Abstract
Objectives:
To examine the associations of various sedentary behaviors (SB) to health-related quality of life (HRQOL) and the possible mediating role of sleep quality in these relationships.
Methods:
Participants were 363 middle-aged adults (Mage = 44.25, SD = 4.72, 64% male) from Amazon MTurk. Self-reported measures of socio-demographic status, time spent doing 10 different types of SB, sleep quality, and HRQOL were collected. Exploratory factor analysis was used to classify SB. Mediation analysis with PROCESS for SPPS examined the mediational paths.
Results:
Exploratory factor analysis categorized 10 sedentary activities into Common Engaging SB, High Engaging/Leisure SB, and Less Engaging/Passive SB. Findings suggested that Common Engaging SB was negatively associated with HRQOL, whereas High Engaging/Leisure SB was positively related to HRQOL. Sleep quality appeared to mediate the associations of Common Engaging SB and High Engaging/Leisure SB to HRQOL.
Conclusions:
Reducing sitting time, particularly Common Engaging SB, could be a useful strategy to improve HRQOL. Health promotion programs should support mentally engaging leisure activities because such activities might increase middle-aged adults’ HRQOL. Additionally, health promotion programs are needed to raise public awareness regarding the importance of sleep quality.
Keywords: sedentary behaviors, sitting time, quality of life, sleep quality
Health-related quality of life (HRQOL), an individual’s perception of physical capability, psychological problems, and broader general health, has been increasingly recognized as an important indicator of health status.1 Poor HRQOL is associated with future adverse health status, such as hospitalization and mortality.2,3 Sedentary behaviors (SB) have emerged as a risk factor for poor HRQOL.4 SB may be defined as sitting or reclining with low energy expenditure ranging from 1.0 to 1.5 basal metabolic rate.5 Most studies examined SB and HRQOL in older populations or people with chronic diseases.6–9 Limited research investigated the association of SB with HRQOL among general middle-aged Americans. Lifestyle information from middle-aged adults is critical, as health behaviors developed earlier in life significantly impact future health status.10,11
It has been reported that prolonged SB are related to adverse health outcomes.12–15 Some researchers found that time spent watching TV was strongly associated with poor mental well-being,16 low HRQOL,17 increased risk of type 2 diabetes, cardiovascular disease, and all-cause mortality.18 Additionally, time spent in the car was related to weight gain and a more-adverse clustered cardiometabolic risk.19,20
The evidence is not uniform, however, and other studies have suggested that particular SB have beneficial effects on individuals’ well-being.21–25 For example, a longitudinal study that followed over 3,600 participants in the nationally representative Health and Retirement Study revealed that a 20% reduction in mortality was observed for those who read books while sitting compared to those who did not read books.21 A cross-sectional study found more time spent listening to the radio or music and using a computer were associated with lower odds of having a mood disorder among middle-aged and older adults.22 Other research found a positive association between computer use, particularly Internet use, and well-being,23,24 suggesting that computer use could enhance HRQOL by providing social support and better life satisfaction. In light of these findings, health outcomes might not be equivalent across different SB types; thus, it is essential to examine the associations between different types of SB and health.
Poor sleep quality is another factor that might be closely associated with lower levels of HRQOL.26–28 A cross-sectional study indicated that a diary-based measure of sleep quality correlated with physical and mental HRQOL among older adults.26 Another study that examined sleep quality and HRQOL in people with chronic illness found that poor sleep quality was associated with impaired HRQOL.27 A recent study of 14,571 adults in Australia reported that those with poor sleep quality also reported poor physical, emotional, and social functioning compared to good-quality sleepers.28 While HRQOL has been increasingly acknowledged as an important health outcome measure, limited studies have focused on sleep quality and HRQOL among healthy middle-aged adults in the United States.
Evidence supports the idea that SB could influence sleep quality. For instance, research has indicated that screen time can adversely affect sleep quality.29 Similarly, a community-based longitudinal study of 3,914 adults aged 30 and older found that individuals who watched 2 or more hours of TV per day found themselves at higher risk for problems falling asleep, middle-of-the-night awakening, and waking early with inability to sleep again.30 Further, longer sitting time was associated with worse sleep quality in women with chronic illness.31 Given the evidence that SB are associated with health, sleep quality might be a potential mediator in the relationship between different types of SB and HRQOL. However, the meditational role of sleep quality in this link has not been explored in general middle-aged Americans.
Although some research suggests that SB have harmful effects on health, the nature of the relationship between SB and HRQOL has not yet been sufficiently investigated. Presently, studies have examined the relationship between SB and HRQOL, but most have focused on older adults7,8,23,24 or people with chronic illness.6,9 Limited research has been conducted on the relationship between SB and its effects on HRQOL in general middle-aged populations. Better knowledge of these associations is needed to understand how best to promote health through lifestyle approaches in middle-aged adults. Sleep quality also plays a critical role in both physical and mental health. Yet little is known about the effects of different types of SB on sleep quality and how such effects could, in turn, affect middle-aged adults’ HRQOL. Building on previous research and addressing current literature gaps, the purpose of this study was to examine the associations of different types of SB to HRQOL in middle-aged adults residing in the United States. Additionally, the study investigated whether sleep quality mediates these relationships.
METHODS
Design
A cross-sectional online survey study was conducted. The recruitment period occurred between June 19, 2019 and July 21, 2019. The current study was approved by the Institutional Research Board of The University of Texas at Austin. It followed standard ethical procedures.
Sample
Participants aged 40 and older were recruited from Amazon’s Mechanical Turk (MTurk, http://www.mturk.com) participant database. MTurk is an online crowdsourcing marketplace for recruiting and collecting surveys data online. This database provides a diverse participant pool, often resulting in quality data.32,33 We collected and checked each participant’s unique “Worker ID” to prevent the same individuals from completing our quesiotnnaire more than once. After participants selected the study and read a brief description of the study on MTurk, a link was provided to the Qualtrics survey. Individuals provided informed consent by electronically indicating that they agreed to participate in the study. To determine eligibility, MTurk participants who were interested in the study completed a 3 pre-secreening questions as part of a linked survey on Qualtrics. The questions posed were: 1) Are you at least 40 years old?; 2) Can you read English?; and 3) Do you currently reside in the United States? Participants received 50¢ for survey completion. Four hundred respondents agreed to participate and completed the survey. Because this study focused on middle-aged participants, those aged above 61 years were removed (n = 37), leaving 363 middle-aged adults.
Measures
The following valid and reliable instruments were used in the study, the RAND Survey Short Form-36 (RAND SF-36), the Sedentary Behaviors Questionnaire, and the Pittsburgh Sleep Quality Index, to collect data on the variables of HRQOL, sedentary behaviors, and sleep quality in this study. Demographic information was also requested and included in the surveys.
Health-related quality of life (HRQOL).
