Abstract
The WHO just released in May 2022 a report on the state of the obesity pandemic in Europe, stating that 60% of citizens in the area of Europe are either overweight or obese, and highlighting the implications of the obesity pandemic, especially as it interacts with the COVID pandemic to create a twin pandemic, to increase morbidity and mortality. Obesity is a complex disease which has reached pandemic dimensions. The worldwide prevalence of obesity has nearly tripled since 1975, mainly due to the adoption of a progressively more sedentary lifestyle and the consumption of less healthy diets. We first report herein updated prevalence rates of overweight and obesity by sex, age, and region first in Europe, per the WHO report, and then worldwide between 1980 and 2019, as we analyze and present herein the data provided by the Global Burden of Disease Study. The prevalence of obesity is higher in women than in men of any age and the prevalence of both overweight and obesity increases with age and has reached their highest point between the ages of 50 to 65 years showing a slight downward trend afterwards. The age-standardized prevalence of obesity has increased from 4.6% in 1980 to 14.0% in 2019. The American and European region have the highest obesity prevalence and the USA and Russia are the countries with the most obese residents. Given dire implications in terms of comorbidities and mortality, these updated epidemiological findings call for coordinated actions from local and regional governments, the scientific community and individual patients alike, as well as the food industry for the obesity pandemic to be controlled and alleviated. We can hopefully learn from the COVID-19 pandemic, where collaborative efforts worldwide, focused intense work at both the local and global level and well-coordinated leadership have demonstrated that humankind is capable of amazing accomplishments by leveraging science and public health, and that we can finally make strides in terms of understanding and combating the obesity pandemic and its dire comorbidities including diabetes, NAFLD, CVD and obesity associated malignancies.
Keywords: Prevalence, BMI, Adiposity, Obesity, Overweight, Health risk
1. Introduction
Obesity is a chronic disease that is increasing in prevalence and is now considered to be a global epidemic. Epidemiologic studies have revealed an association between high body mass index (BMI) and an extensive range of chronic diseases such as Non Alcoholic Fatty Liver (NAFL), cardiovascular disease [1], [2], diabetes mellitus [1], several malignancies [3], [4], musculoskeletal diseases [5], [6], chronic kidney disease [1], and mental disorders [7], [8], which consequently, affect negatively subjects' quality of life and raise healthcare costs [9], [10]. Interestingly, it has been demonstrated that BMI 30–40 kg/m2 is associated with almost 50%, and BMI over 40 kg/m2 is associated with 100% greater healthcare expenditures due to treatment of obesity comorbidities [11]. Similarly, BMI >30 kg/m2 has been linked with an increase in annual healthcare costs of approximately 37% [12].
The World Health Organization (WHO) defines overweight as BMI >25 kg/m2 and obesity >30 kg/m2 and describes these conditions as abnormal or excessive fat accumulation that is associated with increased health risk. BMI, although not the most accurate metric of excess fat [13], is easy to assess and is thus the most commonly accepted first step to determine the degree of overweight or obesity. It is calculated using the weight in Kg divided by the square of the height in meters and it is associated well with the percentage of body fat and body fat mass [14] in most groups.
The sedentary lifestyle and the decline in overall physical activity in combination with consumption of unhealthy diets, e.g. a high sugar and refined carb diet, building upon the myriad of genetic, endocrine, metabolic, and environmental factors, are currently considered the main common causes for the obesity epidemic that is taking over many parts of the world during the last decades [15], [16].
Studies examining the trends in obesity have shown that its prevalence has raised in all age groups, regardless the ethnicity or socioeconomic status [17]. From 1999 through 2018, the obesity prevalence in the United States increased from 30.5% to 42.4%. Notably, the obesity prevalence was 40% among adults aged 20 to 39 years, 45% among adults aged 40 to 59 years, and 43% among the group aged 60 years and older.
Prevalence data on obesity have been obtained using two platforms in the USA; the annual phone call surveys conducted by state Departments of Health in collaboration with the Centers for Disease Control and Prevention (the Behavioral Risk Factor Surveillance System [BRFSS]), and surveys by the National Center for Health Statistics as the National Health and Nutrition Examination Survey (NHANES), providing a sample selected through a complex, multistage probability design [18]. The age-adjusted prevalence of obesity among US adults based upon data collected for NHANES was 42.4% in 2017–2018. Data from BRFSS consistently report obesity prevalence rates lower than those from the NHANES surveys (30.9% in 2019), probably due to the self-report bias on phone surveys. Moreover, the CDC report on obesity prevalence in the USA estimates that 31.4% of adults were obese in 2019 [19]. Thus, it is crucial to identify the data source when evaluating obesity prevalence information. It would also be interesting to evaluate and report the prevalence of obesity in the USA and the world in the post COVID-19 pandemic, a pandemic that caused 15 million deaths (estimates vary between 12 and 22 million) during the past two years and mainly deaths of patients with obesity and metabolic comorbidities.
On the occasion of the newly released WHO report on the status of Obesity in the European region stating that both overweight and obesity rates have reached epidemic proportions across the European Region, where 59% of adults and almost 1 in 3 children are suffering from overweight or obesity [20], we publish this report as an update on the epidemiology of obesity [21]. The purpose of this update is to re-evaluate the global and regional prevalence and trends of overweight and obesity given the new advances in our knowledge on the pathophysiology of obesity and the resultant new therapeutic tools that have been introduced recently in the field [22], [23]. The purpose of this update is also to draw attention to the obesity pandemic, and the need for more research and care and public health efforts as a call to action. Now that the COVID-19 pandemic appears to be receding, we need to learn from our successes in that front as we prioritize work on the other pandemic, that of obesity and its comorbidities e.g. diabetes which will continue to plague our society unless global leaders provide the guidance and resources needed to create a meaningful difference.
