Abstract
Purpose of Review
Anterior cruciate ligament reconstruction (ACLR) is a common surgical procedure with an estimated 120,000 cases performed in the USA each year. Physical therapy plays a critical role in the successful recovery of both surgically and non-surgically managed patients. Interestingly, ACL rehabilitation protocols vary greatly with little consensus among practitioners. Nonetheless, there has been agreement over the last decade to shift from conservative, standardized length protocols to more accelerated, individualized protocols that vary in length and modalities based on patient-specific findings and preferences. This review summarizes the most recent trends, opinions, and modalities in ACL rehabilitation research, with a specific focus on novel methods to treat the specific psychosocial needs of ACL deficient patients.
Recent Findings
We found that new protocols emphasize early weight bearing, open kinetic chain (OKC) exercises, and other alternative modalities such as neuromuscular electrical stimulation and blood flow restriction. We also found a recent trend toward the use of clinical milestones to determine when a patient is ready for the next phase of a “step-up” rehabilitation program. One particularly nascent topic of research is the inclusion of methods to treat the psychosocial impacts of ACL injury, recovery, and the anxiety around return to sport.
Summary
Rehabilitation strategy has become increasingly patient-dependent, and the new modalities being utilized are accelerating patient recovery. Return to sport is a particularly important factor for many ACLR patients, and recovery has an important psychological component that has only recently been addressed in the literature, with positive preliminary findings.
Keywords: ACL, Physical therapy, Return to sport, Psychosocial
Introduction
The anterior cruciate ligament (ACL) is a broad, intraarticular, extra synovial ligament with attachments running from the postero-medial surface of the lateral femoral condyle to the anterior intercondylar surface of the tibia [1]. ACL tears are a relatively common injury with 80,000 and 120,000 cases each year in the USA [2–5]. Most patients with ACL injuries present after an acute, traumatic injury during sport or activity. The ACL is particularly susceptible to rotational stress, and tears are frequent in pivoting cutting and landing maneuvers. Patients with acute ACL rupture will classically present with a large joint effusion, instability, decreased range of motion, and pain with weight bearing after an acute, twisting injury of the knee. Patients with chronic ACL tears will experience periodic instability in the knee and generalized knee pain, specifically with cutting or pivoting movements. Physical exam findings and patient history are sufficient to diagnose the ACL-deficient knee. However, magnetic resonance imaging (MRI) remains critical in the evaluation and surgical planning of the ACL-deficient knee since concomitant meniscal injury is common and may require a combined or two-stage repair. There is no gold standard treatment for complete ACL rupture, with several studies finding no difference in satisfaction or activities of daily living between non-operative and operative groups [6–10]. Therefore, the decision to perform ACL reconstruction should take many factors into account, including the patient’s activity level, sports involvement, the extent of instability, and meniscal pathology [11, 12].
Interestingly, physical therapy has been shown to be critical to both surgical and non-surgical recovery and remains the most effective intervention clinicians can prescribe to regain strength, range of motion, and patient satisfaction [5, 7, 12, 13]. A great deal of research has gone into optimizing physical rehabilitation protocols for both surgical and non-surgical patients in recent years [11, 12, 14]. Specifically, the timing, duration, number of treatment modalities, and goals of therapy have been greatly debated, and options have expanded at an increasing rate [14–19]. The purpose of this article is to provide a concise and clinically relevant summary to the most recently published methods and trends in ACL rehabilitation, with a particular focus on recent evidence suggesting that patients, especially athletes, may benefit from psychosocial support during their recovery.
Differences in Surgical vs. Non-operative ACL Rehabilitation
The ACL-deficient knee is tolerated better by some than others, and the decision to perform surgery requires a lengthy and informed discussion based around the goals of the patient and their ability to tolerate rigorous rehabilitation. Non-operative treatment has typically been chosen by older, less active individuals and consists of early therapy, bracing, and activity modification [7,20]. There is debate about the efficacy of non-operative treatment of ACL injuries with some studies reporting satisfactory results, while others report that conservative management is inferior to operative management [4, 6, 8, 20]. A tool to help physicians identify who would benefit most from non-operative versus operative treatment was developed by the University of Delaware. This method seeks to identify patients who are able to tolerate ACL deficiency versus those that cannot by using a combination of provocative tests, such as single leg hop, in addition to frequency of instability after injury [7, 21]. This tool has been shown to be helpful in determining which patients may have enough compensatory restraint to tolerate ACL deficiency without repair and may be a useful tool to help stratify patients [21].
Segawa et al. looked at the outcomes of 89 non-operative ACL patients who were assigned to non-operative treatment due to age >40 or refusal of reconstruction with willingness to quit sport showed favorable patient-reported outcomes and an average satisfaction of 75% [10]. These results mirror previous work by Ciccotti et al. that showed satisfactory outcomes in 83% of patients treated with guided rehabilitation and activity modification although this cohort of patients were not offered operative management [6]. While these results are favorable, there is a consensus that younger individuals or those who want to maintain preinjury activity level should receive operative treatment [20].
Preoperative Rehabilitation
Preoperative rehabilitation, also known as “prehab,” has been actively researched in recent years with evidence to suggest a benefit with both subjective and objective patient outcomes. A multi-center cohort study compared outcomes from a prehab cohort (n = 192) and a control cohort (n = 1995) who did not undergo prehab and found that the prehab group had better international knee documentation committee (IKDC) scores and knee injury and osteoarthritis outcomes scores (KOOS) as well as a higher likelihood of returning to preinjury sport [22]. Additionally, several studies have suggested that prehab has the additional benefit of helping patients feel mentally prepared for the surgery itself [23–25]. The largest systematic review to date took place in 2017 and included 439 patients who either received full prehab or no prehab regimen. They found multiple studies that highlighted improved knee and muscle strength in the prehab group but no significant difference in quality of life or satisfaction between the prehab and the non-prehab groups [26]. More recently, a systematic review containing multiple randomized control trials by Giesche et al. concluded that prehabilitation was beneficial for patient-reported knee outcomes, improved physical exam findings, and allowed faster return to sport (34 weeks in prehab group versus 43 weeks in control group) [15, 16]. One small study (n = 20) demonstrating minimal differences with use of prehab showed a larger quadriceps cross-sectional area at the time of surgery in the prehab group that returned to baseline by 12 weeks post-op [15]. Interestingly, the same study observed higher single leg jump values in prehab group at 12 weeks postoperatively without any significant difference in the time to return to sport [15].
