Abstract
Objectives
To describe the use of a Theory of Change to meaningfully engage community members from or support underserved communities in two National Institutes of Health‐funded implementation science projects aimed at promoting equitable access to COVID‐19 testing and vaccination for underserved communities.
Study setting
Both projects focused on Latino, Black, and immigrant and refugee communities in South/Central San Diego and/or individuals accessing care at a federally qualified health center near the US/Mexico border during December 2020–April 2021.
Study design
By using a participatory action research design, Community Advisory Boards (CABs) were established for each project with 11 and 22 members. CAB members included community organizers, promotores de salud (community health workers), clinic providers and administrators, and public health researchers. The CABs were guided through a seven‐session Theory of Change process, focused on identifying necessary conditions that must exist to eliminate COVID‐19 disparities along with specified actions to create those conditions and a blueprint for assessing the impact of those actions.
Data collection
Each session lasted 2 h hosted virtually and was augmented by interactive web‐based activities. There was a live interpreter who facilitated the participation of Spanish‐speaking CAB members. A Theory of Change for each project was completed in approximately 4 months.
Principal findings
Nine necessary conditions were identified related to (1) accessible and available services; (2) culturally and linguistically competent programming; (3) investment in trusted community and faith leaders; (4) social safety nets to provide ancillary services. Corresponding actions to create these conditions and measures to indicate success in creating these conditions were operationalized by the CAB.
Conclusions
While resource‐intensive, a CAB‐led Theory of Change process yielded a rich opportunity to engage diverse groups that typically are not invited to inform these processes.
Keywords: community engagement, COVID‐19, implementation, methods, testing, Theory of Change, vaccination
What is known on this topic
Meaningful and representative community engagement is essential to equitably and inclusively maximizing impact, scalability, and sustainment of public health interventions.
There are a few examples of how to respectfully incorporate and amplify the lived experience and wisdom of underserved communities when addressing public health emergencies such as the COVID‐19 pandemic.
The Theory of Change approach adds value to such efforts by amplifying community voice in the framing and design of research aims, conduct of research, and development of programs beyond enlisting community members as active participants in predefined studies.
What this study adds
We describe a generalizable Theory of Change community engagement method to identify necessary conditions, actions, and measures to reduce disparities in health and access to care associated with COVID‐19 testing, clinical trial participation, and vaccination among immigrants, refugees, Latinos, and people of color communities.
Suggested actions highlighted by the CAB were materials translation in multiple languages and native‐speaking interpreters, extended hours and mobile clinics for testing and vaccination, low‐technology solutions for scheduling, and culturally appropriate target outreach by trusted messengers.
The methods and findings reported in this paper offer solution‐oriented, community‐driven strategies to address the well‐documented inequities in health outcomes and access to care associated with COVID‐19 experienced by underserved communities in the United States.
1. INTRODUCTION
The COVID‐19 pandemic dramatically illustrated widening health disparities among immigrant, refugee, and Black, Indigenous, People of Color (BIPOC) communities nationally in the United States and within specific geographic regions. 1 These communities were significantly more likely to experience mortality and morbidity from COVID‐19 along with lagging testing and vaccination rates compared to White individuals in the United States. 2 Drivers of these disparities were multifactorial, multilevel, and often intersected with cumulative and compounding impacts. 3 , 4 For example, racial and ethnic minority communities had a higher likelihood of COVID‐19 exposure from living in crowded conditions or in multigenerational households, being employed in jobs that could not be performed remotely, or relying on public transportation for commuting to work. Once infected, individuals from underserved communities experienced greater morbidity and mortality from COVID‐19 related to poor access to healthcare and chronic medical comorbidities that are common among BIPOC communities. A contributing factor to both COVID‐19 exposure and health disparities is structural racism experienced by and observed within minority communities. 5 These health disparities are particularly evident in Southern California, particularly South and Central San Diego, where a significant proportion of residents are BIPOC, experience poor housing and employment conditions, and suffer from co‐occurring chronic health conditions that increase their risk of COVID‐19 and negative sequalae. 6 , 7
