Abstract
Background
Previous studies reported that transnasal ileus tube was a new and useful method for rapid relief of small intestinal obstruction. However, no study reported the impacts of the transnasal ileus tube for Crohn’s disease combined with intestinal obstruction. We aimed to describe the strategy to the small intestine obstruction caused by Crohn’s disease on the basis of transnasal ileus tube insertion.
Methods
From November 2019 to November 2021, the data of 6 hospitalized patients with CD, diagnosed and conservatively treated in The Second Hospital of Nanjing, were not relived and retrospectively collected. After the insertion of transnasal ileus tube, demographic information, clinical features and treatment data were extracted from medical records.
Results
Six Crohn’s disease patients with intestinal obstruction were included. Half of them were male. The patients aged from 29 to 70 years. Five patients had chronic intestinal obstruction more than one year. Three patients had intestinal surgery history. One patient had colonic abdominal fistula and anastomotic fistula, when she took intermittent usage of sulfsalazine and steroid. On admission, all the patients had abdominal pain, distention and mass. Five patients had anemia, low albumin and cholinesterase. All CDAI scores were more than 400. Compared to 19 patients with incomplete intestinal obstruction improved by nasogastric decompression tube, 6 patients with intestinal obstruction catheter had significant difference in time for relieving abdominal pain and distension (p = 0.003), time for alleviating abnormal mass (p ≤ 0.01), drainage volume (p = 0.004), and preoperative CDAI score (p = 0.001). Compared with X-ray image before insertion, complete remission of obstruction of 5 patients were observed in intestinal cavity after insertion. After 1–2 months nutrition, all the patients had small intestine resection and ileostomy, half of them underwent colectomy and fistula repair, and 4 patients were performed enterolysis at the same time, the residual small intestine length ranging from 250 to 400 cm. 1 patient had permanent ileostomy;1 patient had abdominal infection after operation. The typical manifestations of acute and chronic inflammation, transmural inflammation, pseudopolyps and serous fiber hyperplasia could be seen in pathological findings of patients 1 to 5. All the patients continued enteral nutrition after surgery. Four patients were treated with infliximab or vedolizumab.
Conclusion
The current intestinal obstruction catheter which is used to treat patients with Crohn's combined obstruction can afford quick clinical remission, longer nutrition time, and suitable preoperative CDAI score for operation, which is worthy of wildly being used.
Keywords: Transnasal ileus tube, Obstructions, Crohn’s disease
Background
Crohn's disease, one of chronic autoimmune disease, is typically characterized by intestinal transmural damage. The key features for diagnosing CD comprises a combination of radiographic, endoscopic and pathological findings demonstrating focal, asymmetric, transmural or granulomatous features. Intestinal lesions include hyperplasia, stenosis, ulcerative bleeding, transmural perforation, etc. Crohn's disease, is usually complicated with obstruction, especially chronic incomplete obstruction, which required surgical operation. The perioperative principle of Crohn's disease is different from the enhanced recovery after surgery or fast track surgery of general gastrointestinal tumors. If there are no life-threatening complications, the operation should not be performed too hasty. Because of persistence of intestinal lesions and the incurability of surgery, the preoperative optimization strategy is expected to reduce postoperative complications, preserve intestinal segments, solve the complications of Crohn's disease, avoid the risk of short bowel syndrome, achieve the purpose of remission, improve nutritional status, reduce drug dependence, and improve the quality of life [1].
Surgical operation should be avoided at the active stage of Crohn's disease. During the perioperative period, they should withdraw steroid dependence as much as possible and ablate the use of hormones, immunosuppressor and other drugs. If the disease condition is stable, and the Crohn's disease activity index score(CDAI) is less than 150, qualitative surgical treatment can be carried out [2].
The perioperative strategy of incomplete obstruction need stop using the medication that can control Crohn's activity, relieve the obstruction as soon as possible, improve the nutritional status of patients, and provide surgical conditions for the optimization of surgery. Conservative management is the preferred option in the absence of peritonitis, including bowel rest, intravenous fluid therapy,and gastric decompression [3]. The nasogastric decompression tube can only be placed in the stomach and has no direct decompression effect on the contents of the small intestine, so it can not achieve the ideal remission effect [4]. Transnasal intestinal obstruction tube is a new method for rapid relief of intestinal obstruction in Crohn's disease complicated with small intestinal obstruction. In contrast to nasogastric decompression tube, the complete decompression site of the transnasal intestinal obstruction tube is directly above the obstruction plane of the proximal small intestine. Inhalation and decompression of gas and intestinal contents at the obstruction site can quickly alleviate the symptoms of small intestinal obstruction [5]. Resection and anastomosis of obstructive lesions can be successfully performed on most patients after preoperative preparation through catheter [6, 7]. This study describes the treatment, that is, surgical procedure on the basis of transnasal ileus tube insertion, of 6 cases of Crohn's complicated with small intestinal obstruction.