Historical Goals of ACL Rehabilitation
Although rehabilitation methods have changed dramatically, the goals of ACLR protocols have changed little over time, focusing heavily on preventing deficits in knee extension, restoring strength, and preserving stability. Indeed, multiple studies have shown that reestablishing quadriceps strength following ACLR contributes to dynamic stability for lower extremity, while preventing a predisposition to osteoarthritis [27, 28]. Moreover, patients with substantial preoperative quadriceps strength deficits have been shown to have decreased knee function after surgery [29, 30]. One of the first revised clinical practice guidelines to the orthopedic section of the American Physical Therapy Association (APTA) recommends immediate mobilization of the affected knee within 1 week after ACLR to increase range of motion and reduce adverse risk to surrounding soft tissue structures [31]. This early modification improved range of motion and spurred a wave of more aggressive studies culminating in the landmark review by Adams et al. in 2013 which definitively showed delayed weight bearing and ranging was associated with poor subjective and objective outcomes [32]. These data led to a major overhaul of the original ACLR rehabilitation guidelines created in 1996. The revised guidelines are centered around early weight bearing, immediate mobilization, incorporation of a step-up approach to non-weight-bearing and weight-bearing activities, and early achievement of full knee extension [32]. Furthermore, a 2013 study by Logerstedt et al. demonstrated that preoperative quadriceps strength levels are a significant predictor for self-reported knee function 6 months after surgery [33]. A 2009 cohort study by Eitzen et al. sought to identify preoperative indicators for knee function 2 years following ACLR and found that preoperative quadriceps strength level deficits above 20% had significantly larger strength deficits 2 years after surgery [29].
Although it became clear that early activity and weight bearing was critical to preserving range and function, a new debate opened as to what specific early activities were the safest to achieve this goal. This created a discussion as to what was considered “too aggressive,” placing the patient at unnecessary risk of reinjury for increasingly diminished returns. This debate is ongoing and particularly active around the safety and efficacy of closed chain vs. open chain kinetic exercise.
The question of how and when to utilize closed chain kinetic exercises (CKC) and/or open chain kinetic exercises (OKC) during ACLR postoperative rehabilitation has been a relatively new and ongoing topic of debate. Many studies have attempted to delineate whether CKC or OKC are equivalent, with mixed results across time. In 2010, Glass et al. performed a systematic review of six randomized control trials comparing CKC vs. OKC and found no differences between the two rehabilitation groups in terms of knee stability, anterior tibial translation, and pain for both ACL deficient and reconstructed patients [34]. Table 1 provides a list of the literature for open versus closed kinetic chain exercises during ACL rehabilitation.
Table 1.
Summary of recent open-chain vs. closed-chain evidence in ACLR rehabilitation
| Source | Primary outcomes | Study design | Findings | Level of evidence |
|---|---|---|---|---|
| Glass et al. [34] | Pain, ROM, laxity, and strength | Systematic review: OKC vs. CKC | No difference in subjective or objective outcomes | Level 2 |
| Lobb et al. [35] | Pain, ROM, laxity, and strength | Systematic review : OKC vs. CKC | No difference in strength, laxity, or patient-reported function | Level 2 |
| Wright et al. [36] | Pain, ROM, laxity, and strength | Systematic review: OKC vs. CKC | CKC group experienced lower pain and laxity. | Level 2 |
| Taggeson et al. [37] | Tibial translation, jump performance, ROM | RCT: OKC vs. CCK | Increased strength in OKC group. No differences in laxity, strength, and function | Level 1 |
| Mikkelsen et al. [38] | Knee laxity, quadriceps strength, hamstring torque, patient satisfaction | Prospective case-control: CKC vs. CKC + OKC | Increased strength in OCK group. No differences in laxity, strength, pain, and satisfaction | Level 2 |
| Fukuda et al. [39] | Strength, single-legged hop, and laxity | RCT: early-start vs. late-start OCK | Early start group showed greater quadriceps strength. No other significant differences between groups | Level 1 |
| Melick et al. [40] | Anterior knee laxity, quadriceps strength, hamstring torque, patient satisfaction | Retrospective cohort: OKC vs. CKC | No difference in laxity, strength, ROM, or physical function with early or late introduction of OKC | Level 3 |
| Heijne et al. [41] | ROM, knee laxity, postural sway, thigh muscle torque, and anterior knee pain | RCT: early post-op OKC vs. late | Early start OKC showed significantly increased anterior knee laxity in comparison with late start for hamstring graft. No difference between groups for BPTB grafts | Level 1 |
Whether open kinetic chain (OKC) exercise is safe and beneficial for ACLR rehabilitation remains a topic of active debate. OKC exercise has been avoided in ACLR rehabilitation due to early studies by groups like Henning et al. [42] that suggested OKC produced greater strain through than closed kinetic chain (CKC) exercise. Interestingly, the majority of studies have found no differences between OKC and CKC in terms of reinjury rate and time to return to sport. Above is the summary of the evidence surrounding OKC versus CKC exercises in the setting of ACLR.
New Methods in ACL Rehabilitation
The implementation of neuromuscular electrical stimulation (NMES), blood flow restriction, psychosocial support, and early contralateral lower extremity conditioning are a few relatively new and exciting modalities in ACLR rehabilitation that are gaining in popularity [11]. Kinesio taping has been another type of support utilized in the acute phase of ACLR recovery and one randomized control trial to date has shown that when used with standard rehabilitation, kinesio taping can help to reduce subjective pain and swelling [17].
