.9%, respectively, in 2020 vs 2019.
Conclusions
The pandemic led to fewer FIT screenings and colonoscopies in 2020 vs 2019; however, after the lifting of shelter-in-place orders, FIT screenings exceeded, and colonoscopy volumes nearly reached numbers from those same months in 2019. Overall, there was an 8.7% reduction in CRC cases diagnosed by colonoscopy in 2020. These data may help inform the development of strategies for CRC screening and diagnostic testing during future national emergencies.
Keywords: Colonoscopy, COVID-19, Pandemic, Screening, Cancer
The COVID-19 pandemic led to declines in colonoscopy volumes and the number of colorectal cancer and advanced adenoma cases detected in 2020 compared with 2019.
What You Need to Know.
Background and Context
COVID-19 has affected clinical services globally, including colorectal cancer screening and diagnostic testing; however, the magnitude of this impact remains unclear, particularly from population-based studies in the United States.
New Findings
Fecal immunochemical test mailings ceased in mid-March through April 2020 but rebounded afterward. Colonoscopy volumes, colorectal cancer cases, and advanced adenomas declined by 26.9%, 8.7%, and 26.9%, respectively, in 2020 vs 2019.
Limitations
We used a proxy method to ascertain colorectal cases during our study period; however, this method was highly accurate for case capture when validated against cancer registry data in previous years.
Impact
Improved understanding of the impact of COVID-19 on colorectal cancer screening, diagnostic testing, and its outcomes should inform strategies to mitigate these effects for future emergencies.
In December 2019, a cluster of viral pneumonia cases caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV2 or COVID-19) was discovered in Wuhan, China, and rapidly progressed from a local epidemic to a global pandemic.1 In March 2020, following guidance from the Centers for Disease Control and Prevention, county public health departments, and gastroenterology and professional societies, many US medical facilities ceased nonurgent endoscopic procedures, including colonoscopies for colorectal cancer (CRC) screening and post-polypectomy surveillance.2 Some organizations also elected to suspend fecal immunochemical test (FIT) screening to decrease the potential for a backlog of patients who were FIT-positive and needing colonoscopy.
The pandemic-related decrease in CRC screening and diagnostic testing services has fueled concerns of a potential negative impact on cancer prevention and care. Recent studies from European and Asian countries have reported sustained declines in screening colonoscopy volumes and CRC detection associated with the pandemic.3, 4, 5, 6, 7 Also, modeling studies early in the pandemic estimated an excess of 10,000 additional deaths from breast cancer and CRC in the United States related to delayed diagnoses.8 However, there has been little direct evidence quantifying the impact of the pandemic on CRC screening, diagnostic testing, and neoplasia detection in the United States, which has been among the hardest hit by COVID-19 in number of cases and deaths.1 Understanding the magnitude of the decline in CRC testing and neoplasia detection due to the pandemic is critical to understanding how many people will ultimately be affected and to inform subsequent screening strategies during national emergencies.9
To improve our understanding of the impact of the COVID-19 pandemic, we investigated changes in FIT screening, colonoscopy services, and colorectal neoplasia detection in 2020 compared with 2019, in a large, community-based, integrated health care setting in the United States.
Methods
Study Setting and Oversight
This study was conducted within Kaiser Permanente Northern California (KPNC), a large integrated health care organization that provides comprehensive inpatient and outpatient services to more than 4.5 million members in suburban, urban, and semi-rural regions throughout Northern California. All KPNC members are insured with complete access to primary and specialty care. All patient encounters, medical diagnoses, procedures, laboratory results, vital statistics, and information on demographics, membership, and social behaviors are recorded in electronic databases. KPNC membership is similar in demographic and socioeconomic characteristics to the Northern California region.10 KPNC has a well-established organized CRC screening program that offers annual mailing of FIT kits to screening-eligible members who are 50 to 75 years of age and not up to date with screening by another method, and colonoscopy screening by request. Colonoscopies of all indications are performed at 26 KPNC endoscopy centers.
The study was approved by the KPNC Institutional Review Board and the requirement for written informed consent was waived. The study was funded by the Garfield Foundation; the National Cancer Institute–funded Population-based Research to Optimize the Screening Process II (PROSPR II) consortium (UM1 CA222035), which conducts multisite, coordinated, transdisciplinary research to evaluate and improve cancer screening processes; and National Cancer Institute K-award (K07CA212057). The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Study Design, Eligibility Criteria, and Outcomes
The study was a retrospective cohort study of KPNC health plan members ages 18 to 89 years during 2019 and 2020. Cohort members were tracked each year for the following: FIT kit mailings (FIT mailings), completed FITs, positive FITs, colonoscopies performed in total and by indication (ie, screening, surveillance, diagnostic, and FIT positive), and colorectal neoplasia detection associated with the colonoscopy (ie, adenomas, advanced adenomas, and CRC).
Data Sources and Definitions
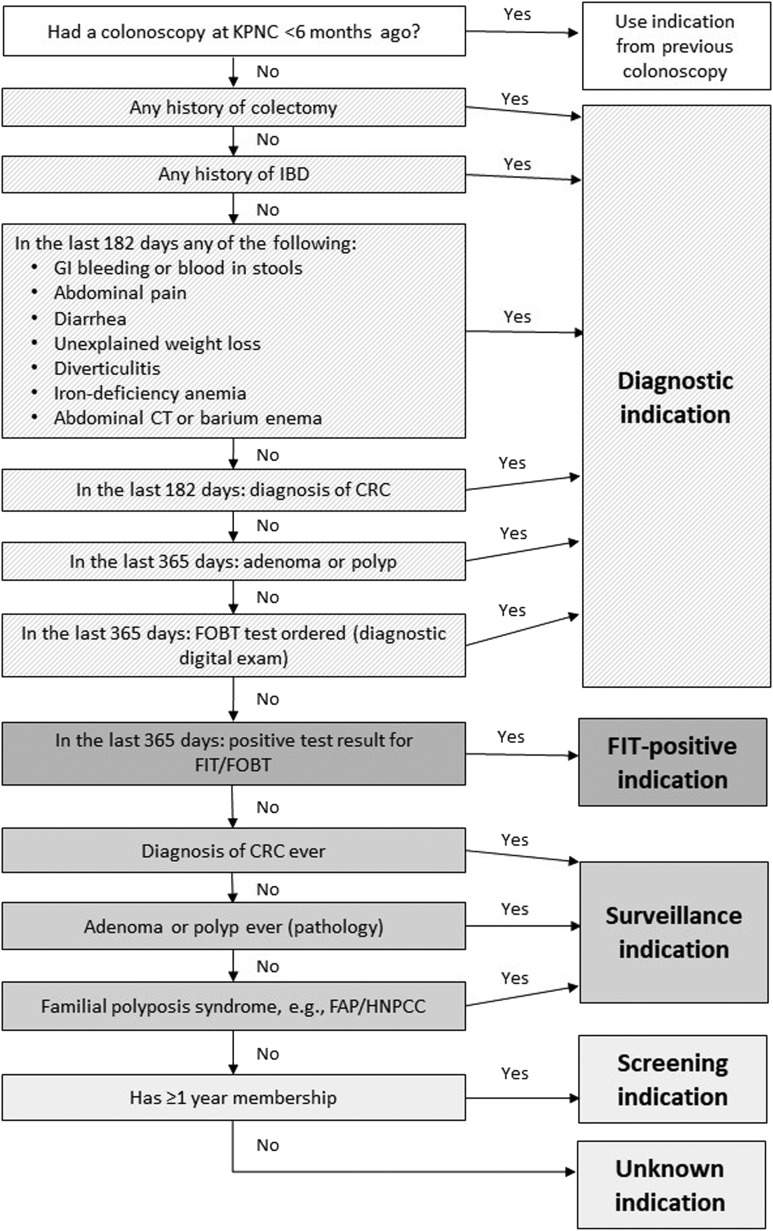
Demographic and clinical data were obtained from KPNC electronic health records and databases. Socioeconomic measures were obtained from the US Census American Community Survey 5-year 2015 to 2019 estimates for census tract, linked to individuals’ home address in 2019 and 2020.11 FIT mailings were ascertained from the regional screening program tracking database and completed test results from the laboratory database. Colonoscopy procedures were identified using Current Procedural Terminology codes, International Classification of Diseases, 10th Revision procedure codes, Healthcare Common Procedure Coding System codes, and KPNC-specific local codes. KPNC endoscopy data were captured using a uniform, structured flow sheet in the electronic medical record. Colonoscopy-related pathology results were identified using a combination of Systematized Nomenclature of Medicine (SNOMED) codes, synoptic reporting (surgical pathology only), and natural language processing of pathology reports. A validated algorithm depicted in Supplementary Figure 1 was used to assign colonoscopy indication, and FIT-positive colonoscopy was a distinct indication separate from diagnostic indication.12
Supplementary Figure 1.
