Abstract
Objective
The objective of this study is to determine the linkage between multidimensional structural racism typologies and preterm birth (PTB), low birthweight (LBW), and small‐for‐gestational‐age (SGA) birth among infants of White, US‐born Black, and foreign‐born Black pregnant people in Minnesota.
Data Sources
The measures of structural racism were based on the 2017 American Community Survey 5‐year estimates and the 2017 jail incarceration data from the Vera Institute of Justice. Birth outcomes of infants born in 2018 were based on birth records from the Minnesota Department of Health.
Study Design
We conducted a latent class analysis to identify multidimensional structural racism typologies in 2017 and related these typologies to birth outcomes of pregnant people who gave birth in Minnesota in 2018 using Vermunt's 3‐step approach. Racial group‐specific age‐adjusted risks of PTB, LBW, and SGA by structural racism typologies were estimated.
Data Collection
Study data were from public sources.
Principal Findings
Our analysis identified three multidimensional structural racism typologies in Minnesota in 2017. These typologies can have high structural racism in some dimensions but low in others. The interactive patterns among various dimensions cannot simply be classified as “high” (i.e., high structural racism in all dimensions), “medium,” or “low.” The risks of PTB, LBW, and SGA for US‐born Black pregnant Minnesotans were always higher than for their White counterparts regardless of the typologies in which they lived during pregnancy. Furthermore, these excess risks among US‐born Black pregnant people did not vary significantly across the typologies. We did not find clear patterns when comparing the predicted risks for infants of US‐ and foreign‐born Black pregnant people.
Conclusion
Multidimensional structural racism increases the risks of adverse birth outcomes for US‐born Black Minnesotans. Policy interventions to dismantle structural racism and eliminate birth inequities must be multi‐sectoral as changes in one or a few dimensions, but not all, will unlikely reduce birth inequities.
Keywords: birth outcomes, latent construct, measurement, racial inequities, structural racism
What is known on this topic
Structural racism is a multidimensional system driving inequities in various sectors (e.g., education, labor market, housing, public safety, etc.).
Residence in areas with high structural racism is associated with adverse birth outcomes for US‐born Black pregnant people.
The association between each dimension of structural racism and poor health is often examined independently; the multidimensional effect is difficult to examine.
What this study adds
Structural racism is conceptualized as a multidimensional latent construct; a latent class analysis is used to identify multidimensional structural racism typologies.
Multidimensional structural racism explains birth inequities between US‐born Black pregnant people and their White counterparts.
Policy solutions to dismantle structural racism and eliminate birth inequities must be multi‐sectoral.
1. INTRODUCTION
Racial inequities in birth outcomes, particularly those between White and United States (US)‐born Black pregnant people, have persisted for as long as the data have been collected. In Minnesota, where the overall incidences of adverse birth outcomes are much lower than other states, 1 11.5% of singletons born to US‐born Black pregnant people in 2018 were preterm (born before 37 weeks of gestation; PTB), 11.5% were low birthweight (lower than 2500 g; LBW), and 20.7% were small for their gestational age (birthweight below the 10th percentile for their gestational age; SGA). These rates are approximately double those seen among infants born to White pregnant people in the state. 2 Infants with these conditions are at elevated risk of infant mortality or a lifetime of poor health, limited life chances, and the risk of transmitting the same conditions to their offspring. 3 , 4 , 5 , 6
In the past decade, scholars and policymakers have increasingly sought to understand the upstream (systemic and structural) factors that have contributed to the disproportionate risk Black pregnant people experience during pregnancy and childbirth. 7 Structural racism—carefully designed “macro‐level systems, social forces, institutions, ideologies, and processes that interact with one another to generate and reinforce inequities among racial and ethnic groups” 8 that are present in all facets of our lives—has been identified as a critical determinant of adverse birth outcomes for Black pregnant people. 7 Historically, as a fundamental cause of health inequities, 9 structural racism is not only killing Black men and women; it is also killing their infants. In fact, in Minnesota, Black infants are twice as likely to die in their first year of life compared to their White counterparts. 10 Living in areas with high structural racism is associated with adverse birth outcomes and infant mortality for Black pregnant people. 11 , 12 , 13 , 14 , 15 , 16 , 17 One study also suggests that this same effect can be seen among infants born to White pregnant people. 17
Understanding the connection between structural racism and adverse birth outcomes continues to be an active area of research, with an increasing number of scholars calling for rigorous and theory‐driven approaches to operationalize and measure structural racism. 18 , 19 , 20 , 21 , 22 Building on important groundwork which has operationalized and measured residential segregation as a form of structural racism, 16 , 19 , 23 , 24 , 25 scholars now also measure other forms of structural racism (e.g., racial inequities in political participation, employment, education, income, homeownership, and judicial treatment) 19 —all of which have been linked to adverse birth outcomes in US cohorts. 11 , 12 , 13 , 14 , 15 , 16 , 17 However, the deleterious effects of each dimension are often examined independently. Structural racism is a multidimensional determinant of health, where various dimensions may share the same pathway (e.g., education inequity leads to employment inequity) or interact with one another (e.g., education inequity among residents in racially segregated neighborhoods) to generate joint effects on health. 21 , 26 , 27 Several theoretical frameworks over the years have offered a foundational grounding of the ways in which dimensions of structural racism intersect. 28 , 29 Yet, there has been limited effort to address how these dimensions interact or to characterize their potential reinforcing effects on birth inequities and other health outcomes.