Neuromuscular electrical stimulation (NMES) during postoperative ACLR rehabilitation has demonstrated the ability to effectively increase quadriceps strength and reduce strength deficits [31, 43]. To maximize quadriceps strength following ACLR, NMES seeks to facilitate recruitment of inhibited arthrogenic muscle (AMI) resulting in increased activation of a larger proportion of type IIA muscle fibers, delaying muscle atrophy [44]. When applied at high intensity during the recovery period, NMES has shown to be successful in combating early muscle atrophy and preserving strength [36]. A randomized clinical trial by Snyder et al. found that 4 weeks of active exercise combined with high-intensity NMES resulted in quadriceps strength of nearly 70% relative to the uninjured limb at postoperative 2 months. This is in contrast to patients in the active exercise only group who demonstrated quadriceps strength of 51% relative to the uninjured limb [45]. However, the intensity of electrode application during NMES can be intolerable for patients, especially during certain knee flexion angles, thus modified NMES methods have focused on reduction of electrode intensity, allowing patients to dictate maximum tolerable intensity and have yielded favorable results [46]. A 2019 randomized control trial by Wright et al. showed that electrical stimulation helped to increase quadriceps circumference and combat atrophy more than exercise alone [18]. Fitzgerald et al. performed another randomized control trial between an NMES training and non-NMES training group during ACLR recovery and found the NMES group demonstrated greater quadriceps strength and higher levels of self-reported knee function at 12 weeks postoperatively in addition to advancing to agility training faster at 16 weeks postoperatively [46]. Furthermore, a 2019 randomized control trial by Kaya et al. studying ACLR recovery in two groups, one using lower extremity neuromuscular control exercises and the other using standard therapy, found that lower extremity strength recovered more quickly in neuromuscular control exercise group but that there was no difference in proprioception [47]. Future studies should continue to evaluate the effects of NMES ACLR rehabilitation programs for different time periods, graft types, and athletes of all activity levels.
Cross-education of the contralateral leg during ACLR rehabilitation can be helpful in alleviating bilateral impairments due to deviations of the sensorimotor and musculoskeletal system because of injury and surgery. A 2018 randomized control trial by Zult et al. with a cross-education group and standard ACLR rehabilitation group found no significant difference in functional measures or speed of ACLR recovery between the groups [48]. However, another randomized control trial in 2019 by Harput et al. showed that concentric and eccentric quadriceps strength levels recovered more quickly when patients utilized cross-education, especially in the early rehabilitation phase of ACLR [49].
Blood flow restriction is another modality that is being used during rehabilitation to accelerate recovery. Two recent systematic reviews concluded that there is evidence for blood flow restriction therapy in promoting muscle hypertrophy, increasing strength, and decreasing patient-reported pain scores, but both suggested that more research is needed before recommending clinically [50, 51]. Blood flow restriction in addition to traditional rehabilitation helps to reverse muscle atrophy, decrease the recovery time, and also prevents bone loss [52].
Psychosocial Approach to Return to Sport
Returning to sport and preinjury level of performance is a primary goal following ACLR surgery, yet reinjury always poses a barrier to achieving this goal. At 2 years postoperatively following ACLR, patients are nearly six times more likely to suffer a second ACL injury with females at a significantly greater risk than men [53]. Although subsequent ACL injuries occur with a high frequency, substantial variability in the rate of second injuries remains, due to several functional, surgical, rehabilitation, and biological factors [54–57]. A 2014 systematic review performed by Ardern et al., based on 69 articles and including 7556 patients who underwent ACLR surgery, demonstrated that 81% returned to any sport, 65% returned to preinjury level of sport, and 55% returned to competitive level sport following ACLR [58]. These numbers were updated from a previous 2011 review by Ardern et al. of 48 studies and 5770 patients that demonstrated an 82% return to sport of some kind, 63% return to preinjury level sport, and 44% return to competitive sport at final follow-up [59]. Both recent reviews suggest return to sport rate at preinjury and competitive levels may be less than expected following ACLR. Moreover, a 2018 systematic review of ACLR return to sport by Kay et al. of 20 studies and 1156 patients with a mean age of 14.3 found a 92% return to sport of any kind, 78.6% return to preinjury level, and 81% return to competitive sport, suggesting a higher return to sport rate for the younger athlete following ACLR [60].
Return to sport also puts graft healing, rupture, and incorporation at risk, thus determining an exact timeframe to resumption of sport participation can be difficult [61]. In 2020, the Panther Symposium ACL Injury Return to Sport Consensus Group, a multidisciplinary group of international ACL and research experts, sought to develop a definitive return to sport criteria and a description of the dynamic return to sport continuum after ACLR [62]. The resultant consensus stated return to sport is characterized by “achieving the preinjury level of sports participation as defined by the same type, frequency, intensity, and quality of performance as before injury” [62]. Furthermore, the consensus recommends abandoning purely time-based return to sport protocol and advancing through a multidisciplinary, criterion-based progression focused on meeting specific clinical and objective milestones that involve validated, peer-reviewed return to sport testing of functional assessment and psychological readiness which consider biological healing, concomitant injuries, and contextual factors in the ACLR recovery process [62].
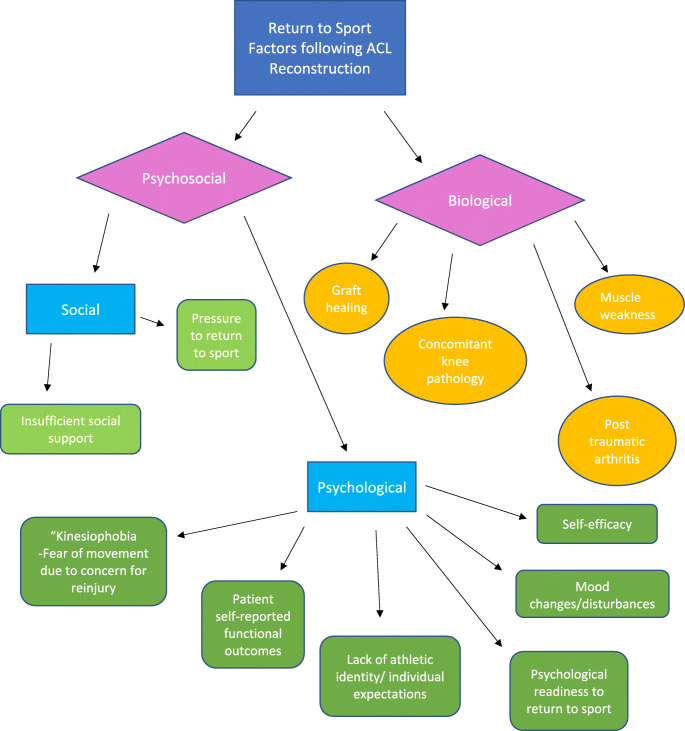
ACL injuries often occur concomitantly with other knee pathology including ligamentous, meniscus, and cartilage injuries that may affect return to sport rates and functional outcomes. Cartilaginous lesions suffered prior to or during ACL injury can lengthen the return to sport timeline of patients following ACLR given the longer healing period required for cartilaginous lesions within the knee joint [63]. The same review emphasized the need to evaluate concomitant knee pathology and preexisting injuries or conditions that may interfere with postoperative rehabilitation. They found that patient sport must also be considered when choosing a rehabilitation plan and will help to identify unique functional goals that could necessitate larger emphasis on pivoting, cutting, and shifting [63]. Thus, returning to sport too early following ACLR poses a risk of sustaining damage to menisci and other or articular surfaces within the knee joint. A 2016 editorial by Culvenor et al. suggested that return to sport less than 12 months after ACLR may cause an increased risk of osteoarthritis and reinjury and advocated for a longer return to sport timeline to optimize long-term functional performance [64]. The complex biopsychosocial components to return to sport are detailed in Fig. 1.
