Abstract
Introduction
Breast cancer is the most common type of cancer among women, particularly in low and middle-income countries. Breast self-examination is one of the non-invasive methods of screening in which a woman looks at her breast for any abnormal findings like lumps, distortions, or swellings. Despite, realized effects of breast self-examination in detecting breast cancer earlier, the vast majority of the cases still present with an advanced stage.
Objective
This study aimed to assess knowledge, attitude, and practices toward breast self-examination and associated factors among women in Gondar Town, Northwest Ethiopia, 2021.
Methods
A community-based cross-sectional study was conducted on women living in Gondar town. A simple random sampling method was used to select 571 participants. Interviewer administered questionnaires were used for data collection. Data was entered into Epi-data version 4.6 and exported to Statistical Package for Social Science (SPSS) version 25 for analysis. Multivariate logistic regression was used where a p-value < 0.05 was used to identify variables significantly associated with the outcome variable.
Result
From the total of 571 women, about 541 participants were involved in the study with a response rate of 94.7%. Of these, 56%, 46% and 45.8% of women had adequate knowledge, favourable attitudes, and performed breast self-examination (BSE) respectively. Women College and above AOR: 3.8 (95% CI: 1.43–10.14) and spouses College and above AOR: 3.03 (95% CI: 1.04–8.84), Women College and above AOR: 4.18 (95% CI: 1.59–10.92) and history of breast cancer AOR: 6.06 (95% CI: 2.19–16.74) and knowledge level AOR: 2.67 (95% CI: 1.18–6.04) were significantly associated with knowledge, attitudes, and practices towards breast self-examination respectively.
Conclusion
The findings of this study were considerable for inadequate knowledge, unfavourable attitude and poor practice towards BSE among women. Emphasis should be made on boosting the knowledge, attitude, and practice of the women toward breast self-examination and strengthening the implementation of comprehensive, systematic, and continuous BSE educational programs that were recommended along with a breast cancer awareness campaign.
Keywords: Attitude, Knowledge, Practice, Breast self-examination, Factors, Ethiopia
Introduction
Breast cancer is a type of malignant tumor that starts in the cells of the breast and commonly occurs in women [1]. This abnormal cell could destroy healthy tissue and then, spread beyond its usual boundaries [2]. Non-communicable diseases (NCD) including breast cancer considered not prevented, which is a noticeable common false perception of the community but it is a preventable cause of morbidity, disability, and mortality [3]. The most common risk factors of breast cancer are being a woman and getting ≥ 50 years old, having dense breasts, having a family history of breast cancer, early menstruation, and late menopause, late pregnancy, being on birth control pills, race, atypical hyperplasia of the breast, and previous treatment using radiation therapy [4, 5]. Lifestyle factors are obesity, lower amounts of physical activity, alcohol, and foods like high fats and low fiber diets [5]. Evidence suggested that; getting regular physical activity, staying at a healthy weight, limiting the amount of alcohol drink, avoiding the use of postmenopausal hormone therapy, breastfeeding, eating more fruits, vegetables, and fewer animal fats is linked with many health benefits and lower the risk of breast cancer [5]. Besides, it not only affect the breast tissue, but also spread to other part of the body organs like liver and lungs [6, 7].
According to global cancer statistics; breast cancer accounts for about 25% and 15% of total incidence and death respectively [8, 9]. In American an average risk of a woman of developing a breast cancer was 13% which is equivalent to one in every eight women had a chance of developing in their life time [10]. It is an important public health issues, not only in the developed world but also in resource limited nations [11]. It is the most frequent cause of death among women and estimated that 70% of all breast cancer cases worldwide were reported in low and middle-resource countries [12]. The incidence of breast cancer accounts for 22.6% of all cases of cancer in Ethiopia [13]. Breast self-examination (BSE) is one of the non-invasive methods of screening in which a woman looks at her breast for any abnormal findings like lumps, distortions, discharges or swellings with an intention to detect it early for early initiation of treatment and better chance of survival for breast cancer patients [14, 15].
Knowledge, attitude and practice of BSE have been reported in different countries. In regards to BSE knowledge 22.7% in Vietnam [16], 63.8% in Turkey [17], 41.5% in Libya [18], 34% in Sudan [19], 78% in Cameroon [20], 25.6% in Addis Ababa [21], 34.2% in Arba Minch [22], 43.1% in Jima [23], and 55.5% in Adwa town [24] had an adequate knowledge about breast self-examination. As per women’s attitude 64.01% in Saudi Arabia [25], 87.2% in Pakistan [26], 74.9% in Libya [18], 53.4% in Addis Ababa [21], and 46.3% in Adwa town [24] had a favorable attitude towards BSE. Considering practice towards BSE 43% in Saudi Arabia [27], 24.9% in Pakistan[26], 21% in Oman [28], 15.8% in Vietnam [16], 8.5% in turkey [17], 37.6% in Ghana [29], 38.5% in Cameroon [30], 39.2% in Egypt [31], 12.1% in Libya [18], 20.6% in Sudan [19], 13.3% in Arba Minch [32], and 18.6% in Addis Ababa [33] had a good practice of breast self-examination.
Factors affecting knowledge of the BSE were reported from the different countries. These are age, marital status, level of education, information of BSE, medical background, access to internet, source of information, and level of income. However, only the education levels and medical background for attitude towards BSE [16, 18, 26, 31, 33, 34]. Practice factors are almost similar to that of knowledge other than health education on breast cancer, knowing BSE techniques, occupation, and family history of breast cancer were related to women’s knowledge, attitude and practice towards BSE [16, 18, 33–38].
BSE is the only feasible approach that is cheap and easily applied method across wide population. Its ultimate purpose is early detection and treatment. Despite, its importance as an early detection strategy, poor knowledge of women has been a major obstacle. So, amplifying women’s knowledge, attitude, and practice towards BSE through creating breast cancer awareness campaign [39–43].
In our study area, there is a lack of evidence on women’s knowledge, attitude, and practice towards breast self-examination (BSE). Therefore, this study was aimed at assessing women’s knowledge, attitude, and practice on breast self-examination and thereby generates appropriate information that can be used by the central Gondar zonal health office and non-governmental organizations in the prevention and interventions of breast cancer.
Methods and materials
Study design, and period
A community-based cross-sectional study was conducted from April to May 2021.
Study setting
The study was conducted at Gondar Town, Northwest Ethiopia. Gondar Town is located 748 km from Addis Ababa the capital city of Ethiopia and 180 km from Bahir Dar capital city of Amhara regional state. The town has 6 sub-cities with 25 Kebele and 127,115 houses. Gondar Town is one of the ancient and densely populated towns in Ethiopia. According to the central Gondar zonal health office 2021 GC report, Gondar has a total population of 432,191 of whom 215,663 are men and 216,538 women. Nowadays the town is growing and it had 8 health centers, more than 15 private medical clinics, one private primary hospital, and one Comprehensive Specialized Hospital serving about 5 million populations.
Source population and study population
All adult women who are living in Gondar town were the source population. All women who are living in Gondar town during the data collection period were considered as the study population.