Flow diagram summarizing algorithm used to assign colonoscopy indication.
Adenomas were defined as tubular adenomas, tubulovillous adenomas, villous adenomas, or adenomas with high-grade dysplasia. Advanced adenomas were defined as any adenoma with advanced histology (ie, villous or tubulovillous histology), high-grade dysplasia, or having an adenoma or polyp ≥10 mm in size. Adenoma histology was identified using SNOMED codes. High-grade dysplasia was identified using natural language processing–based text analysis of pathology reports; using a validation data set of 300 reports, we found a positive predictive value, sensitivity, and specificity for identifying high-grade dysplasia of 92%, 92%, and 100%, respectively.13 Adenoma or polyp size was identified from the colonoscopy procedure report.
CRC was defined as a colorectal adenocarcinoma diagnosed within 7 days of colonoscopy. Cases identified as stage 0 (ie, adenocarcinoma in situ) were not included. KPNC cancer registry data were not available for 2020; therefore, we identified CRC cases using synoptic reporting of surgical pathology when available and/or a combination of SNOMED pathology codes and International Classification of Diseases, 10th Revision or KPNC-specific diagnostic codes. We used the cancer registry to validate this proxy method of CRC identification among colonoscopies performed in 2018 and 2019; the method was found to be 94.1% sensitive and 99.6% specific (unpublished data). Therefore, the proxy method was used to identify CRC cases detected by colonoscopy for both 2019 and 2020.
Statistical Analyses
In all analyses, data are presented as the monthly and yearly number of tests or neoplasia findings in 2019 and 2020. Percentage changes in yearly and monthly figures were calculated by comparing the numbers in 2020 with the comparable yearly or monthly numbers in 2019 (the pre-COVID-19 baseline period).
Results
Demographic Characteristics
The KPNC membership population was relatively stable across 2019 and 2020. There were 3,366,645 members ages 18 to 89 years in July 2019, which increased 2.9% to 3,464,000 in July 2020. Those who completed a FIT in 2019 compared with 2020 were similar in age, sex, and race and ethnicity, as they were for those who completed a colonoscopy in 2019 compared with 2020 (Table 1 ). Indications for colonoscopy by age group in 2019 and 2020 are shown in Supplementary Table 1.
Table 1.
Characteristics of Individuals Who Completed a FIT or Underwent a Colonoscopy in 2019 and 2020
| Characteristics | Completed a FIT |
Underwent a colonoscopy |
||
|---|---|---|---|---|
| 2019 | 2020 | 2019 | 2020 | |
| Total persons, n | 614,051 | 558,810 | 110,594 | 80,863 |
| Age, y | ||||
| Mean (SD) | 61 (7) | 61 (7) | 60 (12) | 60 (13) |
| Median (interquartile range) | 60 (55–66) | 60 (55–67) | 61 (53–69) | 61 (52–69) |
| Range | 18–89 | 18–89 | 18–89 | 18–89 |
| Sex | ||||
| Female | 328,801 (53.5) | 296,682 (53.1) | 56,645 (51.2) | 41,285 (51.1) |
| Male | 285,250 (46.5) | 262,128 (46.9) | 53,949 (48.8) | 39,578 (48.9) |
| Race and ethnicity | ||||
| Asian or Pacific Islander | 129,809 (21.1) | 120,712 (21.6) | 19,922 (18.0) | 14,043 (17.4) |
| Non-Hispanic Black | 44,576 (7.3) | 42,301 (7.6) | 8,202 (7.4) | 6,561 (8.1) |
| Hispanic | 94,988 (15.5) | 86,083 (15.4) | 16,630 (15.0) | 12,886 (15.9) |
| Non-Hispanic White | 319,662 (52.1) | 283,461 (50.7) | 63,034 (57.0) | 44,937 (55.6) |
| Other/Unknown | 25,016 (4.1) | 26,253 (4.7) | 2,806 (2.5) | 2,436 (3.0) |
| Indication for colonoscopy | ||||
| Screening | 18,105 (16.4) | 10,593 (13.1) | ||
| Surveillance | 18,091 (16.4) | 11,156 (13.8) | ||
| FIT positive | 14,686 (13.3) | 11,748 (14.5) | ||
| Diagnostic | 57,191 (51.7) | 45,783 (56.6) | ||
| Unknown (member <1 year) | 2,521 (2.3) | 1,583 (2.0) | ||
| Percent with 4-year college degree in census tracta | ||||
| Median (interquartile range) | 38 (24–54) | 38 (24–55) | 39 (25–55) | 39 (25–56) |
| Median household income ($) in census tracta | ||||
| Median (interquartile range) | 95,000 (71,506–124,643) | 95,515 (72,059–124,874) | 96,481 (72,985–127,409) | 96,313 (72,841–127,125) |
NOTE. Values are % (n) unless otherwise indicated.
Using US Census American Community Survey 2015–2019 5-year estimates for home address census tract in 2019 and 2020.
FIT Screening
During 2019, 832,438 total FITs were mailed (mean ± standard deviation [SD]: 69,370 ± 24,904 kits/month) and monthly FIT mailings peaked at 95,529 in July and reached a low of 19,225 in December (Figure 1 and Supplementary Table 2).
