Abstract
Purpose
Quantitative epidemiological tools are routinely used to assess adolescent diet and physical activity (PA) constructs (behaviour, knowledge, and awareness) as risk factors for non-communicable diseases. This study sought to synthesize evidence on the quantitative epidemiological tools that have been used to assess adolescent diet and PA constructs in low to middle-income countries (LMIC).
Methods
A systematised review was conducted using 3 databases (EbscoHost, Scopus and Web of Science).
Results
We identified 292 LMIC studies assessing adolescent diet and PA. Identified studies predominantly explored behavioural (90%) constructs with a paucity of studies investigating knowledge and awareness. The majority of studies used subjective (94%) and self-administered (78%) tools. Only 39% of LMIC studies used tools validated for their contexts.
Conclusions
The findings highlight the need for more contextual tools for assessing adolescent diet and PA in LMICs. Diet and PA measurement tools used in future research will need to incorporate measures of knowledge and awareness for a more comprehensive understanding of the epidemiology of diet and PA in adolescents. Furthermore, there is a need for more evidence on the reliability and validity of these tools for use, in both cross sectional and longitudinal studies, in LMIC contexts.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-022-13160-6.
Keywords: Adolescent; Diet; Physical activity; Assessment; Epidemiological tools, low- and middle-income countries; LMIC
Background
The burden of non-communicable disease (NCD) is disproportionately higher in low- and middle-income countries (LMICs) [1]. In 2019, 75% of global all-cause mortality was attributable to NCDs, with 77% of NCD deaths reported in LMICs [1, 2]. Increasing morbidity and mortality, particularly in LMICs, has prompted the need for innovative interventions to address modifiable NCD risk factors, notably unhealthy diet and physical inactivity [3]. Diet and physical activity (PA) are both implicated in the aetiology of the main NCDs-cardiovascular diseases, cancers, respiratory diseases, and diabetes [3, 4]. In LMICs, NCD occurrence is disproportionally higher in adults aged above 30 years but associated behavioural risk factors begin to develop and are reinforced during adolescence. The life course approach recognises that an individual’s health status is a function of past (and present) biopsychosocial pathways operating at key developmental stages [5]. This approach further recognizes that developmental and behavioural changes [6, 7] occurring at the adolescent stage provide opportunities for disease prevention through the promotion of healthy diets and PA.
The development and implementation of contextually appropriate NCD prevention strategies in LMICs relies on the ability to accurately collect data on adolescent diet and PA behaviours. At the global level, various epidemiological tools have been developed to provide quantitative and qualitative measures of diet and PA; with these tools being either objective or subjective [8, 9]. Subjective tools rely on individual self-report of diet or PA constructs over defined periods. Examples include questionnaires and logbooks [10, 11]. Conversely, objective tools quantify dietary or PA constructs by recording phenomena that translate to dietary or PA estimates [12]. Examples include accelerometers that measure body movement to estimate PA [12, 13], and nutritional biomarkers that assess dietary consumption [8].
Research evidence indicates an increasing number of studies exploring adolescent diet and PA trends in LMICs. However, the majority of tools used by these studies to assess adolescent diet and PA behaviours and knowledge have been developed in high-income country (HIC) contexts [14] which may not adequately capture adolescent diet and PA behaviours in LMIC contexts.
This systematised literature review sought to identify and describe the quantitative epidemiological tools used for assessing adolescent diet and physical activity in LMICs, using the constructs of behaviour, knowledge, and awareness. We further explored the origin and validation of these tools for use in LMICs.
Methods
Overview
The systemized literature review typology was selected to guide our literature search. Systematised reviews combine elements from both systematic and traditional literature reviews [15], and follow a comprehensive search strategy that is uniformly executed across databases to identify relevant literature. Quality assessment of retrieved articles is not required [15].
Search strategy
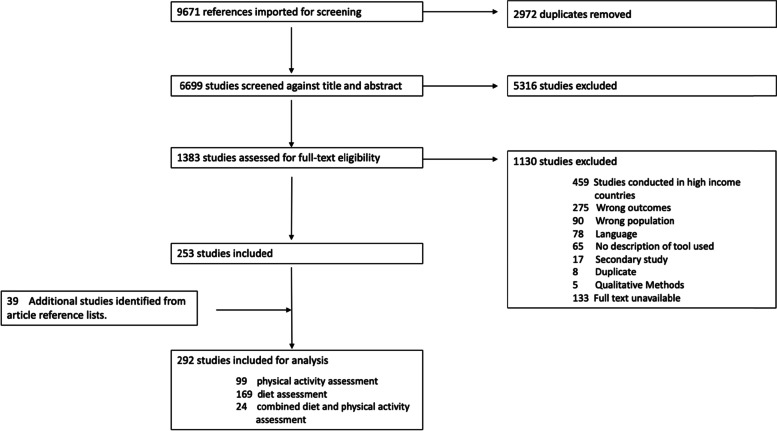
An initial search was conducted in Google Scholar and PubMed to identify key literature and keywords for use in the literature search. The finalised literature search strategy (Additional file 1 Tables 1A and 1B) included variations of the following terms “knowledge”, “awareness”, “behaviour” “epidemiology”, “adolescents”, “physical activity” and “diet”. Between August – December 2019, the search terms were applied uniformly across three databases – EbscoHost [16], Scopus [17] and Web of Science [18]. The search yielded a total of 9098 studies (Scopus – 3688, EbscoHost – 3845, Web of Science- 1565). Article abstracts were uploaded onto Covidence [19], a web-based online screening software, for both abstract and full text screening. Duplicates (n = 2922) were automatically removed by Covidence. Titles and abstracts (n = 6176) were screened by two independent reviewers (authors TM and MK) to identify eligible studies that met the inclusion criteria. Full text screening of the remaining 1337 articles was undertaken by the same two reviewers. Any discrepancies were resolved by a third reviewer. The systematised search was subsequently updated in January 2022. A total of 573 (Scopus – 106, EbscoHost – 215, Web of Science – 252) studies were identified. Retrieved studies underwent title, abstract and full text screening, of which 26 studies met the inclusion criteria. The reference lists of included studies were thereafter examined to identify additional relevant studies. This process yielded a further 39 articles. As highlighted in the PRISMA flow diagram (Fig. 1), 292 LMIC studies were included for data analysis.
Fig. 1.
PRISMA Diagram of the literature review process
Inclusion criteria
To meet the research objective, the following inclusion criteria were applied: the main outcome included reported scores for adolescent diet or PA; the study utilised quantitative epidemiological approaches in both data collection and analysis; study population included adolescents aged between 10 and 19 years; articles were written in English or translated versions were available. There were no limitations on geographical location. However, given the focus on studies from LMICs, locations were recorded to highlight the country in which the studies were conducted. The World Bank Group’s income classification grouping was used to identify LMICs (Additional file 2) [20]. To capture instrument diversity, there were no limitations on the date of publication or on data collection methods. Studies were excluded from the literature review if they did not meet these criteria (Fig. 1).
Results
We identified 292 studies conducted in LMICs. Of these, 24 assessed diet and PA in the same study (Additional file 3 Table 3A), 99 studies assessed PA constructs only (97% assessed behaviour; 3% knowledge and awareness) (Additional file 3 Table 3B), and 169 studies assessed dietary constructs only (86% assessed behaviour; 14% knowledge and awareness) (Additional file 3 Table 3C).
Assessing adolescent physical activity constructs
The majority (97%) of studies assessed PA behaviour (both subjectively and objectively) (n = 96/99). The remaining three studies assessed PA knowledge and awareness exclusively (n = 1) or concurrently with PA behaviour (n = 2). PA behaviour was reported under four domains – transport, household, occupational (school related) and leisure time. Leisure time PA encompassed walking, running, recreational sport and playful activities.
Physical activity behaviour
LMIC adolescent PA behaviour was predominantly measured using subjective tools – exclusive questionnaires (n = 75), questionnaires in conjunction with another tool (n = 7), 24-h PA recall reports (n = 3), and one PA real-time record. (Additional file 3 Table 3B). Utilised questionnaires included tools originally developed in HICs (n = 47), regionally (n = 4) and locally (n = 25). Tools developed in HIC included the International Physical Activity Questionnaire (IPAQ) (n = 15) [21–35], Physical Activity Questionnaire (PAQ) (n = 5) [21, 36–39], Health Behavior School-aged Children Survey Questionnaire (HBSC) [40] and the Three Day Physical Activity Recall (3DPAR) [41].
We found two regional tools, Arab Teens Lifestyle Study (ATLS) [42–47] and South American Youth/Child Cardiovascular and Environment (SAYCARE) [48], developed for use in Arab and Latin American countries, respectively. The development of regional tools was guided by pre-existing tools with adaptations made to suit the regional context. For example, the SAYCARE questionnaire assessed 3 domains of PA - school, leisure time and transport - as adolescents living in the region were most likely to engage in moderate to vigorous PA [48]. Similarly, in adapting to the cultural context in the Middle-East region, only girls were asked about their participation in dancing as a means for PA in the ATLS questionnaire [42–44, 49].
Nineteen studies used locally developed (country-specific) tools. These studies were conducted in 11 countries – Brazil (n = 6) [50–55], Malaysia (n = 3) [56–58], Thailand (n = 1) [59], Vietnam (n = 2) [60, 61], Mozambique (n = 2) [62, 63], India (n = 1) [64], China (n = 1) [65], Colombia (n = 1) [66], Ecuador (n = 1) [67], Iran (n = 1) [68], and Ghana (n = 1) [69]. Although developed locally, the questions and PA domains were similar to those used in HICs.
Only 16 studies used objective measures to assess LMIC adolescent PA using accelerometery (n = 14), heart rate monitors (n = 1), pedometer (n = 1) and direct observation (n = 1). We also found 5 studies that utilised a combination of questionnaires and accelerometers concurrently when assessing PA [35, 70–73].
Physical activity knowledge and awareness
We identified three LMIC studies assessing PA knowledge and awareness using bespoke questions [74–76]. These studies assessed perceived benefits and barriers to regular PA [74], PA self-efficacy [76], and the association between health and PA [75].
Assessing adolescent dietary constructs
We identified 169 studies (Additional file 3 Table 3C) assessing adolescent dietary constructs only, with a majority of the studies (n = 145) assessing behaviour. Behaviour constructs included the quantity, frequency and type of food habitually consumed. Adolescent dietary knowledge and awareness were assessed exclusively in seven studies, with an additional 17 studies measuring knowledge and awareness alongside dietary behaviour.
Dietary behaviour
Of the 145 studies documenting adolescent dietary behaviour, 108 used questionnaires, 11 dietary records, 17 dietary recall, one used an observational method and nine used a combination of questionnaires and dietary recall methods.
Internationally developed tools were used in 27 LMIC studies. Examples of tools used include the Global School Health Survey – GSHS [77, 78], WHO & FAO 1 day diversity questionnaire [79], and the Nutrition Transition Food Frequency Questionnaire - NT-FFQ [80]. The Arabic Eating Habits Questionnaire (AEHQ) was the only identified LMIC regional tools assessing diet [81]. The AEHQ aimed to identify the food consumption and snacking patterns of Arab adolescents and included a food list characteristic of the Arab diet as well as a dedicated segment to assess fast food consumption.