Fig. 1.
Psychosocial factors effecting recovery after ACLR. The flow chart above represents the many different physical and psychosocial factors effecting ACL injury and recovery. Until recently, many of these psychosocial factors were not addressed by the clinician or therapist. However, recent evidence suggests that addressing the anxiety and depression associated with ACLR, especially regarding return to sport, positively benefits patient outcomes. These data suggest that including simple support mechanisms in ACLR recovery protocols would likely have a positive effect and should be considered by both clinicians and physical therapists
Psychosocial Impact and Support After ACL Injury
Physical and biological factors alone cannot solely explain reasons for not returning to sport in a timely fashion. Recent evidence has shown that social and psychological variables may explain a delay in both performance and return to play following ACLR. A case-control study performed by Lentz et al. identified potential motivational and psychosocial barriers that can affect return to sport outcomes following ACLR [65]. They found that pain-related fear of movement and reinjury can cause patients to have delayed or lack of return to sport due to fear of reinjury or lack of confidence [65]. Additionally, these psychosocial characteristics that delayed return to sport timelines were associated with quadriceps weakness and lower self-reported levels of function, suggesting that a larger focus should be placed on the multifactorial variables that affect functional outcomes following ACLR [65].
Recent literature has highlighted the effect of psychological factors in patients sustaining ACL injuries and during ACLR recovery [59, 66–69]. Readiness to return to sport, fear of reinjury, patient-reported outcomes, and adherence to rehabilitation have been described to be affected by psychological variables for athletes during ACLR rehabilitation [66, 68, 69]. For instance, a 2004 study by Brewer et al. demonstrated a significant positive correlation between adherence to postoperative physical therapy and patient subjective outcomes 6 months following ACLR [70]. Thomeé et al. developed an established Knee Self Efficacy Scale (K-SES) and found that higher postoperative self-efficacy was positively associated with higher postoperative activity levels and physical functioning [71]. Another study by Thomeé et al. demonstrated preoperative self-efficacy levels are significant predictors of postoperative physical activity, return to sport, subjective knee function, and single leg hop test 1 year following ACLR [72]. Additionally, a study by Udry et al. indicated that preoperative mood levels and psychological readiness for ACLR surgery may influence adherence to postoperative physical therapy and patient levels of self-efficacy following surgery [73].
Fear of reinjury and readiness to return to sport are among the most common psychological issues athletes face during ACLR recovery. Commonly, athletes’ concerns include the inability to perform at previous athletic levels, insufficient social support, lack of athletic identity, or pressure to return to sport [74]. Kinesiophobia is defined as the “fear of movement as a result of a feeling of susceptibility to pain or reinjury” and a 2019 study by Theunissen et al. revealed preoperative kinesiophobia is a strong predictor for postoperative kinesiophobia [75]. Moreover, a study by Kvist et al. revealed a 53% return to preinjury level activity up to 4 years following ACLR and patients who did not return to preinjury activity had more fear of reinjury, as measured by the Tampa Scale of Kinesiophobia (TSK) [76]. A 2012 study by McCullough et al. of high school and college football athletes found a 63% and 69% return to sport, respectively, but only 43% of athletes were able to return to preinjury level performance [77]. This same study revealed fear of reinjury cited by 50% of athletes for their main reason of sport cessation [77]. In a 2011 meta-analysis and systematic review by Ardern et al. of 48 studies and 57,770 patients, at a mean of 41.5 months follow-up only 44% of athletes returned to a competitive level of sport and cited fear of reinjury as the most common reason for sport participation cessation and postoperative activity reduction [59]. Furthermore, a 2013 case-control study by Ardern et al. of 187 athletes demonstrated a 31% return preinjury level of sports participation 12 months following ACLR surgery and that psychological readiness to return to sport, fear of reinjury, locus of control, and individual athletic expectations were significant predictors to return to preinjury sport performance 12 months postoperatively [67].
ACLR surgery and recovery requires substantial emotional and physical commitment from athletes that may result in psychological and emotional disturbances that affect the course of rehabilitation. A prospective longitudinal study by Morrey et al. found that competitive athletes experienced significant mood changes 6 months following surgery with greater mood disturbances and recovery rates compared with recreational athletes [78]. Moreover, Langford et al. showed that athletes who returned to competitive sport at 12 months postoperatively scored significantly higher on the ACL Return to Sport After Injury Scale (ACL-RSI) at both 6 and 12 months following ACLR, demonstrating a more positive psychological response about resuming sports participation at both periods [79]. After injury, athletes may suffer from a loss of athletic identity in response to a threat to positive self-image associated with previous sport ability [66]. A prospective study by Brewer et al. revealed a significant decrease in athletic identity over the 24-month postoperative period as measured by the Athletic Identity Measurement Scale (AIMS), with the most substantial decrease between 6 and 12 months postoperatively [80]. Additionally, a 2021 study by Ohji et al. revealed that athletes who returned to preinjury level competitive levels of sport following ACLR reported significantly higher levels of athletic identity and sport commitment and lower kinesiophobia [81].
In order to better understand the psychological and emotional variables that affect patients during ACLR recovery, the orthopedic surgeon should be equipped with a baseline knowledge of the multifactorial psychosocial variables that affect the trajectory of a patient’s rehabilitation following ACLR surgery. While the detailed psychological assessment of a patient’s psyche and emotional state are beyond the scope of an orthopedic surgeon’s expertise, the surgeon can still play a critical role in screening for maladaptive psychological behavior and identifying psychological at-risk patients early in the surgical and rehabilitation process. Future considerations for ACLR recovery should consider the psychological and emotional factors that influence ACLR recovery and the importance of incorporating a more holistic approach to maximize patient outcomes.
