Abstract
Purpose
Symptoms often persistent for more than 4 weeks after COVID-19—now commonly referred to as ‘Long COVID’. Independent of initial disease severity or pathological pulmonary functions tests, fatigue, exertional intolerance and dyspnea are among the most common COVID-19 sequelae. We hypothesized that respiratory muscle dysfunction might be prevalent in persistently symptomatic patients after COVID-19 with self-reported exercise intolerance.
Methods
In a small cross-sectional pilot study (n = 67) of mild-to-moderate (nonhospitalized) and moderate-to-critical convalescent (formerly hospitalized) patients presenting to our outpatient clinic approx. 5 months after acute infection, we measured neuroventilatory activity P0.1, inspiratory muscle strength (PImax) and total respiratory muscle strain (P0.1/PImax) in addition to standard pulmonary functions tests, capillary blood gas analysis, 6 min walking tests and functional questionnaires.
Results
Pathological P0.1/PImax was found in 88% of symptomatic patients. Mean PImax was reduced in hospitalized patients, but reduced PImax was also found in 65% of nonhospitalized patients. Mean P0.1 was pathologically increased in both groups. Increased P0.1 was associated with exercise-induced deoxygenation, impaired exercise tolerance, decreased activity and productivity and worse Post-COVID-19 functional status scale. Pathological changes in P0.1, PImax or P0.1/PImax were not associated with pre-existing conditions.
Conclusions
Our findings point towards respiratory muscle dysfunction as a novel aspect of COVID-19 sequelae. Thus, we strongly advocate for systematic respiratory muscle testing during the diagnostic workup of persistently symptomatic, convalescent COVID-19 patients.
Keywords: SARS-CoV-2, COVID-19, P0.1, PImax, P0.1/PImax, Long COVID
Introduction
While lung, kidney and the vascular system appear to be the main sites of acute Severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2)-related complications [1, 2], early sequelae of coronavirus disease (COVID)-19 are reported by the vast majority of convalescent patients [3, 4]. Sequelae persisting for longer than 4 weeks are now phenotypically summarized under the umbrella term “Long COVID” [4]. The most commonly reported symptoms include persistent dyspnea and fatigue in up to 51% and 63% of cases, respectively, which are also among the longest lasting sequelae [3, 5]. As recently reported, exertional intolerance and dyspnea can also be observed in Long COVID patients with preserved lung function [6]. In this light, in addition to a growing body of evidence regarding pulmonary parenchymal and cardiac sequelae, exercise intolerance in Long COVID patients might have additional causes related to respiratory muscular dysfunction.
In a cross-sectional approach, we have therefore prospectively investigated respiratory drive and effort in Long COVID-19 patients with self-reported exercise intolerance presenting to our outpatient department (OPD).
Methods
Sixty-seven adult convalescent COVID-19 patients (30 female, 37 male, mean age: 49 years, baseline characteristics are given in Table 1) presenting after mild to critical disease (according to World Health Organization (WHO) classification) completed general symptom, activity and productivity (modified Work Productivity and Activity Impairment (WPAI) score) questionnaires before undergoing complete pulmonary function testing (PFT), including spirometry, body plethysmography, capillary blood gas analyses (CBG) at rest and immediately after performing a 6 min walk test (6MWT). Assessment of dyspnea intensity at rest and during the 6MWT using the Modified BORG Dyspnea Scale (Borg CR10) was performed. In addition, respiratory muscle testing to assess respiratory drive and effort was conducted following current guidelines [7, 8]. All adult patients with persisting symptoms for ≥ 4 weeks after COVID-19 with a proven record of SARS-CoV-2 infection (positive PCR for SARS-CoV-2 or presence of SARS-CoV-2-specific nucleocapsid antibodies) were eligible after informed consent. Patients < 18 years or without proven SARS-CoV-2 infection were excluded. Patients were recruited via the Post COVID Clinics of the Divisions of Pneumology and Infectious Diseases at the University Medical Center Hamburg Eppendorf. Eligible patients categorized as hospitalized had to be hospitalized due to COVID-19.
Table 1.