The majority of questionnaires (n = 71) used were either adapted (from regional or international tools) or specifically developed (country-specific) for use in the country. For example the Adolescent Eating Attitudes Questionnaire (Brazil) was adapted from the Project EAT (Eating Among Teens) questionnaire (USA) [82], and a food frequency questionnaire (FFQ) (Jamaica) was adapted from a regional 1997 Caribbean Youth Survey [83]. Other country-specific questionnaires used bespoke food frequency questionnaires (FFQs) that contained contextually relevant food lists designed to capture the variation in local diets. Consequentially, although country-specific tools all assessed dietary behaviour, differences in the actual content limited the comparability of study findings across different populations.
Eleven studies reported dietary behaviour using prospective dietary records over periods ranging from 24 h, 1 week to 3 months [84–94]. Participants were first trained on data collection procedures and thereafter kept detailed records (in a notebook) of dietary practices over a set period, typically 24 h. In some instances, dietary records allowed researchers to collect information on food preparation methods as exemplified in a Brazilian study where participants took notes on food preparation methods as well as places of consumption [86]. Paper notebooks were the main equipment for recording data.
The dietary recall method was used in 17 studies by asking adolescents to recall all the food they had consumed in the previous day [95–111]. Using the dietary recall method, participants provided information on food consumed in the preceding 24 h over one to 7 days depending on the objectives of the study. In seven of these studies, participant recall was facilitated by a researcher providing questions and prompts to aid recall [95, 96, 99, 100, 106, 107, 112]. The 24-h time period used in dietary recall assessments gave an indication of food intake. However, there was potential to overlook infrequently consumed foods that contribute towards an individual’s total food intake. To mitigate this limitation, some studies conducted dietary recall every 24 h over two to 7 days [96, 103, 113].
Dietary knowledge and awareness
We identified 24 questionnaires investigating adolescent dietary knowledge and awareness. Adolescent nutritional knowledge was assessed in 13 studies using close-ended questions [104, 113–124]. Nine studies used questionnaires to assess information on dietary attitudes, perceptions, and food choices [92, 104, 114, 116, 125–129]. Examples include a Turkish study that measured knowledge of a local Food Guide Pyramid (FGP), by asking adolescents to list food groups recommended in the FGP in order of recommended consumption frequency relative to their own daily consumption [130].
Validation and reliability of tools used in low- and middle-income countries
Only 39% (n = 113/292) of the 292 studies used subjective epidemiological tools validated for use in their geographical contexts. Measures of reliability included test-retest reliability (n = 51) and internal consistency (n = 17). Validation methods were construct validity (n = 4), content validity (n = 24), criterion validity (n = 43) and face validity (n = 17), with some studies utilising multiple methods. The types of validation methods used are detailed in Additional file 3 (Tables 3A, 3B, 3C). Tool validation was described either as part of the study methods or in reference to prior studies showing validity and reliability of the tool in a similar geographical context. With respect to validation of tools for the adolescent population group, 58% (n = 65/113) of studies using validated tools specifically mentioned use of tools originally designed for adolescents. None of the identified objective tools, were explicitly validated for use in LMIC settings.
Validation of tools measuring PA constructs
Of the 113 studies detailing validation methods in LMIC, 50 were focused on PA (46 questionnaires, 1 PA recall, 1 pedometer and 2 logbook). When disaggregated by tool origin, 29 studies used tools initially developed in HICs, 4 studies used regionally developed tools and 16 were developed within the country. Validated tools developed in HIC included the IPAQ (n = 13), PAQ (n = 4), 3DPAR (n = 1) and the GSHS (n = 1), with validation conducted to assess suitability of tools to the local contexts. Face validity of the IPAQ was consistently assessed in different regions including Brazil, Iran, Thailand, Turkey and Macedonia to assess if participants and subject experts thought, at face value, these tools where appropriate for assessing PA in the local context [27, 28, 31, 33–35, 131–135]. The content validity of international tools (IPAQ, GSHS and PAQ) was assessed in 10 studies [22, 27, 33, 35, 39, 60, 133, 136–138]. For example, after translation, the GSHS was validated by a group of experts prior to use in Iran [33]. Construct validity of international tools was also assessed in Indonesia [28], Brazil [139], and Ecuador [67].
In addition to international tools, we found two regional tools that had been validated for local contexts – ATLS [42–44] and the SAYCARE [48]. Although ATLS was initially comparatively validated against pedometer readings in adolescents, subsequent studies further tested the tool for reproducibility (using the test-retest method) [43]. The SAYCARE was tested for reproducibility and criterion validity (against accelerometery) in seven cities (Lima, Buenos Aires, Medellin, Montevideo, Santiago, Sao Paulo and Teresina) [48].
Four questionnaires identified were developed and validated at the country level: Thailand PA Children Survey (TPACS-SQ), Vietnamese Adolescent PA Recall Questionnaire (VAPARQ), Madras Diabetes Research Foundation – Physical Activity Questionnaire for Children and Adolescents (MPAQ©) and, National Adolescent School-based Health Survey (Brazil (PeNSE) [53, 59, 61, 64]. The TPACS-SQ was developed by modifying a previous questionnaire, Child and Adolescent PA and Nutrition Survey (CAPANS) which was validated in comparison to accelerometery [59]. Given that the contents and constructs of the CAPANS had demonstrated validity, the current TPACS-SQ was tested for reproducibility using the test-retest method. The VAPARQ was adapted and translated from the Australia Adolescent Physical Activity Recall Questionnaire (APARQ) and given the tropical climate in Vietnam, validation involved qualitative discussions to identify the range of activities to be included [61].
Validation of tools measuring dietary constructs
Fifty-three studies highlighted the use of validated tools in the assessment of adolescent dietary constructs (50 questionnaires, one dietary record and two dietary recall). Of these, 16 were developed in HICs. These tools included the GSHS (Iran and Uganda) [77, 78], Eating Habits Questionnaire for Adolescents – (Ghana) [140], Adolescent Food Frequency Questionnaire (Brazil) [141], Block Questionnaire (Brazil) [142], Food Consumption Markers form (Brazil) [143]. To test reproducibility, eight studies used the test-retest methods [77, 78, 80, 141, 144–147], and six used the internal consistency method in pilot studies [119, 140, 144, 148–150]. Content validity was assessed for the GSHS in Iran [78], NTFFQ in Brazil [151], and Adolescents’ Knowledge of Healthy Eating Questionnaire in Nigeria [148] to ensure that the tool assessed all facets of dietary consumption in adolescents.
Twenty-eight studies developed and validated context specific FFQs within their country. Examples include an FFQ to assess adolescent food consumption amongst Isfahan female students that consisted of a 53-item food list of items commonly consumed in Iran [152]. Similarly, a Brazilian study used a food list with food items commonly eaten by adolescents based of previous 24 h food records [153].
Of the 50 validated dietary questionnaires identified, 14 used criterion validity against the 24-h dietary recall method [104, 115, 154–170]. Validity was confirmed if there was correlation between dietary scores or outcomes from both methods. Face validity was estimated in six studies by asking experts in nutrition, behaviour and education to assess the suitability of questions presented in the questionnaire [78, 127, 144, 148, 150, 171]. Content validity was conducted in a similar fashion [146, 148, 151, 171–174]. Reproducibility of tools was assessed using the test-retest and internal consistency methods.
Validation of tools measuring both dietary and PA constructs
We identified 10 questionnaires assessing both food and PA concurrently that were also validated for their contexts [49, 175–183]. Tools used included the Global School Based Student Health Survey (GSHS) [176, 178], ATLS [49], and a combination of diet (FFQ) and PA (IPAQ, PAQ-A tools) [175, 177, 181]. Validation was assessed using a combination of face, content, and construct, and criterion validation methods.
Tool administration
The majority of studies used school-based adolescent sampling strategies (75%, n = 218/292). Two types of tool administration were utilised in LMIC studies: self- (n = 230/292, 79%) and researcher-led (n = 64, 21%) administration. For both types, questions were first explained to the adolescents at the beginning or during data collection with opportunities to ask questions made available by the researcher. Other methods such as dietary and PA recall and records lend themselves to self-administration by design.
When disaggregated, 10% (n = 10/99), 28% (n = 48/169), and 25% (n = 6/24) of studies assessing PA, diet, and combined PA and diet, respectively, used interviewer-administered tools for data collection. Interview administration for dietary assessment was reported to be useful in probing the participant to report in detail their dietary habits or awareness. However, studies acknowledged limitations associated with interviewer administration, noting efforts to reduce bias when possible.
Objective assessments of PA (n = 17) were self-administered (with guidance from research team members), because the devices used in data collection -accelerometers, pedometers, and heart rate monitors – are either attached or worn by the adolescent over a set period of data collection.
Nearly half of the studies used paper-based tools (n = 121/292), and 11 studies used computer-based tools [58, 99, 106, 118, 143, 184–189], of which only three were online. Seventeen studies used digital devices such as accelerometers for data collection. The remaining studies did not explicitly specify how data were collected.
Discussion
This systematised review explored the availability and use of tools for assessing adolescent dietary and PA behaviour, knowledge, and awareness in LMICs. We found that self-administered subjective instruments were extensively used to assess adolescent dietary and PA constructs, with a significant focus on the behavioural construct and a minority assessing the knowledge and awareness that underpin such behaviours. Of the 292 studies identified in this study, only 39% used tools assessed for validity or reliability for their context. Tool administration was predominantly self-administered, and 80% of studies used school-based sampling as a population base.
The majority of studies assessed behavioural aspects of adolescent diet and PA constructs (90%), with only 10% assessing knowledge and awareness constructs. Although individual and group behaviour are important entry points for NCD prevention and intervention, socio-cultural environments, knowledge and awareness are key drivers of behaviour change [190]. This highlights a need for the inclusion of knowledge, attitudes and awareness constructs in future epidemiological studies assessing adolescent diet and PA.
Subjective tools were more commonly utilised. This is despite evidence suggesting that the objective tools provide more accurate measures of diet and PA [191–193]. The lower usage of objective tools in LMIC is unsurprising given the relatively high cost of procuring equipment and the need for experienced technicians for data analysis and interpretation. Indeed, global research initiatives, as well as global public health agencies [194] rely on the use of subjective questionnaires to collate information on NCD risk factors trends worldwide owing, in part, to the limited accessibility of objective tools in many parts of the world. Given that subjective tools are currently a more feasible alternative for data collection in LMICs, it is imperative to improve the validation and reliability of existing subjective methods for use in LMICs.
Innovations in the field of mHealth provide a potential avenue to improve objective assessment for both diet and PA. As of 2019, mobile cellular subscriptions was estimated at 105% for people living in LMICs [195]. This extensive mobile coverage in LMIC can be leveraged to collect objective adolescent diet and PA using various techniques [196]. One example is the use of mobile food record apps with fluidical markers (a measured object placed next to the food as a portion size reference) to objectively record types of foods consumed as well as estimate portions sizes [197].