Methods
Population and exclusion criteria
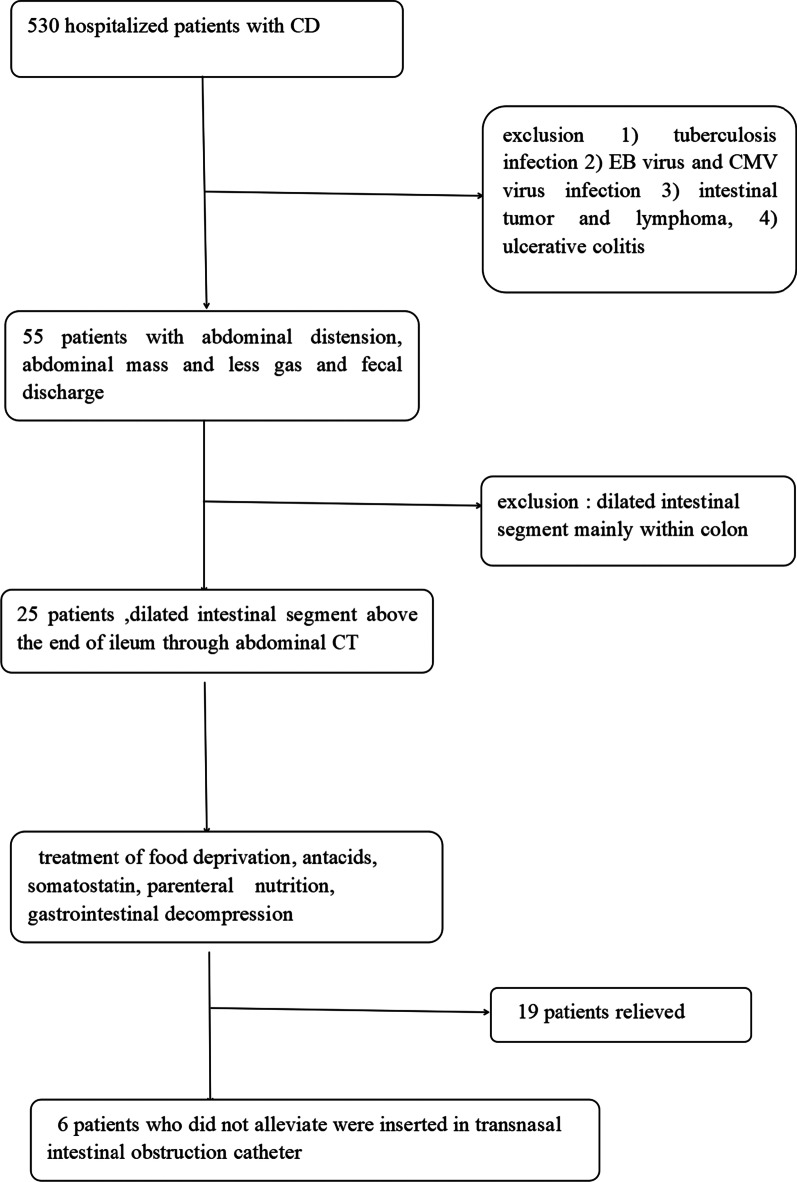
From November 2019 to November 2021, the data of 530 hospitalized patients with CD, diagnosed by clinical manifestations, radiographic and endoscopic findings in The Second Hospital of Nanjing, were retrospectively collected. At the same time, the following conditions were excluded: (1) tuberculosis infection, (2) EB virus and CMV virus infection, (3) intestinal tumor and lymphoma, (4) ulcerative colitis. Among 55 patients with abdominal distension, abdominal mass, less gas discharge and defecant discharge, 25 patients were confirmed to have intestinal obstruction according to dilated intestinal segment above the end of ileum through abdominal CT screening. 19 patients relieved after they were treated through the nasogastric decompression tube, food deprivation, antacids, somatostatin, and parenteral nutrition. 6 patients inserted transnasal intestinal obstruction catheter without remission. The screening process can be seen in Fig. 1.
Fig. 1.
Process of cases screening
Procedure
The clinical data of 6 patients were firstly reviewed, then the transnasal intestinal obstruction catheter (CLINY Ileus Tube suite, Create Medic, Tokyo, Japan. The tube is 300 cm in length, 16 Fr or 18 Fr) [8] were implanted into small intestine as deep as possible under endoscopic guidance. After 24–48 h, the catheter depth can be adjusted according to radiography result so that the catheter can be located near the obstruction to help decompress. The next step is to collect the data which includes relief time of clinical symptoms, daily drainage volume, nutritional mode, NRS2002 score, and CDAI score before insertion. 1–2 months after transnasal ileus tube insertion, all the patients underwent individual preoperative evaluation and corresponding resection operation which were performed by senior expert groups of department of General Surgery at Jinling Hospital of Medical School of Nanjing University between January 2020 and October 2021. Surgical specimen were pictured and observed through microscopy after hematoxylin–eosin staining. Meanwhile, postoperative treatment were recorded.
Laboratory and radiologic information
The laboratory tests included blood routine tests, liver function, PT, inflammatory biomarkers. Abdominal enhanced computed tomography (CT), X-ray or digestive tract radiography were performed for each patient and the results were collected.
Statistical analysis
The continuous variables were presented as medians (interquartile range (IQR)). Categorical variables were shown as the counts. The independent group t tests or Mann–Whitney U were used to compare continuous variables between groups. Chi-square or Fisher exact test was used for the comparisons of categorical variables. P < 0.05 was considered as statistically significant. All data analysis was performed using SPSS version 22.0 software (SPSS Inc., Chicago, IL, United States).
Results
Clinical characteristics of the patients
The medical history of the patients were presented in Table 1. Half of the patients were male. The patients aged from 29 to 70 years. One patient had breast tumor and received the corresponding treatment. All the patients had no cigarette and alcoholic history. The clinical characteristics before and after occurrence /aggravation of intestinal obstruction were described (Tables 2,3). 5 patients had a history of taking immunosuppressive agents and steroids for more than 1 year, but stopped the medication on their own willing. We mark the immunosuppressant intake for more than 1 year as YES, and no less than 1 year as NO, and the discontinuous drugs for more than half a year and retaking for more than half a year as intermittent.
Table 1.
The demographic characteristics and medical history of 6 patients
| Characteristics | Patient1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 |
|---|---|---|---|---|---|---|
| Age | 39 | 29 | 55 | 57 | 36 | 70 |
| Sex | M | M | F | F | M | F |
| Anal fistula | No | No | No | No | Yes | No |
| Anal stenosis | No | No | Yes | No | Yes | No |
| Gallstones | No | No | No | No | Yes | No |
| Kidney stones | No | No | No | No | Yes | No |
| Ureterectasis | No | No | No | No | Yes | No |
| Abdominal abscess | No | No | Yes | No | Yes | No |
| Fatty liver | No | No | Yes | No | No | No |
| Malnutrition | No | No | No | Yes | No | No |
| Anemia | No | Yes | Yes | Yes | No | No |
| History of tumor | No | No | No | Breast cancer | No | No |
| History of non-intestinal surgery | No | No | No | Mastectomy | No | No |
Table 2.
Clinical characteristics before occurrence/aggravation of intestinal obstruction
| Characteristics | Patient1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 |
|---|---|---|---|---|---|---|
| Diet | Normal diet | Element diet | Enteral nutrition transition to normal diet | Normal diet | EN transition to ordinary diet | normal diet |
| Intermittent EN | No | Yes | Yes | No | No | No |
| Abdominal pain, abdominal distension | Intermittent | Intermittent | Intermittent | Recurrent | Intermittent | Intermittent |
| Vomit | No | No | No | Recurrent | No | No |
| Bloody stool | No | No | No | No | Yes | No |
| Abdominal mass | No | No | Yes | No | Yes | No |
| Abdominal scars | Yes | No | Yes | No | Yes | No |
| Ascites | No | No | No | No | Yes | No |
| CD diagnosed years | 2 W | 4Y | 15Y | 12Y | 16Y | 23Y |
| Chronic intestinal obstruction time | 3 W | 3Y | 2Y | 11Y | 1Y | 4 M |
| History of intestinal surgery (years) | 6Y | No |
18Y first time 14Y second time |
NO | 7Y | No |
| Excision site | appendix | No | Small intestine 1 m, ileum 30 cm, transverse colon 20 cm | No | Right hemicolon, small intestine | No |
| Intestinal perforation | No | No | No | No | Yes | No |
| Intestinal fistula | ||||||
| Internal fistula | No | No | Colonic abdominal fistula, anastomotic fistula | No | No | No |
| External fistula | No | No | No | No | No | No |
| Treatment | ||||||
| Mesalazine | No | Yes | No | Yes | Yes | No |
| Sulfasalazine | No | No | Intermittent | No | Yes | No |
| Steroid | No | No | Intermittent | Yes | Yes | No |
| Biological agents | No | No | No | Trastuzumab | No | No |
| Azathioprine | Yes | No | Yes | Yes | Yes | No |
Table 3.