Baseline characteristics of the study cohort at the time of presentation to the outpatient department
| Hospitalization during COVID-19 | No n = 30 | Yes n = 37 | p value |
|---|---|---|---|
| Age (years) Mean ± SD | 41.1 ± 10.7 | 55.9 ± 12.5 | < 0.001 |
| Sex (n, %) | |||
| Female | 17 (56.7) | 13 (35.1) | 0.130 |
| BMI (kg/m2) mean ± SD | 25.3 ± 4.5 | 28.6 ± 5.3 | < 0.001 |
| Time from Dx (days) mean ± SD | 123.6 ± 69.4 | 147.5 ± 70.8 | 0.170 |
| Smoking status (n, %) | 0.322 | ||
| Active | 4 (13.3) | 2 (5.4) | |
| Former | 8 (26.7) | 16 (43.2) | |
| Never | 18 (60.0) | 18 (48.6) | |
| Unknown | 0 (0.0) | 1 (2.7) | |
| Disease severity (n, %) | < 0.001 | ||
| WHO class | |||
| Mild | 20 (66.7) | 2 (5.4) | |
| Moderate | 10 (33.3) | 12 (32.4) | |
| Severe | 0 (0.0) | 7 (18.9) | |
| Critical | 0 (0.0) | 16 (43.2) | |
| ARDS (n, %) | |||
| yes | 0 (0.0) | 15 (40.5) | < 0.001 |
| Total no. of comorbidities median (IQR) | 0 (0–1) | 2 (0–3) | < 0.001 |
| Comorbidities (n, %) | |||
| Diabetes | 0 (0) | 6 (16.7) | 0.028 |
| Cardiovascular disease | 2 (6.7) | 9 (24.3) | 0.043 |
| Hypertension | 4 (13.3) | 13 (35.1) | 0.037 |
| Renal insufficiency | 0 (0) | 5 (13.9) | 0.011 |
| Adipositas | 0 (0–0) | 0 (0–1) | 0.030 |
| Liver disease | 0 (0–0) | 0 (0–1) | 0.003 |
| Thyroid dysfunction | 2 (6.7) | 4 (10.8) | 0.550 |
| Neurological disease / myopathies | 0 (0) | 0 (0) | – |
| Asthma | 8 (26.7) | 5 (13.5) | 0.176 |
| COPD | 0 (0) | 1 (2.7) | 0.364 |
| Other lung disease | 1 (3.3) | 1 (2.7) | 0.880 |
| PFT (%) | |||
| Mean ± SD | |||
| FVC | 98.2 ± 12.4 | 83.7 ± 21.5 | 0.002 |
| FEV1 | 97.2 ± 11.9 | 87.3 ± 18.0 | 0.012 |
| FEV1/FVC | 99.3 ± 8.0 | 105.7 ± 8.6 | 0.003 |
| RV | 107.4 ± 28.3 | 91.4 ± 28.4 | 0.025 |
| TLC | 103.5 ± 14.5 | 87.5 ± 18.9 | < 0.001 |
| FRC | 96.3 ± 21.6 | 82.2 ± 21.9 | 0.012 |
| DLCO | 83.0 ± 12.6 | 68.8 ± 17.7 | 0.001 |
| PFT Pattern (n, %) | |||
| Restrictive | 1 (3.3) | 13 (35.1) | < 0.001 |
| Obstructive | 3 (10.0%) | 1 (2.7%) | 0.210 |
| 6MWT | |||
| Mean ± SD | |||
| 6MWD (m) | 607.0 ± 53.7 | 514.7 ± 127.2 | < 0.001 |
| CBG (mmHg) | |||
| Median (IQR) | |||
| ΔPaO2 | 1.5 (− 7.8–5.2) | − 7.8 (− 12.1–− 0.4) | 0.021 |
| ΔPaCO2 | 0.8 (− 0.8–2.4) | − 0.5 (− 1.1–− 2.2) | 0.406 |
| Dyspnea (Borg CR10) | |||
| Median (IQR) | |||
| Difference | 1.00 (0.62–3.00) | 2.00 (0.50–2.25) | 0.984 |
| Mean ± SD | |||
| At rest | 0.4 ± 0.8 | 0.6 ± 1.1 | 0.462 |
| Exercise | 2.2 ± 1.7 | 2.3 ± 1.7 | 0.829 |
| Productivity (modified WPAI) | |||
| Median (IQR) | 5.5 (3.0–11.5) | 10.0 (4.0–15.25) | 0.104 |
| PCFS Scale | |||
| Median (IQR) | 2 (1–3) | 2 (1–3) | 0.698 |