Inclusion and exclusion criteria
All women who were 20–70 age group living in Gondar town during the study period were included. Women who are severely ill during data collection time and those who refuse to participate in the study were excluded.
Sample size determination and calculation
The actual sample size for the study was determined using single population proportion formula with the assumption of 34.2% knowledgeable of BSE [32], 95% confidence interval; (α = 0.05), 5% margin of error, 10% none response rate, and 1.5 design effect.
where n = is the minimum sample required; P = population proportion, 0.342; d = the margin of error, 0.05; Z = the upper percentile of the normal distribution at 95% CI.
By Multiply 1.5 design effect n = 519, adding 10% non-response rate = 52 and the final sample size would be 571 (Table 1). Sample size calculation on second the objective in the same study showed that only practice was significantly associated with BSE (Table 2).
Table 1.
Sample size calculation for the dependent and independent variables among women in Gondar town, Northwest Ethiopia, 2021
| Variable | Assumption | P-value (%) | Sample size | Non-response (10%) | Design effect (1.5) | Reference |
|---|---|---|---|---|---|---|
| Knowledge | CI = 95% margin of error (α = 5%) | 34.2 | 346 | 381 | 571 | [32] |
| Attitude | 14.5 | 191 | 210 | 315 | ||
| Practices | 21.3 | 258 | 284 | 426 |
Table 2.
Sample size calculation for associated factors with breast self-examination among women in Gondar town, Northwest Ethiopia, 2021
| Factors | Assumption | Proportion | Initial sample size | 1.5 Design effect | 10% Non-response | Reference |
|---|---|---|---|---|---|---|
| Age of the women | CI = 95% | P1 = 23.22% | 242 | 363 | 400 | [32] |
| Power = 80 | P2 = 39.19% | |||||
| Women’s level of education | Ratio 1:1 | P1 = 15.81% | 136 | 204 | 225 | |
| P2 = 38.46% | ||||||
| Women’s level of knowledge | Practice of BSE | P1 = 13.28% | 138 | 207 | 228 | |
| P2 = 35.02% |
The final sample size was from a single population proportion and the second objective was used the maximal one take from single population proportion knowledge of BSE = 571.
Sampling technique and procedures
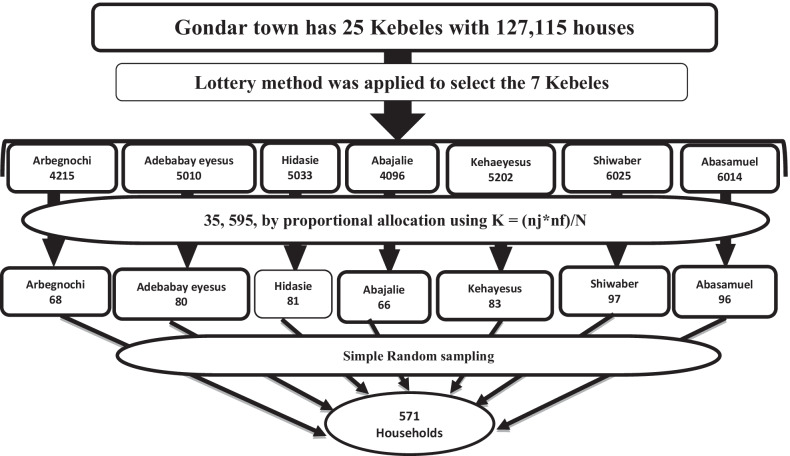
A multi-stage sampling method was applied for the selection of houses from each Kebele. Firstly, Out of 25 kebeles in the Gondar town, 7 kebeles such as Aribengochi, Adebabayeyesuse, Abajalie, kehaeyesus, Shiwaber, Hidasie, and Aba Samuel kebele were randomly selected by lottery method to represent all kebeles (28% representativeness). Secondly, a systematic sampling technique was used to label the households within each Kebele The proportional allocation formula for each Kebele is ; Were, nf = final sample size, nj = total number of houses each Kebele, N = total number of houses (Fig. 1). Lastly, a simple random sampling was used to select 571 study participants within households using the sampling frame.
Fig. 1.
The schematic presentation of sampling procedure to select the study households of women aged 20–70 at Gondar Town, Northwest Ethiopia, 2021 (n = 571)
Data collection tools and procedures
The questionnaire was adapted from different works of literature [26, 44, 45]. The questionnaire was first prepared in English, and then it was translated into Amharic language and back to English. It contains four parts such as socio-demographic characteristics (n = 9), knowledge (n = 12), attitude (n = 13), and practice (n = 8) items. Then the data were collected by 5 data collectors using face-to-face interviewer administer questionnaires. The overall supervision was carried out by the principal investigator.
Operational definition
Adequate knowledge: It refers to participants who scored mean and above values 8 from the provided 12 close-ended questions about the knowledge of BSE [46].
Inadequate knowledge: It refers to participants who scored below mean values 8 from the provided 12 close-ended questions about the knowledge of BSE [46].
Favorable attitude: It refers to participants who scored mean and above values 6 for attitude-related questions towards BSE, which was measured by the provided 12 questions [46].
Unfavorable attitude: It refers to participants who scored below mean values 6 for attitude-related questions towards BSE, which was measured by the provided 12 questions [46].
Good practice: It refers to those who checked or perform BSE at least once per month just a week after each menses [47].
Poor practice: It refers to those who practice BSE other than the correct time in the cycle [47].
Data quality control
Pretest was done on 5% of the total sample size from the non-selected kebele of the same population before 4 days of actual data collected. Two days of training were given for data collectors and supervisors by investigators on the objectives of the study, ethical considerations, the content of the questionnaire, and how to conduct the interview. Based on the pre-test, questionnaires were edited, and necessary corrections made were on order of questions and that poses participant to confusion. The reliability of the tool on Cronbach’s alpha results knowledge = 0.81, attitude = 0.86, and practice = 0.71. The collected data was checked out for completeness, accuracy, and clarity by the principal Investigators before data entry.
Data processing and analysis
Data were entered using Epi data version 4.6 software and analyzed using SPSS version 25. Data cleaning and cross-checking were done before analysis. Descriptive statistics were summarized using the mean, and standard deviation. Frequencies and percentages were used in the presented table, figures and text. Multivariate logistic regression analysis were used to identify factors where p-value < 0.05 was declared as significantly associated with knowledge, attitudes, and practices of breast self-examination.
Result
Socio-demographic characteristics
Out of 571 participants, 541 agree to participate in the study, yielding a response rate of 95%. Nearly half (47.5%) of the participants were within the age range between 20 and 29 years. The minimum and maximum age of the participants was 20 and 69 respectively, the majority of women (87.4%) and 36.8% were orthodox and completed secondary education level respectively. Among the participants, 62.1% and 49.9% were married and housewives respectively (Table 3).
Table 3.