A key barrier to studying structural racism as a multidimensional determinant of health is the challenge of studying highly correlated dimensions of structural racism together as a system. Using a common practice of evaluating the independent effect of each dimension of structural racism and their interactive effects with n‐way interaction terms separately will result in biased effect estimation. 30 While a biased estimate with a similar effect direction as the true estimate but different effect size may lead to erroneous power calculation in future studies and/or miscalculation of intervention effectiveness, concluding a null result for what genuinely is a significant causal relationship can misguide future research and policies for generations. Recent cross‐disciplinary collaborations have proposed using latent‐construct approaches to overcome this methodological hurdle. 21 , 22 , 27 , 31 The latent‐construct approaches assume collinearity among unidimensional structural racism measures. The latent‐class models identify multidimensional structural racism typologies, integrating the independent and reinforcing effects of various dimensions. When used to study population health patterns, the multidimensional structural racism typologies can provide additional information compared to fitting multiple unidimensional measures together in regression models. 21
Characterizing the potential reinforcing effects of dimensions of structural racism on birth inequities is important for tailoring policy interventions and filling in a critical gap in the literature. Understanding the interconnection between dimensions of structural racism and how this hard‐to‐quantify force affects health outcomes may also shed light on why birth inequities continue to persist despite increasing policy efforts to address social determinants of health. 32 Thus, the objective of our study is to apply a latent‐class model to determine the linkage between multidimensional structural racism typologies and the risks of PTB, LBW, and SGA for infants born to White, US‐born Black, and foreign‐born Black pregnant Minnesotans. Specifically, we aimed to answer two questions:
Do the risks of PTB, LBW, and SGA for White, US‐born Black, and foreign‐born Black pregnant people exposed to the same structural racism typology (i.e., residence in an area with the same pattern of structural racism) differ?
Do the risks of PTB, LBW, and SGA differ for people of the same racial background in different structural racism typologies?
2. METHODS
2.1. Data and study population
We used birth records of singletons born to White and Black pregnant people in 2018 from the Minnesota Department of Health. Because Minnesota is home to one of the largest Black immigrant populations in the US, together with the heterogeneity in the experience of structural racism, culture, and health status between US‐ and foreign‐born Black people, 33 we distinguished Black pregnant people into two groups in our study. We geocoded the address on the birth records to assign area‐based measures of structural racism (described later); only the records that could be assigned an address point or a street address were used in our analysis. The final sample included 40,875 infants of White (3.4% excluded), 2,782 of US‐born Black (4.4% excluded), and 4,648 of foreign‐born Black pregnant people (5.7% excluded).
2.2. Measurement
2.2.1. Structural racism
We adapted the latent‐class method proposed by Chantarat et al. (2021) to derive multidimensional structural racism typologies. 21 This method consists of two steps.
First, we measured structural racism in six domains for all Public Use Microdata Areas (PUMAs) in the US: (1) Black‐White residential segregation, (2) Black‐White educational inequity, (3) Black‐White employment inequity, (4) Black‐White income inequity, (5) Black‐White homeownership inequity, and (6) Black‐White criminal justice inequity. We used the data from the 2017 American Community Survey (ACS) 5‐year estimates 34 to derive measures (1) to (5) and the 2017 jail incarceration data from the Vera Institute of Justice for measure (6). 35 Detailed discussion of these validated measures is available in Supplement S1. Compared to state‐ or county‐level measures commonly seen in the structural racism literature, the PUMA‐level measures likely capture the heterogeneity of structural racism better, especially for densely populated areas (e.g., the two‐county Minneapolis‐Saint Paul area consists of 14 PUMAs). 21 All measures were dichotomized to high or low structural racism at the national median. We subsequently merged these measures with the birth records based on their geocoded PUMA (43 PUMAs in Minnesota).
Second, we conducted latent class analysis (LCA) to identify the structural racism typologies based on the six aforementioned structural racism measures. We specified our models to identify two to six typologies, not exceeding the number of measures included. The best‐fitted model was selected based on three criteria: model parsimony (based on Bayesian Information Criteria [BIC]; the lower value indicates more parsimonious), model clustering (based on standardized entropy ranging from 0 to 1; the value closer to 1 indicates that the typologies the model identified are more distinct from one another), and relative size of typologies (models with all typologies larger than 10% of the sample are preferred). 36 When these criteria suggested models with a different number of typologies, we selected a smaller number of typologies for ease of interpretation and preventing small cell count issues in regression analyses.
To understand the areal sociodemographic context of the structural racism typologies from the LCA, we calculated the median and interquartile range of PUMA‐level percentages of White population, Black population, population of other races, foreign‐born population, population 16 years and older in the labor force, and household income with the 2017 ACS data.
2.2.2. Birth outcomes
Based on their birth records, infants born before 37 weeks of gestation were considered PTB. 1 Infants whose birthweight was lower than 2500 g were considered LBW. 1 Infants whose birthweight was lower than the 10th percentile 37 among infants born in Minnesota of the same gestational age in 2018 were considered SGA.
2.2.3. Other covariates
We extracted pregnant people's age from the birth records. We also extracted marital status, parity, prenatal care use, primary payer, and diagnoses of health conditions associated with adverse birth outcomes from birth records. Except for age, these covariates were not used in our regression model because they are mediators in the relationship between structural racism and adverse birth outcomes 38 ; including such covariates in the regression model would have biased the estimates to the null. 39 This information is available in Supplement S3 for reference.
