Abstract
Objective
To identify work–environment characteristics associated with Veterans Health Administration (VHA) behavioral health provider (BHP) burnout among psychiatrists, psychologists, and social workers.
Data Sources
The 2015–2018 data from Annual All Employee Survey (AES); Mental Health Provider Survey (MHPS); N = 57,397 respondents; facility‐level Mental Health Onboard Clinical (MHOC) staffing and productivity data, N = 140 facilities.
Study Design
For AES and MHPS separately, we used mixed‐effects logistic regression to predict BHP burnout using surveys from year pairs (2015–2016, 2016–2017, 2017–2018; six models). Within each year‐pair, we used the earlier year of data to train models and tested the model in the later year, with burnout (emotional exhaustion and/or depersonalization) as the outcome for each survey. We used potentially modifiable work–environment characteristics as predictors, controlling for employee demographic characteristics as covariates, and employment facility as random intercepts.
Data Collection/Extraction Methods
We included work–environment predictors that appeared in all 4 years (11 in AES; 17 in MHPS).
Principal Findings
In 2015–2018, 31.0%–38.0% of BHPs reported burnout in AES or MHPS. Work characteristics consistently associated with significantly lower burnout were included for AES: reasonable workload; having appropriate resources to perform a job well; supervisors address concerns; given an opportunity to improve skills. For MHPS, characteristics included: reasonable workload; work improves veterans' lives; mental health care provided is well‐coordinated; and three reverse‐coded items: staffing vacancies; daily work that clerical/support staff could complete; and collateral duties reduce availability for patient care. Facility‐level staffing ratios and productivity did not significantly predict individual‐level burnout. Workload represented the strongest predictor of burnout in both surveys.
Conclusions
This study demonstrated substantial, ongoing impacts that having appropriate resources including staff, workload, and supervisor support had on VHA BHP burnout. VHA may consider investing in approaches to mitigate the impact of BHP burnout on employees and their patients through providing staff supports, managing workload, and goal setting.
Keywords: burnout, mental health providers, supervisor support, workload
What is known on this topic
Veterans Health Administration (VHA) behavioral health providers (BHPs) face high risk of burnout due to large organizational demands, and a vulnerable, complex patient population.
BHPs have the highest risk of burnout after primary care providers in VHA.
The field has made limited progress to date on mitigating BHP burnout, and clinician turnover can prove expensive and exacerbate burnout among clinicians who remain within VHA.
What this study adds
Using multiple years of data from two national health system surveys, we conducted the largest study to date of characteristics associated with BHP burnout.
In addition to having a reasonable workload, having appropriate resources, opportunities to improve, and managerial support had consistent and significant associations with lower BHP burnout.
This study indicates potentially modifiable targets for policy makers and stakeholders to address persistent characteristics that contribute to burnout among essential providers in the nation's largest integrated health system.
1. INTRODUCTION
Behavioral health providers (BHPs)—“mission critical” psychiatrists, psychologists, and social workers in the Veterans Health Administration (VHA)—report the second highest level of burnout after primary care physicians. 1 VHA oversees the largest mental health system in the United States, and VHA BHPs may face high risks of burnout due to VHA's unique patient population and bureaucratic demands. 2 In VHA, as elsewhere, insufficient BHP staffing relative to patient need can lead to burnout, turnover, lasting job vacancies, and decreased patient access to care. 3 , 4
BHP burnout is associated with negative conditions at the individual and organizational levels, however, many existing studies are small and/or correlational. Limited attention has focused on reducing or preventing burnout among these clinical professionals. 5 This limited evidence suggests a need for multivariable models to better understand factors consistently associated with BHP burnout, including relative strengths of associations between such characteristics relative to one another to inform targeted strategies to prevent and mitigate burnout.
Internal organizational policies, such as changing clinical requirements and productivity targets, and external stressors, such as external audits, can increase burnout. 6 , 7 Increasing the number of qualified providers could decrease burnout. 8 The global pandemic due to the novel coronavirus disease (COVID‐19) likely exacerbated burnout among VHA BHPs as shown in recent studies of BHP experiences outside VHA. 9 , 10 , 11
We sought to identify potentially modifiable work–environment characteristics associated with BHP burnout in VHA, the largest integrated health care system in the United States. 12 With few exceptions, 13 , 14 prior VHA studies on burnout have focused on other provider types, such as primary care physicians or all clinicians and/or conducted facility‐level analyses that could not incorporate individuals' experiences in the workplace. 15 , 16 , 17
This study provided a unique opportunity to take advantage of rich individual‐level data from two large annual national surveys that included BHPs: All Employee Survey (AES) 18 and Mental Health Provider Survey (MHPS). 19 We supplemented analyses with facility‐level Mental Health Onboard Clinical (MHOC) staffing and productivity data, which identify and track provider productivity across settings, including mental health outpatient. 20 , 21 , 22 , 23 Published findings of VHA surveys have tended to use facility‐level data and thus could not address potentially modifiable individual‐level work–environment characteristics associated with burnout. No prior study features this combination of empirical analysis of longitudinal data, multiple data sources, and characteristics potentially associated with BHP burnout in a large health system.
We hypothesized that unfavorable work–environment characteristics would be associated with higher levels of BHP burnout. This study's findings can inform policy and practice on how best for a large health system to identify and attempt to mitigate and address BHP burnout.
2. METHODS
2.1. Study design
The present study comprises one component of a larger mixed‐methods study assessing predictors and consequences of mental health provider burnout in VHA, which aims to understand barriers and facilitators to address this vexing and costly public health issue. 24 Work–environment characteristics from the two surveys comprised the following domains: organizational climate, high performing workplace, managing risk, workgroup perceptions, and supervisory behaviors in AES and timely access to mental health care, quality of mental health care, and collaborative mental health care in MHPS. These domains can be conceptualized as actions and behaviors (what we do), workplace climate (where we are), and employee attitudes (how we feel). 25 Given the strong overlap with burnout, we did not include items focused on overall job satisfaction. 19
For the present analyses, we used individual‐level, de‐identified data from AES and MHPS from 2015 to 2018 and conducted all analyses separately for AES and MHPS. Since participants provided anonymous responses, we could not link data by respondent over time within each survey or between the two surveys. For robust and consistent findings, we split data from AES and MHPS into year pairs (2015–2016, 2016–2017, 2017–2018; six models) and repeated the analyses for each set. We used the earlier year data to train the model (e.g., 2015) and tested the model in the later year (e.g., 2016) in every analysis. We used burnout as the outcome and potentially modifiable work–environment characteristics as predictors, controlling for employee demographic characteristics as covariates.