Socio-demographic characteristics of the women aged 20–70 at Gondar Town, Northwest Ethiopia, 2021
| Variables | Response | Frequency | Percent |
|---|---|---|---|
| Age of the women | 20–29 years | 257 | 47.5 |
| 30–39 years | 153 | 28.3 | |
| 40–49 years | 54 | 10.0 | |
| 50–70 years | 77 | 14.2 | |
| Marital status | Single | 125 | 23.1 |
| Married | 336 | 62.1 | |
| Widowed | 36 | 6.7 | |
| Divorced | 44 | 8.1 | |
| Religion | Orthodox | 473 | 87.4 |
| Muslim | 54 | 10.0 | |
| Protestant | 13 | 2.4 | |
| Catholic | 1 | 0.2 | |
| Level of education | Illiterate | 76 | 14.0 |
| Primary school | 105 | 19.4 | |
| Secondary school | 199 | 36.8 | |
| College and University | 161 | 29.8 | |
| Occupation | Housewife | 270 | 49.9 |
| Merchant | 60 | 11.1 | |
| Student | 76 | 14.0 | |
| Governmental employee | 81 | 15.0 | |
| House worker | 54 | 10.0 | |
| Husband’s educational level | Illiterate | 44 | 13.1 |
| Primary | 70 | 20.8 | |
| Secondary | 105 | 31.3 | |
| College and University | 117 | 34.8 | |
| Monthly income | < 500 Birr | 22 | 4.1 |
| 500–1000 Birr | 36 | 6.7 | |
| ≥ 1001 Birr | 483 | 89.3 | |
| History of breast cancer | Yes, I have | 35 | 6.5 |
| No, I don't have | 506 | 93.5 |
Knowledge towards breast self-examination and their information source
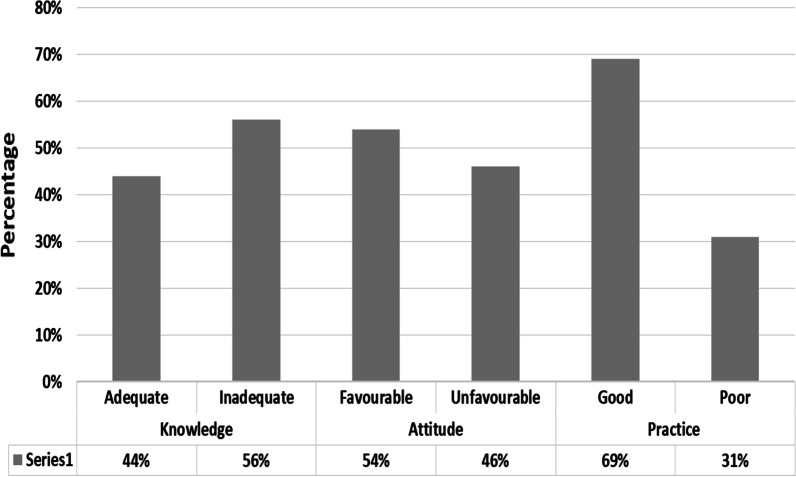
Among the respondents, 66% of participants heard about breast self-examination. The majority (56%) (95% CI: 51–61) of participants had adequate knowledge (Fig. 2) and their main source of information was television/radio (43.2%), health institution/profession (30.8%), peer group, and school training (15.6%) and from newspaper and internet (10.2%) (Table 4).
Fig. 2.
The overall status of knowledge, attitude, and practice towards Breast self- examination among women aged 20–70 at Gondar Town, Northwest Ethiopia, 2021 (n = 571)
Table 4.
Knowledge towards breast self-examination among women aged 20–70 at Gondar Town, Northwest Ethiopia, 2021
| Questions | Responses | Percentage/frequency |
|---|---|---|
| Have you ever heard of breast self-examination before? | Yes | 66.0% (n = 357) |
| No | 34.0% (n = 184) | |
| Where did heard from? | Healthcare provider | 28.9% (n = 103) |
| Peer group | 20.4% (n = 73) | |
| Television/Radio | 38.1% (n = 136) | |
| Newspaper | 12.6 (n = 45) | |
| Does early detection of breast cancer improve chances of survival? | Yes | 86.0% (n = 307) |
| No | 14.0% (n = 50) | |
| Who should perform BSE? | Males only | 0 |
| Females only | 81.0% (n = 289) | |
| Both | 19.0% (n = 68) | |
| Don’t know | 0 | |
| Is BSE important in the early detection of breast cancer? | Important | 68.3% (n = 244) |
| Not important | 31.7% (n = 113) | |
| I don’t know | 0 | |
| How often should breast self-examination be performed? | Weekly | 39.2% (n = 104) |
| Monthly | 54.3% (n = 144) | |
| Yearly | 4.9% (n = 13) | |
| Don’t know | 1.5% (n = 4) | |
| Where did the appropriate place to perform BSE? | While lying in the bed | 43.2% (n = 236) |
| In front of the mirror | 17.6% (n = 96) | |
| While having a bath | 39.3% (n = 215) | |
| Changes in the shape and color of the breast are the signs of breast cancer | Yes | 37.0% (n = 132) |
| No | 63.0% (n = 225) | |
| Lumps in the breast and around the armpit are the signs of breast cancer | Yes | 66.4% (n = 237) |
| No | 33.6% (n = 120) | |
| Nipple discharge and retraction are the signs of breast cancer | Yes | 66.9% (n = 238) |
| No | 33.1% (n = 118) | |
| How do you prefer your breast examination to be done? | By nurse/doctor | 65.0% (n = 232) |
| By yourself | 35.0% (n = 125) | |
| Where will you go, if there are any symptoms of breast cancer | Health facility | 99.2% (n = 354) |
| Traditional healer | 0.8% (n = 3) |
Attitude towards breast self-examination
Among 541 study participants, 46.0% (95% CI: 42–52) had positive attitudes towards breast self-examination, 60.3% of the respondents score breast self-examination as necessary (Table 5).
Table 5.
Attitude towards breast self-examination among women aged 20–70 at Gondar Town, Northwest Ethiopia, 2021
| Questions | Responses | Percentage/frequency |
|---|---|---|
| Breast self-examination is necessary | Yes | 60.3% (n = 326) |
| No | 39.7% (n = 215) | |
| Do you think breast self-examination can give you a benefit | Yes | 60.1% (n = 325) |
| No | 39.9% (n = 216) | |
| During BSE makes me feel so funny | Yes | 6.3% (n = 34) |
| No | 93.7% (n = 507) | |
| BSE is not embarrassing to me | Yes | 79.7% (n = 431) |
| No | 20.3% (n = 110) | |
| Doing BSE is not wasting time | Yes | 44.9% (n = 243) |
| No | 55.1% (n = 298) | |
| After doing BSE makes me feel satisfying | Yes | 44.2% (n = 239) |
| No | 55.8% (n = 302) | |
| If there is a lump, I prefer to get treatment from a health institution | Yes | 46.2% (n = 250) |
| No | 53.8% (n = 291) | |
| If I can do BSE once a month, I feel comfortable | Yes | 41.8% (n = 226) |
| No | 58.2% (n = 315) | |
| All women should do BSE | Yes | 44.7% (n = 242) |
| No | 55.3% (n = 299) | |
| I care about my breasts | Yes | 44.4% (n = 240) |
| No | 55.6% (n = 301) | |
| I'm afraid to think about the breast cancer | Yes | 87.1% (n = 471) |
| No | 12.9% (n = 71) | |
| Because I always worry about having breast cancer, I want to do BSE | Yes | 39.9% (n = 216) |
| No | 60.1% (n = 325) |
Practices towards breast self-examination
Among 541 study participants, 248 (45.8%) performing breast self-examination and 31% (95% CI: 25–37%) had good practices of breast self-examination (Fig. 2). From the total respondents, more than half 54.2% (n = 293) of them did not practice BSE. The main reasons for not practicing BSE 175 (57.4%) were not having breast problems and 31.7% (n = 93) don’t know how to breast self-examine (Table 6).