2.3. Statistical analysis
First, we compared the areal sociodemographic characteristics across structural racism typologies using the Kruskal–Wallis test. Second, we compared the proportion of pregnant people in each structural racism typology and incidence of PTB, LBW, and SGA by racial group using Pearson's chi‐square test. Third, we related structural racism typology to the risks of PTB, LBW, and SGA using Vermunt's “3‐step approach,” wherein steps 1 and 2 are latent class model fitting and assigning each pregnant person to the most likely structural racism typology (described earlier), and step 3 is relating the structural racism typology to the risks of PTB, LBW, and SGA using racial group‐stratified logistic regression. This approach adjusts for potential misclassification from the use of modal typology assignments. 40 Finally, we calculated the age‐adjusted predicted risks with 95% confidence intervals of PTB, LBW, and SGA for pregnant people by racial group and structural racism typology. We chose not to calculate relative risks because the interaction between dimensions of structural racism will likely not create an apparent “low” typology (i.e., PUMAs with low structural racism on all dimensions), which would have been the most appropriate reference group. 21 Instead, we compared the typology‐specific estimates to understand racial group differences (our first research question) and compared the racial group‐specific estimates to understand the extent to which residence in various typologies contribute to difference risks for a particular racial group (our second research question).
The protocol for this study was reviewed and determined to be non‐human subjects' research by the University of Minnesota Institutional Review Board. Geocoding was conducted in ArcGIS version 10.6.1. LCA and relating typology to birth outcomes were conducted in Mplus version 8.6. The rest of the analyses were conducted in R version 4.0.3.
3. RESULTS
3.1. Birth inequities
In 2018, infants of US‐born Black pregnant people were more likely to be PTB, LBW, and SGA than White infants and foreign‐born Black pregnant people (see Supplement S3). Specifically, the incidence seen among infants of US‐born Black pregnant people (12.2% PTB, 13.3% LBW, and 19.6% SGA) was approximately two to three times the incidence seen among infants of White (6.6% PTB, 4.2% LBW, 7.5% SGA) and foreign‐born Black pregnant people (5.7% PTB, 5.9% LBW, 14.5% SGA).
3.2. Structural racism typologies
The most parsimonious latent class model identified three completely distinct (standardized entropy equal to 1) structural racism typologies in Minnesota (see Supplement S2 for model fit statistics). Figure 1 shows the probabilities that levels of structural racism for the six domains of interest are greater than the national median (“high”) for these three structural racism typologies. Type A PUMAs have high education, income, and criminal justice inequities, and moderately high residential segregation and homeownership inequity, but low employment inequity. Type B PUMAs have high education, employment, and homeownership inequities, but moderately high levels of residential segregation, income, and criminal justice inequities. Lastly, Type C PUMAs have high income inequity, are moderately high on residential segregation, and employment, homeownership, and criminal justice inequities, but are low on education inequity.
FIGURE 1.
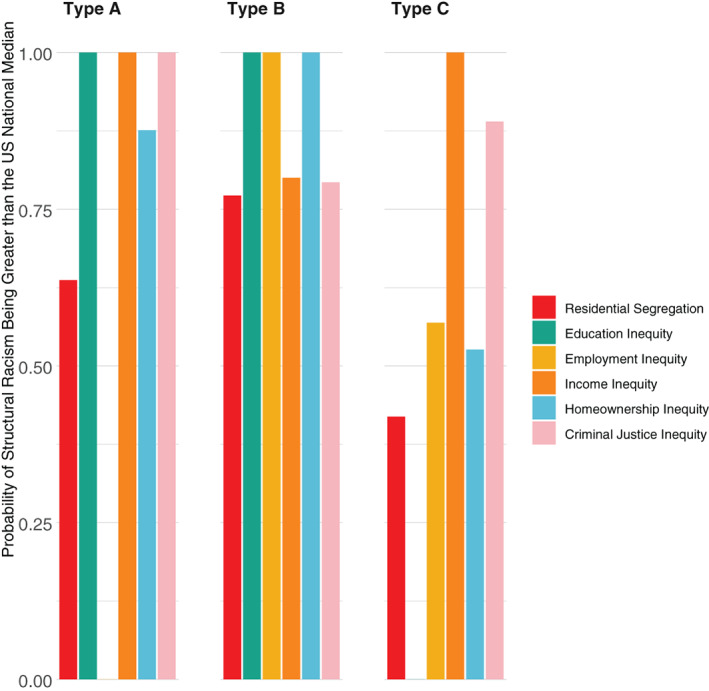
Structural racism typologies in Minnesota, 2017. Missing of bars for any particular structural racism dimension indicates a zero probability for that particular dimension being higher than the U.S. national median [Color figure can be viewed at wileyonlinelibrary.com]
Figure 2 shows the geographic distribution of the three structural racism typologies in Minnesota, and Table 1 shows their areal sociodemographic characteristics. The median household income for Type C PUMAs was $79,632, significantly higher than the median household income in Type A PUMAs ($74,608, p < 0.05) and Type B PUMAs ($60,607, p < 0.05). The racial and ethnic compositions for the three typologies are relatively similar, except that the median percentage of the Black population in the Type B PUMAs (5.9%) was significantly higher than in Type C PUMAs (2.9%, p < 0.05).
FIGURE 2.