For achieving health equity in COVID‐19 testing and vaccination access and uptake, public health interventions must have high acceptability and uptake across population groups, especially those that experience high rates of health disparities. Meaningful community engagement throughout phases of design, implementation, adaptation, and evaluation provides a critical, evidence‐based, albeit resource‐intensive approach to increasing vaccination access and uptake. 8 , 9 , 10 Health promotion interventions and their implementation are likely to have greater reach and impact when the focus is on interweaving health promotion strategies, practices, programs, and policies to fit within or enhance existing settings and environmental contexts rather than focusing solely on individual changes. 11 These principles are at the heart of implementation science, community‐based participatory action research, and public health. In particular, the use of a Theory of Change framework and participatory cocreation methods through an assembly of Community Advisory Boards can ensure meaningful engagement of community stakeholders and maximize public health impact for underserved communities. Integrating these methods can accelerate accounting for the complex, dynamic, real‐world contexts in which these strategies need to be implemented to promote equitable access and engagement. 9
Theories of Change have been broadly used to guide the planning, implementation, and evaluation of public health programs for underserved communities 12 and provide a comprehensive description and illustration of how and why a desired change is expected to happen in a particular context. Theories of Change provide a means for advancing “community science,” that is, a community‐university relationship where community knowledge contributes to the coevolution of the research questions asked, plus ideas for understanding and improving the methods of inquiry involved. 13 Community Science is a civically engaged approach to scientific inquiry and discovery that “flips the community‐university dynamic, asking communities to identify civic priorities ripe for innovation and then to partner with researchers to address those priorities.” 13 There is increasing emphasis on the importance of community engagement as a way to tap useful insights for research purposes. 14 , 15
Theories of Change are customized to the specific community project, needs, and context and involve seven general steps. These include: (1) identify the long‐term goal(s) (i.e., the “North Star”); (2) specify the contributing factors preventing the long‐term goal(s) from happening; (3) map and connect the essential conditions necessary to achieve that goal; (4) identify basic assumptions about the context; (5) identify the implementation strategies needed to create the desired change; (6) develop indicators to measure outcomes; (7) write a narrative to explain the logic of the initiative. Theories of Change guided by the voices of diverse Community Advisory Board members can inform opportunities for refinement, as well as document generalizable lessons for future scale‐up. The Theory of Change approach adds value to such efforts by amplifying community voice in the framing and design of research aims, conduct of research, and developing programs beyond enlisting community members as active participants in predefined studies.
In response to the alarming health disparities experienced by underserved communities related to the COVID‐19 pandemic, the National Institutes of Health heavily invested in community engagement research efforts to eliminate disparities in testing, clinical trial participation, access to care, and vaccine uptake. 16 Two of these programs are the Community Engagement Alliance Against COVID‐19 Disparities and the Rapid Acceleration of Diagnostics for Underserved Populations. Our objective is to describe the use of a Theory of Change process to meaningfully engage community members from or support underserved communities in two implementation science projects funded by the Community Engagement Alliance Against COVID‐19 Disparities and Rapid Acceleration of Diagnostics for Underserved Populations National Institutes of Health programs aimed at promoting equitable access to COVID‐19 testing, vaccination, and inclusion in clinical trials. The two projects are: (1) Community‐driven Optimization of COVID‐19 testing to Reach and Engage underserved Areas for Testing Equity (CO‐CREATE) and (2) Share, Trust, Organize, Partner: The COVID‐19 California Alliance (STOP COVID‐19 CA).
2. METHODS
2.1. Community‐driven Optimization of COVID‐19 testing to Reach and Engage Underserved Areas for Testing Equity
CO‐CREATE is a 2‐year study initiated and funded through the National Institutes of Health Rapid Acceleration of Diagnostics for Underserved Population. The key objective is to understand practices, barriers, and facilitators to access and uptake of COVID‐19 testing and follow‐up for underserved community members from the perspectives of patients, providers, and organizational leaders at a federally qualified health center with clinics in South San Diego near the US/Mexico border.