Conclusion
ACLR rehabilitation has become increasingly individualized due to advancements in surgical techniques and rehabilitation methods. Rehabilitation protocols have shown a shift toward a patient-centered approach, with protocols modifiable to patient-specific needs and pace of progress. These patient-specific protocols have shown increased patient performance and earlier return to sport. The current literature behind non-operative treatment of ACL injuries and prehabilitation prior to ACL surgery are evaluated to determine its proper implementation and efficacy. An accelerated ACLR rehabilitation protocol continues to be an ongoing topic of debate behind ACL literature, and we report data pertaining to its effectiveness, utilization, and safety. The latest studies and strategies toward regaining strength and range of motion after ACLR are assessed in hopes of establishing a clearer consensus for the implementation strength and range of motion modalities during rehabilitation. Return to sport rates and outcomes are thoroughly assessed from a multidisciplinary perspective. Biological and physical factors alone cannot predict patient return to sport rates and functional outcomes after surgery, and we emphasize the necessity for the surgeon and all members of the healthcare team to screen for and evaluate patient psychological variables that may influence the patient’s return to sport timeline and functionality following ACLR. With this review, we present a careful analysis and summary of non-operative and preoperative rehabilitation treatment strategies, accelerated rehabilitation protocols, strategies toward gaining strength and range of motion during ACLR recovery, and the biopsychosocial factors that influence return to sport, while stressing the value of further clinical research into these rehabilitation topics to optimize patient outcomes following surgery.
Declarations
Conflict of Interest
Sarah Jenkins, Alvarho Guzman, Brandon Gardner, Stewart Bryant, Shane Rayos del Sol, and Patrick McGahan declare that they have no conflict of interest. James Chen has received personal fees from Arthrex outside of published work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Sports Injuries and Rehabilitation: Getting Athletes Back to Play
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.DePhillipo NN, Moatshe G, Brady A, Chahla J, Aman ZS, Dornan GJ, et al. Effect of meniscocapsular and meniscotibial lesions in ACL-deficient and ACL-reconstructed knees: a biomechanical study. Am J Sports Med. 2018;46:2422–2431. doi: 10.1177/0363546518774315. [DOI] [PubMed] [Google Scholar]
- 2.Gornitzky AL, Lott A, Yellin JL, Fabricant PD, Lawrence JT, Ganley TJ. Sport-specific yearly risk and incidence of anterior cruciate ligament tears in high school athletes: a systematic review and meta-analysis. Am J Sports Med. 2016;44:2716–2723. doi: 10.1177/0363546515617742. [DOI] [PubMed] [Google Scholar]
- 3.Cimino F, Volk BS, Setter D. Anterior cruciate ligament injury: diagnosis, management, and prevention. Am Fam Physician. 2010;82:917–922. [PubMed] [Google Scholar]
- 4.Ramski DE, Kanj WW, Franklin CC, Baldwin KD, Ganley TJ. Anterior cruciate ligament tears in children and adolescents: a meta-analysis of nonoperative versus operative treatment. Am J Sports Med. 2014;42:2769–2776. doi: 10.1177/0363546513510889. [DOI] [PubMed] [Google Scholar]
- 5.Bogunovic L, Matava MJ. Operative and nonoperative treatment options for ACL tears in the adult patient: a conceptual review. Phys Sportsmed. 2013;41:33–40. doi: 10.3810/psm.2013.11.2034. [DOI] [PubMed] [Google Scholar]
- 6.Ciccotti MG, Lombardo SJ, Nonweiler B, Pink M. Non-operative treatment of ruptures of the anterior cruciate ligament in middle-aged patients. Results after long-term follow-up. J Bone Joint Surg Am. 1994;76:1315–1321. doi: 10.2106/00004623-199409000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Paterno MV. Non-operative care of the patient with an ACL-deficient knee. Curr Rev Musculoskelet Med. 2017;10:322–327. doi: 10.1007/s12178-017-9431-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moksnes H, Risberg MA. Performance-based functional evaluation of non-operative and operative treatment after anterior cruciate ligament injury. Scand J Med Sci Sports. 2009;19:345–355. doi: 10.1111/j.1600-0838.2008.00816.x. [DOI] [PubMed] [Google Scholar]
- 9.Smith TO, Postle K, Penny F, McNamara I, Mann CJV. Is reconstruction the best management strategy for anterior cruciate ligament rupture? A systematic review and meta-analysis comparing anterior cruciate ligament reconstruction versus non-operative treatment. Knee. 2014;21:462–470. doi: 10.1016/j.knee.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 10.Segawa H, Omori G, Koga Y. Long-term results of non-operative treatment of anterior cruciate ligament injury. Knee. 2001;8:5–11. doi: 10.1016/S0968-0160(00)00062-4. [DOI] [PubMed] [Google Scholar]
- 11.Andrade R, Pereira R, van Cingel R, Staal JB, Espregueira-Mendes J. How should clinicians rehabilitate patients after ACL reconstruction? A systematic review of clinical practice guidelines (CPGs) with a focus on quality appraisal (AGREE II) Br J Sports Med. 2020;54:512–519. doi: 10.1136/bjsports-2018-100310. [DOI] [PubMed] [Google Scholar]
- 12.Filbay SR, Grindem H. Evidence-based recommendations for the management of anterior cruciate ligament (ACL) rupture. Best Pract Res Clin Rheumatol. 2019;33:33–47. doi: 10.1016/j.berh.2019.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paterno MV, Schmitt LC, Thomas S, Duke N, Russo R, Quatman-Yates CC. Patient and parent perceptions of rehabilitation factors that influence outcomes after anterior cruciate ligament reconstruction and clearance to return to sport in adolescents and young adults. J Orthop Sports Phys Ther. 2019;49:576–583. doi: 10.2519/jospt.2019.8608. [DOI] [PubMed] [Google Scholar]
- 14.Forrester LA, Schweppe EA, Popkin CA. Variability in rehabilitation protocols following pediatric anterior cruciate ligament (ACL) reconstruction. Phys Sportsmed. 2019;47:448–454. doi: 10.1080/00913847.2019.1622472. [DOI] [PubMed] [Google Scholar]