2.2. Data sources
We obtained data and included respondents who self‐identified as psychiatrists, psychologists, or social workers on the AES and included all respondents in the MHPS during 2015–2018. We obtained facility‐level data on MHOC staffing and productivity data during the same period. The Institutional Review Board in the VA Ann Arbor Healthcare System approved this study.
2.2.1. AES
The National Center for Organizational Development (NCOD) administers the AES to all VHA employees as an annual organizational census of workplace perceptions and satisfaction. Further information on creation of AES, its measures, and how they inform organizational developments in VHA appears elsewhere. 18 From its inception in 2001 through the present, AES data provide organizational feedback and lead to workplace improvement, published as best practices among large organization survey efforts. 26 All AES responses remain anonymous. During the study period, the average AES response rate among all employees reached 60%: 54% of psychiatrists, 66% of psychologists, and 67% of social workers responded.
2.2.2. MHPS
The Office of Mental Health and Suicide Prevention (OMHSP) invites all VHA licensed and non‐licensed independent mental health providers to complete the online MHPS annually to assess mental health provider perceptions about access to and quality of mental health care, and job satisfaction. 27 Analyses found MHPS data reliable, valid, and consistent. 19 The MHPS response rate during the study period exceeded 50%.
2.2.3. MHOC
OMHSP developed a staffing model that estimates the number of full‐time equivalent mental health staff per 1000 veterans treated in outpatient mental health settings, a population‐based measure (staffing ratio). 21 MHOC includes an efficiency‐based measure of provider productivity calculated as the sum of work relative value units divided by time spent providing direct clinical care in outpatient mental health settings (productivity). 20
2.3. Study measures
2.3.1. Dependent variable: provider burnout
For both AES and MHPS surveys, we defined burnout as a dichotomous variable using a validated approach to define burnout for AES, 15 and sought a comparable interpretation for findings across the two surveys.
AES
We classified whether respondents indicated experiencing burnout according to methods used by other VHA researchers. 15 This approach used two burnout questions: emotional exhaustion (“I feel burned out from my work”) and depersonalization (“I worry that this job is hardening me emotionally”). Each of these two burnout questions had a seven‐point response scale (1 = Never; 2 = A few times a year or less; 3 = Once a month or less; 4 = A few times a month; 5 = Once a week; 6 = A few times a week; 7 = Every day). We generated a dichotomous variable such that if the respondent answered either question with 5 or higher (once a week or higher frequency), we classified the response as endorsing burnout; otherwise, we classified the respondent as not endorsing burnout.
To test validity of the burnout variable cutoff, we compared it with another AES variable: turnover plans (“I plan to leave my job within the next six months”). Of various threshold values (e.g., ≥3, ≥4, ≥5, ≥6), we found the threshold value of ≥5 to have the highest sensitivity among thresholds with false positive rate less than 30%. We found this variable highly correlated with burnout in every study year.
MHPS
We generated a dichotomous variable to classify respondent burnout using the sole burnout question of “Overall, based on your definition of burnout, how would you rate your level of burnout?” The response options from 1 to 5 appeared as follows: 1 = I enjoy my work. I have no symptoms of burnout; 2 = Occasionally I am under stress, and I don't always have as much energy as I once did, but I don't feel burned out; 3 = I am definitely burning out and have one or more symptoms of burnout, such as physical and emotional exhaustion; 4 = The symptoms of burnout that I'm experiencing will not go away. I think about frustration at work a lot; 5 = I feel completely burned out and often wonder if I can go on. I am at the point where I may need some changes or may need to seek some sort of help.
We used ≥3 as the threshold endorsing burnout and 1 or 2 as not endorsing burnout after comparing facility‐level MHPS burnout rate to facility‐level AES burnout rate in each year and finding that classifying responses of ≥3 as burnout for MHPS produced the highest correlation with facility‐level burnout rate in AES. Across 2015–2018 surveys, the Pearson correlation coefficient was 0.64 between facility burnout rate based on AES versus facility burnout rate based on MHPS using the threshold of ≥3.
2.3.2. Independent variables: work–environment characteristics as potential predictors of burnout
AES
Many of the AES items changed from year to year. To facilitate comparisons across time, we included 11 work–environment characteristics that appeared in each of the 2015–2018 surveys in our analyses. We used VHA‐provided documentation that grouped together questions with similar but not identical wording to preserve as many items as possible for our analyses. 28 All work–environment items appear in Table 1 and used a scale of 1–5, following either an agreement scale (“strongly disagree” to “strongly agree”) or a feeling scale (“very poor” to “very good”), where higher scores reflect the preferred environment. For example, for the item “disputes or conflicts are resolved fairly,” 1 corresponds to “strongly disagree,” and 5 corresponds to “strongly agree.”
TABLE 1.
Consistent work–environment items in AES (N = 11) and MHPS (N = 17), 2015–2018
| Survey, domain a | Item | Label |
|---|---|---|
| AES | ||
| Organizational climate | My workload is reasonable | Reasonable workload |
| High performing workplace | I am given a real opportunity to improve my skills | Skill building |
| People treat each other with respect in my workgroup | Respectful workgroup | |
| Supervisor sets challenging and yet attainable performance goals for workgroup | Attainable goals | |
| Members able to bring up problems and tough issues | Can bring up tough issues | |
| Disputes and conflicts are resolved fairly | Fair conflict resolution | |
| Managing risk | It is worthwhile in my workgroup to speak up because something will be done to address our concerns | Supervisor addresses concerns |
| Workgroup perceptions | I have the appropriate supplies, materials, and equipment to perform my job well | Have appropriate resources |
| Supervisors/team leaders understand and support employee family/personal life responsibilities in my work group | Supervisor supports personal life | |
| Supervisory behaviors | In my work unit, differences in performance are recognized in a meaningful way | Performance recognized |
| My supervisor does not engage in favoritism | No supervisor favoritism | |
| MHPS | ||
| Timely access to MH care | My workload is reasonable given my job | Reasonable workload |
| Some of my daily work could be done by clerical and/or clinical support staff b | Support staff could do daily work* | |
| Mental health staffing vacancies significantly affect patient care needs at my facility b | Staffing vacancies affect patient care* | |
| My available time for direct patient mental health care is reduced because of assigned collateral duties b | Collateral duties reduce time* | |
| I can schedule my patients as frequently as is clinically indicated | Flexible patient scheduling | |
| I am working at my highest level of licensure or scope | Working at highest level of licensure | |
| Quality of MH care | Through my work, I help veterans improve their lives | Improve veterans' lives |
| Care is well coordinated in veterans receiving mental health care at my facility | MH care well‐coordinated | |
| My facility offers best practices in mental health treatment | Facility offers best practices MH treatment | |
| Mental health care at my facility is Veteran‐centric and recovery‐oriented | Veteran‐centric and recovery‐oriented MH care | |
| Mental health integration with primary care is working well at my site | Primary care and MH integration working well | |
| My facility has mental health programs that are effective in helping veterans | Facility has effective programs for veterans | |
| Collaborative MH care | A spirit of cooperation and teamwork exists in my work group c | Workgroup has spirit of teamwork |
| My team regularly discusses meeting the requirements of the Uniform Mental Health Services Handbook | Discusses Uniform MH Services Handbook requirements | |
| I participate in discussions about performance measures and related opportunities for improvement | I participate in performance discussions | |
| My team regularly meets to plan improvements in patient access | Team plans patient access improvements | |
| I have been involved in actions to improve patient access in my clinics | I'm involved in improving patient access | |
Note: Bold variables indicate consistently significantly associated with burnout in the presented analyses.
