Abstract
Background
A substantial drop in emergency department (ED) visit volume was previously demonstrated at the onset of the COVID-19 pandemic.
Objective
To examine changes in the number of non-COVID adult ED visits and their associated 30-day mortality during 14 months of the pandemic in Israel.
Methods
This is a retrospective cohort study including 1,285,270 adult ED visits between 1st March, 2018 and 30th April, 2021 to the internal and surgical EDS in eight general hospitals of the largest healthcare organization in Israel. The 14 months of the pandemic period (March 2020–April 2021) were divided into seven periods according to dates of the three lockdowns. Exposure to each of these periods was compared to the parallel period during the two previous years. March 2020–April 2021 was compared to the parallel periods in 2018 and 2019.
Results
During the pandemic period, the largest decline in ED visits (44.6% and 50.9% for internal and surgical EDs, respectively) and the highest excess 30-day mortality following an ED visit (internal EDs Adjusted OR (ORadj), 1.49; 95% CI, 1.34–1.66 and surgical EDs: ORadj 1.50; CI, 1.16–1.94) were 95%, observed during the first lockdown. Both gradually levelled-off subsequently until near-normalization was reached in March–April 2021 for both parameters.
Conclusions
A substantial decline in non-COVID ED visits and excess mortality at the beginning of the pandemic, are probably the results of social distancing restrictions alongside patients’ fear of exposure to COVID-19, which gradually moderated thereafter, until near normalization was reached after 14 months. Gradual return to pre-pandemic ED utilization patterns were noticed as the population and the healthcare system acclimatize to life alongside COVID.
Keywords: COVID-19, Emergency department visits, Healthcare utilization, Proactive follow-up, Low-value care
Introduction
The coronavirus disease 2019 (COVID-19) continues to spread around the globe since being declared a pandemic by the WHO in March 2020 [1]. During the first months of the pandemic, a decline in emergency department (ED) visits among all age groups was observed in numerous countries (the US (42%) [2], the UK (42%) [3], Northern Italy (66%) [4], and Thailand (36%) [5], among others). The level of ED visits picked up in subsequent months but remained lower than pre-pandemic levels throughout 2020 (in the US, for example, the decline was 23%), even in the case of acute non-COVID-19-related emergencies, such as myocardial infarctions and cerebrovascular accidents [6]. This phenomenon may have had a significant effect on public health. Understanding the impact of the pandemic and the associated social distancing measures on ED visits can improve the response by healthcare systems to the pandemic and generate greater preparedness for future global or national events.
In this study, we examine changes in ED visits unrelated to COVID, and associated mortality rates up to 14 months since the pandemic onset in Israel, using the comprehensive databases of Clalit Health Services (Clalit), the largest healthcare organization in Israel. The last two months of the study period, i.e., March and April 2021, can be viewed as a "post-vaccine” period during which most of the Israeli adult population had already been vaccinated and most of the social distancing restrictions had been lifted.
Methods
Study design and participants
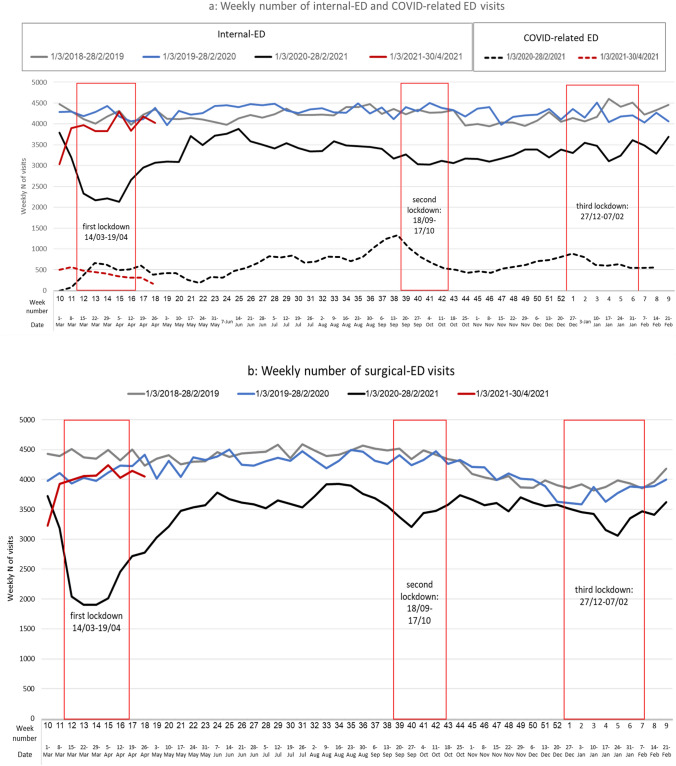
A retrospective cohort study was carried out which included all internal and surgical ED visits by adult Clalit members (aged 18 or older) at all eight of Clalit’s general hospitals, during the period from March 1, 2020 to April 30, 2021. The internal and surgical EDs are physically separated and the patient is triaged into the relevant ED by the hospital staff based on his chief acute complaint, before entering the ED. ED visits were classified as internal (general internal including cardiology, dermatology, nephrology and pulmonology EDs), or surgical (general surgery, gynecology, orthopedics, trauma, ophthalmology, otolaryngology, oral and maxillofacial EDs) based on hospitals' records. Pediatric-EDs and psychiatric-EDs were not included in the study. COVID-related ED visits are also identified (based on hospitals' coded diagnosis) and separated out (see Fig. 1a).
Fig. 1.
Weekly number of ED visits, by year a Internal and COVID-related ED visits; b surgical ED visits 03/2108–02/2019; 03/2019–02/2020; 03/2020–02/2021; and March–April 2021
This study was approved by the Clalit institutional review board. The study was exempt from the requirement for informed consent.