Encouragingly, we noted the emergence of regional and country-specific tools developed and validated for use in LMIC settings. However, only 39% of studies conducted in LMICs used tools validated for use in their specific context. As some of the tools such as the IPAQ (for PA) and YAQ (for diet) have been validated globally, validity may have been assumed for the geographical context. Although adaptation of relevant tools is encouraged, validation of tools is important to reduce errors in outcome reporting that may arise from contextual effects [198]. Regional tools – ATLS [199] and SAYCARE – were developed and validated across countries in the Middle-East and South America to provide a reliable means of comparing food and PA across similar populations. Similarly, TEQ and the MyUM AFFQ were developed for use in Thailand and Malaysia, respectively. Development and validation of diet and PA assessment tools in the contexts in which they are to be used is beneficial as it improves the prospects of accurately capturing local nuances that might be otherwise missed. That said, increased used of locally adapted contextualised tools limits the comparability of research findings across different contexts. This challenge was highlighted in a recent systematic review stating that variations in assessment tools and data collection methods limited the comparability of adolescent girls dietary intake and practices across LMIC regions [200]. Possible strategies for mitigating comparability issues include the inclusion, across all tools, of standardised indicators that conceptually measure the same behavioural constructs [200, 201].
The majority of adolescent participants (75%) in reviewed studies were recruited in school-based studies, with these settings providing access to a captive group of adolescents that can be easily sampled [202, 203]. School-based participant recruitment is suitable in settings, such as European and North American countries, that have low adolescent out of school rates [204]. However, in many LMICs, high school education is not always free, and adolescents from poorer households may not attend school consistently [204]. United Nations Educational, Scientific and Cultural Organization’s reports show that one in three adolescents of school-going age in Sub-Saharan Africa are not in school for various reasons [204]. As such, issues of sampling bias may arise as a school-based sampling may systematically exclude potentially more vulnerable adolescents. Studies in LMICs will therefore need to take this into consideration when developing sampling strategies to ensure greater representation from households, religious groups, and the wider community.
Studies predominantly used self-administered tools for data collection in adolescents. This is based on the assumption that adolescents (aged 10–19 years) have received some formal education and are able to follow instructions and adequately respond to questions during data collection [205]. However, self-administered methods assume a level of literacy that may not always be present in adolescents particularly those living in resource poor regions where access to primary education is not always guaranteed. As such, tools that rely on the adolescent’s ability to read and write, such as dietary or food records, may not be appropriate in populations with low literacy rates [206–208]. In such instances, researcher-led administration of tools to assist participants in completing the data collection task may be more appropriate.
Lastly, the majority of studies identified used a cross-sectional study design with only 4% being longitudinal cohort studies. These findings highlighted a paucity of evidence on the validity and reliability of these tools to capture changes in diet and PA constructs over time. The lack of longitudinal evidence is an important knowledge gap particularly in LMIC contexts where rapid urbanisation means food and built environments are dynamic as this may result in more dynamic changes in diet and activity behaviour, knowledge and awareness over time.
Study limitations
Qualitative studies on adolescent dietary and PA were not included in this review because of the limited generalisability of qualitative research findings [209]. Consequently, it is possible that relevant research in the area of knowledge and awareness (traditionally measured using qualitative methods) was missed. Therefore, future research may seek to consolidate quantitative and qualitative methods used to assess adolescent diet and PA. Full text articles were only included for review if they were written in English or translated versions were readily available. As a result, we may have excluded contextually relevant studies published in other languages. As the aim of this review was to synthesise existing evidence on validated instruments used to measure diet and physical activity in the context of adolescents in low and middle-income settings, a synthesis of findings on patterns of diet and physical activity behaviour from papers identified was beyond the scope of this paper and not included.
Conclusions
Our findings point to a plethora of subjective quantitative epidemiological tools for assessing adolescent diet and PA in LMICs, predominantly measuring the behaviour construct. Research studies in LMICs provide useful insights on diet and PA trends, however, more research is required on the reliability and validity of these tools for use, in both cross sectional and longitudinal studies, in LMIC contexts. Furthermore, we recommend that future LMIC study protocols consider adolescent population demographics and socio-economic contexts and adjust sampling and tool administration strategies accordingly. Lastly, this review highlights a need for the inclusion of measures of adolescent knowledge and awareness on diet and PA in future research in LMICs for a more comprehensive understanding of the epidemiology of diet and PA in adolescents and to inform contextually relevant interventions for NCD prevention at this critical life stage.
Supplementary Information
Acknowledgements
Not applicable.
Abbreviations
- LMIC
Low to middle-income countries
- NCD
Non-communicable disease
- PA
Physical activity
- HIC
High-income country
- IPAQ
International Physical Activity Questionnaire
- PAQ
Physical Activity Questionnaire
- HBSC
Health Behavior School-aged Children Survey Questionnaire
- 3DPAR
Three Day Physical Activity Recall
- ATLS
Arab Teens Lifestyle Study
- SAYCARE
South American Youth/Child Cardiovascular and Environment
- GSHS
Global School Health Survey
- NTFFQ
Nutrition Transition Food Frequency Questionnaire
- AEHQ
The Arabic Eating Habits Questionnaire
- FFQ
Food frequency questionnaire
- FGP
Food Guide Pyramid
- TPACS-SQ
Thailand PA Children Survey
- VAPARQ
Vietnamese Adolescent PA Recall Questionnaire
- PeNSE
Brazil National Adolescent School-based Health Survey
- CAPANS
Child and Adolescent PA and Nutrition Survey
- APARQ
Australia Adolescent Physical Activity Recall Questionnaire
Authors’ contributions
JB, TO and TM initiated and developed the study protocol. TM conducted the literature search, drafted the manuscript, prepared the final draft. MK and TM reviewed the articles for eligibility. All the authors reviewed the draft and approved the final manuscript.
Funding
This study was funded by Urban Food Systems Governance for NCD Prevention in South Africa, Kenya and Namibia (Nourishing Spaces) IDRC, Canada Project [grant number 108458]. TO is supported by the National Institute for Health Research (NIHR) [grant number 16/137/34] using UK aid from the UK Government to support global health research. The views expressed in this publication are those of the authors and not necessarily those of the NIHR or the UK Department of Health and Social Care. MK was supported by the South African National Research Foundation (NRF) under joint funding with the German Academic Exchange Service (DAAD) for her PhD.
Availability of data and materials
All data generated or analysed during this study are included in this published article [and its supplementary information files].
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization . Noncommunicable diseases. 2021. [Google Scholar]
- 2.The World Bank. Cause of death, by non-communicable diseases (% of total): The World Bank; 2020. Available from: https://data.worldbank.org/indicator/SH.DTH.NCOM.ZS
- 3.World Health Organization . Global action plan for the prevention and control of noncommunicable diseases 2013–2020. Geneva: World Health Organization; 2013. [Google Scholar]
- 4.World Health Organization . Noncommunicable diseases. Geneva: World Health Organization; 2021. [Google Scholar]
- 5.Heikkinen E. A life course approach: research orientations and future challenges. Eur Rev Aging Phys Act. 2011;8(1):7–12. doi: 10.1007/s11556-010-0069-2. [DOI] [Google Scholar]
- 6.Salwa M, Haque MA, Khalequzzaman M, Al Mamun MA, Bhuiyan MR, Choudhury SR. Towards reducing behavioral risk factors of non-communicable diseases among adolescents: protocol for a school-based health education program in Bangladesh. BMC Public Health. 2019;19(1):1002. doi: 10.1186/s12889-019-7229-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sawyer SM, Afifi RA, Bearinger LH, Blakemore S-J, Dick B, Ezeh AC, et al. Adolescence: a foundation for future health. Lancet. 2012;379(9826):1630–1640. doi: 10.1016/S0140-6736(12)60072-5. [DOI] [PubMed] [Google Scholar]
- 8.Rutishauser IH. Dietary intake measurements. Public Health Nutr. 2005;8(7a):1100–1107. doi: 10.1079/PHN2005798. [DOI] [PubMed] [Google Scholar]
- 9.Westerterp KR. Assessment of physical activity: a critical appraisal. Eur J Appl Physiol. 2009;105(6):823–828. doi: 10.1007/s00421-009-1000-2. [DOI] [PubMed] [Google Scholar]
- 10.Kohl HW, III, Fulton JE, Caspersen CJ. Assessment of physical activity among children and adolescents: a review and synthesis. Prev Med. 2000;31(2):S54–S76. doi: 10.1006/pmed.1999.0542. [DOI] [Google Scholar]
- 11.Collins CE, Watson J, Burrows T. Measuring dietary intake in children and adolescents in the context of overweight and obesity. Int J Obes. 2010;34(7):1103–1115. doi: 10.1038/ijo.2009.241. [DOI] [PubMed] [Google Scholar]
- 12.Sirard JR, Pate RR. Physical activity assessment in children and adolescents. Sports Med. 2001;31(6):439–454. doi: 10.2165/00007256-200131060-00004. [DOI] [PubMed] [Google Scholar]
- 13.Clemes SA, Biddle SJ. The use of pedometers for monitoring physical activity in children and adolescents: measurement considerations. J Phys Act Health. 2013;10(2):249–262. doi: 10.1123/jpah.10.2.249. [DOI] [PubMed] [Google Scholar]
- 14.Moreno LA, Kersting M, de Henauw S, González-Gross M, Sichert-Hellert W, Matthys C, et al. How to measure dietary intake and food habits in adolescence: the European perspective. Int J Obes. 2005;29:S66–S77. doi: 10.1038/sj.ijo.0803063. [DOI] [PubMed] [Google Scholar]
- 15.Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26(2):91–108. doi: 10.1111/j.1471-1842.2009.00848.x. [DOI] [PubMed] [Google Scholar]
- 16.EBSCOhost Available from: https://web.b.ebscohost.com/ehost/search/basic?vid=1&sid=fcbffcdb-5c75-4379-9ba8-ea9588faccc1%40pdc-v-sessmgr01.
- 17.Scopus. 2019. Available from: https://www.scopus.com/search/form.uri?display=basic#basic.
- 18.Web of Science [Internet]. Available from: https://apps.webofknowledge.com/WOS_GeneralSearch_input.do?product=WOS&search_mode=GeneralSearch&SID=F5mLk6OSQ6DmoLycm25&preferencesSaved=.
- 19.Covidence. Available from: https://www.covidence.org/about-us-covidence/.