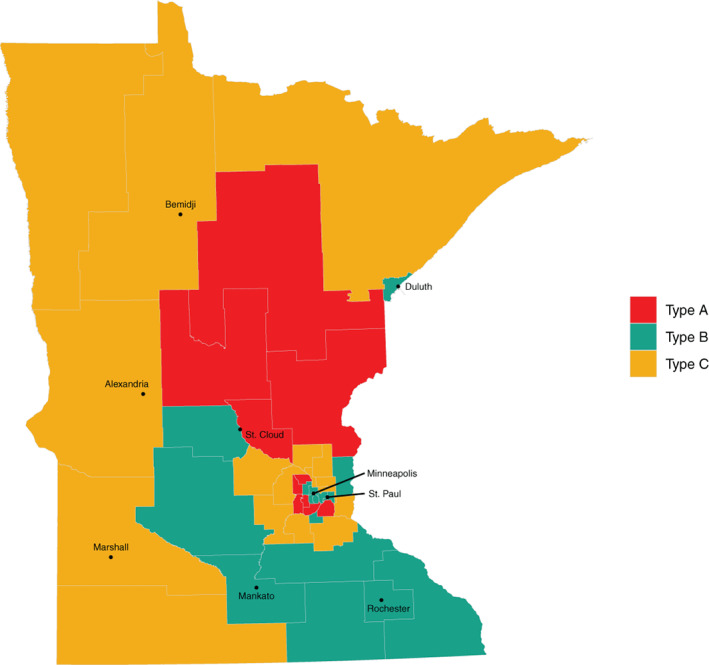
Geographic distribution of structural racism typologies in Minnesota, 2017. Type A: high education, income, and criminal justice inequities, and moderately high residential segregation and homeownership inequity, but low employment inequity. Type B: high education, employment, and homeownership inequities, but moderately high level of residential segregation, income, and criminal justice inequities. Type C: high income inequity, moderately high on residential segregation, and employment, homeownership, and criminal justice inequities, but low education inequity [Color figure can be viewed at wileyonlinelibrary.com]
TABLE 1.
Sociodemographic characteristics of PUMAs in each structural racism typology
| Type A | Type B | Type C | ||||
|---|---|---|---|---|---|---|
| (n = 10) | (n = 16) | (n = 17) | ||||
| Median | IQR | Median | IQR | Median | IQR | |
| % White population | 81.8 | (11.7) | 86.5 | (24.1) | 90.8 | (9.2) |
| % Black population c | 5.5 | (6.0) | 5.9 | (13.1) | 2.4 | (2.9) |
| % Population of other racial groups | 14.1 | (9.3) | 11.5 | (11.8) | 9.1 | (7.0) |
| % Foreign‐born population | 11.5 | (11.4) | 8.8 | (9.8) | 5.5 | (5.5) |
| % Population 16 years and older in labor force | 71.2 | (6.3) | 70.5 | (3.4) | 70.5 | (6.6) |
| Median household income a , b | 74,608.0 | (11,393.3) | 60,607.0 | (7891.3) | 79,632.0 | (38,207.0) |
Note: Type A: high education, income, and criminal justice inequities, and moderately high residential segregation and homeownership inequity, but low employment inequity. Type B: high education, employment, and homeownership inequities, but moderately high level of residential segregation, income, and criminal justice inequities. Type C: high income inequity, moderately high on residential segregation, and employment, homeownership, and criminal justice inequities, but low education inequity. Unit of analysis is PUMA (n = 10 for Type A, n = 16 for Type B, n = 17 for Type C). The Kruskal–Wallis test was used for the comparison of median.
Abbreviation: IQR, interquartile range.
Significant difference at p < 0.05 between Type A and Type B.
Significant difference at p < 0.05 between Type A and Type C.
Significant difference at p < 0.05 between Type B and Type C.
3.3. Predicted risks of PTB, LBW, and SGA
The age‐adjusted risk of PTB for infants of US‐born Black pregnant people are 0.12 (CI: 0.09–0.16) if they reside in Type A PUMA, 0.16 (CI: 0.13–0.19) in Type B PUMA, and 0.13 (CI: 0.10–0.16) (Figure 3). These predicted risks were significantly higher than the estimates for White (Type A: 0.08, CI: 0.07–0.09; Type B: 0.08, CI: 0.07–0.08; Type C: 0.08, CI: 0.07–0.09) and for foreign‐born Black pregnant people in the same typology (Type A: 0.07, CI: 0.05–0.09; Type B: 0.06, CI: 0.05–0.07; Type C: 0.07, CI: 0.06–0.09).
FIGURE 3.
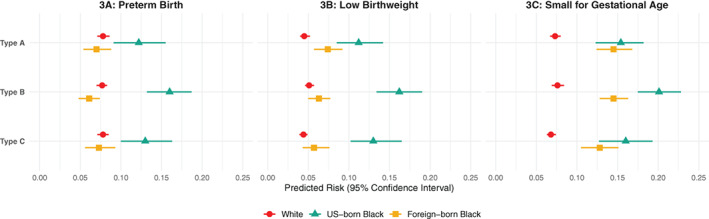
Age‐adjusted predicted risks of preterm birth, low birthweight, and small‐for‐gestational‐age birth for infants of White, US‐born Black, and foreign‐born Black pregnant people by structural racism typology. This figure compares predicted risks of preterm birth (A), low birthweight birth (B), and small‐for‐gestational‐age birth (C) for infants of White (red circle), US‐born Black (green triangle), and foreign‐born Black pregnant people (yellow square). The lines in this figure symbolize 95% confident intervals; overlapping of any lines indicate that the predicted risks are not statistically significant from each other. Type A: high education, income, and criminal justice inequities, and moderately high residential segregation and homeownership inequity, but low employment inequity. Type B: high education, employment, and homeownership inequities, but moderately high level of residential segregation, income, and criminal justice inequities. Type C: high income inequity, moderately high on residential segregation, and employment, homeownership, and criminal justice inequities, but low education inequity [Color figure can be viewed at wileyonlinelibrary.com]
For LBW, the predicted risks for infants of US‐born Black pregnant people (Type A: 0.11, CI: 0.09–0.14; Type B: 0.16, CI: 0.13–0.19; Type C: 0.13, CI: 0.10–0.17) were significantly higher for infants of White pregnant people in all typologies (Type A: 0.05, CI: 0.04–0.05; Type B: 0.05, CI: 0.05–0.06; Type C: 0.04, CI: 0.04–0.05), but not significantly higher for foreign‐born Black pregnant people in Type A PUMA (0.07, CI: 0.06–0.09).