Data source and study variables
Clalit is the largest health fund (insurer and provider) in Israel, where health insurance is universal and mandatory [7]. Clalit provides primary, secondary and tertiary care to 4.7 million individuals (52% of the population), owns and operates a network of eight general hospitals which account for 30% of all general hospital beds in the country. Clalit's information systems are fully digitized and feed into a central data warehouse. The following data were retrieved from Clalit's data warehouse: demographic information, ED visits, clinical comorbidities and patient's date of death. The data on clinical background diagnoses made it possible to calculate the Charlson Comorbidity Index—CCI (not adjusted for age), which measures comorbidity load.
Comparison study period
The first case of COVID-19 in Israel was identified on February 27th, 2020. During the subsequent months, Israel experienced three distinct waves of the COVID-19 pandemic and imposed closures in response. During March 2020, social distancing measures were gradually introduced, culminating in a general closure of the education system and places of congregation starting on March 14th. Following a decline in new case numbers, the closure was gradually lifted, starting on April 19th. On September 18th, a second lockdown was imposed, which lasted until October 17th. The third lockdown was declared on December 27th and gradually lifted starting from February 7th 2021, in parallel to the rapidly implemented vaccination rollout campaign [8].
We have, therefore, divided the 12-month "COVID-19 year" into six periods according to the lockdown dates and compared them to the parallel periods (defined as the equivalent weeks of the calendar year) during the two years prior to the pandemic (March 2018–February 2020). The first two weeks of March 2020 (pre-first lockdown) are included in the comparison of weekly number of visits (Fig. 1 and Table 2), but not in the other analyses. Thus, the periods are defined as follows:
Table 2.
Total and mean daily visits, by period—internal and surgical EDs
| COVID-19 period | Pre-pandemic baseline | p value | % Change | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean (SD) | LCI 95% | UCI 95% | N | Mean (SD) | LCI 95% | UCI 95% | |||
| Internal EDs | ||||||||||
| Pre-first lockdown | 6985 | 521.7 (102.3) | 519.3 | 524.1 | 17,366 | 634.3 (91.5) | 632.9 | 635.6 | < 0.001 | − 17.8% |
| First lockdown | 11,486 | 337.0 (56.3) | 336.0 | 338 | 41,742 | 608.2 (82.1) | 607.4 | 609.0 | < 0.001 | − 44.6% |
| Post-first lockdown | 75,475 | 502.3 (76.7) | 501.8 | 502.9 | 188,005 | 622.5 (84.9) | 622.2 | 622.9 | < 0.001 | − 19.3% |
| Second lockdown | 12,432 | 450.8 (53.1) | 449.9 | 451.7 | 34,724 | 633.8 (93.1) | 632.8 | 634.7 | < 0.001 | − 28.9% |
| Post-second lockdown | 32,247 | 469.3 (61.3) | 468.7 | 470 | 82,990 | 604.0 (80.0) | 603.5 | 604.6 | < 0.001 | − 22.3% |
| Third lockdown | 20,285 | 493.2 (68.5) | 492.3 | 494.2 | 51,343 | 621.9 (79.9) | 621.3 | 622.6 | < 0.001 | − 20.7% |
| Post-third lockdown | 10,465 | 508.2 (68.3) | 506.9 | 509.5 | 24,908 | 603.3 (76.4) | 602.4 | 604.3 | < 0.001 | − 15.8% |
| Total (year) | 169,375 | 481.1 (82.9) | 480.7 | 481.5 | 441,078 | 617.9 (84.3) | 617.6 | 618.1 | < 0.001 | − 22.1% |
| March–April 2021 | 35,108 | 580.3 (87.6) | 579.4 | 581.3 | 73,571 | 615.9 (87.3) | 615.3 | 616.6 | < 0.001 | − 5.6% |
| Surgical EDs | ||||||||||
| Pre-first lockdown | 6908 | 517.9 (103.0) | 515.4 | 520.3 | 16,899 | 616.7 (86.3) | 615.4 | 618.0 | < 0.001 | − 16.0% |
| First lockdown | 10,316 | 304.4 (54.9) | 303.3 | 305.5 | 42,310 | 619.7 (94.2) | 618.9 | 620.7 | < 0.001 | − 50.9% |
| Post-first lockdown | 77,728 | 518.3 (80.2) | 517.8 | 518.9 | 192,270 | 638.3 (91.4) | 637.9 | 638.7 | < 0.001 | − 18.8% |
| Second lockdown | 13,490 | 493.9 (71.6) | 492.7 | 495.1 | 35,203 | 649.3 (107.6) | 648.2 | 650.4 | < 0.001 | − 23.9% |
| Post-second lockdown | 36,054 | 524.6 (66.9) | 523.9 | 525.3 | 81,066 | 593.7 (89.6) | 593.1 | 594.4 | < 0.001 | − 11.6% |
| Third lockdown | 19,954 | 485 (66.4) | 484.1 | 485.9 | 45,742 | 555.7 (74) | 555.0 | 556.4 | < 0.001 | − 12.7% |
| Post-third lockdown | 8485 | 415.4 (71.2) | 413.9 | 416.9 | 17,960 | 467.2 (53.8) | 466.4 | 468.0 | < 0.001 | − 11.1% |
| Total (year) | 172,935 | 496.1 (92.3) | 495.6 | 496.5 | 431,450 | 612.3 (98.7) | 612.0 | 612.6 | < 0.001 | − 19.0% |
| March–April 2021 | 35,324 | 591.9 (82.9) | 591.0 | 592.7 | 71,391 | 625 (92.7) | 624.3 | 625.7 | < 0.001 | − 5.3% |
(i) First lockdown—weeks 12–16; (ii) post-first lockdown—weeks 17–38; (iii) second lockdown—weeks 39–42; (iv) post-second lockdown—weeks 43–52; (v) third lockdown—weeks 1–6; (vi) post-third lockdown (until February 28th 2021)—weeks 7–9. By March 1st 2021, 75% of all Israeli adults (> 18 years old) were at least partially vaccinated or had a previous laboratory-confirmed diagnosis of SARS-CoV-2 infection, which rose to 87% by the end of April [9]. We, therefore, characterize this period (March–April 2021) as "post-vaccine" and compare it to March–April 2018–19 as the seventh period for comparison.