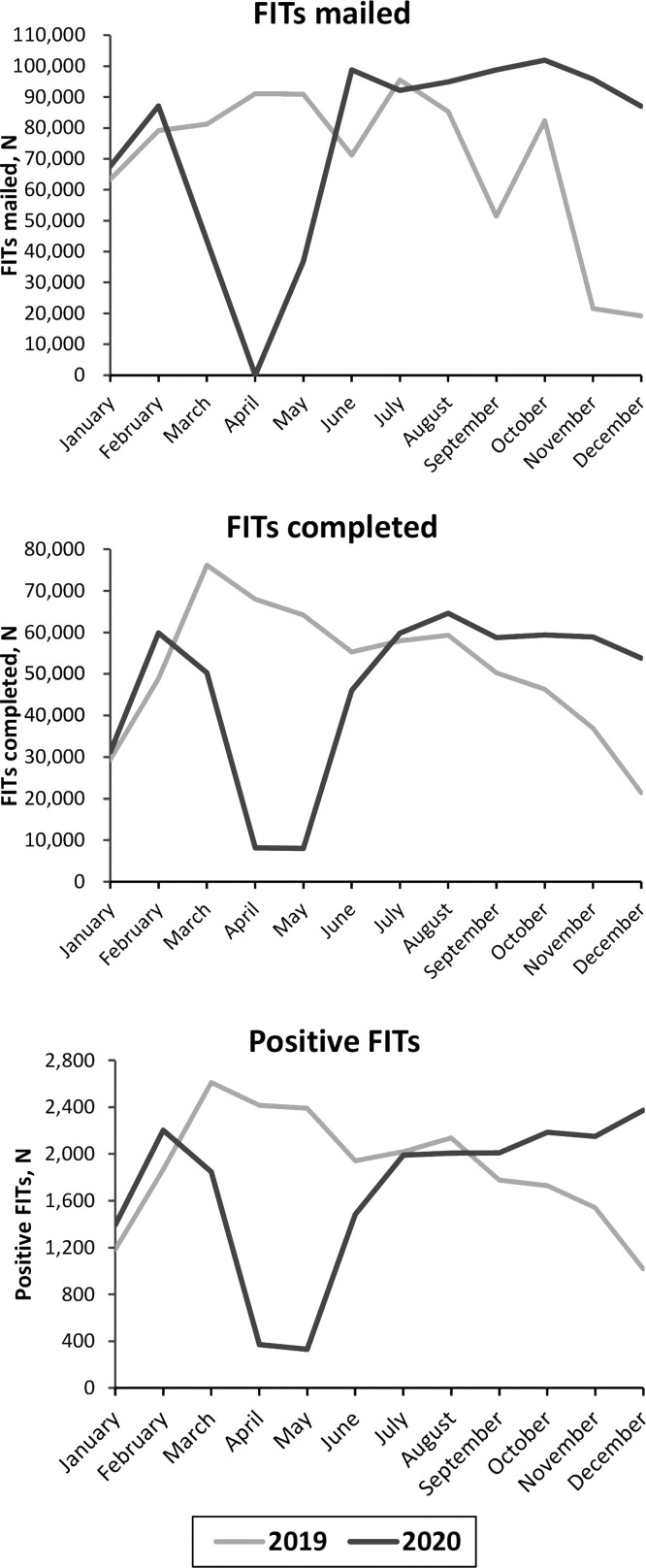
Figure 1.
The number of patients who were mailed a FIT kit, completed the FIT, and tested positive in 2019 and 2020.
In 2020, due to the inclusion of African American individuals aged 45 to 49 and all members beginning at the age of 50 (instead of commencing in the calendar year of their 51st birthday), 904,547 total FITs were mailed (mean ± SD: 75,379 ± 30,815 kits/month), representing an 8.7% increase from 2019, but with greater monthly variability. Specifically, beginning in March 2020 when the pandemic-related shelter-in-place order was issued, FIT mailings sharply declined and no FITs were mailed in April 2020, compared with the 91,082 FITs mailed in April 2019. By June 2020, there was a rapid recovery in FIT mailings, and from June through December 2020, FIT mailings were comparable to or greater than the corresponding months in 2019. FIT distribution in 2020 was heavily skewed toward the last third of the year, accounting for 41% of the total FITs mailed; by comparison, 21% of the total annual FITs mailed were accounted for in that period in 2019.
With the shift in FIT mailings toward the latter part of 2020, there were fewer FITs completed in 2020 compared with 2019. In 2019, 614,051 FITs were completed in total (mean ± SD: 51,171 ± 15,260 FITs completed/month), and monthly FIT completion numbers ranged from a high of 76,152 in March 2019, followed by a monthly decline to a low of 21,438 in December 2019 (Figure 1 and Supplementary Table 2). In 2020, 558,810 FITs were completed in total (mean ± SD: 46,568 ± 19,150 FITs completed/month), a 9.0% reduction from 2019; this included a sharp decline in completed tests in April and May 2020, a ramping up in June 2020, and then numbers that were higher in July through December 2020 compared with those same months in 2019. Overall, in 2019, 73.8% of FITs offered were completed (614,051 of 832,438), whereas in 2020, 61.8% of FITs offered were completed (558,810 of 904,547), an absolute difference of 12%. The number of positive FITs followed a similar pattern, and overall, there were 20,348 positive FITs in 2020, compared with 22,635 in 2019, a reduction of 10.1%. Overall, in 2019, 3.7% of FITs completed were positive (22,635 of 5614,057) and in 2020, 3.6% were positive (20,348 of 558,810).
Colonoscopy Utilization
In 2019, 110,594 total colonoscopies were performed (mean ± SD: 9216 ± 688 colonoscopies/month) and the monthly numbers of colonoscopies performed ranged from a low of 8125 in February to a high of 10,036 in April 2019 (Figure 2 and Supplementary Table 3).