2.2. Share, Trust, Organize, Partner: The COVID‐19 California Alliance
The STOP COVID‐19 CA project is part of the National Institutes of Health Community Engagement Alliance Against COVID‐19 Disparities. The Community Engagement Alliance Against COVID‐19 Disparities program includes community‐academic teams in 11 states throughout the United States, and focuses on COVID‐19 awareness and education research, especially among Black, Latino, Indigenous, refugee, and immigrant populations. These groups account for over half of reported US cases. The California Community Engagement Alliance Against COVID‐19 Disparities team is locally known as STOP COVID‐19‐CA and involves a network of 11 institutions in California, including UC San Diego. The aims of the UC San Diego Community Engagement Alliance Against COVID‐19 Disparities project are to conduct a rapid community engagement project to assess multilevel barriers, facilitators, and processes to engage individuals from underserved communities, particularly BIPOC, African, Asian, and Middle Eastern immigrant and refugee communities, in COVID‐19 screening and vaccine trials, as well as to advance vaccine uptake.
The University of California San Diego Institutional Review Board approved both studies.
2.3. Community Advisory Boards
Both CO‐CREATE and STOP COVID‐19 CA projects relied on the expertise of diverse stakeholders through the creation of Community Advisory Boards (CAB). Identification and initial engagement of CAB members for both projects were led by the Global Action Research Center (ARC), a nonprofit social change organization with expertise in conducting participatory action research to address public health and environmental justice needs. The Global ARC has strong ties within the broader San Diego area and is considered a trusted resource to many of the grassroot organizations. The Global ARC was in an excellent position to engage key members of the community, considering the target communities' familiarity with Global ARC, knowledge of community culture, and existing formal and informal community leadership. The composition of the CAB differed across the two projects and reflected the specific focus and goals of each project. Table 1 provides a summary of the CAB members for each project.
TABLE 1.
Community Advisory Boards for CO‐CREATE and University of California San Diego STOP COVID‐19 CA
| CO‐CREATE | STOP COVID‐19 CA |
|---|---|
9 community partners
|
11 community leaders
|
6 public health research partners
|
2 policy partners (nonvoting CAB members)
|
7 clinic partners
|
Note: STOP COVID‐19 CA is the Community Engagement Alliance Against COVID‐19 Disparities in California.
Abbreviation: CAB, Community Advisory Boards; CO‐CREATE, Community‐driven Optimization of COVID‐19 testing to Reach and Engage Underserved Areas for Testing Equity.
The CO‐CREATE CAB included 22 members representing community residents, public health partners (i.e., public health researchers), and clinical partners (i.e., clinicians and administrators). The goal of the CO‐CREATE CAB was to directly inform cocreated implementation strategies for a tailored COVID‐19 testing program that is currently being implemented. The STOP COVID‐19 CA CAB was composed of 11 community leaders representing 10 local grassroots community organizations and two policy partners. The goal of the STOP COVID‐19 CA CAB was to inform materials and resources needed to support vaccine clinical trial participation and equity initiatives in underserved communities. Each CAB member was offered a $100 stipend per meeting for their participation.
CAB meetings were conducted virtually using the Zoom and Miro platforms. Sessions lasted an average of 2 h every other week at a set late afternoon/early evening time. Professional Spanish translators were hired and participated in each CAB session to provide live, concurrent interpretation. A bilingual community outreach specialist from the Global ARC produced written translations of materials that were provided for both CAB prior to meetings, during meetings, and in follow‐up communication, as needed. Participants were invited to complete an online engagement survey after each session to share their experience with the quality and extent of engagement. Data from the community engagement surveys will be reported in a separate publication.
2.4. Theory of Change sessions
A total of seven sessions were conducted for each project to complete the Theory of Change process. Table 2 summarizes the goals, agenda and activities, and outcomes for each session. Sessions used a combination of large and small group activities using the breakout room function of the Zoom platform. The process for each session followed a similar consensus‐building agenda: (1) a focus question was posed related to a component of the Theory of Change; (2) CAB members were asked to develop individual responses to the focus question; (3) CAB members were divided into small groups (virtual breakout rooms), and a scribe who was a non‐CAB member of the research team encouraged the small group to share their individual responses and transcribed them on the Miro platform; (4) CAB members rejoined the full group where the Theory of Change facilitator guided the CAB to sort all small group responses into thematic categories that operationalized the components of the Theory of Change (e.g., the Contributing Factors or Necessary Conditions); (5) the Theory of Change facilitators engaged in a final round of consensus‐checking to ensure that the small group responses were accurately sorted, and CAB members agreed on the wording of all text. By the end of each CAB meeting, at least one component of the Theory of Change was completed. Each subsequent CAB meeting was dedicated to codesigning another Theory of Change component, culminating in the final products displayed in Figures 1 and S1 of Supporting information.