Data analysis
We analyzed differences in daily mean ED visits, patient characteristics (age, sex, and CCI), and 30-day all-cause mortality rates between the seven COVID-19 periods and the corresponding pre-pandemic periods during the previous two years. The analysis was done separately for internal and surgical ED's.
Student's t tests were applied for continuous variables and Chi-Square tests for dichotomous variables. We used a separate generalized estimation equation (GEE) model to calculate odds ratios for 30-day mortality in each comparison period, adjusted for age, sex and CCI, accounting for repeated ED visits. CCI is a widely accepted comorbidity summary measure, which is included in mortality-predicting models in order to account for variability in the known burden of patient comorbidities between periods [10, 11]. Analyses were performed using IBM SPSS Statistics v25.
Results
A total of 1,285,270 ED visits at the eight Clalit general hospitals during the period March 2018–April 2021 were included in our primary analyses, of which 645,561 were internal ED visits and 639,709 were surgical ED visits. The 35,419 COVID-related ED visits at Clalit’s hospital network during March 2020–April 2021 are presented separately and were not included in the analyses (see Fig. 1a).
Patient characteristics
We compared the characteristics of the patients (internal and surgical separately) between the pandemic year and the two baseline years. Patients who visited internal EDs during the pandemic year were slightly younger (SD): 58.3 years (20.67) vs 59.1 years (20.94), p < 0.001, and had less comorbidities, as indicated by a lower mean CCI: 2.69 (3.09) vs. 2.79 (3.12), p < 0.001. Fewer female patients visited internal EDs during the pandemic year relative to the baseline (49.7% vs. 50.2%, p < 0.001). Similarly, patients who visited internal EDs during the two "post-vaccine" months were younger relative to the baseline: mean age (SD)—58.4 (21.03) vs, 59.8 (20.84) years, p < 0.001. The age of surgical ED patients during the pandemic year was only slightly lower than the baseline (mean age (SD): 46.4 years (20.13) vs. 46.7 years (20.23), p < 0.001, and they included fewer female patients (53.5% vs. 55.2%, p < 0.001) (Table 1).
Table 1.
Baseline characteristics of patients who visited—internal and surgical EDs during COVID-19 pandemic in Israel, compared to pre-pandemic baseline periods
| COVID-19 period (SD) | Pre-pandemic baseline period | p value | |
|---|---|---|---|
| Internal ED | |||
| Age, mean | |||
| First lockdown | 58.7 (20.48) | 59.3 (20.91) | < 0.001 |
| Post-first lockdown | 58.2 (20.68) | 58.6 (21.02) | < 0.001 |
| Second lockdown | 57.4 (20.61) | 58.5 (20.93) | < 0.001 |
| Post-second lockdown | 58.8 (20.67) | 59.5 (20.87) | < 0.001 |
| Third lockdown | 58.5 (20.61) | 60.2 (20.80) | < 0.001 |
| Post-third lockdown | 58.1 (20.62) | 59.7 (20.78) | < 0.001 |
| Total (year) | 58.3 (20.67) | 59.1 (20.94) | < 0.001 |
| March–April 2021 | 58.4 (21.03) | 59.8 (20.84) | < 0.001 |
| CCI without age, mean (SD) | |||
| First lockdown | 2.81 (3.17) | 2.86 (3.16) | 0.002 |
| Post-first lockdown | 2.69 (3.09) | 2.73 (3.06) | < 0.001 |
| Second lockdown | 2.50 (2.99) | 2.66 (3.04) | < 0.001 |
| Post-second lockdown | 2.57 (2.96) | 2.71 (3.04) | < 0.001 |
| Third lockdown | 2.83 (3.21) | 3.03 (3.26) | < 0.001 |
| Post-third lockdown | 2.77 (3.15) | 2.95 (3.29) | < 0.001 |