2. Methods
We report data from the May 2022 European Regional Report on Obesity by the WHO. We also used the data published from the Global Burden of Disease Study (Institute for Health Metrics and Evaluation, Seattle, WA) [17]. The full data file is available online from Global Health Data Exchange (http://ghdx.heathdata.org).
We adopted the WHO division of the world into six regions; namely African, Americas, Eastern Mediterranean, European, South East Asian, and Western Pacific. We isolated the data for the five most populous countries from each region: the African region included Nigeria, Ethiopia, Congo, the United Republic of Tanzania, and South Africa; the Americas included the United States of America, Brazil, Mexico, Colombia, and Argentina; the Eastern Mediterranean included Pakistan, Egypt, Iran, Iraq, and Afghanistan; the European region included Russian Federation, Germany, Turkey, United Kingdom, and France; the South East Asian region included India, Indonesia, Bangladesh, Thailand and Myanmar; and finally, the Western Pacific region included China, Japan, Philippines, Viet Nam, and Republic of Korea. The aforementioned selected countries represent ~78% of the world's population.
We report prevalence rates (%) of overweight and obesity by sex, age, and region between 1980 and 2019.
3. Results
3.1. Prevalence of overweight and obesity in the European region by the WHO
Obesity has been recognized as an important public health issue globally and a major determinant of morbidity and mortality in the WHO European Region which raises the risk of noncommunicable diseases. Overweight and obesity have reached epidemic dimensions in the WHO European Region, impairing almost 60% of adults [20]. Children are also affected, with almost 8% of children younger than 5 years and one in three school-aged children living with overweight or obesity. Prevalence decreases temporarily in the age group 10–19 years, where one in four live with overweight or obesity. Repercussions of obesity on health include those that result from the mechanical effects of excess body weight, such as some musculoskeletal complications, metabolic effects such as diabetes and cardiovascular risk, and the effects on mental health. Obesity is also considered to be responsible for more than 13 types of malignancies. Overweight and obese people have been disproportionately impaired by the effects of the COVID-19 pandemic. The report concludes by recommending a series of interventions in general population and policy options that Member States can follow in preventing and managing obesity in the Region, focusing on building back better after the COVID-19 pandemic.
3.2. Global burden of disease study results
3.2.1. Prevalence of overweight and obesity by sex and age
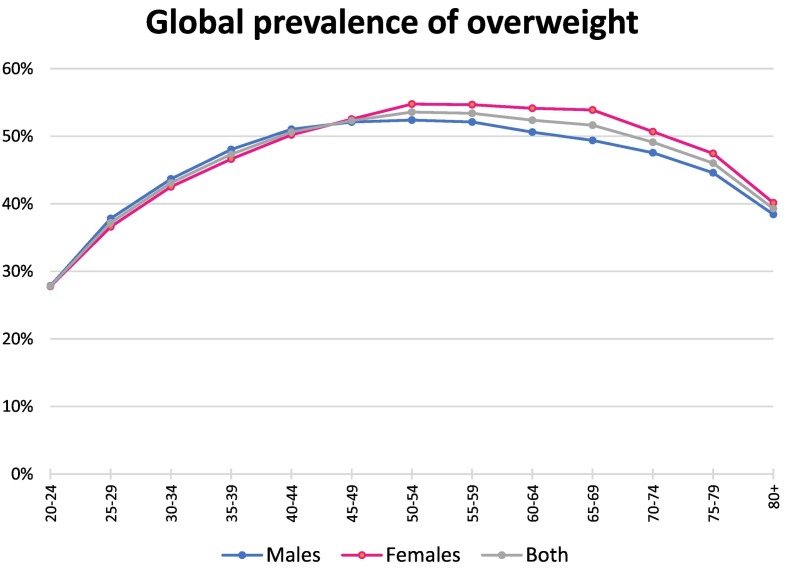
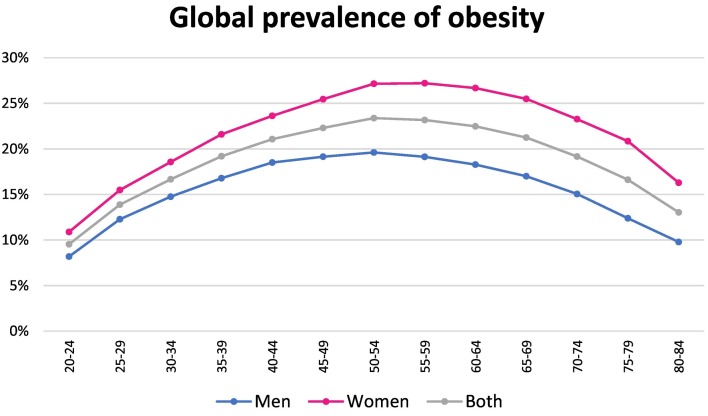
Fig. 1 depicts the global prevalence rates of overweight and obesity in 2019, for men and women over 20 years, by age group. In 2019, the prevalence of overweight was slightly lower in young females than in young males aged 20–44 years whilst this trend was inverted among the age groups over 45 years, probably because of the menopause occurring in women. The prevalence of obesity is in general higher in women than in men of any age. [Fig. 2 ] The prevalence of both overweight and obesity increased with age, reached their highest point between the ages of 50 to 65 years, and showed a slight downward trend afterwards.
Fig. 1.
Global prevalence of overweight in adults >20 years old by age group and sex (ca. 2019). [Data from the Global Burden of Disease Study (Institute for Health Metrics and Evaluation, Seattle, WA)] [17].
Fig. 2.
Global prevalence of obesity in adults >20 years old by age group and sex (ca. 2019). [Data from the Global Burden of Disease Study (Institute for Health Metrics and Evaluation, Seattle, WA)] [14].