The RAND SF-36 questionnaire assessed participants’ HRQOL over 4 weeks. Its validity and internal consistency have been established.34,35 The questionnaire contains 36 items scored to measure HRQOL’s 8 domains relating to both physical and mental health. The physical functioning, role limitations due to physical health, bodily pain, and general health domains comprised HRQOL’s physical component (Cronbach’s α for the present sample = 0.81). The vitality, social functioning, role limitations due to emotional health, and mental health domains comprised HRQOL’s mental component (Cronbach’s α = 0.75). Both physical and mental components scores ranged from 0 – 100; higher scores indicated a better HRQOL.36
Sedentary behaviors.
Self-reported SB were assessed using a modified version of the Sedentary Behavior Questionnaire for adults; its validity and reliability have been reported.37 Participants separately reported time spent in hours doing 10 different types of SB on a typical weekday and weekend. The SB consist of (1) watching TV, (2) playing computer games, (3) listening to music, (4) sitting and talking on the phone, (5) doing paperwork or computer work, (6) sitting reading a book or magazine, (7) playing a musical instrument, (8) sitting and driving in a car, (9) social chatting, (10) and doing hobbies.37,38 The last 2 SB items, social chatting and doing hobbies, were adapted from a previous leisure time sitting measurement developed for the general adult population.38 To obtain weekly SB for each measure, weekday hours were multiplied by 5 and weekend hours were multiplied by 2, then summed for total weekly hours (Cronbach’s α = 0.88).
Sleep quality.
Sleep quality was assessed using the validated and reliable Pittsburgh Sleep Quality Index (PSQI).39 This 19-item self-administered questionnaire assesses sleep quality and disturbances over a one-month interval. Responses to each item range from 0 (best) to 3 (worst). Seven sub-scores on a 0–3 scale were calculated. A sum of the 7 component scores yielded a global PSQI score ranging from 0–21. A higher score indicated poorer sleep quality40 (Cronbach’s α = 0.61).
Covariates.
Age, sex, race/ethnicity, education level, marital status, household income, and height/weight (for calculating BMI) have been found to be associated with HRQOL.41–45 These socio-demographic variables were controlled for in the mediational analyses. Health behavior factors controlled in the study, including physical activity and smoking status. Physical activity was assessed using the validated and widely-used International Physical Activity Questionnaire (IPAQ-short).46 Smoking status, which is associated with HRQOL and sleep quality, was also controlled in the analyses.42
Data Analysis
Preliminary analyses included descriptive statistics and Pearson product-moment correlation analyses. An exploratory factor analysis (EFA) with varimax rotation examined subgroups of the 10 different SB types using SPSS to determine the best representation of the 10 types of SB. Mediation analysis with PROCESS47 version 3.1.4 for SPPS examined the mediational paths. The bootstrapping method was used to examine mediation. This does not require the assumption of normality of the sampling distribution. Following Hughes and Lachman,48 when examining each type of SB with HRQOL, other SB were entered as covariates. The statistical significance of each indirect effect was examined and considered signigicant when the bias corrected and accelerated confidence intervals did not include zero. Statistical significance is set at alpha < .05.
RESULTS
Table 1 describes this study’s main characteristics of interest. Amazon Mechanical Turk provided a total sample of 363 middle-aged adults (Mage = 44.25, SD = 4.72, 64% male). Table 2 shows Pearson correlations among the 10 different SB types.
Table 1.
Sample Characteristics (N = 363)
| n (%) | Range | Mean | SD | |
|---|---|---|---|---|
| Socio-demographic variables | ||||
| Age, years | − | 40−60 | 44.25 | 4.72 |
| Sex | ||||
| Male | 232 (63.9) | |||
| Female | 131 (36.1) | |||
| Race/ethnicity | ||||
| White | 184 (50.7) | |||
| African American | 62 (17.1) | |||
| Hispanic | 27 (7.4) | |||
| Asian and others | 90 (24.8) | |||
| Education | ||||
| Associate degree or less | 75 (20.7) | |||
| Bachelor’s degree or higher | 288 (79.3) | |||
| Marital status | ||||
| Not married | 90 (24.8) | |||
| Married | 273 (75.2) | |||
| Household income levels | ||||
| < $50,000 | 174 (47.9) | |||
| ≥ $50,000 | 189 (52.1) | |||
| Obesity | ||||
| Not-obese | 328 (90.4) | |||
| Obese | 35 (9.6) | |||
| Physical activity levels | ||||
| < 600 MET | 27 (7.4) | |||
| 600–2999 MET | 148 (40.8) | |||
| ≥ 3000 MET | 104 (28.7) | |||
| Current smoking status | ||||
| Non-smokers | 92 (25.3) | |||
| aIntermittent smokers | 255 (70.2) | |||
| Daily smokers | 16 (4.4) | |||
| Sedentary behaviors (hours/week) | ||||
| Common Engaging SB | 0−26.69 | 9.96 | 4.45 | |
| High Engaging/Leisure SB | 0−26.06 | 9.07 | 4.51 | |
| Less Engaging/Passive SB | 0−46.50 | 17.56 | 8.28 | |
| Sleep quality | ||||
| PSQI Global Score | 0−18 | 9.24 | 3.69 | |
| Health-related QOL | ||||
| Physical QOL | 12.50−100 | 58.26 | 20.87 | |
| Mental QOL | 3.00−100 | 55.95 | 19.67 |
Note.
SD = standard deviation; METs = metabolic equivalent tasks; SB = sedentary behavior; PSQI = Pittsburgh Sleep Quality Index; QOL = quality of life.
Intermittent smokers were defined as people who smoked between 1 to 29 days in the past month.
Table 2.
Descriptive Statistics and Pearson Correlations among 10 Sedentary Behaviors (N = 363)
| Mean (Hours/week) | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Watching television | 16.26 | 8.55 | − | |||||||||
| 2. Playing computer or video games | 10.23 | 7.33 | −0.07 | − | ||||||||
| 3. Sitting listening to music on the radio, tapes, or CDs | 11.67 | 8.16 | 0.02 | 0.14** | − | |||||||
| 4. Sitting and talking on the phone | 8.99 | 6.55 | 0.03 | 0.03 | 0.16** | − | ||||||
| 5. Doing paperwork or computer work | 18.86 | 11.38 | 0.37** | −0.09 | −0.002 | −0.01 | − | |||||
| 6. Sitting reading a book or magazine | 9.48 | 7.13 | −0.09 | 0.07 | 0.08 | 0.32** | −0.12* | − | ||||
| 7. Playing a musical instrument | 5.43 | 5.55 | −0.06 | 0.23** | 0.22** | 0.23** | −0.02 | 0.24** | − | |||
| 8. Sitting and driving in a car, bus, or train | 10.34 | 7.31 | 0.03 | 0.04 | 0.01 | 0.29** | −0.08 | 0.20** | 0.23** | − | ||
| 9. Socializing with friends or family when sitting | 11.01 | 6.73 | 0.02 | 0.02 | 0.14** | 0.20** | 0.04 | 0.19** | 0.14** | 0.11* | − | |
| 10. Doing hobbies when sitting | 8.94 | 6.67 | −0.08 | 0.16** | 0.25** | 0.20** | −0.10 | 0.13* | 0.44** | 0.12* | 0.17** | − |
p < .05.
p < .01
Note.
SD = standard deviation; SB = sedentary behavior; PSQI = Pittsburgh Sleep Quality Index; QOL = quality of life.