| Total (year) | 2.69 (3.09) | 2.79 (3.12) | < 0.001 |
| March–April 2021 | 2.77 (3.15) | 2.91 (3.17) | < 0.001 |
| Female, N (%) | |||
| First lockdown | 5379 (46.8%) | 30,901 (50.2%) | < 0.001 |
| Post-first lockdown | 37,776 (50.1%) | 99,473 (50.8%) | < 0.001 |
| Second lockdown | 6261 (50.4%) | 17,609 (50.7%) | NS |
| Post-second lockdown | 16,074 (49.8%) | 40,857 (49.2%) | NS |
| Third lockdown | 10,082 (49.7%) | 25,501 (49.7%) | NS |
| Post-third lockdown | 5210 (49.8%) | 12,235 (49.1%) | NS |
| Total (year) | 80,782 (49.7%) | 226,576 (50.2%) | < 0.001 |
| March–April 2021 | 17,662 (50.6%) | 36,331 (50.5%) | NS |
| Surgical ED | |||
| Age, mean | |||
| First lockdown | 46.3 (20.14) | 46.7 (20.27) | < 0.001 |
| Post-first lockdown | 46.3 (20.07) | 46.5 (20.17) | < 0.001 |
| Second lockdown | 45.7 (19.78) | 46.7 (20.06) | < 0.001 |
| Post-second lockdown | 46.5 (20.27) | 46.9 (20.33) | < 0.001 |
| Third lockdown | 46.4 (20.28) | 47.1 (20.42) | < 0.001 |
| Post-third lockdown | 46.8 (20.24) | 47.0 (20.27) | < 0.001 |
| Total (year) | 46.4 (20.13) | 46.7 (20.23) | < 0.001 |
| March–April 2021 | 46.8 (20.40) | 46.6 (20.25) | < 0.001 |
| CCI without age, mean (SD) | |||
| First lockdown | 1.46 (2.40) | 1.42 (2.30) | 0.002 |
| Post-first lockdown | 1.35 (2.23) | 1.36 (2.22) | < 0.001 |
| Second lockdown | 1.30 (2.14) | 1.33 (2.18) | < 0.001 |
| Post-second lockdown | 1.33 (2.18) | 1.35 (2.20) | < 0.001 |
| Third lockdown | 1.44 (2.32) | 1.49 (2.37) | < 0.001 |
| Post-third lockdown | 1.42 (2.28) | 1.46 (2.35) | < 0.001 |
| Total (year) | 1.37 (2.24) | 1.39 (2.25) | < 0.001 |
| March–April 2021 | 1.44 (2.30) | 1.41 (2.29) | < 0.001 |
| Female, N (%) | |||
| First lockdown | 5435 (52.7%) | 34,492 (55.0%) | < 0.001 |
| Post-first lockdown | 41,264 (53.1%) | 110,225 (55.1%) | < 0.001 |
| Second lockdown | 7162 (53.1%) | 19,508 (55.4%) | NS |
| Post-second lockdown | 19,309 (53.6%) | 45,006 (55.5%) | NS |
| Third lockdown | 10,949 (54.9%) | 25,242 (55.2%) | NS |
| Post-third lockdown | 5729 (54.6%) | 12,744 (54.8%) | NS |
| Total (year) | 89,848 (53.5%) | 247,217 (55.2%) | < 0.001 |
| March–April 2021 | 19,257 (53.9%) | 41,158 (55.7%) | NS |
CCI excluding age
Changes in the number of ED visits
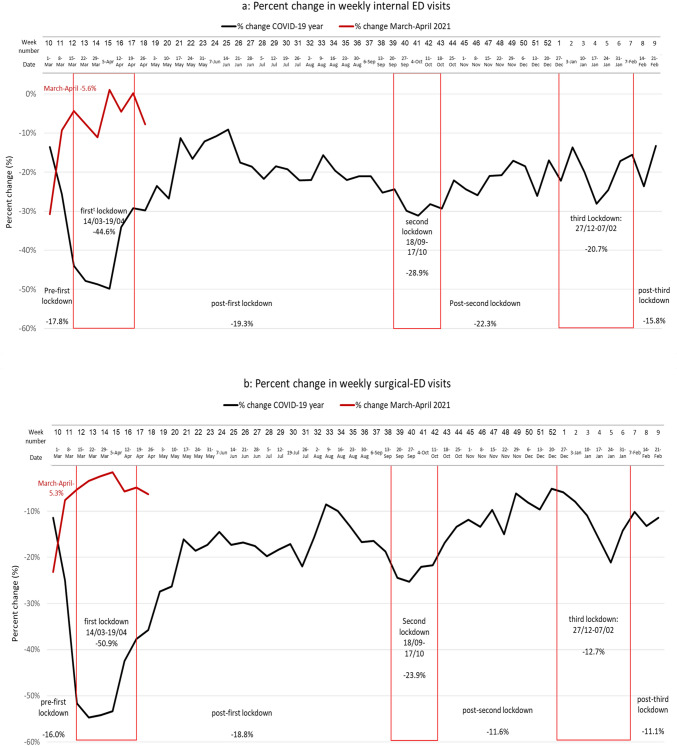
Changes in the number of weekly ED visits are presented in Fig. 1. During the first 12-month pandemic period, internal ED visits [as mean visits per day (SD)] dropped by 22.1% compared to the pre-pandemic baseline (from 617.9 (84.3) to 481.1 (82.9), p < 0.001, whereas surgical ED visits dropped by 19.0% (from 612.3 (98.7) to 496.1 (92.3), p < 0.001) (Table 2). The largest decrease was observed in the first lockdown, during which internal ED visits dropped by 44.6% (from 608.2 (82.1) to 337.0 (56.3), p < 0.001), and surgical ED visits dropped by 50.9% relative to the pre-pandemic baseline (from 619.7 (94.2) to 304.4 (54.9), p < 0.001). The total number of internal and surgical ED visits remained lower than the baseline during the subsequent periods, with declines of 19.3% and 18.8% during the post-first-lockdown period; 28.9% and 23.9% during the second lockdown; 22.3% and 11.6% during the post-second lockdown period; 20.7% and 12.7% during the third lockdown; and 15.8% and11.1% during the post-third lockdown period for internal and surgical EDs, respectively. During March–April 2021, the declines were 5.6% and 5.3%, respectively, relative to the baseline (see Table 2 and Fig. 2).
Fig. 2.