Clinical characteristics on the admission of 6 patients
| Characteristics | Patient1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 |
|---|---|---|---|---|---|---|
| Occurrence/aggravation of intestinal obstruction | 3 W | 1 M | 1 M | 1Y | 2 W | 1 M |
| Abdominal pain and distension | Yes | Yes | Yes | Yes | Yes | Yes |
| vomit | No | No | Yes | No | No | No |
| Bloody stool | Yes | No | No | No | No | No |
| Abdominal mass | No | Yes | Yes | Yes | Yes | No |
| Abdominal scar | Yes | No | Yes | No | Yes | No |
| Ascites | Yes | Yes | No | Yes | Yes | No |
| Fever | No | No | No | No | No | No |
| Intestinal perforation | No | No | No | No | Yes | No |
| Intestinal fistula | ||||||
| Internal fistula | Small intestinal colonic fistula | No | No | Small intestine bladder fistula | No | No |
| External fistula | No | No | No | No | No | No |
| Treatment | ||||||
| Switch EN to fasting | No | Yes | No | No | No | Yes |
| PN | Yes | Yes | Yes | Yes | Yes | Yes |
| Mesalazine (used before fasting) | Yes | No | No | No | No | No |
| Somatostatin | Yes | Yes | Yes | Yes | Yes | Yes |
| Antibiotics | No | No | No | Yes | Yes | No |
| Switch Prednisone to NONE | No | No | No | No | Yes | No |
2 patients had intermittent enteral nutrition (EN) before admission. All the patients stopped EN or regular diet or oral medication when intestinal obstruction was diagnosed. Then all the patients took total parenteral nutrition (TPN), and after insertion they took Partial Enteral Nutrition (PEN) on the basis of their tolerance as soon as possible.
Laboratory and image abnormalities
After admission, 6 patients took blood examination, abdominal X-ray and CT. NRS2002 score and CDAI score were calculated. Five patients(83.3%) had anemia low ALB level, and all the patients had increasing fecal calprotectin and high CDAI scores(seen in Table 4. All the patients had typical Characteristic imaging changes of intestinal obstruction (seen in Fig. 2).
Table 4.
Laboratory abnormalities at the beginning of this hospitalization
| Characteristics | Patient1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 |
|---|---|---|---|---|---|---|
| WBC(3.69–9.16 × 109/L) | 2.26 | 5.66 | 3.49 | 3.93 | 7.47 | 5.33 |
| NE (2–7 × 109/L) | 1.66 | 3.4 | 2.42 | 2.59 | 5.66 | 3.01 |
| LY (0.8–4 × 109/L) | 0.41 | 1.75 | 0.84 | 0.94 | 1.16 | 1.65 |
| HGB (113–151 g/L) | 97 | 89 | 88 | 83 | 105 | 136 |
| PLT (101–320 × 109/L) | 238 | 362 | 237 | 234 | 290 | 206 |
| CRP (0–10 mg/L) | 13.11 | 12.36 | 10.3 | 54.16 | 47.7 | 3 |
| PCT (0.01–0.052 ng/ml) | 0.1 | 0.05 | 0.34 | 0.09 | 0.05 | ≤ 0.01 |
| PT (14–21 Sec) | 12.3 | 12.7 | 14.5 | 24.5 | 12.5 | 17.3 |
| ESR (0–20 mm/h) | 8 | 5 | 8 | 12 | 18 | 9 |
| Fecal calprotectin (0–200 µg/g) | > 1800 | > 1800 | > 1800 | > 1800 | > 1800 | > 1800 |
| ALB (35–55 g/L) | 31.8 | 18 | 33.7 | 33.6 | 27 | 38.9 |
| TBIL (3–19 µmol) | 4.3 | 9.8 | 8.8 | 8.7 | 7.3 | 4.4 |
| DBIL (0.5–6.8 µmol) | 2.4 | 5.2 | 4.6 | 5.5 | 4.2 | 1.2 |
| CHE (4230–13,000 U/L) | 3969 | 2066 | 2524 | 2305 | 1985 | 5770 |
| Ca (2.1–2.6 mmol/L) | 1.8 | 1.81 | 2.00 | 2.17 | 2.05 | 2.35 |
| Fe (5.83–34.5 µmol) | 4.47 | 18.23 | 12.99 | 4.08 | 9.6 | 18.72 |
| NRS2002 | 12 | 10 | 12 | 10 | 12 | 10 |
| CDAI | 498.74 | 518.98 | 511.04 | 485.04 | 515.79 | 401.97 |
Fig. 2.