Table 6.
Practice towards breast self-examination among women aged 20–70 at Gondar Town, Northwest Ethiopia, 2021
| Questions | Responses | Percentage/frequency |
|---|---|---|
| Have you ever done breast self-examination? | Yes | 45.8% (n = 248) |
| No | 54.2% (n = 293) | |
| If ‘Yes’ when did you perform it? | Just a week after each menses | 31% (n = 77) |
| When it comes to mind | 52.4% (n = 130) | |
| Anytime during menses | 10.9% (n = 27) | |
| Before menses | 5.6% (n = 14) | |
| If ‘No’ then why haven’t you performed it? | Fear of detecting an anomaly | 0.3% (n = 1) |
| there are no problems with my breast | 58.4% (n = 171) | |
| Not necessary | 7.5% (n = 22) | |
| Too busy | 2.0% (n = 6) | |
| Don’t know how to self-examine | 31.7% (n = 93) | |
| How is breast self-examination done? | Palpate with one finger | 1.2% (n = 3) |
| Palpate with palm and three fingers | 98.4% (n = 244) | |
| I do not know | 0.4% (n = 1) | |
| At what age did you start breast self-examination? | 20–29 years | 56.5% (n = 140) |
| 30–39 years | 28.6% (n = 71) | |
| 40–49 years | 12.9% (n = 32) | |
| 50-70 years | 2.0% (n = 5) | |
| What time do you normally perform Breast self-examination? | Morning | 21.8% (n = 54) |
| Afternoon | 18.1% (n = 45) | |
| Evening | 60.1% (n = 149) | |
| Where do you usually perform breast self-examination? | In front of the mirror | 18.4% (n = 73) |
| Lying on the bed | 45.8% (n = 182) | |
| In the bathroom | 35.8% (n = 142) | |
| On identifying an abnormality in your breasts, what would you do? | Tell mother | 4.4% (n = 11) |
| Tell spouse | 6.5% (n = 16) | |
| Consult doctor/nurse | 89.1 (n = 221) | |
| Not do anything about it due to embarrassment | 0 | |
| Option for traditional healing | 0 |
Factors associated with breast self-examination
All independent variables entered into the logistic regression (multivariable logistic regression analysis). Women’s and husbands' education level were significantly associated with knowledge. The age of the women and women’s educational level was significantly associated with the attitude of BSE. History of breast cancer and good knowledge of BSE were significantly associated with performing BSE. Women college and above were about 4 times [AOR: 3.8, (95% CI: 1.43–10.14)] more likely to know of BSE than those who uneducated women. The spouses whose educational level College and above was about 3 times [AOR: 3.03, (95% CI: 1.04–8.84)] more likely to be knowledgeable towards BSE than those who had an illiterate husband (Table 7).
Table 7.
Bivariate and multivariate analysis of factors associated with knowledge of BSE among women aged 20–70 at Gondar Town, Northwest Ethiopia, 2021
| Variables | Knowledge of BSE | P-value | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|---|
| Adequate | Inadequate | ||||
| Age of the women | |||||
| 20–29 years | 81 | 72 | 1.0 | 1.0 | 1.0 |
| 30–39 years | 66 | 45 | 0.293 | 1.30 (0.80–2.14) | 1.12 (0.61–2.06)) |
| 40–49 years | 28 | 16 | 0.210 | 1.56 (0.78–3.11) | 2.12 (0.92–4.86)) |
| 50–70 years | 25 | 24 | 0.815 | 0.93 (0.49–1.76) | 1.21 (0.51–2.89) |
| Marital status | |||||
| Single | 39 | 33 | 1.0 | 1.0 | 1.0 |
| Married | 128 | 96 | 0.658 | 1.13 (0.66–1.92) | 0.51 (0.16–1.68) |
| Widowed | 15 | 12 | 0.902 | 1.06 (0.44–2.57) | 1.42 (0.43–4.69) |
| Divorced | 18 | 16 | 0.906 | 0.95 (0.42–2.16) | 1.53 (0.53–4.36) |
| Level of education | |||||
| Illiterate | 9 | 22 | 1.0 | 1.0 | 1.0 |
| Primary school | 21 | 39 | 0.834 | 0.91 (0.38–2.17) | 0.67 (0.26–1.71) |
| Secondary | 72 | 66 | 0.154 | 1.74 (0.81–3.75) | 1.41 (0.59–3.31) |
| College& above | 98 | 30 | 0.000 | 5.53 (2.49–12.28) ** | 3.80 (1.43–10.14) ** |
| Occupation | |||||
| Maid | 11 | 20 | 1.0 | 1.0 | 1.0 |
| Merchant | 28 | 19 | 0.040 | 2.68 (1.05–6.85) * | 1.56 (0.51–4.71) |
| Student | 26 | 17 | 0.036 | 2.78 (1.09–7.24) * | 1.86 (0.65–5.29) |
| Gov’t employee | 53 | 15 | 0.000 | 6.42 (2.53–16.33) ** | 2.11 (0.65–6.85) |
| Housewife | 82 | 86 | 0.175 | 1.73 (0.78–3.84) | 1.38 (0.49–3.90) |
| Spouse educational level | |||||
| Illiterate | 9 | 17 | 1.0 | 1.0 | 1.0 |
| Primary | 19 | 17 | 0.159 | 2.1 (0.75–5.97) | 2.60 (0.83–8.20) |
| Secondary | 32 | 37 | 0.304 | 1.63 (0.64–4.17) | 1.94 (0.68–5.54) |
| College and above | 68 | 25 | 0.001 | 5.14 (2.03–13.01) ** | 3.03 (1.04–8.84) ** |
| Women monthly income | |||||
| < 500 Birr | 7 | 12 | 1.0 | 1.0 | 1.0 |
| 500–1000 Birr | 7 | 16 | 0.661 | 0.75 (0.21–2.72) | 1.43 (0.36–5.68) |
| > 1001 Birr | 186 | 129 | 0.064 | 2.47 (0.95–6.45) | 2.31 (0.81–6.59) |
| History of breast cancer | |||||
| No, I don’t have | 191 | 149 | 1.0 | 1.0 | 1.0 |
| Yes, I have | 9 | 8 | 0.361 | 1.45 (0.65–3.25) | 1.77 (0.71–4.44) |
**Indicates P-value < 0.001 strongly associated, *Indicates P-value < 0.05 weakly associated, 1.0 indicates reference
Women College and above was about 4 times [AOR: 4.18 (95% CI: 1.59–10.92)] and secondary school was about 3 times [AOR: 2.80 (95% CI: 1.25–6.29)] had favorable attitudes towards BSE than those women who are illiterate (Table 8).