Two-tailed test correlation.
Exploratory factor analysis (EFA) was conducted using principle component analysis with varimax rotation on the 10 different SB types to identify underlying constructs. The EFA used several criteria. First, the Kaiser-Meyer-Olkin measure of sampling adequacy was 0.67, above the commonly-recommended value of 0.60,49 and Bartlett’s test of sphericity was significant (χ2 (45) = 355.41, p < .001). Second, the communalities were equal to or above 0.30, reaffirming that each item shared some common variance with other items. Factors with eigenvalues below one were dropped.50 The 3-factor solution, explaining 49% of the variance, was preferred based on the scree plot and eigenvalues. Items loading 0.40 or higher on a single factor were retained. Factor analysis extracted 3 SB elements: 1) Common Engaging SB; 2) High Engaging/Leisure SB; and 3) Less Engaging/Passive SB. Each factor was computed by adding all SB items that loaded on the factor and dividing by the number of SB items to yield an average score for that factor. Table 3 provides the factor loading matrix for each measure.
Table 3.
Exploratory Factor Analysis Loadings and Communalities for 10 Sedentary Behaviors (N = 363)
| Factor | SB | Common Engaging SB | High Engaging/Leisure SB | Less Engaging/Passive SB | Communalities |
|---|---|---|---|---|---|
| Common Engaging SB (Eigenvalue = 2.28) | Sitting and talking on the phone | 0.72 | 0.64 | ||
| Sitting reading a book or magazine | 0.66 | 0.37 | |||
| Sitting and driving in a car, bus, or train | 0.66 | 0.43 | |||
| Socializing with friends or family when sitting | 0.44 | 0.54 | |||
| High Engaging/Leisure SB (Eigenvalue = 1.41) | Doing hobbies when sitting | 0.69 | 0.66 | ||
| Playing a musical instrument | 0.65 | 0.48 | |||
| Sitting listening to music on the radio, tapes, or CDs | 0.64 | 0.55 | |||
| Playing computer or video games | 0.58 | 0.44 | |||
| Less Engaging/Passive SB (Eigenvalue = 1.20) | Watching television | 0.81 | 0.26 | ||
| Doing paperwork or computer work (office work, emails, paying bills, etc.) | 0.80 | 0.53 |
Note.
SB = sedentary behavior.
Bivariate correlations revealed that increased Common Engaging SB related to worse sleep quality and poor physical and mental QOL. More time spent in High Engaging/Leisure SB was associated with better mental QOL. Poor sleep quality correlated with worse physical and mental QOL. No significant associations occurred between Less Engaging/Passive SB and sleep quality, physical, or mental QOL. Table 4 shows Pearson correlations among study variables for the total sample.
Table 4.
Pearson Correlations among Sedentary Behavior Factor Scores, Sleep Quality, Health-Related Quality of Life, and Subjective Memory Function (N = 363)
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| 1. Common Engaging SB | − | |||||
| 2. High Engaging/Leisure SB |
0.28** | − | ||||
| 3. Less Engaging/Passive SB |
−0.05 | −0.09 | − | |||
| 4. Sleep QOL | 0.26** | 0.08 | 0.003 | − | ||
| 5. Physical QOL | −0.33** | −0.03 | −0.03 | −0.39** | − | |
| 6. Mental QOL | −0.27** | 0.11* | −0.06 | −0.41* | 0.83** | − |
p < .05.
p < .01
Note.
SB = sedentary behavior; QOL = quality of life.
Two-tailed test correlation.
Mediation Analyses
Age, sex, BMI, race/ethnicity, education, marital status, income, physical activity, and current smoking status were controlled in the mediation analyses. Model 1 tested whether different SB types related to physical QOL and whether sleep quality would mediate this relationship (see Figure 1). The total effect model, which does not consider the mediator’s effect, indicated that individuals reporting more Common Engaging SB reported worse physical QOL (B = −1.77, p < .001); however, more High Engaging/Leisure SB was associated with better physical QOL (B = 0.77, p < .001). Less Engaging/Passive SB was not significantly related to physical QOL (B = −0.18, p = .18). In addition, participants reporting more Common Engaging SB had worse sleep quality (B = 0.25, p < .001), and more High Engaging/Leisure SB related to better sleep quality (B = −0.17, p < .01). Worse sleep quality related to poor physical QOL (B = −1.68, p < .001). The mediation analysis indicated that sleep quality mediated the relationship between Common Engaging SB and physical QOL (indirect effect = −0.08, 95% bootstrap CI = −0.13, −0.04); the direct path between Common Engaging SB and physical QOL was also significant (B = −1.35, p < .001). The analysis supported mediation for High Engaging/Leisure SB’s effect on physical QOL (indirect effect = 0.06, 95% bootstrap CI = 0.02, 0.10). The direct path between High Engaging/Leisure SB and physical QOL was not significant (B = 0.48, p = .07). For Less Engaging/Passive SB, sleep quality was not a mediator; the direct path between Less Engaging/Passive SB and physical QOL was not significant (B = −0.16, p = .19).
Figure 1.
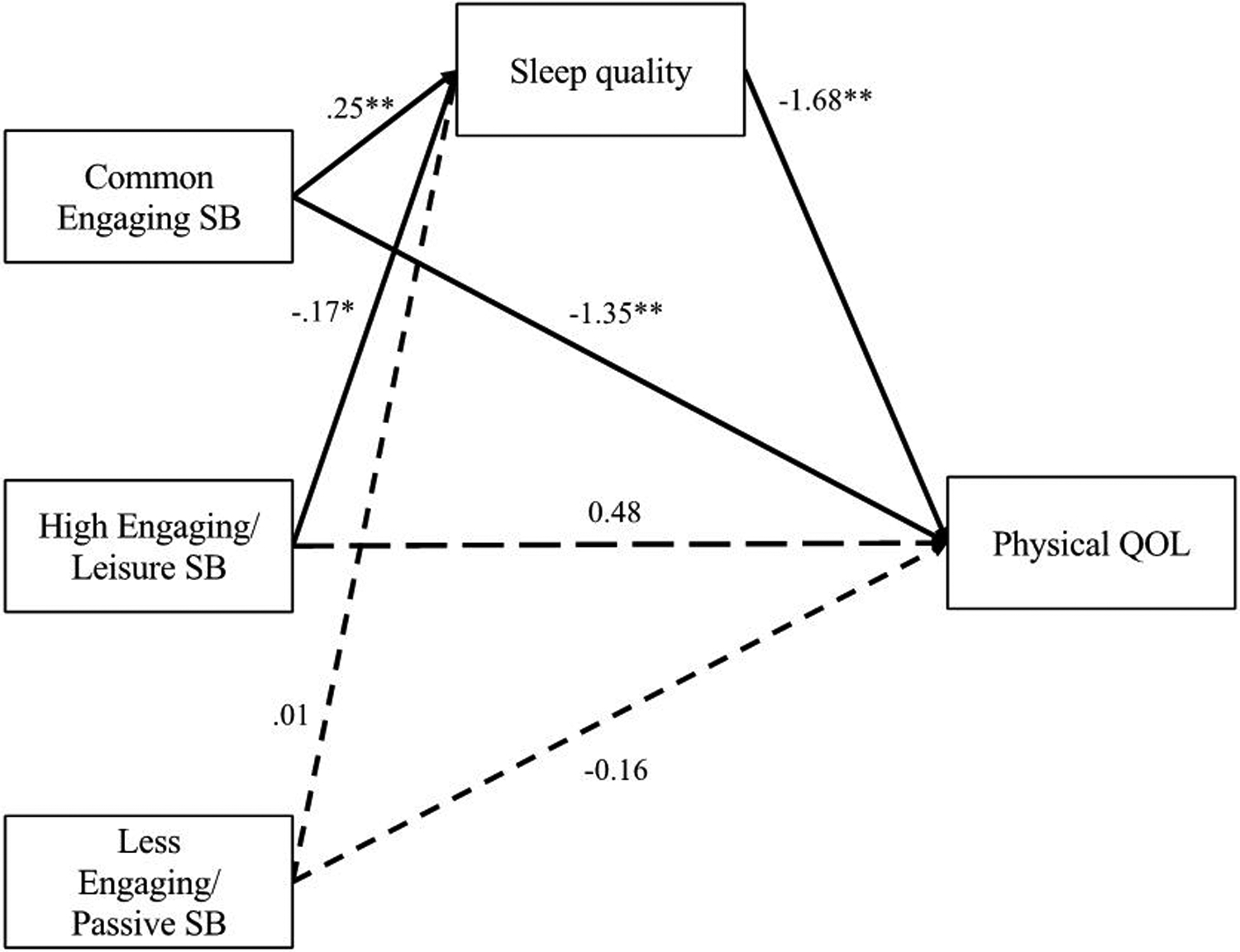
Mediational model for physical QOL
* p < .05. ** p < .001
Note.