SD Standard deviation, BMI Body Mass Index, Dx Diagnosis, IQR Interquartile Range, ARDS Acute respiratory distress syndrome, No Number, COPD: chronic obstructive pulmonary disease, PFT Pulmonary Function Test, FVC Forced vital capacity, FEV1 Forced expiratory volume in 1 s, FEV1/FVC Tiffeneau-Pinelli index, RV Residual volume, TLC Total lung capacity, FRC Functional residual capacity, DLCO Diffusing capacity for carbon monoxide, 6MWT 6-min walk test, CBG Capillary blood gas, Δ Difference between Rest and Exercise, CR Category ratio, WPAI Work Productivity and Activity Index, PCFS Post-COVID-19 Functional Status
PRISM 9 (GraphPad Inc, San Diego, CA) and R for macOS version 4.0.3 (https://cran.r-project.org) with RStudio 1.3 (RStudio, Boston, MA) were used for the following statistical analyses: one-sample t test and Pearson correlation analysis for normally distributed data (D’Agostino-Pearson Test); Mann–Whitney, Spearman correlation and Fisher’s exact test for nonparametric data; corrplot 0.84 library was utilized for principal component clustering.
Results
At the time of presentation to our OPD (median of 152 days, IQR: 65–260 after onset of acute symptoms), patients initially hospitalized due to COVID-19 (55% of cohort) showed reduced PFT parameters compared with nonhospitalized patients. In addition, initially hospitalized patients walked 92.3 m (15.2%) less in the 6MWT and showed a more pronounced decrease in the arterial partial pressure of oxygen (PaO2) during the 6MWT (median: + 1.5 mmHg vs. − 7.8 mmHg). No differences were found in dyspnea perception, functional impairment, daily activity or productivity. While hospitalized patients were older, had a higher body mass index and more comorbidities which were associated with more severe acute disease, history of lung disease was rare and did not differ between hospitalized and nonhospitalized patients (Table 1).
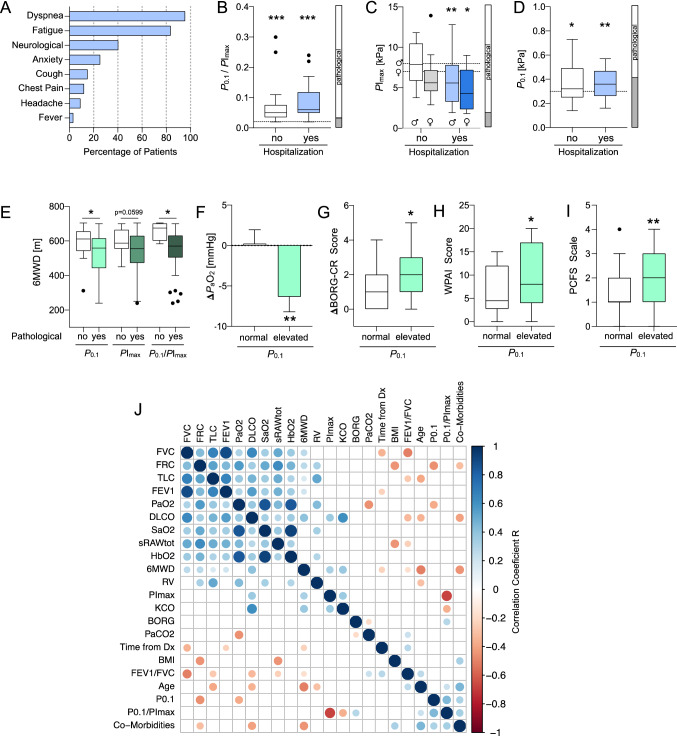
In addition to exercise intolerance reported by all patients, the most frequent symptoms were persistent exertional dyspnea (95.5%) and fatigue (83.6%, Fig. 1A). These symptoms were associated with alterations in respiratory drive and effort. Both hospitalized and nonhospitalized patients had increased total respiratory muscle strain (= occlusion pressure at 0.1 s (P0.1)/ maximal inspiratory pressure (PImax) > 0.02); 97.2 vs. 87.1%, P0.1/PImax range: 3–25%, p = 0.0005 and p = 6.6E-08, Fig. 1B) at the time of presentation to the OPD. Hospitalized patients showed a trend towards more pronounced respiratory muscle strain (P0.1/PImax: 0.05 vs. 0.06, p = 0.056). Inspiratory muscle strength (as determined by the peak value of maximum inspiratory mouth pressure measured from residual volume (PImaxpeak RV) = PImax) was decreased below six and age-specific cutoffs in 88% of patients (Fig. 1C, vertical bar), predominantly in patients previously hospitalized due to COVID-19 (p = 0.0108, female and p = 0.0079, male; Fig. 1C). In addition, inspiratory muscle weakness was more frequent in women (96.4 vs. 79.3%, p = 0.0088, Fisher’s exact test). Neuroventilatory activity as determined by P0.1 > 0.3 kPa (~ 3.1 cmH2O) was elevated in 56% of patients (mean P0.1: 0.36 and 0.37 kPa, p = 0.0291 and p = 0.0029, nonhospitalized and hospitalized, respectively, Fig. 1D), which was independent of hospitalization status (p = 0.64).