TABLE 2.
Structure and content of CO‐CREATE and STOP COVID‐19 CA Theory of Change sessions with Community Advisory Boards
| Session # | Goal | Agenda/activities | Outcomes |
|---|---|---|---|
| #1 |
|
|
|
| #2 |
|
|
|
| #3 |
|
|
|
| #4 |
|
|
|
| #5 |
|
|
|
| #6 |
|
|
|
| #7 |
|
|
|
Abbreviation: CAB, Community Advisory Board.
FIGURE 1.
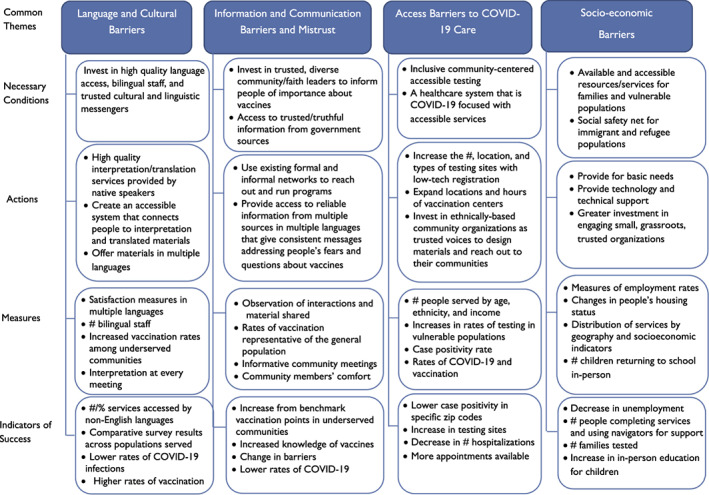
Integrated Theory of Change for CO‐CREATE and UC San Diego STOP COVID‐19 CA [Color figure can be viewed at wileyonlinelibrary.com]
3. RESULTS
3.1. Findings from CO‐CREATE Theory of Change
The CAB identified five factors contributing to disparities in COVID‐19 testing and access to treatment for families with children and/or pregnant women: (1) socioeconomic factors; (2) inconsistent adherence and enforcement of COVID‐19 health guidelines and public rules; (3) the need for in‐person human connection; (4) housing disparities; and (5) conflicting and confusing communication about COVID‐19 prevention and intervention practices. Four necessary conditions were defined to eliminate these disparities: (1) inclusive community centered accessible COVID‐19 testing; (2) culturally and linguistically competent COVID‐19 programming with bilingual staff prepared with accurate materials and information; (3) available and accessible health and social resources and service for vulnerable populations (inclusive of BIPOC, refugee, and immigrant communities); and (4) available and accessible health and social resources and services for families. Based on the necessary conditions, four sets of actions to create these conditions were agreed upon. Examples from each set of actions included increasing the number and location of testing sites such as shelters, mobile testing, work, and home‐based testing; use of existing formal and informal community networks to reach out and run programs; increased resources to reach the hard to reach population; offering basic needs such as childcare, supplemental income, and wrap‐around services. Measures and indicators of success were also identified for each necessary condition by our CAB and included: increase the number of testing sites by 20; decrease case positivity rate; increase vaccination rates among underserved communities; a greater number of family units fully tested; availability of childcare during testing; in‐person education for 90% of children; and more children playing in parks.