Table 8.
Bivariate and multivariate analysis of factors associated with Attitude towards BSE among women aged 20–70 at Gondar Town, Northwest Ethiopia, 2021
| Variables | Attitude of BSE | P-value | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|---|
| Positive | Negative | ||||
| Age of the women | |||||
| 20–29 year | 109 | 148 | 0.015 | 1.0 | 1.0 |
| 30–39 year | 77 | 76 | 0.120 | 1.38 (0.92–2.06) | 1.11 (0.61–2.01) |
| 40–49 year | 29 | 25 | 0.131 | 1.58 (0.87–2.84) | 1.15 (0.48–2.74) |
| 50–70 year | 33 | 44 | 0.945 | 1.02 (0.61–1.70) | 1.12 (0.47–2.66) |
| Marital status | |||||
| Single | 52 | 73 | 0.062 | 1.0 | 1.0 |
| Married | 156 | 180 | 0.355 | 1.22 (0.80–1.84) | 1.29 (0.39–4.25) |
| Widowed | 20 | 16 | 0.140 | 1.76 (0.83–3.71) | 2.52 (0.72–8.78) |
| Divorced | 20 | 24 | 0.657 | 1.17 (0.59–2.34) | 1.43 (0.45–4.48) |
| Level of education | |||||
| Illiterate | 19 | 57 | 0.000 | 1.0 | 1.0 |
| Primary school | 27 | 78 | 0.913 | 1.04 (0.53–2.05) | 1.15 (0.48–2.72) |
| Secondary | 94 | 105 | 0.001 | 2.69 (1.49–4.84)* | 2.80 (1.25–6.29) * |
| College and above | 108 | 53 | 0.000 | 6.11 (3.31–11.30)* | 4.18 (1.59–10.92) ** |
| Occupation | |||||
| Maid | 12 | 42 | 1.0 | 1.0 | 1.0 |
| Merchant | 31 | 29 | 0.002 | 3.74 (1.65–8.47) * | 1.79 (0.55–5.92) |
| Student | 39 | 37 | 0.001 | 3.69 (1.69–8.08)** | 3.17 (0.11–9.02) |
| Gov’t employee | 51 | 30 | 0.000 | 5.95 (2.72–13.03) ** | 1.20 (0.35–4.17) |
| Housewife | 115 | 155 | 0.006 | 2.59 (1.31–5.15)* | 2.88 (0.96–8.66) |
| Spouse educational level | |||||
| Illiterate | 15 | 29 | 1.0 | 1.0 | 1.0 |
| Primary | 19 | 51 | 0.431 | 0.72 (0.32–1.63) | 0.41 (0.14–1.19) |
| Secondary | 46 | 59 | 0.272 | 1.51 (0.72–3.14) | 0.93 (0.35–2.49) |
| College and above | 76 | 41 | 0.001 | 3.58 (1.73–7.44) ** | 1.19 (0.42–3.38) |
| Women monthly income | |||||
| < 500 Birr | 10 | 12 | 1.0 | 1.0 | 1.0 |
| 500–1000 Birr | 10 | 26 | 0.173 | 0.46 (0.15–1.40) | 0.72 (0.16–3.17) |
| > 1001 Birr | 228 | 255 | 0.872 | 1.07 (0.46–2.53) | 0.71 (0.22–2.31) |
| History of cancer | |||||
| No, I don’t have | 226 | 280 | 1.0 | 1.0 | 1.0 |
| Yes, I have | 22 | 13 | 0.040 | 2.096 (1.03–4.26) | 1.56 (0.62–3.94) |
**Indicates P-value < 0.001 strongly associated, *indicates P-value < 0.05 weakly associated, 1.0 indicates reference
Women who have personal and family history of breast cancer were about 6 times [AOR: 6.06, (95% CI: 2.19–16.74)] more likely to perform BSE than women who do have not the history of breast cancer. A woman who has adequate knowledge of BSE about 3 times [AOR: 2.67 (95% CI: 1.18–6.04)] is more likely to perform BSE than women who have inadequate knowledge (Table 9).
Table 9.
Bivariate and multivariate analysis of factors associated with the practice of BSE among women aged 20–70 at Gondar Town, Northwest Ethiopia, 2021
| Variables | Practices of BSE | P-value | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|---|
| Good | Poor | ||||
| Age of the women | |||||
| 20–29 | 30 | 63 | 1.0 | 1.0 | 1.0 |
| 30–39 | 28 | 49 | 0.574 | 1.20 (0.64–2.27) | 0.92 (0.39–2.11) |
| 40–49 | 11 | 24 | 0.929 | 0.96 (0.42–2.22) | 0.93 (0.31–2.75) |
| 50–70 | 8 | 35 | 0.103 | 0.48 (0.12–1.16) | 0.47 (0.14–1.59) |
| Marital status | |||||
| Single | 12 | 32 | 1.0 | 1.0 | 1.0 |
| Married | 51 | 106 | 0.511 | 1.28 (0.61–2.70) | 1.56 (0.27–8.97) |
| Widowed | 7 | 16 | 0.785 | 1.17 (0.39–3.54) | 2.07 (0.41–10.42) |
| Divorced | 7 | 17 | 0.868 | 1.20 (0.37–3.31) | 1.56 (0.34–7.08) |
| Level of education | |||||
| Illiterate | 5 | 17 | 1.0 | 1.0 | 1.0 |
| Primary school | 5 | 35 | 0.301 | 0.49 (0.12–1.91) | 0.35 (0.07–1.78) |
| Secondary | 16 | 66 | 0.739 | 0.82 (0.26–2.57) | 0.88 (0.23–3.43) |
| College and above | 51 | 53 | 0.030 | 3.27 (1.12–9.53) | 3.15 (0.77–12.88) |
| Occupation | |||||
| Maid | 5 | 15 | 1.0 | 1.0 | 1.0 |
| Merchant | 12 | 19 | 0.314 | 1.89 (0.55–6.57) | 1.64 (0.33–8.09) |
| Student | 6 | 20 | 0.880 | 0.90 (0.23–3.52) | 0.76 (0.16–3.65) |
| Gov’t employee | 29 | 29 | 0.058 | 3.00 (0.96–9.34) | 2.75 (0.57–13.39) |
| Housewife | 25 | 88 | 0.777 | 0.85 (0.28–2.57) | 1.27 (0.28–5.78) |
| Spouse educational level | |||||
| Illiterate | 5 | 12 | 1.0 | 1.0 | 1.0 |
| Primary | 5 | 15 | 0.764 | 0.80 (0.18–3.42) | 0.68 (0.12–4.05) |
| Secondary | 8 | 35 | 0.364 | 0.55 (0.15–2.00) | 0.51(0.10–2.55) |
| College above | 33 | 44 | 0.311 | 1.80 (0.58–5.61) | 0.67 (0.15–2.92) |
| History of cancer | |||||
| No, I don’t have | 59 | 154 | 1.0 | 1.0 | 1.0 |
| Yes, I have | 18 | 17 | 0.006 | 2.76 (1.34–5.72) * | 6.06 (2.19–16.74) ** |
| Knowledge | |||||
| Inadequate | 13 | 67 | 1.0 | 1.0 | 1.0 |
| Adequate | 64 | 104 | 0.001 | 3.17 (1.62–6.20) ** | 2.67 (1.18–6.04) * |
| Attitudes | |||||
| Unfavorable | 9 | 39 | 1.0 | 1.0 | 1.0 |
| Favorable | 68 | 132 | 0.044 | 2.23 (1.02–4.88) | 1.99 (0.76–5.27) |
**Indicates P-value < 0.001 strongly associated, *indicates P-value < 0.05 weakly associated, 1.0 indicates reference
Discussion
The aim of this study was to assess knowledge, attitude, practice, and associated factors of breast self-examination among women in Gondar town. In this study, more than half 56% (n = 200) (95% CI: 52–62%) of the study participants had adequate knowledge regarding BSE, which is comparable with study conducted in Ethiopia that indicated 55.5% in Adwa town [24]. This similarities could be due to similar study subjects.