3.2.2. Global trends in obesity
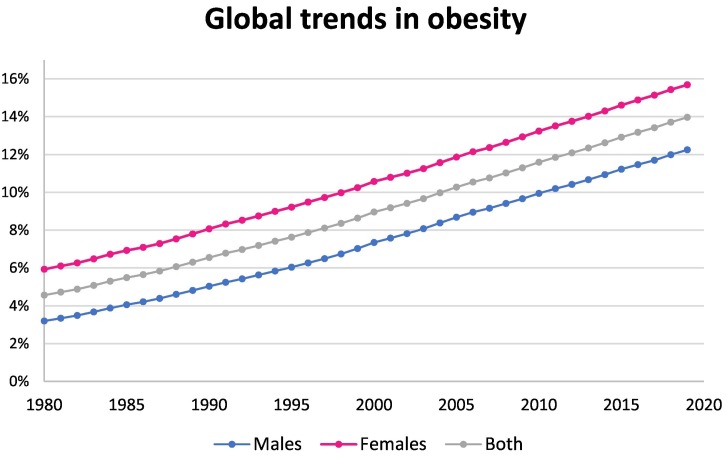
The age-standardized prevalence of obesity increased from 4.6% in 1980 to 14.0% in 2019. Half of this rise occurred in 22 years between 1980 and 2002 and another half occurred in the 17 years between 2002 and 2019. A constant predominance of women in the prevalence rates of obesity compared to men is observed. [Fig. 3 ].
Fig. 3.
Age-standardized global prevalence of obesity in men and women >20 years old by year (ca. 1980–2019). [Data from the Global Burden of Disease Study (Institute for Health Metrics and Evaluation, Seattle, WA)] [17].
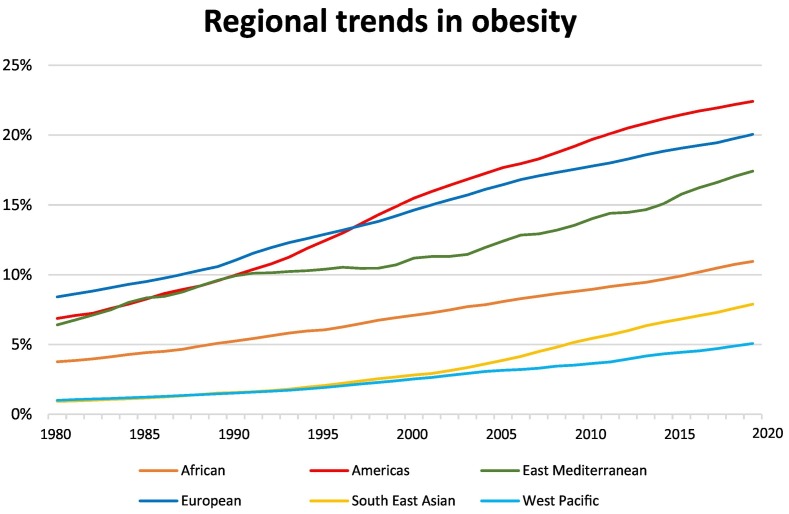
3.2.3. Regional prevalence of obesity
The highest prevalence of obesity was observed in the American and the European region. In the Americas, the prevalence of obesity increased from 6.8% in 1980 to 22.4% in 2019. The countries with the highest prevalence rates were the United States (23.2%) and Mexico (18.4%), while Colombia had the lowest prevalence rate of obesity (9.8%). Likewise, in Europe, the rates increased from 8.4% in 1980 to 20% in 2019 and the countries with the highest percentage of obese inhabitants were Russia (15.9%) and Turkey (17.5%). France had the lowest rate of obesity prevalence (10.3%).
In the Eastern Mediterranean region, the prevalence of obesity increased from 6.4% to 17.4% in 2019, while in the African region the prevalence of obesity increased from 3.8% to 10.9%. Some countries in these two regions presented much fluctuation in the prevalence rates of obesity. For instance, this rate in South Africa increased from 11.8% in 1980 to 23.3% in 2019, and in Iran from 5.9% in 1980 to 20.1% in 2019.
Finally, as for the region with the lowest obesity prevalence rates, the West Pacific, the prevalence of obesity increased approximately fivefold, from 0.9% in 1980 to 5% almost 40 years later. Particularly, in China, the prevalence of obesity increased from 0.4% to 5.8%. In parallel, the prevalence rate of obesity in the South East Asian region started from the same level as that of the West Pacific (0.9% in 1980) and showed a larger increase reaching 7.9% in 2019. [Fig. 4 ].
Fig. 4.
Age-standardized prevalence of obesity in adults >20 years old by geographical region and year (ca. 1980–2019). [Data from the Global Burden of Disease Study (Institute for Health Metrics and Evaluation, Seattle, WA)] [17].
In general, rising trends in the prevalence rates of both obesity and overweight are observed globally over the last 4 decades.
4. Discussion
The worldwide prevalence of obesity has nearly tripled between 1975 and 2016 and has now reached pandemic dimensions [14]. Specifically, the global obesity prevalence has risen approximately 2 percentage points per decade [24]. According to the WHO, there are about 2 billion adults who are overweight, whilst 650 million are obese. If these rates do not slow down, it is expected that 2.7 billion adults will be overweight and over 1 billion will be obese by 2025. The prevalence of obesity increased markedly between 1980 and 2019 from 3.2% to 12.2% in men, and from 6% to 15.7% in women. The fact that females constantly lead in terms of the proportions of obesity is expected, given the biologically driven higher percentage of body fat in women [25], [26]. Fundamental sex differences include distribution and mobilization of adipose tissue storage, different insulin sensitivity and lipoprotein profiles, and effects of gonadal hormones. Although overweight and obesity are considered a high-income country problem, they both are currently on the rise in low- and middle-income countries due to the global free trade, the economic growth and the urbanization these countries are experiencing [27]. Moreover, it has been reported that obesity is concentrated among the rich in low-income countries and the poor in high-income countries [28]. There are several reasons for this. As the income rises people can afford more food. In parallel, their dietary habits change and become more ‘westernized’. Also, the rich adopt a more sedentary lifestyle and occupation. However, this pattern changes at the societies with higher levels of income where the social stigma of being obese prevails. Moreover, access to healthy diets, healthcare, education, and activities promoting weight loss is improved in high-income countries.