Fig. 1.
Respiratory muscle impairment after COVID-19 is associated with impaired exercise tolerance, exercise-induced deoxygenation, activity and functional outcome A Persisting symptoms of convalescent COVID-19 patients at the time of presentation to the outpatient department (OPD) (mean: 152 days after diagnosis, Dx, n = 67). B Respiratory muscle strain P0.1/PImax at OPD presentation after COVID-19 by hospitalization status of acute COVID-19 (***p = 6.0E−08 and ***p = 5.8E−11, respectively; one-sample Wilcoxon test versus upper limit of normal cutoff: 0.02). C Inspiratory muscle strength PImax by sex and hospitalization status (nonhospitalized: male (♂), p = 0.83 and female (♀), p = 0.10; hospitalized: male, **p = 0.0079; female, *p = 0.0269; one-sample Wilcoxon versus cutoff: 8 kPa, male and 7 kPa, female). Fractions of sex- and age-corrected pathological test results are given in the adjacent vertical bar. D Airway occlusion pressure at 0.1 s, P0.1 per same patient as in (B) (*p = 0.0291, **p = 0.0027, one-sample t test versus cutoff: 0.3 kPa) and fraction of pathological test results (adjacent bar). E Six-minute walking test (6MWT) distance (6MWD) in meters (m) by P0.1 (*p = 0.0219), PImax (p = 0.0599) and P0.1/PImax (p = 0.0162), Mann–Whitney test. F Difference in arterial partial pressures for oxygen (ΔPaO2) by P0.1 (**p = 0.0134, unpaired, 2-sided t test) G Difference in self-reported dyspnea perception (BORG-CR score) at rest and immediately after 6MWT by P0.1 (ΔBORG-CR, *p = 0.0299, Mann–Whitney test). H Self-reported activity and productivity impairment (modified WPAI score) in the last seven days before presentation to the OPD by P0.1 (*p = 0.0471, Mann–Whitney test). I Self-reported Post-COVID-19 Functional Status (PCFS) scale at the time of presentation to the OPD by P0.1 (**p = 0.0058, Mann–Whitney test). J Multivariate matrix of significantly (p < 0.05) correlated variables from the study cohort (Pearson or Spearman R values) sorted by first principal component. Box-and-whiskers showing medians + interquartal range (IQR) and outliers (Tukey method). In F, normally distributed data are given as mean ± standard error of the mean. Dashed lines in G, H and I represent pathological (sex-specific) cutoff values. Mann–Whitney test in F, G, H and I was used for comparison of groups with normal vs. elevated P0.1.Vertical bars in B, C and D represent the fraction of pathological (open) and normal (gray) values from the total cohort
Clinically, alterations in respiratory drive and effort after COVID-19 were associated with reduced distance (6MWD) in the 6MWT (P0.1: 595.5 vs. 529.3 m, p = 0.0219; PImax: 600.1 vs. 537.6 m, p = 0.0599; P0.1/PImax: 659.3 vs. 548.5 m, p = 0.0162; Fig. 1E).