For SGA, only the predicted risk for infants of US‐born Black pregnant people in Type B (0.20, CI: 0.18–0.23) was significantly higher than infants of foreign‐born Black pregnant people (0.15, CI: 0.13–0.16), but was similar for the other two typologies. The predicted risks of SGA for infants of White pregnant people (Type A: 0.07, CI: 0.07–0.08; Type B: 0.08, CI: 0.07–0.08; Type C: 0.07, CI: 0.06–0.07) were significantly lower than the risks for infants of US‐ and foreign‐born Black pregnant people.
3.4. Post hoc analysis
The six‐typology model was more parsimonious (lower BIC) than the selected three‐typology model, but the relative sizes of three of the six typologies were less than 10% of the cohort. For sensitivity, we related typologies from the six‐typology model to the risks of PTB and SGA (see Supplement S4). The age‐adjusted risk could not be calculated for LBW because the algorithm did not converge due to zero cell counts in the three small typologies. For PTB and SGA, we observed higher predicted risks for infants of US‐born Black than of White pregnant people in Type C and Type D PUMAs. These two typologies are likely the same as Type B and Type C in the three‐typology model.
4. DISCUSSION
Progress toward birth equity cannot be achieved if scholars and policymakers do not understand the extent to which the upstream social inequities deliberately designed and upheld by White supremacy explain and perpetuate birth inequities. Our study aimed to fill a significant and pervasive gap in the literature—how do we study the health impacts of structural racism as a multidimensional determinant of health? Furthermore, our ability to measure how structural racism affects birth outcomes has limited our ability to intervene in ways that have the greatest impact. Leveraging a latent‐class modeling approach, results from our study offer an even direr picture of structural racism as a fundamental cause of birth inequities but also new insight into how measuring the multidimensionality of structural racism is important.
First, we identified three structural racism typologies in Minnesota in 2017. When looking at structural racism as a multidimensional system, we found that the interactive patterns among various dimensions cannot simply be classified as “high” (i.e., high structural racism in all dimensions), “medium,” or “low.” For example, while Type A PUMAs have high education, income, and criminal justice inequities, employment inequity was low for this typology. However, for Type B PUMAs, where employment inequity was high, we observed only moderately high levels of income and criminal justice inequities. Such intricate interactions among various dimensions of structural racism have not been examined within the large majority of existing research. 11 , 13 , 14 , 15 , 16 , 17 One exception is Wallace et al. (2015), who examined the interaction between income inequity (measured with the Gini coefficient) and employment, education, and incarceration inequities (i.e., 3 two‐way interaction terms). 12 Setting aside the risk of biased effect estimation when putting several highly correlated variables together in regressions, results interpretation from higher‐level interaction terms (e.g., six‐way interaction for six dimensions) become much more difficult and have limited policy utility. While our study did not focus on the mechanism underlying the interaction between various dimensions of structural racism, we demonstrated that the LCA could help identify these unique interactive patterns and, hopefully, motivate future research to study their mechanistic relationships rigorously.
Second, we found that the age‐adjusted risks for PTB, LBW, and SGA for infants born to US‐born Black pregnant people are significantly higher than the risks for those born to White pregnant people, regardless of the structural racism typology in which their birthing parent resides. This finding is not surprising as several previous studies have shown that despite living in high structural racism areas, White people are not negatively affected by structural racism, but US‐born Black people become more vulnerable to poor health either through experiencing barriers in access to health‐promoting resources (mediated relationship) 9 and/or because their bodies become “weathered” (chronic wear and tear due to stress) as a result of cumulative exposure to racism across the life course. 41 Because we operationalized and measured structural racism as a multidimensional determinant of health and the LCA did not identify the apparent “low/absence” of structural racism, our results cannot be used as evidence to support or contradict the claim that White people may accrue health benefits from structural racism. 42
While inequities in birth outcomes between White and US‐born Black pregnant people are clear, we did not find clear patterns when comparing the predicted risks for infants of US‐ and foreign‐born Black pregnant people. Specifically, the predicted risk of PTB for infants of US‐born Black pregnant people is higher in all structural racism typologies. Similarly, the risk of LBW is significantly higher for infants of US‐ than foreign‐born Black pregnant people who reside in Type B and C PUMAs, while a significant difference in the risk of SGA was observed between these two groups who reside in Type B PUMAs. Unlike other foreign‐born Black people in the US that migrated to the US in the 1990s after the passage of the 1986 Immigration Act that allowed high‐skill immigrants to gain legal residency, 33 a large proportion of the foreign‐born Black people in Minnesota are either refugees from war‐torn Somalia or their descendants. Understanding the reason for migration is essential in understanding the Black “healthy immigrant” effects. The selection theory, which attributes better health among immigrants to the fact that only healthy immigrants will migrate/can endure the migration process, is less applicable for foreign‐born Black people in Minnesota. While the inconsistent pattern of inequities in risks of adverse birth outcomes found in our study may result from a small sample size, hence large standard errors, two countervailing forces may also explain our results. While the immigrant enclave effects (Minnesota is the largest settlement for Somalians outside of Somalia) protect foreign‐born Black people against poor health, 43 the increase of anti‐immigrant, anti‐Muslim rhetoric prevalent in Minnesota may be an additional source of stress that harms health similarly to structural racism. 44 Future investigation with a larger sample size and detailed immigration history may help settle this debate.