Obesity prevalence increased in every single country of the world. Interestingly, 12 countries had a prevalence of obesity under 2% in 1980: Ethiopia (0.4%), Pakistan (1.7%), India (0.9%), Indonesia (1.0%), Bangladesh (0.3%), Thailand (1.9%), Myanmar (0.5%), China (0.4%), Japan (1.6%), Philippines (1.8%), Viet Nam (0.5%), and Korea (0.7%). Hunger is high even today in almost all subregions of Africa and to a lesser extent in Latin America and Western Asia, and a large portion of people in those regions experience moderate or severe food insecurity. Nevertheless, a considerable rise in caloric supply across Asia and Africa is observed in recent decades [29]. Of note, nowadays, there is no country with obesity prevalence below 2%.
The absolute rates of obesity varied considerably among regions and countries. In 1980, the obesity prevalence rates ranged from 0.3% in Bangladesh to 12.8% in the USA and in only 5 countries the prevalence rate was over 10%: South Africa (11.8%), USA (12.8%), Egypt (10.7%), Iraq (10.3%), Russia (11.8%). In 2019, obesity prevalence rates ranged from 3.5% in Bangladesh to 32% in the USA and only 13 out of the 30 countries examined had an obesity prevalence rate less than 10%: Nigeria, Ethiopia, Tanzania, Pakistan, Afghanistan, India, Bangladesh, Myanmar, China, Japan, Philippines, Viet Nam, Korea. Interestingly, 9 countries had a prevalence of obesity >20%: South Africa (23.3%), USA (32%), Brazil (21.4%), Mexico (25%), Egypt (30%), Iran (20.1%), Iraq (21%), Russia (21.5%), Turkey (26%).
Alterations in the global food system in combination with the adoption of a sedentary lifestyle represent the main drivers of the obesity pandemic. In addition, regional differences are largely associated with differences in socioeconomic status [30]. Poverty, aspects of the food environment (e.g., accessibility to fast-food restaurants and/or supermarkets, groceries), community characteristics (e.g., cultural norms, education, the way towns are built), and ideal weight and body image unique to particular regions are some of the underlying factors impairing regional disparities in obesity prevalence. It is also of great interest that the economic disparity within a society may cause heterogeneity in obesity prevalence [31], [32]. It has been advocated that wider income gaps cause wider waists [31]. Moreover, at a given BMI, Asian populations apparently have higher health risks in comparison to Caucasians and this may result from the different fat distribution, i.e. more central body fat distribution, these populations have [33]. BMI does not assess body fat directly and in younger population may also reflect muscle mass. The relationship between BMI and body fat is related to the body composition of a specific person and is also affected by sex, age, race, and origin. On the other hand, the waist-to-hip ratio (WHR) is assumed to reflect more accurately the distribution of fat. Variation in waist circumference reflects mainly variation in subcutaneous and visceral fat, whereas variation in hip circumference represents variation in bone structure (pelvic width), gluteal muscle, and subcutaneous gluteal fat [34]. However, the considerable fluctuation in methodology used in the field and the results reported in the literature, apparently reflect the lack of a standardized approach [35].
Another important issue is the observed gender gap in obesity rates in many countries. This seems to be correlated with income. In particular, the gap is much larger for middle-income countries than it is for low- or high-income countries [28], [36]. Specifically, the difference between the two genders in obesity prevalence rates in Tanzania, which is a middle-income country, is about 7% (6.7% the obesity prevalence for males vs 13.1% for females) in 2019, while this difference was only 1.7% in Japan and 1% in Bangladesh, which are countries with high and low income, respectively. For women, there is a non-linear relationship between obesity prevalence and income. This relationship is positive in low-income and negative in high-income countries. Nevertheless, male obesity increases for all income levels, and although the curve plateaus, there is no turning point. In high-income countries, this gender gap mitigates since the increase in female obesity is slower than that of male obesity.
Interestingly, the rate of BMI increase has been slowed down since 2000 in high-income and some-middle income countries than the rates of the previous century [24]. It is worth noting that the rise of obesity prevalence rates has slowed down, especially during the past decade in the developed countries, such as the USA (from 30% in 2009 to 32% in 2019), UK (from 19% in 2009 to 19.7% in 2019) and France (from 13% in 2009 to 14.5% in 2019). Nevertheless, the global obesity prevalence is still rising, since in several, particularly developing regions with large populations the obesity trends have accelerated. For example, China, which belongs to the countries with the largest population in the world [37], experienced a 90% increase in the prevalence of obesity in the last decade (from 3.0% in 2009 to 5.7% in 2019).
We would like to also emphasize the strong relationship between the two pandemics, the obesity and the COVID-19 pandemic, that coexist and synergize, since it has repeatedly been shown after we first reported that, in a way, one exacerbates the other [38]. Several studies have shown that patients with COVID-19 and obesity have increased risk for severe disease, hospitalization, incubation, and death [38], [39], [40], [41], [42], [43]. This is not surprising since it has been described that obesity causes increased work of breathing by inducing the airway resistance and decreases expiratory reserve volume, functional capacity, and pulmonary compliance. Furthermore, obesity impedes diaphragmatic excursion in supine patients by compromising ventilation [44]. In addition, obesity is a chronic inflammatory condition with increased circulating levels of pro-inflammatory cytokines and COVID-19 builds upon that impaired immune system to further exacerbate inflammation and lead to its complications, morbidity and mortality [45]. According to the mortality data examined by a team from Johns Hopkins University and the WHO and released by the World Obesity Federation, global COVID-19 death rates were more than 10 times higher in countries where more than half the adults are overweight, compared to countries where fewer than half are overweight [46]. This report makes the correlation between obesity and mortality rates from COVID-19 clear and compelling and highlights the need for effective actions by individuals, the public, and governments to raise awareness of the risks flowing from obesity.