3.2. Findings from STOP COVID‐19 CA Theory of Change
Through the Theory of Change process, the CAB reached a consensus on five factors contributing to disparities in clinical trial participation and vaccination: (1) medical racism; (2) distrust of government's ability to handle pandemic and vaccinations; (3) information not accessible—not comprehensible to all people due to cultural diversity; (4) fear due to mixed communication of the science behind vaccines; and (5) trusted cultural/linguistic messengers not included in the design of outreach and educational materials. There were five necessary conditions described to eliminate these disparities: (1) healthcare system focused on COVID‐19 services accessible for all; (2) social safety net/services for immigrant and refugee populations; (3) invest resources for high‐quality language access; (4) access to trusted/truthful information from government sources; and (5) investment in trusted community leaders/faith leaders and workers from diverse communities to inform people of the importance of vaccines. The actions to create these conditions were summarized as five main sets. Examples from each set of actions included expanding locations and hours of vaccination centers and bringing vaccines to people (mobile clinics, door‐to‐door, etc.); increasing investment in and expanded Safety Net services; using Zoom to provide interpretation services at vaccination sites; more leadership and engagement by elected officials; expanding investment in community health workers; employing community members and investing in their education. Measures and indicators of success were also identified for each necessary condition by our CAB. Key measures and/or indicators of success included community members being more at ease and comfortable with information received; community concerns addressed by those with information and power; informative community meetings with interpretation at every meeting; lower rates of COVID‐19 infections; increased knowledge of vaccines; higher vaccination rates; more appointments available in the clinics; and measuring success through community member stories.
4. DISCUSSION
This paper summarizes the process and findings from two parallel Theory of Change processes engaging underserved communities to increase equitable COVID‐19 testing, clinical trial participation, and vaccination. In our two projects, we were able to engage a diverse set of representatives from underserved communities to ensure that the perspectives and priorities of the members of these communities are amplified and that we are ethically valuing, making strong use of community knowledge and wisdom in cocreating our strategies.
4.1. Integrated findings from project Theories of Change
Several common themes emerged in the contributing factors, necessary conditions, actions, and measures across the Theories of Change emerging from the two projects. Figure 1 illustrates the shared features. Important overlaps included barriers associated with language, access, technology, and the importance of targeted outreach and support for basic needs and healthcare access. The critical role of language barriers in exacerbating health inequities has been well described in the literature. 17 , 18 , 19 Multiple reviews found that language barriers in healthcare often result in miscommunication between patients and healthcare providers, leading to reduced satisfaction for both parties and a negative impact on the quality of care and patient safety. 17 , 18 , 19 In our Theory of Change process, community members consistently highlighted the need for materials to be translated into multiple languages, the need for interpreters at clinic sites, and when providing information about public health strategies, the importance of using native speakers who can act as cultural weavers and bridge the cultural meanings between diverse cultures. Lack of access to care continued to be perceived as an important barrier for equitable outcomes for underserved communities. In our projects, the two main concerns related to care access were transportation challenges and limited clinic hours. Strategies that were recommended to address these access challenges included the need for extended hours for testing and vaccinations, as well as offering mobile testing options to meet the community where they live. Technology barriers were especially marked for scheduling COVID‐19 testing and/or vaccination appointments. Our CAB members advocated for low‐technology solutions and technical support for those with limited access to computers, mobile phones, and reliable Internet, and low technological literacy. A critical strategy that emerged from both Theories of Change was the need to use targeted outreach that is culturally appropriate, based on information that is reliable and accessible and provided by messengers who are perceived as credible by the community, including community leaders and existing community groups and networks, community‐based organizations, and social services. Finally, CAB members highlighted that the COVID‐19 pandemic does not exist in a vacuum; to successfully address COVID‐19‐related inequity, we need to consider broader issues such as support for basic needs and access to safety net services.
4.2. Aligning findings with extant COVID‐19 research in underserved communities
The findings from the two Theory of Change processes are consistent with existing literature in COVID‐19 related testing and vaccination for underserved communities. Parallel to the Theory of Change process, our team performed a rapid review of the literature (n = 46 included articles) and identified 245 barriers and 317 strategies for COVID‐19 testing and clinical trial participation for underserved populations. 20 When overlaying findings from the rapid review and our Theory Change processes, we found substantial crossover between the themes that emerged across these two sources. For example, the rapid review identified several effective and/or recommended strategies for equitable COVID‐19 testing, such as equitable distribution of resources, cultural adaptation, education, community outreach, and technological advancements. These strategies overlapped naturally with the four necessary conditions of equitable COVID‐19 testing identified through our Theory of Change process (e.g., available and accessible resources and service for vulnerable populations).