However, the finding is higher than that of Vietnam 22.7% [16], 34% Sudan [19], 41.5% Libya [18], 34.2% Arba Minch [32], 43.1% Jimma [23], and 25.6% Addis Ababa [21]. The difference might be due to by self-reporting data collection technique in Vietnam and Sudan, and the clustered sampling procedure was used in Libya. The self-reporting data collection method requires participants to respond to the researcher's questions without his/her interference [48]. In Ethiopia, the possible justification might be the educational level difference. In our study, 29.8% of participants were College and above educational status, but only 14.4% of study participants in Arba Minch, and 18.8% in Jima were college and above educational status. This finding is lower than the study conducted in Cameroon 78% [20], and 63.8% in Turkey [17]. The possible justification might be due to socio-economic, and study population differences. The current study was community-based, but that of Cameroon was conducted on patients attending a surgical outpatient clinic.
In this finding, about 46% (95% CI: 42–52%) of participants had a positive attitude towards breast self-examination, which is comparable with the study conducted in Ethiopia that indicated 46.3% in Adwa town [24].This consistency might be due to similar socio-cultural status and study population whose age were 20–70. However, it is lower than the studies conducted in Saudi Arabia 64.01% [25], 87.2% Pakistan [26], and 74.9% Libya [18]. This difference might be due to sampling size difference, educational level, and participant’s knowledge towards BSE, occupational difference, and information access availability.
In this finding, Nearly one-third 31% (n = 77) (95% CI: 25–37%) of participants had good practices towards BSE, which is comparable with the study done in Addis Ababa, 28.4% [33]. This consistency might be due to similar socio-cultural and economic status. Besides, factors that affect practice for early detection of BSE might be similar in both study settings. On contrary, this study is higher than the studies conducted in Arba Minch 13.3% [32], 12.1% Libya [18], and 8.5% Turkey [17]. The difference might be knowledge difference, and in Arba Minch, the majority (45%) of the participants are illiterate. On the other hand, this finding was lower than the studies conducted in Saudi Arabia 43% [27], and 37.6% in Ghana [29]. The possible justification might be educational and knowledge differences. In Saudi Arabia, the majority (65%) of participants had adequate knowledge about BSE, and 79% of the participant had an educational level completed university, whereas 88% of participants were aware of BSE in Ghana.
In this study, women’s educational level at College and University were about 4 times [AOR: 3.8, 95% CI: (1.43–10.14)] more likely to be knowledgeable with BSE than those who are illiterate. Also, the women whose husbands had an educational level College and University were about 3 times [AOR: 3.03, 95% CI: (1.04–8.84)] more likely to knowledgeable than those had illiterate husbands. Evidence shows that training women about breast self-examination goes correspondingly with their educational attainment of College level and above has a positive impact on their related knowledge and practices [49, 50].
Women’s College and above was also one of the significant factors for the attitudes of breast self-examination, women’s College and above was about 4 times AOR:4.18, (95% CI: 1.59–10.92) and secondary school was about 3 times [AOR: 2.80, 95% CI: (1.25–6.29)] more likely to had positive attitude towards BSE than women those who are illiterate. it was supported by the study done in Libya [18], and Turkey [17]. This might be due to educational attainment of secondary school and above could increase women’s attitudes towards breast self-examination besides it also enhance compliance towards breast self-examination behavior [51].
In this study, women who have a history of breast cancer were about 6 times [AOR: 6.06, 95% CI: (2.19–16.74)] more likely to perform BSE than their counter parts. This study was in line with the studies conducted in Jimma [23], Addis Ababa [36], and Libya [18]. A family history of breast cancer is positively affecting the practice of breast self-examination [52]. This could be women with a history of breast cancer performing breast self-examination at a regular basis and making them more cognizant, which in turn may lead to an earlier diagnosis of breast cancer.
Limitations
As practice was not directly observed rather we used checklist that will not know how exactly they were practicing it. Other limitations were being conducted in a single urban community, which may not be representative of the rural community or other urban communities in Ethiopia.
Conclusion
The findings of this study were considerable for inadequate knowledge, unfavorable attitude and poor practice towards BSE among women. Emphasis should be made to boost the attitude and practice of the women towards breast self-examination and strengthening of the implementation of comprehensive, systematic, and continuous BSE educational programs were recommended along with a breast cancer awareness campaign.
Acknowledgements
Our gratitude goes to the School of Nursing, College of Medicine and Health Sciences, the University of Gondar for giving us the chance to conduct this research. The authors' thank also goes to Gondar Town Kebele administrators and all study participants.
Abbreviations
- ACS
American Cancer Society
- BCA
Breast Cancer
- BSE
Breast self-examination
- CBE
Clinical breast examination
- ECA
Ethiopian Cancer Association
- SPSS
Statistical package social science
- COR
Crude odds ratio
- AOR
Adjusted odds ratio
- CI
Confidence interval
- UoG
University of Gondar
Author contributions
KA, ZW, and YB: Conceived, designed and organized the whole procedure of this article production, performed data analysis and interpreting of findings and performed data analysis, interpreting of findings and coaching and mentoring, and equally prepare the manuscript. All authors read and approved the final manuscript.
Funding
Not applicable.
