Abstract
Bronchial carcinoid tumors are low‐grade malignant and lung‐sparing surgery is preferred for the removal of these tumors. We describe a surgical technique of robot‐assisted sleeve segmentectomy via single utility port approach with three robotic arms. This operation was performed in an aged patient with decreased pulmonary function, whose carcinoid tumor was located at the origin of the right superior segmental bronchus. A 1.5‐cm incision was performed in the eighth intercostal space of the midaxillary line and another 4‐cm incision was made in the fifth intercostal space of the anterior axillary line. Postoperative recovery of the patient was smooth without postoperative complications.
Keywords: carcinoid tumor, lung cancer, robot‐assisted thoracoscopic surgery, sleeve segmentectomy
We describe a surgical technique of robot‐assisted sleeve segmentectomy via single utility port approach with three robotic arms. This operation was performed in an aged patient with decreased pulmonary function, whose carcinoid tumor was located at the origin of the right superior segmental bronchus. A 1.5‐cm incision was performed in the eighth intercostal space of the midaxillary line and another 4‐cm incision was made in the fifth intercostal space of the anterior axillary line.

INTRODUCTION
Sleeve segmentectomy is mainly performed in patients with low‐grade malignant tumors or some early lung cancer invaded segmental bronchus, or elderly patients with decreased pulmonary function. 1 , 2 Several cases of robot‐assisted sleeve resection at the segmental level with a four‐ or five‐ports approach have been reported in previous studies. 3 , 4 , 5 Surgical techniques with fewer incisions, especially the uniportal technique, are associated with less chest pain. 6 , 7 , 8 Here, we describe an aged patient with decreased pulmonary function whose carcinoid tumor invaded the bronchus originating of the right superior segment (S6), who underwent robot‐assisted right S6 sleeve segmentectomy via the single utility port approach with three robotic arms.
CASE REPORT
The patient was a 78‐year‐old woman who presented with 2 months of cough. This patient had no history of smoking. Chest computer tomography (CT) scan showed a mass in the right S6 bronchus (B6) of the right lower lobe and distal atelectasis. The bronchoscopy revealed a nodular lesion at the origin of right B6 (Figure 1). Bronchoscopic biopsy specimens were confirmed as carcinoid tumor under the microscope, which was a low‐grade malignant tumor. The patient was diagnosed with mild restrictive ventilation functional disturbance by the pulmonary function test. Other routine physical examination and laboratory tests were normal. Thus, clinical T1aN0M0 disease was diagnosed according to the eighth edition of the TNM classification for lung cancer. 9 After comprehensive consideration, especially considering the advanced age of the patient and her decreased ventilatory function, we performed a single utility port robot‐assisted right S6 sleeve segmentectomy and lymph node dissection using the three‐arms da Vinci Surgical System (Intuitive Surgical).
FIGURE 1.
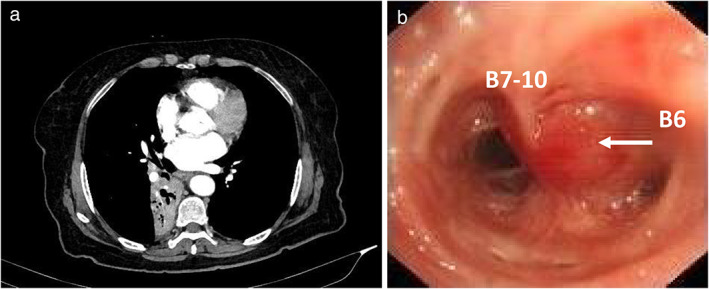
Preoperative physical examination evaluation. (a) Preoperative computed tomographic imaging. (b) Preoperative bronchoscopy showed a nodular lesion at the origin of right B6 (arrow). B6, superior segmental bronchus; B7‐10, basal segmental bronchus
The patient was in a left lateral position with double lumen endotracheal intubation. The three‐arms da Vinci Surgical System was docked on the head side of the patient and slightly turned to the dorsal side. A 1.5‐cm incision was performed in the eighth intercostal space of the midaxillary line, and a small silicon rubber wound protector was placed and used to insert a left robotic arm. Meanwhile, a 4‐cm incision was made in the fifth intercostal space of the anterior axillary line, where a silicon rubber wound protector was placed and used to insert a robotic endoscope and right robotic arm. It is should be noted that the 12‐mm endoscopic trocar was inserted into the upper end of the 4‐cm incision and outside the silicon rubber wound protector, and the trocar of right robotic arm was inserted into the lower end of the 4‐cm incision (Figure 2). The assistant inserted into the approximately 2 cm gap between the endoscopic trocar and right arm trocar using curved suction apparatus and other conventional long instruments to assist surgery.
FIGURE 2.