While many publications discussed the uneven epidemiologic burden of the COVID‐19 pandemic, less has been published on community‐focused solutions for addressing care inequities. We highlight a few recent examples that well‐align with our cocreated community findings. Murphy and colleagues reported on a COVID‐19 testing program for underserved communities in Rhode Island, highlighting the importance of culturally appropriate approaches to testing. 21 Wilkins and colleagues emphasized the importance of acknowledging both upstream factors (e.g., housing inequality, food insecurity, and racism) addressed through local policy strategies such as eviction moratoriums along with downstream opportunities for addressing immediate needs for inequities in care, suggesting locally relevant measures and goals of success. 22 Thielke and colleagues called for a multiprong approach to addressing COVID‐19 inequities through an immediate change in healthcare access through Medicaid programs while also addressing systemic biases for long‐term solutions. 23 Finally, Risendal and colleagues proposed a multilevel COVID‐19 response, mirroring efforts of cancer control that demonstrated the essential role of community‐level solutions, including development and dissemination of evidence‐based, culturally relevant messages to promote informed decision making. 24
4.3. Public health implications
The COVID‐19 pandemic has exacerbated health inequities and sharpened the need to engage diverse community stakeholders from underserved communities in cocreating public health solutions that are meaningful and feasible in their communities. Application of a CAB‐led Theory of Change process yielded a unique and rich opportunity to convene diverse communities and community members to drive collaborative problem‐solving and solution‐making. Findings highlighted the importance and redirected our attention to larger, systemic challenges in public health and healthcare that are common root causes for health inequity regardless of specific conditions. While we set out to identify specific solutions to address inequity in COVID‐19 testing, vaccination, and clinical trial participation, we learned that larger, system‐level gaps and inadequacies were priorities for our community partners and transcended a narrow focus on COVID‐19 care. Findings from our joint projects contribute to an emerging, much needed, evidence‐based scholarship that documents the value and tangible merits of authentic community engagement. 9
Balanced with the high value of these CAB‐led Theories of Change is acknowledging the significant resources needed for these community engagement processes. These resources included time, conceptual and experiential contributions from the CAB members, stipends and technology support (e.g., purchased mobile devices) for CAB members to participate, personnel from community partners to lead the Theory of Change sessions, translation and interpretation services to facilitate inclusive participation of CAB members, and research team contributions to lead evaluation efforts. Dedicated funding and technical support for community engagement methods like CAB‐led Theory of Change are crucial for successful and sustained public health interventions. Because of the intensive nature of the Theory of Change process, we recommended this process when there are adequate resources (time, fiscal, personnel) for and shared values between community partners, members, and researchers to meaningfully, and ideally, equitably contribute to the process. We were fortunate that the funding sources for both projects prioritized the explicit sharing of resources between community and academic partners. We hope that this is a trend that will continue to grow across funding sources and research priorities. A separate publication is in production to report the specific time, capital, and fiscal resources invested in our codesigned Theory of Change work.
We acknowledge that the community engagement work reported had limitations. First, due to both the required speed for project launch and fiscal constraints, it was not possible to engage all underserved communities in our geographic region. Second, we necessarily limited the language access options for CAB participation to Spanish and English. Concurrent translation and interpretation of additional languages would have added costs for new translators and time for high‐quality translation within the already lengthy 2‐h CAB sessions. Third, Theories of Change are less commonly used consensus‐building methods in research contexts (e.g., as opposed to Delphi methods or group modeling). However, Theories of Change are widely embraced in real‐world program development and evaluation settings and had been previously used by our community partners who led the CAB sessions.
Data from these Theories of Change drive and will continue to inform community‐engaged next steps that include: (1) implementation of a community‐based testing program in collaboration with our clinic partners; (2) an Appreciative Inquiry process that directly engages the CAB through ongoing meetings to evaluate selection and implementation of cocreated COVID‐19 public health strategies; (3) development of culturally, linguistically sensitive and accessible materials and resources to support current and ongoing COVID‐19 mitigation needs such as vaccine uptake.