Availability of data and materials
The datasets used/or analyzed during the current study is available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Ethical clearance was obtained from the Institutional Review Board (IRB) of the School of Nursing from the University of Gondar with reference number: S/N/121/5/2011. A permission letter was written from the School of Nursing to each Kebele Administrator of Gondar town. Then, the Kebele administrator allowed to conduct the study. The informed verbal consent was obtained from each study participant. Confidentiality was maintained by avoiding registration of personal identifiers like name, resident identification, and also no raw data was given to any other person. All methods were carried out in accordance with the Helsinki declarations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Kibret Asmare, Email: 2009kibretasmare@gmail.com.
Yeneabat Birhanu, Email: birhanuyeneabat@gmail.com.
Zerko Wako, Email: zerkowako1992@gmail.com.
References
- 1.Akram M, Iqbal M, Daniyal M, Khan AU. Awareness and current knowledge of breast cancer. Biol Res. 2017;50(1):1–23. doi: 10.1186/s40659-017-0140-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Milosevic M, Jankovic D, Milenkovic A, Stojanov D. Early diagnosis and detection of breast cancer. Technol Health Care. 2018;26(4):729–759. doi: 10.3233/THC-181277. [DOI] [PubMed] [Google Scholar]
- 3.Makary MA, Daniel M. Medical error—the third leading cause of death in the US. BMJ. 2016;353:i2139. doi: 10.1136/bmj.i2139. [DOI] [PubMed] [Google Scholar]
- 4.Kamińska M, Ciszewski T, Łopacka-Szatan K, Miotła P, Starosławska E. Breast cancer risk factors. Menopause Rev. 2015;14(3):196. doi: 10.5114/pm.2015.54346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sun Y-S, Zhao Z, Yang Z-N, Xu F, Lu H-J, Zhu Z-Y, et al. Risk factors and preventions of breast cancer. Int J Biol Sci. 2017;13(11):1387. doi: 10.7150/ijbs.21635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Waks AG, Winer EP. Breast cancer treatment: a review. JAMA. 2019;321(3):288–300. doi: 10.1001/jama.2018.19323. [DOI] [PubMed] [Google Scholar]
- 7.Tan PH, Ellis I, Allison K, Brogi E, Fox SB, Lakhani S, et al. The 2019 World Health Organization classification of tumours of the breast. Histopathology. 2020;77:181–185. doi: 10.1111/his.14091. [DOI] [PubMed] [Google Scholar]
- 8.Iacorossi L, Gambalunga F, Fabi A, Giannarelli D, Facchinetti G, Piredda M, et al. Adherence to hormone therapy in women with breast cancer: a quantitative study. Prof Inferm. 2016;69(2). [DOI] [PubMed]
- 9.Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA A Cancer J Clin. 2015;65(2):87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 10.DeSantis CE, Ma J, Gaudet MM, Newman LA, Miller KD, Goding Sauer A, et al. Breast cancer statistics 2019. CA A Cancer J Clin. 2019;69(6):438–51. doi: 10.3322/caac.21583. [DOI] [PubMed] [Google Scholar]
- 11.Roy I, Othieno E. Breast Carcinoma in Uganda. Arch Pathol Lab Med. 2011;135:194–199. doi: 10.5858/2008-0421-SOR1.1. [DOI] [PubMed] [Google Scholar]
- 12.Lera T, Beyene A, Bekele B, Abreha S. Breast self-examination and associated factors among women in Wolaita Sodo, Ethiopia: a community-based cross-sectional study. BMC Womens Health. 2020;20(1):1–10. doi: 10.1186/s12905-020-01042-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.John R. Global cancer facts and figures 4th edition-special section, the obesity epidemic. Am Cancer Soc. 2018;76:1–73. [Google Scholar]
- 14.DeSantis C, Ma J, Bryan L, Jemal A. Breast cancer facts and figures 2013–2014. Atlanda: American Cancer Society, Inc.; 2013. [Google Scholar]
- 15.Tarver T. Cancer facts and figures 2012. American Cancer Society (ACS) Atlanta, GA: American Cancer Society, 2012. Available from Taylor & Francis; 2012.
- 16.Tuyen DQ, Dung TV, Dong HV, Kien TT, Huong TT. Breast self-examination: knowledge and practice among female textile workers in Vietnam. Cancer Control. 2019;26(1):1073274819862788. doi: 10.1177/1073274819862788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Karahan N. Prevalence and determinants of breast self-examination in Karabuk. Turkey Cukurova Med J. 2019;44(3):1046–1054. [Google Scholar]
- 18.Ziuo FM, Twoier AA, Huria TR, El-Khewisky FS. Low awareness about breast self-examination and risk factors of breast cancer in Benghazi, Libya. Ibnosina J Med Biomed Sci. 2018;10(2):54. doi: 10.4103/ijmbs.ijmbs_16_17. [DOI] [Google Scholar]
- 19.Nugod SMAM. Breast self examination knowledge among females in Salha, Omdurman locality, Khartoum State, Sudan (2016): University of Gezira; 2016.
- 20.Alegbeleye BJ, Jantchou P. Knowledge and practices of breast self-examination amongst women attending a surgical outpatient clinic, Cameroon. Breast cancer. 2018;13.
- 21.Chimdi C. Assessment of knowledge, attitude and practice of breast self-examination among women aged 20–49 years in Addis Ababa. Ethiopia: Addis Ababa University; 2017. [Google Scholar]
- 22.Mereta B, Shegaze M, Mekonnen B, Desalegn N, Getie A, Abdilwohab MG. Assessment of breast self-examination and associated factors among women age 20–64 years at Arba Minch Zuria District, Gamo Zone Snnpr Ethiopia, 2019. 2020.
- 23.Terfa YB, Kebede EB, Akuma AO. Breast self-examination practice among women in Jimma, Southwest Ethiopia: A Community-Based Cross-Sectional Study. Breast Cancer Targets Ther. 2020;12:181. doi: 10.2147/BCTT.S279148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abay M, Tuke G, Zewdie E, Abraha TH, Grum T, Brhane E. Breast self-examination practice and associated factors among women aged 20–70 years attending public health institutions of Adwa town. North Ethiopia BMC Res Notes. 2018;11(1):1–7. doi: 10.1186/s13104-017-3088-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alomair AN, Felemban D, Felemban M, Awadain J, Altowargi A, Alfawzan NF. Knowledge, attitude and practice of breast self-examination toward breast cancer among female students at king Saud University in Riyadh. Saudi Arabia EC Gynaecol. 2020;9(1):01–8. [Google Scholar]
- 26.Ahmed A, Zahid I, Ladiwala ZFR, Sheikh R, Memon AS. Breast self-examination awareness and practices in young women in developing countries: A survey of female students in Karachi. Pakistan. J Educ Health Promot. 2018;7:90. doi: 10.4103/jehp.jehp_147_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Al-Mulhim F, Bakr R, Almedallah D, Alkaltham N, Alotaibi A, Alnoaim S. Screening mammography and breast self-examination: attitudes and practices of women in the Eastern Province of Saudi Arabia. Screening. 2018;7(2):89–100. [Google Scholar]
- 28.Chattu VK, Kumary S, Bhagavathula AS. Community-based study on the knowledge, awareness, and practices of females towards breast cancer in Buraimi, Oman. South Asian J Cancer. 2018;7(4):215. doi: 10.4103/sajc.sajc_71_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dadzi R, Adam A. Assessment of knowledge and practice of breast self-examination among reproductive age women in Akatsi South district of Volta region of Ghana. PLOS ONE. 2019;14(12):e0226925. doi: 10.1371/journal.pone.0226925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sama C-B, Dzekem B, Kehbila J, Ekabe CJ, Vofo B, Abua NL, et al. Awareness of breast cancer and breast self-examination among female undergraduate students in a higher teachers training college in Cameroon. Pan African Med J. 2017;28(1):164. doi: 10.11604/pamj.2017.28.91.10986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Salem MAA, Al Shazly HA, Ibrahem RA, Kasemy ZA, Abd El-Roaf SY. Knowledge, attitude, and practice of breast self-examination among women attending primary health care facility, Menoufia Governorate. Egypt Menoufia Med J. 2020;33(1):44. doi: 10.4103/mmj.mmj_557_15. [DOI] [Google Scholar]
- 32.Getie A, Mereta B, Shegaze M, Mekonnen B, Desalegn N, Abdilwohab M. Assessment of breast self-examination and associated factors among women age 20–64 years at Arba Minch Zuria District, Gamo Zone Snnpr Ethiopia, 2019. 2020.