To the relief of everyone, the negative impacts of the COVID-19 pandemic appear to be receding. It is too early to declare ‘the end of the pandemic’ but the lower virulence of the Omicron variant of SARS-CoV-2, in conjunction with the increasing coverage of the populations by vaccination and the reduced burden on healthcare systems create hope for a subdued pandemic. Disappointingly, and in contrast to the COVID-19 pandemic, the obesity epidemic is continuing to worsen, and it is acknowledged as a global public health issue which continues to growth in significance.
The COVID-19 pandemic had an unprecedented impact on research and education for medical and healthcare professions. Healthcare professionals have been forced to concentrate on COVID-19 patients and, for a long time, not seeing and caring for the patients in their own clinics. The education of medical students has been discontinued and the graduation of many final year students was expedited so they could start work as junior doctors on the frontline of the COVID-19 pandemic earlier. Patients have had restricted access to healthcare. Researchers have been prevented from working in their laboratories, as well as from their interactions with colleagues. Clinical studies have been delayed or even cancelled. The effects of all this remain to be determined.
The experience from the last two years is expected to be decisive. Recently, the WHO announced the global excess-deaths estimate for 2020 and 2021 due to COVID-19 (14.9 million) [47], which is comparable to that of diabetes. For this reason, we should orient ourselves again to the ongoing pandemic that we are battling—the obesity pandemic which causes morbidity and mortality from diabetes, cardiovascular diseases and other metabolic disorders, without losing focus on the COVID-19 pandemic which has subsided but continues to be with us.
Undoubtedly, the golden key for combating the obesity pandemic, is dual, first understanding its pathophysiology and then designing the best prevention, education of the population and treatment approach. No intervention would flourish if the patient continues a sedentary lifestyle and the adoption of a balanced dietary practice, such as the Mediterranean diet, which is reputed for its demonstrated preventive effect of cardiovascular and metabolic disorders and obesity is of critical importance [48]. There is also an urgent need for collaboration and communication between the government, public health authorities, community organizations, the food industry, physical therapists, dietitians, clinicians, and schools to promote healthier eating habits and regular physical activity. Important first steps in this direction would be educational programs and advertisements, restructuring urban and educational environments to facilitate physical activity, incentives for healthy living, as well as policy changes, such as taxes on sugar-sweetened beverages or mandatory standards for meals at schools. It is of great interest and encouragement that taxing sugar-sweetened beverages in Chile and Mexico led to a highly significant decrease in the purchase of this kind of drinks by 21.6% in Chile and 6.3% in Mexico [49], [50]. Additionally, the food industry should make efforts to reduce the fat, sugar, and salt content of processed foods, ensure the availability of affordable healthy food choices and limit the advertisement of foods high in sugar, salt, and fat especially those targeting the kids and teen market [14].
A stepwise approach to the obesity pandemic includes lifestyle intervention with physical activity and diet [20], [51] but this is generally associated with moderate weight loss which is gradually regained, as well as pharmacotherapy, and the most efficacious method, bariatric surgery, which however costs more, is not really available to all, and may be accompanied by complications. In terms of pharmacotherapy, a special case of obesity derives from congenital or acquired leptin deficiency. Leptin is an adipokine which reflects the amount of energy stored in the adipose tissue, acts centrally and decreases appetite. Thus it plays a key role in the pathogenesis of obesity. In this case, leptin replacement ‘dramatically’ improves obesity and for this purpose the US Food and Drug Administration (FDA), the European Medicines Agency (EMA), and the Japanese Pharmaceuticals and Medical Devices Agency (PMDA) approved metreleptin as a replacement therapy for leptin deficiency in patients with lipodystrophy as is provided to extremely obese persons with congenital leptin deficiency on a compassionate basis where it cannot be compensated [52]. Except that, at the end of 2020, the US FDA approved setmelanotide, a melanocortin 4 receptor agonist for use in individuals with severe obesity due to the rare genetic leptin receptor deficiency [53]. Concerning pharmacotherapy for the more conventional cases of obesity, glucagon-like peptide-1 (GLP-1) analogs or receptor agonists play a role in regulating eating behavior by slowing gastric emptying, inducing postprandial satiety, and reducing appetite and food consumption by acting on the hypothalamus, limbic reward system and cortex. Liraglutide and semaglutide have been suggested to be the most efficacious GLP-1 receptor agonists to induce weight loss over at least 12 weeks of treatment (−4.49 kg and − 9.88 kg, respectively) [54]. Importantly, it has been demonstrated that the weight reducing effect of these agents is associated with changes in regional fat stores while lean body mass is preserved resulting in a favorable effect on metabolic and cardiovascular risks of obesity [55]. Thus, these agents currently appear as promising anti-obesity treatment options. Recently, tirzepatide, a once weekly glucose-dependent insulinotropic polypeptide (GIP) receptor and GLP-1 receptor agonist that integrates the actions of both incretins into a single novel molecule, was shown to achieve superior weight loss compared to placebo at 72 weeks of treatment [56]. Specifically, 63% of participants taking a dose of 15 mg lost at least 20% of their body weight. If there is inadequate response to initial therapy with a GLP-1 agonist or it is not tolerated, switching to orlistat, a lipase inhibitor, is recommended. Phentermine, the most widely prescribed weight loss drug in the USA, is only approved for the short-term treatment of obesity [57]. Additionally, existing anti-obesity strategies we have recently reviewed extensively [58], other potential anti-obesity strategies are being explored, including novel drug delivery systems, vaccines, modulators of the gut microbiome, and gene therapy are currently under investigation. Undoubtedly, choosing a drug for weight loss, which should definitely be safe and accessible, should be individualized, shared decision-making process that accounts for patients' preferences, comorbidities, and out-of-pocket expenses, especially during the economic downturn period following the pandemic.