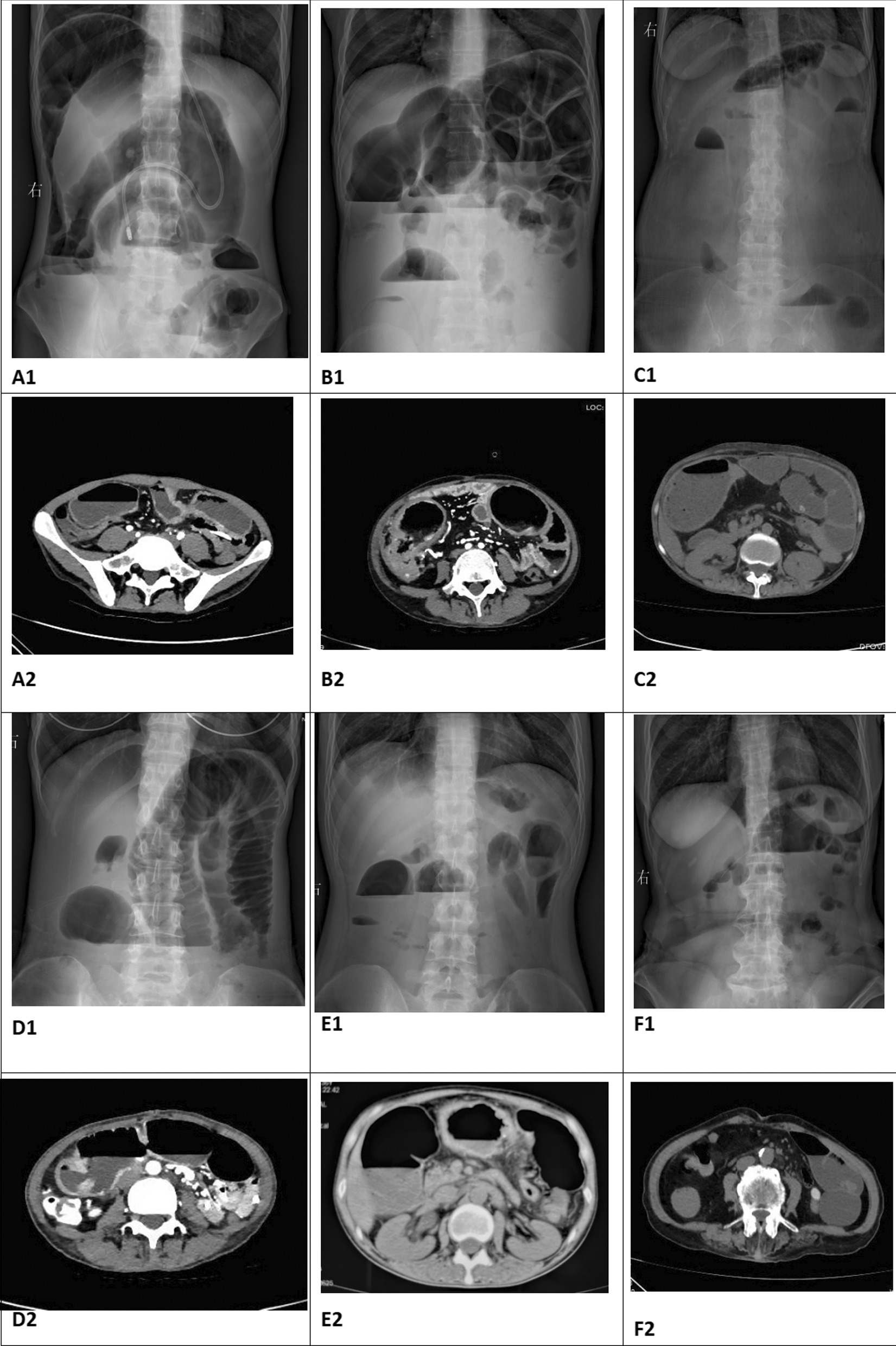
Abdominal X-Ray and CT at the beginning of obstruction confirmation. A1 and A2 showed the obstruction sign before tube insertion of patient 1; B1 and B2 showed the showed the obstruction sign before tube insertion of patient 2; C1 and C2 showed the obstruction sign before tube insertion of patient 3; D1 and D2 showed the obstruction sign before tube insertion of patient 4; E1 and E2 showed the obstruction sign before tube insertion of patient 5; F1 and F2 showed the obstruction sign before tube insertion of patient 6
Therapeutic efficacies
19 patients with incomplete intestinal obstruction improved by nasogastric decompression tube and 6 patients treated with intestinal obstruction catheter were selected to observe the relief of clinical symptoms, nutrition time, volume of drainage, and the variation of CRP, ESR, CDAI before surgery, as well as complication after operation. See Table 5. From that table, we can see significant difference in time for relieving abdominal pain and distension (p = 0.003), time for alleviating abnormal mass (p ≤ 0.01), volume of drainage (p = 0.004), preoperative nutrition time (p ≤ 0.01), and preoperative CDAI scores (p = 0.001).
Table 5.
Comparison of two groups on therapeutic effect
| Parameter | Group 1 (transnasal ileus tube n = 6) | Group 2 (nasogastruic tube n = 19) | Statistical value | P |
|---|---|---|---|---|
| Time for relieving abdominal pain and distension(day) | 1.33 ± 0.516 | 2.68 ± 0.946 | 3.313 | 0.003 |
| time for alleviating abnormal mass(day) | 2.33 ± 0.516 | 4.74 ± 2.156 | 4.470 | ≤ 0.01 |
| Volume of drainage(ml/day) | 666.67 ± 250.333 | 167.37 ± 76.583 | 4.815 | 0.004 |
| Preoperative nutrition time(week) | 6.67 ± 1.506 | 2.05 ± 0.970 | 8.886 | ≤ 0.01 |
| CRP | 4.17 ± 1.472 | 5.95 ± 4.116 | 1.026 | 0.315 |
| ESR | 8.17 ± 2.858 | 14.42 ± 10.249 | 1.457 | 0.159 |
| Preoperative CDAI score | 163.48 ± 30.14 | 231.20 ± 26.43 | 4.937 | 0.001 |
| Postoperative complications | 1 (16.7%) | 6 (31.6%) | 0.483 | 0.487 |
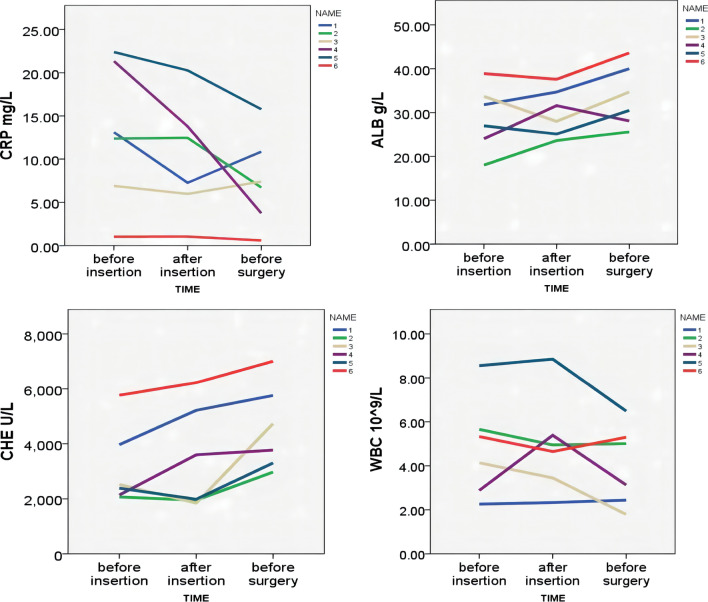
For 6 patients, the blood examinations were performed before tube insertion, before and after surgical operation so as to investigate the variation of CRP, ALB, CHE, WBC (seen Fig. 3).
Fig. 3.
Parameters comparison of 6 patients before catheter insertion, 1W after insertion and before surgery
The abdominal X-ray was taken 2-4 weeks after the insertion of intestinal obstruction catheter. The digestive radiography examinations were performed before operation.
Except for patient 1, the other 5 patients were found obvious alleviation (seen Fig. 4). Part of the patients (4/6) had gastrointestinal radiography to make the obstruction position clear (Fig. 5). The intestinal obstruction of P1 alleviated partially due to multiple segmental stenosis which could be observed by gastrointestinal radiography.
Fig. 4.