Abbreviations: AES, All Employee Survey; MH, mental health; MHPS, Mental Health Provider Survey.
MHPS does not specify domains; Items have slightly different wording across years; our team used VHA guidance to group similar items. 28
Reverse coded.
“Members of my work group communicate well with each other” dropped from original list due to high correlation with spirit of teamwork variable.
MHPS
Like the AES, we included 17 items that appeared in all four study years. MHPS questions appear in Table 1 and used a scale from 1 to 5 reflecting agreement, satisfaction, or frequency, with higher scores reflecting better, preferable conditions.
MHOC
We used two facility‐level variables (staffing ratio and productivity) in sensitivity analyses as possible predictors of the relationship between self‐reported work–environment characteristics and burnout. Further details outlining the purpose—origins and definitions—of these two metrics appear elsewhere. 20 , 21 , 22
2.3.3. Demographic characteristics as covariates
Demographic characteristics in AES (Table 2) included sex (male, female), ethnicity (Spanish, Hispanic, or Latino: yes, no), race (Black or African American, American Indian or Alaskan Native, Asian, Native Hawaiian or other Pacific Islander: mark one or more), VHA tenure (<6 months, between 6 months and 1 year, between 1 and 2 years, between 2 and 5 years, between 5 and 10 years, between 10 and 20 years, more than 20 years), level of supervisory responsibility (none, team leader, first line supervisor, manager, executive), VHA training before becoming a VHA employee (yes, no), ever served as active duty (yes, no), disabled (yes, no), assigned to Patient Aligned Care Team (PACT; the VHA's implementation of the Patient Centered Medical Home model for primary care; yes, no, not sure), 29 a supervisor of health professionals (yes, no), and faculty appointment (none, professor, associate professor, assistant professor, lecturer, other).
TABLE 2.
Burnout rate and characteristics of mental health providers in VHA AES, MHPS, MHOC, 2015–2018
| 2015 | 2016 | 2017 | 2018 | |||||
|---|---|---|---|---|---|---|---|---|
| Characteristic | N | % | N | % | N | % | N | % |
| AES | 7907 | 100 | 8341 | 100 | 8889 | 100 | 10,364 | 100 |
| Burnout | ||||||||
| Yes | 2704 | 34.2 | 2943 | 35.28 | 3282 | 36.92 | 3208 | 30.95 |
| No | 5203 | 65.8 | 5398 | 64.72 | 5607 | 63.08 | 7156 | 69.04 |
| Supervisory role | ||||||||
| None | 5653 | 71.50 | 5758 | 69.03 | 6094 | 68.56 | 7152 | 69.01 |
| Team leader | 1332 | 16.85 | 1301 | 15.6 | 1452 | 16.33 | 1536 | 14.82 |
| First line supervisor | 632 | 7.99 | 797 | 9.56 | 832 | 9.36 | 994 | 9.59 |
| Manager | 265 | 3.35 | 447 | 5.36 | 454 | 5.11 | 613 | 5.91 |
| Executive | 25 | 0.32 | 38 | 0.46 | 57 | 0.64 | 69 | 0.67 |
| PACT team | ||||||||
| Yes | 863 | 10.91 | 898 | 10.77 | 994 | 11.18 | 1141 | 11.01 |
| No | 7044 | 89.09 | 7443 | 89.23 | 7895 | 88.82 | 9223 | 88.99 |
| Teach or supervise health professions trainees | ||||||||
| Yes | 3514 | 44.44 | 3682 | 44.14 | 3965 | 44.61 | 4618 | 44.56 |
| No | 4393 | 55.56 | 4659 | 55.86 | 4924 | 55.39 | 5746 | 55.44 |
| Faculty appointment | ||||||||
| None | 6469 | 81.81 | 6876 | 82.44 | 7343 | 82.61 | 8530 | 82.30 |
| Professor | 119 | 1.51 | 107 | 1.28 | 142 | 1.6 | 166 | 1.60 |
| Associate Professor | 238 | 3.01 | 286 | 3.43 | 291 | 3.27 | 362 | 3.49 |
| Assistant Professor | 605 | 7.65 | 596 | 7.15 | 627 | 7.05 | 787 | 7.59 |
| Lecturer or instructor | 73 | 0.92 | 282 | 3.38 | 306 | 3.44 | 323 | 3.12 |
| Other | 403 | 5.1 | 194 | 2.33 | 180 | 2.03 | 196 | 1.89 |
| MHPS | 4510 | 100 | 5258 | 100 | 5664 | 100 | 6464 | 100 |
| Burnout | ||||||||
| Yes | 1534 | 34.01 | 1995 | 37.94 | 2104 | 37.15 | 2456 | 38 |
| No | 2976 | 66 | 3263 | 62.1 | 3560 | 62.9 | 4008 | 62.01 |
| Licensed independent provider | ||||||||
| Yes | 3685 | 81.71 | 4421 | 84.08 | 4712 | 83.19 | 5295 | 81.92 |
| No | 825 | 18.29 | 837 | 15.92 | 952 | 16.81 | 1169 | 18.08 |
| Type of mental health services provided | ||||||||
| Inpatient | 176 | 3.9 | 237 | 4.51 | 239 | 4.22 | 242 | 3.74 |
| Outpatient | 3197 | 70.87 | 3774 | 71.78 | 4076 | 71.96 | 4806 | 74.35 |
| Both inpatient and outpatient | 1137 | 25.21 | 1247 | 23.72 | 1349 | 23.82 | 1416 | 21.91 |
| Discipline | ||||||||
| Psychiatrist | 795 | 17.63 | 876 | 16.66 | 901 | 15.91 | 936 | 14.48 |
| Psychologist | 1379 | 30.58 | 1590 | 30.24 | 1839 | 32.47 | 1967 | 30.43 |
| Social worker | 1339 | 29.69 | 1619 | 30.79 | 1700 | 30.01 | 1999 | 30.93 |
| Nursing | 492 | 10.91 | 569 | 10.82 | 593 | 10.45 | 736 | 11.39 |
| Clinical pharmacist a | — | — | 47 | 0.89 | 53 | 1.45 | 65 | 1.01 |
| Addiction therapist a | — | — | 76 | 0.94 | 85 | 1.5 | 92 | 1.42 |
| Peer specialist | 113 | 2.51 | 117 | 2.23 | 130 | 2.3 | 160 | 2.48 |
| Licensed professional mental health counselor | 89 | 1.97 | 102 | 1.94 | 86 | 1.52 | 145 | 2.24 |
| Licensed marriage and family therapist | 13 | 0.29 | 15 | 0.29 | 13 | 0.23 | 28 | 0.43 |