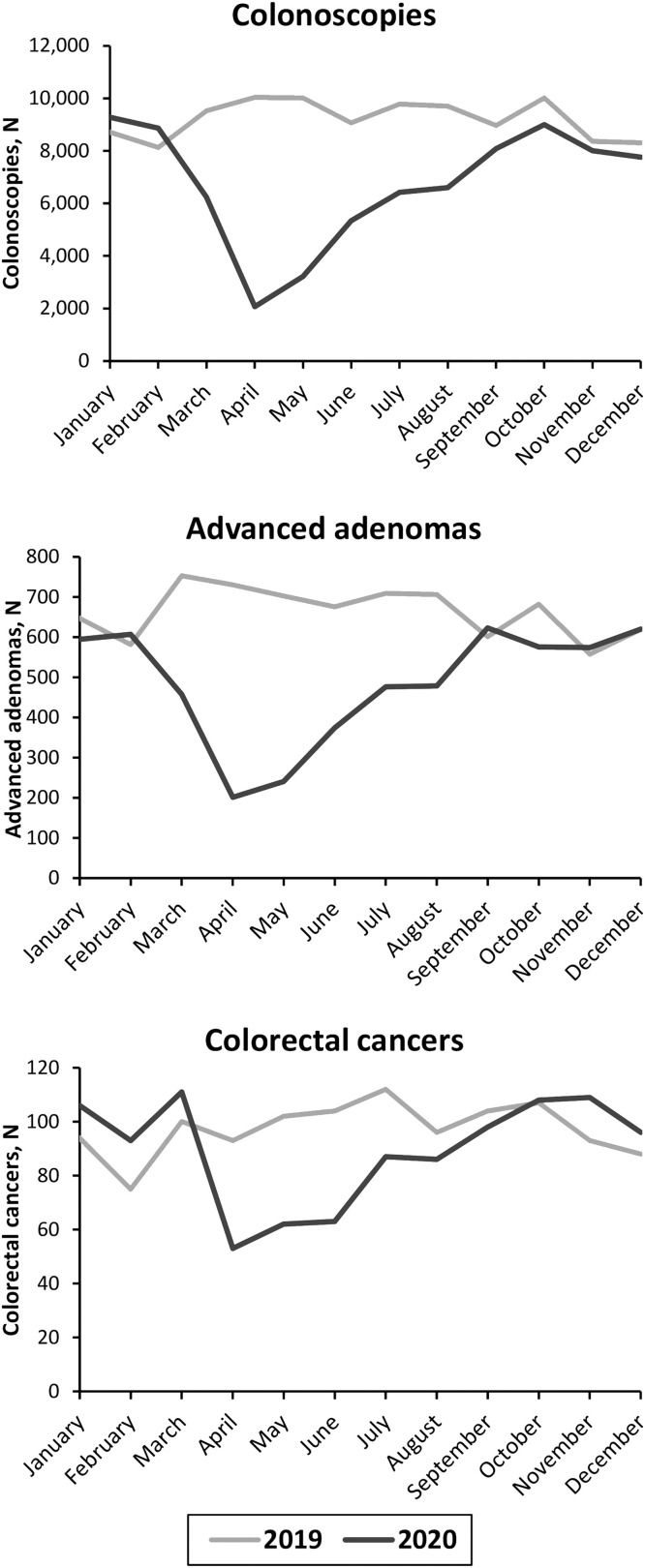
Figure 2.
The number of colonoscopies performed, advanced adenomas detected, and CRCs detected in 2019 and 2020.
In 2020, 80,863 total colonoscopies were performed (mean ± SD: 6739 ± 2180 colonoscopies/month), a 26.9% reduction from 2019, with greater monthly variability. Specifically, starting in March 2020 when the shelter-in-place order was issued, procedure volumes sharply declined and reached a low of 2068 in April 2020, representing a 79.4% decline from the 10,036 procedures performed in April 2019. There was a gradual but not full recovery in procedure volume in the months that followed. From September through December 2020, colonoscopy volumes were only 4.2% to 10.1% lower than they were for those same months in 2019.
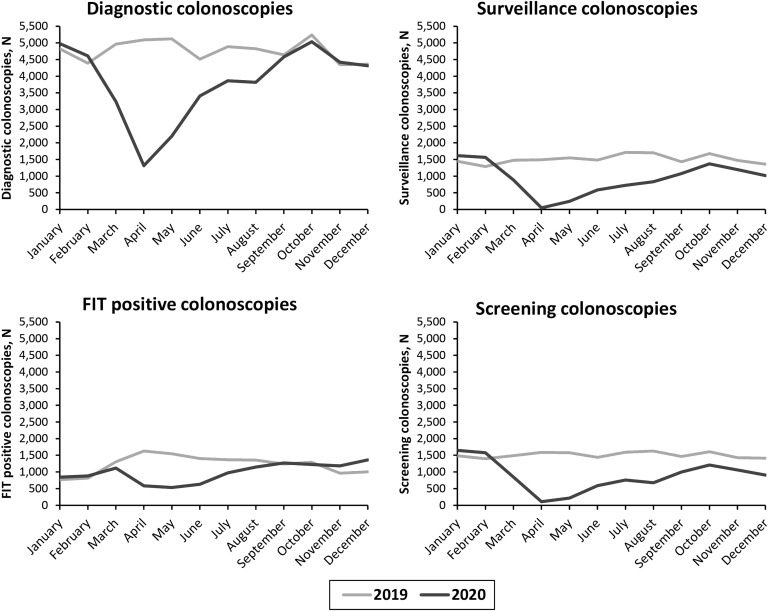
As shown in Figure 3 and Supplementary Table 4, compared with 2019, in 2020 the percentage declines in the total numbers of screening and surveillance colonoscopies performed were greater than for diagnostic and FIT-positive colonoscopies performed. Specifically, there was a 41.5% decline in screening colonoscopies (10,593 vs 18,105), a 38.3% decline in surveillance procedures (11,156 vs 18,091), a 20.0% decline in FIT-positive colonoscopies (11,748 vs 14,686), a 19.9% decline in diagnostic examinations (45,783 vs 57,191), and a 37.2% decline in procedures with an unknown indication (1583 vs 2521).
Figure 3.
The number of colonoscopies performed in 2019 and 2020 by procedure indication.
Adenoma Detection
In 2019, 51,846 individuals had at least 1 adenoma detected at colonoscopy (mean ± SD: 4321 ± 355 patients detected/month) (Supplementary Table 5). In 2020, 38,268 individuals had at least 1 adenoma detected at colonoscopy (mean ± SD: 3189 ± 1074 patients/month), a 26.2% reduction compared with the prior year, and with much greater monthly variability. Similar to the pattern seen with colonoscopy volume, starting in March 2020, the number of patients with an adenoma detected sharply declined and reached a low of 964 in April, representing a 79.1% reduction compared with the 4603 patients with an adenoma detected in April 2019. There was a gradual recovery in the total numbers of patients with adenomas detected in the months that followed, paralleling the gradual increase in procedure volume, and from September through December 2020, the numbers of individuals with an adenoma detected were just 4.8% to 8.6% lower than they were for those same months in 2019. Adenoma detection rate, defined as the percentage of all colonoscopies in which at least 1 adenoma was detected, remained stable during the study period with rates of 47% for both 2019 and 2020.
Advanced Adenoma and CRC Detection
In 2019, 8254 individuals had at least 1 advanced adenoma detected at colonoscopy (mean ± SD: 688 ± 61 patients/month) (Figure 2 and Supplementary Table 5). In 2020, 6022 individuals had an advanced adenoma detected (mean ± SD: 502 ± 143 patients/month), representing a 27.0% reduction compared with 2019, and there was much greater variability month-to-month. For example, in April 2020, there were just 209 individuals who had an advanced adenoma detected, representing a 72.2% reduction compared with the 751 individuals detected in April 2019. In subsequent months, there was a gradual recovery in the number of patients with an advanced adenoma detected at colonoscopy, and in November and December of 2020, there was little to no difference in the number of patients with an advanced adenoma compared with those same months in 2019.
In 2019, CRC was detected at colonoscopy in 1225 individuals (mean ± SD: 102 ± 10 cases/month) (Figure 2 and Supplementary Table 5). In 2020, CRC was detected at colonoscopy in 1118 individuals (mean ± SD: 93 ± 20 cases/month), an 8.7% reduction compared with the prior year and there was much greater variability in detection month-to-month. For example, in April 2020, 55 CRCs were detected, representing a 43.9% reduction compared with the 98 cases detected in April 2019. In subsequent months, there was a gradual recovery in the number of patients with CRC diagnosed by colonoscopy and in November and December, the numbers of patients were 18.8% and 4.2% higher, respectively, than those same months in 2019.