Relief after 2w-4w transnasal ileum tube insertion by X-ray. A image of X-RAY after transnasal ileum tube insertion of patient 1; B image of X-RAY after X-RAY of patient 2; C image of X-AY after transnasal ileum tube insertion of patient 3; D image of X-AY after transnasal ileum tube insertion of patient 4; E image of X-AY after transnasal ileum tube insertion of patient 5; F image of X-AY after transnasal ileum tube insertion of patient 6. B–F indicated fully relieved; A indicated partially relieved
Fig. 5.
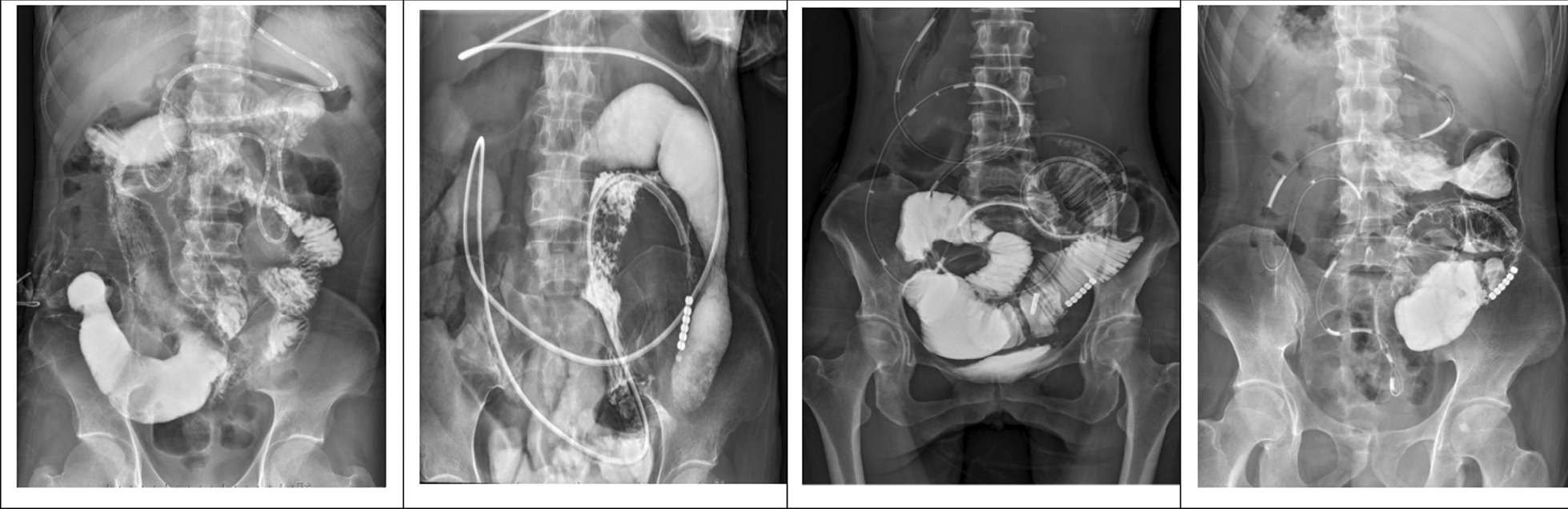
Gastrointestinal radiological findings of stricture location of before surgery. From left to right: Patient 1, Patient 3, Patient 4, Patient 5. P1: segmental ileal stenosis, P3: multiple dilatation and segmental stenosis of small bowel, P4: ileal stenosis above ileocecal region, P5: stricture of ileocolic anastomosis, dilated ileum
Therapeutic outcome of surgery and Postoperative treatment
6 patients were performed different optimal operation in accordance with their different condition. Then macroscopic and microscopic findings of their own intestinal resection were observed, as shown in Table 6 and Fig. 6.
Table 6.
Nutrition time, operative methods, postoperative pathology and postoperative treatment of 6 patients
| Characteristics | Patient1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 |
|---|---|---|---|---|---|---|
| Retention time of intestinal obstruction catheter (week) | 4 | 7 | 4 | 6 | 3 | 6 |
| Reasons for pulling out of intestinal obstruction catheter | Throat pain | Surgery | Throat pain | Throat pain | Throat pain | Surgery |
| Nutrition period after tube insertion(week) | 8 | 7 | 6 | 7 | 4 | 6 |
| Operative methods | ||||||
| Small intestine resection | Yes | Yes | Yes | Yes | Yes | Yes |
| Colectomy | No | No | Yes | No | Yes | Yes |
| Residual small intestine length | 300 cm | 400 cm | 300 cm | 250 cm | 290 cm | 300 cm |
| Intestinal lysis | Yes | No | Yes | Yes | Yes | No |
| Fistula repair | Yes | No | No | Yes | Yes | No |
| Ileostomy | ||||||
| Stoma number | 2 | 1 | 1 | 2 | 1 | 1 |
| Permanent | No | No | Yes | No | No | No |
| Closure enterostomy | Yes | No | No | Yes | No | No |
| Postoperative fistula | No | No | No | No | No | No |
| Incision infection/abdominal infection | No | Yes | No | No | No | No |
| Postoperative pathology | ||||||
| Acute an chronic inflammation | Moderate-severe | Moderate-severe | Moderate | Moderate | Moderate | Moderate |
| Transmural inflammation | Yes | Yes | Yes | No | Yes | No |
| Pseudopolyp | Yes | Yes | No | Yes | Yes | Yes |
| Ulcer | Superficial | Transmural | Superficial | No | Transmural | No |
| Serous fibrous hyperplasia | No | Yes | Yes | Yes | Yes | No |
| Postoperative treatment | ||||||
| Immunosuppressant | No | No |
AZA for 0.5y Thalidomide for 1y |
No | No | No |
| EN | Yes | Yes | Yes | Yes | Yes | Yes |
| Biological agents | Infliximab (start form 1 mon after surgery) | No | Vedolizumab (start form 1 year after surgery) | Vedolizumab (start form 4 mon after surgery) | NO YET | Vedolizumab (start form 1 mon after surgery) |
| Follow-up postoperation | 13M | Lost | 3M | 7M | 2W | 2M |
Fig. 6.