At Metabolism, the pandemic has been intellectually and physically demanding for the entire journal's personnel, who had all to preserve productivity beyond extraordinary personal and professional circumstances in our everyday lives. Despite this and thanks to the magnificent efforts of everyone involved, the journal did not cease to deliver a high-quality science, our metrics have continued to increase considerably (e.g. our cite score, i.e. our 4 year impact factor, has increased to 16.5 bringing us to the top 3% of Endocrinology and Diabetes journals) and provides a notable platform for the outstanding research into obesity, diabetes and metabolism and their complications.
In the post-COVID-19 pandemic era it will be of utmost importance for all of us to learn from the COVID-19 pandemic, where collaborative efforts worldwide have proven that science is capable of estimable achievements. Obesity, diabetes and metabolism research and care demand currently to be prioritized if we want to cast off the obesity pandemic.
In conclusion, the rise in obesity has accelerated in the last decade. Its prevalence is higher in females than males and increases with age. Simultaneously, regional differences also exist. This obesity pandemic demands actions and interventions to reverse and address this problem. Prevention is the golden key in this direction and requires combined efforts from the governments, the scientific community, and the food industry to introduce the appropriate lifestyle modifications.
In this context, recently, on May 4, 2022, the President of the USA Joe Biden announced a White House conference on hunger, nutrition, and health to take place in September 2022 with a view to amplifying and attenuating long-standing health inequities and disparities. This conference is expected to reflect evidence-based nutrition research and science, it should promote future research on nutrition science and focus on ensuring nutrition security and preventing and managing diet-related diseases in the US and beyond. We need similar initiatives, ideally coordinated, worldwide, we need more research, we need new diagnostic and therapeutic tools that need to be safe, effective and affordable and we need better and broader implementation of novel therapies to make progress and thus help the obese live longer, happier and healthier lives.
Declaration of competing interest
Over the past 3 years, CSM has been a shareholder of and reports grants through his institution from Merck, grants through his Institution and personal consulting fees from Coherus Inc. and AltrixBio, he reports grants through his institution and personal consulting fees from Novo Nordisk, reports personal consulting fees and support with research reagents from Ansh Inc., reports personal consulting fees from Genfit, Lumos, Amgen, Corcept, Intercept, Astra Zeneca and Regeneron, reports support (educational activity meals at and through his institution) from Amarin, Novo Nordisk and travel support and fees from TMIOA, Elsevier, College Internationale Researche Servier and the Cardio Metabolic Health Conference. None is related to the work presented herein. C.S.M. also reports that in the past he was a shareholder of Pangea Inc., member of the California Walnut Commission Scientific Advisory Board and has received travel and grant support by the California Walnut Commission, outside the submitted work. CB declares no conflicts of interest.
References
- 1.Singh G.M., Danaei G., Farzadfar F., Stevens G.A., Woodward M., Wormser D., et al. The age-specific quantitative effects of metabolic risk factors on cardiovascular diseases and diabetes: a pooled analysis. PLoS One. 2013;8 doi: 10.1371/JOURNAL.PONE.0065174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wormser D., Kaptoge S., Di Angelantonio E., Wood A.M., Pennells L., Thompson A., et al. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet. 2011;377:1085. doi: 10.1016/S0140-6736(11)60105-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lauby-Secretan B., Scoccianti C., Loomis D., Grosse Y., Bianchini F., Straif K. Body fatness and cancer — viewpoint of the IARC working group. N Engl J Med. 2016;375:794. doi: 10.1056/NEJMSR1606602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barb D., Pazaitou-Panayiotou K.M.C. Adiponectin: a link between obesity and cancer. Expert Opin Investig Drugs. 2006;15:917–931. doi: 10.1517/13543784.15.8.917. [DOI] [PubMed] [Google Scholar]
- 5.Jiang L., Tian W., Wang Y., Rong J., Bao C., Liu Y., et al. Body mass index and susceptibility to knee osteoarthritis: a systematic review and meta-analysis. Jt Bone Spine. 2012;79:291–297. doi: 10.1016/J.JBSPIN.2011.05.015. [DOI] [PubMed] [Google Scholar]
- 6.Jiang L., Rong J., Wang Y., Hu F., Bao C., Li X., et al. The relationship between body mass index and hip osteoarthritis: a systematic review and meta-analysis. Jt Bone Spine. 2011;78:150–155. doi: 10.1016/J.JBSPIN.2010.04.011. [DOI] [PubMed] [Google Scholar]
- 7.Anstey K.J., Cherbuin N., Budge M., Young J. Body mass index in midlife and late-life as a risk factor for dementia: a meta-analysis of prospective studies. Obes Rev. 2011;12 doi: 10.1111/J.1467-789X.2010.00825.X. [DOI] [PubMed] [Google Scholar]
- 8.Alford S., Patel D., Perakakis N., Mantzoros C.S. Obesity as a risk factor for Alzheimer's disease: weighing the evidence. Obes Rev. 2018;19:269–280. doi: 10.1111/OBR.12629. [DOI] [PubMed] [Google Scholar]
- 9.Vityala Y., Tagaev T., Zhumabekova A., Mamatov S. Evaluation of metabolic syndrome, insulin secretion and insulin resistance in adolescents with overweight and obesity. MetabClin Exp. 2022;128 doi: 10.1016/J.METABOL.2021.155011. [DOI] [Google Scholar]
- 10.Morosanu A., Morosanu M. Relations between food intake, weight status and cardio-metabolic disturbances in area representative group. MetabClin Exp. 2022;128 doi: 10.1016/J.METABOL.2021.155022. [DOI] [Google Scholar]
- 11.Andreyeva T., Sturm R., Ringel J.S. Moderate and severe obesity have large differences in health care costs. Obes Res. 2004;12:1936–1943. doi: 10.1038/OBY.2004.243. [DOI] [PubMed] [Google Scholar]
- 12.Kjellberg J., Larsen A.T., Ibsen R., Højgaard B. The socioeconomic burden of obesity. Obes Facts. 2017;10:493–502. doi: 10.1159/000480404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Woolcott O.O., Seuring T. Prevalence trends in obesity defined by the relative fat mass (RFM) index among adults in the United States: 1999–2018. MetabClin Exp. 2022;128 doi: 10.1016/J.METABOL.2021.155027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Obesity and overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight 2009.