SB = sedentary behavior; QOL = quality of life.
Unstandardized betas are included for each path. Sleep quality mediated the relationship between Common Engaging SB and physical QOL (indirect effect = −0.08, 95% bootstrap CI = −0.13, −0.04). Sleep quality mediated the relationship between High Engaging/Leisure SB and physical QOL (indirect effect = 0.06, 95% bootstrap CI = 0.02, 0.10). Black arrows indicate significant effects. Dotted black arrows indicate non-significant effects.
Model 2 tested whether different SB types were associated with mental QOL and whether sleep quality would mediate this relationship (see Figure 2). The total effect model demonstrated that higher levels of Common Engaging SB were associated with worse mental QOL (B = −1.53, p < .001); however, more High Engaging/Leisure SB related to better mental QOL (B = 1.45, p < .001). Less Engaging/Passive SB was not significantly related to mental QOL (B = −0.22, p = .08). Participants reporting more Common Engaging SB had worse sleep quality (B = 0.25, p < .001). High Engaging/Leisure SB related to better sleep quality (B = −0.17, p < .01). Worse sleep quality related to poor mental QOL (B = −1.63, p < .001). The mediation analysis indicated that sleep quality mediated the relationship between Common Engaging SB and mental QOL (indirect effect = −0.09, 95% bootstrap CI = −0.14, −0.04); the direct path between Common Engaging SB and mental QOL was also significant (B = −1.13, p < .001). The mediation results indicated that sleep quality mediated the relationship between High Engaging/Leisure SB and mental QOL (indirect effect = 0.06, 95% bootstrap CI = 0.02, 0.10). The direct path between High Engaging/Leisure SB and mental QOL was significant (B = 1.17, p < .001). For Less Engaging/Passive SB, sleep quality was not a mediator; the direct path between Less Engaging/Passive SB and mental QOL was not significant (B = −0.21, p = .08).
Figure 2.
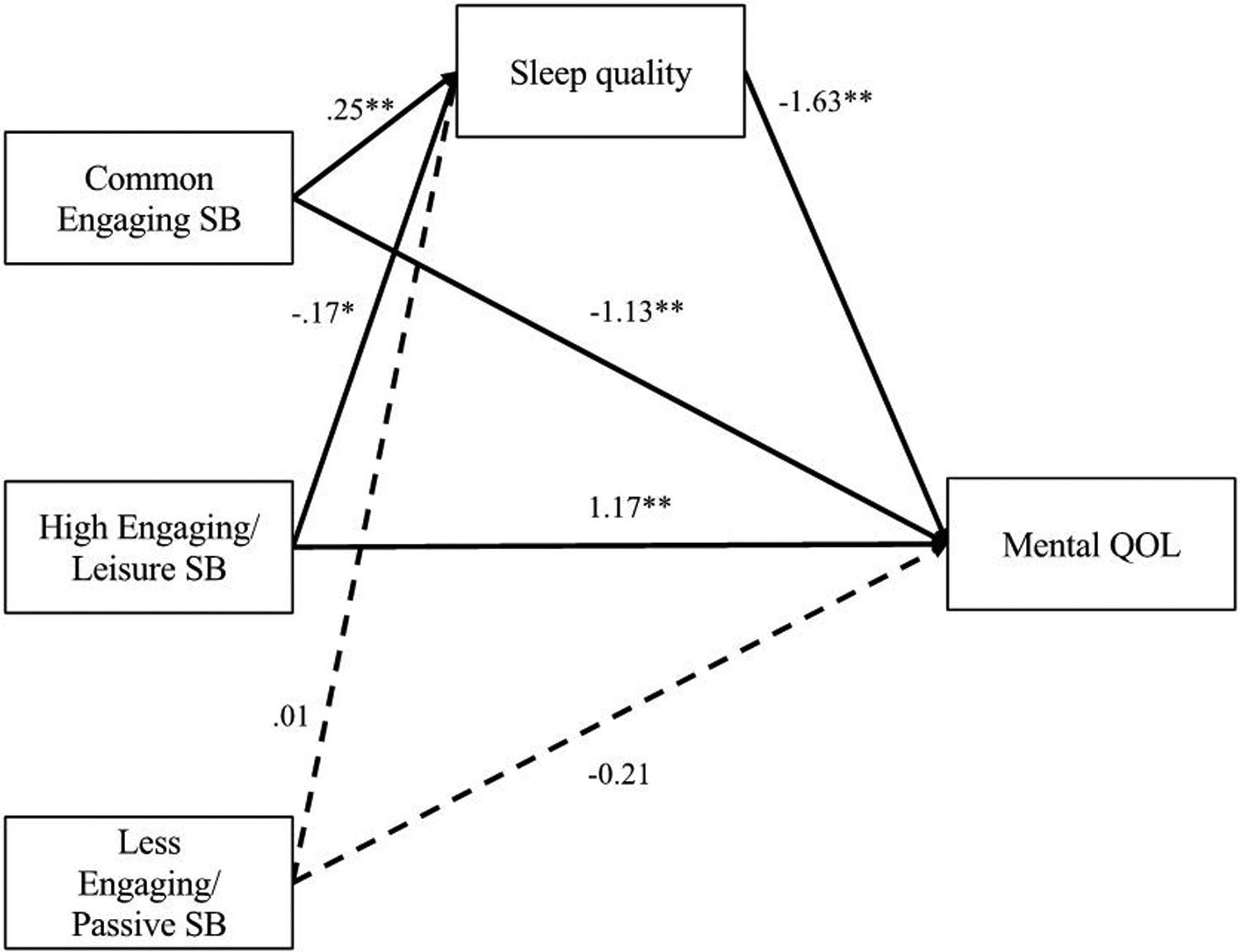
Mediational model for mental QOL
* p < .05. ** p < .001
Note.