- 15.Shaarani SR, O’Hare C, Quinn A, Moyna N, Moran R, O’Byrne JM. Effect of prehabilitation on the outcome of anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41:2117–2127. doi: 10.1177/0363546513493594. [DOI] [PubMed] [Google Scholar]
- 16.Giesche F, Niederer D, Banzer W, Vogt L. Evidence for the effects of prehabilitation before ACL-reconstruction on return to sport-related and self-reported knee function: a systematic review. PLoS One. 2020;15:e0240192. doi: 10.1371/journal.pone.0240192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Balki S, Göktaş HE, Öztemur Z. Kinesio taping as a treatment method in the acute phase of ACL reconstruction: a double-blind, placebo-controlled study. Acta Orthop Traumatol Turc. 2016;50:628–634. doi: 10.1016/j.aott.2016.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wright AR, Richardson AB, Kikuchi CK, Goldberg DB, Marumoto JM, Kan DM. Effectiveness of accelerated recovery performance for post-ACL reconstruction rehabilitation. Hawaii J Health Soc Welf. 2019;78:41–46. [PMC free article] [PubMed] [Google Scholar]
- 19.Beynnon BD, Johnson RJ, Naud S, Fleming BC, Abate JA, Brattbakk B, et al. Accelerated versus nonaccelerated rehabilitation after anterior cruciate ligament reconstruction: a prospective, randomized, double-blind investigation evaluating knee joint laxity using roentgen stereophotogrammetric analysis. Am J Sports Med. 2011;39:2536–2548. doi: 10.1177/0363546511422349. [DOI] [PubMed] [Google Scholar]
- 20.Fabricant PD, Lakomkin N, Cruz AI, Spitzer E, Marx RG. ACL reconstruction in youth athletes results in an improved rate of return to athletic activity when compared with non-operative treatment: a systematic review of the literature. J ISAKOS: Joint Disord Orthop Sports Med. 2016;1:62–69. doi: 10.1136/jisakos-2015-000013. [DOI] [Google Scholar]
- 21.Fitzgerald GK, Axe MJ, Snyder-Mackler L. A decision-making scheme for returning patients to high-level activity with nonoperative treatment after anterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc. 2000;8:76–82. doi: 10.1007/s001670050190. [DOI] [PubMed] [Google Scholar]
- 22.Failla MJ, Logerstedt DS, Grindem H, Axe MJ, Risberg MA, Engebretsen L, et al. Does extended preoperative rehabilitation influence outcomes 2 years after ACL reconstruction?: a comparative effectiveness study between the MOON and Delaware-Oslo ACL cohorts. Am J Sports Med. 2016;44:2608–2614. doi: 10.1177/0363546516652594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gokeler A, Dingenen B, Mouton C, Seil R. Clinical course and recommendations for patients after anterior cruciate ligament injury and subsequent reconstruction: a narrative review. EFORT open reviews. Br Editorial Soc Bone Joint Surg Lond. 2017;2:410–420. doi: 10.1302/2058-5241.2.170011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wilk KE, Arrigo CA. Preoperative phase in the rehabilitation of the patient undergoing anterior cruciate ligament reconstruction. Oper Tech Sports Med. 2016;24:12–20. doi: 10.1053/j.otsm.2015.10.003. [DOI] [Google Scholar]
- 25.Claudia-Camelia B. Study on the effectiveness of the accelerated rehabilitation strategies of the knee in professional athletes after anterior cruciate ligament injury. Procedia-Soc Behav Sci. 2013;76:151–155. doi: 10.1016/j.sbspro.2013.04.090. [DOI] [Google Scholar]
- 26.Alshewaier S, Yeowell G, Fatoye F. The effectiveness of pre-operative exercise physiotherapy rehabilitation on the outcomes of treatment following anterior cruciate ligament injury: a systematic review. Clin Rehabil. 2017;31:34–44. doi: 10.1177/0269215516628617. [DOI] [PubMed] [Google Scholar]
- 27.Suter E, Herzog W. Does muscle inhibition after knee injury increase the risk of osteoarthritis. Exerc Sport Sci Rev. 2000;28:15–18. [PubMed] [Google Scholar]
- 28.Thomas AC, Villwock M, Wojtys EM, Palmieri-Smith RM. Lower extremity muscle strength after anterior cruciate ligament injury and reconstruction. J Athl Train. 2013;48:610–620. doi: 10.4085/1062-6050-48.3.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eitzen I, Holm I, Risberg MA. Preoperative quadriceps strength is a significant predictor of knee function two years after anterior cruciate ligament reconstruction. Br J Sports Med. 2009;43:371–376. doi: 10.1136/bjsm.2008.057059. [DOI] [PubMed] [Google Scholar]
- 30.de Jong SN, van Caspel DR, van Haeff MJ, Saris DBF. Functional assessment and muscle strength before and after reconstruction of chronic anterior cruciate ligament lesions. Arthroscopy. 2007;23(21–8):28.e1–28.e3. doi: 10.1016/j.arthro.2006.08.024. [DOI] [PubMed] [Google Scholar]
- 31.Logerstedt DS, Snyder-Mackler L, Ritter RC, Axe MJ, Godges JJ. Knee stability and movement coordination impairments: knee ligament sprain. J Orthop Sports Phys Ther. 2010;40:A1–37. doi: 10.2519/jospt.2010.0303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Adams D, Logerstedt D, Hunter-Giordano A, Axe MJ, Snyder-Mackler L. Current concepts for anterior cruciate ligament reconstruction: a criterion-based rehabilitation progression. J Orthop Sports Phys Ther. 2012;42:601–614. doi: 10.2519/jospt.2012.3871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Logerstedt D, Lynch A, Axe MJ, Snyder-Mackler L. Pre-operative quadriceps strength predicts IKDC2000 scores 6 months after anterior cruciate ligament reconstruction. Knee. 2013;20:208–212. doi: 10.1016/j.knee.2012.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Glass R, Waddell J, Hoogenboom B. The effects of open versus closed kinetic chain exercises on patients with ACL deficient or reconstructed knees: a systematic review. N Am J Sports Phys Ther. 2010;5:74–84. [PMC free article] [PubMed] [Google Scholar]
- 35.Lobb R, Tumilty S, Claydon LS. A review of systematic reviews on anterior cruciate ligament reconstruction rehabilitation. Phys Ther Sport Off J Assoc Chart Physiother Sports Med. 2012;13:270–8. [DOI] [PubMed]