- 15.Upadhyay J., Farr O., Perakakis N., Ghaly W., Mantzoros C. Obesity as a disease. Med Clin North Am. 2018;102:13–33. doi: 10.1016/J.MCNA.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 16.Polyzos S.A., Mantzoros C.S. Obesity: seize the day, fight the fat. Metabolism. 2019;92:1–5. doi: 10.1016/j.metabol.2018.12.011. [DOI] [PubMed] [Google Scholar]
- 17.Global Burden of Disease Study 2019 (GBD 2019) Covariates 1980-2019 | GHDx. https://ghdx.healthdata.org/record/global-burden-disease-study-2019-gbd-2019-covariates-1980-2019 n.d.
- 18.Hales C.M., Carroll M.D., Fryar C.D., Ogden C.L. 2017. Prevalence of obesity and severe obesity among adults: United States, 2017-2018 Key findings Data from the National Health and Nutrition Examination Survey. [Google Scholar]
- 19.DNPAO Data Trends and maps: explore by topic | CDC. https://nccd.cdc.gov/dnpao_dtm/rdPage.aspx?rdReport=DNPAO_DTM.ExploreByTopic&islClass=OWS&islTopic=&go=GO n.d.
- 20.Kluge H.H.P. 2022. Weltgesundheitsorganisation Regionalbüro für Europa. WHO European regional obesity report. n.d. [Google Scholar]
- 21.Chooi Y.C., Ding C., Magkos F. The epidemiology of obesity. Metabolism. 2019;92:6–10. doi: 10.1016/j.metabol.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 22.Toumba M., Fanis P., Vlachakis D., Neocleous V., Phylactou L.A., Skordis N., et al. Molecular modelling of novel ADCY3 variant predicts a molecular target for tackling obesity. Int J Mol Med. 2022;49 doi: 10.3892/IJMM.2021.5065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Angelidi A.M., Belanger M.J., Kokkinos A., Koliaki C.C., Mantzoros C.S. Novel non-invasive approaches to the treatment of obesity: from pharmacotherapy to gene therapy. Endocr Rev. 2021 doi: 10.1210/ENDREV/BNAB034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet (London, England) 2017;390:2627–2642. doi: 10.1016/S0140-6736(17)32129-3. 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mathew H., Castracane V.D., Mantzoros C. Adipose tissue and reproductive health. Metabolism. 2018;86:18–32. doi: 10.1016/J.METABOL.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 26.Wells J.C.K., Marphatia A.A., Cole T.J., McCoy D. Associations of economic and gender inequality with global obesity prevalence: understanding the female excess. Soc Sci Med. 2012;75:482–490. doi: 10.1016/J.SOCSCIMED.2012.03.029. [DOI] [PubMed] [Google Scholar]
- 27.Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377:13–27. doi: 10.1056/NEJMOA1614362/SUPPL_FILE/NEJMOA1614362_DISCLOSURES.PDF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ameye H., Swinnen J. Obesity, income and gender: the changing global relationship. Glob Food Sec. 2019;23:267–281. doi: 10.1016/J.GFS.2019.09.003. [DOI] [Google Scholar]
- 29.Food supply - our world in data. https://ourworldindata.org/food-supply n.d.
- 30.Blüher M. Obesity: global epidemiology and pathogenesis. Nat Rev Endocrinol. 2019;15:288–298. doi: 10.1038/S41574-019-0176-8. [DOI] [PubMed] [Google Scholar]
- 31.Wilkinson R.G., Pickett K. 2009. The Spirit level: why more equal societies almost always do better. [Google Scholar]
- 32.Loomis W.F. Why inequality is fatal. Nature. 2009;4587242(458):1109–1110. doi: 10.1038/4581109a. 2009. [DOI] [Google Scholar]
- 33.Nishida C., Barba C., Cavalli-Sforza T., Cutter J., Deurenberg P., Darnton-Hill I., et al. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet (London, England) 2004;363:157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 34.Seidell J.C., Pérusse L., Després J.P., Bouchard C. Waist and hip circumferences have independent and opposite effects on cardiovascular disease risk factors: the Quebec Family Study. Am J Clin Nutr. 2001;74:315–321. doi: 10.1093/AJCN/74.3.315. [DOI] [PubMed] [Google Scholar]
- 35.Lear S.A., James P.T., Ko G.T., Kumanyika S. Appropriateness of waist circumference and waist-to-hip ratio cutoffs for different ethnic groups. Eur J Clin Nutr. 2010;641(64):42–61. doi: 10.1038/ejcn.2009.70. 2009. [DOI] [PubMed] [Google Scholar]
- 36.Garawi F., Devries K., Thorogood N., Uauy R. Global differences between women and men in the prevalence of obesity: is there an association with gender inequality? Eur J Clin Nutr. 2014;6810(68):1101–1106. doi: 10.1038/ejcn.2014.86. 2014. [DOI] [PubMed] [Google Scholar]