| Other | 290 | 6.43 | 247 | 4.70 | 264 | 4.66 | 336 | 5.20 |
| BHIP member | ||||||||
| Yes | 1807 | 40.07 | 2087 | 39.69 | 2255 | 39.81 | 2819 | 43.61 |
| No | 2703 | 59.93 | 3171 | 60.31 | 3409 | 60.19 | 3645 | 56.39 |
| MHOC (facility‐level, N = 140 in each year) | Mean | SD | Mean | SD | Mean | SD | Mean | SD |
| Staffing ratio b | 7.46 | 1.73 | 7.36 | 1.61 | 7.46 | 1.73 | 7.36 | 1.61 |
| Productivity | 398.78 | 70.80 | 451.88 | 74.68 | 398.78 | 70.80 | 451.88 | 74.68 |
Abbreviations: AES, All Employee Survey; BHIP, Behavioral Health Interdisciplinary Program; MHOC, Mental Health Onboard Clinical; MHPS, Mental Health Provider Survey; PACT, Patient Aligned Care Team; VHA, Veterans Health Administration.
Answer choices absent in 2015 MHPS survey.
<6.00 = critical; 6.01–7.72 = moderate; >7.72 = good.
Demographic characteristics in MHPS (Table 2) included VHA tenure (<6 months, between 6 months and 1 year, between 1 and 2 years, between 2 and 5 years, between 5 and 10 years, between 10 and 20 years, more than 20 years), VHA training before becoming a VHA employee (yes, no), licensed independent provider (LIP: yes, no), type of mental health services provided (outpatient, inpatient, both), discipline (psychiatrist, psychologist, social worker, nursing, clinical pharmacist, addiction therapist, peer specialist, licensed professional mental health counselor, licensed marriage and family therapist, other), member of Behavioral Health Interdisciplinary Program (BHIP: an inter‐professional team‐based approach to mental health care coordination; yes, no). 30
2.4. Statistical analysis
We calculated the overall burnout rates and summarized the demographic characteristics (e.g., sex, race, VHA) for VHA BHPs over the study period separately for AES and for MHPS. To avoid multicollinearity across predictors, for each yearly survey, we first assessed pair‐wise correlations between 11 AES items and between 18 MHPS items and found 2 items in MHPS with a correlation higher than 0.90: “members of my work group communicate well with each other” and “a spirit of cooperation and teamwork exists in my work group.” The latter item appeared more predictive of burnout: we retained it and dropped the former for multivariable analyses and included 17 MHPS items in our models. Otherwise, we included all work–environment characteristics as continuous variables in each adjusted model.
Next, we used mixed‐effects logistic regression models to predict VHA employee burnout. We first split the AES and MHPS data into three pairs of years: 2015–2016, 2016–2017, and 2017–2018. We conducted analyses within each pair of years to assess if predictive factors remained consistent across years.
Within each pair, we used the earlier year's data to train the logistic regression model with burnout as the outcome and potentially modifiable work–environment items as the predictors. We included individual employee demographic characteristics as covariates and included VHA facilities (N = 140) as random intercepts to account for correlation of data of employees within same facilities. We used the later year's data in each pair of years as a test set to obtain the final summary measures of the association between work–environment characteristics and burnout and to evaluate the performance of the model from the training set. We used average marginal effects (AME) 31 , 32 as the summary measure of association. To assess model fit, we computed each model's area under the curve (AUROC) and Brier score 33 , 34 for predicting burnout in the test set. Prediction models with an AUROC value of 1 have perfect prediction, and thus values closer to 1.0 have higher predictability of burnout, and Brier scores of 0 have perfect prediction, and thus values closer to 0 have higher predictability of burnout.
2.5. Sensitivity analyses
We conducted three sensitivity analyses. We combined all the responses for 2015–2018 for each respective survey and repeated the analyses using the AES data pooled across years (N = 35,501) and MHPS data pooled across years (N = 21,896). We trained a model on 80% of the pooled data (N = 28,401 [AES], N = 17,517 [MHPS]), then evaluated the model on the remaining 20% (N = 7100 [AES], N = 4379 [MHPS]). We also repeated this train‐test process 100 times and obtained AUROC values and Brier scores on the test sets. We assessed if actual workload (using the staffing ratio and productivity) was associated with burnout, and further assessed if the association between self‐reported work–environment variables and burnout remained even after accounting for actual measures of workload by adding separately the staffing ratio variable and productivity variable to each of the six original models.
3. RESULTS
Our study sample of AES and MHPS respondents without missing data included 57,397 respondents. Study cohorts for each survey and year appear in Figure 1.
FIGURE 1.