Third, we found that the predicted risks of PTB, LBW, and SGA for infants of US‐born Black pregnant people are, in general, the same regardless of structural racism typology in which those who gave birth to them lived during pregnancy. Creating an environment where US‐born Black people live, learn, work, play and have the health trajectories on a par with their White counterparts will require dismantling the whole system, not one dimension of structural racism at a time. This finding contradicts most previous studies that measured various dimensions of structural racism but did not examine the multidimensionality. 11 , 13 , 14 , 15 , 16 , 17 For example, studies that examined the linkage between education inequity and the increased risk of SGA 12 generally suggest that the elimination of racist policies and practices that disadvantage Black students from accessing higher education relative to their White peers will contribute to the elimination of racial inequity in SGA. 12 Relating that recommendation to our study context, however, transforming Type A or B PUMAs (high education inequity) to Type C PUMAs (low education inequity) will unlikely eliminate the SGA inequity; instead, it simply shifts from one deleterious mechanism to another. While focused policy recommendations may result from studies that consider only one or a few dimensions of structural racism, these recommendations may be undermined by the interplay among these and other dimensions of structural racism.
Our findings that the intricate interactions among dimensions of structural racism are associated with higher risks of adverse birth outcomes for US‐born Black pregnant people call for future studies to treat structural racism as a multidimensional determinant of health. Future studies should also examine how various dimensions of structural racism interact in addition to identifying the patterns like in the current study, to better inform the design of policy intervention to dismantle structural racism and eliminate health inequities. Additionally, since the national reckoning of the deadly effects of structural racism on Black people's lives may lead to change in patterns of structural racism, we encourage other scholars to use more recent data to examine transitions in structural racism over time and evaluate how such transitions (or lack thereof) result in the change of population health trends for Black populations.
4.1. Implications
Structural racism is a multidimensional determinant of health; therefore, our approach to policy solutions must lead with this in mind. Indeed, a policy solution to closing a gap in one dimension of structural racism at best may be effective while simultaneously failing to have the fully intended impact given the multiple other dimensions of structural racism at play. At worst, there is potential for a single policy solution to exacerbate inequity in different dimensions without fully understanding its role in multidimensionality. Our findings that there is no “high,” “medium,” or “low” structural racism, instead uniquely intricate interactions across the dimensions, call for policies enacted to close racial gaps in birth outcomes to seek to address all dimensions of structural racism. One way to do this is through a comprehensive reparations bill that acknowledges the historical context of structural racism and White supremacy in the US and offers a comprehensive set of policy solutions that address all dimensions of structural racism and inequities (or as many as possible) to level the playing field for generations to come.
4.2. Limitations
Our study has several limitations. We used the time‐lag cross‐sectional design for this study, wherein the structural racism measures (explanatory variables) were derived with the 2017 ACS data, and the birth outcomes (outcome variables) were from 2018. Because the people who give birth in 2018 may not reside at the same address or in the same PUMA during pregnancy, misclassification of structural racism typology was possible. Our study also used birth data from only 1 year from a White‐majority state where the population of foreign‐born Black people is larger than US‐born Black people, which may limit the generalizability of our findings. Future studies should incorporate the life‐course framework to examine the linkage between exposure to structural racism in early life and birth inequities of reproductive‐age people using multi‐state and/or longitudinal data.
5. CONCLUSION
Our findings call for careful consideration for how Minnesota policymakers design and implement health and social policies. Specifically, our findings suggest that dismantling structural racism requires dismantling the whole system, not one dimension of structural racism at a time. Failing to understand the multidimensionality of structural racism will result in a piecemeal approach to policymaking that fails to analyze how the dimensions of structural racism are intertwined critically. Findings from this study offer important implications for the next steps in creating policies that create equity.
A concerted effort to specifically address the issues of structural racism and to uncover and change the structures shaped by racism is necessary to achieve health equity in communities across Minnesota which, while often ranked as the healthiest state in the nation, suffer from some of the worst health inequities in the country. We have identified three multidimensional structural racism typologies in Minnesota, and none of them are safe for US‐born Black pregnant people. Given the persistent inequities in infant outcomes for Black pregnant people, understanding the intricate reinforcing dimensions of structural racism that contribute to these outcomes is critical for achieving health equities. Our findings are a first step on the path in considering solutions to birth inequities in Minnesota that take into consideration the totality of ways in which societies foster racial discrimination through mutually reinforcing systems.
Supporting information
Supplement S1. Description of unidimensional structural racism measures used to derive the multidimensional structural racism typologies.
Supplement S2: Latent class model enumeration, fit statistics, and relative size of typologies.
Supplement S3: Demographic characteristics, downstream determinants, and birth outcomes of White, US‐born Black, and foreign‐born Black people giving birth in Minnesota, 2018.
Supplement S4: Post hoc analysis.
ACKNOWLEDGMENTS
This project was funded by the Robert J. Jones Urban Research and Outreach‐Engagement Center, University of Minnesota. Additional support was provided by the Minnesota Population Center which is funded by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (Grant P2C HD041023). All funders have no involvement in the design, data analysis, interpretation of the study results, drafting of the manuscript, or the decision to submit this paper for publication. The authors would like to thank Miamon Queeglay and Alyssa Fritz for their help with project management and background literature search.