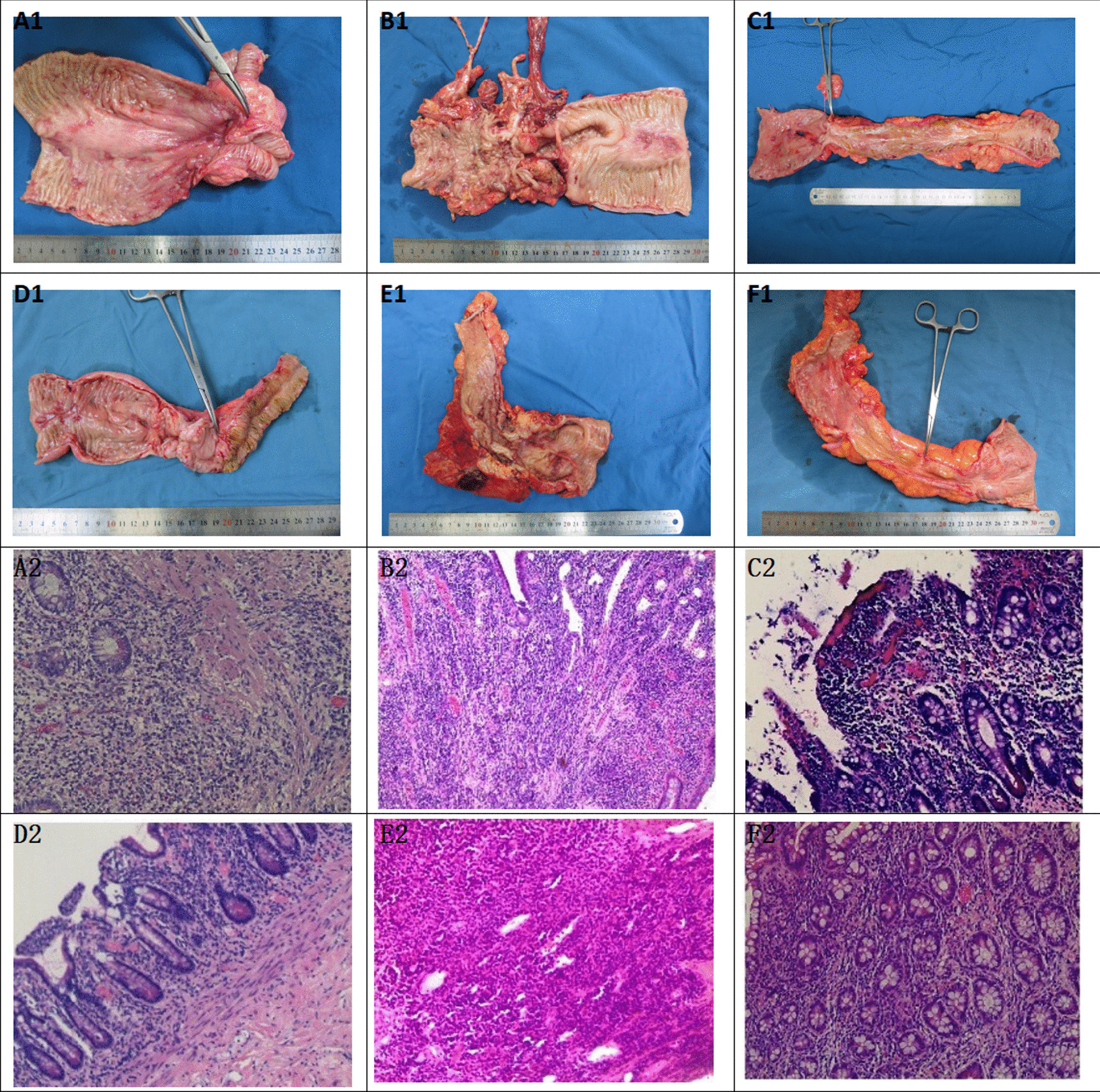
Macroscopic and microscopic findings of excisional intestinal specimen of 6 patients. A1 and A2 macroscopic and microscopic findings of patient 1; B1 and B2 macroscopic and microscopic findings of patient 2; C1 and C2 macroscopic and microscopic findings of patient 3; D1 and D2 macroscopic and microscopic findings of patient 4; E1 and E2 macroscopic and microscopic findings of patient 5; F1 and F2 macroscopic and microscopic findings of patient 6
All the patients had small intestine resection and ileostomy, half of whom underwent colectomy and fistula repair. Meanwhile, 4 patients were performed intestinal lysis, with residual small intestine length ranging from 250 to 400 cm. 1 patient had permanent ileostomy;1 patient had abdominal infection after operation.
The typical manifestations of acute and chronic inflammation, transmural inflammation, pseudopolyps and serous fiber hyperplasia can be seen in pathological findings of patients 1 to 5. All the patients continued enteral nutrition after surgery. Four patients were treated with infliximab or vedolizumab.
Discussion
The benefits of surgical treatment of Crohn's disease have been greatly improved. However, it remains challenging for surgeons because gastrointestinal surgery is still a high-risk operation for Crohn's disease patients [9]. Most patients with Crohn's disease have obvious severe symptoms when the urgent operation is needed, many of whom were even misdiagnosed or delayed being diagnosed for a long time. The physiological homeostasis environment function in vivo disordered, and the surgical complications such as obstruction, bleeding and fistula further make the body function worsen. In addition, patients with Crohn's disease often suffered immune dysfunction, infection, anemia, malnutrition, and they usually took many immunosuppressants and biological agents. All the complication and therapeutic destroyed the immune function and increased the risk of postoperative complications [10]. Therefore, the perioperative optimization strategy to reduce postoperative complications, avoid future recurrence and maintain postoperative remission is particularly important. A logistic regression analysis of one study was revealed that operative age and preoperative EN were independent risk factors for postoperative complications [10]. A number of studies [11–14] have also confirmed that preoperative parenteral nutrition support can significantly reduce postoperative complications, and the nutritional status and inflammation of patients can be improved. The research results of Grivceva et al. [15] suggested that the use of TPN had no obvious relationship with postoperative complications, but indicated the positive significance of PN for surgical optimization in different ways. Therefore, prolonging the nutritional time as long as possible is an important treatment strategy in the perioperative period.