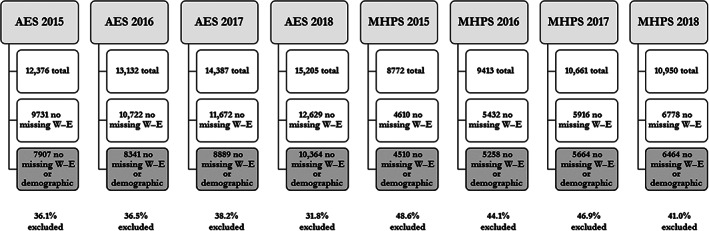
Study cohorts. AES, All Employee Survey; demographic, demographic characteristics; MHPS, Mental Health Provider Survey; W–E, work–environment characteristics
Table 2 summarizes the VHA BHP characteristics across the 4 years from the two surveys. In AES, 34.2%, 35.3%, 36.9%, and 31.0% of respondents and in MHPS, 34.0%, 37.9%, 37.1%, and 38.0% of respondents endorsed burnout in 2015, 2016, 2017, and 2018, respectively. Of note, 30% had a supervisory role, 11% participated in a PACT team, 44% taught or supervised health professions trainees, and less than 20% had a faculty appointment. Corresponding demographic characteristics appear in Table S1, including that in AES, approximately two‐thirds of respondents were women, 8% of Hispanic ethnicity, and over 80% were White, over 10% were Black, with less than 10% other races. Approximately half of the respondents had worked at the VA for less than 5 years, with the other half between 5 and more than 20 years, roughly half had prior VHA training, 13% had prior active duty, and 11% were disabled.
MHPS respondents had similar tenure characteristics and prior VHA training. Over 80% were a licensed independent provider, with less than 5% exclusively focused on inpatient services, over 70% focused exclusively on outpatient services, and less than 25% providing both inpatient and outpatient services. Psychiatrists comprised approximately 15% of respondents, psychologists 30%, social workers 30%, with the remainder a variety of associated disciplines. Roughly 40% participated as BHIP members.
Figures 2 and 3 include results of the adjusted mixed‐effects logistic regression models developed using AES and MHPS survey data from pairs of consecutive years. Across years, models showed good predictability for burnout with similar AUROC values ranging from 0.77 to 0.83 and Brier scores ranging from 0.16 to 0.18 across years.
FIGURE 2.
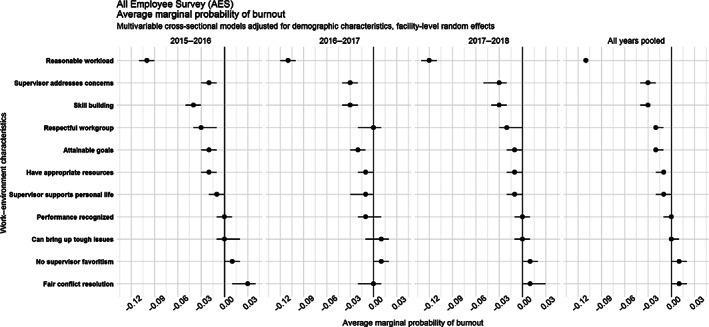
Adjusted logistic regression model results showing work–environment predictors of burnout in AES, 2015–2018: forest plots with 95% CI. Each model adjusted for demographic characteristics (Table 2, gender, Hispanic, race, VHA tenure, supervisory role, prior VHA training, prior active duty, disabled, PACT team, teach/supervise health professions trainees, and faculty appointment) as fixed effects, and facility as random intercepts. Interpretation: An AME associated with reasonable workload of −0.11 corresponds to an 11 percentage point reduction associated with a one unit increase in the reasonable workload item. AES, All Employee Survey; MH, mental health. X‐axis: average marginal effect; Y‐axis: work–environment characteristics
FIGURE 3.
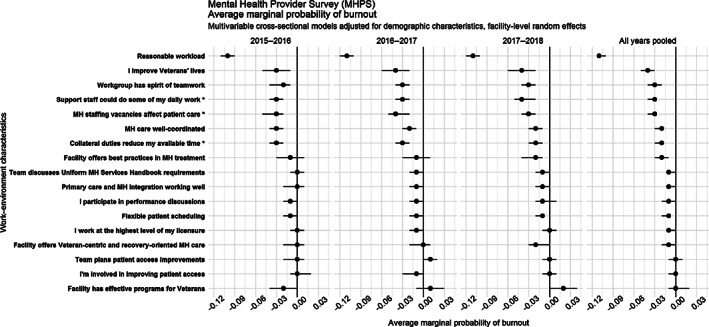
Adjusted logistic regression model results showing work–environment predictors of burnout in MHPS, 2015–2018: forest plots with 95% CI. Each model adjusted for demographic characteristics (Table 2, VHA tenure, prior VHA training, licensed independent provider, type of mental health services provided, discipline, and BHIP member as fixed effects) as fixed effects, and facilities as random intercepts. Interpretation: An AME associated with reasonable workload of −0.11 corresponds to an 11 percentage point reduction associated with a one unit increase in the reasonable workload item. MH, mental health; MHPS, Mental Health Provider Survey; VHA, Veterans Health Administration. X‐axis: adjusted burnout average marginal effect; Y‐axis: work–environment characteristics
In AES models (Figure 2), we found four work–environment characteristics consistently associated with significantly lower burnout in each of the three pairs of years from 2015 to 2018: (1) “My workload is reasonable [Reasonable workload],” (2) “I have the appropriate supplies, materials, and equipment to perform my job well [I have resources for the job],” (3) “It is worthwhile in my workgroup to speak up because something will be done to address our concerns [Supervisor address concerns],” and (4) “I am given a real opportunity to improve my skills [Skill building].”
Compared with the three other work characteristics noted, having a reasonable workload had by far the largest negative association with burnout in BHPs across all years. AMEs associated with reasonable workload ranged from −0.12 to −0.11, corresponding to an 11–12 percentage point reduction associated with a one unit increase in the reasonable workload item.
In MHPS models (Figure 3), we found three work–environment characteristics associated with decreased risks of burnout in 2015–2018: (1) “My workload is reasonable given my job [reasonable workload],” (2) “Through my work, I help Veterans improve their lives [improve Veterans' lives],” (3) “Care is well coordinated in Veterans receiving mental health care at my facility [MH care well‐coordinated].” We found three additional work–environment characteristics associated with decreased risks of burnout that appear as reverse‐coded items in the data, which included: (1) “Mental health staffing vacancies significantly affect patient care needs at my facility [staffing vacancies affect patient care]”; (2) “Some of my daily work could be done by clerical and/or clinical support staff [support staff could do daily work]”; and (3) “My available time for direct patient mental health care is reduced because of assigned collateral duties [collateral duties reduce time].” Stated another way, the more respondents felt that staffing vacancies did not affect patient care, the less likely they were to report burnout.
As in AES, compared with the five other work characteristics, having a reasonable workload had by far the strongest negative association with burnout across all years (AME: −0.11, 95% CIs: −0.11, −0.11).