- 20.World Bank Country and Lending Groups. 2021. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. Cited 28 April 2021
- 21.Lachat CK, Verstraeten R, Khanh LNB, Hagströmer M, Khan NC, Van NDA, et al. Validity of two physical activity questionnaires (IPAQ and PAQA) for Vietnamese adolescents in rural and urban areas. Int J Behav Nutr Phys Act. 2008;5:1-8. [DOI] [PMC free article] [PubMed]
- 22.Abasi MH, Eslami AA, Rakhshani F, Shiri M. A self-efficacy questionnaire regarding leisure time physical activity: psychometric properties among Iranian male adolescents. Iran J Nurs Midwifery Res. 2016;21(1):20–28. doi: 10.4103/1735-9066.174751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fortes LS, Morgado FFR, Almeida SS, Ferreira MEC. Eating behavior and physical activity in adolescents. Revista de Nutrição. 2013;26(5):529–537. doi: 10.1590/S1415-52732013000500004. [DOI] [Google Scholar]
- 24.Iskandar MM, Mohamad N, Othman S. Physical activity and BMI level: youth in low-cost housing Kuala Lumpur. Pertanika J Soc Sci Humanit. 2017;25(June):43–53. [Google Scholar]
- 25.Masocha V, Czyż SH, Moss SJ, Monyeki AM. Two-year changes in body composition, physical activity and selected metabolic risk factors among adolescents living in Tlokwe municipality area, north West Province, South Africa: the PAHL study. SAfr J Res Sport Phys Educ Recreation. 2018;40(2):99–114. [Google Scholar]
- 26.Paudel S, Subedi N, Bhandari R, Bastola R, Niroula R, Poudyal AK. Estimation of leisure time physical activity and sedentary behaviour among school adolescents in Nepal. BMC Public Health. 2014;14(1):1449–1465. doi: 10.1186/1471-2458-14-637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Straatmann VS, Almquist YB, Oliveira AJ, Veiga GV, Rostila M, Lopes CS. Stability and bidirectional relationship between physical activity and sedentary behaviours in Brazilian adolescents: longitudinal findings from a school cohort study. Plos One. 2019;14(1):e0211470. [DOI] [PMC free article] [PubMed]
- 28.Suyoto PST, Huriyati E, Susilowati R, Julia M. Relative validity of administered indonesian version of the short-form international physical activity questionnaire (IPAQ-SF) among obese adolescent girl population. Pak J Nutr. 2016;15(9):816–820. doi: 10.3923/pjn.2016.816.820. [DOI] [Google Scholar]
- 29.Wang H, Zhang YF, Xu LL, Jiang CM. Step rate-determined walking intensity and walking recommendation in Chinese young adults: a cross-sectional study. BMJ Open. 2013;3(1):e001801. [DOI] [PMC free article] [PubMed]
- 30.Werneck AO, Vancampfort D, Oyeyemi AL, Stubbs B, Silva DR. Associations between TV viewing, sitting time, physical activity and insomnia among 100,839 Brazilian adolescents. Psychiatry Res. 2018;269:700–706. doi: 10.1016/j.psychres.2018.08.101. [DOI] [PubMed] [Google Scholar]
- 31.Yildizer G, Yilmaz İ, Novak D. Social capital and physical activity participation among Turkish adolescents in urban centres: a preliminary study. S Afr J Res Sport Phys Educ Recreation. 2019;41(2):117–129. [Google Scholar]
- 32.Zhu Z, Tang Y, Zhuang J, Liu Y, Wu X, Cai Y, et al. Physical activity, screen viewing time, and overweight/obesity among Chinese children and adolescents: an update from the 2017 physical activity and fitness in China - the youth study. BMC Public Health. 2019;19(1):1-8. [DOI] [PMC free article] [PubMed]
- 33.Kelishadi R, Ardalan G, Gheiratmand R, Gouya MM, Razaghi EM, Delavari A, et al. Association of physical activity and dietary behaviours in relation to the body mass index in a national sample of Iranian children and adolescents: CASPIAN study. Asociación de la actividad física y los hábitos alimentarios en relación con el índice de masa corporal en una muestra nacional de niños y adolescentes iraníes: estudio CASPIAN. 2007;85(1):19–26. doi: 10.2471/BLT.06.030783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pelegrini A, Silva DAS, Claumann GS, Cardoso TE, e Silva JMFL, Petroski EL. Practice of walking, moderate and vigorous physical activity and associated factors in adolescents from a state capital of southern Brazil. Revista Brasileira de Cineantropometria e Desempenho Humano. 2014;17(1):11–20. doi: 10.5007/1980-0037.2015v17n1p11. [DOI] [Google Scholar]
- 35.da Silva ICM, Hino AA, Lopes A, Ekelund U, Brage S, Goncalves H, et al. Built environment and physical activity: domain- and activity-specific associations among Brazilian adolescents. BMC Public Health. 2017;17(1):1-11. [DOI] [PMC free article] [PubMed]
- 36.Asare M, Danquah SA. The relationship between physical activity, sedentary behaviour and mental health in Ghanaian adolescents. Child Adolesc Psychiatry Mental Health. 2015;9(1):1-8. [DOI] [PMC free article] [PubMed]
- 37.Dave H, Nimbalkar SM, Vasa R, Phatak AG. Assessment of physical activity among adolescents: a cross-sectional study. J Clin Diagn Res. 2017;11(11):SC21–SSC4. [Google Scholar]
- 38.Kundapur R, Baisil S. Assessment of difference in physical activities in urban and rural adolescents of Mangalore. Indian J Community Health. 2017;29(1):75–80. [Google Scholar]
- 39.Motamed-Gorji N, Qorbani M, Nikkho F, Asadi M, Motlagh ME, Safari O, et al. Association of screen time and physical activity with health-related quality of life in Iranian children and adolescents. Health Qual Life Outcomes. 2019;17(1):1. doi: 10.1186/s12955-018-1071-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chen ST, Liu Y, Hong JT, Tang Y, Cao ZB, Zhuang J, et al. Co-existence of physical activity and sedentary behavior among children and adolescents in Shanghai, China: do gender and age matter? BMC Public Health. 2018;18(1):1-9. [DOI] [PMC free article] [PubMed]
- 41.Khan A, Burton NW, Trost SG. Patterns and correlates of physical activity in adolescents in Dhaka city, Bangladesh. Public Health. 2017;145:75–82. doi: 10.1016/j.puhe.2016.12.011. [DOI] [PubMed] [Google Scholar]
- 42.Abu-Mweis SS, Tayyem RF, Bawadi HA, Musaiger AO, Al-Hazzaa HM. Eating habits, physical activity, and sedentary behaviors of Jordanian adolescents’ residents of Amman. Mediterr J Nutr Metab. 2014;7(1):67–74. doi: 10.3233/MNM-140007. [DOI] [Google Scholar]
- 43.El Achhab Y, Marfa A, Echarbaoui I, Chater R, El-Haidani A, Filali-Zegzouti Y. Physical inactivity, sedentary behaviors and dietary habits among Moroccan adolescents in secondary school. Science Sports. 2018;33(1):58–62. doi: 10.1016/j.scispo.2017.07.012. [DOI] [Google Scholar]
- 44.Hamrani A, Mehdad S, El Kari K, El Hamdouchi A, El Menchawy I, Belghiti H, et al. Physical activity and dietary habits among Moroccan adolescents. Public Health Nutr. 2015;18(10):1793–1800. doi: 10.1017/S1368980014002274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Al-Hazzaa HM, Abahussain NA, Al-Sobayel HI, Qahwaji DM, Musaiger AO. Physical activity, sedentary behaviors and dietary habits among Saudi adolescents relative to age, gender and region. Int J Behav Nutr Phys Act. 2011;8(1):1-4. [DOI] [PMC free article] [PubMed]
- 46.Al-Hazzaa HM, Al-Sobayel HI, Abahussain NA, Qahwaji DM, Alahmadi MA, Musaiger AO. Association of dietary habits with levels of physical activity and screen time among adolescents living in Saudi Arabia. J Hum Nutr Diet. 2014;27(SUPPL2):204–213. doi: 10.1111/jhn.12147. [DOI] [PubMed] [Google Scholar]
- 47.Qahwaji DM. Physical activity and life style among male adolescents in Jeddah, Saudi Arabia. Life Sci J. 2012;9(4):1163–1172. [Google Scholar]
- 48.Nascimento-Ferreira MV, De Moraes ACF, Toazza-Oliveira PV, Forjaz CLM, Aristizabal JC, Santaliesra-Pasías AM, et al. Reliability and validity of a questionnaire for physical activity assessment in south American children and adolescents: the SAYCARE study. Obesity. 2018;26(Suppl 1):S23–S30. doi: 10.1002/oby.22116. [DOI] [PubMed] [Google Scholar]
- 49.Musaiger AO, Al-Mufty BA, Al-Hazzaa HM. Eating habits, inactivity, and sedentary behavior among adolescents in Iraq: sex differences in the hidden risks of noncommunicable diseases. Food Nutr Bull. 2014;35(1):12–19. doi: 10.1177/156482651403500102. [DOI] [PubMed] [Google Scholar]
- 50.Zieff SG, Guedes CM, Wiley J. Youth knowledge of physical activity health benefits: a Brazilian case study. Sci World J. 2006;6:1713–1721. doi: 10.1100/tsw.2006.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.de Lima TR, Silva DAS. Prevalence of physical activity among adolescents in southern Brazil. J Bodyw Mov Ther. 2018;22(1):57–63. doi: 10.1016/j.jbmt.2017.03.022. [DOI] [PubMed] [Google Scholar]
- 52.Florindo AA, Romero A, Peres SV, da Silva MV, Slater B. Development and validation of a physical activity assessment questionnaire for adolescents. Rev Saude Publica. 2006;40(5):802–809. doi: 10.1590/S0034-89102006000600009. [DOI] [PubMed] [Google Scholar]