Six patients with Crohn's disease were followed up. Five of them were definitely diagnosed with CD several years ago. One of them just diagnosed Crohn's disease with intestinal obstruction after this admission. Three patients with incomplete obstruction had a history of abdominal surgery several years ago, and P3 had multiple operations due to recurrent intestinal obstruction. Five patients took the different immunosuppressive medications to control disease activity. In spite of the usage of strong immunesuppressive drugs, CD patients frequently experience the recurrence and over half will have an intestinal resection within 10 years after diagnosis, one-third undergo a repeat resection within 5 years [16]. Different from general gastrointestinal diseases, The resection of the intestines of patients with Crohn's disease at the lesion site can not completely cure the disease and will eventually inevitably relapse [17], while the intestinal fistula and other diseases during abdominal surgery are active factors for incomplete obstruction [18]. Preoperative treatment measures are to maximize the effect of postoperative resection remission, prolong the recurrence cycle, reduce the recurrence rate and reduce perioperative complications. With the proposal of nutritional immunity and nutritional ecology, nutritional support plays an important role in intentional rehabilitation. These 6 patients were mainly took element diet and normal diet before the onset of intestinal obstruction. The nutritional status of the patients were usually poor after obstruction, and there were weight loss, anemia, albumin, cholinesterase reduction, low iron and calcium. In order to reduce intestinal secretion and protect intestinal mucosa, all the patients fasted, took parenteral nutrition, and were injected somatostatin. After the placement of intestinal obstruction catheter, except for P1, intestinal dilatation of other five patients obviously relived to different extents, which could be seen from X-ray image. Through angiography, P1 was observed multiple segmental stenosis before surgery which possibly resulted into partially-relieved obstruction. Two patients used enteral combined parenteral nutrition to improve nutritional status. Studies have shown that the usage of total enteral nutrition for 3 months before operation can significantly increase the nutritional reserve, reduce adverse reactions and reduce the incidence of postoperative complications in patients of Crohn's with intestinal fistula [11]. For CD patients presenting with acute small-bowel obstruction without bowel ischaemia or peritonitis, deferred surgery is the preferred option [3], so all six patients took comparatively long time to improve the nutrition condition before surgery in order to decrease the incidence of adverse surgical outcome. Regarding intestinal stricture treatment, endoscopic balloon dilation(EBD) and surgical treatment can be both considered as one of the options. Studies have shown EBD is more effective and safer for a small number (< 4) or short segment (< 4-5 cm) of strictures in a close proximity, while multiple strictures or long segment strictures(> 5 cm) of bowel may benefit more from surgical resection, anastomosis or stricturoplasty as a result of the involvement of stenotic bowel angulation [19]. That’s the reason why the six patients underwent surgery to relieve the stenosis.
It is knonwn that malnutrition is an independent dangerous factor for adverse postoperative outcomes of CD. Therefore, oral or enteral nutrition is the priority of nutritional support;[20]. Compared with 19 patients with nasogastric tube decompression whose nutrition time is about 2 weeks, the nutrition time of the 6 patients with transnasal ileus tube is about 1–2 months which was beneficial to intestinal resection. however, the period of nutrition was still less than 3 months, which may be due to 1.after the insertion, enteral nutrition is usually fed through the intestinal obstruction catheter. The position of enteral nutrition is close to the obstruction site, and there are relatively less enteral tubes that can effectively absorb enteral nutrition. 2. The intestinal obstruction catheter is too thick for some patients to tolerate the long-term compression of the nasal cavity and throat, resulting in a short retention time of the obstruction catheter and affecting the time of enteral nutrition. 3. The site of obstruction is mostly located in the small intestine, and the effective area of enteral nutrition absorption is restricted, which affects enteral nutrition. 4. In addition to obstruction, some patients also have internal fistula. For patient 1 and patient 4 and 5, nutrition infusion to the small intestine may enter into colon or bladder fistula, affecting the absorption of the small intestine, which is not conducive to the healing of fistula and has an adverse impact on the correction of patients' nutritional status. To solve those dilemma, the nasogastric tube or nasointestinal tube may be inserted to nutrition the proximal small intestine in addition to the small intestinal decompression tube. However, if the patient has gastric or duodenal fistula, the nutrition effect is expected not to be satisfied. It is an important method to prolong the period of enteral nutrition as far as possible in the treatment of Crohn's patients with small intestinal obstruction. It is worth mentioning that there is no significant difference in postoperative complications,the results of CRP and ESR between the two groups of patients with different decompression tubes, possibly as a result of the small sample size.
A study [21] have shown that the way to combine mesalazine with enteral nutrition is effective in the treatment of active Crohn's disease, which can induce remission, improve the nutritional status and improve the surgical tolerance of patients. Five patients had used mesalazine or azathioprine before the onset of this disease, but enteral nutrition was not sustainable. In case of obstruction and internal fistula, patients stopped immunosuppressants, including azathioprine, thalidomide and hormones, corrected the nutritional status as much as possible, and resected the intestinal canal as little as possible during the operation, so as to avoid postoperative complications. The macrosopic and microscopic change of the intestinal resection are consistent with the typical manifestations of Crohn’s disease complicated with intestinal obstruction. The typical manifestations of acute and chronic inflammation, transmural inflammation, pseudopolyps and serous fiber hyperplasia can be seen in patients 1 to 5, and pseudopolyps can be seen in patients 6. Even there was no typical transmural inflammation, the diagnosis of Crohn’s disease still can not be excluded accrouding to the lesion location and clinical symptoms. Four patients were treated with infliximab or vedolizumab. One patient was lost to follow-up after operation, and one was currently observed after operation. Vedolizumab was planned to be given one month after operation. All patients continued EN for now and will gradually adjust to their appropriate diet in the future.
From the comparison of short-tube usage(recommended by all the CD-related guidelines present) group and long-tube application group, we can conclude the patients can still benefit from long-tube insertion even though the patients of short-tube insertion experience the failure of effective treatment of intestinal obstruction. Studies show that long tube decompression have succeeded in more than 70% of the patients with benign adhesive small bowel obstruction [22, 23]; This procedure has been regarded as a simple, safe and minimally invasive approach. As a result, it is recommended as the initial treatment for benign adhesive bowel obstruction [24]. However, short tube insertion treatment is not appropriate for complicated intestinal obstruction.
This article described the medical history, diagnosis, perioperative treatment, operation process, postoperative pathology and biological treatment of 6 Crohn’s patients with incomplete obstruction and they were treated with transnasal ileus tube by abstracting their medical record. There were several limitations to this study. Firstly, This was a single-centered, retrospective study. Secondly, the sample size is small. The results need to be confirmed by a larger sample study. In addition, follow-up time was not long enough to observe clinical outcomes. When we confronted with complicated cases of obstruction CD which is still a great challenge for experts of both gastroentergolgy and general surgery department, the treatment strategy may be adopted as followed, first step is rapid decompression, second condition is to prolong the nutrition time as much as possible and improve general condition, and third part is when CDAI scores increased as high as to meet the satisfaction to operation, final method is usage of biological agents and TPN to control the CD activity.
Conclusion
By comparing the two groups of patients with small sample size, the current intestinal obstruction catheter which was used to treat patients with Crohn's combined obstruction could afford quick clinical remission, longer nutrition time, and suitable preoperative CDAI score for operation, which is worthy of being wildly used. More similar data should be collected and analyzed to draw statistically significant conclusions.
Acknowledgements
We appreciated Daoping Hou for revising the manuscript.