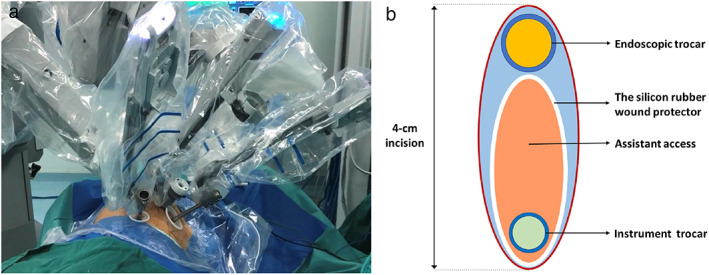
View of robotic instruments. (a) Position of the incisions. (b) The layout of arms in the 4‐cm incision
We first dissected the hilar and pulmonary ligament. Then, the mediastinal, hilar, interlobar and segmental lymph nodes were dissected. The superior segmental vein (V6), the superior segmental artery (A6), and the segmental plane of the right S6 were dissected, which is similar to the procedure for conventional S6 segmentectomy. The staplers were mainly inserted via the assistant gap. During the operation, the right robotic arm can be withdrawn to facilitate the safe and stable operations of the staplers. If the angle of the staplers is not satisfactory in the assistant gap, the 1.5‐cm incision can be used as an alternative operation approach for the staplers. Bronchus invaded by the tumor, including the right B6 and the partial right lower lobe bronchus, was resected with the robotic scissors to achieve macroscopically sufficient margins. The right middle lobe was preserved. Radical resection (R0) was confirmed by intraoperative frozen section. End‐to‐end anastomosis was performed between the right lower bronchus and the basal segmental bronchus by the half‐continuous suturing method 10 (Figure 3). No air leakage at the bronchial anastomosis was confirmed by a sealing test under 25 cm H2O ventilation positive end‐expiratory pressure.
FIGURE 3.
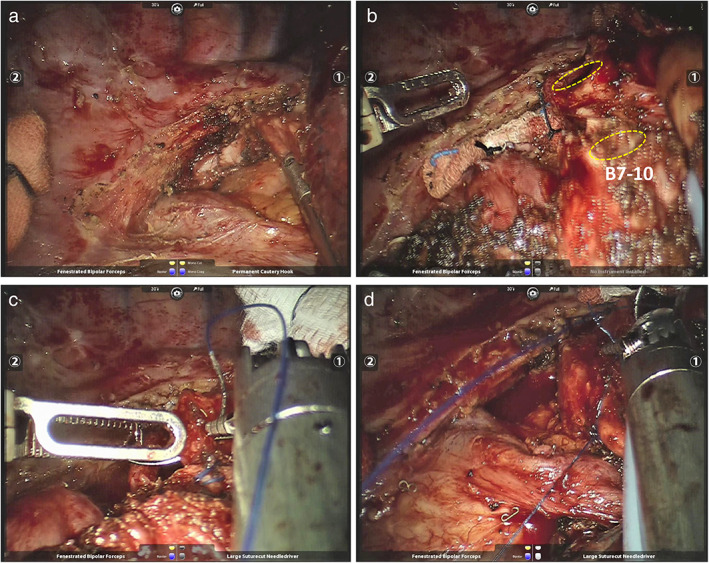
Intraoperative view. (a) Group 7 lymph nodes were dissected. (b) The stumps of the right lower bronchus and basal segmental bronchus (yellow circle). (c) The anastomosis was performed by the half‐continuous suturing method. (d) The anastomosis was completed and the knot tied
Postoperative recovery of the patient was smooth without postoperative complications. The chest X‐ray on the first postoperative day showed the lung was well ventilated (Figure 4). Bronchial anastomosis was confirmed by fibrotic bronchoscopy before discharge. The chest CT scan of the patient 1 month after the operation showed no abnormality. The follow‐up showed that the patient had survived for 8 months without recurrence.
FIGURE 4.
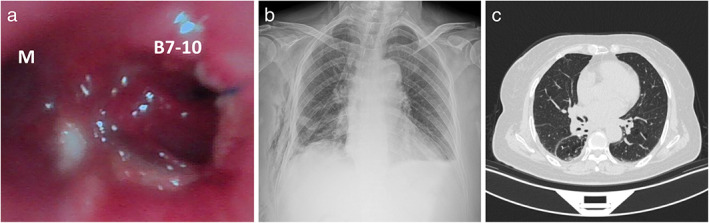
Postoperative physical examination evaluation. (a) Postoperative view at the anastomosis. (b) Chest X‐ray on the first postoperative day. (c) Chest CT scan 1 month after the operation. M, middle lower bronchus; B7‐10, basal segmental bronchus
DISCUSSION
Bronchial carcinoids are rare neuroendocrine tumors that are recognized as low‐grade malignant tumors. 2 , 11 Sleeve segmentectomy can avoid lobectomy or pneumonectomy to preserve more pulmonary function for aged patients with low‐grade malignant tumors and decreased pulmonary function, thus it is safe and useful as a lung‐saving operation. 1 , 2 Furthermore, surgical techniques with fewer incisions, especially the uniportal technique, are associated with less chest pain. 6 , 7 , 8 We therefore performed a single utility port robot‐assisted right S6 sleeve segmentectomy with three robotic arms, which can further reduce the excess surgical trauma caused by another port or more ports, and simultaneously preserve more functional lung tissues. To the best of our knowledge, this is the first report on robot‐assisted sleeve segmentectomy with the single utility port approach.