- 36.Wright RW, Preston E, Fleming BC, Amendola A, Andrish JT, Bergfeld JA, et al. A systematic review of anterior cruciate ligament reconstruction rehabilitation – part II: open versus closed kinetic chain exercises, neuromuscular electrical stimulation, accelerated rehabilitation, and miscellaneous topics. J Knee Surg. 2008;21:225–234. doi: 10.1055/s-0030-1247823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tagesson S, Öberg B, Good L, Kvist J. A Comprehensive Rehabilitation Program with Quadriceps Strengthening in Closed versus Open Kinetic Chain Exercise in Patients with Anterior Cruciate Ligament Deficiency: A Randomized Clinical Trial Evaluating Dynamic Tibial Translation and Muscle Function. Am J Sports Med. SAGE Publications Inc STM; 2008;36:298–307. [DOI] [PubMed]
- 38.Mikkelsen C, Werner S, Eriksson E. Closed kinetic chain alone compared to combined open and closed kinetic chain exercises for quadriceps strengthening after anterior cruciate ligament reconstruction with respect to return to sports: a prospective matched follow-up study. Knee Surg Sports Traumatol Arthrosc. Springer; 2000;8:337–42. [DOI] [PubMed]
- 39.Fukuda TY, Fingerhut D, Moreira VC, Camarini PMF, Scodeller NF, Duarte A, et al. Open Kinetic Chain Exercises in a Restricted Range of Motion After Anterior Cruciate Ligament Reconstruction: A Randomized Controlled Clinical Trial. Am J Sports Med. SAGE Publications Inc STM; 2013;41:788–94. [DOI] [PubMed]
- 40.Melick N van, Cingel REH van, Brooijmans F, Neeter C, Tienen T van, Hullegie W, et al. Evidence-based clinical practice update: practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br J Sports Med. BMJ Publishing Group Ltd and British Association of Sport and Exercise Medicine; 2016;50:1506–15. [DOI] [PubMed]
- 41.Heijne A, Werner S. Early versus late start of open kinetic chain quadriceps exercises after ACL reconstruction with patellar tendon or hamstring grafts: a prospective randomized outcome study. Knee Surg Sports Traumatol Arthrosc. 2007;15:402–14. [DOI] [PubMed]
- 42.Henning CE, Lynch MA, Glick KR. An in vivo strain gage study of elongation of the anterior cruciate ligament. Am J Sports Med. SAGE Publications Inc STM; 1985;13:22–6. [DOI] [PubMed]
- 43.Kim K-M, Croy T, Hertel J, Saliba S. Effects of neuromuscular electrical stimulation after anterior cruciate ligament reconstruction on quadriceps strength, function, and patient-oriented outcomes: a systematic review. J Orthop Sports Phys Ther. 2010;40:383–391. doi: 10.2519/jospt.2010.3184. [DOI] [PubMed] [Google Scholar]
- 44.Palmieri-Smith RM, Thomas AC, Wojtys EM. Maximizing quadriceps strength after ACL reconstruction. Clin Sports Med. 2008;27:405–424. doi: 10.1016/j.csm.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 45.Snyder-Mackler L, Delitto A, Bailey SL, Stralka SW. Strength of the quadriceps femoris muscle and functional recovery after reconstruction of the anterior cruciate ligament. A prospective, randomized clinical trial of electrical stimulation. JBJS. 1995;77:1166–1173. doi: 10.2106/00004623-199508000-00004. [DOI] [PubMed] [Google Scholar]
- 46.Fitzgerald GK, Piva SR, Irrgang JJ. A modified neuromuscular electrical stimulation protocol for quadriceps strength training following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2003;33:492–501. doi: 10.2519/jospt.2003.33.9.492. [DOI] [PubMed] [Google Scholar]
- 47.Kaya D, Guney-Deniz H, Sayaca C, Calik M, Doral MN. Effects on lower extremity neuromuscular control exercises on knee proprioception, muscle strength, and functional level in patients with ACL reconstruction. Biomed Res Int. 2019;2019:1694695. doi: 10.1155/2019/1694695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zult T, Gokeler A, van Raay JJAM, Brouwer RW, Zijdewind I, Farthing JP, et al. Cross-education does not accelerate the rehabilitation of neuromuscular functions after ACL reconstruction: a randomized controlled clinical trial. Eur J Appl Physiol. 2018;118:1609–1623. doi: 10.1007/s00421-018-3892-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Harput G, Ulusoy B, Yildiz TI, Demirci S, Eraslan L, Turhan E, et al. Cross-education improves quadriceps strength recovery after ACL reconstruction: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2019;27:68–75. doi: 10.1007/s00167-018-5040-1. [DOI] [PubMed] [Google Scholar]
- 50.Lu Y, Patel BH, Kym C, Nwachukwu BU, Beletksy A, Forsythe B, et al. Perioperative blood flow restriction rehabilitation in patients undergoing ACL reconstruction: a systematic review. Orthop J Sports Med. 2020;8:2325967120906822. doi: 10.1177/2325967120906822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Charles D, White R, Reyes C, Palmer D. A systematic review of the effects of blood flow restriction training on quadriceps muscle atrophy and circumference post ACL reconstruction. Int J Sports Phys Ther. 2020;15:882–891. doi: 10.26603/ijspt20200882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lambert B, Hedt CA, Jack RA, Moreno M, Delgado D, Harris JD, et al. Blood flow restriction therapy preserves whole limb bone and muscle following ACL reconstruction. Orthop J Sports Med. 2019;7:2325967119S00196. doi: 10.1177/2325967119S00196. [DOI] [Google Scholar]
- 53.Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42:1567–1573. doi: 10.1177/0363546514530088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kaeding CC, Aros B, Pedroza A, Pifel E, Amendola A, Andrish JT, et al. Allograft versus autograft anterior cruciate ligament reconstruction: predictors of failure from a MOON prospective longitudinal cohort. Sports Health. 2011;3:73–81. doi: 10.1177/1941738110386185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J. A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med. 2007;35:564–574. doi: 10.1177/0363546506296042. [DOI] [PubMed] [Google Scholar]
- 56.Salmon L, Russell V, Musgrove T, Pinczewski L, Refshauge K. Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. Arthrosc J Arthrosc Relat Surg. 2005;21:948–957. doi: 10.1016/j.arthro.2005.04.110. [DOI] [PubMed] [Google Scholar]
- 57.Wright RW, Dunn WR, Amendola A, Andrish JT, Bergfeld J, Kaeding CC, et al. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a prospective MOON cohort study. Am J Sports Med. 2007;35:1131–1134. doi: 10.1177/0363546507301318. [DOI] [PubMed] [Google Scholar]
- 58.Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48:1543–1552. doi: 10.1136/bjsports-2013-093398. [DOI] [PubMed] [Google Scholar]