Discussion
In a large, diverse, US-based integrated health care system, there was a dramatic decline in FIT mailings in March and April 2020 when the pandemic-related shelter-in-place order was issued. Although there was a rapid recovery in FIT mailings in the latter half of 2020, there was still an overall decline in the total number of FITs completed and positive FITs. The reduction in FITs completed relative to the number mailed in 2020, as compared with 2019, suggests that patients may have been reluctant or unable to undergo screening. Total colonoscopies performed also declined in 2020 compared with 2019, and declines were greater for screening and surveillance indications compared with diagnostic and FIT-positive indications. Finally, the total numbers of CRC and advanced adenoma cases detected by colonoscopy declined in 2020 compared with 2019.
These findings expand our understanding of the COVID-19 pandemic’s impact on FIT screening and colonoscopy services both during and after the initial shelter-in-place period. In a study from Taiwan, FIT completion rate was approximately 11% lower for the period of December 2019 to April 2020 than during the corresponding period of the prior 3 years.14 A decline in the FIT completion rate of 60.6% was seen in a US-based integrated health care system during the cessation of elective endoscopies starting in March and extending into May 2020, but rates slowly recovered thereafter.15 Like the latter study, we found that FIT completion rates declined during the early months of the pandemic but recovered in the subsequent months, although overall the number of FITs completed was 9% lower in 2020 compared with 2019. Nonetheless, our findings underscore that if faced with a situation in which colonoscopy services are sharply curtailed in the future, established organized programs offering mailed FITs have the potential to ramp up quickly to help close the CRC screening gap.
Consistent with our findings, others have also reported sharp reductions in colonoscopy services due to the pandemic (Supplementary Table 6). In data from the UK National Endoscopy Database, compared with the period of January 6 to March 15, 2020, colonoscopy procedures declined 88% during the period of March 23 to May 31, 2020.16 In England, there was a 92% reduction in the number of colonoscopies performed in April 2020 compared with the monthly average in 2019, with numbers recovering by October 2020.4 In a US study of 41 health care organizations, there were 85% fewer colonoscopies performed from March 15 to July 15, 2020, compared with the same period in 2019.6 Additional consolidated data from 8 large health care organizations across 7 states (the National Cancer Institute’s Population-based Research to Optimize the Screening Process consortium, inclusive of KPNC) demonstrated that CRC screening declined by 82% in April to May 2020 compared with April to September 2019, concomitant with dramatic declines in colonoscopy utilization.17 In data from the French national health data system, there were 69% fewer colonoscopy bowel preparations dispensed (a surrogate for colonoscopies performed) early in the pandemic from March 16 to May 10, 2020, compared with the preceding 4 weeks, February 17 to March 15, 2020.7 In 15 Dutch hospitals, 45% fewer colonoscopies were performed from March 15 to June 25, 2020, compared with the same period in 2019; colonoscopy volumes started to return to pre-pandemic levels afterward, but screening colonoscopies remained low at least through June 25, 2020.5 In data from all public hospitals in Hong Kong, the average number of weekly lower endoscopy procedures declined 60% from January 21 to March 31, 2020, compared with the period of October 1, 2019, to January 20, 2020.3
When the goal of COVID-19 containment in the United States was no longer realistic, our health care system developed a mitigation program seeking to slow the spread of the virus while resuming colonoscopy services. Mitigation strategies included tailored isolation approaches to reduce COVID-19 surges, expanded COVID testing capabilities to increase hospital capacity,18 adhering to gastrointestinal multisociety recommendations for airborne precaution use for all patients,19 and adopting extended room dwell times of 45 minutes to allow adequate air exchange.20 These initial protocols required endoscopy unit operation at reduced staff and patient capacity and were followed by transition to mandated pre-procedural SARS-CoV-2 testing for all patients on rapid expansion of testing capability. Pre-procedural testing allowed normalization of room turnaround times and de-escalation of personal protective equipment to standard surgical masks,21 thereby facilitating recovery of procedural volumes to near pre-pandemic levels by the end of 2020, but also put added demands on scheduling staff and led some patients to forego procedures altogether. The resumption of colonoscopy services and near-recovery of utilization to pre-pandemic volumes was not equal across all colonoscopy indications; relative to colonoscopies performed for diagnostic and FIT-positive indications, there were greater declines in colonoscopies performed for screening and surveillance indications in 2020 compared with 2019. These were also slower to recover to pre-pandemic levels, as diagnostic and FIT-positive procedures were prioritized. As health care systems seek to understand how lessons learned and applied for fast catch up can be adopted elsewhere, additional research on cost-effectiveness and health economics studies for optimizing recovery would be informative.
Our study also highlights the impact of COVID-19 on CRC and advanced adenoma detection. The approximate 9% and 27% reductions in the number of patients diagnosed by colonoscopy with CRC and advanced adenomas in 2020 compared with 2019 supports concerns about delayed cancer and advanced adenoma diagnoses due to the pandemic. Such delays may lead to cancers being detected at more advanced stages with potential for poorer clinical outcomes. KPNC resumed colonoscopies for abnormal FIT and other indications much earlier than many health care systems, thus, impacts on clinical outcomes may be even more pronounced for systems that had multi-months of paused/decreased activities and/or more limited colonoscopy resources. Pandemic-related declines in CRC detection have been reported in studies from England and the United Kingdom,4 , 16 the United States,6 the Netherlands,5 Hong Kong,3 France,22 and Spain.23 In data from the GI Quality Improvement Consortium registry involving 451 sites in the United States and 3514 endoscopists, the average monthly volume of colonoscopies dropped by 38.5% during the first 7 months of the pandemic (March–September 2020) compared with before the pandemic (January 2019–February 2020), and 30% fewer CRCs were diagnosed compared with expected.24 During the same 7-month period in our study, 22% fewer CRCs were detected compared with the same months in 2019 and there were just 8.7% fewer CRCs detected overall in 2020 compared with 2019. It is likely that our existing organized FIT-based CRC screening program mitigated the pandemic impact somewhat by providing consistent outreach with a noninvasive at-home screening option. Further studies are needed to investigate the longer-term impact of the pandemic on trends in CRC stage at diagnosis (ie, stage shift).
Consistent with the trends observed for CRC and advanced adenomas, there was also a 26% decline in the number of adenomas detected in 2020 compared with 2019. Although the decline was greater than what was observed for CRC, adenomas typically progress slowly. However, timely resumption of screening is needed for CRC prevention efforts, as declines in CRC incidence over the past 3 decades in the United States have largely been attributed to the early detection and removal of adenomas.
This study has several strengths and limitations to consider. Strengths include reliable and timely FIT, colonoscopy, and colorectal neoplasia detection data from a large, community-based population. To our knowledge, this is the first study to demonstrate year-long trends in the numbers of FIT mailings, FIT completions, positive FITs, and colonoscopies performed by indication before and after the pandemic lockdown. Importantly, this is the first to also report colonoscopy-linked pathology findings for both adenomas and CRC. Limitations include the absence of cancer registry data to ascertain CRC cases because of a lag in reporting for 2020; however, we used a proxy method to ascertain CRC cases, which included the evaluation of pathology codes, diagnostic codes, and synoptic reporting from surgical pathology, and was highly accurate for case capture when validated against cancer registry data in previous years. The absence of cancer registry data for 2020 also prevented an examination of changes in cancer stage at diagnosis in 2020 vs 2019. Also, eligibility for FIT screening invitations widened in 2020 compared with 2019, resulting in an 8.7% increase in FIT invitations, and this could have blunted the extent of the decline in FITs completed in 2020 compared with 2019.