SB = sedentary behavior; QOL = quality of life.
Unstandardized betas are included for each path. Sleep quality mediated the relationship between Common Engaging SB and mental QOL (indirect effect = −0.09, 95% bootstrap CI = −0.14, −0.04). Sleep quality mediated the relationship between High Engaging/Leisure SB and mental QOL (indirect effect = 0.06, 95% bootstrap CI = 0.02, 0.10). Black arrows indicate significant effects. Dotted black arrows indicate non-significant effects.
DISCUSSION
This study contributes to the current literature by examining how different types of SB relate to HRQOL as well as whether sleep quality mediates these relationships among middle-aged adults living in the U.S. The results indicate that middle-aged participants who spent more time in Common Engaging SB were more likely to report poor HRQOL compared to those who spent less time in Common Engaging SB. Additionally, High Engaging/Leisure SB was associated with better HRQOL. This study further found that sleep quality statistically mediated the association of both Common Engaging SB and High Engaging/Leisure SB to HRQOL.
The results of the present study indicated that higher levels of Common Engaging SB were negatively associated with both physical and mental well-being among middle-aged adults. This finding is consistent with previous research based on the analysis of overall sitting time.7,8 Prior research suggests several underlying mechanisms for the relation of prolonged SB to poor health outcomes. First, sitting for long periods might affect health through physiological mechanisms. SB involves very little energy expenditure and has been linked to metabolic dysfunction51 and reduced bone mineral density.52 Also, the amount of time spent in SB tends to replace the time spent being active, thereby preventing individuals from receiving the health benefits of healthy behaviors (eg, physical activity). Specific SB, such as time spent driving, is associated with higher BMI and more adverse markers of cardio-metabolic risk.19,20 These findings indicate that prolonged SB could negatively contribute to HRQOL, which concurs with our results. Surprisingly, social chatting was categorized under Common Engaging SB in the current study. We did not collect information regarding the types (eg, face-to-face or virtually) and content (eg, supportive, relaxing, or stressful conversations) of the chats. As a result, we cannot determine if the participants reported the same types of socializing with friends and family as previous research (ie, physically visiting others),22 which might affect our findings.
Although most studies have designated sedentary lifestyles as unhealthy behavior, the current study showed that engaging in High Engaging/Leisure SB could positively impact HRQOL. This study provided similar evidence of health benefits from certain types of SB (eg, listening to the radio or music, computer use) found in recent studies.22–24 Limited research has explicitly examined the underlying mechanisms between leisure SB and HRQOL. Potential considerations could be that High Engaging/Leisure SB promotes beneficial processes that mitigate the negative impact of SB in middle-aged adults. For example, High Engaging/Leisure SB generally includes spending time on an activity people enjoy, which might improve mental well-being. Research demonstrates that individuals who spent time on hobbies are more likely to report better physical and mental health.53–55 In addition, High Engaging/Leisure SB activities, such as listening to music, might help people cope with stress56 and feel less anxious and fatigued.57 Another explanation could be that some sedentary activities contain social stimulation or mentally-engaging activity (eg, playing video games, using a computer, playing a musical instrument). Research has shown that social engagement is associated with better physiological functioning, lower risks of physical disorders, and a longer life span.58
Another important finding of this study is that Less Engaging/Passive SB (ie, watching TV, doing paperwork or computer work) was not associated with either physical or mental HRQOL. This result contradicts previous findings, showing that prolonged TV watching was associated with poor health outcomes and lower HRQOL.16–18 One possible explanation for this contradiction could be that the current study’s participants might be younger and healthier compared to those in previous research. Studies among older adults and cancer survivors have reported mixed patterns of outcomes between TV viewing time and well-being. In a study examining the causal relationship between TV viewing time and HRQOL among colorectal cancer survivors, Lynch and colleagues17 found a negative association of TV viewing time with HRQOL. One study, however, found that TV viewing proved beneficial for subjective well-being among adults aged ≥ 70 years old.25 This might be because time spent watching TV can satisfy some of the older adults’ needs, such as companionship and continued learning (ie, acquiring new information). In light of these findings, Less Engaging/Passive SB could have more impact on older adults or individuals with chronic illnesses than healthy middle-aged adults.
The results of the current study suggested that poor sleep quality is associated with low HRQOL on both physical and mental scales. A study of Australian adults also found that sleep quality negatively affects people’s physical, emotional, and social functioning.28 Another study suggested that sleep quality was a predictor of physical and mental health composites.27 Possible alternative explanations for the relationship between sleep quality and HRQOL could be reverse causation and confounding variables. For instance, individuals with low levels of HRQOL might already have poor sleep quality and have more physical and psychological problems compared to people with better HRQOL. Physical symptoms (eg, pain and fatigue) and psychological problems (eg, depressive symptoms and stress) are associated with poor sleep quality and low levels of HRQOL.59–62
This study examined the mediational role of sleep quality in the association of SB to HRQOL. In the past, the physical health impact of SB has been emphasized by exercise scientists, whereas some clinicians and health psychologists have examined the role of sleep quality in adults’ HRQOL. We found that sleep quality statistically mediated the association of both Common Engaging SB and High Engaging/Leisure SB to HRQOL. For Common Engaging SB, the findings support previous research asserting that a prolonged period of SB is associated with worse sleep quality.29,30 When individuals reported poor sleep quality, they were more likely to perceive both lower levels of physical and mental HRQOL.27,28 This suggested the importance of sleep quality on HRQOL; in essence, a decrease in sleep quality due to an increase in Common Engaging SB could be detrimental to later HRQOL. Interestingly, High Engaging/Leisure SB was associated with better sleep quality, and better sleep quality was related to both high physical and mental HRQOL. One possible reason for this result could be that High Engaging/Leisure SB enhances an individual’s mood, which affects sleep quality; in turn, that increases perceptions of physical and mental well-being.
Since research found a negative relationship between SB and HRQOL, it is essential to include SB, especially reducing Common Engaging SB, in health promotion programs to improve HRQOL. In conjunction with previous research findings, our results suggest that High Engaging/Leisure SB might be instrumental for the development of wellness programs in middle-aged adults. Adding regular leisure activities into health promotion programs could contribute to middle-aged adults’ well-being. More specifically, health promotion programs could help individuals find or develop personal hobbies and provide an enriched environment to make sitting activities more educational, social, and relaxing.
Building on previous research on sleep quality and HRQOL, our study found that sleep quality mediated the relationship between SB and HRQOL. Besides the high amount of sitting time reported by middle-aged adults, poor sleep quality commonly occurs among middle-aged American adults. A need exists for increased public awareness in the U.S. regarding the importance of sleep quality and appropriate management of poor sleep quality among middle-aged adults. Additionally, public health programs that promote sleep quality and education about the potential influences of poor sleep quality on health are needed to improve HRQOL among middle-aged adults.