Although we developed Theories of Change specific to addressing COVID‐19 disparities, the Theory of Change process is generalizable to other public health topics or needs. In fact, our concurrent Theory of Change production across both projects illustrated the feasibility and utility of the Theory of Change process in engaging diverse and unique communities to address highly related but unique aspects of the COVID‐19 pandemic, such as testing versus trial participation and vaccination. In addition, several general findings of actions needed to address the specific COVID‐19 project needs were identified. These included tailored attention to language and literacy needs, service access and availability of structures or procedures, and appropriate inclusion of individuals who are providing and crafting resources and materials. Further, the Theory of Change process highlighted the overarching need for a community‐inclusive public health system that extends beyond COVID‐19 prevention and care services. This raises challenges from a broader “civic infrastructure” perspective with respect to better aligning research and action. While understanding the value of community input is a necessary first step, the goal should be to create supportive civic infrastructure in the form of resources, new rules of engagement, trust bridges (i.e., established partnerships or relationships that promote mutual respect and trust between stakeholders), and protocols necessary to enable community voices to be presented, heard and acted upon in significant ways.
Supporting information
Figure S1. Project‐specific Theories of Change developed by Community Advisory Boards to address disparities in COVID‐19 testing, vaccinations, and clinical trial participation in underserved communities.
ACKNOWLEDGMENTS
We would like to extend our gratitude for the time and wisdom shared by the University of California San Diego STOP COVID‐19‐CA and CO‐CREATE Community Advisory Board members.
Stadnick NA, Cain KL, Oswald W, et al. Co‐creating a Theory of Change to advance COVID‐19 testing and vaccine uptake in underserved communities. Health Serv Res. 2022;57(Suppl. 1):149‐157. doi: 10.1111/1475-6773.13910
Findings from this work have been presented at two scientific conferences: 1. Oral presentation at the Annual UK Implementation Science Research Conference, virtual. 2. Poster presentation at the Colorado Pragmatic Research in Health Conference, virtual.
Funding information This work was funded by the National Institutes of Health: P42 ES010337‐19S2 RADx‐UP Supplement (Laurent, Tukey); OTA‐21‐312‐0217571‐66106L (Rabin, Stadnick); K23 MH110602 (Stadnick); R34 MH120190 (Stadnick), and the UC San Diego ACTRI Dissemination and Implementation Science Center (Rabin, Stadnick).
REFERENCES
- 1. Price‐Haywood EG, Burton J, Fort D, Seoane L. Hospitalization and mortality among Black patients and White patients with Covid‐19. N Engl J Med. 2020;382:2534‐2543. doi: 10.1056/nejmsa2011686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pham O, Ndugga N, Hill L, Artiga S, Alam R, Parker N. Latest Data on COVID‐19 Vaccinations Race/Ethnicity. Kaiser Family Foundation. Accessed July 2, 2021. https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-race-ethnicity/
- 3. Mackey K, Ayers CK, Kondo KK, et al. Racial and ethnic disparities in COVID‐19–related infections, hospitalizations, and deaths: A systematic review. Ann Intern Med. 2021;174(3):362‐373. doi: 10.7326/m20-6306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lopez L, Hart LH, Katz MH. Racial and ethnic health disparities related to COVID‐19. JAMA. 2021;325(8):719‐720. doi: 10.1001/jama.2020.26443 [DOI] [PubMed] [Google Scholar]
- 5. Tan SB, de Souza P, Raifman M. Structural racism and COVID‐19 in the USA: a county‐level empirical analysis. J Racial Ethn Health Disparities. 2021;1‐11. doi: 10.1007/s40615-020-00948-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. County of San Diego . San Diego County: Demographics Profile. Accessed July 2, 2021. https://www.sandiegocounty.gov/content/dam/sdc/hhsa/programs/phs/CHS/demographics/2017%20Demographic%20Profiles.pdf
- 7. HealthDAT ‐ Diseases and Conditions. www.healthdat.org. Accessed July 2, 2021. http://www.healthdat.org/diseases.php