Because the endoscope cannot be withdrawn during the operation, we placed the endoscopic arm at the upper end of the 4‐cm incision and outside the silicon rubber wound protector to make the best use of space and minimize the disturbance of the endoscopic arm during the operation process. On the contrary, the robotic instrument arm was inserted into the incisions which were placed by the silicon rubber wound protectors. In this way, we were able to withdraw any robotic instrument arm at any time to insert the staplers or ensure the safe operation of the staplers, and protect the incision from tumor invasion. Interference between the endoscopic arm and the right robotic arm was inevitable because these two arms were insert into the same incision. After determining the appropriate position and angle of the robotic arms, the surgical operation via single utility port approach with three arms was feasible based on our experience. The movement range of the right arm should not be larger to avoid additional trauma.
In conclusion, we consider that robot‐assisted leeve segmentectomy via the single utility port approach is feasible and safe for carefully selected patients.
Liu A, Zhao Y, Qiu T, Xuan Y, Qin Y, Sun X, et al. Single utility port approach in robot‐assisted sleeve segmentectomy for bronchial carcinoid tumor. Thorac Cancer. 2022;13:1537–1540. 10.1111/1759-7714.14409
REFERENCES
- 1. Tsutani Y, Okada M. Bronchoplasties at the segmental level. Thorac Surg Clin. 2018;28(3):299–304. [DOI] [PubMed] [Google Scholar]
- 2. Anile M, Diso D, Rendina EA, Venuta F. Bronchoplastic procedures for carcinoid tumors. Thorac Surg Clin. 2014;24(3):299–303. [DOI] [PubMed] [Google Scholar]
- 3. Pan X, Gu C, Wang R, Zhao H, Shi J, Chen H. Initial experience of robotic sleeve resection for lung cancer patients. Ann Thorac Surg. 2016;102(6):1892–7. [DOI] [PubMed] [Google Scholar]
- 4. Gu C, Pan X, Chen Y, Yang J, Zhao H, Shi J. Short‐term and mid‐term survival in bronchial sleeve resection by robotic system versus thoracotomy for centrally located lung cancer. Eur J Cardiothorac Surg. 2018;53(3):648–55. [DOI] [PubMed] [Google Scholar]
- 5. Li C, Zhou B, Han Y, Jin R, Xiang J, Li H. Robotic sleeve resection for pulmonary disease. World J Surg Oncol. 2018;16(1):74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Magouliotis DE, Fergadi MP, Spiliopoulos K, Athanassiadi K. Uniportal versus multiportal video‐assisted thoracoscopic lobectomy for lung cancer: an updated meta‐analysis. Lung. 2021;199(1):43–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sano Y, Okazaki M, Shigematsu H, Yamashita N, Sugimoto R, Sakao N, et al. Quality of life after partial lung resection with uniportal versus 3‐port video‐assisted thoracoscopic surgery: a prospective randomized controlled study. Surg Today. 2021;51:1755–63. [DOI] [PubMed] [Google Scholar]
- 8. Ueda K, Umehara T, Maeda K, Suzuki S, Yokomakura N, Kariatsumari K, et al. Three‐incision robotic major lung resection for cancer. Transl Cancer Res. 2021;10(11):4617–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Goldstraw P, Chansky K, Crowley J, Rami‐Porta R, Asamura H, Eberhardt WEE, et al. The IASLC lung cancer staging project: proposals for revision of the TNM stage groupings in the forthcoming (eighth) edition of the TNM classification for lung cancer. J Thorac Oncol. 2016;11(1):39–51. [DOI] [PubMed] [Google Scholar]
- 10. Jiao W, Zhao Y, Qiu T, Xuan Y, Sun X, Qin Y, et al. Robotic bronchial sleeve lobectomy for central lung tumors: technique and outcome. Ann Thorac Surg. 2019;108(1):211–8. [DOI] [PubMed] [Google Scholar]
- 11. Travis WD, Brambilla E, Nicholson AG, Yatabe Y, Austin JHM, Beasley MB, et al. The 2015 World Health Organization classification of lung tumors: impact of genetic, clinical and radiologic advances since the 2004 classification. J Thoracic Oncol. 2015;10(9):1243–60. [DOI] [PubMed] [Google Scholar]