Work–environment characteristics that did not appear significantly associated with burnout in AES included performance recognition and ability to bring up difficult issues, and in MHPS included working at the highest level of licensure and planning improvements in patient access.
Noteworthy demographic characteristics (Table S2) consistently indicated in AES: higher burnout among those with 1–20 years of tenure compared with those with more than 20 years; in MHPS, consistently higher burnout appeared among those with less than 1 year of tenure compared with those with over 20 years.
In sensitivity analyses using pooled data, we found similar work–environment characteristics as seen in the analyses across consecutive pairs of years to be associated with decreased or increased probability of burnout and found similar AUROC values and Brier scores on test sets. In the separate analyses that added the staffing ratio and productivity variables, neither of those two variables were significant predictors of burnout, nor did they notably change the magnitude or direction of other self‐reported work–environment predictors.
4. DISCUSSION
In a large study of burnout among BHPs over time within an integrated health system, and one of the largest mental health systems nationally, we found several key components associated with burnout. Having a reasonable workload represented the strongest and most consistent predictor of burnout in both surveys and across time. In addition, appropriate resources, supportive supervisors, opportunities for skill development, and staff support all significantly decreased likelihood of burnout. Individuals who also felt a sense of mission, such as improving the lives of veterans, and who believed that VA mental health care was well‐coordinated also had a lower likelihood of burnout than BHPs who did not endorse these items.
Our findings are consistent with the few previous studies that examined related topics. Yanchus et al. used civility, procedural justice, autonomy, and psychological safety as predictors of job satisfaction and turnover in four different VHA mental health occupations (psychiatrists, psychologists, social workers, mental health nurses). 14 They found all of these predictors significantly related to turnover intention, either directly or indirectly through job satisfaction. Interestingly, a direct path between psychological safety and turnover intention resulted in a better model fit in all the mental health occupations that Yanchus et al. examined, compared with an indirect path via job satisfaction. Given these and our findings, as well as a substantial overlap between burnout and job satisfaction and the key role of both in predicting turnover intentions, future research should examine a potential role of burnout as a mediator of predictive relationship between various organizational climate variables and turnover.
Pragmatically, our findings provide important potential targets for VHA to address employee engagement and well‐being. Some may require adjustments that involve capital outlays, such as hiring, which could have important budget ramifications. Other targets may require modifying relationships between providers and their supervisors and/or support staff as well as increasing self‐awareness, particularly among workplace leaders, of how their own well‐being and burnout levels may impact their workplace relationships. The latter suggestion (focus on self‐awareness) is consistent with previous findings. 35 , 36
As Hernandez et al. documented using AES data from 2008 to 2012, supervisors' burnout was associated with negative workplace climate outcomes in supervised groups; however, supervisors' self‐awareness served as an important mediator in these relationships. 35 Specifically, when supervisors had awareness of their own burnout, it reduced the negative impact of supervisory behaviors and attributes on work‐related outcomes, such as climate of civility and psychological safety (i.e., high performing workplace) in their supervised workgroups.
Few rigorous studies have tested organizational strategies for reducing burnout. However, several randomized controlled trials and cohort studies have demonstrated the effectiveness of targeting some of the variables we identified. These strategies include modifying provider workload, enhancing communication strategies, and task‐shifting to reduce the administrative burden on providers. Workload: Adjusting physician work schedules can reduce physician burnout. In a randomized controlled trial of 2‐ versus 4‐week physician inpatient rotations, the 2‐week rotation was associated with lower burnout. 37 Shortening resident physician shifts reduced burnout in another randomized controlled trial. 38 In addition, a number of studies have demonstrated that work‐hour limitations for resident physicians reduce burnout. 39 , 40 , 41 Communication: In three randomized controlled trials, facilitated discussion groups addressing topics relevant to physicians improved physician empowerment and engagement and reduced burnout. 42 , 43 , 44 Task‐shifting: Burnout became reduced in a study of locally initiated projects targeting workflow redesign, communication, and quality improvement projects based on clinician concerns. 45
Examples of additional potential approaches could include training supervisors on how best to respond to employees; systemwide, facility, and/or supervisor efforts to determine what type of clerical, administrative, or collateral duties most interfere with patient care and identifying how best to mitigate these barriers; and learning more about professional development opportunities sought by BHPs and facilitating access to such activities.
4.1. Limitations
This study has some limitations. We excluded responses for individuals with missingness for any variables included in the analysis, which represented 31.8%–48.6% of eligible respondents each year. Missing data on burnout questions ranged between 2.2% and 3.3% in each year of AES and 3.8% and 4.8% in each year of MHPS. Most work–environment items had missing data in less than 5% of patients, with one item in MHPS having the highest missingness of 13.3%. We found similar burnout rates each year between those included in or excluded from the analysis.
Questions differed substantially over time in the AES, and although we could account for some minor changes in wording, we eliminated many additional potential variables that could have informed our analyses because they did not appear in all study years. As with all survey data, higher response rates could have influenced findings. Findings may not generalize to other clinical specialties or health systems.
We did not have access to provider compensation data; therefore, we could not assess the extent to which compensation and retention packages might mitigate provider experiences of burnout. We could not link patient data on severity, episodes, admissions, suicides, or any other individual‐level data on patient complexity to de‐identified provider responses, which might have partially elucidated the difficulty of workload and demands associated with employment. Although VA has extensive data systems for tracking, we did not have access to information such as numbers of patients seen per day. Using de‐identified provider data means we could not determine whether and when providers left their positions within VHA and whether providers experiencing burnout make worse medical and treatment decisions.
4.2. Implications for practice, policy, and research
Although multiple work–environment characteristics influenced BHP burnout, a reasonable workload stood out in both surveys as the consistent single largest predictor of burnout. This finding may appear intuitive yet may also represent a thorny issue to address in practice. What defines a reasonable workload and how does either a health system, work team, or individual achieve this objective? To what extent can health systems allocate or reallocate staff resources such that clinical providers can work to the top of their licensure and decrease administrative burdens? Would improving supervisor support and employee training opportunities help mitigate potentially challenging workload and staff availability challenges? These questions may also serve as guideposts for others seeking to address and prevent burnout among BHPs.