Chantarat T, Van Riper DC, Hardeman RR. Multidimensional structural racism predicts birth outcomes for Black and White Minnesotans. Health Serv Res. 2022;57(3):448‐457. doi: 10.1111/1475-6773.13976
See related debate‐commentary by Brown et al.
Funding information Eunice Kennedy Shriver National Institute of Child Health and Human Development, Grant/Award Number: P2C HD041023; Robert J. Jones Urban Research and Outreach‐Engagement Center, University of Minnesota
REFERENCES
- 1. Martin JA, Hamilton BE, Osterman MJK, Driscoll AK. Births: final data for 2018. Natl Vital Stat Rep. 2019;68(13):1‐47. [PubMed] [Google Scholar]
- 2. Office of the Vital Records MD of H. Birth Outcome Data. 2021.
- 3. Schwartz GL, Leifheit KM, Berkman LF, Chen JT, Arcaya MC. Health selection into eviction: adverse birth outcomes and children's risk of eviction through age 5 years. Am J Epidemiol. 2021;190(7):1260‐1269. doi: 10.1093/aje/kwab007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Crump C. Preterm birth and mortality in adulthood: a systematic review. J Perinatol. 2020;40:833‐843. doi: 10.1038/s41372-019-0563-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Currie J, Moretti E. Biology as destiny? Short‐ and long‐run determinants of intergenerational transmission of birth weight. J Labor Econ. 2007;25(2):231‐264. doi: 10.1086/511377 [DOI] [Google Scholar]
- 6. Lorenz JM, Ananth CV, Polin RA, D'Alton ME. Infant mortality in the United States. J Perinatol. 2016;36(10):797‐801. doi: 10.1038/jp.2016.63 [DOI] [PubMed] [Google Scholar]
- 7. Alson JG, Robinson WR, Pittman L, Doll KM. Incorporating measures of structural racism into population studies of reproductive health in the United States: a narrative review. Health Equity. 2021;5:49‐58. doi: 10.1089/heq.2020.0081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Powell JA. Structural racism: building upon the insights of John Calmore recommended citation. NC Law Rev. 2008;86(3):791‐816. [Google Scholar]
- 9. Phelan JC, Link BG. Is racism a fundamental cause of inequalities in health? Annu Rev Sociol. 2015;41:311‐330. doi: 10.1146/annurev-soc-073014-112305 [DOI] [Google Scholar]
- 10. Minnesota Department of Health . Advancing Health Equity in Minnesota: Report to the Legislature. Saint Paul, MN; 2014. http://www.health.state.mn.us/divs/chs/healthequity/ahe_leg_report_020414.pdf [Google Scholar]
- 11. Wallace M, Crear‐Perry J, Richardson L, Tarver M, Theall K. Separate and unequal: structural racism and infant mortality in the US. Health Place. 2017;45:140‐144. doi: 10.1016/j.healthplace.2017.03.012 [DOI] [PubMed] [Google Scholar]
- 12. Wallace ME, Mendola P, Liu D, Grantz KL. Joint effects of structural racism and income inequality on small‐for‐gestational‐age birth. Am J Public Health. 2015;105(8):1681‐1688. doi: 10.2105/AJPH.2015.302613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chambers BD, Erausquin JT, Tanner AE, Nichols TR, Brown‐Jeffy S. Testing the association between traditional and novel indicators of county‐level structural racism and birth outcomes among Black and White women. J Racial Ethn Health Disparities. 2018;5(5):966‐977. doi: 10.1007/s40615-017-0444-z [DOI] [PubMed] [Google Scholar]
- 14. Chambers BD, Baer RJ, McLemore MR, Jelliffe‐Pawlowski LL. Using index of concentration at the extremes as indicators of structural racism to evaluate the association with preterm birth and infant mortality—California, 2011‐2012. J Urban Health. 2019;96:159‐170. doi: 10.1007/s11524-018-0272-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Pabayo R, Ehntholt A, Davis K, Liu SY, Muennig P, Cook DM. Structural racism and odds for infant mortality among infants born in the United States 2010. J Racial Ethn Health Disparities. 2019;6:1095‐1106. doi: 10.1007/s40615-019-00612-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mendez DD, Hogan VK, Culhane JF. Institutional racism, neighborhood factors, stress, and preterm birth. Ethn Health. 2014;19(5):479‐499. doi: 10.1080/13557858.2013.846300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hardeman RR, Chantarat T, Smith ML, Karbeah J, Van Riper DC, Mendez DD. Association of residence in high‐police contact neighborhoods with preterm birth among Black and White individuals in Minneapolis. JAMA Netw Open. 2021;4(12):e2130290. doi: 10.1001/JAMANETWORKOPEN.2021.30290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gee GC, Hicken MT. Structural racism: the rules and relations of inequity. Ethn Dis. 2021;31:293‐300. doi: 10.18865/ED.31.S1.293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Groos M, Wallace ME, Hardeman RR, Theall K. Measuring inequity: a systematic review of methods used to quantify structural racism. J Health Dispar Res Pract. 2018;11(2):190‐206. [Google Scholar]