Limitations and Future Directions
There are several limitations to this study. The first is that the current study uses a cross-sectional design, limiting conclusions regarding the directionality of the relationships among SB, HRQOL, and sleep quality. In light of this, future research could focus on longitudinal designs to establish whether SB is a predictor of HRQOL and sleep quality among middle-aged adults. The second limitation is that the current study has a wide range of subcomponents under the Less Engaging/Passive SB category; therefore, this could explain the lack of association between Less Engaging/Passive SB and other study variables. Since previous research found that Less Engaging/Passive SB, especially TV watching, tends to be negatively related to both physical and mental health outcomes,16–18 future research could focus separately on each subcomponent of Less Engaging/Passive SB, such as time spent in TV watching, including the types of TV shows (eg, documentary/educational, travel, or drama), doing paperwork, and computer work such as performing office work, composing emails, or paying bills to better understand the lack of significant relationships between Less Engaging/Passive SB and HRQOL in the study. A third limitation of this study is that self-reported SB could be influenced by recall biases. To reduce such biases, the next logical step would be to include an objective measurement (eg, accelerometer for assessing SB). The current sample showed a low internal consistency for the PSQI global score (Cronbach’s α = 0.61) compared to the original PSQI publication (Cronbach’s α = 0.83).40 One possible explanation could be due to the characteristics of current sample. Although studies investigating an ethnically-diverse population have used PSQI to assess sleep quality,63,64 the sleep measurement is not well-validated in a racially- and ethnically-diverse group in studies from the U.S. Additionally, sleep disturbances and alternations such as snoring65 and work schedule (ie, day or night shift)66 that might affect sleep quality and health outcomes were not assessed. Although the current study targets a non-clinical, middle-aged population, chronic diseases might emerge in middle age after long exposure to an unhealthy lifestyle. Thus, future studies should consider obtaining information on chronic illnesses. Finally, the results from this study might not be generalizable to the U.S. general population since participant selection occurred via the Internet, and the present study consisted of higher percentage of Asians compared to the current U.S. population. A slightly higher number of male workers than female workers joined the Mturk participant pool, and overall participant educational level is higher than the general U.S. population.67
CONCLUSIONS
The findings emphasize the need to examine the influence of different types of SB, particularly Common Engaging and High Engaging/Leisure SB since these 2 types of SB differentially related to middle-aged adults’ HRQOL. Reducing overall SB can be an effective method to promote middle-aged adults’ health. Even so, health promotion programs might also emphasize spending time in leisure activities. Although not physiologically optimal, people often enjoy mentally engaging in sedentary activities, such as doing hobbies or listening to music. High Engaging/Leisure SB could provide mental stimulation that enhances positive emotions, thus providing benefits to improve middle-aged adults’ HRQOL. The variety of self-report SB items in Less Engaging/Passive SB and sleep quality provided an incomplete picture of other potential underlying factors that might affect HRQOL. This requires further research that will examine each sedentary activity separately under the Less Engaging/Passive SB category. Finally, these findings warrant further experimental and longitudinal studies to better understand the association among SB, sleep quality, and HRQOL by adding objective measurements.
Acknowledgments
The authors thank the participants for their participation in this study. The project was not funded.
Footnotes
Human Subjects Approval Statement
The University of Texas at Austin’s Institutional Research Board approved the current study. The approval document number for the current study is 2018-10-0026. Informed consent was obtained from participants prior to data collection.
Conflict of Interest Disclosure Statement
The authors declare that there is no conflict of interest.
Contributor Information
Yen T. Chen, Department of Physical Medicine and Rehabilitation, University of Michigan, Ann Arbor, MI, United States..
Carole K. Holahan, Department of Kinesiology and Health Education, The University of Texas at Austin, Austin, TX, United States..
Darla M. Castelli, Department of Kinesiology and Health Education, The University of Texas at Austin, Austin, TX..
References
- 1.Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life: a conceptual model of patient outcomes. JAMA. 1995;273(1):59–65. doi: 10.1001/jama.1995.03520250075037 [DOI] [PubMed] [Google Scholar]
- 2.Brown DS, Thompson WW, Zack MM, Arnold SE, Barile JP. Associations between health-related quality of life and mortality in older adults. Prev Sci. 2015;16(1):21–30. doi: 10.1007/s11121-013-0437-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cavrini G, Broccoli S, Puccini A, Zoli M. EQ-5D as a predictor of mortality and hospitalization in elderly people. Qual Life Res. 2012;21(2):269–280. doi: 10.1007/s11136-011-9937-0 [DOI] [PubMed] [Google Scholar]
- 4.Boberska M, Szczuka Z, Kruk M, et al. Sedentary behaviours and health-related quality of life. A systematic review and meta-analysis. Health Psychol Rev. 2018;12(2):195–210. doi: 10.1080/17437199.2017.1396191 [DOI] [PubMed] [Google Scholar]
- 5.Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(9 SUPPL.):S498–S504. doi: 10.1097/00005768-200009001-00009 [DOI] [PubMed] [Google Scholar]
- 6.Hartman SJ, Marinac CR, Bellettiere J, et al. Objectively measured sedentary behavior and quality of life among survivors of early stage breast cancer. Support Care Cancer. 2017;25(8):2495–2503. doi: 10.1007/s00520-017-3657-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Meneguci J, Sasaki JE, Santos A, Scatena LM, Damião R. Sitting time and quality of life in older adults: a population-based study. J Phys Act Health. 2015;12(11):1513–1519. doi: 10.1123/jpah.2014-0233 [DOI] [PubMed] [Google Scholar]
- 8.Vallance JK, Eurich D, Marshall AL, Lavallee CM, Johnson ST. Associations between sitting time and health-related quality of life among older men. Ment Health Phys Act. 2013;6(1):49–54. doi: 10.1016/j.mhpa.2013.02.002 [DOI] [Google Scholar]