- 33.Abeje S, Seme A, Tibelt A. Factors associated with breast cancer screening awareness and practices of women in Addis Ababa. Ethiopia BMC Women's Health. 2019;19(1):1–8. doi: 10.1186/s12905-018-0705-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Karim NKA, Sooi LK, Mangantig E. Factors associated with breast-self examination practice and mammogram breast density among Malaysian women. Malays J Med Health Sci. 2019;15(109):96–101. [Google Scholar]
- 35.Olaogun JG, Emmanuel EE, Dada SA, Odesanmi OM, Adesua OA. The prevalence of practicing breast self-examination and knowledge of breast cancer disease among women attending secondary health facility. Int Surg J. 2017;4(10):3211–3217. doi: 10.18203/2349-2902.isj20174491. [DOI] [Google Scholar]
- 36.Getu MA, Kassaw MW, Tlaye KG, Gebrekiristos AF. Assessment of breast self-examination practice and its associated factors among female undergraduate students in Addis Ababa University, Addis Ababa, Ethiopia, 2016. Breast Cancer: Targets Ther. 2019;11:21. doi: 10.2147/BCTT.S189023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mengie T, Yifru A, Fikre A, Niguse W, Demsie D, Ekubay M. Assessment of knowledge, attitude and practice regarding breast self-examination among female students in Debre Birhan University, North Shewa Ethiopia. Am J Clin Exp Med. 2020;8(3):48–54. doi: 10.11648/j.ajcem.20200803.13. [DOI] [Google Scholar]
- 38.Ebrahim S. Knowledge of students toward breast cancer and breast self-examination practice at high school nursing in Basra city. Rev J Kufa for Nurs Sci. 2014;4(1):0.
- 39.Suh MAB, Atashili J, Fuh EA, Eta VA. Breast self-examination and breast cancer awareness in women in developing countries: a survey of women in Buea. Cameroon BMC Res Notes. 2012;5(1):1–6. doi: 10.1186/1756-0500-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Birhane K, Alemayehu M, Anawte B, Gebremariyam G, Daniel R, Addis S, et al. Practices of breast self-examination and associated factors among female Debre Berhan University students. Int J Breast Cancer. 2017;207:1–6. doi: 10.1155/2017/8026297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mohamed AOA, Nori MMM, Ahmed ASM, Altamih RAA, Kunna ESM. Knowledge, attitude, and practice of breast cancer and breast self-examination among female detainees in Khartoum, Sudan 2018. J Prev Med Hyg. 2020;61(3):E470. doi: 10.15167/2421-4248/jpmh2020.61.3.1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sapountzi-Krepia D, Rekleiti M, Lavdaniti M, Psychogiou M, Chaliou M, Xenofontos M, et al. Evaluating female nursing students' knowledge and attitudes regarding breast self-examination. Health Care Women Int. 2017;38(8):786–795. doi: 10.1080/07399332.2017.1326921. [DOI] [PubMed] [Google Scholar]
- 43.Dir EDPC. National Cancer Control Plan Federal Ministry of Health, 2016–2020
- 44.Toan DTT, Son DT, Hung LX, Minh LN, Mai DL, Hoat LN. Knowledge, attitude, and practice regarding breast cancer early detection among women in a mountainous Area in Northern Vietnam. Cancer Control. 2019;26(1):1073274819863777. doi: 10.1177/1073274819863777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Desta F, Workicho A, Atomsa A, Workneh D, Tebeje B. Knowledge, practice and associated factors of breast self examination among female students of the College of Public Health and Medical Science, Jimma University, Ethiopia. Am J Health Res. 2018;6:44–50. doi: 10.11648/j.ajhr.20180602.12. [DOI] [Google Scholar]
- 46.Ameer K, Abdulie SM, Pal SK, Arebo K, Kassa GG. Breast cancer awareness and practice of breast self-examination among female medical students in Haramaya University, Harar, Ethiopia. Ethiopia IJIMS. 2014;2(2):109–119. [Google Scholar]
- 47.Desta F, Workicho A, Atomsa A, Workneh D, Tebeje B. Knowledge, practice and associated factors of breast self examination among female students of the college of public health and medical science, Jimma University, Ethiopia. Am J Health Res. 2018;6(2):44. doi: 10.11648/j.ajhr.20180602.12. [DOI] [Google Scholar]
- 48.Althubaiti A. Information bias in health research: definition, pitfalls, and adjustment methods. J Multidiscip Healthc. 2016;9:211. doi: 10.2147/JMDH.S104807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sani AM, Naab F, Aziato L. Influence of educational level on knowledge and practice of breast self-examination among women in Sokoto, Nigeria. J Basic Clin Reprod Sci. 2016;5(2):100–106. doi: 10.4103/2278-960X.194482. [DOI] [Google Scholar]
- 50.Ibrahim SQ, Abdullah WH, Ahmed HM, Al-Banna DA. Impact of education program on breast self examination among a group of women in the Kurdistan Women Union, Erbil city. Zanco J Med Sci. 2016;20(3):1450–1457. doi: 10.15218/zjms.2016.0044. [DOI] [Google Scholar]
- 51.Khiyali Z, Aliyan F, Kashfi SH, Mansourian M, Jeihooni AK. Educational intervention on breast self-examination behavior in women referred to health centers: application of Health Belief Model. Asian Pac J Cancer Prevent APJCP. 2017;18(10):2833. doi: 10.22034/APJCP.2017.18.10.2833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dewi TK, Massar K, Ruiter RA, Leonardi T. Determinants of breast self-examination practice among women in Surabaya, Indonesia: an application of the health belief model. BMC Public Health. 2019;19(1):1–8. doi: 10.1186/s12889-019-7951-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used/or analyzed during the current study is available from the corresponding author on reasonable request.