- 53.Silva DAS, Chaput JP, Tremblay MS. Participation frequency in physical education classes and physical activity and sitting time in Brazilian adolescents. Plos One. 2019;14(3):e0213785. [DOI] [PMC free article] [PubMed]
- 54.Bastos JP, Araújo CLP, Hallal PC. Prevalence of insufficient physical activity and associated factors in Brazilian adolescents. J Phys Act Health. 2008;5(6):777–794. doi: 10.1123/jpah.5.6.777. [DOI] [PubMed] [Google Scholar]
- 55.Coll CDVN, Knuth AG, Bastos JP, Hallal PC, Bertoldi AD. Time trends of physical activity among Brazilian adolescents over a 7-year period. J Adolesc Health. 2014;54(2):209–213. doi: 10.1016/j.jadohealth.2013.08.010. [DOI] [PubMed] [Google Scholar]
- 56.Kee CC, Lim KH, Sumarni MG, Ismail MN, Poh BK, Amal NM. Physical activity and sedentary behaviour among adolescents in petaling district, Selangor, Malaysia. Malaysian J Med Health Sci. 2011;7(1):83–93. [Google Scholar]
- 57.Su TT, Sim PY, Nahar AM, Majid HA, Murray LJ, Cantwell MM, et al. Association between self-reported physical activity and indicators of body composition in Malaysian adolescents. Prev Med. 2014;67:100–105. doi: 10.1016/j.ypmed.2014.07.001. [DOI] [PubMed] [Google Scholar]
- 58.Teo PS, Nurul-Fadhilah A, Foo LH. Development of a new computer-based physical activity questionnaire to estimate habitual physical activity level in Malaysian adolescents. J Sci Med Sport. 2013;16(4):327–331. doi: 10.1016/j.jsams.2012.06.012. [DOI] [PubMed] [Google Scholar]
- 59.Amornsriwatanakul A, Lester L, Bull FC, Rosenberg M. Are Thai children and youth sufficiently active? Prevalence and correlates of physical activity from a nationally representative cross-sectional study. Int J Behav Nutr Phys Act. 2017;14(1):1-9. [DOI] [PMC free article] [PubMed]
- 60.Hong TK, Trang NHHD, van der Ploeg HP, Hardy LL, Dibley MJ. Validity and reliability of a physical activity questionnaire for Vietnamese adolescents. Int J Behav Nutr Phys Act. 2012;9(1):1-7. [DOI] [PMC free article] [PubMed]
- 61.Trang NH, Hong TK, Van der Ploeg HP, Hardy LL, Kelly PJ, Dibley MJ. Longitudinal physical activity changes in adolescents: Ho Chi Minh City youth cohort. Med Sci Sports Exerc. 2012;44(8):1481–1489. doi: 10.1249/MSS.0b013e31824e50dc. [DOI] [PubMed] [Google Scholar]
- 62.Prista A, Marques AT, Maia J. Relationship between physical activity, socioeconomic status, and physical fitness of 8-15-year-old youth from Mozambique. Am J Hum Biol. 1997;9(4):449–457. doi: 10.1002/(SICI)1520-6300(1997)9:4<449::AID-AJHB4>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 63.Prista A, Marques AT, Maia JAR. Empirical validation of an instrument to measure habitual physical activity in youth from Maputo, Mozambique. Am J Hum Biol. 2000;12(4):437–446. doi: 10.1002/1520-6300(200007/08)12:4<437::AID-AJHB2>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 64.Mehreen TS, Ranjani H, Anitha C, Jagannathan N, Pratt M, Mohan V, et al. Reliability and validity of a physical activity questionnaire for Indian children and adolescents. Indian Pediatr. 2020;57(8):707–711. doi: 10.1007/s13312-020-1912-9. [DOI] [PubMed] [Google Scholar]
- 65.TudorLocke C, Ainsworth BE, Adair LS, Du S, Popkin BM. Physical activity and inactivity in Chinese school-aged youth: the China health and nutrition survey. Int J Obesity Relat Metab Disord. 2003;27(9):1093. doi: 10.1038/sj.ijo.0802377. [DOI] [PubMed] [Google Scholar]
- 66.Barbosa N, Sanchez CE, Patiño E, Lozano B, Thalabard JC, Lebozec S, et al. Quantification of physical activity using the QAPACE questionnaire: a two stage cluster sample design survey of children and adolescents attending urban school. J Sports Med Phys Fitness. 2016;56(5):587–596. [PubMed] [Google Scholar]
- 67.Verstraeten R, Lachat C, Ochoa-Avilés A, Hagströmer M, Huybregts L, Andrade S, et al. Predictors of validity and reliability of a physical activity record in adolescents. BMC Public Health. 2013;13(1):1–20. doi: 10.1186/1471-2458-13-1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ghavamzadeh S, Khalkhali HR, Alizadeh M. TV viewing, independent of physical activity and obesogenic foods, increases overweight and obesity in adolescents. J Health Popul Nutr. 2013;31(3):334–342. doi: 10.3329/jhpn.v31i3.16825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Afrifa-Anane E, Agyemang C, Codjoe SNA, Ogedegbe G, Aikins AD. The association of physical activity, body mass index and the blood pressure levels among urban poor youth in Accra, Ghana. BMC Public Health. 2015;15(1):1-9. [DOI] [PMC free article] [PubMed]
- 70.Beets MW. A step in the right direction: commentary on expected values for pedometer-determined physical activity in youth. Res Q Exerc Sport. 2010;81(2):123–124. doi: 10.1080/02701367.2010.10599657. [DOI] [PubMed] [Google Scholar]
- 71.Tudor-Locke C, Ainsworth BE, Adair LS, Popkin BM. Physical activity in Filipino youth: the Cebu longitudinal health and nutrition survey. Int J Obes. 2003;27(2):181–190. doi: 10.1038/sj.ijo.802207. [DOI] [PubMed] [Google Scholar]
- 72.Corder K, Brage S, Wright A, Ramachandran A, Snehalatha C, Yamuna A, et al. Physical activity energy expenditure of adolescents in India. Obesity. 2010;18(11):2212–2219. doi: 10.1038/oby.2010.4. [DOI] [PubMed] [Google Scholar]
- 73.Prista A, Nhantumbo L, Saranga S, Lopes V, Maia J, Seabra A, et al. Physical activity assessed by accelerometry in rural african school-age children and adolescents. Pediatr Exerc Sci. 2009;21(4):384–399. doi: 10.1123/pes.21.4.384. [DOI] [PubMed] [Google Scholar]
- 74.Ramezankhani A, Tavassoli E, Ghafari M, Alidosti M, Daniali SS, Gharlipour Z. Physical activity in adolescent girls and their perceptions of obesity prevention in Shahr-e Kord, Iran. Int J Pediatr. 2016;4(8):3249–3262. [Google Scholar]
- 75.Zieff SG, Guedes CM, Wiley J. Youth knowledge of physical activity health benefits: a Brazilian case study. Sci World J. 2006;6:1713–1721. doi: 10.1100/tsw.2006.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Shokrvash B, Majlessi F, Montazeri A, Nedjat S, Rahimi A, Djazayeri A, et al. Correlates of physical activity in adolescence: a study from a developing country. Glob Health Action. 2013;6(1):20327. [DOI] [PMC free article] [PubMed]
- 77.Ndagire CT, Muyonga JH, Nakimbugwe D. Fruit and vegetable consumption, leisure-time physical activity, and sedentary behavior among children and adolescent students in Uganda. Food Sci Nutr. 2019;7(2):599–607. doi: 10.1002/fsn3.883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zahedi H, Kelishadi R, Heshmat R, Motlagh ME, Ranjbar SH, Ardalan G, et al. Association between junk food consumption and mental health in a national sample of Iranian children and adolescents: the CASPIAN-IV study. Nutrition. 2014;30(11/12):1391–1397. doi: 10.1016/j.nut.2014.04.014. [DOI] [PubMed] [Google Scholar]
- 79.Vakili M, Abedi P, Sharifi M, Hosseini M. Dietary diversity and its related factors among adolescents: a survey in Ahvaz-Iran. Global J Health Sci. 2013;5(2):181–186. doi: 10.5539/gjhs.v5n2p181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Shaikh NI, Frediani JK, Ramakrishnan U, Patil SS, Yount KM, Martorell R, et al. Development and evaluation of a nutrition transition-FFQ for adolescents in South India. Public Health Nutr. 2017;20(7):1162–1172. doi: 10.1017/S1368980016003335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Dalky HF, Al Momani MH, Al-Drabaah TK, Jarrah S. Eating habits and associated factors among adolescent students in Jordan. Clin Nurs Res. 2017;26(4):538–552. doi: 10.1177/1054773816646308. [DOI] [PubMed] [Google Scholar]
- 82.Araki EL, Philippi ST, Martinez MF, Estima CCP, Leal GVS, Alvarenga MS. Pattern of meals eaten by adolescents from technical schools of São Paulo, SP, Brazil. Revista Paulista de Pediatria. 2011;29(2):164–170. doi: 10.1590/S0103-05822011000200006. [DOI] [Google Scholar]
- 83.Francis DK, Van den Broeck J, Younger N, McFarlane S, Rudder K, Gordon-Strachan G, et al. Fast-food and sweetened beverage consumption: association with overweight and high waist circumference in adolescents. Public Health Nutr. 2009;12(8):1106–1114. doi: 10.1017/S1368980009004960. [DOI] [PubMed] [Google Scholar]
- 84.Borges CA, Marchioni DML, Levy RB, Slater B. Dietary patterns associated with overweight among Brazilian adolescents. Appetite. 2018;123:402–409. doi: 10.1016/j.appet.2018.01.001. [DOI] [PubMed] [Google Scholar]
- 85.Bullecer ER, Rabuco LB, Aninao DAB, De Roxas RC, Esguerra JCA, Lim PRU, et al. Dietary diversity score as an indicator of nutritional adequacy of diets among 16-19-year-old adolescents. Acta Medica Philippina. 2012;46(1):28–33. [Google Scholar]
- 86.Cunha DB, Bezerra IN, Pereira RA, Sichieri R. At-home and away-from-home dietary patterns and BMI z-scores in Brazilian adolescents. Appetite. 2018;120:374–380. doi: 10.1016/j.appet.2017.09.028. [DOI] [PubMed] [Google Scholar]