At this time, our comment on these questions reflects a purely conceptual standpoint; we believe the job demands–resources model 46 offers a useful framework to examine relationships between workload and other work process aspects on one hand, and burnout on the other hand. Job demands represent a sum of psychological, physical, or emotional efforts required by the job. Job resources include aspects instrumental to accomplishing the job successfully, buffer the workers from job demands, or support personal and professional growth on the job. 46 This distinction between demands and resources remains critical: work's impact on the employee conceptually creates a difference between demands and resources, not the work itself. It follows that, for a demanding job motivate employees, a high level of resources must accompany it. 46
Motivating jobs (i.e., high demands and high resources) may be less likely to create burnout and more likely to create positive work outcomes, such as organizational commitment. 47 Jobs that cause strain, however, have both high demands and also lack necessary resources to buffer those demands. 46
Demanding work leads to employee burnout. 48 Workload may represent a job demand, which proves detrimental when not balanced by appropriate job resources. Importantly, job resources include not only objective and monetizable aspects, such as more equipment and staff, but also the intangible workplace climate aspects, such as coworker support, positive organizational climate, and teamwork. The latter has an important role in balancing high workload demands and reducing workplace burnout. We acknowledge that our models in this study could not account for all possible variables that could appear in a job demands–resources model.
This study will guide our future work. We will assess moderators of burnout and the potentially bidirectional relationship between burnout and turnover. Finally, we will compare VHA BHPs with other VHA providers to assess similarities and differences in relative strengths of associations between work–environment characteristics and burnout.
5. CONCLUSIONS
This large study of two national surveys in the VHA health system pointed to work–environment characteristics consistently associated with BHP burnout. Health systems and other stakeholders may wish to consider the relative opportunities and challenges associated with addressing factors associated with burnout to weigh the costs and benefits of organizational and structural approaches to ensuring employee engagement, well‐being, and preventing costly turnover.
Supporting information
Table S1. Demographic characteristics of mental health providers in VHA AES, MHPS, MHOC, 2015‐2018.
Table S2. Demographic and work‐environment predictors of burnout in AES and MHPS adjusted models using average marginal effects (AME; year pairs and pooled years, 2015‐2018).
ACKNOWLEDGMENTS
The VA Health Services Research and Development Service provided funding for this study (VA IIR 17‐262; VA RCS 21‐138).
Zivin K, Chang M‐UM, Van T, et al. Relationships between work–environment characteristics and behavioral health provider burnout in the Veterans Health Administration. Health Serv Res. 2022;57(Suppl. 1):83‐94. doi: 10.1111/1475-6773.13964
Funding information Health Services Research and Development, Grant/Award Numbers: VA IIR 17‐262, VA RCS 21‐138
REFERENCES
- 1. National Center for Organization Development. What we know about burnout in VHA: quick facts. US Department of Veterans Affairs. 2017.
- 2. Garcia HA, McGeary CA, Finley EP, Ketchum NS, McGeary DD, Peterson AL. Burnout among psychiatrists in the veterans health administration. Burn Res. 2015;2(4):108‐114. [Google Scholar]
- 3. VHA Office of Mental Health Operations . How does the facility's mental health staffing relate to other characteristics of the mental health treatment program? 2016.
- 4. Paris M, Hoge MA. Burnout in the mental health workforce: a review. J Behav Health Serv Res. 2010;37(4):519‐528. [DOI] [PubMed] [Google Scholar]
- 5. Morse G, Salyers MP, Rollins AL, Monroe‐DeVita M, Pfahler C. Burnout in mental health services: a review of the problem and its remediation. Admin Pol Ment Health. 2012;39(5):341‐352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mirvis DM, Graney MJ, Kilpatrick AO. Trends in burnout and related measures of organizational stress among leaders of Department of Veterans Affairs medical centers. J Healthc Manag. 1999;44(5):353‐365. [PubMed] [Google Scholar]
- 7. VA Office of Inspector General . Audit of VHA's efforts to improve Veterans' access to outpatient psychiatrists. Washington, DC: VA Office of Inspector General. 2015.
- 8. Department of Veterans Affairs . Productivity and staffing in outpatient clinical encounters for mental health providers. Department of Veterans Affairs, Veterans Health Administration. 2013.
- 9. Sklar M, Ehrhart MG, Aarons GA. COVID‐related work changes, burnout, and turnover intentions in mental health providers: a moderated mediation analysis. Psychiatr Rehabil J. 2021;44(3):219‐228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Joshi G, Sharma G. Burnout: a risk factor amongst mental health professionals during COVID‐19. Asian J Psychiatr. 2020;54:102300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Alkhamees AA, Assiri H, Alharbi HY, Nasser A, Alkhamees MA. Burnout and depression among psychiatry residents during COVID‐19 pandemic. Hum Resour Health. 2021;19(1):46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kizer KW, Dudley RA. Extreme makeover: transformation of the veterans health care system. Annu Rev Public Health. 2009;30:313‐339. [DOI] [PubMed] [Google Scholar]
- 13. Yanchus NJ, Beckstrand J, Osatuke K. Examining burnout profiles in the Veterans Administration: All Employee Survey narrative comments. Burn Res. 2015;2(4):97‐107. [Google Scholar]
- 14. Yanchus NJ, Periard D, Moore SC, Carle AC, Osatuke K. Predictors of job satisfaction and turnover intention in VHA mental health employees: a comparison between psychiatrists, psychologists, social workers, and mental health nurses. Hum Serv Organ Manag Leadersh Gov. 2015;39(3):219‐244. [Google Scholar]
- 15. Rinne ST, Mohr DC, Swamy L, Blok AC, Wong ES, Charns MP. National burnout trends among physicians working in the Department of Veterans Affairs. J Gen Intern Med. 2020;35(5):1382‐1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Schult TM, Mohr DC, Osatuke K. Examining burnout profiles in relation to health and well‐being in the veterans health administration employee population. Stress Health. 2018;34(4):490‐499. [DOI] [PubMed] [Google Scholar]
- 17. Edwards ST, Helfrich CD, Grembowski D, et al. Task delegation and burnout trade‐offs among primary care providers and nurses in veterans affairs patient aligned care teams (VA PACTs). J Am Board Fam Med. 2018;31(1):83‐93. [DOI] [PubMed] [Google Scholar]
- 18. Osatuke K, Draime J, Moore SC, et al. Organization development in the Department of Veterans Affairs. The Praeger Handbook of Veteran's Health: History, Challenges, Issues, and Developments Volume IV: Future Directions in Veterans Healthcare. 2012. pp. 21–76.