- 8. Levin MB, Bowie JV, Ragsdale SK, Gawad AL, Cooper LA, Sharfstein JM. Enhancing community engagement by schools and programs of public health in the United States. Annu Rev Public Health. 2021;42(1):405‐421. doi: 10.1146/annurev-publhealth-090419-102324 [DOI] [PubMed] [Google Scholar]
- 9. O'Mara‐Eves A, Brunton G, Oliver S, Kavanagh J, Jamal F, Thomas J. The effectiveness of community engagement in public health interventions for disadvantaged groups: a meta‐analysis. BMC Public Health. 2015;15(1):129. doi: 10.1186/s12889-015-1352-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Brunton G, Thomas J, O'Mara‐Eves A, Jamal F, Oliver S, Kavanagh J. Narratives of community engagement: a systematic review‐derived conceptual framework for public health interventions. BMC Public Health. 2017;17(1):944. doi: 10.1186/s12889-017-4958-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Springer AE, Evans AE, Ortuño J, Salvo D, Varela Arévalo MT. Health by design: interweaving health promotion into environments and settings. Front Public Health. 2017;5:268. doi: 10.3389/fpubh.2017.00268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Breuer E, Lee L, De Silva M, Lund C. Using theory of change to design and evaluate public health interventions: a systematic review. Implementation Sci. 2015;11(1):63. doi: 10.1186/s13012-016-0422-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Civic Innovation Challenge: A Research and Action Competition in the Smart and Connected Communities Domain. NSF.GOV. Accessed July 2, 2021. https://www.nsf.gov/pubs/2020/nsf20562/nsf20562.htm?WT.mc_id=USNSF_179
- 14. Cottler LB, McCloskey DJ, Aguilar‐Gaxiola S, Bennett NM, Strelnick H, Dwyer‐White M. Community needs, concerns, and perceptions about health research: findings from the clinical and translational science award sentinel network. Am J Public Health. 2013;103:1685‐1692. doi: 10.2105/AJPH.2012.300941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Frerichs L, Lich KH, Dave G, Corbie‐Smith G. Integrating systems science and community‐based participatory research to achieve health equity. Am J Public Health. 2016;106:215‐222. doi: 10.2105/AJPH.2015.302944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.NIH to invest $29 million to address COVID‐19 disparities. National Institutes of Health (NIH). Accessed July 2, 2021. https://www.nih.gov/news‐events/news‐releases/nih‐invest‐29‐million‐address‐covid‐19‐disparities
- 17. Yeo S. Language barriers and access to care. Annu Rev Nurs Res. 2004;22(1):59‐73. doi: 10.1891/0739-6686.22.1.59 [DOI] [PubMed] [Google Scholar]
- 18. Al Shamsi H, Almutairi AG, Al Mashrafi S, Al Kalbani T. Implications of language barriers for healthcare: a systematic review. Oman Med J. 2020;35(2):e122. doi: 10.5001/omj.2020.40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Saha S, Fernandez A, Perez‐Stable E. Reducing language barriers and racial/ethnic disparities in health care: an Investment in our future. J Gen Intern Med. 2007;22(Suppl 2):371‐372. doi: 10.1007/s11606-007-0372-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lee N, Abasta J, Rabin B et al. COVID‐19 Testing in Underserved Communities: Rapid Evidence Review. https://medschool.ucsd.edu/research/actri/centers/DIR/Documents/COCREATE%20Rapid%20Evidence%20Review.pdf
- 21. Murphy M, Dhrolia I, Zanowick‐Marr A, et al. A community‐adapted approach to SARS‐CoV‐2 testing for medically underserved populations, Rhode Island, USA. Emerg Infect Dis. 2021;27(9):2445‐2449. doi: 10.3201/eid2709.204874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wilkins CH, Friedman EC, Churchwell AL, et al. A Systems Approach to Addressing Covid‐19 Health Inequities. Vol. 2(1); January 2021. doi: 10.1056/CAT.20.0374 [DOI]
- 23. Thielke A, Curtis P, King V. Addressing COVID‐19 Health Disparities: Opportunities for Medicaid Programs. The Milbank Memorial Fund. Published June 28, 2021.
- 24. Risendal BC, Hébert JR, Morrato EH, et al. Addressing COVID‐19 using a public health approach: perspectives from the cancer prevention and control research network. Am J Prev Med. 2021;60(6):877‐882. doi: 10.1016/j.amepre.2021.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Project‐specific Theories of Change developed by Community Advisory Boards to address disparities in COVID‐19 testing, vaccinations, and clinical trial participation in underserved communities.