- 87.da Costa Louzada ML, Baraldi LG, Steele EM, Bortoletto Martins AP, Canella DS, Moubarac J-C, et al. Consumption of ultra-processed foods and obesity in Brazilian adolescents and adults. Prev Med. 2015;81:9–15. doi: 10.1016/j.ypmed.2015.07.018. [DOI] [PubMed] [Google Scholar]
- 88.Das G, Pathania R, Das G. Assessment of dietary pattern of adolescents in Himachal Pradesh of India. J Paramed Sci. 2016;7(3):1–7. [Google Scholar]
- 89.Estrada-Reyes C, Tlatempa-Sotelo P, Valdés-Ramos R, Cabañas-Armesilla M, Manjarrez-Montes-De-Oca R. Dietary patterns and fitness level in Mexican teenagers. J Nutr Metab. 2018;2018:1-5. [DOI] [PMC free article] [PubMed]
- 90.Garipagaoglu M, Oner N, Vatansever U, Inan M, Kucukugurluoglu Y, Turan C. Dietary intakes of adolescents living in Edirne, Turkey. J Am Coll Nutr. 2008;27(3):394–400. doi: 10.1080/07315724.2008.10719716. [DOI] [PubMed] [Google Scholar]
- 91.Magbuhat RMT, Borazon EQ, Villarino BJ. Food preferences and dietary intakes of Filipino adolescents in metro Manila, The Philippines. Malaysian J Nutr. 2011;17(1):31–41. [PubMed] [Google Scholar]
- 92.Monge-Rojas R. Dietary intake as a cardiovascular risk factor in Costa Rican adolescents. J Adolesc Health. 2001;28(4):328–337. doi: 10.1016/S1054-139X(00)00214-7. [DOI] [PubMed] [Google Scholar]
- 93.Mascarenhas JMO, Silva RDCR, De Assis AMO, De Santana MLP, De Moraes LTLP, Barreto ML. Identification of food intake patterns and associated factors in teenagers. Revista de Nutrição. 2014;27(1):45–54. doi: 10.1590/1415-52732014000100005. [DOI] [Google Scholar]
- 94.Pangan MRL, Dela Cruz KKL, Nachura MSC, Padolina JL, Ramos MM, Sadorra AQ. Dietary energy density and fast food consumption of 16-21 year-old adolescents. Acta Medica Philippina. 2012;46(3):75–80. doi: 10.47895/amp.v46i3.2104. [DOI] [Google Scholar]
- 95.Majid HA, Ramli L, Ying SP, Su TT, Jalaludin MY, Mohsein N. Dietary intake among adolescents in a middle-income country: an outcome from the Malaysian health and adolescents longitudinal research team study (the MyHeARTs study). Plos One. 2016;11(5):e0155447. [DOI] [PMC free article] [PubMed]
- 96.Ochoa-Avilés A, Verstraeten R, Lachat C, Andrade S, Van Camp J, Donoso S, et al. Dietary intake practices associated with cardiovascular risk in urban and rural Ecuadorian adolescents: a cross-sectional study. BMC Public Health. 2014;14(1):939. doi: 10.1186/1471-2458-14-939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Abizari AR, Ali Z. Dietary patterns and associated factors of schooling Ghanaian adolescents. J Health Popul Nutr. 2019;38(1):5. doi: 10.1186/s41043-019-0162-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bakir BO, Akan H, Akman M, Zahmacioglu O, Hayran O. Nutritional status, healthy eating index and eating attitudes of the adolescents in Istanbul: a cross-sectional study. Int J Adolesc Med Health. 2017;29(3):20150082. [DOI] [PubMed]
- 99.Birru SM, Tariku A, Belew AK. Improved dietary diversity of school adolescent girls in the context of urban Northwest Ethiopia: 2017. Italian J Pediatr. 2018;44(1):1–6. doi: 10.1186/s13052-017-0437-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.de Andrade SC, Barros MBD, Carandina L, Goldbaum M, Cesar CLG, Fisberg RM. Dietary quality index and associated factors among adolescents of the state of Sao Paulo, Brazil. J Pediatr. 2010;156(3):456–460. doi: 10.1016/j.jpeds.2009.09.066. [DOI] [PubMed] [Google Scholar]
- 101.de Morais CMM, Pinheiro LGB, Lima S, Lyra CO, Evangelista K, Lima KC, et al. Dietary patterns of young adolescents in urban areas of Northeast Brazil. Nutricion Hospitalaria. 2013;28(6):1977–1984. [PubMed] [Google Scholar]
- 102.Dixit S, Singh JV, Kant S, Agarwal GG, Dubey A, Kumari N. A cross-sectional study on predictors and significance of eating behavior of adolescent girls. Vulnerable Child Youth Stud. 2014;9(1):10–16. doi: 10.1080/17450128.2013.804971. [DOI] [Google Scholar]
- 103.Majid HA, Amiri M, Azmi NM, Su TT, Jalaludin MY, Al-Sadat N. Physical activity, body composition and lipids changes in adolescents: analysis from the MyHeART study. Sci Rep. 2016;6(1):1-8. [DOI] [PMC free article] [PubMed]
- 104.Mirmiran P, Azadbakht L, Azizi F. Dietary behaviour of Tehranian adolescents does not accord with their nutritional knowledge. Public Health Nutr. 2007;10(9):897–901. doi: 10.1017/S1368980007246701. [DOI] [PubMed] [Google Scholar]
- 105.Rezali FW, Chin YS, Shariff ZM, Mohd Yusof BN, Sanker K, Woon FC. Evaluation of diet quality and its associated factors among adolescents in Kuala Lumpur, Malaysia. Nutr Res Pract. 2015;9(5):511–516. doi: 10.4162/nrp.2015.9.5.511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ronca DB, Blume CA, Cureau FV, Camey SA, Leotti VB, Drehmer M, et al. Diet quality index for Brazilian adolescents: the ERICA study. Eur J Nutr. 2019;59(2):539-56. [DOI] [PubMed]
- 107.Tek NA, Yildiran H, Akbulut G, Bilici S, Koksal E, Karadag MG, et al. Evaluation of dietary quality of adolescents using Healthy Eating Index. Nutr Res Pract. 2011;5(4):322–328. doi: 10.4162/nrp.2011.5.4.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.López IMR, Martín-Matillas M, Delgado-Fernández M, Delgado-Rico E, Folgoso CC, Verdejo-García A. Effect of increased physical activity on physical fitness in an overweight and/or obese group of adolescents. Sport TK. 2021;10(1):17–28. doi: 10.6018/sportk.461551. [DOI] [Google Scholar]
- 109.Neta A, Farias JC, Ferreira F, Marchioni DM. Prospective association between dietary patterns and BMI Z-score in Brazilian adolescents. Public Health Nutr. 2021;24(13):4230–4237. doi: 10.1017/S1368980021000252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Giguère-Johnson M, Ward S, Ndéné Ndiaye A, Galibois I, Blaney S. Dietary intake and food behaviours of Senegalese adolescent girls. BMC Nutr. 2021;7(1):1-10. [DOI] [PMC free article] [PubMed]
- 111.Bezerra IN, Medeiros HB, de Moura SA, Sichieri R. Contribution of away-from-home food to the energy and nutrient intake among Brazilian adolescents. Public Health Nutr. 2021;24(11):3371–3378. doi: 10.1017/S1368980020001573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Bakir BO, Akan H, Akman M, Zahmacioglu O, Hayran O. Nutritional status, healthy eating index and eating attitudes of the adolescents in Istanbul: a cross-sectional study. Int J Adolesc Med Health. 2015;29(3):20150082. [DOI] [PubMed]
- 113.Nabhani-Zeidan M, Naja F, Nasreddine L. Dietary intake and nutrition-related knowledge in a sample of Lebanese adolescents of contrasting socioeconomic status. Food Nutr Bull. 2011;32(2):75–83. doi: 10.1177/156482651103200201. [DOI] [PubMed] [Google Scholar]
- 114.Alavi M, Eftekhari MB, Noot R, Rafinejad J, Chinekesh A. Dietary habits among adolescent girls and their association with parental educational levels. Global J Health Sci. 2013;5(5):202–206. doi: 10.5539/gjhs.v5n5p202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Joulaei H, Keshani P, Kaveh MH. Nutrition literacy as a determinant for diet quality amongst young adolescents: a cross sectional study. Prog Nutr. 2018;20(3):455–464. [Google Scholar]
- 116.Niu J, Seo D-C, Lohrmann D. Weight perception and dietary intake among Chinese youth, 2004-2009. Int J Behav Med. 2014;21(4):691–699. doi: 10.1007/s12529-013-9332-z. [DOI] [PubMed] [Google Scholar]
- 117.Venter I, Winterbach A. Dietary fat knowledge and intake of mid-adolescents attending public schools in the Bellville/Durbanville area of the Western Cape Province. SAfr J Clin Nutr. 2014;23(2):75-83.
- 118.Melaku Y, Dirar A, Feyissa GT, Tamiru D. Optimal dietary practices and nutritional knowledge of school adolescent girls in Jimma town, south West Ethiopia. Int J Adolesc Youth. 2018;23(3):299–307. doi: 10.1080/02673843.2017.1369889. [DOI] [Google Scholar]
- 119.Whati LH. The development of a valid and reliable nutrition knowledge questionnaire and performance-rating scale for urban South African adolescents participating in the ‘birth-to-twenty’ study. 2005. [DOI] [PubMed] [Google Scholar]
- 120.Akman M, Akan H, Izbirak G, Tanriover O, Tilev SM, Yildiz A, et al. Eating patterns of Turkish adolescents: a crosssectional survey. Nutr J. 2010;9(1):1-5. [DOI] [PMC free article] [PubMed]
- 121.Fatikhani DA, Setiawan A. The relationship between the level of knowledge regarding fast food and the dietary habits among adolescents in Jakarta, Indonesia. Enfermeria Clinica. 2019;29:172–175. doi: 10.1016/j.enfcli.2019.04.025. [DOI] [Google Scholar]
- 122.Pajuelo SR, Saintila J, Vásquez MR, Calizaya-Milla YE. Knowledge, attitudes and practices about healthy eating in a Peruvian adolescent population: A cross-sectional study. Revista Espanola de Nutricion Comunitaria. 2021;27(2):91-98.