While no patient was hypoxemic at rest, convalescent COVID-19 patients with elevated P0.1 showed a significant decrease in arterial oxygen partial pressure (PaO2) during the 6MWT (ΔPaO2: − 6.6 mmHg, p = 0.0134; Fig. 1F). In all patients with exertional deoxygenation, pulmonary thromboembolic disease was ruled out by subsequent ventilation/perfusion scans.
Patients with elevated P0.1 after COVID-19 reported increased dyspnea during the 6MWT, as informed by a larger difference (Δ) in BORG scores at rest and upon exercise (+ 1.3 vs. + 2.1, p = 0.0299; larger = worse, Fig. 1G). In addition, patients with elevated P0.1 > 0.3 kPa also reported less daily activity and productivity due to persisting symptoms (modified WPAI score, 6.3 vs. 9.8, p = 0.0471; higher = larger impairment, Fig. 1H) as well as increased overall functional impairment as determined by the Post-COVID functional status (PCFS, [9]) scale (1 vs. 2, p = 0.0058; higher = larger impairment, Fig. 1I).
In univariate regression analysis, P0.1 was associated with functional residual capacity (FRC, r = − 0.27, p = 0.046), ΔPaO2 (r = − 0.30, p = 0.007), number of comorbidities (r = 0.27, p = 0.044) and P0.1/PImax (r = 0.30, p = 0.007). PImax was correlated with the diffusing capacity of carbon monoxide (DLCO, r = 0.37, p = 0.006), 6MWD (r = 0.33, p = 0.014), Carbon monoxide transfer coefficient (KCO, r = 0.36, p = 0.006) and P0.1/PImax (r = − 0.54, p = 2.1E-05). P0.1/PImax was associated with KCO (r = − 0.33, p = 0.015), ΔBORG score (r = 0.33, p = 0.013), age (r = 0.26, p = 0.05) and number of comorbidities (r = 0.40, p = 0.003) (Fig. 1J).
In a principal component-based multivariate analysis, P0.1 and P0.1/PImax clustered with age, body-mass-index (BMI), number of comorbidities, FEV1/FVC, time from diagnosis and CBG while PImax, did not clearly cluster with any of the parameters (Fig. 1J).
Comorbidities were not associated with pathologically altered P0.1, PImax or P0.1/PImax (all p > 0.05). Patients with a history of asthma were less likely to show pathological P0.1/PImax (χ2 = 5.41, p = 0.020).
Discussion
In our cross-sectional pilot study of convalescent COVID-19 patients with persistent exercise intolerance, we identified a high prevalence of impaired respiratory muscle function and upregulated neuroventilatory activity ~ 5 months after diagnosis. Functionally, this was associated with reduced 6MWD and daily activity/productivity in connection with exercise-induced deoxygenation.
Recently, published PFT data of COVID-19 patients show reduced TLC and DLCO up to 6 months after infection, which occurred more often in patients with severe disease [5]. This is in line with our data showing that patients initially hospitalized for COVID-19 had significantly lower PFT parameters, including TLC and DLCO, up to 5 months after infection. This was also associated with reduced exercise capacity in hospitalized patients after COVID-19 as measured by 6MWD. Our study extends these findings, as we report a high prevalence of increased respiratory drive and impaired respiratory muscle capacity in convalescent, persistently symptomatic COVID-19 patients.
In our cohort, patients requiring hospitalizations, including ICU treatment, also had impaired respiratory muscle strength as demonstrated by reduced PImax, which is consistent with recently reported findings of fibrotic diaphragm remodeling in patients who died due to COVID-19-related ARDS [10].