- 59.Ardern CL, Webster KE, Taylor NF, Feller JA. Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011;45:596–606. doi: 10.1136/bjsm.2010.076364. [DOI] [PubMed] [Google Scholar]
- 60.Kay J, Memon M, Marx RG, Peterson D, Simunovic N, Ayeni OR. Over 90% of children and adolescents return to sport after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2018;26:1019–1036. doi: 10.1007/s00167-018-4830-9. [DOI] [PubMed] [Google Scholar]
- 61.Webster KE, Feller JA. A research update on the state of play for return to sport after anterior cruciate ligament reconstruction. J Orthop Traumatol. 2019;20:10. doi: 10.1186/s10195-018-0516-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Meredith SJ, Rauer T, Chmielewski TL, Fink C, Diermeier T, Rothrauff BB, et al. Return to sport after anterior cruciate ligament injury: Panther Symposium ACL Injury Return to Sport Consensus Group. Orthop J Sports Med. 2020;8:2325967120930829. doi: 10.1177/2325967120930829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zaffagnini S, Grassi A, Serra M, Marcacci M. Return to sport after ACL reconstruction: how, when and why? A narrative review of current evidence. Joints. 2015;3:25–30. [PMC free article] [PubMed] [Google Scholar]
- 64.Culvenor AG, Crossley KM. Accelerated return to sport after anterior cruciate ligament injury: a risk factor for early knee osteoarthritis? Br J Sports Med. 2016;50:260–261. doi: 10.1136/bjsports-2015-095542. [DOI] [PubMed] [Google Scholar]
- 65.Lentz TA, Zeppieri G, Jr, George SZ, Tillman SM, Moser MW, Farmer KW, et al. Comparison of physical impairment, functional, and psychosocial measures based on fear of reinjury/lack of confidence and return-to-sport status after ACL reconstruction. Am J Sports Med. 2015;43:345–353. doi: 10.1177/0363546514559707. [DOI] [PubMed] [Google Scholar]
- 66.Christino MA, Fantry AJ, Vopat BG. Psychological aspects of recovery following anterior cruciate ligament reconstruction. JAAOS – J Am Acad Orthop Surg. 2015;23:501–509. doi: 10.5435/JAAOS-D-14-00173. [DOI] [PubMed] [Google Scholar]
- 67.Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE. Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2013;41:1549–1558. doi: 10.1177/0363546513489284. [DOI] [PubMed] [Google Scholar]
- 68.Brand E, Nyland J. Patient outcomes following anterior cruciate ligament reconstruction: the influence of psychological factors. Orthopedics. 2009;32:335. doi: 10.3928/01477447-20090502-01. [DOI] [PubMed] [Google Scholar]
- 69.Te Wierike SCM, van der Sluis VDA, van den Akker‐Scheek I, Elferink‐Gemser MT, Visscher C. Psychosocial factors influencing the recovery of athletes with anterior cruciate ligament injury: a systematic review. Scand J Med Sci Sports. 2013;23:527–540. doi: 10.1111/sms.12010. [DOI] [PubMed] [Google Scholar]
- 70.Brewer BW, Cornelius AE, Raalte JV, Brickner JC, Sklar JH, Corsetti JR, et al. Rehabilitation adherence and anterior cruciate ligament reconstruction outcome. Psychol Health Med. 2004;9:163–175. doi: 10.1080/13548500410001670690. [DOI] [Google Scholar]
- 71.Thomeé P, Währborg P, Börjesson M, Thomeé R, Eriksson BI, Karlsson J. Determinants of self-efficacy in the rehabilitation of patients with anterior cruciate ligament injury. J Rehabil Med. 2007;39:486–492. doi: 10.2340/16501977-0079. [DOI] [PubMed] [Google Scholar]
- 72.Thomeé P, Währborg P, Börjesson M, Thomeé R, Eriksson BI, Karlsson J. Self-efficacy of knee function as a pre-operative predictor of outcome 1 year after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2008;16:118–127. doi: 10.1007/s00167-007-0433-6. [DOI] [PubMed] [Google Scholar]
- 73.Udry E, Donald Shelbourne K, Gray T. Psychological readiness for anterior cruciate ligament surgery: describing and comparing the adolescent and adult experiences. J Athl Train. 2003;38:167–171. [PMC free article] [PubMed] [Google Scholar]
- 74.Podlog L, Dimmock J, Miller J. A review of return to sport concerns following injury rehabilitation: practitioner strategies for enhancing recovery outcomes. Phys Ther Sport. 2011;12:36–42. doi: 10.1016/j.ptsp.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 75.Theunissen WWES, van der Steen MC, Liu WY, Janssen RPA. Timing of anterior cruciate ligament reconstruction and preoperative pain are important predictors for postoperative kinesiophobia. Knee Surg Sports Traumatol Arthrosc. 2020;28:2502–2510. doi: 10.1007/s00167-019-05838-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kvist J, Ek A, Sporrstedt K, Good L. Fear of re-injury: a hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2005;13:393–397. doi: 10.1007/s00167-004-0591-8. [DOI] [PubMed] [Google Scholar]
- 77.McCullough KA, Phelps KD, Spindler KP, Matava MJ, Dunn WR, Parker RD, et al. Return to high school– and college-level football after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) cohort study. Am J Sports Med. 2012;40:2523–2529. doi: 10.1177/0363546512456836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Morrey MA, Stuart MJ, Smith AM, Wiese-Bjornstal DM. A longitudinal examination of athletes’ emotional and cognitive responses to anterior cruciate ligament injury. Clin J Sport Med. 1999;9:63–69. doi: 10.1097/00042752-199904000-00004. [DOI] [PubMed] [Google Scholar]
- 79.Langford JL, Webster KE, Feller JA. A prospective longitudinal study to assess psychological changes following anterior cruciate ligament reconstruction surgery. Br J Sports Med. 2009;43:377–378. doi: 10.1136/bjsm.2007.044818. [DOI] [PubMed] [Google Scholar]
- 80.Brewer BW, Cornelius AE, Stephan Y, Van Raalte J. Self-protective changes in athletic identity following anterior cruciate ligament reconstruction. Psychol Sport Exerc. 2010;11:1–5. doi: 10.1016/j.psychsport.2009.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ohji S, Aizawa J, Hirohata K, Mitomo S, Ohmi T, Jinno T, et al. Athletic identity and sport commitment in athletes after anterior cruciate ligament reconstruction who have returned to sports at their pre-injury level of competition. BMC Sports Sci Med Rehabil. 2021;13:37. doi: 10.1186/s13102-021-00264-6. [DOI] [PMC free article] [PubMed] [Google Scholar]