Percentage change in weekly ED visits, compared to baseline period; a internal EDs; b surgical EDs. *Compared to average weekly N of admissions in the 2-previous pre-pandemic years
Differences in mortality rates
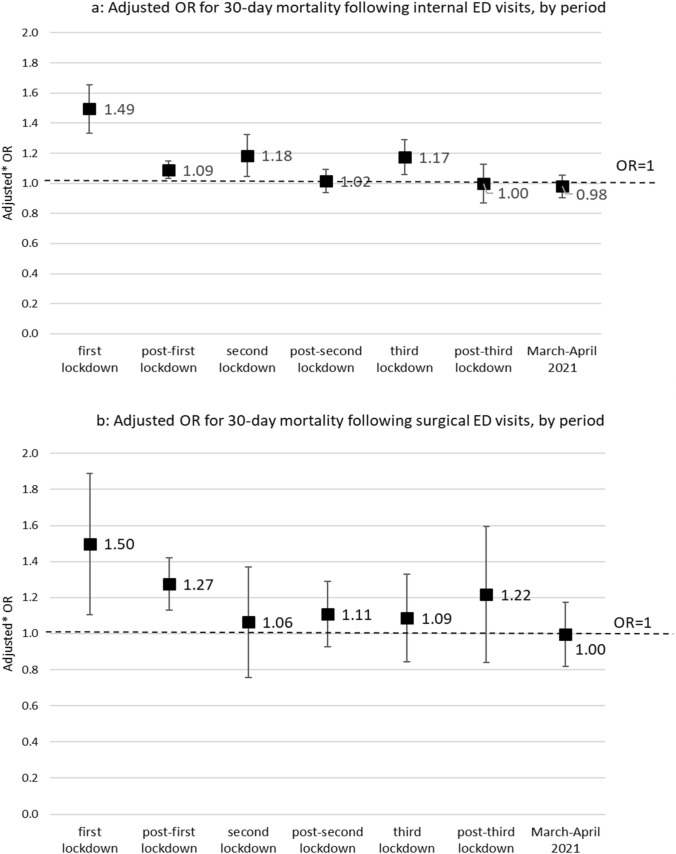
Overall, 30-day mortality rates following an internal ED visit were 40.47 per 1,000 visits during 12 months of the pandemic year as compared to 38.76 per 1000 visits during the baseline period (adjusted OR (ORadj) 1.08; 95% CI 1.05–1.12, p < 0.001) (Table 3). The highest excess mortality was observed during the first lockdown: 54.38 per 1,000 visits as compared to 41.10 per 1000 visits (ORadj 1.49; 95% CI 1.34–1.66; p < 0.001). The level declined in subsequent periods, but remained higher than baseline in the post-first lockdown period (ORadj 1.09; 95% CI 1.03–1.15; p = 0.001) and during the following lockdowns (in the second lockdown: ORadj 1.18; 95% CI 1.05–1.33; p = 0.005, and in the third lockdown: (ORadj 1.17; 95% CI 1.06–1.30; p = 0.002)), but not in the post-second and third lockdown periods, nor during March–April 2021 (see Fig. 3a and Table 3).
Table 3.
30-day mortality rates (per 1000 visits) following ED visits and odds ratios, by period—internal and surgical EDs
| 30-day mortality | Results from adjusted* models | |||||||
|---|---|---|---|---|---|---|---|---|
| COVID-19 period | Pre-pandemic baseline | ORadj | LCI 95% | UCI 95% | p value | |||
| N | Rates per 1000 visits | Average N per year | Rates per 1000 visits | |||||
| Internal EDs | ||||||||
| First lockdown | 630 | 54.38 | 582 | 41.10 | 1.49 | 1.34 | 1.66 | < 0.001 |
| Post-first lockdown | 2803 | 36.66 | 2194 | 34.51 | 1.09 | 1.03 | 1.15 | 0.001 |
| Second lockdown | 505 | 39.86 | 445 | 37.19 | 1.18 | 1.05 | 1.33 | 0.005 |
| Post-second lockdown | 1298 | 39.32 | 1148 | 40.58 | 1.02 | 0.94 | 1.09 | NS |
| Third lockdown | 1023 | 49.45 | 836 | 47.89 | 1.17 | 1.06 | 1.3 | 0.002 |
| Post-third lockdown | 421 | 38.37 | 369 | 43.65 | 1 | 0.88 | 1.13 | NS |
| Total (year) | 6680 | 40.47 | 5574 | 38.76 | 1.08 | 1.05 | 1.12 | < 0.001 |
| March–April 2021 | 1351 | 33.50 | 1020 | 41.00 | 0.98 | 0.91 | 1.06 | NS |
| Surgical EDs | ||||||||
| First lockdown | 88 | 8.51 | 82 | 5.70 | 1.5 | 1.16 | 1.94 | < 0.001 |
| Post-first lockdown | 542 | 6.77 | 348 | 5.28 | 1.27 | 1.14 | 1.43 | < 0.001 |
| Second lockdown | 75 | 5.13 | 65 | 5.51 | 1.06 | 0.8 | 1.41 | NS |
| Post-second lockdown | 252 | 6.93 | 172 | 6.25 | 1.11 | 0.94 | 1.3 | NS |
| Third lockdown | 168 | 8.22 | 117 | 7.33 | 1.09 | 0.87 | 1.36 | NS |
| Post-third lockdown | 67 | 7.27 | 41 | 6.35 | 1.22 | 0.9 | 1.65 | NS |
| Total (year) | 1192 | 6.98 | 825 | 5.81 | 1.18 | 1.09 | 1.27 | < 0.001 |
| March–April 2021 | 212 | 4.80 | 140 | 5.70 | 1 | 0.83 | 1.19 | NS |
*Results from GEE models, adjusted for age, sex, and CCI
Fig. 3.
Adjusted* OR for 30-day mortality following ED visits, by period; A internal EDs; B surgical EDs. *from GEE models, adjusted for age, sex, and CCI. OR are presented with 95% confidence interval
In the case of surgical ED visits, overall 30-day mortality rate during the pandemic year was 6.98 per 1,000 visits vs. 5.70 per 1,000 visits during the baseline period (ORadj 1.18; 95% CI 1.09–1.27, p < 0.001). As in the case of internal EDs, the highest excess mortality was observed during the first lockdown (ORadj 1.50; 95% CI 1.16–1.94; p < 0.001), then diminished but remained significant in the post-first lockdown period (ORadj 1.27; 95% CI 1.14–1.43; p < 0.001). In the following periods no excess mortality was observed (see Fig. 3b and Table 3).