- 37.Mi Y.J., Zhang B., Wang H.J., Yan J., Han W., Zhao J., et al. Prevalence and secular trends in obesity among Chinese adults, 1991–2011. Am J Prev Med. 2015;49:661–669. doi: 10.1016/J.AMEPRE.2015.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Palaiodimos L., Kokkinidis D.G., Li W., Karamanis D., Ognibene J., Arora S., et al. Severe obesity, increasing age and male sex are independently associated with worse in-hospital outcomes, and higher in-hospital mortality, in a cohort of patients with COVID-19 in the Bronx,New York. Metabolism. 2020;108 doi: 10.1016/J.METABOL.2020.154262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Favre G., Legueult K., Pradier C., Raffaelli C., Ichai C., Iannelli A., et al. Visceral fat is associated to the severity of COVID-19. Metabolism. 2021;115 doi: 10.1016/J.METABOL.2020.154440/ATTACHMENT/6E45EDD2-EB7F-4609-A8BB-3F59D53FC351/MMC2.PDF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Huang Y., Lu Y., Huang Y.M., Wang M., Ling W., Sui Y., et al. Obesity in patients with COVID-19: a systematic review and meta-analysis. Metabolism. 2020;113 doi: 10.1016/J.METABOL.2020.154378/ATTACHMENT/554D76D1-70FA-4F5F-9AD1-CB630BDD72C5/MMC1.DOCX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Qu H.Q., Qu J., Glessner J., Hakonarson H. Mendelian randomization study of obesity and type 2 diabetes in hospitalized COVID-19 patients. Metabolism. 2022;129 doi: 10.1016/J.METABOL.2022.155156/ATTACHMENT/701A9F6A-50CC-4E5D-9A8C-D42725EEF909/MMC5.PDF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sanoudou D., Hill M.A., Belanger M.J., Arao K., Mantzoros C.S. Editorial: obesity, metabolic phenotypes and COVID-19. MetabClin Exp. 2022;128 doi: 10.1016/J.METABOL.2021.155121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang Y., Xu J., Wang Y., Hou H., Feng H., Yang H. An updated meta-analysis on the relationship between obesity and COVID-19 mortality. MetabClin Exp. 2021;122 doi: 10.1016/J.METABOL.2021.154820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Muscogiuri G., Pugliese G., Barrea L., Savastano S., Colao A. Commentary: obesity: the “Achilles heel” for COVID-19? Metabolism. 2020;108 doi: 10.1016/J.METABOL.2020.154251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dietz W., Santos-Burgoa C. 2020. Obesity obesity and its implications for COVID-19 mortality. [DOI] [PubMed] [Google Scholar]
- 46.Obesity report: COVID-19 death rates 10 times higher in countries where most adults are overweight - CNN. https://edition.cnn.com/2021/03/04/health/obesity-covid-death-rate-intl/index.html n.d.
- 47.Global excess deaths associated with COVID-19, January 2020 - December 2021. https://www.who.int/data/stories/global-excess-deaths-associated-with-covid-19-january-2020-december-2021 n.d.
- 48.Angelidi A.M., Kokkinos A., Katechaki E., Ros E., Mantzoros C.S. Mediterranean diet as a nutritional approach for COVID-19. MetabClin Exp. 2021;114 doi: 10.1016/J.METABOL.2020.154407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nakamura R., Mirelman A.J., Cuadrado C., Silva-Illanes N., Dunstan J., Suhrcke M. Evaluating the 2014 sugar-sweetened beverage tax in Chile: an observational study in urban areas. PLoS Med. 2018;15 doi: 10.1371/JOURNAL.PMED.1002596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Colchero M.A., Molina M., Guerrero-López C.M. After Mexico implemented a tax, purchases of sugar-sweetened beverages decreased and water increased: difference by place of residence, household composition, and income level. J Nutr. 2017;147:1552–1557. doi: 10.3945/JN.117.251892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Strategies to prevent & manage obesity | Overweight & Obesity | CDC. https://www.cdc.gov/obesity/strategies/index.html n.d.
- 52.SA Polyzos CS. Mantzoros Metreleptin for the treatment of lipodystrophy: leading the way among novel therapeutics for this unmet clinical need n.d. doi:10.1080/03007995.2022.2059974. [DOI] [PubMed]
- 53.GSH Yeo, DHM Chao, Siegert A.M., Koerperich Z.M., Ericson M.D., Simonds S.E., et al. The melanocortin pathway and energy homeostasis: from discovery to obesity therapy. Mol Metab. 2021;48 doi: 10.1016/J.MOLMET.2021.101206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Vosoughi K., Atieh J., Khanna L., Khoshbin K., Prokop L.J., Davitkov P., et al. Association of glucagon-like peptide 1 analogs and agonists administered for obesity with weight loss and adverse events: a systematic review and network meta-analysis-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/) eClinicalMedicine. 2021;42 doi: 10.1016/j.eclinm.2021.101213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kadouh H., Chedid V., Halawi H., Burton D.D., Clark M.M., Khemani D., et al. GLP-1 analog modulates appetite, taste preference, gut hormones, and regional body fat stores in adults with obesity. J Clin Endocrinol Metab. 2020;105 doi: 10.1210/CLINEM/DGZ140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lilly's tirzepatide delivered up to 22.5% weight loss in adults with obesity or overweight in SURMOUNT-1 2022.
- 57.Pilitsi E., Farr O.M., Polyzos S.A., Perakakis N., Nolen-Doerr E., Papathanasiou A.E., et al. Pharmacotherapy of obesity: available medications and drugs under investigation. MetabClin Exp. 2019;92:170–192. doi: 10.1016/J.METABOL.2018.10.010. [DOI] [PubMed] [Google Scholar]
- 58.Angelidi A.M., Belanger M.J., Kokkinos A., Koliaki C.C., Mantzoros C.S. Novel non-invasive approaches to the treatment of obesity: from pharmacotherapy to gene therapy. Endocr Rev. 2021 doi: 10.1210/ENDREV/BNAB034. [DOI] [PMC free article] [PubMed] [Google Scholar]