- 123.Letlape S, Mokwena K, Oguntibeju OO. Knowledge of students attending a high school in Pretoria, South Africa, on diet, nutrition and exercise. 2011. [PubMed] [Google Scholar]
- 124.Alam N, Roy SK, Ahmed T, Ahmed AS. Nutritional status, dietary intake, and relevant knowledge of adolescent girls in rural Bangladesh. J Health Popul Nutr. 2010;28(1):86. doi: 10.3329/jhpn.v28i1.4527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Gitau TM, Micklesfield LK, Pettifor JM, Norris SA. Ethnic differences in eating attitudes, body image and self-esteem among adolescent females living in urban South Africa. Afr J Psychiatry (South Africa) 2014;17(1):468–474. [Google Scholar]
- 126.AllehdanSabika S, Tayyem RF, Bawadi HA, Al-Awwad NJ, Al-Mannai M, Musaiger AO. Fast foods perception among adolescents by gender and weight status. Nutr Health. 2017;23(1):39–45. doi: 10.1177/0260106016685724. [DOI] [PubMed] [Google Scholar]
- 127.Seubsman SA, Kelly M, Yuthapornpinit P, Sleigh A. Cultural resistance to fast-food consumption? A study of youth in north eastern Thailand. Int J Consum Stud. 2009;33(6):669–675. doi: 10.1111/j.1470-6431.2009.00795.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Maulida R, Nanishi K, Green J, Shibanuma A, Jimba M. Food-choice motives of adolescents in Jakarta, Indonesia: the roles of gender and family income. Public Health Nutr. 2016;19(15):2760–2768. doi: 10.1017/S136898001600094X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Soyer MT, Ergin I, Gursoy ST. Effects of social determinants on food choice and skipping meals among Turkish adolescents. Asia Pac J Clin Nutr. 2008;17(2):208–215. [PubMed] [Google Scholar]
- 130.Akman M, Akan H, Izbirak G, Tanriöver Ö, Tilev SM, Yildiz A, et al. Eating patterns of Turkish adolescents: a cross-sectional survey. Nutr J. 2010;9:67–70. doi: 10.1186/1475-2891-9-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Lachat CK, Verstraeten R, Hagströmer M, Khan NC, Van NDA, Dung NQ, et al. Validity of two physical activity questionnaires (IPAQ and PAQA) for Vietnamese adolescents in rural and urban areas. Int J Behav Nutr Phys Act. 2008;5(1):37. doi: 10.1186/1479-5868-5-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Abasi MH, Eslami AA, Rakhshani F, Shiri M. Development and psychometric properties of a selfregulation scale about leisure time physical activity in Iranian male adolescents. Iran J Nurs Midwifery Res. 2016;21(2):183–190. doi: 10.4103/1735-9066.178246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Fortes LS, FFR M, Almeida SS, MEC F. Eating behavior and physical activity in adolescents. Rev Nutr. 2013;26(5):529–537. doi: 10.1590/S1415-52732013000500004. [DOI] [Google Scholar]
- 134.WerneckAndré O, Vancampfort D, Oyeyemi AL, Stubbs B, Silva DR. Associations between TV viewing, sitting time, physical activity and insomnia among 100,839 Brazilian adolescents. Psychiatry Res. 2018;269:700–706. doi: 10.1016/j.psychres.2018.08.101. [DOI] [PubMed] [Google Scholar]
- 135.Wang C, Chen P, Zhuang J. Validity and reliability of international physical activity questionnaire–short form in Chinese youth. Res Q Exerc Sport. 2013;84:S80–SS6. doi: 10.1080/02701367.2013.850991. [DOI] [PubMed] [Google Scholar]
- 136.Azizi-Soleiman F, Motlagh ME, Qorbani M, Heshmat R, Ardalan G, Mansourian M, et al. Dietary habits and health related behaviors in Iranian children and adolescents: the CASPIAN- IV study. Int J Pediatr. 2016;4(7):2087–2097. [Google Scholar]
- 137.Pelegrini A, Silva DAS, Corseuil HX, Silva J, Petroski EL. Stages of change in physical activity-related behavior in adolescents from a Brazilian state capital. Motriz-Revista De Educacao Fisica. 2013;19(4):770–775. doi: 10.1590/S1980-65742013000400015. [DOI] [Google Scholar]
- 138.Werneck AO, Vancampfort D, Oyeyemi AL, Stubbs B, Silva DR. Associations between TV viewing, sitting time, physical activity and insomnia among 100,839 Brazilian adolescents. Psychiatry Res. 2018;269:700–706. doi: 10.1016/j.psychres.2018.08.101. [DOI] [PubMed] [Google Scholar]
- 139.BGC S, ICM S, Ekelund U, Brage S, Ong KK, De Lucia Rolfe E, et al. Associations of physical activity and sedentary time with body composition in Brazilian young adults. Sci Rep. 2019;9(1):1-10. [DOI] [PMC free article] [PubMed]
- 140.Amos PM, Intiful FD, Boateng L. Factors that were found to influence Ghanaian Adolescents’ Eating Habits. Sage Open. 2012;2(4):1–6. doi: 10.1177/2158244012468140. [DOI] [Google Scholar]
- 141.Marchioni DML, Voci SM, De Lima FEL, Fisberg RM, Slater B. Reproducibility of a food frequency questionnaire for adolescents. Cadernos de saude publica. 2007;23(9):2187–2196. doi: 10.1590/S0102-311X2007000900026. [DOI] [PubMed] [Google Scholar]
- 142.Neutzling MB, Assuncao MCF, Malcon MC, Hallal PC, Menezes AMB. Food habits of adolescent students from Pelotas, Brazil. Revista De Nutricao-Brazilian Journal of Nutrition. 2010;23(3):379–388. doi: 10.1590/S1415-52732010000300006. [DOI] [Google Scholar]
- 143.Correa RD, Vencato PH, Rockett FC, Bosa VL. Dietary patterns: are there differences between children and adolescents? Ciencia Saude Coletiva. 2017;22(2):553–562. doi: 10.1590/1413-81232017222.09422016. [DOI] [Google Scholar]
- 144.Loh DA, Moy FM, Zaharan NL, Mohamed Z. Eating behaviour among multi-ethnic adolescents in a middle-income country as measured by the self-reported children’s eating behaviour questionnaire. Plos One. 2013;8(12):1. doi: 10.1371/journal.pone.0082885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Morales A, Montilva M, Gómez N, Cordero M. Adaptación transcultural de la escala de evaluación de conductas alimentarias en adolescentes: “Adolescent food habits checklist”. Trans-cultural adaptation of the eating behaviors rating scale in adolescents: “Adolescent food habits checklist”. An Venez Nutr. 2012;25(1):25–33. [Google Scholar]
- 146.Olumakaiye MF, Atinmo T, Olubayo-Fatiregun MA. Food consumption patterns of Nigerian adolescents and effect on body weight. J Nutr Educ Behav. 2010;42(3):144–151. doi: 10.1016/j.jneb.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 147.Zhang C-X, Chen Y-M, Chen W-Q, Su Y-X, Wang C-L, Wu J-N. Food group intake among adolescents in Guangzhou city compared with the Chinese dietary guidelines. Asia Pac J Clin Nutr. 2012;21(3):450–456. [PubMed] [Google Scholar]
- 148.Ogunsile SE, Ogundele BO. Effect of game-enhanced nutrition education on knowledge, attitude and practice of healthy eating among adolescents in Ibadan, Nigeria. Int J Health Promot Educ. 2016;54(5):207–216. doi: 10.1080/14635240.2016.1157509. [DOI] [Google Scholar]
- 149.Said L, Gubbels JS, SPJ K. Dietary Knowledge, Dietary Adherence, and BMI of Lebanese Adolescents and Their Parents. Nutrients. 2020;12(8):2398. [DOI] [PMC free article] [PubMed]
- 150.Agofure O, Odjimogho S, Okandeji-Barry O, Moses V. Dietary pattern and nutritional status of female adolescents in Amai secondary school, Delta state, Nigeria. Pan Afr Med J. 2021;38(32):15824. [DOI] [PMC free article] [PubMed]
- 151.Shaikh NI, Frediani JK, Ramakrishnan U, Patil SS, Yount KM, Martorell R, et al. Development and evaluation of a nutrition transition-FFQ for adolescents in South India. Public Health Nutr. 2017;20(7):1162–1172. doi: 10.1017/S1368980016003335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Rouhani MH, Kelishadi R, Hashemipour M, Esmaillzadeh A, Azadbakht L. The effect of an energy restricted low glycemic index diet on blood lipids, apolipoproteins and lipoprotein (a) among adolescent girls with excess weight: a randomized clinical trial. Lipids. 2013;48(12):1197–1205. doi: 10.1007/s11745-013-3834-y. [DOI] [PubMed] [Google Scholar]
- 153.Araujo J, Teixeira J, Gaio AR, Lopes C, Ramos E. Dietary patterns among 13-y-old Portuguese adolescents. Nutrition. 2015;31(1):148–154. doi: 10.1016/j.nut.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 154.Araujo MC, Yokoo EM, Pereira RA. Validation and calibration of a Semiquantitative food frequency questionnaire designed for adolescents. J Am Diet Assoc. 2010;110(8):1170–1177. doi: 10.1016/j.jada.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 155.Borges CA, Enes CC, Slater B, Conde WL. BMI changes associated with dietary trends among Brazilian adolescents. Infant Child Adolesc Nutr. 2012;4(6):361–368. doi: 10.1177/1941406412451995. [DOI] [Google Scholar]
- 156.de Assumpção D, Barros MBA, Fisberg RM, Carandina L, Goldbaum M, Cesar CLG. Diet quality among adolescents: a population-based study in Campinas, Brazil. Revista Brasileira de Epidemiologia. 2012;15(3):605–616. doi: 10.1590/S1415-790X2012000300014. [DOI] [PubMed] [Google Scholar]
- 157.Henn RL, Fuchs SC, Moreira LB, Fuchs FD. Development and validation of a food frequency questionnaire (FFQ-Porto Alegre) for adolescent, adult and elderly populations from southern Brazil. Cad Saude Publica. 2010;26(11):2068–2079. doi: 10.1590/S0102-311X2010001100008. [DOI] [PubMed] [Google Scholar]
- 158.Mascarenhas JMO, Silva RCR, Machado MEPC, Santos CAST, Marchioni DML, Barreto ML. Validation of a food frequency questionnaire designed for adolescents in Salvador, Bahia, Brazil. Revista de Nutricao. 2016;29(2):163–171. doi: 10.1590/1678-98652016000200002. [DOI] [Google Scholar]
- 159.Slater B, Enes CC, López RVM, Damasceno NRT, Voci SM. Validation of a food frequency questionnaire to assess the consumption of carotenoids, fruits and vegetables among adolescents: the method of triads. Cadernos de saude publica. 2010;26(11):2090–2100. doi: 10.1590/S0102-311X2010001100010. [DOI] [PubMed] [Google Scholar]
- 160.Azadbakht L, Akbari F, Esmaillzadeh A. Diet quality among Iranian adolescents needs improvement. Public Health Nutr. 2015;18(4):615–621. doi: 10.1017/S1368980014000767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Rouhani MH, Mirseifinezhad M, Omrani N, Esmaillzadeh A, Azadbakht L. Fast food consumption, quality of diet, and obesity among Isfahanian adolescent girls. J Obesity. 2012;2012:597924. [DOI] [PMC free article] [PubMed]
- 162.Tehrani AN, Farhadnejad H, Salehpour A, Beyzai B, Hekmatdoost A, Rashidkhani B. The association between nutrition knowledge and adherence to a Mediterranean dietary pattern in Iranian female adolescents. Int J Adolesc Med Health. 2019;33(4):e20180188. [DOI] [PubMed]
- 163.Mohamed K, Tin TS, Jalaludin MY, Al-Sadat N, Majid HA. Comparative validity of a Food Frequency Questionnaire (MyUM Adolescent FFQ) to estimate the habitual dietary intake of adolescents in Malaysia. Asia Pac J Clin Nutr. 2018;27(4):898–907. doi: 10.6133/apjcn.022018.03. [DOI] [PubMed] [Google Scholar]
- 164.Wei X, Caihong S, Li Z, Xin Z, Jiajia W, Hui W, et al. Reproducibility and Relative Validity of a Food Frequency Questionnaire Developed for Female Adolescents in Suihua, North China. Plos One. 2011;6(5):1–7. doi: 10.1371/journal.pone.0020154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Said L, Gubbels JS, Kremers SPJ. Development of dietary knowledge and adherence questionnaires for lebanese adolescents and their parents. Int J Environ Res Public Health. 2020;17(1):147. [DOI] [PMC free article] [PubMed]
- 166.Thorne-Lyman AL, Shaikh S, Mehra S, LSF W, Ali H, Alland K, et al. Dietary patterns of >30,000 adolescents 9–15 years of age in rural Bangladesh. Ann N Y Acad Sci. 2020;1468(1):3–15. [DOI] [PMC free article] [PubMed]
- 167.Nurul-Fadhilah A, Teo PS, Foo LH. Validity and reproducibility of a food frequency questionnaire (FFQ) for dietary assessment in Malay adolescents in Malaysia. Asia Pac J Clin Nutr. 2012;21(1):97–103. [PubMed] [Google Scholar]
- 168.Nurul-Fadhilah A, Teo PS, Huybrechts I, Foo LH. Infrequent breakfast consumption is associated with higher body adiposity and abdominal obesity in Malaysian school-aged adolescents. Plos One. 2013;8(3):e59297. doi: 10.1371/journal.pone.0059297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Slater B, Philippi S, Fisberg R, Latorre M. Validation of a semi-quantitative adolescent food frequency questionnaire applied at a public school in São Paulo, Brazil. Eur J Clin Nutr. 2003;57(5):629–635. doi: 10.1038/sj.ejcn.1601588. [DOI] [PubMed] [Google Scholar]
- 170.Xia W, Sun C, Zhang L, Zhang X, Wang J, Wang H, et al. Reproducibility and relative validity of a food frequency questionnaire developed for female adolescents in Suihua, North China. Plos One. 2011;6(5):e19656. doi: 10.1371/journal.pone.0019656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Patcheep K. Factors influencing URBAN Adolescents’ eating behavior, RATCHABURI province, Thailand: an application of the theory of planned behavior. J Health Res. 2015;29(6):441–447. [Google Scholar]
- 172.Ogunkunle MO, Oludele AS. Food intake and meal pattern of adolescents in school in Ila Orangun, South-West Nigeria. South Afr J Clin Nutr. 2013;26(4):188–193. doi: 10.1080/16070658.2013.11734471. [DOI] [Google Scholar]
- 173.Itani L, Chatila H, Dimassi H, El Sahn F. Development and validation of an Arabic questionnaire to assess psychosocial determinants of eating behavior among adolescents: a cross-sectional study. J Health Popul Nutr. 2017;36:1–8. doi: 10.1186/s41043-017-0086-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Olumakaiye MF, Atinmo T, Olubayo-Fatiregun MA. Food consumption patterns of Nigerian adolescents and effect on body weight. J Nutr Educ Behav. 2010;42(3):144–151. doi: 10.1016/j.jneb.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 175.Hatami M, Taib MN, Jamaluddin R, Saad HA, Djazayery A, Chamari M, et al. Dietary factors as the major determinants of overweight and obesity among Iranian adolescents a cross-sectional study. Appetite. 2014;82:194–201. doi: 10.1016/j.appet.2014.07.026. [DOI] [PubMed] [Google Scholar]
- 176.Kafeshani O, Sarrafzadegan N, Nouri F, Mohammadifard N. Major dietary patterns in Iranian adolescents: Isfahan Healthy Heart Program, Iran. 2015. pp. 61–68. [PMC free article] [PubMed] [Google Scholar]
- 177.Masoomi H, Taheri M, Irandoust K, H’Mida C, Chtourou H. The relationship of breakfast and snack foods with cognitive and academic performance and physical activity levels of adolescent students. Biol Rhythm Res. 2019;51(3):481-8.