Elevated P0.1, as found in the majority of our patients, is strongly associated with heightened dyspnea perception [11]. This was also the case in our cohort, as shown by elevated BORG-CR scores and everyday activity, productivity and COVID-related functional impairment (PCFS). Strikingly, this was not only the case in hospitalized patients where elevated P0.1 might be a consequence of reduced inspiratory muscle strength PImax but also in nonhospitalized patients.
Therefore, our data support that, pathophysiologically, elevated P0.1 might be a function of exercise-induced deoxygenation in convalescent, persistently symptomatic COVID-19 patients. While pulmonary thromboembolic disease was not detected by V/Q scan (as described above), six patients showed signs of ground-glass opacity and (mostly minor) fibrotic changes and exercise-induced deoxygenation was associated with lower DLCO (Fig. 1J). Systematic analysis of these changes, however, was out of the scope of the present study, which is a limitation. Additionally, due to unavailability of data in some patients, we cannot exclude pre-existing changes in respiratory drive and effort sustained from before SARS-CoV-2 infection. Additional limitations include putatively biased patient selection, as most patients reported to our OPD with persistent symptoms after COVID-19, with very few patients referred for routine follow-up after COVID-19. Patients and staff were also not blinded to the overall testing, possibly inserting additional bias in the measurement as does lack of historical PFT data. Particularly for ICU patients, muscular deconditioning associated with intensive care might contribute to respiratory muscle impairment. Although it was not possible to differentiate inspiratory muscle impairment from generalized muscle weakness or postinfection myopathy, in our cohort, creatine kinase and myoglobin serum levels did not differ between patients with normal or abnormal respiratory muscle function (p = 0.202 and p = 0.075, respectively). In addition, pre-existing conditions/comorbidities did not correlate with abnormal respiratory muscle function in our cohort. Also, inspiratory muscle weakness also occurred frequently in nonhospitalized patients (65%). We also cannot specifically attribute the detected changes in respiratory drive and inspiratory muscle function to SARS-CoV-2, as we cannot rule out a general effect of viral infections. Regardless of SARS-CoV-2 specificity, the high prevalence in our pilot study points toward a relevant healthcare burden given the pandemic nature of COVID-19.
As there is strong evidence that chronic fatigue syndrome (CFS) is associated with COVID-19 [3, 5], it is compelling to speculate to what extent heightened neuroventilatory activity, as documented by P0.1 in our cohort, contributes to COVID-19-CFS. Particularly, the inability to adequately increase respiratory effort upon increased respiratory drive is known to worsen respiratory distress [11]. Therefore, more invasive techniques such as twitch interpolation might help to further characterize dysregulation of respiratory drive and effort in Long COVID patients.
Conclusion
We were able to detect increased respiratory drive as well as inspiratory muscle dysfunction in persistently symptomatic patients approx. 5 months after COVID-19. Notwithstanding the small sample size, our findings reveal a previously unidentified neuromuscular component of COVID-19 sequelae.
Given the wide accessibility of respiratory muscle testing as a relatively low-cost approach (in particular in comparison with imaging and immunological laboratory studies), we strongly advocate for systematic respiratory muscle testing in the diagnostic workup of persistently symptomatic, convalescent COVID-19 (Long COVID) patients.
Acknowledgements
JKH is part of the Clinician Scientist Career Development Program of the University of Hamburg/University Medical Center Hamburg-Eppendorf.
Abbreviations
- ARDS
Acute respiratory distress syndrome
- BMI
Body-Mass-Index
- CBG
Capillary blood gas
- Δ
Difference between rest and exercise
- CR
Category ratio
- Dx
Diagnosis
- DLCO
Diffusion capacity for carbon monoxide
- FEV1
Forced expiratory volume in 1 s
- FRC
Functional residual capacity
- FVC
Forced vital capacity
- IQR
Inter-Quartile Range
- P0.1
Airway occlusion pressure at 100 ms
- PImax
Maximum inspiratory mouth pressure
- PImaxpeak RV
Peak value of maximum inspiratory mouth pressure measured from residual volume
- PCFS
Post-COVID-19 functional status
- PFT
Pulmonary Function Test
- RV
Residual volume
- 6MWT
6-Minute walk test
- 6MWD
6-Minute walking distance
- TLC
Total lung capacity
- WPAI
Work Productivity and Activity Index
Author contributions
Conceptualization, oversight and design: JKH, SK, HK; data acquisition: JKH, MH, AH, TO, MS, SS, JSzW; contribution of data/analysis tools: LH, JK, MMA, HK; data analysis: JKH, MH, TO. Writing of manuscript: JKH. All authors read and approved the manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL. This work received no specific funding.