Discussion
During the first 12 months of the pandemic in Israel, there was a substantial decline in the number of non-COVID ED visits relative to the pre-pandemic baseline periods: 22% in the case of internal ED visits and 19% in the case of surgical visits. The largest decline was observed during the first lockdown (45% in internal ED visits and 51% in surgical ED visits) with a gradual narrowing of the gaps during subsequent periods. Nonetheless, the number of ED visits remained lower relative to the baseline throughout the 12-month period. There were only small changes in patient characteristics: patients who did visit the EDs during the pandemic were slightly younger. The difference was only up to 1 year and without clinical significance, but statistical significance was observed due to our large study population. ORadj for 30-day mortality was higher than during the baseline periods, especially in the case of the first lockdown period (internal EDs: ORadj 1.49; 95% CI 1.34–1.66; p < 0.001 and surgical EDs: ORadj 1.50; 95% CI 1.16–1.94; p < 0.001). Finally, there was a gradual reduction in excess mortality throughout the pandemic year, in parallel to the increase in number of visits.
The last two months of our study (March–April 2021) can be characterized as a return to normalcy, with respect to both the number of ED visits and the rates of mortality. This period—in which most of the Israeli adult population had already been vaccinated, most of the restrictions had been lifted and the ED utilization patterns returned to almost pre-pandemic levels—can, therefore, be viewed as a “post-vaccine” period.
Population-level changes in ED visits are likely to be the result of multiple factors. Current evidence suggests that this decrease in ED visits may be the result of deferred care [12–14], whereby certain patient populations reported forgoing medical care, mainly owing to fear of SARS-CoV2 transmission, or in an attempt to mitigate the burden on the healthcare system [15–17]. This trend is in line with public health messages communicated by governments, especially at the beginning of the pandemic, which advised individuals to avoid unnecessary healthcare use to reduce transmission of the virus and ensure that hospital capacity can accommodate surges in COVID-19 cases [19].
The US Centers for Disease Control and Prevention (CDC) reported a similar trend in the US, namely a steep decline in ED visits at the beginning of the pandemic which remained below pre-pandemic levels throughout 2020 [18].
The decline in ED visits has been previously reported also for urgent medical conditions, such as myocardial infarction and stroke [14, 21]. A potential and concerning consequence of patients not seeking appropriate care for medical emergencies might be an increase in mortality and disability over various time frames [12, 14]. Therefore, public health officials should encourage patients to avoid delaying necessary medical care during the pandemic, especially in emergency situations, and should initiate targeted follow-up of the affected population over time in order to identify these consequences [12].
Furthermore, findings from the US National Syndromic Surveillance Program indicate a reduction in ED visits during the pandemic in the case of diagnoses that represent less urgent conditions (e.g., sinusitis, otitis media, intestinal infection, cornea and external disease) [20]. This was further reinforced in a large US study which revealed a steep decline in ED visits for conjunctivitis and dermatitis, which are classified as low-acuity conditions [22]. Reports prior to the pandemic classified at least 30% of all ED visits in the US as non-urgent [23]. This reduction in low-value care due to COVID-19 constraints creates an opportunity to re-evaluate and reduce the frequency of future non-necessary ED visits and thus lighten the burden on the emergency and hospitalization systems. Further segmentation of our findings according to clinical diagnosis and patient characteristics will provide an enhanced understanding of this trend, with the goal of revising post-COVID health policy [24, 25].
The reported excess 30-day mortality rates in Israel during the pandemic year, especially in the case of the first lockdown period, may reflect a higher proportion of more acute clinical conditions, and may be explained in two ways: a reduction in the number of patients with mild conditions who would have visited the ED in normal periods, and an increase in higher acuity problems due to delayed arrival in a worse condition [as exemplified in a recent Israeli study of STEMI patients with substantial increase in the time from symptom onset to reperfusions and in the risk for complications [26]]. These explanations are supported by the fact that the crude number of deaths were also higher in each of the seven COVID periods compared to pre-pandemic periods. Both explanations were likely the result of social distancing restrictions imposed by the Israeli government at an early stage of the pandemic in order to avoid pressure on the hospitals, alongside patients' fear of exposure to COVID-19 and their resultant avoidance and deferment of treatment.
The shift of system resources in favor of treating COVID-19 patients at the expense of providing optimal care to other patients is less likely to explain our findings, in view of the fact that the burden of COVID-19 morbidity and the shift in system resources increased over the course of the year, while mortality rates in fact declined [27]. While we found the highest odds of mortality after the ED visit occurred in the first lockdown, studies evaluating excess national mortality found that it was most common in Israel toward the end of 2020—suggesting that patients in our sample were likely experiencing death due to causes other that COVID-19 [28].
The declining trend in excess odds for 30-day mortality during the pandemic months in parallel to the increase in visits implies a gradual return to pre-pandemic routine, as the population and the healthcare system acclimatize to life alongside COVID, together with vaccination access (vaccination rollout began on January 2021) that probably changed public behavior. Another possible explanation that may contribute to the declining mortality trend may be the improvement in the ED staff learning curve of treating and managing COVID patients.
The study provides a number of insights that should be of benefit to healthcare systems as the pandemic continues to spread around the globe. First, practitioners and public health officials should emphasize the importance of visiting the ED immediately for serious and acute symptoms that cannot be managed in other settings [19]. The public should understand the importance of seeking guidance and emergency care for acute health conditions, and possible barriers to necessary medical care should be addressed with targeted public health messaging [29]. Understanding factors associated with medical care avoidance can inform targeted care delivery approaches and communication efforts encouraging persons to safely seek timely routine emergency care [16].