- 20. Hardeman RR, Homan PA, Chantarat T, Davis BA, Brown TH. We can't change what we don't measure: improving measurement of structural racism for antiracist health policy research. Health Aff. 2022;41:179‐186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chantarat T, Van Riper D, Hardeman RR. The intricacy of structural racism measurement: a pilot development of a latent‐class multidimensional measure. EClinicalMedicine. 2021;000:101092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Adkins‐Jackson P, Chantarat T, Bailey ZD, Ponce NA. Measuring structural racism: a guide for epidemiologists and other health researchers. Am J Epidemiol. 2022;191(4):539‐547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Massey DS, Denton NA. The dimensions of residential segregation. Soc Forces. 1988;67(2):281‐315. doi: 10.1093/sf/67.2.281 [DOI] [Google Scholar]
- 24. Krieger N, Feldman JM, Waterman PD, Chen JT, Coull BA, Hemenway D. Local residential segregation matters: stronger association of census tract compared to conventional city‐level measures with fatal and non‐fatal assaults (total and firearm related), using the index of concentration at the extremes (ICE) for racial, economic, and racialized economic segregation, Massachusetts (US), 1995‐2010. J Urban Heal. 2017;94:244‐258. doi: 10.1007/s11524-016-0116-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116:404‐416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Riley AR. Advancing the study of health inequality: fundamental causes as systems of exposure. SSM Popul Health. 2020;10:100555. doi: 10.1016/j.ssmph.2020.100555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Dougherty GB, Golden SH, Gross AL, Colantuoni E, Dean LT. Measuring structural racism and its association with BMI. Am J Prev Med. 2020;59(4):1‐8. doi: 10.1016/j.amepre.2020.05.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bonilla‐Silva E. Rethinking racism: toward a structural interpretation. Am Sociol Rev. 1997;62(3):465‐480. [Google Scholar]
- 29. Reskin B. The race discrimination system. Annu Rev Sociol. 2012;38:17‐35. doi: 10.1146/annurev-soc-071811-145508 [DOI] [Google Scholar]
- 30. Barker L, Brown C. Logistic regression when binary predictor variables are highly correlated. Stat Med. 2001;20(9–10):1431‐1442. doi: 10.1002/sim.680 [DOI] [PubMed] [Google Scholar]
- 31. Brown T, Homan PA. Structural Racism and Health Stratification in the U.S.: Connecting Theory to Measurement. Interdisciplinary Association for Population Health Sciences; 2020. [Google Scholar]
- 32. Healthy People . Maternal, Infant, and Child Health. 2020. Accessed December 8, 2021. https://www.healthypeople.gov/2020/leading-health-indicators/2020-lhi-topics/Maternal-Infant-and-Child-Health
- 33. Hamilton TG. Immigration and the Remaking of Black America. Russell Sage Foundation; 2019. [Google Scholar]
- 34. Manson S, Schroeder J, Van Riper D, Kugler T, Ruggles S. IPUMS National Historical Geographic Information System: Version 15.0 [Database]. 2020.
- 35. Kang‐Brown J, Hinds O, Schattner‐Elmaleh E, Wallace‐Lee J. Incarceration Trends Project: Data and Methods for Historical Jail Populations in U.S. Counties, 1970–2018. Brooklyn, NY: Vera Institute of Justice; 2020. [Google Scholar]
- 36. Collins LM, Lanza ST. Latent Class and Latent Transition Analysis. Wiley; 2009. ISBN: 978‐0‐470‐22839‐5. [Google Scholar]
- 37. Oken E, Kleinman KP, Rich‐Edwards J, Gillman MW. A nearly continuous measure of birth weight for gestational age using a United States national reference. BMC Pediatr. 2003;3(6):1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Cobo T, Kacerovsky M, Jacobsson B. Risk factors for spontaneous preterm delivery. Int J Gynecol Obstet. 2020;150(1):17‐23. doi: 10.1002/ijgo.13184 [DOI] [PubMed] [Google Scholar]
- 39. Schisterman EF, Cole SR, Platt RW. Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology. 2009;20(4):488‐495. doi: 10.1097/EDE.0b013e3181a819a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Vermunt JK. Latent class modeling with covariates: two improved three‐step approaches. Polit Anal. 2010;18(4):450‐469. doi: 10.1093/pan/mpq025 [DOI] [Google Scholar]
- 41. Geronimus AT. The weathering hypothesis and the health of African‐American women and infants: evidence and speculations. Ethn Dis. 1992;2(3):207‐221. [PubMed] [Google Scholar]
- 42. Malat J, Mayorga‐Gallo S, Williams DR. The effects of whiteness on the health of Whites in the USA. Soc Sci Med. 2018;199:148‐156. doi: 10.1016/j.socscimed.2017.06.034 [DOI] [PubMed] [Google Scholar]
- 43. Mason SM, Kaufman JS, Emch ME, Hogan VK, Savitz DA. Ethnic density and preterm birth in African‐, Caribbean‐, and US‐born non‐Hispanic Black populations in New York City. Am J Epidemiol. 2010;172(7):800‐808. doi: 10.1093/aje/kwq209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Herndon A. ‘These People Aren't Coming From Norway’: Refugees in a Minnesota City Face a Backlash–The New York Times. The New York Times. Published 2019. Accessed August 3, 2020. https://www.nytimes.com/2019/06/20/us/politics/minnesota-refugees-trump.html
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplement S1. Description of unidimensional structural racism measures used to derive the multidimensional structural racism typologies.
Supplement S2: Latent class model enumeration, fit statistics, and relative size of typologies.
Supplement S3: Demographic characteristics, downstream determinants, and birth outcomes of White, US‐born Black, and foreign‐born Black people giving birth in Minnesota, 2018.
Supplement S4: Post hoc analysis.