- 19. Lemke S, Boden MT, Kearney LK, et al. Measurement‐based management of mental health quality and access in VHA: SAIL mental health domain. Psychol Serv. 2017;14(1):1‐12. [DOI] [PubMed] [Google Scholar]
- 20. Boden M, Smith CA, Trafton JA. Investigation of population‐based mental health staffing and efficiency‐based mental health productivity using an information‐theoretic approach. PLoS One. 2021;16(8):e0256268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Boden MT, Smith CA, Klocek JW, Trafton JA. Mental health treatment quality, access, and satisfaction: optimizing staffing in an era of fiscal accountability. Psychiatr Serv. 2019;70(3):168‐175. [DOI] [PubMed] [Google Scholar]
- 22. Kearney LK, Smith C, Kivlahan DR, et al. Mental health productivity monitoring in the veterans health administration: challenges and lessons learned. Psychol Serv. 2018;15(4):486‐495. [DOI] [PubMed] [Google Scholar]
- 23. Veterans Health Administration . VHA Directive 1161, Productivity and staffing in clinical encounters for mental health providers. Washington, DC. 2020.
- 24. Zivin K, Kononowech J, Boden M, et al. Predictors and consequences of veterans affairs mental health provider burnout: protocol for a mixed methods study. JMIR Res Protoc. 2020;9(12):e18345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. National Center for Organization Development. 2018 Department of Veterans Affairs All Employee Survey Federal Employee Viewpoint Survey Technical Report. 2018.
- 26. Department of Veterans Affairs. 2017 VA All Employee Survey. 2017.
- 27. Schmidt EM, Krahn DD, McGuire MH, et al. Using organizational and clinical performance data to increase the value of mental health care. Psychol Serv. 2017;14(1):13‐22. [DOI] [PubMed] [Google Scholar]
- 28. Department of Veterans Affairs. Crosswalk of VA All Employee Survey (AES) items by year. National Center for Organizational Development. 2018.
- 29. Ladebue AC, Helfrich CD, Gerdes ZT, Fihn SD, Nelson KM, Sayre GG. The experience of patient aligned care team (PACT) members. Health Care Manag Rev. 2016;41(1):2‐10. [DOI] [PubMed] [Google Scholar]
- 30. Barry CN, Abraham KM, Weaver KR, Bowersox NW. Innovating team‐based outpatient mental health care in the veterans health administration: staff‐perceived benefits and challenges to pilot implementation of the behavioral health interdisciplinary program (BHIP). Psychol Serv. 2016;13(2):148‐155. [DOI] [PubMed] [Google Scholar]
- 31. Norton EC, Dowd BE. Log odds and the interpretation of logit models. Health Serv Res. 2018;53(2):859‐878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Norton EC, Dowd BE, Maciejewski ML. Odds ratios‐current best practice and use. JAMA. 2018;320(1):84‐85. [DOI] [PubMed] [Google Scholar]
- 33. Brier GW. Verification of forecasts expressed in terms of probability. Mon Weather Rev. 1950;78(1):1‐3. [Google Scholar]
- 34. Rufibach K. Use of Brier score to assess binary predictions. J Clin Epidemiol. 2010;63(8):938‐939. [DOI] [PubMed] [Google Scholar]
- 35. Hernandez W, Luthanen A, Ramsel D, Osatuke K. The mediating relationship of self‐awareness on supervisor burnout and workgroup civility & psychological safety: a multilevel path analysis. Burn Res. 2015;2(1):36‐49. [Google Scholar]
- 36. Hernandez W, Yanchus NJP, Osatuke KP. Evolving the JD‐R model: the moderating effects of job resources and burnout taxonomies. Organ Dev J. 2018;36(1):31‐53. [Google Scholar]
- 37. Lucas BP, Trick WE, Evans AT, et al. Effects of 2‐ vs 4‐week attending physician inpatient rotations on unplanned patient revisits, evaluations by trainees, and attending physician burnout: a randomized trial. JAMA. 2012;308(21):2199‐2207. [DOI] [PubMed] [Google Scholar]
- 38. Parshuram CS, Amaral ACKB, Ferguson ND, et al. Patient safety, resident well‐being and continuity of care with different resident duty schedules in the intensive care unit: a randomized trial. Can Med Assoc J. 2015;187(5):321‐329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Goitein L, Shanafelt TD, Wipf JE, Slatore CG, Back AL. The effects of work‐hour limitations on resident well‐being, patient care, and education in an internal medicine residency program. Arch Intern Med. 2005;165(22):2601‐2606. [DOI] [PubMed] [Google Scholar]
- 40. Martini S, Arfken CL, Balon R. Comparison of burnout among medical residents before and after the implementation of work hours limits. Acad Psychiatry. 2006;30(4):352‐355. [DOI] [PubMed] [Google Scholar]
- 41. Landrigan CP, Fahrenkopf AM, Lewin D, et al. Effects of the accreditation council for graduate medical education duty hour limits on sleep, work hours, and safety. Pediatrics. 2008;122(2):250‐258. [DOI] [PubMed] [Google Scholar]
- 42. West CP, Dyrbye LN, Rabatin JT, et al. Intervention to promote physician well‐being, job satisfaction, and professionalism a randomized clinical trial. JAMA Intern Med. 2014;174(4):527‐533. [DOI] [PubMed] [Google Scholar]
- 43. Ripp JA, Fallar R, Korenstein D. A randomized controlled trial to decrease job burnout in first‐year internal medicine residents using a facilitated discussion group intervention. J Grad Med Educ. 2016;8(2):256‐259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. West CP, Hauer KE. Reducing burnout in primary care: a step toward solutions. J Gen Intern Med. 2015;30(8):1056‐1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Linzer M, Poplau S, Grossman E, et al. A cluster randomized trial of interventions to improve work conditions and clinician burnout in primary care: results from the healthy work place (HWP) study. J Gen Intern Med. 2015;30(8):1105‐1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Bakker AB, Demerouti E. The job demands‐resources model: state of the art. J Manag Psychol. 2007;22(3):309‐328. [Google Scholar]
- 47. Bakker AB, Van Veldhoven M, Xanthopoulou D. Beyond the demand‐control model. J Pers Psychol. 2010;9(1):3‐16. [Google Scholar]
- 48. Schaufeli WB, Bakker AB, Van Rhenen W. How changes in job demands and resources predict burnout, work engagement, and sickness absenteeism. J Organ Behav. 2009;30(7):893‐917. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Demographic characteristics of mental health providers in VHA AES, MHPS, MHOC, 2015‐2018.
Table S2. Demographic and work‐environment predictors of burnout in AES and MHPS adjusted models using average marginal effects (AME; year pairs and pooled years, 2015‐2018).