Availability of data and materials
Data analyzed during this study are available from the corresponding authors upon reasonable request.
Declarations
Conflict of interests
The authors declare no competing interests.
Ethics approval
The ethics committee of the Hamburg Chamber of Physicians (Hamburger Ärztekammer) approved the data collection (PV7298 and PV7343).
Consent to participate
Informed consent was obtained from the participants.
References
- 1.Wichmann D, Sperhake JP, Lutgehetmann M, Steurer S, Edler C, Heinemann A, Heinrich F, Mushumba H, Kniep I, Schroder AS, et al. Autopsy findings and venous thromboembolism in patients with COVID-19: a prospective cohort study. Ann Intern Med. 2020;173:268–277. doi: 10.7326/M20-2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Puelles VG, Lutgehetmann M, Lindenmeyer MT, Sperhake JP, Wong MN, Allweiss L, Chilla S, Heinemann A, Wanner N, Liu S, et al. Multiorgan and renal tropism of SARS-CoV-2. N Engl J Med. 2020;383:590–592. doi: 10.1056/NEJMc2011400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sudre CH, Murray B, Varsavsky T, Graham MS, Penfold RS, Bowyer RC, Pujol JC, Klaser K, Antonelli M, Canas LS, et al. Attributes and predictors of long COVID. Nat Med. 2021;27:626–631. doi: 10.1038/s41591-021-01292-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hennigs JK, Oqueka T, Harbaum L, Klose H. Organ-specific sequelae of COVID-19 in adults. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2022;65:462–470. doi: 10.1007/s00103-022-03513-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, Kang L, Guo L, Liu M, Zhou X, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397:220–232. doi: 10.1016/S0140-6736(20)32656-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lam GY, Befus AD, Damant RW, Ferrara G, Fuhr DP, Stickland MK, Varughese RA, Wong EY, Smith MP. Exertional intolerance and dyspnea with preserved lung function: an emerging long COVID phenotype? Respir Res. 2021;22:222. doi: 10.1186/s12931-021-01814-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Laveneziana P, Albuquerque A, Aliverti A, Babb T, Barreiro E, Dres M, Dube BP, Fauroux B, Gea J, Guenette JA, et al. ERS statement on respiratory muscle testing at rest and during exercise. Eur Respir J. 2019 doi: 10.1183/13993003.01214-2018. [DOI] [PubMed] [Google Scholar]
- 8.Kabitz HJ, Windisch W. Respiratory muscle testing: state of the art. Pneumologie. 2007;61:582–587. doi: 10.1055/s-2007-980080. [DOI] [PubMed] [Google Scholar]
- 9.Klok FA, Boon G, Barco S, Endres M, Geelhoed JJM, Knauss S, Rezek SA, Spruit MA, Vehreschild J, Siegerink B. The post-COVID-19 functional status scale: a tool to measure functional status over time after COVID-19. Eur Respir J. 2020 doi: 10.1183/13993003.01494-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shi Z, de Vries HJ, Vlaar APJ, van der Hoeven J, Boon RA, Heunks LMA, Ottenheijm CAC. Dutch C-DI: diaphragm pathology in critically ill patients with COVID-19 and postmortem findings from 3 medical centers. JAMA Intern Med. 2020 doi: 10.1001/jamainternmed.2020.6278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Parshall MB, Schwartzstein RM, Adams L, Banzett RB, Manning HL, Bourbeau J, Calverley PM, Gift AG, Harver A, Lareau SC, et al. An official American Thoracic Society statement: update on the mechanisms, assessment, and management of dyspnea. Am J Respir Crit Care Med. 2012;185:435–452. doi: 10.1164/rccm.201111-2042ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data analyzed during this study are available from the corresponding authors upon reasonable request.