In conclusion, the pandemic led to fewer FIT screenings and colonoscopies in 2020 vs 2019; however, after the lifting of shelter-in-place orders, FIT screenings exceeded, and colonoscopy volumes nearly reached numbers from those same months in 2019. Overall, there was an 8.7% reduction in the number of CRC cases diagnosed by colonoscopy in 2020. These data may help inform the development of strategies for CRC screening and diagnostic testing during future national emergencies.
CRediT Authorship Contributions
Order of Authors (with Contributor Roles):
Jeffrey K. Lee, MD, MPH (Conceptualization: Lead; Formal analysis: Lead; Investigation: Lead; Methodology: Lead; Writing – original draft: Lead; Writing – review & editing: Lead)
Angela Y. Lam, MD (Formal analysis: Equal; Investigation: Equal; Writing – original draft: Lead; Writing – review & editing: Supporting)
Christopher D. Jensen, PhD, MPH (Conceptualization: Lead; Formal analysis: Lead; Funding acquisition: Lead; Investigation: Lead; Methodology: Lead; Writing – original draft: Equal; Writing – review & editing: Lead)
Amy R. Marks, MPH (Data curation: Lead; Formal analysis: Lead; Investigation: Equal; Methodology: Equal; Writing – review & editing: Equal)
Jessica Badalov, MS (Project administration: Lead; Writing – review & editing: Equal)
Evan Layefsky, BS (Project administration: Supporting; Writing – review & editing: Equal)
Kevin Kao, MD (Writing – review & editing: Equal)
Ngoc J. Ho, PhD (Writing – review & editing: Equal)
Joanne E. Schottinger, MD (Writing – review & editing: Equal)
Nirupa R. Ghai, PhD (Writing – review & editing: Equal)
Cheryl M. Carlson, MPH (Writing – review & editing: Equal)
Ethan A. Halm, MD (Writing – review & editing: Equal)
Beverly Green, MD (Writing – review & editing: Equal)
Dan Li, MD (Writing – review & editing: Equal)
Douglas A. Corley, MD, PhD (Writing – review & editing: Equal)
Theodore R. Levin, MD (Conceptualization: Lead; Formal analysis: Lead; Funding acquisition: Lead; Investigation: Lead; Methodology: Lead; Writing – review & editing: Lead)
Footnotes
Conflicts of interest The authors disclose no conflicts.
Funding This study received grant support from the National Cancer Institute (K07CA212057), Population-based Research to Optimize the Screening Process II (PROSPR II) consortium (UM1 CA222035), and the Garfield Foundation.
Note: To access the supplementary material accompanying this article, visit the online version of Gastroenterology at www.gastrojournal.org, and at https://doi.org/10.1053/j.gastro.2022.05.014.
Supplementary Material
Supplementary Table 1.
Indications for Colonoscopy by Age Group in 2019 and 2020
| 2019 n (%) |
2020 n (%) |
|
|---|---|---|
| Age 18 to 44 years | ||
| Screening | 1279 (11.5) | 1036 (10.7) |
| Surveillance | 338 (3.0) | 275 (2.8) |
| FIT positive | 17 (0.2) | 10 (0.1) |
| Diagnostic | 9208 (82.9) | 8115 (83.9) |
| Unknown | 264 (2.4) | 241 (2.5) |
| Total | 11,106 (100) | 9,677 (100) |
| Age 45 to 75 years | ||
| Screening | 16,102 (18.0) | 9108 (14.3) |
| Surveillance | 15,589 (17.4) | 9519 (14.9) |
| FIT positive | 14,532 (16.2) | 11,623 (18.2) |
| Diagnostic | 41,105 (45.9) | 32,144 (50.5) |
| Unknown | 2207 (2.5) | 1315 (2.1) |
| Total | 89,535 (100) | 63,709 (100) |
| Age 76 to 89 years | ||
| Screening | 724 (7.3) | 449 (6.0) |
| Surveillance | 2164 (21.7) | 1362 (18.2) |
| FIT positive | 137 (1.4) | 115 (1.5) |
| Diagnostic | 6878 (69.1) | 5524 (73.9) |
| Unknown | 50 (0.5) | 27 (0.4) |
| Total | 9953 (100) | 7477 (100) |
Supplementary Table 2.
The Number of Patients Who Were Mailed a FIT Kit, Completed the FIT, and Tested Positive in 2019 and 2020, and the Percentage Change in 2020 Compared With 2019
| Month | FIT mailed |
FIT results |
FIT positive |
||||||
|---|---|---|---|---|---|---|---|---|---|
| 2019 | 2020 | % Change | 2019 | 2020 | % Change | 2019 | 2020 | % Change | |
| January | 63,434 | 67,697 | 6.7 | 29,441 | 31,315 | 6.4 | 1185 | 1395 | 17.7 |
| February | 79,136 | 87,090 | 10.1 | 48,848 | 59,866 | 22.6 | 1866 | 2203 | 18.1 |
| March | 81,213 | 43,565 | −46.4 | 76,152 | 50,273 | −34.0 | 2611 | 1848 | −29.2 |
| April | 91,082 | 0 | −100.0 | 67,998 | 8,172 | −88.0 | 2416 | 370 | −84.7 |
| May | 90,932 | 36,806 | −59.5 | 64,174 | 7,998 | −87.5 | 2390 | 331 | −86.2 |
| June | 71,227 | 98,801 | 38.7 | 55,283 | 46,029 | −16.7 | 1943 | 1484 | −23.6 |
| July | 95,529 | 92,160 | −3.5 | 57,939 | 59,791 | 3.2 | 2019 | 1990 | −1.4 |
| August | 85,317 | 94,952 | 11.3 | 59,282 | 64,595 | 9.0 | 2138 | 2008 | −6.1 |
| September | 51,418 | 98,763 | 92.1 | 50,298 | 58,717 | 16.7 | 1777 | 2010 | 13.1 |
| October | 82,378 | 101,931 | 23.7 | 46,291 | 59,348 | 28.2 | 1730 | 2185 | 26.3 |
| November | 21,547 | 95,796 | 344.6 | 36,907 | 58,914 | 59.6 | 1542 | 2151 | 39.5 |
| December | 19,225 | 86,986 | 352.5 | 21,438 | 53,792 | 150.9 | 1018 | 2373 | 133.1 |
| Total | 832,438 | 904,547 | 8.7 | 614,051 | 558,810 | −9.0 | 22,635 | 20,348 | −10.1 |
| Mean | 69,370 | 75,379 | 51,171 | 46,568 | 1886 | 1696 | |||
| SD | 24,904 | 30,815 | 15,260 | 19,150 | 461 | 660 | |||
Supplementary Table 3.