Abbreviations
- WBC
White blood cell
- ALB
: Albumin
- CHE
: Cholinesterase
- ESR
: Erythrocyte sedimentation rate
- CRP
: C-reactive protein
- PT
Prothrombin
Author contributions
BZ designed the study; LZ collected the data and wrote the draft; LC conceived of this study and collected the data; CD and HT analyzed the data; CW, LY and HW collected the data. All authors were involved in writing the manuscript. All authors read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
The research protocol was established, according to the ethical guidelines of the Helsinki Declaration and was approved by the Human Ethics Committee of The Second Hospital of Nanjing. Written informed consent was obtained from individual participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflicts of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Lingyun Zuo and Lei Cao contributed equally to this work
References
- 1.Spinelli A, Allocca M, Jovani M, et al. Review article:optimal preparation for surgery in Crohn's disease. Aliment Pharmacol Ther. 2014;40(9):1009–1022. doi: 10.1111/apt.12947. [DOI] [PubMed] [Google Scholar]
- 2.Ferrari L. Mukta K Krane, Alessandro Fichera, “Inflammatory bowel disease surgery in the biologic era”. World J Gastrointest Surg. 2016;8(5):363–370. doi: 10.4240/wjgs.v8.i5.363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Adamina M, Bonovas S, Raine T, et al. ECCO guidelines on therapeutics in Crohn's disease: surgical treatment. J Crohns Colitis. 2020;14(2):155–168. doi: 10.1093/ecco-jcc/jjz187. [DOI] [PubMed] [Google Scholar]
- 4.Sakakibara T, Harada A, Ishikawa T, et al. Parameter predicting the recurrence of adhesive small bowel obstruction in patients managed with a long tube. World J Surg. 2007;31(1):80–85. doi: 10.1007/s00268-006-0158-6. [DOI] [PubMed] [Google Scholar]
- 5.Chen XL, Ji F, Lin Q, et al. A prospective randomized trial of transnasal ileus tube vs nasogastric tube for adhesive small bowel obstruction. World J Gastroenterol. 2012;18(16):1968–1974. doi: 10.3748/wjg.v18.i16.1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ketcham AS, Hoye RC, Pilch YH, et al. Delayedintestinal obstruction following treatment for cancer. Cancer. 2015;25(2):406–410. doi: 10.1002/1097-0142(197002)25:2<406::AID-CNCR2820250219>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 7.Barrand KR. A case of canine intestinal obstruction due to ingestion of a super absorbent polymer bead. J Small Anim Pract. 2018;59(3):196. doi: 10.1111/jsap.12812. [DOI] [PubMed] [Google Scholar]
- 8.Tan Y, Chen H, Mao W, et al. Short-term clinical outcomes after using novel deeper intubation technique (DIT) of ileus tube for acute bowel obstruction patients. Gastroenterol Res Pract. 2020 doi: 10.1155/2020/1625154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patel KV, Darakhshan AA, Griffin N, et al. Patient optimization for surgery relating to Crohn’s disease. Nat Rev Gastroenterol Hepatol. 2016;13(12):707–719. doi: 10.1038/nrgastro.2016.158. [DOI] [PubMed] [Google Scholar]
- 10.Li G, Ren J, Wang G, et al. Preoperative exclusive enteral nutrition reduces the postoperative septic complications of fistulizing Crohn’s disease. Eur J Clin Nutr. 2014;68(4):441–446. doi: 10.1038/ejcn.2014.16. [DOI] [PubMed] [Google Scholar]
- 11.Jacobson S. Early postoperative complications in patients with Crohn's disease given and not given preoperative total parenteral nutrition. Scand J Gastroenterol. 2012;47(2):170–177. doi: 10.3109/00365521.2011.648954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lashner BA, Evans AA, Hanauer SB. Preoperative total parenteral nutrition for bowel resection in Crohn's disease. Dig Dis Sci. 1989;34(5):741–746. doi: 10.1007/BF01540346. [DOI] [PubMed] [Google Scholar]
- 13.Yao GX, Wang XR, Jiang ZM, et al. Role of perioperative parenteral nutrition in severely malnourished patients with Crohn's disease. World J Gastroenterol. 2005;11(36):5732–5734. doi: 10.3748/wjg.v11.i36.5732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mcintyre PB, Powell-Tuck J, Wood SR, et al. Controlled trial of bowel rest in the treatment of severe acute colitis. Gut. 1986;27(5):481–485. doi: 10.1136/gut.27.5.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grivceva Stardelova K, Misevska P, Zdravkovska M, et al. Total parenteral nutrition in treatment of patients with inflammatory bowel disease. Prilozi. 2008;29(1):21–43. [PubMed] [Google Scholar]
- 16.Lauro A, D’Amico F, Gondolesi G. The current therapeutic options for Crohn's disease: from medical therapy to intestinal transplantation. Expert Rev Gastroenterol Hepatol. 2017;11(12):1105–1117. doi: 10.1080/17474124.2017.1367665. [DOI] [PubMed] [Google Scholar]
- 17.Nyabanga C, Kochhar G, Costa G, et al. Management of Crohn’s disease in the new era of gut rehabilitation and intestinal transplantation. Inflamm Bowel Dis. 2016;22(7):1763–1776. doi: 10.1097/MIB.0000000000000792. [DOI] [PubMed] [Google Scholar]
- 18.Landerholm K, Reali C, Mortensen NJ, et al. Short- and long-term outcomes of strictureplasty for obstructive Crohn’s disease. Colorectal Dis. 2020;22(9):1159–1168. doi: 10.1111/codi.15013. [DOI] [PubMed] [Google Scholar]
- 19.Shen B, Kochhar G, Navaneethan U, et al. Practical guidelines on endoscopic treatment for Crohn’s disease strictures: a consensus statement from the Global Interventional Inflammatory Bowel Disease Group. Lancet Gastroenterol Hepatol. 2020;5(4):393–405. doi: 10.1016/S2468-1253(19)30366-8. [DOI] [PubMed] [Google Scholar]
- 20.Stoner PL, Kamel A, Ayoub F, et al. Perioperative care of patients with inflammatory bowel disease: focus on nutritional support. Gastroenterol Res Pract. 2018;2018:7890161. doi: 10.1155/2018/7890161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tao QS, Ren JA, Yu BJ, et al. Early therapeutic benefit of enteral nutrition in active Crohn disease. Nutr Res. 2007;27(2):92–96. doi: 10.1016/j.nutres.2006.12.013. [DOI] [Google Scholar]
- 22.Li RH, Li DC. Lv XP : Radiophotographically controlled nasointestinal intubation to treat recurrent postoperative adhesive ileus. Cell Biochem Biophys. 2015;72:509–514. doi: 10.1007/s12013-014-0496-1. [DOI] [PubMed] [Google Scholar]
- 23.Gowen GF. Long tube decompression is successful in 90% of patients with adhesive small bowel obstruction. Am J Surg. 2003;185:512–515. doi: 10.1016/S0002-9610(03)00074-6. [DOI] [PubMed] [Google Scholar]
- 24.Xan XJ, et al. Outcome of decompression using a transnasal ileus tube in malignant adhesive bowel obstruction: a retrospective study. Mol Clin Oncol. 2017;7(4):701–705. doi: 10.3892/mco.2017.1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.