- 9.Trinh L, Plotnikoff RC, Rhodes RE, North S, Courneya KS. Associations between sitting time and quality of life in a population-based sample of kidney cancer survivors. Ment Health Phys Act. 2013;6(1):16–23. doi: 10.1016/j.mhpa.2012.09.001 [DOI] [Google Scholar]
- 10.Andel R, Crowe M, Pedersen NL, Fratiglioni L, Johansson B, Gatz M. Physical exercise at midlife and risk of dementia three decades later: a population-based study of Swedish twins. J Gerontol Ser A. 2008;63(1):62–66. doi: 10.1093/gerona/63.1.62 [DOI] [PubMed] [Google Scholar]
- 11.Sun Q, Townsend MK, Okereke OI, Franco OH, Hu FB, Grodstein F. Physical activity at midlife in relation to successful survival in women at age 70 years or older. Arch Intern Med. 2010;170(2):194–201. doi: 10.1001/archinternmed.2009.503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rezende LFM, Sá TH, Mielke GI, Viscondi JYK, Rey-López JP, Garcia LMT. All-cause mortality attributable to sitting time: analysis of 54 countries worldwide. Am J Prev Med. 2016;51(2):253–263. doi: 10.1016/j.amepre.2016.01.022 [DOI] [PubMed] [Google Scholar]
- 13.Wilmot EG, Edwardson CL, Achana FA, et al. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Diabetologia. 2012;55(11):2895–2905. doi: 10.1007/s00125-012-2677-z [DOI] [PubMed] [Google Scholar]
- 14.Ma P, Yao Y, Sun W, Dai S, Zhou C. Daily sedentary time and its association with risk for colorectal cancer in adults. Medicine (Baltimore). 2017;96(22). doi: 10.1097/MD.0000000000007049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schuch F, Vancampfort D, Firth J, et al. Physical activity and sedentary behavior in people with major depressive disorder: a systematic review and meta-analysis. J Affect Disord. 2017;210:139–150. doi: 10.1016/j.jad.2016.10.050 [DOI] [PubMed] [Google Scholar]
- 16.Hamer M, Stamatakis E, Mishra GD. Television- and screen-based activity and mental well-being in adults. Am J Prev Med. 2010;38(4):375–380. doi: 10.1016/j.amepre.2009.12.030 [DOI] [PubMed] [Google Scholar]
- 17.Lynch BM, Cerin E, Owen N, Hawkes AL, Aitken JF. Television viewing time of colorectal cancer survivors is associated prospectively with quality of life. Cancer Causes Control. 2011;22(8):1111–1120. doi: 10.1007/s10552-011-9786-8 [DOI] [PubMed] [Google Scholar]
- 18.Grøntved A, Hu FB. Television viewing and risk of type 2 diabetes, cardiovascular disease, and all-cause mortality: a meta-analysis. JAMA. 2011;305(23):2448–2455. doi: 10.1001/jama.2011.812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sugiyama T, Ding D, Owen N. Commuting by car: weight gain among physically active adults. Am J Prev Med. 2013;44(2):169–173. doi: 10.1016/j.amepre.2012.09.063 [DOI] [PubMed] [Google Scholar]
- 20.Sugiyama T, Wijndaele K, Koohsari MJ, Tanamas SK, Dunstan DW, Owen N. Adverse associations of car time with markers of cardio-metabolic risk. Prev Med. 2016;83:26–30. doi: 10.1016/j.ypmed.2015.11.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bavishi A, Slade MD, Levy BR. A chapter a day: association of book reading with longevity. Soc Sci Med. 2016;164:44–48. doi: 10.1016/j.socscimed.2016.07.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.O’Neill C, Dogra S. Different types of sedentary activities and their association with perceived health and wellness among middle-aged and older adults: a cross-sectional analysis. Am J Health Promot. 2016;30(5):314–322. doi: 10.1177/0890117116646334 [DOI] [PubMed] [Google Scholar]
- 23.Heo J, Chun S, Lee S, Lee KH, Kim J. Internet use and well-being in older adults. Cyberpsychology Behav Soc Netw. 2015;18(5):268–272. doi: 10.1089/cyber.2014.0549 [DOI] [PubMed] [Google Scholar]
- 24.Erickson J, Johnson GM. Internet use and psychological wellness during late adulthood. Canadian Journal on Aging/la Revue canadienne du vieillissement. 2011;30(2):197–209. doi: 10.1017/S0714980811000109 [DOI] [PubMed] [Google Scholar]
- 25.Ku P-W, Fox KR, Chen L-J. Leisure-time physical activity, sedentary behaviors and subjective well-being in older adults: an eight-year longitudinal research. Soc Indic Res. 2016;127(3):1349–1361. doi: 10.1007/s11205-015-1005-7 [DOI] [Google Scholar]
- 26.Driscoll HC, Serody L, Patrick S, et al. Sleeping well, aging well: a descriptive and cross-sectional study of sleep in “successful agers” 75 and older. Am J Geriatr Psychiatry Off J Am Assoc Geriatr Psychiatry. 2008;16(1):74–82. doi: 10.1097/JGP.0b013e3181557b69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sarraf P, Azizi S, Moghaddasi AN, Sahraian MA, Tafakhori A, Ghajarzadeh M. Relationship between sleep quality and quality of life in patients with multiple sclerosis. Int J Prev Med. 2014;5(12):1582–1586. [PMC free article] [PubMed] [Google Scholar]
- 28.Lallukka T, Sivertsen B, Kronholm E, Bin YS, Øverland S, Glozier N. Association of sleep duration and sleep quality with the physical, social, and emotional functioning among Australian adults. Sleep Health. 2018;4(2):194–200. doi: 10.1016/j.sleh.2017.11.006 [DOI] [PubMed] [Google Scholar]
- 29.Vallance JK, Buman MP, Stevinson C, Lynch BM. Associations of overall sedentary time and screen time with sleep outcomes. Am J Health Behav. 2015;39(1):62–67. doi: 10.5993/AJHB.39.1.7 [DOI] [PubMed] [Google Scholar]
- 30.Serrano S, Lee JW, Dehom S, Tonstad S. The association of tv watching to sleep problems in a church-going population. Fam Community Health. 2014;37(4):279–287. doi: 10.1097/FCH.0000000000000038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Borges-Cosic M, Aparicio VA, Estévez‐López F, et al. Sedentary time, physical activity, and sleep quality in fibromyalgia: the al-Ándalus project. Scand J Med Sci Sports. 2019;29(2):266–274. doi: 10.1111/sms.13318 [DOI] [PubMed] [Google Scholar]
- 32.Peer E, Vosgerau J, Acquisti A. Reputation as a sufficient condition for data quality on Amazon Mechanical Turk. Behav Res Methods. 2014;46(4):1023–1031. doi: 10.3758/s13428-013-0434-y [DOI] [PubMed] [Google Scholar]
- 33.Sheehan KB. Crowdsourcing research: data collection with Amazon’s Mechanical Turk. Commun Monogr. 2018;85(1):140–156. doi: 10.1080/03637751.2017.1342043 [DOI] [Google Scholar]
- 34.Hays RD, Sherbourne CD, Mazel RM. The rand 36-item health survey 1.0. Health Econ. 1993;2(3):217–227. doi: 10.1002/hec.4730020305 [DOI] [PubMed] [Google Scholar]
- 35.McHorney CA, Ware JE, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31(3):247–263. doi: 10.1097/00005650-199303000-00006 [DOI] [PubMed] [Google Scholar]
- 36.Ware JE, Sherbourne CD. The MOS 36-Item Short-Form Health Survey (SF-36): I. conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 37.Rosenberg DE, Norman GJ, Wagner N, Patrick K, Calfas KJ, Sallis JF. Reliability and validity of the Sedentary Behavior Questionnaire (SBQ) for adults. J Phys Act Health. 2010;7(6):697–705. [DOI] [PubMed] [Google Scholar]