The Number of Colonoscopies Performed in 2019 and 2020, and the Percentage Change in 2020 Compared With 2019
| 2019 (n) | 2020 (n) | Change (%) | |
|---|---|---|---|
| January | 8712 | 9275 | 6.5 |
| February | 8125 | 8860 | 9.0 |
| March | 9518 | 6240 | −34.4 |
| April | 10,036 | 2068 | −79.4 |
| May | 10,015 | 3220 | −67.8 |
| June | 9064 | 5333 | −41.2 |
| July | 9780 | 6416 | −34.4 |
| August | 9700 | 6604 | −31.9 |
| September | 8967 | 8080 | −9.9 |
| October | 10,010 | 9001 | −10.1 |
| November | 8364 | 8009 | −4.2 |
| December | 8303 | 7757 | −6.6 |
| Total | 110,594 | 80,863 | −26.9 |
| Mean | 9216 | 6739 | |
| SD | 688 | 2180 |
Supplementary Table 4.
The Number of Colonoscopies Performed in 2019 and 2020 by Procedure Indication, and the Percentage Change in 2020 Compared With 2019
| Screening |
Surveillance |
Diagnostic |
FIT positive |
Unknown |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2019 (n) | 2020 (n) | Change (%) | 2019 (n) | 2020 (n) | Change (%) | 2019 (n) | 2020 (n) | Change (%) | 2019 (n) | 2020 (n) | Change (%) | 2019 (n) | 2020 (n) | Change (%) | |
| January | 1483 | 1648 | 11.1 | 1445 | 1616 | 11.8 | 4821 | 4981 | 3.3 | 770 | 844 | 9.6 | 193 | 186 | −3.6 |
| February | 1396 | 1579 | 13.1 | 1290 | 1567 | 21.5 | 4391 | 4609 | 5.0 | 813 | 883 | 8.6 | 235 | 222 | −5.5 |
| March | 1491 | 843 | −43.5 | 1479 | 883 | −40.3 | 4961 | 3240 | −34.7 | 1306 | 1118 | −14.4 | 281 | 156 | −44.5 |
| April | 1587 | 108 | −93.2 | 1494 | 47 | −96.9 | 5091 | 1313 | −74.2 | 1627 | 585 | −64.0 | 237 | 15 | −93.7 |
| May | 1578 | 217 | −86.2 | 1547 | 242 | −84.4 | 5122 | 2200 | −57.0 | 1545 | 530 | −65.7 | 223 | 31 | −86.1 |
| June | 1441 | 590 | −59.1 | 1484 | 586 | −60.5 | 4512 | 3409 | −24.4 | 1405 | 632 | −55.0 | 222 | 116 | −47.7 |
| July | 1592 | 759 | −52.3 | 1715 | 727 | −57.6 | 4887 | 3863 | −21.0 | 1367 | 972 | −28.9 | 219 | 95 | −56.6 |
| August | 1628 | 675 | −58.5 | 1701 | 832 | −51.1 | 4825 | 3819 | −20.8 | 1359 | 1147 | −15.6 | 187 | 131 | −29.9 |
| September | 1464 | 1000 | −31.7 | 1430 | 1076 | −24.8 | 4640 | 4578 | −1.3 | 1241 | 1268 | 2.2 | 192 | 158 | −17.7 |
| October | 1606 | 1206 | −24.9 | 1676 | 1369 | −18.3 | 5240 | 5037 | −3.9 | 1292 | 1225 | −5.2 | 196 | 164 | −16.3 |
| November | 1427 | 1060 | −25.7 | 1472 | 1195 | −18.8 | 4342 | 4420 | 1.8 | 960 | 1181 | 23.0 | 163 | 153 | −6.1 |
| December | 1412 | 908 | −35.7 | 1358 | 1016 | −25.2 | 4359 | 4314 | −1.0 | 1001 | 1363 | 36.2 | 173 | 156 | −9.8 |
| Total | 18,105 | 10,593 | −41.5 | 18,091 | 11,156 | −38.3 | 57,191 | 45,783 | −19.9 | 14,686 | 11,748 | −20.0 | 2521 | 1583 | −37.2 |
| Mean | 1509 | 883 | 1508 | 930 | 4766 | 3815 | 1224 | 979 | 210 | 132 | |||||
| SD | 81 | 448 | 127 | 465 | 300 | 1082 | 265 | 272 | 31 | 58 | |||||
Supplementary Table 5.
The Number of Patients With Any Adenoma, Advanced Adenoma, CRC, or Advanced Neoplasia (Advanced Adenoma or CRC) Detected by Colonoscopy in 2019 and 2020, and the Percentage Change in 2020 Compared With 2019
| Adenoma |
Advanced adenoma |
CRC |
Advanced neoplasia |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2019 (n) | 2020 (n) | Change (%) | 2019 (n) | 2020 (n) | Change (%) | 2019 (n) | 2020 (n) | Change (%) | 2019 (n) | 2020 (n) | Change (%) | |
| January | 3912 | 4493 | 14.9 | 661 | 595 | −10.0 | 95 | 109 | 14.7 | 733 | 669 | −8.7 |
| February | 3778 | 4293 | 13.6 | 592 | 614 | 3.7 | 80 | 97 | 21.3 | 650 | 683 | 5.1 |
| March | 4461 | 3082 | −30.9 | 768 | 470 | −38.8 | 103 | 116 | 12.6 | 838 | 558 | −33.4 |
| April | 4603 | 964 | −79.1 | 751 | 209 | −72.2 | 98 | 55 | −43.9 | 817 | 251 | −69.3 |
| May | 4776 | 1403 | −70.6 | 734 | 254 | −65.4 | 108 | 63 | −41.7 | 812 | 306 | −62.3 |
| June | 4366 | 2403 | −45.0 | 702 | 389 | −44.6 | 109 | 67 | −38.5 | 780 | 443 | −43.2 |
| July | 4662 | 2982 | −36.0 | 749 | 502 | −33.0 | 118 | 91 | −22.9 | 833 | 568 | −31.8 |
| August | 4682 | 3142 | −32.9 | 734 | 492 | −33.0 | 103 | 91 | −11.7 | 807 | 561 | −30.5 |
| September | 4118 | 3880 | −5.8 | 624 | 659 | 5.6 | 108 | 102 | −5.6 | 698 | 735 | 5.3 |
| October | 4663 | 4264 | −8.6 | 707 | 596 | −15.7 | 112 | 114 | 1.8 | 785 | 690 | −12.1 |
| November | 3961 | 3682 | −7.0 | 587 | 600 | 2.2 | 96 | 114 | 18.8 | 662 | 683 | 3.2 |
| December | 3864 | 3680 | −4.8 | 645 | 642 | −0.5 | 95 | 99 | 4.2 | 721 | 713 | −1.1 |
| Total | 51,846 | 38,268 | −26.2 | 8254 | 6022 | −27.0 | 1225 | 1118 | −8.7 | 9136 | 6860 | −24.9 |
| Mean | 4321 | 3189 | 688 | 502 | 102 | 93 | 761 | 572 | ||||
| SD | 355 | 1074 | 61 | 143 | 10 | 20 | 63 | 154 | ||||
Supplementary Table 6.