Second, there should be proactive long-term follow-up in order to identify possible health consequences of the suspected sub-optimal treatment received by some patients with acute medical conditions during the COVID period.
Third, a deeper analysis of our findings according to clinical diagnosis and patient’s clinical and sociodemographic characteristics may be useful in exploiting the unique opportunity to identify low-value care cases that should be systematically addressed in a non-ED setting (such as community-based care, telehealth, and home-based care) [27]. This can facilitate a wiser allocation of limited healthcare resources and the achievement of a better healthcare system in the post-COVID-19 era [25].
This study has several strengths. It examines the effect of the pandemic on ED utilization patterns in a large integrative healthcare organization over a relatively long period, including two months in which most of the country's adult population had already been vaccinated. Further advantages of the study include the extent of population coverage and the availability of computerized up-to-date data gathered in both inpatient and community settings, thus enabling the monitoring of patients over time. Our study's limitations include a lack of information regarding the reasons for ED visits, which would have facilitated an analysis of possible changes in ED patient case-mix and changes in the acuity of clinical conditions during the study period. Furthermore, we acknowledge the lack of available data on the causes of death and mortality rates of patients who did not present for care at EDs. Another limitation of the study may be related to the fact that not all COVID cases may have been identified (especially at the beginning of the pandemic) and some of the excess mortality found may reflect COVID infection. As the COVID burden increased throughout the study period, in contrary to our parameters' trends, we believe the effect of this limitation is minor. The study is also limited to EDs in Israel, and the results may not be generalizable to other countries.
Conclusions
In this retrospective cohort study, we demonstrate the decline in non-COVID ED visits from March 2020 to April 2021 and the increase in 30-day mortality rates observed in the eight EDs operated by the Clalit general hospitals in Israel. These effects of the COVID pandemic diminished during the study period and the situation returned to near-normal during March–April 2021. The findings suggest that the population and the healthcare system acclimatize to life alongside COVID. Practitioners and public health officials should encourage patients, in future epidemic waves, to avoid delaying essential medical care that cannot be managed in other settings. Further study is needed in order to characterize the patients whose use of ED services was most affected. This will make it possible to monitor the consequences of deferral of care for acute conditions over time, and will support efforts to maintain the lower ED utilization rates for non-urgent cases observed during the COVID pandemic, with the goal of improving healthcare preparedness.
Author contributions
The corresponding author attests that all listed authors participated in the research and preparation of the manuscript. All authors had access to the data and a role in writing the manuscript.
Funding
There was no funding for this study.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights statement and Informed consent
This study was approved by the Clalit institutional review board. The study was exempt from the requirement for informed consent.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Yael Wolff Sagy, Email: yaelwo@clalit.org.il.
Assi Cicurel, Email: assi2@docurel.net.
Erez Battat, Email: ErezB@clalit.org.il.
Walid Saliba, Email: saliba_wa@clalit.org.il.
Gil Lavie, Email: gillav76@gmail.com, Email: gillav@clalit.org.il.
References
- 1.World Health Organization (2021) COVID-19 Weekly Epidemiological Update 34. World Health Organization. Published January 10, 2021. https://www.who.int/docs/defaultsource/coronaviruse/situationreports/weekly_epidemiological_update_22.pdf. Accessed 16 Mar 2021
- 2.Hartnett, Kathleen P, Kite-Powell A, DeVies J, Coletta MA, Boehmer TK, Adjemian J et al. (2020) Impact of the COVID-19 pandemic on emergency department visits. Morb Mortal Wkly Rep 69(23):699–704. Published June 3 2020. . cdc.gov/mmwr/volumes/69/wr/pdfs/mm6923e1-H.pdf. Accessed 20 Mar 2021 [DOI] [PMC free article] [PubMed]
- 3.Hughes HE, Hughes TC, Morbey R, Challen K, Oliver I, Smith GE, et al. Emergency department use during COVID-19 as described by syndromic surveillance. Emerg Med J. 2020;37(10):600–604. doi: 10.1136/emermed-2020-209980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Santi L, Golinelli D, Tampieri A, Farina G, Greco M, Rosa S, et al. Non-COVID-19 patients in times of pandemic: emergency department visits, hospitalizations and cause-specific mortality in Northern Italy. PLoS ONE. 2021;16(3):e0248995. doi: 10.1371/journal.pone.0248995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wongtanasarasin W, Srisawang T, Yothiya W, Phinyo P. Impact of national lockdown towards emergency department visits and admission rates during the COVID-19 pandemic in Thailand: a hospital-based study. EMA Emerg Med Australas. 2021;33(2):316–323. doi: 10.1111/1742-6723.13666. [DOI] [PubMed] [Google Scholar]
- 6.Venkatesh AK, Janke AT, Shu-Xia L, Rothenberg C, Goyal P, Terry A, et al. Emergency department utilization for emergency conditions during COVID-19. Ann Emerg Med. 2021 doi: 10.1016/j.annemergmed.2021.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.OECD (2012) Reviews of health care quality: Israel, Executive Summary, Assessment and Recommendations. Available at http://www.oecd.org/els/healthsystems/ReviewofHealthCareQualityISRAEL_ExecutiveSummary.pdf. Accessed 7 Mar 2015