- 38.Gardiner PA, Clark BK, Healy GN, Eakin EG, Winkler EAH, Owen N. Measuring older adults’ sedentary time: reliability, validity, and responsiveness. Med Sci Sports Exerc. 2011;43(11):2127–2133. doi: 10.1249/MSS.0b013e31821b94f7 [DOI] [PubMed] [Google Scholar]
- 39.Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res. 2002;53(3):737–740. doi: 10.1016/s0022-3999(02)00330-6 [DOI] [PubMed] [Google Scholar]
- 40.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 41.Atkins J, Naismith SL, Luscombe GM, Hickie IB. Psychological distress and quality of life in older persons: relative contributions of fixed and modifiable risk factors. BMC Psychiatry. 2013;13(1):249. doi: 10.1186/1471-244X-13-249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Coste J, Quinquis L, D’Almeida S, Audureau E. Smoking and health-related quality of life in the general population. Independent relationships and large differences according to patterns and quantity of smoking and to gender. PLOS ONE. 2014;9(3):e91562. doi: 10.1371/journal.pone.0091562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Davies CA, Vandelanotte C, Duncan MJ, van Uffelen JGZ. Associations of physical activity and screen-time on health related quality of life in adults. Prev Med. 2012;55(1):46–49. doi: 10.1016/j.ypmed.2012.05.003 [DOI] [PubMed] [Google Scholar]
- 44.Ford ES, Li C. Metabolic syndrome and health-related quality of life among U.S. adults. Ann Epidemiol. 2008;18(3):165–171. doi: 10.1016/j.annepidem.2007.10.009 [DOI] [PubMed] [Google Scholar]
- 45.Heesch KC, van Uffelen JGZ, van Gellecum YR, Brown WJ. Dose–response relationships between physical activity, walking and health-related quality of life in mid-age and older women. J Epidemiol Community Health. 2012;66(8):670–677. doi: 10.1136/jech-2011-200850 [DOI] [PubMed] [Google Scholar]
- 46.Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB [DOI] [PubMed] [Google Scholar]
- 47.Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Guilford Press; 2013. [Google Scholar]
- 48.Hughes ML, Lachman ME. Social comparisons of health and cognitive functioning contribute to changes in subjective age. J Gerontol B Psychol Sci Soc Sci. 2018;73(5):816–824. doi: 10.1093/geronb/gbw044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cerny BA, Kaiser HF. A study of a measure of sampling adequacy for factor-analytic correlation matrices. Multivar Behav Res. 1977;12(1):43–47. doi: 10.1207/s15327906mbr1201_3 [DOI] [PubMed] [Google Scholar]
- 50.Kaiser HF. The application of electronic computers to factor analysis. Educ Psychol Meas. 1960;20(1):141–151. doi: 10.1177/001316446002000116 [DOI] [Google Scholar]
- 51.Bankoski A, Harris TB, McClain JJ, et al. Sedentary activity associated with metabolic syndrome independent of physical activity. Diabetes Care. 2011;34(2):497–503. doi: 10.2337/dc10-0987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chastin SFM, Mandrichenko O, Helbostadt JL, Skelton DA. Associations between objectively-measured sedentary behaviour and physical activity with bone mineral density in adults and older adults, the NHANES study. Bone. 2014;64:254–262. doi: 10.1016/j.bone.2014.04.009 [DOI] [PubMed] [Google Scholar]
- 53.Conner TS, DeYoung CG, Silvia PJ. Everyday creative activity as a path to flourishing. J Posit Psychol. 2018;13(2):181–189. doi: 10.1080/17439760.2016.1257049 [DOI] [Google Scholar]
- 54.Davies C, Knuiman M, Rosenberg M. The art of being mentally healthy: a study to quantify the relationship between recreational arts engagement and mental well-being in the general population. BMC Public Health. 2015;16(1):1–10. doi: 10.1186/s12889-015-2672-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pressman SD, Matthews KA, Cohen S, et al. Association of enjoyable leisure activities with psychological and physical well-being. Psychosom Med. 2009;71(7):725–732. doi: 10.1097/PSY.0b013e3181ad7978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Thoma MV, La Marca R, Brönnimann R, Finkel L, Ehlert U, Nater UM. The effect of music on the human stress response. PLOS ONE. 2013;8(8). doi: 10.1371/journal.pone.0070156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Choi YK. The effect of music and progressive muscle relaxation on anxiety, fatigue, and quality of life in family caregivers of hospice patients. J Music Ther. 2010;47(1):53–69. doi: 10.1093/jmt/47.1.53 [DOI] [PubMed] [Google Scholar]
- 58.Yang YC, Boen C, Gerken K, Li T, Schorpp K, Harris KM. Social relationships and physiological determinants of longevity across the human life span. Proc Natl Acad Sci. 2016;113(3):578–583. doi: 10.1073/pnas.1511085112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Aree-Ue S, Kongsombun U, Roopsawang I, Youngcharoen P. Path model of factors influencing health-related quality of life among older people with knee osteoarthritis. Nurs Health Sci. 2019;21(3):345–351. doi: 10.1111/nhs.12602 [DOI] [PubMed] [Google Scholar]
- 60.Nicassio PM, Moxham EG, Schuman CE, Gevirtz RN. The contribution of pain, reported sleep quality, and depressive symptoms to fatigue in fibromyalgia. Pain. 2002;100(3):271–279. doi: 10.1016/S0304-3959(02)00300-7 [DOI] [PubMed] [Google Scholar]
- 61.Reyes-Gibby CC, Anderson KO, Morrow PK, Shete S, Hassan S. Depressive symptoms and health-related quality of life in breast cancer survivors. J Womens Health. 2011;21(3):311–318. doi: 10.1089/jwh.2011.2852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Åkerstedt T, Orsini N, Petersen H, Axelsson J, Lekander M, Kecklund G. Predicting sleep quality from stress and prior sleep – A study of day-to-day covariation across sixweeks. Sleep Med. 2012;13(6):674–679. doi: 10.1016/j.sleep.2011.12.013 [DOI] [PubMed] [Google Scholar]
- 63.Carnethon MR, De Chavez PJ, Zee PC, et al. Disparities in sleep characteristics by race/ethnicity in a population-based sample: Chicago Area Sleep Study. Sleep Med. 2016;18:50–55. doi: 10.1016/j.sleep.2015.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.George KM, Peterson RL, Gilsanz P, et al. Racial/ethnic differences in sleep quality among older adults: Kaiser Healthy Aging and Diverse Life Experiences (KHANDLE) Study. Ethn Dis. 30(3):469–478. doi: 10.18865/ed.30.3.469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bhattacharyya N. Sleep and health implications of snoring: a populational analysis. The Laryngoscope. 2015;125(10):2413–2416. doi: 10.1002/lary.25346 [DOI] [PubMed] [Google Scholar]
- 66.Lim YC, Hoe VCW, Darus A, Bhoo-Pathy N. Association between night-shift work, sleep quality and metabolic syndrome. Occup Environ Med. 2018;75(10):716–723. doi: 10.1136/oemed-2018-105104 [DOI] [PubMed] [Google Scholar]
- 67.Ipeirotis PG. Demographics of Mechanical Turk (on-line). http://papers.ssrn.com/abstract=1585030. Published April 6, 2010. Accessed December 5, 2020.