Summary of International Studies Evaluating the Impact of the COVID-19 Pandemic on Colonoscopy and CRC Screening Services
| Setting, Database | Service studied | Pre-pandemic timeframe | Pandemic timeframe | Percent reductions during pandemic |
|---|---|---|---|---|
| United Kingdom, National Endoscopy Database16 | Average weekly colonoscopies | January 6–March 15, 2020 | March 23–May 31, 2020 | 88% |
| England, National Health Service4 | Average monthly colonoscopies | April 1–April 30, 2019 | April 1–April 30, 2020 | 92% |
| United States, TriNetX Database6 | Number of colonoscopies | March 15–July 15, 2019 | March 15–July 15, 2020 | 85% |
| United States, PROSPR Consortium17 | Colorectal cancer screening through FIT and colonoscopy | April 1–September 30, 2019 | April 1–May 31, 2020 | 82% |
| France, Système National des Données de Santé7 | Colonoscopy bowel preparation dispenses | February 17–March 15, 2020 | March 16–May 10, 2020 | 69% |
| Netherlands, Trans.IT Endoscopy Database5 | Number of colonoscopies | March 15–June 25, 2019 | March 15–June 25, 2020 | 45% |
| Hong Kong, Hong Kong Hospital Authority3 | Average weekly colonoscopies | October 1, 2016–January 20, 2020 | January 28–March 31, 2020 | 60% |
References
- 1.Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Medicare & Medicaid Services Non-emergent, elective medical services, and treatment recommendations. https://www.cdc.gov/coronavirus/2019-ncov/healthcare-facilities/index.html Available at: Accessed December 4, 2021.
- 3.Lui T.K., Leung K., Guo C.-G., et al. Impacts of COVID-19 pandemic on gastrointestinal endoscopy volume and diagnosis of gastric and colorectal cancers: a population-based study. Gastroenterology. 2020;159:1164–1166.e3. doi: 10.1053/j.gastro.2020.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morris E., Goldacre R., Spata E., et al. Impact of the COVID-19 pandemic on the detection and management of colorectal cancer in England: a population-based study. Lancet Gastroenterol Hepatol. 2021;6:199–208. doi: 10.1016/S2468-1253(21)00005-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lantinga M., Theunissen F., Borg P Ter, et al. Impact of the COVID-19 pandemic on gastrointestinal endoscopy in the Netherlands: analysis of a prospective endoscopy database. Endoscopy. 2021;53:166–170. doi: 10.1055/a-1272-3788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khan A., Bilal M., Morrow V., et al. Impact of the coronavirus disease 2019 pandemic on gastrointestinal procedures and cancers in the United States: a multicenter research network study. Gastroenterology. 2021;160:2602–2604.e5. doi: 10.1053/j.gastro.2021.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Meyer A., Drouin J., Zureik M., et al. Colonoscopy in France during the COVID-19 pandemic. Int J Colorectal Dis. 2021;36:1073–1075. doi: 10.1007/s00384-020-03816-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sharpless N.E. COVID-19 and cancer. Science. 2020;368:1290. doi: 10.1126/science.abd3377. [DOI] [PubMed] [Google Scholar]
- 9.Carethers J.M., Sengupta R., Blakey R., et al. Disparities in cancer prevention in the COVID-19 era. Cancer Prev Res. 2020;13:893–896. doi: 10.1158/1940-6207.CAPR-20-0447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gordon N.P. 2020. Similarity of adult Kaiser Permanente members to the adult population in Kaiser Permanente’s Northern California service area: comparisons based on the 2017/2018 cycle of the California Health Interview Survey. Oakland. Available at: https://divisionofresearch.kaiserpermanente.org/projects/memberhealthsurvey/SiteCollectionDocuments/compare_kp_ncal_chis2017-18.pdf. Accessed December 20, 2021. [Google Scholar]
- 11.American Community Survey Summary File. https://www.census.gov/programs-surveys/acs/data/summary-file.2019.html Available at: Accessed November 15, 2021.
- 12.Burnett-Hartman A.N., Kamineni A., Corley D.A., et al. Colonoscopy indication algorithm performance across diverse health care systems in the PROSPR Consortium. EGEMS (Wash DC) 2019;7:37. doi: 10.5334/egems.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee J.K., Jensen C.D., Levin T.R., et al. Long-term risk of colorectal cancer and related death after adenoma removal in a large, community-based population. Gastroenterology. 2020;158:884–894.e5. doi: 10.1053/j.gastro.2019.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cheng S.Y., Chen C.F., He H.C., et al. Impact of COVID-19 pandemic on fecal immunochemical test screening uptake and compliance to diagnostic colonoscopy. J Gastroenterol Hepatol. 2021;36:1614–1619. doi: 10.1111/jgh.15325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Myint A., Roh L., Yang L., et al. Noninvasive colorectal cancer screening tests help close screening gaps during Coronavirus Disease 2019 pandemic. Gastroenterology. 2021;161:712–714.e1. doi: 10.1053/j.gastro.2021.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rutter M.D., Brookes M., Lee T.J., et al. Impact of the COVID-19 pandemic on UK endoscopic activity and cancer detection: a National Endoscopy Database Analysis. Gut. 2021;70:537–543. doi: 10.1136/gutjnl-2020-322179. [DOI] [PubMed] [Google Scholar]
- 17.Corley D.A., Sedki M., Ritzwoller D.P., et al. Cancer screening during COVID-19: a perspective from NCI’s PROSPR consortium. Gastroenterology. 2021;160:999–1002. doi: 10.1053/j.gastro.2020.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Parodi S.M., Liu V.X. From containment to mitigation of COVID-19 in the US. JAMA. 2020;323:1441–1442. doi: 10.1001/jama.2020.3882. [DOI] [PubMed] [Google Scholar]
- 19.Sultan S., Lim J.K., Altayar O., et al. AGA rapid recommendations for gastrointestinal procedures during the COVID-19 pandemic. Gastroenterology. 2020;159:739. doi: 10.1053/j.gastro.2020.03.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rouillard S., Liu V.X., Corley D.A. COVID-19 and long-term planning for procedure-based specialties during extended mitigation and suppression strategies. Gastroenterology. 2021;160:4. doi: 10.1053/j.gastro.2020.05.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sultan S., Siddique S.M., Altayar O., et al. AGA Institute rapid review and recommendations on the role of pre-procedure SARS-CoV-2 testing and endoscopy. Gastroenterology. 2020;159:1935. doi: 10.1053/j.gastro.2020.07.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Priou S., Lamé G., Chatellier G., et al. Effect of the COVID-19 pandemic on colorectal cancer care in France. Lancet Gastroenterol Hepatol. 2021;6:342–343. doi: 10.1016/S2468-1253(21)00095-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ruiz-Medina S., Gil S., Jimenez B., et al. Significant decrease in annual cancer diagnoses in spain during the covid-19 pandemic: a real-data study. Cancers (Basel) 2021;13:3215. doi: 10.3390/cancers13133215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Calderwood A.H., Calderwood M.S., Williams J.L., et al. Impact of the COVID-19 pandemic on utilization of EGD and colonoscopy in the United States: an analysis of the GIQuIC Registry. Tech Innov Gastrointest Endosc. 2021;23:313–321. doi: 10.1016/j.tige.2021.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]