- 8.Ritchie H, Ortiz-Ospina E, Beltekian D, Mathieu E et al (2020) Coronavirus Pandemic (COVID-19). https://ourworldindata.org/coronavirus. Accessed 12 May 2021
- 9.Israel Ministry of Health (2021) COVID-19 Data Dashboard- Vaccinations. Published 1 March 2021. https://datadashboard.health.gov.il/COVID-19/general. Accessed 15 Jun 2021
- 10.Romano PS, Roos LL, Jollis JG. Adapting a clinical comorbidity index for use with ICD-9-CM administrative data: differing perspectives. J Clin Epidemiol. 1993;46(10):1075–1079. doi: 10.1016/0895-4356(93)90103-8. [DOI] [PubMed] [Google Scholar]
- 11.Austin SR, Wong YN, Uzzo RG, Beck JR, Egleston BL. Why summary comorbidity measures such as the Charlson Comorbidity Index and Elixhauser Score Work. Med Care. 2015;53(9):e65–72. doi: 10.1097/MLR.0b013e318297429c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nourazari S, Davis SR, Granovsky R, Austin R, Straff DJ, Joseph JW, et al. Decreased hospital admissions through emergency departments during the COVID-19 pandemic. Am J Emerg Med. 2021;42:203–210. doi: 10.1016/j.ajem.2020.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rubin R. COVID-19's crushing effects on medical practices, some of which might not survive. JAMA. 2020;324(4):321–323. doi: 10.1001/jama.2020.11254. [DOI] [PubMed] [Google Scholar]
- 14.Bodilsen J, Nielsen PB, Søgaard M, Dalager-Pedersen M, Speiser LOZ, Yndigegn T, et al. Hospital admission and mortality rates for non-COVID diseases in Denmark during COVID-19 pandemic: nationwide population based cohort study. BMJ. 2021;373:n1135. doi: 10.1136/bmj.n1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kelly EA, Emma EM, Rachel P, Colleen LB. Reports of forgone medical care among US adults during the initial phase of the COVID-19 pandemic. JAMA Netw Open. 2021;4(1):e2034882. doi: 10.1001/jamanetworkopen.2020.34882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mark ÉC, Kristy M, Kristie ENC et al (2020) Delay or avoidance of medical care because of COVID-19–related concerns —United States, June 2020. MMWR/September 11, 2020/Vol. 69/No. 36 [DOI] [PMC free article] [PubMed]
- 17.Rosenbaum L. The untold toll: the pandemic’s effects on patients without COVID-19. N Engl J Med. 2020;382(24):2368–2371. doi: 10.1056/NEJMms2009984. [DOI] [PubMed] [Google Scholar]
- 18.Gale R, Eberlein S, Fuller G, Khalil C, Almario CV, Spiegel BM. Public perspectives on decisions about emergency care seeking for care unrelated to COVID-19 during the COVID-19 pandemic. JAMA Netw Open. 2021;4(8):e2120940. doi: 10.1001/jamanetworkopen.2021.20940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jeffery MM, D’Onofrio G, Paek H, Platts-Mills TF, Soares WE, III, Hoppe JA, et al. Trends in emergency department visits and hospital admissions in health care systems in 5 states in the first months of the COVID-19 pandemic in the US. JAMA Intern Med. 2020;180(10):1328–1333. doi: 10.1001/jamainternmed.2020.3288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Adjemian J, Hartnett KP, Kite-Powell A, et al. Update: COVID-19 pandemic-associated changes in emergency department visits—United States, December 2020–January 2021. MMWR Morb Mortal Wkly Rep. 2021;70:552–556. doi: 10.15585/mmwr.mm7015a3externalicon. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Solomon MD, Nguyen-Huynh M, Leong TK, et al. Changes in patterns of hospital visits for acute myocardial infarction or ischemic stroke during COVID-19 surges. JAMA. 2021;326(1):82–84. doi: 10.1001/jama.2021.8414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Noel A, Alban C, Trinkl J, Butler S et al (2021) Fewer visits, sicker patients: the changing character of emergency department visits during the COVID-19 pandemic. Epic Health Res Netw. Published February 3, 2021
- 23.Uscher-Pines L, Pines J, Kellermann A, Gillen E, Mehrotra A. Emergency department visits for nonurgent conditions: systematic literature review. Am J Manag Care. 2013;19(1):47–59. [PMC free article] [PubMed] [Google Scholar]
- 24.Roth AR, Lazris A. Benefits of avoiding unnecessary medical care during the COVID-19 pandemic. Am Fam Physician. 2021;103(10):584–585. [PubMed] [Google Scholar]
- 25.Sorenson C, Japinga M, Crook H, McClellan M. Building a better health care system post-COVID-19: steps for reducing low-value and wasteful care. NEJM Catalyst. 2020 doi: 10.1056/CAT.20.0368. [DOI] [Google Scholar]
- 26.Fardman A, Zahger D, Orvin K, Oren D, Kofman N, Mohsen J, et al. Acute myocardial infarction in the COVID-19 era: incidence, clinical characteristics and in-hospital outcomes—a multicenter registry. PLoS ONE. 2021;16(6):e0253524. doi: 10.1371/journal.pone.0253524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rennert-May E, Leal J, Thanh NX, Lang E, Dowling S, Manns B, Wasylak T, Ronksley PE. The impact of COVID-19 on hospital admissions and emergency department visits: a population-based study. PLoS ONE. 2021;16(6):e0252441. doi: 10.1371/journal.pone.0252441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Haklai Z, Aburbeh M, Goldberger N, Gordon E-S. Excess mortality during the COVID-19 pandemic in Israel, March–November 2020: when, where, and for whom? Isr J Health Policy Res. 2021;10(1):17. doi: 10.1186/s13584-021-00450-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.CDC (2020) COVID-19: framework for healthcare systems providing non-COVID-19 clinical care during the COVID-19 pandemic. Atlanta, GA: US Department of Health and Human Services, CDC. https://www.cdc.gov/coronavirus/2019-ncov/hcp/framework-non-COVID-care.html. Accessed 11 Jan 2020