- 178.Safiri S, Kelishadi R, Qorbani M, Lotfi R, Djalalinia S, Salehifar D, et al. Association of dietary behaviors with physical activity in a nationally representative sample of children and adolescents: The CASPIAN- IV study. Int J Pediatr. 2016;4(3):1505–1517. [Google Scholar]
- 179.Musaiger AO, Al-Mannai M, Tayyem R, Al-Lalla O, Ali EY, Kalam F, et al. Risk of disordered eating attitudes among adolescents in seven Arab countries by gender and obesity: a cross-cultural study. Appetite. 2013;60:162–167. doi: 10.1016/j.appet.2012.10.012. [DOI] [PubMed] [Google Scholar]
- 180.Musaiger AO, Nabag FO, Al-Mannai M. Obesity, dietary habits, and sedentary behaviors among adolescents in Sudan. Food Nutr Bull. 2016;37(1):65–72. doi: 10.1177/0379572116629244. [DOI] [PubMed] [Google Scholar]
- 181.DGD C, De Andrade SM, Mesas AE, Fernandes RA, Farias Júnior JC. Higher screen time is associated with overweight, poor dietary habits and physical inactivity in Brazilian adolescents, mainly among girls. Eur J Sport Sci. 2016;16(4):498–506. doi: 10.1080/17461391.2015.1068868. [DOI] [PubMed] [Google Scholar]
- 182.Djordjević-Nikić M, Dopsaj M, Vesković A. Nutritional and physical activity behaviours and habits in adolescent population of Belgrade. Ponašanje i navike u ishrani i fizičkoj aktivnosti kod beogradskih adolescenata. 2013;70(6):548–554. doi: 10.2298/vsp1306548d. [DOI] [PubMed] [Google Scholar]
- 183.da Costa BGG, Chaput JP, Lopes MVV, Gaya AR, Silva DAS, Silva KS. Association between sociodemographic, dietary, and substance use factors and accelerometer-measured 24-hour movement behaviours in Brazilian adolescents. Eur J Pediatr. 2021;180(11):3297–3305. doi: 10.1007/s00431-021-04112-0. [DOI] [PubMed] [Google Scholar]
- 184.Abdullah NF, Teo PS, Foo LH. Ethnic differences in the food intake patterns and its associated factors of adolescents in Kelantan, Malaysia. Nutrients. 2016;8(9):551. [DOI] [PMC free article] [PubMed]
- 185.Barufaldi LA, Abreu GD, Oliveira JS, dos Santos DF, Fujimori E, SML V, et al. ERICA: prevalence of healthy eating habits among Brazilian adolescents. Rev Saude Publica. 2016;50(1):6s. [DOI] [PMC free article] [PubMed]
- 186.Barufaldi LA, Abreu GDA, Veiga GVD, Sichieri R, Kuschnir MCC, Cunha DB, et al. Software to record 24-hour food recall: application in the study of cardiovascular risks in adolescents. Revista Brasileira de Epidemiologia. 2016;19(2):464–468. doi: 10.1590/1980-5497201600020020. [DOI] [PubMed] [Google Scholar]
- 187.De Oliveira LMFT, Da Silva AO, Dos Santos MAM, Ritti-Dias RM, Diniz PRB. Exercise or physical activity: which is more strongly associated with the perception of sleep quality by adolescents? Revista Paulista de Pediatria. 2018;36(3):322–328. doi: 10.1590/1984-0462/;2018;36;3;00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.ACB N, MIS DA, De Menezes Lima VL, ADS D. Body weight and food consumption scores in adolescents from northeast Brazil. Revista Paulista de Pediatria. 2015;33(3):319–326. doi: 10.1016/j.rpped.2015.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Teo PS, Nurul-Fadhilah A, Foo LH. Development of a new computer-based physical activity questionnaire to estimate habitual physical activity level in Malaysian adolescents. J Sci Med Sport. 2013;16(4):327–331. doi: 10.1016/j.jsams.2012.06.012. [DOI] [PubMed] [Google Scholar]
- 190.Lien N, Lytle LA, Komro KA. Applying theory of planned behavior to fruit and vegetable consumption of young adolescents. Am J Health Promot. 2002;16(4):189–197. doi: 10.4278/0890-1171-16.4.189. [DOI] [PubMed] [Google Scholar]
- 191.Janz K. Physical activity in epidemiology: moving from questionnaire to objective measurement. Br J Sports Med. 2006;40(3):191–192. doi: 10.1136/bjsm.2005.023036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Shim J-S, Oh K, Kim HC. Dietary assessment methods in epidemiologic studies. Epidemiol Health. 2014;36:e2014009. [DOI] [PMC free article] [PubMed]
- 193.Reilly JJ, Penpraze V, Hislop J, Davies G, Grant S, Paton JY. Objective measurement of physical activity and sedentary behaviour: review with new data. Arch Dis Child. 2008;93(7):614–619. doi: 10.1136/adc.2007.133272. [DOI] [PubMed] [Google Scholar]
- 194.World Health Organization. STEPwise Approach to NCD Risk Factor Surveillance (STEPS). STEPS Instrument: World Health Organization; 2021. Available from: https://www.who.int/teams/noncommunicable-diseases/surveillance/systems-tools/steps
- 195.World Bank Group . Mobile cellular subscriptions (per 100 people) 2021. [Google Scholar]
- 196.Hyder AA, Wosu AC, Gibson DG, Labrique AB, Ali J, Pariyo GW. Noncommunicable disease risk factors and mobile phones: a proposed research agenda. J Med Internet Res. 2017;19(5):e133. doi: 10.2196/jmir.7246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Casperson SL, Sieling J, Moon J, Johnson L, Roemmich JN, Whigham L. A mobile phone food record app to digitally capture dietary intake for adolescents in a free-living environment: usability study. JMIR Mhealth Uhealth. 2015;3(1):e3324. [DOI] [PMC free article] [PubMed]
- 198.Hallal PC, Matsudo S, Farias JC. Measurement of physical activity by self-report in low-and middle-income countries: more of the same is not enough. J Phys Act Health. 2012;9(s1):S88–S90. doi: 10.1123/jpah.9.s1.s88. [DOI] [PubMed] [Google Scholar]
- 199.Al-Hazzaa HM, Musaiger AO, Group AR . Arab Teens Lifestyle Study (ATLS): objectives, design, methodology and implications. Diabetes, metabolic syndrome and obesity: targets and therapy. 2011. p. 417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Keats EC, Rappaport AI, Shah S, Oh C, Jain R, Bhutta ZA. The dietary intake and practices of adolescent girls in low-and middle-income countries: a systematic review. Nutrients. 2018;10(12):1978. doi: 10.3390/nu10121978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Strengthening Partnerships Results and Innovations in Nutrition Globally. Adolescent Nutrition CALL TO ACTION: Better Data Now to Drive Better Policies and Programs in the Future Arlington, VA Arlington, VA. 2018 Available from: https://www.spring-nutrition.org/about-us/news/adolescent-nutrition-call-action-better-data-now-drive-better-policies-and-programs.
- 202.Peltzer K. Leisure time physical activity and sedentary behavior and substance use among in-school adolescents in eight African countries. Int J Behav Med. 2010;17(4):271–278. doi: 10.1007/s12529-009-9073-1. [DOI] [PubMed] [Google Scholar]
- 203.Micklesfield LK, Pedro TM, Kahn K, Kinsman J, Pettifor JM, Tollman S, et al. Physical activity and sedentary behavior among adolescents in rural South Africa: levels, patterns and correlates. BMC Public Health. 2014;14(1):1–19. doi: 10.1186/1471-2458-14-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.United Nations Educational Scientific and Cultural Organization. Education data release: one in every five children, Adolescents and Youth is Out of School [Internet]. 2018. Paris: United Nations Educational, Scientific and Cultural Organization; [updated 2018 Feb 28; cited 2022 April 22]. Available from: http://uis.unesco.org/en/news/education-data-release-one-every-five-children-adolescents-and-youth-out-school.
- 205.Moore DW, Bean TW, Birdyshaw D, Rycik JA. Adolescent literacy: a position statement. J Adolesc Adult Lit. 1999;43(1):97–112. [Google Scholar]
- 206.Bandeira FM, Freitas MP, László M, Silva MC, Hallal PC, Rombaldi AJ. Mode of administration does matter: comparability study using IPAQ. Motriz: Revista de Educação Física. 2015;21(4):370–374. [Google Scholar]
- 207.Wright B, Ogbuehi AO. Surveying adolescents: the impact of data collection methodology on response quality. Electron J Bus Res Methods. 2014;12(1):41. [Google Scholar]
- 208.Bowling A. Mode of questionnaire administration can have serious effects on data quality. J Public Health. 2005;27(3):281–291. doi: 10.1093/pubmed/fdi031. [DOI] [PubMed] [Google Scholar]
- 209.Myers M. Qualitative research and the generalizability question: standing firm with Proteus. Qual Rep. 2000;4(3):9. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analysed during this study are included in this published article [and its supplementary information files].